Wrist and hand
An intricate interaction of numerous structures in the wrist and hand is necessary to produce the remarkable dexterity and precision that characterizes this joint complex.15 The entire upper limb is apparently subservient to the hand in its use as a tactile organ, a means of expression, and a weapon. The study of the hand is inseparable from that of the wrist and the forearm, which function as a single physiologic unit, with the wrist being the key joint.3 The wrist serves as a flexible spacer between the forearm and hand and is critical in setting the length-tension relationship for the extrinsic finger muscles. By far the most important musculoskeletal function of the hand is its ability to grasp objects. However the hand is also an important sensory organ (kinesthetic) and helps to express emotion though gestures, touch, and art. Because of it biomechanical complexity, the function of the hand involves a disproportionately large region of the cortex of the brain. Therefore, dysfunction of the hand can create equally disproportionate disabilities. The hand is the main manipulative organ of the body, performing many different types of functions, and it should not be overlooked in the evaluation for dysfunction.
Functional anatomy
Osseous Structures
Interestingly, although the ulna plays a highly significant role in the function of the elbow, it is secondary in the wrist, whereas the radius, having a secondary role in the elbow, has a dominant part in the wrist. The radius flares to become much larger at the distal end, terminating with a lateral extension, called the radial styloid process. The distal end of the ulna also ends in a styloid process, but it is much smaller in comparison with the radial styloid. The distal aspects of the radius and ulna form an articulation with the proximal row of carpal bones directly in the radius and indirectly via an intracapsular disc in the ulna. The eight carpal bones that make up the wrist are arranged in two rows that greatly enhance the hand’s mobility. The proximal row consists of the scaphoid, lunate, triquetrum, and pisiform (in order from medial to lateral). The pisiform overlies the triquetrum, which forms an articulation with the proximal ulna via the interarticular disc. The scaphoid and lunate articulate directly with the radius. The distal row of carpals consists of the trapezium, trapezoid, capitate, and hamate (in order from lateral to medial). The proximal and distal rows of carpal bones collectively form an intercarpal joint, although some movement also occurs between the individual carpal bones (Figure 6-102).
The base of each of the five metacarpals articulates with the distal row of carpals. Five proximal phalanges articulate with each of the metacarpals, followed by a middle and distal phalanx for each of the fingers and a distal phalanx for the thumb.
Ligamentous Structures
The numerous ligaments of the wrist, many of which are unnamed, are not all separate entities. They form a crisscross pattern of connections between the radius and ulna to the carpals, between the carpals, from the carpals to the metacarpals, and between the metacarpals (Figure 6-103). The volar radiocarpal and radioulnar carpal ligaments strengthen the joint capsule and wrist anteriorly, while the dorsal radiocarpal ligament provides support posteriorly (Figure 6-104). Radial collateral and ulnar collateral ligaments stabilize the wrist laterally and medially, respectively. Collateral ligaments also support the MP and the interphalangeal joints (Figure 6-105).
Musculature
Extrinsic and intrinsic muscles function for the wrist and hand (Table 6-10). The wrist flexors and extensors are located in the forearm, attached to the epicondyles of the humerus. As the muscles head distally, their tendons are enclosed in sheaths that offer a smooth environment for sliding. Intrinsic muscles include the interosseous and lumbricales muscles, as well as those responsible for the movements of the thumb and little finger. Six passageways transport the extensor tendons through fibro-osseous tunnels. Fibrous bands running from the retinaculum to the carpal bones form the tunnels (Figure 6-106). The flexor retinaculum spans the scaphoid, trapezium, hamate, and pisiform. It forms a tunnel out of the carpal arch to allow passage of the median nerve and the flexor tendons (Figure 6-107).
TABLE 6-10 Actions of the Muscles of the Wrist and Hand
| Actions | Muscles |
|---|---|
| Wrist flexion | Flexor carpi radialis, abductor pollicis longus, palmaris longus, flexor pollicis longus, flexor carpi ulnaris, and flexor digitorum superficialis and profundus |
| Wrist extension | Extensor carpi radialis, extensor digitorum, extensor carpi ulnaris, and extensor pollicis longus |
| Wrist adduction (ulnar deviation) | Extensor carpi ulnaris and flexor carpi ulnaris |
| Wrist abduction (radial deviation) | Extensor carpi radialis, abductor pollicis longus, and extensor pollicis longus and brevis |
| Finger flexion | Flexor digitorum superficialis and profundus |
| Finger extension | Extensor digitorum, extensor digiti minimi, and extensor indicis |
| Finger abduction | Interosseous muscles |
Biomechanics
The complex movements of the wrist are accomplished by the distal radioulnar joint, the radiocarpal joint, and the midcarpal joint. The radiocarpal and midcarpal joints produce the motion at the wrist joint. Wrist flexion and extension, as well as radial and ulnar deviation, are thought to occur around an axis of movement that passes through the capitate (Figure 6-108). However, the multiplicity of wrist articulations and the complexity of joint motion make it difficult to calculate the precise instantaneous axis of motion.12 The close-packed position for the wrist is full extension (Table 6-11). The wrist can undergo approximately 160 degrees of flexion and extension, with extension being slightly greater. Radial and ulnar deviation are possible to 60 degrees, and ulnar deviation is almost twice as great as radial deviation (Figure 6-109). Radial deviation is limited by contact of the scaphoid against the radial styloid process. ROMs for the wrist and hand are listed in Table 6-12.
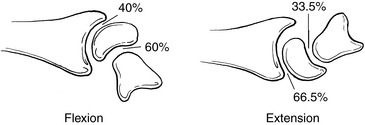
Figure 6-108 Most wrist flexion occurs at the intercarpal joint, and most wrist extension occurs in the radiocarpal joint.
TABLE 6-11 Close-Packed and Loose-Packed (Rest) Positions for the Wrist and Hand Joints
| Closed-Packed Position | Loose-Packed Position | |
|---|---|---|
| Wrist | Full dorsiflexion | Palmar flexion with slight ulnar deviation |
| Hand | Full extension | Flexion with slight ulnar deviation |
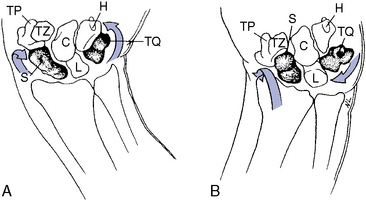
Figure 6-109 Dorsal view of the right wrist. A, With ulnar deviation, some extension of proximal carpals occurs. B, With radial deviation, some flexion of the proximal carpal occurs. C, Capitate; H, hamate; L, lunate; S, scaphoid; TP, trapezium; TQ, triquetrum; TZ, trapezoid.
TABLE 6-12 Arthrokinematic and Osteokinematic Movements of the Wrist and Hand Joints
| Osteokinematic Movements | Degrees | Arthrokinematic Movements |
|---|---|---|
| Wrist flexion | 80 | Roll and glide |
| Wrist extension | 70 | Roll and glide |
| Ulnar deviation | 30 | Roll and glide |
| Radial deviation | 20 | Roll and glide |
| MCP flexion | 90 | Roll and glide |
| MCP extension | 30–45 | Roll and glide |
| PIP flexion | 100 | Roll and glide |
| PIP extension | 0 | Roll and glide |
| DIP flexion | 90 | Roll and glide |
| DIP extension | 10 | Roll and glide |
| Finger abduction | 20 | Roll and glide |
DIP, Distal interphalangeal joint; MCP, metacarpophalangeal joint; PIP, proximal interphalangeal joint.
With dorsiflexion of the wrist, a supinatory rotation of the carpal bones also occurs, which is mostly a result of the scaphoid moving more with respect to the radius while the lunate and triquetrum relate to the ulna. Furthermore, when moving from flexion to dorsiflexion, the distal row of carpals becomes close-packed with respect to the scaphoid first. This results in the scaphoid moving with the distal row into dorsiflexion, necessitating movement between the scaphoid and lunate as full dorsiflexion is approached. With extension of the wrist, the proximal row of carpals rolls and glides anteriorly with respect to the radius and ulna, and the distal row of carpals moves similarly with respect to the proximal row of carpals. The converse is true of wrist flexion; the proximal row moves posteriorly relative to the radius and ulna as the proximal row moves posteriorly relative to the proximal row of carpals.
Radial and ulnar deviation involve rotary movements between the proximal row of carpals and the radius, as well as between the proximal row and distal row of carpals. Moreover, during radial deviation, the proximal row combines pronation, flexion, and ulnar glide movements with respect to the radius as the distal row combines supination, extension, and ulnar glide movements with respect to the proximal row. Ulnar deviation has the opposite movements.3,16
The hand must be able to change its shape to grasp objects. Three physiologic functional arches running in different directions provide the means for the wrist and hand to conform to a position for grasping (Figure 6-110). Transversely, an arch through the carpal region corresponds to the concavity of the wrist, and distally, the metacarpal arch is formed by the metacarpal heads. Longitudinal arches are formed along each finger by the corresponding metacarpal bone and phalanges. Obliquely, arches are formed by the thumb during opposition with the other fingers. These arches allow coordinating synergistic digital flexion and opposition of the thumb and little finger.
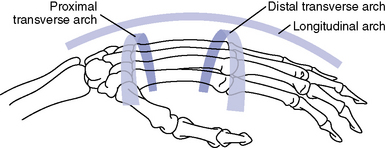
Figure 6-110 The three physiologic arches of the wrist and hand.
(Modified from Nordin M, Frankel VH: Basic biomechanics of the musculoskeletal system, ed 2, Philadelphia, 1989, Lea & Febiger.)
The wrist provides a stable base for the hand, and its position controls the length of the extrinsic muscles to the digits. The muscles stabilize the wrist, as well as provide for the fine movements of the hand, to place it in its functioning position. The positioning of the wrist has a significant influence on the strength of the fingers. For most effective action of the extrinsic muscles of the fingers, the wrist usually must move in a direction opposite the movement of the fingers.
The naturally assumed position of the hand to grasp an object, or the position from which optimal function is most likely to occur, is termed the functional position (Figure 6-111). The functional position occurs when the wrist is extended 20 degrees and the ulna is deviated 10 degrees, the fingers are flexed at all of their joints, and the thumb is in a midrange position, with the MP joint moderately flexed and the interphalangeal joints slightly flexed. Prehensile functions of the hand are unique and fundamental characteristics (Figure 6-112).
Evaluation
The wrist and hand are prone to injuries from trauma, commonly a fall on the outstretched hand. The radial side of the wrist and hand tends to take the majority of the force from such a trauma. Displacement, instability, and rotary subluxation of the scaphoid often occur, creating pain on dorsiflexion of the wrist and limited ROM. Palpable tenderness will be present over the joint space between the scaphoid and the lunate. Occasionally, the scaphoid can be felt slipping as the wrist is moved, or a painful click may be perceived. A space of more than 3 mm between the scaphoid and lunate may be seen on a closed-fist supinated radiographic view of the wrist.
Trauma to an outstretched hand that is forcefully flexed or extended may cause a fracture to the radius. A Colles fracture occurs when the wrist is in dorsiflexion and the forearm is in pronation. Local pain and tenderness to palpation and vibration are important physical findings; however, the radiograph is the most important tool for determining the presence of a fracture. Manipulative therapy to this area is then contraindicated.
Singular trauma, such as a fall, or repetitive activities may lead to a sprain of the ligaments of the wrist. Moreover, when the wrist is subjected to sudden increases in workload, such as in gripping or lifting, or racquet games that require flexion and extension of the wrist, the tendons crossing the wrist can become inflamed, resulting in tendinitis. In addition, a possible response to repeated twisting and straining is a localized nodular swelling, called a ganglion. Likely a defense mechanism, the ganglion is characterized by a fibrous outer coat that covers a thick gelatinous fluid derived from the synovium lining the tendon sheaths.
Undoubtedly, the most noted condition affecting the wrist and hand is carpal tunnel syndrome, a peripheral entrapment neuropathy involving the median nerve. The median nerve lies superficial to the flexor tendons beneath the tense transverse carpal ligament (flexor retinaculum), making the carpal tunnel just barely adequate to accommodate these structures. In the act of grasping an object, particularly with the wrist in flexion, the flexor tendons are displaced forward and can compress the nerve against the unyielding ligament. Narrowing of the carpal tunnel can occur through bony deformity after fracture, degenerative joint disease, synovial swelling of a tendon or of the wrist joint ligaments, and thickening of the transverse carpal ligament (Figure 6-113). Most often, however, no definitive local cause for nerve compression can be detected. Moreover, Upton and McComas20 has identified the possibility that peripheral nerves can be compressed at more than one spot along their course, creating “double-,” “triple-,” and “quadruple-crush” syndromes. Therefore, although the patient’s clinical picture may be defined as carpal tunnel syndrome, the nerve compression may not necessarily be at the wrist but may be at the elbow, shoulder, or neck. This syndrome occurs more often in women, with onset commonly between 40 and 50 years of age. Slight paresthesias may precede the onset of the acute symptoms for several months. Then, paroxysms of pain, paresthesia, and numbness occur in the area of the median nerve distribution. The patient is often awakened at night by numbness or pain that can be described as burning, aching, prickly, or pins-and-needles. Motor weakness of the thumb adductor or opposer may be found. The patient may describe relief from dangling the hand over the side of the bed, shaking the hand vigorously, or rubbing it.
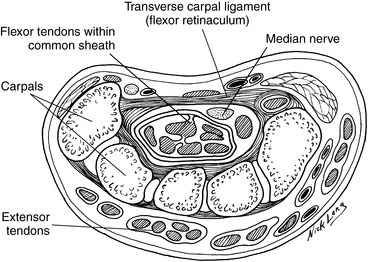
Figure 6-113 Cross-section of the wrist, showing the relationship between the carpal bones, tendons, flexor retinaculum, and median nerve.
Because the wrist structures are innervated primarily from segments C6 through C8, lesions affecting structures of similar derivation may refer pain to the wrist and vice versa. Symptoms experienced at the wrist and hand must always be suspected as possibly having a more proximal origin (Figure 6-114).
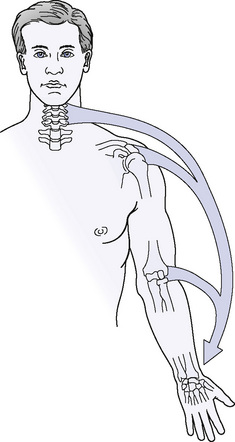
Figure 6-114 Symptoms in the hand and wrist must be suspected of having a more proximal origin.
(From Magee DJ: Orthopedic Physical Assessment, ed 5, St Louis, 2008, Sauders.)
Observe the wrist and hand for general posture and attitude. In the resting attitude of the hand, the MP and interphalangeal joints are held in a position of slight flexion. Observe the arm and hand for natural swing when the patient walks. Also, note functional activities of the hand and wrist, including the firmness of the person’s handshake, as well as temperature and moisture of the hand. The dominant hand should be determined. Sometimes this can be done by noting the hand with more developed musculature, but is most easily done simply by asking the patient.
To begin the evaluation of the wrist and hand, osseous symmetry, bony relationships, and pain production are identified through static palpation of the wrist and hand (Figure 6-115). Palpate the radius and ulna distally, identifying each of their styloid processes. Just distal to the radial styloid and in the anatomic snuffbox, the scaphoid can be palpated. Wrist flexion will facilitate the palpation of the lunate, which lies next to the scaphoid. The triquetrum and pisiform overlie one another and are just distal to the ulnar styloid. The trapezium can be identified at the base of the first metacarpal. The trapezoid lies at the base of the second metacarpal. The capitate is found between the base of the third metacarpal and the lunate. The hook of the hamate, and hence the hamate, can be found on the palmar surface, just distal and to the thumb side of the pisiform. Then palpate the metacarpals through the palm of the hand, with the fingers along the shaft of the metacarpal on the palmar surface while the thumb is over the dorsal surface. Finally, palpate the 14 phalanges (2 for the thumb and 3 for each finger).
Identify tone, texture, and tenderness changes through soft tissue palpation of the flexor and extensor tendons, the thenar eminence, and the hypothenar eminence. Determine patency of the radial and ulnar arteries (Allen test) and take a radial pulse.
Evaluate accessory joint motions for the wrist and hand articulations to determine the presence of joint dysfunction (Table 6-13). Assess A-P and P-A glide of the distal radioulnar joint with the patient supine or sitting. Grasp the distal radius with one hand and the distal ulna with the other. Apply an opposing A-P and P-A shearing stress between the radius and ulna (Figure 6-116).
TABLE 6-13 Accessory Joint Movements of the Wrist and Hand Joints
| Joint | Movement |
|---|---|
| Distal radioulnar | |
| Intercarpal | |
| Individual carpals | |
| Intermetacarpal | |
| Metacarpophalangeal and interphalangeal |
A-P, Anterior-to-posterior; L-M, lateral-to-medial; M-L, medial-to-lateral; P-A, posterior- to-anterior.
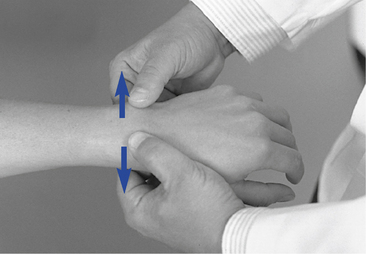
 Figure 6-116 Assessment of anterior-to-posterior and posterior-to-anterior glide of the distal left radioulnar joint.
Figure 6-116 Assessment of anterior-to-posterior and posterior-to-anterior glide of the distal left radioulnar joint.
Conduct M-L compression of the distal radioulnar joint with the patient supine or sitting, and use both hands to encircle the distal radius and ulna. Use both hands to apply an M-L compression stress to the distal radius and ulna (Figure 6-117).
In evaluating long-axis distraction of the intercarpal joint, the patient can be seated or supine. Grasp the distal forearm with one hand and the distal wrist with the other. While stabilizing the forearm, distract the wrist in the long axis (Figure 6-118).
Perform M-L tilt and glide of the intercarpal joints with the patient seated and the affected arm raised in forward flexion. Stand on the affected side, facing the lateral aspect of the arm. Grasp the distal radius and ulna with your proximal hand while grasping the patient’s distal wrist with your distal hand. Use both hands to create opposing forces, creating a shearing stress (M-L glide) (Figure 6-119) and radial and ulnar deviation stress (M-L tilt) (Figure 6-120).
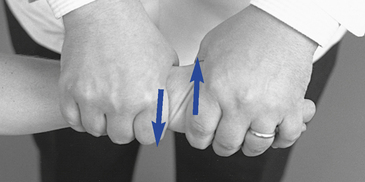
 Figure 6-119 Assessment of medial-to-lateral and lateral-to-medial glide of the left intercarpal joint.
Figure 6-119 Assessment of medial-to-lateral and lateral-to-medial glide of the left intercarpal joint.
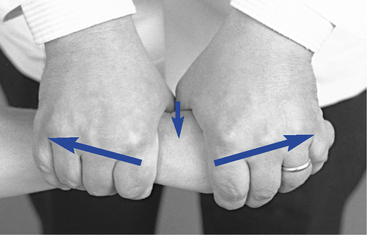
 Figure 6-120 Assessment of medial-to-lateral and lateral-to-medial tilt of the left intercarpal joint.
Figure 6-120 Assessment of medial-to-lateral and lateral-to-medial tilt of the left intercarpal joint.
Assess A-P and P-A glide of the intercarpal joint, with the patient seated and arm raised in forward flexion. Stand on the affected side. Grasp the distal radius and ulna with your proximal hand while grasping the patient’s distal wrist with your distal hand. Using both hands to create opposing forces, stress the intercarpal joints in an A-P and P-A glide, looking for a springing joint play movement (Figure 6-121).
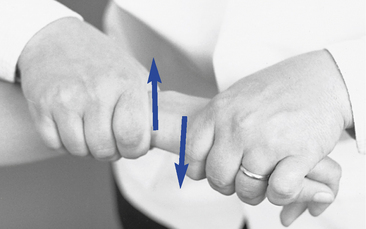
 Figure 6-121 Assessment of anterior-to-posterior and posterior-to-anterior glide of the left intercarpal joint.
Figure 6-121 Assessment of anterior-to-posterior and posterior-to-anterior glide of the left intercarpal joint.
Assess A-P and P-A glide of the individual carpal bones with the patient seated and the affected arm raised in forward flexion. Stand and face the patient. Use your thumb and index or middle fingers to contact the anterior and posterior surfaces of the carpal bone to be evaluated while using your other hand to stabilize the rest of the wrist. Apply an A-P and P-A stress to each individual carpal bone, looking for a springing joint play movement (Figure 6-122, A and B).
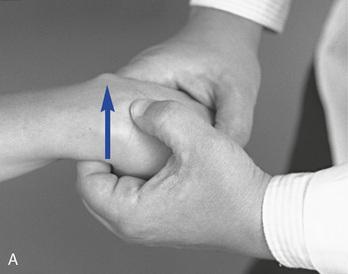
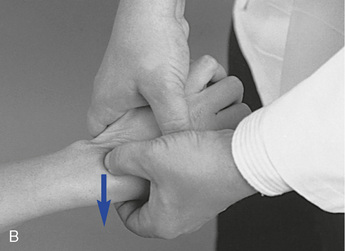
 Figure 6-122 Assessment of posterior-to-anterior (A) and anterior-to-posterior (B) glide of the individual carpals of the left wrist.
Figure 6-122 Assessment of posterior-to-anterior (A) and anterior-to-posterior (B) glide of the individual carpals of the left wrist.
Assess A-P and P-A glide of the intermetacarpal joints with the patient seated and the affected arm raised in forward flexion. Stand and face the patient, grasp the adjacent metacarpals with both hands, and stress them in an A-P and P-A glide (Figure 6-123).

Figure 6-123 Assessment of anterior-to-posterior and posterior-to-anterior glide of the left intermetacarpal joints.
Evaluate the MP and interphalangeal joints in a similar fashion. With the patient seated, grasp the proximal member of the joint to be tested with one hand while grasping the distal member of the joint being tested with the other hand. Then stress each MP or interphalangeal joint with long-axis distraction, A-P and P-A glide, L-M and M-L glide, and internal and external rotation (Figures 6-124 and 6-125).
Adjustive procedures
The application of an impulse thrust often can be performed using the accessory joint motion test procedure and adding the impulse thrust at the end. Although this is true of any joint in the body, fewer adjustive procedures are unique or different from the testing procedure for the wrist and hand. Box 6-8 identifies the adjustive procedures for the joints of the wrist and hand.
BOX 6-8 Wrist and Hand Adjustive Techniques
Wrist supine or sitting:
Wrist sitting:
Hand sitting:
Wrist
Supine or Sitting:
Sitting:
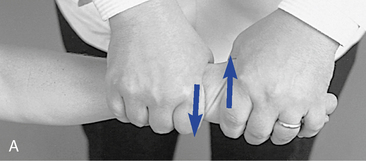
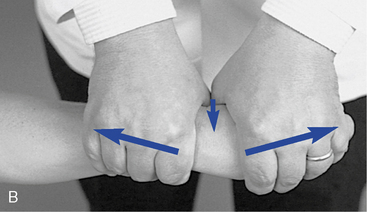
 Figure 6-130 Adjustment for medial-to-lateral and lateral-to-medial glide (A) and medial-to-lateral and lateral-to-medial tilt (B) of the left intercarpal joint.
Figure 6-130 Adjustment for medial-to-lateral and lateral-to-medial glide (A) and medial-to-lateral and lateral-to-medial tilt (B) of the left intercarpal joint.
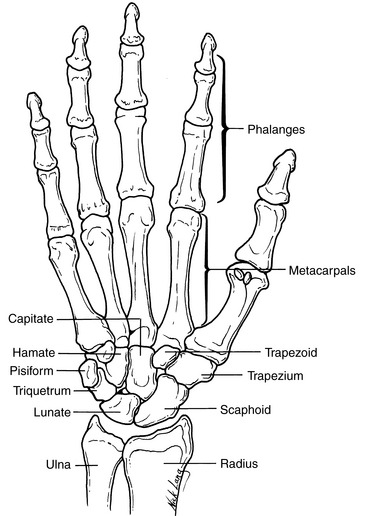
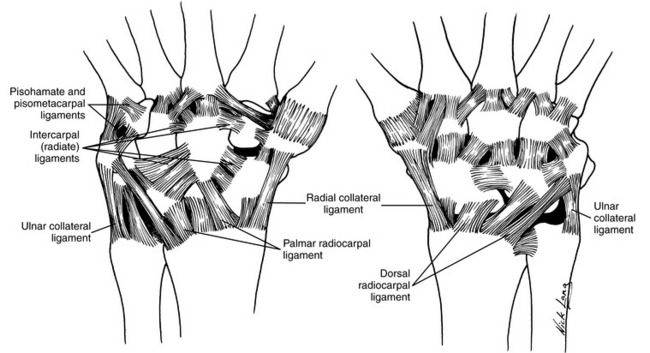
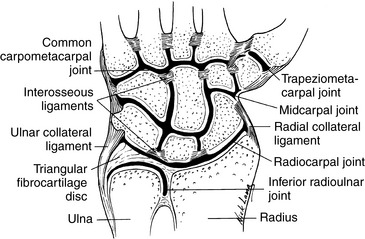
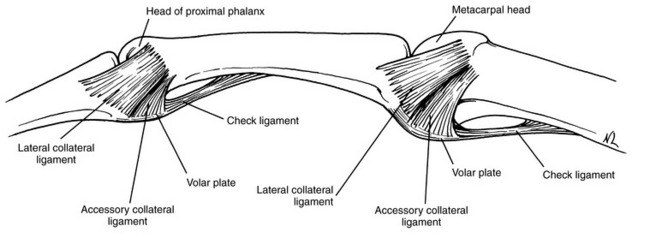
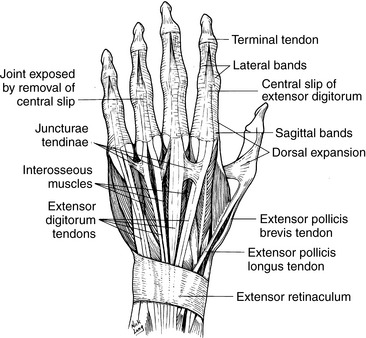
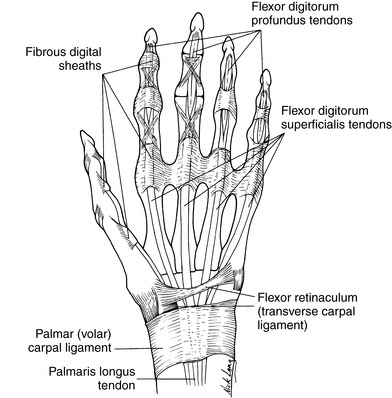

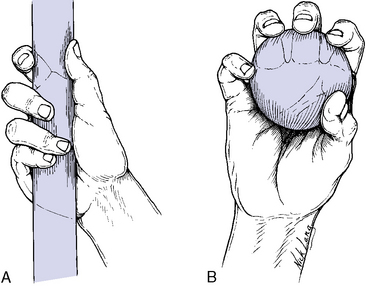
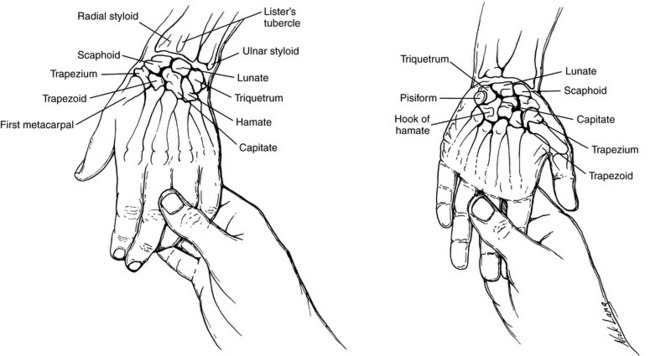
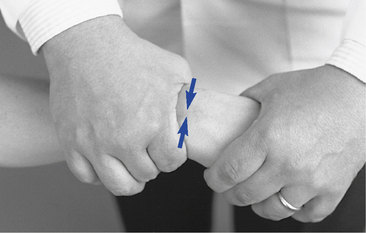
 Figure 6-117
Figure 6-117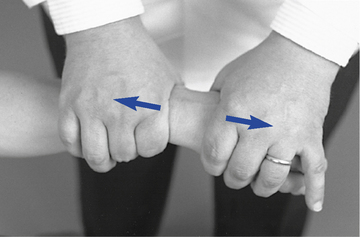
 Figure 6-118
Figure 6-118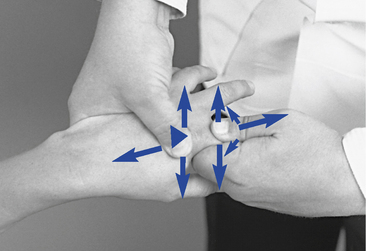
 Figure 6-124
Figure 6-124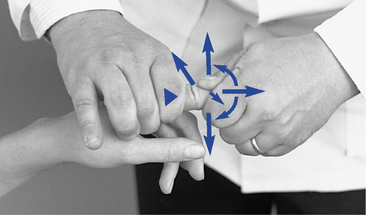
 Figure 6-125
Figure 6-125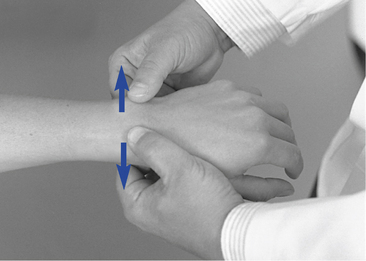
 Figure 6-126
Figure 6-126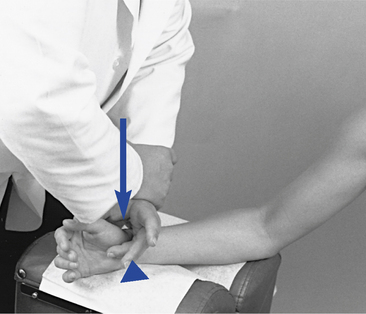
 Figure 6-127
Figure 6-127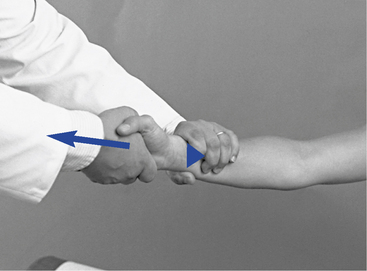
 Figure 6-128
Figure 6-128
 Figure 6-129
Figure 6-129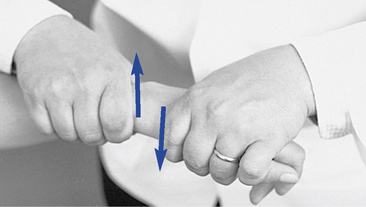
 Figure 6-131
Figure 6-131

 Figure 6-132
Figure 6-132
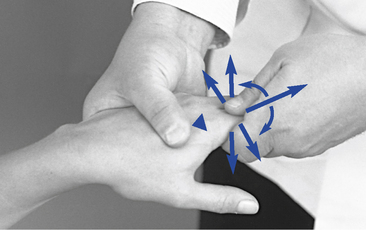
 Figure 6-134
Figure 6-134
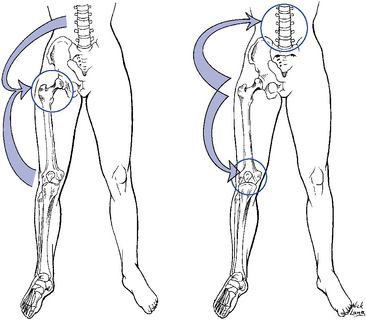
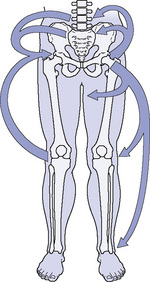
 Figure 6-149
Figure 6-149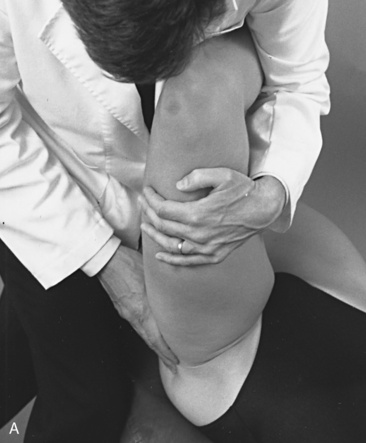

 Figure 6-150
Figure 6-150

 Figure 6-151
Figure 6-151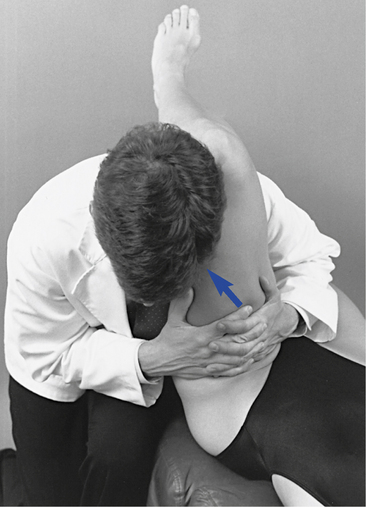
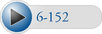 Figure 6-152
Figure 6-152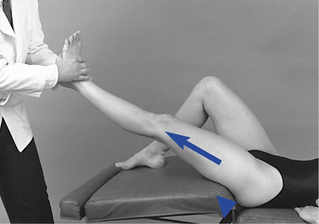
 Figure 6-153
Figure 6-153
 Figure 6-154
Figure 6-154
 Figure 6-155
Figure 6-155
 Figure 6-156
Figure 6-156
 Figure 6-157
Figure 6-157
 Figure 6-158
Figure 6-158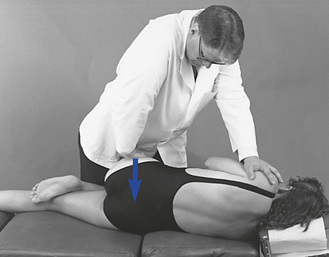
 Figure 6-159
Figure 6-159
 Figure 6-160
Figure 6-160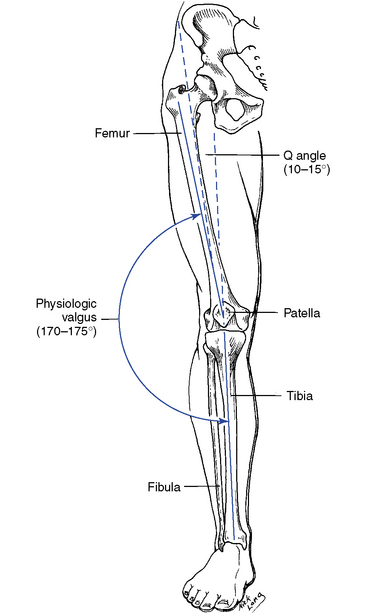
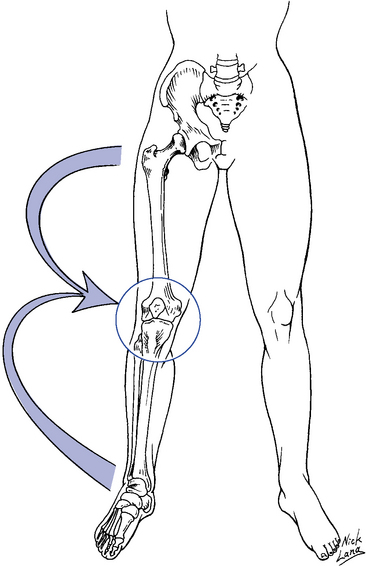
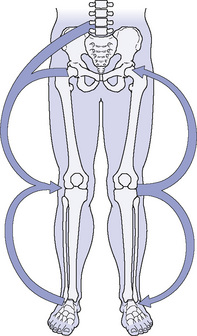

 Figure 6-178
Figure 6-178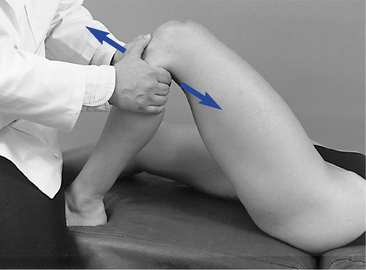
 Figure 6-179
Figure 6-179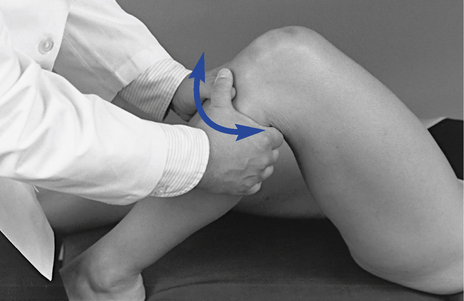
 Figure 6-180
Figure 6-180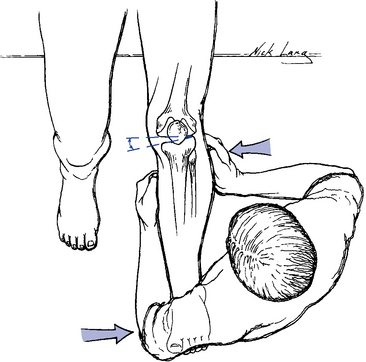
 Figure 6-181
Figure 6-181
 Figure 6-182
Figure 6-182
 Figure 6-183
Figure 6-183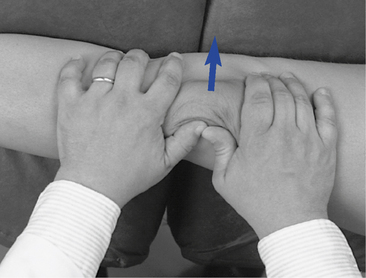
 Figure 6-184
Figure 6-184
 Figure 6-185
Figure 6-185
 Figure 6-186
Figure 6-186
 Figure 6-187
Figure 6-187
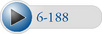 Figure 6-188
Figure 6-188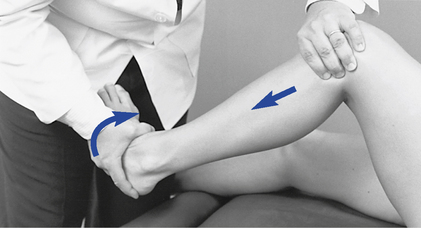
 Figure 6-189
Figure 6-189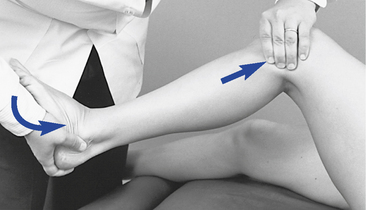
 Figure 6-190
Figure 6-190
 Figure 6-191
Figure 6-191
 Figure 6-192
Figure 6-192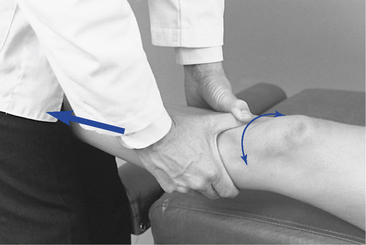
 Figure 6-193
Figure 6-193
 Figure 6-194
Figure 6-194
 Figure 6-195
Figure 6-195
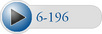 Figure 6-196
Figure 6-196
 Figure 6-197
Figure 6-197

 Figure 6-198
Figure 6-198
 Figure 6-199
Figure 6-199
 Figure 6-200
Figure 6-200
 Figure 6-201
Figure 6-201
 Figure 6-202
Figure 6-202
 Figure 6-203
Figure 6-203
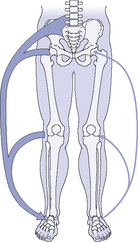
 Figure 6-214
Figure 6-214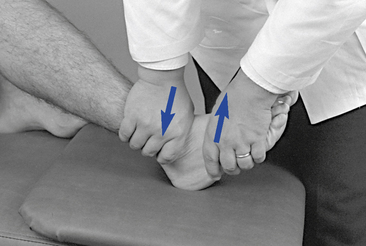
 Figure 6-215
Figure 6-215

 Figure 6-216
Figure 6-216
 Figure 6-217
Figure 6-217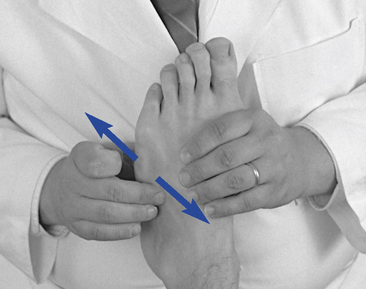
 Figure 6-218
Figure 6-218
 Figure 6-219
Figure 6-219
 Figure 6-220
Figure 6-220
 Figure 6-221
Figure 6-221
 Figure 6-222
Figure 6-222

 Figure 6-223
Figure 6-223
 Figure 6-224
Figure 6-224
 Figure 6-225
Figure 6-225

 Figure 6-227
Figure 6-227
 Figure 6-228
Figure 6-228
 Figure 6-229
Figure 6-229
 Figure 6-230
Figure 6-230
 Figure 6-231
Figure 6-231
 Figure 6-232
Figure 6-232
 Figure 6-233
Figure 6-233
 Figure 6-234
Figure 6-234
 Figure 6-235
Figure 6-235
 Figure 6-236
Figure 6-236
 Figure 6-237
Figure 6-237
 Figure 6-238
Figure 6-238