
Figure 27-1 Second- and third-degree frostbite. Note the large bullae, some of which contain hemorrhagic fluid.
▪ Frostbite is a severe, freezing-temperature, cold-induced injury.
▪ Tissue injury occurs by two mechanisms: cellular injury due to ice crystal formation, and progressive tissue ischemia.
▪ Frostbite primarily affects three groups: (1) the military, (2) the homeless, alcoholic or drug-addicted, and those with psychiatric illness, and (3) cold-weather sports enthusiasts.
▪ The traditional grading of frostbite injury by “degrees” of severity does not correlate well with outcomes.
▪ The risk of bony amputation correlates with the proximal extent of injury.
▪ Rapid rewarming is the cornerstone of management in the emergency department, but thawing and refreezing in the field should be avoided at all costs.
▪ Treatments aimed at blocking the arachidonic acid cascade likely reduces tissue injury.
▪ Rehabilitation goals include edema control, wound care, and preservation of motion.
Cold-induced injuries can be divided into major and minor categories. Major cold injuries include frostbite and immersion foot (also known as trench foot). Minor cold injuries include pernio (or chilblains) and frostnip. Cold-induced injuries can also be categorized by the temperature at which they occur. Frostbite and frostnip both occur at freezing ambient temperatures, whereas pernio (chilblains) and immersion foot occur at above-freezing temperatures.
Frostbite is defined as the freezing of tissues with accompanying ice crystal formation leading to tissue injury and death. It is a severe injury that can result in tissue loss and permanent disability. Frostnip, on the other hand, is not as clearly defined in the literature. Clinical signs of frostnip include numbness, pallor, and paresthesias that resolve immediately on warming. Although this has not been clearly demonstrated, ice crystals may temporarily form in frostnip.1 Unlike frostbite, frostnip does not result in permanent tissue injury. Pernio (chilblains) is a mild cold-induced injury that occurs with prolonged and repetitive exposure to above-freezing cold temperatures. Clinical findings include a patch of erythematous, edematous, and pruritic skin. Pathologic studies reveal vascular and perieccrine inflammation.2 The condition is usually self-limiting and resolves in a matter of weeks.3 If pernio occurs in the same anatomic location season after season, a chronic form (which may include skin ulceration) can develop. Immersion foot (trench foot) is the result of prolonged exposure to above-freezing cold temperatures and moisture. Initially the foot is blanched or mottled, and the patient experiences an anesthetic effect described as “walking on air.”4 Clinical findings include poor pulses and sluggish capillary refill due to vasoconstriction. After rewarming, the extremity becomes hyperemic with bounding pulses. However, capillary refill remains poor and petechiae are seen, indicating damaged microcirculation. Blisters and desquamation follow. After healing, it can take months or years for cold sensitivity, hyperhydrosis, paresthesias, and pain to resolve.
Frostnip and pernio are mild self-limiting injuries that rarely require the services of a surgeon or hand therapist. Immersion foot occurs almost exclusively in the lower extremity and is not the focus of this chapter. Of the previously mentioned cold-induced injuries, frostbite is most likely to result in a significant injury to the hand.
Frostbite injuries have been well documented throughout history because they frequently occurred during large military campaigns. For example, historical records suggest that thousands of soldiers died from frostbite and other cold-induced injuries when Hannibal and his troops crossed the Alps in 218 BCE. The first large medical report of frostbite was made in the early 19th century by Baron Larrey, the surgeon-in-chief for Napoleon during the winter campaign in Russia. He also introduced “snow friction massage,” a treatment method that was used until the 1950s. Frostbite injuries continued to plague military campaigns into the 20th century. During World Wars I and II and the Korean War, there were an estimated 1 million cases of frostbite.1 Frostbite injuries were particularly common among high-altitude bombers who were exposed to below-freezing temperatures.5 Frostbite management took a great stride forward in the 1950s and 1960s when Merryman and Mills introduced the concept of rapid rewarming, a treatment modality that remains the basis of management today.6-9
Frostbite most often occurs in adults aged 30 to 50 years, and it predominantly affects males (10 : 1). As would be expected, it is more common in colder climates. In Finland, for example, the yearly incidence is 2.5 cases per 100,000. In Antarctica, the incidence is much higher at 65.6 cases per 1000. Unfortunately, there are no large population studies in the United States, but it is fair to assume that frostbite occurs more commonly in the northern parts of the country.
Three population groups tend to be affected by frostbite: (1) the military, (2) the homeless, drug-dependent, or those with psychiatric illnesses, and (3) cold-weather sports enthusiasts. Throughout history, frostbite has been considered a military disease. However, a recent 19-year study of cold-weather injuries by the U.S. Army revealed that the yearly incidence has been decreasing rapidly, likely due to increased awareness and efforts aimed at prevention.10 Alcohol and drug use, homelessness, and psychiatric illness are also strongly associated with frostbite injuries. A 12-year retrospective epidemiologic study performed in the northern prairies of Saskatchewan showed an association with alcohol consumption in 46% of cases, and psychiatric illness in 17% of cases.11 Another study from Montreal noted that alcohol was involved in 62% of cases, psychiatric illness in 19%, other drugs in 15%, and homelessness in 8%.12 Some authorities suggest that in the urban setting, psychiatric illness plays a role in as many as 65% of cases. Finally, cold-weather sports enthusiasts such as mountain climbers, snow-mobile riders, skiers, and sky-divers commonly suffer frostbite injuries. A recent survey of 637 experienced mountaineers showed an incidence of 366 frostbite injuries per 1000.13
Tissue freezing occurs more rapidly as the ambient temperature falls further below the freezing point (of water). In addition, the duration of cold exposure and the conduction properties of the substance to which the body is exposed are crucial factors. For example, because metal is a more efficient conductor of heat than is wood, a cold metallic object pressed against the skin induces frostbite more rapidly than a piece of wood can at the same temperature. Like wood, air is a relatively poor conductor of heat. However, as the wind-speed rises, heat loss through convection increases, creating the basis for the wind chill index.14 For example, at 20°F with a brisk 35-mph wind the risk of frostbite is equivalent to that at 0°F with no wind. Other variables like skin moisture15 or insulating clothing also affect the speed at which frostbite occurs.
Physiologic factors also play an important role in the pathogenesis of frostbite. Normal cutaneous circulation is approximately 200 mL/min, but can vary dramatically. When a person is exerting physical effort, cutaneous circulation can rise to 8000 mL/min. On the other hand, an immobile person in a cold environment might have cutaneous circulation as low as 20 mL/min.1 Increased cutaneous circulation results in loss of body heat but an increase in skin temperature. Conversely, a slowing of cutaneous circulation results in a drop in skin temperature, with preservation of body heat. As the ambient temperature drops, cutaneous vasoconstriction occurs. This allows the body to preserve heat, but also results in a decrease in skin temperature, making it more susceptible to frostbite. As the ambient temperature continues to decrease, another phenomenon called cutaneous intermittent vasodilation (CIVD) occurs.16 During CIVD, blood vessels in the skin periodically dilate for a short period of time, increasing blood flow and warming the skin without a significant loss of body heat. CIVD has a protective effect for the skin and helps to prevent tissue freezing during cold exposure. The CIVD response varies from person to person and may account for differences in individual susceptibility to frostbite. Other physiologic factors contribute to frostbite, including impaired local circulation from smoking, diabetes, peripheral vascular occlusive disease, or vasoconstrictive medications.17 Exertion and physiologic stress also alter cutaneous circulation and can affect susceptibility to frostbite.
Tissue injury occurs by two mechanisms in frostbite: direct cellular damage and progressive tissue ischemia.17,18 Direct cellular damage occurs with the formation of extra- and intracellular ice crystals. Extracellular ice crystals form first as tissue temperature drops. These crystals create an osmotic gradient that draws water out of the cell and into the extracellular tissue. This results in high electrolyte concentrations within the cell, which trigger programmed cell death (apoptosis).17 As temperatures continue to decline, ice crystals form within the cell, resulting in expansion and mechanical destruction.19
The second mechanism of tissue injury, progressive tissue ischemia, is more complex. Cold-induced vasoconstriction and direct endothelial injury initiate a cascade of fibrin deposition, platelet aggregation, and the release of local and systemic mediators.17 Thrombosis occurs, resulting in further ischemia and propagation of the cycle. Prostaglandin F2-alpha and thromboxane A2 are important mediators of this process. They are found in high concentrations in frostbite blister fluid,20 and drugs that block their effects have been shown to reduce tissue damage in animal studies.21
Frostbite has traditionally been divided into four degrees of increasing severity (Table 27-1). First-degree frostbite is a numb white plaque with surrounding erythema. Second-degree frostbite involves clear blister formation. In third-degree injury, hemorrhagic blisters form and eschar may develop, an indication that the reticular dermis is involved (Figs. 27-1 and 27-2). Fourth-degree frostbite presents as frank tissue necrosis, with involvement of subcutaneous tissue, muscle, or bone.1 Unfortunately, this traditional classification system does not correlate well with final outcomes.17 Because of this a number of other classifications have been devised.

Figure 27-1 Second- and third-degree frostbite. Note the large bullae, some of which contain hemorrhagic fluid.

Figure 27-2 Frostbite of a different patient demonstrating sparing of the fingertips, due to clenched fist position at time of exposure.
Table 27-1 Traditional Classification of Frostbite
Degree |
Findings |
1st |
Numb white plaque, surrounding edema, or erythema |
2nd |
Blisters, filled with clear or milky fluid |
3rd |
Hemorrhagic blisters (reticular dermal damage), eschar formation |
4th |
Frankly necrotic tissue, into subcutaneous tissue, muscle, or bone |
Data from McCauley R, Killyon G, Smith D, et al. Frostbite. In: Auerbach P, ed. Wilderness Medicine, 5th ed. Philadelphia: Elsevier; 2007.
The Cauchy classification system (Table 27-2) defines four grades of increasing severity, based on physical examination immediately after rapid rewarming and again on injury day 2. It also incorporates the results of a technetium-99 bone scan on injury day 2.22 The advantage of the Cauchy system is that it attempts to provide prognostic information for each grade. Cauchy also demonstrated that in the hand, the risk of amputation correlates with the proximal extent of the injury.22 If the distal phalanx alone is affected, there is only a 1% chance of amputation. If the injury extends into the middle phalanx, the risk increases to 31%. Proximal phalangeal extension results in a 67% chance of amputation at some level, and metacarpal or carpal extension means almost certain amputation.
Table 27-2 Cauchy Classification
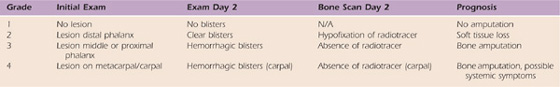
Data from Cauchy E, Chetaille E, Marchand V, Marsigny B. Retrospective study of 70 cases of severe frostbite lesions: a proposed new classification scheme. Wilderness Environ Med. 2001;12:248-255.
One of the most important features of frostbite is the prolonged demarcation period. On average it takes 3 weeks for frostbitten tissue to fully demarcate, although it is not unusual for it to take many months. Often remarkable improvement takes place over time, and tissue that initially appeared necrotic or severely injured can survive. This characteristic of frostbite injuries is the basis for delaying surgical débridement as long as possible.17
The utility of imaging studies in frostbite injury is controversial. Plain radiographs should always be obtained, not for diagnostic purposes, but to provide a baseline for future comparison. A number of other imaging modalities have been advocated, with the goal of identifying tissue demarcation levels earlier in the course of treatment. Radioisotope scans including 131I (iodine-131), 133Xe (xenon-133), and 99Tc (technetium-99) have been used.23-25 Angiography, MRI, and magnetic resonance angiography (MRA) have also been studied.17,26-28 Although some of these imaging techniques may become useful in the future, it currently appears that none is completely accurate until 2 to 3 weeks after frostbite injury.1,17 By then, physical examination can usually determine demarcation levels reliably.
Initial management in the field should include removal of any wet clothing, followed by padding of the hand and application of an orthosis. No attempt should be made to rewarm the hand in the field or during transport to the hospital. Thawing followed by refreezing causes a more severe injury than freezing alone.17 Rubbing the skin, or “snow friction massage,” should also be avoided. Frostbitten skin is fragile and susceptible to shear injury. Once in the emergency department, hypothermia should be treated before any attempt at rewarming of the hand. Once hypothermia has been addressed, rapid rewarming should be performed.
Rapid rewarming was developed and studied by Merryman and Mills in Alaska during the 1950s and 1960s.6-9 Studies that have since been performed comparing slow rewarming with rapid rewarming (with or without adjunctive therapies) demonstrate better results with rapid rewarming.29-31 Rapid rewarming involves immersion of the hand in circulating warm water with a dilute antimicrobial agent. The temperature should be carefully maintained at 40–42°C (104–108°F). Higher temperatures can result in thermal injury to the skin, and lower temperatures are less effective. Rapid rewarming takes 20 to 30 minutes in most cases and should be performed until the skin is pliable.19,32
After rapid rewarming, treatment is largely nonoperative. Surgical débridement should be delayed for at least 3 weeks and should not be considered until tissue has clearly demarcated. Early surgery should be reserved for surgical infections or escharotomy. There are case reports of early soft tissue débridement and coverage of ischemic bone with vascularized soft tissue transfers.33 Although this approach may be useful in some situations, it has not yet become the standard of care. Figures 27-3 through 27-8 demonstrate the demarcation and healing of a frostbite injury over time. Although this injury initially appeared quite severe, the patient went on to heal completely without surgery.

Figure 27-3 Another patient. Dorsal view within days of injury. Note that most of the bullae contain nonhemorrhagic fluid.

Figure 27-5 Dorsal view 3 weeks after injury. Note that most areas have healed, with the exception of the fingertips.

Figure 27-6 Palmar view 3 weeks after injury. Note eschar formation at fingertips, consistent with deeper dermal injury.

Figure 27-7 Dorsal view at 3 months after injury. Note complete healing of skin, with persistent discoloration of nail beds. Also note loss of nail plate on bilateral long fingers.

Figure 27-8 Palmar view at 3 months after injury. Note well-demarcated eschar at fingertips. Patient went on to heal completely over the next 2 months without surgical débridement or skin grafting.
Standard nonoperative management after rapid rewarming includes (1) ibuprofen, (2) penicillin, (3) tetanus prophylaxis, (4) débridement of clear blisters, (5) topical aloe vera, and (6) elevation of the hand. Ibuprofen (400 mg PO q12h) is used to block the arachidonic acid cascade. Clear blisters are gently débrided at the bedside or in a whirlpool in order to remove thromboxane and prostaglandins from the wound surface. Hemorrhagic blisters should be left intact to prevent exposure and desiccation of the deep dermis. Topical aloe vera (applied q6h) is also believed to reduce thromboxane levels.1,17
A number of other modalities, including hyperbaric oxygen, dextran, heparin, and thrombolytics, have been used.18,34-38 Some evidence from animal studies indicates that these adjuncts might prove useful, but as of yet there are no compelling human studies.
The hand therapist plays a crucial role in the treatment of frostbite, both in terms of acute wound management, and in the maintenance of mobility. Early in the postinjury period edema formation occurs. If untreated, it causes a number of problems. It results in a relative decrease in tissue oxygen tension and can potentially worsen the severity of the injury. It also reduces the natural antistreptococcal properties of the skin. Finally, it severely limits active and passive motion. Orthotic use and elevation, as well as periodic active finger flexion and extension, are appropriate edema control measures. Compressive wraps or garments should be avoided in the early postinjury period to reduce the risk of compressive ischemia or shear injury.
Daily whirlpool and hydrotherapy should be instituted. Whirlpool fluid should be warmed to about 40°C (104°F) and should contain a dilute antimicrobial agent. Whirlpool/hydrotherapy sessions should focus on two goals: débridement and maintenance of motion. Whirlpool and gentle pulse lavage can be used to assist with débridement of broken blisters and loose necrotic tissue. This is also an ideal time to work on passive and active range of motion. These sessions have the added benefit of improving circulation. It is important to note that the dependent position of the hand during the whirlpool treatment can contribute to an increase in edema. For this reason limiting the duration of the whirlpool treatment to 5 minutes at a time is recommended.39
Postinjury orthosis use should focus on prevention of contractures, and protocols similar to those used in burn patients are appropriate. The hand and wrist should be fixed in a comfortable position of function. Tight Velcro straps should be avoided. Initially the orthosis may be held in place with lightly applied gauze wrap. As edema resolves, the orthosis will need to be adjusted and Velcro straps may be applied to allow a more secure fit.
The patient should be instructed in active and passive motion out of the orthosis. In areas where the degree of tissue injury is unclear, it is important to limit stress to the injured tissue through very gentle exercise. Light functional activities may begin as soon as wound healing permits. An assessment of the patient’s ability to perform activities of daily living is called for with provision of assistive equipment or adaptive techniques as needed. The extent to which the injury affects the individual’s ability to work and fulfill his or her roles and responsibilities in relation to family and home is addressed and adaptations are suggested. Finally, the hand therapist may be asked to assist with scar management and desensitization after the wounds have healed.
Frostbite is a severe cold-induced injury that occurs at below-freezing temperatures. It primarily affects three types of patients: (1) those in the military, (2) the homeless, drug-addicted, or mentally ill, and (3) cold-weather sports enthusiasts. Tissue injury occurs by two mechanisms: direct cellular injury by ice crystals, and progressive tissue ischemia mediated by the arachidonic acid cascade. The initial management of frostbite involves transfer of the patient to a treatment center where rapid rewarming can be performed. Post-thaw treatment includes ibuprofen, penicillin, tetanus prophylaxis, débridement of clear blisters, topical aloe vera, and elevation of the hand. Surgical débridement should be delayed until tissue has clearly demarcated. This may take weeks or months, and tissue that initially appears severely injured often survives. The hand therapist should be involved early on in the care of the patient. Orthotic use, elevation, and range of motion should be initiated at the time of injury. Compressive dressings should be avoided. Whirlpool and hydrotherapy can be helpful for débridement and assist during range of motion exercises. Postinjury orthotic use should focus on prevention of contractures, with care taken to avoid tissue compression. Finally, the therapist plays an important role in scar management and desensitization after the wounds are healed.
1. McCauley R, Killyon G, Smith D, et al. Frostbite. In: Auerbach P, ed. Wilderness Medicine. 5th ed Philadelphia: Elsevier; 2007:195–210.
2. Cribier B, Djeridi N, Peltre B, Grosshans E. A histologic and immunohistochemical study of chilblains. J Am Acad Dermatol. 2001;45:924–929.
3. Simon TD, Soep JB, Hollister JR. Pernio in pediatrics. Pediatrics. 2005;116:e472–e475.
4. Ungley CC, Channell GD, Richards RL. The immersion foot syndrome. 1946. Wilderness Environ Med. 2003;14:135–141. discussion, 134
5. Simeone FA. The surgical volumes of the history of the United States Army Medical Department in World War II. Cold injury. Arch Surg. 1960;80:396–405.
6. Mills WJ Jr. A study of frostbite treatment. J R Nav Med Serv. 1963;49:237–243.
7. Mills WJ Jr. Frostbite. A method of management including rapid thawing. Northwest Med. 1966;65:119–125.
8. Mills WJ Jr, Douglas JD, Gottmann AW. Clinical experiences in treatment and rehabilitation of frostbite in Alaska. Tech Rep Arct Aeromed Lab US. 1960;59-24:1–9.
9. Meryman HT. Mechanisms of freezing in living cells and tissues. Science. 1956;124:515–521.
10. DeGroot DW, Castellani JW, Williams JO, Amoroso PJ. Epidemiology of U.S. Army cold weather injuries, 1980-1999. Aviat Space Environ Med. 2003;74:564–570.
11. Valnicek SM, Chasmar LR, Clapson JB. Frostbite in the prairies: a 12-year review. Plast Reconstr Surg. 1993;92:633–641.
12. Koutsavlis AT, Kosatsky T. Environmental-temperature injury in a Canadian metropolis. J Environ Health. 2003;66:40–45.
13. Harirchi I, Arvin A, Vash JH, Zafarmand V. Frostbite: incidence and predisposing factors in mountaineers. Br J Sports Med. 2005;39:898–901. discussion, 901
14. Wilson O, Goldman RF. Role of air temperature and wind in the time necessary for a finger to freeze. J Appl Physiol. 1970;29:658–664.
15. Molnar GW, Hughes AL, Wilson O, Goldman RF. Effect of skin wetting on finger cooling and freezing. J Appl Physiol. 1973;35:205–207.
16. Daanen HA, van Ruiten HJ. Cold-induced peripheral vasodilation at high altitudes—a field study. High Alt Med Biol. 2000;1:323–329.
17. Murphy JV, Banwell PE, Roberts AH, McGrouther DA. Frostbite: pathogenesis and treatment. J Trauma. 2000;48:171–178.
18. Weatherley-White RC, Sjostrom B, Paton BC. Experimental studies in cold injury. Ii. The pathogenesis of frostbite. J Surg Res. 1964;4:17–22.
19. Heggers JP, Robson MC, Manavalen K, et al. Experimental and clinical observations on frostbite. Ann Emerg Med. 1987;16:1056–1062.
20. Robson MC, Heggers JP. Evaluation of hand frostbite blister fluid as a clue to pathogenesis. J Hand Surg [Am]. 1981;6:43–47.
21. Raine TJ, London MD, Goluch L. Antiprostaglandins and antithromboxanes for the treatment of frostbite. Surg Forum. 1980;31:557–559.
22. Cauchy E, Chetaille E, Marchand V, Marsigny B. Retrospective study of 70 cases of severe frostbite lesions: a proposed new classification scheme. Wilderness Environ Med. 2001;12:248–255.
23. Cauchy E, Chetaille E, Lefevre M, et al. The role of bone scanning in severe frostbite of the extremities: a retrospective study of 88 cases. Eur J Nucl Med. 2000;27:497–502.
24. Junila J, Torniainen P, Kaarela O, et al. Assessment of tissue viability in frostbite by 99Tcm-HDP scintigraphy: an experimental study in New Zealand white rabbits. Nucl Med Commun. 1992;13:542–546.
25. Bhatnagar A, Sarker BB, Sawroop K, et al. Diagnosis, characterisation and evaluation of treatment response of frostbite using pertechnetate scintigraphy: a prospective study. Eur J Nucl Med Mol Imaging. 2002;29:170–175.
26. Barker JR, Haws MJ, Brown RE, et al. Magnetic resonance imaging of severe frostbite injuries. Ann Plast Surg. 1997;38:275–279.
27. Gralino BJ, Porter JM, Rosch J. Angiography in the diagnosis and therapy of frostbite. Radiology. 1976;119:301–305.
28. Likhoded VI. [Angiography in the diagnosis of frostbite]. Vestn Khir Im I I Grek. 1973;110:90–93.
29. Martinez Villen G, Garcia Bescos G, Rodriguez Sosa V, Morandeira Garcia JR. Effects of haemodilution and rewarming with regard to digital amputation in frostbite injury: an experimental study in the rabbit. J Hand Surg [Br]. 2002;27:224–228.
30. Dawson D, Hardenbergh E. Effect of rapid rewarming on tissue survival of frozen rabbits’ feet. J Appl Physiol. 1958;12. 255–163
31. Carpenter HM, Hurley LA, Hardenbergh E, Williams RB. Vascular injury due to cold. Affects of rapid rewarming. Arch Pathol. 1971;92:153–161.
32. Fuhrman FA, Crismon JM. Studies on gangrene following cold injury. Vii. Treatment of cold injury by means of immediate rapid warming. J Clin Invest. 1947;26:476–485.
33. Greenwald D, Cooper B, Gottlieb L. An algorithm for early aggressive treatment of frostbite with limb salvage directed by triple-phase scanning. Plast Reconstr Surg. 1998;102:1069–1074.
34. von Heimburg D, Noah EM, Sieckmann UP, Pallua N. Hyperbaric oxygen treatment in deep frostbite of both hands in a boy. Burns. 2001;27:404–408.
35. Fuhrman FA, Crismon JM. Studies on gangrene following cold injury. Ix. The effect of rutin and other chemical agents on the course of experimental frostbite in rabbits. J Clin Invest. 1948;27(3 Pt 1):364–371.
36. Shumacker HB Jr, Radigan LR, Ziperman HH, Hughes RR. Studies in experimental frostbite. VI. Effect of rutin and Benadryl with some notes on plaster casts and the role of edema. Angiology. 1951;2:100–107.
37. Lempke RE, Shumacker HB Jr. Studies in experimental frostbite. VIII. Treatment with ACTH. Angiology. 1951;2:340–344.
38. Twomey JA, Peltier GL, Zera RT. An open-label study to evaluate the safety and efficacy of tissue plasminogen activator in treatment of severe frostbite. J Trauma. 2005;59:1350–1354. discussion, 1354-1355
39. Brown FE, Hamlet MP, Feehan L. Acute care and rehabilitation of the hand after cold injury. In: Mackin EJ, ed., et al. Rehabilitation of the Hand and Upper Extremity. 5th ed St. Louis: Mosby; 2002.