Bacteriuria in the Elderly
UTIs in the elderly are a common and expanding health problem (Kaye, 1980). In 2003 there were almost 34 million Americans older than 65 years (U.S. Census Bureau, 2003). As the life expectancy increases, the diagnosis, treatment, morbidity, and mortality of UTIs in the elderly will assume increasing importance.
Epidemiology
At least 20% of women and 10% of men older than 65 years have bacteriuria (Boscia and Kaye, 1987). In contrast to young adults, in whom bacteriuria is 30 times more prevalent in women than in men, the ratio in women to men with bacteriuria progressively decreases to 2:1. Most elderly patients with bacteriuria are asymptomatic; estimates among women living in nursing homes range from 17% to 55%, as compared with 15% to 31% for their male cohorts (Nicolle, 1994). The prevalence of bacteriuria in the elderly increases with age (Table 10–27) (Sourander, 1966; Brocklehurst et al, 1968) and concurrent disease (Fig. 10–38) and may exceed 50% in selective groups (Boscia and Kaye, 1987; Schaeffer, 1991). Risk factors can be compounded. In a study of 373 women and 150 men older than 68 years, 24% of functionally impaired nursing home residents had bacteriuria compared with 12% of healthy domiciliary subjects (Boscia et al, 1986). Longitudinal studies have clarified the dynamic aspect of bacteriuria in the elderly with frequent, spontaneous alteration between positive and negative urine cultures (Monane et al, 1995) (Fig. 10–39). There is only a small pool of elderly patients with persistent bacteriuria (Kaye, 1980). The incidence of asymptomatic bacteriuria is much more common than is apparent from a single survey, implying that most elderly will eventually have episodes of bacteriuria (Boscia et al, 1986).
Table 10–27 Bacteriuria in Two Population Surveys
| AGE (yr) | MEN (%) | WOMEN (%) |
|---|---|---|
| 65-70 | 2-3 | 20-21 |
| >80 | 21-22 | 23-50 |
Data from Brocklehurst JC, Dillane JB, Griffiths L, et al. Prevalence and symptomatology of urinary infection in an aged population. Gerontol Clin 1968;10:242–53; and Sourander LB. Urinary tract infections in the aged: an epidemiological study. Ann Med Intern Fenn 1966;55(Suppl. 45):7–55.
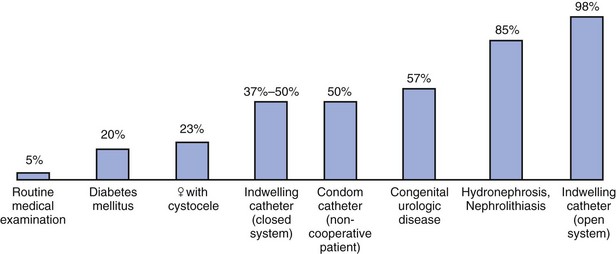
Figure 10–38 Frequency of significant bacteriuria related to underlying disease.
(Adapted from Jackson GG, Arana-Sialer JA, Andersen BR. Profiles of pyelonephritis. Arch Intern Med 1962;110:663–75.)
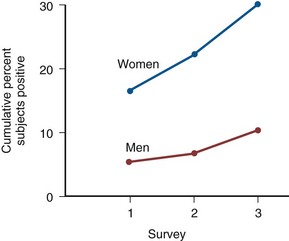
Figure 10–39 Cumulative percentage of subjects (age = 65 years) with at least one positive urine culture survey result over three surveys performed at 6-month intervals.
(From Boscia JA, Kobasa WD, Knight RA, et al. Epidemiology of bacteriuria in an elderly ambulatory population. Am J Med 1986;80:208.)
Pathogenesis
The pathophysiology of increased susceptibility is multifactorial and poorly understood. Age-related changes include decline in cell-mediated immunity, neurogenic bladder dysfunction, increased perineal soiling as a result of fecal and urinary incontinence, increased incidence of urethral catheter placement, and, in women, changes in the vaginal environment associated with estrogen depletion (Schaeffer, 1991; Raz and Stamm, 1993). Increased receptivity of uroepithelial cells (Reid et al, 1984) and a decrease in prostatic and vaginal antimicrobial factors associated with changes in pH and levels of zinc and hormones have been observed (Boscia et al, 1986). Bacteriologic characteristics of infection in the elderly differ from those in younger patients (Baldassarre and Kaye, 1991). E. coli remains the most common uropathogen, causing 75% of these infections. There is a significant increase in the incidence of Proteus, Klebsiella, Enterobacter, Serratia, and Pseudomonas species, as well as enterococci. Bacteriuria due to gram-positive bacteria is much more common in elderly men than in elderly women (Jackson et al, 1962). S. saprophyticus is not seen in this population. Polymicrobial bacteriuria is more common among the elderly (Nicolle et al, 1987). The shift in the pattern of uropathogens, the high frequency of polymicrobial infections, and antimicrobial resistance in UTIs in the elderly are due in large part to the high frequency of institutionalization and hospitalization, catheterization, and antimicrobial usage in this population (Fig. 10–40).
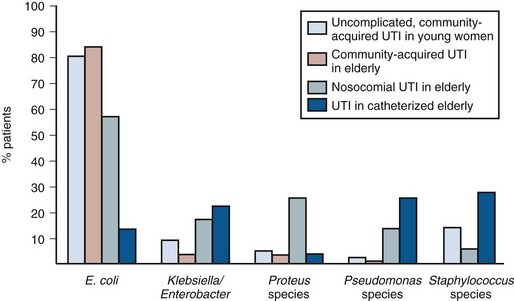
Figure 10–40 Microbiology of urinary tract infections.
(Data compiled from Stark RP, Maki DG. Bacteriuria in the catheterized patient: what quantitative level of bacteriuria is relevant? N Engl J Med 1984;311:560–4; Kunin CM. Detection, prevention, and management of urinary tract infections. 4th ed. Philadelphia: Lea & Febiger; 1987. p. xiii; Nicolle LE, Bjornson J, Harding GKM. Bacteriuria in elderly institutionalized men. N Engl J Med 1983;309:1420–5; Krieger JN, Kaiser DL, Wenzel RP. Urinary tract etiology of bloodstream infections in hospitalized patients. J Infect Dis 1983;148:57–62.)
Laboratory Diagnosis
Diagnosis of bacteriuria and UTIs in the elderly can be difficult. Urinary tract symptoms are often absent, and concomitant disease can mask or mimic UTI. Even severe upper tract infections may not be associated with fever or leukocytosis (Baldassarre and Kaye, 1991). Therefore a high index of suspicion is warranted, and diagnosis should rely on the results of a carefully obtained urinalysis and culture. The presence of greater than 105 cfu/mL of urine remains the standard for diagnosis in these patients. However, counts of 102 or more bacteria are clinically significant in catheterized specimens (Kunin, 1987; Nicolle et al, 2005).
Pyuria alone is not a good predictor nor an indication for antimicrobial treatment of bacteriuria in this population (Ouslander et al, 1996; Nicolle et al, 2005). Boscia and associates (1989) reported that more than 60% of women with pyuria of 10 WBCs/mm3 or greater (noted in midstream specimens) did not have a concurrent bacteriuria. However, the absence of pyuria was a good predictor of the absence of bacteriuria.
Because urinary tract abnormalities can often predispose and complicate bacteriuria in the elderly, a thorough urologic evaluation is warranted. Renal dysfunction, calculi, hydronephrosis, urinary retention, neurogenic bladder dysfunction, and other abnormalities should be identified by serum creatinine measurement, excretory urography, CT, ultrasonography, urodynamics, and/or cystoscopy. The timing and sequence of these tests should be dictated by the clinical setting.
Significance of Screening Bacteriuria
Screening for asymptomatic bacteriuria in elderly residents in the community or long-term care facilities is not recommended (Nicolle et al, 1983; Nordenstam et al, 1986; Boscia et al, 1987; Abutryn et al, 1994). There is no documented relationship between asymptomatic bacteriuria and uncomplicated UTIs and worsening renal function in this population. The treatment of asymptomatic bacteriuria to improve incontinence has not been justified (Baldassarre and Kaye, 1991; Ouslander et al, 1995). Although studies have demonstrated decreased survival in bacteriuric patients compared with nonbacteriuric control subjects, it is unclear whether increased mortality rates and bacteriuria are causally related (Baldassarre and Kaye, 1991; Abutryn et al, 1994).
Studies that have found a significantly increased mortality among persons with bacteriuria have looked at populations that were heterogeneous in terms of age and underlying disease (Dontas et al, 1981; Latham et al, 1985). An age difference of only 2 years increases mortality by 20% (Dontas et al, 1968). Therefore, in the studies mentioned previously (Dontas et al, 1968) and others (Abutryn et al, 1994), it is not clear how much of the observed association between bacteriuria and mortality was due to differences in age between the bacteriuric and the abacteriuric groups. In a study of bacteriuria and mortality in a homogeneous 70-year-old population, the association between bacteriuria and mortality was weaker and linked to fatal diseases not attributable to bacteriuria (Dontas et al, 1968). Nicolle and associates (1987) randomized institutionalized women with bacteriuria to treatment or observation and followed these patients for more than 1 year. Treatment did not result in improved survival and was associated with a number of adverse effects.
Bacteriuria that leads to UTIs in elderly subjects in the presence of underlying structural urinary tract abnormalities (e.g., obstruction with hydronephrosis) or systemic conditions (e.g., severe diabetes mellitus) are clinically significant, can lead to renal failure, and require prompt therapy. In addition, UTIs caused by urea-splitting bacteria, such as Proteus or Klebsiella species that cause formation of infection stones, may also lead to severe renal damage.
Sepsis and its sequelae (sepsis syndrome and septic shock) are increasingly common in the elderly. This is in part due to the aggressive use of catheters (Kunin et al, 1992) and other invasive equipment, implantation of prosthetic devices, and the administration of chemotherapy to cancer patients or corticosteroids in other immunosuppressed patients with organ transplants or inflammatory diseases. In addition, modern medical care has given longer life spans to the elderly and patients with metabolic, neoplastic, or immunodeficiency disorders, who remain at increased risk for infection.
Management
Prospective randomized comparative trials of antimicrobial or no therapy in elderly male and female nursing home residents with asymptomatic bacteriuria consistently document no benefit of antimicrobial therapy. There was no decrease in symptomatic episodes and no improvement in survival. In fact, treatment with antimicrobial therapy increases the occurrence of adverse drug effects and reinfection with resistant organisms and increases the cost of treatment. Therefore asymptomatic bacteriuria in elderly residents of long-term care facilities should not be treated with antimicrobial agents.
If patients present with lower tract symptoms, 7 days of therapy is recommended. For individuals presenting with fever or more severe systemic infection 10 to 14 days of therapy is recommended. The goal in this population is to eliminate symptoms but not sterilize the urine (McMurdo and Gillespie, 2000).
The 10% to 15% decrease in susceptibility of uropathogens to β-lactams, TMP-SMX, and fluoroquinolones in isolates from nursing home residents is disturbing and most likely due to a pattern of empirical prescribing in the nursing homes. In contrast, the susceptibility of isolates from patients with acute uncomplicated UTI in an outpatient setting has not changed appreciably in 10 years. The difference in susceptibility between the isolates from the outpatient and nursing home settings can be attributed to the presence of additional risk factors for antimicrobial resistance in the latter group. These risk factors include frequent antimicrobial usage, overcrowding, underlying pathology, and the presence of catheters and other invasive devices. Antimicrobial use needs to be guided by current surveillance studies of targeted uropathogenic bacteria and implemented (Vromen et al, 1999).
The elderly population is more susceptible than young patients to the toxic and adverse effects of antimicrobial agents (Grieco, 1980; Carty et al, 1981; Boscia et al, 1986) because the metabolism and excretion of antimicrobial agents may be impaired and the resulting increased serum levels can further damage renal function. Interactions with other medications can occur (Stahlmann and Lode, 2003). The safety margin between therapeutic and toxic doses is significantly narrowed. Therefore antimicrobial agents must be used judiciously, and dosing and drug levels should be carefully monitored.
The fluoroquinolones are effective in this population, and the side effects are not more apparent than in a younger population. However, fluoroquinolones can cause QT interval prolongation; therefore they should be avoided in patients with known prolongation of the QT interval, patients with uncorrected hypokalemia or hypomagnesemia, and patients receiving some antiarrhythmic agents (Stahlmann and Lode, 2003).
Chondrotoxicity of fluoroquinolones has led to restricted use in pediatric patients, but there is no indication that similar effects could occur in joint cartilage of adults. Tendinitis and tendon ruptures have occurred in rare cases. Chronic renal diseases, concomitant use of corticosteroids, and age older than 60 years have been recognized as risk factors for fluoroquinolone-induced tendon disorders (Stahlmann and Lode, 2003).
Key Points
Bacteriuria in the Elderly
Catheter-Associated Bacteriuria
Catheter-associated bacteriuria is the most common hospital-acquired infection, accounting for up to 40% of such infections and more than 1 million per year (Haley et al, 1985; Stamm, 1991). The development of bacteriuria in the presence of an indwelling catheter is inevitable and occurs at an incidence of approximately 10% per day of catheterization. Sterile and clean intermittent catheterization has been associated with rates of bacteriuria ranging from 1% to 3% per catheterization (Warren, 1997). The most important risk factors associated with increased likelihood of developing catheter-associated bacteriuria are duration of catheterization, female gender, absence of systemic antimicrobial agents, and catheter-care violations (Stamm, 1991). Most catheter-associated UTIs are asymptomatic. In patients with short-term catheter placement, only 10% to 30% of bacteriuric episodes produce typical symptoms of acute infection (Haley et al, 1981; Hartstein et al, 1981). Similarly, although patients with long-term catheters are bacteriuric, the incidence of febrile episodes occurs at a rate of only 1 per 100 days of catheterization (Warren, 1991). The extra direct cost associated with catheter-associated UTIs is about $600 per year per patient. The nosocomial costs for E. coli infections with relatively susceptible strains are considerably lower than for those caused by resistant gram-negative bacteria, which often require expensive parenteral antimicrobial therapy (Tambyah et al, 2002). Recently, the Center for Medicare Services (CMS) announced that they will no longer reimburse hospitals for the extra costs resulting from catheter-associated UTIs.
Pathogenesis
Bacteria enter the urinary tract of a catheterized patient by several routes. Bacteria can be introduced at the time of initial catheter placement by either mechanical inoculation of urethral bacteria or contamination from poor technique. Subsequently the bacteria most commonly gain access via a periurethral or intraluminal route (Stamm, 1991). In women, periurethral entry is the most prevalent. Daifuku and Stamm (1984) found that among 18 women who developed catheter-associated bacteriuria, 12 had antecedent urethral colonization with the infecting strain. Bacteria may also enter the drainage bag and follow the intraluminal route to the bladder. This route is particularly common in patients who are clustered among other patients with indwelling catheters (Maizels and Schaeffer, 1980; Tambyah et al, 1999).
The urinary catheter system provides a unique environment that allows for two distinct populations of bacteria: those that grow within the urine and another population that grows on the catheter surface. A biofilm represents a microbial environment of bacteria embedded in an extracellular matrix of bacterial products and host proteins that often lead to catheter encrustation (Stamm, 1991; Bonadio et al, 2001). Certain bacteria, particularly of the Pseudomonas and Proteus species, are adept at biofilm growth, which may explain their higher incidence in this clinical setting (Mobley and Warren, 1987). The uropathogens isolated from the catheterized urinary tract often differ from those found in noncatheterized ambulatory patients. E. coli is still the most common organism isolated, but Pseudomonas, Proteus, and Enterococcus species are very prevalent (Warren, 1991). In patients with long-term catheterization of more than 30 days, the bacteriuria is usually polymicrobial and the presence of four or five pathogens is not uncommon (Warren et al, 1982). Although certain species may persist for long periods, the bacterial populations in these patients tend to be dynamic.
Clinical Presentation
Most patients are asymptomatic. Suprapubic discomfort and development of fever, chills, or flank pain may indicate a symptomatic UTI.
Laboratory Diagnosis
Significant bacteriuria in patients with catheters is present when greater than 100 cfu/mL is present because even this low level progresses to greater than 105 cfu/mL in almost all patients (Maizels and Schaeffer, 1980; Stark and Maki, 1984). Pyuria is not a discriminate indicator of infection in this population.
Management
Careful aseptic insertion of the catheter and maintenance of a closed dependent drainage system are essential to minimize development of bacteriuria. The catheter-meatal junction should be cleaned daily with water, but antimicrobial agents should be avoided because they lead to colonization with resistant pathogens, such as Pseudomonas.
Incorporation of silver oxide (Schaeffer et al, 1988) or silver alloy (Saint et al, 1998) into the catheter and hydrogen peroxide into the drainage bag has been reported to decrease the incidence of bacteriuria in some studies (Schaeffer et al, 1988) but not in other populations (Stamm, 1991). The major benefit of silver alloy is in decreasing the likelihood of bacteriuria in hospitalized adults catheterized for the short-term (Saint et al, 2000; Newton et al, 2002; Brosnahan et al, 2004). If an asymptomatic catheterized patient has had an indwelling catheter for 3 or more days, and will have the catheter removed, a dipstick test can be used to rule out bacteriuria (Tissot et al, 2001). Concurrent administration of systemic antimicrobial agents transiently decreases the incidence of bacteriuria associated with short-term catheterization, but after 3 to 4 days the incidence of bacteriuria is similar to the rate in catheterized patients not taking systemic antimicrobials agents, and the prevalence of resistant bacteria and side effects is substantial. The concept of instilling nonvirulent bacteria into the bladder to completely block colonization and infection by pathogens has been tested in patients with spinal cord injuries (Hull et al, 2000). Patients successfully colonized with the nonvirulent strain had reduced symptomatic UTI and a subjective improvement in quality of life.
Patients with indwelling catheters should be treated only if they become symptomatic (e.g., febrile). Urine cultures should be performed before initiating antimicrobial therapy. The antimicrobial agent should be discontinued within 48 hours of resolution of the infection. If the catheter has been indwelling for several weeks, encrustation may shelter bacteria from the antimicrobial agent; therefore the catheter should be changed.
When a catheter is to be removed and there is a high probability of bacteriuria or the dipstick test is positive, a culture should be obtained 24 hours before removal (Tissot et al, 2001). If the probability is low or the dipstick is negative, a culture may not be necessary. The patient should be started on empirical antimicrobial therapy such as TMP-SMX or a fluoroquinolone just before decatheterization and maintained on therapy for 2 days. A post-therapy culture should be obtained 7 to 10 days later to confirm the eradication of the bacteriuria.
Key Points
Catheter-Associated Bacteriuria
Management of UTI in Patients with Spinal Cord Injury
Patients with spinal cord injury have unique concerns that affect the risk, diagnosis, and management of UTIs, which are all considered complicated.
Epidemiology
UTIs are among the most common urologic complications of spinal cord injury. It has been estimated that approximately 33% of spinal cord-injured patients have bacteriuria at any time (Stover et al, 1989) and that eventually almost all of spinal cord-injured patients will become bacteriuric and many will suffer significant morbidity and mortality. One prospective study of patients on intermittent catheterization or condom catheterization reported an incidence of significant bacteriuria of 18 episodes per person per year and an annual incidence of febrile UTIs of 1.8 per person per year (Waites et al, 1993). In addition, UTI is the most common cause of fever in the spinal cord–injured patient (Beraldo et al, 1993). The 1992 National Institute on Disability and Rehabilitation Research Consensus Conference (1993) examined the problems associated with UTIs in spinal cord–injured patients. Among the risk factors identified were impaired voiding, overdistention of the bladder, elevated intravesical pressure, increased risk of urinary obstruction, vesicoureteral reflux, instrumentation, and increased incidence of stones. Other factors that have been implicated are decreased fluid intake, poor hygiene, perineal colonization, decubiti and other evidence of local tissue trauma, and reduced host defense associated with chronic illness (Gilmore et al, 1992; Waites et al, 1993).
Pathogenesis
The method of bladder management has profound impact on UTI. The National Institute on Disability and Rehabilitation Research Consensus Conference (1993) noted that indwelling catheters were most likely to lead to UTI and that the vast majority of patients with an indwelling catheter for 30 days are bacteriuric. Suprapubic catheters and indwelling urethral catheters eventually have an equivalent infection rate (Kunin et al, 1987; Tambyah and Maki, 2000; Biering-Sorensen, 2002). However, the onset of bacteriuria may be delayed using a suprapubic catheter compared with a urethral catheter. During a 2-year period, 170 patients with spinal cord injury were evaluated regarding type of urinary drainage and infection (Warren et al, 1982). In patients using indwelling urethral catheters, all urine cultures were positive. The corresponding values for the suprapubic catheter group were 44%. Condom drainage systems are also associated with an incidence of bacteriuria from 63% (Dukes, 1928) to almost 100% (Pyrah et al, 1955).
Since its introduction by Lapides and colleagues (1972), clean (but not sterile) intermittent catheterization (CIC) has earned general recognition in the management of spinal cord injury patients (National Institute on Disability and Rehabilitation Research, 1993). Although never rigorously compared with indwelling urethral catheterization, CIC has been shown to decrease lower tract complications by maintaining low intravesical pressure and reducing the incidence of stones (Stover et al, 1989). CIC also appears to reduce complications associated with an indwelling catheter, such as UTI, fever, bacteremia, and local infections such as epididymitis and prostatitis. Weld and Dmochowski (2000) followed 316 patients with spinal cord injury with different bladder management for a mean of 18.3 years and recorded all complications. The CIC group had statistically significantly lower complication rates compared with the urethral catheterization group and no significantly higher complication rates relative to all other management methods for each type of complication studied. Thus it is generally agreed that CIC places patients with spinal cord injury at the lowest risk for significant long-term urinary tract complications (Stamm, 1975).
There is conflicting evidence over the value of sterile versus nonsterile or “no touch” methods of CIC. Some studies have reported a lower incidence of infection in patients treated with sterile techniques (Foley, 1929), whereas others have not (Pyrah et al, 1955; Nyren et al, 1981). Bennett and coworkers (1997) reported on a sterile method of CIC that uses an introducer tip to bypass the distal 1.5 cm of the urethra and showed a significant decrease in UTI with the use of the urethral introducer tip. Different types of catheters have been used for CIC. The low-friction catheters might be less traumatic for the urethra (Casewell and Phillips, 1977; Garibaldi et al, 1980), but their impact on bacteriuria and UTI has to be studied.
Clinical Presentation
The majority of patients with spinal cord injury with bacteriuria are asymptomatic. Because of a loss of sensation, patients usually do not experience frequency, urgency, or dysuria. More often they complain of flank, back, or abdominal discomfort, leakage between catheterizations, increased spasticity, malaise, lethargy, and/or cloudy, malodorous urine. UTI is the most common cause of fever in spinal cord–injured patients (Beraldo et al, 1993).
Bacteriology and Laboratory Diagnosis
Urinalysis will show bacteriuria and pyuria. Pyuria is not diagnostic of infections, because it may occur from the irritative effects of the catheter. The National Institute on Disability and Rehabilitation Research Consensus Statement (1993) recommended the following criteria for the diagnosis of significant bacteriuria in spinal cord–injured patients. Any detectable bacteria from indwelling or suprapubic catheter aspirates was considered significant because the vast majority of patients with an indwelling catheter and low-level bacteriuria showed an increase to greater than 105 cfu/mL within a short period of time (Cardenas and Hooton, 1995). For patients on CIC, greater than or equal to 102 cfu/mL was considered significant. For catheter-free males, a clean voided specimen showing greater than or equal to 104 cfu/mL was considered significant.
Bacteriuria in patients with spinal cord injury differs from that in patients with intact spinal cords in its etiology, complexity, and antimicrobial susceptibility and is influenced by the type and duration of catheterization. E. coli is isolated in approximately 20% of patients. Enterococci, P. mirabilis, and Pseudomonas are more common among spinal cord–injured patients than patients with intact spinal cords. Other common organisms are Klebsiella species, Serratia species, Staphylococcus, and Candida species. Most bacteriuria in short-term catheterization is of a single organism, whereas patients catheterized for longer than a month will usually demonstrate a polymicrobial flora caused by a wide range of gram-negative and gram-positive bacterial species (Edwards et al, 1983). Such specimens commonly have two to four bacterial species, each at concentrations of 105 cfu/mL or more (Monson and Kunin, 1974; Nickel et al, 1987). Some may have up to six to eight species at that concentration (Monson and Kunin, 1974). This phenomenon is due to an incidence of new episodes of bacteriuria approximately every 2 weeks and the ability of these strains to persist for weeks and months in the catheterized urinary tract (Edwards et al, 1983; Gabriel et al, 1996). Two of the most persistent species are E. coli and Providencia stuartii. P. stuartii is rarely found outside the long-term catheterized urinary tract and may use the catheter itself as a niche (Lindberg et al, 1975; Hockstra, 1999).
Management
Because of the diverse flora and high probability of bacterial resistance, a urine culture must be obtained before initiating empirical therapy. For afebrile patients, an oral fluoroquinolone is the agent of choice (Cardenas and Hooton, 1995). β-Lactams, TMP-SMX, and nitrofurantoin are not recommended because of the high prevalence of bacterial resistance to these drugs. An indwelling catheter should be changed to ensure maximal drainage and eliminate bacterial foci in catheter encrustations. Spinal cord–injured patients with fever or chills are usually admitted and treated with a parenteral aminoglycoside and a penicillin or a third-generation cephalosporin (Cardenas and Hooton, 1995). In this patient population, consultation with a physician with expertise in antimicrobial management may be necessary, especially in a patient with recurrent infections.
If clinical improvement does not occur within 24 to 48 hours, reculture and adjustment of antimicrobial therapy based on the initial culture and susceptibility should be performed. Imaging studies should be obtained to rule out obstruction, stones, and abscess. The duration of therapy is not established, but 4 to 5 days is recommended for the mildly symptomatic patient and 10 to 14 days for sicker patients (Cardenas and Hooton, 1995). Post-therapy cultures are usually not necessary because asymptomatic recolonization is common and not clinically significant. However, if a urea-splitting bacterium is identified, a follow-up culture should be obtained to ensure its eradication. Spinal cord–injured patients with recurrent symptomatic UTIs should undergo urinary tract imaging and urodynamic testing and a review of their bladder management program with particular attention to catheter drainage, intermittent catheterization techniques, and frequency of intermittent catheterization or voiding schedule (Cardenas and Hooton, 1995).
Antimicrobial prophylaxis is not supported for most patients who have neurogenic bladder caused by spinal cord injury (Morton et al, 2002). Antimicrobial prophylaxis did not significantly decrease symptomatic UTIs and resulted in an approximately twofold increase in antimicrobial-resistant bacteria.
Recurrent UTIs may be associated with high storage pressures, and intervention to decrease storage pressure may decrease the incidence of symptomatic UTI. Evidence from studies in spinal cord–injured patients suggests that bladder catheterization for longer than 10 years is associated with an increased risk of carcinoma of the bladder. West and colleagues (1999) examined two databases with more than 33,000 spinal cord–injured patients and identified 130 patients with bladder cancer (0.4%) during a 5-year period. Several risk factors for bladder cancer have been proposed. Vereczky and associates (cited in Weyrauch and Bassett, 1951) tested different risk factors based on the outcome of 153 spinal cord-injured patients in which 7 were diagnosed with bladder cancer. Of a total of 31 possible predictors, only duration of catheterization was significant. Chronic infection and inflammation of the bladder mucosa could be the carcinogenic stimulus in these patients (Pyrah et al, 1955). Nitrosamines produced in infected urine have also been implicated (Najenson et al, 1969).
For further discussion of spinal cord injury and urinary infection, see Chapter 65.
Key Points
Management of UTI in Patients with Spinal Cord Injury
Other Infections
Fournier Gangrene
Fournier gangrene is a potentially life-threatening form of necrotizing fasciitis involving the male genitalia. It is also known as idiopathic gangrene of the scrotum, streptococcal scrotal gangrene, perineal phlegmon, and spontaneous fulminant gangrene of the scrotum (Fournier, 1883, 1884). As originally reported by Baurienne in 1764, and by Fournier in 1883, it was characterized by an abrupt onset of a rapidly fulminating genital gangrene of idiopathic origin in previously healthy young patients that resulted in gangrenous destruction of the genitalia. The disease now differs from these descriptions in that it involves a broader age range, including older patients (Bejanga, 1979; Wolach et al, 1989), follows a more indolent course, and has a less abrupt onset; and, in approximately 95% of the cases, a source can now be identified (Macrea, 1945; Burpee and Edwards, 1972; Kearney and Carling, 1983; Jamieson et al, 1984; Spirnak et al, 1984).
Infection most commonly arises from the skin, urethra, or rectal regions. An association between urethral obstruction associated with strictures and extravasation and instrumentation has been well documented. Predisposing factors include diabetes mellitus, local trauma, paraphimosis, periurethral extravasation or urine, perirectal or perianal infections, and surgery such as circumcision or herniorrhaphy. In cases originating in the genitalia the infecting bacteria probably pass through the Buck fascia of the penis and spread along the dartos fascia of the scrotum and penis, the Colles fascia of the perineum, and the Scarpa fascia of the anterior abdominal wall. In view of the typical foul odor associated with this condition, a major role for anaerobic bacteria is likely. Wound cultures generally yield multiple organisms, implicating anaerobic-aerobic synergy (Meleney, 1933; Miller, 1983; Cohen, 1986). Mixed cultures containing facultative organisms (E. coli, Klebsiella, enterococci) along with anaerobes (Bacteroides, Fusobacterium, Clostridium, microaerophilic streptococci) have been obtained from the lesions.
Clinical Presentation
Patients frequently have a history of recent perineal trauma, instrumentation, urethral stricture associated with sexually transmitted disease, or urethral cutaneous fistula. Pain, rectal bleeding, and a history of anal fissures suggest a rectal source of infection. Dermal sources are suggested by history of acute and chronic infections of the scrotum and spreading recurrent hidradenitis suppurativa or balanitis.
The infection commonly starts as cellulitis adjacent to the portal of entry. Early on, the involved area is swollen, erythematous, and tender as the infection begins to involve the deep fascia. Pain is prominent, and fever and systemic toxicity are marked (Paty and Smith, 1992). The swelling and crepitus of the scrotum quickly increase, and dark purple areas develop and progress to extensive gangrene. If the abdominal wall becomes involved in an obese patient with diabetes, the process can spread very rapidly. Specific genitourinary symptoms associated with the condition include dysuria, urethral discharge, and obstructed voiding. Alterations in mental status, tachypnea, tachycardia, and temperature greater than 38.3° C (101° F) or less than 35.6° C (96° F) suggest gram-negative sepsis.
Laboratory Diagnosis and Radiologic Findings
Anemia occurs secondary to a decreased functioning erythrocyte mass caused by thrombosis and ecchymosis coupled with decreased production secondary to sepsis (Miller, 1983). Elevated serum creatinine levels, hyponatremia, and hypocalcemia are common. Hypocalcemia is believed to be secondary to bacterial lipases that destroy triglycerides and release free fatty acids that chelate calcium in its ionized form.
Because crepitus is often an early finding, a plain film of the abdomen may be helpful in identifying air. Scrotal ultrasonography is also useful in this regard. Biopsy of the base of an ulcer is characterized by superficially intact epidermis, dermal necrosis, and vascular thrombosis and polymorphonuclear leukocyte invasion with subcutaneous tissue necrosis. Stamenkovic and Lew (1984) noted that the use of frozen sections within 21 hours after the onset of symptoms could confirm a diagnosis earlier and lead to early institution of appropriate treatment.
Management
Prompt diagnosis is critical because of the rapidity with which the process can progress. The clinical differentiation of necrotizing fasciitis from cellulitis may be difficult because the initial signs including pain, edema, and erythema are not distinctive. However, the presence of marked systemic toxicity out of proportion to the local finding should alert the clinician. Intravenous hydration and antimicrobial therapy are indicated in preparation for surgical debridement. Antimicrobial regimens include combinations of ampicillin plus sulbactam or a parenteral third-generation cephalosporin such as ceftriaxone, gentamicin, and clindamycin. If there is no response to clindamycin, chloramphenicol may be used.
Immediate debridement is essential. In the patient in whom diagnosis is clearly suspected on clinical grounds (deep pain with patchy areas of surface hypoesthesia or crepitation, or bullae and skin necrosis), direct operative intervention is indicated. Extensive incision should be made through the skin and subcutaneous tissues, going beyond the areas of involvement until normal fascia is found. Necrotic fat and fascia should be excised, and the wound should be left open. A second procedure 24 to 48 hours later is indicated if there is any question about the adequacy of initial debridement. Orchiectomy is almost never required, because the testes have their own blood supply independent of the compromised fascial and cutaneous circulation to the scrotum. Suprapubic diversion should be performed in cases in which urethral trauma or extravasation is suspected. Colostomy should be performed if there is colonic or rectal perforation. Hyperbaric oxygen therapy has shown some promise in shortening hospital stays, increasing wound healing, and decreasing the gangrenous spread when used in conjunction with debridement and antimicrobial agents (Paty and Smith, 1992). Once wound healing is complete, reconstruction, for example, using myocutaneous flaps, improves cosmetic results.
Outcome
The mortality rate averages approximately 20% (Cohen, 1986; Baskin et al, 1990; Clayton et al, 1990) but ranges from 7% to 75%. Higher mortality rates are found in diabetics, alcoholics, and those with colorectal sources of infection who often have a less typical presentation, greater delay in diagnosis, and more widespread extension. Regardless of the presentation, Fournier gangrene is a true urologic emergency that demands early recognition, aggressive treatment with antimicrobial agents, and surgical debridement to reduce morbidity and mortality.
Periurethral Abscess
Periurethral abscess is a life-threatening infection of the male urethra and periurethral tissues. Initially, the area of involvement can be small and localized by Buck fascia. However, when Buck fascia is penetrated there can be extensive necrosis of the subcutaneous tissue and fascia. Fasciitis can spread as far as the buttocks posteriorly and the clavicle superiorly. Rapid diagnosis and treatment are essential to reduce the morbidity and high mortality historically associated with this disease.
Pathogenesis
Periurethral abscess is frequently a sequela of gonorrhea, urethral stricture disease, or urethral catheterization. Frequent instrumentation is also associated with periurethral abscess formation. The source of the infecting organism is the urine. Gram-negative rods, enterococci, and anaerobes are most frequently identified. The presence of multiple organisms is common. Anaerobes, normal residents of the male urethra, are also frequently found in wound cultures.
Clinical Presentation
Presenting signs and symptoms include scrotal swelling in 94% of patients, fever (70%), acute urinary retention (19%), spontaneously drained abscess (11%), and dysuria or urethral discharge (5% to 8%). The average interval between initial symptoms and presentation is 21 days. Urinalysis of the first glass specimen reveals pyuria and bacteriuria.
Management
Treatment consists of immediate suprapubic urinary drainage and wide debridement. Antimicrobial therapy with an aminoglycoside and a cephalosporin is usually adequate for empirical coverage. More selective antimicrobial therapy can be instituted when the antimicrobial susceptibility of the organisms is available. Perineal urethrostomy or chronic suprapubic diversion occasionally has been helpful to prevent recurrences, and it should be considered in patients with diffuse stricture disease. The presence of a malignancy is unusual, but biopsy is important.
Anderson GG, Dodson KW, Hooton TM, et al. Intracellular bacterial communities of uropathogenic Escherichia coli in urinary tract pathogenesis. Trends Microbiol. 2004;12:424-430.
Asscher AW, Chick S, Radford N, et al. Natural history of asymptomatic bacteriuria in nonpregnant women. In: Brumfitt W, Asscher AW, editors. Urinary tract infection. London: University Press; 1973:51.
Dajani AS, Taubert KA, Wilson W, et al. Prevention of bacterial endocarditis: recommendations by the American Heart Association. JAMA. 1997;277:1794-1801.
Eknoyan G, Qunibi WY, Grissom RT, et al. Renal papillary necrosis: an update. Medicine (Baltimore). 1982;61:55-73.
Elliott TS, Reed L, Slack RC, et al. Bacteriology and ultrastructure of the bladder in patients with urinary tract infections. J Infect. 1985;11:191-199.
Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002;113(Suppl. 1A):5S-13S.
Gupta K, Scholes D, Stamm WE. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999;281:736-738.
Hooton TM, Stamm WE. Management of acute uncomplicated urinary tract infection in adults. Med Clin North Am. 1991;75:339-357.
Hultgren SJ, Porter TN, Schaeffer AJ, et al. Role of type 1 pili and effects of phase variation on lower urinary tract infections produced by Escherichia coli. Infect Immun. 1985;50:370-377.
Hultgren SJ, Schwan WR, Schaeffer AJ, et al. Regulation of production of type 1 pili among urinary tract isolates of Escherichia coli. Infect Immun. 1986;54:613-620.
Mabeck CE. Treatment of uncomplicated urinary tract infection in non-pregnant women. Postgrad Med J. 1972;48:69-75.
Martinez JJ, Hultgren SJ. Requirement of Rho-family GTPases in the invasion of type 1-piliated uropathogenic Escherichia coli. Cell Microbiol. 2002;4:19-28.
Mulvey MA. Adhesion and entry of uropathogenic Escherichia coli. Cell Microbiol. 2002;4:257-271.
Mulvey MA, Lopez-Boado YS, Wilson CL, et al. Induction and evasion of host defenses by type 1-piliated uropathogenic Escherichia coli. Science. 1998;282:1494-1497.
Mulvey MA, Schilling JD, Martinez JJ, et al. Bad bugs and beleaguered bladders: interplay between uropathogenic Escherichia coli and innate host defenses. Proc Natl Acad Sci U S A. 2000;97:8829-8835.
National Institute on Disability and Rehabilitation Research. The prevention and management of urinary tract infections among people with spinal cord injuries. National Institute on Disability and Rehabilitation Research consensus statement. January 27–29, 1992. SCI Nurs. 1993;10:49-61.
Nicolle LE, Bradley S, Colgan R, et al. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40:643-654.
Schaeffer AJ, Jones JM, Dunn JK. Association of in vitro Escherichia coli adherence to vaginal and buccal epithelial cells with susceptibility of women to recurrent urinary-tract infections. N Engl J Med. 1981;304:1062-1066.
Stamey TA. Pathogenesis and treatment of urinary tract infections. Baltimore: Williams & Wilkins; 1980.
Stamey TA, Govan DE, Palmer JM. The localization and treatment of urinary tract infections: the role of bactericidal urine levels as opposed to serum levels. Medicine (Baltimore). 1965;44:1-36.
Stamm WE. Recent developments in the diagnosis and treatment of urinary tract infections. West J Med. 1982;137:213-220.
Stamm WE. Catheter-associated urinary tract infections: epidemiology, pathogenesis, and prevention. Am J Med. 1991;91:65S-71S.
Turck M, Goffe B, Petersdorf RG. The urethral catheter and urinary tract infection. J Urol. 1962;88:834-837.
Vromen M, van der Ven AJ, Knols A, et al. Antimicrobial resistance patterns in urinary isolates from nursing home residents: fifteen years of data reviewed. J Antimicrob Chemother. 1999;44:113-116.
Warren JW, Abrutyn E, Hebel JR, et al. Guidelines for antimicrobial treatment of uncomplicated acute bacterial cystitis and acute pyelonephritis in women. Infectious Diseases Society of America (IDSA). Clin Infect Dis. 1999;29:745-758.
Abarbanel J, Engelstein D, Lask D, et al. Urinary tract infection in men younger than 45 years of age: is there a need for urologic investigation? Urology. 2003;62:27-29.
Abdou NI, NaPombejara C, Sagawa A, et al. Malakoplakia: evidence for monocyte lysosomal abnormality correctable by cholinergic agonist in vitro and in vivo. N Engl J Med. 1977;297:1413-1419.
Abutryn E, Mossey J, Berlin JA, et al. Does asymptomatic bacteriuria predict mortality and does antimicrobial treatment reduce mortality in elderly ambulatory women? Ann Intern Med. 1994;120:827-833.
Alonso MD, Marcos C, Davila I, et al. Hypersensitivity to trimethoprim. Allergy. 1992;47:340-342.
American Urological Association, American Academy of Orthopaedic Surgeons. Antibiotic prophylaxis for urological patients with total joint replacements. J Urol. 2003;169:1796-1797.
Anderson G, Dodson K, Hooton T, et al. Intracellular bacterial communities of uropathogenic Escherichia coli in urinary tract pathogenesis. Trends Microbiol. 2004;12:424-430.
Anderson G, Martin S, Hultgren S. Host subversion by formation of intracellular bacterial communities in the urinary tract. Microbes Infect. 2004;6:1094-1101.
Anderson K, McAninch J. Renal abscesses: classification and review of 40 cases. Urology. 1980;16:333-338.
Andrews SJ, Brooks PT, Hanbury DC, et al. Ultrasonography and abdominal radiography versus intravenous urography in investigation of urinary tract infection in men: prospective incident cohort study. BMJ. 2002;324:454-456.
Anhalt MA, Cawood CD, Scott RJr. Xanthogranulomatous pyelonephritis: a comprehensive review with report of 4 additional cases. J Urol. 1971;105:10-17.
Aronson M, Medalia O, Schori L, et al. Prevention of colonization of the urinary tract of mice with Escherichia coli by blocking of bacterial adherence with methyl alpha-D-mannopyranoside. J Infect Dis. 1979;139:329-332.
Asscher AW. The challenge of urinary tract infection. New York: Academy Press; 1980.
Asscher A, Chick S, Radford N, et al. Natural history of bacteriuria in nonpregnant women. In: Brumfitt W, Asscher A, editors. Urinary tract infection. London: University Press; 1973:51.
Asscher A, Sussman M, Weiser R. Bacterial growth in human urine. In: O’Grady F, Brumfitt W, editors. Urinary tract infection. London: Oxford University Press, 1968.
Avorn J, Monane M, Gurwitz JH, et al. Reduction of bacteriuria and pyuria after ingestion of cranberry juice. JAMA. 1994;271:751-754.
Backhed F, Alsen B, Roche N, et al. Identification of target tissue glycosphingolipid receptors for uropathogenic, F1C-fimbriated Escherichia coli and its role in mucosal inflammation. J Biol Chem. 2002;277:18198-18205.
Baijal SS, Basarge N, Srinadh ES, et al. Percutaneous management of renal hydatidosis: a minimally invasive therapeutic option. J Urol. 1995;153:1199-1201.
Bailey RR, Little PJ, Rolleston GL. Renal damage after acute pyelonephritis. BMJ. 1969;1:550-551.
Baldassarre JS, Kaye D. Special problems of urinary tract infection in the elderly. Med Clin North Am. 1991;75:375-390.
Bartlett JG, Gorbach SL. Anaerobic bacteria in suppurative infections of the male genitourinary system. J Urol. 1981;125:376-378.
Baskin LS, Carroll PR, Cattolica EV, et al. Necrotising soft tissue infections of the perineum and genitalia. Bacteriology, treatment and risk assessment. Br J Urol. 1990;65:524-529.
Baumgarten DA, Baumgartner BR. Imaging and radiologic management of upper urinary tract infections. Urol Clin North Am. 1997;24:545-569.
Beeson PB, Guze LB. Experimental pyelonephritis. I. Effect of ureteral ligation on the course of bacterial infection in the kidney of the rat. J Exp Med. 1956;104:803-815.
Behr MA, Drummond R, Libman MD, et al. Fever duration in hospitalized acute pyelonephritis patients. Am J Med. 1996;101:277-280.
Bejanga BI. Fournier’s gangrene. Br J Urol. 1979;51:312-316.
Bennett CJ, Young MN, Razi SS, et al. The effect of urethral introducer tip catheters on the incidence of urinary tract infection outcomes in spinal cord injured patients. J Urol. 1997;158:519-521.
Bent S, Nallamothu BK, Simel DL, et al. Does this woman have an acute uncomplicated urinary tract infection? JAMA. 2002;287:2701-2710.
Beraldo PS, Neves EG, Alves CM, et al. Pyrexia in hospitalised spinal cord injury patients. Paraplegia. 1993;31:186-191.
Bercowsky E, Shalhav AL, Portis A, et al. Is the laparoscopic approach justified in patients with xanthogranulomatous pyelonephritis? Urology. 1999;54:437-442. discussion 442–433
Bernard GR, Vincent JL, Laterre PF, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001;344:699-709.
Berry A, Barratt A. Prophylatic antibiotic use in transurethral prostatic resection: a meta-analysis. J Urol. 2002;167:571-577.
Best CD, Terris MK, Tacker JR, et al. Clinical and radiological findings in patients with gas forming renal abscess treated conservatively. J Urol. 1999;162:1273-1276.
Biering-Sorensen F. Urinary tract infection in individuals with spinal cord lesion. Curr Opin Urol. 2002;12:45-49.
Blom M, Sorensen TL, Espersen F, et al. Validation of FLEXICULT SSI-Urinary Kit for use in the primary health care setting. Scand J Infect Dis. 2002;34:430-435.
Bonadio M, Meini M, Spitaleri P, et al. Current microbiological and clinical aspects of urinary tract infections. Eur Urol. 2001;40:439-445.
Bone RC. Sepsis, the sepsis syndrome, multi-organ failure: a plea for comparable definitions. Ann Intern Med. 1991;114:332-333.
Boscia JA, Abrutyn E, Levison ME, et al. Pyuria and asymptomatic bacteriuria in elderly ambulatory women. Ann Intern Med. 1989;110:404-405.
Boscia JA, Kaye D. Asymptomatic bacteriuria in the elderly. Infect Dis Clin North Am. 1987;1:893-905.
Boscia JA, Kobasa WD, Knight RA, et al. Epidemiology of bacteriuria in an elderly ambulatory population. Am J Med. 1986;80:208-214.
Boscia JA, Kobasa WD, Knight RA, et al. Therapy vs no therapy for bacteriuria in elderly ambulatory nonhospitalized women. JAMA. 1987;257:1067-1071.
Bowers JH, Cathey WJ. Malakoplakia of the kidney with renal failure. Am J Clin Pathol. 1971;55:765-769.
Bratzler DW, Houck PM. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Clin Infect Dis. 2004;38:1706-1715.
Braude AI. Current concepts of pyelonephritis. Medicine (Baltimore). 1973;52:257-264.
Brenbridge AN, Buschi AJ, Cochrane JA, et al. Renal emphysema of the tranplanted kidney: sonographic appearance. AJR Am J Roentgenol. 1979;132:656-658.
Brocklehurst JC, Dillane JB, Griffiths L, et al. The prevalence and symptomatology of urinary infection in an aged population. Gerontol Clin (Basel). 1968;10:242-253.
Bromberg K, Gleich S, Ginsberg MB. Clostridia in urinary tract infections. South Med J. 1982;75:1298-1300.
Brooker WJ, Aufderheide AC. Genitourinary tract infections due to atypical mycobacteria. J Urol. 1980;124:242-244.
Brosnahan J, Jull A, Tracy C. Types of urethral catheters for management of short-term voiding problems in hospitalised adults. Cochrane Database Syst Rev 2004:CD004013.
Brown PD, Freeman A, Foxman B. Prevalence and predictors of trimethoprim-sulfamethoxazole resistance among uropathogenic Escherichia coli isolates in Michigan. Clin Infect Dis. 2002;34:1061-1066.
Brumfitt W, Gruneberg R, Leigh D. Bacteriuria in pregnancy, with reference to prematurity and long-term effects on the mother. In: Symposium on Pyelonephritis. Edinburgh: E&S Livingstone; 1967.
Buckley RJ, Smith S, Herschorn S, et al. Echinococcal disease of the kidney presenting as a renal filling defect. J Urol. 1985;133:660-661.
Bukowski TP, Betrus GG, Aquilina JW, et al. Urinary tract infections and pregnancy in women who underwent antireflux surgery in childhood. J Urol. 1998;159:1286-1289.
Buonocore E, Vidt DG, Montie JE. Ultrasonography in the diagnosis of obstructive uropathy caused by papillary necrosis. Cleve Clin Q. 1980;47:109-114.
Burke DM, Shackley DC, O’Reilly PH. The community-based morbidity of flexible cystoscopy. BJU Int. 2002;89:347-349.
Burman L. Significance of the sulfonamide component for the clinical efficacy of trimethoprim-sulfonamide combinations. Scand J Infect Dis. 1986;18:89-99.
Burpee JF, Edwards P. Fournier’s gangrene. J Urol. 1972;107:812-814.
Busch R, Huland H. Correlation of symptoms and results of direct bacterial localization in patients with urinary tract infections. J Urol. 1984;132:282-285.
Calandra T, Glauser MP, Schellekens J, et al. Treatment of gram-negative septic shock with human IgG antibody to Escherichia coli J5: a prospective, double-blind, randomized trial. J Infect Dis. 1988;158:312-319.
Callea F, Van Damme B, Desmet VJ. Alpha-1-antitrypsin in malakoplakia. Virchows Arch A Pathol Anat Histol. 1982;395:1-9.
Callen PW. Computed tomographic evaluation of abdominal and pelvic abscesses. Radiology. 1979;131:171-175.
Campbell M. Perinephric abscess. Surg Gynecol Obstet. 1930;51:654.
Campbell-Brown M, McFadyen IR, Seal DV, et al. Is screening for bacteriuria in pregnancy worth while? BMJ (Clin Res Ed). 1987;294:1579-1582.
Camunez F, Echenagusia A, Prieto ML, et al. Percutaneous nephrostomy in pyonephrosis. Urol Radiol. 1989;11:77-81.
Cardenas DD, Hooton TM. Urinary tract infection in persons with spinal cord injury. Arch Phys Med Rehabil. 1995;76:272-280.
Carlson KJ, Mulley AG. Management of acute dysuria. A decision-analysis model of alternative strategies. Ann Intern Med. 1985;102:244-249.
Carty M, Brocklehurst JC, Carty J. Bacteriuria and its correlates in old age. Gerontology. 1981;27:72-75.
Casewell M, Phillips I. Hands as route of transmission for Klebsiella species. BMJ. 1977;2:1315-1317.
Cattell WR. The localization of urinary tract infection and its relationship to relapse, reinfection and treatment. London: Oxford University Press; 1973.
Cattell WR, McSherry MA, Northeast A, et al. Periurethral enterobacterial carriage in pathogenesis of recurrent urinary infection. BMJ. 1974;4:136-139.
Cavins JA, Goldstein AM. Renal malacoplakia. Urology. 1977;10:155-158.
Chan RC, Bruce AW, Reid G. Adherence of cervical, vaginal and distal urethral normal microbial flora to human uroepithelial cells and the inhibition of adherence of gram-negative uropathogens by competitive exclusion. J Urol. 1984;131:596-601.
Charboneau J. Malakoplakia of the urniary tract with renal parenchymal involvement. Urol Radiol. 1980;2:89.
Charlton CA, Crowther A, Davies JG, et al. Three-day and ten-day chemotherapy for urinary tract infections in general practice. Br Med J. 1976;1:124-126.
Chernow B, Zaloga GP, Soldano S, et al. Measurement of urinary leukocyte esterase activity: a screening test for urinary tract infections. Ann Emerg Med. 1984;13:150-154.
Christ W, Lehnert T, Ulbrich B. Specific toxicologic aspects of the quinolones. Rev Infect Dis. 1988;10(Suppl. 1):S141-S146.
Chuang CK, Lai MK, Chang PL, et al. Xanthogranulomatous pyelonephritis: experience in 36 cases. J Urol. 1992;147:333-336.
Clark KR, Higgs MJ. Urinary infection following out-patient flexible cystoscopy. Br J Urol. 1990;66:503-505.
Clarke SA, Samuel M, Boddy SA. Are prophylactic antibiotics necessary with clean intermittent catheterization? A randomized controlled trial. J Pediatr Surg. 2005;40:568-571.
Clayton MD, Fowler JEJr, Sharifi R, et al. Causes, presentation and survival of fifty-seven patients with necrotizing fasciitis of the male genitalia. Surg Gynecol Obstet. 1990;170:49-55.
Cockerill F, Edson R. Trimethoprim-sulfamethoxazole. Mayo Clin Proc. 1991;66:1260-1269.
Cohen M. Fournier’s gangrene. AUA Update. 1986;5:6.
Cohen M. Epidemiology of drug resistance: implications for a post-antimicrobial era. Science. 1992;257:1050-1055.
Coltorti EA, Varela-Diaz VM. Detection of antibodies against Echinococcus granulosus arc 5 antigens by double diffusion test. Trans R Soc Trop Med Hyg. 1978;72:226-229.
Connell I, Agace W, Klemm P, et al. Type 1 fimbrial expression enhances Escherichia coli virulence for the urinary tract. Proc Natl Acad Sci U S A. 1996;93:9827-9832.
Conrad MR, Bregman R, Kilman WJ. Ultrasonic recognition of parenchymal gas. AJR Am J Roentgenol. 1979;132:395-399.
Consumer Reports. Go ahead: find the berry. Consumer Reports. 2001;66:8-9.
Conte JEJr, Cohen SN, Roe BB, et al. Antibiotic prophylaxis and cardiac surgery. A prospective double-blind comparison of single-dose versus multiple-dose regimens. Ann Intern Med. 1972;76:943-949.
Corriere JNJr, Sandler CM. The diagnosis and immediate therapy of acute renal and perirenal infections. Urol Clin North Am. 1982;9:219-228.
Cotran R. Experimental pyelonephritis. In: Rouiller C, Muller A, editors. The Kidney. New York: Academic; 1969:269-361.
Cox CE, Hinman FJr. Experiments with induced bacteriuria, vesical emptying and bacterial growth on the mechanism of bladder defense to infection. J Urol. 1961;86:739-748.
Cruse P. Surgical wound infection. In: Wonsiewicz M, editor. Infectious disease. Philadelphia: WB Saunders; 1992:758-764.
Cundiff GW, McLennan MT, Bent AE. Randomized trial of antibiotic prophylaxis for combined urodynamics and cystourethroscopy. Obstet Gynecol. 1999;93:749-752.
Cunningham FG, Morris GB, Mickal A. Acute pyelonephritis of pregnancy: a clinical review. Obstet Gynecol. 1973;42:112-117.
Daifuku R, Stamm WE. Association of rectal and urethral colonization with urinary tract infection in patients with indwelling catheters. JAMA. 1984;252:2028-2030.
Daikos GK, Kontomichalou P, Bilalis D, et al. Intestinal flora ecology after oral use of antibiotics: terramycin, chloramphenicol, ampicillin, neomycin, paromomycin, aminodidin. Chemotherapy. 1968;13:146-160.
Dajani AS, Taubert KA, Wilson W, et al. Prevention of bacterial endocarditis: recommendations by the American Heart Association. JAMA. 1997;277:1794-1801.
Dalkin B, Schaeffer A. Fluoroquinolone antimicrobial agents—use in the treatment of urinary tract infections and clinical urologic practice. In: Carson CI, editor. Problems in urology, vol. 2. Philadelphia: JB Lippincott; 1988:476-485.
Datta N, Faiers MC, Reeves DS, et al. R factors in Escherichia coli in faeces after oral chemotherapy in general practice. Lancet. 1971;1:312-315.
Davidson AJ, Talner LB. Urographic and angiographic abnormalities in adult-onset acute bacterial nephritis. Radiology. 1973;106:249-256.
Davidson AJ, Talner LB. Late sequelae of adult-onset acute bacterial nephritis. Radiology. 1978;127:367-371.
Davies AG, McLachlan MS, Asscher AW. Progressive kidney damage after non-obstructive urinary tract infection. BMJ. 1972;4:406-407.
Davies B, Maesen F. Drug interactions with quinolones. Rev Infect Dis. 1989;11(Suppl. 5):S1083-S1090.
Davison JM, Lindheimer MD. Renal disease in pregnant women. Clin Obstet Gynecol. 1978;21:411-427.
Dellinger RP, Carlet JM, Masur H, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32:858-873.
DeNavasquez S. Experimental pyelonephritis in the rabbit produced by staphylococcal infection. J Pathol Bacteriol. 1950;62:429-436.
Deridder PA, Koff SA, Gikas PW, et al. Renal malacoplakia. J Urol. 1977;117:428-432.
Dogan HS, Sahin A, Cetinkaya Y, et al. Antibiotic prophylaxis in percutaneous nephrolithotomy: prospective study in 81 patients. J Endourol. 2002;16:649-653.
Donlan RM, Costerton JW. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev. 2002;15:167-193.
Dontas AS, Kasviki-Charvati P, Papanayiotou PC, et al. Bacteriuria and survival in old age. N Engl J Med. 1981;304:939-943.
Dontas AS, Papanayiotou P, Marketos SG, et al. The effect of bacteriuria on renal functional patterns in old age. Clin Sci. 1968;34:73-81.
Duguid JP, Anderson ES, Campbell I. Fimbriae and adhesive properties in Salmonellae. J Pathol Bacteriol. 1966;92:107-138.
Duguid JP, Clegg S, Wilson MI. The fimbrial and non-fimbrial haemagglutinins of Escherichia coli. J Med Microbiol. 1979;12:213-227.
Dukes C. Urinary infections after excision of the rectum: their cause and prevention. Proc R Soc Med. 1928;22:1.
Duncan JL. Differential effect of Tamm-Horsfall protein on adherence of Escherichia coli to transitional epithelial cells. J Infect Dis. 1988;158:1379-1382.
Eastham J, Ahlering T, Skinner E. Xanthogranulomatous pyelonephritis: clinical findings and surgical considerations. Urology. 1994;43:295-299.
Edelstein H, McCabe RE. Perinephric abscess: modern diagnosis and treatment in 47 cases. Medicine (Baltimore). 1988;67:118-131.
Edwards LE, Lock R, Powell C, et al. Post-catheterisation urethral strictures: a clinical and experimental study. Br J Urol. 1983;55:53-56.
Eisenstein BI. Phase variation of type 1 fimbriae in Escherichia coli is under transcriptional control. Science. 1981;214:337-339.
Elder HA, Santamarina BA, Smith S, et al. The natural history of asymptomatic bacteriuria during pregnancy: the effect of tetracycline on the clinical course and the outcome of pregnancy. Am J Obstet Gynecol. 1971;111:441-462.
Elder J. Xanthogranulomatous pyelonephritis and gas forming infections of the urinary tract. AUA Update. III, 1984. lesson 31
Elliott TS, Reed L, Slack RC, et al. Bacteriology and ultrastructure of the bladder in patients with urinary tract infections. J Infect. 1985;11:191-199.
Elyaderani MK, Subramanian VP, Burgess JE. Diagnosis and percutaneous drainage of a perinephric abscess by ultrasound and fluoroscopy. J Urol. 1981;125:405-407.
Ena J, Amador C, Martinez C, et al. Risk factors for acquisition of urinary tract infections caused by ciprofloxacin resistant Escherichia coli. J Urol. 1995;153:117-120.
Engel G, Schaeffer AJ, Grayhack JT, et al. The role of excretory urography and cystoscopy in the evaluation and management of women with recurrent urinary tract infection. J Urol. 1980;123:190-191.
Eskandari MK, Bolgos G, Miller C, et al. Anti-tumor necrosis factor antibody therapy fails to prevent lethality after cecal ligation and puncture or endotoxemia. J Immunol. 1992;148:2724-2730.
Esparza AR, McKay DB, Cronan JJ, et al. Renal parenchymal malakoplakia: histologic spectrum and its relationship to megalocytic interstitial nephritis and xanthogranulomatous pyelonephritis. Am J Surg Pathol. 1989;13:225-236.
Evans DA, Williams DN, Laughlin LW, et al. Bacteriuria in a population-based cohort of women. J Infect Dis. 1978;138:768-773.
Eykyn S, Lloyd-Davies RW, Shuttleworth KE, et al. The localization of urinary tract infection by ureteric catheterization. Invest Urol. 1972;9:271-275.
Fader RC, Davis CP. Klebsiella pneumoniae-induced experimental pyelitis: the effect of piliation on infectivity. J Urol. 1982;128:197-201.
Fagerholm M. Case of the autumn season. Semin Ultrasound. 1983;4:145.
Fair WR, McClennan BL, Jost RG. Are excretory urograms necessary in evaluating women with urinary tract infection? J Urol. 1979;121:313-315.
Fair WR, Timothy MM, Millar MA, et al. Bacteriologic and hormonal observations of the urethra and vaginal vestibule in normal, premenopausal women. J Urol. 1970;104:426-431.
Fairchild TN, Shuman W, Berger RE. Radiographic studies for women with recurrent urinary tract infections. J Urol. 1982;128:344-345.
Fairley K. The routine determination of the site of infection in the investigation of patients with urinary tract infection. In: Kincaid-Smith P, Fairley K, editors. Renal infection and renal scarring. Melbourne: Mercedes, 1972.
Fairley K, Birch DF. Detection of bladder bacteriuria in patients with acute urinary symptoms. J Infect Dis. 1989;159:226-231.
Fairley K, Bond A, Adey F. The site of infection in pregnancy bacteriuria. Lancet. 1966;1:939-941.
Fairley K, Bond AG, Brown RB, et al. Simple test to determine the site of urinary-tract infection. Lancet. 1967;2:427-428.
Fairley K, Hubbard M, Whitworth JA. Prophylactic long-term cephalexin in recurrent urinary infection. Med J Aust. 1974;1:318-319.
Fairley K, Whitworth JA, Radford NJ, et al. Pregnancy bacteriuria: the significance of site of infection. Med J Aust. 1973;2:424-427.
Faro S, Pastorek JG2nd, Plauche WC, et al. Short-course parenteral antibiotic therapy for pyelonephritis in pregnancy. South Med J. 1984;77:455-457.
Feldberg MA. Bilateral adult-onset acute bacterial pyelonephritis and its late unusual sequelae: a case report. Diagn Imaging. 1982;51:296-300.
Fernandez JA, Miles BJ, Buck AS, et al. Renal carbuncle: comparison between surgical open drainage and closed percutaneous drainage. Urology. 1985;25:142-144.
Fiegler W. Ultrasound in acute renal inflammatory lesions. Eur J Radiol. 1983;3:354-357.
Fihn SD. Clinical practice: acute uncomplicated urinary tract infection in women. N Engl J Med. 2003;349:259-266.
Fihn SD, Johnson C, Roberts PL, et al. Trimethoprim-sulfamethoxazole for acute dysuria in women: a single-dose or 10-day course. A double-blind, randomized trial. Ann Intern Med. 1988;108:350-357.
Fihn SD, Latham RH, Roberts P, et al. Association between diaphragm use and urinary tract infection. JAMA. 1985;254:240-245.
Finegold S. Urniary tract infections. In: Finegold S, editor. Anaerobic bacteria in human disease. New York: Academic; 1977:311-349.
Fischman NH, Roberts JA. Clinical studies in acute pyelonephritis: is there a place for renal quantitative camera study? J Urol. 1982;128:452-455.
Flynn JT, Molland EA, Paris AM, et al. The underestimated hazards of xanthogranulomatous pyelonephritis. Br J Urol. 1979;51:443-444.
Foley F. Cystoscopic prostatectomy: a new procedure and instrument; preliminary report. J Urol. 1929;21:289.
Foo LY, Lu Y, Howell AB, et al. A-Type proanthocyanidin trimers from cranberry that inhibit adherence of uropathogenic P-fimbriated Escherichia coli. J Nat Prod. 2000;63:1225-1228.
Forland M, Thomas V, Shelokov A. Urinary tract infections in patients with diabetes mellitus: studies on antibody coating of bacteria. JAMA. 1977;238:1924-1926.
Fournier J. Gangrene-foudroyante de la verge. Semin Med. 1883;3:345.
Fournier J. Étude clinique de la gangrene-foudroyante de la verge. Semin Med. 1884;4:64.
Fowler JEJr, Perkins T. Presentation, diagnosis and treatment of renal abscesses: 1972–1988. J Urol. 1994;151:847-851.
Fowler JEJr, Pulaski ET. Excretory urography, cystography, and cystoscopy in the evaluation of women with urinary-tract infection: a prospective study. N Engl J Med. 1981;304:462-465.
Fowler JEJr, Stamey TA. Studies of introital colonization in women with recurrent urinary infections: VII. The role of bacterial adherence. J Urol. 1977;117:472-476.
Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med. 2002;113(Suppl. 1A):5S-13S.
Foxman B, Barlow R, D’Arcy H, et al. Urinary tract infection: self-reported incidence and associated costs. Ann Epidemiol. 2000;10:509-515.
Foxman B, Zhang L, Tallman P, et al. Virulence characteristics of Escherichia coli causing first urinary tract infection predict risk of second infection. J Infect Dis. 1995;172:1536-1541.
Fraser IR, Birch D, Fairley KF, et al. A prospective study of cortical scarring in acute febrile pyelonephritis in adults: clinical and bacteriological characteristics. Clin Nephrol. 1995;43:159-164.
Freedman L. Natural history of urinary infection in adults. Kidney Int Suppl. 1975;4:S96-100.
Freedman L. Interstitial renal inflammation, including pyelonephritis and urinary tract infection. In: Early L, Gottschalk C, editors. Strauss and Welt’s diseases of the kidney. Boston: Little & Brown, 1979.
Freedman LR, Beeson PB. Experimental pyelonephritis: IV. Observations on infections resulting from direct inoculation of bacteria in different zones of the kidney. Yale J Biol Med. 1958;30:406-414.
Freiha F, Messing E, Fross D. Emphysematous pyelonephritis. J Contin Ed Urol. 1979;18:9.
Friedenberg MJ, Spjut HJ. Xanthogranulomatous pyelonephritis. Am J Roentgenol Radium Ther Nucl Med. 1963;90:97-108.
Gabriel MM, Mayo MS, May LL, et al. In vitro evaluation of the efficacy of a silver-coated catheter. Curr Microbiol. 1996;33:1-5.
Gaffney RA, Venegas MF, Kanerva C, et al. Effect of vaginal fluid on adherence of type 1 piliated Escherichia coli to epithelial cells. J Infect Dis. 1995;172:1528-1535.
Garibaldi RA, Burke JP, Britt MR, et al. Meatal colonization and catheter-associated bacteriuria. N Engl J Med. 1980;303:316-318.
Geerlings SE, Stolk RP, Camps MJ, et al. Risk factors for symptomatic urinary tract infection in women with diabetes. Diabetes Care. 2000;23:1737-1741.
Gerzof SG, Gale ME. Computed tomography and ultrasonography for diagnosis and treatment of renal and retroperitoneal abscesses. Urol Clin North Am. 1982;9:185-193.
Ghosh H. Chronic pyelonephritis with xanthogranulomatous change; report of 3 cases. Am J Clin Pathol. 1955;25:1043-1049.
Gilbert D. Once-daily aminoglycoside therapy. Antimicrob Agents Chemother. 1991;35:399-405.
Gillenwater JY, Harrison RB, Kunin CM. Natural history of bacteriuria in schoolgirls: a long-term case-control study. N Engl J Med. 1979;301:396-399.
Gilmore DS, Schick DG, Young MN, et al. Effect of external urinary collection system on colonization and urinary tract infections with Pseudomonas and Klebsiella in men with spinal cord injury. J Am Paraplegia Soc. 1992;15:155-157.
Gilsanz V, Lozano G, Jimenez J. Renal hydatid cysts: communicating with collecting system. AJR Am J Roentgenol. 1980;135:357-361.
Gilstrap LC, Leveno KJ, Cunningham FG, et al. Renal infection and pregnancy outcome. Am J Obstet Gynecol. 1981;141:709-716.
Girardin E, Grau GE, Dayer JM, et al. Tumor necrosis factor and interleukin-1 in the serum of children with severe infectious purpura. N Engl J Med. 1988;319:397-400.
Goldman SM, Hartman DS, Fishman EK, et al. CT of xanthogranulomatous pyelonephritis: radiologic-pathologic correlation. AJR Am J Roentgenol. 1984;142:963-969.
Goldmann DA, Hopkins CC, Karchmer AW, et al. Cephalothin prophylaxis in cardiac valve surgery: a prospective, double-blind comparison of two-day and six-day regimens. J Thorac Cardiovasc Surg. 1977;73:470-479.
Goodman M, Curry T, Russell T. Xanthogranulomatous pyelonephritis (XGP): a local disease with systemic manifestations. Report of 23 patients and review of the literature. Medicine (Baltimore). 1979;58:171-181.
Goransson M, Uhlin BE. Environmental temperature regulates transcription of a virulence pili operon in E. coli. EMBO J. 1984;3:2885-2888.
Gorbach SL, Bartlett JG. Anaerobic infections (second of three parts). N Engl J Med. 1974;290:1237-1245.
Gower PE. The use of small doses of cephalexin (125 mg) in the management of recurrent urinary tract infection in women. J Antimicrob Chemother. 1975;1:93-98.
Gower PE. A prospective study of patients with radiological pyelonephritis, papillary necrosis and obstructive atrophy. Q J Med. 1976;45:315-349.
Grainger RG, Longstaff AJ, Parsons MA. Xanthogranulomatous pyelonephritis: a reappraisal. Lancet. 1982;1:1398-1401.
Greenberg M, Falkowski WS, Sakowicz BA, et al. Use of computerized tomography in the evaluation of filling defects of the renal pelvis. J Urol. 1982;127:1172-1176.
Greene B. Physical therapist management of fluoroquinolone-induced Achilles tendinopathy. Phys Ther. 2002;82:1224-1231.
Gregg CR, Rogers TE, Munford RS. Xanthogranulomatous pyelonephritis. Curr Clin Top Infect Dis. 1999;19:287-304.
Grieco MH. Use of antibiotics in the elderly. Bull N Y Acad Med. 1980;56:197-208.
Griffith BC, Morey AF, Ali-Khan MM, et al. Single dose levofloxacin prophylaxis for prostate biopsy in patients at low risk. J Urol. 2002;168:1021-1023.
Gruneberg R, Smellie J, Leaky A. Changes in the antibiotic sensitivities of faecal organisms in response to treatment in children with urinary tract infection. In: Brumfitt W, Asscher A, editors. Urinary tract infection. London: Oxford University Press; 1973:131.
Gupta K, Hillier SL, Hooton TM, et al. Effects of contraceptive method on the vaginal microbial flora: a prospective evaluation. J Infect Dis. 2000;181:595-601.
Gupta K, Hooton TM, Stamm WE. Increasing antimicrobial resistance and the management of uncomplicated community-acquired urinary tract infections. Ann Intern Med. 2001;135:41-50.
Gupta K, Scholes D, Stamm W. Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA. 1999;281:736-738.
Gupta K, Stamm W. Outcomes associated with trimethoprim/sulphamethoxazole (TMP/SMX) therapy in TMP/SMX resistant community-acquired UTI. Int J Antimicrob Agents. 2002;19:554-556.
Guttmann D. Follow-up of urinary tract infection in domiciliary patients. In: Brumfitt W, Asscher A, editors. Urinary tract infection. London: Oxford University Press; 1973:62.
Guyer DM, Henderson IR, Nataro JP, et al. Identification of sat, an autotransporter toxin produced by uropathogenic Escherichia coli. Mol Microbiol. 2000;38:53-66.
Guyer DM, Radulovic S, Jones FE, et al. Sat, the secreted autotransporter toxin of uropathogenic Escherichia coli, is a vacuolating cytotoxin for bladder and kidney epithelial cells. Infect Immun. 2002;70:4539-4546.
Haaga JR, Weinstein AJ. CT-guided percutaneous aspiration and drainage of abscesses. AJR Am J Roentgenol. 1980;135:1187-1194.
Hacker J. Pathogenicity islands of extraintestinal Escherichia coli. In: Kaper J, Hacker J, editors. Pathogenicity islands and other mobile virulence elements. Baltimore: American Society for Microbiology; 1999:59-75.
Hagberg L, Engberg I, Freter R, et al. Ascending, unobstructed urinary tract infection in mice caused by pyelonephritogenic Escherichia coli of human origin. Infect Immun. 1983;40:273-283.
Hagberg L, Hull R, Hull S, et al. Contribution of adhesion to bacterial persistence in the mouse urinary tract. Infect Immun. 1983;40:265-272.
Haley RW, Culver DH, White JW, et al. The nationwide nosocomial infection rate: a new need for vital statistics. Am J Epidemiol. 1985;121:159-167.
Haley RW, Hooton TM, Culver DH, et al. Nosocomial infections in U.S. hospitals, 1975–1976: estimated frequency by selected characteristics of patients. Am J Med. 1981;70:947-959.
Handley MA, Reingold AL, Shiboski S, et al. Incidence of acute urinary tract infection in young women and use of male condoms with and without nonoxynol-9 spermicides. Epidemiology. 2002;13:431-436.
Harber MJ, Chick S, Mackenzie R, et al. Lack of adherence to epithelial cells by freshly isolated urinary pathogens. Lancet. 1982;1:586-588.
Harbord RB, Gruneberg RN. Treatment of urinary tract infection with a single dose of amoxycillin, co-trimoxazole, or trimethoprim. BMJ (Clin Res Ed). 1981;283:1301-1302.
Harding GK, Nicolle LE, Ronald AR, et al. How long should catheter-acquired urinary tract infection in women be treated? A randomized controlled study. Ann Intern Med. 1991;114:713-719.
Harding GK, Ronald AR, Nicolle LE, et al. Long-term antimicrobial prophylaxis for recurrent urinary tract infection in women. Rev Infect Dis. 1982;4:438-443.
Harris RE, Thomas VL, Shelokov A. Asymptomatic bacteriuria in pregnancy: antibody-coated bacteria, renal function, and intrauterine growth retardation. Am J Obstet Gynecol. 1976;126:20-25.
Harrison W, Holmes K, Belding M. A prospective evaluation of recurrent urinary tract infection in women. Clin Res. 125A, 1974.
Hartman D. Radiologic pathologic correlation of the infectious granulomatous diseases of the kidney: III and. IV. Monogr Urol. 1985;6:26.
Hartman D, Davis C, Lichtenstein J, et al. Renal parenchymal malacoplakia. Radiology. 1980;136:33-42.
Hartman DS, Davis CJJr, Goldman SM, et al. Xanthogranulomatous pyelonephritis: sonographic-pathologic correlation of 16 cases. J Ultrasound Med. 1984;3:481-488.
Hartstein AI, Garber SB, Ward TT, et al. Nosocomial urinary tract infection: a prospective evaluation of 108 catheterized patients. Infect Control. 1981;2:380-386.
Hawes S. Emphysematous pyelonephritis. Infect Surg. 1983;2:191.
Heineman HS, Lee JH. Bacteriuria in pregnancy: a heterogeneous entity. Obstet Gynecol. 1973;41:22-26.
Henderson IR, Nataro JP. Virulence functions of autotransporter proteins. Infect Immun. 2001;69:1231-1243.
Henry DCJr, Bettis RB, Riffer E, et al. Comparison of once-daily extended-release ciprofloxacin and conventional twice-daily ciprofloxacin for the treatment of uncomplicated urinary tract infection in women. Clin Ther. 2002;24:2088-2104.
Heptinstall R. Pathology of the kidney. Boston: Little & Brown; 1974.
Herlitz H, Westberg G, Nilson AE. A perinephric abscess in a diabetic woman: successful conservative treatment. A case report. Scand J Urol Nephrol. 1981;15:337-340.
Hernandez GV, King AS, Needle MA. Nephrosis and papillary necrosis after pyelonephritis. N Engl J Med. 1975;293:1347-1349.
Hinton NA. The effect of oral tetracycline HCl and doxycycline on the intestinal flora. Curr Ther Res Clin Exp. 1970;12:341-352.
Hockstra D. Hyaluronan-modified surfaces for medical devices. Med Device Diagn Industry. 1999:48-56.
Hodson C. Natural history of chronic pyelonephritis scarring. BMJ. 1965;2:191.
Hodson C. Coarse pyelonephritic scarring or ‘atrophic pyelonephritis. Proc R Soc Med. 1965;58:785-788.
Hodson CJ, Edwards D. Chronic pyelonephritis and vesico-ureteric reflex. Clin Radiol. 1960;11:219-231.
Hoffman JC, Schnur MJ, Koenigsberg M. Demonstration of renal papillary necrosis by sonography. Radiology. 1982;145:785-787.
Hootkins R, Fenves A, Stephens M. Acute renal failure secondary to oral ciprofloxacin therapy: a presentation of three cases and a review of the literature. Clin Nephrol. 1989;32:75-78.
Hooton TM, Besser R, Foxman B, et al. Acute uncomplicated cystitis in an era of increasing antibiotic resistance: a proposed approach to empirical therapy. Clin Infect Dis. 2004;39:75-80.
Hooton TM, Fennell CL, Clark AM, et al. Nonoxynol-9: differential antibacterial activity and enhancement of bacterial adherence to vaginal epithelial cells. J Infect Dis. 1991;164:1216-1219.
Hooton TM, Hillier S, Johnson C, et al. Escherichia coli bacteriuria and contraceptive method. JAMA. 1991;265:64-69.
Hooton TM, Latham RH, Wong ES, et al. Ofloxacin versus trimethoprim-sulfamethoxazole for treatment of acute cystitis. Antimicrob Agents Chemother. 1989;33:1308-1312.
Hooton TM, Scholes D, Hughes JP, et al. A prospective study of risk factors for symptomatic urinary tract infection in young women. N Engl J Med. 1996;335:468-474.
Hooton TM, Scholes D, Stapleton AE, et al. A prospective study of asymptomatic bacteriuria in sexually active young women. N Engl J Med. 2000;343:992-997.
Hooton TM, Stamm WE. Management of acute uncomplicated urinary tract infection in adults. Med Clin North Am. 1991;75:339-357.
Hooton TM, Stamm WE. Diagnosis and treatment of uncomplicated urinary tract infection. Infect Dis Clin North Am. 1997;11:551-581.
Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med. 2003;348:138-150.
Hovelius B, Mardh PA. Staphylococcus saprophyticus as a common cause of urinary tract infections. Rev Infect Dis. 1984;6:328-337.
Hoverman IV, Gentry LO, Jones DW, et al. Intrarenal abscess. Report of 14 cases. Arch Intern Med. 1980;140:914-916.
Huang JJ, Tseng CC. Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med. 2000;160:797-805.
Hudson MA, Weyman PJ, van der Vliet AH, et al. Emphysematous pyelonephritis: successful management by percutaneous drainage. J Urol. 1986;136:884-886.
Huland H, Busch R. Chronic pyelonephritis as a cause of end stage renal disease. J Urol. 1982;127:642-643.
Huland H, Gonnermann D, Clausen C. Bacterial localization in patients with end stage renal disease to avoid bilateral nephrectomy before renal transplantation. J Urol. 1983;129:915-917.
Hull R, Rudy D, Donovan W, et al. Urinary tract infection prophylaxis using Escherichia coli 83972 in spinal cord injured patients. J Urol. 2000;163:872-877.
Hultgren SJ, Porter TN, Schaeffer AJ, et al. Role of type 1 pili and effects of phase variation on lower urinary tract infections produced by Escherichia coli. Infect Immun. 1985;50:370-377.
Hultgren SJ, Schwan WR, Schaeffer AJ, et al. Regulation of production of type 1 pili among urinary tract isolates of Escherichia coli. Infect Immun. 1986;54:613-620.
Hurlbut TA3rd, Littenberg B. The diagnostic accuracy of rapid dipstick tests to predict urinary tract infection. Am J Clin Pathol. 1991;96:582-588.
Iravani A. Advances in the understanding and treatment of urinary tract infections in young women. Urology. 1991;37:503-511.
Ishitoya S, Yamamoto S, Mitsumori K, et al. Non-secretor status is associated with female acute uncomplicated pyelonephritis. BJU Int. 2002;89:851-854.
Ispahani P, Pearson NJ, Greenwood D. An analysis of community and hospital-acquired bacteraemia in a large teaching hospital in the United Kingdom. Q J Med. 1987;63:427-440.
Israel RS, Lowenstein SR, Marx JA, et al. Management of acute pyelonephritis in an emergency department observation unit. Ann Emerg Med. 1991;20:253-257.
Iwahi T, Abe Y, Nakao M, et al. Role of type 1 fimbriae in the pathogenesis of ascending urinary tract infection induced by Escherichia coli in mice. Infect Immun. 1983;39:1307-1315.
Jackson B, Kirkland JA, Lawrence JR, et al. Urine cytology findings in analgesic nephropathy. J Urol. 1978;120:145-147.
Jackson G, Arana-Sialer J, Grieble HAB, et al. Profiles of pyelonephritis. Arch Intern Med. 1962;110:63-75.
Jameson RM, Heal MR. The surgical management of acute renal papillary necrosis. Br J Surg. 1973;60:428-430.
Jamieson NV, Everett WG, Bullock KN. Delayed recognition of an intersphincteric abscess as the underlying cause of Fournier’s scrotal gangrene. Ann R Coll Surg Engl. 1984;66:434-435.
Jarvis WR. Selected aspects of the socioeconomic impact of nosocomial infections: morbidity, mortality, cost, and prevention. Infect Control Hosp Epidemiol. 1996;17:552-557.
Jenkins RD, Fenn JP, Matsen JM. Review of urine microscopy for bacteriuria. JAMA. 1986;255:3397-3403.
Jepson R, Mihaljevic L, Craig J. Cranberries for preventing urinary tract infections. Cochrane Database Syst Rev. 2001;(3):CD001321.
Johnson JR. Microbial virulence determinants and the pathogenesis of urinary tract infection. Infect Dis Clin North Am. 2003;17:261-278. viii
Johnson JR, Moseley SL, Roberts PL, et al. Aerobactin and other virulence factor genes among strains of Escherichia coli causing urosepsis: association with patient characteristics. Infect Immun. 1988;56:405-412.
Johnson JR, Stamm WE. Diagnosis and treatment of acute urinary tract infections. Infect Dis Clin North Am. 1987;1:773-791.
Johnson JR, Stamm WE. Urinary tract infections in women: diagnosis and treatment. Ann Intern Med. 1989;111:906-917.
Johnson MI, Merrilees D, Robson WA, et al. Oral ciprofloxacin or trimethoprim reduces bacteriuria after flexible cystoscopy. BJU Int. 2007;100:826-829.
Jones CH, Pinkner JS, Roth R, et al. FimH adhesin of type 1 pili is assembled into a fibrillar tip structure in the Enterobacteriaceae. Proc Natl Acad Sci U S A. 1995;92:2081-2085.
Jordan PA, Iravani A, Richard GA, et al. Urinary tract infection caused by Staphylococcus saprophyticus. J Infect Dis. 1980;142:510-515.
Josephson S, Thomason J, Sturino K, et al. Gardnerella vaginalis in the urinary tract: incidence and significance in a hospital population. Obstet Gynecol. 1988;71:245-250.
Juhasz J, Galambos J, Surjan LJr. Renal actinomycosis associated with bilateral necrosing renal papillitis. Int Urol Nephrol. 1980;12:199-203.
Justice SS, Hung C, Theriot JA, et al. Differentiation and developmental pathways of uropathogenic Escherichia coli in urinary tract pathogenesis. Proc Natl Acad Sci U S A. 2004;101:1333-1338.
Juthani-Mehta M. Asymptomatic bacteriuria and urinary tract infection in older adults. Clin Geriatr Med. 2007;23:585-594. vii
Kahlmeter G, Menday P. Cross-resistance and associated resistance in 2478 Escherichia coli isolates from the Pan-European ECO.SENS Project surveying the antimicrobial susceptibility of pathogens from uncomplicated urinary tract infections. J Antimicrob Chemother. 2003;52:128-131.
Kaijser B, Hanson LA, Jodal U, et al. Frequency of E. coli K antigens in urinary tract infections in children. Lancet. 1977;1:663-666.
Kallenius G, Mollby R, Svenson S. Adhesion of Escherichia coli to human periurethral cells correlated to mannose-resistant agglutination of human erythrocytes. FEMS Microbiol Lett. 1979:295.
Kallenius G, Mollby R, Svenson S. The pk antigen as receptor for the haemagglutinin of pyelonephritic Escherichia coli. FEMS Microbiol Lett. 1980:297.
Kallenius G, Mollby R, Svenson S, et al. Occurrence of P-fimbriated Escherichia coli in urinary tract infections. Lancet. 1981;2:1369-1372.
Kaplan DM, Rosenfield AT, Smith RC. Advances in the imaging of renal infection: helical CT and modern coordinated imaging. Infect Dis Clin North Am. 1997;11:681-705.
Karlowsky J, Jones M, Thornsberry C, et al. Trends in antimicrobial susceptibilities among Enterobacteriaceae isolated from hospitalized patients in the United States from 1998 to 2001. Antimicrob Agents Chemother. 2003;47:1672-1680.
Kartal ED, Yenilmez A, Kiremitci A, et al. Effectiveness of ciprofloxacin prophylaxis in preventing bacteriuria caused by urodynamic study: a blind, randomized study of 192 patients. Urology. 2006;67:1149-1153.
Kasanen A, Anttila M, Elfving R, et al. Trimethoprim: pharmacology, antimicrobial activity and clinical use in urinary tract infections. Ann Clin Res. 1978;10(Suppl. 22):1-39.
Kass EH. Asymptomatic infections of the urinary tract. Trans Assoc Am Physicians. 1956;69:56-64.
Kass EH. The role of asymptomatic bacteriuria in the pathogenesis of pyelonephritis. In: Quinn E, Kass EH, editors. Biology of pyelonephritis. Boston: Little, Brown; 1960:399.
Kass EH. Pyelonephritis and bacteriuria: a major problem in preventive medicine. Ann Intern Med. 1962;56:46-53.
Kaul AK, Khan S, Martens MG, et al. Experimental gestational pyelonephritis induces preterm births and low birth weights in C3H/HeJ mice. Infect Immun. 1999;67:5958-5966.
Kaye D. Antibacterial activity of human urine. J Clin Invest. 1968;47:2374-2390.
Kaye D. Urinary tract infections in the elderly. Bull N Y Acad Med. 1980;56:209-220.
Kearney GP, Carling PC. Fournier’s gangrene: an approach to its management. J Urol. 1983;130:695-698.
Kennedy RP, Plorde JJ, Petersdorf RG. Studies on the epidemiology of Escherichia coli infections. IV. Evidence for a nosocomial flora. J Clin Invest. 1965;44:193-201.
Khalyl-Mawad J, Greco MA, Schinella RA. Ultrastructural demonstration of intracellular bacteria in xanthogranulomatous pyelonephritis. Hum Pathol. 1982;13:41-47.
Kincaid-Smith P. Management of renal and urinary tract disorders during pregnancy. In: Harrison J, Gittes R, editors. Campbell’s urology. Philadelphia: WB Saunders; 1978:2518.
Kincaid-Smith P, Bullen M. Bacteriuria in pregnancy. Lancet. 1965;191:395-399.
Kisielius PV, Schwan WR, Amundsen SK, et al. In vivo expression and variation of Escherichia coli type 1 and P pili in the urine of adults with acute urinary tract infections. Infect Immun. 1989;57:1656-1662.
Klein M. Vaccinium macrocarpon and urinary tract infection. Bethesda (MD): National Center for Complementary and Alternative Medicine; 2002.
Klemm P. Fimbrial adhesions of Escherichia coli. Rev Infect Dis. 1985;7:321-340.
Klumpp DJ, Weiser AC, Sengupta S, et al. Uropathogenic Escherichia coli potentiates type 1 pilus-induced apoptosis by suppressing NF-kappaB. Infect Immun. 2001;69:6689-6695.
Kluytmans J. Surgical infections including burns. In: Wenzel R, editor. Prevention and control of nosocomial infections. Baltimore: Williams & Wilkins; 1997:841.
Knopf HJ, Graff HJ, Schulze H. Perioperative antibiotic prophylaxis in ureteroscopic stone removal. Eur Urol. 2003;44:115-118.
Komaroff AL. Acute dysuria in women. N Engl J Med. 1984;310:368-375.
Komaroff AL. Urinalysis and urine culture in women with dysuria. Ann Intern Med. 1986;104:212-218.
Kontiokari T, Sundqvist K, Nuutinen M, et al. Randomised trial of cranberry-lingonberry juice and Lactobacillus GG drink for the prevention of urinary tract infections in women. BMJ. 2001;322:1571.
Kraft JK, Stamey TA. The natural history of symptomatic recurrent bacteriuria in women. Medicine (Baltimore). 1977;56:55-60.
Kreger BE, Craven DE, Carling PC, et al. Gram-negative bacteremia. III. Reassessment of etiology, epidemiology and ecology in 612 patients. Am J Med. 1980;68:332-343.
Krieger JN, Ross SO, Simonsen JM. Urinary tract infections in healthy university men. J Urol. 1993;149:1046-1048.
Kuhn JP, Berger PE. Computed tomography of the kidney in infancy and childhood. Radiol Clin North Am. 1981;19:445-461.
Kumar S, Muchmore A. Tamm-Horsfall protein—uromodulin (1950–1990). Kidney Int. 1990;37:1395-1401.
Kunin CM. The quantitative significance of bacteria visualized in the unstained urinary sediment. N Engl J Med. 1961;265:589-590.
Kunin CM. Use of antimicrobial agents in treating urinary tract infection. Adv Nephrol Necker Hosp. 1985;14:39-65.
Kunin CM. Detection, prevention and management of urinary tract infections. Philadelphia: Lea & Febiger; 1987.
Kunin CM, Douthitt S, Dancing J, et al. The association between the use of urinary catheters and morbidity and mortality among elderly patients in nursing homes. Am J Epidemiol. 1992;135:291-301.
Kunin CM, Chin QF, Chambers S. Morbidity and mortality associated with indwelling urinary catheters in elderly patients in a nursing home—confounding due to the presence of associated diseases. J Am Geriatr Soc. 1987;35:1001-1006.
Kunin CM, Zacha E, Paquin AJJr. Urinary-tract infections in schoolchildren. I. Prevalence of bacteriuria and associated urologic findings. N Engl J Med. 1962;266:1287-1296.
Kunz HH, Sieberth HG, Freiberg J, et al. The value of suprapubic bladder aspiration in the diagnosis of bacteriuria. Dtsch Med Wochenschr. 1975;100:2252-2256. 2261–54 [in German]
Langermann S, Palaszynski S, Barnhart M, et al. Prevention of mucosal Escherichia coli infection by FimH-adhesin-based systemic vaccination. Science. 1997;276:607-611.
Lapides J, Diokno AC, Silber SJ, et al. Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol. 1972;107:458-461.
Latham RH, Running K, Stamm WE. Urinary tract infections in young adult women caused by Staphylococcus saprophyticus. JAMA. 1983;250:3063-3066.
Latham RH, Wong ES, Larson A, et al. Laboratory diagnosis of urinary tract infection in ambulatory women. JAMA. 1985;254:3333-3336.
Lee JK, McClennan BL, Melson GL, et al. Acute focal bacterial nephritis: emphasis on gray scale sonography and computed tomography. AJR Am J Roentgenol. 1980;135:87-92.
Leffler H, Svanborg-Eden C. Chemical identification of glycosphingolipid receptor for Escherichia coli attaching tp human urinary tract epithelial cells and agglutinating erythrocytes. FEMS Microbiol Lett. 1980:127.
Leibovici L, Greenshtain S, Cohen O, et al. Toward improved empiric management of moderate to severe urinary tract infections. Arch Intern Med. 1992;152:2481-2486.
Levin R, Burbige KA, Abramson S, et al. Diagnosis and management of renal inflammatory processes in children. J Urol. 1984;132:718-721.
Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31:1250-1256.
Lewin KJ, Fair WR, Steigbigel RT, et al. Clinical and laboratory studies into the pathogenesis of malacoplakia. J Clin Pathol. 1976;29:354-363.
Liedl B. Catheter-associated urinary tract infections. Curr Opin Urol. 2001;11:75-79.
Lincoln K, Lidin-Janson G, Winberg J. Resistant urinary infections resulting from changes in resistance pattern of faecal flora induced by sulphonamide and hospital environment. BMJ. 1970;3:305-309.
Lindberg U, Hanson LA, Jodal U, et al. Asymptomatic bacteriuria in schoolgirls. II. Differences in Escherichia coli causing asymptomatic bacteriuria. Acta Paediatr Scand. 1975;64:432-436.
Lindner LE, Jones RN, Haber MH. A specific urinary cast in acute pyelonephritis. Am J Clin Pathol. 1980;73:809-811.
Lindvall N. Radiological changes of renal papillary necrosis. Kidney Int. 1978;13:93-106.
Lipsky BA. Urinary tract infections in men: epidemiology, pathophysiology, diagnosis, and treatment. Ann Intern Med. 1989;110:138-150.
Ljungh A, Wadstrom T. Fimbriation of Escherichia coli in urinary tract infections: comparisons between bacteria in the urine and subcultured bacterial isolates. Curr Microbiol. 1983;8:263.
Lo E, Nicolle L, Classen D, et al. Strategies to prevent catheter-associated urinary tract infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29(Suppl. 1):S41-S50.
Lomberg H, Hanson LA, Jacobsson B, et al. Correlation of P blood group, vesicoureteral reflux, and bacterial attachment in patients with recurrent pyelonephritis. N Engl J Med. 1983;308:1189-1192.
Lorentzen M, Nielsen HO. Xanthogranulomatous pyelonephritis. Scand J Urol Nephrol. 1980;14:193-200.
Lyons RW, Long JM, Lytton B, et al. Arteriography and antibiotic therapy of a renal carbuncle. J Urol. 1972;107:524-526.
Mabeck CE. Studies in urinary tract infections. I. The diagnosis of bacteriuria in women. Acta Med Scand. 1969;186:35-38.
Mabeck CE. Treatment of uncomplicated urinary tract infection in non-pregnant women. Postgrad Med J. 1972;48:69-75.
MacDonald P, Alexander D, Catz C, et al. Summary of a workshop on maternal genitourinary infections and the outcome of pregnancy. J Infect Dis. 1983;147:596-605.
Macrea L. Fulminant gangrene of the penis. Clinic. 1945;4:796.
Maderazo EG, Berlin BB, Morhardt C. Treatment of malakoplakia with trimethoprim-sulfamethoxazole. Urology. 1979;13:70-73.
Madge GE, Lombardias S. Chronic liver disease and renal papillary necrosis with Aspergillus. South Med J. 1973;66:486-488.
Maizels M, Schaeffer AJ. Decreased incidence of bacteriuria associated with periodic instillations of hydrogen peroxide into the urethral catheter drainage bag. J Urol. 1980;123:841-845.
Malek RS, Elder JS. Xanthogranulomatous pyelonephritis: a critical analysis of 26 cases and of the literature. J Urol. 1978;119:589-593.
Malek RS, Greene LF, DeWeerd JH, et al. Xanthogranulomatous pyelonephritis. Br J Urol. 1972;44:296-308.
Manges AR, Dietrich PS, Riley LW. Multidrug-resistant Escherichia coli clonal groups causing community-acquired pyelonephritis. Clin Infect Dis. 2004;38:329-334.
Manson AL. Is antibiotic administration indicated after outpatient cystoscopy. J Urol. 1988;140:316-317.
Marrie TJ, Harding GK, Ronald AR. Anaerobic and aerobic urethral flora in healthy females. J Clin Microbiol. 1978;8:67-72.
Martens M, Kaul A, Nowicki S. Presence of receptors for Dr-hemagglutinin of uropathogenic E. coli in the uterus of pregnant rats, Acapulco, Mexico. Proc. Third World Congress for Infectious Diseases in OB/GYN, 1993.
Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546-1554.
Martinez F, Kindrachuk R, Thomas E, et al. Effect of prophylactic, low dose cephalexin on fecal and vaginal bacteria. J Urol. 1985;133:994-996.
Martinez JJ, Hultgren SJ. Requirement of Rho-family GTPases in the invasion of type 1-piliated uropathogenic Escherichia coli. Cell Microbiol. 2002;4:19-28.
Martorana G, Giberti C, Pescatore D. Giant echinococcal cyst of the kidney associated with hypertension evaluated by computerized tomography. J Urol. 1981;126:99-100.
Mauro MA, Balfe DM, Stanley RJ, et al. Computed tomography in the diagnosis and management of the renal mass. JAMA. 1982;248:2894-2896.
McAfee JG. Radionuclide imaging in the assessment of primary chronic pyelonephritis. Radiology. 1979;133:203-206.
McCabe WR, Jackson GG. Treatment of pyelonephritis: bacterial, drug and host factors in success or failure among 252 patients. N Engl J Med. 1965;272:0137-0144.
McClure J. Malakoplakia. J Pathol. 1983;140:275-330.
McCue JD. Urinary tract infection and dysuria: cost-conscious evaluation and antibiotic therapy. Postgrad Med. 1986;80:133-134. 139–42
McDonald GS. Xanthogranulomatous pyelonephritis. J Pathol. 1981;133:203-213.
McFadyen IR, Eykyn SJ, Gardner NH, et al. Bacteriuria in pregnancy. J Obstet Gynaecol Br Commonw. 1973;80:385-405.
McIsaac WJ, Low DE, Biringer A, et al. The impact of empirical management of acute cystitis on unnecessary antibiotic use. Arch Intern Med. 2002;162:600-605.
McMurdo ME, Argo I, Phillips G, et al. Cranberry or trimethoprim for the prevention of recurrent urinary tract infections? A randomized controlled trial in older women. J Antimicrob Chemother. 2009;63:389-395.
McMurdo ME, Gillespie ND. Urinary tract infection in old age: over-diagnosed and over-treated. Age Ageing. 2000;29:297-298.
McNair R, MacDonald S, Dooley S, et al. Evaluation of the centrifuged and Gram-stained smear, urinalysis, and reagent strip testing to detect asymptomatic bacteriuria in obstetric patients. Am J Obstet Gynecol. 2000;182:1076-1079.
Mears E. Campbell’s urology. Philadelphia: WB Saunders; 1978.
Meiland R, Geerlings SE, Hoepelman AI. Management of bacterial urinary tract infections in adult patients with diabetes mellitus. Drugs. 2002;62:1859-1868.
Melekos MD, Asbach HW, Gerharz E, et al. Post-intercourse versus daily ciprofloxacin prophylaxis for recurrent urinary tract infections in premenopausal women. J Urol. 1997;157:935-939.
Meleney F. A diiferential diagnosis between certain types of infectious gangrene of the skin, with particular reference to hemolytic streptococcal gangrene and bacterial synergistic gangrene. Surg Gynecol Obstet. 1933;56:842.
Merenich WM, Popky GL. Radiology of renal infection. Med Clin North Am. 1991;75:425-469.
Mering JH, Kaplan GW, McLaughlin AP3rd. Xanthogranulomatous pyelonephritis. Unusual clinical presentations. Urology. 1973;1:338-342.
Michaelis L, Gutmann C. Über Einschlüsse in Blasentumoren. Z Klin Med. 1902;47:208.
Michaels EK, Fowler JEJr, Mariano M. Bacteriuria following extracorporeal shock wave lithotripsy of infection stones. J Urol. 1988;140:254-256.
Miller JD. The importance of early diagnosis and surgical treatment of necrotizing fasciitis. Surg Gynecol Obstet. 1983;157:197-200.
Miller K, O’Neill A, Chopra I. Escherichia coli mutators present an enhanced risk for emergence of antibiotic resistance during urinary tract infections. Antimicrob Agents Chemother. 2004;48:23-29.
Mobley HL, Warren JW. Urease-positive bacteriuria and obstruction of long-term urinary catheters. J Clin Microbiol. 1987;25:2216-2217.
Mollier S, Descotes JL, Pasquier D, et al. Pseudoneoplastic xanthogranulomatous pyelonephritis: a typical clinical presentation but unusual diagnosis and treatment. Eur Urol. 1995;27:170-173.
Monane M, Gurwitz JH, Lipsitz LA, et al. Epidemiologic and diagnostic aspects of bacteriuria: a longitudinal study in older women. J Am Geriatr Soc. 1995;43:618-622.
Monson T, Kunin CM. Evaluation of a polymer-coated indwelling catheter in prevention of infection. J Urol. 1974;111:220-222.
Moreno E, Andreu A, Pigrau C, et al. Relationship between Escherichia coli strains causing acute cystitis in women and the fecal E. coli population of the host. J Clin Microbiol. 2008;46:2529-2534.
Morris MJ, Golovsky D, Guinness MD, et al. The value of prophylactic antibiotics in transurethral prostatic resection: a controlled trial, with observations on the origin of postoperative infection. Br J Urol. 1976;48:479-484.
Morton SC, Shekelle PG, Adams JL, et al. Antimicrobial prophylaxis for urinary tract infection in persons with spinal cord dysfunction. Arch Phys Med Rehabil. 2002;83:129-138.
Mulvey MA. Adhesion and entry of uropathogenic Escherichia coli. Cell Microbiol. 2002;4:257-271.
Mulvey MA, Lopez-Boado YS, Wilson CL, et al. Induction and evasion of host defenses by type 1-piliated uropathogenic Escherichia coli. Science. 1998;282:1494-1497.
Mulvey MA, Schilling JD, Hultgren SJ. Establishment of a persistent Escherichia coli reservoir during the acute phase of a bladder infection. Infect Immun. 2001;69:4572-4579.
Mulvey MA, Schilling JD, Martinez JJ, et al. Bad bugs and beleaguered bladders: interplay between uropathogenic Escherichia coli and innate host defenses. Proc Natl Acad Sci U S A. 2000;97:8829-8835.
Murray T, Goldberg M. Chronic interstitial nephritis: etiologic factors. Ann Intern Med. 1975;82:453-459.
Nabizadeh I, Morehouse HT, Freed SZ. Hydatid disease of kidney. Urology. 1983;22:176-178.
Najenson T, Mendelson L, Sabransky H, et al. Upper urinary tract in patients after traumatic spinal cord injury. Paraplegia. 1969;7:85-96.
Nataluk EA, McCullough DL, Scharling EO. Xanthogranulomatous pyelonephritis, the gatekeeper’s dilemma: a contemporary look at an old problem. Urology. 1995;45:377-380.
National Institute on Disability and Rehabilitation Research. The prevention and management of urinary tract infections among people with spinal cord injuries. National Institute on Disability and Rehabilitation Research consensus statement. January 27–29, 1992. SCI Nurs. 1993;10:49-61.
Navas EL, Venegas MF, Duncan JL, et al. Blood group antigen expression on vaginal and buccal epithelial cells and mucus in secretor and nonsecretor women. J Urol. 1993;149:1492-1498.
Newman CG, O’Neill P, Parker A. Pyuria in infancy, and the role of suprapubic aspiration of urine in diagnosis of infection of urinary tract. BMJ. 1967;2:277-279.
Newton T, Still JM, Law E. A comparison of the effect of early insertion of standard latex and silver-impregnated latex foley catheters on urinary tract infections in burn patients. Infect Control Hosp Epidemiol. 2002;23:217-218.
Nickel JC, Grant SK, Costerton JW. Catheter-associated bacteriuria: an experimental study. Urology. 1985;26:369-375.
Nickel JC, Olson ME, Costerton JW. In vivo coefficient of kinetic friction: study of urinary catheter biocompatibility. Urology. 1987;29:501-503.
Nicolau D, Freeman C, Belliveau P, et al. Experience with a once-daily aminoglycoside program administered to 2,184 adult patients. Antimicrob Agents Chemother. 1995;39:650-655.
Nicolle LE. Use of antimicrobials during pregnancy. Can Fam Physician. 1987;33:1247-1251.
Nicolle LE. Urinary tract infection in the elderly. J Antimicrob Chemother. 1994;33(Suppl. A):99-109.
Nicolle LE, Bjornson J, Harding GK, et al. Bacteriuria in elderly institutionalized men. N Engl J Med. 1983;309:1420-1425.
Nicolle LE, Bradley S, Colgan R, et al. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clin Infect Dis. 2005;40:643-654.
Nicolle LE, Friesen D, Harding GK, et al. Hospitalization for acute pyelonephritis in Manitoba, Canada, during the period from 1989 to 1992; impact of diabetes, pregnancy, and aboriginal origin. Clin Infect Dis. 1996;22:1051-1056.
Nicolle LE, Harding GK, Preiksaitis J, et al. The association of urinary tract infection with sexual intercourse. J Infect Dis. 1982;146:579-583.
Nicolle LE, Harding GK, Thompson M, et al. Prospective, randomized, placebo-controlled trial of norfloxacin for the prophylaxis of recurrent urinary tract infection in women. Antimicrob Agents Chemother. 1989;33:1032-1035.
Nicolle LE, Mayhew WJ, Bryan L. Prospective randomized comparison of therapy and no therapy for asymptomatic bacteriuria in institutionalized elderly women. Am J Med. 1987;83:27-33.
Nicolle LE, Ronald AR. Recurrent urinary tract infection in adult women: diagnosis and treatment. Infect Dis Clin North Am. 1987;1:793-806.
Nielsen HO, Lorentzen M. Xanthogranulomatous pyelonephritis: an immunohistochemical and ultrastructural study on the occurrence of bacteria and bacterial antigen. Urol Int. 1981;36:335-340.
Niël-Weise BS, van den Broek PJ. Antibiotic policies for short-term catheter bladder drainage in adults. Cochrane Database Syst Rev. 2005;(3):CD005428.
Nord CE. Effect of new quinolones on the human gastrointestinal microflora. Rev Infect Dis. 1988;10(Suppl. 1):S193-S196.
Norden CW, Kass EH. Bacteriuria of pregnancy—a critical appraisal. Annu Rev Med. 1968;19:431-470.
Nordenstam GR, Brandberg CA, Oden AS, et al. Bacteriuria and mortality in an elderly population. N Engl J Med. 1986;314:1152-1156.
Norrby SR. Short-term treatment of uncomplicated lower urinary tract infections in women. Rev Infect Dis. 1990;12:458-467.
Nowicki B, Martens M, Hart A, et al. Gestational age-dependent distribution of Escherichia coli fimbriae in pregnant patients with pyelonephritis. Ann N Y Acad Sci. 1994;730:290-291.
Nyren P, Runeberg L, Kostiala AI, et al. Prophylactic methenamine hippurate or nitrofurantoin in patients with an indwelling urinary catheter. Ann Clin Res. 1981;13:16-21.
O’Hanley P. A globoside binding E. coli pilus vaccine prevents pyelonephritis. Clin Res. 1983:327A.
Oelschlaeger TA, Dobrindt U, Hacker J. Pathogenicity islands of uropathogenic E. coli and the evolution of virulence. Int J Antimicrob Agents. 2002;19:517-521.
Ofek I, Mosek A, Sharon N. Mannose-specific adherence of Escherichia coli freshly excreted in the urine of patients with urinary tract infections, and of isolates subcultured from the infected urine. Infect Immun. 1981;34:708-711.
Olsson PJ, Black JR, Gaffney E, et al. Reversible acute renal failure secondary to acute pyelonephritis. South Med J. 1980;73:374-376.
Ooi BS, Chen BT, Yu M. Prevalence and site of bacteriuria in diabetes mellitus. Postgrad Med J. 1974;50:497-499.
Osca JM, Peiro MJ, Rodrigo M, et al. Focal xanthogranulomatous pyelonephritis: partial nephrectomy as definitive treatment. Eur Urol. 1997;32:375-379.
Ouslander JG, Schapira M, Schnelle JF, et al. Does eradicating bacteriuria affect the severity of chronic urinary incontinence in nursing home residents? Ann Intern Med. 1995;122:749-754.
Ouslander JG, Schapira M, Schnelle JF, et al. Pyuria among chronically incontinent but otherwise asymptomatic nursing home residents. J Am Geriatr Soc. 1996;44:420-423.
Parker J, Kunin C. Pyelonephritis in young women: a 10- to 20- year follow-up. JAMA. 1973;224:585-590.
Parsons MA, Harris SC, Longstaff AJ, et al. Xanthogranulomatous pyelonephritis: a pathological, clinical and aetiological analysis of 87 cases. Diagn Histopathol. 1983;6:203-219.
Patterson T, Andriole V. Bacteriuria in pregnancy. Infect Dis Clin North Am. 1987;1:807-822.
Patton JP, Nash DB, Abrutyn E. Urinary tract infection: economic considerations. Med Clin North Am. 1991;75:495-513.
Paty R, Smith AD. Gangrene and Fournier’s gangrene. Urol Clin North Am. 1992;19:149-162.
Payne SR, Timoney AG, McKenning ST, et al. Microbiological look at urodynamic studies. Lancet. 1988;2:1123-1126.
Pearle MS, Roehrborn CG. Antimicrobial prophylaxis prior to shock wave lithotripsy in patients with sterile urine before treatment: a meta-analysis and cost-effectiveness analysis. Urology. 1997;49:679-686.
Pearson NJ, Towner KJ, McSherry AM, et al. Emergence of trimethoprim-resistant enterobacteria in patients receiving long-term co-trimoxazole for the control of intractable urinary-tract infection. Lancet. 1979;2:1205-1208.
Pedler SJ, Bint AJ. Management of bacteriuria in pregnancy. Drugs. 1987;33:413-421.
Pels RJ, Bor DH, Woolhandler S, et al. Dipstick urinalysis screening of asymptomatic adults for urinary tract disorders. II. Bacteriuria. JAMA. 1989;262:1221-1224.
Peschers UM, Kempf V, Jundt K, et al. Antibiotic treatment to prevent urinary tract infections after urodynamic evaluation. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12:254-257.
Petronic V, Buturovic J, Isvaneski M. Xanthogranulomatous pyelonephritis. Br J Urol. 1989;64:336-338.
Pezzlo M. Detection of urinary tract infections by rapid methods. Clin Microbiol Rev. 1988;1:268-280.
Pfaller MA, Koontz FP. Laboratory evaluation of leukocyte esterase and nitrite tests for the detection of bacteriuria. J Clin Microbiol. 1985;21:840-842.
Pfau A, Rosenmann E. Unilateral chronic pyelonephritis and hypertension: coincidental or causal relationship? Am J Med. 1978;65:499-506.
Pfau A, Sacks T. The bacterial flora of the vaginal vestibule, urethra and vagina in the normal premenopausal woman. J Urol. 1977;118:292-295.
Pfau A, Sacks T, Engelstein D. Recurrent urinary tract infections in premenopausal women: prophylaxis based on an understanding of the pathogenesis. J Urol. 1983;129:1153-1157.
Pfau A, Sacks T. Effective prophylaxis for recurrent urinary tract infections during pregnancy. Clin Infect Dis. 1992;14:810-814.
Pinson AG, Philbrick JT, Lindbeck GH, et al. ED management of acute pyelonephritis in women: a cohort study. Am J Emerg Med. 1994;12:271-278.
Pitts JC, Peterson NE, Conley MC. Calcified functionless kidney in a 51-year-old man. J Urol. 125, 1981. 398–341
Plorde L. Echinococciasis. In: Thorn G, editor. Harrison’s principles of internal medicine. New York: McGraw-Hill; 1977:117-118.
Polastri F, Auckenthaler R, Loew F, et al. Absence of significant bacteremia during urinary catheter manipulation in patients with chronic indwelling catheters. J Am Geriatr Soc. 1990;38:1203-1208.
Poljakovic M, Persson K. Urinary tract infection in iNOS-deficient mice with focus on bacterial sensitivity to nitric oxide. Am J Physiol Renal Physiol. 2003;284:F22-F31.
Poljakovic M, Svensson ML, Svanborg C, et al. Escherichia coli-induced inducible nitric oxide synthase and cyclooxygenase expression in the mouse bladder and kidney. Kidney Int. 2001;59:893-904.
Poole JH, Thorsen MS. Acute renal failure in pregnancy. Am J Maternal/Child Nurs. 1999;24:66-73.
Poulios C. Echinococcal disease of the urinary tract: review of the management of 7 cases. J Urol. 1991;145:924-927.
Povysil C, Konickova L. Experimental xanthogranulomatous pyelonephritis. Invest Urol. 1972;9:313-318.
Preiksaitis JK, Thompson L, Harding GK, et al. A comparison of the efficacy of nalidixic acid and cephalexin in bacteriuric women and their effect on fecal and periurethral carriage of enterobacteriaceae. J Infect Dis. 1981;143:603-608.
Preston A, O’Donnell T, Phillips CA. Screening for urinary tract infections in a gynaecological setting: validity and cost-effectiveness of reagent strips. Br J Biomed Sci. 1999;56:253-257.
Pyrah LN, Goldie W, Parsons FM, et al. Control of Pseudomonas pyocyanea infection in a urological ward. Lancet. 1955;269:314-317.
Rajan N, Cao Q, Anderson BE, et al. Roles of glycoproteins and oligosaccharides found in human vaginal fluid in bacterial adherence. Infect Immun. 1999;67:5027-5032.
Rane A, Cahill D, Saleemi A, et al. The issue of prophylactic antibiotics prior to flexible cystoscopy. Eur Urol. 2001;39:212-214.
Raz R, Boger S. Long-term prophylaxis with norfloxacin versus nitrofurantoin in women with recurrent urinary tract infection. Antimicrob Agents Chemother. 1991;35:1241-1242.
Raz R, Chazan B, Dan M. Cranberry juice and urinary tract infection. Clin Infect Dis. 2004;38:1413-1419.
Raz R, Sakran W, Chazan B, et al. Long-term follow-up of women hospitalized for acute pyelonephritis. Clin Infect Dis. 2003;37:1014-1020.
Raz R, Stamm WE. A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. N Engl J Med. 1993;329:753-756.
Reid G, Sobel JD. Bacterial adherence in the pathogenesis of urinary tract infection: a review. Rev Infect Dis. 1987;9:470-487.
Reid G, Zorzitto M, Bruce A. Pathogenesis of urinary tract infection in the elderly: the role of bacterial adherence to uroepithelial cells. Cell Microbiol. 1984;11:67.
Ribot S, Gal K, Goldblat MV, et al. The role of anaerobic bacteria in the pathogenesis of urinary tract infections. J Urol. 1981;126:852-853.
Richet G, Mayaud C. The course of acute renal failure in pyelonephritis and other types of interstitial nephritis. Nephron. 1978;22:124-127.
Robbins S, Tucker A. The cause of death in diabetes. N Engl J Med. 1944:865.
Roberts AP, Phillips R. Bacteria causing symptomatic urinary tract infection or asymptomatic bacteriuria. J Clin Pathol. 1979;32:492-496.
Rocha H, Santos LCS. Relapse of urinary infection in the presence of urinary tract calculi: the role of bacteria within the calculi. J Med Microbiol. 1969;2:372-376.
Romano JM, Kaye D. UTI in the elderly: common yet atypical. Geriatrics. 1981;36:113-115. 20
Ronald A. The etiology of urinary tract infection: traditional and emerging pathogens. Am J Med. 2002;113(Suppl. 1A):14S-19S.
Ronald AR, Jagdis FA, Harding GK, et al. Amoxicillin therapy of acute urinary infections in adults. Antimicrob Agents Chemother. 1977;11:780-784.
Rosenberg M. Pharmacoeconomics of treating uncomplicated urinary tract infections. Int J Antimicrob Agents. 1999;11:247-251. discussion 261–244
Rosenfield AT, Glickman MG, Taylor KJ, et al. Acute focal bacterial nephritis (acute lobar nephronia). Radiology. 1979;132:553-561.
Rubin RH, Beam TRJr, Stamm WE. An approach to evaluating antibacterial agents in the treatment of urinary tract infection. Clin Infect Dis. 1992;14(Suppl. 2):S246-S251. discussion S253–44
Russo TA, Carlino UB, Mong A, et al. Identification of genes in an extraintestinal isolate of Escherichia coli with increased expression after exposure to human urine. Infect Immun. 1999;67:5306-5314.
Sabbagh R, McCormack M, Peloquin F, et al. A prospective randomized trial of 1-day versus 3-day antibiotic prophylaxis for transrectal ultrasound guided prostate biopsy. Can J Urol. 2004;11:2216-2219.
Saeed SM, Fine G. Xanthogranulomatous pyelonephritis. Am J Clin Pathol. 1963;39:616-625.
Saint S, Elmore JG, Sullivan SD, et al. The efficacy of silver alloy-coated urinary catheters in preventing urinary tract infection: a meta-analysis. Am J Med. 1998;105:236-241.
Saint S, Veenstra DL, Sullivan SD, et al. The potential clinical and economic benefits of silver alloy urinary catheters in preventing urinary tract infection. Arch Intern Med. 2000;160:2670-2675.
Saint Martin G, Chiesa JC. “Falling snowflakes,” an ultrasound sign of hydatid sand. J Ultrasound Med. 1984;3:257-260.
Salvatierra OJr, Bucklew WB, Morrow JW. Perinephric abscess: a report of 71 cases. J Urol. 1967;98:296-302.
Sanchez-Ramos L, McAlpine KJ, Adair CD, et al. Pyelonephritis in pregnancy: once-a-day ceftriaxone versus multiple doses of cefazolin. A randomized, double-blind trial. Am J Obstet Gynecol. 1995;172:129-133.
Sandberg T, Brorson JE. Efficacy of long-term antimicrobial prophylaxis after acute pyelonephritis in pregnancy. Scand J Infect Dis. 1991;23:221-223.
Sanford JP, Favour CB, Mao FH, et al. Evaluation of the positive urine culture: an approach to the differentiation of significant bacteria from contaminants. Am J Med. 1956;20:88-93.
Schaeffer A. Urinary tract infections in the elderly. Eur Urol. 1991;19(Suppl. 1):2-6.
Schaeffer A. Role of vaginal colonization in urinary tract infections (UTIs). In: Baskin LS, editor. Advances in bladder research, vol. 462. New York: Kluwer Academic/Plenum Publishers; 1999:339-349.
Schaeffer A, Jones DM, Dunn JK. Association of in vitro E. coli adherence to vaginal and buccal epithelial cells with susceptibility of women to recurrent urinary tract infections. N Engl J Med. 1981;304:1062-1066.
Schaeffer A, Navas EL, Venegas MF, et al. Variation of blood group antigen expression on vaginal cells and mucus in secretor and nonsecretor women. J Urol. 1994;152:859-864.
Schaeffer A, Radvany R, Chmiel J. Human leukocyte antigens in women with recurrent urinary tract infections. J Infect Dis. 1983;148:604.
Schaeffer A, Schwan W, Hultgren S, et al. Relationship of type 1 pilus expression in Escherichia coli to ascending urinary tract infections in mice. Infect Immun. 1987;55:373-380.
Schaeffer A, Story K, Johnson S. Effect of silver oxide/trichloroisocyanuric acid antimicrobial urinary drainage system on catheter-associated bacteriuria. J Urol. 1988;139:69-73.
Schaeffer A, Stuppy B. Efficacy and safety of self-start therapy in women with recurrent urinary tract infections. J Urol. 1999;161:207-211.
Schaeffer E. Prophylactic use of antimicrobials in commonly performed outpatient urologic procedures. Nat Clin Pract Urol. 2006;3:24-31.
Schainuck LI, Fouty R, Cutler RE. Emphysematous pyelonephritis: a new case and review of previous observations. Am J Med. 1968;44:134-139.
Schappert SM. Ambulatory care visits of physician offices, hospital outpatient departments, and emergency departments: United States, 1995. Vital Health Stat 13. 1997:1-38.
Schechter H, Leonard CD, Scribner BH. Chronic pyelonephritis as a cause of renal failure in dialysis candidates: analysis of 173 patients. JAMA. 1971;216:514-517.
Schiff MJr, Glickman M, Weiss RM, et al. Antibiotic treatment of renal carbuncle. Ann Intern Med. 1977;87:305-308.
Schlager TA, Hendley JO, Bell AL, et al. Clonal diversity of Escherichia coli colonizing stools and urinary tracts of young girls. Infect Immun. 2002;70:1225-1229.
Schneider M, Becker JA, Staiano S, et al. Sonographic-radiographic correlations of renal and perirenal infections. AJR Am J Roentgenol. 1976;127:1007-1014.
Schoborg TW, Saffos RO, Urdaneta L, et al. Xanthogranulomatous pyelonephritis associated with renal carcinoma. J Urol. 1980;124:125-127.
Schonwald S, Begovac J, Skerk V. Urinary tract infections in HIV disease. Int J Antimicrob Agents. 1999;11:309-311.
Schultz HJ, McCaffrey LA, Keys TF, et al. Acute cystitis: a prospective study of laboratory tests and duration of therapy. Mayo Clin Proc. 1984;59:391-397.
Sedor J, Mulholland SG. Hospital-acquired urinary tract infections associated with the indwelling catheter. Urol Clin North Am. 1999;26:821-828.
Segura JW, Kelalis PP. Localized renal parenchymal infections in children. J Urol. 1973;109:1029-1032.
Semeniuk H, Church D. Evaluation of the leukocyte esterase and nitrite urine dipstick screening tests for detection of bacteriuria in women with suspected uncomplicated urinary tract infections. J Clin Microbiol. 1999;37:3051-3052.
Sessler CN, Perry JC, Varney KL. Management of severe sepsis and septic shock. Curr Opin Crit Care. 2004;10:354-363.
Sexton CC, Lowman RM, Nyongo AO, et al. Malacoplakia presenting as complete unilateral ureteral obstruction. J Urol. 1982;128:139-141.
Sharp JL. The growth of Candida albicans during antibiotic therapy. Lancet. 1954;266:390-392.
Sheinfeld J, Schaeffer AJ, Cordon-Cardo C, et al. Association of the Lewis blood-group phenotype with recurrent urinary tract infections in women. N Engl J Med. 1989;320:773-777.
Shen Y, Brown MA. Renal imaging in pyelonephritis. Nephrology (Carlton). 2004;9:22-25.
Shetty SD, al-Saigh A, Ibrahim AI, et al. Management of hydatid cysts of the urinary tract. Br J Urol. 1992;70:258-261.
Shimizu S, Takimoto Y, Niimura T, et al. A case of prostatic malacoplakia. J Urol. 1981;126:277-279.
Shortliffe LM, McNeal JE, Wehner N, et al. Persistent urinary infections in a young woman with bilateral renal stones. J Urol. 1984;131:1147-1151.
Shu T, Green JM, Orihuela E. Renal and perirenal abscesses in patients with otherwise anatomically normal urinary tracts. J Urol. 2004;172:148-150.
Sieber PR, Rommel FM, Agusta VE, et al. Antibiotic prophylaxis in ultrasound guided transrectal prostate biopsy. J Urol. 1997;157:2199-2200.
Siegel J, Smith A, Moldwin R. Minimally invasive treatment of renal abscess. J Urol. 1996;155:52-55.
Silverblatt FJ, Dreyer JS, Schauer S. Effect of pili on susceptibility of Escherichia coli to phagocytosis. Infect Immun. 1979;24:218-223.
Silverman DE, Stamey TA. Management of infection stones: the Stanford experience. Medicine (Baltimore). 1983;62:44-51.
Siroky MB, Moylan R, Austen GJr, et al. Metastatic infection secondary to genitourinary tract sepsis. Am J Med. 1976;61:351-360.
Smaill F. Antibiotics for asymptomatic bacteriuria in preganancy. Cochrane Database Syst Rev. 2001;(2):CD000490.
Smeets F, Gower PE. The site of infection in 133 patients with bacteriuria. Clin Nephrol. 1973;1:290-296.
Smellie J, Edwards D, Hunter N, et al. Vesico-ureteric reflux and renal scarring. Kidney Int Suppl. 1975;4:S65-S72.
Soler R, Pombo F, Gayol A, et al. Focal xanthogranulomatous pyelonephritis in a teenager: MR and CT findings. Eur J Radiol. 1997;24:77-79.
Solomon A, Braf Z, Papo J, et al. Computerized tomography in xanthogranulomatous pyelonephritis. J Urol. 1983;130:323-325.
Sorsa LJ, Dufke S, Heesemann J, et al. Characterization of an iroBCDEN gene cluster on a transmissible plasmid of uropathogenic Escherichia coli: evidence for horizontal transfer of a chromosomal virulence factor. Infect Immun. 2003;71:3285-3293.
Soulen MC, Fishman EK, Goldman SM, et al. Bacterial renal infection: role of CT. Radiology. 1989;171:703-707.
Sourander L. Urinary tract infections in the aged: an epidemiological study. Ann Med Intern Fenn. 1966;55:7.
Sparks A, Connor D, Neafie R. Echinococcosis. In: Binford C, Connor D, editors. Pathology of tropical and extraordinary diseases. Washington DC: Armed Forces Institute of Pathology; 1976:530-533.
Spirnak JP, Resnick MI, Hampel N, et al. Fournier’s gangrene: report of 20 patients. J Urol. 1984;131:289-291.
Stahlmann R, Lode H. Fluoroquinolones in the elderly: safety considerations. Drugs Aging. 2003;20:289-302.
Stamenkovic I, Lew PD. Early recognition of potentially fatal necrotizing fasciitis: the use of frozen-section biopsy. N Engl J Med. 1984;310:1689-1693.
Stamey T. Pathogenesis and treatment of urinary tract infections. Baltimore: Williams & Wilkins Company; 1980.
Stamey T, Condy M. The diffusion and concentration of trimethoprim in human vaginal fluid. J Infect Dis. 1975;131:261-266.
Stamey T, Condy M, Mihara G. Prophylactic efficacy of nitrofurantoin macrocrystals and trimethoprim-sulfamethoxazole in urinary infections: biologic effects on the vaginal and rectal flora. N Engl J Med. 1977;296:780-783.
Stamey T, Fair W, Timothy M, et al. Serum versus urinary antimicrobial concentrations in cure of urinary-tract infections. N Engl J Med. 1974;291:1159-1163.
Stamey T, Govan D, Palmer J. The localization and treatment of urinary tract infections: the role of bactericidal urine levels as opposed to serum levels. Medicine (Baltimore). 1965;44:1-36.
Stamey T, Pfau A. Some functional, pathologic, bacteriologic, and chemotherapeutic characteristics of unilateral pyelonephritis in man. II. Bacteriologic and chemotherapeutic characteristics. Invest Urol. 1963;1:162-172.
Stamey TA, Timothy MM. Studies of introital colonization in women with recurrent urinary infections. I. The role of vaginal pH. J Urol. 1975;114:261-263.
Stamey TA, Wehner N, Mihara G, et al. The immunologic basis of recurrent bacteriuria: role of cervicovaginal antibody in enterobacterial colonization of the introital mucosa. Medicine (Baltimore). 1978;57:47-56.
Stamm WE. Guidelines for prevention of catheter-associated urinary tract infections. Ann Intern Med. 1975;82:386-390.
Stamm WE. Recent developments in the diagnosis and treatment of urinary tract infections. West J Med. 1982;137:213-220.
Stamm WE. When should we use urine cultures? Infect Control. 1986;7:431-433.
Stamm WE. Catheter-associated urinary tract infections: epidemiology, pathogenesis, and prevention. Am J Med. 1991;91:65S-71S.
Stamm WE, Counts G, McKevitt M, et al. Urinary prophylaxis with trimethoprim and trimethoprim-sulfamethoxazole: efficacy, influence on the natural history of recurrent bacteriuria, and cost control. Rev Infect Dis. 1982;4:450-455.
Stamm WE, Counts GW, Running KR, et al. Diagnosis of coliform infection in acutely dysuric women. N Engl J Med. 1982;307:463-468.
Stamm WE, Counts GW, Wagner KF, et al. Antimicrobial prophylaxis of recurrent urinary tract infections: a double-blind, placebo-controlled trial. Ann Intern Med. 1980;92:770-775.
Stamm WE, Hooton T. Management of urinary tract infections in adults. N Engl J Med. 1993;329:1328-1334.
Stamm WE, Running K, McKevitt M, et al. Treatment of the acute urethral syndrome. N Engl J Med. 1981;304:956-958.
Stamm WE, Wagner KF, Amsel R, et al. Causes of the acute urethral syndrome in women. N Engl J Med. 1980;303:409-415.
Stanton MJ, Lynch JH, Maxted WC, et al. Malacoplakia of the bladder: a case report of resolution with bethanechol, trimethoprim-sulfamethoxazole and ascorbic acid. J Urol. 1983;130:1174-1175.
Stanton MJ, Maxted W. Malacoplakia: a study of the literature and current concepts of pathogenesis, diagnosis and treatment. J Urol. 1981;125:139-146.
Stapleton A. Urinary tract infections in patients with diabetes. Am J Med. 2002;113(Suppl. 1A):80S-84S.
Stapleton A, Hooton TM, Fennell C, et al. Effect of secretor status on vaginal and rectal colonization with fimbriated Escherichia coli in women with and without recurrent urinary tract infection. J Infect Dis. 1995;171:717-720.
Stark RP, Maki DG. Bacteriuria in the catheterized patient: what quantitative level of bacteriuria is relevant? N Engl J Med. 1984;311:560-564.
Stenqvist K, Dahlen-Nilsson I, Lidin-Janson G, et al. Bacteriuria in pregnancy: frequency and risk of acquisition. Am J Epidemiol. 1989;129:372-379.
Stothers L. A randomized trial to evaluate effectiveness and cost effectiveness of naturopathic cranberry products as prophylaxis against urinary tract infection in women. Can J Urol. 2002;9:1558-1562.
Stover SL, Lloyd LK, Waites KB, et al. Urinary tract infection in spinal cord injury. Arch Phys Med Rehabil. 1989;70:47-54.
Sun TT. Epithelial growth and differentiation: an overview. Mol Biol Rep. 1996;23:1-2.
Svanborg C, Godaly G. Bacterial virulence in urinary tract infection. Infect Dis Clin North Am. 1997;11:513-529.
Svanborg-Eden C, Svennerholm AM. Secretory immunoglobulin A and G antibodies prevent adhesion of Escherichia coli to human urinary tract epithelial cells. Infect.Immun.. 1978;22:790-797.
Svenson SB, Hultberg H, Kallenius G, et al. P-fimbriae of pyelonephritogenic Escherichia coli: identification and chemical characterization of receptors. Infection. 1983;11:61-67.
Svenson SB, Kallenius G, Korhonen TK, et al. Initiation of clinical pyelonephritis—the role of P-fimbriae–mediated bacterial adhesion. Contrib Nephrol. 1984;39:252-272.
Svensson R, Larsson P, Lincoln K. Low-dose trimethoprim prophylaxis in long-term control of chronic recurrent urinary tract infection. Scand J Infect Dis. 1982;14:139-142.
Sweet R. Bacteriuria and pyelonephritis during pregnancy. Semin Perinatol. 1977;1:25-40.
Sweet R, Keane WF. Perinephric abscess in patients with polycystic kidney disease undergoing chronic hemodialysis. Nephron. 1979;23:237-240.
Talan DA, Stamm WE, Hooton TM, et al. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis pyelonephritis in women: a randomized trial. JAMA. 2000;283:1583-1590.
Tambyah PA, Halvorson KT, Maki DG. A prospective study of pathogenesis of catheter-associated urinary tract infections. Mayo Clin Proc. 1999;74:131-136.
Tambyah PA, Knasinski V, Maki DG. The direct costs of nosocomial catheter-associated urinary tract infection in the era of managed care. Infect Control Hosp Epidemiol. 2002;23:27-31.
Tambyah PA, Maki DG. Catheter-associated urinary tract infection is rarely symptomatic: a prospective study of 1,497 catheterized patients. Arch Intern Med. 2000;160:678-682.
Tapper H, Herwald H. Modulation of hemostatic mechanisms in bacterial infectious diseases. Blood. 2000;96:2329-2337.
Tartaglione TA, Johnson CR, Brust P, et al. Pharmacodynamic evaluation of ofloxacin and trimethoprim-sulfamethoxazole in vaginal fluid of women treated for acute cystitis. Antimicrob Agents Chemother. 1988;32:1640-1643.
Thankavel K, Madison B, Ikeda T, et al. Localization of a domain in the FimH adhesin of Escherichia coli type 1 fimbriae capable of receptor recognition and use of a domain-specific antibody to confer protection against experimental urinary tract infection. J Clin Invest. 1997;100:1123-1136.
Thiel G, Spuhler O. Catheter infection and so-called infectious (episomal) resistance. Schweiz Med Wochenschr. 1965;95:1155-1157. [in German]
Thomas E, Hillman BJ, Stanisic T. Urinary tract infection with atypical mycobacteria. J Urol. 1980;124:748-750.
Thorley JD, Jones SR, Sanford JP. Perinephric abscess. Medicine (Baltimore). 1974;53:441-451.
Timmons JW, Perlmutter AD. Renal abscess: a changing concept. J Urol. 1976;115:299-301.
Tissot E, Woronoff-Lemsi MC, Cornette C, et al. Cost-effectiveness of urinary dipsticks to screen asymptomatic catheter-associated urinary infections in an intensive care unit. Intensive Care Med. 2001;27:1842-1847.
Toivanen A, Kasan A, Sundquist H, et al. Effect of trimethoprim on the occurrence of drug-resistant coliform bacteria in the faecal flora. Chemotherapy. 1976;22:97-103.
Tolia BM, Iloreta A, Freed SZ, et al. Xanthogranulomatous pyelonephritis: detailed analysis of 29 cases and a brief discussion of atypical presentations. J Urol. 1981;126:437-442.
Tolia BM, Newman HR, Fruchtman B, et al. Xanthogranulomatous pyelonephritis: segmental or generalized disease. J Urol. 1980;124:122-124.
Tolkoff-Rubin NE, Wilson ME, Zuromskis P, et al. Single-dose amoxicillin therapy of acute uncomplicated urinary tract infections in women. Antimicrob Agents Chemother. 1984;25:626-629.
Tomashefski JFJr, Abramowsky CR. Candida-associated renal papillary necrosis. Am J Clin Pathol. 1981;75:190-194.
Trillo A, Lorentz WB, Whitley NO. Malakoplakia of kidney simulating renal neoplasm. Urology. 1977;10:472-477.
Turck M, Goffe B, Petersdorf RG. The urethral catheter and urinary tract infection. J Urol. 1962;88:834-837.
Turck M, Ronald AR, Petersdorf RG. Relapse and reinfection in chronic bacteriuria—the correlation between site of infection and pattern of recurrence in chronic bacteriuria. N Engl J Med. 1968;278:422-427.
Uehling DT, Hopkins WJ, James LJ, et al. Vaginal immunization of monkeys against urinary tract infection with a multi-strain vaccine. J Urol. 1994;151:214-216.
Uhlen P, Laestadius A, Jahnukainen T, et al. Alpha-haemolysin of uropathogenic E. coli induces Ca2+ oscillations in renal epithelial cells. Nature. 2000;405:694-697.
U.S. Census Bureau. 2003 American Community Survey Summary Tables, 2003.
Vaisanen V, Elo J, Tallgren LG, et al. Mannose-resistant haemagglutination and P antigen recognition are characteristic of Escherichia coli causing primary pyelonephritis. Lancet. 1981;2:1366-1369.
Vallorosi CJ, Putzi MJ, Wolf JSJr. Renal malacoplakia. Tech Urol. 1999;5:43-44.
Van Dorsten JP, Lenke RR, Schifrin BS. Pyelonephritis in pregnancy. The role of in-hospital management and nitrofurantoin suppression. J Reprod Med. 1987;32:895-900.
Van Kirk OC, Go RT, Wedel VJ. Sonographic features of xanthogranulomatous pyelonephritis. AJR Am J Roentgenol. 1980;134:1035-1039.
Vejlsgaard R. Studies on urinary infections in diabetics. IV. Significant bacteriuria in pregnancy in relation to age of onset, duration of diabetes, angiopathy and urological symptoms. Acta Med Scand. 1973;193:343-346.
Velasco M, Martinez JA, Moreno-Martinez A, et al. Blood cultures for women with uncomplicated acute pyelonephritis: are they necessary? Clin Infect Dis. 2003;37:1127-1130.
Venegas MF, Navas EL, Gaffney RA, et al. Binding of type 1-piliated Escherichia coli to vaginal mucus. Infect Immun. 1995;63:416-422.
Vidaeff AC, Yeomans ER, Ramin SM. Preganancy in women with renal disease. Part 1: general principles. Am J Perinatol. 2008;25:385-398.
von Hansemann D. Über Malakoplakie der Harnblase. Arch Pathol Anat. 1903;173:302.
Vordermark JS2nd, Modarelli RO, Buck AS. Torulopsis pyelonephritis associated with papillary necrosis: a case report. J Urol. 1980;123:96-97.
Vosti KL. Recurrent urinary tract infections. Prevention by prophylactic antibiotics after sexual intercourse. JAMA. 1975;231:934-940.
Vosti KL. Infections of the urinary tract in women: a prospective, longitudinal study of 235 women observed for 1–19 years. Medicine (Baltimore). 2002;81:369-387.
Vromen M, Ven Avd, Knols A, et al. Antimicrobial resistance patterns in urinary isolates from nursing home residents: fifteen years of data reviewed. J Antimicrob Chemother. 1999;44:113-116.
Waage A, Halstensen A, Espevik T. Association between tumour necrosis factor in serum and fatal outcome in patients with meningococcal disease. Lancet. 1987;1:355-357.
Wadsworth DE, McClennan BL, Stanley RJ. CT of the renal mass. Urol Radiol. 1982;4:85-94.
Waites KB, Canupp KC, DeVivo MJ. Epidemiology and risk factors for urinary tract infection following spinal cord injury. Arch Phys Med Rehabil. 1993;74:691-695.
Waltzer WC. The urinary tract in pregnancy. J Urol. 1981;125:271-276.
Wan YL, Lee TY, Bullard MJ, et al. Acute gas-producing bacterial renal infection: correlation between imaging findings and clinical outcome. Radiology. 1996;198:433-438.
Warren JW. The catheter and urinary tract infection. Med Clin North Am. 1991;75:481-493.
Warren JW. Catheter-associated urinary tract infections. Infect Dis Clin North Am. 1997;11:609-622.
Warren JW, Abrutyn E, Hebel JR, et al. Guidelines for antimicrobial treatment of uncomplicated acute bacterial cystitis and acute pyelonephritis in women. Infectious Diseases Society of America (IDSA). Clin Infect Dis. 1999;29:745-758.
Warren JW, Tenney JH, Hoopes JM, et al. A prospective microbiologic study of bacteriuria in patients with chronic indwelling urethral catheters. J Infect Dis. 1982;146:719-723.
Weld KJ, Dmochowski RR. Effect of bladder management on urological complications in spinal cord injured patients. J Urol. 2000;163:768-772.
West DA, Cummings JM, Longo WE, et al. Role of chronic catheterization in the development of bladder cancer in patients with spinal cord injury. Urology. 1999;53:292-297.
Weyrauch HM, Bassett JB. Ascending infection in an artificial urinary tract: an experimental study. Stanford Med Bull. 1951;9:25-29.
Wheat LJ. Infection and diabetes mellitus. Diabetes Care. 1980;3:187-197.
Wicks JD, Thornbury JR. Acute renal infections in adults. Radiol Clin North Am. 1979;17:245-260.
Wiedermann CJ, Kaneider NC. A meta-analysis of controlled trials of recombinant human activated protein C therapy in patients with sepsis. BMC Emerg Med. 2005;5:7.
Wigton RS, Hoellerich VL, Ornato JP, et al. Use of clinical findings in the diagnosis of urinary tract infection in women. Arch Intern Med. 1985;145:2222-2227.
Wilhelm M, Edson R. Antimicrobial agents in urinary tract infections. Mayo Clin Proc. 1987;62:1025-1031.
Williams J, Reeves D, Brumfitt W. The effects of bacteriuria in pregnancy on maternal health. In: Brumfitt W, Asscher A, editors. Urinary tract infections. London: Oxford University Press; 1973:103.
Williams R, Attia E, Wickiewicz T, et al. The effect of ciprofloxacin on tendon, paratenon, and capsular fibroblast metabolism. Am J Sports Med. 2000;28:364-369.
Winberg J, Bergstrom T, Lincoln K, et al. Treatment trials in urinary tract infection (UTI) with special reference to the effect of antimicrobials on the fecal and periurethral flora. Clin Nephrol. 1973;1:142-148.
Wolach MD, MacDermott JP, Stone AR, et al. Treatment and complications of Fournier’s gangrene. Br J Urol. 1989;64:310-314.
Wolf JSJr, Bennett CJ, Dmochowski RR, et al. Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol. 2008;179:1379-1390.
Wong ES, Fennell CL, Stamm WE. Urinary tract infection among women attending a clinic for sexually transmitted diseases. Sex Transm Dis. 1984;11:18-23.
Wong ES, McKevitt M, Running K, et al. Management of recurrent urinary tract infections with patient-administered single-dose therapy. Ann Intern Med. 1985;102:302-307.
Wright A, Walker R, Barrett D. The fluoroquinolones and their appropriate use in treatment of genitourinary tract infections. In: Ball T, Novicki D, editors. AUA update series. Houston: American Urologic Association, 1993.
Wu XR, Sun TT, Medina JJ. In vitro binding of type 1-fimbriated Escherichia coli to uroplakins Ia and Ib: relation to urinary tract infections. Proc Natl Acad Sci U S A. 1996;93:9630-9635.
Yamamoto S, Tsukamoto T, Terai A, et al. Genetic evidence supporting the fecal-perineal-urethral hypothesis in cystitis caused by Escherichia coli. J Urol. 1997;157:1127-1129.
Yazaki T, Ishikawa S, Ogawa Y, et al. Xanthogranulomatous pyelonephritis in childhood: case report and review of English and Japanese literature. J Urol. 1982;127:80-83.
Zacur HA, Mitch WE. Renal disease in pregnancy. Med Clin North Am. 1977;61:89-109.
Zhanel G, Hoban D, Harding G. The postantibiotic effect: a review of in vitro and in vivo data. Dicp. 1991;25:153-163.
Zhang D, Zhang G, Hayden MS, et al. A Toll-like receptor that prevents infection by uropathogenic bacteria. Science. 2004;303:1522-1526.
Zinner SH, Kass EH. Long-term (10 to 14 years) follow-up of bacteriuria of pregnancy. N Engl J Med. 1971;285:820-824.
Zornow DH, Landes RR, Morganstern SL, et al. Malacoplakia of the bladder: efficacy of bethanechol chloride therapy. J Urol. 1979;122:703-704.