Chapter 121 Neutrophils
The Phagocytic Inflammatory Response
The phagocyte system includes both granulocytes (neutrophils, eosinophils, and basophils) and mononuclear phagocytes (monocytes and tissue macrophages). Neutrophils and mononuclear phagocytes share primary functions, including the defining properties of large particle ingestion and microbial killing. Phagocytes participate primarily in the innate immune response but also help initiate acquired immunity. Mononuclear phagocytes, including tissue macrophages and circulating monocytes, are discussed in Chapter 122.
Neutrophils provide the rapid effector arm of the innate immune system. They circulate in the bloodstream for only about 6 hr (Table 121-1), but upon encountering specific chemotactic signals, they adhere to the vascular endothelium and transmigrate into tissues, where they ingest and kill microbes and release chemotactic signals to recruit more neutrophils and to attract dendritic cells and other initiators of the acquired immune response.
Table 121-1 NEUTROPHIL AND MONOCYTE KINETICS
| NEUTROPHILS | |
| Average time in mitosis (myeloblast to myelocyte) | 7-9 day |
| Average time in postmitosis and storage (metamyelocyte to neutrophil) | 3-7 day |
| Average half-life in the circulation | 6 hr |
| Average total body pool | 6.5 × 108 cells/kg |
| Average circulating pool | 3.2 × 108 cells/kg |
| Average marginating pool | 3.3 × 108 cells/kg |
| Average daily turnover rate | 1.8 × 108 cells/kg |
| MONONUCLEAR PHAGOCYTES | |
| Average time in mitosis | 30-48 hr |
| Average half-life in the circulation | 36-104 hr |
| Average circulating pool (monocytes) | 1.8 × 107 cells/kg |
| Average daily turnover rate | 1.8 × 109 cells/kg |
| Average survival in tissues (macrophages) | Months |
From Boxer LA: Function of neutrophils and mononuclear phagocytes. In Bennett JC, Plum F, editors: Cecil textbook of internal medicine, ed 20, Philadelphia, 1996, WB Saunders.
Hematopoiesis
The hematopoietic progenitor system can be envisioned as a continuum of functional compartments with the most primitive compartment composed of very rare pluripotential stem cells, which have high self-renewal capacity and give rise to more mature stem cells, including cells that are committed to either lymphoid or myeloid development (Fig. 121-1). Common lymphoid progenitor cells give rise to T- and B-cell precursors and their mature progeny (Chapter 117). Common myeloid progenitor cells eventually give rise to committed single-lineage progenitors of the recognizable precursors through a random process of lineage restriction in a stepwise process (Chapter 440). The capacity of lineage-specific committed progenitors to proliferate and differentiate in response to demand provides the hematopoietic system with a remarkable range of response to changing requirements for mature blood cell production.
The proliferation, differentiation, and survival of immature hematopoietic progenitor cells are governed by hematopoietic growth factors (HGFs), a family of glycoproteins (Chapter 440). Besides regulating proliferation and differentiation of progenitors, these factors influence the survival and function of mature blood cells. During granulopoiesis and monopoiesis, multiple cytokines regulate the cells at each stage of differentiation from pluripotent stem cells to nondividing terminally differentiated cells (monocytes, neutrophils, eosinophils, and basophils). As cells mature, they lose receptors for most cytokines, especially those that influence early cell development; however, they retain receptors for cytokines that affect their mobilization and function, such as granulocyte colony–stimulating factor (G-CSF) and macrophage colony–stimulating factor (M-CSF). Mature phagocytes also express receptors for chemokines, which help direct the cells to sites of inflammation. Chemokine receptors such as CXCR4 and its ligand SDF-1 play a key role in retention of developing myeloid cells within bone marrow.
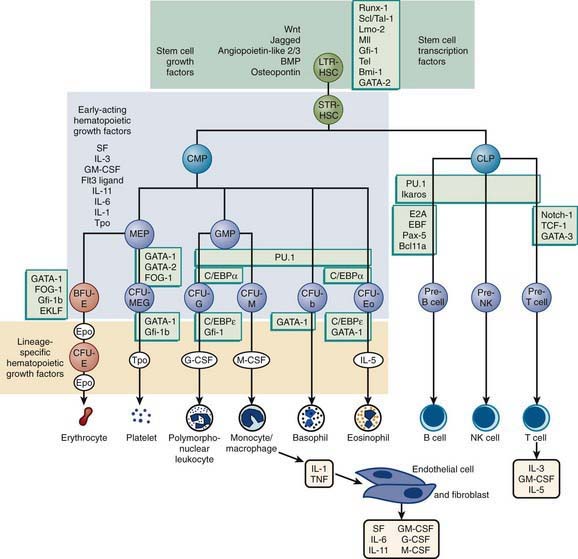
Figure 121-1 Major cytokine sources and actions and transcription factor requirements. Cells of the bone marrow microenvironment such as macrophages, endothelial cells, and reticular fibroblastoid cells produce macrophage colony–stimulating factor (M-CSF), granulocyte-macrophage colony–stimulating factor (GM-CSF), granulocyte colony–stimulating factor (G-CSF), interleukin (IL) 6, and probably Steel factor (SCF) after induction with endotoxin (macrophage) or IL-1/ tumor necrosis factor (TNF) (endothelial cells and fibroblasts). T-cells produce IL-3, GM-CSF, and IL-5 in response to antigenic and IL-1 stimulation. These cytokines have overlapping actions during hematopoietic differentiation, as indicated, and for all lineages optimal development requires a combination of early- and late-acting factors. Transcription factors important for survival or self-renewal of stem cells are shown at the top (light green panel) and stages of hematopoiesis blocked after the depletion of indicated transcription factors for multipotent and committed progenitors are shown in light green boxes throughout. PSC, pluripotent stem cells; MSC, myeloid stem cells; CFU-E/b/M, erythrocyte, basophil, and megakaryocyte colony–forming unit; CFU-E, erythroid colony–forming unit; CFU-G, granulocyte colony–forming unit; CFU-M, macrophage colony–forming unit; CFU-Eo, eosinophil colony–forming unit; NK, natural killer.
(From Nathan DG, Orkin SH, Ginsburg D, et al, editors: Nathan and Oski’s hematology of infancy and childhood, ed 7, Philadelphia, 2009, Saunders.)
Neutrophil Maturation and Kinetics
The process of intramedullary granulocyte maturation involves changes in nuclear configuration and accumulation of specific intracytoplasmic granules. The bone marrow microenvironment supports the normal steady-state renewal of peripheral blood neutrophils through the generation of growth and differentiation factors by stromal cells. Growth factors such as G-CSF and GM-CSF not only stimulate cell division, but also induce the expression of transcription factors that regulate the biosynthesis of functional components of the neutrophil, such as granule proteins. The transcription factor PU.1 is essential for myelopoiesis, both as a positive regulatory element and as a suppressor of GATA-1, a transcription factor that directs nonmyeloid differentiation. Other transcription factors such as Runx1 (AML1), c-myb, CDP, C/EBPα, C/EBPγ, and MEF are expressed in the myeloblast and promyelocyte, and some of these are required for azurophil granule protein expression. As cells enter the myelocyte stage, RUNX1 and myb are downregulated, whereas PU.1 and C/EBPε expression rises to initiate terminal differentiation.
Granulocytes survive for only 6-12 hr in the circulation, and therefore daily production of 2 × 104 granulocytes/µL of blood is required to maintain a level of circulating granulocytes of 5 × 103/µL (see Table 121-1). The relatively small peripheral blood pool includes the rapidly interchanging circulating and marginating pools; the latter provides entrance into the tissue phase, where neutrophils may survive for hours or days. The circulating pool is fed and buffered by a much larger marrow population of mature neutrophils and myeloid precursors, representing the marrow reserve and proliferating pools, respectively. Proliferation of myeloid cells, encompassing approximately 5 mitotic divisions, takes place only during the 1st 3 stages of neutrophil development, in myeloblasts, promyelocytes, and myelocytes. After the myelocyte stage, the cells terminally differentiate into nondividing, maturing metamyelocytes, bands, and neutrophils.
Neutrophil maturation is associated with nuclear condensation and lobulation and with the sequential production of characteristic granule populations. A myeloblast is a relatively undifferentiated cell with a large oval nucleus, a sizeable nucleolus, and a deficiency of granules. Promyelocytes acquire peroxidase-positive azurophilic (primary) granules, and then myelocytes and metamyelocytes acquire specific (secondary) granules; tertiary granules and secretory vesicles develop in the final stage of neutrophil maturation.
Neutrophil Function
Neutrophil responses are initiated as circulating neutrophils flowing through the postcapillary venules detect low levels of chemokines and other chemotactic substances released from a site of infection. These soluble effectors of inflammation trigger subtle changes in the array and activity of surface molecules on both endothelial cells and neutrophils. The initial associations are low affinity, reversible, and mediated primarily by selectin-carbohydrate interactions. This leads to leukocyte rolling, in which loose adhesions are made and broken, causing neutrophils to move reversibly along the endothelial surface. The rolling of neutrophils allows more intense exposure of neutrophils to activating factors such as tumor necrosis factor (TNF) or IL-1 (Fig. 121-2). Neutrophil activation leads to induction of qualitative and quantitative changes in the family of β2 integrin adhesion receptors (the CD11/CD18 group of surface molecules), leading to tight heterotypic adhesion between neutrophils and endothelial cells and homotypic adhesion of neutrophils with each other. The net result of these interdependent intercellular interactions is that neutrophils flatten onto the endothelial cells, while neutrophil/neutrophil and neutrophil/platelet aggregates partially occlude the venule and reduce blood flow.
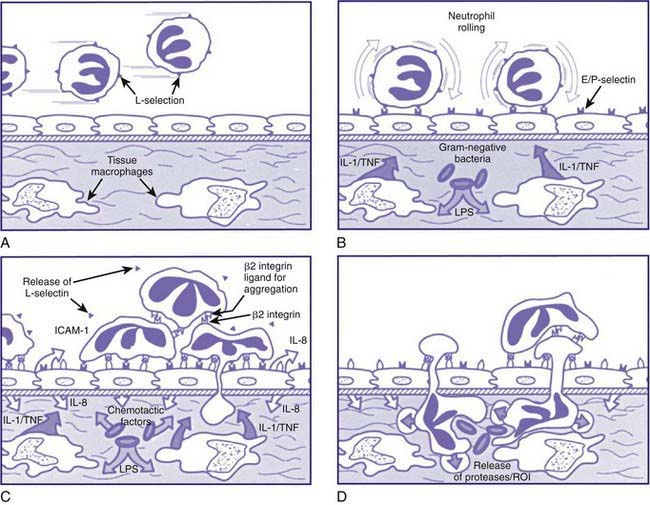
Figure 121-2 The neutrophil-mediated inflammatory response. A, Unstimulated neutrophils (expressing L-selectin) entering a postcapillary venule. B, Invasion of gram-negative bacteria with release of lipopolysaccharide stimulates tissue macrophages to secrete inflammatory monokines, interleukin 1 (IL-1), and tumor necrosis factor (TNF), which, in turn, activate endothelial cells to express E- and P-selectins. E- and P-selectins serve as counter receptors for neutrophils sialyl Lewis X and Lewis X to cause low-avidity neutrophil rolling. C, Activated endothelial cells express ICAM-1, which serves as a counter-receptor for neutrophil β2 integrin molecules, leading to high-avidity leukocyte spreading and the start of transendothelial migration. Transendothelial migration of activated neutrophils is stimulated by chemotactic factors such as endothelial cell–derived IL-8 and formylated bacterial factors. Chemoattractants promote neutrophil activation with release of L-selectin and an increase in β2 integrin affinity for ICAM-1 and for other counter-receptors promoting intravascular and neutrophil aggregation. D, Neutrophils invade through the vascular basement membrane with the release of proteases and reactive oxidative intermediates, causing local destruction of surrounding tissue at sites of high concentrations of chemotactic factors.
(From Smolen JE, Boxer LA: Functions of neutrophils. In Williams WJ, Beutler E, Erslev AJ, et al, editors: Hematology, ed 5, New York, 1994, McGraw-Hill, with permission of The McGraw-Hill Companies.)
The next phase involves loosening of the integrin adhesion through the process of mobilizing integrin receptors to the trailing pseudopod of the neutrophil. The neutrophil is able to displace its integrin receptors and undergo conformational changes, allowing it to migrate between endothelial cell junctions into the extravascular tissue. Once through the endothelium, the neutrophil senses the gradient of chemokines or other chemoattractants and migrates to sites of infection. Neutrophil migration is a complex process involving rounds of receptor engagement, signal transduction, and remodeling of the actin-microfilaments composing in part the cytoskeleton. Additionally, secretion of specific granules or related secretory vesicular elements containing gelatinase, heparinase, and other enzymes allows the neutrophil to cross the basement membrane and transit through connective tissues. When the neutrophil reaches the site of infection, it recognizes pathogens by means of Fc immunoglobulin and complement receptors, Toll-like receptors, fibronectin receptors, and other adhesion molecules.
The neutrophil ingests microbes that are opsonized (prepared for ingestion) by opsonins, serum proteins such as immunoglobulin and complement component C3. The opsonins facilitate phagocytosis, in which the pathogens are engulfed into a closed vacuole, the phagosome (Fig. 121-3). As phagocytosis proceeds, two cellular responses essential for optimal microbicidal activity occur concomitantly: degranulation and activation of nicotinamide-adenine dinucleotide phosphate (NADPH)–dependent oxidase. Fusion of neutrophil granule membranes with the phagosome membrane occurs, resulting in the delivery of potent antimicrobial proteins and small peptides into the phagosome. In coordinated succession, the contents of the specific granules and then contents of the azurophil granules are secreted into the phagosome.
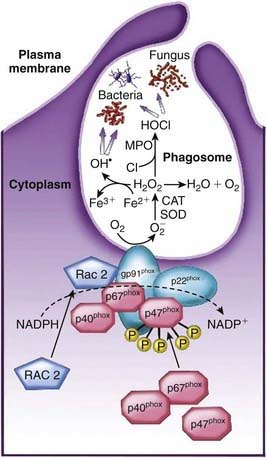
Figure 121-3 NADPH oxidase components and activation. On activation of phagocytic cells, the 3 cytosolic components (red) of the NADPH oxidase (p67phox, p47phox, and p40phox), plus the small GTPase protein Rac2, are translocated to the membrane of the phagocytic vacuole. The p47phox subunit binds to the flavocytochromeb558 membrane component (blue-green) of the NADPH oxidase (gp91phox plus p22phox). The NADPH oxidase catalyses the formation of superoxide by transferring an electron from NADPH to molecular oxygen (O2), thereby forming the superoxide free radical. The unstable superoxide anion is converted to hydrogen peroxide, either spontaneously or by superoxide dismutase (SOD). Hydrogen peroxide can follow different metabolic pathways into more potent reactive oxidants (such as OH• or HOCl) or degradation to H2O + O2.
(Modified from Stiehm ER, Ochs HD, Winkelstein JA: Immunologic disorders in infants and children, ed 5, Philadelphia, 2004, Elsevier/Saunders, p 622.)
Occurring concomitantly are assembly and activation of NADPH oxidase at the phagosome membrane (see Fig. 121-3). This enzyme generates large amounts of superoxide (O2−) from molecular oxygen that in turn decomposes to produce hydrogen peroxide (H2O2) and singlet oxygen. H2O2 can react with O2− to form hydroxyl radicals. Myeloperoxidase, a major azurophil granule component, catalyzes the reaction of H2O2 with ubiquitously present chloride ions to create hypochlorous acid (HOCl) in the phagosome. H2O2 and HOCl are potent microbicidal agents that can directly denature proteins and nucleic acids as well as activate some of the neutrophil proteases. These events, together with the acidification of the lysosomal vacuole, break down and clear pathogens from sites of infection.
In addition, neutrophils secrete a wide variety of cytokines and chemokines that recruit more neutrophils to fight the infection, attract monocytes and macrophages that possess both microbicidal and scavenger functions, and promote antigen presentation to help initiate the adaptive immune response. Also, the reactive oxidants can inactivate chemotactic factors and may serve to terminate the process of neutrophil influx, thereby attenuating the inflammatory process. Finally, the release of reactive oxygen species, granule proteins, and cytokines can also damage local tissues, leading to the classic temporary signs of inflammation or to more permanent impairment of tissue integrity and function.
Dinauer MC, Newburger PE. The phagocyte system and disorders of granulopoiesis and granulocyte function. In: Orkin SH, Ginsburg D, Nathan DG, et al, editors. Nathan and Oski’s hematology of infancy and childhood. Philadelphia: Saunders Elsevier; 2009:1109-1217.
Eyles JL, Roberts AW, Metcalf D, et al. Granulocyte colony-stimulating factor and neutrophils—forgotten mediators of inflammatory disease. Nat Clin Pract Rheumatol. 2006;2:500-510.
Ley K, Laudanna C, Cybulsky MI, et al. Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nat Rev Immunol. 2007;7:678-689.
Nauseef WM. How human neutrophils kill and degrade microbes: an integrated view. Immunol Rev. 2007;219:88-102.
Scapini P, Lapinet-Vera JA, Gasperini S, et al. The neutrophil as a cellular source of chemokines. Immunol Rev. 2000;177:195-203.