26 CHRONIC COUGH: WHAT TO LOOK FOR
There are numerous causes for a chronic cough (Table 26.1). In adults the common causes can be identified4: cigarette smoking; medication with an angiotensin-converting enzyme (ACE) inhibitor; upper airway cough syndrome (UACS)…sometimes referred to as post-nasal drip syndrome (PNDS); asthma; gastro-oesophageal reflux disease (GORD); and non-asthmatic eosinophilic bronchitis (NAEB)4.
Table 26.1 Causes of a chronic cough.
| Pulmonary | |
| Extra-pulmonary | |
| Drugs | |
| Idiopathic2,7 |
* NAEB: Patients with a chronic cough, sputum eosinophilia, normal spirometry and normal peak expiratory flow variability. NAEB is responsive to inhaled corticosteroids2.
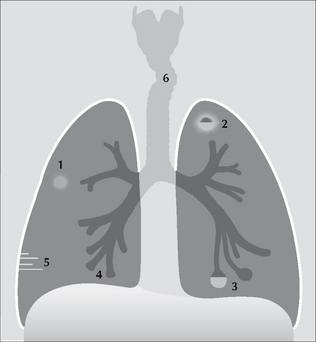
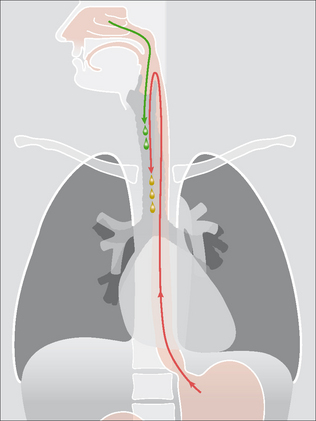
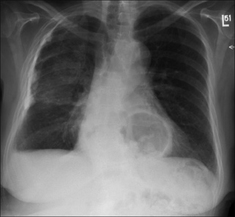
Figure 26.1 Some causes for a chronic cough.1 = Bronchial carcinoma;2 = Tuberculosis;3 = Bronchiectasis—cystic changes;4 = Bronchiectasis—tubular changes;5 = Septal lines in pulmonary oedema;6 = Tracheal compression by a goitre.
INVESTIGATING A CHRONIC COUGH
A patient presents with a chronic cough and:
“…an approach focused on detecting the presence of UACS, asthma, NAEB, or GORD, alone, or in combination, is likely to have a far higher yield than routinely searching for relatively uncommon or obscure diagnoses”4.
CHRONIC COUGH—CXR FINDINGS
The CXR can be very helpful—whether abnormal or entirely normal.
CXR ABNORMAL—THE LIKELY DIAGNOSIS IS REVEALED
The CXR is obviously abnormal. As a consequence the physician’s confidence as to the probable diagnosis will be high (Table 26.2).
Table 26.2 Abnormal CXR—likely diagnoses.
| Appearance | Default diagnosis |
|---|---|
| Consolidation | |
| Lobar collapse | |
| Ring shadows or tubular shadows | Bronchiectasis (Fig. 26.5) |
| Mass lesion | Tumour (Fig. 26.6) |
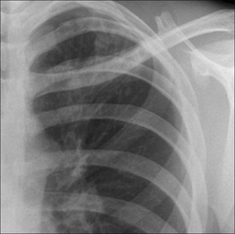
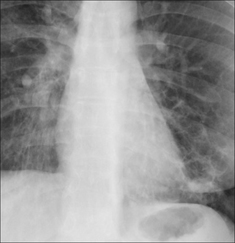
Figure 26.3 Chronic cough. Ill-defined shadowing at the left apex raises the probability of post-primary tuberculosis. Subsequently, tuberculosis confirmed.
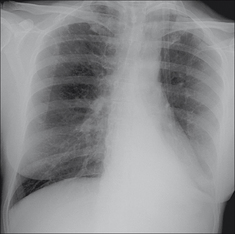
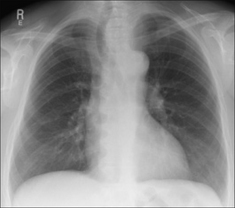
Figure 26.4 Chronic cough. Asthmatic patient. A mucus plug has caused collapse of the left lower lobe. The collapse occurred some weeks previously. Note the collapsed lobe behind the heart gives the classic sail sign appearance.
CXR ABNORMAL—A POSSIBLE DIAGNOSIS IS SUGGESTED
The CXR is abnormal but the abnormality is not in itself specific. Nevertheless, the CXR findings will suggest that a particular cause for the chronic cough now needs further consideration (Table 26.3).
Table 26.3 Abnormal CXR—possible diagnoses.
| Appearance | Possible diagnosis |
|---|---|
| Large heart and interstitial or alveolar shadowing | Pulmonary oedema (Fig. 26.7) |
| Tracheal deviation in the neck | Goitre (Fig. 26.8) |
| Hiatus hernia | GORD (Fig. 26.9) |
CXR NORMAL—REASSURANCE AND GUIDANCE
Reassurance: Middle-aged and elderly patients—both smokers and non-smokers—are concerned that the persistent cough signifies a cancer. Careful analysis of the CXR with particular attention to the hidden, tricky areas (Chapter 1, p. 13) enables the physician—with a high degree of confidence—to tell the patient that there is no evidence of a cancer.
Guidance: A normal CXR is an important negative finding. In an adult who is a non-smoker and is not being treated with an ACE inhibitor6,7, a normal CXR allows the physician to concentrate further investigations on the remaining four most common possibilities (listed once more in Table 26.4).
Table 26.4 Reiteration: four common causes for a chronic cough4.
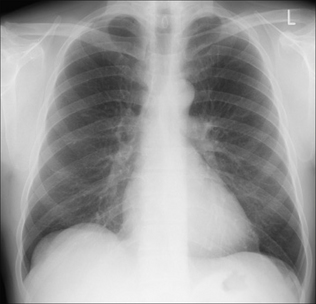
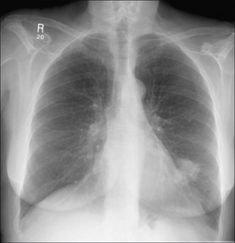
Figure 26.10 Chronic cough. Normal CXR. This is a most useful finding. In an adult, it allows the physician to concentrate on a limited number of causes for a chronic cough (Table 26.4).
An interesting condition—Bronchiectasis13-15
Aetiology/pathology
Bronchial obstruction causes severe inflammation which results in permanent damage to the bronchi and bronchioles.
Clinical features
Chronic cough. Usually with foul smelling sputum. Recurrent episodes of acute infection. Sometimes haemoptysis.
The CXR
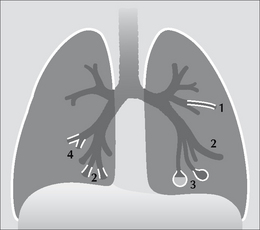
Figure 26.11 In most cases of bronchiectasis the CXR will be abnormal. The abnormality may be subtle or gross, and may include any of the following:1 & 4 = tramlines (thickened bronchial walls); 2 = tubular shadows (dilated & fluid filled bronchi); 3 = ring or cystic shadows (extreme bronchial dilatation). Slight or severe volume loss may also be present indicating fibrosis and shrinkage of the affected lung.
1. Morice AH. Epidemiology of cough. Pulm Pharmacol Ther. 2002;15:253-259.
2. Haque RA, Usmani OS, Barns PJ. Chronic idiopathic cough: a discrete clinical entity? Chest. 2005;127:1710-1713.
3. Pratter MR, Abouzgheib W. Make the cough go away. Chest. 2006;129:1121-1122.
4. Pratter MR. Overview of common causes of chronic cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129:59S-62S.
5. Schaefer OP, Irwin RS. Unsuspected bacterial suppurative disease of the airways presenting as chronic cough. Am J Med. 2003;114:602-606.
6. Israili ZH, Hall WD. Cough and angioneurotic edema associated with angiotensin-converting enzyme inhibitor therapy. A review of the literature and pathophysiology. Ann Intern Med. 1992;117:234-242.
7. Wood R. Bronchospasm and cough as adverse reactions to the ACE inhibitors captopril, enalapril and lisinopril. A controlled retrospective cohort study. Br J Clin Pharmacol. 1995;39:265-270.
8. Pratter MR. Unexplained (idiopathic) cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129:220S-221S.
9. Irwin RS. Chronic cough due to gastroesophageal reflux disease. ACCP evidence-based clinical practice guidelines. Chest. 2006;129:80S-94S.
10. Sifrim D, Dupont L, Blondeau K, et al. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut. 2005;54:449-454.
11. Chang AB, Lasserson TJ, Kiljander TO, et al. Systematic review and meta-analysis of randomised controlled trials of gastro-oesophageal reflux interventions for chronic cough associated with gastro-oesophageal reflux. BMJ. 2006;332:11-17.
12. Brightling CE, Ward R, Goh KL, et al. Eosinophilic bronchitis is an important cause of chronic cough. Am J Respir Crit Care Med. 1999;160:406-410.
13. Gudbjerg CE. Roentgenologic diagnosis of bronchiectasis. An analysis of 112 cases. Acta Radiol. 1955;43:210-226.
14. Fraser RG, Muller NL, Colman NC, Pare PD. Fraser and Pare’s Diagnosis of Diseases of the Chest, 4th ed. Philadelphia, PA: WB Saunders, 1999.
15. Morrissey BM. Pathogenesis of bronchiectasis. Clin Chest Med. 2007;28:289-296.