CHAPTER 48 Proprioceptive Neuromuscular Facilitation for the Shoulder
The shoulder consists of several joints that function optimally when there are precise recruitment and coordination of the muscles attaching to these joints. Perry1 describes 17 muscle groups that contribute in varying proportions to the composite movement of the scapula and humerus during movement of the upper extremity.
The recruitment and timing of muscle activity during function must be consistently precise, because the bone stability of the primary joints of the shoulder is not particularly good compared with most of the other major joints in the body. The scapula is a sesamoid bone embedded in muscles and without direct articulation with the posterior thorax. To complicate matters, the bones and soft tissues around the glenohumeral joint provide little support for the relatively long lever of the rotating upper extremity. These factors have led many researchers to conclude that the shoulder represents one of the best examples of dynamic stability in the human body. Dynamic stability results in neuromuscular recruitment of muscles to stabilize and coordinate movement around a joint complex.2 Specifically, the muscles and their synergistic actions (muscle working in concert to produce a particular motion) around the shoulder provide its inherent stability.
Lephart and colleagues3 reported that neuromotor control impairments are ubiquitous after shoulder injury and surgery. Although isolated strengthening of weak muscles is important in shoulder rehabilitation, the key to rehabilitation of the shoulder, particularly for the overhead athlete, is to restore the precise temporal pattern of muscle recruitment necessary for smooth coordinated shoulder movement. Rehabilitation specialists should have the requisite skills and knowledge to integrate patterns of muscle activity throughout all stages of shoulder rehabilitation. Fortunately, we have a strategy to facilitate neuromuscular control of the shoulder.
Proprioceptive neuromuscular facilitation (PNF) is a neurophysiologic approach to therapeutic exercises that can be used during all phases of shoulder rehabilitation to address multiple and different impairments and functional losses. PNF applies neurophysiologic principles of the sensory and motor system to coordinate and efficiently perform purposeful movements at the shoulder.4 PNF can be used effectively as part of an overall progressive rehabilitation program for the shoulder to facilitate neural adaptation and motor control, to improve strength and flexibility, and to promote functional progression. Modifications to the original patterns of movement of Knott and Voss5 can be performed for select shoulder pathologies while considering the same neurophysiologic concepts.
This chapter reviews the theoretical basis of PNF, describes the guidelines for the clinical use of PNF in shoulder rehabilitation, describes the use of PNF techniques to address common impairments and functional losses associated with shoulder conditions, and reviews the current evidence for the use of PNF on shoulder outcomes. Although there are many excellent courses that teach precise PNF techniques, and I encourage readers to pursue such training, my clinical experience indicates that one does not have to be an expert in PNF to successfully integrate many of its techniques into a shoulder rehabilitation program.
THEORETICAL BASIS
The theoretical basis of PNF for affecting motor changes is a controversial subject. We should remember that PNF is promoted as an example of a neurofacilitation approach to motor control. Motor control is the ability to regulate or direct the mechanism essential to movement.6 Neurofacilitation techniques such as PNF are largely associated with both the reflex and hierarchical theories of motor control.7 These approaches in general suggest that normal movement results from a chain of reflexes organized hierarchically within the central nervous system (CNS). According to these theories, normal movement is organized at higher and higher levels in the spinal cord and brain neuronal circuits. A great emphasis is placed on the understanding that incoming sensory information stimulates and thus drives a normal movement pattern.
Although new research shows that motor control is more complex than reflex or hierarchical theories suggest,6 the importance of sensory input for stimulating movement is still widely accepted and integrated into clinical practice. Such PNF techniques as repeated quick stretches are believed to stimulate muscle spindles that enhance input and excitation of the alpha motor neuron to the targeted agonist muscles for optimal muscle fiber recruitment and contractions.8 Conversely, elongation and stretching of muscles that are antagonistic to a particular PNF pattern can facilitate the Golgi tendon organs of those muscles, resulting in inhibition and relaxation of the antagonist muscle groups. Finally, techniques such as joint compression and traction used during active PNF patterns are believed to excite joint mechanoreceptors such as Pacinian corpuscles and Ruffini endings that respond to joint angle changes, velocity, and direction of movement and can enhance joint position sense and dynamic reflect stabilization.9 In recent years, the use of PNF has evolved to put greater emphasis on explicitly training function and less emphasis on inhibiting reflexes and retraining normal patterns of movement.
EVIDENCE
A 1997 survey by Surburg and Schrader10 indicated the wide application of PNF techniques by athletic trainers to treat various musculoskeletal conditions using PNF. In addition, one of us (BHG) has observed during years of academic and clinical practice the integration of PNF into therapeutic applications in both orthopedic and neurologic practice settings. Despite the ubiquitous use of PNF for shoulder rehabilitation, evidence is scant on its effectiveness. In an earlier study, Surberg11 examined the effects of PNF on reaction time, movement time, and response time in the shoulders of 42 subjects. Subjects were randomly assigned to one of three training groups: weight training, target throwing, and PNF. Subjects engaged in three training sessions a week for 6 weeks. Analysis revealed a significant improvement for the PNF group compared with the other groups in response time and movement time of the shoulders.
Perhaps the most compelling study of the effectiveness of PNF in shoulder outcomes measures was presented by Padua and coworkers.12 The authors randomly assigned 54 healthy subjects to one of three groups: closed kinetic chain (CKC), open kinetic chain (OKC), and upper-extremity PNF diagonal patterns to compare the effectiveness of these exercises on select upper-extremity performance outcomes including isokinetic rotator cuff strength, active angle reproduction, single-arm dynamic stability, and functional throwing performance. Groups trained three times a week for 6 weeks. Outcomes indicated that the OKC and PNF groups demonstrated significant pretest to post-test improvement for isokinetic rotational strength, but only the PNF group demonstrated significant improvement in functional performance.
The fact that the PNF improved functional throwing capabilities might not be surprising given the similarities in the PNF D2 flexion pattern and the overhand throwing motion. Both motions require reciprocal patterns of shoulder external rotation, abduction, and flexion (wind-up and cocking phases of throwing), followed rapidly by internal rotation, adduction, and extension (acceleration and deceleration phases of throwing). What may be more surprising is that PNF was as effective as isolated rotator-cuff strengthening performed in the OKC group (both groups demonstrated a 15% increase in rotational strength). The authors concluded that by improving shoulder rotation strength as well as functional performance, PNF exercise appears to be the most efficient of the training methods used in their study. The results of this study seem to support the use of manually resisted PNF techniques to selectively strengthen the rotator cuff muscles while working functional movements.
BASIC PROCEDURE
Several basic procedures promote the effective use of PNF during rehabilitation. These procedures should be used to optimize the desired movement pattern and should be practiced for consistent application. Clinicians performing PNF procedures use basic techniques to facilitate or inhibit smooth coordinated movement patterns. These techniques include the proper manual contacts, resistance, quick stretch, irradiation, traction and approximation, verbal commands, and visual cues.13,14
Manual Contacts
Many clinicians prefer to use PNF techniques throughout treatment because of their ability to manually guide and control movement. Manual control may be particularly important when certain ranges of motion need to be limited in the presence of healing tissue or pain. In postsurgical shoulder cases, the rehabilitation specialist should have a clear understanding of the progression of range-ofmotion (ROM) constraints for proper tissue healing. In the presence of muscle weakness, proper use of hand contacts can provide the patient with sensory cues that purportedly enhance neuromuscular control and eliminate, correct, or minimize substitution patterns. A lumbrical grip is usually a preferred method of applying manual contacts, particularly when resistance is required. Ideally, the clinician should touch only the surface of the area to be facilitated. Usually one manual contact is placed distally and one manual contact is placed proximally on a segment to facilitate distal-to-proximal movement.
Resistance
Clinicians apply manual resistance to strengthen weak muscles in isolation or in functional patterns of movement. A common question is how much resistance is appropriate? A simple answer is that optimal resistance is defined as resistance that is graded appropriately for the intended movement.14 A rule of thumb is that optimal resistance should be the maximum resistance that results in a smooth, coordinated movement pattern. The clinician should remember when working with a movement pattern of the upper extremity, it is the quality of movement that is the desired outcome. Once a patient is smoothly and effortlessly moving his or her upper extremity, the clinician may choose to apply increased resistance to that pattern. Too much manual resistance applied too early can result in substitution patterns of movement, muscle juddering, loss of control, pain, and, at times, injury.
To apply the proper amount of resistance, the clinician considers the patient’s age, general health, gender, comorbidities, stage of healing, the muscle performance deficits, and functional needs. Early in rehabilitation, clinicians often apply submaximal resistance to overcome muscle inhibition due to pain. In addition, submaximal resistance tends to recruit type 1 or slow twitch muscle fibers that facilitate stability and postural control.15 As strength and motor control improve, resistance can be applied maximally using concentric, eccentric, and isometric muscle contractions, or in combinations.
Saliba and colleagues14 summarized the uses of appropriate resistance: to teach and increase awareness of a movement, to stimulate appropriate irradiation from strong to weak components, and to reinforce weak patterns by irradiation from strong patterns.
Traction and Approximation
The use of joint traction (separation) and approximation (compressive forces) further stimulates facilitation of the desired response through the joint receptor system and can be used to protect healing tissue. Stimulation of these mechanoreceptors helps to signal the muscle for a response. This is critical in the shoulder for enhancing stability (approximation) and mobility (traction). For example, early application of manual approximation of the humerus into the glenoid fossa is used to facilitate co-contraction of the musculature in patients with multidirectional instability (MDI) in the glenohumeral joint.16 Conversely, the clinician may choose to provide tractive forces on the humerus during a diagonal pattern to protect a healing labrum in a patient with a superior labral anterior-posterior tear (SLAP lesion).
Quick Stretch
Quick stretch is a neurophysiologic technique that is used to increase excitation to the muscle before a concentric contraction. The clinician applies a gentle quick nudge or tap to the muscle under tension to use the muscle’s stretch reflex for excitation of a specific movement response. The shoulder joint is taken into a position to apply a controlled manual stretch to all components of the movement. Often, in the presence of a patient presenting with muscle weakness throughout his or her ROM, I apply a consistent series of quick stretches to facilitate movement, an advantage that manually applied PNF has that is not offered by traditional muscle training.
Verbal Commands
Verbal communication further enhances the facilitation process by increasing muscle excitation. Directions to patients are also more clearly defined. Verbal tone might also be important to monitor, because it can serve an excitation role. An important consideration is the consistency of the verbal stimuli. The clinician should use the same simple understandable cues each time a movement is performed.
Visual Stimuli
Visual cues and stimuli help the patient learn movement patterns more easily, coordinating the head, trunk, and extremities. During upper extremity diagonal patterns, early on, it is often useful for the clinician to encourage the patient to coordinate head movement with the extremity elevation to maintain visual contact. Eventually, however, the patient should be encouraged to perform movement patterns using only proprioceptive input by eliminating all visual cues.
Irradiation
Conceptually, irradiation occurs at the level of the anterior horn cell and is the spread of facilitation with increased effort across muscles that work in synergy to produce a particular movement pattern. The practical application of irradiation occurs with the clinician’s judicious use of quick stretches and resistance. Typically, overflow is directly proportional to the amount of strength in the resisted muscle groups and the amount of resistance the clinician applies. The advantage of irradiation in a patient with shoulder weakness in the rotator cuff and deltoid muscles is to resist the stronger distal muscles around the elbow and the wrist and hand during a particular diagonal motion to reinforce the weaker proximal muscles. As in much PNF, the application of the right amount of resistance and quick stretch to produce the appropriate amount of irradiation is more art than not, so the clinician should practice these techniques but be careful to closely monitor the patient’s responses and modify the amount of resistance for the best results. The basic precept of “do no harm” should always guide treatment, particularly after surgery. If the clinician is not sure about the status of the healing tissue, the best advice is to err on the side of less resistance.
PATTERNS OF FACILITATION FOR THE UPPER EXTREMITIES
This section describes the classic upper extremity and shoulder PNF patterns. The objective is for the interested reader to practice and master these patterns so as to be able to integrate and modify them for individual shoulder rehabilitation programs.
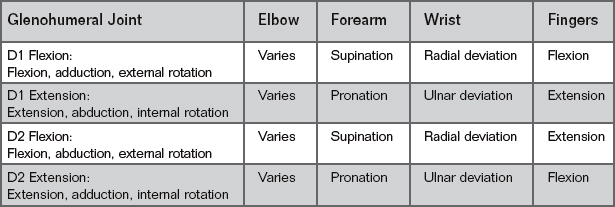
Performance of PNF revolves around specific spiral and diagonal patterns that include three integrated mechanical motions: flexion and extension, abduction and adduction, and internal and external rotation. There are four shoulder patterns: flexion–abduction–external rotation, extension–adduction–internal rotation, flexion–adduction–external rotation, and extension–abduction–internal rotation.4 Classically, the patterns of movement are named by two different ways: either by diagonal (e.g., D1 flexion pattern) or, more simply, for the motion occurring at the proximal joint. Table 48-1 lists the components for the two upper extremity motions. Table 48-2 lists the classic scapular patterns. Initially, four isolated scapular diagonal patterns can be incorporated, including anterior elevation, posterior depression, and posterior elevation and anterior depression. Figures 48-1 through 48-8 illustrate the PNF patterns listed in the tables.
| Exercise | Location | Motion |
|---|---|---|
| D1 Flexion | Scapula | Anterior elevation |
| D1 Extension | Scapula | Posterior depression |
| D2 Flexion | Scapula | Posterior elevation |
| D2 Extension | Scapula | Anterior depression |
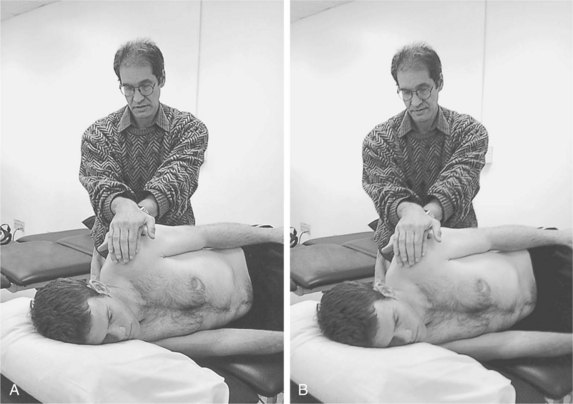
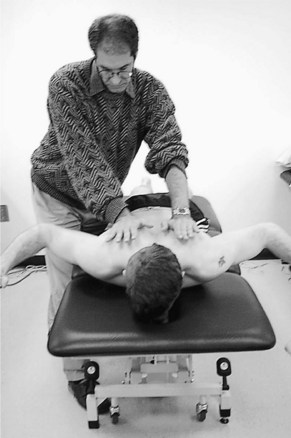
Figure 48-1 Scapular anterior elevation. Purpose is to facilitate the D2 upper extremity flexion pattern by improving neuromuscular control of the scapula through strengthening the levator scapulae and serratus anterior muscles in a diagonal pattern. Concomitantly, this pattern stretches and elongates the rhomboids, latissmus dorsi, and lower trapezius muscles. A, The patient is placed side lying with the clinician standing behind the patient’s hips in the line of motion, facing the patient’s head. Both hands overlap on the anterior glenohumeral joint and acromion. B, The clinician gently takes up the slack, moving the scapula into a posterior depressed position (starting position), and applies a quick stretch. The patient anteriorly elevates the scapula against appropriate resistance. Movement is a diagonal arc up toward the patient’s nose.

Figure 48-2 Scapular posterior depression. Purpose is to facilitate the D2 upper extremity extension pattern by improving neuromuscular control of the scapula through strengthening the rhomboids, lower trapezius, and latissimus dorsi muscles in a diagonal pattern. This pattern stretches and elongates the levator scapulae, upper trapezius, and serratus anterior muscles. A, The patient is placed side lying with the clinician standing behind the patient’s hips in the line of motion, facing the patient’s head. Both hands are flat palmed on the middle to lower scapulae, along the vertebral border. B, Movement is down to the ipsilateral ischial tuberosity.

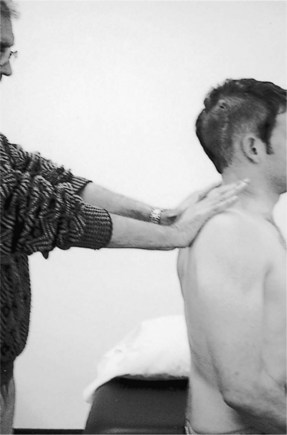
Figure 48-3 Scapular posterior elevation. Purpose is to facilitate the D1 upper extremity flexion pattern by improving neuromuscular control of the scapula through strengthening the trapezius and levator scapula muscles in diagonal plane of the scapula. A, Client is side lying. The clinician stands at the client’s head, facing the hips. Manual contacts are placed on the distal edge of the upper trapezius, close to the acromion. B, Movement is an arc as the client shrugs up toward the ear.
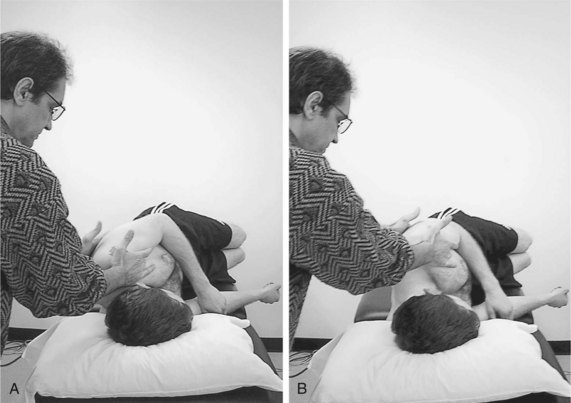
Figure 48-4 Scapular anterior depression. Purpose is to facilitate the D1 upper extremity extension pattern by improving neuromuscular control of the scapula through strengthening the rhomboids and pectoralis minor and major muscles in the diagonal plane of the scapula. A, Client is side lying. The clinician stands at the client’s head, facing the hips. Manual contacts are placed on either side of the axilla, on the pectoral muscle and corocoid process anteriorly and on the lateral border of the scapula posteriorly. B, The patient pulls the shoulder down toward the umbilicus.

Figure 48-5 Upper extremity flexion–adduction–external rotation (D1 flexion). This pattern facilitates the function of the upper extremity in reaching up and across the body while facilitating external rotation at the glenohumeral joint. This pattern is useful early in rehabilitation for initiating rotator cuff activities while minimizing the shear forces of the humeral head along the glenoid fossa produced by deltoid muscle activity. However, the clinician must be certain that the patient has adequate humeral head external rotation and scapular anterior elevation to avoid shoulder impingement at end range of flexion. A, The client lies supine with the shoulder in slight extension with the hand near the hip. The clinician stands at the client’s elbow, facing the feet. Distal manual contact on the palm provides most of the traction and rotatory control. Proximal contact can be on the biceps or the pectorals. B, The patient is told, “Turn and squeeze my hand then pull up and across your nose.” The clinician pivots toward the patient’s head as the arm moves past. The diagonal movement ends with the elbow crossing the midline around the nose.

Figure 48-6 Upper extremity extension–abduction–internal rotation (D1 extension). This pattern facilitates the function of the upper extremity reaching down and back, similar to leaning back on the arm to support oneself while sitting. This technique is useful to activate the posterior deltoid muscle to counteract anterior shear forces of the humeral head in a patient with anterior glenohumeral joint instability. Other muscles activated during this pattern are the teres major, the latissimus dorsi, and the long head of the triceps. A, The patient lies supine. The clinician stands at the patient’s side near the head. The patient’s upper extremity is flexed and adducted. Manual contacts are placed along the dorsal surface of the hand (distal) and on the posterior surface of the humerus or scapula (proximal). B, A quick stretch, especially in the form of traction, can be applied simultaneously to the hand and shoulder. The patient is told, “Pull your wrist up and push your arm down to the side.” As the upper extremity moves past the clinician, traction can be switched to approximation to increase recruitment of the proximal muscles. The pattern ends with the wrist extended and the upper extremity at the patient’s hip.

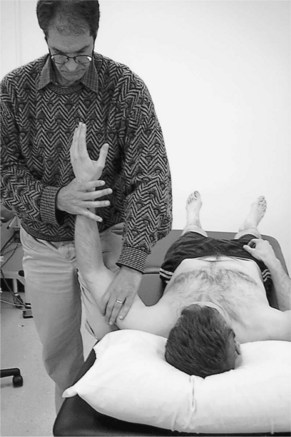
Figure 48-7 Upper-extremity flexion–abduction– external rotation (D2 flexion). This pattern facilitates the functional movement of reaching up and out and helps to restore external rotation early in rehabilitation. To avoid potential subacromial impingement, the clinician should restore scapula posterior elevation before working toward the end range of flexion associated with this pattern. Because the movement of this pattern mimics the overhead throwing motion, clinicians use this pattern to promote muscle timing and recruitment during the functional stages of rehabilitation. A, The patient lies supine with the clinician standing at the patient’s shoulder facing the patient’s feet with a wide base of support in the diagonal of movement. The patient’s upper extremity starts from across the body in an elongated, extended position, with the elbow crossing the body near the hip. Distal manual contact is placed on the dorsal hand, and contact either on the proximal humerus or on the scapula emphasizes shoulder and scapular motion. B, The clinician takes the patient’s upper extremity to a fully elongated position, taking up all the slack in the muscle groups, and gently applies a quick stretch. The patient is told, “Pull your wrist up and reach.” The wrist completes extension before the other components.

Figure 48-8 Upper-extremity extension–adduction–internal rotation (D2 extension). This pattern facilitates the movement of the upper extremity to move down and across the body and mimics the acceleration and deceleration phases of the overhead throwing motion. A, The patient lies supine while the clinician stands near the patient’s shoulder. The clinician applies distal manual contact palm to palm with the patient. The clinician applies proximal contact on the pectoral muscles to emphasize recruitment of the trunk and scapula or on the proximal humerus. B, The clinician applies initial elongation and a quick stretch. The patient is told, “Squeeze and turn your hand.” The clinician pivots slightly as the limb passes the clinician’s center of gravity. The pattern ends in shoulder extension, forearm pronation, with the elbow across the midline.
Box 48-1 lists several strategies that should be used by clinicians to optimize their patients’ performances of PNF patterns.13 These strategies should be modified depending on the impairments and functional needs of a particular patient. For example, the sequencing of motions associated with normal timing is recruitment of the distal joint segments (such as the fingers, wrist, and hand) to proximal segments (elbow, glenohumeral joint, and scapulothoracic joint) of a freely moving multiple joint segment and proximal to distal with a fixed multiple joint segment. Changes in normal timing can be used, however, to emphasize a specific component of the movement pattern. For example, a clinician may choose to isolate glenohumeral joint external rotation at the beginning of the flexion–abduction– external rotation upper extremity D2 diagonal pattern. In the upper extremity, I recommend correcting proximal impairments before correcting distal impairments by working isolated scapular and glenohumeral patterns before commencing with entire upper-extremity diagonal patterns. In that way, the clinician restores scapular stability in preparation for exercising distal patterns.
In additions to these strategies, the clinician should practice some of the basic PNF techniques.13 These techniques require the clinician to control the patient’s muscular effort, movement patterns, and joint position. The patterns of movement are designed to rhythmically stimulate the agonist of the movement while causing relaxation of the antagonist.
Rhythmic Initiation
The purpose of rhythmic initiation is to passively move a segment through a ROM to assess the available amount of motion and to help the patient learn a direction of motion that is supposedly normal. I use rhythmic initiation as a form of passive ROM and warm-up before active and active-resistive ROM. As rhythmic initiation progresses, the patient slowly assists the direction of movement through concentric muscle contractions.
Repeated Quick Stretch
In repeated quick stretch, the therapist applies a stretch force to invoke a reflex to further stimulate muscular contraction. The stretch mechanism stimulates a response by the gamma system in the musculotendinous unit. This technique is helpful in cases of fatigue and specific areas of inhibition. Repeated quick stretch is useful as the patient progresses from rhythmic initiation to active and active-resistive concentric contractions.
Combination of Isotonics
The use of concentric, eccentric, and maintained isotonic techniques facilitates control of movement. Combination of isotonics is a progression from rhythmic initiation and can be used throughout the available ROM of a particular segment.
Reversal of Antagonists
Reversal of antagonists is crucial in normal function to allow a movement to occur without excessive resistance of the antagonistic muscle. The technique consists of reciprocal isometric (stabilizing reversal) or isotonic (isotonic reversal) contractions through the desired ROM. The goal is to work on facilitation of the agonist and antagonist.
Rhythmic Stabilization
Rhythmic stabilization employs isometric contractions of the agonist and antagonist muscles in different points of the ROM. Rhythmic stabilization results in a buildup of holding power around a joint. The patient must not be defeated with so much resistance that he or she finds it necessary to contract isotonically to recover or maintain position. The grading of resistance will be as accurate as the clinician’s ability to feel the patient’s response. Rhythmic stabilization is particularly useful with joint compression in the presence of MDI to facilitate co contractions and stabilization of the glenohumeral joint.
Relaxation Techniques
Relaxation of synergistic muscle groups stimulates the agonist and inhibits the antagonist to increase ROM. Hold-relax, and contract-relax techniques are used to relax muscles that exhibit increased tone or increased passive resistance to elongation (stretch). Hold-relax should produce an isometric muscle contraction resulting in negligible movement of the targeted segment. During hold-relax, the clinician should take care to build up resistance slowly by telling the patient, “Give me what I give you.” Contract-relax produces a more abrupt contraction, and the clinician imparts enough force to move the segment, producing an eccentric contraction. I use hold-relax earlier in rehabilitation in the presence of pain and tissue healing. The amount of time to ask the patient to hold or contract varies from a few seconds to 10 seconds.
TECHNIQUES AND PROGRESSIONS
The clinician faces several decisions about performing these patterns. These decisions are predicated on firmly establishing a physical therapy diagnosis that includes stage of healing, biomechanical constraints of surgery, nature and extent of impairments, functional losses, and functional needs to return to full activity.
Procedures for Shoulder Impairments and Functional Losses
Patterns can be altered by choosing among unilateral or bilateral, symmetrical or asymmetrical, elbow straight or flexion-extension, timing for emphasis, submaximal or maximal efforts, and full range or partial range of motion. For example, linear patterns instead of the classic diagonal patterns are sometimes necessary postoperatively when scapula and clavicle rotation produces pain at the rotator cuff, acromioclavicular joint, or capsular restraints. The use of linear patterns can also help when diagonal patterns are limited by soft tissue and myofascial restrictions secondary to chronic postural impairments.
Shirley Sahrmann17 observed that clinically most movement impairment syndromes involving the shoulder arise from impairments in the timing and control of scapular motion. I have found it useful to begin most shoulder rehabilitation programs by focusing on restoring scapular control. It is particularly important to restore the counterbalancing forces of the muscles that attach to the scapula. Two muscles in particular—the serratus anterior and lower trapezius—seem to lose strength after surgery or immobilization. These muscles are critical to restore the correct force-couple mechanism to the scapula during overhead elevation. In particular, these muscles produce scapular outward rotation during upper extremity elevation. Early application of PNF can be applied in the classic side-lying position (see Figs. 48-1 to 48-4) immediately after surgery without fear of injuring healing tissue. The clinician can begin with rhythmic initiation to mediate losses of ROM and slowly progress to passive and active resistance, initially in limited ranges and progressively working the patterns into larger ROMs. Contract or hold-relax techniques are useful in producing reciprocal inhibition of shortened and tight antagonist muscles.18
Patients with the forward-head and rounded-shoulder posture often exhibit an abducted and elevated position of the scapulae. These patients exhibit elongation and weakness in their rhomboid, middle trapezius and lower trapezius muscles and shortening and tightness in their pectoralis major, levator scapulae, serratus anterior, and subscapularis muscles.17 Scapular adduction in prone (Fig. 48-9) and sitting (Fig. 48-10) can assist in correcting this type of upper quarter alignment. Resistance of the shoulder extensors at end range of the extension and abduction pattern can facilitate middle and lower trapezius activity via posterior depression of the scapula.
The serratus anterior can be facilitated in several ways. Early in rehabilitation, scapular anterior depression with the patient side lying activates the lower and middle fibers of the serratus anterior, which are critical to produce outward rotation of the scapula during overhead elevation. Anterior elevation can help recruit the upper fibers of the serratus anterior, which contract along with the upper trapezius muscle to produce elevation and the upward portion of the scapular force-couple during overhead elevation. Input to the lower trapezius muscle can be initially facilitated using the pattern of posterior depression in a side-lying position. The clinician may also choose to exercise the serratus anterior as an abductor or protractor by resisting scapular abduction with a combination of isotonic techniques at various angle positions (Figs. 48-11 and 48-12). As strength and healing improve, the patient can be instructed in performing a standard push-up with a plus with pronounced scapular protraction. When the patient has adequate strength and scapular and upper-extremity control, the clinician can apply resistance to both upper extremities simultaneously with the patient supine to produce cross facilitation in shoulder elevation. This pattern produces posterior elevation of the scapulae as well as strength in the upper extremities in flexion, abduction, and external rotation. Bars of varying weights can offer resistance in addition to that provided by the clinician.
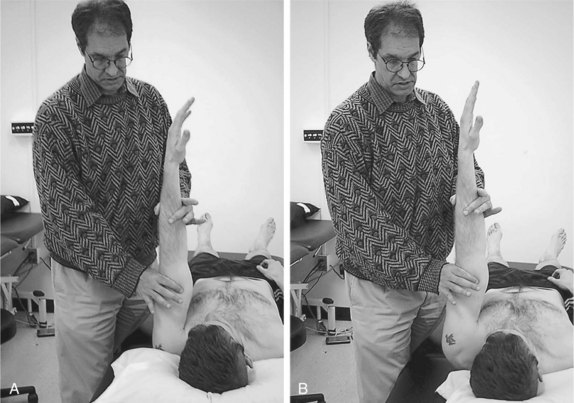
Figure 48-11 Resisted scapular abduction. A, Initiating scapular protraction with patient supine using quick stretch. B, End range of scapular protraction.

Figure 48-12 Resisted scapular abduction. A, Initiating scapular protraction with patient sitting using quick stretch. B, End range of scapular protraction.
While the clinician concentrates initially on restoring scapular control and movement, input to the rotator cuff can be increased by having the patient hold the shoulder isometrically at one point in the ROM while performing synergistic scapular movements. This is a particularly useful technique for the baseball pitcher. For example, scapular elevation patterns with the shoulder maintained in 90 degrees includes the deltoid and supraspinatus in the exercise pattern with the serratus anterior and the upper trapezius and levator scapulae muscles. The clinician can gauge improvement in rotator-cuff muscle control by watching for the onset of a lag sign (loss of shoulder external rotation) over exercise sessions. As rotator cuff muscle strength increases, the clinician can use combined isotonics and progress from isometric and concentric contractions to eccentric contraction of the posterior cuff and deltoid muscles (Fig. 48-13). Rhythmic stabilization exercises can be used to facilitate rotator cuff and deltoid muscle activity during isometric contraction of the protracted scapula (Figs. 48-14 and 48-15). As adjuncts to the manual techniques, scapular exercises can be performed with dumbbells or elastic cords. Individual components of the scapula in throwing movements can be facilitated. After re-establishing normal scapular mobility, strength, and stability in this manner, the scapula treatment can be integrated with treatment of the glenohumeral joint.

Figure 48-14 Rhythmic stabilization of the upper extremity with isometric scapular protraction (patient supine).
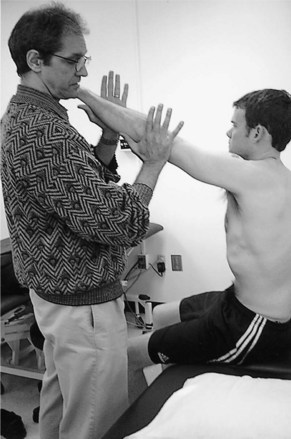
Figure 48-15 Rhythmic stabilization of the upper extremity with isometric scapular protraction (patient sitting).
Each exercise technique and pattern must have a specific goal, and the clinician must consider its effect on various structures (primarily the rotator cuff, capsuloligamentous stabilizers, acromioclavicular joint, and the upper quarter of the body). The flexion–abduction–external rotation and extension–adduction–internal rotation diagonals are the most commonly used PNF diagonals for the overhead athlete because they mimic the throwing motion. Resistance to external rotation motion in the flexion–abduction–external rotation pattern can be modified to be isometric as well as isotonic. This is especially important in cases of infraspinatus tendinitis or partial tears in which overload must be avoided. Full glenohumeral elevation can create subacromial impingement of the rotator cuff against the coracoacromial arch. Predictably, this leads to far greater problems than it solves, especially in patients with partial or full rotator cuff tears, history of classic impingement syndrome, and encroachment of the supraspinatus outlet secondary to acromial morphology or bony changes. When applied appropriately, this pattern can be extremely useful in facilitating the shoulder elevators. Supine, prone, or upright positioning of the patient can be used as well as bilateral and asymmetrical techniques. Slight modification of this pattern can put the patient in an elevation and plane-of-scapula movement, which is also very effective and usually less stressful to the rotator cuff than beginning from an adducted position. Bilateral techniques for cross facilitation and positioning the glenohumeral joint in midranges from a supine position are good starting points for scapula and rotator cuff stabilization in elevation.
Extension–adduction–internal rotation is the diagonal pattern opposite to flexion–abduction–external rotation. It has mechanical characteristics similar to the acceleration, follow-through, and deceleration phases of throwing. Again, as in flexion and abduction, this pattern is excellent for subscapularis facilitation in conjunction with other glenohumeral components. Patients with posterior shoulder instabilities must be monitored carefully to avoid subluxation and overloading of the capsuloligamentous restraints. Supine, standing, and sitting positions may also be used for this exercise.
In the throwing athlete, the flexion–adduction–external rotation and extension–abduction–internal rotation are more important for the glove or nonthrowing side because that extremity functions opposite to the throwing side. End-range flexion and adduction can produce overcompression or repetitive microtrauma at the acromioclavicular joint.
The end range of extension and abduction resisted in an upright position with trunk rotation can assist in facilitation of the posterior glenohumeral, scapular adductor and depressor, and trunk rotator muscle groups used during the course of the throwing motion. From this same position, reciprocal shoulder flexion and extension motions can be facilitated with concentric and eccentric techniques through an appropriate ROM synergistically with trunk rotation.
Facilitation of the shoulder rotators in isolated patterns is extremely important because the rotator cuff muscles are directly affected. Initially, the shoulder is positioned slightly abducted in the plane of the scapula (approximately 30 degrees of forward flexion at 70 degrees of abduction) (Fig. 48-16). This position has been shown by Greenfield and colleagues19 to be optimal for rotational strengthening over the more traditional neutral arm at the side position. Similarly, the shoulder can be manually resisted for both internal and external rotation at 90 degrees of abduction. This position is associated with anterior instability and is used for strengthening the subscapularis as described in many rehabilitation programs with various exercise devices (free weights, tubing, mechanical weights). External rotation in this position is associated with cocking phases of throwing and can be important for facilitation of the posterior rotator cuff. Maximal external rotation at 90 degrees of abduction, however, stresses the inferior glenohumeral ligament complex, which is the main restraint to anterior instability and is often associated with patient apprehension.
External rotation at 90 degrees of flexion is a component of the flexion and abduction diagonal. Flexion and abduction is isometrically resisted at 90 degrees of flexion while working isotonically in external rotation. Maximal internal rotation ROM will impinge the rotator cuff against the coracoacromial arch and is a contraindication. Over-resistance to a weak external rotator group should also be avoided. Infraspinatus and teres minor strengthening in this pattern is an effective technique for the posterior subluxation patient when applied correctly.
Trunk and Neck Patterns
Patterns that include the upper extremities with the trunk and neck provide a higher functional level of neuromuscular training and movement re-education. These procedures, however, demand a higher degree of skill on the part of clinician and patient. Normal functional activity includes whole body involvement, making this type of treatment pattern very valuable in rehabilitation programs.
Adjunctive Procedures
The principles and specific techniques presented may be enhanced by using more effective exercise devices as well as manual techniques. On the market today are a variety of elastic cords, weights, resistive exercise machines, and other equipment that can be modified for rehabilitation of the shoulder patient (Figs. 48-17 and 48-18). Plyometric exercise activities can also be applied in diagonal patterns and other components of shoulder complex motion. The goals of adding resistance are to build strength, endurance, stabilization, and coordination at higher velocities, which are considered more functional.
CASE STUDY
A 19-year old male competitive football quarterback presented on referral from his orthopedist with a diagnosis of secondary impingement to his dominant (right) shoulder. He reported anterior shoulder pain during the cocking and acceleration phases of throwing.
Examination indicated that the right scapular was in a downwardly rotated position compared with the left. Repetitive overhead elevation indicated increased winging of the medial border of both scapulae. The inferior angle of the scapula did not reach the axillary midline of the chest with full overhead elevation. Manual active assist for scapular upward rotation applied during overhead elevation eliminated much of the right shoulder pain. The full can test recommended by Itio and colleagues20 to isolate the supraspinatus indicated pain and weakness. Both the Neer and Hawkins-Kennedy impingement tests were positive.21 The Jobe subluxation-relocation test was positive for anterior shoulder pain.22
The manual muscle test (MMT) indicated the following: serratus anterior, 3+1/5; lower trapezius, 4/5; middle trapezius, 4/5; teres minor and infraspinatus, 4/5.
Assessment
The patient presented with occult subluxation that contributed to overuse and impingement of the supraspinatus tendon. Primary impairments contributing to his pathology included reduced upward scapular rotation during elevation and concomitant muscle weakness. The initial goals of treatment were to reduce pain and inflammation at the tendinous insertion of the supraspinatus muscle; to improve scapular control, including upward scapular rotation during overhead elevation, by increasing muscle strength and control of the serratus anterior, lower trapezius, and middle trapezius muscles; and to improve dynamic stability of the glenohumeral joint by increasing muscle strength and control of the supraspinatus, infraspinatus, and teres minor muscles.
Intervention
The patient was directed to apply ice to the affected shoulder.
PNF was initiated. The PNF pattern of anterior elevation and posterior depression and posterior elevation and anterior depression of the right scapula began with the patient side lying. The clinician began with rhythmic initiation and progressed to slow reversals, emphasizing concentric activity of muscles. Quick stretches were used throughout the ROM to facilitate muscle activity. The clinician used no set recommended number of repetitions but gauged the number of repetitions based on the patient’s fatigue and ability to produce a smooth coordinated contraction.
Isolated manual scapular protraction in supine and sitting was instituted.
The patient performed isolated external rotation in the plane of the scapula using isometrics in various points in the range followed by concentric and then eccentric contractions (combined isotonics). The patient progressed to isolated external and internal rotation in prone and standing positions using combined isotonics in pain-free ranges.
The home program included corrective taping for downward rotation, various scapular exercises including shoulder pinches (scapular retraction) and wall push-ups with a plus, and isolated rotator cuff strengthening in a side-lying position using a 1-lb weight to fatigue.
Progression
One Week after Initial Treatment
At the time of re-examination, the patient presented with pain-free active overhead elevation of his right upper extremity with improving strength in all muscles to 4/5 ranges.
Clinic treatment continued with manually resisted PNF patterns, progressing to unilateral full-range D2 flexion and extension for the right upper extremity, using combination isotonics. Standing activities were introduced, including PNF D2 flexion and extension diagonals and 90/90 external rotation using a Theraband to produce concentric and eccentric contractions. Treatment was supplemented with high-speed isokinetic training for external and internal rotation.
The home program consisted of various exercises for the rotator cuff muscles and scapular muscles, emphasizing light weights (<5 lbs) with high repetitions to produce muscle fatigue.
Two Weeks after Initial Examination
After 2 weeks of intervention, examination indicated pain-free ROM in the right upper extremity and improving strength. All provocation tests for impingement were negative. Functionally, the patient reported that he had begun throwing the football without pain. The goals at this time were to continue to strengthen the rotator cuff and scapular muscles and progress functional training to the right upper extremity (see Chapter 50).
SUMMARY
The specific techniques of PNF combining diagonal patterns with facilitatory and inhibitory input using manual contact makes this approach extremely useful for rehabilitating the shoulder. Selected techniques that are modified to limit range and resistance appropriately facilitate muscle activity early in rehabilitation while protecting healing tissue and controlling pain. The clinician can slowly elicit different muscle contractions combined with more complex movement patterns as pain and tissue healing improve. Integrated upper-extremity diagonal patterns in different positions are particularly useful to restore the motor needs for the throwing athlete.
ACKNOWLEDGMENT
The author would like to acknowledge the late Robert P. Engle, PT, ATC. I incorporated sections of his chapter “Proprioceptive Neuromuscular Facilitation for the Shoulder,” which appeared in the first edition, for this updated chapter. His expertise in the application of PNF for the athlete was well recognized and highly respected by many members of the orthopedics and sports rehabilitation communities.
1 Perry J. Muscle control of the shoulder. In: Rowe C, editor. The Shoulder. New York: Churchill Livingstone, 1988.
2 Davies G, Dickoff-Hoffman S. Neuromuscular testing and rehabilitation of the shoulder complex. J Orthop Sports Phys Ther. 1993;18:449-458.
3 Lephart SM, Pincivero DM, Giraldo JL, Fu FH. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med. 1997;25(1):130-137.
4 Voss DE, Ionta MK, Myers BJ. Proprioceptive Neuromuscular Facilitation, 3rd ed. Philadelphia: Harper and Row, 1985.
5 Knott M, Voss DE. Proprioceptive Neuromuscular Facilitation. New York: Harper and Row, 1968.
6 Shumway-Cook A, Woollacott MH. Motor Control: Theory and Practical Applications, 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 2001.
7 Kabat H. Central mechanisms for recovery of neuromuscular function. Science. 1950;112:23-24.
8 Gordon J, Ghez C: Muscle receptors and spinal reflexes: The stretch reflex. In Kandel E, Schwartz JH, Jessel TM (eds): Principles of Neural Science. New York, Elsevier, pp 564-580.
9 Minaki Y, Yamashita T, Takebayashi T, Ishii S. Mechanosensitive afferent units in the shoulder and adjacent tissues. Clin Orthop Relat Res. 1999;369:349-356.
10 Surburg PR, Schrader JW. Proprioceptive neuromuscular facilitation techniques in sports medicine: A reassesment. J Athletic Train. 1997;32(1):34-39.
11 Surburg PR. The effect of proprioceptive facilitation patterning upon reaction, response, and movement times. Phys Ther. 1977;57(5):513-517.
12 Padua D, Guskiewicz KM, Prentice WE, et al. The effect of select shoulder exercises on strength, active angle reproduction, single-arm balance, and functional performance. J Sport Rehabil. 2004;13:75-95.
13 Stalvey MH. Proprioceptive neuromuscular facilitation. In: Bandy W, Sanders B, editors. Therapeutic Exercise: Techniques for Intervention. Philadelphia: Lippincott Williams & Wilkins; 2001:145-177.
14 Saliba V, Johnson GS, Wardlaw C. Proprioceptive neuromuscular facilitation. In: Basmajian JV, Nyberg RE, editors. Rational Manual Therapies. Baltimore: Williams & Wilkins; 1983:243-285.
15 Milner-Brown H, Stein RB, Yemm R. The contractile properties of human motor units during voluntary isometric contraction. J Physiol (London). 1973;228:285-306.
16 Lephart SM, Warner JP, Borsa PA, Fu FH. Proprioception of the unstable shoulder joint in healthy, unstable and surgically repaired shoulders. J Shoulder Elbow Surg. 1994;3:371-380.
17 Sahrmann S. Diagnosis and Treatment of Movement Impairments. St. Louis: Mosby, 2002.
18 Sherrington C. Integrative activity of the nervous system. New Haven: Yale University Press, 1960.
19 Greenfield BH, Donatelli R, Wooden MJ, Wilkes J. Isokinetic evaluation of shoulder rotational strength between the plane of scapula and the frontal plane. Am J Sports Med. 1990;18(2):124-128.
20 Itoi E, Kido T, Sano A, et al. Which is more useful, the “full can test” or the “empty can test,” in detecting the torn supraspinatus tendon? Am J Sports Med. 1999;27(1):65-68.
21 Tennent T, Beach WR, Meyers JF. Current concepts: Clinical sports medicine update: A review of the special tests associated with shoulder examination Part I: The rotator cuff tests. Am J Sports Med. 2003;31:154-160.
22 Tennent T, Beach WR, Meyers JF. Current concepts: Clinical sports medicine update. A review of the special tests associated with shoulder examination. Part II: Laxity, instability, and superior labral anterior and posterior (SLAP) lesions. Am J Sports Med. 2003;31:301-307.