Chapter 611 Examination of the Eye
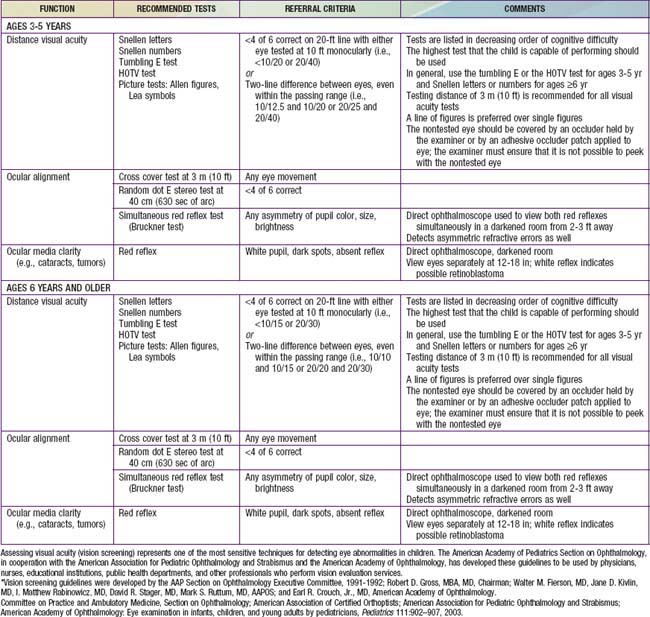
Examination of the eyes is a routine part of the periodic pediatric assessment beginning in the newborn period. The primary care physician is very important in detecting both obvious and insidious asymptomatic eye diseases. Screening by lay persons in schools and community programs can also be effective in detecting problems early. The best method of screening (ages 3-5 yrs) is currently being investigated. The American Academy of Ophthalmology recommend preschool vision screening as a means of reducing preventable visual loss (Table 611-1). This testing should also be done by pediatricians during well child visits. Children should be examined by an ophthalmologist whenever a significant ocular abnormality or vision defect is noted or suspected. Children who are at high risk of ophthalmologic problems, such as genetically inherited ocular conditions and various systemic disorders, should also be examined by an ophthalmologist.
Basic examination, whether done by a pediatrician or an ophthalmologist, must include evaluation of visual acuity and the visual fields, assessment of the pupils, ocular motility and alignment, a general external examination, and an ophthalmoscopic examination of the media and fundi. When indicated, biomicroscopy (slit-lamp examination), cycloplegic refraction, and tonometry are performed by an ophthalmologist. Special diagnostic procedures, such as ultrasonic examination, fluorescein angiography, electroretinography, or visual evoked response (VER) testing, are also indicated for specific conditions.
Visual Acuity
There are many tests of visual acuity. Which test is used depends on a child’s age and ability to cooperate, as well as a clinician’s preference and experience with each test. The most common visual acuity test in infants is an assessment of their ability to fixate and follow a target. If appropriate targets are used, this reflex can be demonstrated by about 6 weeks of age. The test is performed by seating the child comfortably in the caretaker’s lap. The object of visual interest, usually a bright-colored toy, is slowly moved to the right and to the left. The examiner observes whether the infant’s eyes turn toward the object and follow its movements. The examiner can use a thumb to occlude one of the infant’s eyes and test each eye separately. Although a sound-producing object might compromise the purity of the visual stimulus, in practice, toys that squeak or rattle heighten an infant’s awareness and interest in the test.
The human face is a better target than test objects. The examiner can exploit this by moving his or her face slowly in front of the infant’s face. If the appropriate following movements are not elicited, the test should be repeated with the caretaker’s face as the test stimulus. It should be remembered that even children with poor vision can follow a large object without apparent difficulty, especially if only one eye is affected.
An objective measurement of visual acuity is usually possible when children reach 2.5-3 years of age. Children this age are tested using a schematic picture or other illiterate eye chart. Each eye should be tested separately. It is essential to prevent peeking. The examiner should hold the occluder in place and observe the child throughout the test. The child should be reassured and encouraged throughout the test because many children are intimidated by the procedure and fear a “bad grade” or punishment for errors.
The E test, in which a child points in the direction of the letter, is the most widely used visual acuity test for preschool children. Right-left presentations are more confusing than up-down presentations. With pretest practice, this test can be performed by most children 3-4 years of age.
An adult-type Snellen acuity chart can be used at about 5 or 6 years of age if the child knows letters. An acuity of 20/40 is generally accepted as normal for 3 yr old children. At 4 yr of age, 20/30 is typical. By 5 or 6 years of age, most children attain 20/20 vision.
Optokinetic nystagmus (the response to a sequence of moving targets; “railroad” nystagmus) can also be used to assess vision; this can be calibrated by targets of various sizes (stripes or dots) or by a rotating drum at specified distances. The VER, an electrophysiologic method of evaluating the response to light and special visual stimuli, such as calibrated stripes or a checkerboard pattern, can also be used to study visual function in selected cases. Preferential looking tests are also used for evaluating vision in infants and children who cannot respond to standard acuity tests. This is a behavioral technique based on the observation that given a choice, an infant prefers to look at patterned rather than unpatterned stimuli. Because these tests require the presence of a skilled examiner, their use is often limited to research protocols involving preverbal children.
Visual Field Assessment
Like visual acuity testing, visual field assessment must be geared to a child’s age and abilities. Formal visual field examination (perimetry and scotometry) can often be accomplished in school-aged children. The examiner must often rely on confrontation techniques and finger counting in quadrants of the visual field. In many children, only testing by attraction can be accomplished; the examiner observes a child’s response to familiar objects brought into each of the four quadrants of the visual field of each eye in turn. The child’s bottle, a favorite toy, and lollipops are particularly effective attention-getting items. These gross methods can often detect diagnostically significant field changes such as the bitemporal hemianopia of a chiasmal lesion or the homonymous hemianopia of a cerebral lesion.
Color Vision Testing
Color vision testing can be accomplished whenever a child is able to name or trace the test symbols; these may be numbers, Xs, Os, triangles, or other symbols. Color vision testing is not often necessary in young children, but parents sometimes request it, particularly if their child seems to be slow in learning colors. Parents are often reassured to know that “color-deficient” children do not misname colors and that true “color blindness” is very rare and not compatible with normal vision. Defective color vision is common in male patients but is rare in female patients. Achromatopsia, a total color vision defect with subnormal visual acuity, nystagmus, and photophobia, is encountered occasionally. A change in color discrimination can be a sign of optic nerve or retinal disease.
Pupillary Examination
Examination of the pupils includes evaluation of both, the direct and consensual reactions to light, the reaction on near gaze, and the response to reduced illumination, noting the size and symmetry of the pupils under all conditions. Special care must be taken to differentiate the reaction to light from the reaction to near gaze. A child’s natural tendency is to look directly at the approaching light, inducing the near gaze reflex when one is attempting to test only the reaction to light; accordingly, every effort must be made to control fixation. The swinging flashlight test is especially useful for detecting unilateral or asymmetric prechiasmatic afferent defects in children (see “Marcus Gunn Pupil” section in Chapter 614).
Ocular Motility
Ocular motility is tested by having a child follow an object into the various positions of gaze. Movements of each eye individually (ductions) and of the two eyes together (versions, conjugate movements, and convergence) are assessed. Alignment is judged by the symmetry of the corneal light reflexes and by the response to alternate occlusion of each eye (see discussion on cover tests for strabismus in Chapter 615).
Binocular Vision
A determination of the degree of binocular vision is commonly performed by an ophthalmologist. The Titmus test is probably the most commonly used test; a series of three-dimensional images are shown to the child while he or she wears a set of Polaroid glasses. The level of difficulty with which these images can be detected correlates with the degree of binocular vision that is present. Other tests may also be used to detect the presence of abnormal binocular adaptations secondary to poor vision or strabismus.
External Examination
The external examination begins with general inspection in good illumination noting size, shape, and symmetry of the orbits; position and movement of the lids; and position and symmetry of the globes. Viewing the eyes and lids from above aids in detecting orbital asymmetry, lid masses, proptosis (exophthalmos), and abnormal pulsations. Palpation is also important in detecting orbital and lid masses.
The lacrimal apparatus is assessed by looking for evidence of tear deficiency, overflow of tears (epiphora), erythema, and swelling in the region of the tear sac or gland. The sac is massaged to check for reflux when obstruction is suspected. The presence and position of the puncta are also checked.
The lids and conjunctivae are specifically examined for focal lesions, foreign bodies, and inflammatory signs; loss and maldirection of lashes should also be noted. When necessary, the lids can be everted in the following manner: (1) instruct the patient to look down; (2) grasp the lashes of the patient’s upper lid between the thumb and index finger of one hand; (3) place a probe, a cotton-tipped applicator, or the thumb of the other hand at the upper margin of the tarsal plate; and (4) pull the lid down and outward, everting it over the probe, using the instrument as a fulcrum. Foreign bodies commonly lodge in the concavity just above the lid margin and are exposed only by fully everting the lid.
The anterior segment of the eye is then evaluated with oblique focal illumination, noting the luster and clarity of the cornea, the depth and clarity of the anterior chamber, and the features of the iris. Transillumination of the anterior segment aids in detecting opacities and in demonstrating atrophy or hypopigmentation of the iris; these latter signs are important when ocular albinism is suspected. When necessary, fluorescein dye can be used to aid in diagnosing abrasions, ulcerations, and foreign bodies.
Biomicroscopy (Slit-Lamp Examination)
The slit-lamp examination provides a highly magnified view of the various structures of the eye and an optical section through the media of the eye—the cornea, aqueous humor, lens, and vitreous. Lesions can be identified and localized according to their depth within the eye; the resolution is sufficient to detect individual inflammatory cells in the aqueous and vitreous. With the addition of special lenses and prisms, the angle of the anterior chamber and regions of the fundus also can be examined with a slit lamp. Biomicroscopy is often crucial in trauma and in examining for iritis. It is also helpful in diagnosing many metabolic diseases of childhood.
Fundus Examination (Ophthalmoscopy)
Ophthalmoscopy is best done with the pupil dilated unless there are neurologic or other contraindications. Tropicamide (Mydriacyl) 0.5-1% and phenylephrine (Neo-Synephrine) 2.5% are recommended as mydriatics of short duration. These are safe for most children, but the possibility of adverse systemic effects must be recognized. For very small infants, more-dilute preparations may be advisable. Beginning with posterior landmarks, the disc and the macula, the four quadrants are systematically examined by following each of the major vessel groups to the periphery. More of the fundus can be seen if a child is directed to look up and down and to the right and left. Even with care, only a limited amount of the fundus can be seen with a direct or hand-held ophthalmoscope. For examination of the far periphery, an indirect ophthalmoscope is used, and full dilation of the pupil is essential.
Refraction
A test of refraction determines the refractive state of the eye: the degree of nearsightedness, farsightedness, or astigmatism. Retinoscopy provides an objective determination of the amount of correction needed and can be performed at any age. In young children, it is best done with cycloplegia. Subjective refinement of refraction involves asking patients for preferences in the strength and axis of corrective lenses; it can be accomplished in many school-aged children. Refraction and determination of visual acuity with appropriate corrective lenses in place are essential steps in deciding whether a patient has a visual defect or amblyopia. Photoscreening cameras aid ancillary medical personnel in screening for abnormal refractive errors in preverbal children. The accuracy and practical usefulness of these devices are still being investigated.
Tonometry
Tonometry measures intraocular pressure; it may be performed with a portable, stand-alone instrument or by the applanation method with the slit lamp. Alternative methods are pneumatic, electronic, or rebound tonometry. When accurate measurement of the pressure is necessary in a child who cannot cooperate, it may be performed with sedation or general anesthesia. A gross estimate of pressure can be made by palpating the globe with the index fingers placed side by side on the upper lid above the tarsal plate.
Bennett DM, Gordon G, Dutton GN. The useful field of view test, normative data in children of school age. Optom Vis Sci. 2009;86:717-721.
Committee on Practice and Ambulatory Medicine, Section on Ophthalmology; American Association of Certified Orthoptists; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology. Eye examination in infants, children, and young adults by pediatricians. Pediatrics. 2003;111:902-907.
Donahue SP, Johnson TM, Ottar W, et al. Sensitivity of photoscreening to detect high-magnitude amblyogenic factors. J AAPOS. 2002;6:86-91.
Fulton A. Screening preschool children to detect visual and ocular disorders. Arch Ophthalmol. 1992;110:1553-1554.
Isenberg SJ. Clinical application of the pupil examination in neonates. J Pediatr. 1991;118:650-652.
Powell C, Hatt SR: Vision screening for amblyopia in childhood. Cochrane Database Syst Rev (3):CD005020, 2009.
Reinecke RD. Screening 3-year olds for visual problems: are we gaining or falling behind? Arch Ophthalmol. 1986;104:245-248.
Salcido AA, Bradley J, Donahue SP. Predictive value of photoscreening and traditional screening of preschool children. J AAPOS. 2005;9:114-120.
Simons K. Preschool vision screening: rationale, methodology and outcome. Surv Ophthalmol. 1996;41:3-30.
Solouki AM, Verhoeven VJM, van Duijn CM, et al. A genome-wide association study identifies a susceptibility locus for refractive errors and myopia at 15q14. Nat Genet. 2010;42(10):897-901.
US Preventive Services Task Force. Vision screening for children 1 to 5 years of age: US preventive services task force recommendation statement. Pediatrics. 2011;127:340-346.