Manual Edema Mobilization: An Edema Reduction Technique for the Orthopedic Patient
THEORETICAL FOUNDATION: ANATOMIC AND PHYSIOLOGIC SUPPORT
MANUAL EDEMA MOBILIZATION CONCEPTS
▪ Stimulation of the lymphatic system is necessary to decrease subacute and chronic edema.
▪ The proteins associated with subacute and chronic edema need to disperse through the lymphatic system, as they are too large to permeate the venous system.
▪ The initial lymphatic system is superficial, fine, and fragile, therefore firm compression may collapse the system.
▪ Diaphragmatic breathing, light massage, and exercises help to stimulate the lymphatic system.
Manual edema mobilization (MEM) is a lymphatic stimulation technique used for recalcitrant subacute or chronic limb/hand edema in the orthopedic population. The phrase popularized by Watson-Jones in 1941,1 “Oedema is glue,” summarizes the importance of reducing edema in swollen hands because persistent edema can contribute to fibrosis, stiffness, and limited range of motion (ROM). Historically, many edema treatment techniques were developed with the rationale that the technique “stimulated the venous and lymphatic systems,”2-4 giving the impression that one technique would affect both systems equally. However, current literature now describes differences between how the venous and lymphatic systems remove excess fluid,5 thereby lending credence to the fact that not all edema reduction techniques work for all types of edema. Clinically, therapists have seen that some edemas reduce with little effort, whereas others progress into a gel-like and fibrotic state regardless of intense therapy. This phenomenon can be puzzling and frustrating for therapists. However, an understanding of the different types of edema and an understanding of the differences between the venous system and lymphatic system with regard to edema reduction can help therapists understand why some common edema treatment techniques may not work on all types of edema (Table 65-1). The purpose of this chapter is to describe the MEM technique, which is an edema reduction technique used to stimulate the lymphatic system to decrease subacute and chronic edema in the orthopedic population.
Table 65-1Types of Edemas Seen by Hand Therapists
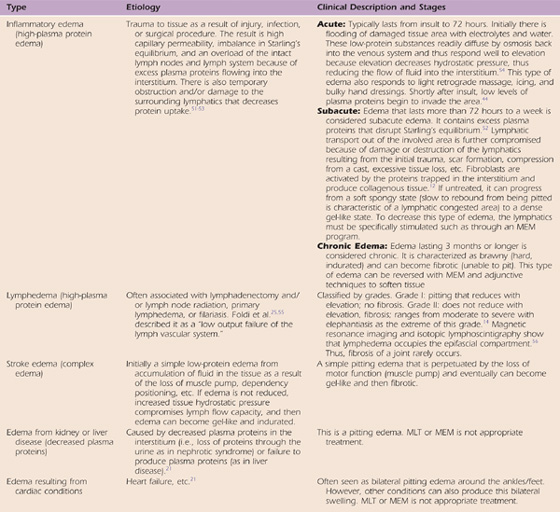
Note: The table shows that all edemas are not alike: there are types of the edemas such as high protein and low protein; there are stages labeled acute, subacute, and chronic that reflect component changes in the edema; there are cardiac and renal edemas and lymphedema; there are comorbidities that affect the edema reduction or increase it. When a therapist understands these factors, he or she will no longer treat all edemas alike by just trying one technique after the other without a physiologic rationale. This is the new learning and challenge in treating orthopedic hand and arm edema.
MEM was first described in the late 1990s as a method of decreasing subacute and chronic edema in orthopedic patients through stimulation of the lymphatic system.6,7 Using lymphatic treatment techniques for orthopedic patients to decrease subacute and chronic edema in people with healthy but overloaded lymphatic systems is relatively new. However, although the concept of MEM is relatively new, the history of MEM from a physiologic perspective is closely linked with historical revelations regarding the lymphatic system.
Throughout the 17th and 18th centuries, scientists, anatomists, and physicians described the role of the lymphatic system as part of the circulation system within the body,5,8,9 with lymph flowing from tissues, through the lymphatics, and into the bloodstream.10 Additionally, during this time frame, the connection between the lymphatic system and edema was also appearing in the literature.11 Treatment techniques designed to capitalize on this link between the lymphatic system and edema started appearing in the literature during the 19th and 20th centuries, as several massage therapists and physicians designed different manual techniques to stimulate the lymphatic system for edema reduction purposes.5,12 The most well-known lymphatic massage technique, known today as manual lymphatic drainage (MLD), was developed in the 1960s through a collaboration of different German health care specialists.12 Since then, variations of the MLD technique have been reported in the literature under terms such as decongestive lymphatic therapy, complex decongestive physiotherapy, and lymph drainage therapy.5,13,14 Recently, the term manual lymphatic treatment (MLT) has been increasingly used in scientific publications5 to describe principles common to all schools of lymphatic drainage, and, therefore, despite the numerous acronyms, all these aforementioned techniques are designed to stimulate the lymphatic system through the application of light compression bandages, light massage, exercises, and skin care.5,13,14
Currently, there is one published quasiexperimental study on MEM.15 This study demonstrated statistically significant reductions in edema in four of the five subjects by using a single-subject design study when MEM was entered into the standard treatment protocol.15 Additionally, there is one published case study on MEM demonstrating how MEM can be incorporated into a treatment program for a patient with multiple traumas to the upper limb.16 Although MEM is starting to appear in the literature as an effective treatment option for specific patient populations,16,17 there is still a need for continued research on the use of lymphatic therapies for orthopedic patients because such research may alter how therapists initially treat orthopedic edema.
MEM is built on the same theoretical foundation as manual lymphatic therapies.6,7,18 The anatomical and physiological support for manual lymphatic therapies is that stimulation of the lymphatic system is necessary to decrease high-protein edema.5,19 Normally, plasma proteins, which are proteins found in the blood, are present in lower concentrations in the interstitial fluid compared with the microvessels.20 Typically, the concentration of these larger proteins in the interstitial spaces remains low because these proteins do not diffuse easily through the microvessels.21,22 However, after an injury, the inflammatory response changes the permeability of the microvessels, allowing these plasma proteins to leak into the interstitial spaces.22,23
These plasma proteins that leak into the interstitium are too large to permeate the venous system5,24 and need to be disposed of through the lymphatic system21,20 because a primary role of the lymphatic system is to dispose of matter that is too large for the venous system.5,20,21,24 However, after an injury, the lymphatic system may be damaged or overloaded, which can hinder its ability to dispose of these larger plasma proteins.5,25 If these plasma proteins remain in the interstitium, the colloid osmotic pressure, which is “the pressure to diffuse exerted by proteins and macromolecules,”5 of the interstitial fluid increases.21 This increase in the interstitial colloid osmotic pressure subsequently draws more fluid into the interstitial spaces.19,22,23,26 Therefore, if these proteins remain in the interstitium, the edema will persist because of the pull of fluid into the interstitium.25 Prolonged stagnation of plasma proteins in the interstitium leads to chronic inflammation.27 As stated by Casley-Smith and Casley Smith,19 “If edema lasts several weeks, this promotes chronic inflammation with its aftermath of excess fibroblasts and collagen deposition in the tissue.”
The lymphatic tissue drainage system consists of three levels of structures. The lymph capillaries, called the initial lymphatics and precollectors, make up the first level.14,28 These structures are finger-shaped, closed at one end, netlike vessels located in the interstitium that directly or indirectly drain every part of the body.21 The vessels consist of a single layer of overlapping endothelial cells that have connector filaments anchoring them to surrounding connective tissue14,29 (Fig. 65-1). The flaplike junctions formed by the overlapping endothelial cells open when the local interstitial pressure changes. When the junctions open, fluid flows in, changing the internal pressure of the lymphatic from low to high, thus closing the flaplike junctions.21,29
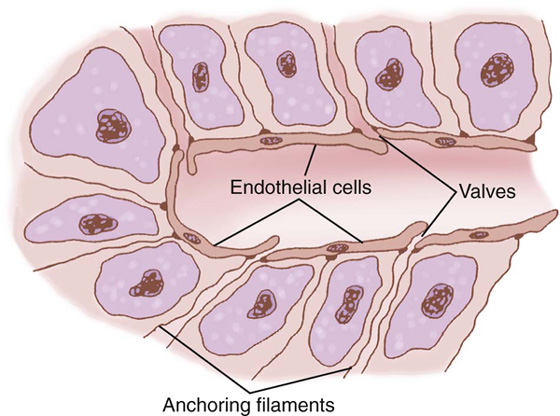
Figure 65-1 Special structure of the lymphatic capillaries that permits passage of substances of high molecular weight into the lymph.(From Guyton AC, Hall JE. Textbook of Medical Physiology. Philadelphia: WB Saunders; 1996.)
Lymph then enters the deeper tube-shaped collector lymphatics. The collector lymphatics have walls consisting of three layers. The inner layer is called the intima or endothelium.30 The media or middle layer consists of smooth muscle and thin strands of collagen fibers30 that respond to the stretch reflex. The outer layer, called the adventitia, is formed by connective tissue.21 Every 6 to 20 mm within the tube-shaped collectors are valves that prevent the backflow of lymph.30 The space, or chamber, between the valves is called a lymphangion.31 As fluid enters a lymphangion, it fills the segment, stimulating a stretch reflex of the medial smooth muscle layer. The ensuing contraction causes the proximal valve to open and propel the lymph to the next proximal lymphangion30,31 (Fig. 65-2). At rest, lymphangions pump 6 to 10 times per minute.21 However, with muscle contraction from exercise, lymphangions can pump 10 times that amount.14,21
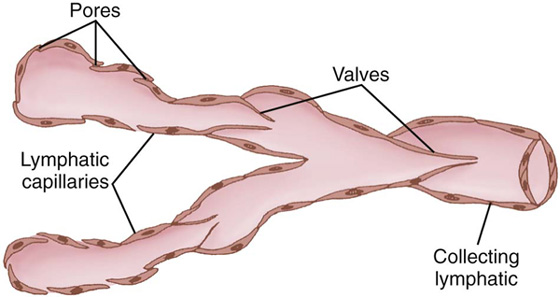
Figure 65-2 Structure of lymphatic capillaries and a collecting lymphatic, showing also the lymphatic valves.(From Guyton AC, Hall JE. Textbook of Medical Physiology. Philadelphia: WB Saunders; 1996.)
The collector lymphatics propel lymph to the nodes.29 The nodes consist of a complex of sinuses that perform immunologic functions. After leaving the nodes, lymph either enters the venous system through lymph-venous anastomoses or continues to move into deeper lymphatic trunks and eventually returns to the blood circulatory system via the left and right subclavian veins.
Anatomically, the trunk is divided into four lymphatic quadrants, or lymphotomes(drainage territories).14 These consist of left and right upper quadrants, called thoracic lymphotomes, and left and right lower quadrants, called abdominal lymphotomes.14 The thoracic lymphotomes extend from the anterior midline to the vertebral column on both the left and right sides of the upper trunk. Lymph drains within the lymphotomes from superficial to deeper vessels that connect to nodes. Between the lymphotomes are watershed areas (i.e., dividing areas) where normal drainage is away from the watershed, moving toward the nodes.32,33 There are only a few superficial and deep connecting lymph vessels across watershed areas, but there are superficial collateral vessels.14 These collateral connections across watersheds are very important because when there is lymph congestion, they provide alternative pathways to uncongested lymph vessels. The extremities also have lymphotomes. The upper extremity lymphotomes drain mainly into the axillary nodes. Detail of this information and more extensive drawings can be found in the work of Kubik.33
Lymph from the right thoracic lymphotome, right upper extremity, and right side of the head drains into trunks that eventually empty into the right lymphatic duct. This duct empties into the right subclavian vein and into the superior vena cava of the heart. Both lower extremities, both abdominal lymphotomes, the left thoracic lymphotome, and the left side of the head drain into the thoracic duct, which is the largest lymphatic vessel in the body and extends from L2 to T4.30,33 The thoracic duct empties into the venous system at the juncture of the left subclavian and jugular veins. As described by Chikly,5 “the lymphatic system is therefore a second pathway back to the heart, parallel to the blood venous system.”
The lymphatic system is described as “a ‘scavenger’ system that removes excess fluid, debris and other materials from the tissue spaces.”21 It is an alternate path for those substances that are too large to be disposed of through the venous system.24 There is a close link, therefore, between an adequately functioning lymphatic system and edema because “oedema can only occur if the lymphatic system has failed.”14
Therefore, the overall theory of lymphatic therapies, including MEM, is to remove plasma proteins from edematous areas by stimulating the lymphatic system, which subsequently enables these proteins to leave the interstitial spaces and enter the lymphatic structures. By ridding the interstitial spaces of these hydrophilic proteins, subacute and chronic edema decreases.
Despite physiologic similarities between MLT and MEM, there are differences worth noting. One difference between the MLT technique and the MEM technique is the patient population. MLT techniques were originally devised for individuals with lymphedema, which is a high plasma protein edema associated with a mechanical obstruction or insufficiency of the lymphatic system.32 MEM was designed for orthopedic patients with subacute and chronic edema in whom the lymphatic system is intact but temporarily overloaded.
Another difference between the MLT techniques and the MEM technique is the length of the treatment. Because MLT is used on people with a permanently insufficient lymphatic system, the treatment sessions are longer and more involved because large amounts of fluid may need to be rerouted throughout the body. Conversely, because the MEM technique is used on people with intact lymphatic systems, the treatment sessions are shorter and typically involve moving less fluid. Also, unique to MEM is the use of pump point stimulation, which helps to eliminate the extensive massage time spent on an involved extremity because of the simultaneous stimulation of areas in the body with concentrated lymphatic structures. When using MEM on someone with subacute edema that has been present for 3 to 4 weeks, it is not unusual to see the edema decrease after two 20-minute sessions, especially if the patient is compliant with the home MEM program. These shorter treatment sessions are conducive to the needs of today’s clinicians in the orthopedic setting.
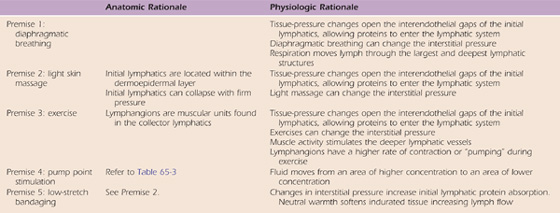
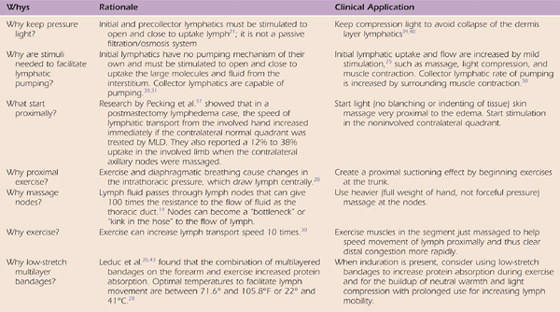
The basic MEM technique consists of diaphragmatic breathing, light skin-traction massage, exercise, pump point stimulation, and a self-management program. Adjunctive methods such as chip bags, low-stretch bandaging, and Kinesio taping may also be used for patients with chronic edema, when lymph softening techniques are necessary. To effectively use the MEM treatment method, therapists need an understanding of the physiologic and anatomic rationale underlying the five basic treatment concepts as related to lymphatic stimulation (Table 65-2).
Table 65-2 Anatomic and Physiologic Rationale for Manual Edema Mobilization Premises
All MEM sessions begin with deep, diaphragmatic breathing. This “belly” breathing involves breathing in deeply through the nose, causing the abdomen to expand, and then slowly exhaling through “pursed” lips. Feeling or seeing the rise and fall of the abdomen can help the therapist ensure that the patient is correctly performing the technique.34,35
Respiration changes tissue pressure,33 and thus lymphatic absorption is stimulated.29 The thoracic duct is the largest and one of the deepest lymphatic structures. It lies anterior to and parallel with the spine beginning at L2 and terminating into the left subclavian vein at approximately T4.30 Diaphragmatic breathing, also known as the pulmonary pump,5 changes pressure within the thoracic duct.5,33 The thoracic duct functions on hydrodynamic principles.33 Therefore, the pressure differential created from diaphragmatic breathing helps propel the lymph centrally toward the subclavian veins.36 These pressure changes in the thoracic duct then create a vacuum (suction), pulling lymph from the peripheral structures centrally.14,28,33
A light skin-traction massage is a massage so light that no blanching or indentation of the skin occurs yet it is firm enough to move the skin, thereby preventing the hand from sliding on the skin. The light skin-traction massage technique involves a rhythmical massage that forms U shapes on the skin, with the opening of each U in the direction of lymphatic flow proximally to an uninvolved or previously decongested area. The massage technique should remain light and should follow lymphatic pathways.
Initially, the therapist performs the MEM massage technique (the U technique) in one segment of the body, starting proximally (or centrally) and moving distally down the segment. This proximal- (or central-) to-distal massage technique is referred to as the “clearing Us,” and its purpose is to clear the lymphatic system within that segment. The clearing Us technique consists of performing five consecutive U massages in the most proximal (or central) location within that segment, then performing another five U massages just distal to the previous five, and continuing in this manner down to the distal portion of that segment. For example, if edema is in the right hand, the clearing Us would start with five Us at the left shoulder region, then five at the left clavicle, five over the sternum, five over the right clavicle, five at the right shoulder region, and so on down the arm until the therapist reached the hand.
Immediately after performing the clearing U massage technique in each section (trunk, upper arm, elbow, forearm, hand), active and/or passive exercises that move the joints and muscles associated with the recently cleared body segment are performed. In the example given, active and/or passive shoulder flexion, shoulder abduction, elbow flexion/extension, wrist flexion/extension, and fisting exercises would be performed after the clearing U massage.
Once the clearing U massages have been performed throughout the entire segment and the active and/or passive exercises have been performed, that segment is then considered cleared. The purpose of clearing a segment is to open and clear out the lymphatic pathways to allow the flow of lymph into the central structures.
After a segment has been cleared, the therapist changes the direction of the massage technique to promote the flow of lymph through the recently cleared segment. During the flow portion, the U massage is performed distally to proximally (or centrally) within the newly cleared segment. This distal-to-proximal (or -central) massage technique is referred to as “flowing Us,” and it consists of performing one U massage in a distal location within the cleared segment, then performing another U massage just proximal to the previous one, and continuing up to the most proximal portion of the segment. At this point, the sequence is repeated until five U massages have “flowed” up the cleared segment.
In the previous example, after the right arm had been cleared, the therapist would perform one U massage over the dorsum of the right hand, then over the right volar wrist, the right volar forearm, the right cubital tunnel, the right volar upper arm, the right shoulder, the right clavicle, the sternum, the left clavicle, and then finally the left axilla. This entire sequence would then be performed a total of five times to “flow” the lymph up the right arm over to the left axilla, so it drains centrally. Flowing U massage consists of sequential Us (one following another) starting in the distal part of the segment being treated and moving proximally past the nearest set of lymph nodes. The flowing can be described as “waltzing” up the arm. After the five flowing Us have been performed within a segment, active and/or passive exercises associated with the body area are performed.
Although the clearing U massage and the flowing U massage are performed in the same segmental area, they differ from each other in two ways. First, the clearing U massage is performed in a proximal- (or central-) to-distal fashion, whereas the flowing U massage is performed in a distal-to-proximal (or -central) fashion. Second, the clearing U massage consists of performing five U massages in each location before moving distally, whereas the flowing U massage consists of performing only one U massage distally within a segment, and then moving sequentially up the segment until the proximal (or central) portion of that segment is reached. The flowing U massage sequence is then repeated a total of five times (Figs. 65-3 through 65-5).

Figure 65-3 Trunk: Clear A, B, C, and flow C, B, A. Upper arm: Clear A, B, C by tractioning the skin from posterior to the biceps. Flow massage C, B, A up to the sternum or to the uninvolved quadrant.
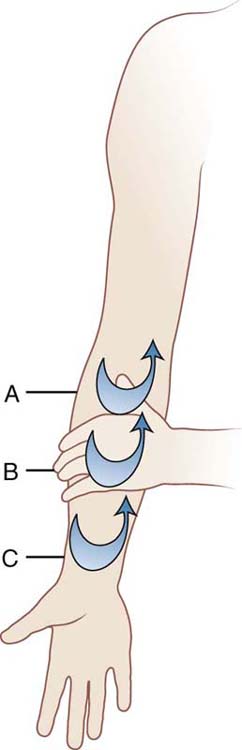
Figure 65-4 Forearm: Clear A, B, C. Flow massage C, B, A. Clear elbow node five times and continue massage to the biceps or the head of the humerus. Pronate the forearm and repeat the same sequence on the dorsum of the arm.
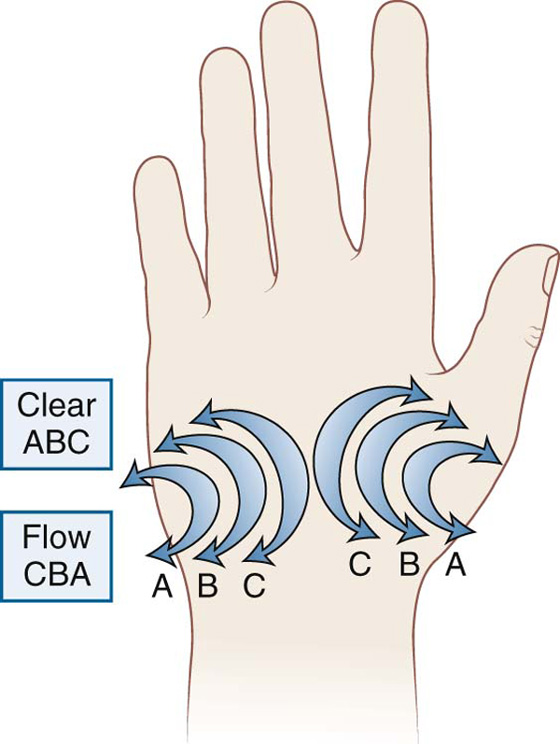
Figure 65-5 Palm: Lateral side of the therapist’s thumbs are placed along the lateral sides of the patient’s first and fifth metacarpals. Clear A, B, C and flow massage C, B, A sliding across the flexor retinaculum to the outside edges of the hand. Flow massage the dorsum of the hand to the mid-forearm.
The light skin-traction massage influences the lymphatics on a superficial level. As mentioned earlier, the initial lymphatics are the small lymphatic channels that create a meshlike network14,33 throughout the dermoepidermal layer of the skin.5 Attached to these small lymphatic channels are the anchoring filaments, which connect these cells to the surrounding tissues, and between these cells are junctures known as interendothelial gaps5 (Fig. 65-6). As tissue pressure changes, the anchoring filaments assist in opening these interendothelial gaps,5,33 thereby allowing fluid within the interstitial spaces to enter the lymphatic system.37 Therefore, any mechanism that changes interstitial pressure ultimately stimulates lymphatic flow, and massage is one of those variables reported to change tissue pressure.14,38
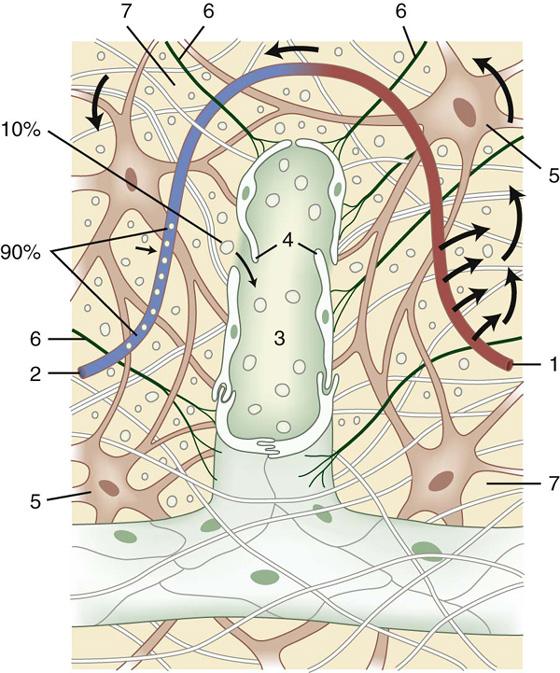
Figure 65-6 Incorporation of the lymph capillary in the interstitium. 1, Arterial section of the blood capillary; 2, venous section of the blood capillary; 3, lymph capillary; 4, open intercellular groove–swinging tip; 5, fibrocyte; 6, anchor filaments; 7, intercellular space. Small arrows indicate the direction of the blood flow; large arrows indicate the direction of the intercellular fluid flow.(From Kubic, S. Anatomy of the Lymphatic System. In: Foldi M, Foldi E, Kubik S (eds). The Textbook of Lymphology for Physicians and Lymphedema Therapists, 2003 Elsevier Gmbh, Munchen.)
Additionally, because the initial lymphatics are considered “feather fine” fragile vessels,5 firm pressure can collapse them. Miller and Seale39 found that a pressure of 60 mm Hg initiated lymphatic closure, with complete closure at 75 mm Hg.39 Furthermore, it has been demonstrated that a 3- to 5-minute massage at 70 to 100 mm Hg on edematous tissue caused temporary damage to the endothelial lining of the initial and collector lymphatics.40 Therefore, the MEM massage technique is light, just enough to move the skin without blanching it.
Active and/or passive exercise is an integral part of MEM. The MEM exercise routine normally begins with trunk exercises immediately after the diaphragmatic breathing. The active/passive exercises then move to the periphery and correlate with the area on the body recently massaged with the clear and flow techniques. For example, if the MEM massage technique was just performed over the volar aspect of the wrist, then active and/or passive wrist flexion and extension would occur immediately after the massage.
Similar to light massage, muscle contractions also influence tissue pressure, allowing fluid to flow into the initial lymphatic system by opening the interendothelial gaps.14 Additionally, after the fluid enters the initial lymphatics, it then travels through deeper lymphatic vessels, the collector lymphatics5,14,33 (Fig. 65-7). At the level of the collector lymphatics, the lymphatic system has muscular units known as lymphangions. Simultaneous muscle activity has been found to stimulate the deeper layers of the lymphatic system14 because the lymphangions have a higher rate of contraction or “pumping” during exercise,41 and lymphatic flow can increase by 10 to 30 times through the lymphangions with exercise.5,30 Exercise then stimulates the superficial lymphatics by altering tissue pressure and stimulates the deeper lymphatics, which aids in propelling the lymph through the deeper vessels.14
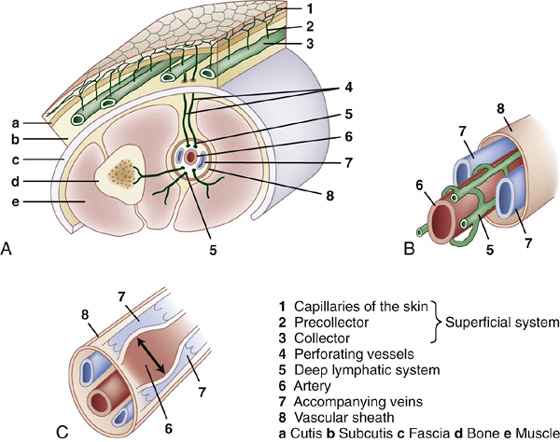
Figure 65-7 Structure of the lymphatic system. Layers (A), content of the vascular sheath (B), lymph transport by arterial pulsation (C).(From Kubic, S. Anatomy of the Lymphatic System. In: Foldi M, Foldi E, Kubik S (eds). The Textbook of Lymphology for Physicians and Lymphedema Therapists, 2003 Elsevier Gmbh, Munchen.)
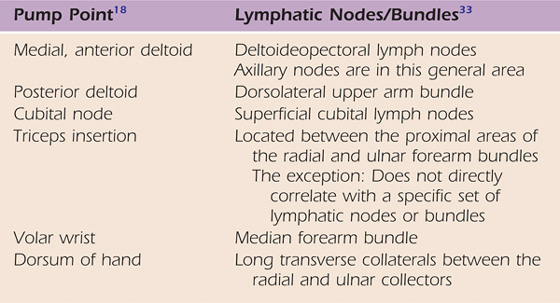
In the extremities, there are areas of concentrated lymphatic bundles or lymphatic nodes (Table 65-3). The term pump point stimulation refers to simultaneously massaging two areas of concentrated lymphatic structures versus one set of lymphatic structures as in clear and flow massage. These are points of stimulation done in a U-shaped pumping motion. For instance, after the light skin-traction massage of clear and flow is done across the upper trunk, pump point stimulation is performed on the involved extremity followed by flow massage to a proximal site and exercise of the muscles in the area. The concept underlying pump points is based on the theory that massage creates a locally negative pressure gradient, thereby draining the lymphatic system distally18,41 (Figs. 65-8 and 65-9). The MEM study,15 which primarily included the use of pump point stimulation, showed a decrease in post orthopedic edema.
Table 65-3 Correlation of Pump Points to Lymphatic Nodes/Bundles
Although there is currently no anatomic research that supports the use of pumppoints to decrease edema, there is speculation by the authors that the observed decrease in edema after pump point stimulation may be the result of changes in pressure gradients. The circulatory system, which includes the lymphatic system, functions on pressure gradients, meaning that substances diffuse across cell membranes from areas of higher concentration to areas of lower concentration. This diffusion is known as Starling’s forces or Starling’s equilibrium.5 The permeability of membranes and changes in hydrostatic and colloid osmotic pressure (either in the capillaries or the surrounding tissue) influence how fluid diffuses across capillaries.14 It is known that the interendothelial gaps open when total tissue pressure is low and close when total pressure is high.14 Therefore, it is plausible that creating a locally negative pressure gradient in the lymphatic system could entice fluids to flow from the tissues (the area with a higher pressure gradient) into the lymphatic system (the area with a lower pressure gradient). The authors speculate that simultaneously massaging these areas of increased lymphatic structures (referred to as pump points) creates a negative pressure gradient, although there is currently no supporting literature for this speculation.
Low-stretch arm and/or finger bandages are applied to an edematous limb if after two MEM treatment sessions, the edema has not decreased significantly, refills shortly after treatment, or induration (hardness of tissue) remains. Low-stretch bandages look like an Ace bandage in color and thickness but are 100% cotton and, because of the weave, have only a 20% stretch factor. Because these bandages have little stretch, they provide a compressive counterforce to an expanding muscle belly. This counterforce causes a change in interstitial pressure, which stimulates the lymphatics to absorb fluid and other materials from the interstitium. When the muscle belly relaxes, the bandages only contract 20% and thus do not give a strong force that could collapse the initial lymphatics. Light compression is obtained from the layering of multiple bandages, not from the applied stretch. The MEM bandaging system usually consists of three layers. The first two layers are stockinette and cast padding. The third layer consists of one or two short stretch bandages placed in a gradient pattern, thereby providing greater compression distally. For bandage use guidelines, see the “Frequently Asked Questions” section.
Leduc and colleagues26,43 found that the combination of multilayered bandages on the forearm combined with exercise increased protein absorption by the lymphatic capillaries. Additionally, external pressure39 and temperature28 also facilitate lymph movement because it has been shown that the flow of lymph within the vessel is best between 22°C and 41°C (71.6°F and 105°F) and sharply slows down or stops below and above those temperatures.28 Thus, bandaging can influence protein absorption by providing light compression and perhaps by providing a buildup of body heat that is within the mid-range of ideal temperature to mobilize lymph.
The precautions/contraindications related to MEM are those universal to most massage programs and specific to the impact of moving large volumes of fluid through the system (Box 65-1). A physician should always be consulted if the therapist is concerned about the patient’s present or past cardiac or pulmonary status. For instance, if there is a significant volumetric difference between the two extremities, a therapist should inform the physician that there is the potential to move that much fluid through the heart and lungs. The physician should be asked whether this would compromise the patient’s cardiac status.
BOX 65-1 Manual Edema Mobilization Contraindications and Precautions
CONTRAINDICATIONS AND PRECAUTIONS TO CONSIDER
Do not do MEM
• If an infection is present because there is the potential to spread the infection
• Over areas of inflammation because of the likelihood of increasing the inflammation and pain. In this case, do MEM proximal to the inflammation to decrease congested fluid, thus decreasing congestion and pain.
• If there is a blood clot or hematoma in the area because there is a chance of activating or moving the clot.
• If the patient currently has congestive heart failure, severe cardiac problems, renal failure, severe kidney disease, liver disease, or pulmonary problems because there is the potential to overload these already failing systems. These people usually have low protein edemas, and MEM is for high protein edemas.
• If there is active cancer; a controversial theory notes the opportunity to spread the cancer. Absolutely never do MEM if the cancer is not being medically treated and always seek a physician’s advice.
• If the patient has primary lymphedema (congenital) or secondary lymphedema (i.e., post-mastectomy). To successfully treat this condition, it involves knowing how to reroute lymph to other parts of the body and how to perform specific treatment techniques that are beyond the scope of this chapter.
Be aware that with MEM, there is the potential to:
• Increase the feeling of morning sickness during the first trisemester of pregnancy because of increased movement of fluid throughout body
• Alter blood sugar levels in someone with diabetes
• Lower blood pressure further in patient with preexisting low blood pressure
The results of using MEM can be seen in the following case examples. The first case example, Mrs. M.G., shows the results of using MEM and low-stretch bandaging exclusively at the beginning of treatment, with progression to ROM and modalities once edema reduction started. The second example, Matthew, demonstrates the effect MEM can have in one session with early subacute edema.
M.G. is a 75-year-old woman who was referred to hand therapy 8 weeks after a left (L) hand infection that involved the thumb, thenar eminence, and first dorsal interosseous space (Fig. 65-10). The infection was resolved after a series of antibiotics. The exact cause of the infection was never determined but was thought to be related to a (L) thumb nail bed infection. An evaluation revealed severe hand inflammation, severe swelling in the left hand thenar eminence and over the dorsum of the hand, a “spongy pitting” dorsal hand and digit edema, shiny taut tissue on the dorsum of the hand and digits, a visual analog scale (VAS) pain rating of 8 out of 10, active flexion ranging 0 to 20 degrees for each joint of each digit, full active extension to 0 of all digits, pain prohibiting passive flexion, no functional use of the hand, and sensory limitations ranging from decreased to loss of protective sensation throughout the entire hand. The hand pain prevented Mrs. M.G. from sleeping throughout the night for 8 weeks. Left and right comparison girth measurements were taken at the elbow, palm, wrist, and proximal phalanx of each digit. These girth measurements were totaled for each upper extremity from the elbow to the fingertips. The total girth measurement for the left was 102.5 cm compared with 89 cm on the right, a 13.5-cm girth difference.

Figure 65-10 Mrs. M.G. before manual edema mobilization and therapy.(Courtesy Janine Hareau, PhD, PT, OT.)
The initial treatment consisted of performing MEM proximal to the inflammation and using low-stretch bandaging to the forearm and hand. After 2 consecutive days of treatment, total edema from the elbow to fingertips decreased 3.5 cm. Mrs. M.G. had no pain and was able to sleep throughout the night for the first time in 2 months. One month later, the total left lower arm and hand girth was only 3 cm greater than that of the right. In other words, Mrs. M.G. lost 10.5 cm of girth from the initial 13.5-cm girth difference between the two extremities. After the 2 days that it took to reduce the initial edema, an exercise program was initiated, which included isometric exercises and tendon gliding for 1 week. This exercise program promoted joint/tendon motion without causing tissue inflammation. Beginning the second week of treatment, a progressive exercise program was started that included electrical stimulation and the use of a continuous passive motion machine. At the end of 2 months of treatment, sensation throughout the hand had improved, ranging from normal light touch to decreased light touch, and the patient had complete active flexion and extension ROM of all digits (Fig. 65-11). At the 1-year follow-up, reevaluation revealed that the left hand girth was 1 cm less than that of the right hand.
Matthew is a 42-year old construction worker whose right middle finger was caught in an up and down moving cylinder device. As a result of the injury, he sustained a traumatic boutonniere deformity. One and a half weeks later he sought hand therapy. The evaluation revealed a total circumference girth difference between the right and left middle fingers of 3 cm. Active and passive proximal interphalangeal (PIP) ROM was 30/90 degrees. Passive PIP extension beyond −30 degrees was too painful to pursue. Active distal interphalangeal (DIP) range with PIP blocked into extension was 0/20 degrees.
After the evaluation, a 20-minute MEM program was performed by the therapist. This program consisted of diaphragmatic breathing; massage of the supraclavicular areas (terminus); trunk exercise; bilateral axilla massage; MEM clear and flow massage to the uninvolved axilla across the chest; pump points 1, 3, 4, and 5 followed by flow massage and exercise; two specific MEM techniques to the hand/finger; MEM flow massage to the uninvolved axilla; and fisting above the head. There was a visible and measurable 50% decrease in edema in the right middle finger when measurements were taken at the end of this first treatment. The same evaluation revealed that the PIP could be passively extended to 5 degrees from full extension, causing a VAS pain rating of 2 on a scale of 10, and active PIP ROM improved to 10/100. A custom simple safety pin type orthosis enabling functional use while doing construction work was fabricated for the patient. The home program consisted of two appropriate ROM exercises for the PIP and DIP plus a very brief 5-minute MEM program to do twice daily (Fig. 65-12).
The patient cancelled a follow-up appointment the next week because of his work schedule. He stated that he did not think that he needed to reschedule because swelling was “all down in his finger.” Also, he informed the therapist that he could fully bend and straighten the finger at all joints. He did experience moderate finger pain at the end of a work day, but this was relieved by doing the brief MEM home program and wearing the orthosis at night. The patient was informed that he should continue wearing the orthosis 7 days per week, 24 hours per day for at least 2 more weeks.
Three weeks later, the therapist ran into the patient in the grocery store. The patient showed her that he had full ROM of the right middle finger, no pain, and only did the brief MEM program and/or wore the orthosis when the finger swelled or to reduce pain from “overstretching” at work tasks.
Who are candidates for MEM? Patients who have stagnant high-protein edema are candidates for MEM. This includes patients who have edema beyond the normal acute phase that is not reducing with the usual acute-phase treatment methods (see Table 65-1). MEM can also be used to prevent edema and/or reduce the amount of edema for the trauma or postsurgical hand problems that are beyond the acute phase, meaning those whose edema is barely visible or not visible at all, but are being seen for other treatment needs such as ROM. The lymphatics have a safety valve function5,28 and can take on considerably more than the usual 10% of excess interstitial fluid before they become overloaded and edema becomes visible. From this it can be theorized, but research is needed, that doing MEM on the trunk and upper arm and performing pump point stimulation at the beginning of one or two sessions can decongest lymphatics that are reaching maximum capacity, thereby preventing a lymphatic overload that would likely have resulted in edema. Clinically, it is commonly seen that those patients with minimal or nonvisible edema will say “my hand feels lighter” or “my fingers move easier” after a MEM treatment.
Table 65-4 Activating Lymph Uptake Review
Would MEM be effective in reducing edema in the acute stage? During the acute stage (72 hours or less), fibrin plugs prevent lymphatic uptake by the initial lymphatics surrounding a wound.44 Therefore, if the edema is acute, uptake near the wound may not occur. However, at a minimum, MEM would stimulate and clear the proximal lymphatic pathways, and this might be helpful. In a study by Hutzschenreuter and Brummer,45 tissue on two groups of sheep was lacerated and sutured. One group was administered MLD from day 1 postoperatively, whereas the control group received no MLD. There was no difference in edema reduction in either group until the end of the first week. Then, in the following weeks, the MLD group had a significantly greater increase in fluid movement and edema reduction than the control group. Thus lymphatic stimulation had no effect on reducing edema in the acute inflammation stage (less than 72 hours), but did affect the edema reduction within a week. This study provides further insight into the effectiveness of lymphatic massage performed in the acute stage of wound healing.
When should MEM begin? Usually 1 week after surgery/trauma as long as there is no infection, the sutures have been removed (so dehiscing of healing tissue does not occur), and there are no other contraindications. Because the lymphatic system can become congested before edema is visible, performing MEM on the trunk and stimulating pump points 1 and 3 one week after surgery/trauma might decongest the lymphatic system proximally and thus lessen or prevent future edema.
How can a therapist determine whether edema is high in protein? An edema that is “spongy” and has slow tissue rebound when indented is often a high-plasma protein edema. The best way to determine the type of edema is to look at the etiology and determine whether there are coexisting edemas (e.g., cardiac edema).
Do I always begin MEM at the trunk, even when there is just edema in the finger (e.g., from a finger fracture)? Yes, because when there is visible or barely visible edema, lymph congestion can often be palpated as proximal as the posterior deltoid. This edema needs to be moved out first so that the more distal edema can move proximally. Sometimes this has to be done only once (i.e., the first treatment session). The next session would begin with diaphragmatic breathing, proximal trunk exercises, pump point 1, and axillary and cubital node massage, and then MEM would begin at the volar forearm.
What are pump points? This is a term coined to describe a massage technique that appears, in the authors’ opinion, to get a faster flow of congested lymph out of an area.18,42,46,47 Refer to concept 4 and Tables 65-2 and 65-3 for more information related to pump points.
For a geriatric patient with multiple diagnoses, should I perform MEM on the entire extremity in one session? No, you could easily overload the cardiopulmonary system. Often this edema moves out of an area quickly because it is a complex edema. Thus, treating only one segment the first time and observing whether any complications occur are recommended. Complications to look for would be signs of congestive heart failure, decreased blood pressure, and decreased blood sugar level for the diabetic patient. If none occurs, the therapist may decide to gradually include more segments in further treatment. A MEM course is needed to teach how to safely work with this population and how to modify other aspects of MEM.
How long should I do MEM? The first session may take 20 minutes and consist of MEM in the trunk (diaphragmatic breathing, trunk exercise, bilateral axillary massage, clear and flow massage across the upper trunk axilla to axilla pathway, trunk exercise, diaphragmatic breathing) and then pump point 1 with flow back to the uninvolved axilla plus shoulder and trunk exercises. Usually hand edema will begin to reduce or soften because of this proximal work. The patient is taught a home program to do several times daily. At the next session, MEM might be performed on the entire extremity, and the patient is instructed in an expanded home therapy program. Subsequent treatments might involve the therapist doing MEM on the trunk and pump points and then beginning extensive MEM just proximal to the edema. Care must be taken not to add treatment techniques that could cause reinflammation of tissue (e.g., an overly aggressive strengthening program). A Kinesio taping program is an excellent addition to MEM to have more continuous lymphatic stimulation as the patient performs routine daily tasks.
When are low-stretch bandages used? After two or three MEM sessions, bandages might be advised if (1) tissue remains indurated, (2) edema recurs because of the presence of plasma proteins, (3) tissue has lost its elasticity from being stretched for a prolonged period and thus refills with tissue fluid, or (4) there is decreased motor function.
What are chip bags and what is their function? These are items described by Casley-Smith and Casley-Smith.14 Chip bags can consist of pieces of 1-inch foam of various densities that are enclosed in a stockinette bag and placed on the skin over indurated areas of edema. The chip bags can be secured with a low-stretch bandage or can be worn under an elastic glove. This gives light stimulating compression and retains body heat, resulting in further tissue softening.
Can one of the various types of elastic/cotton stockinette tubes be a substitute for a low-stretch bandage? Yes, for minimal edema. The tube does not have gradient pressure. It must not be too tight, which would result in collapsing the initial lymphatics. A clinical guide regarding tightness is that the therapist should be able to get his or her whole hand under the proximal end of the elastic/cotton stockinette tube with a comfortable, not excessive, compression felt on his or her hand. The distal end of the tube might have to be tapered with stitching to accommodate the shape of the arm. Two methods have been used clinically to prevent rolling down of the tube on the extremity that could cause more edema distally. A 2-inch wide piece of foam strapping material is lightly placed around the proximal end of the tube 1 inch below the top of the tube. The proximal end of the tube material is then overlapped (cuffed) on to the foam strap. This helps to secure the tube from rolling proximally down the arm. The same thing is also possible using a 3- to 4-inch wide piece of Coban bandage that the therapist completely stretches all the elastic out of and lightly places around the arm at the proximal end of the tube bandage and then folds the tube end over the top of the Coban, as described previously.
If the patient previously had lymphedema from a mastectomy and then has a hand injury and/or surgery on the same side and the edema gets worse, can I effectively use MEM? No, MEM does not teach rerouting around areas of node removal or around fibrotic radiated tissue. The therapist must seek the help of a person adequately trained in MLT techniques.
How is rerouting around scar done? The goal is to reroute congested lymph around areas of tissue damage into adjacent functioning lymph capillaries (lymphatics). The therapist begins clear and flow massage proximal to the incision or congested site. Then the therapist creates a vacuum, drawing the congested lymph around the scar by having her proximal hand form Us near where the lymph is to be directed toward a node, and the other hand is just proximal the edematous area performing flowing Us toward the proximal hand.
If current edema control techniques are working, why change to MEM? The challenge is to reexamine the success of these techniques in light of what stimulates the lymphatics. Fisting above the head is often prescribed to reduce edema.48 A closer examination of this technique reveals motion beginning proximal to the trunk and proceeding distally as the scapula rotates along with stretching of the trunk and arm muscles and ending with distal active muscle contraction from fisting as the arm is extended above the head. This technique follows the principles that stimulate lymphatic flow. Are elastic gloves effective because they are loose fitting, giving light compression and thus stimulating the lymphatics? Is use of the pneumatic pump effective because the pressure is set at 35 mm Hg or less rather than diastolic pressure, which exceeds the pressure needed to collapse the lymphatics and prevent lymph uptake? Is the retrograde massage effective because it is being used on a low-protein edema such as early stroke edema or on very early stages of subacute edema before stagnation of lymph occurs? Is the use of sponge-type finger wraps effective to soften hard edema and scars because they are providing prolonged light compression and neutral warmth? Possibly all of these techniques would make the more distal edema reduce faster if a couple of sessions included MEM on the trunk, upper arm, and pump points because of the decongesting effect on the proximal nodes and lymphatics.
What is the number 1 mistake therapists make when performing the MEM technique? Therapists forget that edema is congested significantly proximal to the visible edema and so do not start the MEM at the uninvolved axilla and clear and flow massage across the chest to the uninvolved axilla. Starting MEM at a set of nodes just proximal to the visible edema will just congest the lymph more proximally and it will return. A pathway must be created so that the more distal edema can move proximally. A useful analogy is that of a clogged sink filled with nondraining water (edema). When the clog in the pipe (proximal congestion) is eliminated, the water (edema) drains out of the sink.
There are four key factors related to subacute and chronic edema that validate the use of lymphatic therapies on people with orthopedic subacute and chronic edema. First, it has been shown in an animal model that if excess plasma proteins remain in the interstitium, they can cause chronic inflammation,32 possibly leading to fibrosis.32 Second, orthopedic subacute and chronic edemas are high-protein types of edema with increased plasma proteins in the interstitium.14,44 Third, it is well documented that the role of the lymphatic system is to remove these excess plasma proteins and other lymph constituents from the interstitium.5,14,21,30,33 Fourth, existing research from the lymphedema literature validates techniques that effectively stimulate lymphatic uptake for people with lymphedema, thereby diminishing the interstitial plasma proteins.5,14,25,49,50 These four key factors provide the foundation for MEM, which is a technique that adapts lymphatic drainage principles for application to the orthopedic population. The clinical results have been very positive, and MEM opens a door to another facet of orthopedic edema reduction that needs further research and clinical publications.
1. Watson-Jones R. Fractures and Other Bone and Joint Injuries. 2nd ed Baltimore: Williams & Wilkins; 1941.
2. Griffin J, Newsome L, Stralka S, et al. Reduction of chronic posttraumatic hand edema: a comparison of high voltage pulsed current, intermittent pneumatic compression, and placebo treatments. Phys Ther. 1990;70:279.
3. Miles W. Soft tissue trauma. Hand Clin. 1986;2:33–43.
4. Sorenson MK. The edematous hand. Phys Ther. 1989;69:1059–1065.
5. Chikly B. Silent Waves: Theory and Practice of Lymph Drainage Therapy. 2nd ed Scottsdale AZ: International Health and Healing; 2002.
6. Artzberger S. Edema control: new perspectives. Phys Disabil Special Interest Section Quarterly. March 1997;20:1–4.
7. Artzberger S. Manual Edema Mobilization for the Hand and Arm. Portland, ME: Symposium conducted through Hand Therapy Consulting Services; 2000.
8. Shields JW. High points in the history of lymphology 1602-2001. Lymphology. 2001;34:51–68.
9. Shields JW. The evolution of circulation, homeostasis and immunity: an historical account from a lymphologist/hematologist viewpoint. Lymphology. 2005;38:34–41.
10. Olszewski W. Continuing discovery of the lymphatic system in the twenty-first century: a brief overview of the past. Lymphology. 2002;35:99–104.
11. Földi M. Lymphology in the second millennium. Lymphology. 2001;34:12–21.
12. Kasseroller R. Compendium of Dr. Vodder’s Manual Lymph Drainage. Heidelberg: Haug; 1998.
13. Andersen L, Hoijris I, Erlandsen M, Andersen J. Treatment of breast cancer-related lymphedema with or without manual lymphatic drainage. Acta Oncologica. 2002;39(3):399–405.
14. Casley-Smith JR, Casley-Smith JR. Modern Treatment for Lymphoedema. 5th ed Adelaide, Australia: The Lymphoedema Association of Australia; 1997.
15. Priganc V, Ito M. Changes in edema, pain, or range of motion following manual edema mobilization: a single-case design study. J Hand Ther. 2008;21:326–335.
16. Howard S, Krishnagiri S. The use of manual edema mobilization for the reduction of persistent edema in the upper limb. J Hand Ther. 2001;14:291–301.
17. Harden NR, Swan M, King A, et al. Treatment of complex regional pain syndrome: functional restoration. Clin J Pain. 2006;22(5):420–424.
18. Artzberger S. Manual edema mobilization: treatment for edema in the subacute hand. In: Mackin EJ, ed., et al. Rehabilitation of the Hand and Upper Extremity. 5th ed St. Louis: Mosby; 2002:899–913.
19. Casley-Smith JR, Casley-Smith JR. The pathophysiology of lymphoedema and the action of benzo-pyrones in reducing it. Lymphology. 1988;21:190.
20. Villeco J, Mackin E, Hunter J. Edema: therapist’s management. In: Mackin EJ, ed., et al. Rehabilitation of the Hand and Upper Extremity. 5th ed St. Louis: Mosby; 2002:183–193.
21. Guyton A, Hall J. Textbook of Medical Physiology. 9th ed Philadelphia: WB Saunders; 2000.
22. Reed B, Zarro V. Inflammation and repair and the use of thermal agents. In: Michlovitz S, ed. Thermal Agents in Rehabilitation. 2nd ed Philadelphia: F.A. Davis; 1990:3–17.
23. Reed B. Effect of high voltage pulsed electrical stimulation on microvascular permeability to plasma proteins. Phys Ther. 1988;68(4):491–495.
24. Mortimer P. The pathophysiology of lymphedema. Cancer. 1998;83(Suppl 1):2798–2801.
25. Foldi E, Foldi M, Clodius M. The lymphedema chaos: a lancet. Ann Plast Surg. 1989;22:505–515.
26. Leduc O, Leduc A, Bourgeois P, et al. The physical treatment of upper limb edema. Cancer. 1998;15(83):2835–2839.
27. Casley-Smith JR, Gaffney RM. Excess plasma proteins as a cause of chronic inflammation and lymphedema. quantitative electron microscopy. J Pathol. 1981;133:243–272.
28. Kurz I. 4th ed Textbook of Dr. Vodder’s Manual Lymph Drainage. vol 2. Heidelberg: Haug; 1997.
29. Hole JW. Human Anatomy and Physiology. 4th ed Dubuque, Iowa: William C Brown; 1987.
30. Weissleder H, Schuchhardt C. Lymphedema Diagnosis and Therapy. 2nd ed Bonn: Kagerer Kommunikation; 1997.
31. Földi M, Földi E. Lymphoedema Methods of Treatment and Control: A Guide for Patients and Therapist. Victoria, Australia: Lymphoedema Association of Victoria; 1991.
32. Casley-Smith JR. Modern treatment of lymphoedema. Mod Med. May 1992.70–84.
33. Kubik S. Anatomy of the lymphatic system. In: Foldi M, Foldi E, Kubik S, eds. Textbook of Lymphology for Physicians and Lymphedema Therapists. 1st ed Munich, Germany: Elsevier; 2003:2–164.
34. Huntley N. Cardiac and pulmonary disease. In: Trombly C, Radomski M, eds. Occupational Therapy for Physical Dysfunction. 5th ed Baltimore, MD: Lippincott, Williams, & Wilkins; 2002:1071–1089.
35. Matthews M. Cardiac and pulmonary diseases. In: Pedretti L, Early M, eds. Occupational Therapy: Practice Skills for Physical Dysfunction. 5th ed St. Louis: MO, Mosby; 2001:966–980.
36. Moseley A, Piller N, Carati C. The effect of gentle arm exercise and deep breathing on secondary arm lymphedema. Lymphology. 2005;38:136–145.
37. Zuther J. Lymphedema Management: The Comprehensive Guide for Practitioners. New York: Thieme Medical; 2005.
38. Xujian S. Effect of massage and temperature on the permeability of initial lymphatics. Lymphology. 1990;23:48–50.
39. Miller GE, Seale J. Lymphatic clearance during compressive loading. Lymphology. 1981;14:161–166.
40. Eliska O, Eliskova M. Are peripheral lymphatics damaged by high pressure manual massage?. Lymphology. 1995;28(21):21–30.
41. Zuther J. Lymphedema Management: the Comprehensive Guide for Practitioners. New York: Thieme Medical; 2005.
42. Artzberger S, Rodrick J. Manual edema mobilization: a new concept in sub-acute hand edema reduction. Isr J Occup Ther. 2002;11(2):E37–E63.
43. Leduc O, Peeters A, Bourgeois P. Bandages: scintigraphic demonstration of its efficacy on colloidal protein reabsorption during muscle activity. Progress in Lymphology XII, Excerpta Med, Int Cong Ser. 1990;887:421–423.
44. Kloth L, Miller K. The inflammatory response to wounding. In: Kloth L, McCulloch J, Feddar J, eds. Wound Healing: Alternatives in Management. Philadelphia: J.F.A. Davis; 1990:1–12.
45. Hutzschenreuter P, Brummer H. Die manuelle lympdrainage bei der wundheilung mit decollement. Lymphologica. 1989;97:100.
46. Artzberger S. A critical analysis of edema control techniques. Phys Disabil Special Interest Section Quarterly. June 2005;28(2):1–4.
47. Artzberger S. Edema reduction techniques: a biologic rationale for selection. In: Cooper C, ed. Fundamentals of Hand Therapy: Clinical Reasoning and Treatment Guidelines for Common Diagnoses of the Upper Extremity. St Louis: Elsevier; 2006:36–52.
48. Hunter J, Mackin E. Edema techniques of evaluation and management. 4th edHunter J, Mackin E, Callahan A, eds. Rehabilitation of the Hand: Surgery and Therapy.vol 1. St Louis: Mosby; 1995.
49. Casley-Smith JR, Foldi M, Ryan TJ, et al. Lymphedema summary of the 10th international congress of lymphology working group discussions and recommendations. Lymphology. 1985;10:175–182.
50. Mondry T, Riffenburgh R, Johnston P. Prospetive trial of complex decongestive therapy for upper extremity lymphedema after breast cancer therapy. Cancer J. 2004;10(1):42–48.
51. Bryant WM. Wound healing. Clin Symp. 1977;29:1.
52. Crowley L. Introduction to Human Disease. 3rd ed Boston: Jones and Bartlett; 1992.
53. Olszewski W. On the pathomechanism of development of postsurgical lymphedema. Lymphology. 1973;6:35–38.
54. Vasudevan S, Melvin J. Upper extremity edema control: rationale of treatment techniques. Am J Occup Ther. 1979;33:520–526.
55. Foldi E. The treatment of lymphedema. Cancer. 1998;83(suppl 1):2833–2834.
56. Szuba A, Rockson S. Lymphedema: classification, diagnosis and therapy. Vas Med. 1998;3:145.
57. Pecking A, Cluzan R, Desprez-Curely JP. Indirect lymphoscintigraphy in patients with limb edema. Progress in Lymphology 1985; Proceedings of the Ninth International Congress of Lymphology: 201-206.
Sandra M. Artzberger is the author of the Lymphedema and Manual Edema Mobilization Kit (Visual Health Information, Tacoma, Washington) and receives compensation from kits sold.