Chapter 65 Respiratory Distress and Failure
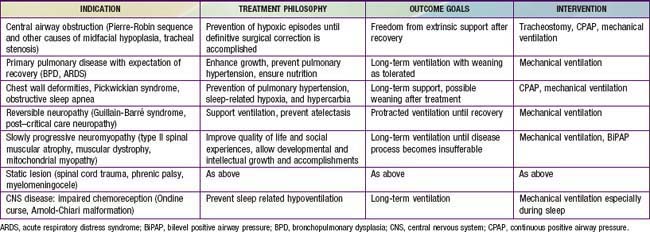
The term respiratory distress is often used to indicate signs and symptoms of abnormal respiratory pattern. A child with nasal flaring, tachypnea, chest wall retractions, stridor, grunting, dyspnea, and wheezing is often judged as having respiratory distress. The magnitude of these findings is used to judge the clinical severity of respiratory distress. Although nasal flaring is a nonspecific sign, the other signs may be useful in localizing the site of pathology (Chapter 365). Respiratory failure is defined as inability of the lungs to provide sufficient oxygen (hypoxic respiratory failure) or remove carbon dioxide (ventilatory failure) to meet metabolic demands. Whereas respiratory distress is a clinical impression, the diagnosis of respiratory failure indicates inadequacy of oxygenation or ventilation or both. Respiratory distress can occur in patients without respiratory disease, and respiratory failure can occur in patients without respiratory distress.
Respiratory Distress
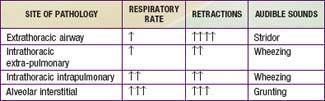
Nasal flaring is an extremely important sign of distress, especially in infants. It is indicative of discomfort, pain, fatigue, or breathing difficulty. The state of responsiveness is another crucial sign. Lethargy, disinterest in surroundings, and poor cry are suggestive of exhaustion, hypercarbia, and impending respiratory failure. Abnormalities of the rate and depth of respirations can occur with both pulmonary and nonpulmonary causes of respiratory distress. In diseases of decreased lung compliance, such as pneumonia and pulmonary edema, respirations are characteristically rapid and shallow (decreased tidal volume). In obstructive airway diseases, such as asthma and laryngotracheitis, respirations are deep (increased tidal volume) but less rapid. Rapid and deep respirations without other respiratory signs should alert the physician to the possibility of nonrespiratory causes of respiratory distress, such as response to metabolic acidosis (diabetic ketoacidosis, renal tubular acidosis) or stimulation of the respiratory center (encephalitis, ingestion of central nervous system [CNS] stimulants). Chest wall, suprasternal, and subcostal retractions are manifestations of increased inspiratory effort, weak chest wall, or both. Inspiratory stridor indicates airway obstruction above the thoracic inlet, whereas expiratory wheezing results from airway obstruction below the thoracic inlet. Grunting is most commonly heard in diseases with decreased functional residual capacity (e.g., pneumonia, pulmonary edema) and peripheral airway obstruction (e.g., bronchiolitis).
Respiratory Disease Manifesting as Respiratory Distress
Clinical examination is important in localizing the site of pathology (Chapter 365). Extrathoracic airway obstruction occurs anywhere above the thoracic inlet. Inspiratory stridor, suprasternal, chest wall, and subcostal retractions, and prolongation of inspiration are hallmarks of extrathoracic airway obstruction. By comparison, features of intrathoracic airway obstruction are prolongation of expiration and expiratory wheezing. Typical manifestations of alveolar interstitial pathology are rapid, shallow respirations, chest wall retractions, and grunting. The site of pathology can be localized and the differential diagnosis established on the basis of the clinical signs and symptoms (Tables 65-1 and 65-2).
Table 65-2 EXAMPLES OF ANATOMIC SITES OF LESIONS CAUSING RESPIRATORY FAILURE
| LUNG | RESPIRATORY PUMP |
|---|---|
| CENTRAL AIRWAY OBSTRUCTION | THORACIC CAGE |
| PERIPHERAL AIRWAY OBSTRUCTION | BRAINSTEM |
| Alveolar-Interstitial Disease | Spinal Cord |
| NEUROMUSCULAR | |
ARDS, acute respiratory distress syndrome; CNS, central nervous system.
Respiratory Distress without Respiratory Disease
Although respiratory distress most commonly results from diseases of lungs, airways, and chest wall, pathology in other organ systems can manifest as “respiratory distress” and lead to misdiagnosis and inappropriate management (Table 65-3). Respiratory distress resulting from heart failure or diabetic ketoacidosis may be misdiagnosed as asthma and improperly treated with albuterol, resulting in worsened hemodynamic state or ketoacidosis.
Table 65-3 NONPULMONARY CAUSES OF RESPIRATORY DISTRESS
| EXAMPLE(S) | MECHANISM(S) | |
|---|---|---|
| Cardiovascular | ||
| Central nervous system | Stimulation of brainstem respiratory centers | |
| Metabolic | Stimulation of central and peripheral chemoreceptors | |
| Renal | Renal tubular acidosis | Stimulation of central and peripheral chemoreceptors |
| Hypertension | Left ventricular dysfunction → increased pulmonary blood/water content | |
| Sepsis |
Cardiovascular Disease Manifesting as Respiratory Distress
A child with cardiovascular pathology may present with respiratory distress caused by 2 mechanisms: (1) decreased lung compliance and (2) cardiogenic shock (Table 65-4). Diseases that result in an increased pulmonary arterial blood flow (e.g., left-to-right shunts) or increased pulmonary venous pressure (e.g., left ventricular dysfunction from hypertension or myocarditis, obstructed total anomalous pulmonary venous return) cause an increase in pulmonary capillary pressure and transudation of fluid into the pulmonary interstitium and alveoli. The increased pulmonary blood and water content leads to decreased lung compliance and results in rapid shallow respirations.
Table 65-4 CARDIOVASCULAR PATHOLOGY MANIFESTING AS RESPIRATORY DISTRESS
Interstitial edema often results in small airway obstruction, manifesting as expiratory wheezing. Patients with cardiac lesions that result in a low cardiac output state, such as obstructive lesions of left side of the heart and acquired or congenital cardiomyopathy, often present in a state of shock with decreased tissue perfusion and metabolic acidosis. Such children demonstrate respiratory distress because of stimulation of chemoreceptors by metabolic acidosis and stimulation of baroreceptors by decreased blood pressure.
Neurologic Disease Manifesting as Respiratory Distress
CNS dysfunction can lead to alterations in respiratory patterns. Increased intracranial pressure (ICP) may manifest as respiratory distress. Early rise in ICP results in stimulation of respiratory centers, leading to increases in the rate (tachypnea) and depth (hyperpnea) of respiration. The resultant decrease in PaCO2 and elevation of cerebrospinal fluid pH lead to cerebral vasoconstriction and amelioration of intracranial hypertension. Cerebral hemispheric and midbrain lesions often result in hyperpnea as well as tachypnea. In such situations, blood gas measurements typically show respiratory alkalosis without hypoxemia. Pathology affecting the pons and medulla manifests as irregular breathing patterns such as apneustic breathing (prolonged inspiration with brief expiratory periods), Cheyne-Stokes breathing (alternate periods of rapid and slow breathing), and irregular, ineffective breathing or apnea. Level of consciousness is most often impaired when abnormal breathing pattern from a brainstem disorder is present. Along with respiratory changes, other manifestations of CNS dysfunction and increased ICP may be present, such as focal neurologic signs, pupillary changes, hypertension, and bradycardia (Chapter 63). Occasionally, severe CNS dysfunction can result in neurogenic pulmonary edema (NPE) and respiratory distress, which may be due to excessive sympathetic discharge resulting in increased pulmonary venous hydrostatic pressure as well as increased pulmonary capillary permeability. Central neurogenic hyperventilation is characteristically observed in CNS involvement by illnesses such as Reye syndrome and encephalitis. Bradycardia and apnea may be due to CNS-depressant medications, poisoning, prolonged hypoxia, trauma, or infection (see Table 65-2).
Toxic-Metabolic States Manifesting as Respiratory Distress
Direct stimulation of respiratory centers resulting in respiratory alkalosis is encountered in certain intoxications, such as those involving salicylates and theophylline. Similarly, intoxication with general CNS stimulants such as cocaine and amphetamines may manifest as increased respirations. Presence of endogenous and exogenous toxins, such as organic acidemias, ingestion of methanol and ethylene glycol, and late stages of salicylism, cause metabolic acidosis and compensatory hyperventilation, which can manifest as respiratory distress. Blood gas measurements show decreased pH and compensatory hypocarbia with normal oxygenation. Metabolic disorders causing hyperammonemia, on the other hand, cause respiratory alkalosis (decreased PaCO2 with increased pH) because ammonia is a stimulant of respiratory centers.
Other Nonpulmonary Entities Manifesting as Respiratory Distress
Sepsis and septic shock may manifest as respiratory distress by causing acute respiratory distress syndrome [ARDS], hypovolemic stimulation of baroreceptors, stimulation of respiratory centers by cytokines, and lactic acidosis. Similarly, renal disease may manifest as respiratory distress by causing metabolic acidosis (e.g., renal tubular acidosis or renal failure) or hypertensive left ventricular failure and fluid overload.
Respiratory Failure
Respiratory failure occurs when oxygenation and ventilation are insufficient to meet the metabolic demands of the body. Respiratory failure may result from an abnormality in (1) lung and airways, (2) chest wall and muscles of respiration, or (3) central and peripheral chemoreceptors (Fig. 65-1). Clinical manifestations depend largely on the site of pathology. Although respiratory failure is traditionally defined as respiratory dysfunction resulting in PaO2 < 60 torr with breathing of room air and PaCO2 > 50 torr resulting in acidosis, the patient’s general state, respiratory effort, and potential for impending exhaustion are more important indicators than blood gas values.
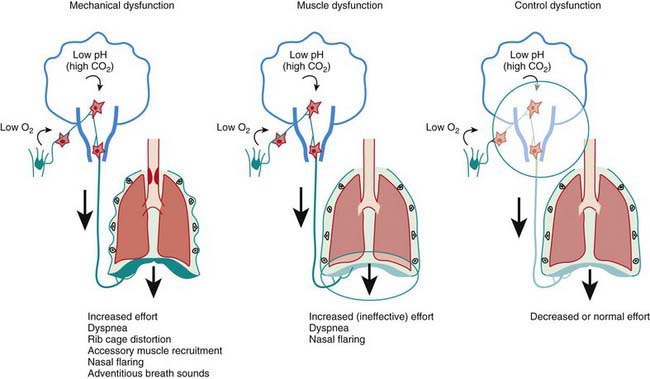
Figure 65-1 Presentation profiles of respiratory failure in childhood. When a mechanical dysfunction is present (by far, the most common circumstance), arterial hypoxemia and hypercapnia (and hence pH) are sensed by peripheral (carotid bodies) and central (medullary) chemoreceptors. After the information is integrated with other sensory information from the lungs and chest wall, chemoreceptor activation triggers an increase in the neural output to the respiratory muscles (vertical arrows), which results in the physical signs that characterize respiratory distress. When the problem resides with the respiratory muscles (or their innervation), the same increase in neural output occurs (arrow), but the respiratory muscles cannot increase their effort as demanded; therefore, the physical signs of distress are more subtle. Finally, when the control of breathing is itself affected by disease, the neural response to hypoxemia and hypercapnia is absent or blunted, and the gas exchange abnormalities are not accompanied by respiratory distress.
Acute lung injury due to pneumonia, sepsis, aspiration, drowning, embolism, trauma, smoke inhalation, or drug overdose often leads to the acute respiratory distress syndrome (Table 65-5; Fig. 65-2).
Table 65-5 SIMPLIFIED CONSENSUS DEFINITION OF ACUTE LUNG INJURY
From Wheeler AP, Bernard GR: Acute lung injury and the acute respiratory distress syndrome: a clinical review, Lancet 369:1553–1564, 2007.

Figure 65-2 Frontal portal chest radiograph showing diffuse bilateral infiltrates consistent with acute lung injury.
(From Wheeler AP, Bernard GR: Acute lung injury and the acute respiratory distress syndrome: a clinical review, Lancet 369:1553–1564, 2007.)
Pathophysiology of Respiratory Failure
Respiratory failure can be classified into 2 categories: (1) hypoxic respiratory failure (failure of oxygenation) and (2) hypercarbic respiratory failure (failure of ventilation). The two entities may coexist as a combined failure of oxygenation and ventilation. The main function of the respiratory system is to move atmospheric gases into the alveolar capillary units of the lung and to move alveolar gas back out into the atmosphere. Systemic venous (pulmonary arterial) blood is arterialized after mixing with the alveolar gas and being carried back to the heart by pulmonary veins. The arterial gas composition depends on the gas composition of the atmosphere and the effectiveness of alveolar ventilation, pulmonary capillary perfusion, and diffusion across the alveolar capillary membrane. Abnormality at any of these steps can result in respiratory failure.
Inspired Gas Composition
Unless modified by the caretaker, inspired gas consists mainly of oxygen and nitrogen. The atmospheric pressure of inspired air depends on altitude. At sea level, it is 760 torr (mm Hg). At higher altitude, atmospheric pressure is lower; in Denver, for instance, the barometric pressure is around 630 torr. When the atmospheric gas reaches alveoli, it is 100% humidified. At 100% humidity and a temperature of 37°C, the water vapor pressure is 47 torr regardless of altitude. Therefore, pressure of inspired gases is calculated as barometric pressure minus 47 torr. Because the fraction of inspired oxygen (FIO2) is 0.2093 (close to 0.21) throughout our atmosphere, the PO2 of inspired gas (PIO2) is (760 − 47) × 0.21 = 150 torr in San Diego (sea level) and (630 − 47) × 0.21 = 122 torr in Denver. Lower PIO2 value at a higher altitude has a potentially adverse effect on oxygenation in respiratory disease. PIO2 can be increased by either an increase in FIO2 or administration of oxygen at greater than atmospheric pressure, such as in a hyperbaric chamber. For a person breathing 40% oxygen, the PIO2 would be 285 torr in San Diego and 234 torr in Denver.
Alveolar Gas Composition
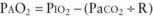
When atmospheric gas enters alveoli, oxygen is exchanged for carbon dioxide. This exchange is not equimolar because the body’s average oxygen consumption is greater than carbon dioxide production, as represented by the respiratory quotient (R), which is CO2 production ÷ O2 consumption. Alveolar gas composition is roughly estimated by the following equation:
where PAO2 is the expected partial pressure of oxygen in alveoli. Under normal metabolic conditions, R is assumed to be 0.8. PAO2 is traditionally compared with PaO2 to determine the extent of oxygenation abnormality; this comparison is referred to as the alveolar-arterial oxygen gradient (A-aO2).
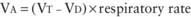
Alveolar Ventilation and Dead Space Ventilation
The amount of air breathed in a minute is termed minute volume, which is a product of tidal volume (VT) and respiratory rate. Part of the VT occupies conducting airways (anatomic dead space) and does not participate in gas exchange. Additionally, air that enters alveoli that are not perfused (e.g., from pulmonary embolism) or poorly perfused (e.g., because of decreased cardiac output) also does not contribute to gas exchange (physiologic dead space). Total dead space (VD) is a sum of anatomic and physiologic dead spaces. Alveolar ventilation (VA) therefore is calculated as follows:
At a constant level of CO2 production, PaCO2 is inversely proportional to alveolar ventilation. An increase in PaCO2 from 40 torr to 80 torr is indicative of a 50% decrease in VA, and a decrease in PaCO2 from 40 torr to 20 torr reflects doubling of VA. An elevated PaCO2, which is indicative of alveolar hypoventilation, can occur from airway obstruction, weakness of respiratory muscles, or CNS dysfunction (hypoventilation).
Ventilation-Perfusion Mismatch, Venous Admixture, Intrapulmonary Shunt
For exchange of O2 and CO2 to occur, alveolar gas must be exposed to blood in pulmonary capillaries. Both ventilation and perfusion are lower in nondependent areas of the lung and higher in dependent areas of the lung. The difference in perfusion ( ) is greater than the difference in ventilation (
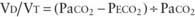
) is greater than the difference in ventilation ( ). Perfusion in excess of ventilation results in incomplete “arterialization” of systemic venous (pulmonary arterial) blood and is referred to as venous admixture. Perfusion of unventilated areas is referred to as intrapulmonary shunting of systemic venous blood to systemic arterial circulation. Conversely, ventilation that is in excess of perfusion is “wasted”; that is, it does not contribute to gas exchange and is referred to as dead space ventilation. Dead space ventilation results in return of greater amounts of atmospheric gas (which has not participated in gas exchange and has negligible CO2) to the atmosphere during exhalation. The end result is a decrease in mixed expired PCO2 (PECO2) and an increase in the PaCO2-PECO2 gradient. The fraction of tidal volume that occupies dead space (VD/VT) is calculated as follows:
). Perfusion in excess of ventilation results in incomplete “arterialization” of systemic venous (pulmonary arterial) blood and is referred to as venous admixture. Perfusion of unventilated areas is referred to as intrapulmonary shunting of systemic venous blood to systemic arterial circulation. Conversely, ventilation that is in excess of perfusion is “wasted”; that is, it does not contribute to gas exchange and is referred to as dead space ventilation. Dead space ventilation results in return of greater amounts of atmospheric gas (which has not participated in gas exchange and has negligible CO2) to the atmosphere during exhalation. The end result is a decrease in mixed expired PCO2 (PECO2) and an increase in the PaCO2-PECO2 gradient. The fraction of tidal volume that occupies dead space (VD/VT) is calculated as follows:
Normal VD/VT is around 0.33. VD/VT increases in states that result in decreased pulmonary perfusion, such as pulmonary hypertension, hypovolemia, and decreased cardiac output. Venous admixture and intrapulmonary shunting predominantly affect oxygenation, resulting in a PAO2-PaO2 (A-aO2) gradient without elevation in PaCO2. The reason is the greater ventilation of perfused areas, which is sufficient to normalize PaCO2 but not PaO2 because of their respective dissociation curves (Chapter 365). The relative straight-line relationship of hemoglobin-CO2 dissociation allows for averaging of PCO2 from hyperventilated and hypoventilated areas. Because the association between oxygen tension and hemoglobin saturation plateaus with increasing PaO2, the decreased hemoglobin-O2 saturation in poorly ventilated areas cannot be compensated for by well-ventilated areas where hemoglobin-O2 saturation has already reached near-maximum. This results in decreased SaO2 and PaO2. Elevation of PaCO2 in such situations is indicative of attendant alveolar hypoventilation. Examples of diseases leading to venous admixture include asthma and aspiration pneumonia, and those of intrapulmonary shunt include lobar pneumonia and acute respiratory distress syndrome.
Diffusion
Even if ventilation and perfusion are matched, gas exchange requires diffusion across the interstitial space between alveoli and pulmonary capillaries. Under normal conditions, there is sufficient time for the pulmonary capillary blood to equilibrate with alveolar gas across the interstitial space. When the interstitial space is filled with inflammatory cells or fluid, diffusion is impaired. Because the diffusion capacity of CO2 is 20 times greater than that of O2, diffusion defects manifest as hypoxemia rather than hypercarbia. Even with the administration of 100% oxygen, PAO2 increases to around 660 torr from 100 torr at sea level, and the concentration gradient for diffusion of O2 is increased by only 6.6 times. Therefore, with diffusion defects, lethal hypoxemia will set in before clinically significant CO2 retention results. In fact, in such situations PCO2 is often decreased because of the hyperventilation that accompanies hypoxemia. Presence of hypercarbia in diseases that impair diffusion is indicative of alveolar hypoventilation from coexisting airway obstruction, exhaustion, or CNS depression. Examples of disease that impair diffusion are interstitial pneumonia, ARDS, scleroderma, and pulmonary lymphangiectasia.
Monitoring a Child in Respiratory Distress and Respiratory Failure
Clinical Examination
Clinical observation is the most important component of monitoring. The presence and magnitude of abnormal clinical findings, their progression with time, and their temporal relation to therapeutic interventions serve as guides to diagnosis and management (Chapter 365). The child with respiratory distress or failure should be observed in the position of greatest comfort and in the least threatening environment.
Pulse oximetry is the most commonly utilized technique to monitor oxygenation. Noninvasive and safe, it is the standard of care in bedside monitoring of children during transport, procedural sedation, surgery, and critical illness. It indirectly measures arterial hemoglobin-O2 saturation by differentiating oxyhemoglobin from deoxygenated hemoglobin using their respective light absorption at wavelengths of 660 nm (red) and 940 nm (infrared). A pulsatile circulation is required to enable detection of oxygenated blood entering the capillary bed. Percentage of oxyhemoglobin is reported as arterial oxyhemoglobin saturation (SaO2); however, the correct description is oxyhemoglobin saturation as measured by pulse oximetry (SpO2). This is because SpO2 may not reflect SaO2 in certain situations. It is important to be familiar with the hemoglobin-O2 dissociation curve (Chapter 365) in order to estimate PaO2 at a given oxyhemoglobin saturation. Because of the shape of the hemoglobin-O2 dissociation curve, changes in PaO2 above 70 torr are not readily identified by pulse oximetry. Also, at the same PaO2 level, there may be a significant change in SpO2 at a different blood pH value. In most situations, an SpO2 value greater than 95% is a reasonable goal, especially in emergency situations. There are exceptions, such as in patients with single ventricle cardiac lesions, in whom the pulmonary and systemic circulations are receiving blood flow from the same ventricle (e.g., after Norwood procedure for hypoplastic left heart syndrome), or with large left-to-right shunts (e.g., ventriculoseptal defect [VSD] and patent ductus arteriosus). In these types of pathophysiologic situations, a lower SpO2 is desired to avoid excessive blood flow to the lungs and pulmonary edema from the pulmonary vasodilatory effects of oxygen, and, in the patient with a single ventricle, diverting blood flow away from the systemic circulation. Because pulse oximetry recognizes all types of hemoglobin as either oxyhemoglobin or deoxygenated hemoglobin, it provides inaccurate information in the presence of carboxyhemoglobin and methemoglobin. Percentage of oxyhemoglobin is overestimated in carbon monoxide poisoning and methemoglobinemia. It should be recognized that dangerous levels of hypercarbia may exist in patients with ventilatory failure, who have satisfactory SpO2 if they are receiving supplemental oxygen. Pulse oximetry should not be the only monitoring method in patients with primary ventilatory failure, such as neuromuscular weakness and CNS depression. It is also unreliable in patients with poor perfusion and poor pulsatile flow to the extremities. Despite these limitations, pulse oximetry is a noninvasive, easily applicable, and effective means of evaluating the percentage of oxyhemoglobin in most patients.
Capnography (end-tidal CO2 measurement) is helpful in determining the effectiveness of ventilation and pulmonary circulation. This method is especially useful for monitoring the level of ventilation in intubated patients. It should be kept in mind that diseases that increase dead space or decrease pulmonary blood flow lead to decreases in end-tidal CO2 and an overestimation of the adequacy of ventilation.
Blood Gas Abnormalities in Respiratory Distress and Respiratory Failure
(See Chapters 52.7 and 365.)
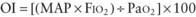
Assessment of Oxygenation and Ventilation Deficits
Indicators for following clinical progress and for determining the prognosis in patients with defects in oxygenation or ventilation include:
 mismatch, intrapulmonary shunt, and diffusion defect, the status of alveolar hypoventilation could have a significant impact on PaO2/FIO2.
mismatch, intrapulmonary shunt, and diffusion defect, the status of alveolar hypoventilation could have a significant impact on PaO2/FIO2. mismatch and alveolar capillary integrity.
mismatch and alveolar capillary integrity.Management
The goal of management for respiratory distress and respiratory failure is to ensure a patent airway and provide necessary support for adequate oxygenation of the blood and removal of CO2. Compared with hypercapnia, hypoxemia is a life-threatening condition, initial therapy for which should be aimed at ensuring adequate oxygenation.
Oxygen Administration
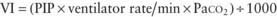
Supplemental oxygen administration is the least invasive and most easily tolerated therapy for hypoxemic respiratory failure. Nasal cannula oxygen provides low levels of oxygen supplementation and is easy to administer. Oxygen is humidified in a bubble humidifier and delivered via nasal prongs inserted in to the nares. In children, a flow rate <5 L/min is most often used because of increasing nasal irritation with higher rates. A common formula for an estimation of the FIO2 during use of a nasal cannula in older children and adults is as follows:
The typical FIO2 value using this method is between 23 and 40%, although the fraction of inspired oxygen varies according to the size of the child, the respiratory rate, and the volume of air moved with each breath. In a young child, because typical nasal cannula flows are a greater percentage of total minute ventilation, significantly higher FIO2 may be provided. Alternately, a simple mask may be employed, which consists of a mask with open side ports and a valveless oxygen source. Variable amounts of room air are entrained through the ports and around the side of the mask, depending on the fit, size, and minute volume of the child. Oxygen flow rates vary from 5 to 10 L/min, yielding typical FIO2 values between 0.30 and 0.65. If more precise delivery of oxygen is desired, other mask devices should be used.
A Venturi mask delivers preset fractions of oxygen through a mask and reservoir system by entraining precise amounts of room air into the reservoir with high-flow oxygen. The amount of room air entrainment and subsequent FIO2 are determined by the adapter at the end of each mask reservoir. The adapter can be chosen to provide between 30 and 50% oxygen concentrations. Oxygen flow rates of 5-10 L/min are recommended to achieve desired FIO2 and to prevent rebreathing. Partial rebreather and nonrebreather masks utilize a reservoir bag attached to a mask to provide higher fractions of oxygen. Partial rebreather masks have two open exhalation ports and contain a valveless oxygen reservoir bag. Some exhaled gas can mix with reservoir gas during exhalation, although most exits the mask via the exhalation ports. Through these ports, room air is also entrained during inspiration. A partial rebreather mask can provide up to 0.6 FIO2 as long as oxygen flow is adequate to keep the bag from collapsing (typically 10-15 L/min). As with nasal cannulas, smaller children with smaller tidal volumes entrain less room air, and their FIO2 values will be higher. Nonrebreather masks include two one-way valves, one between the oxygen reservoir bag and the mask and one on one of the two exhalation ports. This arrangement minimizes mixing of exhaled and fresh gas and entrainment of room air during inspiration. The second exhalation port has no valve, a safeguard to allow some room air to enter the mask in the event of disconnection from the oxygen source. A nonrebreather mask can provide up to 0.95 FIO2. The use of a nonrebreather mask in conjunction with an oxygen blender allows delivery of fractions of oxygen between 0.50 and 0.95. When supplemental oxygen alone is inadequate to improve oxygenation, or when ventilation problems coexist, additional therapies may be necessary.
Airway Adjuncts
Maintenance of a patent airway is a critical step in maintaining adequate oxygenation and ventilation. Artificial pharyngeal airways may be useful in patients with oropharyngeal or nasopharyngeal airway obstruction and in those with neuromuscular weakness in whom native extrathoracic airway resistance contributes to respiratory compromise. An oropharyngeal airway is a stiff plastic spacer with grooves along each side that can be placed in the mouth to run from the teeth along the tongue to its base just above the vallecula. The spacer prevents the tongue from opposing the posterior pharynx and occluding the airway. Because the tip sits at the base of the tongue, it is usually not tolerated by patients who are awake or whose gag reflex is strong. The nasopharyngeal airway, or nasal trumpet, is a flexible tube that can be inserted into the nose to run from the nasal opening along the top of the hard and soft palate with the tip ending in the hypopharynx. It is useful in bypassing obstruction from enlarged adenoids or from contact of the soft palate with the posterior nasopharynx. Because it is inserted past the adenoids, a nasopharyngeal airway should be used with caution in patients with bleeding tendencies.
Inhaled Gases
Helium-oxygen mixture (heliox) is useful in overcoming airway obstruction and improving ventilation. Helium is much less dense and slightly more viscous than nitrogen. When substituted for nitrogen, helium helps maintain laminar flow across an obstructed airway, decreases airway resistance, and improves ventilation. It is especially helpful in diseases of large airway obstruction in which turbulent airflow is more common, such as acute laryngotracheobronchitis, subglottic stenosis, and vascular ring. It is also used in patients with severe status asthmaticus. To be effective, helium should be administered in concentrations of at least 60%, so associated hypoxemia may limit its use in patients requiring more than 40% oxygen. Nitric oxide (NO) is a powerful inhaled pulmonary vasodilator. Its use may improve pulmonary blood flow and  mismatch in patients with diseases that elevate pulmonary vascular resistance, such as persistent pulmonary hypertension of the newborn (PPHN), primary pulmonary hypertension, and secondary pulmonary hypertension due to chronic excess pulmonary blood flow (e.g., VSD) or collagen vascular diseases. NO is administered in doses ranging from 5 to 20 parts per million (ppm). Although administration of NO to unintubated patients is possible, it is usually administered to patients receiving mechanical ventilation through endotracheal tubes, because of the need for precision in NO dosing.
mismatch in patients with diseases that elevate pulmonary vascular resistance, such as persistent pulmonary hypertension of the newborn (PPHN), primary pulmonary hypertension, and secondary pulmonary hypertension due to chronic excess pulmonary blood flow (e.g., VSD) or collagen vascular diseases. NO is administered in doses ranging from 5 to 20 parts per million (ppm). Although administration of NO to unintubated patients is possible, it is usually administered to patients receiving mechanical ventilation through endotracheal tubes, because of the need for precision in NO dosing.
Positive Pressure Respiratory Support
Noninvasive positive pressure respiratory support is useful in treating both hypoxemic and hypoventilatory respiratory failure. Positive airway pressure helps aerate partially atelectatic or filled alveoli, prevent alveolar collapse at end exhalation, and increase functional residual capacity (FRC). This improves pulmonary compliance and hypoxemia and decreases intrapulmonary shunt. In addition, positive pressure ventilation is useful in preventing collapse of extrathoracic airways by maintaining positive airway pressure during inspiration. Improving compliance and overcoming airway resistance also improves tidal volume and therefore ventilation. A high-flow nasal cannula delivers gas flow at 4-16 L/min, providing significant continuous positive airway pressure (CPAP). The amount of CPAP provided is not quantifiable and varies with each patient, depending on the percentage of total inspiratory flow that is delivered from the cannula, airway anatomy, and degree of mouth breathing. In small children, the relative amount of CPAP for a given flow is usually greater than in older children and may provide significant positive pressure. The FIO2 can be adjusted by provision of gas flow through an oxygen blender. For delivery of high-flow air or oxygen, adequate humidification is essential and is achieved with use of a separate heated humidification chamber. CPAP can also be provided through snugly fitting nasal prongs or a tight-fitting facial mask attached to a ventilator or other positive pressure device. Noninvasive CPAP is most useful in diseases of mildly decreased lung compliance and low FRC, such as atelectasis and pneumonia. Diseases of extrathoracic airway obstruction in which extrathoracic negative airway pressures during inspiration lead to airway narrowing (e.g., laryngotracheitis, obstructive sleep apnea, postextubation airway edema) may also benefit from CPAP.
Bilevel positive airway pressure (BiPAP) machines provide positive airway pressure during exhalation and additional positive pressure during inspiration. A BiPAP device allows one to set an expiratory positive pressure (EPAP) and an inspiratory positive pressure (IPAP). The additional positive pressure during inspiration helps augment tidal volume and improve alveolar ventilation in low compliance and obstructive lung disease. The inspiratory and expiratory pressures can be adjusted independently to suit individual needs and comfort. Because of the additional support during inspiration, patients with neuromuscular weakness in particular tend to benefit from BiPAP support.
Endotracheal Intubation and Mechanical Ventilation
When hypoxemia or significant hypoventilation persists despite the interventions already described, tracheal intubation and mechanical ventilation are indicated. Additional indications for intubation include maintaining airway patency in patients who have the potential for airway compromise, such as those with actual or potential neurologic deterioration, and in patients with hemodynamic instability.
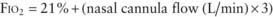
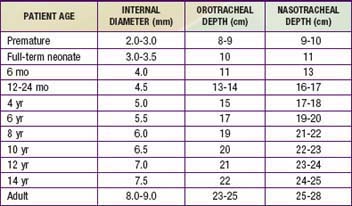
Proper monitoring is essential to ensuring a safe and successful tracheal intubation. Pulse oximetry, heart rate, and blood pressure monitoring are mandatory and should be forgone only in situations calling for emergency intubation. All necessary equipment, including bag-mask ventilation device, laryngoscope, tracheal tube with stylet, and suction equipment, must be available and working properly prior to initiation of intubation. The proper internal diameter (ID) for the tracheal tube can be estimated using the following formula:
Average values for age, size, and depth of insertion for tracheal tubes are given in Table 65-6. Preoxygenation of the patient with high fractions of inspired oxygen is essential and will allow maximum procedure time prior to the onset of hypoxemia.
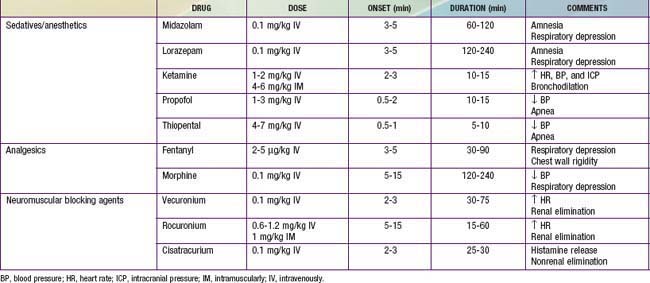
Although intubation can be accomplished without sedation and pharmacologic paralysis in selected patients, the physiologic benefits of these measures to the patient as well as to the facilitation of the intubation usually far outweigh the risks; sedation and paralysis should be considered standard unless contraindicated. Administration of a sedative and analgesic followed by a paralytic agent is a common pharmacologic regimen for facilitating intubation. The particular type and dose of each agent often depends on the underlying disease and clinician preference. Commonly used agents are listed in Table 65-7. An alternative to this pharmacologic approach, especially when intubation is urgent or the patient is suspected of having a full stomach, increasing the risk of aspiration, is rapid sequence intubation (Chapter 62).
Once adequate sedation and/or paralysis has been achieved, ventilation should be assisted with a bag-mask device. After optimal preoxygenation, intubation can be performed. The clinician uses his/her dominant hand to open the patient’s mouth and inserts the laryngoscope blade gently along the tongue to its base. The airway opening can be visualized by applying lift up and away from the clinician, along the axis of the laryngoscope handle. If a straight (Miller) laryngoscope blade is used, the epiglottis is lifted anteriorly by the tip of the blade to visualize the glottis. If a curved (Macintosh) blade is used, the tip should be advanced into the vallecula and then lifted to visualize the glottis. Secretions often obscure visualizations at this step and should be suctioned clear. Once clear visualization of the vocal cords is accomplished, the tube can be placed through the cords. Rapid confirmation of tube placement is essential and should be assessed by as many of the flowing steps as possible: Auscultation of both lung fields as well as the epigastrium for equal breath sounds and good air movement and evaluation of the abdomen for increasing distention should be performed. Adequate bilateral chest expansion and misting inside the tracheal tube with each breath are suggestive of proper tube placement. An increasing heart rate, if heart rate has decreased during the attempt, and a rising or normal pulse oximetry reading are suggestive of successful tube placement. Preoxygenation may significantly delay a drop in SpO2 with improper tube placement, leading to a significant delay in its recognition. Confirmation of exhaled CO2 is mandatory. It can be accomplished with use of a disposable colorimetric CO2 detector or with capnography. In situations of very low pulmonary perfusion, such as cardiac arrest, exhaled CO2 may not be detected. A chest radiograph should also be obtained to confirm proper placement of the tracheal tube, which should lie roughly halfway between the glottis and the carina (Chapter 62).
Transient Manual Ventilation in the Immediate Preintubation and Postintubation Periods
Establishment of ventilation via bag and mask or bag and tracheal tube is required prior to transport of the patient to a setting of continued critical care. The technique of manual ventilation should take into account the underlying pathology. Ventilation of patients with diseases characterized by low FRC (pneumonia, pulmonary edema, ARDS, etc.) should include the application of positive end-expiratory pressure (PEEP) to prevent alveolar derecruitment. This can be accomplished with use of a PEEP valve on a self-inflating ventilation bag or by careful manipulation of exhaust gas using an anesthesia bag. Such diseases are also characterized by a short time constant (Chapter 70) and therefore are best managed with relatively small tidal volumes and high ventilation rates. Diseases characterized by airway obstruction have prolonged time constants and are therefore best managed with relatively slow rates and high tidal volumes.
Chernick V, West J. The functional basis of respiratory disease. In: Chernick V, Boat TF, Wilmott RW, et al, editors. Kendig’s disorders of the respiratory tract in children. ed 7. Philadelphia: Saunders; 2006:29-64.
de Caen A, et al. Airway management. In: Nichols DG, Ackerman AD, Carcillo JA, et al, editors. Rogers’ textbook of pediatric intensive care. ed 4. Philadelphia: Lippincott Williams & Wilkins; 2008:303-322.
Kilpatrick FA, Wilson W. Arterial and capillary blood gas analysis. In: Barnhart S, Czervinske M, editors. Perinatal and pediatric respiratory care. Philadelphia: Saunders; 1995:114-129.
Leaver SK, Evans TW. Acute respiratory distress syndrome. BMJ. 2007;335:389-394.
Lumb AM. Pulmonary ventilation. In Nunn’s applied respiratory physiology, ed 6, Philadelphia: Elsevier/Butterworth Heinemann; 2005:76-91.
Vender J, Clemency M. Oxygen delivery systems, inhalational therapy and respiratory therapy. In: Benumof J, editor. Airway management: principles and practice. Philadelphia: Mosby; 1996:205-227.
Wheeler AP, Bernard GR. Acute lung injury and the acute respiratory distress syndrome: a clinical review. Lancet. 2007;369:1553-1564.
Wratney A, Hamel D, Cheifetz I. Inhaled gases. In: Nichols DG, Ackerman AD, Carcillo JA, et al, editors. Rogers’ textbook of pediatric intensive care. ed 4. Philadelphia: Lippincott Williams & Wilkins; 2008:532-543.
65.1 Mechanical Ventilation
The decision to institute mechanical ventilation is based mainly on the need to assist lung function; supporting left ventricular performance and treating intracranial hypertension are additional indications. Although there are no absolute criteria for derangement of gas exchange, PaO2 <60 torr while breathing >60% oxygen, PaCO2 >60 torr, and pH <7.25 are often reasons to initiate mechanical ventilation. Clinical impressions of fatigue and impending exhaustion are also indications for ventilatory support even in the presence of adequate gas exchange. Positive pressure ventilation is a powerful means of decreasing left ventricular afterload, and it is used for this purpose in patients with cardiogenic shock resulting from left ventricular dysfunction. Mechanical ventilation is also used in patients whose respirations are unreliable (e.g., unconscious patients, those with neuromuscular dysfunction) and when deliberate hyperventilation is desired, such as in patients with intracranial hypertension.
Mechanical ventilation neither is intended to normalize gas exchange nor is a form of cure. The goals are to maintain sufficient oxygenation and ventilation to ensure tissue viability until the disease process has resolved and to minimize the inevitable complications of the therapeutic intervention itself. PaO2, PaCO2, and pH levels are maintained in ranges that provide a safe environment for the patient while protecting the lungs from damage due to oxygen toxicity, pressure (barotrauma), tidal volume overdistention (volutrauma), atelectotrauma, and cytokine release (biotrauma) (Figs. 65-3 and 65-4).
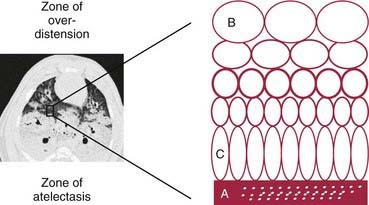
Figure 65-3 Atelectotrauma. The interface between collapsed and consolidated lung (A) and overdistended lung units (B) is heterogeneous and unstable. Depending on ambient conditions, this region is prone to cyclic recruitment and derecruitment and localized asymmetric stretch of lung units (C) immediately apposed to regions of collapsed lung.
(From Pinhu L, Whitehead T, Evans T, et al: Ventilator-associated lung injury, Lancet 361:332–340, 2003.)
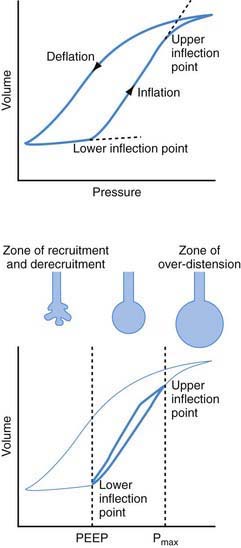
Figure 65-4 Pulmonary pressure-volume relation in a patient with acute lung injury. Top, The lower inflection point is typically 12-18 cm H2O, and the upper inflection point 26-32 cm H2O. Bottom, Specific protective ventilation strategies require that positive end-expiratory pressure is set just above the lower inflection point and the pressure limit (Pmax) just below the upper inflection point. Hence the lung is ventilated in the safe zone between the zone of recruitment and derecruitment and the zone of overdistention, and both high-volume and low-volume injury are avoided.
(From Pinhu L, Whitehead T, Evans T, et al: Ventilator-associated lung injury, Lancet 361:332–340, 2003.)
Basic Concepts of Ventilator Management
Equation of Motion
A pressure gradient is required for air to move from one place to another (Fig. 65-5). During natural spontaneous ventilation, inspiration results from generation of negative intrapleural pressure from contraction of the diaphragm and intercostal muscles, drawing air from the atmosphere across the airways into the alveoli. During mechanical ventilation, inspiration results from positive pressure created by compressed gases through the ventilator, which pushes air across the airways into alveoli. In both spontaneous and mechanical ventilation, exhalation results from alveolar pressure generated by the elastic recoil of the lung and the chest wall. Pressure necessary to move a given amount of air into the lung is determined by two factors: lung and chest wall elastance, and airway resistance. The relationship among pressure gradient, compliance, and resistance is described in Figure 65-5. Elastance—defined as the change in pressure (ΔP) divided by the change in volume (ΔV)—refers to the property of a substance to oppose deformation. It is opposite of compliance (ΔV ÷ ΔP), the property of a substance to allow distention or lengthening when subjected to pressure. Compliance (C) is therefore expressed as 1/elastance.
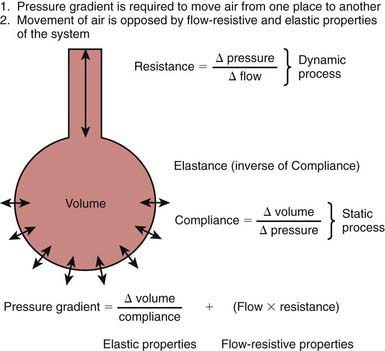
Figure 65-5 Equation of motion. A pressure gradient is required to move air from one place to another. In the lungs, the required pressure gradient must overcome the lung and chest wall elastance (static component) and the flow-resistive properties (dynamic component). The static component is increased in alveolar interstitial diseases and stiff chest wall, whereas the dynamic component is increased with airway obstruction.
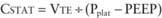
The pressure needed to overcome tissue elastance is measured in conditions in which there is no flow (at end-inspiration and end-expiration) and is therefore a reflection of static conditions in the lung. It is influenced by tidal volume and compliance (P = ΔV ÷ C). It is increased with high tidal volume and low compliance. This pressure gradient is used to calculate the static compliance of the respiratory system (CSTAT).
Resistance (R) refers to the opposition to generation of flow. It is measured as the amount of pressure needed to generate a unit of flow (Δ P ÷ ΔFlow). Pressure needed to overcome airway resistance is calculated as flow multiplied by resistance. Because this pressure is needed only when the flow is occurring through the airways, it is referred to as the dynamic component. Pressure to overcome flow-resistive properties is measured when there is maximum flow and is therefore under dynamic conditions. It is increased in conditions with greater airway resistance and flow rate. Flow rate depends on the time allowed for inspiration and expiration. At higher respiratory rates, there is less time available for each inspiration and expiration, necessitating higher flows; therefore higher pressure is required to overcome flow-resistive properties. The pressure gradient necessary to move air from one place to another is the sum of pressure needed to overcome the elastic and flow-resistive properties of the lung. This pressure gradient is taken into account to calculate the dynamic compliance of the respiratory system (CDYN). The difference in change in pressure between static conditions and dynamic conditions is attributable to airway resistance.
Functional Residual Capacity
Also see Chapter 365.
During inspiration, oxygen-enriched gas enters alveoli. During exhalation, oxygen continues to be removed by the pulmonary capillary circulation. Functional residual capacity is the volume of gas left in the alveoli at the end of expiration. It is the only source of gas available for gas exchange during exhalation. In diseases with decreased FRC (e.g., ARDS, pulmonary edema), alveolar oxygen concentration declines sharply throughout expiration, resulting in hypoxemia. Two ventilator strategies commonly employed to improve oxygenation in such situations are the application of PEEP and increasing the inspiratory time (TI) (Fig. 65-6). PEEP increases FRC, whereas a longer TI allows longer exposure of pulmonary capillary blood to a higher concentration of O2 during inspiration.
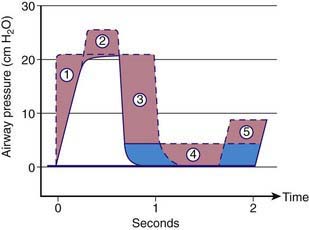
Figure 65-6 Five different ways to increase mean airway pressure: (1) Increase the respiratory flow rate, producing a square wave inspiratory pattern; (2) increase the peak inspiratory pressure; (3) reverse the inspiratory-expiratory ratio or prolong the inspiratory time without changing the rate; (4) increase positive end-expiratory pressure; and (5) increase the ventilatory rate by reducing the expiratory time without changing the inspiratory time.
(From Harris TR, Wood BR: Physiologic principles. In Goldsmith JP, Karotkin EH, editors: Assisted ventilation of the neonate, ed 3. Philadelphia, 1996, WB Saunders.)
Time Constant
At the beginning of inspiration, the atmospheric pressure is higher than the pressure in the alveoli, resulting in movement of air into the alveoli. During mechanical ventilation, the ventilator circuit serves as the patient’s atmosphere. As alveoli expand with air, the alveolar pressure rises throughout inspiration until it equilibrates with the ventilator pressure, at which time airflow ceases. Expiration starts when the ventilator pressure falls below the alveolar pressure. Alveolar pressure decreases throughout expiration until it reaches the ventilator pressure, at which time no further egress of air from the alveoli occurs. If inspiration or expiration is terminated before pressure equilibration between alveoli and the ventilator is allowed to occur, alveolar expansion during inspiration or alveolar emptying during expiration is incomplete. Incomplete inspiration results in delivery of decreased tidal volume, whereas incomplete expiration is associated with air trapping and the presence of residual PEEP in the alveoli that is greater than the ventilator pressure, referred to as auto-PEEP. Some time is required for pressure equilibration to occur between alveoli and the atmosphere, which is reflected in the time constant (TC). It takes 3 TCs for 95%, and 5 TCs for 99%, of pressure equilibration to occur. The time constant depends on compliance and resistance, and their relationship is depicted in Figure 65-7. Time constant is calculated as compliance multiplied by resistance (C × R) and is measured in seconds.
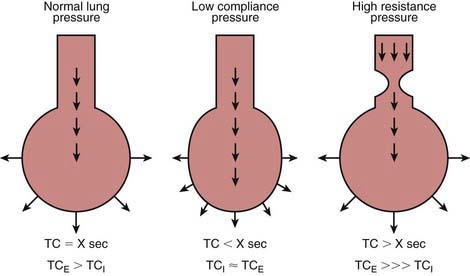
Figure 65-7 Time constant (TC). A certain amount of time is necessary for pressure equilibration (and therefore completion of delivery of gas) to occur between proximal airway and alveoli. TC, a reflection of time required for pressure equilibration, is a product of compliance and resistance. In diseases of decreased lung compliance, less time is needed for pressure equilibration to occur, whereas in diseases of increased airway resistance, more time is required. Expiratory TC is increased much more than inspiratory TC in obstructive airway diseases, because airway narrowing is exaggerated during expiration.
Diseases with decreased compliance (increased elastance) are characterized by high elastic recoil pressure, which results in more rapid equilibration of alveolar and ventilator pressures, thereby decreasing TC. Diseases with increased airway resistance are associated with slower flow rates, require longer time for movement of air from one place to another, and therefore have increased TC. Airways expand during inspiration and narrow during expiration (Chapter 365). Therefore, expiratory time constant (TCE) is longer than inspiratory time constant (TCI). In intrathoracic airway obstruction (asthma, bronchiolitis, aspiration syndromes), airway narrowing is much more pronounced during expiration. Therefore, although both TCE and TCI are prolonged in such diseases, TCE is much more prolonged than TCI. Patients with such diseases therefore are best ventilated with slower rates, higher tidal volume, and longer expiratory time than inspiratory time. In diseases characterized by decreased compliance, both TCE and TCI are short; however, the TCE is closer to TCI than in normal lungs because of the stiffer alveoli recoil with greater force. Patients with these diseases are best ventilated with small VT to prevent ventilator-induced lung injury and with a relatively longer inspiratory time in each breath to improve oxygenation.
Critical Opening Pressure
Collapsed or atelectatic alveoli require a considerable amount of pressure to open. Once open, the alveoli require relatively less pressure for continued expansion. The process of opening atelectatic alveoli is called recruitment. In a normal lung, alveoli remain open at the end of expiration, and therefore the lung requires relatively less pressure to receive its tidal volume. In a disease process in which the alveoli collapse at the end of expiration (e.g., ARDS), a substantial amount of pressure is required to open the alveoli during inspiration. This pressure causes ventilator-induced lung injury via two mechanisms: (1) barotrauma at the terminal airway–alveolar junction and (2) volutrauma due to overdistention of alveoli that are already open (see Figs. 65-3 and 65-4). Although a pulmonary parenchymal disease process is rarely uniform, and each of the millions of alveoli may have its own mechanical characteristics, a composite volume-pressure relationship could be conceptualized for the whole lung (Fig. 65-8).
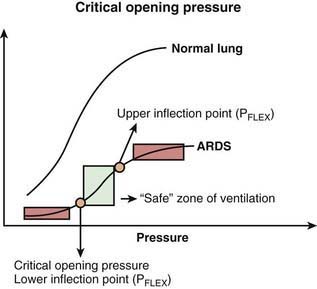
Figure 65-8 Volume-pressure relationship in normal lung and in acute respiratory distress syndrome (ARDS). In ARDS, atelectatic alveoli require a considerable amount of pressure to open. Critical opening pressure, also referred to as lower PFLEX, is the airway pressure above which further alveolar expansion occurs with relatively less pressure. Upper PFLEX is the airway pressure above which further increase in pressure results in less alveolar expansion; this is the area of alveolar overdistention. Keeping tidal volume between upper and lower PFLEX values is considered less injurious to the lung.
In these situations, the lower and upper portions of the curve are relatively horizontal, and the middle portion is more vertical. At the beginning of inspiration, atelectatic alveoli are being recruited, requiring high pressure for a relatively small increase in volume. Once they are recruited, further increase in volume requires relatively less pressure. The pressure at which most alveoli are open is called critical opening pressure; this point is also referred to as the lower inflection point (lower PFLEX). After the lower PFLEX, greater volume can be delivered for relatively less pressure until the upper PFLEX is reached, at which the volume-pressure curve again becomes relatively horizontal. The goal of mechanical ventilation in alveolar interstitial pathology is to deliver a tidal volume between the lower and upper inflection points, the so-called safe zone of ventilation. If tidal volume is delivered with a change in inflation pressure that includes the lower PFLEX, alveoli are likely to open AND close during every breath, a process termed tidal recruitment that is injurious to the lung, especially at the terminal airway–alveolar junction. If tidal volume is delivered with a change of pressure that includes the upper PFLEX, overdistention of alveoli is likely to occur, resulting in volutrauma and barotrauma. Keeping tidal ventilation between the upper and lower PFLEX values is accomplished by maintaining a level of PEEP to produce baseline alveolar recruitment and delivering a relatively small (6 mL/kg) tidal volume. Termed “open lung” strategy, this approach has proved to be beneficial in alveolar interstitial diseases such as ARDS.
Phases of Mechanical Ventilation
The planning of a ventilatory strategy must consider the four phases of the respiratory cycle separately, taking into account the patient’s clinical characteristics. These are: (1) initiation of respiration and a variable that is controlled, often referred to as mode; (2) inspiratory phase characteristics, which determine the duration of inspiration and how the pressure or volume is delivered; (3) termination of inspiration, often referred to as cycle; and (4) expiratory phase characteristics. Ideally, mechanical ventilation should not completely take over the work of breathing but, rather, should assist the patient’s own respiratory effort. In the absence of the patient’s effort, respiratory muscle deconditioning may occur, making weaning from mechanical ventilation more difficult.
Initiation of Inspiration and the Control Variable (Mode)
The initiation of inspiration may be set to occur at a predetermined rate and interval regardless of patient effort, or it could be timed in response to patient effort. Once inspiration is initiated, the ventilator breath either is controlled entirely by the ventilator (control mode) or supports the patient’s inspiratory effort to a predetermined inspiratory volume or pressure target (support mode). Advances in technology allow for greater patient-ventilator synchrony to occur. The ventilator may be set to be “triggered” by the signal it receives as a result of patient effort. This may be in the form of lowering of either pressure (pressure trigger) or airflow (flow trigger) in the ventilator circuit generated by the patient’s inspiratory effort. If no such signal is received because of lack of patient effort, the ventilator delivers a breath at an interval selected by the operator.
Control Modes
Intermittent Mandatory Ventilation Mode
In intermittent mandatory ventilation (IMV), the inspiration is initiated at a set frequency with a timing mechanism independent of patient effort. In between machine-delivered breaths, the patient can breathe spontaneously from a fresh source of gas. IMV allows for adjustment of ventilator support according to the patient’s needs and is therefore useful in the weaning process. Lack of synchrony between machine-delivered breaths and patient efforts may result in ineffective ventilation and patient discomfort, especially when IMV is delivered at a high rate. In such cases, the patient may require sedation and pharmacologic paralysis for efficient delivery of tidal volume. To obviate this problem, synchronized IMV (SIMV) is used, whereby the machine-delivered breaths are triggered by the patient’s inspiratory efforts (Fig. 65-9). In between the machine-delivered breaths, a fresh source of gas is available for spontaneous patient breaths. In the absence of patient effort, the patient receives a backup rate much like in IMV mode. Even with SIMV, ventilator-patient asynchrony can occur, because tidal volume, inflation pressure, and inspiratory time are determined by the ventilator alone.
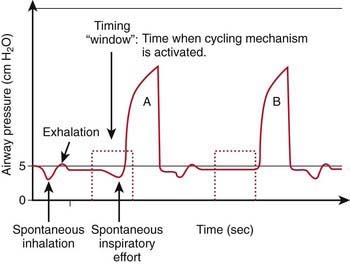
Figure 65-9 Synchronized intermittent mandatory ventilation. At set intervals, the ventilator’s timing circuit becomes activated and a timing “window” appears (shaded area). If the patient initiates a breath in the timing window, the ventilator delivers a mandatory breath. If no spontaneous effort occurs, the ventilator delivers a mandatory breath at a fixed time after the timing window.
(From Banner MJ, Gallagher TJ: Respiratory failure in the adult: ventilatory support. In Kirby RR, Smith RA, Desautels DA, editors: Mechanical ventilation, New York, 1985, Churchill Livingstone.)
Assist-Control Mode
In assist-control (AC) mode, each and every patient breath is triggered by pressure or flow generated by patient inspiratory effort and “assisted” with either preselected inspiratory pressure or volume. The rate of respirations is therefore determined by the patient’s inherent rate. A backup total (patient and ventilator) obligatory rate is set to deliver a minimum number of breaths. On AC mode with a backup rate of 20 breaths/min, all of the breaths of a patient with an inherent respiratory rate of 15 breaths/min will be assisted by the ventilator, and the patient will receive 5 additional breaths/min. On the other hand, a patient with an inherent rate of 25 breaths/min will receive all 25 breaths assisted. Although useful in some patients, the AC mode cannot be used in the weaning process, which involves gradual decrease in ventilator support.
Control Variable
Once initiated, either the tidal volume or the pressure delivered by the machine can be controlled. The machine-delivered breath is thus referred to as either volume-controlled or pressure-controlled (Table 65-8).
Table 65-8 CHARACTERISTICS OF PRESSURE-CONTROLLED AND VOLUME-CONTROLLED METHODS OF VENTILATION
| PRESSURE-CONTROLLED VENTILATION | VOLUME-CONTROLLED VENTILATION | |
|---|---|---|
| Control setting(s) | ||
| Machine-delivered volume | Depends on respiratory system compliance and resistance | Constant |
| Inflation pressure | Constant | Depends on respiratory system compliance and resistance |
| Endotracheal tube leak | Somewhat compensated | Leaked volume part of VT |
| Distribution of ventilation | More uniform in lungs with varying time constant units | Less uniform in lungs with varying time constant units |
| Patient comfort | Possibly compromised | Possibly enhanced |
| Weaning | Inflation pressure adjustment required to deliver desired VT | VT remains constant, inflation pressure automatically weaned |
VT, tidal volume.
With volume-controlled ventilation (VCV), machine-delivered volume is the primary control, and the inflation pressure generated depends on the respiratory system’s compliance and resistance. Changes in respiratory system compliance and resistance are therefore easily detected from changes observed in inflation pressure. In pressure-controlled ventilation (PCV), the pressure change above the baseline is the primary control, and the tidal volume delivered to the lungs depends on the respiratory system’s compliance and resistance. Changes in respiratory system compliance and resistance do not affect inflation pressure and may therefore go undetected unless the exhaled VT is monitored. VCV and PCV have their own advantages and disadvantages (see Table 65-8). Generally speaking, PCV is more efficient than VCV in terms of amount of tidal volume delivered for a given inflation pressure during ventilation of a lung that has nonuniform time constants, such as asthma. In VCV, relatively less-obstructed airways are likely to receive more of the machine-delivered volume throughout inspiration than relatively more-obstructed airways with longer time constants (Fig. 65-10A). This situation would result in uneven ventilation, higher PIP, and a decrease in dynamic compliance. In PCV, because of a constant inflation pressure that is held throughout inspiration, relatively less-obstructed lung units with shorter time constants would achieve pressure equilibration earlier during inspiration than the relatively more-obstructed areas. Thus, units with shorter time constants would attain their final volume earlier in inspiration, and those with longer time constants would continue to receive additional volume later in inspiration (Fig. 65-10B). This situation would result in more even distribution of inspired gas, delivery of more tidal volume for the same inflation pressure, and improved dynamic compliance in comparison with VCV.
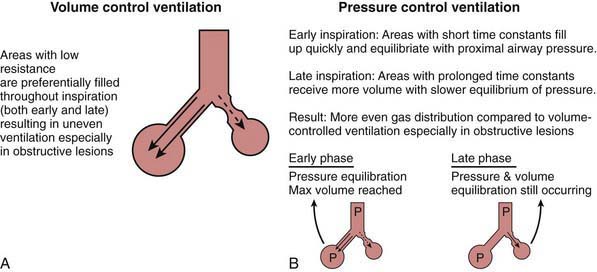
Figure 65-10 A, In volume-controlled ventilation, tidal volume is delivered to the less obstructed areas throughout inspiration. Obstructed areas of the lung therefore receive a lower proportion of tidal volume, resulting in uneven ventilation. B, In pressure-controlled ventilation, less obstructed areas equilibrate with inflation pressure and therefore receive most of their tidal volume early during inspiration. More obstructed areas, with prolonged time constants, require longer time for pressure equilibration and therefore continue to receive a portion of their tidal volume later during inspiration. The entire tidal volume is more evenly distributed than with volume-cycled ventilation.
Pressure-regulated volume control (PRVC) combines the advantages of VCV and PCV. In this mode, the VT and inspiratory time are controlled as primary variables but the ventilator determines the amount of pressure needed to deliver the desired tidal volume. Inflation pressure is thus adjusted to deliver the prescribed tidal volume over the inspiratory time, depending on the patient’s respiratory compliance and resistance.
Support Modes
Pressure support ventilation (PSV) and volume support ventilation (VSV) are designed to support the patient’s spontaneous respirations. With PSV, initiation of inspiration is triggered by the patient’s spontaneous breath, which is then “supported” by a rapid rise in ventilator pressure to a preselected level. The inspiration is continued until the inspiratory flow rate falls to a set level (generally 25% of peak flow rate) as the patient’s lungs fill up. Thus, inspiratory time is controlled by the patient’s own efforts. PSV can be combined with SIMV so that any breath above the SIMV rate is supported by PSV. Allowing the patient to control as much of the rate, tidal volume, and inspiratory time as possible is considered a gentler form of mechanical ventilation than SIMV, in which the tidal volume (or inflation pressure) and inspiratory time are preset. PSV as the sole source of mechanical ventilator support is often not adequate for patients with severe lung disease; however, it is especially useful in patients in the process of being weaned and in patients who require mechanical ventilation for relatively minor lung disease or for neuromuscular weakness. VSV is similar to PSV, in that all the spontaneous breaths are supported. In VSV, inspiratory pressure to support spontaneous breaths is adjusted to guarantee a preset tidal volume. If there is a change in respiratory mechanics or patient effort, the inspiratory pressure to support the breath initiated by patient effort is automatically adjusted to deliver the set tidal volume.
Inspiratory Phase Characteristics
Inspiratory time, inspiratory flow waveform, and pressure rise time can be adjusted in the inspiratory phase to suit the patient’s respiratory mechanics.
In PCV, the duration of inspiratory time (TI) is directly set in seconds. In VCV, the inspiratory time can be adjusted by adjusting the inspiratory flow (volume/time). The choice of TI value depends on the respiratory rate, which determines the total duration of each breath, and on the estimation of inspiratory and expiratory time constants. Decreasing the flow rate delivery increases TI, and vice versa. With an increase in TI, the pulmonary capillary blood is exposed to a higher level of alveolar PO2 for a longer time. This is beneficial in diseases with decreased FRC, such as ARDS and pulmonary edema. An increase in TI also increases VT without increasing inflation pressure in PCV if inspiratory flow is still occurring at the end of expiration. It must be recognized that at a given ventilator rate, an increase in TI decreases expiratory time (TE). Therefore, any strategy that employs an increase in the inspiratory component of the respiratory cycle should ensure that the decreased TE is still sufficient for complete exhalation.
Inspiratory flow waveform can be adjusted in VCV mode as either a constant flow (square waveform) or a decelerating flow (descending ramp waveform). With a square waveform, flow is held constant throughout inspiration. In a descending ramp waveform, the flow is maximum at the start of inspiration and declines throughout its duration. It is debatable which flow pattern is better for a given disease. In PCV and PSV, the prescribed PIP is reached through delivery of airflow. The time required for the ventilator to reach PIP is reflected in the pressure rise time, which can be adjusted by control of flow at the beginning of the inspiratory phase. The inspiratory flow rise time is adjusted to provide comfort for a patient who is awake and also to prevent an extremely rapid rise in inspiratory pressure, which might result in barotrauma.
Termination of Inspiration (Cycle)
The two most commonly used inspiratory terminating mechanisms in control modes are time-cycled and volume-cycled. With a time-cycled mechanical breath, inspiration is terminated after a preselected inspiratory time has elapsed, whereas with volume-cycled breath, the inspiration ends after a preselected volume has been delivered by the machine into the ventilator circuit. A time-cycled breath is almost always pressure-limited, with the PIP held constant for the duration of inspiration. A volume-cycled breath can be pressure-limited as a safety mechanism to avoid barotrauma. The inspiration-terminating mechanism is set somewhat differently in support modes. In PSV, the inspiration is set to end after the inspiratory flow decreases below a certain percentage (usually 25%) of peak inspiratory flow. This happens when the patient no longer desires to receive additional tidal volume. Such a breath can be termed flow-cycled. In volume support mode, inspiration is terminated when the patient has received the desired tidal volume.
Expiratory Phase Maneuvers
The most useful expiratory phase maneuver is the application of PEEP, which is applied to both the control breath and the assisted breath. The most important clinical benefits of PEEP are to recruit atelectatic alveoli and to increase FRC in patients with alveolar-interstitial diseases and thereby improve oxygenation. There is growing recognition that even a brief disconnection from a ventilator, and therefore having zero end-expiratory pressure, can result in significant alveolar derecruitment and decline in oxygenation. In patients with obstructive lesions in which insufficient exhalation results in air trapping and auto-PEEP, extrinsic PEEP (that applied through a mechanical device) can prevent airway closure during expiration and improve ventilation. Other salutary effects of PEEP include redistribution of extravascular lung water away from gas-exchanging areas, improved ventilation-perfusion relationship, and stabilization of the chest wall. The effect of PEEP on lung compliance is variable, depending on the level of PEEP provided and the patient’s pulmonary mechanics. By shifting the tidal volume ventilation to a more favorable part of the pressure-volume curve, PEEP may recruit more alveoli, delay airway closure, and improve lung compliance. Excessive PEEP, on the other hand, may lead to overdistention of alveoli and reduced compliance. The effect of PEEP in individual patients can be ascertained by measuring exhaled tidal volume and calculating dynamic compliance. Other deleterious effects of PEEP include decreased venous return, increased pulmonary vascular resistance, and decreased cardiac output.
Additional Ventilatory Modalities
Airway Pressure Release Ventilation
Airway pressure release ventilation (APRV) improves oxygenation in cases of severe hypoxemic respiratory failure resulting from alveolar-interstitial disease. This modality applies a continuous positive airway pressure, designated CPAPHIGH, to recruit and maintain FRC with brief intermittent release phases of CPAPLOW to allow alveolar gas to escape. CPAPHIGH is analogous to PIP, and CPAPLOW is similar to setting PEEP. In contrast to the patient receiving conventional mechanical ventilation, a patient receiving APRV spends the majority of time in the CPAPHIGH phase, which may last as long as 3-5 sec with a brief (0.3-0.5 sec) time in the CPAPLOW phase. These atypically long inspiratory times are tolerated because of a floating expiratory valve in the ventilator circuit that permits spontaneous breathing during CPAPHIGH phase. Therefore, even if CPAPHIGH phase can be considered inspiratory and CPAPLOW phase can be considered expiratory as far as the ventilator is concerned, the patient is able to breathe spontaneously during both of these phases. The longer ventilator inspiratory times recruit lung units, and the ability to breathe spontaneously during this phase allows distribution of gas flow to atelectatic lung regions. The outcome benefit of APRV in pediatric hypoxemic respiratory failure has not been proven.
High-Frequency Ventilation
Mechanical ventilation at supraphysiologic rates and low tidal volumes, known as high-frequency ventilation (HFV), improves gas exchange in a selected group of patients who show no response to traditional ventilatory modalities. The mechanism of alveolar ventilation in HFV is very different from that in conventional ventilation, in that HFV is less dependent on tidal volume and more dependent on asymmetric velocities and convective dispersion of inspired gas. Patients with severe persistent hypoxic failure are most likely to benefit from HFV. HFV is also helpful in patients with bronchopleural fistula and persistent air leaks. The main tenet of HFV is to recruit lung volume with a high MAP and produce smaller fluctuations in alveolar pressure during inspiration and expiration, thus maintaining a satisfactory FRC and reducing alveolar stretch. The two most investigated techniques of HFV are high-frequency oscillation (HFO) and high-frequency jet ventilation (HFJV).
The most commonly used HFV modality is HFO, which employs a mechanism to generate to-and-fro air movement. Additional air is dragged in (entrained) through a parallel circuit via a Venturi effect. Air is pushed in during inspiration and actively sucked out during expiration. The main determinants of oxygenation are FIo2 and MAP, whereas ventilation is determined by changes in pressure (amplitude) from the MAP. Commonly used respiratory frequency varies from 5 Hz (300 breaths/min) in adults and older children, to 6-8 Hz (360-480 breaths/min) in young children, 8-10 Hz (480-600 breaths/min) in infants, and 10-12 Hz (600-720 breaths/min) in newborn and premature babies.
In HFJV, a high-frequency interrupter is interposed between a high-pressure gas source and a small cannula that is incorporated in the endotracheal tube (ET). The cannula propels tiny amounts of gas (jets) at high velocity and high frequency through the ET. An additional amount of gas is entrained from a parallel circuit. Unlike in HFO, expiration occurs passively in HFJV as a result of elastic recoil of the lung and the chest wall. PEEP is set through the parallel circuit by a conventional ventilator in line. Respiratory rate is generally set at 420 breaths/min. Major determinants of oxygenation are FIO2 and PEEP, and the major determinant of ventilation is PIP.
Conventional Ventilator Settings
FIO2
The shape of the hemoglobin-oxygen dissociation curve dictates that oxygen content in the blood is not linearly related to PaO2. A PaO2 value that results in an oxyhemoglobin saturation of 95% is reasonable in most situations, because a higher PaO2 would cause minimal increase in arterial oxygen content, and a modest (≈10 torr) drop in PaO2 would result in minimal decrease in oxyhemoglobin saturation. In most cases, a PaO2 value of 70-75 torr is a reasonable goal. FIO2 values that are higher than those necessary to attain oxyhemoglobin saturations of 95% expose the patient to unnecessary oxygen toxicity. Whenever possible, FIO2 values should be decreased to a level ≤0.4 as long as oxyhemoglobin saturation remains 95% or above.
Mode
The choice of mode of ventilation depends on how much ventilator-patient interaction is desired and the disease entity that is being treated. SIMV or AC is chosen as the control mode, PCV, VCV, or PRVC is chosen as the variable that is to be controlled, and PS and VS are the choices for support modes.
Tidal Volume and Rate
As previously discussed, alveolar ventilation, the chief determinant of PaCO2, is calculated using tidal volume, respiratory rate, and dead space volume. A change in VT results in a corresponding change in VA without affecting the dead space ventilation. A change in respiratory rate will affect the VA as well as the dead space ventilation. As mentioned earlier, the choice of VT and rate depends on the time constant. In a patient with relatively normal lungs, an age-appropriate ventilator rate and a tidal volume of 7-10 mL/kg would be appropriate initial settings. Diseases associated with decreased time constants (decreased static compliance, e.g., ARDS, pneumonia, pulmonary edema) are best treated with small (6 mL/kg) tidal volume and relatively rapid rates (25-40 breaths/min). Diseases associated with prolonged time constants (increased airway resistance, e.g., asthma, bronchiolitis) are best treated with relatively slow rates and higher (10-12 mL/kg) tidal volume. In PCV, the delivered VT depends on the compliance and resistance of the patient’s respiratory system and needs to be monitored to ensure the appropriate amount for a given situation. An inflation pressure of 15 to 25 cm H2O is sufficient for most patients, but it may need adjustment, depending on the amount of exhaled tidal volume observed. It should be emphasized that achieving a “normal” PaCO2 value is not a requirement for mechanical ventilation. Mild hypercapnia (permissive hypercapnia) should be acceptable, especially when one is attempting to limit injurious inflation pressures or tidal volumes.
Inspiratory Time and Expiratory Time
Inspiratory time and expiratory time are adjusted by setting inspiratory flow rate in VCV and by setting the precise TI in PCV. Increasing the inspiratory time results in an increase in MAP, improvement in oxygenation in diseases with decreased FRC, and better distribution of tidal volume in obstructive lung disease. Sufficient expiratory time must be provided to ensure adequate emptying of the alveoli.
Patient-Ventilator Asynchrony
Patient-ventilator asynchrony occurs when the patient’s respiratory pattern does not match that of the ventilator. This can occur during all phases of respiration. Adverse effects of patient-ventilator asynchrony include wasted effort, ineffective delivery of desired tidal volume, excessive generation of intrathoracic pressure resulting in barotrauma and adverse effects on cardiac output, increased work of breathing, and patient discomfort. Although several mechanisms exist to facilitate patient-ventilator asynchrony, a certain amount of asynchrony is inevitable unless the patient is pharmacologically sedated and paralyzed.
Triggering the Ventilator
The patient must be able to trigger the ventilator without extraordinary effort. Ventilators can be pressure-triggered or flow-triggered. With pressure triggering, the inspiratory valve opens and flow is delivered when a set negative pressure is generated within the patient-ventilator circuit during both inspiration and expiration. The amount of pressure required to trigger an inspiration depends on the pressure trigger sensitivity. In flow triggering, the ventilator provides a base flow of gas through the ventilator-patient circuit. When a flow sensor on the expiratory limb of the patient-ventilator circuit detects a decrease in flow as a result of the patient’s inspiratory effort, the inspiratory valve opens and a ventilator breath is delivered. The degree of change in flow required to trigger an inspiration depends on the flow trigger sensitivity. Flow triggering is considered to be more comfortable, primarily because the patient receives some flow prior to triggering the ventilator, in contrast to pressure triggering, in which no flow is provided until the ventilator breath is triggered. Increasing the trigger sensitivity by decreasing the change in either pressure or flow needed to trigger an inspiration decreases the work of breathing. However, reducing the required pressure or flow excessively could result in accidental triggering and unwanted breaths by turbulence caused by condensation in the ventilator circuit, ET leaks, or cardiac oscillations.
Selection of Appropriate Inspiratory Time
The duration of TI should match the patient’s own inspiratory phase. If TI is too long, the patient’s drive to exhale may begin before the ventilator breath has cycled off. When this occurs, exhalation occurs against inspiratory flow and a closed exhalation valve, resulting in increased work of breathing, excessive rise in intrathoracic pressure, and discomfort. If TI is too short, the patient may be still inhaling without respirator support. In general terms, TI is usually initiated at 0.5-0.7 sec for neonates, 0.8-1 sec in older children, and 1-1.2 sec for adolescents and adults. Adjustments need to be made through individual patient observations and according to the type of lung disease present. In patients with severe lung disease (both obstructive and restrictive), unnatural TI and TE values may have to be selected, as discussed earlier. In such situations, adequate analgesia, sedation, and, in extreme cases, neuromuscular blockade may be needed.
Selection of Inspiratory Flow Pattern
In VCV, inappropriate flow may be another source of patient-ventilator dyssynchrony. After initiation of inspiration, if the set amount of flow is inadequate to meet patient demand, a state of “flow starvation” occurs, resulting in excessive work of breathing and discomfort. Such cases may require a decelerating inspiratory flow pattern, in which a higher flow is provided in the beginning of inspiration and less toward the end as the lungs fill up. On the other hand, such a pattern may be uncomfortable for a patient who desires more gradual alveolar filling. The selection of inspiratory flow pattern should be based on the individual patient’s respiratory mechanics. In PCV and PSV, the inspiratory rise time determines the manner in which the airway pressure is raised and tidal volume delivered. Considerations for choosing the appropriate rise time in PCV and PSV are similar to those for choosing the inspiratory flow pattern in VCV.
Use of Support Modes
As much as possible, a conscious patient should be allowed to have spontaneous breaths that are supported by either PSV or VSV. This approach minimizes the mandatory breaths generated by the ventilator that are beyond the patient’s control to modulate. Therefore, continued assessments should be made to determine whether the patient is able to maintain ventilatory requirements more in support modes and less in control modes.
Use of Sedation and Pharmacologic Paralysis
Having a conscious but comfortable patient is a desirable goal during mechanical ventilation. Spontaneous breaths with good muscle tone and presence of cough are important for adequate clearance of tracheobronchial secretions. The patient’s ability to indicate distress is also important in identifying and preventing potential injurious factors. In certain situations, management of patient-ventilator asynchrony assumes far greater importance when the asynchrony is causing unacceptable derangement of gas exchange and ventilator-induced lung injury. Both alveolar interstitial lung pathology and obstructive airway diseases may necessitate unnatural and uncomfortable settings for respiratory rate, TI, and inflation pressures. In such situations, deep sedation is often necessary. Benzodiazepines and opiates are the agents most commonly used for this purpose. In extreme situations, pharmacologic paralysis with a nondepolarizing agent such as vecuronium is required to abolish any patient effort and respiratory muscle tone. When pharmacologic paralysis is used, deep sedation must be ensured so that the patient does not sense pain and discomfort. Pharmacologic sedation and paralysis can ensure total control of the patient’s ventilation by mechanical means and may result in lifesaving improvement in gas exchange with reduction in inflation pressures. However, long-term use of such agents may be associated with undesirable consequences and higher morbidity. The risk of inadequate tracheobronchial secretions and atelectasis is potentially greater. Long-term use of pharmacologic sedation may be associated with chemical dependency and withdrawal manifestations, and prolonged neuromuscular blockade is associated with neuromyopathy in critically ill patients. The benefits of sedation and pharmacologic paralysis therefore should be carefully balanced with the risks, and periodic assessments should be made to determine the need for their continuation.
Monitoring Respiratory Mechanics
Exhaled Tidal Volume
Exhaled tidal volume (VTE) is measured by a pneumotachometer in the ventilator circuit during exhalation. In VCV, part of the machine-delivered volume may leak out during inspiration and therefore never reach the patient. Measurement of VTE more accurately describes the tidal volume that is contributing to the patient’s alveolar ventilation. In PCV, the VTE depends on the patient’s respiratory system compliance and resistance, and therefore offers valuable diagnostic clues. A decrease in VTE during PCV is indicative of either decrease in compliance or increase in resistance and is helpful in directing the clinician to appropriate investigation and management. An increase in VTE is indicative of improvement and may require weaning of inflation pressures to adjust the VTE.
Peak Inspiratory Pressure
In VCV and PRVC, the PIP is the secondary variable determined by the patient’s respiratory system compliance and resistance. An increase in PIP in these modes is indicative of decreased compliance (e.g., atelectasis, pulmonary edema, pneumothorax) or increased resistance (e.g., bronchospasm, obstructed ET). During VCV and PRVC, decreasing the respiratory rate or prolonging the TI will result in a lower PIP in patients with prolonged time constants because more time will be available for alveoli to fill. In such patients, a decrease in PIP suggests increased compliance or decreased resistance of the respiratory system.
Respiratory System Dynamic Compliance and Static Compliance
The changes in PIP during VCV and PRVC, and in VTE during PCV, are determined by CDYN of the respiratory system (lung and chest wall). Dynamic compliance is calculated as follows:
It takes into account both the flow-resistive and the elastic properties of the respiratory system. Changes in CDYN can be used to assess effects of different levels of PEEP as tidal ventilation is shifted along the slope of the volume-pressure curve (see Fig. 65-8). After an increase in PEEP in alveolar-interstitial diseases (increased elastance), an increase in CDYN suggests alveolar recruitment, whereas a decrease in CDYN may indicate overdistention. Similarly, in obstructive diseases (increased resistance), adjustment in PEEP levels to ameliorate airway collapse during exhalation can be guided by monitoring CDYN. To assess only the elastic recoil of the lung, measurement of CSTAT when there is no airflow is required. This measurement is performed by using an inspiratory hold maneuver with the patient under neuromuscular blockade and observing pressure-time and flow-time waveforms (Fig. 65-11). During this maneuver, inspiratory flow ceases while the expiratory valve continues to remain closed, thus allowing pressure to equilibrate throughout the ventilator circuit and the patient’s lungs. This pressure, referred to as the plateau pressure (Pplat), is reflective of alveolar pressure. CSTAT is calculated as follows:
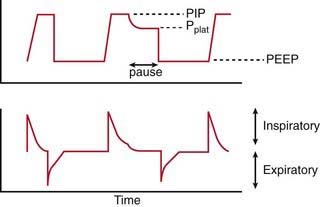
Figure 65-11 Alveolar pressure is best determined by measurement of plateau pressure (Pplat). Inspiration is paused for an extended period, and alveolar gas pressure is allowed to equilibrate with the ventilator circuit pressure. Airway pressure at the end of the inspiratory pause is Pplat. The difference between peak inspiratory pressure (PIP) and Pplat is to overcome flow-resistive properties of the lung, whereas Pplat reflects the pressure needed to overcome elastic properties of lung and chest wall.
The difference between CDYN and CSTAT is attributable to airway resistance. This difference is minimal in alveolar-interstitial diseases but substantial in airway obstruction.
Assessment of Auto-PEEP
Auto-PEEP is assessed with the use of an expiratory pause maneuver in which inspiration is delayed and alveolar pressure is allowed to equilibrate with the airway. In diseases with airway obstruction, insufficient alveolar emptying may occur if exhalation time is not adequate. The alveolar pressure in excess of the set PEEP at the completion of the expiratory pause is measured as auto-PEEP or intrinsic PEEP. Auto-PEEP can have adverse effects on ventilation and hemodynamic status. It can be managed by decreasing the respiratory rate or inspiratory time and thus allowing greater time for exhalation. Auto-PEEP may also be managed by increasing the set PEEP (“extrinsic” PEEP), thereby delaying airway closure during exhalation and improving alveolar emptying.
Assessment of Dead Space Ventilation
Positive pressure ventilation and application of PEEP may result in a decrease in venous return, cardiac output, and, therefore, also the pulmonary perfusion. Ventilation of poorly perfused alveoli results in dead space ventilation, which does not contribute to gas exchange. The dead space–tidal volume fraction can be calculated with the following equation:
Normal VD/VT is 0.33. Increased VD/VT is indicative of poorly perfused alveoli. Patients with increased VD/VT may require intravascular volume infusion or other means of augmenting the cardiac output to improve pulmonary perfusion. The VD/VT fraction is calculated and displayed by commercially available capnographs, which measure endotracheal PCO2 continuously.
Ventilator-Induced Lung Injury
Like most medical therapies, mechanical ventilation can be harmful if appropriate principles are not followed. Lung volumes that are too high or too low should be avoided. In attempting to recruit and maintain FRC, the clinician must be careful not to overdistend alveoli. Excessive PIP and VT can lead to unwelcome stress and strain on alveolar walls. This volutrauma and barotrauma can lead to disruption of tight junctions between alveolar epithelial and capillary endothelial cells, causing fluid and protein transudation in the alveoli. Inflammatory mediators and cytokines are released, exacerbating the injury and promoting exudative fluid formation. Decreased production and inactivation of surfactant result in atelectasis and further impairment of gas exchange. Evidence shows that in patients with severe acute hypoxemic respiratory failure, avoidance of VT ≥ 10 mL/kg and Pplat ≥ 30 cm H2O limits diffuse alveolar damage.
Insufficient PEEP is another important mechanism of ventilator-induced lung injury. Alveoli that are recruited during inspiration must remain open during expiration; if they do not, atelectrauma occurs, which is defined as undesirable shear stress on alveolar walls as they are opened and closed repeatedly. Therefore, the ideal PEEP for a patient should maximize the number of open alveoli and minimize the number of overdistended alveoli. Careful adjustments of PEEP may also permit the clinician to wean a patient from a high inspired oxygen concentration, another potential source of lung injury (oxytrauma). Though most patients receive an inspired oxygen concentration of 100% during endotracheal intubation and at the beginning of mechanical ventilation, increasing PEEP to recruit alveoli without overdistention should be quickly instituted to improve oxygenation and permit weaning of the FIO2. Although an FIO2 value below which there is no risk of oxygen toxicity is unknown, most clinicians aim for a value <0.6.
Ventilator-Associated Pneumonia
The pathophysiology of ventilator-associated pneumonia (VAP) is multifactorial. Aspiration of oral and/or gastric secretions, colonization of ETs, and suppression of cough reflexes with sedation all play a role. New-onset fever and leukocytosis accompanied by demonstration of an infiltrative process by chest radiographs are consistent with a diagnosis of VAP. This complication can lead to worsened gas exchange, increased duration of ventilation, and even death. Elevation of the head of the bed to 30 degrees after initiation of mechanical ventilation and use of a protocol for oral decontamination during mechanical ventilation are two means of reducing the risk for VAP. The most effective strategy to minimize any of the aforementioned complications is regular assessment of extubation readiness and liberation from mechanical ventilation as soon as clinically possible.
Weaning
Weaning from mechanical ventilation should be considered as a patient’s respiratory insufficiency begins to improve. Most pediatricians favor gradual weaning from ventilator support. With SIMV, the ventilator rate is slowly reduced, allowing the patient’s spontaneous breaths (typically assisted with pressure or volume support) to assume a larger proportion of the minute ventilation. When the ventilator rate is low (<5 breaths/min) such that its contribution to minute ventilation is minimal, assessment of extubation readiness is performed. An alternative method of gradual weaning is transition to a pressure support mode of ventilation. In this mode, no ventilator rate is set, allowing all triggered breaths to be assisted with pressure support. The clinician reduces the pressure support slowly to a low value (<5-10 cm H2O), at which point assessment of extubation readiness is performed. During either technique, weaning should be halted if tachypnea, increased work of breathing, hypoxemia, hypercapnia, acidosis, diaphoresis, tachycardia, or hypotension occurs.
The most objective means of assessing extubation readiness is a spontaneous breathing trial (SBT). Prior to performance of an SBT, a patient should be awake with intact airway reflexes, capable of handling oropharyngeal secretions, and with stable hemodynamic status. In addition, gas exchange should be adequate, defined as a PaO2 >60 mm Hg while receiving an FIO2 <0.4 and PEEP ≤5 cm H2O. If these criteria are present, a patient should be started on CPAP with minimal or no pressure support (≤5 cm H2O). If this SBT is tolerated with no episodes of respiratory or cardiovascular decompensation, successful extubation is likely. Some neonates and small children cannot be calmed or consoled long enough to complete the SBT. In this situation, extubation readiness must be assessed on a low level of ventilator support. Data suggest that there is a low risk of extubation failure if the patient is comfortable and has stable hemodynamic status with adequate gas exchange and spontaneous VT >6.5 mL/kg while receiving <20% of total minute ventilation from the ventilator. Certain patient populations are at increased risk for extubation failure, such as young infants, children mechanically ventilated for >7 days, and patients with chronic respiratory or neurologic conditions. These children often benefit from transition to a noninvasive form of positive pressure ventilation (e.g., high-flow nasal cannula, CPAP, or BiPAP) delivered via nasal prongs or face mask to increase the odds of successful extubation. The likelihood of postextubation upper airway obstruction, the most common cause of extubation failure in children, cannot be predicted on the basis of an SBT result or bedside measurements of physiologic variables. Traumatic endotracheal intubation and subglottic swelling from the ET irritation, especially in patients who exhibit agitation while receiving mechanical ventilation, are common causes of airway narrowing after extubation. Administration of intravenous corticosteroids (dexamethasone 0.5 mg/kg every 6 hours for 4 doses prior to extubation) has been shown to minimize the incidence of postextubation airway obstruction. In patients in whom postextubation airway obstruction develops, the need for re-intubation may be obviated by administration of nebulized racemic epinephrine and helium-oxygen mixture.
Albuali WH, Singh RN, Frasier DD, et al. Have changes in ventilation practices improved outcome in children with acute lung injury? Pediatr Crit Care Med. 2007;8:324-330.
Brower RG, Lanken PN, MacIntyre N, et al. National Heart, Lung, and Blood Institute ARDS Clinical Trials Network: Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351:327-336.
Campbell RS, Davis BR. Pressure-controlled versus volume-controlled ventilation: does it matter? Respir Care. 2002;47:416-424.
Greenough A, Dimitriou G, Prendergast M, et al: Synchronized mechanical ventilation for respiratory support in newborn infants, Cochrane Database Syst Rev (1):CD000456, 2008.
Marraro GA. Innovative practices of ventilatory support with pediatric patients. Pediatr Crit Care Med. 2004;4:8-17.
Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome. JAMA. 2008;299:637-645.
Mercat A, Richard JCM, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome. JAMA. 2008;299:646-654.
Newth CJ, Venkataraman S, Willson DF, et al. Weaning and extubation readiness in pediatric patients. Pediatr Crit Care Med. 2009;10:1-11.
Papazian L, Forel JM, Gacouin A, et al: Neuromuscular blockers in early acute respiratory distress syndrome, N Engl J Med 363(12):1107–1116.
Pearse RM, Young JD. Steroids to prevent postextubation laryngeal oedema. Lancet. 2007;369:1060-1061.
Pinhu L, Whitehead T, Evans T, et al. Ventilator-associated lung injury. Lancet. 2003;361:332-340.
Priestley MA, Helfaer MA. Approaches in the management of acute respiratory failure in children. Curr Opin Pediatr. 2004;16:293-298.
Randolph A. Management of acute lung injury and acute respiratory distress syndrome in children. Crit Care Med. 2009;37:2448-2454.
Sarnaik AP, Daphtary K, Meert KL, et al. Pressure controlled ventilation in children with status asthmaticus. Pediatr Crit Care Med. 2004;5:133-138.
Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomized controlled trial. Lancet. 2009;373:1874-1882.
Srinivasan R, Asselin J, Gildengorin G, et al. A prospective study of ventilator-associated pneumonia in children. Pediatrics. 2009;123:1108-1115.
65.2 Long-Term Mechanical Ventilation
Technology has made mechanical support possible for patients with chronic disorders in various settings outside the intensive care unit (ICU), allowing such patients to live fulfilling lives and even improving their chances of survival. Although short-term mechanical ventilation has allowed many children to survive and to be weaned from life-sustaining therapies, it has also led to an increase in the number of patients who are chronically dependent on technology for survival.
Goals of Long-Term Mechanical Ventilation
The goals of home mechanical ventilation, based on 2007 American Association of Respiratory Care (AARC) guidelines, are to: sustain and extend life, enhance quality of life, reduce morbidity, enhance growth and development, and provide cost-effective care. Limitations on the use of home mechanical ventilation include FIO2 requirement of >0.40, positive end-expiratory pressure >10 cm H2O, inadequate interface (i.e., tracheostomy or noninvasive mask), lack of appropriate discharge plan, and inadequacy of finances, infrastructure, or personnel in the home environment.
The goals should be both optimistic and realistic, and they should be individualized for a given situation. Optimism provides hope and enthusiasm for the care providers, whereas realism avoids unreasonable expectations, unnecessary treatment interventions and pain, as well as disappointment and feelings of anger and hostility. Expected outcomes may range from long-term recovery and liberation from respiratory support to improved patient comfort and a rewarding existence with continued dependence on technology. Patients in whom long-term support of respiration is intended to be a bridge to complete recovery and independence include those with reversible neuropathies, bronchopulmonary dysplasia and pulmonary hypertension, airway abnormalities, and congenital heart disease before or after surgical intervention. Patients for whom the use of long-term respiratory support is intended to prevent morbidity and to allow them to live longer and fulfilling lives include those with congenital myopathies and neuropathies, obstructive sleep apnea, and progressive lung disease.
Patient Selection and Ethical Considerations
There are several incentives to provide long-term mechanical ventilation to children with chronic respiratory failure at home instead of in the hospital. The cost of home care for these children is significantly less than that of hospital care. The avoidance of hospital-acquired infections and the developmental and psychological benefits of living at home are increasingly recognized. Children who are managed at home become integral parts of their families and may even go to school, participate in social functions, and live near-normal lives. Patients selected for long-term respiratory support either have chronic persistent life-threatening respiratory failure or are at risk for acute deterioration.
Indications
Optimal patient selection for home mechanical ventilation requires identification of the cause of chronic respiratory failure and awareness of the long-term outlook for the patient. Many of the causative conditions have the potential to improve with therapy, time, growth, or age. Some are amenable to surgical correction and have the potential for weaning of the patient from mechanical ventilation after an appropriate intervention is performed. Conditions requiring long-term respiratory support may involve a primary pulmonary parenchymal or airway pathology, neuromuscular or musculoskeletal abnormality, or inadequate CNS control of the respiratory system. In some cases, home mechanical ventilation is indicated to prevent the development of pulmonary hypertension and cor pulmonale from chronic hypoxic pulmonary vasoconstriction (bronchopulmonary dysplasia, obstructive sleep apnea). Other candidates for home ventilation include patients with cardiopulmonary or airway problems who are able to sustain oxygenation and ventilation but are not thriving because of excessive caloric expenditure from increased work of breathing. Tachypnea can also negatively affect oral feeding in infants, further compromising the positive caloric balance needed for growth. This scenario is very common in patients with bronchopulmonary dysplasia and congenital heart disease. Some conditions that cause chronic respiratory failure are slowly progressive and/or irreversible; some patients with these conditions are still excellent candidates for home ventilation. Many children with spinal cord injuries, muscular dystrophy, and type II spinal muscular atrophy enjoy excellent quality of life with long-term ventilation, and some have even graduated from college and become productive members of society. The type of respiratory support needs to be tailored to the individual patient’s needs and resources. Availability of resources may depend on local conditions. Also, treatment philosophy and outcome goals vary from patient to patient (Table 65-9).
Conditions for Which Long-Term Ventilation May Be Inappropriate
The decision to employ long-term ventilation must be made judiciously and carefully, weighing the harms against the benefits of the intervention. If the patient has no capacity to participate even minimally in the human experience (e.g., persistent vegetative state, trisomy 18), the harm of continued technologic intervention is unjustified, carrying with it only prolongation of pain and suffering with no net benefit to the patient. Such a patient may have enough rudimentary brain function to sense pain and discomfort. Similarly, patients with rapidly progressive neurodegenerative disease (e.g., Werdnig-Hoffman disease) experience severe weakness and are unable to move, but are able to mentally process every noxious stimulus. Subjecting such patients to long-term ventilation would cause unjustified harm with no long-term benefit; instead, compassionate palliative care should be the goal in such individuals. Although the individual patient’s interest is of the utmost importance, adverse effects on family dynamics, allocation of scarce resources, and economic costs to society are also important considerations.
In-Hospital Management and Discharge Planning
Optimal care of children with chronic respiratory failure begins in the hospital. As soon as the child is identified as one who may need long-term ventilation, there should be open communication between the physician and the family. Many families need time to accept the fact that their children will require therapies at home. Taking the child home for the first time after a prolonged hospital course marks a tremendous life change for the family and often causes emotional and financial strain. The family often needs time to get affairs in order, such as to secure time off from work and to arrange for help in caring for the child and payment for medical care. Because these tasks take time, the planning process must start as early as possible so that the discharge process is organized and expeditious. Ideally, the decision to initiate home mechanical ventilation is made electively. In patients whose neuromuscular weakness is slowly progressive, indicating impending respiratory failure, it would not be beneficial to wait for an episode of acute respiratory failure. This can lead to prolonged hospital and ICU stays and greater morbidity, because these patients are often debilitated from their acute illness. Similarly, physicians should be proactive in initiating mechanical ventilation in a patient who would benefit from its positive effects on caloric balance, instead of waiting until the child fails to thrive. In most children with neuromuscular diseases, home mechanical ventilation is initiated nonelectively, after an acute episode of respiratory failure, and without prior effective discussions of available options. Because these children often have several preceding hospitalizations for episodes of acute respiratory failure, it is evident that health care providers are missing opportunities to adequately prepare their families.
If the best interface for mechanical ventilation is a tracheostomy, a pediatric otolaryngologist must be consulted for the surgical procedure. If the child is not likely to be able to meet caloric demands for growth with oral feeding, a pediatric surgeon is usually consulted for placement of a gastrostomy tube, and the procedure is often performed at the same time as the tracheostomy. Observation in the ICU for approximately 5 days is usually required to allow the tract of the tracheostomy to mature, at which point the tracheostomy tube is replaced.
Team Structure for Home Mechanical Ventilation Program
For optimal management of the child undergoing home mechanical ventilation, a comprehensive, multidisciplinary approach at a tertiary care center is required (Table 65-10). Indeed, in these cases, life-sustaining therapies are being delivered outside the ICU and often outside the hospital. Several disciplines of health care provision must be involved, and the family must be thoroughly trained to ensure the safety, growth, psychosocial development, and possible clinical improvement of the child.
Table 65-10 TEAM APPROACH TO INSTITUTIONAL HOME VENTILATION PROGRAM
| TASK | PERSON(S) INVOLVED |
|---|---|
| Decision to institute long-term ventilation | Family, intensivist/neonatologist, pulmonologist |
| In-hospital management | Intensivist/neonatologist |
| Assuming overall leadership of long-term care | Pulmonologist or other qualified physician |
| Medical/surgical issues | Otolaryngologist, general surgeon, neurologist, neurosurgeon, craniofacial surgeon |
| Training: Suctioning, tracheostomy care, ventilator function and trouble shooting | Respiratory therapist, nurse, medical equipment company, family |
| Arranging financial and nursing resources | Social worker |
| Assessment of nutrition, feeding, speech | Dietician, occupational/speech therapist |
| Primary care: Immunization, growth and development assessment | Primary care physician or pulmonologist |
| Home medication instructions | Pharmacist, nurse, physician |
| Follow-up regarding ventilator adjustments | Pulmonologist |
| Assessment of home suitability | Medical equipment company |
| Home care | Family, home health nursing company |
The team of physicians who will follow a child as an outpatient must become involved while the child is still in the hospital. The primary inpatient physician is usually an intensivist or a neonatologist. A physician leader (usually a pulmonologist) must be identified who is well versed in managing such children and organizing community resources, and who will direct long-term care while remaining in close communication with the family. This arrangement will allow for home ventilator settings to be established and documented before hospital discharge, and long-term reduction of or weaning from mechanical ventilation on an outpatient basis. In many cases, the pulmonologist also serves as the primary care physician, overseeing the child’s immunizations, growth, development, and other medical issues. If the family lives far from a tertiary care center, a primary care physician who is willing and qualified to care for the child must be chosen and communicated with prior to the patient’s discharge. Even in this situation, a follow-up appointment with a pediatric pulmonologist is required.
It cannot be stressed enough how dangerous it would be for a child to receive life-sustaining therapies at home without thorough training of the family, which includes use and troubleshooting of all of the medical equipment, recognition of signs of worsening illness, and cardiopulmonary resuscitation (CPR). Training should begin well in advance of hospital discharge. Generally, a respiratory therapist is responsible for teaching the family how to suction the airway, to change the tracheostomy tube both routinely and emergently, and to connect, use, and troubleshoot the ventilator and oxygen supply. A child who would die without an artificial airway should never be left alone without someone who knows how to change the tube. A dietary plan should be in place prior to hospital discharge, with the child demonstrating tolerance of calories adequate to sustain growth. This may require consultation with occupational or speech therapists to evaluate adequacy of oral feeding skills and with a nutritionist to establish follow-up and adjustment of enteral feeding after discharge.
A social worker should also be involved early in the discharge process to assess the adequacy of the social environment and infrastructure in the home. The family should demonstrate a clear understanding of a daily, weekly, and monthly schedule with respect to home nursing and care of the child. Depending on the complexity of the child’s needs, or the work schedules of the family, home nursing may be needed every day. This need requires identification of a home nursing company able to meet these personnel demands, which is difficult in some cases. Arrangements with the health insurance company should also be made, to avoid any delays in hospital discharge. Also, all necessary equipment must be ordered in advance from the medical equipment company.
Follow-up plans with these disciplines and organizations, as well as with services managing the child’s other chronic problems, must be made prior to hospital discharge. Ideally, the physician leader would work with the other specialists in a multidisciplinary clinic where other children requiring such care are managed. This arrangement would streamline the care of the child as well as make it more convenient for the family, because transporting such children is very difficult and sometimes even requires an ambulance service. Another approach to address the multidisciplinary needs of a patient, especially one who lives far from the tertiary care center, would be regularly scheduled, short-term hospitalizations every 6-12 months. Such an arrangement would allow for overnight monitoring and adjustment of ventilator settings, if needed, as well as a multidisciplinary assessment, including nutrition, growth, and development.
A well-thought-out plan for emergency care must be established in advance. This process involves interaction with local emergency medical services and emergency departments. Many of the patients requiring long-term ventilation have unique characteristics. A patient with myelomeningocele, for example, may require emergency evaluation of a ventriculoperitoneal shunt, whereas one with a single-ventricle lesion may have special requirements or restrictions for intravascular fluid expansion, oxygen administration, and alveolar inflation pressures. It is useful to have the family always carry a document containing a brief summary of the patient’s clinical characteristics and resuscitation requirements along with contact information for subspecialists. Similarly, families of patients who have prepared to forgo resuscitation in their final days of life should have an advanced directive or resuscitation instructions in their possession so that inappropriate and undignified interventions are avoided.
Methods of Long-Term Mechanical Ventilation
Respiratory Support at Home Through Tracheostomy Interface
Positive pressure ventilation through a tracheostomy is the most commonly employed method of providing home mechanical ventilation. Tracheostomy gives the patient a stable airway for reliable delivery of tidal volume and affords better pulmonary toilet and clearance of secretions. Sudden death can occur from displacement or obstruction of the tracheostomy or from unrecognized disconnection from the ventilator. To ensure patient safety, suctioning equipment and an extra tracheostomy tube should always be immediately available, as well as someone proficient in changing the tube, troubleshooting the equipment, and performing CPR.
The versatility of home ventilators has enabled clinicians to tailor settings to the patient’s needs. These features include constant-flow generators, pressure support, flow triggering, and variable rise time adjustment. A leak around the tracheostomy tube is desirable if tolerated by the patient, because it is beneficial for speech development and leads to less irritation of the trachea. Traditional volume-control ventilators cannot provide a consistent minute ventilation with a leak around the tracheostomy, because the degree of leak is often variable and dependent on positioning. Pressure-control ventilators can provide consistent minute ventilation because of leak compensation. The ideal home ventilator is also portable, lightweight, and user-friendly. Alarms for high pressure, low exhaled volume, and patient disconnection should be loud enough to alert the caregiver to an adverse event, with minimal occurrences of false alarms. The primary power source for home ventilators is alternating current (AC). Most models have an internal battery that charges during AC operation and will provide a power source for up to 4 hr when disconnected from the outlet. Oxygen delivery at home is usually in the form of a concentrator, which is limited to a maximum flow rate of 6 L/min.
Noninvasive Home Ventilation
The primary benefit of noninvasive ventilation for respiratory failure in children is avoiding a tracheostomy, which carries risks of tracheal stenosis, tracheitis, and ventilator-associated pneumonia as well as social stigma. Some patients are able to maintain adequate airway patency, oxygenation, and ventilation while awake but need positive pressure ventilation at night because of a decrease in airway tone or respiratory muscle excursion. This subset of patients includes those with obstructive sleep apnea, cystic fibrosis, and neuromuscular disorders.
Appropriate fit of the interface is extremely important, to minimize leaks and discomfort. Interfaces include nasal masks, facial masks covering the nose and mouth, nasal pillows, and mouthpieces. It is important for the child to tolerate and receive time free of mechanical ventilation to avoid facial skin and nasal bridge breakdown, as well as to vent the stomach if necessary. Initiation of the chosen interface method should occur in the inpatient setting, and the patient’s tolerance of it must be demonstrated prior to hospital discharge. Ventilators to deliver noninvasive positive pressure ventilation (NIPPV), CPAP or BiPAP machines, are often different from those used in the ICU and invasive home ventilators. CPAP provides airflow at the same level of pressure during inhalation and expiration to keep the airways open throughout the respiratory cycle. Patients eligible for this therapy include those with obstructive sleep apnea, lower airway disease such as tracheomalacia or bronchomalacia, and milder degrees of neuromuscular disease. Patients with more advanced neuromuscular disease may lack the capacity for the respiratory muscle excursion needed for inspiration and would benefit from a higher pressure during inspiration, which can be provided with BiPAP. In the spontaneous BiPAP mode, the difference in pressure between inspiration and expiration is analogous to pressure support in traditional ICU ventilators. Alternatively, BiPAP may be time-cycled to deliver mandatory breaths. One major disadvantage of NIPPV is its impact on airway clearance. It is difficult for patients receiving continuous positive pressure to cough and clear secretions, especially in a weakened state. Secretions may also be forced further down the bronchial tree by the positive pressure. For this reason, patients may benefit from adjunctive airway clearance therapies, such as cough-assistor devices, chest vest vibration, and intermittent positive pressure breathing.
High-flow nasal cannula systems are capable of delivering airflow from 2 to 8 L/min with adequate heat and humidity so as to minimize injury to the respiratory tract. The use of high-flow nasal cannula has increased over the last decade and has been well-studied in the neonatal population. It has been demonstrated in the neonatal population to provide positive distending pressure of 4-5 cm H2O and respiratory support comparable to that of nasal CPAP. One drawback to this therapy is the variability of the amount of pressure generated, which depends on the fit of the prongs, the flow rate, and the open or closed position of the mouth. In contrast, CPAP devices provide a tight seal and a pressure-release valve to limit the pressure. Therefore, to minimize the risk of excessive pressure, it may be beneficial to choose the smallest high-flow nasal cannula required to provide enough support to the patient.
Diaphragm Pacing
Patients with congenital central hypoventilation syndrome or high cervical spinal cord injury may benefit from electrical stimulation of the phrenic nerves to pace the diaphragm. A surgical procedure is required to implant receivers adjacent to the phrenic nerves, usually bilaterally, and the patient wears a radiofrequency transmitter. The primary benefit of this mode of ventilation is that the transmitter is small and portable enough to give the patient more mobility and freedom from the ventilator for prolonged periods. Risks include diaphragm fatigue, injury to the phrenic nerve from repeated stimulation, and extrathoracic airway obstruction. Because of these concerns, diaphragm pacing is not continuous in most patients, thus requiring CPAP or mechanical ventilation during sleep.
AARC, Respiratory Home Care Focus Group. AARC Clinical Practice Guideline: Long-term invasive mechanical ventilation in the home—2007 revision & update. Respir Care. 2007;52:1056-1062.
Eigen H, Zander J. Home mechanical ventilation of pediatric patients. American Thoracic Society. Am Rev Respir Dis. 1990;141:258-259.
Kacmarek RM, Steven D, Mack CW. Home respiratory care and mechanical ventilation: the essentials of respiratory care. St Louis: Elsevier/Mosby; 2005. pp 569–589
MacDuff A, Grant IS. Critical care management of neuromuscular disease including long-term ventilation. Curr Opin Crit Care. 2003;9:106-112.
Ottonello G, Ferrari I, Pirroddi IMG, et al. Home mechanical ventilation in children: retrospective survey of a pediatric population. Pediatr Int. 2007;49:801-805.
Robert D, Argaud L. Clinical review: long-term noninvasive ventilation. Crit Care. 2007;11:210-230.
Sarnaik AP, Daphtary K, Sarnaik AA. Ethical issues in pediatric intensive care in developing countries: combining western technology and eastern wisdom. Indian J Pediatr. 2005;72:339-342.
Simmonds AK. Home ventilation. Eur Respir J. 2003;22(Suppl 47):38S-46S.
Sritippayawan S, Kun SS, Keens TG, et al. Initiation of home ventilation in children with neuromuscular diseases. J Pediatr. 2003;142:481-485.