Chapter 52 Venous Thrombosis
Definitions
Deep vein thrombosis (DVT) refers to an obstruction of a deep vein by thrombus, usually in the legs or pelvis but occasionally in the arms. Thrombus from these sites can travel to the lungs to produce pulmonary embolism (PE), which occurs when the thrombus obstructs a pulmonary artery. This process is known as venous thromboembolism (VTE). Blockage of blood flow through the lungs and the resultant increased pressure in the right ventricle are responsible for the symptoms and signs of PE,1 whereas obstructed outflow of blood from occluded veins in the legs or arms produces symptoms and signs of DVT.
Epidemiology
Venous thromboembolism, which includes DVT and PE, represents the third most common cause of cardiovascular death after myocardial infarction (MI) and strokes. A first episode of VTE occurs in about 1 person per 1000 each year in the United States.2 The incidence rises exponentially with age, with 5 cases per 1000 persons per year by the age of 80 years. Although men and women are affected equally, the incidence is higher in Caucasians and African Americans than in Hispanic persons and Asian Pacific Islanders.3
Approximately one third of patients with symptomatic VTE present with PE; the remainder present with DVT alone.4 Up to half of patients with a first episode of VTE have no identifiable risk factors and are described as having unprovoked or idiopathic VTE. The remainder develop VTE secondary to well-recognized transient risk factors such as surgery or immobilization. Pulmonary embolism accounts for an estimated 15% of deaths in hospitalized patients, with at least 100,000 deaths from PE each year in the United States.
Pathobiology
Pulmonary embolism and DVT are part of the spectrum of VTE and share the same genetic and acquired risk factors that determine the intrinsic risk of VTE for each individual5 (Fig. 52-1). Genetic risk factors include abnormalities associated with hypercoagulability of the blood, the most common of which are factor V Leiden and the prothrombin 20210 gene mutations. Acquired risk factors include advanced age, history of previous VTE, obesity, and active cancer, all of which limit mobility and may be associated with hypercoagulability. Superimposed on this background risk, VTE often occurs in the presence of a triggering factor that increases risk above the critical threshold. Such triggering factors (e.g., surgery, pregnancy, estrogen therapy) lead to vascular damage, stasis, and/or hypercoagulability, the components of Virchow’s triad.
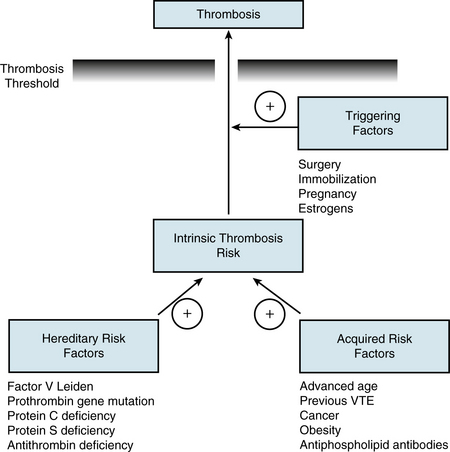
Figure 52-1 Thrombosis threshold. Hereditary and acquired risk factors combine to create an intrinsic risk of thrombosis for each individual. This risk is increased by extrinsic triggering factors. If intrinsic and extrinsic forces exceed a critical threshold where thrombin generation overwhelms protective mechanisms, thrombosis occurs. VTE, venous thrombembolism.
In at least 90% of patients, PE originates from DVT in the lower limbs, and up to 70% of patients with proven PE still have demonstrable DVT upon presentation. Thrombi usually start in the calf veins.4 About 20% of these calf vein thrombi then extend into the popliteal and more proximal veins of the leg, from which they are more likely to embolize. Although often asymptomatic, PE can be detected in about 50% of patients with proximal DVT. Upper-extremity DVT involving the axillary and/or subclavian veins also can give rise to PE, but only 10% to 15% of such patients develop PE. Upper-extremity DVT most often occurs in patients with cancer, particularly those with indwelling central venous catheters. Unprovoked upper-extremity DVT, usually involving the dominant arm, can occur with strenuous effort—the so-called Paget-Schroetter’s syndrome.6
Clinical Manifestations
Recognizing VTE can be challenging because the symptoms and signs of both DVT and PE are neither sensitive nor specific for these disorders.1 A high index of suspicion is needed because DVT is often asymptomatic, and many cases of fatal PE go unsuspected prior to death. The clinical suspicion of VTE should be prompted by a constellation of risk factors, symptoms, signs, findings on electrocardiography, chest radiography, echocardiography, and blood test results. Although clinical assessment alone is insufficient to establish or exclude the diagnosis of VTE, clinical prediction rules are useful for establishing a pretest probability in which patients can either be classified as being at low, medium, or high probability of having DVT and/or PE, or as being unlikely or likely to have DVT and/or PE based on the estimated prevalence of the disease. Therefore, clinical pretest probability assessment serves as the root of algorithms for the diagnosis of DVT and PE.7
Symptoms and Signs
Although most DVT originates in the calf veins, symptoms and signs are uncommon until there is extension into the more proximal veins, which obstructs outflow of blood from the leg. The symptoms and signs of DVT may be acute and progressive, or they may resolve spontaneously if the thrombus undergoes lysis or embolism. Clinical manifestations of DVT may include tenderness or pain, swelling, and warmth and erythema of the skin. Pain on forced dorsiflexion of the foot (Homans sign) is neither sensitive nor specific for DVT. The differential diagnosis of DVT should be framed in the context of clinical presentation and underlying risk factors for VTE. Trauma, cellulitis, ruptured Baker cyst, musculoskeletal pain, or asymmetrical swelling unrelated to DVT may produce signs and symptoms compatible with acute DVT.
Diagnosis of Deep Vein Thrombosis
Because the clinical features are nonspecific, diagnosis of DVT requires objective testing. Patients who need such testing can be identified by their pretest likelihood of DVT, using validated clinical prediction rules (Table 52-1) that include components of the clinical assessment, presence of risk factors for VTE, and absence of an alternative diagnosis to explain the symptoms and signs.8 Based on the results of such an assessment, the pretest likelihood of VTE can be designated either as low, moderate, or high, or as unlikely or likely, and this assessment then guides subsequent selection of blood tests, such as the D-dimer assay, and noninvasive or invasive tests for definitive diagnosis of DVT. Tests for diagnosis of DVT also are relevant in patients with suspected PE because a diagnosis of proximal DVT in such patients provides sufficient grounds for initiation of treatment, and the treatment of DVT and PE are usually the same. Noninvasive tests include computed tomographic (CT) pulmonary angiography or ventilation/perfusion (V/Q) lung scanning for diagnosis of PE, and venous compression ultrasound for diagnosis of DVT. These tests have largely replaced pulmonary angiography (for the diagnosis of PE) and venography (for the diagnosis of DVT).
Table 52-1 Wells Clinical Prediction Model for Likelihood of Deep Vein Thrombosis
| Variable | Points |
|---|---|
| Predisposing Factors | |
| Active cancer | 1 |
| Paralysis, paresis, or recent cast immobilization | 1 |
| Bedridden more than 3 days or recent major surgery | 1 |
| Previous VTE | 1 |
| Symptoms | |
| Localized tenderness along deep veins | 1 |
| Swelling of entire leg | 1 |
| Signs | |
| Calf swelling over 3 cm compared with asymptomatic limb | 1 |
| Pitting edema | 1 |
| Collateral superficial veins | 1 |
| Clinical Judgment | |
| Alternative diagnosis at least as likely | − 2 |
| Clinical Probability | Total Points |
|---|---|
| Low | <1 |
| Intermediate | 1-2 |
| High | >2 |
| Unlikely | <2 |
| Likely | ≥2 |
VTE, venous thromboembolism.
Adapted from Scarvelis D, Wells PS: Diagnosis and treatment of deep-vein thrombosis. CMAJ 175:1087–1092, 2006.
Diagnostic Tests
D-dimer
A plasmin-derived degradation product of cross-linked fibrin, D-dimer can be measured in whole blood or plasma to provide an indirect index of ongoing activation of the coagulation system. Sensitivity of an elevated D-dimer level for the diagnosis of VTE ranges from 85% to 98%, but all available D-dimer assays have low specificities.9 False-positive D-dimer elevations can occur with advanced age, chronic inflammatory conditions, malignancy, and during the later stages of pregnancy and the postpartum period. In addition, hospitalized patients are more likely to have an elevated D-dimer level than outpatients, which renders the test less useful in this setting. Because of this lack of specificity, the value of the D-dimer assay resides with its high negative predictive value and the ability of a normal D-dimer to reduce the probability of VTE sufficiently to avoid further diagnostic testing in patients with a low or moderate pretest likelihood, who represent up to 30% of patients with suspected VTE.
Compression ultrasound
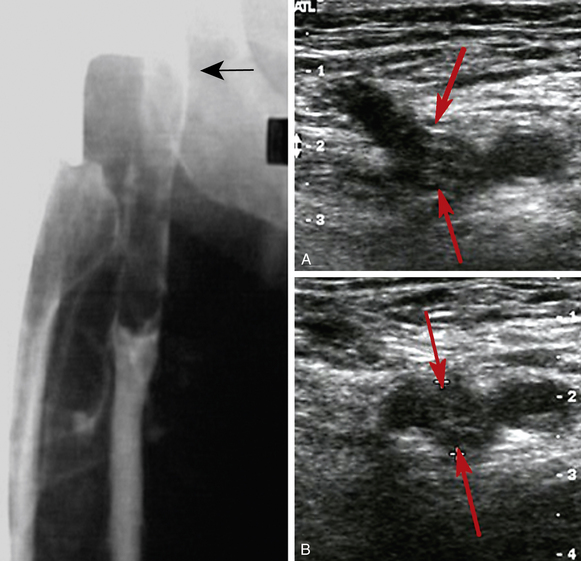
The diagnosis of DVT (also see Chapter 12) is usually based on venous compression ultrasound (Fig. 52-2), which has a sensitivity and specificity of about 95% for the diagnosis of proximal DVT.10 For calf DVT, the sensitivity of compression ultrasound is only about 73%. Because of the reduced sensitivity for detection of calf DVT, many centers restrict ultrasound testing to the proximal veins and only scan the region of the calf veins where they join the popliteal vein.
Computed tomographic venography
When combined with CT pulmonary angiography, CT venography is a simple test to diagnose DVT because both tests require only one injection of contrast dye. Compared with CT pulmonary angiography alone, the combination of CT pulmonary angiography plus CT venography increases sensitivity from 83% to 90%, but specificity remains unchanged, thereby resulting in only a modest increase in negative predictive value.8 Computed tomography venography adds significant radiation exposure and only marginally increases overall detection rate, so venous compression ultrasound is preferred because it provides the same information without exposing patients to ionizing radiation. Standard venography is not recommended in patients with suspected PE.
Contrast venography
Although contrast venography remains the gold standard for diagnosing DVT,11 the test is rarely performed in many centers (see Fig. 52-2). Venography is generally safe, but it can be uncomfortable and may be complicated by hypersensitivity reactions or superficial phlebitis. If the test is available, it should be considered when noninvasive testing is not diagnostic.
Diagnostic Strategies
Diagnostic strategies usually start with assessment of the pretest probability of VTE, using validated risk assessment models for either DVT (see Table 52-1) or PE (see Chapter 14), depending on the clinical presentation.12 Patients can be classified as having a low, intermediate, or high pretest likelihood of VTE, or as being unlikely or likely to have VTE, and can then undergo further evaluation according to the appropriate algorithm.
Algorithm for diagnosis of deep vein thrombosis
Patients with a low pretest likelihood of DVT or those unlikely to have DVT should undergo D-dimer testing (Fig. 52-3). A negative D-dimer test excludes the diagnosis of DVT, whereas a positive test should prompt compression ultrasound examination.13 A negative ultrasound excludes the diagnosis, whereas a positive test establishes it. Patients with an intermediate or high pretest likelihood of DVT or those likely to have DVT should be sent directly for compression ultrasound examination. A positive compression ultrasound establishes the diagnosis. If the ultrasound is negative, it is helpful to then perform D-dimer testing. If the D-dimer test is negative, the diagnosis of DVT can be excluded. In contrast, a positive D-dimer test should prompt a follow-up compression ultrasound in 1 week to exclude the possibility of calf DVT with interval extension. Follow-up ultrasound testing in 1 week should be done routinely if D-dimer testing is not performed. The diagnosis of DVT can be excluded if the follow-up test is negative.
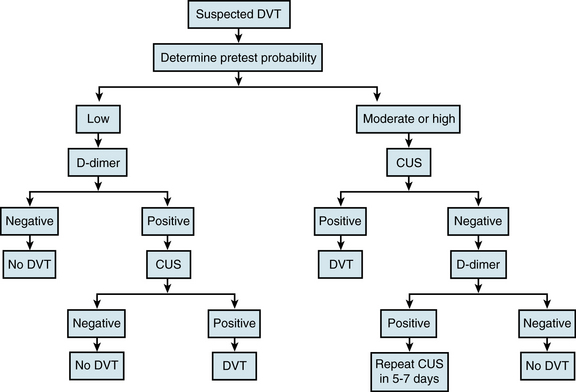
Figure 52-3 Clinical management of patients with suspected deep vein thrombosis (DVT). CUS; venous compression ultrasound.
Whole-leg compression ultrasound examination can prevent the need for a follow-up examination in 1 week.14 This more time-consuming technique, which involves careful evaluation of the entire venous system, requires a high-performance scanner and an experienced operator. The advantage of this approach is that it will detect calf DVT as well as those in the more proximal veins. However, the accuracy of compression ultrasound for detection of calf DVT is lower than that for proximal DVT. Consequently, whole-leg ultrasound examination should only be performed in centers where the test has been validated.
Other tests
Once a diagnosis of DVT has been established, other routinely ordered tests should include a complete blood cell count (CBC), platelet count, baseline international normalized ratio (INR), and activated partial thromboplastin time (APTT) to help guide anticoagulation. A creatinine (Cr) level and blood urea nitrogen (BUN) level also provide useful information to guide the choice of therapy, as do serum electrolytes and liver enzymes.
Thrombophilia testing has been advocated to identify patients with unprovoked (idiopathic) VTE who are at high risk of recurrence and who may therefore benefit from indefinite anticoagulation therapy. Although the common inherited thrombophilic disorders (see Fig. 52-1) are predictive of an increased risk of first-ever VTE, they do not appear to be associated with an increased risk of recurrence in patients who have already had an episode of VTE. Consequently, the results of thrombophilia testing rarely alter clinical management.15 Exceptions may include rare patients who are homozygous for factor V Leiden or prothrombin gene mutations, those with antithrombin, protein C, or protein S deficiency, patients with more than one thrombophilic disorder, and those with antiphospholipid antibody syndrome; such patients may benefit from long-term anticoagulation treatment (see Treatment).
Treatment
Although anticoagulant therapy remains the mainstay of treatment of VTE, patients with severe PE may require urgent reperfusion therapy to increase blood flow to the pulmonary arteries, thereby reducing pulmonary artery pressure. Therefore, rapid risk stratification is crucial to help guide treatment (see Chapter 14). The role of reperfusion therapy in patients with DVT is less clear. Venous thromboembolism patients who have contraindications to anticoagulant therapy may require insertion of an inferior vena cava filter.
Reperfusion Therapy
Patients with severe PE associated with hypotension or shock may benefit from pharmacological, mechanical, or surgical reperfusion therapy. Pharmacological reperfusion therapy involves systemic administration of a fibrinolytic agent. Mechanical reperfusion includes percutaneous catheter embolectomy with thrombus fragmentation, an approach that avoids the need for fibrinolytic drugs altogether,16 or catheter-directed fibrinolytic therapy, which requires lower doses of fibrinolytic agents than used for systemic administration. In some centers, surgical pulmonary embolectomy may be an option for patients who have severe PE and are at high risk for bleeding with systemic fibrinolytic therapy or who have failed such treatment.17 Mechanical techniques require skilled operators but provide useful alternatives to systemic fibrinolytic therapy for patients who have severe PE and are at high risk for bleeding.
The role of reperfusion therapy for DVT is less certain.18 Typically, such treatment is reserved for patients with extensive DVT involving the iliac and femoral veins. Systemic fibrinolytic therapy is rarely effective in this setting, so catheter-directed fibrinolysis or pharmacomechanical therapy is preferred. Pharmacomechanical therapy, which involves the use of clot maceration or extraction devices in conjunction with fibrinolytic therapy, not only produces more rapid lysis than that achieved with catheter-directed fibrinolytic therapy but is also associated with less bleeding because lower doses of fibrinolytic drugs are employed.
Although there is mounting evidence that reperfusion therapy results in higher rates of patency than are achieved with anticoagulant therapy alone, which lowers the risk of postthrombotic syndrome, definitive evidence of long-term benefit is lacking. Consequently, reperfusion therapy should only be considered for patients who are at low risk of bleeding and for those whose life expectancy is such that delayed benefits may be realized. For patients with extensive iliofemoral DVT or inferior vena cava thrombosis that is threatening the limb, reperfusion therapy may be the best option. In patients with less extensive DVT involving the iliac-femoral or femoral-popliteal veins, an ongoing clinical trial is assessing whether reperfusion therapy results in more rapid improvement in symptoms and reduces the risk of postthrombotic syndrome compared with anticoagulation therapy alone (www.clinicaltrials.gov: NCT00790335).
Anticoagulation Therapy
Anticoagulation therapy is the cornerstone of VTE treatment and should be initiated immediately with parenteral anticoagulants such as heparin, low-molecular-weight heparin (LMWH), or fondaparinux, even while patients with suspected VTE are awaiting results of confirmatory tests.19 Heparin is generally preferred in patients with severe PE or extensive DVT because neither LMWH nor fondaparinux has been well evaluated in this setting. Heparin also should be used in patients with severe renal impairment (Cr clearance <30 mL/min) because LMWH and fondaparinux are cleared by the kidneys. If LMWH or fondaparinux is used for extended periods in patients with moderate renal impairment (Cr clearance of 30 to 50 mL/min), anti–factor Xa levels should be measured at trough to ensure there is no accumulation.
Heparin should be administered by continuous intravenous (IV) infusion and dosed using weight-based nomograms. Typically, an 80 unit/kg bolus is followed by an infusion at the rate of 18 units/kg/h, and subsequent doses are adjusted based on results of the APTT.20 Rapid achievement and maintenance of a therapeutic APTT are important to reduce the risk of recurrent VTE. In addition to APTT monitoring, platelet count should be measured frequently because of the risk of heparin-induced thrombocytopenia (HIT).
Low-molecular-weight heparin or fondaparinux can be used for the majority of patients with DVT, using the regimens illustrated in Table 52-2.19 Unlike heparin, these agents do not require coagulation monitoring. In addition, the risk of HIT is lower with LMWH than with heparin, and the risk is minimal with fondaparinux. Out-of-hospital management is safe for low-risk PE patients and for most patients with DVT. In PE patients at intermediate risk, outpatient management can be considered, but brief admission to hospital may be a safer approach.
Table 52-2 Low-Molecular-Weight Heparin and Fondaparinux Regimens for Treatment of Venous Thromboembolism
| Agent | Dose | Interval |
|---|---|---|
| Enoxaparin | 1 mg/kg | Twice daily |
| 1.5 mg/kg | Once daily | |
| Dalteparin | 100 units/kg | Twice daily |
| 200 units/kg | Once daily | |
| Tinzaparin | 175 units/kg | Once daily |
| Fondaparinux | 5 mg (weight <50 kg) | Once daily |
| 7.5 mg (weight 50-100 kg) | Once daily | |
| 10 mg (weight >100 kg) | Once daily |
After initial treatment with a parenteral anticoagulant, most patients with VTE receive extended therapy with a vitamin K antagonist (e.g., warfarin) to prevent recurrent DVT and PE. In most patients with DVT, warfarin can be started on the same day parenteral anticoagulant therapy is initiated. Parenteral anticoagulant therapy should be continued for at least 5 days and should only be stopped when the INR has been within the therapeutic range of 2 to 3, which is needed for long-term therapy, for 2 consecutive days. Initiation of warfarin therapy should be delayed in patients with extensive DVT involving the iliac-femoral veins; such patients should receive treatment with a parenteral anticoagulant until they have stabilized.
There are several emerging options to replace warfarin. These include dabigatran etexilate, an oral thrombin inhibitor,21 and rivaroxaban, apixaban, and edoxaban, which are oral factor Xa inhibitors. With no food interactions and few drug-drug interactions, these new oral anticoagulants produce such a predictable level of anticoagulation that they can be given in fixed doses without routine coagulation monitoring.22 In patients with VTE, rates of recurrent VTE and bleeding were similar with dabigatran (150 mg twice daily) and dose-adjusted warfarin. Dabigatran etexilate has been licensed as an alternative to warfarin for stroke prevention in patients with atrial fibrillation,23 but the drug has not yet been approved for VTE treatment.
Rivaroxaban has been compared with conventional anticoagulation therapy (LMWH followed by warfarin) in patients with DVT24; a study in PE patients has been completed, but results have not yet been reported. In DVT patients, rates of recurrent VTE and bleeding with rivaroxaban (15 mg twice daily for 3 weeks, followed by 20 mg once daily thereafter) were similar to those with conventional anticoagulation therapy. Ongoing trials are investigating apixaban or edoxaban as other alternatives to warfarin.
Patients who develop VTE as a complication of a reversible risk factor such as surgery, trauma, or medical illness have a low risk of recurrence when anticoagulant therapy is stopped.19 Consequently, a 3-month course of warfarin therapy represents adequate treatment in such patients, provided their risk factors have resolved. Women who develop VTE with estrogen therapy also can be treated for 3 months, provided hormonal treatment is withdrawn.
In contrast, patients with unprovoked VTE have a higher rate of recurrence when anticoagulant therapy stops, and often receive longer-duration treatment. Some experts recommend indefinite anticoagulant therapy, provided risk of bleeding remains low.19 At 1 month after stopping anticoagulant therapy, an elevated D-dimer level or residual venous compression ultrasound abnormalities identify patients at higher risk for recurrence who may benefit from indefinite anticoagulation therapy.25,26 After a minimum 3-month course of usual-intensity warfarin (target INR between 2 and 3), a lower-intensity regimen (target INR between 1.5 and 2.0) may simplify management by decreasing frequency of INR monitoring and reducing risk of bleeding, but the risk of recurrent VTE is slightly higher with this lower-intensity warfarin regimen.27
Caval Filters
Inferior vena cava filters, which are inserted percutaneously, are usually placed below the level of the renal veins, but can be placed higher for thrombus in the inferior vena cava. Both permanent and retrievable filters reduce the risk of recurrent PE but have not been shown to prolong survival, possibly because permanent filters can be associated with long-term complications that include inferior vena cava occlusion due to thrombus, recurrent DVT, and postthrombotic syndrome.28 Retrievable filters, designed to be removed within 2 to 4 weeks of implantation, can circumvent these long-term complications, but device migration or thrombosis occur in up to 10% of patients with temporary filters because the majority are not removed. Owing to these potential problems, caval filters should be restricted to patients who have high risk for recurrent PE and an absolute contraindication for anticoagulation, such as patients who develop a PE in the lead-up to or shortly after major surgery, those who experience major bleeding with anticoagulant therapy, or pregnant women who have a PE shortly before delivery. Retrievable filters should be used in these cases, and the devices should be removed as soon as anticoagulant therapy can safely be administered. Permanent filters are suitable for patients who have ongoing contraindications to anticoagulation. If a permanent filter is implanted, lifelong anticoagulation therapy should be considered once the contraindications have resolved, so as to reduce the risk of clotting of the filter.29
Specific Patient Subgroups
Patients with VTE in the setting of active cancer, women who suffer VTE during pregnancy, and patients with chronic thromboembolic pulmonary hypertension require special treatment. In addition, management of upper-extremity DVT and superficial thrombophlebitis also are worthy of comment.
Cancer
Active cancer and its treatment with chemotherapy, radiation therapy, and growth factors or other biological agents increase the risk of VTE.30 Patients with advanced cancer often have limited mobility, which adds to their risk of VTE. In addition, indwelling central venous access catheters can trigger upper-extremity DVT, which can lead to PE. Therefore, the index of suspicion should be high in cancer patients who present with symptoms and signs suggestive of PE and/or DVT.31 With advances in diagnostic imaging, incidental PE may be discovered on CT scans performed for staging purposes or for monitoring response to treatment. Although 20% of patients with VTE have an underlying malignancy, there is no evidence of a benefit of routine cancer screening in patients with VTE.32
As in patients without cancer, initial treatment of VTE in cancer patients involves administration of a rapidly acting parenteral anticoagulant. For extended treatment, however, LMWH reduces the risk of recurrent VTE to a greater extent than warfarin.33 In addition, in the face of poor nutritional intake, severe nausea and vomiting, transient thrombocytopenia, or invasive procedures, LMWH is easier to manage than warfarin.
Cancer patients who develop VTE after curative surgery or with adjuvant chemotherapy for limited-stage disease should be treated for at least 3 months or until they have completed their chemotherapy. Those with VTE against a background of advanced cancer have a risk of recurrence of at least 20% in the first year after stopping anticoagulant therapy, so they require indefinite treatment.21
Venous thromboembolism in pregnancy
Treatment of VTE in pregnancy centers mainly on heparin or LMWH because, unlike warfarin, these agents do not cross the placenta.34 Although both agents can be given subcutaneously, weight-adjusted LMWH has advantages over heparin because it can be given once daily without routine monitoring, and because the risks of HIT and osteoporosis are lower with LMWH than with heparin.35 Anti–factor Xa monitoring of LMWH should be considered in women at extremes of body weight or in those with renal impairment. Fondaparinux should be considered for pregnant women who have a history of HIT or develop injection-site reactions to heparin or LMWH.
Heparin or LMWH should be continued throughout pregnancy. Warfarin must be avoided because it crosses the placenta and can cause bone and central nervous system (CNS) abnormalities, fetal hemorrhage, or placental abruption.36 During labor and delivery, epidural analgesia should be avoided unless prophylactic-dose LMWH has been stopped at least 12 hours and therapeutic dose LMWH has been stopped at least 24 hours before insertion of the epidural catheter; treatment can be resumed within 6 hours of catheter withdrawal.37 After delivery, anticoagulation therapy should be continued for at least 3 months; warfarin can be used because it does not appear in breast milk.
Fibrinolytic agents have been used successfully for treatment of severe PE in pregnancy but can cause bleeding, usually from the genital tract. If PE develops late in pregnancy, a retrievable filter may prevent recurrence during delivery when anticoagulant therapy must be withheld.
Upper-extremity deep vein thrombosis
Usually involving the axillary and/or subclavian veins, upper-extremity DVT can be unprovoked, related to effort, or can be secondary to indwelling central venous catheters.38 Unprovoked upper-extremity DVT is unusual. More common is effort-related upper-extremity DVT, known as Paget-Schroetter’s syndrome, which usually affects the dominant arm of young, otherwise healthy individuals and occurs after strenuous exercise such as rowing or weight lifting. It is likely the unusual exertion causes injury to the vein wall, and with repeated trauma, this is sufficient to induce thrombosis, particularly if there is associated mechanical obstruction to blood flow. Such obstruction can result from compression of the subclavian vein as it exits the thoracic inlet, which can be caused by muscle hypertrophy or anomalies of the cervical ribs or spine. These abnormalities can often be detected on plain radiographs of the chest and cervical spine. However, most cases of upper-extremity DVT develop in patients with central venous catheters, particularly in patients with cancer.
Patients with upper-extremity DVT usually present with pain and swelling in the arm and may complain of associated shoulder or neck discomfort. If the DVT extends to involve the superior vena cava, there may be edema of the neck and face. Patients with thoracic outlet syndrome may have pain radiating to the fourth and fifth digits as a result of concomitant injury to the brachial plexus, and symptoms may be exacerbated by hyperabduction of the shoulder or lifting heavy objects.
The diagnosis of upper-extremity DVT is usually established by compression ultrasonography.39 Contrast venography or magnetic resonance (MR) venography can be helpful if the ultrasound is inconclusive. D-dimer testing may be less useful for upper-extremity DVT diagnosis than it is for the diagnosis of lower-extremity DVT because of the smaller thrombus volume in the upper limbs. Therefore, a negative D-dimer test is insufficient to exclude the possibility of upper-extremity DVT.
Anticoagulation is the cornerstone of treatment for upper-extremity DVT.19 Treatment usually starts with LMWH, and patients can then be transitioned to warfarin. Treatment should be given for at least 3 months. Patients with catheter-related upper-extremity DVT in the setting of cancer are best treated with extended LMWH, which should be continued as long as the catheter remains in place. Because of the importance of venous access in such patients, central venous catheters do not have to be removed, provided they are functional. Catheter-directed or pharmacomechanical fibrinolytic therapy can be considered for young, healthy patients with extensive upper-extremity DVT to reduce the risk of postthrombotic syndrome. This is an important consideration because recent evidence suggests that postthrombotic syndrome is a frequent and often disabling complication of upper-extremity DVT, particularly DVT involving the dominant arm.40 Surgical decompression of thoracic outlet obstruction can be considered if symptoms fail to resolve with more conservative treatment.41
Superficial thrombophlebitis
Thrombosis in superficial veins can occur spontaneously or as a complication of IV catheter insertion.42 Spontaneous thrombophlebitis is sterile; thrombophlebitis complicating catheter placement may be sterile or septic. Sterile thrombophlebitis is characterized by a tender cord that follows the course of superficial veins, usually on an extremity. The overlying skin may be erythematous and warm to touch. These features are magnified with septic thrombophlebitis, and a purulent discharge from a previous IV catheter puncture site is a common finding.
Superficial thrombophlebitis can extend into the deep venous system via perforating veins and can lead to PE.43 Therefore, ultrasonography should be performed to exclude DVT in patients whose superficial thrombophlebitis is associated with limb swelling, or in those with involvement of the proximal segment of the greater saphenous vein.
Septic thrombophlebitis often requires antibiotic treatment. Localized sterile thrombophlebitis can be treated with antiinflammatory agents such as ibuprofen or naproxen. Patients with severe symptoms or with more extensive disease obtain faster relief with anticoagulation therapy with either LMWH or fondaparinux.44,45 Therapeutic doses of these drugs can be given subcutaneously for 4 to 6 weeks or until symptoms have resolved.
Most patients with superficial thrombophlebitis have an excellent prognosis. Patients with superficial thrombophlebitis complicating varicose veins often benefit from graduated compression stockings. Recurrent or migratory superficial thrombophlebitis can occur in patients with vasculitis, such as polyarteritis nodosa or Buerger’s disease, or in patients with cancer, particularly pancreatic cancer.
Venous Thromboembolism Prevention
At least half of outpatients with newly diagnosed VTE have a history of recent hospitalization, and most failed to receive thromboprophylaxis during their hospital stay. As a result, PE is the most common preventable cause of death in hospitalized patients in the United States. Guidelines for primary prophylaxis are available and should be followed.46
Prognosis
With the diagnosis established and adequate anticoagulant therapy initiated, most patients with VTE survive.47,48 Case fatality rates 1 month after diagnosis of DVT or PE are 6% and 12%, respectively. Patients with severe PE who present with shock have the highest mortality, and many die within an hour of presentation. Although the case fatality rate in patients with PE is twice that in those with DVT, many deaths are the result of comorbid conditions rather than the PE itself, and are therefore unlikely to be prevented by anticoagulant therapy. Factors associated with early mortality after VTE include presentation as PE, advanced age, cancer, and underlying cardiovascular disease. The most serious long-term complication of PE is chronic thromboembolic pulmonary hypertension, a rare condition associated with significant morbidity and mortality (discussed earlier).
Postthrombotic syndrome is the major complication of lower-extremity DVT49 (also see Chapter 55). Characterized by dependent leg swelling and discomfort, skin induration, itchiness and telangiectasias, the incidence of postthrombotic syndrome ranges from 20% to 40%. The incidence of severe postthrombotic syndrome, which can lead to venous ulcers, is about 3% at 1 year and 9% after 5 years, even with the use of graduated compression stockings.
Postthrombotic syndrome is triggered by damage to the venous valves. Venous occlusion due to residual thrombus and reflux of blood through incompetent valves leads to increased venous pressure, reduced calf muscle perfusion, increased vascular permeability, and subsequent dependent edema and discomfort. Catheter-directed or pharmacomechanical fibrinolytic therapy may improve venous patency in patients with extensive DVT and prevent valve damage, thereby reducing the risk of postthrombotic syndrome.
Inadequate anticoagulation therapy and recurrent DVT are risk factors for postthrombotic syndrome.50 Therefore, adequate intensity and duration of anticoagulation therapy is a goal of DVT treatment. Patients with extensive proximal DVT are more likely to develop postthrombotic syndrome than those with distal DVT. Use of graduated compression stockings by DVT patients appears to reduce the risk of postthrombotic syndrome.
Despite anticoagulant therapy, about 6% of patients suffer recurrent VTE during the first 6 months. While on anticoagulation treatment, patients with unprovoked VTE and those with secondary VTE have similar risks of recurrence. In contrast, when anticoagulant therapy is stopped, patients with unprovoked VTE have a risk of recurrence of 10% at 1 year and 30% at 5 years, whereas those with secondary VTE have recurrence rates of 3% at 1 year and 10% at 5 years. Recurrent events often mirror the index events; after an initial PE, about 60% of recurrences are PE, whereas after an initial DVT, about 60% of the recurrences are DVT. Because of the high risk of recurrence in patients with unprovoked VTE, many experts recommend indefinite anticoagulant therapy for such patients.19 In contrast, because of the lower risk of recurrence, anticoagulation therapy can be stopped after 3 months in patients with secondary VTE whose risk factors have resolved.
1 Torbicki A., Perrier A., Konstantinides S., et al. Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur Heart J. 2008;29(18):2276–2315.
2 Silverstein M.D., Heit J.A., Mohr D.N., et al. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 1998;158(6):585–593.
3 White R.H., Zhou H., Romano R.S. Incidence of idiopathic deep venous thrombosis and secondary thromboembolism among ethnic groups in California. Ann Intern Med. 1998;128(9):737–740.
4 Kearon C. Natural history of venous thromboembolism. Circulation. 2003;107(23 Suppl 1):122–130.
5 Lijfering W.M., Rosendaal F.R., Cannegieter S.C. Risk factors for venous thrombosis – current understanding from an epidemiological point of view. Br J Haematol. 2010;149(6):824–833.
6 Bernardi E., Pesavento R., Prandoni P. Upper extremity deep venous thrombosis. Semin Thromb Hemost. 2006;32(7):729–736.
7 Agnelli G., Becattini C. Acute pulmonary embolism. N Engl J Med. 2010;363(3):266–274.
8 van Belle A., Buller H.R., Huisman M.V., et al. Effectiveness of managing suspected pulmonary embolism under an algorithm combining clinical probability, D-dimer testing and computed tomography. JAMA. 2006;295(2):172–179.
9 Stein P.D., Hull R.D., Patel K.C., et al. D-dimer for the exclusion of acute venous thrombosis and pulmonary embolism: a systematic review. Ann Intern Med. 2004;140(8):589–602.
10 Lensing A.W.A., Prandoni P., Brandjes D.P.M., et al. Detection of deep-vein thrombosis by real-time B-mode ultrasonography. N Engl J Med. 1989;320(6):342–345.
11 Lensing A.W.A., Buller H.R., Prandoni P., et al. Contrast venography, the gold standard for the diagnosis of deep-vein thrombosis: improvement in observer agreement. Thromb Haemost. 1992;67(1):8–12.
12 Goodacre S., Sutton A.J., Sampson F.C. Meta-analysis: the value of clinical assessment in the diagnosis of deep venous thrombosis. Ann Intern Med. 2005;143(2):129–139.
13 Wells P.S., Anderson D.R., Bormanis J., et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet. 1997;350(9094):1795–1798.
14 Elias A.D., Colombier D., Victor G., et al. Diagnostic performance of complete lower limb venous ultrasound in patients with clinically suspected acute pulmonary embolism. Thromb Haemost. 2004;91(1):187–195.
15 Middeldorp S. van Hylckama Vlieg A: Does thrombophilia testing help in the clinical management of patients? Br J Haematol. 2008;143(3):321–335.
16 Brady A.J., Crake T., Oakley C.M. Percutaneous catheter fragmentation and distal dispersion of proximal pulmonary embolus. Lancet. 1991;338(8776):1186–1189.
17 Leacche M., Unic D., Goldhaber S.Z., et al. Modern surgical treatment of massive pulmonary embolism: results in 47 consecutive patients after rapid diagnosis and aggressive surgical approach. J Thorac Cardiovasc Surg. 2005;129(5):1018–1023.
18 Watson L.I., Armon M.P. Thrombolysis for acute deep vein thrombosis. Cochrane Database Syst Rev. 4, 2004. CD002783
19 Kearon C., Kahn S.R., Agnelli G., et al. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest. 2008;133(6 Suppl):454S–545S.
20 Raschke R.A., Gollihare B., Peirce J.C. The effectiveness of implementing the weight-based heparin nomogram as a practice guideline. Arch Intern Med. 1996;156(15):1645–1649.
21 Schulman S., Kearon C., Kakkar A.K., et al. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361(24):2342–2352.
22 Eikelboom J.W., Weitz J.I. New anticoagulants. Circulation. 2010;121(13):1523–1532.
23 Connolly S.J., Ezekowitz M.D., Yusuf S., et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–1151.
24 Einstein Investigators, Bauersachs R., Berkowitz S.D., et al. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363(26):2499–2510.
25 Bruinstroop E., Klok F.A., Van De Ree M.A., et al. Elevated D-dimer levels predict recurrence in patients with idiopathic venous thromboembolism: a meta-analysis. J Thromb Haemost. 2009;7(4):611–618.
26 Prandoni P., Lensing A.W.A., Prins M.H., et al. Residual venous thrombosis as a predictive factor of recurrent venous thromboembolism. Ann Intern Med. 2002;137(12):955–960.
27 Ridker P.M., Goldhaber S.Z., Danielson E., et al. Long-term, low-intensity warfarin therapy for the prevention of recurrent venous thromboembolism. N Engl J Med. 2003;348(15):1425–1434.
28 PREPIC Study Group. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d’Embolie Pulmonaire par Interruption Cave) randomized study. Circulation. 2005;112(3):416–422.
29 Decousus H., Leizorovicz A., Parent F., et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. N Engl J Med. 1998;338(7):409–415.
30 Heit J.A., Silverstein M.D., Mohr D.N., et al. Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med. 2000;160(6):809–815.
31 Blom J.W., Doggen C.J., Osanto S., et al. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA. 2005;293(6):715–722.
32 Monreal M., Lensing A.W.A., Prins M.H., et al. Screening for occult cancer in patients with acute deep vein thrombosis or pulmonary embolism. J Thromb Haemost. 2004;2(6):876–881.
33 Lee A.Y.Y., Levine M.N., Baker R.I., et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med. 2003;349(2):146–153.
34 Bates S.M., Greer I.A., Pabinger I., et al. Venous thromboembolism, thrombophilia, antithrombotic therapy, and pregnancy: American College of Chest Physicians: evidence-based clinical practice guidelines (8th edition). Chest. 2008;133(6 Suppl):844S–886S.
35 Bourjeily G., Paidas M.J., Khalil H., et al. Pulmonary embolism in pregnancy. Lancet. 2010;375(9713):500–512.
36 Shaul W.L., Hall J.G. Multiple congenital anomalies associated with oral anticoagulants. Am J Obstet Gynecol. 1977;127(2):191–198.
37 Horlocker T.T., Wedel D.J., Benzon H., et al. Regional anesthesia in the anticoagulated patient: defining the risks (the second ASRA Consensus Conference on Neuraxial Anesthesia and Anticoagulation). Reg Anesth Pain Med. 2003;28(3):172–197.
38 Joffe H.V., Kucher N., Tapson V.F., et al. Upper-extremity deep vein thrombosis: a prospective registry of 592 patients. Circulation. 2004;110(12):1605–1611.
39 Prandoni P., Polistena P., Bernardi E., et al. Upper-extremity deep vein thrombosis. Risk factors, diagnosis and complications. Arch Intern Med. 1997;157(1):57–62.
40 Elman E.E., Kahn S.R. The post-thrombotic syndrome after upper extremity deep venous thrombosis in adults: a systematic review. Thromb Res. 2006;117(6):609–614.
41 Becker D.M., Philbrick J.T., Walker F.B.IV. Axillary and subclavian venous thrombosis. Prognosis and treatment. Arch Intern Med. 1991;151(10):1934–1943.
42 Leon L., Giannoukas A.D., Dodd D., et al. Clinical significance of superficial vein thrombosis. Eur J Vasc Endovasc Surg. 2005;29(1):10–17.
43 Decousus H., Quere I., Presles E., et al. Superficial venous thrombosis and venous thromboembolism in a large, prospective epidemiologic study. Ann Intern Med. 2010;152(4):218–224.
44 Di Nisio M., Wichers I.M., Middeldorp S. Treatment for superficial thrombophlebitis of the leg. Cochrane Database Syst Rev. 2, 2007. CD004982
45 Decousus H., Prandoni P., Mismetti P., et al. Fondaparinux for the treatment of superficial-vein thrombosis of the legs. N Engl J Med. 2010;363(13):1222–1232.
46 Geerts W.H., Bergqvist D., Pineo G.F., et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest. 2008;133(6 Suppl):381S–453S.
47 Kasper W., Konstantinides S., Geibel A., et al. Management strategies and determinants of outcome in acute major pulmonary embolism: results of a multicenter registry. J Am Coll Cardiol. 1997;30(5):1165–1171.
48 Goldhaber S.Z., Visani L., De Rosa M. Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet. 1999;353(9162):1386–1389.
49 Prandoni P., Lensing A.W.A., Cogo A., et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996;125(1):1–7.
50 van Dongen C.J., Prandoni P., Frulla M., et al. Relation between quality of anticoagulant treatment and the development of the postthrombotic syndrome. J Thromb Haemost. 2005;3(5):939–942.