Chapter 7 Nonthrust Procedures
Mobilization, Traction, and Soft Tissue Techniques
Whereas most chiropractic adjustive techniques impart a thrust, many manual therapy procedures are designed to affect physiologic processes without using a thrust. The principal procedures that do not incorporate a thrust include joint mobilization, traction, and soft tissue manipulation (STM). This chapter presents a description and overview of the practical application of many of the common nonthrust procedures applied in manual therapy and chiropractic.
The chiropractic profession did not develop most of the techniques and procedures discussed in this chapter. Therefore, they should not be considered unique to the chiropractic profession. Moreover, a small percentage of chiropractic professionals do not use them because of the exclusiveness of thrust techniques. However, they are important forms of manual therapy that can be used alone or in combination with thrust procedures. Procedures characterized by a high-velocity thrust (adjustment) may indeed have effects that are different than and, in certain clinical situations, superior to nonthrust procedures.1,2
Nevertheless, both procedures share common physical attributes and overlapping potential positive clinical effects. Grieve3 contends that all mobilizations and manipulations are actually soft tissue techniques, because it is in the soft tissue that the lesions treated and the effects produced are found.
Chiropractors commonly encounter circumstances in which thrust manipulation is contraindicated or the primary neuromusculoskeletal (NMS) disorder is not the product of joint dysfunction or a pathologic condition. In such circumstances, it benefits both the doctor and the patient if the chiropractor is skilled in alternative nonthrust manual procedures. Indeed, various and numerous forms of manual therapy exist within the profession of chiropractic.4 Examples of circumstances in which nonthrust procedures might be more appropriate include the treatment of the older adults or patients with osteoporotic or extremely acute conditions, treatment of patients in the later stages of pregnancy, or treatment of patients with a diagnosis of myofascial pain syndrome (trigger point).
Nonthrust procedures are also viable options in circumstances in which the doctor is unable to produce a thrusting force that is capable of producing joint cavitation. If the doctor’s size, strength, or ability to develop the needed speed and amplitude is inadequate to produce the necessary force, some other type of technique application may provide an effective alternative. This is suitable only in the circumstance in which both thrust and nonthrust procedures are assumed to have the same physical effects. All manual therapies are not equivalent simply because a wide variety of methods exist.5 Most of the procedures described in this chapter were developed empirically. Typically they are associated with a particular innovator or profession, but invariably development, refinement, and modification by subsequent innovators has led to an environment of multiple definitions, descriptions, and variations of the same procedure. The intention of this chapter is not to present a comprehensive discussion of the variations and nuances of each procedure, but to offer a fair representation of techniques and an overview of each method presented. Ideally, the descriptions of the procedures contained within this chapter will broaden your awareness of nonthrust manual procedures and stimulate further critical evaluation of those procedures that pique your interest.
Joint mobilization
Definition
Joint mobilization may be defined as a passive therapeutic movement up to but not exceeding the anatomic end range of joint movement. A nonthrust maneuver is not commonly applied beyond a joint’s elastic barrier. Movement beyond the elastic barrier takes the joint into the paraphysiologic joint space and is typically associated with an audible pop or click. Therefore mobilization is less commonly associated with an audible crack than manipulation. Grieve3 considers spinal mobilization a more gentle, persuasive pressure performed within the available accessory range or at the end of the accessory range. However, mobilization can be applied over a wide range and can thus involve a series of movements (stages or grades). Mobilization is a coaxing, repetitive, rhythmic movement of a joint that can be resisted by the patient. Inherent within a nonthrust manipulation is a patient feedback mechanism. Because the motion is relatively slow, controlled, and gentle, the patient can report the effect of the technique during the application.
Primary goal
The primary goal of mobilization is to restore optimal range of motion (ROM), quality of movement, and comfort to the joint being addressed. Indirect benefit is thought to accrue because of improved function within each part of the kinetic chain in need of treatment. For example, compensatory mechanical stress on adjacent structures may be reduced when a previously painful or restricted part of the chain is returned to normal function. Such return to comfortable, maximal ROM usually serves as a passive treatment end point.6 Mobilization can be performed in a physiologic direction (rotation, flexion, extension, or lateral flexion) or in a nonphysiologic direction (e.g., longitudinal traction or posterior-to-anterior [P-A] gliding). Furthermore, various types of mobilization can be used to restore segmental motion and perhaps reduce pain in the spine and extremities. Graded oscillation, progressive stretch, and continuous stretch mobilization form the basis for most types of mobilization techniques.
Various types
Graded oscillation technique is a form of mobilization whereby alternate pressure (on and off) is delivered at different parts of the available range.7 The amplitude of the oscillation may also vary according to the purpose of the technique. Oscillatory technique is graded on a 1-to-4 scale based on the amplitude of the motion and part of the range being reached (Box 7-1). The vibratory nature of the graded oscillation technique is thought to activate sensory mechanoreceptors that may help reduce pain and improve proprioceptive function. Box 7-2 lists generalized procedural steps for the application of graded oscillatory mobilization.
BOX 7-1 Amplitude Grades for Oscillatory Technique
| Grade I | A small-amplitude movement near the starting position of the range |
| Grade II | A larger-amplitude movement that carries well into the range, occupying any part of the range that is free of stiffness or muscle spasm |
| Grade III | A large-amplitude movement that moves into stiffness or muscle spasm |
| Grade IV | A small-amplitude movement that stretches into stiffness or muscle spasm |
BOX 7-2 Generalized Graded Oscillatory Mobilization Procedure
Progressive stretch mobilization involves a series of successive short-amplitude, spring-type pressures or a series of short-amplitude stretch movements.8 The pressure or stretch is imparted at progressive increments of the range. Progressive stretch is graded on a 1-to-4 scale, as is graded oscillation. The major indication for the use of progressive stretch mobilization is mechanical or soft tissue restriction or both.
Continuous stretch is a sustained, gradually increased stretch or pressure without interruption. Maintaining a stretch or pressure throughout the mobilization procedure is recommended when immediate tissue feedback is desired. Adaptively shortened periarticular soft tissue structures are most likely to be affected using continuous stretch technique. Improving extensibility of the periarticular soft tissues about a spinal joint by means of collagen fiber realignment and viscosity change allows for improved joint mobility.
Mobilization can be performed at general regions or at specific joint levels. The difference between these procedures rests in the localization of forces. To produce a specific mobilization, a particular segment must be placed in its most favorable position for movement, and contacts must be placed on or close to the segment being mobilized. A general or regional mobilization incorporates the use of longer levers or contacts placed at points distal to the area being mobilized. In addition, the arc of movement for a generalized or regional mobilization will be greater than the arc of motion used for the specific or segmental mobilization.
In addition, special attention should be given to the traction component of mobilization. Where anatomic relationships allow traction to accompany mobilization, traction should be used as an integral part of the treatment program. In many cases of pain-induced failure of a mobilization technique, that is, when angular or even translational force vectors produce increased pain, pure traction techniques may still be useful. This fact reinforces the concept that traction is one of the least invasive mobilization methods.9
Selected examples
The following is a representative sample of spinal and extremity mobilization procedures. These procedures have been selected because they represent a variety of methods, not because they demonstrate superior effectiveness as compared with other mobilization procedures.
Oscillatory Cervical Lateral Flexion (Figure 7-1)
The patient lies in the supine position, with the head and neck supported on the headrest and by the clinician’s hands. The clinician sits or stands at the head end of the table. To produce left lateral flexion mobilization of the cervical spine, the clinician’s right hand comfortably grasps the patient’s chin while the forearm rests on the side of the head. The other hand supports the patient’s occiput. Both hands support the patient’s head and produce a repetitive, rhythmic left lateral flexion movement around the z-axis. An oscillatory movement is produced as the hands move reciprocally, and all excursions have equal value.
Oscillatory Atlas Lateral Glide (Figure 7-2)
The patient lies in the side-posture position with both knees bent to maintain pelvic stability, the upper arm resting along the side of the body and the hand grasping the thigh, and the head placed in a neutral position on an elevated headrest. The clinician sits or stands, facing the patient, and contacts the lateral aspect of the atlas transverse process with both thumbs, one on top of the other. A lateral-to-medial oscillatory movement is produced, developing a translational lateral glide movement.
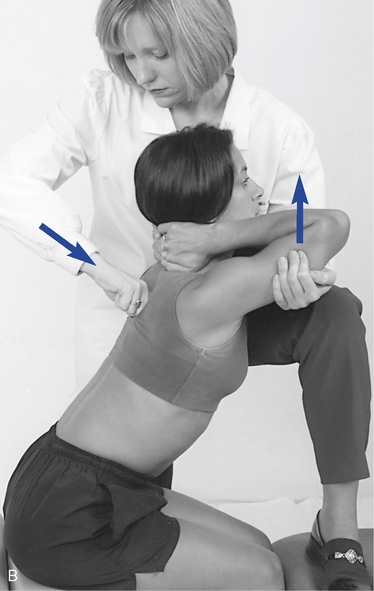
Progressive Stretch Thoracic Extension (Figure 7-3)
The patient lies in the prone position with the hands interlaced behind the neck and the elbows together (Figure 7-3, A). The clinician stands on the side of the table and grasps the patient’s arms from underneath with the cephalic hand. The caudal hand is used to establish a broad contact over the spine below the section to be mobilized. The clinician simultaneously and progressively raises the arms to the patient’s tolerance while applying stabilizing pressure over the spine. This procedure may also be done in the seated position (Figure 7-3, B). There is powerful leverage produced in both positions, and caution must be used to prevent injury.
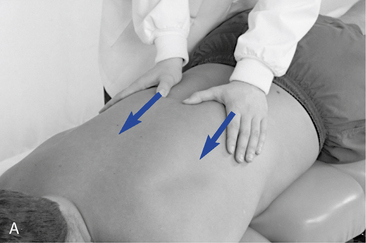
Oscillatory Posterior-to-Anterior Glide (Figure 7-4)
The patient lies in the prone position. The clinician stands on the side of the table facing cephalically and in a lunge position (fencer stance). The clinician establishes bilateral thumb contacts over the articular processes of a cervical segment, the transverse processes of a thoracic segment, or the mammillary processes of a lumbar segment. The thumbs may be on the same side of the patient or can cross the spine. The clinician produces a P-A oscillatory movement over the vertebra.

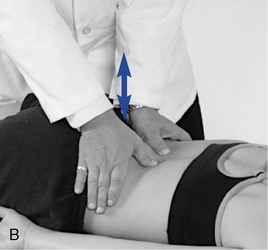
Figure 7-4 Oscillatory posterior-to-anterior (P-A) glide applied to the L3 vertebra. The patient lies in the prone position. The clinician stands on the side of the table, facing cephalically, in a lunge position (fencer stance). The clinician establishes bilateral thumb contacts over the articular processes of a lumbar segment. The thumbs may be on the same side of the patient or may cross the spine (A). A bilateral contact can also be established (B). A P-A oscillatory movement is produced over the vertebra.
Progressive Stretch Lumbar Rotation (Figure 7-5)
The patient lies in a prone position over an elevated table or Dutchman roll. The clinician stands in a square stance at the side of the table opposite the area to be mobilized. The clinician’s caudal hand grasps the anterior superior iliac spine while the cephalic hand establishes a broad contact over the lower rib cage on the side to be mobilized. The clinician raises and lowers the pelvis against the resistance provided by the cephalic hand, producing a rhythmic rocking lumbar rotation of small amplitude.
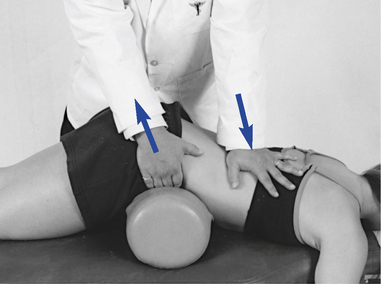
Figure 7-5 Progressive stretch lumbar rotation to mobilize the right side of the lumbar spine. The patient lies in a prone position over an elevated table or Dutchman roll. The clinician stands in a square stance at the side of the table opposite the area to be mobilized. The clinician’s caudal hand grasps the anterior superior iliac spine while the cephalic hand establishes a broad contact over the lower rib cage on the side to be mobilized. The clinician raises and lowers the pelvis against the resistance provided by the cephalic hand, producing a rhythmic lumbar rotation of small amplitude.
Continuous Stretch Rotation (Figure 7-6)
The patient lies in a prone position over an elevated table or Dutchman roll. The clinician stands at the side of the table, facing cephalically, in a lunge position (fencer stance). The clinician establishes a thumb contact against the lateral aspect of a spinous process with the caudal hand. The cephalic hand is placed over the lateral aspect of the pelvis. A firm, continuous pressure to the patient’s tolerance is applied against the L5 spinous process while the pelvis is stabilized. Continuous pressure is held for 8 to 12 seconds and repeated up to three times.

Figure 7-6 Continuous stretch rotation of L4, producing a left rotational mobilization of L4 over L5. The patient lies in a prone position over an elevated table or Dutchman roll. The clinician stands at the side of the table, facing cephalically, in a lunge position (fencer stance). The clinician establishes a thumb contact against the lateral aspect of the pelvis. A firm, continuous pressure to the patient’s tolerance is applied against the L5 spinous process while the pelvis is stabilized. Continuous pressure is held for 8 to 12 seconds and repeated up to three times.
Manual traction-distraction
Definition
The term traction refers to the process of pulling one body in relationship to another, which results in separation of the two bodies. Traction is passive translational movement of a joint, which occurs at right angles to the plane of the joint, resulting in separation of the joint surface. Kaltenborn10 graded manual traction by the three effects it produces. With the first effect, there is no appreciable joint separation because only enough traction force is applied to nullify the compressive forces acting on the joint. The compressive forces are the result of muscle tension, cohesive forces between articular surfaces, and atmospheric pressure. The second effect produces a tightening in the tissue surrounding the joint that is described as “taking up the slack.” The third grade of traction requires more traction force to produce a stretching effect into the tissues crossing the joint. The principal aim of treatment is restoration of normal painless ROM (Box 7-3).
Traction produces measurable separation of vertebral bodies and centripetal forces exerted by the tension applied to surrounding soft tissues. However, traction has other effects as well. Grieve11 identifies some other effects that are the result of both sustained and rhythmic traction (Box 7-4).
Manual traction is not a unique and separate form of treatment but is simply one form of passive mobilization.12 Traction can be varied in many ways; almost any form of passive handling may be used, with some form of oscillation or as a static hold. Therefore, a longitudinal movement may be performed as an oscillatory mobilization, as a slow rhythmic stretch, or as a static traction. Traction may be manual or mechanical, static or rhythmic, or fast or slow; the force applied may be strong or gentle, and it may be applied symmetrically or asymmetrically. These variations must be explored to determine which combination is most suitable for the patient’s needs or the clinician’s abilities. The effects of traction are not necessarily localized, but may be made more specific by careful positioning.
For traction to achieve maximal success in a minimal amount of time, the patient must be positioned accurately, a minimal effective force must be used, and each patient’s treatment must be based on his or her signs and symptoms rather than the diagnosis. The potential theoretic effects of traction on the spine include stretching of the muscles and ligaments, improving glide of the dural root sleeves, freeing fixation of articular facets, changing hydrostatic pressure in the discs and repositioning nuclear fragments, and improving the blood supply to the spine and its surrounding structures.13
Specific procedures
Manual Lumbar Flexion-Distraction (Cox Method)
Flexion-distraction is a mechanically assisted form of joint mobilization or distraction, blending osteopathic and chiropractic principles into one technique. Flexion-distraction has been advanced in the chiropractic profession largely by the work of chiropractor James Cox. Much of Cox’s initial work in developing his technique of flexion-distraction was based on the work of the osteopath J.V. McManis. Moreover, the design of the early Cox table was a direct emulation of the McManis table of the early 1900s. This manual table provided an advantage to both the patient and the clinician, allowing a multiple-plane approach to distraction, including flexion-extension, lateral flexion, and rotation. The McManis table incorporated many of the features that appear on contemporary tables, including split headpieces, multiple sections adjustable for patient comfort, and positioning for various adjustive maneuvers.14
A number of lumbar disorders have been presented as conditions suitable for treatment with lumbar flexion-distraction. They include lumbar disc protrusion, spondylolisthesis, facet syndrome, subluxation, and scoliotic curves of a nonsurgical nature.15 The theoretic benefits that have been associated with this form of spinal manipulation are presented in Box 7-5.
The Cox method uses a process of analysis that incorporates physical examination, orthopedic and neurologic testing, and imaging as indicated to establish the presence of a disc lesion, facet syndrome, or any other condition affecting the low back. Cox distraction therapy typically consists of three 20-second flexion-distraction sessions. Once the patient is properly positioned on the table and the tolerance of the patient to flexion is determined, the sessions can begin. The hand is placed over the spinous process of the superior vertebra of the motion segment to be distracted (e.g., to distract the L5–S1 segment, contact is on the L5 spinous process). The contact hand is slightly cupped, creating an indentation between the thenar and hypothenar eminence to receive the prominence of the spinous process without placing undue pressure and causing subsequent discomfort to the patient.16 The patient is encouraged to relax, and the clinician depresses the handle at the foot of the table. If there is no handle, the clinician depresses the foot of the table (pelvic section) by hand. The handle is an improvement over placing the hand on the caudal section of the table because it provides increased leverage and a better stance position for the clinician (Figure 7-7).

Figure 7-7 Cox flexion distraction for the L4 disc (L4–L5 segment) with a contact established over L4 spinous process as the caudal section is depressed, producing distraction.
The pelvic section is then depressed until the clinician’s hand detects that the musculature has reached a point of tautness and all tissue and joint play have been removed from the area under treatment. This point is maintained, and an additional 2 to 3 inches of table depression is achieved manually. The caudal section is then allowed to return to neutral, followed by another downward movement to the previous point over a 20-second period. This process creates a “pumping action” and is repeated three times, with a break of a few seconds between each 20-second session (Box 7-6).
BOX 7-6 Essential Steps of Flexion-Distraction Treatment
A patient with a protruding disc may sense mild pain on traction, whereas a prolapsed disc does not usually produce such a sensation. Too much traction during the session should be avoided because it may produce further annular injury and impairment. In the case of disc involvement, the disc and motion segment are potentially sensitized to pain and mechanical stimuli, and the patient is probably sensitive and sore at the point of the injury. Therefore, it is better to undertreat the patient than to overtreat, and caution is encouraged in the application of the technique. Furthermore, if the patient does not tolerate the flexion-distraction movement or if the pain is peripheralized, the process should not continue. Further traction should concentrate on relieving the pain before the therapeutic distraction begins in earnest. Any intolerance should be viewed with caution and, although this does not become a clear contraindication for the treatment, it certainly should be treated with respect and restraint. In this instance, more is not better but, in fact, may make the patient’s condition worse.
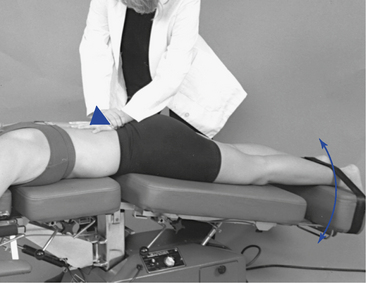
Motorized Lumbar Distraction (Leader Method)
A motorized traction table, such as the Leader table, can be used to assist in the production of lumbar traction (Figure 7-8). Traction to the lumbar spine is applied in the prone position while the pelvic section of the table produces continuous passive motion in the long axis of the spine. The clinician can apply a stabilizing pressure, using both hands over the spinous process of the segment to be distracted to produce a counterpressure against the distractive force produced by the table.
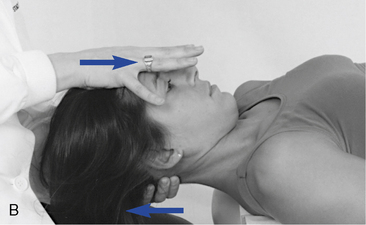
Manual Cervical Traction
Cervical traction can be applied manually or with mechanical assistance. Manual cervical traction is generally accomplished with the patient in the supine position. The clinician sits or stands at the head end of the table and establishes contacts with the fingers of both hands on the posterior aspect of the cervical spine. Contacts taken over the C5–C6 segment (Figure 7-9, A) will allow the neck to extend slightly to provide more distractive separation and stretch to the anterior structures (the disc and longus coli muscles). Contacts taken under the base of the occiput (see Figure 7-9, B) will allow the neck to flex slightly to provide more distractive separation and stretch to the posterior structures (facets and paraspinal muscles). A towel may be substituted for hand contacts (see Figure 7-9, C).
Motorized Cervical Traction
A motorized traction table, such as the Leader table, can be used to assist in the production of cervical traction (Figure 7-10). Traction to the cervical spine is usually applied in the prone position while the pelvic section of the table produces continuous passive motion in the long axis of the spine. The clinician can apply a stabilizing pressure at the base of the occiput or anywhere in the cervical spine to produce a counterpressure against the distractive force produced by the table’s moving pelvic piece (Box 7-7).
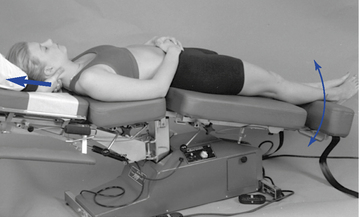
Figure 7-10 Motorized cervical distraction. Contact at base of occiput applying resistance to moving pelvic piece (may also be done in the prone position).
BOX 7-7 Motorized Cervical Traction
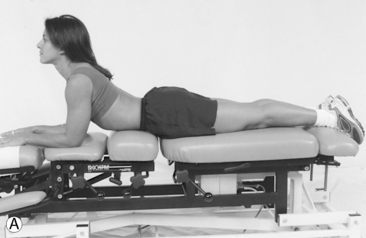
Mckenzie method
The McKenzie method is most commonly associated with the promotion and application of lumbar extension exercises for the treatment of low back pain (LBP). Consequently, it is often viewed incorrectly as only a treatment method. The McKenzie method is both an evaluation and treatment approach to the management of painful spinal conditions. It is based on a structured and focused assessment of the effects of repeated movements and sustained postures on a patient’s symptoms and spinal biomechanics. The information gained about the patient’s symptomatic and mechanical responses to loading allows the clinician to determine which specific movements, positions, and activities to either pursue or avoid in the treatment plan. This information is specific to a particular patient at a specific point in time and provides reproducible objective and subjective criteria on which to base clinical decisions. It has been shown to reliably differentiate discogenic from nondiscogenic pain, and a competent from incompetent annulus.17 In comparison with magnetic resonance imaging, it demonstrates superior ability in distinguishing painful from nonpainful discs.17
Treatment principles
The McKenzie approach to treatment is based on the application of mechanical forces and the patient’s symptomatic and mechanical responses to those forces. The central premise is that those movements that decrease or “centralize” the patient’s pain are the movements that should be applied in the treatment of the disorder. Centralization refers to the process of peripheral symptom resolution. With centralization, a patient’s spine pain may persist or temporarily increase. Centralization has been shown to predict a beneficial clinical outcome.18 Increasing symptoms most distal to the spine are known as peripheralization and have been shown to correlate with a loss of competence of the disc annulus18 and predict a poor response to McKenzie treatment procedures. In the McKenzie treatment approach, there is a significant amount of self-applied therapy. The patient learns to appreciate the role of prophylactic procedures from the beginning of treatment and how to interpret which exercises, postures, or activities are beneficial or not. A primary consideration is that all applied procedures should be done in such away that the patient is able to self-treat more effectively. McKenzie19 suggests that clinician-applied forms of spinal manipulative therapy should not be performed on the entire population with back and neck pain, but rather on the minority of patients who have not been able to adequately resolve their symptoms through self-treatment.
Three syndromes: postural, dysfunctional, and derangement
Information obtained through the McKenzie evaluation allows for the classification of mechanical pain into one of three syndromes: postural, dysfunctional, or derangement. Each of the syndromes is considered a unique and separate disorder; however, they often coexist within the same individual. They are distinguished from one another by location of symptoms, presence or absence of acute spinal deformity, and effects of repeated movements and sustained end range positions altering pain patterns.20
The postural syndrome characteristically has pain appearing after prolonged static loading, which causes overstretching and mechanical deformation of normal spinal tissue. Pain diminishes when the loading is removed. The aim of treatment is to correct posture, relieving the painful tension in normal tissues.
With the dysfunctional syndrome, pain appears immediately when shortened spinal tissues are mechanically deformed by overstretching. ROM is often decreased, and pain is increased at the end range of movement and decreased with the removal of end range stress.
The derangement syndrome is a product of anatomic disruption or displacement of the intervertebral segment. Pain may occur immediately with injury or develop over time and is often felt in the midrange of movement. The derangements are divided into one anterior and six posterior categories. Their history and repeated movement examination (Box 7-8) differentiate the three syndromes. Because the three identified syndromes of mechanical pain are separate entities, they each require a different approach to treatment.
Postural Syndrome
For those patients presenting characteristics of the postural syndrome, applying an understanding of the basic mechanics of postural stresses and their removal is fundamental in treatment. Once an abnormal posture has been identified as the source of the patient’s symptoms, treatment is directed toward postural correction. The primary consideration is to develop within the patient the ability to control pain-producing mechanisms.
Slouch-Overcorrect Exercise (Figure 7-11)
The patient sits in a slouched posture, provoking LBP. This posture is then corrected by forming an increased lumbar lordosis and retraction of the head. The patient should be able to feel that the pain can be abolished or at least reduced by changing the posture. Regular performance of the exercise encourages a postural awareness that reduces or eliminates pain of postural origins. The exercise can also be done in the standing position.
Dysfunctional Syndrome
Treatment of the dysfunction syndrome is directed at remodeling of adaptively shortened structures by stretching maneuvers. The most common pattern of the dysfunction syndrome is loss of spinal extension, except in the upper to middle cervical spine, where flexion is most likely to be limited.21 To achieve the required tissue response, end-range stretching procedures should be performed in a slow, repeated movement in sets of 10 to 15 every 2 hours throughout the day. The presence of significant degenerative changes or stretch irritation to neural structures may make the repetitive rate difficult to tolerate. The involved spinal region and the specific loss of movement pattern determine the movement chosen for treatment. In this case, correction of posture alone is not likely to enhance the lengthening of shortened structures. However, postural dysfunction, if present, must still be addressed because chronic poor posture often leads to tissue shortening and dysfunction. Moreover, when progress is slow or nonexistent, the use of manual procedures or other external forces is introduced. This can include the use of rhythmic end-range mobilizations designed to assist in the phenomenon of creep to lengthen soft tissue. However, these are used to augment, not replace, the exercise program. The repeated movements used in evaluation and treatment of the dysfunction syndrome include flexion, extension, and side-gliding in both the seated and lying positions (Figure 7-12). The treatment exercises will reproduce the patient’s pain, but the increased pain should not persist for prolonged periods after treatment.
Derangement Syndrome
For treatment of the derangement syndrome, a conceptual model of disc pathomechanics must be considered. The model is based on the premise that certain movements can be applied to reduce internal disc derangements and bulging intervertebral discs (IVDs). Movements that are successful in reducing disc protrusion are accompanied by a reduction in the patient’s most distal symptoms (centralization) as the conflict between the protruding disc and associated spinal nerve root is reduced. As symptoms centralize, it is also common for the patient’s repeated ROM to increase with exercise. Using this approach, the suspected derangement patient is directed through a series of movements to ascertain which movements or positions will be most effective in reducing the segmental derangement. The evaluation results in the patient being classified into one of seven derangement categories. The first six derangements are variations of posterior disc disruptions, often requiring extension reductions. In certain instances, coronal plane movements, such as side-gliding (Figure 7-13), or even rotational movements will be required for reduction. The seventh derangement is an anterior disc derangement, requiring a flexion reduction (Figure 7-14).

Figure 7-14 McKenzie method (flexion reduction exercise). The seventh derangement is an anterior disc derangement, requiring a flexion reduction.
To complement the use of extension (or flexion) reduction exercises, avoidance of stressful static and dynamic flexion (or extension) postures and activities must be reinforced. These activities often cause peripheralization of the patient’s symptoms, as well as painfully reduced ROMs. Recovery of function is considered complete when full normal repeated weight-bearing flexion produces no more than the expected strain at the end range of all movements.21
Cranial manipulation
Cranial manipulation developed along parallel lines in both the osteopathic and chiropractic professions beginning in the mid- 1930s. Misperceptions and misunderstandings have led to controversy over cranial manipulation. Much of the controversy comes from those who look at the cranium as a fused structure and therefore believe that manipulation has no basis. Cranial manipulation was begun in the chiropractic profession by Cottam and in the osteopathic profession by Sutherland. Both Cottam and Sutherland hypothesized that the cranial bones moved and formed the basis for most cranial techniques. The concept of cranial bone motion, and the therapeutic application of forces on the cranium, is by no means universally accepted. However, the previously held belief that the cranial bones fuse in relatively early life has been shown to be faulty.22 23 24 Although the process of ossification starts in the mid-20s, sutures may remain open throughout life, and some motion flexibility may last into old age.25 The cranial bones are connected and held together by connective tissue called the sutural ligament or membrane, which remains nonossified. Nerve fibers accompany the collagenous connective tissue, although their exact function has not been established.
There are three hypotheses regarding cranial motion. Sutherland suggested that there is a continuous, rhythmic, oscillating motion within the dural tube. Dysfunction in the dural tension system leads to lesions that are identifiable and correctable. A second concept is that the cranium moves in a spontaneous and unpredictable motion that is influenced by the pressures of vascular and cerebrospinal fluid (CSF) circulation. The third idea it is that the cranium does not actually move, and stresses and pressures that can be influenced by cranial manipulation build up in the joints and bones.
Practitioners incorporating cranial manipulation purport to be able to palpate a rhythmic (8 to 14 oscillations per minute) cranial movement.26 27 28 However, there have been no interrater reliability studies published. Sutherland called the rhythmic movement within the dural system the primary respiratory mechanism. The pulsations within the dural tube are thought to aid in the circulation of CSF. CSF bathes and nourishes the central nervous system. The potential effects of cranial dysfunction are listed in Box 7-9.
Although the mechanism of cranial movement remains unknown, there is agreement that sutural asymmetry, jamming of the sutures, and pain and muscle tightness can be palpated.25 The evaluation for cranial dysfunction includes observation for skull asymmetries; palpation of skull contours and the sutures themselves to identify widening, narrowing, or tenderness; and determination of the rate, rhythm, and amplitude of the craniosacral mechanism. The goal of cranial manipulation is to improve sutural motion, reduce membranous tension, improve circulation, and increase the vitality of the primary respiratory mechanism. Direct and indirect manipulative procedures have been described for the treatment of cranial dysfunction. Mild forces are used in conjunction with the patient’s breathing pattern.
Sagittal suture spread (Figure 7-15)
With the patient in a seated or supine position, use digital contacts of your four fingers of both hands on either side of the sagittal suture. Use a gentle tractioning to separate the suture. This same procedure can be done on any of the sutures.
Cranial universal (Figure 7-16)
With the patient prone, grasp the mastoid processes with the thumb and middle finger of one hand. Place the fingers of the other hand over the occipital bone. Rotate both hands in the same direction, using mild pressure and repeating four or five times.
Parietal lift (Figure 7-17)
With the patient supine, apply digital contacts of the fingers of both hands on the inferior aspect of the parietal bone at the squamosal suture. Use the thumbs of both hands to hold at the parietal suture. Use the digital contacts, applying a mild lifting pressure and repeating four or five times.
Soft tissue manipulation
Humans have been performing therapeutic procedures to the soft tissues for as long as humans have been able to touch one another. STM techniques are defined as those physical methods applied to muscles, ligaments, tendons, fascia, and other connective tissues with the goal of therapeutically affecting the body.29 A common source of pain and disability is soft tissue injury with its resultant fibrosis and loss of elasticity and strength. Soft tissue injury and fibrosis may result from acute or repetitive trauma to muscular, tendinous, myofascial, or ligamentous tissue.30 31 32 Although all manual techniques have some effect on the soft tissues, the justification for a separate STM classification is to draw attention to the prime importance of including techniques that have the specific purpose of improving the vascularity and extensibility of the soft tissues.11 One of the signs of joint dysfunction and subluxation is the presence of muscle hypertonicity. Localized increased paraspinal muscle tone can be detected with palpation. Janda33 recognizes five different types of increased muscle tone: limbic dysfunction, segmental spasm, reflex spasm, trigger points, and muscle tightness. Liebenson34 has discussed the treatment of these five types using active muscle contraction and relaxation procedures. Reflex muscle spasm or splinting follows trauma or injury to any of the pain-sensitive structures of the spine. The pain-sensitive spinal tissues include the zygapophyseal joints, posterior ligaments, paravertebral muscles, dura mater, anterior and posterior longitudinal ligaments, and IVD.35 Mechanical deformation or chemical irritation of any of these tissues will cause restricted motion by way of muscle spasm. Treatment directed at the tissue source of pain will reduce the reflex muscle spasm and increase the ROM; however, if the muscle spasm has been present for some time, it may require direct treatment as well.
Visceral disease can also cause reflex muscle splinting. The diagnosis of a viscerosomatic reflex is based on a history of visceral disease or current visceral disease symptomatology and objective palpation findings.36 Objective palpation findings include two or more adjacent spinal segments that show evidence of fixation located within a specific autonomic reflex area; a deep paraspinal muscle splinting reaction; resistance to segmental joint motion; and skin and subcutaneous tissue changes consistent with the acuteness or chronicity of the reflex.36
Effects of soft tissue manipulation
When considering the use of treatment procedures directed toward the soft tissues, a working knowledge of the fundamental principles behind them is necessary and helpful. Manual procedures applied to the soft tissues are intended to enhance proper tone and extensibility or both through a number of proposed mechanisms. Although specific and singular effects are presented, invariably it will be a combination of effects that occur.
Blood Flow and Temperature Effects
STM has been purported to produce an increase in blood flow and cutaneous temperature. Deep stroking and kneading of the soft tissues in the extremities of normal patients, patients with rheumatoid arthritis, and patients with spasmodic paralysis create a consistent and clinically significant increase in blood flow and cutaneous temperature.37 These findings are supported by other studies.38 39 40 However, it must be emphasized that the clinical procedure being tested in all of these reports was a deep or heavy massage application. Therefore, conclusions on the effects of light-force stimulation of the body wall cannot be drawn from these data.
Massage can induce a fall in blood viscosity, hematocrit count, and plasma viscosity. Ernst, Matrai, and Magyarosy41 found massage to equal pharmacologic agents used to treat blood flow problems. The proposed mechanism may be hemodilation resulting from either an increase in blood plasma volume or reactive hyperemia. Therefore, the effect of massage and circulation appears to be an increased perfusion of blood with plasma fluid, allowing for improved blood flow.
Metabolic Effects
Cuthbertson42 performed a literature review on the effects of massage on metabolic processes, including vital signs and waste products of the body. He reported that in normal subjects there was no increase in basal consumption of oxygen, pulse rate, or blood pressure, although an increase in urine output was observed. His conclusion hypothesized that to effect a change in the vital signs, a systemic effect must be achieved and that the massage procedures used did not do it. Schneider and Havens43 did find that STM produced an increase in red blood cells needed to bring oxygen to the tissues. This provides some support for soft tissue procedures being able to increase circulation and nutrition to desired areas. Again, these were vigorous massage procedures described, so caution is necessary when trying to apply these principles to other procedures.
Massage therapy has been further evaluated as a treatment for reducing blood pressure. Hernandez-Reif and colleagues44 reported that 10 30-minute massage sessions over 5 weeks reduced diastolic blood pressure, as well as anxiety and depression, to a statistically significant level over a control group receiving progressive muscle relaxation instructions. These findings supported an earlier study also demonstrating a decrease in diastolic and systolic blood pressure.45 In a study of light massage of preoperative patients, it was reported that there was a relaxation response from the parasympathetic nervous system producing a decrease in both blood pressure and heart rate, as well as an increase in skin temperature.46
Reflex Muscle Spasm Effects
Changes in muscle length and tension are monitored by two stretch receptors: muscle spindles and Golgi tendon organs (GTOs). The muscle spindle has a highly sensitive filament, the annulospiral ending, that fires rapidly and with high velocity with the smallest change in length. It also has smaller filaments and slower spray receptors, which are slower in response and more likely to respond to the magnitude and speed of stretch. The GTOs are located at the junction of the muscle and its tendon and monitor the tension exerted on the contracting muscle or imposed by external forces. Massage procedures can cause an overload of the GTOs, resulting in reflex inhibition and muscle relaxation.47 Lumbar muscle strain with concomitant hypertonicity has been treated by many means with mixed results. Yu48 reports on 55 cases treated with massage therapy that showed good results in decreasing pain, inflammation, and hypertonicity. In a review article, Goats49 reports on the effectiveness of massage therapy for reducing muscle spasm. Massage was shown to significantly diminish motorneuron excitability when compared with controls, forming the basis for suggesting that massage can lead to muscle relaxation.50 The effect of massage intensity was also studied.51 Light-pressure and deep-pressure massage was applied to the triceps surae muscle. H-reflex amplitudes were significantly reduced in both massage groups as compared with the control group. Moreover, deep massage reduced the H-reflex more than the light massage, suggesting that the mechanism involved is pressure-sensitive.51
Specific techniques
What follows is a description of manual therapies used by chiropractic physicians and other health care providers to primarily influence the soft tissues of the body. It is not intended to be a compendium of all STM and reflex techniques. The procedures presented have been selected to illustrate the fundamental concepts applicable to many of the forms of STM and to present the specific application of commonly applied procedures. One of the main functions of soft tissue therapy is to prepare the irritated region for subsequent mobilizations or manipulations. STM can be stationary (done on one spot) or progressive (done by moving hands from one place to another). Moreover, it may be variable in the intensity of pressure exerted, surface area treated, and frequency of application.
STM includes massage (stroking or effleurage, kneading or pétrissage, vibration or tapotement, and transverse friction massage), connective tissue massage, trigger point therapy (Nimmo technique), myofascial release techniques (MRTs; muscle energy techniques [METs], postisometric relaxation [PIR], and proprioceptive neuromuscular facilitation [PNF]), and body wall reflex techniques (Chapman lymphatic reflexes, Bennett vascular reflexes, and acupressure point stimulation) (Box 7-10).
Massage Techniques
Massage therapy is older than recorded time, and rubbing was the primary form of treatment until the pharmaceutical revolution of the 1940s.52 Today, classical or traditional massage procedures form the basis for many other procedures. Simply defined, massage consists of hand motions applied to the surface of the body with a defined therapeutic goal.53 In a more clinical or practical definition, massage is a term used to describe certain manipulations of the soft tissues; it is a form of manipulation most effectively performed by the hands and administered for the purpose of producing effects on the nervous, muscular, circulatory, and lymph systems.54 The variations of massage movements include effleurage, pétrissage, roulomont, tapotement, and friction. With most forms of massage, some form of lubricant is useful. It is recommended that for short sessions, a water-based lotion be used, because it will be absorbed by the skin. For longer sessions, an oil-based lotion is preferred.
Effleurage
Effleurage is a French word that means gliding or stroking, and it is applied over a large area using broad contacts. It may be deep or very superficial, creating general relaxation and a superficial warming as a result of a mild erythema. During a single therapeutic session, it is desirable and recommended to begin and end with effleurage. This maneuver is a slow rhythmic stroking in which the hands of the clinician make light contact with the skin of the patient (Figure 7-18). A broad palmar contact is used over large surfaces, but the thumbs or fingers can be used over smaller areas. The clinician’s hand should be sufficiently relaxed to mold itself to the area being treated as it passes almost insensibly from distal to proximal over the region being treated. Hand pressure is evenly dispersed, and the degree of pressure varies with the size and the region of the part being treated. The strokes are made in long, gliding sweeps. The movement should be slow, at the rate of about 15 sweeps per minute, with the returning stroke traveling a little faster than the treating stroke. Effleurage produces a soothing relaxation and mild hyperemia for the patient while decreasing pain in the superficial soft tissues and reducing muscle tension (Box 7-11).
Pétrissage
Pétrissage involves grasping the skin and underlying muscular tissue while applying a cross-fiber stroking or stretching action to the tissue beneath. Pétrissage is a French word for kneading, although it has also been called pinching. This technique is directed at improving the tissue-fluid exchange, vascularity, and normal texture of subcutaneous and deep soft tissue. This is accomplished through alternate traction, or taking up or squeezing and relaxing movements of a localized mass of tissue held between the thumb and fingers. The hands raise a large fold of skin and underlying muscle between the thumbs and other fingers (Figure 7-19). The tissues are rolled, squeezed, and raised by alternately tightening and loosening the grasp. As the hold is loosened, the tissues are allowed to fall back to their original position because of their elasticity. The fingers should be held close together. The hands work together, changing the direction of the torsion. If the hands slip over the surface or pinch the skin, the maneuver will be painful.
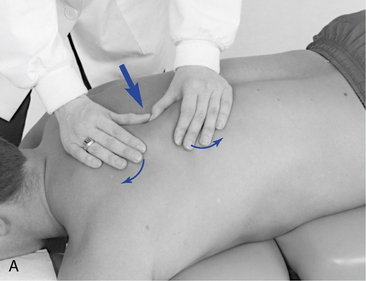

Figure 7-19 Pétrissage (focus is across muscle fibers). A, Two hands grasping. B, Grasping and lifting tissue.
Pétrissage is thought to diminish swelling and fluid accumulations, produce hyperemia in muscle, and improve elasticity and contractility of connective tissue. Furthermore, pétrissage can decrease muscle tone as the lifting, rolling, and squeezing action affects the spindle cell proprioceptors in the muscle belly. As the muscle belly is squeezed, the muscle feels less stretched. The lifting action produces stretch in the tendons, causing a potential reaction by the Golgi tendon receptors. When these two phenomena occur, the sensory input can reflexively relax the muscle. Pétrissage also has the mechanical effect of softening and creating space around the actual muscle fibers and making the tendons more pliable.55 Moreover, it has the potential to break cross-linkage adhesions that have formed between fascial planes, connective tissue, or muscle fibers (Box 7-12).
Roulomont
Roulomont, or skin rolling, lifts the skin away from fascial surfaces beneath; when adhesive areas are encountered, a pull is applied to the skin to allow freer movement (Figure 7-20). Skin rolling is a procedure suitable for long muscles. Skin rolling has been considered a variation of pétrissage. However, with skin rolling, only the skin is lifted from the underlying muscle layer; pétrissage attempts to lift the muscular layer. Skin rolling has a warming and softening effect on the superficial fascia and can cause reflexive stimulation of cutaneous receptors. It can also be used directly over the spine. Areas where the skin does not easily come away from the fascia may have an underlying joint dysfunction problem (Box 7-13).
Tapotement
Tapotement is described as a tapping or vibratory action applied to the soft tissue in a rapid fashion creating a stimulatory effect. The tapping vibration is produced typically through a rapid series of blows by the hands that are held with the palms facing each other. The fingers and wrist remain relaxed as the elbows flex and extend. The ulnar borders of the hands and the fingers produce a rapid multiple percussive stimulation over the area being treated (Figure 7-21, A). In addition, the fingertips can be used to produce a compressive tapping by rapidly alternating wrist flexion and extension (Figure 7-21, B). This procedure is most useful in the extremities. A variation of tapping uses the cupped hand to produce a deep percussive vibration especially useful over the thorax and abdomen (Figure 7-21, C). The vibration is applied perpendicular to the muscle fibers, with an impulse frequency of 8 to 10 sinusoidal vibrations per second. The resulting tonal effect may not immediately be apparent; the average time needed before results can be seen is 2 to 5 minutes. Vibration must be done long enough and at a sufficient intensity to produce reflexive physiologic effects. Vibration is used to tone muscles and to produce sensory stimulation. It may be given with the entire hand or with the fingertips, depending on the area to be treated. Rapid continuous vibrations are transmitted to the skin through movements of the hands. Initially, the hand contacts produce tissue compression, followed by the trembling form of vibration produced by alternating contraction and relaxation of forearm muscles (Box 7-14).
Friction
Friction is the application of moderate, steady pressure, typically with the palmar aspects or edges of the thumbs in small areas. During the application of friction massage, the thumb induces rapid side-to-side or small circular movements, moving the skin over the subcutaneous tissues and muscular layer (Figure 7-22, A). The fingers, palm, or flat part of the elbow can be used as alternative contacts (Figure 7-22, B and C). The purpose of using friction is to move tissue under the skin; therefore, lubricant is usually avoided to prevent sliding of the tissues. The goal is to induce rapid transverse movements through the underlying myofascial or ligamentous tissue (Box 7-15).
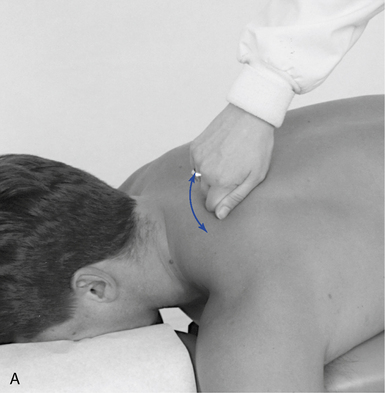

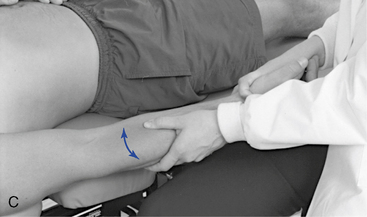
Figure 7-22 Friction. A, Edge of supported thumb moves rapidly across muscle fibers (levator muscle). B, Stabilized fingers move across muscle fibers (rhomboids). C, Forearm and elbow stretch along muscle fibers and move across fibers.
When applied vigorously across the fibers of the tissue treated, it is called transverse friction massage. The treatment goal of friction is to break up adhesions and to encourage absorption of exudates. The focus of friction is to produce a controlled inflammatory response that causes heat and redness from the release of histamine and increased circulation. Although a small amount of edema will occur as water binds with the connective tissue, there should not be any bruising. Friction can also be used in combination with compression and passive joint movement. This is considered a form of myofascial release and is discussed in that section.
Friction massage is a vigorous procedure and because of the forceful nature, the patient’s tolerance must be considered. As the procedure is applied, a “friction anesthesia” will be produced, allowing the contact pressure to increase. Friction massage is generally performed for 30 seconds to 10 minutes, depending on the patient’s tolerance and treatment goals. Friction is a mechanical approach best applied to areas of high connective tissue concentration, such as the musculotendinous junction. Consideration can be given to whether the myofascial tissue in the area to be treated should be in a stretched or relaxed position.
Connective Tissue Massage
Elizabeth Dicke, a German physical therapist, developed connective tissue massage in 1929. Ebner56 defines connective tissue massage as a form of STM carried out in the layers of connective tissue on the body surface. This stroking technique is a form of friction that consists of a tangential pull on the skin and subcutaneous tissues away from the fascia with tips of the third and fourth fingers. It is applied to identified segmental changes in the tension of the skin and subcutaneous and other connective tissue corresponding to the location of head reflex zones. Head zones are hyperalgesic areas of the skin speculated to be to be referred from diseased internal organs. The systematic application of connective tissue massage is time-consuming to learn and apply; however, aspects of this technique can be used without applying the whole system. This technique may have both a reflex (circulation and pain) and a physical (stretching and mobilizing connective tissue) effect.
The essential feature of connective tissue massage is that a tensile strain is applied to the connective tissue to produce the desired physical and reflex effects. The patient is most commonly in a seated position with the knees and hips at right angles. However, the side-posture, prone, and supine positions may also be used. Assessment begins with observation for symmetry, followed by palpation. The palpatory procedure moves the skin against the deep fascia by using the middle and ring fingers to produce small pushing strokes. Comparison is made from side to side, with asymmetric increased tension indicating a problem. The stroke produces a pressure that causes a bulge of tissue. Alteration in the tension of connective tissue will change the size of the bulge and the sensation produced, indicating a compromise in the fascial tissue. A combination of short and long strokes applied to specific regions of the body are done to locate fascial changes. One commonly used procedure incorporates a long vertical stroke performed by the middle and ring fingers, starting along the L5 segment and pulling up along the spine to C7.
Treatment is applied with a long or short stroking action, carried out using the second and third fingertips of the relaxed hand to draw the skin slack (Figure 7-23, A and B). A pulling stroke similar to the one used in assessment is used for treatment. Sufficient tension must be developed between the fingers in the skin; therefore, a lubricant is not used. The treatment strokes start at the sacrum and work up along the trunk and neck. Although connective tissue massage exerts an effect using the skin and subcutaneous tissue, it is primarily a superficial form of STM on the lighter end of the depth spectrum. Cantu and Grodin57 suggest that connective tissue massage can be applied to individuals who have hypersensitivity of the autonomic nervous system, such as in the case of reflex sympathetic dystrophy. The purported effects include a marked hyperemia and sweat gland stimulation. Bruising sometimes occurs after treatment, depending on the degree of capillary fragility.
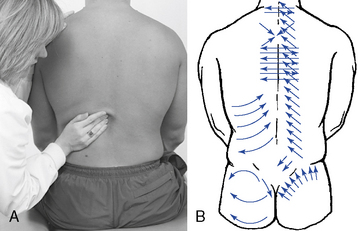
Figure 7-23 Connective tissue massage. A, Second and third fingertips draw skin slack. B, Pattern of long and short strokes.
The mechanism for the effect of connective tissue massage is based on a reflex hypothesis. This procedure is purported to cause a release of a histamine-like substance that acts on the autonomic nervous system. Histamine acts as a powerful vasodilator of small blood vessels and causes an increase in vascular permeability that leads to increased fluid loss from fine blood vessels. It is thought that the mechanical stimulation of the pulling stroke on the connective tissue is an adequate stimulus to elicit the proposed reflex. Excitation of neurologic receptors in the skin produces impulses that travel from the skin either through the somatosensory spinal nerve via a posterior root ganglion to the gray matter or over the vascular plexus to the same segmental sympathetic ganglia or to the ganglia of the neighboring segment.58
Functional Techniques
This group of techniques focuses on the interrelationship of structure and function in the body with the tendency toward self-regulation.59 These procedures place emphasis on motion rather than position and quality of movement rather than quantity of movement. The theory is that dysfunctional motion segments alter neural input, which in turn produce abnormal efferent signals, particularly to the NMS system.59 Functional technique restores normal ease of movement and reduction of abnormal afferent input. These techniques have in common the goal of reducing exaggerated mechanoreceptor and nociceptor input and spindle responses from facilitated segmental muscles, thereby restoring joint mobility and muscle tone. Typically, the involved joint is passively positioned so that the facilitated muscle spindle is shortened, reducing the afferent discharge.
Strain-Counterstrain
Strain-counterstrain uses muscle positioning based on concepts developed by the osteopath, Lawrence Jones, to assist in the reduction of trigger point (tender point) pain, muscle spasm, and joint immobility.60 Dr. Jones noted that acute joint problems were associated with tender points that he called trigger points, although they were not the same as Travell’s or Nimmo’s concepts (see pages 7-28-32). Dr. Jones also serendipitously discovered that patients’ painful complaints could be permanently relieved if the patients were placed for a period in a position of comfort (“position of ease”). From this accidental discovery, Dr. Jones went on to develop a method of examination and treatment procedures used to identify offending triggers (tender points) and inhibit them by moving the offending joint or limb away from pain to a sustained position of comfort.
This procedure is based on the hypothesis that the initially strained (stretched) muscle is not necessarily the only source of the patient’s continued discomfort. Rather, it is theorized that abnormal input and sustained contraction from the muscle that is antagonistic to an overstretched muscle may be the source of continued pain and stiffness. This purportedly occurs during an overstretching injury when the antagonistic muscle is suddenly and maximally shortened, producing an increase rate of gamma motor neuron firing. The initial increased rate of gamma motor neuron activity is theorized to induce sustained contraction of the muscle spindle within the affected muscle. The resultant tension in the intrafusal mechanism causes excitation of the central nervous system, stimulation of alpha motor neurons, and the maintenance of extrafusal fiber contraction. When the involved muscles return to a normal resting length, abnormal tension is maintained as a result of abnormal spindle activity. This produces a cycle of increased spasm and tension in the antagonistic muscle and abnormal pulling forces against the apposing muscles.
Counterstrain theory proposes that restoration of pain-free movement can only be established when the antagonistic muscle is coerced to return to a normal resting length. This is accomplished by placing the involved muscle in a position of maximal shortening, followed by a stretch and slow return to neutral length.60 The position is held for 90 seconds to allow gamma motor neuron activity to decrease and the spindle to reset to normal activity status.
Positional Release Therapy
Positional release therapy (PRT) is a form of counterstrain developed by D’Ambrogio and Roth.61 Its major characteristics include specific body positioning, the use of tender points, and an indirect approach to treatment. Treatment using PRT is accomplished by placing the involved tissues in an ideal position of comfort. This is designed to reduce the irritability of the tender points and normalize the tissues associated with the dysfunction. This ideal position is determined subjectively by the patient’s perception of tenderness and objectively by the reduction in palpable tone of the tender point. PRT theoretically addresses neuromuscular hyperirritability and muscular hypertonicity as mediated by the proprioceptive system.61
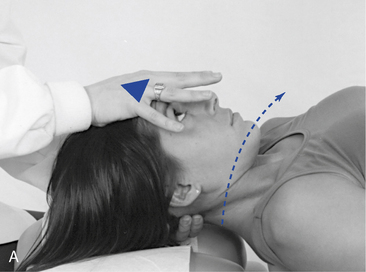
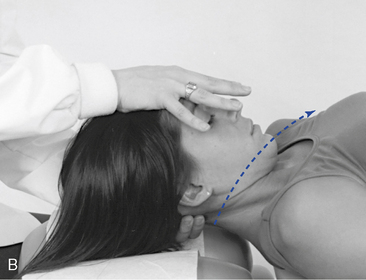
These procedures involve localization of a sensitive myofascial tender point followed by positioning of the muscle and related joint into a position of comfort or ease (Figure 7-24, A and B). Pressure is applied to the tender point while the muscle and related joint are maintained in the position of maximal relaxation. The abnormal reflex and resultant muscle spasm are inhibited by the tender point pressure and opposite counterstrain created by the positioning. The pressure and position are held for 90 seconds, followed by a slow passive return to neutral. A return to normal length of the muscle is achieved through the positional release of abnormal neural reflexive activities. This has led to this procedure also being called positional release technique.


Figure 7-24 Strain and counterstrain (positional release). A, Tender point located on the posterior aspect of the C3 articular pillar. Patient’s head is laterally flexed and rotated away. B, Tender point located at the upper lateral border of the scapula. Patient sits with arm at the side and elbow bent. Clinician grasps the forearm and extends, adducts, and externally rotates the shoulder.
Myofascial Release Technique
Although used for decades, very little has been documented or written about MRT. MRT procedures are the product of a variety of concepts originating from orthopedics, physiotherapy, osteopathy, and chiropractic. Today MRT is most frequently associated with physical therapist John F. Barnes. Barnes62 defines MRT as a whole-body, hands-on approach for the evaluation and treatment of the human structure, focusing on the fascial system. MRT evaluation of the fascial system includes analysis of the human frame by palpating the tissue texture of the fascial layers and observing the rate and rhythm of the craniosacral mechanism.62 Release, in the myofascial release concept, is the tissue relaxation (including muscle relaxation) that follows adequate application of stress on the tissue.59
The goal of myofascial release treatment is to establish functional three-dimensional whole-body symmetry and motion by removing fascial restrictions and restoring the body’s equilibrium.63 The indicated application of this method requires the determination of the best location of entry into the musculoskeletal system, selection of the most suitable types of stress to induce the inhibitory effect, and sensitivity in palpation to react properly to tissue response.64
MRT is reported to reduce muscle spasm and fascial restrictions, eliminating irritation to these pain-sensitive structures and allowing increased ROM.62 Myofascial release is thought to soften connective tissue, rehydrate it, and remold it. This is done by spreading the tissue, pulling or stretching it, and creating motion where the tissue was adhered. The effect of myofascial release is a relaxation of tissue tension and subsequent decrease in myofascial tightness. Therefore, MRT is used to normalize myofascial activity, regain tissue extensibility, and reduce pain.
MRT is performed by applying carefully directed manual forces against soft tissue barriers (Figure 7-25). Deep, long, gliding strokes using the palms, fists, or forearms to engage various layers of the fascia are used to spread and lengthen the fascia. A lifting and twisting motion is used more often than compression.65 When a fascial restriction is identified, gentle pressure is applied in the direction of restriction. This pressure pulls the elastic fibers, producing a springy feel. As the stretch continues, a firm barrier will be engaged, representing the collagenous connective tissue component. Sustained pressure is maintained until a “release” is felt.62 Connective tissue stretching occurs when the tissue is taken to a point of resistance and then stretched. This is usually done across fibers with the muscle in a specific position. Box 7-16 identifies the ways that myofascial releases can occur. MRTs are not always painless, although the initial discomfort typically subsides as the contact is maintained over time.


Figure 7-25 Myofascial release (Barnes method). A, Cervical release to relieve fascial restrictions through the neck and upper back. Patient’s occiput is cradled in the clinician’s hands with cephalic traction sustained without producing too much flexion. B, Alternate cervical release emphasizing the sternocleidomastoid and levator areas.
Active MRT (active release technique [ART]) is a modification promoted by Leahy.66 Leahy asserts that ART is best suited for treatment of soft tissue conditions that fall under the category of cumulative injury disorders.66 These problems result from acute injury, repetitive injury, or a constant pressure-tension injury. The soft tissues are examined for changes in texture, tension, movement, and function. When any of these factors are altered, there are changes in the mechanical function of the joints and soft tissues. The identified affected tissue is placed in a shortened position at the start of treatment. The soft tissue lesion is contacted, pressure is applied, and the tissue is stretched through slow active or passive movements (Figure 7-26).
Manual Resistance Techniques
This general classification of soft tissue manipulative techniques includes those procedures that have varying degrees of contact pressure and joint movement or positioning. They also use varying degrees of muscle contraction from none to strong sustained contractions. Some use light or no contact pressure over painful areas, and others use heavy pressure. This variability has the advantage for these procedures to be applied based on the clinical presentation (acute or chronic) and patient ability (tolerance). These procedures have similar characteristics, which leads to some confusion in terminology and specific intent.
Muscle Energy Technique
MET was developed by Fred Mitchell, D.O., as a procedure that incorporates the use of the patient’s muscular effort in the application of the procedure. The primary effect of MET is to influence joint function, although there will certainly be effects on the muscles being used as well. The aim of MET is to restore normal joint position and function while influencing proper posture. Mitchell’s basic principle is that voluntary muscle contractions are exerted against a precisely executed counterforce to loosen the specifically localized joints for passive articulation during postcontraction relaxation.67 Patient-initiated muscle contractions are used at varying intensities from a precisely controlled position, in a specific direction, against a distinctly executed counterforce. The corrective process requires active patient participation, encouraging the patient to assume responsibility for self-care.64 METs are applied with facilitation and gravity during the lengthening phase, classically with no passive stretching performed by the therapist. However, many modifications and variations have led to different applications of this procedure and significant confusion in nomenclature, as well as in proposed therapeutic intent.
METs involve two opposing forces, the patient’s and the clinician’s, producing isometric or isotonic contractions or both. Variability in the direction, type of contraction (isometric or isotonic), patterns, and amount of force produced by the patient or the clinician serves to distinguish the various forms of MET. To effectively deliver MET procedures, the restrictive barrier must be found and accurately engaged.
The barrier phenomenon was first described in relationship to joints, but it can be applied to nearly all structures of the locomotor system. The barrier concept provides an important distinction between massage procedures and manipulative procedures for the soft tissues. The barrier is perceived by the clinician when the slightest resistance is engaged. Slight overpressure should produce a springing movement characteristic of elastic. Characteristics of specific dysfunctional barriers are identified in Table 7-1.
TABLE 7-1 Types and Characteristics of Dysfunctional Barriers
| Barrier Type | Palpatory Finding | Cause |
|---|---|---|
| Neuromuscular barrier | Elastic quality | Increased myotonus |
| Fascial barrier | Inelastic quality | Fibrosis |
| Passive congestion barrier | Abrupt but fades | Edema |
| Osseous barrier | Abrupt but unyielding | Intraarticular joint locking |
| Anatomic barrier | Hard with increased ROM | Hypermobility, instability |
ROM, Range of motion.
The barrier phenomenon makes accuracy of diagnosis and positioning very important. Localization of the force to the affected spinal level is more important than the amount of force and counterforce (Figure 7-27). Full maximal contraction of the muscles is not required for this method of joint treatment, and often very light force is desirable. It is sometimes necessary to caution the patient not to use too much force. The patient should use only enough force to match that provided by the physician. If excessive force is used, accessory muscles will be brought in, and this detracts from the effectiveness of the treatment on the specific tissues that need to relax. The procedure for applying muscle energy for joint mobilization is detailed in Box 7-17.


Figure 7-27 Muscle energy technique for joint dysfunction (L4–L5). A, Isometric procedure for a right rotational restriction and right lateral flexion restriction with barrier engaged. Patient is instructed to left rotate and left laterally flex against the clinician’s resistance. B, Isotonic procedure for a right rotational restriction and right lateral flexion restriction with barrier engaged. Patient is instructed to right rotate and right laterally flex against the clinician’s resistance.
BOX 7-17 Muscle Energy Technique Procedure for Joint Mobilization
Postisometric Relaxation
METs have undergone significant modification and evolution with many variations. With modification, METs can increase joint mobility and muscle flexibility. PIR is one such evolution. The focus of PIR techniques is on the muscular system and on inducing muscle lengthening, whereas MET focuses primarily on joint changes. However, both MET and PIR affect the joint and related muscles. PIR refers to the effect of subsequent relaxation experienced by muscle after brief periods of isometric contraction. PIR techniques tend to be simplistic and gentle and can be given as home treatment. Because PIR has evolved from MET, both procedures are being used interchangeably. Moreover, modifications to PIR techniques have also occurred.
MET techniques are applied to aid in the lengthening of shortened tissue by reducing the limiting effects of active muscle contraction and contracture. These procedures can be helpful even in instances in which muscle shortening may not be just a product of active muscle contraction but rather a product of contractures within the muscle’s connective tissue. By relaxing the active elements within the muscle, the lengthening procedure may be more effective at stretching the connective tissue elements, normalizing the function of the contractile and noncontractile elements in the muscle.
These MET procedures are based on the observed phenomenon that maximal muscle relaxation often follows strong isometric muscle contraction. Sherrington68 first noted this phenomenon in 1909. This principle is applied in the variation of MET known as PIR. Modified forms of MET involve three phases: contraction, relaxation, and stretch. The patient contracts into the resistance provided by the clinician. This is followed by a period of muscle relaxation and passive stretching by the therapist (Figure 7-28).

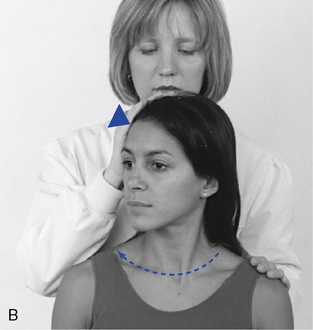


Figure 7-28 Example of modified muscle energy technique applied for decreased right cervical rotation.
Different models of how these procedures may produce a therapeutic effect have been presented, but the precise mechanism by which these techniques accomplish a soft tissue change remains unclear. One theory stresses the role of the GTOs. In this model, sustained isometric contraction increases tension in the already contracted muscle, causing the Golgi receptor system to sense the increased tension and reflexively induce muscle relaxation or lengthening.
Another method of induced muscle relaxation is generated by taking advantage of the phenomenon of reciprocal inhibition (RI). When a muscle contracts isometrically, its antagonist is inhibited, and the antagonist relaxes immediately after the contraction. This principle is applied in procedures that imitate isometric muscle contraction in the direction of reduced flexibility.
PIR appears to work best in chronic cases, and RI is better in acute settings.69 However, both may be used in either case, providing that no pain is produced or no attempt is made to force or stretch joint structures.69 When applying PIR, the isometric contraction phase of treatment is held for approximately 7 seconds (range of 4 to 10 seconds; increasing contraction time enhances the effect of PIR) and the relaxation and passive stretching phase lasts approximately 15 seconds (Figures 7-29 and 7-30). The isometric contraction should be of minimal force, and it is important that it equal the force exerted by the patient and be unyielding. The patient should be instructed to match the resistive force of the doctor and not overpower the doctor. Failure to maintain the position and failure to reach the barrier accurately will make the treatment less effective.


Figure 7-30 Postisometric relaxation procedure for the hamstring muscle.
The barrier concept is very important to the application of PIR techniques. During the relaxation phase, the clinician applies gentle pressure and lengthens the muscle to engage a new barrier, the point at which restriction or pain is again felt. This process is repeated using the newly achieved ROM until the restriction of mobility is reduced, the spasm of the muscle is relieved, and the intensity of the pain can be alleviated (Box 7-18).
The patients themselves can also carry out many useful types of self-administered PIR. After patient education, such procedures are useful in bridging the intervals between patient visits. Although they are useful, they have limitations in their efficiency. This is particularly true in the upper cervical and occipital regions.
Evjenth and Hamberg70 recommend modifying PIR by stimulating the antagonistic muscle or muscles at the end of the treatment sequence. This variation of PIR incorporates an additional active contraction on the part of the patient. In this method, the patient assists in producing the desired movement after the stretching phase by actively contracting the antagonist muscles. This is accomplished by having the patient actively increase movement in the direction of restriction against mild resistance applied by the clinician. This modification of PIR is referred to as the contract, relax, antagonist contract method or RI. When a muscle contracts isometrically, its antagonist is inhibited from contracting. Therefore, by isometrically contracting the antagonist of a shortened muscle, the shortened muscle relaxes through RI. Contraction of antagonist muscles may be useful when the shortened (agonist) muscle is too painful to contract. There are a number of other procedures that use the antagonist contraction mechanism.
Proprioceptive Neuromuscular Facilitation
PNF was developed by Herman Kabat, M.D., and Margaret Knott, P.T., as a method to treat patients with neurologic dysfunction. Dr. Kabat developed the PNF method during the 1950s after being introduced to the work of Sister Elisabeth Kenny, the “Kenny method,” and Sister Kenny’s treatment of polio patients. The early focus of their methods paralleled that of Sister Kenny and focused on the treatment of patients with paralysis and polio. Over the years, the procedures have evolved and techniques have been applied to a broadening array of conditions affecting motor function and the NMS system. It is now common for these procedures to be applied in a wide variety of conditions, ranging from rehabilitation of stroke and spinal cord injury patients to the management of common NMS injuries and disorders.71 Kabat’s conceptual goals for PNF were to neurologically strengthen weak muscles. Mitchell, in developing MET, adapted these concepts for use in joint mobilization, which were in turn modified to release muscle shortness (PIR). These procedures, with their proposed mechanisms and uses, continue to evolve.
PNF is defined as the use of proprioceptors to hasten or make easier the learning of a neuromuscular task.64 Patients are directed through a series of complex movement patterns directed to effect maximal elongation of muscle. These patterns involve spiral and diagonal movements and are modeled after normal patterns of motion associated with tasks and movements of daily living. It is through the learning or relearning (facilitation) of these complex patterns that PNF is speculated to stimulate proprioceptors and hasten recovery. PNF is considered by its developers to be a philosophy of treatment rather than a technique. It purports to have a global effect on function, involving multiple muscles and multiple planes of movement.
The basic neurophysiologic principles that serve as a foundation for this procedure include the concept that a muscle response can be influenced by resistance, stretch reflex, and other proprioceptive input. Therefore, PNF uses the concepts of resistance, stretch reflex, approximation, traction, and manual contacts to facilitate efficient motor or recruitment patterns. Through applying these basic principles, the patient’s postural responses, movement pattern, strengths, and endurance can be assessed and theoretically enhanced.
Physical manipulations using proprioceptive neuromuscular technique often use hold-relax-stretch procedures to obtain an increase in ROM and normalize muscle function about a joint. The hold-relax-stretch technique and terminology is comparable with the contract-relax-stretch technique in both application and effect.72 The PNF approach is based on the ability to identify dysfunctions of neuromuscular control using observation, palpation, and motion evaluation. The evaluation procedures used to identify dysfunctions are listed in Box 7-19.
BOX 7-19 Proprioceptive Neuromuscular Facilitation Evaluative Procedures for Identifying Dysfunction
Definitions and descriptions for the evaluation procedures listed in Box 7-19 follow. Passive mobility assesses a PNF diagonal for the presence of an accessible passive ROM and the patient’s ability to relax. Active mobility adds active muscle contraction to move the part through the PNF diagonal that was previously tested passively. The quality of movement initiation is evaluated for sluggishness, delayed response, hyperactive response, or inappropriate recruitment.
Coordination and control are evaluated with the addition of resistance to initiated movements to identify deviations of movement or jerky and uncoordinated movements. Again through the use of resistance, the strength of muscle and speed of contraction can be evaluated for insufficiencies. A combination of isotonics assesses the performance of and transition between the types of isotonic contractions (concentric, eccentric, and maintained). In addition to isotonic contractions, isometric contraction is evaluated for weakness.
The ability to reverse direction is a necessary feature of the neuromuscular system, and inadequate control, speed, or strength of the reciprocal movement results in altered arthrokinematics. Identification of a functional imbalance of the agonist and antagonist muscles is important because it may result secondarily from structural dysfunction, disc herniations, or overuse syndromes. Trunk control depends on the integration of stability and mobility and is essential for efficient function and health of associated structures.
The extensive array of procedures and principles associated with PNF make it a difficult procedure to classify. Although initially perceived as a program of rehabilitative exercise, it is clear that many of the techniques applied in PNF are not easily categorized as exercise. The common incorporation of muscular effort during the application of these procedures has led to the common classification of PNF as an MET, which is likely an oversimplification. There are nine variations in the application of PNF that can be applied based on the patient’s functional needs (Box 7-20). Each of these has a specific purpose, indication, and application.
Rhythmic Initiation
Rhythmic initiation (Figures 7-31 and 7-32) is used to evaluate and treat the patient’s ability to allow passive motion; actively contract in a smooth, rhythmic fashion; and perform movement at a constant rhythm against resistance. It is therefore used to treat those functions that affect the initiation, speed, direction, or quality of the contraction. To apply the procedure, the patient is positioned in a posture conducive to relaxation and the clinician performs the desired joint movement passively. Once a smooth and rhythmic passive movement is achieved, the clinician asks the patient to minimally assist with the movement. Resistance by the clinician is applied as the patient increases active participation.
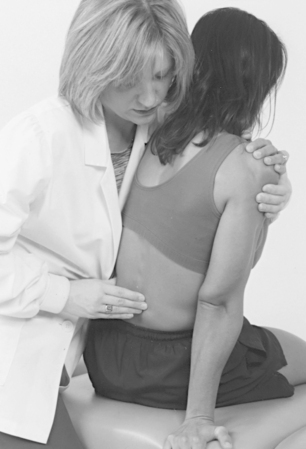
Figure 7-31 PNF rhythmic initiation for acute pain. Patient is positioned in a posture conducive the relaxation, and the clinician produces the desired motion passively. Patient then minimally assists with the movement.


Figure 7-32 Proprioceptive neuromuscular facilitation rhythmic initiation facilitating gluteus maximus contraction (hip extension) activity for low back stability. A, Hip extension (crawling) begins. B, Hip extension is complete. This procedure is done passively, actively, and with resistance to facilitate trunk stability.
Combination of Isotonics
Combination of isotonics (Figure 7-33) is used to evaluate and develop the ability to perform controlled, purposeful movements. It is indicated for the treatment of deficiencies in strength, ROM, and decreased neuromuscular coordination. It is applied to problems of concentric contraction, eccentric contraction, or efficient maintained (isometric) contraction. Concentric, eccentric, and isometric contractions of the agonist muscle pattern are combined in any sequence with relaxation to perform controlled, purposeful movements.


Figure 7-33 Proprioceptive neuromuscular facilitation combination of isotonics applied to the scapula patterns. A, Scapula is protracted, elevated, and abducted. B, The scapula is retracted, depressed, and adducted. The sequence of treatment is: (1) passive movements produced by the clinician, (2) some patient assistance with the movement pattern, (3) Fall active movement by the patient, and (4) resisted movement.
Repeated Quick Stretch
Repeated quick stretch incorporates the repeated use of a stretch reflex to assist with initiation of a muscular response. It is therefore indicated to reduce fatigue, improve endurance, and increase the patient’s awareness of the motion. Repeated excitation of a pathway in the central nervous system promotes transmission of impulses through that pathway. It can be applied with elongation or contraction. The muscle components will be placed in either a stretched or approximated position. The patient is then instructed to initiate a reflex contraction that is resisted by the clinician.
Reversal of Antagonists
Reversal of antagonists is designed to influence the antagonistic muscle groups that fail to work in accordance with the demand of a specific activity. It is achieved by applying resisted alternating concentric contractions or by resisting alternating isometric contractions.
Contract-Relax
Contract-relax uses muscle tension developed through concentric contraction to facilitate relaxation. It is used to increase ROM of the myofascial unit by facilitating relaxation and improving extensibility of the myofascial tissues. The segment to be treated is placed at its point of limitation within the movement pattern, and resistance is given to a concentric contraction of either the restricted agonist or antagonist. After the contraction, the patient is asked to relax completely, and the segment is passively or actively taken into a new available ROM.
Hold-Relax
Hold-relax is used to facilitate relaxation and increase ROM using an isometric rather than isotonic contraction. It is indicated when pain limits the use of isotonic contraction. It is applied by placing the joint in a pain-free position and then slowly invoking isometric contraction. The patient is told to hold the position while a resisted stress is applied.
Ischemic compression
Ischemic compression is a generic procedure, the definition of which has become confused because of the many proprietary approaches that use it. Receptor-tonus (Nimmo), trigger point therapy (Travell and Simons), neuromuscular technique (Chaitow and St. John), myotherapy (Prudden), ART (Leahy), shiatsu, and acupressure have all used this term to describe aspects of their individual therapeutic approach or mechanism of treatment.
The advocates of these procedures have different explanations and theories, but the clinical application is very similar: deep manual pressure over tender muscular nodules. Travell and Simons73 were the first to use the term ischemic compression to describe the manual pressure applied over myofascial trigger points. Many methods of trigger point therapy, using forms of ischemic compression, including PIR and spray-and-stretch techniques, are thought to achieve their results through neurologic mediation of reflex pathways.
Several theories have been suggested to explain the mechanism of ischemic compression. Travell and Simons73 believe that by holding pressure over a specific site, ischemia is induced to the sensory nerves, producing a nerve block from lack of oxygen. Travell and Simons73 believe that the deep pressure produces a concentrated stretch to contracted sarcomeres associated with a trigger point, creating a separation of the actin-myosin heads. Another explanation is that after the release of pressure, a reflex vasodilation and hyperemia occur, producing a circulatory increase capable of removing chemical irritants and metabolites and bringing in oxygen and adenosine triphosphates. The last theory considers the mechanism that deep pressure produces pain that hyperstimulates interneurons in the dorsal horn to release endorphins that block pain perception. In all likelihood, the effects of ischemic compression are the result of a combination of mechanisms.
Receptor-Tonus Technique (Nimmo)
Dr. Raymond Nimmo was one of the first chiropractors to focus on the soft tissue component of dysfunction and subluxation, advocating specific soft tissue treatment since 1950. Clinically, Nimmo observed spots on the shoulders that, when pressed, referred pain to various areas that he called noxious generative points.74 In 1952, he discovered the work of individuals such as Travell and later Simons in researching myofascial pain and dysfunction. The term Travell used for the painful areas in the myofascia was trigger points. Nimmo called the procedure for treating trigger points the receptor-tonus technique to emphasize his theory that it is a reflex technique and not a form of massage therapy.75
In the Nimmo method, evaluation and treatment emphasis is placed on posture and related muscular involvement. The soft tissues are palpated for tenderness, spasm, and trigger points with their characteristic patterns of referred pain. Nimmo devised treatment procedures that involved the application of firm manual pressure at the site of the trigger points. Nimmo technique uses deep pressure applied directly over the irritable lesion for approximately 5 to 7 seconds to produce the compression effect.75 76 77
The pressure is applied evenly throughout the treatment and then is quickly released. As pressure is applied, the patient will feel local or referred pain or both, which usually increases in intensity even though the manual pressure remains steady. Once the pressure is released, the initial pain intensity will slowly drop to a lower level. This process is repeated over the same trigger point once or twice more during a single office visit. Methods of applying pressure include the thumb, the index or middle finger, the elbow, a pincer grasp (thumb against the middle and index fingers), a knife-edge contact (ulnar side of the hand), and a T-bar (a mechanical hand-held device with a rubber tip) (Figure 7-34). The steps involved in Nimmo’s form of ischemic compression are summarized in Box 7-21.


Figure 7-34 Nimmo receptor-tonus technique to disperse a trigger point in the levator scapulae muscle using thumb pressure (A) and a T-bar (B).
Before treating a trigger point for a second or third time on the same visit, it is important to assess the muscle tissue for changes in tension and nodularity. Many times after the first application of pressure, the patient notes a significant reduction in the local or referred pain or both. Additional treatment of a trigger point on the same office visit should not be done if substantial decrease in tension or nodularity is noted after the first application of pressure. Moreover, if the trigger point still does not show signs of improvement after three applications of treatment, an interval of a few days is recommended before attempting further treatment. Common mistakes are using excessive pressure and treating patients too frequently. Excessive pressure, beyond the compliance of the tissues, becomes a form of trauma that may result in a hematoma or new trigger point formation.
Frail patients or those with capillary fragility, vascular disease, or a history of corticosteroid use should be treated very gently to avoid iatrogenic sequelae. Larger muscles, such as the gluteal group, may require more pressure to achieve ischemic compression, whereas small muscles, such as the suboccipital group, require very little pressure. The clinician must always work within the pain tolerance of the patient; when in doubt, it is wiser to use too little pressure than too much.
It also appears that even patients with well-developed musculature develop some post-treatment soreness the day after a treatment and should be advised accordingly. It is recommended that a day or two be interposed between office visits and that patients get treated on a twice-weekly basis (three times weekly in acute cases). This allows the muscle tissue a chance to heal from any treatment microbruising and gives the nervous system a chance to reestablish equilibrium in the sensory-motor reflex pathways. Some chiropractors perform daily spinal manipulations with good results. However, daily treatments with Nimmo’s method may lead to delayed healing from post-treatment bruising and is not recommended.
Nimmo postulated that local application of deep pressure hyperstimulates nociceptors, which in turn produce neurologic modulation, resulting in reflex inhibition of motor output and a reduction of muscle tonus. He suspected a neurologic explanation of treatment results because patients reported instantaneous pain relief after a treatment. He reasoned that only the nervous system was capable of creating changes in muscle tone within a few seconds. Clinically, release of contracted muscle has been noted to occur before the usual 5- to 7-second application time has finished. Receptor-tonus technique is therefore presented as a reflex technique that is thought to reduce muscle tonus through reflexes mediated by the central nervous system.
Trigger Point Therapy (Travell and Simons)
Janet Travell,73 a medical doctor, placed a significant emphasis on the role of the myofascia in health and disease. She was the first to use the term trigger point to describe the tender nodules in the soft tissues. Travell and Simons73 define a trigger point as a hyperirritable spot, usually located in a taut band of skeletal muscle, that is painful on compression and can give rise to characteristic referred pain, tenderness, and autonomic phenomena.
Evaluation consists of postural assessment to identify gross muscle imbalances and specific palpation of the myofascia. Charts have been developed identifying the referral patterns of pain that are specific to individual muscles (Figure 7-35). Examination findings are summarized in Box 7-22. Travell73 promotes the use of vapocoolant spray while the irritable tissue is being stretched, as well as the injection of an anti-inflammatory medication (e.g., procaine) into the trigger point.
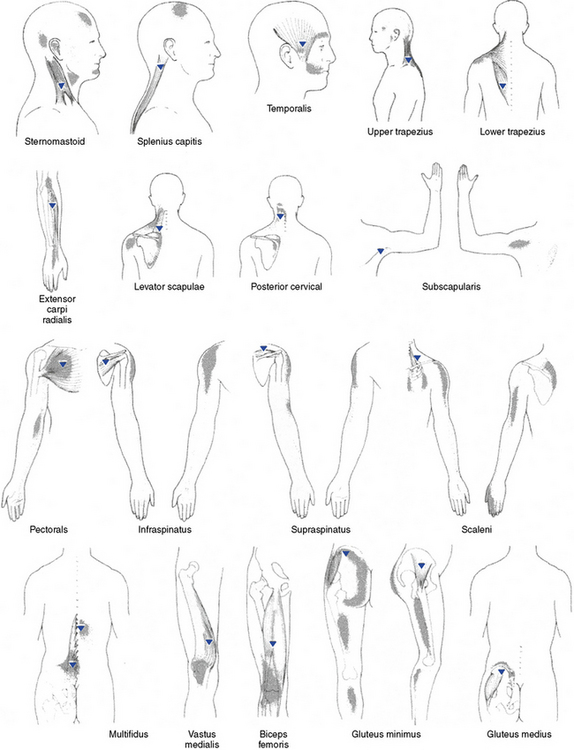
Figure 7-35 Chart of common trigger points (triangle) and referral patterns.
(Modified from Chaitow L: Modern neuromuscular techniques, London, 1996, Churchill Livingstone.)
BOX 7-22 Examination Findings for Myofascial Trigger Points
Manual pressure is also advocated to inactivate a trigger point. Travell and Simons73 were the first to use the term ischemic compression to refer to this procedure. The length of applied pressure is significantly longer in duration than the ischemic compression method described by Nimmo. Travell’s method uses firm digital pressure with deep stroking massage, kneading massage, or vibratory massage to produce hypoxia, followed by a reactive hyperemia. Pressure is gradually increased over a period of 30 to 60 seconds or until the trigger point tenderness is eliminated. Massage, stretch without spray, ultrasound, heat, drug therapy, biofeedback, and transcutaneous electrical nerve stimulation (TENS) are all discussed as alternative means to inactivate a trigger point.
Body wall reflex techniques
Body wall reflex techniques incorporate a number of different procedures. All are applied to identify a wide variety of different types of discrete soft tissue changes that are sensitive to palpation. The explanation for the presence of this palpatory sensitivity is a reflex pain mechanism. With prolonged pain impulses, a vicious cycle that spreads through an internuncial pool with connections upward, downward, and across the spinal cord, potentially reaching the thalamus occurs. Depending on the extent of these connections, it is possible to detect the presence of pain and sympathetic disturbance at a distance from the site of injury and sometimes on the other side of the body.
A factor common to the various reflex systems is that the irritable lesion appears to be situated in fascial tissue.78 The one thing that all of these reflexes seem to have in common is that they are all responses to various types and degrees of tissue injury, including physical trauma, infection, degeneration, and chemical injury.78
When a body wall reflex is present, there is the potential for negative effects on the skin locally, changes to blood and lymph flow, and neurologic stimulation. It is believed that intelligent and scientific manipulation of the skin and soft tissues of the body places the physiologic status of the skin at an optimum, invigorates the circulation of blood and lymph, and alerts the central and peripheral nervous systems.79
There is much overlap of the various body wall reflexes, suggesting that each purveyor recognized a similar characteristic but explained it differently. Moreover, if all the body wall reflex points described in acupuncture and those points described by Travell (trigger points), Chapman (lymphatic reflexes), Jones (strain-counterstrain), Bennett (vascular reflexes), and others were placed together on one map of the body surface, the entire body surface would be covered.78 Furthermore, many of the referred pain patterns from visceral disease coincide with these points. This implies that the body wall is rich in receptors and can easily serve as a source of noxious irritation to the entire body. Although there are a number of different names with different philosophical intents, many procedures are very similar in application.
Acupressure Point Stimulation
Acupressure is a method of massage or point pressure applied to acupuncture points for the usual purpose of producing analgesia.64 Much has been written on the clinical aspects of acupuncture, acupressure, and meridian therapy. Acupuncture points are organized along meridians that have no known neurologic or vascular pattern. There appears to be a measurable change in electrical potential in irritable points, and they can be treated by electrical stimulation, needle application, or manual pressure. Theoretically, blockage or other dysfunction in the meridian causes a departure from health.29
There is a growing body of clinical research exploring the effectiveness of acupuncture. As with any treatment procedure, there are a number of contradictory studies. In a randomized single blind trial examining the effects of acupuncture on chronic myofascial neck pain, acupuncture was found to produce a modest pain reduction.80 In a study of diabetic patients with chronic painful peripheral neuropathy treated with acupuncture analgesia, it was found that acupuncture was a safe and effective therapy for long-term management of painful diabetic neuropathy, although its mechanism of action could not be determined.81 Acupressure was studied for effectiveness in reducing nausea and vomiting of pregnancy. The results indicated that acupressure was effective in reducing symptoms of nausea but not frequency of vomiting in pregnant women.82 A small population study on acupuncture for neck pain revealed no significant difference between acupuncture and placebo, although both groups demonstrated moderate improvement. The conclusion was that acupuncture may have no greater effect than a placebo.83 Ernst84 reports in a systematic review of the literature that the results of studies are highly contradictory with many trials suffering from methodologic flaws. In a randomized placebo-controlled clinical trial of acupressure for weight loss, it was concluded that acupressure appeared to be safe but did not promote significantly greater weight or fat loss, nor did it promote a decline in blood pressure.85 A particularly disturbing concern was identified in an article about acupuncture for chronic conditions in the United Kingdom. The survey86 revealed that acupuncture was widely used in the treatment of chronic pain but that one fifth of the practitioners had not received any formal training in acupuncture. This brings to light concerns that many individuals may be practicing forms of complementary care without adequate training. The conclusions of a consensus process on acupuncture identified that there were many studies of potential usefulness, but that these studies provide equivocal results because of flaws in design and sample size.87 However, promising results exist demonstrating efficacy of acupuncture in adult postoperative and chemotherapy nausea and vomiting.87 Furthermore, there are conditions such as addiction, stroke rehabilitation, headache, menstrual cramps, tennis elbow, fibromyalgia, myofascial pain, osteoporosis, LBP, carpal tunnel syndrome, and asthma in which acupuncture may be useful as an adjunct treatment or an acceptable alternative or may be included in a comprehensive management program.87
Acupuncture points are usually located beneath the skin, although at times they are deep enough to require penetration of the needle to reach tendons and ligaments. It is thought that an acupuncture point becomes active and in need of treatment because of some form of reflex stimulation. They become sensitive to pressure, which therefore serves as a diagnostic finding. Acupuncture points are located in palpable depressions, with the skin over the point being somewhat thinner.88 Beneath each acupuncture point lies a combination of tissues including fibrous tissue, fat, nerves and nerve trunks, large veins, muscle, and tendon receptors. Therefore, a number of tissues are simultaneously affected by the application of an acupuncture needle or finger pressure.
Active acupuncture points will typically be sensitive to correctly applied pressure and can often be neutralized by manual pressure or a combination of chilling, manual pressure, and stretching.78 Acupressure is typically applied with the fingertip to produce pressure in a circular, transverse, or deep fashion (Figure 7-36). The applied pressure should produce some local tenderness that decreases during the treatment session. The pressure is usually applied for 30 to 90 seconds, although one point can be treated for as long as 3 to 4 minutes. To sedate an overactive acupuncture point, up to 5 minutes of sustained or intermittent pressure or rotary massage maybe required. To stimulate an acupuncture point, pressure is applied from 20 seconds to 2 minutes. The caveat is that pressure sustained beyond a certain point can produce the opposite effect.
Acupressure and acupuncture are theorized to have an effect on pain reduction through the modulation of endorphin levels64 or through the stimulation of local mechanoreceptors and nociceptors (stimulus-produced analgesia) or both. Nociceptor activity may be reduced by the activation of sensory mechanoreceptors and nociceptors in the involved myofascial area.64 The nerve reflex theory of acupuncture contends that when an abnormal condition occurs in an internal organ, alterations will take place in the skin and muscles related to that organ by means of the nervous system. Reflex symptoms are classified into sensation reflexes, interlocking reflexes, and autonomic system reflexes. A sensation reflex occurs when an abnormal impulse travels to the spinal cord and the reflex action causes a hypersensitivity reaction in the skin. An interlocked reflex occurs when an abnormality in any internal organ causes a limited contraction or stiffening of muscles in an area near the part of the body that is connected neurologically to the affected organ. An autonomic system reflex occurs when abnormalities in the internal organs set up a reflex action in the sweat glands, sebaceous glands, pilomotor muscles, and blood vessels in the skin. Acupuncture points represent areas of abnormal physiologic activity that produces a continuous, low-level input to the central nervous system.89 This might lead to a combining with noxious stimuli from other structures innervated by the same segments. Melzack, Stillwell, and Fox89 report and that there is a 70% correlation between trigger point maps and acupuncture point charts.
Chapman (Neurolymphatic) Reflexes
The surface changes associated with Chapman reflexes are presented as palpable and are thought to be from contractions found in the deep fascia, located at specific points. The amount of tenderness is an important consideration in differentiating the contractions from subcutaneous fat globules. These palpable changes are located in specific anatomic areas on the anterior and posterior aspects of the body and are reported to be associated with specific viscera. The palpatory findings may vary in size from a pellet to a large bean. It is thought that these reflexes can be used as a diagnostic aid to locate a pathologic change without knowing its nature and to influence visceral function through nervous system input. Frank Chapman, D.O., was of the opinion that these body wall reflexes are clinically useful for diagnosis of visceral pathologic conditions; for influencing the motion of fluids, mostly lymph; and for influencing visceral function through the nervous system.
The anterior reflexes are located in the intercostal spaces near the sternum, and the posterior reflexes are found along the spine midway between the spinous processes and the tips of the transverse processes (Figure 7-37). There are also points located on the pelvis and the thighs. However, points on the surface of the body are never likely to be precisely located or identifiable by description of anatomic position, although general identification is possible. Therefore, in terms of charts and maps, the positions identified are approximate, and there is great variation from individual to individual.
Figure 7-37 Chart for the location of Chapman reflexes (neurolymphatic).
| Reflex | Symptoms or area |
|---|---|
| 1 | Conjunctivitis |
| 2 | Nasal problems |
| 3 | Arms (circulation) |
| 4 | Tonsillitis |
| 5 | Thyroid |
| 6 | Bronchitis |
| 7 | Esophagus |
| 8 | Myocarditis |
| 9 | Upper lung |
| 10 | Neuritis of upper limb |
| 11 | Lower lung |
| 12 | Small intestines |
| 13 | Gastric hypercongestion |
| 14 | Gastric hyperacidity |
| 15 | Cystitis |
| 16 | Kidneys |
| 17 | Atonic constipation |
| 18 | Abdominal tension |
| 19 | Urethra |
| 20 | Arm and shoulder pain |
| 21 | Cerebral congestion (paralysis and paresis) |
| 22 | Clitoral irritation or vaginismus |
| 23 | Prostate |
| 24 | Spastic constipation or colitis |
| 25 | Leukorrhea |
| 26 | Sciatic neuritis |
| 27 | Torpid liver (nausea, fullness, malaise) |
| 28 | Cerebellar congestion (memory and concentration) |
| 29 | Otitis media |
| 30 | Pharyngitis |
| 31 | Laryngitis |
| 32 | Sinusitis |
| 33 | Pyloric stenosis |
| 34 | Neurasthenia |
| 35 | Wry neck (torticollis) |
| 36 | Splenitis |
| 37 | Adrenals (allergies, exhaustion) |
| 38 | Mesoappendix |
| 39 | Pancreas |
| 40 | Liver and gallbladder congestion |
| 41 | Salpingitis or vasiculitis |
| 42 | Ovaries |
| 43 | Uterus |
| 44 | Uterine fibroma |
| 45 | Rectum |
| 46 | Broad ligament (uterine involvement) |
| 47 | Groin glands (circulation and drainage of legs and pelvic organs) |
| 48 | Hemorrhoids |
| 49 | Tongue |
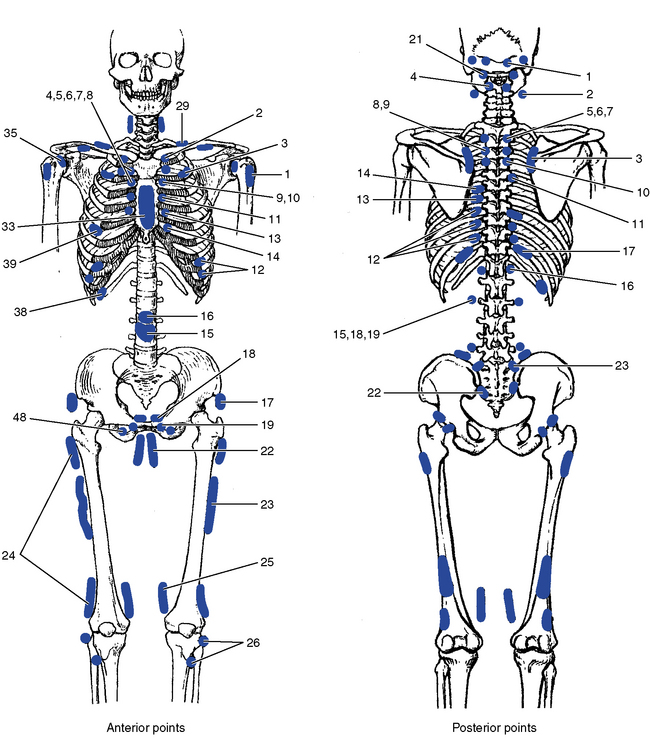
Chapman reflexes are treated by light digital pressure applied to the anterior point and then the posterior point. After the pad of the middle finger has contacted the surface locus, a firm, gentle contact is maintained, and a rotary motion is imparted to the finger through the arm and hand to express the fluid content of the locus into the surrounding tissues (Figure 7-38). The actual application to a given reflex is expressed in terms of seconds, but in practice it is actually determined by a response to palpation. Therefore, treatment time may vary from 20 seconds to 2 minutes or more.78 If the sensitivity of the reflex point has diminished, no more treatment is applied. If the sensitivity of the reflex point is unchanged, a second application is applied. The application of pressure should follow the guideline that overtreatment is counterproductive and may produce an unwanted effect.


Figure 7-38 Treatment of Chapman (neurolymphatic) reflex for sinus involvement, using rapid circular massage over anterior reflex located between the second and third intercostal spaces parasternally (A) and posterior reflex located over the lamina of C2 (B).
The proposed mechanism by which these reflexes located in the intercostal spaces act is through stimulation of receptors lying between the anterior and posterior layers of the anterior intercostal fascia and acting on the intercostal nerve. The intercostal nerve innervates the internal and external intercostal muscles and through its connection with sympathetic fibers can affect the intercostal arteries, veins, and lymph nodes. Impulses from afferent and efferent vessels draining these tissues may increase or decrease because of the stimulation. With involvement of sympathetic fibers associated with specific tissue sites, lymph nodes of vital organs can be affected.78
Regardless of the proposed mechanism, there is some research evidence to support the clinical application of Chapman reflexes. In a study determining whether stimulation of a Chapman reflex could reduce blood pressure, it was found that there was no effect on blood pressure but that there was an alteration in aldosterone levels.90 Many hypertensive patients have high aldosterone and low renin levels affecting the renal tubules and causing sodium retention. Abnormalities in aldosterone levels have been shown in populations of essential hypertension. Stimulation of Chapman reflexes caused a consistent lowering of aldosterone levels. It was suggested that not enough time was allowed to see the blood pressure lower, because even with drugs that lower aldosterone, it takes 5 to 7 days for the blood pressure to lower.
Bennett (Neurovascular) Reflexes
Terrence Bennett, D.C., described reflex points mainly on the skull but also on other body parts that he believed were irritable reflexes reflecting the vascular condition of organs.91,92 These reflex points are used both diagnostically and therapeutically. Bennett developed the neurovascular dynamics technique, which he proposed alters and restores autonomic homeostasis as a means to treat visceral and functional physiologic changes.
Bennett describes the palpable tissue changes in much the same way as Chapman: as a change in texture when the tissue is contracted or indurated. Many of the points are located on the head, although there are some on the anterior aspect of the torso as well (Figure 7-39). Treatment of Bennett reflexes consists of a slight degree of digital pressure combined with a slight stretching or tugging of the skin (Figure 7-40). As the skin is stretched, the fingertips are drawn apart slightly and a yielding sensation occurs. Also perceived within a few seconds after the contact is taken is a slight pulsation, believed to be from the microscopic capillary bed. If no pulsation is perceived, change direction of the skin stretch. The contact is maintained until a response is noted in the form of tissue alteration, relaxation, and pulsation. Treatment could take from a few seconds to a couple of minutes for these changes to emerge. As with other body wall reflex techniques, caution must be given not to overtreat.
Figure 7-39 Chart for the location of Bennett reflexes (neurovascular).
| Reflex | Area affected |
|---|---|
| 1 | Parotid gland |
| 2 | Cardiac sphincter |
| 3 | Liver |
| 4 | Gallbladder |
| 5 | Pancreas |
| 6 | Pylorus |
| 7 | Second segment of duodenum |
| 8 | Third segment of duodenum |
| 9 | Fourth segment of duodenum |
| 10 | Kidneys |
| 11 | Ileocecal valve |
| 12 | Internal rectal sphincter |
| 13 | Appendix |
| 14 | Bladder |
| 15 | Prostate or uterus |
| 16 | Spermatic cord or ovary |
| 17 | Super-renal |
| 18 | Anterior pituitary |
| 19 | Posterior pituitary |
| 20 | Thyroid |
| 21 | Carotid sinus |
| 22 | Aortic sinus |
| 23 | Heart tone |
| 24 | Subclavian lymphatics |
| 25 | Femoral lymphatics |
| 26 | Maxillary sinus |
| 27 | Bronchial region |
| 28 | Frontal-emotional |
| 29 | Vagal |
| 30 | Parietal |
| 31 | Temporal-emotional |
| 32 | Anterior fontanel |
| 33 | Midsylvian |
| 34 | Fissure of Rolando |
| 35 | Frontal eye muscles |
| 36 | Extrinsic eye muscles |
| 37 | Posterior fontanel |
| 38 | Menopause-glandular |
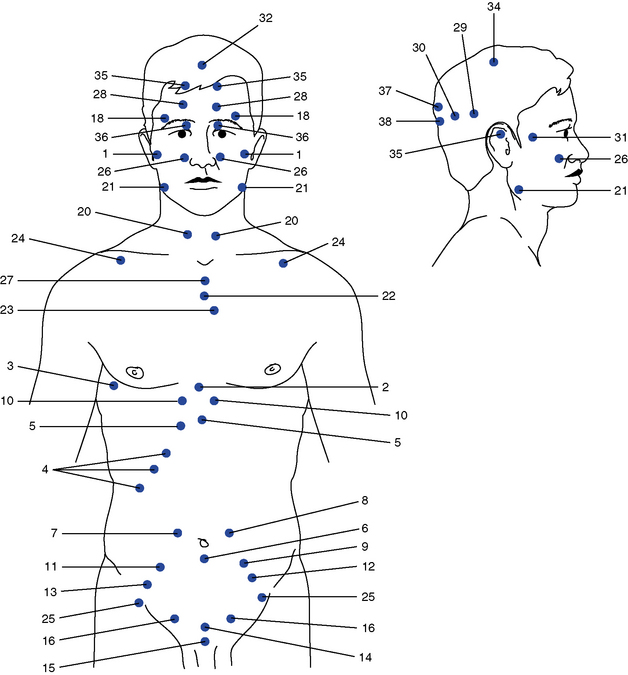

Figure 7-40 Treatment of Bennett (neurovascular) reflex for the pancreas, holding a light tugging pressure just medial to the sixth and seventh rib heads until a pulsation is felt.
Bennett reflexes are hypothesized as being viscerosomatic reflexes. Therefore, they are believed to have the same characteristics and neurologic mechanisms as viscerosomatic reflexes. Persistent pathologic conditions in visceral structures have the theoretic potential to induce reflexive dysfunction in somatic structures. Visceral disease or dysfunction may activate the autonomic nervous system through connections with the lateral horn cells in the cord to produce vasomotor, trophic, visceral, or metabolic changes. Viscerosomatic reflexes result from afferent stimuli arising from dysfunction of a visceral structure. The reflex is initiated by afferent impulses arising from visceral receptors that are transmitted to the dorsal horn of the spinal cord, where they synapse with interconnecting neurons. The stimuli are then conveyed to sympathetic and motor efferents, resulting in changes in the somatic tissues.
It has been suggested that the body wall manifestations of visceral disease are an integral part of the disease process, rather than just physical signs and symptoms.93 Korr suggests that viscerosomatic reflex activity may be noted before any clinically identifiable symptoms of visceral change and therefore has diagnostic and prognostic value,94 although the definitive etiologic factors and the characteristic response of the individual reflex are still unknown. There have been no clinical trials using Bennett reflexes reported in the retrievable literature. There are case reports that suggest there is benefit from treatment of these reflexes, concluding that more study is needed.92,95
Logan basic technique
Hugh B. Logan, D.C.,96 developed the Logan basic technique, emphasizing that the body must have normal structure to have normal function. In part, this system takes into account the effects of gravity on the spine and its related structures. Logan hypothesized that the body of the lowest freely moveable vertebra will rotate toward the side of the inferiorly displaced sacrum (or the vertebra upon which it rests), that is, that the body of that vertebra rotates toward the side of least support. This is usually the low side of the sacrum. Unequal weight-bearing support offered at the base of the spine or unequal weight transfer from above and through the sacrum becomes an etiologic factor of spinal distortions and segmental subluxation. Priority of treatment shifts to providing more equal weight-bearing support below the spine, sacral base leveling, and more equal weight transfer from the body above.
Logan96 and others noted that if the spine is posturally deficient because of the effects of gravity, it places a greater energy demand on the body, which over time could lead to more serious effects on the human body. The reduction of distortions is approached from balancing weight-bearing support to the spine, balancing muscular efforts to reduce the distortion, and balancing ligamentous resistance to distortion. One major concept produced and developed by Logan was the value of the foundational support elements to the spinal column. Deviations in lower limbs, pelvic alignment, sacral position, and lower lumbar vertebrae were categorized as possible initiators of spinal distortions and subsequent segmental subluxation. Differences between the lower limbs resulting in altered spinal support included arch height; ankle, knee, and hip joint space; tibia and fibula lengths; femur length; and ankle, knee, and hip angulation. These were classified as variables in weight-bearing support of the pelvis and then of the spine.
Spinal mechanics are evaluated through postural analysis, spinal palpation and analysis (static and kinetic), full-spine x-ray mensuration, spinal posture musculature activity, lowered pain threshold points and patterns, bilateral scales, and other instrumentation. More specifically, Logan’s analysis96,97 seeks to determine significant factors of foot, leg, pelvic, and sacral roles in altered weight-bearing support of the lumbar spine. Furthermore, these effects to the lumbar spine are evidenced by lateral bending, rotation, curvature, fragmentation (subluxation), reactive muscular activity, unequal ligamentous tensions, and others.
Logan96 believed that the sacrum was the biomechanical keystone of the body, because it supported the spine and allowed for locomotion, and he believed that the spine would respond to changes in the sacrum. Thus, returning the sacrum to normal relationships with its articulating bones was essential in reducing spinal involvements. He thought that this could be accomplished by applying light to moderate force to specific contacts established along the sacrotuberous and sacrospinous ligaments. The amount of pressure applied is described as the amount a person could withstand against the eyeball. Pressure is applied steadily to these contacts with no true thrust delivered. One of the most common contacts involves approximately 2 to 10 ounces of pressure applied to the junction of the sacrotuberous and sacrospinous ligaments (Figure 7-41). Somatic changes in muscle tone, skin and core body temperature, respiration, and perspiration have been reported as anecdotes.96,97 Basic technique uses many procedures, including balancing weight-bearing to the spine, temporary lifts, lower extremity therapy, sacroiliac therapy, balancing muscle efforts, postural education, notch and ulnar adjustment, and balancing ligamentous resistance.
Logan96 includes all of the suggested vertebrogenic causes and involvements presented in classical chiropractic principles. The rationale at this level is simply “if the clinical entity has any possible connection to vertebral subluxation [initial or sustaining] then the reduction of same would have therapeutic value [the chiropractic adjustment of spinal segments].”96 Logan further asserts that vertebrogenic involvement of a single segmental lesion with its neurologic elements can extend the effect to multiple neurologic functions and levels. This level of spinogenic involvement has two routes of neurologic pathophysiology: the direct route of neurologic involvement associated with spinal distortions and the indirect route of neurologic involvement associated with fragmentation of the system (vertebral subluxation).
Logan’s treatment procedures96 are aimed at the first route: the reduction of spinal distortions and associated neurologic involvement directly and indirectly reducing the segmental lesions and specific levels of neurologic involvement. The Logan approach is the correction of spinal distortions and the reduction of pathomechanical processes associated with those distortions. Spinal biomechanics of motion and support adversely affected by or as part of spinal distortions are specific targets of diagnosis and therapy directly. Specifically, Logan’s treatment procedures are aimed at correction of altered supportive elements and altered motion elements of the complete system, sections, and units.
Logan’s teachings96 give clinical significance to altered weight-bearing support transfer down through the spine. These alterations are recognized as etiologically significant in spinal distortions, postural faults, spinal asymmetries, curves, sectional towering, and spinal system fragmentation (vertebral subluxation). The clinical significance of vertebral subluxation in Logan’s programs are those established by other classical chiropractic principles and spinal adjusting techniques that recognize the value of subluxation reduction to improved homeostasis and physical well-being and the adverse potentials of subluxation presence in full-spectrum pathophysiology.
Spondylotherapy
Spondylotherapy is defined by Janse98 as a method of treating visceral disease through the stimulation of the related reflexes by the application of a mechanical or electrical force in a properly judged fashion on the autonomically related vertebra. The principle of interrupted percussion or vibration is usually used.
Spondylotherapy is accomplished by placing a contact over either the spinous process or both transverse processes with the middle or index fingers or both (Figure 7-42). The other hand is used over the contact in a series of rapidly rebounding percussions for approximately 5 seconds. About 15 percussions should be applied during this time. Treatment is typically applied to three or four adjacent vertebrae to provide neurologic input to the viscera with the same segmental innervation (Table 7-2).

Figure 7-42 Spondylotherapy applied to the transverse processes of T5 to T9 to influence the sympathetic nerve distribution to the stomach.
TABLE 7-2 Segmental Innervation Related to Viscera
| Viscera | Segment |
|---|---|
| Heart | T1-T8 |
| Lung | T3-T9 |
| Esophagus | T5-T6 |
| Stomach | T5-T9 |
| Duodenum | T6-T10 |
| Jejunum | T8-T11 |
| Large Bowel | T9-L1 |
| Appendix | T9-L1 |
| Liver | T6-T11 |
| Gallbladder | T6-T11 |
| Spleen | T7-T10 |
| Pancreas | T7-T9 |
| Kidney | T9-L2 |
| Ureter | T9-L2 |
| Testis/Ovary | T10-T11 |
| Prostate | T11-L1 |
| Uterus | T12-L1 |
Usually the segments to be treated are painful to palpation, and a mild increased sensitivity in the treated area is thought to indicate that the desired degree of stimulation has been achieved. A light, continuous contact held beyond the initial stimulation time is thought to produce relaxation through sedation, whereas a heavy continuous contact will eventually produce inhibition because of actual nerve blockage. Continuous percussion, concussion, or vibration will eventually produce inhibition as a result of fatiguing of the reflexes involved. Interrupted moderate percussion, concussion, vibration, or sinusoidal current will prolong the initial stimulation of the reflexes involved.
Direct percussion techniques have long been used by practitioners of manual therapy to influence organs through spinal pathways. Vibratory percussion is thought to invoke a somatovisceral reflex and stimulation of the segmental innervated viscera. This hypothesis suggests that persistent afferent input, driven by percussive vibration, mechanical alteration, pain, and potential local inflammation, triggers a segmental cord response, which in turn induces the development of a somatovisceral reflex. The persistent altered afferent input is then theorized to produce sensitization of local spinal neuron pools and the breakdown of abnormal somatovisceral reflexes.99 100 101 102 103
Conclusions
With the introduction of these procedures into chiropractic practice, the scope of indications for their use undoubtedly will increase. The lack of irritation, as well as the protective gentleness associated with these techniques, allows their use when thrusting forms of manual therapy might be contraindicated. A further advantage of nonthrust procedures is that they can be effective when psychologic factors influence the picture of illness.
Little evidence exists to distinguish the effectiveness or comparative effectiveness of the procedures presented in this chapter. Although a few case reports have been published, no comparative studies have been done to date. Full understanding and absolute validation may not be attainable with the technology and knowledge of today. The notion of clinical success is relative and fragile. It behooves practitioners to make every effort to substantiate the principles and procedures of clinical practice.104