11 CARDIAC DISEASE
The CXR has several important roles: alerting the physician that the heart is enlarged, sometimes revealing a complication resulting from cardiac disease, occasionally suggesting a specific cardiac diagnosis…frequently providing reassurance that all is well.
ACQUIRED CARDIAC DISEASE—WHAT TO LOOK FOR
HEART SIZE
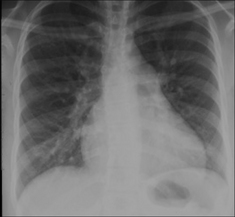
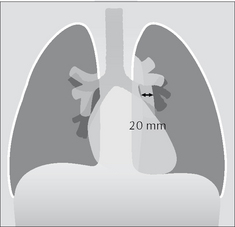
Rules of thumb: Most normal adult hearts have a cardiothoracic ratio (CTR, Fig. 11.1) that does not exceed 50% when assessed on a PA CXR obtained in full inspiration1. Some people (perhaps as few as 5%) have an entirely normal heart and yet the CTR exceeds 50%.
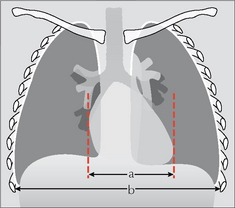
Figure 11.1 Measuring the CTR. On a PA chest radiograph obtained in full inspiration, if a/b > 50% the heart is likely to be enlarged1. (a = maximum transverse diameter of the heart; b = maximum internal diameter of the thorax.)
In young children the normal CTR can be slightly larger than 50%2.
 The transverse cardiac diameter of a normal heart may vary from one PA CXR to another. In 200 normal adults having three CXRs at monthly/yearly intervals3:
The transverse cardiac diameter of a normal heart may vary from one PA CXR to another. In 200 normal adults having three CXRs at monthly/yearly intervals3:
 On a PA radiograph variation in the transverse cardiac diameter or the CTR may be caused by:
On a PA radiograph variation in the transverse cardiac diameter or the CTR may be caused by:
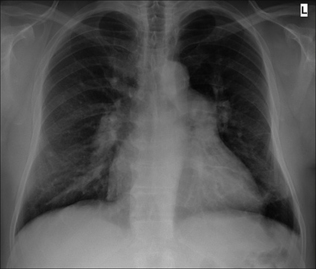
 A heart may have a CTR of less than 50% but it can still be enlarged—if its transverse diameter was very narrow to begin with. It may take some time before an enlarged heart reaches and exceeds a CTR of 50% (Fig. 11.2).
A heart may have a CTR of less than 50% but it can still be enlarged—if its transverse diameter was very narrow to begin with. It may take some time before an enlarged heart reaches and exceeds a CTR of 50% (Fig. 11.2).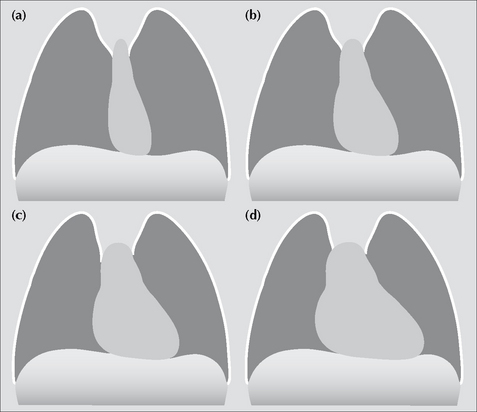
Figure 11.2 A heart may be enlarged and yet the CTR can be less than 50%. Take this example. (a) The CTR is well within normal limits. The heart is very narrow. (b) Six months later, the heart has enlarged but the CTR remains at less than 50%. (c) After a further six months the heart has further increased in size but still remains less than 50%.(d) Eventually, additional enlargement occurs and the CTR exceeds 50%.
Rule of thumb: On interval PA CXRs, an increase in transverse cardiac diameter of more than 2.0 cm is significant.
CHAMBERS AND BORDERS
The margins of the cardiac silhouette are formed by the chambers of the heart. We need to be aware which chamber accounts for which particular border on both the frontal and the lateral CXR (Figs 11.3-11.6).
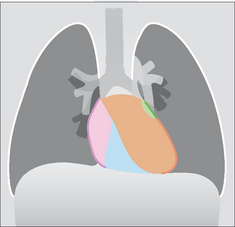
Figure 11.4 The border-forming chambers:pink = right atrium; blue = right ventricle; brown = left ventricle.
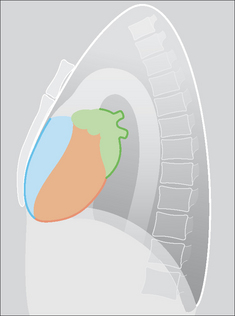
Figure 11.6 The border-forming chambers:green = left atrium; blue = right ventricle; brown = left ventricle.
Potential pitfalls:
Two incidental appearances on a frontal CXR are not pathological:
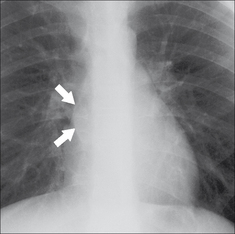
Figure 11.7 Normal pulmonary venous confluence (arrows)1,2. Sometimes the structure is very prominent; in others it can be slight and subtle. On a PA CXR it can be identified in 10% of patients aged 50 or over (see Chapter 16, p. 239).
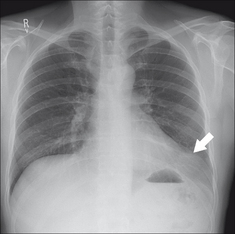
Figure 11.8 Fat collections can occur at either or both cardiophrenic angles. It is very common in well-fed people aged 50 or older (see Chapter 16, p. 239). In this 53-year-old male (who presented with lower abdominal pain) a large fat collection (arrow) causes a prominent shadow at the left cardiophrenic angle.
CHAMBER ENLARGEMENT ON THE FRONTAL CXR2,5,6
The CXR can be very useful in suggesting whether or not a heart is enlarged. Echocardiography will determine whether enlargement is due to a pericardial effusion or to chamber enlargement.
The CXR appearance does not have the definitive role in the precise assessment of chamber enlargement. Echocardiography is definitive. All the same, it is worth being familiar with some of the features of specific chamber enlargement as deduced by analysing the CXR (Table 11.1 and Figs 11.9-11.12).
Table 11.1 Chamber enlargement on the frontal CXR — some basic guidelines.
| Enlarged | Features |
|---|---|
| Left ventricle | |
| Right ventricle | |
| Left atrium |
 A bulge of the left heart border just inferior to the main pulmonary trunk. This bulge is the left atrial appendage. A bulge of the left heart border just inferior to the main pulmonary trunk. This bulge is the left atrial appendage. |
| Right atrium |

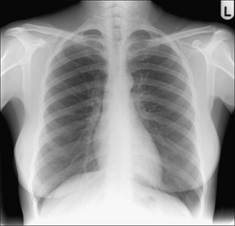
Figure 11.9 Enlarged left ventricle and left atrium. Note the prominence (bulge) of the left atrial appendage just below and to the left of the main pulmonary trunk. Mitral stenosis and mitral incompetence.
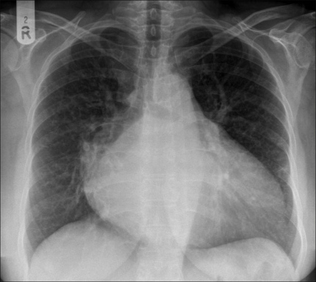
Figure 11.10 Enlarged left ventricle and left atrium. In this patient the enlarged left atrium is evident because it is producing a distinctive double shadow seen through the heart and it is also pushing the right and left main bronchi apart. Mitral stenosis and mitral incompetence.
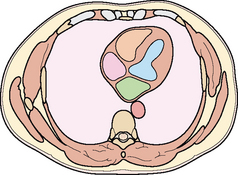
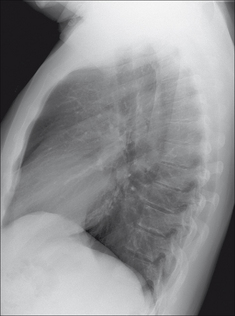
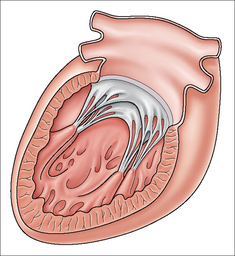
Figure 11.11 Left atrium of normal size. Cross-sectional image. The atrium is not extending outside the normal cardiac shadow—i.e. its left and right margins are not prominent. Green = left atrium;brown = left ventricle; pink = right atrium; blue = right ventricle.
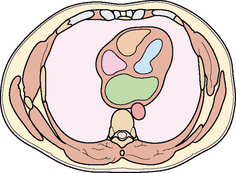
Figure 11.12 An enlarged left atrium (green). Cross-sectional image. The posterior and side-to-side enlargement of this chamber causes it to emerge from the mediastinal silhouette and its borders become outlined by the air in the lungs. This air-around-the-atrium explains why a double shadow is seen on a frontal CXR.
LEFT VENTRICULAR ANEURYSM
Aneurysmal dilatation results from myocardial infarction. On a frontal CXR the appearance is often highly characteristic (Figs 11.13 and 11.14).
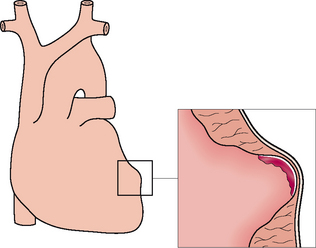
PERICARDIAL EFFUSION
The CXR appearance of fluid in the pericardial sac is very difficult to distinguish from simple chamber enlargement (Fig. 11.15). The distinction is rapidly and easily made using echocardiogaphy. The following2 are worth noting:
 The claim that a pericardial effusion will produce a globular cardiac outline or a well-defined cardiac contour because of the tamponading effect of the effusion on cardiac motion is unsound2.
The claim that a pericardial effusion will produce a globular cardiac outline or a well-defined cardiac contour because of the tamponading effect of the effusion on cardiac motion is unsound2. Rule of thumb: The single most important sign of an effusion on a CXR is a rapid alteration in heart size or shape without any changes in the lungs2.
Rule of thumb: The single most important sign of an effusion on a CXR is a rapid alteration in heart size or shape without any changes in the lungs2.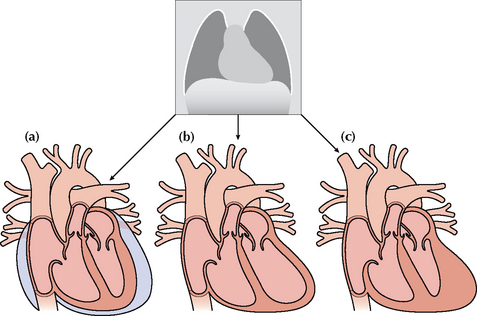
Figure 11.15 An enlarged cardiac silhouette may be due to chamber enlargement, to a pericardial effusion, to inflammation/hypertrophy of the cardiac musculature…or to a combination of these possibilities. The CXR appearance of the cardiac shadow alone is insensitive in making a distinction between these causes of an enlarged heart. This is illustrated: (a) pericardial effusion; (b) ventricular dilatation (i.e. chamber enlargement with thin walls); (c) hypertrophy of the myocardium.
VALVE CALCIFICATION7,8
Clinically important
 Mitral leaflets. Usually consequent on rheumatic heart disease.
Mitral leaflets. Usually consequent on rheumatic heart disease.
 The normal valve consists of a fibrous annulus (or ring), valve leaflets (or cusps), chordae tendinae and papillary muscles (Fig. 11.18).
The normal valve consists of a fibrous annulus (or ring), valve leaflets (or cusps), chordae tendinae and papillary muscles (Fig. 11.18).Clinically unimportant
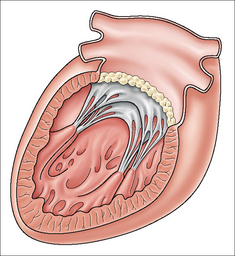
 Mitral ring. An age related phenomenon: calcification affects the ring around the mitral valve leaflets (Fig. 11.19). Clinically significant mitral stenosis resulting from this ageing process is very, very rare. This age related calcification is usually an incidental finding on a CXR. It has a very characteristic configuration—doughnut shaped (Fig. 11.20), circular, or a reverse C. This calcification is most commonly seen in elderly women.
Mitral ring. An age related phenomenon: calcification affects the ring around the mitral valve leaflets (Fig. 11.19). Clinically significant mitral stenosis resulting from this ageing process is very, very rare. This age related calcification is usually an incidental finding on a CXR. It has a very characteristic configuration—doughnut shaped (Fig. 11.20), circular, or a reverse C. This calcification is most commonly seen in elderly women.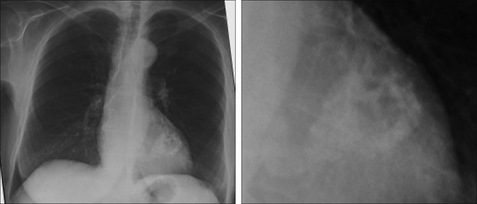
Figure 11.20 Elderly patient. Female. Prominent age related calcification of the mitral valve ring. The doughnut shape, or reverse C shape, of this calcification (i.e. it adopts the shape of the annulus) is highly characteristic. This is a common incidental CXR finding in elderly people. It is very rarely of clinical significance.
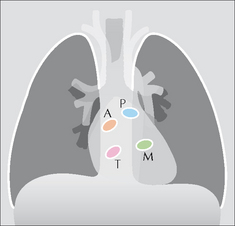
Figure 11.16 The position of the valves on the frontal CXR.P = pulmonary; A = aortic;M = mitral; T = tricuspid.
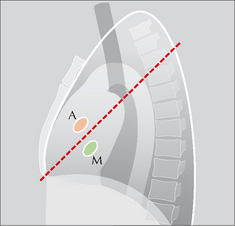
Figure 11.17 The position of the aortic (A) and mitral (M) valves on the lateral CXR. The dotted line extends from the carina to the anterior costophrenic angle. A useful rule of thumb: calcification situated mainly above this line will lie in the aortic valve; calcification situated mainly below this line will lie in the mitral valve2.
LEFT VENTRICULAR FAILURE (LVF)6,9,10,11
The following features may be present on a PA CXR.
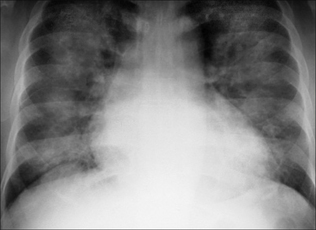
Almost all patients with pulmonary opacities due to LVF have cardiomegaly. An occasional exception: a patient with an acute myocardial infarction may have pulmonary oedema and a normal CTR.
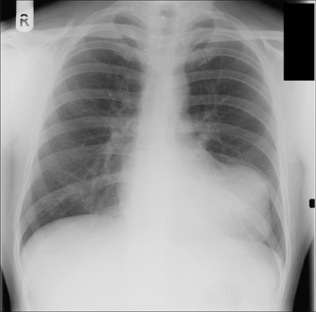
When the pulmonary venous pressure is normal the upper lobe vessels are smaller in diameter than the lower lobe vessels on an erect CXR. As the venous pressure begins to rise these diameters are reversed and the upper lobe vessels enlarge and the lower lobe vessels constrict (Fig. 11.21). NB: this radiological appearance of upper lobe blood diversion is usually very, very, subtle, and often overdiagnosed.
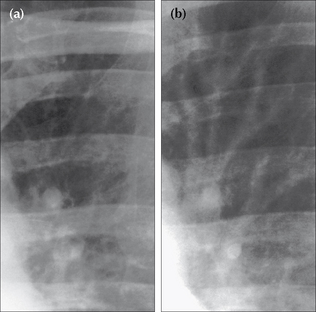
Figure 11.21 Early LVF. Change in size of the upper lobe vessels. The pulmonary venous pressure was normal in (a). Subsequently (b), prior to developing florid pulmonary oedema. The upper lobe vessels are dilated in (b) as compared with (a). This example is provided to illustrate that changes in vessel size do occur. Nevertheless, it is emphasised that evaluation of vessel size in early pulmonary venous hypertension can be very, very difficult.
Various changes may occur as the pulmonary venous pressure rises even further (Table 11.2). The precise changes will differ between individuals. When a pleural effusion results from LVF it is commonly bilateral. Occasionally it will be unilateral; when this occurs it is usually on the right side. The mechanism for this right-sided selectivity is controversial…but may be related to the anatomical arrangement of lymphatics draining the lungs.
Table 11.2 LVF — signs on an erect CXR.
| Early | |
| Later |
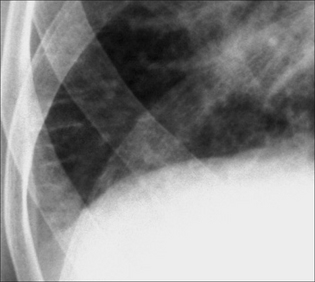
Figure 11.23 Early LVF. Septal lines (Kerley B lines) caused by fluid in the interstitium. These short, straight lines reach the pleural surface and have this characteristic appearance.
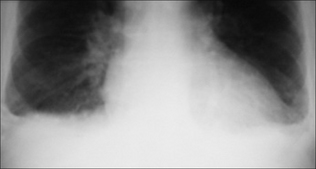
Figure 11.24 Early LVF. Small pleural effusions. Slight blunting of the costophrenic angles. Effusions in LVF are usually bilateral.

Figure 11.25 Florid LVF. Extensive interstitial oedema. The fluid lies mainly in the interstitium of the lung.
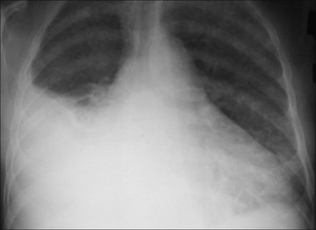
Figure 11.27 Florid LVF. The main finding is a large pleural effusion. When pleural effusions occur they are usually bilateral. Unilateral effusions do occur and are most often situated on the right side. This predilection for the right side might be related to the differences in lymphatic drainage between the right and left lungs.
CONGENITAL HEART DISEASE2,11
A detailed description of the numerous congenital cardiovascular conditions is beyond the scope of this book. In clinical practice most congenital cardiovascular abnormalities present in childhood (with heart failure or cyanosis) rather than in adults. Nevertheless, there is one condition where an adult’s CXR can show abnormal features that may suggest the likely diagnosis.
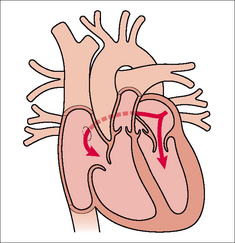
Atrial septal defect (ASD)2
The defect between the low pressure atria can remain clinically silent until adulthood. Eventually, the patient may present with non-specific dyspnoea, a cardiac arrhythmia, and/or paradoxical arterial embolism. Normally, the left atrium is at a slightly higher pressure than the right atrium and so blood is shunted through an ASD from the left to the right side. This results in an increased blood flow through the lungs. If the shunt is very small—the CXRmay appear entirely normal. The classical CXR features of a larger ASD are:
 A small aortic knuckle. This is a constant feature2. The shadow of the ascending aorta on the right side of the mediastinum is absent because the aortic root is displaced by the dilated right atrium and right ventricle—i.e. causing leftward rotation of the heart and the great vessels.
A small aortic knuckle. This is a constant feature2. The shadow of the ascending aorta on the right side of the mediastinum is absent because the aortic root is displaced by the dilated right atrium and right ventricle—i.e. causing leftward rotation of the heart and the great vessels.PULMONARY ARTERIAL HYPERTENSION
 Increased pressure in the pulmonary arteries causes the arteries to become enlarged (i.e. increased calibre), or hypertrophied…or both of these.
Increased pressure in the pulmonary arteries causes the arteries to become enlarged (i.e. increased calibre), or hypertrophied…or both of these. It is often difficult to distinguish between the various causes of pulmonary arterial hypertension (Table 11.3) from the CXR alone. Primary pulmonary hypertension is a diagnosis of exclusion. It is only accepted as the likely diagnosis after all the other causes for pulmonary arterial hypertension have been eliminated.
It is often difficult to distinguish between the various causes of pulmonary arterial hypertension (Table 11.3) from the CXR alone. Primary pulmonary hypertension is a diagnosis of exclusion. It is only accepted as the likely diagnosis after all the other causes for pulmonary arterial hypertension have been eliminated. A common dilemma: when viewing a CXR—are these pulmonary arteries enlarged? Rule of thumb: The diameter at the mid point of a normal descending pulmonary artery should not measure more than 9 mm in women and 10 mm in men.
A common dilemma: when viewing a CXR—are these pulmonary arteries enlarged? Rule of thumb: The diameter at the mid point of a normal descending pulmonary artery should not measure more than 9 mm in women and 10 mm in men.Table 11.3 Causes of pulmonary arterial hypertension2,12.
1. Felson B. Chest Roentgenology. Philadelphia, PA: WB Saunders, 1973.
2. Jefferson K, Rees S. Clinical Cardiac Radiology, 2nd ed. London: Butterworth, 1980.
3. Simon G. Principles of Chest X-ray Diagnosis. London: Butterworth, 1962.
4. Gammill SL, Krebs C, Meyers P, et al. Cardiac measurements in systole and diastole. Radiology. 1970;94:115-119.
5. Boxt LM, Reagan K, Katz J. Normal plain film examination of the heart and great arteries in the adult. J Thorac Imaging. 1994;9:208-218.
6. Chen JT. The plain radiograph in the diagnosis of cardiovascular disease. Radiol Clin North Am. 1983;21:609-621.
7. Carpentier AF, Pellerin M, Fuzellier JF, et al. Extensive calcification of the mitral valve anulus: pathology and surgical management. J Thorac Cardiovasc Surg. 1996;111:718-729.
8. Woodring JH, West JW. CT of aortic and mitral valve calcification. J Ky Med Assoc. 1989;87:177-180.
9. Gluecker T, Capasso P, Schnyder P, et al. Clinical and radiologic features of pulmonary edema. Radiographics. 1999;19:1507-1531.
10. Fraser RG, Muller NL, Colman NC, Pare PD. Fraser and Pare’s Diagnosis of Diseases of the Chest, 4th ed. Philadelphia, PA: WB Saunders, 1999.
11. Gross GW, Steiner RM. Radiographic manifestations of congenital heart disease in the adult patient. Radiol Clin North Am. 1991;29:293-317.
12. Gaine S. Pulmonary hypertension. JAMA. 2000;284:3160-3168.