Analgesics
The long-term, appropriate use of pain medications forms an integral part of the treatment of a chronic pain condition such as IC. Most patients can be helped markedly with medical pain management using pain medications commonly used for chronic neuropathic pain syndromes, including antidepressants, anticonvulsants, and opioids (Wesselmann et al, 1997). Many nonopioid analgesics including acetaminophen and the nonsteroidal anti-inflammatory drugs (NSAIDs) and even antispasmodic agents (Rummans, 1994) have a place in therapy along with agents designed to specifically treat the disorder itself.
Studies on the use of analgesics for BPS are sparse, and the majority of data is inferred from non-BPS types of pain and expert opinion. Health care professionals should ask about pain, and the patient’s self-report should be the primary source of assessment. Clinicians should assess pain with easily administered rating scales and should document the efficacy of pain relief at regular intervals after starting or changing treatment.
Unlike opioids, with increasing doses acetaminophen, aspirin, and the other NSAIDs all reach a ceiling for their maximum analgesic effect (Drugs for pain, 1998). Gabapentin, introduced in 1994 as an anticonvulsant, has found efficacy in neuropathic pain disorders including diabetic neuropathy (Backonja et al, 1998) and postherpetic neuralgia (Rowbotham et al, 1998). It demonstrates synergism with morphine in neuropathic pain (Gilron et al, 2005). It may give some benefit in chronic pelvic pain syndromes and BPS/IC (Sasaki et al, 2001). Pregabalin is also reported to be effective for neuropathic pain and the pain of fibromyalgia (Freynhagen et al, 2005; Arnold et al, 2008).
With the results of major surgery anything but certain, the use of long-term opioid therapy in the patient who has failed more conservative therapies also may be considered (Table 12–13). Opiates are seldom the first choice of analgesics in chronic pain states, but they should not be withheld if less powerful analgesics have failed (Portenoy et al, 1997; Bennett, 1999). This is a difficult decision that requires much thought and discussion between patient and urologist, and involvement of a pain specialist is indicated. A single practitioner has to take responsibility for pain treatment and write all prescriptions for pain medications (Brookoff, 1997). Opioids are effective for most forms of moderate and severe pain and have no ceiling effect other than that imposed by adverse effects. The common side effects include sedation, nausea, mild confusion, and pruritus. These are generally transient and easily managed. Respiratory depression is extremely rare if they are used as prescribed. Constipation is common, and a mild laxative is generally necessary. The major impediment to the proper use of these drugs when they are prescribed for long-term nonmalignant pain is the fear of addiction. Studies suggest the risk is low (Gourlay, 1994). The long-acting narcotic formulations that result in steady levels of drug over many hours are preferable.
Table 12–13 General Guidelines for the Use of Opioids in Chronic/Nonacute Urogenital Pain
Modified from Fall M, Baranowski A, Elneil S et al. Guidelines on chronic pelvic pain. In: European Association of Urology; 2008. p. 1–99. www.uroweb.org/professional-resources/guidelines/.
Chronic pain patients often receive inadequate doses of short-acting pain medications, which put them on cycles of short-term relief, anxiety, and pain. It leads to doctor shopping and to drug-seeking behavior confused by physicians with drug addiction. Although physical dependence to opioids will be unavoidable, physical addiction, a chronic disorder characterized by the compulsive use of a substance resulting in physical, psychological, or social harm to the user and the continued use despite that harm, is rare. Chronic opioid therapy can be considered in carefully selected patients. It is best administered in a pain clinic setting, requiring frequent reassessment by both patient and physician (Portenoy and Foley, 1986).
Intravesical and Intradetrusor Therapies
Assessments according to the Oxford System for intravesical therapy for BPS are shown in Table 12–14.
Table 12–14 Intravesical Therapy for BPS: Assessments According to Oxford System
| INTRAVESICAL AGENT | LEVEL OF EVIDENCE | GRADE OF RECOMMENDATION |
|---|---|---|
| DMSO | 2 | B |
| Heparin | 3 | C |
| Hyaluronic acid | 1 | D |
| Chondroitin sulfate | 4 | D |
| Pentosan polysulfate | 4 | D |
| Capsaicin/resiniferatoxin | 1 | −A (ineffective) |
| Bacillus Calmette-Guérin (BCG) | 1 | −A (ineffective |
| Oxybutynin | 4 | D |
| Lidocaine | 2 | C |
| Botulinum toxin | 4 | D |
From Hanno P, Lin AT, Nordling J, et al. Bladder pain syndrome. In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence. Paris: Health Publication Ltd.; 2009. p. 1459–518.
Silver Nitrate
Although the evidence base for treating BPS/IC using intravesical preparations is limited and the potential for meta-analysis reduced by variation in the outcome measures used (Dawson and Jamison, 2007), intravesical lavage with one of a variety of preparations has remained a mainstay of treatment in the therapeutic armamentarium of BPS. Perhaps the oldest of the intravesical therapies is silver nitrate. The use of silver nitrate has been attributed to Mercier (cited in Pool and Rives, 1944), who reported in 1855 that excellent results with bladder instillations had been obtained in patients suffering from symptoms compatible with IC. Dodson (1926) advocated the use of solutions of silver nitrate in increasing strengths as the treatment of choice for this condition. Pool and Rives (1944) reported on 74 patients with IC treated with intravesical silver nitrate. The treatment was carried out as follows:
A urethral catheter is inserted and the contents of the bladder are evacuated. The bladder is then irrigated with a saturated solution of boric acid. Then 30 to 60 mL of a 1 : 5000 solution of silver nitrate is instilled into the bladder and permitted to remain there for 3 or 4 minutes if it does not cause intolerable irritation. At the end of this period the solution is permitted to run out through the catheter, which is then withdrawn. The patient usually experiences some dysuria and vesical irritability for 2 or 3 hours. Treatments are repeated every other day. At subsequent treatments the concentration of silver nitrate in the solution is increased to 1 : 2500, 1 : 1000, 1 : 750, 1 : 500, 1 : 400, 1 : 200, and finally 1 : 100. If at any time the reaction is too severe, the concentration is increased more slowly (Pool and Rives, 1944).
Although the initial treatments are performed with the patient under general anesthesia, later treatments are given on an outpatient basis. Ureteral reflux would be a contraindication, and it goes without saying that bladder biopsy would be contraindicated just before instillation for fear of extravasation. Twenty-three years later, Pool (1967) wrote that he still considered this treatment regimen the most efficacious form of treatment. He reported excellent results in 70% of patients with a mean response of 7.6 months. Burford and Burford (1958) reported a 14% cure rate and 79% improved figure. DeJuana and Everett (1977) had a 50% response rate in 102 patients.
Although silver nitrate is rarely used in the current treatment of BPS, an animal study showing that intravesical administration of nanocrystalline silver (1%) decreased urine histamine, bladder TNF-α, and mast cell activation in an experimental inflammation model without any toxic effect may restimulate interest in silver compounds (Boucher et al, 2008).
Clorpactin
O’Connor (1955) reported the use of intravesical Clorpactin WCS 90. Clorpactin is a generic term for closely related, highly reactive chemical compositions having a modified derivative of hypochlorous acid in a buffered base. Its activity depends on the liberation of hypochlorous acid and its resulting oxidizing effects, wetting and penetrating properties, and detergency. Wishard treated 20 patients with 0.2% Clorpactin gently lavaged in the bladder for 3 to 5 minutes without anesthesia, of whom 14 reported subjective improvement (Wishard et al, 1957). Murnaghan and coworkers (1970) noted improvement in 14 of 17 patients, although 10 required further treatment during the average 2-year follow-up. Most commonly the treatments are given as described by Messing and Stamey (1978), using 0.4% solution administered at 10 cm H2O under anesthesia. Multiple instillations can be given, with a 1-month pause after the first 2 instillations to await a therapeutic response. The success rate of these researchers was 72%, with average 6-month duration of response. La Rock and Sant (1995) noted a 50% to 55% meaningful improvement rate occurring within 4 to 6 weeks of treatment. A case of ureteral fibrosis complicating the treatment prompted the recommendation that vesicoureteral reflux be considered a contraindication to the procedure (Messing and Freiha, 1979). Our method of Clorpactin delivery is as follows:
Reflux is excluded with a cystogram. Under anesthesia the bladder is distended for 2 minutes at 60 to 80 cm H2O and emptied. The perineum is shielded with a moistened towel. A solution of 0.4% freshly prepared Clorpactin (4 g in 1000 mL of sterile water) is instilled by gravity drainage (the Foley catheter held 10 cm above the level of the bladder) in 150- to 200-mL aliquots for a dwell time of 2 to 3 minutes and drained by gravity. This continues until the entire 1000-mL solution has been used. The bladder and introitus are then irrigated with normal saline, and the catheter is removed.
Dimethyl Sulfoxide
A mainstay of the treatment of BPS is the intravesical instillation of 50% DMSO (Sant, 1987). DMSO is a product of the wood pulp industry and a derivative of lignin. It has exceptional solvent properties and is freely miscible with water, lipids, and organic agents. Pharmacologic properties include membrane penetration, enhanced drug absorption, anti-inflammatory, analgesic, collagen dissolution, muscle relaxant, and mast cell histamine release. In-vitro effects on bladder function belie its positive effects in vivo (Freedman et al, 1989), where histamine release has not been demonstrated after treatment (Stout et al, 1995). It has been suggested that DMSO actually desensitizes nociceptive pathways in the lower urinary tract (Birder et al, 1997). Tests for DMSO for treatment of human illness began in the 1960s in the areas of musculoskeletal inflammation and the cutaneous manifestations of scleroderma.
Stewart and colleagues (1968) are credited for popularizing intravesical DMSO for BPS/IC. In the mid 1960s they applied it to the skin over the suprapubic area in a group of patients whose condition was refractory to conventional forms of therapy. Results were poor, but intravesical delivery of 50 mL of a 50% solution instilled for 15 minutes by catheter and repeated at intervals of 2 to 4 weeks showed positive effects in 6 of 8 patients lasting 2 to 12 months. The lack of side effects, other than a garlic-like odor on the breath, and of the need for inpatient administration were significant breakthroughs over previous treatments. Further reports by this group confirmed safety and efficacy (Stewart et al, 1971, 1972; Stewart and Shirley, 1976; Shirley et al, 1978) with symptom-free intervals of 1 to 3 months in 73% of patients. Ek and associates (1978) reported a 70% success rate but found most patients ultimately required re-treatment or further therapy with other modalities. Prospective series of Fowler (1981) and Barker and associates (1987) revealed symptomatic success rates of greater than 80%, although relapse was not uncommon. Fowler noted only minimal improvements in functional bladder capacity and attributed the beneficial effects of DMSO to a direct effect on the sensory nerves of the bladder. Perez-Marrero and associates (1988) compared DMSO with saline and showed a 93% objective improvement and 53% subjective improvement compared with 35% and 18%, respectively, for saline. Patients with bladder instability do not respond (Emerson and Feltis, 1986).
With its ease of administration (Biggers, 1986), low morbidity, and reasonable symptomatic results, DMSO certainly merits its place as a useful treatment for BPS/IC. In-vivo studies on rat bladder strips exposed to various concentrations of DMSO for 7 minutes showed absence of electrical field stimulation contraction at a 40% concentration and diminished compliance at 30% concentration (Melchior et al, 2003). Concentrations of 25% or less had negligible effects in this model. How it relates to use of DMSO in humans is unknown. A rare case of eosinophilic cystitis has been reported after DMSO instillation (Abramov et al, 2004).
Glycosaminoglycans
Exogenous GAGs have been shown to be effective in providing an epithelial permeability barrier in bladders in which the epithelium has been injured with protamine (Nickel et al, 1998). Heparin, which can mimic the activity of the bladder’s own mucopolysaccharide lining (Hanno et al, 1978), has anti-inflammatory effects as well as actions that inhibit fibroblast proliferation, angiogenesis, and smooth muscle cell proliferation. Because of its numerous effects the possibility that heparin could be used for therapeutic reasons other than the control of coagulation has been the subject of much inquiry and speculation (Lane and Adams, 1993). Weaver and associates (1963) first reported intravesical heparin for IC treatment. Given intravesically there is virtually no systemic absorption, even in an inflamed bladder (Caulfield et al, 1995). Although uncontrolled studies suggested some beneficial effect for subcutaneous administration (Lose et al, 1983, 1985), the obvious risks of anticoagulation and osteoporosis have prevented this form of administration from undergoing further trials and general usage. Ten thousand units can be administered intravesically in sterile water either alone or with DMSO at varying intervals, with good results being reported (Perez-Marrero et al, 1993; Parsons et al, 1994a). Kuo (2001) reported 50% or more improvement in the International Prostate Symptom Score in 29 of 40 women with IC treated with 25,000 units intravesically twice weekly for 3 months.
Parsons (2000) has used daily intravesical doses of 40,000 units of heparin in 20-mL sterile water administered by the patient daily and held for 30 to 60 minutes. “Reasonable improvement of symptoms” can be expected between 6 months and 2 years after starting therapy. Adding alkalinized lidocaine to the heparin instillation provides better pain relief (Parsons, 2005). These encouraging outcomes must be kept in perspective, given that they are unproven by any placebo-controlled trial. The addition of 8 mL of 2% lidocaine and 4 mL of 8.4% sodium bicarbonate may improve results (Welk and Teichman, 2008). In fact, a combination of 200 mg of lidocaine with 8.4% sodium bicarbonate (10 mL total solution) without heparin showed a 30% response rate 3 days after completion of daily intravesical administration for 5 days and was statistically superior to a placebo cocktail (Nickel et al, 2009b).
Another GAG analogue, pentosan polysulfate (PPS), administered intravesically at 300 mg twice weekly in 50 mL of normal saline, showed some modest benefit in a small trial (Bade et al, 1997a). A 41-patient trial comparing oral PPS with oral and intravesical administration showed that the 24% reduction in O’Leary-Sant scores with oral therapy alone rose to a 46% reduction in the group that also received intravesical PPS (Davis et al, 2008).
The nonsulfated GAG, hyaluronic acid, has also been used intravesically. Trials using 40 mg dissolved in 40 mL of normal saline weekly for 4 to 6 weeks and then monthly treatments thereafter have had response rates varying from 71% (Morales et al, 1996) to 30% (Porru et al, 1997). In the summer of 2003, Bioniche Life Science (Interstitial Cystitis Association, 2003), and in the spring of 2004 Seikagaku Corporation, reported double-blind, placebo-controlled, multicenter clinical studies of their hyaluronic acid preparations (40 mg or 200 mg/mL, respectively), and neither showed significant efficacy of sodium hyaluronate compared with placebo. These negative studies have not been published in peer-reviewed literature. Neither preparation has been approved for use for BPS/IC in the United States. An Austrian open-label study showed 13 of 27 patients with BPS and a positive potassium test responded to intravesical hyaluronic acid, 40 mg, given weekly for 10 weeks, although initial nonresponders at 5 weeks also were treated with intravesical PPS 200 mg thrice weekly for the remaining 5 weeks (Daha et al, 2008). The best results for hyaluronic acid come from Riedl and colleagues (2008), who studied 126 patients with a positive modified potassium test who could hold the solution for 2 hours, using 40 mg weekly for a minimum 10 weeks. Eight-four percent had significant improvement. Treatment-resistant cases have been managed with a combination of sequential bladder distention under anesthesia accompanied by a hyaluronic acid instillation every 1 to 3 months depending on response, with a 74% success rate in 23 patients (Ahmad et al, 2008). Although used in Europe and Canada, the efficacy of hyaluronic acid for BPS/IC remains unproven in controlled and blinded trials (Iavazzo et al, 2007).
Hurst (2003) has shown by immunohistochemistry a deficit of chondroitin sulfate from the luminal bladder surface in IC patients. Small uncontrolled studies using intravesical chondroitin sulfate have shown success rates of 33% (Steinhoff et al, 2002) to 50% (Sorensen, 2003). A multicenter, open-label study using 2% solution of sodium chondroitin sulfate weekly for 6 weeks and then monthly for 4 months had a 60% response rate with no safety issues (Nickel et al, 2009a). A large open-label experience using the device for all forms of “chronic cystitis” concluded that it was effective in improving urgency, voided volumes, and nocturia and well-tolerated when administered weekly for a maximum of eight instillations (Nordling and van Ophoven, 2008). The GAGs can be combined for instillation (Cervigni et al, 2008).
Other Intravesical Therapies
Doxorubicin (Khanna and Loose, 1990) and the mast cell stabilizer cromolyn sodium (Edwards et al, 1986; Kennelly and Konnak, 1995) have been tried in pilot trials with the promising results we come to expect in such studies. Follow-up studies are lacking, and these drugs have not become a part of the intravesical pharmacopeia.
The use of intravesical bacillus Calmette-Guérin (BCG) for IC was first reported by Zeidman and colleagues (1994). A subsequent randomized, prospective, double-blind, placebo controlled trial of 30 patients treated weekly for 6 weeks and followed for a mean of 8 months noted a 60% response rate compared with a 27% placebo response (Peters et al, 1997). Surprisingly, BCG was tolerated as well as placebo. Even more surprisingly, 8 of 9 BCG responders continued to have an excellent response in all parameters measured at 27 months of follow-up (Peters et al, 1998). It is unclear how BCG achieved this result, but immunologic and/or anti-inflammatory mechanisms have been postulated (Peters et al, 1999). A double-blind crossover Swedish study comparing DMSO to BCG failed to substantiate the efficacy of BCG (Peeker et al, 2000c).
A large multicenter randomized controlled trial by NIDDK comparing BCG with placebo found a 12% response rate for placebo compared with a 21% response for BCG. Placebo responders in the trial had the same durability of response (up to 68 weeks) as the BCG responders (Propert et al, 2008). In a follow-up open-label phase of the trial the response rate was 18% in both the group originally randomized to BCG and the group initially randomized to placebo, indicating a second course of therapy does not improve response rate (Propert et al, 2007). The small response rate in the randomized controlled trial failed to reach statistical significance at the P = .05 level, and this large study of 265 patients suggests that BCG has no place in the treatment of moderate to severe BPS/IC (Mayer et al, 2005). Although the BCG safety profile was considered acceptable in the NIDDK trial, adverse events were not uncommon and rare hypersensitivity reactions to intravesical BCG can occur (Parker et al, 2004). Although small, uncontrolled trials showing efficacy of BCG have been reported (Aghamir et al, 2007; El-Bahnasy et al, 2009), the NIDDK trial dampened enthusiasm for this treatment modality.
Efforts to bring new therapies directly to the bladder continue to be the focus of investigators. Oxybutynin has shown efficacy in preliminary studies when administered intravesically at doses of 10 mg dissolved in saline (Bade et al, 2000; Barbalias et al, 2000). Electromotive drug administration, the active transport of ionized drugs by the application of an electric current, using lidocaine and dexamethasone, has shown a 25% success rate up to 6 months after instillation (Rosamilia et al, 1997). A similar trial using repeated instillations noted success rates of 60% with a mean duration of 6.6 months (Riedl et al, 1997). Capsaicin, the main pungent ingredient in hot peppers of the genus Capsicum, is a specific neurotoxin that desensitizes C fiber afferent neurons. Resiniferatoxin (RTX), an ultrapotent analogue of capsaicin appears to have similar effects with less of the acute pain and irritation associated with capsaicin application. Both compounds have been tested intravesically for the relief of bladder instability and hyperreflexia (Chancellor and de Groat, 1999). Clinical trials for the use of these compounds in bladder pain and urgency/frequency could show this to be a new and viable treatment modality in the future, but current data on efficacy in BPS are lacking (Cruz et al, 1997; Lazzeri et al, 1996, 2000). A phase 2 safety and proof of concept multicenter, placebo-controlled trial conducted by ICOS Corporation (Bothell, WA, USA) found no significant efficacy of a single intravesical administration RTX compared with placebo, although no safety issues were identified (Payne et al, 2005). Studies using other concentrations and multiple administrations may be worthwhile (Peng and Kuo, 2007).
Key Points
Intravesical Therapies
Intradetrusor Therapies
The therapeutic value of botulinum toxin type A (Botox) stems partially from its ability to temporarily inhibit acetylcholine release and cause flaccid paralysis in a dose-related manner. It can correct focal dystonia when injected into a muscle. In recent years there has been increasing evidence that Botox might also have analgesic properties (Rajkumar and Conn, 2004). Initially this was thought to be due to relief of muscle spasm. However, botulinum has been shown to reduce peripheral sensitization by inhibiting the release of several neuronal signaling markers, including glutamate and substance P, and reducing c-FOS gene expression. It may affect the sensory feedback loop to the central nervous system by decreased input from the muscle tissue, possibly by inhibiting acetylcholine release from gamma motor neurons innervating intrafusal fibers of the muscle spindle (Rosales et al, 1996). It inhibits the release of sensory neurotransmitters from isolated bladder preparations in rat bladder models of both acute injury and chronic inflammation (Lucioni et al, 2008). Botox has been used effectively for years in different conditions with muscular hypercontractions. Intravesical Botox administration blocks the acetic acid–induced calcitonin gene–related peptide release from afferent nerve terminals in the bladder mucosal layer in rats (Chuang et al, 2004). In an animal model of bladder permeability barrier disruption, intravesical Botox minimized bladder irritability and restored afferent neural responses to baseline levels (Vemulakonda et al, 2005). These results support clinical trials of Botox for the treatment of BPS/IC and other types of visceral pain (Chancellor and Yoshimura, 2004).
A multi-institutional case series using Botox or Dysport intravesical injections in 13 patients with refractory BPS/IC reported improvement in 9 patients. Improvements in symptoms lasted a mean of 3.72 months (mean, 1 to 8 months). No systemic complications were observed, although 2 patients had a diminished flow with some need to strain to void (Smith et al, 2004). Rackley and colleagues (2005) at the Cleveland Clinic reported no change in objective or subjective outcome measures in a series of 10 BPS/IC patients in whom the trigone was spared in the injection technique. A 1-year follow-up in 15 patients treated with 200 units Botox in 20 mL of normal saline showed that the success rate fell from 86.6% at 3 months to 26.6% at 5 months and was 0 at 12 months (Giannantoni et al, 2008). Bladder biopsy specimens 2 weeks after Botox intradetrusor injection show nerve growth factor production levels fall to those of controls in patients who respond (Liu et al, 2009). It is hypothesized that treatment-refractory patients may have developed antibodies after initial botulinum injection (Schulte-Baukloh, 2008). At this time Botox can be recommended for BPS/IC use only in the context of carefully controlled clinical trials (Cruz and Dinis, 2007; Del Popolo, 2008; Apostolidis et al, 2009).
Submucosal injection of 10 mL of 40 mg/mL triamcinolone acetonide injected in 0.5-mL aliquots was used for the treatment of Hunner lesions in 30 patients (Cox et al, 2009). Seventy percent of patients were very much improved, and duration of improvement was estimated to be 7 to 12 months.
Neuromodulation
Because it is a chronic pain syndrome it is reasonable to consider therapeutic options that directly interface with the nervous system in the treatment of PBS/IC. This approach is further supported by the association of pelvic floor dysfunction with pelvic pain syndromes (Zermann et al, 1999).
Pain diversion by transcutaneous electrical nerve stimulation (TENS) is routine in a variety of painful conditions (Fall, 1987). Fall and colleagues (1980) were the first to use electrical stimulation in IC, reporting on 14 women treated successfully with long-term intravaginal or TENS. Subsequently McGuire and coworkers (1983) noted improvement in 5 of 6 patients treated with electrical stimulation.
The primary intention in applying peripheral electrical nerve stimulation in IC is to relieve pain by stimulating myelinated afferents in order to activate segmental inhibitory circuits. As a secondary effect, urinary frequency may also be reduced. In the most complete review of the subject to date (Fall and Lindstrom, 1994) 33 patients with ulcerative IC and 27 patients with nonulcerative IC were treated by means of suprapubic TENS. Electrodes were positioned 10 to 15 cm apart immediately above the pubic symphysis. High- or low-frequency (2-50 Hz) TENS was employed. If there was no effect with high frequency after 1 month, low frequency was used. Thirty to 120 minutes of TENS was prescribed daily. Pain improved more than frequency. Good results or remission were described in 26% of nonulcer patients and in a surprising 54% of patients with ulcerative disease. The authors caution that the experience is based on open studies, relatively few patients, and the knowledge of a significant placebo effect with peripheral pain stimulation.
Acupuncture has been used to treat frequency, urgency, and dysuria (Chang, 1988). Twenty-two of 26 patients treated at the Sp. 6 point had clinically symptomatic improvement. A study looking at both acupuncture and TENS in IC showed limited effects of both modalities (Geirsson et al, 1993). Lumbar epidural blockade is the subject of a positive recent case report (Pelaez et al, 2004) but in an earlier series resulted in only short-term (mean 15 days) pain relief in IC (Irwin et al, 1993). Posterior tibial nerve stimulation was successful in 60% of 37 patients with symptoms of bladder overactivity in an uncontrolled Dutch study (van Balken et al, 2001). An Australian double-blind placebo controlled study of transdermal posterior tibial nerve laser therapy showed no benefit in 56 patients when comparing active to placebo arms, but the placebo effect was remarkably strong, indicating the importance of such trials when evaluating invasive therapies (O’Reilly et al, 2004). A Chinese study of posterior tibial nerve stimulation twice weekly for 5 weeks in BPS/IC patients failed to show improvement in pain scores, and none of 18 patients thought the treatment had a significant effect (Zhao et al, 2008).
Direct sacral nerve stimulation has been explored in the treatment of IC and urgency/frequency and is referred to as neuromodulation, a technique whose urologic potential was developed through the basic and clinical research of Tanagho and Schmidt (Schmidt, 1993; Fandel and Tanagho, 2005). They and others have observed that patients who do best with this treatment modality are those who have identifiable pain and dysfunction in the pelvic muscles (Everaert et al, 2001; Siegel et al, 2001; Aboseif et al, 2002). Those patients reporting pelvic pain in the absence of demonstrable pelvic floor dysfunction and levator tenderness did poorly (Schmidt, 2001). As initially practiced, trial stimulation was performed with a percutaneous temporary electrode for a 3- to 4-day temporary stimulation period to access efficacy. The S3 nerve is most frequently used. A wire electrode is inserted into the foramen and connected to an external pulse generator (Medtronic Inc., Minneapolis, MN, USA). If the trial is successful, the patient would be considered for implantation of a permanent neural prosthesis. More recently, a staged procedure has supplanted the traditional percutaneous approach, because the response to stimulation can be better assessed with more accurate lead placement and stability than through the more hit-or-miss percutaneous lead placement (Peters et al, 2003). Peters’ test to implant rate increased from 52% to 94%. Other reports have noted a test to implant rate in the percutaneous technique from 76% in 33 PBS/IC patients (Whitmore et al, 2003) to 40% in 211 patients with refractory urge incontinence, urgency-frequency syndrome, and urinary retention (Scheepens et al, 2002b).
Neuromodulation has been shown to be effective in treating refractory urinary urge incontinence (Schmidt et al, 1999; Spinelli et al, 2001). Studies on therapeutic potential in BPS/IC followed (van Kerrebroeck, 1999). The University of Maryland group described decrease in antiproliferative activity and normalization of HB-EGF levels in patients with successful test stimulation (Chai et al, 2000a). Peters and coworkers (2003) reported success in two thirds of BPS/IC patients with sacral nerve stimulation; Global Response Assessment as determined by the patient correlated with objective findings (Peters et al, 2008). In another study (Comiter, 2003) success was noted in 17 of 25 patients with test stimulation and they went on to permanent implantation of the Interstim device (Medtronics, St. Paul, MN). Thirteen of 15 who underwent staged implantation were permanently implanted versus 4 of 10 undergoing percutaneous test stimulation. With a mean follow-up of 14 months, in 16 of 17 patients the treatment was judged successful, giving an intent-to-treat success rate of 64%. Although sacral neuromodulation can decrease narcotic requirements significantly in refractory BPS/IC, the majority of patients taking chronic narcotics for pain will likely continue to use them for pain relief even after implantation (Peters and Konstandt, 2004). One center reported a long-term improvement rate of 45% for the urgency/frequency indication (Elhilali et al, 2005).
Unilateral stimulation should be performed before bilateral sacral stimulation is considered (Oerlemans and van Kerrebroeck, 2008). A bilateral test stimulation could be indicated when a unilateral test fails (Steinberg et al, 2007). The only prospective randomized crossover trial to compare the unilateral with bilateral sacral nerve stimulation found no significant differences comparing the results (Scheepens et al, 2002a). The presence of pain is a predictor of adverse events (White et al, 2009); and although sacral neuromodulation is effective in 56% of patients with urgency/frequency, when pain is the major complaint then caution is indicated. Surgical revision rates are 7% to 18% (van Kerrebroeck et al, 2007). When used for BPS symptoms, frequent reprogramming is often required (Maxwell et al, 2008).
Surgical Therapy
Hydrodistention
Hydrodistention of the bladder under anesthesia, while technically a surgical treatment, is often the first therapeutic modality employed, often as a part of the diagnostic evaluation. Because there have been no standard methods of distention (Turner and Stewart, 2005), results vary markedly. Frontz (1922) first suggested hydraulic overdistention of the bladder for IC, and Bumpus (1930) reported the first series 8 years later. Simple bladder filling at cystoscopy will give relief to some patients (Hald et al, 1986); others have reported an office-based procedure with intravesical lidocaine anesthesia using electromotive drug administration (Rose et al, 2005), whereas Dunn and associates (1977) reported on 25 patients whose bladders were distended under anesthesia to the level of the systolic blood pressure for up to 3 hours. Sixteen of the patients were symptom free with a mean follow-up of 14 months; 2 patients suffered bladder rupture. The bladder in IC patients can be very thin, and the possibility of perforation or rupture must always be kept in mind and discussed with the patient (Badenoch, 1971; Hamer et al, 1992). Prolonged distention probably has little or no benefit over a short-term distention measured in minutes (Taub and Stein, 1994; McCahy and Styles, 1995). Using epidural anesthesia and a balloon distention technique to the mean arterial pressure for 3 hours continuously, Glemain and colleagues (2002) reported good but transient efficacy in patients with a bladder capacity of greater than 150 mL on predistention cystometry. In their prospective series of 30 patients, 18 had maintained a therapeutic response at 6 months and 13 at 1 year of follow-up. Moderate hematuria was almost universal, worsening of symptoms occurred in 5% of patients, and low back and hypogastric pain were common sequelae. There was one bladder rupture, one episode of sepsis, and one episode of prolonged retention.
Our method is to perform an initial cystoscopic examination (which is generally unremarkable), obtain urine for cytology, and distend the bladder for 1 to 2 minutes at a pressure of 80 cm H2O. The bladder is emptied and then refilled to look for glomerulations or ulceration. A therapeutic hydraulic distention follows for another 8 minutes. Biopsy, if indicated, is performed after the second distention. Therapeutic responses in patients with a bladder capacity under anesthesia of less than 600 mL showed 26% with an excellent and 29% with a fair result compared with 12% excellent and 43% with a fair result in patients with larger bladder capacities (Hanno and Wein, 1991). Most favorable responses were extremely brief, however, with the exceptional patient noting improvement for 6 months and thus being a candidate for repeat therapeutic distention.
Acute hydrodistention does not seem to result in any long-term bladder dysfunction (Kang et al, 1992; Lasanen et al, 1992). Any efficacy is probably related to damage to mucosal afferent nerve endings (Dunn et al, 1977). It has no benefits in patients with detrusor hyperreflexia or instability (Taub and Stein, 1994; McCahy and Styles, 1995). Over half of men with prostate pain and without bacteriuria may have glomerulations. Symptoms in this group have been reported to improve with hydrodistention (Berger et al, 1998). While many patients with IC have sensory urgency at awake capacities of less than 100 mL, hydrodistention under anesthesia seems to allow for “staging” of the disease, giving the clinician some idea of the capacity he or she has to work with conservative therapies. A capacity under anesthesia of under 200 mL would not bode well for the likelihood of success of medical therapy. Fortunately these cases are relatively rare.
Surgical Considerations
Please see the Expert Consult website![]() for more discussion on this topic.
for more discussion on this topic.
Major extirpative and/or reconstructive surgical therapy for BPS is an option after all trials of conservative treatment have failed; a point that cannot be overemphasized. BPS/IC, although a cause of significant morbidity, is a nonmalignant process with a temporary spontaneous remission rate of up to 50% (Held et al, 1990) that does not directly result in mortality. Deaths are either self-inflicted or the complications of therapy. Nowhere does the caveat “primum non nocere” bear more relevance; the treatment must be no worse than the disease process (Siegel et al, 1990). Surgery should be reserved for the motivated and well-informed patient who falls into the category of extremely severe, unresponsive disease, a group that comprises less than 10% of patients (Irwin and Galloway, 1994; Parsons, 2000).
Historical Procedures
Many surgical approaches have been employed for IC, and it is worth mentioning a few for historical perspective alone. Sympathectomy and intraspinal alcohol injections have been used to treat pelvic pain (Greenhill, 1947). Differential sacral neurotomy was reported in 3 patients with good results (Meirowsky, 1969) but like most de-innervation procedures never gained popularity because of subsequent poor results. Transvesical infiltration of the pelvic plexuses with phenol failed in 5 of 5 patients with IC (Blackford et al, 1984). With a significant complication rate of 17% (McInerney et al, 1991) it is rarely if ever currently used for sensory urgency disorders or detrusor hyperreflexia. There are several reports on cystolysis going back to Richer in 1929 (Bourque, 1951). Worth (1980) and Worth and Turner-Warwick (1973) reported some short-term benefit, but unpredictable long-term results. Freiha and Stamey (1979) used it in 6 IC patients with good results in 4. Albers and Geyer (1988) reported long-term follow-up in 11 IC patients and had success in only 1. Denervation procedures have a notoriously high late-failure rate, and the procedure is not justified for BPS/IC (Walsh, 1985; Stone 1991). In fact, Rogers (2003) has concluded that there exist no convincing clinical studies to recommend surgical procedures to interrupt visceral nerve pathways in women suffering with any type of chronic pelvic pain.
Surgery of Hunner Lesion
Transurethral resection of a Hunner lesion, as initially reported by Kerr (1971), can provide symptomatic relief. Fall (1985) resected ulcerated lesions in 30 patients, resulting in initial disappearance of pain in all and a decrease in urinary frequency in 21. Similar results have been attained with the neodymium-yttrium-aluminum-garnet (YAG) laser (Shanberg et al, 1985; Shanberg, 1989; Rofeim et al, 2001). Extreme caution is critical if using a laser in a BPS/IC bladder, because forward scatter through these thin bladders with resulting bowel injury is an ever-present danger. There would seem to be no justification in the literature for using the laser to treat areas of glomerulation or in the nonulcerative form of the disease (Shanberg and Malloy, 1997).
Major Surgical Procedures
Supratrigonal cystectomy and the formation of an enterovesical anastomosis with bowel segments (substitution cystoplasty) has been a popular surgical procedure for intractable IC. The diseased bladder is resected in its entirety, sparing only a 1-cm cuff around the trigone to which the bowel segment is anastomosed (Worth and Turner-Warwick 1972; Irwin and Galloway, 1994). Although it is not always clear in the literature how much bladder has been resected, the results reported using these procedures for IC have been mixed at best. Badenoch (1971) operated on 9 patients, with 4 becoming much worse and 3 ultimately undergoing urinary diversion. Flood and colleagues (1995) reviewed 122 augmentation procedures, 21 of which were done for IC. Patients with IC had the poorest results of any group, with only 10 having an “excellent” outcome. Wallack and colleagues (1975) reported two successes; Seddon and associates (1977) had success in 7 of 9 patients; and Freiha and coworkers (1980) ended up performing formal urinary diversion in 2 of 6 patients treated with augmentation cecocystoplasty. Weiss and associates (1984) had success in 3 of 7 patients treated with sigmoidocystoplasty, and Lunghi and colleagues (1984) had no excellent results in 2 patients with IC. Webster and Maggio (1989) reviewed their data in 19 patients and concluded that only patients with bladder capacities under anesthesia less than 350 mL should undergo substitution cystoplasty. Hughes and coworkers (1995) lowered the threshold to less than 250 mL.
More recent series on subtotal cystectomy plus augmentation have been somewhat more positive (Costello et al, 2000; Chesa et al, 2001). Peeker and associates (1998) had good results in all 10 patients with ulcerative IC but poor results in the 3 patients operated on with nonulcerative disease. They no longer perform the procedure in the latter group. Linn and coworkers (1998) had success in 20 of 23 patients (only 2 with ulcerative IC) treated with subtotal cystectomy and orthotopic bladder substitution with an ileocecal pouch. They recommend a supratrigonal cystectomy. In a Spanish series success was reported in 13 of 17 procedures with a mean follow-up of 94 months (Rodriguez Villamil et al, 1999). The University of Alabama group reported long-term success in 1 of 4 patients with orthotopic neobladders and 1 of 3 with augmentation cystoplasty (Lloyd, 1999). A German report on substitution cystoplasty sparing the trigone was quite enthusiastic, detailing a 78% pain-free rate in 18 patients treated with ileocecal augmentation (10 patients) or ileal substitution (8 patients) at a mean follow-up of 57 months (van Ophoven et al, 2002). Two patients failed to get any pain relief, and 4 required either long-term intermittent catheterization or suprapubic drainage to empty the neobladder.
Not all patients empty the bladder spontaneously after substitution cystoplasty. Although the need for clean intermittent catheterization would not obviate a successful outcome in the patient treated for bladder contraction from tuberculous cystitis, it can be a painful disaster in the IC patient. Nurse and colleagues (1991) have gone one step farther, recommending trigone biopsy before substitution cystoplasty. Diversion and/or total cystourethrectomy is recommended if the trigone is “affected” by IC. It is not clear how this is determined histologically, because IC has no pathognomonic findings by histology and generally is not a localized process. Nielsen and coworkers (1990) described 8 women treated with substitution cystoplasty. The treatment failed in 6 patients, and the results of postoperative biopsies from the trigone showed no difference in the amount of fibrosis, degree of degenerative changes in the muscle, and mast cell density between the 2 cured patients and the others.
There has been a controversy over whether the IC process can occur in a transposed bowel patch (McGuire et al, 1973; Kisman et al, 1991; Singh and Thomas, 1996) or even in the ureter (Smith and Christmas, 1996). If so, not only would this be a relative contraindication to the procedure but it would also provide support for the view that a substance in the urine might be involved in pathogenesis. There is, however, evidence that inflammation and fibrosis are the usual reactions of bowel to exposure to urine and, therefore, pathologic findings alone would not be conclusive of spread of IC in those patients (MacDermott et al, 1990).
Augmentation cystoplasty has many potential complications from the rare incidence of bladder neoplasm (Golomb et al, 1989) to the more common complication of upper tract obstruction (Cheng and Whitfield, 1990). In the best of hands complications can involve almost 50% of patients, requiring surgical intervention in 25% (Khoury et al, 1992; Bunyaratavej et al, 1993). Although problems are more common in patients operated on for disorders other than IC, the risk-benefit ratio of substitution cystoplasty seems to have discouraged its use in the past several years.
Urinary diversion with or without cystourethrectomy is the ultimate surgical answer to the dilemma of IC, akin to cutting the “gordian knot.” If diversion alone is chosen, one must keep in mind potential problems that can befall the remaining bladder, including pyocystitis, hemorrhage, severe pain, and unremitting feelings of incomplete emptying and spasm (Eigner and Freiha, 1990; Adeyoju et al, 1996). Bladder carcinoma has also been reported after urinary diversion but is not specifically associated with BPS (Hanno and Tomaszewski, 1982). Consideration of cystourethrectomy is indicated only in patients who are miserable and have not only failed all other therapies but have demonstrated chronicity such that remission is considered extremely unlikely. Fortunately few patients fall into this category. Theoretically, conduit diversion seems to be reasonable if one is concerned about disease occurring in any continent storage type of reconstruction. The extended simple cystectomy performed for intractable IC may lend itself to anterior enterocele formation from weakening of the anterior vaginal wall, and prevention of this entity is warranted at the time of cystectomy (Anderson et al, 1998).
Bejany and Politano (1995) reported excellent results in 5 patients treated with total bladder replacement and recommend neobladder reconstruction. Keselman and coworkers (1995) had two failures in 11 patients treated with continent diversion and attributed this to surgical complications. A Finnish group noted failure in 2 of 4 patients treated with cystectomy and conduit diversion because of persistent pain (Lilius et al, 1973). Baskin and Tanagho (1992) also cautioned about persistence of pelvic pain after cystectomy and continent diversion, discussing 3 such patients. A similar report followed (Irwin and Galloway, 1992). Webster and coworkers (1992) had 10 failures in 14 patients treated with urinary diversion and cystectourethrectomy. Ten patients had persistent pelvic pain, and 4 of them also complained of pouch pain. Only 2 patients had symptom resolution. An English study of 27 patients who underwent cystectomy and bladder replacement with a Kock pouch noted successful treatment of pain in all patients, but follow-up was limited (Christmas et al, 1996a). Parsons suggests that pouch pain will occur in 40% to 50% of patients within 6 to 36 months of surgery (Parsons 2000).
Attempts have been made to improve results by limiting the operation to those without detrusor mastocytosis (Trinka et al, 1993) and those without “neuropathic pelvic pain” (Lotenfoe et al, 1995). Based on the experience of the past decades it is unclear if these efforts will prove any more successful. It would seem that risks of failure peculiar to IC include both the development of pain over time in any continent storage mechanism that is constructed and the risk of phantom pain in the pelvis that persists despite the fact that the stimulus that initially activated the nociceptive neurons (diseased bladder) has been removed (Cross, 1994). Brookoff (1997) has proposed trying a differential spinal anesthetic block before considering cystectomy. If the patient continues to perceive bladder pain after a spinal anesthetic at the T10 level, it can be taken as an indicator that the pain signal is being generated at a higher level in the spinal cord and that surgery on the bladder will not result in pain relief. Some patients with intractable urinary frequency will opt for simple conduit urinary diversion alone, believing that their quality of life will be improved independent of the pain piece of the puzzle. Despite all of the problems, many patients will do well after major surgery and quality of life can measurably improve (Rupp et al, 2000). In the event of neobladder pain after subtotal cystectomy and enterocystoplasty or continent diversion, it appears safe to retubularize a previously used bowel segment to form a urinary conduit for a straightforward urinary diversion without significant risk of conduit pain (Elzawahri et al, 2004).
The Gothenberg experience was recently reviewed, looking at results in 47 patients subjected to reconstructive/extirpative surgery (Rossberger et al, 2007). This included 23 substitution cystoplasties, 12 conduit diversions, and 10 Kock pouches. Twenty-eight of 34 patients with classic Hunner lesions had complete symptom resolution from the initial surgical procedure. Four of the remaining 6 required urinary diversion, cystectomy, or ulcer resection in a trigonal remnant but ultimately did well. Only 3 of 13 patients with non-Hunner disease had successful symptom resolution after reconstructive surgery, 2 of whom required conduit diversion. Peeker’s group concluded that only patients with Hunner lesions that were refractory to standard therapy could be expected to do well after major surgery.
A Thai experience using cystectomy and ileal neobladder in women who failed conservative therapy reported good results in all 35 patients treated (Kochakarn et al, 2007). Spontaneous voiding with minimal residual urine was found in 33 cases, and the remaining 2 cases had spontaneous voiding with residual urine requiring clean intermittent catheterization.
Forty years ago Pool (1967) recognized that “surgical treatment has not been the boon many had hoped it would be. … Diversion of the urine is not the entire answer to the situation. Removal of the lesion in the bladder has been of no benefit. Likewise, removal of almost the entire mobile portion of the bladder proved to be a failure.” Blaivas and associates (2005) and colleagues described results of augmentation enterocystoplasty and continent diversion in 76 consecutive patients with benign disease with a mean 9-year follow-up. All 7 patients with the diagnosis of IC were classified as “failures,” whereas 67 of the remaining 69 patients were cured or improved. When one of the deans of major urologic reconstruction writes, “I find it very difficult to justify such extensive surgery (continent diversion, cystourethrectomy) with such limited results and for these reasons have not been involved in surgery for IC over the past 3 years” (Webster, 1993), it is obvious that one should think carefully and proceed with surgery only after a complete discussion with a very motivated and well-informed patient. Recent reports seem to be more sanguine with regard to these procedures.
Key Points
Surgical Therapy
Assessing Treatment Results
The diversity of BPS/IC therapies underscores the lack of understanding about the treatment of this syndrome (Rovner et al, 2000). It has been not only a difficult condition to diagnose but also a difficult condition for which to assess therapeutic impact. There is a 50% incidence of temporary remission unrelated to therapy, with a mean duration of 8 months (Held et al, 1990). A somewhat surprising finding from the Interstitial Cystitis Database was that although there was initial improvement in symptoms partially due to regression to the mean (Sech et al, 1998) and the intervention effect there was no evidence of a long-term change in average symptom severity over the 4-year course of follow-up (Propert et al, 2000). In a chronic, devastating condition with primarily subjective symptomatology, no known cause, and no cure, patients are desperate and often seem to respond to any new therapy (Fig. 12–12). They are often victims of unorthodox health care providers with untested forms of therapy, some medical, some homeopathic, and some even surgical.
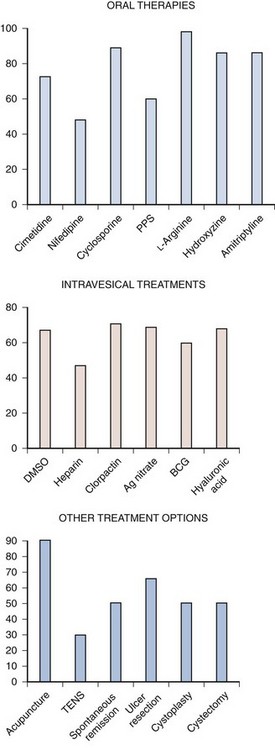
Figure 12–12 Selected reported treatment outcomes in uncontrolled studies in the bladder pain syndrome/interstitial cystitis literature: percentage of patients initially improved. Ag nitrate, silver nitrate; BCG, bacillus Calmette-Guérin; DMSO, dimethyl sulfoxide; PPS, sodium pentosan polysulfate; TENS, transcutaneous electrical nerve stimulation.
The Placebo Conundrum
When possible, the results of randomized controlled studies should be used for decision making. Placebo, double-blind studies are optimal in this disorder for which there is no generally effective standard therapy.
Placebo effects influence patient outcomes after any treatment which the clinician and patients believe is effective, including surgery. Placebo effects plus disease natural history and regression to the mean can result in high rates of good outcomes, which may be misattributed to specific treatment effects (Gillespie et al, 1991; Gillespie, 1994; Turner et al, 1994; Propert et al, 2000). Unfortunately, too few BPS treatments have been subjected to a placebo-controlled trial. This is not to say that what seems effective is not, but rather that a high index of skepticism is healthy, even in treatments tested in controlled trials (Schulz et al, 1995).
Although in many diseases an argument can be made against using a true placebo control as opposed to an orthodox treatment of approved or accepted value (Rothman and Michels, 1994), a good case for true placebo comparison can readily be made for BPS. The vagaries of the natural history, the general lack of progression of symptom severity over time, and the fact that it is not life threatening mean that there is little to lose and much to gain by subjecting new treatments to the vigorous scrutiny of placebo control. Many patients who volunteer for such trials have already run the gamut of accepted (although generally unproved) therapies. It has long been recognized in protocols that use subjective criteria for assessment that “improvement” may be expected in up to 35% of placebo-treated patients (Benson and Epstein, 1976). Because the spontaneous remission rate (although temporary) for BPS is 11% (Oravisto and Alfthan, 1976) to 50% (Held et al, 1990), combined with the placebo improvement it can be difficult to prove efficacy.
Even in placebo-controlled trials it is reasonable to surmise that some degree of unblinding may occur as a result of somatic or psychological side effects of the active arm, impairing the validity of the trial results and giving the active arm a slight edge over placebo (DuBeau et al, 2005; Rees et al, 2005). Failure to recognize unblinding can easily bias results of a study and has not been routinely measured in clinical trials (Desbiens, 2002). When occurring late in a study after one would expect onset of a therapeutic effect, unblinding could be the result of side effect profile or drug efficacy. Early in the trial it reflects poor placebo or study design. The degree of blinding needs to be ascertained throughout the trial. This is of specific concern in BPS and any disorder where primary outcomes may be subject to patient-specific psychological and physiologic factors.
The ethics and necessity of placebo-controlled trials have been questioned, especially in situations in which an effective treatment exists and also when delay in treatment has been shown to result in disease progression (Streiner, 1999; Anderson, 2006; Polman et al, 2008). However, there are methodologic concerns with equivalence and noninferiority active agent comparison trials (Streiner, 2007). These include an inability to determine if the treatments are equally good or equally bad, and the possibility that successive noninferiority trials can lead to a gradual decrease in treatment efficacy. Although the use of placebo-controlled trials raises ethical concerns when proven effective treatment exists for the condition under investigation, they are ethically justified, provided that stringent criteria for protecting research subjects are satisfied (Miller et al, 2004).
The value of placebo-controlled trials is aptly illustrated by the recent decisions by pharmaceutical manufacturers not to pursue FDA approval in the United States for seemingly promising intravesical therapies for BPS/IC (Morales et al, 1996; Chancellor and de Groat, 1999) after placebo-controlled trials failed to establish efficacy. These include low concentration hyaluronic acid (Bioniche, Canada), high concentration hyaluronic acid (SKK, Tokyo), and resiniferatoxin (ICOS, Bothell, WA, USA). Nalmefene, an initially promising oral therapy in the 1990s (Stone, 1994), also failed phase 3 trials (IVAX, Miami). Placebo trials are impractical in surgery and it can be difficult to evaluate surgical reports. The many older medications currently used off label might not meet success if tested in the stringent manner in which new molecular entities are tested. The expense of testing therapies currently used off label often requires dependence on the largesse of government agencies such as the NIH (Propert et al, 2002; Sant et al, 2003; Mayer et al, 2005).
Finally, when considering objective changes, the concept of statistical versus clinical significance is paramount. Investigators should, but rarely do, point out differences between statistical improvement and what they consider to be clinically significant improvement (Wein and Broderick, 1994). As Gertrude Stein reportedly stated, “A difference, to be a difference, must make a difference.” An increase in bladder capacity of 30 mL may be statistically significant but clinically irrelevant. Number needed to treat and number needed to harm data (McQuay, 2003) may be particularly important in BPS/IC and typically have not been included in efficacy analysis.
Clinical Symptom Scales
There are three published BPS/IC symptom questionnaires: the University of Wisconsin IC Scale, the O’Leary-Sant IC Symptom Index and IC Problem Index, and the Pelvic Pain and Urgency/Frequency (PUF) Scale.
The University of Wisconsin IC Scale includes 7 PBS/IC symptom items (Table 12–15 ![]() ). It has not been validated for identification or diagnosis of BPS/IC. It captures severity of symptom expression (Keller et al, 1994; Goin et al, 1998). BPS/IC patients do not appear to indiscriminately report higher scores than controls for different somatic and general complaints (Porru et al, 2005). Unlike the other two instruments it addresses some quality-of-life issues, and this is an advantage when such issues are subject of investigation. Its most attractive aspects are its clinically apparent face validity and its ease of implementation.
). It has not been validated for identification or diagnosis of BPS/IC. It captures severity of symptom expression (Keller et al, 1994; Goin et al, 1998). BPS/IC patients do not appear to indiscriminately report higher scores than controls for different somatic and general complaints (Porru et al, 2005). Unlike the other two instruments it addresses some quality-of-life issues, and this is an advantage when such issues are subject of investigation. Its most attractive aspects are its clinically apparent face validity and its ease of implementation.
Table 12–15 University of Wisconsin Symptom Instrument
| SYMPTOM | SCORE 1-6 (0 = NOT AT ALL) (6 = A LOT) |
|---|---|
| 1. Bladder discomfort | |
| 2. Bladder pain | |
| 3. Other pelvic discomfort | |
| 4. Headache | |
| 5. Backache | |
| 6. Dizziness | |
| 7. Feelings of suffocation | |
| 8. Chest pain | |
| 9. Ringing in ears | |
| 10. Getting up at night to go to the bathroom | |
| 11. Aches in joints | |
| 12. Swollen ankles | |
| 13. Nasal congestion | |
| 14. Flu | |
| 15. Abdominal cramps | |
| 16. Numbness or tingling in fingers or toes | |
| 17. Nausea | |
| 18. Going to the bathroom frequently during the day | |
| 19. Blind spots or blurred vision | |
| 20. Heart pounding | |
| 21. Difficulty sleeping because of bladder symptoms | |
| 22. Sore throat | |
| 23. Urgency to urinate | |
| 24. Coughing | |
| 25. Burning sensation in bladder |
From Sirinian E, Azevedo K, Payne CK. Correlation between 2 interstitial cystitis symptom instruments. J Urol 2005;173:835–40.
The O’Leary-Sant indices (Table 12–16 ![]() ) are a validated questionnaire that was originally developed by focus groups, subjected to test-retest reliability analysis, and validated by administration to IC patients and asymptomatic controls (O’Leary et al, 1997; Lubeck et al, 2001). The questionnaire centers on 3 questions related to urgency/frequency and 1 on bladder-associated pain. It does not address generalized pelvic pain or symptomatology associated with sexual activity. This is not because these questions were not considered in the formulation of the questionnaire. Of 73 questions in the preliminary instrument covering domains of urinary symptoms, pain, sexual function, menstrual variability, and general health, only the 4 questions now in the instrument were needed to reliably and validly describe the illness experience of those with IC and distinguish these patients from those without the disorder (O’Leary and Sant, 1997).
) are a validated questionnaire that was originally developed by focus groups, subjected to test-retest reliability analysis, and validated by administration to IC patients and asymptomatic controls (O’Leary et al, 1997; Lubeck et al, 2001). The questionnaire centers on 3 questions related to urgency/frequency and 1 on bladder-associated pain. It does not address generalized pelvic pain or symptomatology associated with sexual activity. This is not because these questions were not considered in the formulation of the questionnaire. Of 73 questions in the preliminary instrument covering domains of urinary symptoms, pain, sexual function, menstrual variability, and general health, only the 4 questions now in the instrument were needed to reliably and validly describe the illness experience of those with IC and distinguish these patients from those without the disorder (O’Leary and Sant, 1997).
Table 12–16 O’Leary-Sant Indices
| INTERSTITIAL CYSTITIS SYMPTOM INDEX | INTERSTITIAL CYSTITIS PROBLEM INDEX |
|---|---|
| During the past month … | During the past month how much has each of the following been a problem for you: |
| Q1. … how often have you felt the strong need to urinate with little or no warning? |
Q1. Frequent urination during the day |
| Q2. … how often have you had to urinate less than 2 hours after you finished urinating? |
Q2. Getting up at night to urinate? |
| Q3. … how often did you most typically get up at night to urinate? |
Q3. Need to urinate with little warning? |
| Q4. … have you experienced pain or burning in your bladder? |
Q4. Burning, pain, discomfort, or pressure in your bladder? |
| Add the numerical values of the checked entries. | Add the numerical values of the checked entries. |
| Total score: _______ | Total score: _______ |
From O’Leary MP, Sant GR, Fowler FJ, et al. The interstitial cystitis symptom index and problem index. Urology 1997;49:58–63.
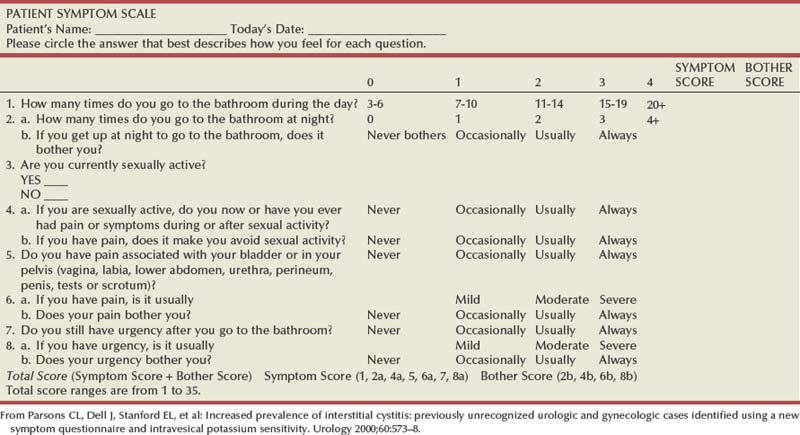
Another instrument is the PUF questionnaire (Parsons et al, 2002a) (Table 12–17 ![]() ). It was specifically designed to include questions that directly reflect a wide variety of the symptoms experienced by patients who are affected by this disorder. One third of the questions address pelvic pain, including pain anywhere in the pelvis: the vagina, labia, lower abdomen, urethra, perineum, testes, penis, or scrotum. A large study utilizing the PUF questionnaire has concluded that up to 23% of American females have BPS/IC (Parsons et al, 2002a). This makes one wary as to the utility and face-validity of the PUF (Ito et al, 2003). A total score of 10 to 14 equals a 74% likelihood of a positive potassium test (PST); 15 to 19 equals 76%; and 20+ equals 91%. To the extent that the PST is suspect, the reliability of PUF data comes into question. Question No. 4 of the PUF is problematic. Patients who are sexually active can gain up to 6 more points than those who are not, and patients who over time begin sexual activity because they are feeling better can actually accumulate a falsely elevated PUF score owing to this anomaly.
). It was specifically designed to include questions that directly reflect a wide variety of the symptoms experienced by patients who are affected by this disorder. One third of the questions address pelvic pain, including pain anywhere in the pelvis: the vagina, labia, lower abdomen, urethra, perineum, testes, penis, or scrotum. A large study utilizing the PUF questionnaire has concluded that up to 23% of American females have BPS/IC (Parsons et al, 2002a). This makes one wary as to the utility and face-validity of the PUF (Ito et al, 2003). A total score of 10 to 14 equals a 74% likelihood of a positive potassium test (PST); 15 to 19 equals 76%; and 20+ equals 91%. To the extent that the PST is suspect, the reliability of PUF data comes into question. Question No. 4 of the PUF is problematic. Patients who are sexually active can gain up to 6 more points than those who are not, and patients who over time begin sexual activity because they are feeling better can actually accumulate a falsely elevated PUF score owing to this anomaly.
None of the questionnaires has been shown to be of value in diagnosis (Moldwin and Kushner, 2004), although they may suggest who should be screened further for the syndrome (Kushner and Moldwin, 2006). The O’Leary-Sant and University of Wisconsin instruments correlate strongly in a large population of patients with BPS/IC (Sirinian and Payne, 2001). Both the O’Leary-Sant and University of Wisconsin questionnaires are responsive to change over time and thus good for following the natural history of the disorder and the results of treatment.
Treatment outcome studies have also used the Global Response Assessment (GRA); a balanced patient self-report on overall response to therapy developed for NIDDK-sponsored multicenter therapeutic trials (Sant et al, 2003) (Table 12–18). A one-category change in GRA correlates with a 1.2-point change in the O’Leary-Sant indices and a 3.1-point change in the University of Wisconsin instrument (Propert et al, 2006).
Table 12–18 Global Response Assessment (GRA)
From Sant GR, Propert KJ, Hanno PM, et al. A pilot clinical trial of oral pentosan polysulfate and oral hydroxyzine in patients with interstitial cystitis. J Urol 2003:170:810–15.
Principles of Management
The information currently available in the literature does not lend itself to easily formulating a diagnostic or treatment guideline that would be universally accepted (Hanno and Dmochowski, 2009). Different groups of “experts” would undoubtedly create different “best practices.” The compromise approach constructed by an experienced cross section of urologists and gynecologists from around the world at the International Consultation on Incontinence 2008 meeting in Paris seems reasonable and allows for significant latitude in individual practice and to account for patient preference (Hanno et al, 2009). It is outlined in Figures 12-13 and 12-14 and in Table 12–19.
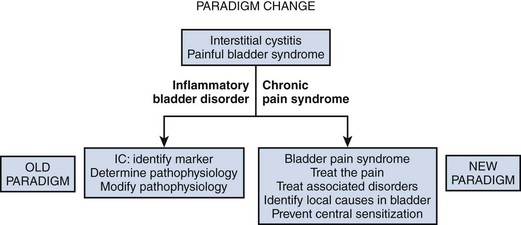
Figure 12–13 Paradigm change: interstitial cystitis (IC) evolves into painful bladder syndrome evolves into bladder pain syndrome.
(From Hanno PM. Proceedings of the International Consultation on Interstitial Cystitis. Japan: Comfortable Urology Network; 2008. p. 2–9.)
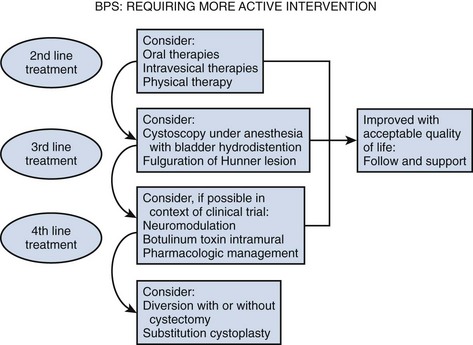
Figure 12–14 Diagnostic and treatment algorithm for bladder pain syndrome (BPS).
(From International Consultation on Incontinence 2008, Paris.)
Table 12–19 Principles of Management from the International Consultation on Incontinence, 2008
| Definition |
| Bladder Pain Syndrome (in the absence of a universally agreed definition, the European Society for the Study of Interstitial Cystitis—ESSIC definition is given along with a slight modification made at a recent international meeting held by the Society for Urodynamics and Female Urology—SUFU) |
| ESSIC: Chronic pelvic pain, pressure or discomfort of greater than 6 months duration perceived to be related to the urinary bladder accompanied by at least one other urinary symptom like persistent urge to void or urinary frequency. Confusable diseases as the cause of the symptoms must be excluded. |
| Consensus Definition from SUFU International Conference (Asia, Europe, North America) held in Miami, Florida February 2008: An unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptom(s) of more than 6 weeks duration, in the absence of infection or other identifiable causes. |
| Bladder Pain Syndrome (BPS) |
| NOMENCLATURE (see Fig. 12–13) |
| The scientific committee of the International Consultation voted to use the term “bladder pain syndrome” for the disorder that has been commonly referred to as interstitial cystitis (IC). The term painful bladder syndrome was dropped from the lexicon. The term IC implies an inflammation within the wall of the urinary bladder, involving gaps or spaces in the bladder tissue. This does not accurately describe the majority of patients with this syndrome. Painful Bladder Syndrome, as defined by the International Continence Society, is too restrictive for the clinical syndrome. Properly defined, the term Bladder Pain Syndrome appears to fit in well with the taxonomy of the International Association for the Study of Pain (IASP), and focuses on the actual symptom complex rather than what appears to be long-held misconception of the underlying pathology. |
| HISTORY/INITIAL ASSESSMENT |
| Males or females with pain, pressure, or discomfort that they perceive to be related to the bladder with at least one urinary symptom, such as frequency not obviously related to high fluid intake, or a persistent urge to void should be evaluated for possible bladder pain syndrome (see Fig. 12–9). The presence of commonly associated disorders including irritable bowel syndrome, chronic fatigue syndrome, and fibromyalgia in the presence of the cardinal symptoms also suggests the diagnosis. Abnormal gynecologic findings in women and well-characterized confusable diseases that may explain the symptoms must be ruled out. |
| The initial assessment consists of a frequency/volume chart, focused physical examination, urinalysis, and urine culture. Urine cytology and cystoscopy are recommended if clinically indicated. Patients with urinary infection should be treated and reassessed. Those with recurrent urinary infection, abnormal urinary cytology, and hematuria are evaluated with appropriate imaging and endoscopic procedures, and only if findings are unable to explain the symptoms, are they diagnosed with BPS. |
| INITIAL TREATMENT |
| Patient education, dietary manipulation, nonprescription analgesics, and pelvic floor relaxation techniques comprise the initial treatment of BPS. The treatment of pain needs to be addressed directly, and in some instances referral to an anesthesia/pain center can be an appropriate early step in conjunction with ongoing treatment of the syndrome. When conservative therapy fails or symptoms are severe and conservative management is unlikely to succeed, oral medication, intravesical treatment, or physical therapy can be prescribed. It is recommended to initiate a single form of therapy and observe results, adding another modality or substituting another modality as indicated by degree of response or lack of response to treatment. Excellence can be the enemy of good. |
| SECONDARY ASSESSMENT |
| If initial oral or intravesical therapy fails, or before beginning such therapy, it is reasonable to consider further evaluation which can include urodynamics, pelvic imaging, and cystoscopy with bladder distention and possible bladder biopsy under anesthesia (see Fig. 12–14). Findings of bladder overactivity suggest a trial of antimuscarinic therapy. Findings of a Hunner’s lesion suggest therapy with transurethral resection or fulguration of the lesion. Distention itself can have therapeutic benefit in 30%-50% of patients, though benefits rarely persist for longer than a few months. |
| REFRACTORY BPS |
| Those patients with persistent, unacceptable symptoms despite oral and/or intravesical therapy are candidates for more aggressive modalities. Many of these are best administered within the context of a clinical trial if possible. These may include neuromodulation, intradetrusor botulinum toxin, or newly described pharmacologic management techniques. At this point, most patients will benefit from the expertise of an anesthesia pain clinic. The last step in treatment is usually some type of surgical intervention aimed at increasing the functional capacity of the bladder or diverting the urinary stream. Urinary diversion with or without cystectomy has been used as a last resort with good results in selected patients. Augmentation or substitution cystoplasty seems less effective and more prone to recurrence of chronic pain in small reported series. |
Philosophy of Management
This author believes that, because of the natural history of the disorder, it is best to cautiously progress through a variety of treatments. Whereas the shotgun approach, starting newly diagnosed patients on a variety of simultaneous medications, seems to have many adherents, employing one treatment at a time makes the natural history of the disease itself an ally in the treatment process. One should encourage patients to maximize their activity and live as normal a life as possible, not becoming a prisoner of the condition. Although some activities or foods may aggravate symptoms, nothing has been shown to negatively affect the disease process itself. Therefore, patients should feel free to experiment and judge for themselves how to modify their lifestyle without the guilt that comes from feeling they have harmed themselves if symptoms flare. Dogmatic restriction and diet are to be avoided unless they are shown to improve symptoms in a particular patient.
In the near future, phenotyping of patients with BPS/IC may improve treatment outcomes but only time and future studies will determine if this is true (Baranowski et al, 2008). To answer the perennial question, “Can we, as health care providers, make evidence-based decisions for BPS/IC at this time?” the answer seems to be a qualified sometimes (Fall et al, 2008).
Baranowski AP, Abrams P, Berger RE, et al. Urogenital pain—time to accept a new approach to phenotyping and, as a consequence, management. Eur Urol. 2008;53:33-36.
Buffington CA, Chew DJ, Woodworth BE. Feline interstitial cystitis. J Am Vet Med Assoc. 1999;215:682-687.
Fall M, Oberpenning F, Peeker R. Treatment of bladder pain syndrome/interstitial cystitis 2008: can we make evidence-based decisions? Eur Urol. 2008;54(1):65-75.
Hand JR. Interstitial cystitis: report of 223 cases (204 women and 19 men). J Urol. 1949;61:291-310.
Hanno P, Lin AT, Nordling J, Nyberg L, et al. Bladder pain syndrome. In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence. Paris, France: Health Publication Ltd; 2009:1459-1518.
Hanno PM, Landis JR, Matthews-Cook Y, et al. The diagnosis of interstitial cystitis revisited: lessons learned from the National Institutes of Health Interstitial Cystitis Database study. J Urol. 1999;161:553-557.
Keay S, Zhang CO, Hise MK, et al. A diagnostic in vitro urine assay for interstitial cystitis. Urology. 1998;52:974-978.
Messing EM, Stamey TA. Interstitial cystitis: early diagnosis, pathology, and treatment. Urology. 1978;12:381-392.
Nordling J, Anjum FH, Bade JJ, et al. Primary evaluation of patients suspected of having interstitial cystitis (IC). Eur Urol. 2004;45:662-669.
Oravisto KJ. Epidemiology of interstitial cystitis. Ann Chir Gynaecol Fenn. 1975;64:75-77.
Parsons CL. Epithelial coating techniques in the treatment of interstitial cystitis. Urology. 1997;49:100-104.
Pool TL. Interstitial cystitis: clinical considerations and treatment. Clin Obstet Gynecol. 1967;185:10.
van de Merwe JP, Nordling J, Bouchelouche P, et al. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: an ESSIC proposal. Eur Urol. 2008;53:60-67.
Warren JW, Howard FM, Cross RK, et al. Antecedent nonbladder syndromes in case-control study of interstitial cystitis/painful bladder syndrome. Urology. 2009;73:52-57.
Aaron LA, Buchwald D. A review of the evidence for overlap among unexplained clinical conditions. Ann Intern Med. 2001;134:868-881.
Aaron LA, Herrell R, Ashton S, et al. Comorbid clinical conditions in chronic fatigue: a co-twin control study. J Gen Intern Med. 2001;16:24-31.
Abbott J, Hawe J, Hunter D, et al. Laparoscopic excision of endometriosis: a randomized, placebo-controlled trial. Fertil Steril. 2004;82:878-884.
Abdel-Mageed AB. NF-kappaB-dependent gene expression of proinflammatory cytokines in T24 cells: possible role in interstitial cystitis. Urol Res. 2003;31:300-305.
Abdel-Mageed AB, Ghoniem GM. Potential role of rel/nuclear factor-kappaB in the pathogenesis of interstitial cystitis. J Urol. 1998;160:2000-2003.
Abelli L, Conte B, Somma V, et al. Mechanical irritation induces neurogenic inflammation in the rat urethra. J Urol. 1991;146:1624-1626.
Aboseif S, Tamaddon K, Vhalfin S, et al. Sacral neuromodulation as an effective treatment for refractory pelvic floor dysfunction. Urology. 2002;60:52-56.
Abraham SN, Malaviya R. Mast cells in infection and immunity. Infect Immun. 1997;65:3501-3508.
Abramov Y, Goldberg RP, McGuire M, et al. Eosinophilic cystitis after bladder instillation with dimethyl sulfoxide. Urology. 2004;63:1182-1183.
Abrams P, Baranowski A, Berger R, et al. A new classification is needed for pelvic pain syndromes—are existing terminologies of spurious diagnostic authority bad for patients? J Urol. 2006;175:1989-1990.
Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21:167-178.
Abrams P, Hanno P, Wein A. Overactive bladder and painful bladder syndrome: there need not be confusion. Neurourol Urodyn. 2005;24:149-150.
Adeyoju AB, Thornhill J, Lynch T, et al. The fate of the defunctioned bladder following supravesical urinary diversion. Br J Urol. 1996;78:80-83.
Agarwal M, Dixon RA. A study to detect Helicobacter pylori in fresh and archival specimens from patients with interstitial cystitis, using amplification methods. BJU Int. 2003;91:814-816.
Aghamir SM, Mohseni MG, Arasteh S. Intravesical bacillus Calmette-Guérin for treatment of refractory interstitial cystitis. Urol J. 2007;4:18-23.
Ahluwalia A, Giuliani S, Scotland R, Maggi CA. Ovalbumin-induced neurogenic inflammation in the bladder of sensitized rats. Br J Pharmacol. 1998;124:190-196.
Ahmad I, Sarath KN, Meddings RN. Sequential hydrodistension and intravesical instillation of hyaluronic acid under general anaesthesia for treatment of refractory interstitial cystitis: a pilot study. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:543-546.
Al Hadithi H, Tincello DG, Vince GS, Richmond DH. Leukocyte populations in interstitial cystitis and idiopathic reduced bladder storage. Urology. 2002;59:851-855.
Alagiri M, Chottiner S, Ratner V, et al. Interstitial cystitis: unexplained associations with other chronic disease and pain syndromes. Urology. 1997;49:52-57.
Albers DD, Geyer JR. Long-term results of cystolysis (supratrigonal denervation) of the bladder for intractable interstitial cystitis. J Urol. 1988;139:1205-1206.
Aldenborg F, Fall M, Enerback L. Proliferation and transepithelial migration of mucosal mast cells in interstitial cystitis. Immunology. 1986;58:411-416.
Aldenborg F, Fall M, Enerback L. Mast cells in interstitial cystitis. Ann Urol (Paris). 1989;23:165-166.
Alexacos N, Pang X, Boucher W, et al. Neurotensin mediates rat bladder mast cell degranulation triggered by acute psychological stress. Urology. 1999;53:1035-1040.
Anderson J, Carrion R, Ordorica R, et al. Anterior enterocele following cystectomy for intractable interstitial cystitis. J Urol. 1998;159:1868-1870.
Anderson JA. The ethics and science of placebo-controlled trials: assay sensitivity and the Duhem-Quine thesis. J Med Philos. 2006;31:65-81.
Anderson JB, Parivar F, Lee G, et al. The enigma of interstitial cystitis—an autoimmune disease? Br J Urol. 1989;63:58-63.
Anderstrom CR, Fall M, Johansson SL. Scanning electron microscopic findings in interstitial cystitis. Br J Urol. 1989;63:270-275.
Apostolidis A, Dasgupta P, Denys P, et al. Recommendations on the use of botulinum toxin in the treatment of lower urinary tract disorders and pelvic floor dysfunctions: a European consensus report. Eur Urol. 2009;55(1):100-119.
Arnold LM, Russell IJ, Diri EW, et al. A 14-week, randomized, double-blinded, placebo-controlled monotherapy trial of pregabalin in patients with fibromyalgia. J Pain. 2008;9(9):792-805.
Atug F, Turkeri L, Atug O, Cal C. Detection of Helicobacter pylori in bladder biopsy specimens of patients with interstitial cystitis by polymerase chain reaction. Urol Res. 2004;32:346-349.
Aubert J, Dore B, Touchard G. [Eosinophilic cystitis. J Urol (Paris). 1983;89:65-70. [in French]
Awad SA, MacDiarmid S, Gajewski JB, Gupta R. Idiopathic reduced bladder storage versus interstitial cystitis. J Urol. 1992;148:1409-1412.
Azadzoi KM, Tarcan T, Kozlowski R, et al. Overactivity and structural changes in the chronically ischemic bladder. J Urol. 1999;162:1768-1778.
Backonja M, Beydoun A, Edwards KR, et al. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus. JAMA. 1998;280:1831-1836.
Bade JJ, Hollants F, Gerkens F, et al. The efficacy of intravesical oxybutynin and pentosanpolysulfate in the treatment of interstitial cystitis: a prospective, double-blind trial. J Urol. 2000;163S:60.
Bade JJ, Laseur M, Nieuwenburg A, et al. A placebo-controlled study of intravesical pentosanpolysulphate for the treatment of interstitial cystitis. Br J Urol. 1997;79:168-171.
Bade JJ, Marrink J, Karrenbeld A, et al. Increased urinary levels of Tamm-Horsfall glycoprotein suggest a systemic etiology of interstitial cystitis. J Urol. 1996;156:943-946.
Bade JJ, Peeters JM, Mensink HJ. Is the diet of patients with interstitial cystitis related to their disease? Eur Urol. 1997;32:179-183.
Bade JJ, Rijcken B, Mensink HJ. Interstitial cystitis in The Netherlands: prevalence, diagnostic criteria and therapeutic preferences. J Urol. 1995;154:2035-2037.
Badenoch AW. Chronic interstitial cystitis. Br J Urol. 1971;43:718-721.
Baldessarini RJ. Drugs and the treatment of psychiatric disorders. In: Gilman AG, Goodman SS, Rall TW, et al, editors. The pharmacological basis of therapeutics. New York: Macmillan Publishing Company; 1985:387-445.
Baranowski A, Abrams P, Berger R, et al. Urogenital pain—time to accept a new approach to phenotyping and, as a consequence, management. Eur Urol. 2008;53:33-36.
Barbalias GA, Liatsikos EN, Athanasopoulos A, Nikiforidis G. Interstitial cystitis: bladder training with intravesical oxybutynin. J Urol. 2000;163:1818-1822.
Barbanti G, Maggi CA, Beneforti P, et al. Relief of pain following intravesical capsaicin in patients with hypersensitive disorders of the lower urinary tract. Br J Urol. 1993;71:686-691.
Barker SB, Matthews PN, Philip PF, et al. Prospective study of intravesical dimethyl sulfoxide in the treatment of chronic inflammatory bladder disease. Br J Urol. 1987;59:142-144.
Baron R. Peripheral neuropathic pain: from mechanisms to symptoms. Clin J Pain. 2000;16:12-20.
Barrett DM, Wein AJ. Voiding dysfunction: diagnosis, classification, and management. In: Gillenwater JY, Grayhack JT, Howards SS, et al, editors. Adult and pediatric urology. Chicago: Year Book Medical Publishers; 1987:863-892.
Barrington JW, Stephenson TP. Pentosanpolysulphate for interstitial cystitis. Int Urogynecol J Pelvic Floor Dysfunct. 1997;8:293-295.
Baskin LS, Tanagho EA. Pelvic pain without pelvic organs. J Urol. 1992;147:683-686.
Batra AK, Hanno PM. Interstitial cystitis in association with scleroderma. Indian J Urol. 1997;13:93.
Baykara M, Erdogru T, Gulkesen KH, et al. Does interstitial cystitis urine include possible factors effecting the nociceptive system of the spinal cord? Urol Int. 2003;71:66-72.
Beier-Holgersen R, Hermann GG, Mortensen SO, Steven K. The in vitro cytotoxicity of urine from patients with interstitial cystitis. J Urol. 1994;151:206-207.
Bejany DE, Politano VA. Ileocolic neobladder in the woman with interstitial cystitis and a small contracted bladder. J Urol. 1995;153:42-43.
Bennett RM. Emerging concepts in the neurobiology of chronic pain: evidence of abnormal sensory processing in fibromyalgia. Mayo Clin Proc. 1999;74:385-398.
Benson H, Epstein MD. The placebo effect. JAMA. 1976;232:1225-1226.
Berger RE, Miller JE, Rothman I, et al. Bladder petechiae after cystoscopy and hydrodistension in men diagnosed with prostate pain. J Urol. 1998;159:83-85.
Bernardini P, Bondavalli C, Luciano M, et al. [Interstitial cystitis: epidemiology. Arch Ital Urol Androl. 1999;71:313-315. [in Italian]
Berry SH, Hayes R, Suttorp M, et al. Health-related quality of life impact of interstitial cystitis/painful bladder syndrome and other symptomatic pelvic disorders, 2009.
Bhone AW, Hodson JM, Rebuck JW, et al. An abnormal leukocyte response in interstitial cystitis. J Urol. 1962;88:387-391.
Biggers RD. Self-administration of dimethyl sulfoxide (DMSO) for interstitial cystitis. Urology. 1986;28:10-11.
Birder LA, Kanai AJ, de Groat WC. DMSO: effect on bladder afferent neurons and nitric oxide release. J Urol. 1997;158:1989-1995.
Birder LA, Wolf-Johnston A, Buffington CA, et al. Altered inducible nitric oxide synthase expression and nitric oxide production in the bladder of cats with feline interstitial cystitis. J Urol. 2005;173:625-629.
Bjorling DE, Jerde TJ, Zine MJ, et al. Mast cells mediate the severity of experimental cystitis in mice. J Urol. 1999;162:231-236.
Bjorling DE, Wang ZY. Estrogen and neuroinflammation. Urology. 2001;57:40-46.
Blackford HN, Murray K, Stephenson TP, et al. Results of transvesical infiltration of the pelvic plexuses with phenol in 116 patients. Br J Urol. 1984;56:647-649.
Blaivas JG. Overactive bladder and the definition of urgency. Neurourol Urodyn. 2007;26:757-758.
Blaivas JG, Panagopoulos G, Weiss JP, Somaroo C. Two types of urgency. Neurourol Urodyn. 2009;28:188-190.
Blaivas JG, Weiss JP, Desai P, et al. Long-term follow-up of augmentation enterocystoplasty and continent diversion in patients with benign disease. J Urol. 2005;173:1631-1634.
Bodden-Heidrich R. [Psychosomatic aspects of urogynaecology: model considerations on the pathogenesis, diagnosis and therapy. Zentralbl Gynakol. 2004;126:237-243. [in German]
Bogart LM, Berry SH, Clemens JQ. Symptoms of interstitial cystitis, painful bladder syndrome and similar diseases in women: a systematic review. J Urol. 2007;177:450-456.
Bouchelouche K, Kristensen B, Nordling J, et al. Increased urinary excretion of leukotriene E(4) in patients with interstitial cystitis. Urology. 2001;57:128.
Bouchelouche K, Nordling J, Hald T, Bouchelouche P. Treatment of interstitial cystitis with montelukast, a leukotriene D(4) receptor antagonist. Urology. 2001;57:118.
Bouchelouche K, Nordling J, Hald T, Bouchelouche P. The cysteinyl leukotriene D4 receptor antagonist montelukast for the treatment of interstitial cystitis. J Urol. 2001;166:1734-1737.
Boucher W, El Mansoury M, Pang X, et al. Elevated mast cell tryptase in the urine of patients with interstitial cystitis. Br J Urol. 1995;76:94-100.
Boucher W, Stern JM, Kotsinyan V, et al. Intravesical nanocrystalline silver decreases experimental bladder inflammation. J Urol. 2008;179:1598-1602.
Bourque JP. Surgical management of the painful bladder. J Urol. 1951;65:25-34.
Boye E, Morse M, Huttner I, et al. Immune complex-mediated interstitial cystitis as a major manifestation of systemic lupus erythematosus. Clin Immunol Immunopathol. 1979;13:67-76.
Bracis R, Sanders CV, Gilbert DN. Methicillin hemorrhagic cystitis. Antimicrob Agents Chemother. 1977;12:438-439.
Bramble FJ, Morley R. Drug-induced cystitis: the need for vigilance. Br J Urol. 1997;79:3-7.
Brookoff D. The causes and treatment of pain in interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:177-192.
Buffington CA. External and internal influences on disease risk in cats. J Am Vet Med Assoc. 2002;220:994.
Buffington CA. Comorbidity of interstitial cystitis with other unexplained clinical conditions. J Urol. 2004;172:1242-1248.
Buffington CA. Developmental influences on medically unexplained symptoms. Psychother Psychosom. 2009;78:139-144.
Buffington CA, Blaisdell JL, Binns SP, et al. Decreased urine glycosaminoglycan excretion in cats with idiopathic cystitis. J Urol. 1996;155:1801-1804.
Buffington CA, Chew DJ, DiBartola SP. On the definition of feline interstitial cystitis. J Am Vet Med Assoc. 1999;215:186-188.
Buffington CA, Pacak K. Increased plasma norepinephrine concentration in cats with interstitial cystitis. J Urol. 2001;165:2051-2054.
Buffington CA, Teng B, Somogyi GT. Norepinephrine content and adrenoceptor function in the bladder of cats with feline interstitial cystitis. J Urol. 2002;167:1876-1880.
Buffington CA, Wolfe SA. High affinity binding sites for 3H substance P in urinary bladders of cats with interstitial cystitis. J Urol. 1998;160:605-611.
Buffington CA, Woodworth BE. Excretion of fluorescein in the urine of women with interstitial cystitis. J Urol. 1997;158:786-789.
Buffington T, Pacak K. Increased plasma norepinephrine concentrations in cats with interstitial cystitis. Urology. 2001;57:102.
Bullock AD, Becich MJ, Klutke CG, Ratliff TL. Experimental autoimmune cystitis: a potential murine model for ulcerative interstitial cystitis. J Urol. 1992;148:1951-1956.
Bumpus HC. Interstitial cystitis: its treatment by overdistention of the bladder. Med Clin North Am. 1930;13:1495-1498.
Bunyaratavej P, La-ornual S, Kongkanand A, et al. Ten years’ experience with enterocystoplasty. J Med Assoc Thai. 1993;76:327-333.
Burford EH, Burford CE. Hunner ulcer of the bladder: a report of 187 cases. J Urol. 1958;79:952-955.
Burgio KL, Engel BT, Locher JL. Normative patterns of diurnal urination across 6 age decades. J Urol. 1991;145:728-731.
Burkhard FC, Blick N, Hochreiter WW, Studer UE. Urinary urgency and frequency, and chronic urethral and/or pelvic pain in females: can doxycycline help? J Urol. 2004;172:232-235.
Burnstock G. Release of vasoactive substances from endothelial cells by shear stress and purinergic mechanosensory transduction. J Anat. 1999;194:335.
Bushman W, Goolsby C, Grayhack JT, Schaeffer AJ. Abnormal flow cytometry profiles in patients with interstitial cystitis. J Urol. 1994;152:2262-2266.
Byrne DS, Sedor JF, Estojak J, et al. The urinary glycoprotein GP51 as a clinical marker for interstitial cystitis. J Urol. 1999;161:1786-1790.
Cameron AP, Gajewski JB. Bladder outlet obstruction in painful bladder syndrome/interstitial cystitis. Neurourol Urodyn. 2009;28(8):944-948.
Carlson K, Rome S, Nitti V. Dysfunctional voiding in women. J Urol. 2001;165:143-148.
Cartledge JJ, Davies AM, Eardley I. A randomized double-blind placebo-controlled crossover trial of the efficacy of L-arginine in the treatment of interstitial cystitis. BJU Int. 2000;85:421-426.
Caulfield J, Phillips R, Steinhardt G. Intravesical heparin instillation: is there systemic absorption? J Urol. 1995;153:289A.
Cervigni M, Natale F, Nasta L, et al. A combined intravesical therapy with hyaluronic acid and chondroitin for refractory painful bladder syndrome/interstitial cystitis. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:943-947.
Chai TC. Diagnosis of the painful bladder syndrome: current approaches to diagnosis. Clin Obstet Gynecol. 2002;45:250-258.
Chai TC, Zhang C, Warren JW, Keay S. Percutaneous sacral third nerve root neurostimulation improves symptoms and normalizes urinary HB-EGF levels and antiproliferative activity in patients with interstitial cystitis. Urology. 2000;55:643-646.
Chai TC, Zhang CO, Shoenfelt JL, et al. Bladder stretch alters urinary heparin-binding epidermal growth factor and antiproliferative factor in patients with interstitial cystitis. J Urol. 2000;163:1440-1444.
Chambers GK, Fenster HN, Cripps S, et al. An assessment of the use of intravesical potassium in the diagnosis of interstitial cystitis. J Urol. 1999;162:699-701.
Chancellor MB, de Groat WC. Intravesical capsaicin and resiniferatoxin therapy: spicing up the ways to treat the overactive bladder. J Urol. 1999;162:3-11.
Chancellor MB, Shenot PJ, Rivas DA, et al. Urological symptomatology in patients with reflex sympathetic dystrophy. J Urol. 1996;155:634-637.
Chancellor MB, Yoshimura N. Treatment of interstitial cystitis. Urology. 2004;63:85-92.
Chang PL. Urodynamic studies in acupuncture for women with frequency, urgency, and dysuria. J Urol. 1988;140:563-566.
Chelsky MJ, Rosen SI, Knight LC, et al. Bladder permeability in interstitial cystitis is similar to that of normal volunteers: direct measurement by transvesical absorption of 99mtechnetium-diethylenetriaminepentaacetic acid. J Urol. 1994;151:346-349.
Chen G-D, Lin L-Y, Gardner JD. The results of laparoscopic adhesiolysis for intractable urinary frequency. J Urol. 1997;158:1714-1716.
Cheng C, Whitfield HN. Cystoplasty: tubularization or detubularization. Br J Urol. 1990;66:30-34.
Chesa PN, Armas MJ, Artiles Hernandez JL, et al. [Enterocystoplasty in the treatment of interstitial cystitis. Actas Urol Esp. 2001;25:489-492. [in Spanish]
Christensen MM, Keith I, Rhodes PR, et al. A guinea pig model for study of bladder mast cell function: histamine release and smooth muscle contraction. J Urol. 1990;144:1293-1300.
Christmas TJ. Lymphocyte sub-populations in the bladder wall in normal bladder, bacterial cystitis and interstitial cystitis. Br J Urol. 1994;73:508-515.
Christmas TJ. Historical aspects of interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:1-8.
Christmas TJ, Holmes SA, Hendry WF. Bladder replacement by ileocystoplasty: the final treatment for interstitial cystitis. Br J Urol. 1996;78:69-73.
Christmas TJ, Rode J. Characteristics of mast cells in normal bladder, bacterial cystitis and interstitial cystitis. Br J Urol. 1991;68:473-478.
Christmas TJ, Rode J, Chapple CR, et al. Nerve fibre proliferation in interstitial cystitis. Virchows Arch A Pathol Anat Histopathol. 1990;416:447-451.
Christmas TJ, Smith GL, Rode J. Detrusor myopathy: an accurate predictor of bladder hypocompliance and contracture in interstitial cystitis. Br J Urol. 1996;78:862-865.
Chuang YC, Yoshimura N, Huang CC, et al. Intravesical botulinum toxin A administration produces analgesia against acetic acid induced bladder pain responses in rats. J Urol. 2004;172:1529-1532.
Chudwin DS, Chesney PJ, Mischler EH, et al. Hematuria associated with carbenicillin and other semisynthetic penicillins [letter]. Am J Dis Child. 1979;133:98-99.
Chung MK. Interstitial cystitis in persistent posthysterectomy chronic pelvic pain. JSLS. 2004;8:329-333.
Clauw DJ, Schmidt M, Radulovic D, et al. The relationship between fibromyalgia and interstitial cystitis. J Psychiatr Res. 1997;31:125-131.
Clemens JQ, Brown SO, Calhoun EA. Mental health diagnoses in patients with interstitial cystitis/painful bladder syndrome and chronic prostatitis/chronic pelvic pain syndrome: a case/control study. J Urol. 2008;180:1378-1382.
Clemens JQ, Joyce GF, Wise M, Payne CK. Interstitial cystitis and painful bladder syndrome. In: Litwin MS, Saigal C, editors. Urologic diseases in America. Washington (DC: National Institutes of Health; 2007:125-154.
Clemens JQ, Link CL, Eggers PW, et al. Prevalence of painful bladder symptoms and effect on quality of life in black, Hispanic and white men and women. J Urol. 2007;177:1390-1394.
Clemens JQ, Markossian T, Calhoun EA. Comparison of economic impact of chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis/painful bladder syndrome. Urology. 2009;73(4):743-746.
Clemens JQ, Meenan RT, O’Keeffe Rosetti MC, et al. Case-control study of medical comorbidities in women with interstitial cystitis. J Urol. 2008;179:2222-2225.
Clemens JQ, Meenan RT, Rosetti MC, et al. Costs of interstitial cystitis in a managed care population. Urology. 2008;71:776-780.
Clemens J, Meenan R, Rosetti M, Calhoun E. Prevalence and incidence of interstitial cystitis in a managed care population. J Urol. 2005;173:98-102.
Clemmensen OJ, Lose G, Holm-Bentzen M, Colstrup H. Skin reactions to urine in patients with interstitial cystitis. Urology. 1988;32:17-20.
Close CE, Carr MC, Burns MW, et al. Interstitial cystitis in children. J Urol. 1996;156:860-862.
Collan Y, Alfthan O, Kivilaakso E, Oravisto KJ. Electron microscopic and histological findings on urinary bladder epithelium in interstitial cystitis. Eur Urol. 1976;2:242-247.
Collas DM, Malone-Lee JG. Age-associated changes in detrusor sensory function in women with lower urinary tract symptoms. Int Urogynecol J. 1996;7:24-29.
Comiter CV. Sacral neuromodulation for the symptomatic treatment of refractory interstitial cystitis: a prospective study. J Urol. 2003;169:1369-1373.
1993 Consensus document on fibromyalgia: The Copenhagen declaration. J Musculoskeletal Pain. 1993;1:295-312.
Cook FV, Farrar WE, Kreutner A. Hemorrhagic cystitis and ureteritis, and interstitial nephritis associated with administration of penicillin G. J Urol. 1979;122:110-111.
Cornish J, Nickel JC, Vanderwee M, et al. Ultrastructural visualization of human bladder mucus. Urol Res. 1990;18:263-264.
Costello AJ, Crowe H, Agarwal D. Supratrigonal cystectomy and ileocystoplasty in management of interstitial cystitis. Aust N Z J Surg. 2000;70:34-38.
Cox M, Klutke JJ, Klutke CG. Assessment of patient outcomes following submucosal injection of triamcinolone for treatment of Hunner’s ulcer subtype interstitial cystitis. Can J Urol. 2009;16:4536-4540.
Creighton SM, Pearce JM, Robson I, et al. Sensory urgency: how full is your bladder? Br J Obstet Gynaecol. 1991;98:1287-1289.
Cross S. Pathophysiology of pain. Mayo Clin Proc. 1994;69:375-383.
Cruz F, Dinis P. Resiniferatoxin and botulinum toxin type A for treatment of lower urinary tract symptoms. Neurourol Urodyn. 2007;26:920-927.
Cruz F, Guimaraes M, Silva C, et al. Desensitization of bladder sensory fibers by intravesical capsaicin has long lasting clinical and urodynamic effects in patients with hyperactive or hypersensitive bladder dysfunction. J Urol. 1997;157:585-589.
Curhan GC, Speizer FE, Hunter DJ, et al. Epidemiology of interstitial cystitis: a population based study. J Urol. 1999;161:549-552.
Daha LK, Riedl CR, Hohlbrugger G, et al. Comparative assessment of maximal bladder capacity, 0.9% NaCl versus 0.2 M KCl, for the diagnosis of interstitial cystitis: a prospective controlled study. J Urol. 2003;170:807-809.
Daha LK, Riedl CR, Lazar D, et al. Effect of intravesical glycosaminoglycan substitution therapy on bladder pain syndrome/interstitial cystitis, bladder capacity and potassium sensitivity. Scand J Urol Nephrol. 2008;42(4):369-372.
Daneshgari F, Zimmern PE, Jacomides L. Magnetic resonance imaging detection of symptomatic noncommunicating intraurethral wall diverticula in women. J Urol. 1999;161:1259-1262.
Dasgupta P, Sharma SD, Womack C, et al. Cimetidine in painful bladder syndrome: a histopathological study. BJU Int. 2001;88:183-186.
Davidson A, Diamond B. Autoimmune diseases. N Engl J Med. 2001;345:340-350.
Davidsson T, Carlen B, Bak-Jensen E, et al. Morphologic changes in intestinal mucosa with urinary contact—effects of urine or disuse. J Urol. 1996;156:226-232.
Davis EL, El Khoudary SR, Talbott EO, et al. Safety and efficacy of the use of intravesical and oral pentosan polysulfate sodium for interstitial cystitis: a randomized double-blind clinical trial. J Urol. 2008;179:177-185.
Dawson TE, Jamison J. Intravesical treatments for painful bladder syndrome/interstitial cystitis. Cochrane Database Syst Rev 2007;CD006113.
DeJuana CP, Everett JCJr. Interstitial cystitis: experience and review of recent literature. Urology. 1977;10:325-329.
De la Serna AR, Alarçon-Segovia D. Chronic interstitial cystitis as an initial major manifestation of systemic lupus erythematosus. J Rheumatol. 1981;8:808-810.
Dell JR, Parsons CL. Multimodal therapy for interstitial cystitis. J Reprod Med. 2004;49:243-252.
Del Popolo G. Botulinum toxin a era: little steps towards a better understanding. Eur Urol. 2008;54:25-27.
Denson MA, Griebling TL, Cohen MB, Kreder KJ. Comparison of cystoscopic and histological findings in patients with suspected interstitial cystitis. J Urol. 2000;164:1908-1911.
Desbiens NA. In randomized controlled trials, should subjects in both placebo and drug groups be expected to guess that they are taking drug 50% of the time? Med Hypotheses. 2002;59:227-232.
Digesu G, Khullar V, Panayi D, et al. Should we explain lower urinary tract symptoms to patients? Neurourol Urodyn. 2008;27(5):368-371.
Diggs C, Meyer WA, Langenberg P, et al. Assessing urgency in interstitial cystitis/painful bladder syndrome. Urology. 2007;69:210-214.
Dimitrakov J, Tchitalov J, Zlatanov T, et al. Corticotropin-releasing hormone perturbations in interstitial cystitis patients: evidence for abnormal sympathetic activity. Urology. 2001;57:128.
Dimitrakov JD. A case of familial clustering of interstitial cystitis and chronic pelvic pain syndrome. Urology. 2001;58:281.
Dimitriadou V, Buzzi MG, Moskowitz MA, et al. Trigeminal sensory fiber stimulation induces morphological changes reflecting secretion in rat dura mater mast cells. Neuroscience. 1991;44:97-112.
Dimitriadou V, Buzzi MG, Theoharides TC, et al. Ultrastructural evidence for neurogenically mediated changes in blood vessels of the rat dura mater and tongue following antidromic trigeminal stimulation. Neuroscience. 1992;48:187-203.
Dixon JS, Holm-Bentzen M, Gilpin CJ, et al. Electron microscopic investigation of the bladder urothelium and glycocalyx in patients with interstitial cystitis. J Urol. 1986;135:621-625.
Dodson AI. Hunner’s ulcer of the bladder: a report of ten cases. Va Med Mon. 1926;53:305-310.
Doggweiler R, Jasmin L, Schmidt RA. Neurogenically mediated cystitis in rats: an animal model. J Urol. 1998;160:1551-1556.
Doggweiler-Wiygul R, Blankenship J, MacDiarmid SA. Review on chronic pelvic pain from a urological point of view. World J Urol. 2001;19:160-165.
Doggweiler-Wiygul R, Wiygul JP. Interstitial cystitis, pelvic pain, and the relationship to myofascial pain and dysfunction: a report on four patients. World J Urol. 2002;20:310-314.
Doi K, Saito Y, Nikai T, et al. Lumbar sympathetic block for pain relief in two patients with interstitial cystitis. Reg Anesth Pain Med. 2001;26:271-273.
Domingue GJ, Ghoniem GM. Occult infection in interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:77-86.
Domingue GJ, Ghoniem GM, Bost KL, et al. Dormant microbes in interstitial cystitis. J Urol. 1995;153:1321-1326.
Dondore PA, Schwartz AM, Semerjian H. Mast cell counts are not useful in the diagnosis of nonulcerative interstitial cystitis. J Urol. 1996;155:885-887.
1998 Drugs for pain. Med Lett. 1998;40:79-84.
DuBeau C, Khullar V, Versi E. “Unblinding” in randomized controlled drug trials for urinary incontinence: implications for assessing outcomes when adverse effects are evident. Neurourol Urodyn. 2005;24(1):13-20.
Duldulao KE, Diokno AC, Mitchell B. Value of urinary cytology in women presenting with urge incontinence and/or irritative voiding symptoms. J Urol. 1997;157:113-116.
Duncan JL, Schaeffer AJ. Do infectious agents cause interstitial cystitis? Urology. 1997;49:48-51.
Dundore PA, Schwartz AM, Semerjian H. Mast cell counts are not useful in the diagnosis of nonulcerative interstitial cystitis. J Urol. 1996;155:885-887.
Dunn M, Ramsden PD, Roberts JB, et al. Interstitial cystitis, treated by prolonged bladder distension. Br J Urol. 1977;49:641-645.
Dupont M, Spitsbergen J, Kim K, et al. Histological and neurotrophic changes triggered by varying models of bladder inflammation. J Urol. 2001;166:1111-1118.
Durier JL. The application of anti-anaerobic antibiotics to the treatment of female bladder dysfunctions. Neurourol Urodyn. 1992;11:418.
Edwards L, Bucknall TE, Makin C. Interstitial cystitis: possible cause and clinical study of sodium cromoglycate. Br J Urol. 1986;58:95-96.
Ehren I, Hosseini A, Herulf M, et al. Measurement of luminal nitric oxide in bladder inflammation using a silicon balloon catheter: a novel minimally invasive method. Urology. 1999;54:264-267.
Ehren I, Lundberg JO, Adolfsson J, Wiklund NP. Effects of L-arginine treatment on symptoms and bladder nitric oxide levels in patients with interstitial cystitis. Urology. 1998;52:1026-1029.
Eigner EB, Freiha FS. The fate of the remaining bladder following supravesical diversion. J Urol. 1990;144:31-33.
Eisen DP, Fraser IR, Sung LM, et al. Decreased viral load and symptoms of polyomavirus-associated chronic interstitial cystitis after intravesical cidofovir treatment. Clin Infect Dis. 2009;48(9):e86-e88.
Ek A, Engberg A, Frodin L, Jonsson G. The use of dimethyl-sulfoxide (DMSO) in the treatment of interstitial cystitis. Scand J Urol Nephrol. 1978;12:129-131.
El Mansoury M, Boucher W, Sant GR, Theoharides TC. Increased urine histamine and methylhistamine in interstitial cystitis. J Urol. 1994;152:350-353.
El-Bahnasy A, Farahat Y, El-Bendary M, et al. A randomized controlled trial of bacillus Calmette-Guérin and botulinum toxin-A for the treatment of refractory interstitial cystitis. UroToday Int. 2009;2:1944.
Elbadawi A. Interstitial cystitis: a critique of current concepts with a new proposal for pathologic diagnosis and pathogenesis. Urology. 1997;49:14-40.
Elbadawi AE, Light JK. Distinctive ultrastructural pathology of nonulcerative interstitial cystitis: new observations and their potential significance in pathogenesis. Urol Int. 1996;56:137-162.
Elgavish A. Epigenetic reprogramming: a possible etiological factor in bladder pain syndrome/interstitial cystitis? J Urol. 2009;181(3):980-984.
Elgavish A, Pattanaik A, Lloyd K, Reed R. Evidence for altered proliferative ability of progenitors of urothelial cells in interstitial cystitis. J Urol. 1997;158:248-252.
Elgavish A, Robert B, Lloyd K, et al. Evidence for a mechanism of bacterial toxin action that may lead to the onset of urothelial injury in the interstitial cystitis bladder [abstract]. J Urol. 1995;153:329A.
Elgebaly SA, Allam ME, Walzak MPJr, et al. Urinary neutrophil chemotactic factors in interstitial cystitis patients and a rabbit model of bladder inflammation. J Urol. 1992;147:1382-1387.
Elhilali MM, Khaled SM, Kashiwabara T, et al. Sacral neuromodulation: long-term experience of one center. Urology. 2005;65:1114-1117.
Elzawahri A, Bissada NK, Herchorn S, et al. Urinary conduit formation using a retubularized bowel from continent urinary diversion or intestinal augmentations. II. Does it have a role in patients with interstitial cystitis? J Urol. 2004;171:1559-1562.
Emerson LE, Feltis JT. Urodynamic factors affecting response to DMSO in the treatment of interstitial cystitis. J Urol. 1986;135:188A.
Enerback L, Fall M, Aldenborg F. Histamine and mucosal mast cells in interstitial cystitis. Agents Actions. 1989;27:113-116.
Engelmann U, Burger R, Jacobi G. Experimental investigations on the absorption of intravesically instilled mitomycin-C in the urinary bladder of the rat. Eur Urol. 1982;8:176-181.
English SF, Liebert M, Cross CA, McGuire EJ. The incidence of Helicobacter pylori in patients with interstitial cystitis. J Urol. 1998;159:772-773.
Ercan F, Oktay S, Erin N. Role of afferent neurons in stress induced degenerative changes of the bladder. J Urol. 2001;165:235-239.
Erickson DR. Glomerulations in women with urethral sphincter deficiency: report of 2 cases (corrected). J Urol. 1995;153:728-729.
Erickson DR. Interstitial cystitis: update on etiologies and therapeutic options. J Womens Health Gend Based Med. 1999;8:745-758.
Erickson DR. Urine markers of interstitial cystitis. Urology. 2001;57:15-21.
Erickson DR, Belchis DA, Dabbs DJ. Inflammatory cell types and clinical features of interstitial cystitis. J Urol. 1997;158:790-793.
Erickson DR, Kunselman AR, Bentley CM, et al. Is urine methylhistamine a useful marker for interstitial cystitis? J Urol. 2004;172:2256-2260.
Erickson DR, Mast S, Ordille S, Bhavanandan VP. Urinary epitectin (MUC-1 glycoprotein) in the menstrual cycle and interstitial cystitis. J Urol. 1996;156:938-942.
Erickson DR, Morgan KC, Ordille S, et al. Nonbladder related symptoms in patients with interstitial cystitis. J Urol. 2001;166:557-561.
Erickson DR, Ordille S, Martin A, Bhavanandan VP. Urinary chondroitin sulfates, heparan sulfate and total sulfated glycosaminoglycans in interstitial cystitis. J Urol. 1997;157:61-64.
Erickson DR, Schwarze SR, Dixon JK, et al. Differentiation associated changes in gene expression profiles of interstitial cystitis and control urothelial cells. J Urol. 2008;180:2681-2687.
Erickson DR, Sheykhnazari M, Ordille S, Bhavanandan VP. Increased urinary hyaluronic acid and interstitial cystitis. J Urol. 1998;160:1282-1284.
Erickson DR, Tomaszewski JE, Kunselman AR, et al. Do the National Institute of Diabetes and Digestive and Kidney Diseases cystoscopic criteria associate with other clinical and objective features of interstitial cystitis? J Urol. 2005;173:93-97.
Erickson DR, Tomaszewski JE, Kunselman AR, et al. Urine markers do not predict biopsy findings or presence of bladder ulcers in interstitial cystitis/painful bladder syndrome. J Urol. 2008;179:1850-1856.
Erickson DR, Xie SX, Bhavanandan VP, et al. A comparison of multiple urine markers for interstitial cystitis. J Urol. 2002;167:2461-2469.
Evans S, Moalem-Taylor G, Tracey DJ. Pain and endometriosis. Pain. 2007;132(Suppl 1):S22-S25.
Everaert K, Devulder J, De Muynck M, et al. The pain cycle: implications for the diagnosis and treatment of pelvic pain syndromes. Int Urogynecol J. 2001;12:9-14.
Ezzo J, Berman B, Hadhazy V, et al. Is acupuncture effective for the treatment of chronic pain? A systematic review. Pain. 2000;86:217-225.
Fall M. Conservative management of chronic interstitial cystitis: transcutaneous electrical nerve stimulation and transurethral resection. J Urol. 1985;133:774-778.
Fall M. Transcutaneous electrical nerve stimulation in interstitial cystitis: update on clinical experience. Urology. 1987;29:40-42.
Fall M, Baranowski A, Elneil S, et al. European Association of Urology guidelines on chronic pelvic pain. European Association of Urology; 2008. p. 1–99
Fall M, Carlsson CA, Erlandson BE. Electrical stimulation in interstitial cystitis. J Urol. 1980;123:192-195.
Fall M, Johansson SL, Aldenborg F. Chronic interstitial cystitis: a heterogeneous syndrome. J Urol. 1987;137:35-38.
Fall M, Lindstrom S. Transcutaneous electrical nerve stimulation in classic and nonulcer interstitial cystitis. Urol Clin North Am. 1994;21:131-139.
Fall M, Oberpenning F, Peeker R. Treatment of bladder pain syndrome/interstitial cystitis 2008: can we make evidence-based decisions? Eur Urol. 2008;54:65-75.
Fandel T, Tanagho EA. Neuromodulation in voiding dysfunction: a historical overview of neurostimulation and its application. Urol Clin North Am. 2005;32:1-10.
Farkas A, Waisman J, Goodwin WE. Interstitial cystitis in adolescent girls. J Urol. 1977;118:837-839.
Felsen D, Frye S, Trimble LA, et al. Inflammatory mediator profile in urine and bladder wash fluid of patients with interstitial cystitis. J Urol. 1994;152:355-361.
Feltis JT, Perez-Marrero R, Emerson LE. Increased mast cells of the bladder in suspected cases of interstitial cystitis: a possible disease marker. J Urol. 1987;138:42-43.
Fenton BW, Durner C, Fanning J. Frequency and distribution of multiple diagnoses in chronic pelvic pain related to previous abuse or drug-seeking behavior. Gynecol Obstet Invest. 2008;65:247-251.
Filippou AS, Sant GR, Theoharides TC. Mast cell in interstitial cystitis. Urol Integrada Invest. 1999;4:315-323.
Fisher BP, Bavendam TG, Roberts BW, et al. Blinded placebo controlled evaluation on the ingestion of acidic foods and their effect on urinary pH and the symptomatology of interstitial cystitis. Orlando, FL: NIDDK; 1993. p. 53
Fister GM. Similarity of interstitial cystitis (Hunner ulcer) to lupus erythematosus. J Urol. 1938;40:37-51.
FitzGerald MP, Anderson RU, Potts J, et al. Randomized multicenter feasability trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. J Urol. 2009:182.
Fitzgerald M, Brubaker L. Variability of 24-hour voiding diary variables among asymptomatic women. J Urol. 2003;160:207-209.
Fitzgerald M, Butler N, Shott S, Brubaker L. Bother arising from urinary frequency in women. Neurourol Urodyn. 2002;21:36-41.
Fitzgerald MP, Link CL, Litman HJ, et al. Beyond the lower urinary tract: the association of urologic and sexual symptoms with common illnesses. Eur Urol. 2007;52:407-415.
Fitzpatrick CC, DeLancey JO, Elkins TE, McGuire EJ. Vulvar vestibulitis and interstitial cystitis: a disorder of urogenital sinus-derived epithelium? Obstet Gynecol. 1993;81:860-862.
Fleischmann J. Calcium channel antagonists in the treatment of interstitial cystitis. Urol Clin North Am. 1994;21:107-111.
Fleischmann JD, Huntley HN, Shingleton WB, Wentworth DB. Clinical and immunological response to nifedipine for the treatment of interstitial cystitis. J Urol. 1991;146:1235-1239.
Flood HD, Malhotra SJ, O’Connell HE, et al. Long-term results and complications using augmentation cystoplasty in reconstructive urology. Neurourol Urodyn. 1995;14:297-309.
Foreman JC. Peptides and neurogenic inflammation. Br Med Bull. 1987;43:386-400.
Forrest JB, Schmidt S. Interstitial cystitis, chronic nonbacterial prostatitis and chronic pelvic pain syndrome in men: a common and frequently identical clinical entity. J Urol. 2004;172:2561-2562.
Forsell TR, Ruutu M, Isoniemi H, et al. Cyclosporine in severe interstitial cystitis. J Urol. 1996;155:1591.
Foster H, Kreder K, FitzGerald MP, et al. Effect of amitriptyline on symptoms in newly diagnosed patients with interstitial cystitis/painful bladder syndrome. J Urol. 2010;183(5):1853-1858.
Foster H, Smith S, Wheeler M, Weiss RM. Nitric oxide and interstitial cystitis. Adv Urol. 1997;10:1-25.
Fowler JEJr. Prospective study of intravesical dimethyl sulfoxide in treatment of suspected early interstitial cystitis. Urology. 1981;18:21-26.
Fowler JEJr, Lynes WL, Lau JL, et al. Interstitial cystitis is associated with intraurothelial Tamm-Horsfall protein. J Urol. 1988;140:1385-1389.
Franke JJ, Stratton CW, Mitchell WM. Chlamydia pneumoniae in patients with interstitial cystitis. J Urol. 1999;161:29.
Frazer MI, Haylen BT, Sissons M. Do women with idiopathic sensory urgency have early interstitial cystitis? Br J Urol. 1990;66:274-278.
Freedman AI, Wein AJ, Whitmore K, et al. In vitro effects of intravesical dimethyl sulfoxide. Neurourol Urodyn. 1989;8:277-283.
Freiha FS, Faysal MH, Stamey TA. The surgical treatment of intractable interstitial cystitis. J Urol. 1980;123:632-634.
Freiha FS, Stamey TA. Cystolysis: a procedure for the selective denervation of the bladder. Trans Am Assoc Genitourin Surg. 1979;71:50-54.
Freynhagen R, Strojek K, Griesing T, et al. Efficacy of pregabalin in neuropathic pain evaluated in a 12-week, randomised, double-blind, multicentre, placebo-controlled trial of flexible- and fixed-dose regimens. Pain. 2005;115:254-263.
Fritjofsson A, Fall M, Juhlin R, et al. Treatment of ulcer and nonulcer interstitial cystitis with sodium pentosanpolysulfate: a multicenter trial. J Urol. 1987;138:508-512.
Frontz WA. Discussion. Trans Am Assoc Genitourin Surg. 1922;15:434-435.
Furuya R, Masumori N, Furuya S, et al. Glomerulation observed during transurethral resection of the prostate for patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia is a common finding but no predictor of clinical outcome. Urology. 2007;70:922-926.
Gajewski JB, Awad SA. Urodynamic evaluation in interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:169-172.
Galli SJ. New concepts about the mast cell. N Engl J Med. 1993;328:257-265.
Galloway NT, Gabale DR, Irwin PP. Interstitial cystitis or reflex sympathetic dystrophy of the bladder? Semin Urol. 1991;9:148-153.
Gambone J, Mittman B, Munro M, et al. Consensus statement for the management of chronic pelvic pain and endometriosis: proceedings of an expert-panel consensus process. Fertil Steril. 2002;78:961-972.
Geirsson G, Wang YH, Lindstrom S, Fall M. Traditional acupuncture and electrical stimulation of the posterior tibial nerve: a trial in chronic interstitial cystitis. Scand J Urol Nephrol. 1993;27:67-70.
Geist RW, Antolak SJJr. Interstitial cystitis in children. J Urol. 1970;104:922-925.
George NJR. Preface. In: George NJR, Gosling JA, editors. Sensory disorders of the bladder and urethra. Berlin: Springer-Verlag; 1986:vii.
Gheyi SK, Robertson A, Atkinson PM. Severe interstitial cystitis caused by tiaprofenic acid. J R Soc Med. 1999;92:17.
Ghoniem GM, Shaaban AM, Clarke MR. Irritable bladder syndrome in an animal model: a continuous monitoring study. Neurourol Urodyn. 1995;14:657-665.
Giannantoni A, Porena M, Costantini E, et al. Botulinum A toxin intravesical injection in patients with painful bladder syndrome: 1-year followup. J Urol. 2008;179:1031-1034.
Gillenwater JY, Wein AJ. Summary of the National Institute of Arthritis, Diabetes, Digestive and Kidney Diseases Workshop on Interstitial Cystitis, National Institutes of Health, Bethesda, MD, August 28–29, 1987. J Urol. 1988;140:203-206.
Gillespie L. Destruction of the vesicoureteric plexus for the treatment of hypersensitive bladder disorders. Br J Urol. 1994;74:40-43.
Gillespie L, Bray R, Levin N, Delamarter R. Lumbar nerve root compression and interstitial cystitis—response to decompressive surgery. Br J Urol. 1991;68:361-364.
Gilron I, Bailey J, Tu D, et al. Morphine, gabapentin, or their combination for neuropathic pain. N Engl J Med. 2005;352:1324-1334.
Glemain P, Riviere C, Lenormand L, et al. Prolonged hydrodistention of the bladder for symptomatic treatment of interstitial cystitis: efficacy at 6 months and 1 year. Eur Urol. 2002;41:79-84.
Glenning PP. Urinary voiding patterns of apparently normal women. Aust NZ J Obstet Gynaecol. 1985;25:62-65.
Goin JE, Olaleye D, Peters KM, et al. Psychometric analysis of the University of Wisconsin Interstitial Cystitis Scale: implications for use in randomized clinical trials. J Urol. 1998;159:1085-1090.
Golomb J, Klutke CG, Lewin KJ, et al. Bladder neoplasms associated with augmentation cystoplasty: report of 2 cases and literature review. J Urol. 1989;142:377-380.
Gordon HL, Rossen RD, Hersh EM, Yium JJ. Immunologic aspects of interstitial cystitis. J Urol. 1973;109:228-233.
Gordon Z, Parsons CL, Monga M. Intravesical ethanol test: an ineffective measure of bladder hyperpermeability. Urology. 2003;61:555-557.
Goris A, Jan R. Reflex sympathetic dystrophy: model of a severe regional inflammatory response syndrome. World J Surg. 1998;22:197-202.
Gourlay GK. Long-term use of opiods in chronic pain patients with nonterminal disease states. Pain Rev. 1994;1:62-76.
Green M, Filippou A, Sant G, Theoharides TC. Expression of intercellular adhesion molecules in the bladder of patients with interstitial cystitis. Urology. 2004;63:688-693.
Greenhill JP. Sympathectomy and intraspinal alcohol injections for relief of pelvic pain. BMJ. 1947;29:859-862.
Gregoire M, Liandier F, Naud A, et al. Does the potassium stimulation test predict cystometric, cystoscopic outcome in interstitial cystitis? J Urol. 2002;168:556-557.
Gupta G, Lu S, Gold M, Chai T. Bladder urothelial cells from patients with interstitial cystitis have an increased sensitivity to carbachol. Neurourol Urodyn. 2009;28(8):1022-1027.
Haarala M, Jalava J, Laato M, et al. Absence of bacterial DNA in the bladder of patients with interstitial cystitis. J Urol. 1996;156:1843-1845.
Haarala M, Kiiholma P, Nurmi M, et al. The role of Borrelia burgdorferi in interstitial cystitis. Eur Urol. 2000;37:395-399.
Hakenberg O, Wirth M. Chronic pelvic pain in men. Urol Int. 2002;68:138-143.
Hald T, Barnard RJ, Holm-Bentzen M. Treatment of interstitial cystitis. In: George NJR, Gosling JA, editors. Sensory disorders of the bladder and urethra. Berlin: Springer-Verlag; 1986:73-78.
Hall SA, Link CL, Pulliam SJ, et al. The relationship of common medical conditions and medication use with symptoms of painful bladder syndrome: results from the Boston area community health survey. J Urol. 2008;180:593-598.
Hamer AJ, Nicholson S, Padfield CJ. Spontaneous rupture of the bladder in interstitial cystitis. Br J Urol. 1992;69:102.
Hampson SJ, Christmas TJ, Moss MT. Search for mycobacteria in interstitial cystitis using mycobacteria-specific DNA probes with signal amplification by polymerase chain reaction. Br J Urol. 1993;72:303-306.
Hampson SJ, Woodhouse CRJ. Sodium pentosanpolysulphate in the management of haemorrhagic cystitis: experience with 14 patients. Eur Urol. 1994;25:40-42.
Hanash KA, Pool TL. Interstitial cystitis in men. J Urol. 1969;102:427-428.
Hanash KA, Pool TL. Interstitial and hemorrhagic cystitis: viral, bacterial and fungal studies. J Urol. 1970;104:705-706.
Hand JR. Interstitial cystitis: report of 223 cases (204 women and 19 men). J Urol. 1949;61:291-310.
Hanno PM. Amitriptyline in the treatment of interstitial cystitis. Urol Clin North Am. 1994;21:89-91.
Hanno PM. Diagnosis of interstitial cystitis. Urol Clin North Am. 1994;21:63-66.
Hanno PM. Analysis of long-term Elmiron therapy for interstitial cystitis. Urology. 1997;49:93-99.
Hanno PM. Interstitial cystitis/painful bladder syndrome/bladder pain syndrome: the evolution of a new paradigm. In: Proceedings of the International Consultation on Interstitial Cystitis. Japan: Comfortable Urology Network; 2008:2-9.
Hanno PM, Baranowski A, Fall M, et al. Painful bladder syndrome (including interstitial cystitis). In: Abrams PH, Wein AJ, Cardozo L, editors. Incontinence. Paris: Health Publications Limited; 2005:1456-1520.
Hanno PM, Buehler J, Wein AJ. Use of amitriptyline in the treatment of interstitial cystitis. J Urol. 1989;141:846-848.
Hanno PM, Dmochowski R. Status of international consensus on interstitial cystitis/bladder pain syndrome/painful bladder syndrome: 2008 snapshot. Neurourol Urodyn. 2009;28(4):274-286.
Hanno PM, Fritz R, Wein AJ. Heparin as an antibacterial agent in rabbit bladder. Urology. 1978;12:411-415.
Hanno PM, Keay S, Moldwin R, van Ophoven A. International Consultation on IC—Rome, September 2004/Forging an International Consensus: progress in painful bladder syndrome/interstitial cystitis. Report and abstracts. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(Suppl 1):S2-34.
Hanno PM, Landis JR, Matthews-Cook Y, Kusek J, et al. Interstitial cystitis: issues of definition. Urol Integr Invest. 1999;4:291-295.
Hanno PM, Landis JR, Matthews-Cook Y, et al. The diagnosis of interstitial cystitis revisited: lessons learned from the National Institutes of Health Interstitial Cystitis Database study. J Urol. 1999;161:553-557.
Hanno PM, Levin RM, Monson FC, et al. Diagnosis of interstitial cystitis. J Urol. 1990;143:278-281.
Hanno PM, Lin AT, Nordling J, et al. Bladder pain syndrome. In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence. Paris, France: Health Publication Ltd; 2009:1459-1518.
Hanno PM, Tomaszewski JE. Bladder carcinoma after urinary diversion. JAMA. 1982;248:2885.
Hanno PM, Wein AJ. Medical treatment of interstitial cystitis (other than Rimso-50/Elmiron). Urology. 1987;29:22-26.
Hanno PM, Wein AJ. Conservative therapy of interstitial cystitis. Semin Urol. 1991;9:143-147.
Hanus T, Zamecnik L, Jansky M, et al. The comparison of clinical and histopathologic features of interstitial cystitis. Urology. 2001;57:131.
Haq A, Morsy M, Webb RJ. A study to detect Helicobacter pylori in fresh and archival specimens from patients with interstitial cystitis, using amplification methods. BJU Int. 2004;93:423.
Harn SD, Keutel HJ, Weaver RG. Immunologic and histologic evaluation of the urinary bladder wall after group A streptococcal infection. Invest Urol. 1973;11:55-64.
Harrington DS, Fall M, Johansson SL. Interstitial cystitis: bladder mucosa lymphocyte immunophenotyping and peripheral blood flow cytometry analysis. J Urol. 1990;144:868-871.
Harrison SCW, Ferguson DR, Hanley MR. Effect of capsaicin on the rabbit urinary bladder. What is the function of sensory nerves that contain substance P? Br J Urol. 1990;66:155-161.
Hauser PJ, Dozmorov MG, Bane BL, et al. Abnormal expression of differentiation related proteins and proteoglycan core proteins in the urothelium of patients with interstitial cystitis. J Urol. 2008;179:764-769.
Haylen BT, Chetty N, Logan V, et al. Is sensory urgency part of the same spectrum of bladder dysfunction as detrusor overactivity? Int Urogynecol. 2007;18:123-128.
Hedelin HH, Mardh PA, Brorson JE, et al. Mycoplasma hominis and interstitial cystitis. Sex Transm Dis. 1983;10:327-330.
Held PJ, Hanno PM, Wein AJ. Epidemiology of interstitial cystitis: 2. In: Hanno PM, Staskin DR, Krane RJ, Wein AJ, editors. Interstitial cystitis. London: Springer-Verlag; 1990:29-48.
Hellstrom HR, Davis BK, Shonnard JW. Eosinophilic cystitis: a study of 16 cases. Am J Clin Pathol. 1979;72:777-784.
Herbst RH, Baumrucker GO, German KL. Elusive ulcer (Hunner) of the bladder with an experimental study of the etiology. Am J Surg. 1937;38:152-167.
Heritz DM, Lacroix JM, Batra SD, et al. Detection of eubacteria in interstitial cystitis by 16S rDNA amplification. J Urol. 1997;158:2291-2295.
Hill JR, Isom-Batz G, Panagopoulos G, et al. Patient perceived outcomes of treatments used for interstitial cystitis. Urology. 2008;71:62-66.
Hofmeister MA, He F, Ratliff TL, et al. Mast cells and nerve fibers in interstitial cystitis (IC): an algorithm for histologic diagnosis via quantitative image analysis and morphometry (QIAM). Urology. 1997;49:41-47.
Hohenfellner M, Nunes L, Schmidt RA, et al. Interstitial cystitis: increased sympathetic innervation and related neuropeptide synthesis. J Urol. 1992;147:587-591.
Hohlbrugger G. Disintegrity of the vesical blood-urine barrier in interstitial cystitis: a vicious circle. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:87-92.
Hohlbrugger G. Urinary potassium and the overactive bladder. BJU Int. 1999;83:22-28.
Hohlbrugger G, Frauscher F, Strasser H, et al. Topical heparin therapy normalizes urothelial permeability and vesical blood flow in urgency/frequency syndrome, urge incontinence and reversible interstitial cystitis. Eur Urol. 1998;33:A38.
Hohlbrugger G, Riedl C. Non-bacterial cystitis. Curr Opin Urol. 2000;10:371-380.
Holm-Bentzen M. Pathology and pathophysiology of painful bladder diseases. Urol Int. 1989;44:327-331.
Holm-Bentzen M, Jacobsen F, Nerstrom B, et al. A prospective double-blind clinically controlled multicenter trial of sodium pentosanpolysulfate in the treatment of interstitial cystitis and related painful bladder disease. J Urol. 1987;138:503-507.
Holm-Bentzen M, Jacobsen F, Nerstrom B, et al. Painful bladder disease: clinical and pathoanatomical differences in 115 patients. J Urol. 1987;138:500-502.
Holm-Bentzen M, Larsen S, Hainau B, et al. Nonobstructive detrusor myopathy in a group of patients with chronic abacterial cystitis. Scand J Urol Nephrol. 1985;19:21-26.
Holm-Bentzen M, Nordling J, Hald T. Etiology: etiologic and pathogenetic theories in interstitial cystitis. In: Hanno PM, Staskin DR, Krane RJ, Wein AJ, editors. Interstitial cystitis. London: Springer-Verlag; 1990:63-77.
Holm-Bentzen M, Sondergaard I, Hald T. Urinary excretion of a metabolite of histamine (1,4-methyl-imidazole-acetic-acid) in painful bladder disease. Br J Urol. 1987;59:230-233.
Holzberg A, Kellog-Spadt S, Lukban J, Whitmore K. Evaluation of transvaginal theile massage as a therapeutic intervention for women with interstitial cystitis. Urology. 2001;57:120.
Homma Y. Lower urinary tract symptomatology: its definition and confusion. Int J Urol. 2008;15:35-43.
Hosseini A, Ehren I, Wiklund NP. Nitric oxide as an objective marker for evaluation of treatment response in patients with classic interstitial cystitis. J Urol. 2004;172:2261-2265.
Houpt KA. Housesoiling: Treatment of a common feline problem. Vet Med. 1991;86:1000-1006.
Howard FM. Chronic pelvic pain. Obstet Gynecol. 2003;101:594-611.
Howard FM. The role of laparoscopy in the chronic pelvic pain patient. Clin Obstet Gynecol. 2003;46:749-766.
Hughes OD, Kynaston HG, Jenkins BJ, et al. Substitution cystoplasty for intractable interstitial cystitis. Br J Urol. 1995;76:172-174.
Hukkanen V, Haarala M, Nurmi M, et al. Viruses and interstitial cystitis: adenovirus genomes cannot be demonstrated in urinary bladder biopsies. Urol Res. 1996;24:235-238.
Hunner GL. A rare type of bladder ulcer in women; report of cases. Boston Med Surg J. 1915;172:660-664.
Hunner GL. A rare type of bladder ulcer: further notes, with a report of eighteen cases. 1918. p. 203–12.
Hurst R. A deficit of proteoglycans on the bladder uroepithelium in interstitial cystitis. Eur Urol. 2003;2(Suppl):10-13.
Hurst RE, Parsons CL, Roy JB, Young JL. Urinary glycosaminoglycan excretion as a laboratory marker in the diagnosis of interstitial cystitis. J Urol. 1993;149:31-35.
Hurst RE, Roy JB, Min KW, et al. A deficit of chondroitin sulfate proteoglycans on the bladder uroepithelium in interstitial cystitis. Urology. 1996;48:817-821.
Hurst RE, Roy JB, Parsons CL. The role of glycosaminoglycans in normal bladder physiology and the pathophysiology of interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:93-100.
Iavazzo C, Athanasiou S, Pitsouni E, Falagas ME. Hyaluronic acid: an effective alternative treatment of interstitial cystitis, recurrent urinary tract infections, and hemorrhagic cystitis? Eur Urol. 2007;51(6):1534-1540.
Ikeda Y, Birder L, Buffington C, et al. Mucosal muscarinic receptors enhance bladder activity in cats with feline interstitial cystitis. J Urol. 2009;181:1415-1422.
Ingber MS, Peters KM, Killinger KA, et al. Dilemmas in diagnosing pelvic pain: multiple pelvic surgeries common in women with interstitial cystitis. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:341-345.
Inoue Y, Mita K, Kakehashi M, et al. Prevalence of painful bladder syndrome (PBS) symptoms in adult women in the general population in Japan. Neurourol Urodyn. 2009;28:214-218.
Interstitial Cystitis Association. Bioniche trial. 2003.
Irwin P, Galloway NT. Impaired bladder perfusion in interstitial cystitis: a study of blood supply using laser Doppler flowmetry. J Urol. 1993;149:890-892.
Irwin P, Galloway NT. Re: Pelvic pain without pelvic organs [letter]. J Urol. 1992;148:1265-1266.
Irwin PP, Galloway NT. Surgical management of interstitial cystitis. Urol Clin North Am. 1994;21:145-151.
Irwin PP, Hammonds WD, Galloway NT. Lumbar epidural blockade for management of pain in interstitial cystitis. Br J Urol. 1993;71:413-416.
Ito T, Miki M, Yamada T. Interstitial cystitis in Japan. BJU Int. 2000;86:634-637.
Ito T, Stein PC, Parsons CL, Schmidt JD. Elevated stress protein in transitional cells exposed to urine from interstitial cystitis patients. Int J Urol. 1998;5:444-448.
Ito T, Tomoe H, Ueda T, et al. Clinical symptoms scale for interstitial cystitis for diagnosis and for following the course of the disease. Int J Urol. 2003;10(Suppl):S24-S26.
Jacob J, Ludgate CM, Forde J, et al. Recent observations on the ultrastructure of human urothelilum. Cell Tiss Res. 1978;193:543-560.
Jacobo E, Stamler FW, Culp DA. Interstitial cystitis followed by total cystectomy. Urology. 1974;3:481-485.
Janicki T. Chronic pelvic pain as a form of complex regional pain syndrome. Clin Obstet Gynecol. 2003;46:797-803.
Jasmin L, Janni G, Manz HJ, Rabkin SD. Activation of CNS circuits produing a neurogenic cystitis: evidence for centrally induced peripheral inflammation. J Neurosci. 1998;18:10016-10029.
Jepsen JV, Sall M, Rhodes PR, et al. Long-term experience with pentosanpolysulfate in interstitial cystitis. Urology. 1998;51:381-387.
Johansson SL, Fall M. Clinical features and spectrum of light microscopic changes in interstitial cystitis. J Urol. 1990;143:1118-1124.
Johansson SL, Fall M. Pathology of interstitial cystitis. Urol Clin North Am. 1994;21:55-62.
Johansson SL, Ogawa K, Fall M. The pathology of interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:143-152.
Jokinen EJ, Alfthan OS, Oravisto KJ. Antitissue antibodies in interstitial cystitis. Clin Exp Immunol. 1972;11:333-339.
Jokinen EJ, Lassus A, Salo OP, Alfthan O. Discoid lupus erythematosus and interstitial cystitis. The presence of bound immunoglobulins in the bladder mucosa. Ann Clin Res. 1972;4:23-25.
Jokinen EJ, Oravisto KJ, Alfthan OS. The effect of cystectomy on antitissue antibodies in interstitial cystitis. Clin Exp Immunol. 1973;15:457-460.
Jones CA, Nyberg L. Epidemiology of interstitial cystitis. Urology. 1997;49:2-9.
Kang J, Wein AJ, Levin RM. Bladder functional recovery following acute overdistention. Neurourol Urodyn. 1992;11:253-260.
Kaplan AP, Haak-Frendscho M, Fuci A, et al. A histamine-releasing factor from activated human mononuclear cells. J Immunol. 1985;135:2027-2032.
Kaplan SA, Ikeguchi EF, Santarosa RP, et al. Etiology of voiding dysfunction in men less than 50 years of age. Urology. 1996;47:836-839.
Kastrup J, Hald T, Larsen S, Nielsen VG. Histamine content and mast cell count of detrusor muscle in patients with interstitial cystitis and other types of chronic cystitis. Br J Urol. 1983;55:495-500.
Katske F, Shoskes DA, Sender M, et al. Treatment of interstitial cystitis with a quercetin supplement. Tech Urol. 2001;7:44-46.
Kau AL, Hunstad DA, Hultgren SJ. Interaction of uropathogenic Escherichia coli with host uroepithelium. Curr Opin Microbiol. 2005;8:54-59.
Keay S. Cell signaling in interstitial cystitis/painful bladder syndrome. Cell Signal. 2008;20:2174-2179.
Keay S, Kleinberg M, Zhang CO, et al. Bladder epithelial cells from patients with interstitial cystitis produce an inhibitor of heparin-binding epidermal growth factor-like growth factor production. J Urol. 2000;164:2112-2118.
Keay S, Seillier-Moiseiwitsch F, Zhang CO, et al. Changes in human bladder epithelial cell gene expression associated with interstitial cystitis or antiproliferative factor treatment. Physiol Genom. 2003;14:107-115.
Keay S, Szekely Z, Conrads TP, et al. An antiproliferative factor from interstitial cystitis patients is a frizzled 8 protein-related sialoglycopeptide. Proc Natl Acad Sci U S A. 2004;101:11803-11808.
Keay S, Warren JW. A hypothesis for the etiology of interstitial cystitis based upon inhibition of bladder epithelial repair. Med Hypotheses. 1998;51:79-83.
Keay S, Warren JW, Zhang CO, et al. Antiproliferative activity is present in bladder but not renal pelvic urine from interstitial cystitis patients. J Urol. 1999;162:1487-1489.
Keay S, Zhang CO, Baldwin BR, et al. Polymerase chain reaction amplification of bacterial 16S rRNA genes in interstitial cystitis and control patient bladder biopsies. J Urol. 1998;159:280-283.
Keay S, Zhang CO, Chai T, et al. Antiproliferative factor, heparin-binding epidermal growth factor-like growth factor, and epidermal growth factor in men with interstitial cystitis versus chronic pelvic pain syndrome. Urology. 2004;63:22-26.
Keay S, Zhang CO, Hise MK, et al. A diagnostic in vitro urine assay for interstitial cystitis. Urology. 1998;52:974-978.
Keay S, Zhang CO, Shoenfelt JL, Chai TC. Decreased in vitro proliferation of bladder epithelial cells from patients with interstitial cystitis. Urology. 2003;61:1278-1284.
Keay SK, Zhang CO, Shoenfelt J, et al. Sensitivity and specificity of antiproliferative factor, heparin-binding epidermal growth factor-like growth factor, and epidermal growth factor as urine markers for interstitial cystitis. Urology. 2001;57:9-14.
Keay S, Zhang CO, Trifillis AL, et al. Decreased 3H-thymidine incorporation by human bladder epithelial cells following exposure to urine from interstitial cystitis patients. J Urol. 1996;156:2073-2078.
Keller ML, McCarthy DO, Neider RS. Measurement of symptoms of interstitial cystitis: a pilot study. Urol Clin North Am. 1994;21:67-71.
Kelly JD, Young MR, Johnston SR, Keane PF. Clinical response to an oral prostaglandin analogue in patients with interstitial cystitis. Eur Urol. 1998;34:53-56.
Kennelly MJ, Konnak JW. Intravesical cromolyn sodium for treatment of interstitial cystitis—a double-blind placebo controlled pilot study. Bethesda, MD: NIDDK; 1995. p. 64
Kerr WSJr. Interstitial cystitis: treatment by transurethral resection. J Urol. 1971;105:664-666.
Keselman I, Austin P, Anderson J, et al. Cystectomy and urethrectomy for disabling interstitial cystitis: a long-term follow up. J Urol. 1995;153:290A.
Khanna OP, Loose JH. Interstitial cystitis treated with intravesical doxorubicin. Urology. 1990;36:139-142.
Khoury JM, Timmons SL, Corbel L, et al. Complications of enterocystoplasty. Urology. 1992;40:9-13.
Kim J, Keay SK, Dimitrakov JD, Freeman MR. p53 mediates interstitial cystitis antiproliferative factor (APF)-induced growth inhibition of human urothelial cells. FEBS Lett. 2007;581:3795-3799.
Kim J, Keay SK, Freeman MR. Heparin-binding epidermal growth factor-like growth factor functionally antagonizes interstitial cystitis antiproliferative factor via mitogen-activated protein kinase pathway activation. BJU Int. 2009;103:541-546.
Kim S, Kim T, Kim S, Oh S. Urodynamic findings of the painful bladder syndrome/interstitial cystitis: a comparison with idiopathic overactive bladder. J Urol. 2009;181:2550-2554.
Kim YS, Levin RM, Wein AJ, Longhurst PA. Effects of sensitization on the permeability of urothelium in guinea pig urinary bladder. J Urol. 1992;147:270-273.
Kirkemo A, Peabody M, Diokno AC, et al. Associations among urodynamic findings and symptoms in women enrolled in the Interstitial Cystitis Data Base (ICDB) Study. Urology. 1997;49:76-80.
Kirkemo AK, Miles BJ, Peters JM. Use of amitriptyline in the treatment of interstitial cystitis. J Urol. 1990;143:279A.
Kirkengen AL, Ulvestad E. [Heavy burdens and complex disease—an integrated perspective. Tidsskr Nor Laegeforen. 2007;127:3228-3231. [in Norwegian]
Kisman OK, Nijeholt AA, van Krieken JH. Mast cell infiltration in intestine used for bladder augmentation in interstitial cystitis. J Urol. 1991;146:1113-1114.
Klumpp DJ, Rudick CN. Summation model of pelvic pain in interstitial cystitis. Nat Clin Pract Urol. 2008;5:494-500.
Klutke CG, Bullock AD, Ratliff TL. Experimental autoimmune cystitis (EAC): an autoimmune model for interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:33-46.
Kochakarn W, Lertsithichai P, Pummangura W. Bladder substitution by ileal neobladder for women with interstitial cystitis. Int Braz J Urol. 2007;33:486-492.
Koff SA, Byard MA. The daytime urinary frequency syndrome of childhood. J Urol. 1988;140:1280-1281.
Kohli N, Sze EHM, Karram MM. Gynecologic aspects of interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:153-164.
Kohn IJ, Filer-Maerten S, Whitmore KE, et al. Lack of effect following repeated in vivo exposure of the rabbit urinary bladder to urine from interstitial cystitis patients at low infusion volumes. Neurourol Urodyn. 1998;17:147-152.
Kontras SB, Bodenbender JG, McClave CR, Smith JP. Interstitial cystitis in chronic granulomatous disease. J Urol. 1971;105:575-578.
Korting GE, Smith SD, Wheeler MA, et al. A randomized double-blind trial of oral L-arginine for treatment of interstitial cystitis. J Urol. 1999;161:558-565.
Koskela LR, Thiel T, Ehren I, et al. Localization and expression of inducible nitric oxide synthase in biopsies from patients with interstitial cystitis. J Urol. 2008;180:737-741.
Koziol JA. Epidemiology of interstitial cystitis. Urol Clin North Am. 1994;21:7-20.
Koziol JA, Clark DC, Gittes RF, Tan EM. The natural history of interstitial cystitis: a survey of 374 patients. J Urol. 1993;149:465-469.
Kruger JM, Osborne CA, Goyal SM, et al. Clinical evaluation of cats with lower urinary tract disease. J Am Vet Med Assoc. 1991;199:211-216.
Kumar V, Chapple CR, Surprenant AM, Chess-Williams R. Enhanced adenosine triphosphate release from the urothelium of patients with painful bladder syndrome: a possible pathophysiological explanation. J Urol. 2007;178:1533-1536.
Kuo HC. Urodynamic results of intravesical heparin therapy for women with frequency urgency syndrome and interstitial cystitis. J Formos Med Assoc. 2001;100:309-314.
Kuo HC. Urodynamic study and potassium sensitivity test for women with frequency-urgency syndrome and interstitial cystitis. Urol Int. 2003;71:61-65.
Kushner L, Moldwin RM. Efficiency of questionnaires used to screen for interstitial cystitis. J Urol. 2006;176:587-592.
Lagunoff FD, Martin TW, Read G. Agents that release histamine from mast cells. Ann Rev Pharmacol Toxicol. 1983;23:331-351.
Lamm DL, Gittes RF. Inflammatory carcinoma of the bladder and interstitial cystitis. J Urol. 1977;117:49-51.
Lane DA, Adams L. Non-anticoagulant uses of heparin. N Engl J Med. 1993;329:129-130.
LaRock DR, Sant GR. Intravesical clorpactin for refractory interstitial cystitis. Infect Urol. 1995; Sept/Oct:151-157.
Larsen MS, Mortensen S, Nordling J, Horn T. Quantifying mast cells in bladder pain syndrome by immunohistochemical analysis. BJU Int. 2008.
Larsen S, Thompson SA, Hald T, et al. Mast cells in interstitial cystitis. Br J Urol. 1982;54:283-286.
Lasanen LT, Tammela TL, Kallioinen M, Waris T. Effect of acute distension on cholinergic innervation of the rat urinary bladder. Urol Res. 1992;20:59-62.
Lavelle JP, Apodaca G, Meyers SA, et al. Disruption of guinea pig urinary bladder permeabliity barrier in noninfectious cystitis. Am J Physiol. 1998;274:F205-F214.
Lavelle JP, Meyers SA, Ruiz WG, et al. Urothelial pathophysiological changes in feline interstitial cystitis: a human model. Am J Physiol Renal Physiol. 2000;278:F540-F553.
Lavelle JP, Yoshiyama M, Doty DA, et al. Capsaicin antagonizes elevated urothelial permeability in rat bladder induced by pelvic nerve stimulation. J Urol. 1999;161S:25.
Lazzeri M, Beneforti P, Benaim G, et al. Intravesical capsaicin for treatment of severe bladder pain: a randomized placebo controlled study. J Urol. 1996;156:947-952.
Lazzeri M, Beneforti P, Turini D, et al. Single dose of intravesical resiniferatoxin for the treatment of interstitial cystitis—preliminary results of a randomised controlled study. J Urol. 2000;163S:60.
Lepinard V, Saint-Andre JP, Rognon LM. [Interstitial cystitis: current aspects]. J Urol (Paris). 1984;90:455-465. [in French]
Leppilahti M, Sairanen J, Tammela TL, et al. Prevalence of clinically confirmed interstitial cystitis in women: a population-based study in Finland. J Urol. 2005;174:581-583.
Leppilahti M, Tammela TL, Huhtala H, Auvinen A. Prevalence of symptoms related to interstitial cystitis in women: a population-based study in Finland. J Urol. 2002;168:139-143.
Leppilahti M, Tammela TL, Huhtala H, et al. Interstitial cystitis-like urinary symptoms among patients with Sjogren’s syndrome: a population-based study in Finland. Am J Med. 2003;115:62-65.
Letourneau R, Pang X, Sant GR, Theoharides TC. Intragranular activation of bladder mast cells and their association with nerve processes in interstitial cystitis. Br J Urol. 1996;77:41-54.
Levander H. [Sensory sensitization, part II: Pathophysiology in dysfunctional disorders: understanding the inner life of the nerve pathways may explain hitherto unexplainable symptoms]. Lakartidningen. 2003;100:1622-1624. [in Swedish]
Levin RM, Lavkar RM, Monson FC, et al. Effect of chronic nitrofurantoin on the rabbit urinary bladder. J Urol. 1988;139:400-404.
Lewi H. Medical therapy in interstitial cystitis: the Essex experience. Urology. 2001;57(6 Suppl 1):120.
Lewi HJ. Cimetidine in the treatment of interstitial cystitis. Br J Urol. 1996;77:28.
Li J, Micevych P, McDonald J, et al. Inflammation in the uterus induces phosphorylated extracellular signal-regulated kinase and substance P immunoreactivity in dorsal root ganglia neurons innervating both uterus and colon in rats. J Neurosci Res. 2008;86(12):2746-2752.
Liebert M. Bladder cell acitvation and mucosal immunity in interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:117-122.
Liebert M, Wedemeyer G, Stein JA, et al. Evidence for urothelial cell activation in interstitial cystitis. J Urol. 1993;149:470-475.
Lilius HG, Oravisto KJ, Valtonen EJ. Origin of pain in interstitial cystitis: effect of ultrasound treatment on the concomitant levator ani spasm syndrome. Scand J Urol Nephrol. 1973;7:150-152.
Lilly JD, Parsons CL. Bladder surface glycosaminoglycans is a human epithelial permeability barrier. Surg Gynecol Obstet. 1990;171:493-496.
Ling FW. Randomized controlled trial of depot leuprolide in patients with chronic pelvic pain and clinically suspected endometriosis. Pelvic Pain Study Group. Obstet Gynecol. 1999;93:51-58.
Link CL, Lutfey K. Is abuse causally related to urologic symptoms? Results from the Boston Area Community Health Survey. Eur Urol. 2007;52:397-406.
Link CL, Pulliam SJ, Hanno PM, et al. Prevalence and psychosocial correlates of symptoms suggestive of painful bladder syndrome: results from the Boston Area Community Health Survey. J Urol. 2008;180:599-606.
Linn JF, Hohenfellner M, Roth S, et al. Treatment of interstitial cystitis: comparison of subtrigonal and supratrigonal cystectomy combined with orthotopic bladder substitution. J Urol. 1998;159:774-778.
Littleton RH, Farah RN, Cerny JC. Eosinophilic cystitis: an uncommon form of cystitis. J Urol. 1982;127:132-133.
Liu HT, Tyagi P, Chancellor MB, Kuo HC. Urinary nerve growth factor level is increased in patients with interstitial cystitis/bladder pain syndrome and decreased in responders to treatment. BJU Int. 2009;104(10):1476-1481.
Liu YK, Harty JI, Steinbock GS, et al. Treatment of radiation- or cyclophosphamide-induced hemorrhagic cystitis using conjugated estrogen. J Urol. 1990;144:41-43.
Lloyd LK. Surgical treatment of interstitial cystitis. AUA News. 1999; September/October:12.
Logadottir YR, Ehren I, Fall M, et al. Intravesical nitric oxide production discriminates between classic and nonulcer interstitial cystitis. J Urol. 2004;171:1148-1150.
Lose G, Frandsen B, Hojensgard JC, et al. Chronic interstitial cystitis: increased levels of eosinophil cationic protein in serum and urine and an ameliorating effect of subcutaneous heparin. Scand J Urol Nephrol. 1983;17:159-161.
Lose G, Frandsen B, Holm-Bentzen M, et al. Urine eosinophil cationic protein in painful bladder disease. Br J Urol. 1987;60:39-42.
Lose G, Jespersen J, Frandsen B, et al. Subcutaneous heparin in the treatment of interstitial cystitis. Scand J Urol Nephrol. 1985;19:27-29.
Lotenfoe RR, Christie J, Parsons A, et al. Absence of neuropathic pelvic pain and favorable psychological profile in the surgical selection of patients with disabling interstitial cystitis. J Urol. 1995;154:2039-2042.
Lotz M, Villiger P, Hugli T, et al. Interleukin-6 and interstitial cystitis. J Urol. 1994;152:869-873.
Low PA, Dotson RM. Symptomatic treatment of painful neuropathy. JAMA. 1998;280:1863-1864.
Lowe EM, Anand P, Terenghi G, et al. Increased nerve growth factor levels in the urinary bladder of women with idiopathic sensory urgency and interstitial cystitis. Br J Urol. 1997;79:572-577.
Lubeck DP, Whitmore K, Sant GR, et al. Psychometric validation of the O’Leary-Sant interstitial cystitis symptom index in a clinical trial of pentosan polysulfate sodium. Urology. 2001;57:62-66.
Luber-Narod J, Austin-Ritchie T, Hollins CIII, et al. Role of substance P in several models of bladder inflammation. Urol Res. 1997;25:395-399.
Lucioni A, Bales GT, Lotan TL, et al. Botulinum toxin type A inhibits sensory neuropeptide release in rat bladder models of acute injury and chronic inflammation. BJU Int. 2008;101:366-370.
Lukban J, Whitmore K, Kellogg-Spadt S, et al. The effect of manual physical therapy in patients diagnosed with interstitial cystitis, high-tone pelvic floor dysfunction, and sacroiliac dysfunction. Urology. 2001;57:121-122.
Lundberg JO, Ehren I, Jansson O, et al. Elevated nitric oxide in the urinary bladder in infectious and noninfectious cystitis. Urology. 1996;48:700-702.
Lundeberg T, Liedberg H, Nordling L, et al. Interstitial cystitis: correlation with nerve fibres, mast cells and histamine. Br J Urol. 1993;71:427-429.
Lunghi F, Nicita G, Selli C, et al. Clinical aspects of augmentation enterocystoplasties. Eur Urol. 1984;10:159-163.
Luo Y. A potential modality for interstitial cystitis: intravesical use of anti-inflammatory peptide RDP58. J Urol. 2005;173:340.
Lutgendorf SK, Kreder KJ. Central and peripheral mechanisms in interstitial symptoms. J Urol. 2005;173:682.
Lutgendorf SK, Kreder KJ, Rothrock NE, et al. Stress and symptomatology in patients with interstitial cystitis: a laboratory stress model. J Urol. 2000;164:1265-1269.
Lutgendorf SK, Kreder KJ, Rothrock NE, et al. Diurnal cortisol variations and symptoms in patients with interstitial cystitis. J Urol. 2002;167:1338-1343.
Lutgendorf SK, Latini JM, Rothrock N, et al. Autonomic response to stress in interstitial cystitis. J Urol. 2004;172:227-231.
Lynes WL, Flynn SD, Shortliffe LD, et al. Mast cell involvement in interstitial cystitis. J Urol. 1987;138:746-752.
Lynes WL, Flynn SD, Shortliffe LD, Stamey TA. The histology of interstitial cystitis. Am J Surg Pathol. 1990;14:969-976.
Lynes WL, Shortliffe LD, Stamey TA. Urinary myotropic substances in interstitial cystitis. Journal of Urology. 1990;143:373A.
Lynn RB, Friedman LS. Irritable bowel syndrome. N Engl J Med. 1993;329:1940-1945.
MacDermott JP, Charpied GC, Tesluk H, Stone AR. Can histological assessment predict the outcome in interstitial cystitis? Br J Urol. 1991;67:44-47.
MacDermott JP, Charpied GL, Tesluk H, Stone AR. Recurrent interstitial cystitis following cystoplasty: fact or fiction? J Urol. 1990;144:37-40.
MacDermott JP, Miller CH, Levy N, Stone AR. Cellular immunity in interstitial cystitis. J Urol. 1991;145:274-278.
Makela M, Heliovaara M. Prevalence of primary fibromyalgia in the Finnish population. BMJ. 1991;303:216-219.
Malykhina AP. Neural mechanisms of pelvic organ cross-sensitization. Neuroscience. 2007;149:660-672.
Marinoff SC, Turner MLC. Vulvar vestibulitis syndrome: an overview. J Obstet Gynecol. 1991;165:1228-1234.
Markwell SJ. Physical therapy managment of pelvi/perineal and perianal syndromes. World J Urol. 2001;19:194-199.
Martins SM, Darlin DJ, Lad PM, Zimmern PE. Interleukin-1B: a clinically relevant urinary marker. J Urol. 1994;151:1198-1201.
Marx CM, Alpert SE. Ticarcillin-induced cystitis. Am J Dis Child. 1984;138:670-672.
Maskell R. Broadening the concept of urinary tract infection. Br J Urol. 1995;76:2-8.
Mattila J. Vascular immunopathology in interstitial cystitis. Clin Immunol Immunopathol. 1982;23:648-655.
Mattila J, Harmoinen A, Hallstrom O. Serum immunoglobulin and complement alterations in interstitial cystitis. Eur Urol. 1983;9:350-352.
Mattila J, Linder E. Immunoglobulin deposits in bladder epithelium and vessels in interstitial cystitis: possible relationship to circulating anti-intermediate filament autoantibodies. Clin Immunol Immunopathol. 1984;32:81-89.
Maxwell KM, Clemens JQ, Mazzenga L, Kielb SJ. Reprogramming requirements after sacral nerve stimulator implantation: correlation with preoperative indication. J Urol. 2008;179:549-551.
Mayer EA, Bushnell M. Functional pain disorders: time for a paradigm shift. In: Mayer EA, Bushnell CD, editors. Functional pain syndromes: presentation and pathophysiology. Seattle: IASP Press; 2009:531-565.
Mayer R, Propert KJ, Peters KM, et al. A randomized controlled trial of intravesical bacillus Calmette-Guérin for treatment refractory interstitial cystitis. J Urol. 2005;173:1186-1191.
McCahy PJ, Styles RA. Prolonged bladder distension: experience in the treatment of detrusor overactivity and interstitial cystitis. Eur Urol. 1995;28:325-327.
McCormack WM. Two urogenital sinus syndromes: interstitial cystitis and focal vulvitis. J Reprod Med. 1990;35:873-876.
McDougald M, Landon CR. The diagnosis of interstitial cystitis: is histology helpful? Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(Suppl 1):S40-S41.
McGuire EJ, Lytton B, Cornog JLJr. Interstitial cystitis following colocystoplasty. Urology. 1973;2:28-29.
McGuire EJ, Shi-chun Z, Horwinski ER, et al. Treatment of motor and sensory detrusor instability by electrical stimulation. J Urol. 1983;129:78-79.
McInerney PD, Vanner TF, Matenhelia S, Stephenson TP. Assessment of the long-term results of subtrigonal phenolisation. Br J Urol. 1991;67:586-587.
McQuay HJ. Numbers need to care. Pain. 2003;106:213-214.
McQuay HJ, Moore RA. Antidepressants and chronic pain. BMJ. 1997;314:763-764.
Meadows E. Treatments for patients with pelvic pain. Urol Nursing. 1999;19:33-35.
Meeus M, Nijs J. Central sensitization: a biopsychological explanation for chronic widespread pain in patients with fibromyalgia and chronic fatigue syndrome. Clin Rheumatol. 2007;26:465-473.
Meirowsky AM. The management of chronic interstitial cystitis by differential sacral neurotomy. J Neurosurg. 1969;30:604-607.
Melchior D, Packer CS, Johnson TC, Kaefer M. Dimethyl sulfoxide: does it change the functional properties of the bladder wall? J Urol. 2003;170:253-258.
Mendelowitz F, Moldwin R. Complementary approaches in the management of interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:235-240.
Messing E, Pauk D, Schaeffer A, et al. Associations among cystoscopic findings and symptoms and physical examination findings in women enrolled in the Interstitial Cystitis Data Base (ICDB) Study. Urology. 1997;49:81-85.
Messing EM. Interstitial cystitis. J Urol. 1994;151:355-356.
Messing EM, Freiha FS. Complication of clorpactin WCS90 therapy for interstitial cystitis. Urology. 1979;13:389-392.
Messing EM, Stamey TA. Interstitial cystitis: early diagnosis, pathology, and treatment. Urology. 1978;12:381-392.
Meulders Q, Michel C, Marteau P, et al. Association of chronic interstitial cystitis, protein-losing enteropathy and paralytic ileus with seronegative systemic lupus erythematosus: case report and review of the literature. Clin Nephrol. 1992;37:239-244.
Michael YL, Kawachi I, Stampfer MJ, et al. Quality of life among women with interstitial cystitis. J Urol. 2000;164:423-427.
Miller CH, MacDermott JP, Quattrocchi KB, et al. Lymphocyte function in patients with interstitial cystitis. J Urol. 1992;147:592-595.
Miller FG, Emanuel EJ, Rosenstein DL, Straus SE. Ethical issues concerning research in complementary and alternative medicine. JAMA. 2004;291:599-604.
Miller JL, Bavendam TG, Berger RE. Interstitial cystitis in men. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:165-168.
Miller JL, Rothman I, Bavendam TG, Berger RE. Prostatodynia and interstitial cystitis: one and the same? Urology. 1995;45:587-590.
Minogiannis P, El Mansoury M, Betances JA, et al. Hydroxyzine inhibits neurogenic bladder mast cell activation. Int J Immunopharmacol. 1998;20:553-563.
Moen M, Stokstad T. A long term followup study of women with asymptomatic endometriosis diagnosed incidentally at sterilization. Fertil Steril. 2002;78:773-776.
Moldwin R, Kushner L. The diagnostic value of interstitial cystitis questionnaires. J Urol. 2004;171(Suppl 4):96.
Moller NE. Carbenicillin-induced hemorrhagic cystitis. Lancet. 1978;2:946.
Moncada S, Higgs A. The L-arginine-nitric oxide pathway. N Engl J Med. 1993;329:2002.
Monga M, Percival C, Zupkas P. Intravesical ethanol as quantitative measure of bladder hyperpermeability. J Endourol. 2001;15:641-644.
Moore KH, Nickson P, Richmond DH, et al. Detrusor mast cells in refractory idiopathic instability. Br J Urol. 1992;70:17-21.
Morales A, Emerson L, Nickel JC, Lundie M. Intravesical hyaluronic acid in the treatment of refractory interstitial cystitis. J Urol. 1996;156:45-48.
Moran PA, Dwyer PL, Carey MP, et al. Oral methotrexate in the management of refractory interstitial cystitis. Aust N Z J Obstet Gynaecol. 1999;39:468-471.
Moskowitz MO, Byrne DS, Callahan HJ, et al. Decreased expression of a glycoprotein component of bladder surface mucin (GP1) in interstitial cystitis. J Urol. 1994;151:343-345.
Mouracade P, Lang H, Jacqmin D, Saussine C. [Using the intersitital cystitis new diagnostic criteria in daily practice: about 156 patients. Prog Urol. 2008;18:674-677.
Mulholland SG, Byrne DS. Interstitial cystitis. J Urol. 1994;152:879-880.
Mulholland SG, Hanno P, Parsons CL, et al. Pentosan polysulfate sodium for therapy of interstitial cystitis: a double-blind placebo-controlled clinical study. Urology. 1990;35:552-558.
Murnaghan GF, Saalfeld J, Farnsworth RH. Interstitial cystitis—treatment with Chlorpactin WCS 90. Br J Urol. 1970;42:744.
Murphy DM, Zincke H, Utz DC. Interstitial cystitis. J Urol. 1982;128:606.
Myers DL, Aguilar VC. Gynecologic manifestations of interstitial cystitis. Clin Obstet Gynecol. 2002;45:233-241.
Naber SP. Molecular pathology—diagnosis of infectious disease. N Engl J Med. 1994;331:1212-1215.
Nagaoka M, Tamaoki J, Gotoh S, et al. [A case of Sjogren syndrome accompanied by interstitial cystitis and interstitial pneumonia improved by suplatast tosilate and prednisolone.]. Arerugi. 2003;52:450-453. [in Japanese]
National Institutes of Health. Clinical trials: physical therapy in women with interstitial cystitis (IC03). http://www.clinicaltrials.gov/ct2/show/NCT00733603?term=interstitial+cystitis&recr=Open&rank=7;2008, 2008. [accessed 15.10.10]
National Institutes of Health. Clinical trials: a randomized multicenter double-blind CT to evaluate the efficacy and safety of mycophenolate mofetil … (ICCRN RCT2). http://www.clinicaltrial.gov/ct2/show/NCT00451867, 2007. [accessed 15.10.10]
National Institutes of Health. NIH launches effort to advance study of urologic chronic pelvic pain disorders. http://www.nih.gov/news/health/sep2008/niddk-05.htm, 2008. [accessed 15.10.10]
National Institutes of Health, Consensus Development Panel. Helicobacter pylori in peptic ulcer disease. JAMA. 1994;272:65-69.
Neal DEJr, Dilworth JP, Kaack MB. Tamm-Horsfall autoantibodies in interstitial cystitis. J Urol. 1991;145:37-39.
Nesse RM. Proximate and evolutionary studies of anxiety, stress and depression: synergy at the interface. Neurosci Biobehav Rev. 1999;23:895-903.
Nguan C, Franciosi LG, Butterfield NN, et al. A prospective, double-blind, randomized cross-over study evaluating changes in urinary pH for relieving the symptoms of interstitial cystitis. BJU Int. 2005;95:91-94.
Nickel J, Barkin J, Forrest J, et al. Randomized, double-blind, dose-ranging study of pentosan polysulfate sodium for interstitial cystitis. J Urol. 2001;165:67A.
Nickel JC, Downey J, Morales A, et al. Relative efficacy of various exogenous glycosaminoglycans in providing a bladder surface permeablility barrier. J Urol. 1998;160:612-614.
Nickel JC, Egerdie B, Downey J, et al. A real-life multicentre clinical practice study to evaluate the efficacy and safety of intravesical chondroitin sulphate for the treatment of interstitial cystitis. BJU Int. 2009;103:56-60.
Nickel JC, Emerson L, Cornish J. The bladder mucus (glycosaminoglycan) layer in interstitial cystitis. J Urol. 1993;149:716-718.
Nickel JC, Moldwin R, Lee S, et al. Intravesical alkalinized lidocaine (PSD597) offers sustained relief from symptoms of interstitial cystitis and painful bladder syndrome. BJU Int. 2009;103:910-918.
Nickel JC, Shoskes DA, Irvine-Bird K. Clinical phenotyping of women with interstitial cystitis/painful bladder syndrome (IC/PBS): a key to classification and potentially improved management. Urology. 2010. [Epub ahead of print
Nickel JC, Teichman JM, Gregoire M, et al. Prevalence, diagnosis, characterization, and treatment of prostatitis, interstitial cystitis, and epididymitis in outpatient urological practice: the Canadian PIE Study. Urology. 2005;66:935-940.
Nickel JC, Tripp D, Teal V, et al. Sexual function is a determinant of poor quality of life for women with treatment refractory interstitial cystitis. J Urol. 2007;177:1832-1836.
Nielsen KK, Kromann-Andersen B, Steven K, Hald T. Failure of combined supratrigonal cystectomy and Mainz ileocecocystoplasty in intractable interstitial cystitis: is histology and mast cell count a reliable predictor for the outcome of surgery? J Urol. 1990;144:255-258.
Nigro DA, Wein AJ. Interstitial cystitis: clinical and endoscopic features. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:137-142.
Nigro DA, Wein AJ, Foy M, et al. Associations among cystoscopic and urodynamic findings for women enrolled in the Interstitial Cystitis Data Base (ICDB) Study. Urology. 1997;49:86-92.
Nordling J. Interstitial cystitis: how should we diagnose it and treat it in 2004? Curr Opin Urol. 2004;14:323-327.
Nordling J, Anderson JB, Mortensen S, et al. Clinical outcome in patients with interstitial cystitis, relative to detrusor myopathy. Poster 42: Research Insights into Interstitial Cystitis. Washington, DC: NIDDK; Oct 30–Nov 1, 2003.
Nordling J, Anjum FH, Bade JJ, et al. Primary evaluation of patients suspected of having interstitial cystitis (IC). Eur Urol. 2004;45:662-669.
Nordling J, van Ophoven A. Intravesical glycosaminoglycan replenishment with chondroitin sulphate in chronic forms of cystitis: a multi-national, multi-centre, prospective observational clinical trial. Arzneimittelforschung. 2008;58:328-335.
Novicki DE, Larson TR, Swanson SK. Interstitial cystitis in men. Urology. 1998;52:621-624.
Nurse DE, Parry JR, Mundy AR. Problems in the surgical treatment of interstitial cystitis. Br J Urol. 1991;68:153-154.
Nyberg L, Kusek J, Mullins C. Multidisciplinary approach to the study of chronic pelvic pain. 2009.
O’Connor VJ. Clorpactin WCS-90 in the treatment of interstitial cystitis. Q Bull Northwest Univ Med Sch. 1955;29:392-395.
O’Leary MP, Sant G. The interstitial cystitis symptom and problem indices: rationale, development, and application. In: Sant G, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:271-276.
O’Leary MP, Sant GR, Fowler FJJr, et al. The interstitial cystitis symptom index and problem index. Urology. 1997;49:58-63.
O’Reilly BA, Dwyer PL, Hawthorne G, et al. Transdermal posterior tibial nerve laser therapy is not effective in women with interstitial cystitis. J Urol. 2004;172:1880-1883.
Ochs RL. Autoantibodies and interstitial cystitis. Clin Lab Med. 1997;17:571-579.
Ochs RL, Stein TWJr, Peebles CL, et al. Autoantibodies in interstitial cystitis. J Urol. 1994;151:587-592.
Oerlemans DJ, van Kerrebroeck PE. Sacral nerve stimulation for neuromodulation of the lower urinary tract. Neurourol Urodyn. 2008;27:28-33.
Okragly AJ, Niles AL, Saban R, et al. Elevated tryptase, nerve growth factor, neurotrophin-3 and glial cell line-derived neurotrophic factor levels in the urine of interstitial cystitis and bladder cancer patients. J Urol. 1999;161:438-441.
Onwude JL, Selo-Ojeme DO. Pregnancy outcomes following the diagnosis of interstitial cystitis. Gynecol Obstet Invest. 2003;56:160-162.
Oravisto KJ. Epidemiology of interstitial cystitis. Ann Chir Gynaecol Fenn. 1975;64:75-77.
Oravisto KJ. Interstitial cystitis as an autoimmune disease: a review. Eur Urol. 1980;6:10-13.
Oravisto KJ, Alfthan OS. Treatment of interstitial cystitis with immunosuppression and chloroquine derivatives. Eur Urol. 1976;2:82-84.
Ottem DP, Carr LK, Perks AE, et al. Interstitial cystitis and female sexual dysfunction. Urology. 2007;69:608-610.
Oyama IA, Rejba A, Lukban JC, et al. Modified Thiele massage as therapeutic intervention for female patients with interstitial cystitis and high-tone pelvic floor dysfunction. Urology. 2004;64:862-865.
Palea S, Artibani W, Ostardo E, et al. Evidence for purinergic neurotransmission in human urinary bladder affected by interstitial cystitis. J Urol. 1993;150:2007-2012.
Pang X, Boucher W, Triadafilopoulos G, et al. Mast cell and substance P-positive nerve involvement in a patient with both irritable bowel syndrome and interstitial cystitis. Urology. 1996;47:436-438.
Pang X, Cotreau-Bibbo MM, Sant GR, Theoharides TC. Bladder mast cell expression of high affinity oestrogen receptors in patients with interstitial cystitis. Br J Urol. 1995;75:154-161.
Pang X, Marchand J, Sant GR, et al. Increased number of substance P positive nerve fibres in interstitial cystitis. Br J Urol. 1995;75:744-750.
Pang X, Sant G, Theoharides TC. Altered expression of bladder mast cell growth factor receptor (c-kit) in interstitial cystitis. Urology. 1998;51:939-944.
Parekh MH, Chichester P, Lobel RW, et al. Effects of castration on female rabbit bladder physiology and morphology. Urology. 2004;64:1048-1051.
Parker C, Steele S, Raghavan R, et al. Hypersensitivity reaction associated with intravesical bacillus Calmette-Guérin for interstitial cystitis. J Urol. 2004;172:537.
Parrish J. Tic doloureux of the urinary bladder. In: Practical observations on strangulated hernia and some of the diseases of the urinary organs. Philadelphia: Key and Biddle; 1836:309-313.
Parsonnet J, Friedman GD, Vandersteen DP, et al. Helicobacter pylori infection and the risk of gastric carcinoma. N Engl J Med. 1991;325:1127-1136.
Parsons CL. Successful management of radiation cystitis with sodium pentosanpolysulfate. J Urol. 1986;136:813-814.
Parsons CL. Interstitial cystitis: clinical manifestations and diagnostic criteria in over 200 cases. Neurourol Urodyn. 1990;9:241-250.
Parsons CL. The role of the glycosaminoglycan layer in bladder defense mechanisms and interstitial cystitis. Int Urogynecol J. 1993;4:373-379.
Parsons CL. A model for the function of glycosaminoglycans in the urinary tract. World J Urol. 1994;12:38-42.
Parsons CL. Interstitial cystitis: new concepts in pathogenesis, diagnosis, and management. 2000. p. 20–31.
Parsons CL. Successful downregulation of bladder sensory nerves with combination of heparin and alkalinized lidocaine in patients with interstitial cystitis. Urology. 2005;65:45-48.
Parsons CL, Albo M. Intravesical potassium sensitivity in patients with prostatitis. J Urol. 2002;168:1054-1057.
Parsons CL, Bautista SL, Stein PC, Zupkas P. Cyto-injury factors in urine: a possible mechanism for the development of interstitial cystitis. J Urol. 2000;164:1381-1384.
Parsons CL, Benson G, Childs SJ, et al. A quantitatively controlled method to study prospectively interstitial cystitis and demonstrate the efficacy of pentosanpolysulfate. J Urol. 1993;150:845-848.
Parsons CL, Bullen M, Kahn BS, et al. Gynecologic presentation of interstitial cystitis as detected by intravesical potassium sensitivity. Obstet Gynecol. 2001;98:127-132.
Parsons CL, Dell J, Stanford EJ, et al. Increased prevalence of interstitial cystitis: previously unrecognized urologic and gynecologic cases identified using a new symptom questionnaire and intravesical potassium sensitivity. Urology. 2002;60:573-578.
Parsons CL, Dell J, Stanford EJ, et al. The prevalence of interstitial cystitis in gynecologic patients with pelvic pain, as detected by intravesical potassium sensitivity. Am J Obstet Gynecol. 2002;187:1395-1400.
Parsons CL, Greenberger M, Gabal L, et al. The role of urinary potassium in the pathogenesis and diagnosis of interstitial cystitis. J Urol. 1998;159:1862-1866.
Parsons CL, Housley T, Schmidt JD, Lebow D. Treatment of interstitial cystitis with intravesical heparin. Br J Urol. 1994;73:504-507.
Parsons CL, Hurst RE. Decreased urinary uronic acid levels in individuals with interstitial cystitis. J Urol. 1990;143:690-693.
Parsons CL, Lilly JD, Stein P. Epithelial dysfunction in nonbacterial cystitis (interstitial cystitis). J Urol. 1991;145:732-735.
Parsons CL, Mulholland SG. Successful therapy of interstitial cystitis with pentosanpolysulfate. J Urol. 1987;138:513-516.
Parsons CL, Rajasekaran M, Arsanjani AH, et al. Role of sialic acid in urinary cytoprotective activity of Tamm-Horsfall protein. Urology. 2007;69:577-581.
Parsons CL, Rosenberg MT, Sassani P, et al. Quantifying symptoms in men with interstitial cystitis/prostatitis, and its correlation with potassium-sensitivity testing. BJU Int. 2005;95:86-90.
Parsons CL, Schmidt JD, Pollen JJ. Successful treatment of interstitial cystitis with sodium pentosanpolysulfate. J Urol. 1983;130:51-53.
Parsons CL, Stein P. Role of toxic urine in interstitial cystitis. J Urol. 1990;143:373A.
Parsons CL, Stein PC, Bidair M, et al. Abnormal sensitivity to intravesical potassium in interstitial cystitis and radiation cystitis. Neurourol Urodyn. 1994;13:515-520.
Parsons CL, Stein PC, Bidair M, Lebow D. Abnormal sensitivity to intravesical potassium in interstitial cystitis and radiation cystitis. Neurourol Urodyn. 1994;13:515-520.
Parsons CL, Tatsis V. Prevalence of interstitial cystitis in young women. Urology. 2004;64:866-870.
Parsons CL, Zupkas P, Parsons JK. Intravesical potassium sensitivity in patients with interstitial cystitis and urethral syndrome. Urology. 2001;57:428-432.
Parsons DL, Boychuk D, Hurst R, Callahan H. Bladder surface glycosaminoglycans: an epithelial permeablility barrier. J Urol. 1990;143:139-142.
Parsons JK, Parsons CL. The historical origins of interstitial cystitis. J Urol. 2004;171:20-22.
Patra PB, Tibbitts FD, Westfall DP. Endocrine status and urinary mast cells: possible relationship to interstitial cystitis. Bethesda, MD: National Institutes of Health; 1995. p. 70
Payne CK, Mosbaugh PG, Forrest JB, et al. Intravesical resiniferatoxin for the treatment of interstitial cystitis: a randomized, double-blind, placebo controlled trial. J Urol. 2005;173:1590-1594.
Peeker R, Aldenborg F, Dahlstrom A, et al. Increased tyrosine hydroxylase immunoreactivity in bladder tissue from patients with classic and nonulcer interstitial cystitis. J Urol. 2000;163:1112-1115.
Peeker R, Aldenborg F, Fall M. The treatment of interstitial cystitis with supratrigonal cystectomy and ileocystoplasty: difference in outcome between classic and nonulcer disease. J Urol. 1998;159:1479-1482.
Peeker R, Enerback L, Fall M, Aldenborg F. Recruitment, distribution and phenotypes of mast cells in interstitial cystitis. J Urol. 2000;163:1009-1015.
Peeker R, Fall M. Toward a precise definition of interstitial cystitis: further evidence of differences in classic and nonulcer disease. J Urol. 2002;167:2470-2472.
Peeker R, Haghsheno MA, Holmang S, Fall M. Intravesical bacillus Calmette-Guérin and dimethyl sulfoxide for treatment of classic and nonulcer interstitial cystitis: a prospective, randomized double-blind study. J Urol. 2000;164:1912-1915.
Pelaez E, Prieto Rodrigo MA, Munoz Zurdo MM, et al. [Epidural spinal cord stimulation for interstitial cystitis. Rev Esp Anestesiol Reanim. 2004;51:549-552. [in Spanish]
Peng CH, Kuo HC. Multiple intravesical instillations of low-dose resiniferatoxin in the treatment of refractory interstitial cystitis. Urol Int. 2007;78:78-81.
Perez-Marrero R, Emerson L, Juma S. Urodynamic studies in interstitial cystitis. Urology. 1987;29:27-30.
Perez-Marrero R, Emerson LE, Feltis JT. A controlled study of dimethyl sulfoxide in interstitial cystitis. J Urol. 1988;140:36-39.
Perez-Marrero R, Emerson LE, Maharajh DO, et al. Prolongation of response to DMSO by heparin maintenance. Urology. 1993;41(Suppl):64-66.
Perzin AD, Hanno PM, Ruggieri MR. Effect of protamine and IC urine on dye penetration across urothelium. J Urol. 1991;145:259A.
Peters K, Diokno A, Steinert B, et al. The efficacy of intravesical Tice strain bacillus Calmette-Guérin in the treatment of interstitial cystitis: a double-blind, prospective, placebo controlled trial. J Urol. 1997;157:2090-2094.
Peters K, Kalinowski S. Fact or fiction? Is abuse prevalent in patients with interstitial cystitis? results from a community survey and clinic population. J Urol. 2007;178:891-895.
Peters KM, Carey JM, Konstandt DB. Sacral neuromodulation for the treatment of refractory interstitial cystitis: outcomes based on technique. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:223-228.
Peters KM, Carrico DJ, Kalinowski SE, et al. Prevalence of pelvic floor dysfunction in patients with interstitial cystitis. Urology. 2007;70:16-18.
Peters KM, Diokno AC, Steinert BW. Preliminary study on urinary cytokine levels in interstitial cystitis: does intravesical bacille Calmette-Guérin treat interstitial cystitis by altering the immune profile in the bladder? Urology. 1999;54:450-453.
Peters KM, Diokno AC, Steinert BW, Gonzalez JA. The efficacy of intravesical bacillus Calmette-Guérin in the treatment of interstitial cystitis: long-term followup. J Urol. 1998;159:1483-1486.
Peters KM, Killinger KA, Carrico DJ, et al. Sexual function and sexual distress in women with interstitial cystitis: a case-control study. Urology. 2007;70:543-547.
Peters KM, Killinger KA, Ibrahim IA, Villalba PS. The relationship between subjective and objective assessments of sacral neuromodulation effectiveness in patients with urgency-frequency. Neurourol Urodyn. 2008;27:775-778.
Peters KM, Konstandt D. Sacral neuromodulation decreases narcotic requirements in refractory interstitial cystitis. BJU Int. 2004;93:777-779.
Pezzone MA, Liang R, Fraser MO. A model of neural cross-talk and irritation in the pelvis: implications for the overlap of chronic pelvic pain disorders. Gastroenterology. 2005;128:1953-1964.
Polman CH, Reingold SC, Barkhof F, et al. Ethics of placebo-controlled clinical trials in multiple sclerosis: a reassessment. Neurology. 2008;70:1134-1140.
Pontari MA, Hanno PM, Ruggieri MR. Comparison of bladder blood flow in patients with and without interstitial cystitis. J Urol. 1999;162:330-334.
Pool TL. Interstitial cystitis: clinical considerations and treatment. Clin Obstet Gynecol. 1967;10:185-191.
Pool TL, Rives HF. Interstitial cystitis: treatment with silver nitrate. J Urol. 1944;51:520-525.
Porru D, Campus G, Tudino D, et al. Results of treatment of refractory interstitial cystitis with intravesical hyaluronic acid. Urol Int. 1997;59:26-29.
Porru D, Politano R, Gerardini M, et al. Different clinical presentation of interstitial cystitis syndrome. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:198-202.
Porru D, Tinelli C, Gerardini M, et al. Evaluation of urinary and general symptoms and correlation with other clinical parameters in interstitial cystitis patients. Neurourol Urodyn. 2005;24:69-73.
Portenoy RK, Dole V, Joseph H, et al. Pain management and chemical dependency. JAMA. 1997;278:592-593.
Portenoy RK, Foley KM. Chronic use of opioid analgesics in nonmalignant pain: report of 38 cases. Pain. 1986:171-186.
Potts JM, Ward AM, Rackley RR. Association of chronic urinary symptoms in women and Ureaplasma urealyticum. Urology. 2000;55:486-489.
Powell NB, Powell EB. The female urethra: a clinico-pathological study. J Urol. 1949;61:557-570.
Pranikoff K, Constantino G. The use of amitriptyline in patients with urinary frequency and pain. Urology. 1998;51:179-181.
Prendergast S, Weiss JM. Screening for musculoskeletal causes of pelvic pain. Clin Obstet Gynecol. 2003;46:773-782.
Press SM, Moldwin R, Kushner L, et al. Decreased expression of GP-51 glycosaminoglycan in cats afflicted with feline interstitial cystitis. J Urol. 1995;153:288A.
Price DT, Maloney KE, Ibrahim GK, et al. Vesical endometriosis: report of two cases and review of the literature. Urology. 1996;48:639-643.
Propert KJ, Mayer R, Nickel JC, et al. Did patients with interstitial cystitis who failed to respond to initial treatment with bacillus Calmette-Guérin or placebo in a randomized clinical trial benefit from a second course of open label bacillus Calmette-Guérin? J Urol. 2007;178:886-890.
Propert KJ, Mayer R, Nickel JC, et al. Followup of patients with interstitial cystitis responsive to treatment with intravesical bacillus Calmette-Guérin or placebo. J Urol. 2008;179:552-555.
Propert KJ, Mayer RD, Wang Y, et al. Responsiveness of symptom scales for interstitial cystitis. Urology. 2006;67:55-59.
Propert KJ, Payne C, Kusek JW, Nyberg LM. Pitfalls in the design of clinical trials for interstitial cystitis. Urology. 2002;60:742-748.
Propert KJ, Schaeffer AJ, Brensinger CM, et al. A prospective study of interstitial cystitis: results of longitudinal followup of the interstitial cystitis data base cohort. The Interstitial Cystitis Data Base Study Group. J Urol. 2000;163:1434-1439.
Qin C, Malykhina AP, Akbarali HI, et al. Acute colitis enhances responsiveness of lumbosacral spinal neurons to colorectal distension in rats. Dig Dis Sci. 2008;53:141-148.
Rackley R, Frenkl T, Abdelmalak J. Botulinum toxin: the promise of therapy for complex voiding dysfunctions. Contemp Urol. 2005:38-52.
Rajkumar GN, Conn IG. Botulinum toxin: a new dimension in the treatment of lower urinary tract dysfunction. Urology. 2004;64:2-8.
Rashid HH, Reeder JE, O’Connell MJ, et al. Interstitial cystitis antiproliferative factor (APF) as a cell-cycle modulator. BMC Urol. 2004;4:3.
Ratliff TL, Klutke CG, McDougall EM. The etiology of interstitial cystitis. Urol Clin North Am. 1994;21:21-30.
Ratner V, Slade D. Interstitial cystitis: a women’s health perspective. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:257-260.
Ratner V, Slade D, Whitmore KE. Interstitial cystitis: a bladder disease finds legitimacy. J Womens Health. 1992;1:63-68.
Ray W, Meredith S, Thapa P, et al. Cyclic antidepressants and the risk of sudden cardiac death. Clin Pharmacol Ther. 2004;75:234-241.
Rees J, Wade T, Levy D, et al. Changes in beliefs identify unblinding in randomized controlled trials: a method to meet CONSORT guidelines. Contemp Clin Trials. 2005;26:25-37.
Reinhart H, Obedeanu N, Hooton T, et al. Urinary excretion of Tamm-Horsfall protein in women with recurrent urinary tract infections. J Urol. 1990;144:1185-1187.
Renshaw DC. Desipramine for interstitial cystitis. JAMA. 1988;260:341.
Rice L, Kennedy D, Veach A. Pentosan induced cerebral sagittal sinus thrombosis: a variant of heparin induced thrombocytopenia. J Urol. 1998;160:2148.
Rickard A, Lagunoff D. A novel model for the role of mast cells in interstitial cystitis. Bethesda, MD: National Institutes of Health; 1995. p. 69
Riedl C, Engelhardt PF, Daha KL, et al. Hyaluronan treatment of interstitial cystitis/painful bladder syndrome. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:717-721.
Riedl CR, Knoll M, Plas E, et al. Intravesical electromotive drug administration for the treatment of non-infectious chronic cystitis. Int Urogynecol J Pelvic Floor Dysfunct. 1997;8:134-137.
Rivas DA, Chancellor MB, Shupp-Byrne S, et al. Molecular marker for development of interstitial cystitis in rat model: isoactin gene expression. J Urol. 1997;157:1937-1940.
Roberto PJ, Reich JD, Hirshberg S, et al. Assessment of bladder permiability and sensation in interstitial cystitis patients. J Urol. 1997;157:317.
Roberts RO, Bergstralh EJ, Bass SE, et al. Incidence of physician-diagnosed interstitial cystitis in Olmsted County: a community-based study. BJU Int. 2003;91:181-185.
Robson WLM, Leung AKC. Extraordinary urinary frequency syndrome. Urology. 1993;42:321-324.
Rodriguez Villamil L, Batista Miranda JE, Smet CE, et al. Supratrigonal cystectomy and enterocystoplasty as treatment of advanced interstitial cystitis. Urol Integrada Invest. 1999;4:350-353.
Rofeim O, Hom D, Freid RM, Moldwin RM. Use of the neodymium:YAG laser for interstitial cystitis: a prospective study. J Urol. 2001;166:134-136.
Rogers R. Pelvic denervation surgery: what the evidence and anatomy teach us. Clin Obstet Gynecol. 2003;46:767-772.
Roppolo JR, Tai C, Booth AM, et al. Bladder Adelta afferent nerve activity in normal cats and cats with feline interstitial cystitis. J Urol. 2005;173:1011-1015.
Rosales RL, Ariumura K, Ikenaga S. Extrafusal and intrafusal muscle effects in experimental botulinum toxin A injection. Muscle Nerve. 1996;19:488-496.
Rosamilia A, Cann L, Dwyer P, et al. Bladder microvasculature in women with interstitial cystitis. J Urol. 1999;161:1865-1870.
Rosamilia A, Clements JA, Dwyer PL, et al. Activation of the kallikrein kinin system in interstitial cystitis. J Urol. 1999;162:129-134.
Rosamilia A, Dwyer PL, Gibson J. Electromotive drug administration of lidocaine and dexamethasone followed by cystodistension in women with interstitial cystitis. Int Urogynecol J Pelvic Floor Dysfunct. 1997;8:142-145.
Rosamilia A, Igawa Y, Higashi S. Pathology of interstitial cystitis. Int J Urol. 2003;10(Suppl):S11-S15.
Rose AE, Azevedo KJ, Payne CK. Office bladder distention with electromotive drug administration (EMDA) is equivalent to distention under general anesthesia (GA). BMC Urol. 2005;5:14.
Rose NR, Bona C. Defining criteria for autoimmune diseases. Immunol Today. 1993;14:426-430.
Rosenberg MT, Hazzard M. Prevalence of interstitial cystitis symptoms in women: a population based study in the primary care office. J Urol. 2005;174:2231-2234.
Rossberger J, Fall M, Jonsson O, Peeker R. Long-term results of reconstructive surgery in patients with bladder pain syndrome/interstitial cystitis: subtyping is imperative. Urology. 2007;70:638-642.
Rothman KJ, Michels KB. The continuing unethical use of placebo controls. N Engl J Med. 1994:394-398.
Rothrock NE, Lutgendorf SK, Hoffman A, Kreder KJ. Depressive symptoms and quality of life in patients with interstitial cystitis. J Urol. 2002;167:1763-1767.
Rothrock NE, Lutgendorf SK, Kreder KJ. Coping strategies in patients with interstitial cystitis: relationships with quality of life and depression. J Urol. 2003;169:233-236.
Rothrock NE, Lutgendorf SK, Kreder KJ, et al. Stress and symptoms in patients with interstitial cystitis: a life stress model. Urology. 2001;57:422-427.
Rovner E, Propert KJ, Brensinger C, et al. Treatments used in women with interstitial cystitis: the interstitial cystitis data base (ICDB) study experience. The Interstitial Cystitis Data Base Study Group. Urology. 2000;56:940-945.
Rovner ES, Wein AJ. Interstitial cystitis: clinical features. Urol Integrada Invest. 1999;4:307-314.
Rowbotham M, Harden N, Stacey B, et al. Gabapentin for the treatment of postherpetic neuralgia. JAMA. 1998;280:1837-1842.
Rubio-Diaz DE, Pozza ME, Dimitrakov J, et al. A candidate serum biomarker for bladder pain syndrome/interstitial cystitis. Analyst. 2009;134:1133-1137.
Rudick CN, Bryce PJ, Guichelaar LA, et al. Mast cell–derived histamine mediates cystitis pain. PLoS ONE. 2008;3:e2096.
Rudick CN, Chen MC, Mongiu AK, Klumpp DJ. Organ cross talk modulates pelvic pain. Am J Physiol Regul Integr Comp Physiol. 2007;293:R1191-R1198.
Ruggieri MR, Hanno PM, Levin RM. Nitrofurantoin not surface active agent in rabbit urinary bladder. Urology. 1987;29:534-537.
Ruggieri MR, Hanno PM, Whitmore KE, Balagani RK. Effect of repeated instillation of interstitial cystitis urine on the rabbit urinary bladder. Urology. 1993;42:646-652.
Ruggieri MR, Monson FC, Levin RM, et al. Interstitial cystitis: animal models. In: Hanno PM, Staskin DR, Krane RJ, Wein AJ, editors. Interstitial cystitis. London: Springer-Verlag; 1990:49-62.
Ruggieri MR, Steinhardt GF, Hanno PM. Comparison of antiadherence activity of bladder extracts from interstitial cystitis patients with recurrent urinary tract infections. Semin Urol. 1991;9:136-142.
Rummans TA. Nonopioid agents for treatment of acute and subacute pain. Mayo Clin Proc. 1994;69:481-490.
Ruoslahti E. Structure and biology of proteoglycans. Ann Rev Cell Biol. 1988;4:229-232.
Rupp BW, Perry BB, Griebling TL, et al. Quality of life in women with interstitial cystitis following cystourethrectomy and continent urinary diversion. J Urol. 2000;163S:62.
Saban R, Keith IM, Bjorling DE. Neuropeptide-mast cell interaction in interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:53-66.
Saban R, Saban MR, Maier J, et al. Urothelial expression of neuropilins and VEGF receptors in control and interstitial cystitis patients. Am J Physiol Renal Physiol. 2008;295:F1613-F1623.
Saban R, Saban MR, Nguyen NB, et al. Mast cell regulation of inflammation and gene expression during antigen-induced bladder inflammation in mice. Physiol Genomics. 2001;7:35-43.
Sahinkanat T, Guven A, Ekerbicer H, Aral M. Prevalence of positive potassium sensitivity test which is an indicator of bladder epithelial permeability dysfunction in a fixed group of Turkish women. Urol Int. 2008;80:52-56.
Sairanen J, Forsell T, Ruutu M. Long-term outcome of patients with interstitial cystitis treated with low dose cyclosporine A. J Urol. 2004;171:2138-2141.
Sairanen J, Hotakainen K, Tammela TL, et al. Urinary epidermal growth factor and interleukin-6 levels in patients with painful bladder syndrome/interstitial cystitis treated with cyclosporine or pentosan polysulfate sodium. Urology. 2008;71:630-633.
Sairanen J, Tammela TL, Leppilahti M, et al. Cyclosporine A and pentosan polysulfate sodium for the treatment of interstitial cystitis: a randomized comparative study. J Urol. 2005;174:2235-2238.
Sairanen J, Tammela TL, Leppilahti M, et al. Cyclosporine A and pentosan polysulfate sodium for the treatment of interstitial cystitis: a randomized comparative study. J Urol. 2005;174:2235-2238.
Sairanen J, Tammela TL, Leppilahti M, et al. Potassium sensitivity test (PST) as a measurement of treatment efficacy of painful bladder syndrome/interstitial cystitis: a prospective study with cyclosporine A and pentosan polysulfate sodium. Neurourol Urodyn. 2007;26:267-270.
Sakakibara R, Uchiyama T, Yoshiyama M, et al. Urinary dysfunction in patients with systemic lupus erythematosis. Neurourol Urodyn. 2003;22:593-596.
Salavatore S, Khullar V, Cardozo L, et al. Evaluating ambulatory urodynamics: a prospective study in asymptomatic women. Br J Obstet Gynaecol. 2003;110:83-84.
Sant GR. Intravesical 50% dimethyl sulfoxide (Rimso-50) in treatment of interstitial cystitis. Urology. 1987;29:17-21.
Sant GR. Interstitial cystitis. Monogr Urol. 1991;12:37-63.
Sant GR, Kilaru P, Ucci AA. Mucosal mast cell contribution to bladder mastocytosis in interstitial cystitis. J Urol. 1988;139:276A.
Sant GR, Propert KJ, Hanno PM, et al. A pilot clinical trial of oral pentosan polysulfate and oral hydroxyzine in patients with interstitial cystitis. J Urol. 2003;170:810-815.
Sant GR, Theoharides TC. The role of the mast cell in interstitial cystitis. Urol Clin North Am. 1994;21:41-53.
Sant GR, Theoharides TC, Letourneau R, Gelfand J. Interstitial cystitis and bladder mastocytosis in a woman with chronic urticaria. Scand J Urol Nephrol. 1997;31:497-500.
Sasaki K, Smith CP, Chuang YC, et al. Oral gabapentin (neurontin) treatment of refractory genitourinary tract pain. Tech Urol. 2001;7:47-49.
Scheepens WA, De Bie RA, Weil EH, van Kerrebroeck PE. Unilateral versus bilateral sacral neuromodulation in patients with chronic voiding dysfunction. J Urol. 2002;168:2046-2050.
Scheepens WA, Jongen M, Nieman F, et al. Predictive factors for sacral neuromodulation in chronic lower urinary tract dysfunction. Urology. 2002;60:598-602.
Schmidt RA. Neurostimulation of bladder and urethra. In: Webster G, Kirby R, King L, Goldwasser B, editors. Reconstructive urology. Boston: Blackwell Scientific Publications; 1993:591-601.
Schmidt RA. Urodynamic features of the pelvic pain patient and the impact of neurostimulation on these parameters. World J Urol. 2001;19:186-193.
Schmidt RA, Jonas U, Oleson KA, et al. Sacral nerve stimulation for treatment of refractory urinary urge incontinence. J Urol. 1999;162:352-357.
Schmidt RA, Vapnek JM. Pelvic floor behavior and interstitial cystitis. Semin Urol. 1991;9:154-159.
Schulte G, Bryja V. The frizzled family of unconventional G-protein–coupled receptors. Trends Pharmacol Sci. 2007;28:518-525.
Schulte-Baukloh H, Bigalke H, Miller K, et al. Botulinum neurotoxin type A in urology: antibodies as a cause of therapy failure. Int J Urol. 2008;15:407-415.
Schulz KF, Chalmers I, Hayes RJ, et al. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408-412.
Sech SM, Montoya JD, Bernier PA, et al. The so-called “placebo effect” in benign prostatic hyperplasia treatment trials represents partially a conditional regression to the mean induced by censoring. Urology. 1998;51:242-250.
Seddon JM, Best L, Bruce AW. Intestinocystoplasty in treatment of interstitial cystitis. Urology. 1977;10:431-435.
Segura J, Opitz J, Greene L. Prostatosis, prostatitis or pelvic floor tension myalgia? J Urol. 1979;122:168.
Serel TA, Soyupek S, Candir O. Association between mast cells and bladder carcinoma. Urol Int. 2004;72:299-302.
Seshadri P, Emerson L, Morales A. Cimetidine in the treatment of interstitial cystitis. Urology. 1994;44:614-616.
Seth A, Teichman JM. Differences in the clinical presentation of interstitial cystitis/painful bladder syndrome in patients with or without sexual abuse history. J Urol. 2008;180:2029-2033.
Shanberg AM. Benign diseases of the bladder. In: Smith JA, Stein BS, Benson RC, editors. Lasers in urologic surgery. Chicago: Year Book Medical Publishers; 1989:50-56.
Shanberg AM, Baghdassarian R, Tansey LA. Treatment of interstitial cystitis with the neodymium-YAG laser. J Urol. 1985;134:885-888.
Shanberg AM, Malloy TR. Use of lasers in interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:215-218.
Shea-O’Malley CC, Sant GR. Quality of life in interstitial cystitis. Urol Integrada Invest. 1999;4:303-306.
Shintani Y, Takashima S, Asano Y, et al. Glycosaminoglycan modification of neuropilin-1 modulates VEGFR2 signaling. Embo J. 2006;25:3045-3055.
Shirley SW, Stewart BH, Mirelman S. Dimethyl sulfoxide in treatment of inflammatory genitourinary disorders. Urology. 1978;11:215-220.
Shorter B, Lesser M, Moldwin RM, Kushner L. Effect of comestibles on symptoms of interstitial cystitis. J Urol. 2007;178:145-152.
Shoskes DA, Nickel C, Rackley R, Pontari M. Clinical phenotyping in chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: a management strategy for urologic chronic pelvic pain syndromes. Prostate Cancer Prostatic Dis. 2009;12(2):177-183.
Shoskes DA, Nickel JC, Dolinga R, Prots D. Clinical phenotyping of patients with chronic prostatitis/chronic pelvic pain syndrome and correlation with symptom severity. Urology. 2009;73:538-542.
Sidh SM, Smith SP, Silber SB, Young JDJr. Eosinophilic cystitis: advanced disease requiring surgical intervention. Urology. 1980;15:23-26.
Siegel A, Snyder J, Raz S. Surgical therapy of interstitial cystitis. In: Hanno PM, Staskin DR, Krane RJ, Wein AJ, editors. Interstitial cystitis. London: Springer-Verlag; 1990:193-205.
Siegel S, Paszkiewicz E, Kirkpatrick C, et al. Sacral nerve stimulation in patients with chronic intractable pelvic pain. J Urol. 2001;166:1742-1745.
Silk MR. Bladder antibodies in interstitial cystitis. J Urol. 1970;103:307-309.
Simmons JL. Interstitial cystitis: an explanation for the beneficial effect of an antihistamine. J Urol. 1961;85:149-155.
Simmons JL, Bunce PL. On the use of an antihistamine in the treatment of interstitial cystitis. Am Surg. 1958;24:664-667.
Simon LJ, Landis JR, Erickson DR, Nyberg LM. The Interstitial Cystitis Data Base Study: concepts and preliminary baseline descriptive statistics. Urology. 1997;49:64-75.
Simons F. Advances in H1-antihistamines. N Engl J Med. 2004;351:2203-2217.
Singh G, Thomas DG. Interstitial cystitis: involvement of the intestine. Eur Urol. 1996;29:322-324.
Sircus SI, Sant GR, Ucci AAJr. Bladder detrusor endometriosis mimicking interstitial cystitis. Urology. 1988;32:339-342.
Sirinian E, Payne CK. Correlation of symptoms between 2 instruments among interstitial cystitis patients. Urology. 2001;57:124-125.
Siroky MB. Is it interstitial cystitis? Diagnostic distinctions in reduced bladder capacity. Contemp Urol. 1994; July:13-22.
Skene AJC. Diseases of the bladder and urethra in women. New York: William Wood; 1887.
Slobodov G, Feloney M, Gran C, et al. Abnormal expression of molecular markers for bladder impermeability and differentiation in the urothelium of patients with interstitial cystitis. J Urol. 2004;171:1554-1558.
Smith BH, Dehner LP. Chronic ulcerating interstitial cystitis (Hunner’s ulcer): a study of 28 cases. Arch Pathol. 1972;93:76-81.
Smith CP, Radziszewski P, Borkowski A, et al. Botulinum toxin a has antinociceptive effects in treating interstitial cystitis. Urology. 2004;64:871-875.
Smith GL, Christmas TJ. Interstitial ureteritis following cystectomy for interstitial cystitis. Br J Urol. 1996;77:607-608.
Smith SD, Wheeler MA, Foster HEJr, Weiss RM. Urinary nitric oxide synthase activity and cyclic GMP levels are decreased with interstitial cystitis and increased with urinary tract infections. J Urol. 1996;155:1432-1435.
Smith SD, Wheeler MA, Foster HEJr, Weiss RM. Improvement in interstitial cystitis symptom scores during treatment with oral L-arginine. J Urol. 1997;158:703-708.
Society for Urodynamics and Female Urology (SUFU) Interstitial Cystitis and Chronic Pelvic Pain. Society Meeting. 2004.
Song Y, Zhang W, Xu B, et al. Prevalence and correlates of painful bladder syndrome symptoms in Fuzhou Chinese women. Neurourol Urodyn. 2009;28:22-25.
Sorensen R. Chondroitin sulphate in the treatment of interstitial cystitis and chronic inflammatory disease of the urinary bladder. Eur Urol. 2003;2(Suppl):14-16.
Spanos C, Pang X, Ligris K, et al. Stress-induced bladder mast cell activation: implications for interstitial cystitis. J Urol. 1997;157:669-672.
Spinelli M, Bertapelle P, Cappellano F, et al. Chronic sacral neuromodulation in patients with lower urinary tract symptoms: results from a national register. J Urol. 2001;166:541-545.
Staehelin L, Chalpowski F, Bonneville M. Luminal plasma membrane of the urinary bladder. I. Three-dimensional reconstruction of freeze-etch images. J Cell Biol. 1972;53:73.
Stamm WE, Wagner KF, Amsel R, et al. Causes of the acute urethral syndrome in women. N Engl J Med. 1980;303:409-415.
Steers WD, Tuttle JB. Neurogenic inflammation and nerve growth factor: possible roles in interstitial cystitis. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:67-76.
Stein PC, Santamaria PJ, Kurtz SB, Parsons CL. Evaluation of urothelial Tamm-Horsfall protein and serum antibody as a potential diagnostic marker for interstitial cystitis. J Urol. 1993;150:1405-1408.
Stein PC, Torri A, Parsons CL. Elevated urinary norepinephrine in interstitial cystitis. Urology. 1999;53:1140-1143.
Steinberg AC, Oyama IA, Whitmore KE. Bilateral S3 stimulator in patients with interstitial cystitis. Urology. 2007;69:441-443.
Steinert BW, Diokno AC, Robinson JE, Mitchell BA. Complement C3, eosinophil cationic protein and symptom evaluation in interstitial cystitis. J Urol. 1994;151:350-354.
Steinhoff G, Ittah B, Rowan S. The efficacy of chondroitin sulfate 0.2% in treating interstitial cystitis. Can J Urol. 2002;9:1454-1458.
Stewart BH, Branson AC, Hewitt CB, et al. The treatment of patients with interstitial cystitis, with special reference to intravesical DMSO. Trans Am Assoc Genitourin Surg. 1971;63:69-74.
Stewart BH, Branson AC, Hewitt CB, et al. The treatment of patients with interstitial cystitis, with special reference to intravesical DMSO. J Urol. 1972;107:377-380.
Stewart BH, Persky L, Kiser WS. The use of dimethyl sulfoxide (DMSO) in the treatment of interstitial cystitis. J Urol. 1968;98:671-672.
Stewart BH, Shirley SW. Further experience with intravesical dimethyl sulfoxide in the treatment of interstitial cystitis. J Urol. 1976;116:36-38.
Stone AR. Treatment of voiding complaints and incontinence in painful bladder syndrome. Urol Clin North Am. 1991;18:317-325.
Stone AR, Vogelsang P, Miller CH, MacDermott JP. Tamm-Horsfall protein as a marker in interstitial cystitis. J Urol. 1992;148:1406-1408.
Stone NN. Nalmefene in the treatment of interstitial cystitis. Urol Clin North Am. 1994;21:101-106.
Stones R. Pelvic vascular congestion—half a century later. Clin Obstet Gynecol. 2003;46:831-836.
Stout L, Gerspach JM, Levy SM, et al. Dimethyl sulfoxide does not trigger urine histamine release in interstitial cystitis. Urology. 1995;46:653-656.
Streiner DL. Placebo-controlled trials: when are they needed? Schizophr Res. 1999;35:201-210.
Streiner DL. Alternatives to placebo-controlled trials. Can J Neurol Sci. 2007;34(Suppl 1):S37-S41.
Sun Y, Chai TC. Up-regulation of P2X3 receptor during stretch of bladder urothelial cells from patients with interstitial cystitis. J Urol. 2004;171:448-452.
Sun Y, Keay S, De Deyne PG, Chai TC. Augmented stretch activated adenosine triphosphate release from bladder uroepithelial cells in patients with interstitial cystitis. J Urol. 2001;166:1951-1956.
Sung JJY, Chung SCS, Ling TKW, et al. Antibacterial treatment of gastric ulcers associated with Helicobacter pylori. N Engl J Med. 1995;332:139-142.
Sutton C, Ewen S, Whitelaw N, Haines P. Prospective, randomized, double-blind, controlled trial of laser laparoscopy in the treatment of pelvic pain associated with minimal, mild, and moderate endometriosis. Fertil Steril. 1995;62:696-700.
Sutton C, Pooley A, Ewen S, et al. Follow-up report on a randomized controlled trial of laser laparoscopy in the treatment of pelvic pain associated with minimal to moderate endometriosis. Fertil Steril. 1997;68:1070-1074.
Talati A, Ponniah K, Strug LJ, et al. Panic disorder, social anxiety disorder, and a possible medical syndrome previously linked to chromosome 13. Biol Psychiatry. 2008;63:594-601.
Tan EM. Antinuclear antibodies: diagnostic markers for autoimmune diseases and probes for cell biology. Adv Immunol. 1989;44:93.
Tanaka T, Kawashima H, Makino T, et al. Hyperbaric oxygen therapy for interstitial cystitis resistant to conventional treatments. Int J Urol. 2007;14:563-565.
Taub HC, Stein M. Bladder distention therapy for symptomatic relief of frequency and urgency: a ten year review. Urology. 1994;43:36-39.
Teichman JM, Nielsen-Omeis BJ. Potassium leak test predicts outcome in interstitial cystitis. J Urol. 1999;161:1791-1794.
Teichman JM, Nielsen-Omeis BJ, McIver BD. Modified urodynamics for interstitial cystitis. Tech Urol. 1997;3:65-68.
Teichman JM, Thompson IM, Taichman NS. Joseph Parrish, tic doloureux of the bladder and interstitial cystitis. J Urol. 2000;164:1473-1475.
Temml C, Wehrberger C, Riedl C, et al. Prevalence and correlates for interstitial cystitis symptoms in women participating in a health screening project. Eur Urol. 2007;51:803-808.
Theoharides TC. Hydroxyzine for interstitial cystitis. J Allergy Clin Immunol. 1993;91:686.
Theoharides TC. Hydroxyzine in the treatment of interstitial cystitis. Urol Clin North Am. 1994;21:113-119.
Theoharides TC. Panic disorder, interstitial cystitis, and mast cells. J Clin Psychopharmacol. 2004;24:361-364.
Theoharides TC, Cochrane DE. Critical role of mast cells in inflammatory diseases and the effect of acute stress. J Neuroimmunol. 2004;146:1-12.
Theoharides TC, Kempuraj D, Sant GR. Mast cell involvement in interstitial cystitis: a review of human and experimental evidence. Urology. 2001;57:47-55.
Theoharides TC, Sant GR. Bladder mast cell activation in interstitial cystitis. Semin Urol. 1991;9:74-87.
Theoharides TC, Sant GR. Hydroxyzine for symptomatic relief of interstitial cystitis symptoms. In: Sant GR, editor. Interstitial cystitis. Philadelphia: Lippincott-Raven; 1997:241-246.
Theoharides TC, Sant GR. Hydroxyzine therapy for interstitial cystitis. Urology. 1997;49:108-110.
Theoharides TC, Sant GR, El Mansoury M, et al. Activation of bladder mast cells in interstitial cystitis: a light and electron microscopic study. J Urol. 1995;153:629-636.
Thilagarajah R, Witherow RO, Walker MM. Oral cimetidine gives effective symptom relief in painful bladder disease: a prospective, randomized, double-blind placebo-controlled trial. BJU Int. 2001;87:207-212.
Tincello DG, Walker AC. Interstitial cystitis in the UK: results of a questionnaire survey of members of the Interstitial Cystitis Support Group. Eur J Obstet Gynecol Reprod Biol. 2005;118:91-95.
Tissot WD, Diokno AC, Peters KM. A referral center’s experience with transitional cell carcinoma misdiagnosed as interstitial cystitis. J Urol. 2004;172:478-480.
Tomaszewski JE, Landis JR, Brensinger C, et al. Baseline associations among pathologic features and patient symptoms in the national interstitial cystitis data base. J Urol. 1999;161S:28.
Tomaszewski JE, Landis JR, Russack V, et al. Biopsy features are associated with primary symptoms in interstitial cystitis: results from the interstitial cystitis database study. Urology. 2001;57:67-81.
Toren P, Norman R. Cyclophosphamide induced hemorrhagic cystitis successfully treated with pentosanpolysulfate. J Urol. 2005;173:103.
Trelstad RL. Glycosaminoglycans: mortar, matrix, mentor. Lab Invest. 1985;53:1-4.
Trinka PJ, Stanley BK, Noble MJ, et al. Mast-cell syndrome: a relative contraindication for continent urinary diversion. J Urol. 1993;149:506A.
Truong LD, Ostrowski ML, Wheeler TM. Tamm-Horsfall protein in bladder tissue. Am J Surg Pathol. 1994;18:615-622.
Tsiriopoulos I, Lee G, O’Reilly A, et al. Primary splenic marginal zone lymphoma with bladder metastases mimicking interstitial cystitis. Int Urol Nephrol. 2006;38:475-476.
Turner JA, Deyo RA, Loeser JD, et al. The importance of placebo effects in pain treatment and research. JAMA. 1994;271:1609-1614.
Turner KJ, Stewart LH. How do you stretch a bladder? A survey of UK practice, a literature review, and a recommendation of a standard approach. Neurourol Urodyn. 2005;24(1):74-76.
Twiss C, Kilpatrick L, Craske M, et al. Increased Startle responses in interstitial cystitis: evidence for central hyperresponsiveness to visceral related threat. J Urol. 2009 May;181(5):2127-2133.
Ueda T, Sant GR, Hanno PM, Yoshimura N. Interstitial cystitis and frequency-urgency syndrome (OAB syndrome). Int J Urol. 2003;10(Suppl):S39-S48.
Ueda T, Tamaki M, Ogawa O, et al. Improvement of interstitial cystitis symptoms and problems that developed during treatment with oral IPD-1151T. J Urol. 2000;164:1917-1920.
Ueda T, Tamaki M, Ogawa O, Yoshimura N. Overexpression of platelet-derived endothelial cell growth factor/thymidine phosphorylase in patients with interstitial cystitis and bladder carcinoma. J Urol. 2002;167:347-351.
Uehling DT, Kelley E, Hopkins J, et al. Urinary glycosaminoglycan levels following induced cystitis in monkeys. J Urol. 1988;139:1103-1105.
Urban L, Nagy I, Bevan S. Chronic neuropathic pain: pathomechanism and pharmacology. Drug Dev Res. 2002;54:159-166.
Utz DC, Zincke H. The masquerade of bladder cancer in situ as interstitial cystitis. Trans Am Assoc Genitourin Surg. 1973;65:64-65.
Utz DC, Zincke H. The masquerade of bladder cancer in situ as interstitial cystitis. J Urol. 1974;111:160-161.
van Balken M, Vandoninck V, Gisolf K, et al. Posterior tibial nerve stimulation as neuromodulative treatment of lower urinary tract dysfunction. J Urol. 2001;166:914-918.
van de Merwe J, Kamerling R, Arendsen E, et al. Sjogren’s syndrome in patients with interstitial cystitis. J Rheumatol. 1993;20:962-966.
van de Merwe JP, Nordling J, Bouchelouche P, et al. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: an ESSIC proposal. Eur Urol. 2008;53:60-67.
van de Merwe JP, Yamada T, Sakamoto Y. Systemic aspects of interstitial cystitis, immunology and linkage with autoimmune disorders. Int J Urol. 2003;10(Suppl):S35-S38.
van Duzen RE, Mustain R. Alphatocopherol in treatment of interstitial cystitis: preliminary report. J Urol. 1951;65:1033-1035.
van Kerrebroeck PEV. Electrical stimulation in the management of interstitial cystitis. Urol Integrada Invest. 1999;4:331-334.
van Kerrebroeck PE, van Voskuilen AC, Heesakkers JP, et al. Results of sacral neuromodulation therapy for urinary voiding dysfunction: outcomes of a prospective, worldwide clinical study. J Urol. 2007;178:2029-2034.
van Ophoven A, Hertle L. Long term results of amitriptyline treatment for interstitial cystitis. J Urol. 2005;173:86.
van Ophoven A, Hertle L. The dual serotonin and noradrenaline reuptake inhibitor duloxetine for the treatment of interstitial cystitis: results of an observational study. J Urol. 2007;177:552-555.
van Ophoven A, Oberpenning F, Hertle L. Long-term results of trigone-preserving orthotopic substitution enterocystoplasty for interstitial cystitis. J Urol. 2002;167:603-607.
van Ophoven A, Pokupic S, Heinecke A, Hertle L. A prospective, randomized, placebo controlled, double-blind study of amitriptyline for the treatment of interstitial cystitis. J Urol. 2004;172:533-536.
van Ophoven A, Rossbach G, Oberpenning F, Hertle L. Hyperbaric oxygen for the treatment of interstitial cystitis: long-term results of a prospective pilot study. Eur Urol. 2004;46:108-113.
van Ophoven A, Rossbach G, Pajonk F, Hertle L. Safety and efficacy of hyperbaric oxygen therapy for the treatment of interstitial cystitis: a randomized, sham controlled, double-blind trial. J Urol. 2006;176:1442-1446.
Vander AJ. Renal physiology. New York: McGraw Hill Health Professions Division; 1995.
Vemulakonda V, Somogyi G, Kiss S, et al. Inhibitory effect of intravesically applied botulinum toxin A in chronic bladder inflammation. J Urol. 2005;173:621-624.
Vercellini P. Endometriosis: what a pain it is. Semin Reprod Endocrinol. 1997;15:251-261.
Verhaak PFM, Kerssens JJ, Dekker J, et al. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain. 1998;77:231-239.
Vliagoftis H, Dimitriadou V, Boucher W, et al. Estradiol augments while tamoxifen inhibits rat mast cell secretion. Int Arch Allergy Immunol. 1992;98:398-409.
Vrinten D, Kalkman C, Adan R, Gispen W. Neuropathic pain: a possible role for the melanocortin system? Eur J Pharmacol. 2001;429:61-69.
Wabner CL, Pak CYC. Effect of orange juice consumption on urinary stone risk factors. J Urol. 1993;149:1405-1408.
Wallack H, Lome LG, Presman D. Management of interstitial cystitis with ileocecocystoplasty. Urology. 1975;5:51-55.
Walsh A. Benzydamine: a new weapon in the treatment of interstitial cystitis. Trans Am Assoc Genitourin Surg. 1976;68:43-44.
Walsh A. Interstitial cystitis. Observations on diagnosis and on treatment with anti-inflammatory drugs, particularly benzydamine. Eur Urol. 1977;3:216-217.
Walsh A. Interstitial cystitis. In: Harrison JH, Gittes RF, Perlmutter AD, et al, editors. Campbell’s urology. Philadelphia: WB Saunders; 1978:693-707.
Walsh A. Cystolysis (supra-trigonal denervation) for intractable interstitial cystitis. Urologists’ Correspondence Club. 1985:142.
Wammack R, Remzi M, Seitz C, et al. Efficacy of oral doxepin and piroxicam treatment for interstitial cystitis. Eur Urol. 2002;41:596-600.
Warren JW. Is interstitial cystitis an infectious disease? Med Hypotheses. 1994;43:183-186.
Warren JW, Brown V, Jacobs S, et al. Urinary tract infection and inflammation at onset of interstitial cystitis/painful bladder syndrome. Urology. 2008;71:1085-1090.
Warren JW, Horne LM, Hebel JR, et al. Pilot study of sequential oral antibiotics for the treatment of interstitial cystitis. J Urol. 2000;163:1685-1688.
Warren JW, Howard FM, Cross RK, et al. Antecedent nonbladder syndromes in case-control study of interstitial cystitis/painful bladder syndrome. Urology. 2009;73:52-57.
Warren JW, Jackson TL, Langenberg P, et al. Prevalence of interstitial cystitis in first-degree relatives of patients with interstitial cystitis. Urology. 2004;63:17-21.
Warren JW, Keay SK, Meyers D, Xu J. Concordance of interstitial cystitis in monozygotic and dizygotic twin pairs. Urology. 2001;57:22-25.
Warren JW, Meyer WA, Greenberg P, et al. Using the International Continence Society’s definition of painful bladder syndrome. Urology. 2006;67:1138-1142.
Waxman JA, Sulak PJ, Kuehl TJ. Cystoscopic findings consistent with interstitial cystitis in normal women undergoing tubal ligation. J Urol. 1998;160:1663-1667.
Weaver RG, Dougherty TF, Natoli CA. Recent concepts of interstitial cystitis. J Urol. 1963;89:377-383.
Webster GD. Doctor’s forum. ICA Update. (summer):1993.
Webster GD, MacDiarmid SA, Timmons SL, et al. Impact of urinary diversion procedures in the treatment of interstitial cystitis and chronic bladder pain. Neurourol Urodyn. 1992;11:417.
Webster GD, Maggio MI. The management of chronic interstitial cystitis by substitution cystoplasty. J Urol. 1989;141:287-291.
Wei DC, Politano VA, Selzer MG, Lokeshwar VB. The association of elevated urinary total to sulfated glycosaminoglycan ratio and high molecular mass hyaluronic acid with interstitial cystitis. J Urol. 2000;163:1577-1583.
Wein A, Hanno PM, Gillenwater JY. Interstitial cystitis: an introduction to the problem. In: Hanno PM, Staskin DR, Krane RJ, Wein AJ, editors. Interstitial cystitis. London: Springer-Verlag; 1990:3-15.
Wein AJ, Broderick GA. Interstitial cystitis: current and future approaches to diagnosis and treatment. Urol Clin North Am. 1994;21:153-161.
Weisman MH, McDanald EC, Wilson CB. Studies of the pathogenesis of interstitial cystitis, obstructive uropathy, and intestinal malabsorption in a patient with systemic lupus erythematosus. Am J Med. 1981;70:875-881.
Weiss JM. Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J Urol. 2001;166:2226-2231.
Weiss JP, Neville EC. Hyperbaric oxygen: primary treatment of radiation-induced hemorrhagic cystitis. J Urol. 1989;142:43-45.
Weiss JP, Wein AJ, Hanno PM. Sigmoidocystoplasty to augment bladder capacity. Surg Gynecol Obstet. 1984;159:377-380.
Weissman MM, Gross R, Fyer A, et al. Interstitial cystitis and panic disorder: a potential genetic syndrome. Arch Gen Psychiatry. 2004;61:273-279.
Welk BK, Teichman JM. Dyspareunia response in patients with interstitial cystitis treated with intravesical lidocaine, bicarbonate, and heparin. Urology. 2008;71:67-70.
Wesselmann U. Interstitial cystitis: a chronic visceral pain syndrome. Urology. 2001;57:32-39.
Wesselmann U, Burnett AL, Heinberg LJ. The urogenital and rectal pain syndromes. Pain. 1997;73:269-294.
Wessely S, White P. There is only one functional somatic syndrome. Br J Psychiatry. 2004;185:95-96.
White WM, Mobley JDIII, Doggweiler R, et al. Incidence and predictors of complications with sacral neuromodulation. Urology. 2009;73:731-735.
Whitmore KE. Self-care regimens for patients with interstitial cystitis. Urol Clin North Am. 1994;21:121-130.
Whitmore KE, Payne CK, Diokno AC, Lukban JC. Sacral neuromodulation in patients with interstitial cystitis: a multicenter clinical trial. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14:305-308.
Wiesenfeld-Hallin Z, Xu X. Neuropeptides in neuropathic and inflammatory pain with special emphasis on cholecystokinin and galanin. Eur J Pharmacol. 2001;429:49-59.
Wilkins EG, Payne SR, Pead PJ, et al. Interstitial cystitis and the urethral syndrome: a possible answer. Br J Urol. 1989;64:39-44.
Wilson CB, Leopard J, Nakamura RM, et al. Selective type IV collagen defects in the urothelial basement membrane in interstitial cystitis. J Urol. 1995;154:1222-1226.
Wishard WNJr, Nourse MH, Mertz JH. Use of clorpactin WCS 90 for relief of symptoms due to interstitial cystitis. J Urol. 1957;77:420-423.
Worth PH. The treatment of interstitial cystitis by cystolysis with observations on cystoplasty: a review after 7 years. Br J Urol. 1980;52:232.
Worth PH, Turner-Warwick R. The treatment of interstitial cystitis by cystolysis with observations on cystoplasty. Br J Urol. 1973;45:65-71.
Worth PHL, Turner-Warwick R. Interstitial cystitis [letter]. BMJ. 1972;April 8:111-112.
Wu EQ, Birnbaum H, Kang YJ, et al. A retrospective claims database analysis to assess patterns of interstitial cystitis diagnosis. Curr Med Res Opin. 2006;22:495-500.
Wyndaele JJ. The normal pattern of perception of bladder filling during cystometry studied in 38 young healthy volunteers. J Urol. 1998;160:479-481.
Yamada T, Murayama T, Mita H, Akiyama K. Subtypes of bladder mast cells in interstitial cystitis. Int J Urol. 2000;7:292-297.
Yamaguchi O, Honda K, Nomiya M, et al. Defining overactive bladder as hypersensitivity. Neurourol Urodyn. 2007;26:904-907.
Yilmaz U, Liu YW, Rothman I, et al. Intravesical potassium chloride sensitivity test in men with chronic pelvic pain syndrome. J Urol. 2004;172:548-550.
Yoshimura N, de Groat WC. Increased excitability of afferent neurons innervating rat urinary bladder after chronic bladder inflammation. J Neurosci. 1999;19:4644-4653.
Yukawa S, Tahara K, Hayashi H, et al. [A case of lupus cystitis in a 74-year-old woman. Nihon Rinsho Meneki Gakkai Kaishi. 2008;31:183-189. [in Japanese]
Yun SK, Laub DJ, Weese DL, et al. Stimulated release of urine histamine in interstitial cystitis. J Urol. 1992;148:1145-1148.
Zaslau S, Riggs DR, Jackson BJ, et al. In vitro effects of pentosan polysulfate against malignant breast cells. Am J Surg. 2004;188:589-592.
Zeidman EJ, Helfrick B, Pollard C, et al. Bacillus Calmette-Guérin immunotherapy for refractory interstitial cystitis. Urology. 1994;43:121-124.
Zeng Y, Wu XX, Homma Y, et al. Uroplakin III-delta4 messenger RNA as a promising marker to identify nonulcerative interstitial cystitis. J Urol. 2007;178:1322-1327.
Zermann DH, Ishigooka M, Doggweiler R, Schmidt RA. Postoperative chronic pain and bladder dysfunction: windup and neuronal plasticity—do we need a more neurourological approach in pelvic surgery? J Urol. 1998;160:102-105.
Zermann D-H, Ishigooka M, Doggweiler R, Schmidt RA. Neurourological insights into the etiology of genitourinary pain in men. J Urol. 1999;161:903-908.
Zhao J, Bai J, Zhou Y, et al. Posterior tibial nerve stimulation twice a week in patients with interstitial cystitis. Urology. 2008;71:1080-1084.
Zuraw BL, Sugimoto S, Parsons CL, et al. Activation of urinary kallikrein in patients with interstitial cystitis. J Urol. 1994;152:874-878.