CHAPTER 50 The Role of the Scapula in Rehabilitation
The body functions as an integrated system in all aspects of sport and work. This integrated system allows variability so that we can respond to specific tasks in an efficient manner. Understanding how the entire system works as a functional unit within its environment is indispensable for appropriate evaluation and intervention to restore patients to their full functional level. Individual patients develop movement patterns and resting postures dependent on their physical characteristics, the demands of the particular task, the environment of the task, and their psychological state. The goal of the treating clinician is to identify these factors as they relate to physical impairments, functional limitations, and particular pathology. Once the factors are identified, there are several ways to intervene. Through our clinical experience we have found that exercises that integrate the entire body and address scapular motion and control have helped our patients return to their normal function. The primary goals of this chapter are to describe our clinical assessment of the scapula and to provide our rehabilitation approach in the upper extremity of a throwing athlete.
BIOMECHANICS
In overhead throwing sports the goal is to throw the ball accurately, for a great distance or at maximum speeds. To impart the necessary force to the ball the entire body is used sequentially in a general proximal-to-distal manner.1-3 This system is commonly referred to as the kinetic chain, which is a coordinated activation of body segments (e.g., leg, trunk, upper arm) that are connected at articulations. To throw a ball at a high rate of speed, the proximal segments of the kinetic chain initiate motion of the entire system. As a proximal segment, such as the front leg of a pitcher, decelerates, momentum is transferred to the next distal segment, the trunk. This process continues throughout the entire kinetic chain until the ball is released. As momentum is transferred to the arm segments (which are smaller in mass), the velocity of the segment increases.4,5 By using the summation of the entire kinetic chain, all segments contribute to the performance of the task. Segment drop out or kinetic chain breakage requires other segments to increase force production or increase loads in distal segments.4,6,7 This is why the evaluation of the injured patient has to be so comprehensive. If the examiner focuses on a sore shoulder and does not discover that the athlete has a weak front leg, the primary culprit of the clinical symptoms has not been identified, and ultimately the rehabilitation program will fail. Lower-body strength has been positively correlated with terminal ball velocity and is more highly correlated than upper body strength.8
A critical segment or link in transferring this force is the scapula, which is the attachment site for approximately 17 muscles involved in upper-extremity motion. Many of the muscles that attach to the scapula, such as the trapezius, serratus anterior, latissimus dorsi, and rhomboids, have proximal attachments to the axial skeleton and are instrumental in maximizing mobility of the upper extremity. The interaction of trunk, scapular, and humeral motion provides a dynamic linked system that is used in many ways in numerous sport activities, from providing a stable base for archery to providing a very mobile system in throwing. The motion provided by the scapula allows the glenohumeral articulation to be the most mobile joint in the human body.9 The scapula provides a dynamic base for humeral motion. The interactive coupling of the scapula and humerus, scapulohumeral rhythm, maintains an optimal muscle length relationship in the rotator cuff musculature and avoids excessive tension on the glenohumeral ligaments.10,11
This sequencing of events not only occurs biomechanically but also occurs in the neuromuscular control of human motion. Activation of proximal trunk musculature, such as the transverse abdominus and multifidius muscles, has been demonstrated to precede activation of distal muscles, such as the anterior deltoid, to prepare the body for positional changes due to the moving segment.12,13 These anticipatory postural adjustments occur both in sitting and standing and occur regardless of the direction of the movement.14,15 These normal motor control patterns are exaggerated in our approach to shoulder rehabilitation by incorporating the entire kinetic chain and focusing the patient’s abilities to activate proximal muscle to control the trunk and scapula before placing demands on more distal musculature.
Proximal control for distal mobility is a basic concept taught in many biomechanics and kinesiology courses. One of us (WBK) put this to work clinically in the 1980s when he started investigating the role of the scapula in upper-extremity pathologies. In observing a swimmer with chronic shoulder pain from the rear while she was wearing a swimming suit, he noted significant scapular winging. By evaluating and appreciating the relationship between symptoms of shoulder impingement and proximal scapular dysfunction, he was able to identify all physical impairments contributing to her pathology. The assessment of scapular dysfunction as part of the clinical examination of the upper extremity is still a relatively new idea to many clinicians. However, since the 1980s the literature on the role of the scapula and the surrounding muscular in shoulder dysfunction and the importance of considering the scapula in treatment interventions has dramatically increased. A Medline search of the word scapula between 1966 and 1988 (22 years) retrieved 1647 citations; the same search between the years 1989 and 2006 (17 years) returned 2281 citations.
Advances in biomechanical techniques that allow evaluation of scapular motion have opened many doors of investigation. Critical research by Karduna and McClure demonstrated that scapular motion could be evaluated with skin sensors attached to the scapula, increasing our understanding of scapular biomechanics. In a series of studies, they instrumented subjects with electromagnetic sensors attached to the skin overlying the scapula and to bone pins placed in the spine of the scapula. They demonstrated that sensors attached to the skin could accurately measure scapular motion during arm motions.16,17 From their research they identified that the scapula rotates about three axes; upward and downward rotation, internal and external rotation, and anterior and posterior tilt (Fig. 50-1).
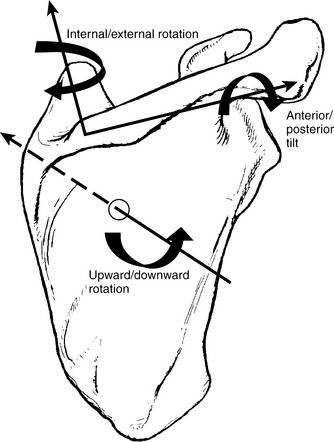
Figure 50-1 This diagram illustrates the three rotational axes of the scapula and the motions that occur around them.
Karduna and McClure found that at maximal humeral elevation in the scapular plane the scapula upwardly rotated 50 ± 5 degrees, externally rotated 24 ± 13 degrees, and posteriorly tilted 30 ± 13 degrees. This motion occurs simultaneously in all three planes, but they demonstrated that the greatest amount of external rotation and posterior tilting occurred above 90 degrees of humeral elevation.17 In addition to these rotations, translatory motion of the scapula occurs. Superior scapular translation along the thoracic wall occurs during forward reaching tasks. Anterior translation around the thoracic wall occurs during forward reaching tasks, and the scapula translates posteriorly during pulling tasks. Medial and lateral translation, the third translation, is limited due to the clavicle strut effect and does not occur unless there is a high-grade acromioclavicular joint separation.17
Understanding the anatomy and biomechanics of the scapula provides the clinician with a firm base to better understand the function and the evaluation of scapular dysfunction. Chapters 1 and 2 address the anatomy and biomechanics of the shoulder complex thoroughly; therefore, we direct the reader to those chapters for further information.
ASSESSMENT OF SCAPULAR DYSKINESIS
The term scapular dyskinesis was coined by JP Warner. He found scapular dyskinesis in 64% of his patients with glenohumeral instability and in nearly 100% of his patients with rotator cuff impingement.18 Several factors can contribute to scapular dyskinesis. They are categorized into two groups: proximal causes and distal causes.19 Proximal categories include neuropathy,20,21 muscle weakness,22 muscle tightness,23 muscle fatigue,24,25 pain,26 and loss of neuromuscular control,27,28 which can respond to physical therapy interventions. Distal categories include glenohumeral pathology29-32 and acromioclavicular joint separations, which usually require surgical intervention to return the patient to full function. Each of these potential factors needs to considered during physical examination of scapular dyskinesis.
The goals of the physical examination of the scapula are to determine the presence or absence of scapular dyskinesis, to evaluate proximal and distal causative factors, and to employ dynamic maneuvers to assess the effect of correction of dyskinesis. The results of the examination help in establishing the complete diagnosis and in guiding rehabilitation.
Posture
To evaluate scapular dyskinesis, the scapula, spine, and clavicle must be adequately exposed and the examiner must view the patient from the posterior aspect.
Observation of resting posture of the spine and scapula should be the first assessment. Resting posture has been implemented as a cause of shoulder and neck pain.33 Thoracic kyphosis has been demonstrated to decrease scapular and humeral motion while also decreasing shoulder strength.34 Rounded shoulder posture is often present in athletes, such as weightlifters and swimmers, who have developed muscle imbalances due to their sport.35 One factor contributing to protracted shoulders can be a shortened or tight pectoralis minor. A short pectoralis minor has been demonstrated to reduce scapular motion during active arm elevation.36 Another factor contributing to scapular dyskinesis is internal rotation deficiency due to tight posterior structures of the glenohumeral joint. This can restrict humeral motion and potentially place increased compressive and tensile loads on glenohumeral tissues. Incorporation of legs and trunk observation in a bipedal and single leg stance is important to evaluate core stability and the lower extremity balance.
The patient should perform a single leg squat. This allows the clinician to screen for poor trunk and hip control, which might need further isolated examination. In clinical assessment of throwing athletes, poor hip and trunk stability are commonly found in the presence of shoulder pain.32 The direct correlation is not currently known, but a significant force contribution originating in the legs has been demonstrated.5,6,8 Therefore, proximal deficiencies must be identified so they can be addressed during the rehabilitation program.
Resting scapular position can be assessed with the patient’s arms at the sides. Excessive scapular internal rotation and lateral translation will be noted as prominence of the medial scapular border. A semidynamic assessment of scapular position using a tape measure is called the lateral scapular slide.37 The distance between the inferior angle of the scapula and a thoracic spinous process is measured in three arm positions; at rest, hands on hips, and arms abducted to 90 degrees and maximally internally rotated. A difference of greater than 1.5 cm suggests a loss of muscular control of the involved shoulder.37 The ability to discriminate this difference in symptomatic and asymptomatic subjects has been supported by Odom.38
Active Range of Motion
Assessment of active and passive range of motion is critical in evaluating shoulder impairments. Assessment of dynamic scapular motion allows the examiner to appreciate scapulohumeral rhythm during arm motion. This dynamic assessment can be facilitated by having the subject perform multiple3-10 repetitions of active arm elevation in both flexion and abduction. By watching the patient move slowly through the range of motion, subtle anomalies can be identified. Additionally, adding 2 to 5 lbs in the hand increases the distal load and can elicit more scapular dysfunction. A categorization of this dynamic scapular observation has been reported and found to have a moderate inter- and intrarater reliability of 40% to 50%.39 The four categories described were normal, superior border pattern, medial border pattern, and inferior angle pattern (Box 50-1). These patterns of scapular motion have not been found to be associated with any specific glenohumeral injury. Further investigations into the patterns of scapular motion have demonstrated that altered scapular motion does not occur in isolation but more commonly occurs in combination. By modifying the categories to a simpler description of whether scapular dyskinesis is present or absent, the sensitivity of clinical observation reached 76% when compared with three-dimensional kinematic assessment of scapular motion (unpublished data).
BOX 50-1 Scapular Dyskinesis System Used to Categorize Abnormal Scapular Motion
Inferior Angle Pattern (Type I)
At rest, the inferior medial scapular border may be prominent dorsally. During arm motion, the predominant movement is that the inferior angle tilts dorsally and the acromion tilts ventrally over the top of the thorax. The axis of rotation for this pattern is in the horizontal plane.
Medial Border Pattern (Type II)
At rest, the entire medial border may be prominent dorsally. During arm motion, the predominant movement is that the medial scapular border tilts dorsally off the thorax. The axis of rotation is vertical in the frontal plane.
Superior Border Pattern (Type III)
At rest, the superior border of the scapula may be elevated, and the scapula can also be anteriorly displaced. During motion, the predominant movement is that a shoulder shrug initiates movement without significant winging of the scapula. The axis of this motion occurs in the sagittal plane.
Symmetrical Scapulohumeral Pattern (Type IV)
At rest, the positions of both scapulae are relatively symmetrical, taking into account that the dominant arm may be slightly lower. During arm motion, the scapulae rotate symmetrically upward so that the inferior angles translate laterally away from the midline and the scapular medial border remains flush against the thoracic wall. The reverse occurs during lowering of the arm.
Corrective maneuvers during the assessment of dynamic scapular motion can help the clinician estimate the effect of the scapular dyskinesis. The scapular assistance test may be used in patients with impingement symptoms. The examiner applies a firm upward rotation and posterior tilt to the scapula’s inferior angle and superior border as the patient elevates the arm (Fig. 50-2).40 The test is positive when the patient’s symptoms of a painful arc are reduced during active elevation with the scapula supported. The scapular assistance test validity has not been quantified. The scapular retraction test may be used in demonstrating rotator cuff weakness (Fig. 50-3).40 The test is positive when rotator cuff strength is increased during the scapular retraction test as compared with rotator cuff strength without the scapula retracted. If either test is positive, rehabilitation of scapular retraction or external rotation should precede rotator cuff–focused exercises.
Proximal Stability
Proximal factors influencing scapular dyskinesis are critical components in evaluating and treating scapular problems. Proximal hip and trunk stability can be screened by having the subject stand on one leg. Poor balance and Trendelenberg (hip-adducted) posture should be noted. A squat maneuver to 60 degrees of knee flexion evaluates dynamic control of the pelvic region. Dramatic loss of hip control such as excessive pelvic rotation in any plane (Fig. 50-4) and poor balance indicates poor dynamic pelvic control and merits further examination of hip and trunk muscular strength and flexibility.41
Strength
Scapular muscle strength can be screened with a wall push-up for gross serratus dysfunction such as is found in long thoracic palsy. A shoulder shrug has been demonstrated to be a valid assessment upper trapezius strength.42 The test originally described by Kendall43 for the lower trapezius has also been found to be a very good assessment of lower trapezius strength and preferentially activates the lower trapezius muscle.42,44 The patient lies prone with arm abducted to 135 degrees and thumb pointing toward the ceiling. A force is applied to the scapula or to the arm to cause shoulder extension. A weak lower trapezius is diagnosed if the subject is unable to hold this position or unable to hold it against minimal resistance. The middle trapezius is best tested by positioning the patient prone with elbow extended and shoulder externally rotated (thumb up) and applying a downward force at the forearm to make the patient produce scapular adduction.45 Various positions of prone horizontal abduction to discriminate the rhomboids from other synergistic muscles have not been able to isolate rhomboid activation.45 Therefore, weakness with shoulder horizontal abduction can be attributed to several muscles, including the middle trapezius and posterior deltoid, along with the rhomboids.
All complete shoulder evaluations include testing of the rotator cuff musculature. A modification of the supraspinatus strength test, the scapular retraction test, has been proposed by one of us (WBK).40 The purpose of this test is to better determine if rotator cuff weakness is true or apparent. The test is performed by first examining the strength of the supraspinatus in the typical manner. Then the patient retracts the scapula and, with the assistance of the examiner, maintains scapular retraction. The test is positive when strength is improved in the retracted position. This is considered an apparent rotator cuff weakness but not a true weakness because the performance improves with additional stabilization of the proximal attachment of the supraspinatus, the scapula. A negative test indicates a true rotator cuff weakness if the patient’s strength did not improve with the scapula stabilized.40 Through the use of a hand-held dynamometer, the scapular retraction test has been found to improve elevation strength by 24% over the traditional empty can strength test for the supraspinatus.46
Following a complete examination of the shoulder including glenohumeral instability, labral pathology, tendinopathy, and acromioclavicular and sternoclavicular joint integrity, a treatment plan to address scapular dysfunction is developed. The first step in an effective intervention is a thorough understanding of normal function and identification of deficits during the examination.47 This allows the clinician to develop a specific rehabilitation program.
REHABILITATION OF SCAPULAR DYSKINESIS
The body functions as an integrated system. Rehabilitation, like evaluation, needs to incorporate the entire functional unit. During rehabilitation our focus needs to shift from isolating the problem to providing interventions that address the athlete’s impairments and functional limitations. We take an integrated approach incorporating the kinetic-chain model, the motor-control pattern of proximal to distal activation, and many principles of proprioceptive neuromuscular facilitation to achieve the goals of restoring function. Consideration of the athlete’s impairments and environment must be integral to the intervention because the athlete is often attempting to return to the same activity that might have precipitated the initial injury.
From the comprehensive evaluation we have identified physical impairments such as tight or weak musculature and specific functional limitations of the patient that are going to be addressed during the rehabilitation program. Often the first two areas to address are posture and proximal stability. As we have mentioned, proximal dysfunctions can contribute to scapular dyskinesis. The position of the spine is intimately involved with the position and motion of the scapula and the humerus.34,48 Therefore, we often address proximal control of the trunk with trunk extension exercises to decrease thoracic kyphosis in concert with scapular retraction exercises.
Posture
Thoracic kyphosis reduces humeral elevation and limits normal scapular motion in such a manner to cause the scapula to be more protracted.34 A protracted scapula has been demonstrated by MRI to reduce the subacromial space49 and diminish humeral elevation strength.50 To address these common problems we recommend a program that facilitates trunk extension and scapular retraction. This can be accomplished in a variety of ways.
A dynamic exercise that is commonly attempted initially is called “elbows in the back pocket” (Fig. 50-5). This exercise starts with a forward flexed trunk and protracted scapula and ends with the patient in thoracic extension and scapular retraction. The patient is instructed to tuck the elbows into the back pocket during this maneuver and is closely watched to ensure he or she is getting good scapular retraction without excessive lumbar lordosis. Key teaching points are not shrugging the shoulders and not overly extending the lumbar spine.
If the back pocket exercise is too painful for the patient or the scapular control is not adequate, this exercise can be simplified to a low row exercise (Fig. 50-6). This exercise also incorporates both trunk and scapular motion simultaneously but has a smaller magnitude of motion and is more of an isometric exercise. The patient places the hand on either an immovable object (e.g., countertop) or uses a heavy elastic resistance. With the arm at the side, the patient extends the shoulder and depresses the scapula as he or she steps forward with the ipsilateral leg. This exercise has been found to produce low to moderate activation of the serratus anterior, lower trapezius, and posterior deltoid without significant activation of the upper trapezius (unpublished observation).
Both of these exercises incorporate one of the fundamental principles in kinetic chain rehabilitation: facilitating distal motion by initially activating the proximal musculature.51,52 Proximal activation of leg and trunk musculature before activating primary movers in to prepare the entire system for motion is called anticipatory postural adjustment.12,13 We emphasize trunk and leg motion to use this natural motor control pattern and to be sure the trunk is properly positioned to allow arm motion.
Flexibility of the surrounding shoulder musculature and spine is addressed early in the rehabilitation program in association with strengthening exercises. Stretching exercises such as corner stretch, scapular retraction on a roll, and biceps stretch (Fig. 50-7) are used to lengthen tight pectoral musculature, which has been demonstrated to negatively affect scapular kinematics.36 Each stretch should be held for 30 seconds and performed two or three times at least once a day.53 Cervical, thoracic, and lumbar spine flexibility exercises are prescribed to address mobility restrictions identified in the examination.

Figure 50-7 Biceps stretch to stretch the anterior shoulder musculature attaching to the scapula. It is critical that the scapula stays retracted and no neurologic symptoms are present during the maneuver.
The combination of stretching and strengthening exercises has been found to positively affect posture. Wang and colleagues54 demonstrated that a program of progressive resistive exercises using elastic resistance of horizontal abduction, scapular retraction with external rotation, shrugs, and shoulder abduction in the scapular plane along with corner stretching performed independently decreased thoracic kyphosis and improved scapular stability. A similar study performing shoulder external rotation, shoulder flexion, and horizontal adduction using elastic resistance exercises three times a week for 3 sets of 10 to 15 repetitions in combination with passively lengthening pectoralis minor and major musculature reduced forward scapular displacement by almost 1 cm in young competitive swimmers.35
Unfortunately, not all patients respond to stretching and strengthening exercises. In some chronic pain conditions, patients cannot correct their own posture and need external assistance. In the past, figure-of-eight clavicle straps and other braces reminding patients of their posture have been used. McConnell taping to either facilitate or inhibit scapular musculature might decrease pain and improve function.55-57 Scapular taping is typically applied to retract, posteriorly tilt, and externally rotate the scapula (Fig. 50-8) to allow the patient to perform functional activities with less pain.55 The tape is applied and left on for several days at a time until the patient demonstrates adequate neuromuscular control of the scapula independent of the tape.
One drawback of taping is that the patient requires the assistance of another to apply the tape. Therefore, the patient has to return to the clinic frequently or have another person trained to tape the scapula. Another drawback is that the tape is expensive and occasionally can irritate the patient’s skin. The spine and scapula stabilizing brace (Scapula Stabilizing System [S3], Alignmed, Santa Ana, Calif) corrects postural alignment of the scapular and spine by simulating the effects of taping (Fig. 50-9). The initial results of the brace on scapular kinematics suggest that the brace alters scapular posterior tilt and scapular external rotation in the lower ranges of arm elevation. Anecdotal reports from our patients with scapular dyskinesis are mixed; however, some patients do have good relief of symptoms from this orthosis. Further research is necessary to determine its effectiveness.
Proximal Stability
Proximal leg, trunk, and scapular musculature is activated to prepare the system for higher demanding distal loads. The proximal-to-distal muscle activation pattern is a normal motor-activation pattern for upper-extremity motions.12,14 To promote a functional rehabilitation approach, we attempt to recreate this activation approach. A common mistake in treating shoulder injuries is the early use of exercises that incorporate the entire length of the arm with resistance applied distally. The load of arm alone is approximately 5% of a person’s body weight.58 The often-inflamed structures about the shoulder are further aggravated when exercises that use even the weight of the arm alone are initiated. We attempt to reduce this occurrence in three ways: Strengthen proximal muscles first to avoid inflaming healing tissues further, use the proximal muscles to assist in moving the distal extremity through momentum, and support the weight of the upper arm by keeping it in contact with a surface during large arcs of motion initially until proper mechanics and neuromuscular control of the motion are demonstrated.
Trunk strength and stability are initially screened during the examination with the single leg stance and squat. In patients demonstrating poor stability, specific strength tests are performed on hip musculature to identify specific strength deficits. The hip deficits are incorporated with the core stabilization exercise program, focusing on activating transverse abdominus and multifidus muscles by performing a drawing in maneuver. Activation of these muscles always precedes distal arm motion.13,59 In patients with significant core stabilization deficits, a basic mat program should be initiated, progressing to functional motions. An ideal period to focus on core stabilization exercises is in the immobilization period following a shoulder surgery or significant injury, when shoulder activities are limited. The core stabilization program can be emphasized on alternating days to break up the redundancy of a rehabilitation program in an athletic environment when patients are seen frequently.
Kinetic chain shoulder exercises attempt to use the trunk and legs to gain control of the trunk and facilitate scapula and shoulder motion. Knott and Voss call this irradiation, a process of facilitating inhibited muscle by activating stronger muscles that are synergistic for a movement pattern.60 We focus on facilitating scapular retraction (external rotation, posterior tilt, depression) as our primary goal to gain proximal stability for the shoulder. The treating clinician needs to have several methods to facilitate this control and progressively increase the demands to strengthen the periscapular musculature. Use of sagittal trunk motion, by starting with trunk flexed and moving into extension, to facilitate scapular retraction is a first-line activity. Integrating horizontal rotation or frontal plane motions can be incorporated to provide variety or if sagittal motions do not produce the desired scapular retraction with correct trunk posture. Incorporating a 4- to 6-inch step into an exercise engages the lower extremity and trunk musculature involuntarily. This additional demand recruits a greater neuromotor pool of the proximal musculature to assist stabilization and requires patients to work on postural stability by challenging their balance.
The individual needs of the patient, the fundamental principles of physiologic healing tissue restrictions, and progressing from low- to high-demand activities are always respected during the course of rehabilitation. Examples of scapular retraction exercises are provided in attempt to meet the goals outlined earlier (Box 50-2 and Figs. 50-10 to 50-13) Typically, the patient can control the scapula with these integrative techniques; however, some patients require manual assistive and resistive techniques described as rhythmic initiation and reversal of antagonists.60 These techniques can be performed with the patient side lying, if necessary, to isolate scapular muscle control as described by Adler,61 or they can be performed standing, applying resistance to the scapula through the motion.
BOX 50-2 Scapular Retraction Exercises
Isometric Exercises
Isometric exercises are used for patients to activate scapular retractors in a controlled environment requiring minimal to no glenohumeral motion.
LOW ROW (SEE FIG. 50-6)
The low row produces scapular retraction and depression. With the hand at the side, extension of the shoulder is coordinated with a forward weight shift to the opposite leg. This can be performed isometrically and progressed to an isotonic exercise. Be certain the lower trapezius is activated and the scapula is depressing.
INFERIOR GLIDE (SEE FIG. 50-10)
The inferior glide produces scapular retraction with shoulder adduction with the arm abducted to approximately 90 degrees. Be certain the lower trapezius is activated and the scapula is depressing.
Dynamic Standing Exercises
Dynamic standing exercise is the most common. The patient takes an astride athletic position to perform these exercises with the opposite side leg slightly forward.
LAWNMOWER (IN SLING)
The patient starts with the trunk flexed and rotated slightly toward the opposite leg. The scapula is retracted and the arm is supported in a sling. The motion is the same as in the standard lawnmower exercise but with small amplitude and low intensity.
LAWNMOWER SUPPORTED (SEE FIG. 50-11)
The patient strives for the same scapular retraction end position, but the arm is free to move and the weight of the arm is supported so as not to overload inflamed tissues in the glenohumeral joint.
LAWNMOWER ON A STEP (SEE FIG. 50-12)
The patient starts with the trunk flexed and rotated trunk the opposite leg. The scapula is retracted with the arm externally rotating. The addition of the step is to facilitate more trunk and pelvic muscle activation to encourage better scapular retraction during the maneuver.
Dynamic Sitting Exercises
Dynamic sitting exercises are for patients who have lower-extremity limitations that preclude them from dynamic standing activities or who need to perform a significant component of their sports in a nonstanding phase such as swimming, water polo, and volleyball. Dynamic sitting activities can be started on a stable chair and progressed to a Swiss ball or a wobble board for home therapy. The patient is progressed to place the feet on the unstable surface to increase trunk demand.
SCAPULAR RETRACTION ON BALL (SEE FIG. 50-13)
The lawnmower exercise is performed in a sitting position to facilitate scapular retraction with greater emphasis placed on trunk and scapular musculature, because the legs cannot contribute as much. The patient sits on a Swiss ball and reaches with the affected arm down toward the weight-bearing ankle. The patient retracts and depresses the scapula while pulling the elbow toward the back pocket and shifting the weight toward the opposite leg.
DIAGONAL ROTATIONS ON BALL
Perform a diagonal resistance pattern while sitting on a ball. This exercise simulates throwing activities such as arm cocking, pulling arm into abduction, and external rotating and it simulates the acceleration phase of throwing, bringing the arm from overhead diagonally across the body.

Figure 50-10 Inferior glide with the scapula posteriorly tilting due to activation of the lower trapezius muscle.
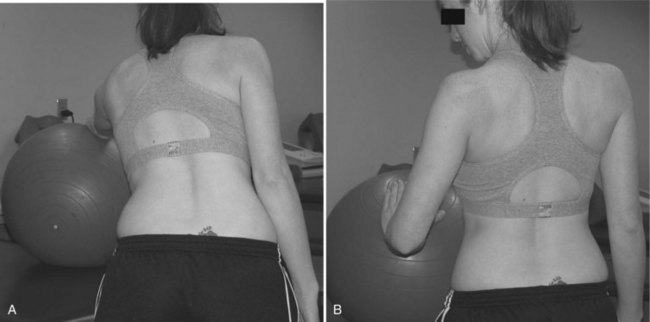
Figure 50-11 Lawnmower exercise, supported, allows the patient to start moving through the functional range of motion but does not overload healing tissues by keeping the weight of the arm supported on the Swiss ball. A, Starting position, to be adjusted to limits of comfort and motion restrictions. B, Ending position to emphasize scapular retraction.
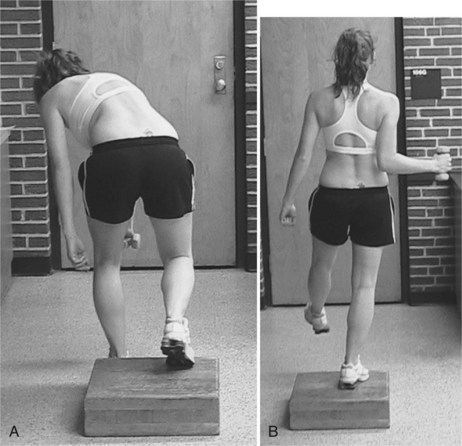
Figure 50-12 Lawnmower exercise on a step to facilitate core muscle activation. A, Starting position to prestretch target musculature, B, Finishing position incorporates lower extremity stability with trunk and scapular retraction in a single exercise.

Figure 50-13 Scapular retraction on a Swiss ball. A, Start by reaching toward the ipsilateral leg with weight on the ipsilateral foot and the contralateral foot slightly off the ground. B, Finish by retracting the scapula and tucking elbow into the back pocket as weight is shifted off the ipsilateral foot onto the contralateral foot.
Overhead Elevation Progression
Arm elevation progression can begin when a patient demonstrates adequate scapular stability with retraction. It is not expected that the athlete will go through an entire retraction program before initiating elevation exercises. However, it is a common rehabilitation error that patients are given elevation exercises that are too demanding, which result in scapular substitutions and inflamed shoulder tissues. The primary aim during this progression is to gain the pain-free and substitution-free full active arm elevation unsupported. Once this is obtained, more-demanding strengthening programs are initiated, leading to task- and sport-specific activities.
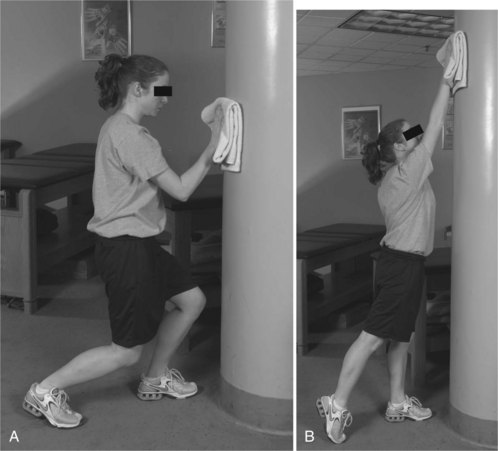
The initial arm elevation exercises should be performed with the arm supported and initiated by the trunk and legs. Support of the arm can be easily obtained by sliding the hand along a surface. Lephart described this type of motion as a “movable boundary with axial load.”62 The friction between these two surfaces should be minimized to allow the patient to move the arm freely. This can be obtained by using a towel on a glass or smooth wooden door or using lotion or powder on a treatment plinth. The arm load is diminished and the demand is lessened on shoulder musculature by placing the hand in contact with a surface.63 Progressing from horizontal limited flexion angle (∼ 60 degrees) to a vertical surface allowing full flexion is a logical progression. However, in arm-elevation exercises that are near 90 degrees, the load of the arm is the greatest and increases the demand on shoulder musculature.63,64 In some cases, patients tolerate vertical motions before they tolerate more diagonal reaching motions that place the arm at 90 degrees. These arm elevation motions are initiated by placing the patient in the astride athletic position, with the hips and knees flexed, and instructing the patient to drive the arm up by extending the lower legs and continuing the reaching task through the upper extremity (Fig. 50-14). This allows momentum to be used. As strength of the shoulder increases, less use of trunk motion is encouraged to decrease the use of momentum. Removal of the support surface makes the exercise a more-functional open-kinetic-chain strengthening exercises.
Strengthening Progression
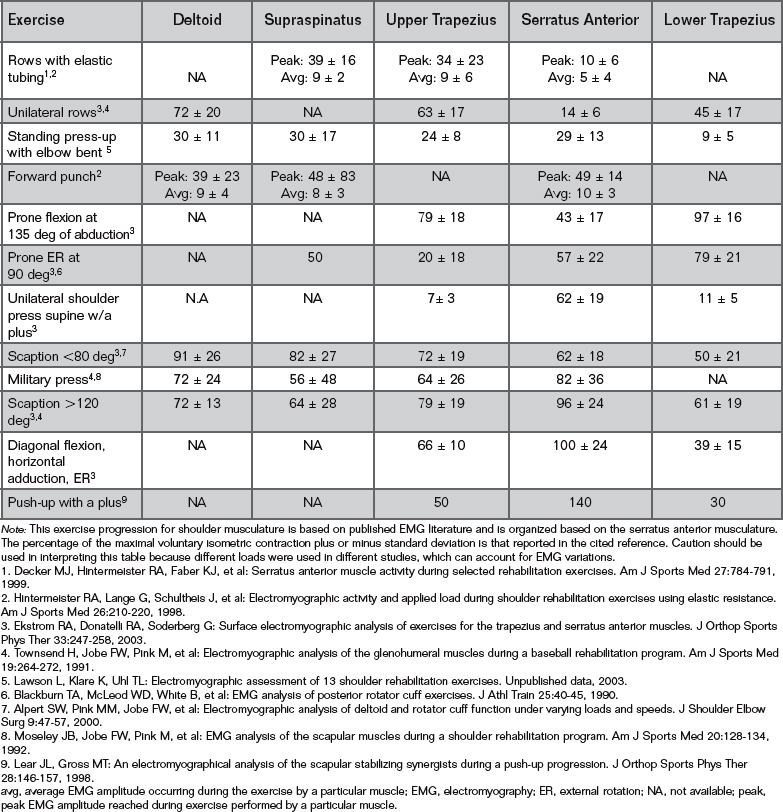
Patients can progress to traditional long-lever-arm resistance exercises to strengthen and gain endurance once they demonstrate proper control of shoulder and scapular motion during both retracting and overhead reaching activities. The patient should be able to elevate at least to 120 degrees without resistance without scapular winging or shrugging (dyskinesis). The exercises described to this point have focused on gaining neuromuscular control of the scapula through using the kinetic chain. Incorporating resistive exercises that have been found to activate shoulder and scapular musculature by electromyographical (EMG) studies is important. The challenge of increasing load, repetitions, and speed are all factors that should be incorporated into the recovery and sport-specific phases of rehabilitation after a solid base of the spine and scapula are established.
EMG studies have focused on identifying which exercise maximally activates the scapular musculature. In 1992, Moseley65 published core exercises to maximally activate the trapezius, serratus anterior, and rhomboids. Other researchers have investigated other shoulder exercises to help develop an exercise progression for clinicians to strengthen scapular and shoulder musculature.44,66-68 One major underlying principle of rehabilitation is to progress from lower-demand to higher-demand activities without overloading healing tissues. This guiding principle in rehabilitation has led us to develop a scapular strengthening exercise progression based on the available literature. The exercise progression starts from the point of the patient demonstrating controlled active forward elevation without scapular substitutions and pain (Table 50-1). The exercise order is changed depending on the target musculature; for this table we targeted the serratus anterior.
SUMMARY
It is important to evaluate dynamic function of the scapula with and without load and evaluate trunk position and control during dynamic activities such as a single-leg squat. If all impairments are not identified in a complete assessment, the athlete is likely to return with similar complaints. Our rehabilitation approach addresses the deficits identified in the examination with particular focus on improving trunk and scapular posture. Rehabilitation that focuses on enhancing proximal stability and control of pelvis, trunk, and scapula should establish a foundation; then, patient-specific exercises that gradually increase the demands of the scapular and shoulder musculature can be built on this foundation.
1 Feltner ME, Dapena J. Three-dimensional interactions in a two-segment kinetic chain. Part I: General model. Int J Sport Biomech. 1989;5:403-419.
2 Putnam CA. Sequential motions of body segments in striking and throwing skills: Description and explanations. J Biomech. 1993;26:125-135.
3 Hirashima M, Kadota H, Sakurai S. Sequential muscle activity and its function role in the upper extremity and trunk during overarm throwing. J Sports Sci. 2002;20:301-310.
4 Fleisig GS, Barrentine SW, Escamilla RF, et al. Biomechanics of overhand throwing with implications for injuries. Sports Med. 1996;21:421-437.
5 Toyoshima S, Hoshikawa T, Miyashita M. Contributions of Body Parts to Throwing Performance. In: Biomechanics IV. Baltimore: University Park Press; 1974:169-174.
6 Kibler WB. Biomechanical analysis of the shoulder during tennis activities. Clin Sports Med. 1996;14:79-85.
7 Davids K, Glazier P, Arajuo D, et al. Movement systems as dynamic systems: The functional role of variability and its implications for sports medicine. Sports Med. 2003;33:245-260.
8 Kraemer WJ, Triplett NT, Fry AC. An in-depth sports medicine profile of women college tennis players. J Sport Rehabil. 1995;4:79-88.
9 Inman VT, Saunders M, Abbott LC. Observations of the function of the shoulder joint. J Bone Joint Surg Am. 1944;26:1-31.
10 Perry J. Anatomy and biomechanics of the shoulder in throwing, swimming, gymnastics, and tennis. Clin Sports Med. 1983;2:247-270.
11 Davidson PA, El Attrache NS, Jobe CM, et al. Rotator cuff and posterior-superior glenoid labrum injury associated with increased glenohumeral motion: A new site of impingement. J Shoulder Elbow Surg. 1995;4:384-390.
12 Zattara M, Bouisset S. Posturo-kinetic organisation during the early phase of voluntary upper limb movement. 1 Normal subjects. J Neurol Neurosurg Psychiatry. 1988;51:956-965.
13 Cordo PJ, Nashner LM. Properties of postural adjustments associated with rapid arm movements. J Neurophysiol. 1982;47:287-308.
14 Bouisset S, Zattara M. A sequence of postural movements precedes voluntary movement. Neurosci Lett. 1981;22:263-270.
15 Le Bozec S, Lesne J, Bouisset S. A sequence of postural muscle excitation precedes and accompanies isometric ramp efforts performed while sitting in human subjects. Neurosci Lett. 2001;303:72-76.
16 Karduna AR, McClure PW, Michener LA, et al. Dynamic measurements of three-dimensional scapular kinematics: A validation study. J Biomech Eng. 2001;123:184-190.
17 McClure PW, Michener LA, Sennett BJ, et al. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg. 2001;10:269-277.
18 Warner JJP, Micheli LJ, Arslanian LE, et al. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome. A study using Moiré topographic analysis. Clin Orthop RelRes. 1992;285:191-199.
19 Rubin BD, Kibler WB. Fundamental principles of shoulder rehabilitation: Conservative to postoperative management. Arthroscopy. 2002;18:29-39.
20 Schultz JS, Leonard AJr. Long thoracic neuropathy from athletic activity. Arch Phys Med Rehabil. 1992;73:87-90.
21 Warner JJ, Navarro RA. Serratus anterior dysfunction. Recognition and treatment. Clin Orthop RelRes. 1998;349:139-148.
22 Cools AM, Witvrouw E, Declercq GA, et al. Evaluation of isokinetic force production and associated muscle activity in the scapular rotators during a protraction-retraction movement in overhead athletes with impingement symptoms. Br J Sports Med. 2004;38:64-68.
23 Borstad JD, Ludewig PM. The effect of pectoralis minor length on scapular kinematics in subjects without shoulder pathology [abstract]. J Orthop Sports Phys Ther. 2004;34(1):A16.
24 McQuade KJ, Dawson JD, Smidt GL. Scapulothoracic muscle fatigue associated with alterations in scapulohumeral rhythm kinematics during maximum resistive shoulder elevation. J Orthop Sports Phys Ther. 1998;28:74-80.
25 Tsai L, Wredmark T, Johansson C, et al. Shoulder function in patients with unoperated anterior shoulder instability. Am J Sports Med. 1991;19:469-473.
26 Brox JI, Roe C, Saugen E, et al. Isometric abduction muscle activation in patients with rotator tendinosis of the shoulder. Arch Phys Med Rehabil. 1997;78(11):1260-1267.
27 Scovazzo ML, Browne A, Pink M, et al. The painful shoulder during freestyle swimming, an electromyographic cinematographic analysis of twelve muscles. Am J Sports Med. 1991;19:577-582.
28 Wadsworth DJ, Bullock-Saxton JE. Recruitment patterns of the scapular rotator muscles in freestyle swimmers with subacromial impingement. Int J Sports Med. 1997;18:618-624.
29 Glousman R, Jobe FW, Tibone JE, et al. Dynamic electromyographic analysis of the throwing shoulder with glenohumeral instability. J Bone Joint Surg Am. 1988;70:220-226.
30 Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80:276-291.
31 Lukasiewicz AC, McClure P, Michener L, et al. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther. 1999;29:574-586.
32 Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: Spectrum of pathology. Part I: Pathoanatomy and biomechanics. Arthroscopy. 2003;19:404-420.
33 Kamkar A, Irrgang JJ, Whitney SL. Nonoperative management of secondary shoulder impingement syndrome. J Orthop Sports Phys Ther. 1993;17:212-224.
34 Kebaetse M, McClure P, Pratt N. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinetics. Arch Phys Med Rehabil. 1999;80:945-950.
35 Kluemper M, Uhl TL, Hazelrigg H. Effect of stretching and strengthening shoulder muscles on forward shoulder posture in competitive swimmers. J Sport Rehabil. 2006;15:58-70.
36 Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35:227-238.
37 Kibler WB. Role of the scapula in the overhead throwing motion. Contemp Orthop. 1991;22:525-532.
38 Odom CJ, Taylor AB, Hurd CE, et al. Measurement of scapular asymmetry and assessment of shoulder dysfunction using the lateral scapular slide test: A reliability and validity study. Phys Ther. 2001;81:799-809.
39 Kibler WB, Uhl TL, Maddux JQ, et al. Qualitative clinical evaluation of scapular dysfunction. A reliability study. J Shoulder Elbow Surg. 2002;11:550-556.
40 Kibler WB, McMullen J. Scapular dyskinesis and its relation to shoulder pain. J Am Acad Orthop Surg. 2003;11:142-151.
41 DiMattia MA, Livengood AL, Uhl TL, et al. What are the validity of the single-leg squat test and its relationship to hip abduction strength. J Sport Rehab. 2005;14:108-123.
42 Michener LA, Boardman ND, Pidcoe PE, et al. Scapula muscle tests in subjects with shoulder pain and functional loss: reliability and construct validity. Phys Ther. 2005;85:1128-1138.
43 Kendall FP, McCreary EK, Provance PG. Upper extremity and shoulder girdle strength test. In: Butler JP, editor. Muscle Testing and Function. Baltimore: Williams & Wilkins; 1993:235-298.
44 Ekstrom RA, Donatelli RA, Soderberg G. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J Orthop Sports Phys Ther. 2003;33:247-258.
45 Smith J, Padgett DJ, Kaufman KR, et al. Rhomboid muscle electromyography activity during 3 different manual muscle tests. Arch Phys Med Rehab. 2004;85:987-992.
46 Kibler WB, Sciascia A, Dome D. Evaluation of apparent and absolute supraspinatus strength in patients with shoulder injury using the scapular retraction test. Am J Sports Med. 2006;34:1643-1647.
47 Kibler WB, Livingston B, Bruce R. Current concepts in shoulder rehabilitation. Adv Oper Orthop. 1995;3:249-299.
48 Kapandji IA. The shoulder. In: Kapandji IA, editor. The Physiology of the Joints. New York: Churchill Livingstone; 1982:2-71.
49 Solem-Bertoft E, Thuomas KA, Westerberg CE. The influence of scapular retraction and protraction on the width of the subacromial space. An MRI study. Clin Orthop Relat Res. 1993;296:99-103.
50 Smith J, Kotajarvi BR, Padgett DJ, Eischen JJ. Effect of scapular protraction and retraction on isometric shoulder elevation strength [abstract]. Arch Phys Med Rehab. 2002;83:367-370.
51 McMullen J, Uhl TL. A kinetic chain approach for shoulder rehabilitation. J Athl Train. 2000;35:329-337.
52 Kibler WB, McMullen J, Uhl T. Shoulder rehabilitation strategies, guidelines, and practice. Orthop Clin North Am. 2001;32:527-538.
53 Bandy WD, Irion JM, Briggler M. The effect of time and frequency of static stretching on flexibility of the hamstring muscles. Phys Ther. 1997;77:1090-1096.
54 Wang C-H, McClure P, Pratt N, et al. Stretching and strengthening exercises: Their effect on three-dimensional scapular kinematics. Arch Phys Med Rehabil. 1999;80:923-929.
55 Host HH. Scapular taping in the treatment of anterior shoulder impingement. Phys Ther. 1995;75:803-811.
56 Cools AM, Witvrouw EE, Danneels LA, et al. Does taping influence electromyographic muscle activity in the scapular rotators in healthy shoulders? Man Ther. 2002;7:154-162.
57 Ackermann B, Adams R, Marshall E. The effect of scapula taping on electromyographic activity and musical performance in professional violinists. Aust J Physiother. 2002;48:197-203.
58 Dempster WT: Space requirements of the seated operator: Geometrical, kinematic, and mechanical aspects of the body, with special reference to the limbs. Technical Report TR-55-159. Wright-Patterson Air Force Base, Ohio, 1955.
59 Hodges PW, Richardson CA. Feedforward contraction of transversus abdominus is not influenced by the direction of arm movement. Exp Brain Res. 1997;114:362-370.
60 Knott M, Voss DE. Proprioceptive Neuromuscular Facilitation Patterns and Techniques. Philadelphia: Harper & Row, 1968.
61 Adler SS, Beckers D, Buck M. PNF in Practice: An Illustrated Guide. New York: Springer-Verlag, 1993.
62 Lephart SM, Henry TJ. The physiological basis for open and closed kinetic chain rehabilitation for the upper extremity. J Sport Rehabil. 1996;5:71-87.
63 Wise MB, Uhl TL, Mattacola CG, et al. The effect of limb support on muscle activation during shoulder exercises. J Shoulder Elbow Surg. 2004;13:614-620.
64 Poppen N, Walker P. Forces at the glenohumeral joint in abduction. Clin Orthop Rel Res. 1978;135:165-170.
65 Moseley JB, Jobe FW, Pink M, et al. EMG analysis of the scapular muscles during a shoulder rehabilitation program. Am J Sports Med. 1992;20:128-134.
66 Decker MJ, Hintermeister RA, Faber KJ, et al. Serratus anterior muscle activity during selected rehabilitation exercises. Am J Sports Med. 1999;27:784-791.
67 Decker MJ, Tokish JM, Ellis HB, et al. Subscapularis muscle activity during selected rehabilitation exercises. Am J Sports Med. 2003;31:126-134.
68 Ekstrom RA, Bifulco KM, Lopau CJ, et al. Comparing the function of the upper and lower parts of the serratus anterior muscle using surface electromyography. J Orthop Sports Phys Ther. 2004;34:235-243.