Chapter 589 Neurocutaneous Syndromes
The neurocutaneous syndromes include a heterogeneous group of disorders characterized by abnormalities of both the integument and central nervous system (CNS). Most disorders are familial and believed to arise from a defect in differentiation of the primitive ectoderm. Disorders classified as neurocutaneous syndromes include neurofibromatosis, tuberous sclerosis, Sturge-Weber syndrome, von Hippel–Lindau disease, PHACE syndrome, ataxia telangiectasia, linear nevus syndrome, hypomelanosis of Ito, and incontinentia pigmenti.
589.1 Neurofibromatosis
Neurofibromatoses are autosomal dominant disorders that cause tumors to grow on nerves and result in other abnormalities such as skin changes and bone deformities. It was previously thought that there were 2 types of neurofibromatosis (type 1 and type 2); it is recognized that they are clinically and genetically distinct diseases and should be considered separate entities: neurofibromatosis 1 (NF-1) and neurofibromatosis 2 (NF-2).
Clinical Manifestations and Diagnosis
NF-1 is the most prevalent type, with an incidence of 1/3,000, and is diagnosed when any 2 of the following 7 features are present: (1) Six or more café-au-lait macules over 5 mm in greatest diameter in prepubertal individuals and over 15 mm in greatest diameter in postpubertal individuals. Café-au-lait spots are the hallmark of neurofibromatosis and are present in almost 100% of patients. They are present at birth but increase in size, number, and pigmentation, especially during the first few yrs of life (Fig. 589-1). The spots are scattered over the body surface, with predilection for the trunk and extremities but sparing the face. (2) Axillary or inguinal freckling consisting of multiple hyperpigmented areas 2-3 mm in diameter. Skinfold freckling usually appears between 3 and 5 yr of age. The frequency of axillary and inguinal freckling has been reported to be greater than 80% by 6 yr of age. (3) Two or more iris Lisch nodules. Lisch nodules are hamartomas located within the iris and are best identified by a slit-lamp examination (Fig. 589-2). They are present in >74% of patients with NF-1 but are not a component of NF-2. The prevalence of Lisch nodules increases with age, from only 5% of children <3 yr of age, to 42% among children 3-4 yr of age, and virtually 100% of adults ≥21 yr of age. (4) Two or more neurofibromas or 1 plexiform neurofibroma. Neurofibromas typically involve the skin, but they may be situated along peripheral nerves and blood vessels and within viscera including the gastrointestinal tract. These lesions appear characteristically during adolescence or pregnancy, suggesting a hormonal influence. They are usually small, rubbery lesions with a slight purplish discoloration of the overlying skin. Plexiform neurofibromas are usually evident at birth and result from diffuse thickening of nerve trunks that are frequently located in the orbital or temporal region of the face. The skin overlying a plexiform neurofibroma may be hyperpigmented to a greater degree than a café-au-lait spot. Plexiform neurofibromas may produce overgrowth of an extremity and a deformity of the corresponding bone. (5) A distinctive osseous lesion such as sphenoid dysplasia (which may cause pulsating exophthalmos) or cortical thinning of long bones (e.g., of the tibia) with or without pseudoarthrosis. (6) Optic gliomas are present in approximately 15% of patients with NF-1 and represent mostly low-grade astrocytomas. They are the main CNS tumor with a marked increased frequency in NF-1. Because of their growth, it is recommended that all children age 10 yr or younger with NF-1 undergo annual ophthalmologic examinations. When they progress, visual symptoms are produced because the tumors enlarge and put pressure on the optic nerves and chiasm resulting in impaired visual acuity and visual fields. Extension into the hypothalamus can lead to endocrine deficiencies or failure to thrive. The MRI findings of an optic glioma include diffuse thickening, localized enlargement, or a distinct focal mass originating from the optic nerve or chiasm (Fig. 589-3). (7) A first-degree relative with NF-1 whose diagnosis was based on the aforementioned criteria.

Figure 589-1 A and B, Multiple café-au-lait spots over the back. Note the dermal neurofibromas below the right scapula and right side of the lower back.
(From Hersh JH, Committee on Genetics: Health supervision for children with neurofibromatosis, Pediatrics 121:633–642, 2008, Fig 1.)

Figure 589-2 Neurofibromatosis 1. Pigmented hamartomas of the iris (Lisch nodules).
(From Zitelli BJ, Davis HW: Atlas of pediatric physical diagnosis, ed 4, St Louis, 2002, Mosby, p 507.)

Figure 589-3 Optic glioma. Sagittal T1-weighted MRI scan of a patient with neurofibromatosis 1 shows thickening of the optic nerve (arrow).
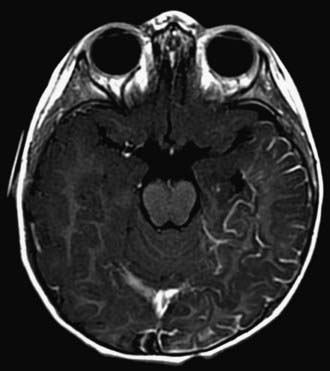
Children with NF-1 are susceptible to neurologic complications. MRI studies of selected children have shown abnormal hyperintense T2 weighted signals in the optic tracts, brainstem, globus pallidus, thalamus, internal capsule, and cerebellum (Fig. 589-4). These signals, “unidentified bright objects (UBOs),” tend to disappear with age; most have disappeared by 30 yr of age. It is unclear what the UBOs represent pathologically, and there is disagreement as to the presence and number of UBOs and their relationship to learning disabilities, attention deficit disorders, behavioral and psychosocial problems, and abnormalities of speech among affected children. Therefore, imaging studies such as brain MRIs should be reserved only for patients with clinical symptoms.
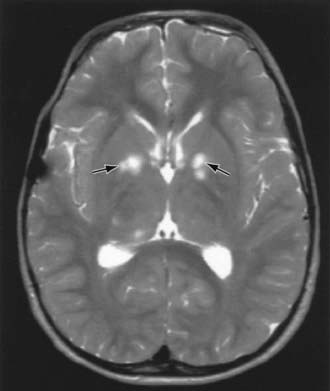
Figure 589-4 T2-weighted MRI scan of a patient with neurofibromatosis 1. Note the high-signal areas (unidentified bright objects) in the basal ganglia (arrows).
One of the most common complications is learning disability affecting approximately 30% of NF-1 children. Seizures are observed in approximately 8% of NF-1 patients. The cerebral vessels may develop aneurysms, or stenosis resulting in moyamoya disease (Chapter 594.1). Neurologic sequelae of these vascular abnormalities include transient cerebrovascular ischemic attacks, hemiparesis, and cognitive defects. Precocious puberty may become evident in the presence or absence of lesions of the optic chiasm and hypothalamus. Malignant neoplasms are also a significant problem in patients with NF-1, affecting approximately 3% of patients. A neurofibroma occasionally differentiates into a malignant peripheral nerve sheath tumor (MPNST). The incidence of pheochromocytoma, rhabdomyosarcoma, leukemia, and Wilms tumor is higher than in the general population. Scoliosis is a common complication found in about 10% of the patients. Patients with NF-1 are at risk for hypertension, which may result from renal vascular stenosis or a pheochromocytoma.
NF-2 is a rarer condition, with an incidence of 1/25,000, and may be diagnosed when 1 of the following 4 features is present: (1) bilateral vestibular schwannomas; (2) a parent, sibling, or child with NF-2 and either unilateral vestibular schwannoma or any 2 of the following: meningioma, schwannoma, glioma, neurofibroma, or posterior subcapsular lenticular opacities; (3) unilateral vestibular schwannoma and any 2 of the following: meningioma, schwannoma, glioma, neurofibroma, or posterior subcapsular lenticular opacities; (4) multiple meningiomas (2 or more) and unilateral vestibular schwannoma or any 2 of the following: schwannoma, glioma, neurofibroma, or cataract. Symptoms of tinnitus, hearing loss, facial weakness, headache, or unsteadiness may appear during childhood, although signs of a cerebellopontine angle mass are more commonly present in the 2nd and 3rd decades of life. Although café-au-lait spots and skin neurofibromas are classic findings in NF-1, they are much less common in NF-2. Posterior subcapsular lens opacities are identified in about 50% of patients with NF-2. The NF2 gene (also known as merlin or schwannomin) is located on chromosome 22q1.11. The frequency of lesions associated with NF-2 is noted in Table 589-1.
Table 589-1 FREQUENCY OF LESIONS ASSOCIATED WITH NEUROFIBROMATOSIS TYPE 2
| FREQUENCY OF ASSOCIATION WITH NF2 | |
|---|---|
| NEUROLOGIC LESIONS | |
| Bilateral vestibular schwannomas | 90-95% |
| Other cranial nerve schwannomas | 24-51% |
| Intracranial meningiomas | 45-58% |
| Spinal tumors | 63-90% |
| Extramedullary | 55-90% |
| Intramedullary | 18-53% |
| Peripheral neuropathy | Up to 66% |
| OPHTHALMOLOGIC LESIONS | |
| Cataracts | 60-81% |
| Epiretinal membranes | 12-40% |
| Retinal hamartomas | 6-22% |
| CUTANEOUS LESIONS | |
| Skin tumors | 59-68% |
| Skin plaques | 41-48% |
| Subcutaneous tumors | 43-48% |
| Intradermal tumors | Rare |
From Asthagiri AR, Parry DM, Butman JA, et al: Neurofibromatosis type 2, Lancet 373:1974–1984, 2009, Table 1.)
Management
Because of the diverse and unpredictable complications associated with NF-1, close multidisciplinary follow-up is necessary. Patients with NF-1 should have regular clinical assessments at least yearly, focusing the history and examination on the potential problems for which they are at increased risk. These assessments include yearly ophthalmologic examination, neurologic assessment, blood pressure monitoring, and scoliosis evaluation. Neuropsychologic and educational testing should be considered as needed. The NIH Consensus Development Conference has advised against routine imaging studies of the brain and optic tracts because treatment in these asymptomatic NF-1 children is rarely required. All symptomatic cases (i.e., those with visual disturbance, proptosis, or increased intracranial pressure) must be studied without delay.
Genetic Counseling
While NF-1 is an autosomal dominant disorder, over half the cases are sporadic, representing de novo mutations. The NF1 gene on chromosome region 17q11.2 encodes a protein also known as neurofibromin. Neurofibromin acts as an inhibitor of the oncogene ras. The diagnosis of NF-1 is based on the clinical features. However, molecular testing for the NF1 gene is available and can be useful in a number of cases. Scenarios in which genetic testing is helpful include patients who have only 1 of the criteria for clinical diagnosis, those with unusually severe disease, and those seeking prenatal/pre-implantation diagnosis.
American Academy of Pediatrics Committee on Genetics. Health supervision for children with neurofibromatosis. Pediatrics. 1995;96:368-372.
Asthagiri AR, Parry DM, Butman JA, et al. Neurofibromatosis type 2. Lancet. 2009;373:1974-1984.
Baser ME, R Evans DG, Gutmann DH. Neurofibromatosis 2. Curr Opin Neurol. 2003;16(1):27-33.
Cnossen MH, de Goede-Bolder A, van den Broek KM, et al. A prospective 10 year follow up study of patients with neurofibromatosis type 1. Arch Dis Child. 1998;78:408-412.
DeBella K, Szudek J, Friedman JM. Use of the National Institutes of Health criteria for diagnosis of neurofibromatosis 1 in children. Pediatrics Mar. 2000;105:608-614.
Evans DGR. Neurofibromatosis type 2 (NF2): a clinical and molecular review. Orphanet J Rare Dis. 2009;4:16.
Hersh JH, Committee on Genetics. Health supervision for children with neurofibromatosis. Pediatrics. 2008;121:633-642.
Hofman KJ, Harris EL, Bryan RN, et al. Neurofibromatosis type 1: the cognitive phenotype. J Pediatr. 1994;124:S1-S8.
Krab LC, Aarsen FK, de Goede-Bolder A, et al. Impact of neurofibromatosis type 1 on school performance. J Child Neurol. 2008;23:1002-1010.
Messiaen L, Yao S, Brems H, et al. Clinical and mutational spectrum of neurofibromatosis type 1-like syndromes. JAMA. 2009;302:2111-2118.
Plotkin SR, Stemmer-Rachamimov AO, Barker FGII, et al. Hearing improvement after bevacizumab in patients with neurofibromatosis type 2. N Engl J Med. 2009;361:358-367.
Rizzo JF, Lessell S. Cerebrovascular abnormalities in neurofibromatosis type 1. Neurology. 1994;44:1000-1002.
Williams VC, Lucas J, Babcock MA, et al. Neurofibromatosis type 1 revisited. Pediatrics. 2009;123:124-133.
589.2 Tuberous Sclerosis
Tuberous sclerosis complex (TSC) is inherited as an autosomal dominant trait with variable expression and a prevalence of 1/6,000 newborns. Spontaneous genetic mutations occur in  of the cases. Molecular genetic studies have identified 2 foci for TSC: the TSC1 gene is located on chromosome 9q34, and the TSC2 gene is on chromosome 16p13. The TSC1 gene encodes a protein called hamartin. The TSC2 gene encodes the protein tuberin. Within a cell, these 2 proteins bind to one another and work together. That is why a mutation in the TSC1 gene and a mutation in the TSC2 gene result in a similar disease in people. The loss of either tuberin or hamartin results in the formation of numerous benign tumors (hamartomas). Thus, the TSC1 and TSC2 genes are tumor suppressor genes. Tuberin and hamartin are involved in a key pathway in the cell that regulates protein synthesis and cell size. One of the ways cells regulate their growth is by controlling the rate of protein synthesis. A protein called mTOR was identified as 1 of the master regulators of cell growth. mTOR, in turn, is controlled by rheb, a small cytoplasmic GTPase. When rheb is activated, the protein synthesis machinery is turned on, most likely via mTOR, and the cell grows in size.
of the cases. Molecular genetic studies have identified 2 foci for TSC: the TSC1 gene is located on chromosome 9q34, and the TSC2 gene is on chromosome 16p13. The TSC1 gene encodes a protein called hamartin. The TSC2 gene encodes the protein tuberin. Within a cell, these 2 proteins bind to one another and work together. That is why a mutation in the TSC1 gene and a mutation in the TSC2 gene result in a similar disease in people. The loss of either tuberin or hamartin results in the formation of numerous benign tumors (hamartomas). Thus, the TSC1 and TSC2 genes are tumor suppressor genes. Tuberin and hamartin are involved in a key pathway in the cell that regulates protein synthesis and cell size. One of the ways cells regulate their growth is by controlling the rate of protein synthesis. A protein called mTOR was identified as 1 of the master regulators of cell growth. mTOR, in turn, is controlled by rheb, a small cytoplasmic GTPase. When rheb is activated, the protein synthesis machinery is turned on, most likely via mTOR, and the cell grows in size.
TSC is an extremely heterogeneous disease with a wide clinical spectrum varying from severe mental retardation and incapacitating seizures to normal intelligence and a lack of seizures, often within the same family. The disease affects many organ systems other than the skin and brain, including the heart, kidney, eyes, lungs, and bone.
Clinical Manifestations and Diagnosis
Definite TSC is diagnosed when at least 2 major or 1 major plus 2 minor features are present see Tables 589-2 and 589-3 for major and minor features, respectively).
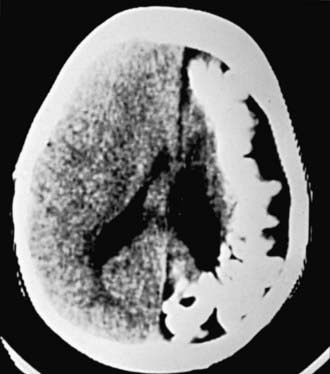
The hallmark of TSC is the involvement of the CNS (Fig. 589-5). Retinal lesions consist of 2 types: hamartomas (elevated mulberry lesions or plaquelike lesions) and white depigmented patches (similar to the hypopigmented skin lesions) (Fig. 589-6). The characteristic brain lesion is a cortical tuber (see Fig. 589-5). Brain MRI is the best way of identifying cortical tubers. Based on fetal MRI studies, we know that cortical tubers are formed while in utero. Subependymal nodules are lesions found along the wall of the lateral ventricles where they undergo calcification and project into the ventricular cavity, producing a candle-dripping appearance. These lesions do not cause any problems; in 5-10% of cases, these benign lesions can grow into subependymal giant cell astrocytomas (SEGAs). These tumors can grow and block the circulation of cerebrospinal fluid (CSF) around the brain and cause hydrocephalus, which requires immediate neurosurgical intervention.

Figure 589-5 Tuberous sclerosis. A, CT scan with subependymal calcifications characteristic of tuberous sclerosis. B, The MRI demonstrates multiple subependymal nodules in the same patient (arrow). Parenchymal tubers are also visible on both the CT and the MRI scan as low-density areas in the brain parenchyma.
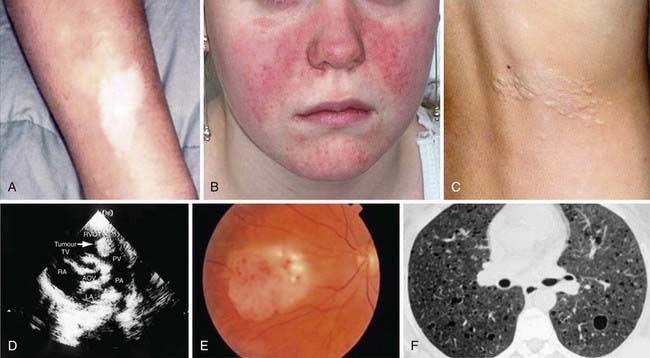
Figure 589-6 Dermatological, cardiac, and pulmonary manifestations of tuberous sclerosis. Hypomelanotic macules (A). Facial angiofibromas (B). Shagreen patch (C). Hyperechoic rhabdomyoma detected by echocardiography (D). Retinal hamartoma (E). Lymphangioleiomyomatosis (F).
(From Curatolo P, Bombardieri R, Jozwiak S: Tuberous sclerosis, Lancet 372:657–668, 2008, Fig 7.)
The most common neurologic manifestations of TSC consist of epilepsy, cognitive impairment, and autism spectrum disorders. TSC may present during infancy with infantile spasms and a hypsarrhythmic electroencephalogram (EEG) pattern. It is important to remember that you can have hypsarrhythmia without infantile spasms and infantile spasms without hypsarrhythmia especially in TSC patients. The seizures may be difficult to control and, at a later age, they may develop into myoclonic epilepsy (Chapter 586). In Europe and Canada, infantile spasms associated with TSC are treated with vigabatrin (rather than ACTH) with good results. In the USA, ACTH had been the drug of choice until vigabatrin was approved by the U.S. Food and Drug Administration (FDA) for use in infantile spasms. Many patients with TSC have normal intelligence and few, if any, neurologic abnormalities.
Skin Lesions
More than 90% of cases show the typical hypomelanotic macules that have been likened to an ash leaf on the trunk and extremities. Visualization of the hypomelanotic macule is enhanced by the use of a Wood ultraviolet lamp (Chapter 645). To count as a major feature, at least 3 hypomelanotic macules must be present (see Fig. 589-6). Facial angiofibromas develop between 4 and 6 yr of age; they appear as tiny red nodules over the nose and cheeks and are sometimes confused with acne (see Fig. 589-6). Later, they enlarge, coalesce, and assume a fleshy appearance. A shagreen patch is also characteristic of TSC and consists of a roughened, raised lesion with an orange-peel consistency located primarily in the lumbosacral region. During adolescence or later, small fibromas or nodules of skin may form around fingernails or toenails in 15-20% of the TSC patients (Fig. 589-7).
Other Organ Involvement
Approximately 50% of children with TSC have cardiac rhabdomyomas, which may be detected in a fetus at risk by an echocardiogram. The rhabdomyomas may be numerous or located at the apex of the left ventricle, and although they can cause congestive heart failure and arrhythmias, they tend to slowly resolve spontaneously. The kidneys in 75-80% of patients >10 yr of age have angiomyolipomas that are usually benign tumors. Angiomyolipomas begin in childhood in many individuals with TSC, but they may not be problematic until young adulthood. By the 3rd decade of life, they may cause lumbar pain and hematuria from slow bleeding, and rarely, they may result in sudden retroperitoneal bleeding. The current recommendation is to follow them by yearly imaging, and when the lesion becomes larger than 4 cm, to use transcatheter tumor embolization for treatment. Single or multiple renal cysts are also commonly present in TSC. Lymphangioleiomyomatosis (LAM) is the classical pulmonary lesion in TSC and only affects women after the age of 20 yr.
Diagnosis of TSC relies on a high index of suspicion when assessing a child with infantile spasms or myoclonic epilepsy. A careful search for the typical skin and retinal lesions should be completed in all patients with a seizure disorder or autism spectrum disorder. Brain MRI confirms the diagnosis in most cases. Genetic testing for TSC1 and TSC2 mutations is available and may be considered when the individual patient does not meet all the clinical criteria. Prenatal testing may be offered when a known TSC mutation exists in that family.
Management
As for routine follow-up of individuals with TSC, the following are recommended in addition to physical examination: brain MRI every 1-3 yr, renal imaging (ultrasound, CT, or MRI) every 1-3 yr, and neurodevelopmental testing at the time of beginning 1st grade. Based on the complications of the disease, additional follow-up testing may be required for each individual. Symptoms and signs of increased intracranial pressure suggest obstruction of the foramen of Monro by a SEGA and warrant immediate investigation and surgical intervention. For treatment of SEGAs in TSC patients, who are not candidates for surgical resection, the FDA approved everolimus in November 2010.
Crino PB, Nathanson KL, Henske EP. The tuberous sclerosis complex. N Engl J Med. 2006;355:1345-1356.
Curatolo P, Bombardieri R, Jazwiak S. Tuberous sclerosis. Lancet. 2008;372:657-668.
Datta AN, Hahn CD, Sahin M. Clinical presentation and diagnosis of tuberous sclerosis complex in infancy. J Child Neurol. 2008;23:268-273.
Ewalt DH, Diamond N, Rees C, et al. Long-term outcome of transcatheter embolization of renal angiomyolipomas due to tuberous sclerosis complex. J Urol. Nov 2005;174(5):1764-1766.
O’Callaghan FJK, Martyn CN, Renowden S, et al. Subependymal nodules, giant cell astrocytomas and the tuberous sclerosis complex: a population-based study. Arch Dis Child. 2008;93:751-754.
Osborne JP, Merrifield J, O’Callaghan FJK. Tuberous sclerosis—what’s new? Arch Dis Child. 2008;93:728-731.
Roach ES, Miller VS. Neurocutaneous disorders. Cambridge, United Kingdom: Cambridge University Press; 2004.
Tworetzky W, McElhinney DB, Margossian R, et al. Association between cardiac tumors and tuberous sclerosis in the fetus and neonate. Am J Cardiol. 2003;92(4):487-489.
589.3 Sturge-Weber Syndrome
Sturge-Weber syndrome (SWS) is a sporadic vascular disorder and consists of a constellation of symptoms and signs including a facial capillary malformation (port-wine stain), abnormal blood vessels of the brain (leptomeningeal angioma), and abnormal blood vessels of the eye leading to glaucoma. Patients present with seizures, hemiparesis, strokelike episodes, headaches and developmental delay. An estimated frequency of approximately 1 per 50,000 live births have SWS.
Etiology
The etiology remains unclear. The sporadic incidence and focal nature of SWS suggest the presence of somatic mutations, but this has not been demonstrated to date. The condition is thought to result from anomalous development of the embryonic vascular bed in the early stages of facial and cerebral development. There are hypotheses about aberrant sympathetic innervation, increased vascular growth factors and defects in extracellular matrix, but these remain to be tested. Low flow angiomatosis of the leptomeninges appears to result in a chronic hypoxic state leading to cortical atrophy and calcifications.
Clinical Manifestations
The facial port-wine stain is present at birth, tends to be unilateral, and always involves the upper face and eyelid, in a distribution consistent with the ophthalmic division of the trigeminal nerve. The capillary malformation may also be evident over the lower face, trunk, and in the mucosa of the mouth and pharynx. It is important to note that not all children with facial port-wine stain have SWS. In fact, the overall incidence of SWS has been reported to be 8-33% in those with a port-wine stain. Buphthalmos and glaucoma of the ipsilateral eye are common complications. The incidence of epilepsy in patients with SWS is 75-90%, and seizures develop in most patients in the 1st yr of life. They are typically focal tonic-clonic and contralateral to the side of the facial capillary malformation. The seizures may become refractory to anticonvulsants and are associated with a slowly progressive hemiparesis in many cases. Transient strokelike episodes or visual defects persisting for several days and unrelated to seizure activity are common and probably result from thrombosis of cortical veins in the affected region. Although neurodevelopment appears to be normal in the 1st yr of life, mental retardation or severe learning disabilities are present in at least 50% in later childhood, probably the result of intractable epilepsy and increasing cerebral atrophy.
Diagnosis
MRI with contrast is the imaging modality of choice for demonstrating the leptomeningeal angioma in SWS (Figure 589-8). White matter abnormalities are common and are thought to be a result of chronic hypoxia. Often, atrophy is noted ipsilateral to the leptomeningeal angiomatosis. Calcifications can be seen best with a head CT (Fig. 589-9). Ophthalmologic evaluation for glaucoma is also necessary. Based on the involvement of the brain and the face, there are 3 types according to the Roach Scale:
Management
Management of SWS is symptomatic and multidisciplinary, but not well studied prospectively. It is aimed at controlling seizures, treating headaches, preventing strokelike episodes, monitoring for glaucoma, and using laser therapy for the cutaneous capillary malformations. Seizures beginning in infancy are not always associated with a poor neurodevelopmental outcome. For patients with well-controlled seizures and normal or near-normal development, management consists of anticonvulsants and surveillance for complications including glaucoma, buphthalmos, and behavioral abnormalities. If the seizures are refractory to anticonvulsant therapy, especially in infancy and the 1st 1-2 yr of life, and arise primarily from 1 hemisphere, most centers advise a hemispherectomy. Because of the risk of glaucoma, regular measurement of intraocular pressure is indicated. The facial port-wine stain is often a target of ridicule by classmates, leading to psychologic trauma. Pulsed dye laser therapy often provides excellent clearing of the port-wine stain, particularly if it is located on the forehead.
Comi AM. Advances in Sturge-Weber syndrome. Curr Opin Neurol. 2006;19(2):124-128.
Cordisco MR. An update on lasers in children. Curr Opin Pediatr. 2009;21(4):499-504.
Kossoff EH, Buck C, Freeman JM. Outcomes of 32 hemispherectomies for Sturge-Weber syndrome worldwide. Neurology. 2002;59:1735-1738.
Tan OT, Sherwood K, Gilchrest BA. Treatment of children with port-wine stains using the flashlamp-pulsed tunable dye laser. N Engl J Med. 1989;320:416-421.
589.4 Von Hippel–Lindau Disease
Von Hippel–Lindau (VHL) disease affects many organs, including the cerebellum, spinal cord, retina, kidney, pancreas, and epididymis. Its incidence is around 1 : 36,000. It results from an autosomal dominant mutation affecting a tumor suppressor gene, VHL. Around 80% of individuals with VHL disease have an affected parent, and around 20% have a de novo gene mutation. Molecular testing is available and detects mutations in almost 100% of probands.
The major neurologic features of the condition include cerebellar hemangioblastomas and retinal angiomas. Patients with cerebellar hemangioblastoma present in early adult life or beyond with symptoms and signs of increased intracranial pressure. A smaller number of patients have hemangioblastoma of the spinal cord, producing abnormalities of proprioception and disturbances of gait and bladder dysfunction. The CT scan and MRI typically show a cystic cerebellar lesion with a vascular mural nodule. Total surgical removal of the tumor is curative.
Approximately 25% of patients with cerebellar hemangioblastoma have retinal angiomas. Retinal angiomas are characterized by small masses of thin-walled capillaries that are fed by large and tortuous arterioles and venules. They are usually located in the peripheral retina so that vision is unaffected. Exudation in the region of the angiomas may lead to retinal detachment and visual loss. Retinal angiomas are treated with photocoagulation and cryocoagulation, and both have produced good results.
Cystic lesions of the kidneys, pancreas, liver, and epididymis as well as pheochromocytoma are frequently associated with von Hippel–Lindau disease. Renal carcinoma is the most common cause of death. Regular follow-up and appropriate imaging studies are necessary to identify lesions that may be treated at an early stage.
Gläsker S. Central nervous system manifestations in VHL: genetics, pathology and clinical phenotypic features. Fam Cancer. 2005;4(1):37-42.
Kaelin WGJr. The von Hippel-Lindau tumour suppressor protein: O2 sensing and cancer. Nat Rev Cancer. 2008;8(11):865-873.
Latif F, Tory K, Gmarra J, et al. Identification of the von Hippel-Lindau disease tumor suppressor gene. Science. 1993;260:1317-1320.
Maher ER, Kaelin WGJr. von Hippel-Lindau disease. Medicine. 1997;76:381-391.
589.5 Linear Nevus Syndrome
This sporadic condition is characterized by a facial nevus and neurodevelopmental abnormalities. The nevus is located on the forehead and nose and tends to be midline in its distribution. It may be quite faint during infancy but later becomes hyperkeratotic, with a yellow-brown appearance. Two thirds of patients with linear nevus syndrome demonstrate associated neurologic findings, including cortical dysplasia, glial hamartomas, and low-grade gliomas. Cerebral and cranial anomalies, predominantly hemimegalencephaly and enlargement of the lateral ventricles, were reported in 72% of cases. Incidence of epilepsy has been reported as high as 75% and mental retardation as high as 60%. Focal neurologic signs including hemiparesis and homonymous hemianopia may also be seen.
589.6 PHACE Syndrome
The syndrome denotes posterior fossa malformations, hemangiomas, arterial anomalies, coarctation of the aorta and other cardiac defects, and eye abnormalities. It is also referred to as PHACES syndrome when ventral developmental defects including sternal clefting and/or a supraumbilical raphe are present. Large facial hemangiomas may be associated with a Dandy-Walker malformation, vascular anomalies (coarctation of aorta, aplasia or hypoplastic carotid arteries, aneurysmal carotid dilation, aberrant left subclavian artery), glaucoma, cataracts, microphthalmia, optic nerve hypoplasia, and ventral defects (sternal clefts). The facial hemangioma is typically ipsilateral to the aortic arch. The Dandy-Walker malformation is the most common developmental abnormality of the brain. Other anomalies included hypoplasia or agenesis of the cerebellum, cerebellar vermis, corpus callosum, cerebrum, and septum pellucidum. Cerebrovascular anomalies can result in acquired, progressive vessel stenosis and acute ischemic stroke. There is a female predominance. The underlying pathogenesis of PHACE syndrome remains unknown.
589.7 Incontinentia Pigmenti
This rare, heritable, multisystem ectodermal disorder features dermatologic, dental, and ocular abnormalities. The phenotype is produced by functional mosaicism caused by random X-inactivation of an X-linked dominant gene that is lethal in males (IKK-gamma/NEMO gene). The paucity of affected males, the occurrence of female-to-female transmission, and an increased frequency of spontaneous abortions in carrier females support this supposition.
Clinical Manifestations and Diagnosis
This disease has 4 phases, not all of which may occur in a given patient. The 1st phase is evident at birth or in the 1st few weeks of life and consists of erythematous linear streaks and plaques of vesicles (Fig. 589-10) that are most pronounced on the limbs and circumferentially on the trunk. The lesions may be confused with those of herpes simplex, bullous impetigo, or mastocytosis, but the linear configuration is unique. Histopathologically, epidermal edema and eosinophil-filled intraepidermal vesicles are present. Eosinophils also infiltrate the adjacent epidermis and dermis. Blood eosinophilia as high as 65% of the white blood cell count is common. The 1st stage generally resolves by 4 mo of age, but mild, short-lived recurrences of blisters may develop during febrile illnesses. In the 2nd phase, as blisters on the distal limbs resolve, they become dry and hyperkeratotic, forming verrucous plaques. The verrucous plaques rarely affect the trunk or face and generally involute within 6 mo. Epidermal hyperplasia, hyperkeratosis, and papillomatosis are characteristic. The 3rd or pigmentary stage is the hallmark of incontinentia pigmenti. It generally develops over weeks to months and may overlap the earlier phases, be evident at birth, or, more commonly, begin to appear in the 1st few weeks of life. Hyperpigmentation is more often apparent on the trunk than the limbs and is distributed in macular whorls, reticulated patches, flecks, and linear streaks that follow Blaschko lines. The axillae and groin are invariably affected. The sites of involvement are not necessarily those of the preceding vesicular and warty lesions. The pigmented lesions, once present, persist throughout childhood. They generally begin to fade by early adolescence and often disappear by age 16 yr. Occasionally, the pigmentation remains permanently, particularly in the groin. The lesion, histopathologically, shows vacuolar degeneration of the epidermal basal cells and melanin in melanophages of the upper dermis as a result of incontinence of pigment. In the 4th stage, hairless, anhidrotic, hypopigmented patches or streaks occur as a late manifestation of incontinentia pigmenti; they may develop, however, before the hyperpigmentation of stage 3 has resolved. The lesions develop mainly on the flexor aspect of the lower legs and less often on the arms and trunk.
Approximately 80% of affected children have other defects. Alopecia, which may be scarring and patchy or diffuse, is most common on the vertex and occurs in up to 40% of patients. Hair may be lusterless, wiry, and coarse. Dental anomalies, which are present in up to 80% of patients and are persistent throughout life, consist of late dentition, hypodontia, conical teeth, and impaction. CNS manifestations, including motor and cognitive developmental retardation, seizures, microcephaly, spasticity, and paralysis, are found in up to  of affected children. Ocular anomalies, such as neovascularization, microphthalmos, strabismus, optic nerve atrophy, cataracts, and retrolenticular masses, occur in >30% of children. Nonetheless, >90% of patients have normal vision. Less common abnormalities include dystrophy of nails (ridging, pitting) and skeletal defects.
of affected children. Ocular anomalies, such as neovascularization, microphthalmos, strabismus, optic nerve atrophy, cataracts, and retrolenticular masses, occur in >30% of children. Nonetheless, >90% of patients have normal vision. Less common abnormalities include dystrophy of nails (ridging, pitting) and skeletal defects.
Diagnosis of incontinentia pigmenti is made on clinical grounds, although major and minor criteria have been established to aid in diagnosis. Wood lamp examination may be useful in older children and adolescents to highlight pigmentary abnormalities. Clinical molecular testing is available, and in 80% of the affected patients a deletion that removes exons 4 through 10 of NEMO can be detected. Differential diagnosis includes hypomelanosis of Ito, which presents with similar skin manifestations and is often associated with chromosomal mosaicism.
Management
The choice of investigative studies and the plan of management depend on the occurrence of particular noncutaneous abnormalities since the skin lesions are benign. The high incidence of associated major anomalies warrants genetic counseling.
Bruckner AL. Incontinentia pigmenti: a window to the role of NF-kappaB function. Semin Cutan Med Surg. 2004;23:116-124.
Smahi A, Courtois G, Vabres P, et al. Genomic rearrangement in NEMO impairs NF-kappaB activation and is a cause of incontinentia pigmenti. The International Incontinentia Pigmenti (IP) Consortium. Nature. 2000;405(6785):466-472.