CHAPTER 53 Surgical Anatomy of Periodontal and Implant Areas
A sound knowledge of the anatomy of the periodontium and the surrounding hard and soft structures is essential to determine the scope and possibilities of periodontal and implant surgical procedures and to minimize their risks. The spacial relationship of bones, muscles, blood vessels, and nerves, as well as the anatomic spaces located in the vicinity of the periodontal/implant surgical field, are particularly important. Only those features of periodontal and implant surgery relevance are mentioned in this chapter; the reader is referred to books on oral anatomy for a more comprehensive description of these structures.4,6
Mandible
The mandible is a horseshoe-shaped bone connected to the skull by the temporomandibular joints. It presents several landmarks of great surgical importance for both periodontal and implant surgical procedures.
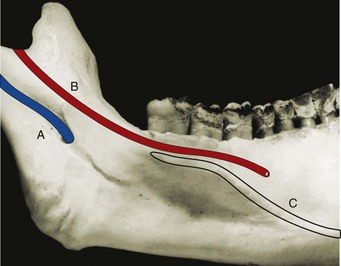
The mandibular canal, occupied by the inferior alveolar nerve and vessels, begins at the mandibular foramen on the medial surface of the mandibular ramus and curves downward and forward, becoming horizontal below the apices of the molars (Figure 53-1). The distance from the canal to the apices of the molars is shorter in the third molar area and increases as it goes forward. A small percentage (1%) of mandibular canals bifurcate in the body of the mandible, resulting in two canals and two mental foramen.5,10 In the premolar area, the mandibular canal divides in two branches, with one exiting the mandible and the other continuing anteriorly: the incisive canal, which continues horizontally to the midline, and the mental canal, which turns upward and opens in the mental foramen.
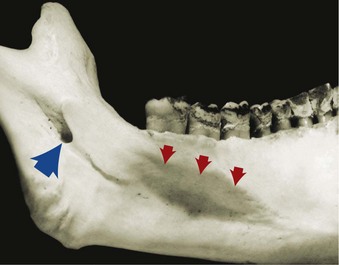
Figure 53-1 Mandible, lingual surface view. Note the lingual, or mandibular, foramen (blue arrow), where the inferior alveolar nerve enters the mandibular canal, and the mylohyoid ridge (red arrows).
The mental foramen, from which the mental nerve and vessels emerge, is located on the buccal surface of the mandible below the apices of the premolars, sometimes closer to the second premolar and usually halfway between the lower border of the mandible and the alveolar margin (Figure 53-2). It is often but not always visible on conventional radiographs. The opening of the mental foramen, which may be oval or round in shape, typically faces upward and distally, with its posterosuperior border slanting gradually to the bone surface. An “anterior loop” of the mental foramen has been described, using cadaver dissection, as a reverse turn and looping back of the mental nerve before its exit out of the mental foramen with lengths ranging from 0.5 to 5.0 mm.10 More recent evaluation of the anterior loop of the mental nerve using cone beam scans and cadaveric dissection reported this loop extension to range from 0.0 to 9.0 mm.22,23 The anterior loop of the mental nerve has a high prevalence (88%), symmetric occurrence, and a mean length of 4.13 ± 1.08 mm.18 As it emerges, the mental nerve divides into three branches. One branch of the nerve turns forward and downward to supply the skin of the chin. The other two branches course anteriorly and upward to supply the skin and mucous membrane of the lower lip and the mucosa of the labial alveolar surface.
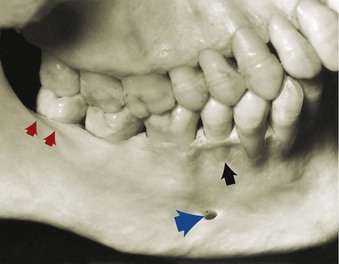
Figure 53-2 Mandible, facial surface view. Note the location of the mental foramen (blue arrow), slightly distal and apical to the apex of the second premolar, and the shelflike area in the region of the molars (red arrows), created by the external oblique ridge. Note also the fenestration present in the second premolar (black arrow).
Surgical trauma (e.g., pressure, manipulation, and postsurgical swelling) to the mental nerve can produce paresthesia of the lip, which recovers slowly. Partial or complete cutting of the nerve can result in permanent paresthesia/dysesthesia. Familiarity with the location and appearance of the mental nerve reduces the likelihood of injury (Figure 53-3).
In partially or totally edentulous jaws, the disappearance of the alveolar portion of the mandible brings the mandibular canal and mental foramen closer to the superior border (Figures 53-4 and 53-5). When these patients are evaluated for placement of implants, the distance between the canal and the superior surface of the bone, as well as the location of the mental foramen, must be carefully determined to avoid surgical injury to the nerve (see Chapter 70).
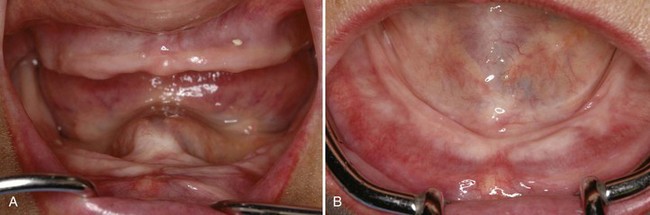
Figure 53-4 Loss of alveolar ridge in edentulous patient brings mental foramen and inferior alveolar nerve canal closer to the surface, which may lead to discomfort for the patient. A, Anterior view demonstrating severe loss of vertical alveolar ridge height. B, Occlusal view of same patient demonstrating loss of vestibular depth with alveolar bone loss.
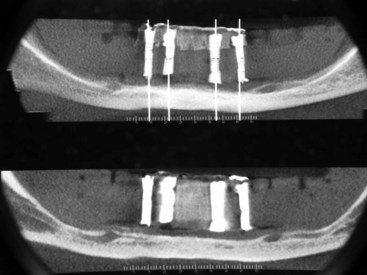
Figure 53-5 Panoramic radiograph of edentulous patient with loss of alveolar bone height resulting in the mental foramen exiting the jaw at the superior aspect of the remaining bone (ridge crest), which is the denture-bearing surface. Pressure from the complete removable denture over this area causes pain.
The anterior extension of the inferior alveolar nerve or incisive nerve has been measured using conventional radiographs, computed tomography (CT) scans, cadaver dissections and cone beam scans.3,10,22,23 This nerve, which is less evident on conventional radiographs and often unnoticed, extends beyond the anterior loop of the mental foramen in a horizontal direction toward the midline. The length of the incisive canal has been reported up to 21.45 mm from the mesial aspect of the mental foramen terminating just 4 mm from the midline.3
The lingual nerve, along with the inferior alveolar nerve, is a branch of the posterior division of the mandibular nerve and descends along the mandibular ramus medial to and in front of the inferior alveolar nerve. The lingual nerve lies close to the surface of the oral mucosa in the third molar area and goes deeper as it travels forward (Figure 53-6). It can be damaged during anesthetic injections and during oral surgery procedures such as third molar extractions.14 Less often, the lingual nerve may be injured when a periodontal partial-thickness flap is raised in the third molar region or when releasing incisions are made in the area.
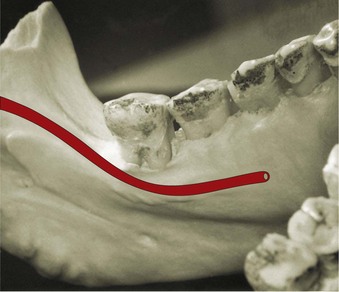
Figure 53-6 Lingual view of mandible showing the pathway of the lingual nerve (red), which goes near the gingiva in the third molar area and then continues forward, going deeper and medially.
The alveolar process, which provides the supporting bone to the teeth, has a narrower distal curvature than the body of the mandible (Figure 53-7), creating a flat surface in the posterior area between the teeth and the anterior border of the ramus. This results in the formation of the external oblique ridge, which runs downward and forward to the region of the second or first molar (Figure 53-8), creating a shelflike bony area. Resective osseous therapy may be difficult or impossible in this area because of the amount of bone that must be removed distally toward the ramus to achieve resection of a periodontal osseous defect on the distal aspect of the mandibular second/third molar.
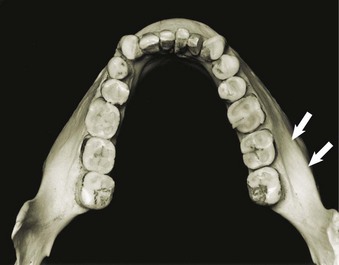
Figure 53-7 Occlusal view of mandible. Note the shelf created in the facial molar areas by the external oblique ridge. Arrows show the attachment of the buccinator muscle.
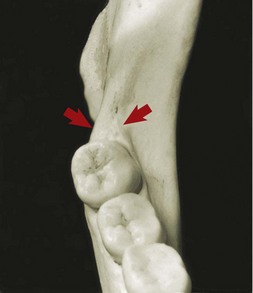
Figure 53-8 Mandible, occlusal view of ramus and molars. Note the retromolar triangle area distal to the third molar (arrows).
Distal to the third molar, the external oblique ridge circumscribes the retromolar triangle (see Figure 53-8). This region is occupied by glandular and adipose tissue and covered by unattached, nonkeratinized mucosa. If sufficient space exists distal to the last molar, a band of attached gingiva may be present; only in such a case can a distal flap procedure be performed effectively.
The medial side of the body of the mandible is traversed obliquely by the mylohyoid ridge, which starts close to the alveolar margin in the third molar area and continues anteriorly in an apical direction, increasing its distance from the osseous margin as it travels forward (Figure 53-9). The mylohyoid muscle inserts along this ridge and separates the sublingual space, located above or more anteriorly and superiorly, from the submandibular space, located below or more posteriorly and inferiorly.
Maxilla
The maxilla is a paired bone that is hollowed out by the maxillary sinus and nasal cavity. The maxilla has the following four processes:
The terminal branches of the nasopalatine nerve and vessels pass through the incisive canal, which opens in the midline anterior area of the palate (Figure 53-10). The mucosa overlying the incisive canal presents a slight protuberance called the incisive papilla. Vessels emerging through the incisive canal are of small caliber, and their surgical interference is of little consequence.
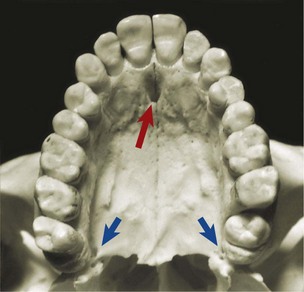
Figure 53-10 Occlusal view of maxilla and palatine bone. Note the opening of the incisive canal or anterior palatine foramen (red arrow) and the greater palatine foramen (blue arrows).
The greater palatine foramen opens 3 to 4 mm anterior to the posterior border of the hard palate (Figure 53-11). The greater palatine nerve and vessels emerge through this foramen and run anteriorly in the submucosa of the palate, between the palatal and alveolar processes (Figure 53-12). Palatal flaps and donor sites for gingival grafts should be carefully performed and selected to avoid invading these areas because profuse hemorrhage may ensue, particularly if vessels are damaged at the palatine foramen. Vertical incisions in the molar region should be avoided.
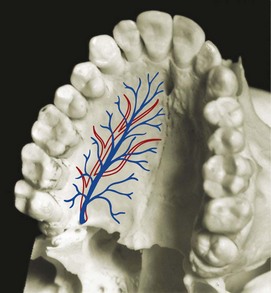
Figure 53-11 Occlusolateral view of palate showing nerves (red) and vessels (blue) emerging from the greater palatine foramen and continuing anteriorly on the palate.
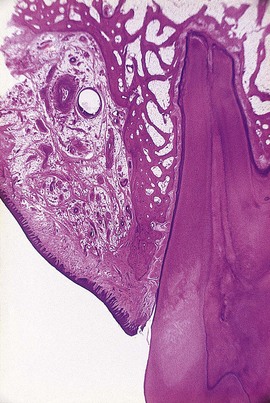
Figure 53-12 Histologic frontal section of human palate at the level of the first molar, showing the location of vessels and nerve, surrounded by adipose and glandular tissue.
The mucous membrane covering the hard palate is firmly attached to the underlying bone. The submucous layer of the palate posterior to the first molars contains the palatal glands, which are more compact in the soft palate and extend anteriorly, filling the gap between the mucosal connective tissue and the periosteum and protecting the underlying vessels and nerve (see Figure 53-22).
The area distal to the last molar, called the maxillary tuberosity, consists of the posterior-inferior angle of the infratemporal surface of the maxilla. Medially it articulates with the pyramidal process of the palatine bone. It is covered by dense, fibrous connective tissue and contains the terminal branches of the middle and posterior palatine nerves. Excision of the area for distal flap surgery may reach medially to the tensor palati muscle. The tensor palati muscle comes from the greater wing of the sphenoid bone and ends in a tendon that forms the palatine aponeurosis, which expands, fanlike, to attach to the posterior border of the hard palate.
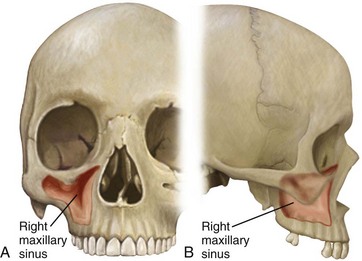
The body of the maxilla is occupied by the maxillary sinus, which is the largest of the paranasal sinuses. It is an air-filled cavity located in the posterior maxilla superior to the teeth. The lateral wall of the nasal cavity borders the sinus medially; it is bordered superiorly by the floor of the orbit and laterally by the lateral wall of the maxilla, the alveolar process, and the zygomatic arch (Figure 53-13). It is pyramidal in shape, with its apex in the zygomatic arch and its base at the lateral wall of the nasal cavity. The size of the maxillary sinus varies from one individual to another (depending on the individual and age), from very small and narrow to quite large and expansive.
The maxillary sinus is frequently subdivided (incompletely) into recesses by one or more septa. Maxillary sinus septa vary in size and location. Clinical and radiographic examinations suggest that septa are frequently present (up to 39% of sinuses).8,13,25 CT scans are the preferred method for detecting septa because panoramic radiographs are not reliable (26.5% false diagnosis of the presence or absence of septa).13,15 Septa are found in the anterior (24%), middle (41%), and posterior (35%) aspects of the maxillary sinus, with the most common location between the second premolar and the first molar.12,25 The height of septa vary as well, ranging from 0 to 20.6 mm.25 Only 0.5% of septa form complete separation of sinus spaces into separate chambers.16
The entire maxillary sinus is lined with a thin mucosal membrane called the schneiderian membrane. The specialized structure of the respiratory mucous membrane, with its motile cilia and rich blood supply, is well adapted to purifying, moistening, and warming air to protect the lungs. The entrance to the maxillary sinus, through the orifice or maxillary duct, is located at the superior medial aspect of the cavity. The orifice is relatively small, measuring only 3 to 6 mm in length and diameter. An accessory opening is occasionally found inferior and posterior to the main opening. The maxillary sinus drains into the middle meatus of the nasal cavity through the maxillary duct, which passes secretions medially to the semilunar hiatus. Normal amounts of secretion are moved from the sinus by the spiral pattern of beating cilia surrounding the orifice. If the maxillary sinus becomes infected or chronically inflamed, swelling of the mucosa around the orifice(s) impairs drainage. The floor of the maxillary sinus extends down below the level of the nasal cavity into the alveolar process.
The roots of the maxillary first and second molars are often close to the floor of the sinus. Less frequently, the roots of the premolars and third molars may protrude into the floor of the sinus. With increasing age the maxillary sinus expands, becoming more and more pneumatized down around the roots of the maxillary teeth, sometimes resulting in exposure of the roots through the bony floor into the sinus, with only the thin mucosal membrane covering the root surface. The ability to perform periodontal osseous surgery in the posterior maxilla may be limited when sinuses are severely pneumatized.
Blood supply to the maxillary sinus arises from the superior alveolar (anterior, middle, and posterior) branches of the maxillary artery (Figure 53-14, A).24 The maxillary artery, a large terminal branch of the external carotid artery, gives off many branches to supply the maxillary sinus, including the infraorbital artery, which travels superiorly and anteriorly and gives off the anterior superior alveolar artery.9 Branches of the greater palatine artery contribute to a lesser extent. Venous blood drains via the pterygoid plexus. Much of the vasculature travels through channels in the bony walls of the maxillary sinus, with many branches anastomosing with the highly vascularized schneiderian membrane. Innervation of the maxillary sinus is supplied by the superior alveolar (anterior, middle, and posterior) nerves, branches of the maxillary nerve (Figure 53-14, B).
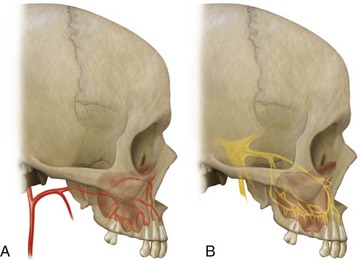
Figure 53-14 Blood supply and innervation of the maxillary sinus. A, Arterial blood supply. B, Innervation of the maxillary sinus.
Knowledge of the arterial blood supply is particularly important when considering a lateral window approach to sinus floor elevation and bone augmentation. Solar et al found an intraosseous branch of the posterior superior alveolar artery anastomosing with the infraorbital artery in 100% of their human cadaver specimens (134 sinuses, all males).19 On average, the vessel was located 18.9 mm from the alveolar crest. Using 50 CT scans from 625 patients (both males and females) undergoing sinus bone augmentation, Elian et al, found that the vessel was radiographically evident in 52.9% of sinuses.7 The vessel was located an average of 16.4 mm from the alveolar crest, which is consistent with the previous study. Human cadaver dissection and CT scan evaluations of the vessels running through the lateral wall of the maxillary sinus reveal that intraosseous vessels are present in the lower two thirds of the anterolateral wall in approximately 10.5% of cases (Figure 53-15).9 In 57.1% of cases (about 6% of all sinuses), the vessel diameter ranged in size from 1 to 2.5 mm. The location of the artery in relation to the position of the lateral window for sinus augmentation presents a risk for bleeding complications in 10-20% of cases.7,9
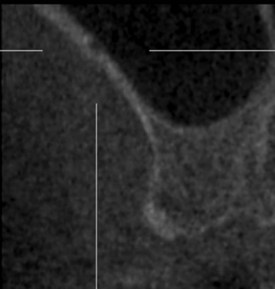
Figure 53-15 Cross-sectional image from a cone-beam computed tomography (CBCT) scan of the maxillary sinus demonstrating the presence of an intraosseous vessel in the lateral wall within the dimensions that a lateral window osteotomy would be created.
The inferior wall of the maxillary sinus is frequently separated from the apices and roots of the maxillary posterior teeth by a thin, bony plate (Figure 53-16). In edentulous posterior areas the maxillary sinus bony wall may be only a thin plate in intimate contact with the alveolar mucosa (Figure 53-17). Adequate determination of the extension of the maxillary sinus into the surgical site is important to avoid creating an oroantral communication, particularly in relation to osseous reduction in periodontal surgery or the placement of implants in edentulous areas. Determining the amount of available bone in the anterior area, below the floor of the nasal cavity, is also critical for the placement of implants (see Chapter 70).
Exostoses
Both the maxilla and the mandible may have exostoses or tori, which are considered to be within the normal range of anatomic variation. Sometimes these structures may hinder the removal of plaque by the patient and may have to be removed to improve the prognosis of neighboring teeth. Additional indications for the removal of exostoses include the inability to comfortably wear removable prostheses over these areas. The most common location of a mandibular torus is in the lingual area of canine and premolars, above the mylohyoid muscle (Figure 53-18). Mandibular tori can also be found on the buccal/labial surfaces of the mandibular teeth. Maxillary tori are usually located in the midline of the hard palate (Figure 53-19). Smaller tori may be seen over the palatal roots of the maxillary molars and in the area above the greater palatine foramen (see Figure 53-19) or on the buccal/labial surfaces of the maxillary teeth (Figure 53-20).
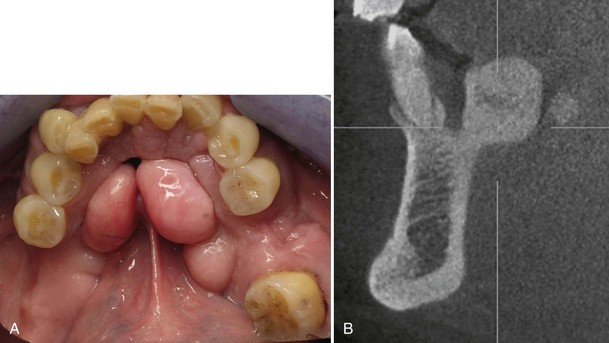
Figure 53-18 A, Clinical photograph of large mandibular tori on the lingual aspect of both right and left mandible. B, Same patient. Cross-sectional image of mandibular torus in the premolar area.
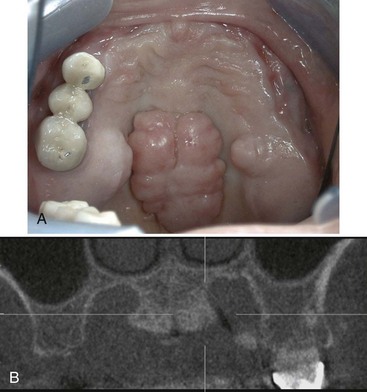
Figure 53-19 A, Clinical photograph of large palatal torus, located in the midline of the palate. Notice the large tori on the palatal aspects of the maxillary alveolar ridge as well. B, Same patient. Cross-sectional image of maxillary midline torus. Notice torus located on the palatal aspect of the alveolar ridge as well.
Muscles
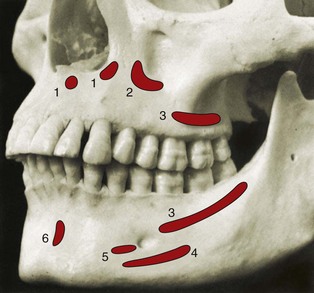
Several muscles may be encountered when performing periodontal and implant flap surgery, particularly in mucogingival surgery and bone augmentation procedures. These are the mentalis, incisivus labii inferioris, depressor labii inferioris, depressor anguli oris (triangularis), incisivus labii superioris, and buccinator muscles. Their bony attachments are shown in Figure 53-21. These muscles provide mobility to the lips and cheeks.
Anatomic Spaces
Several anatomic spaces or compartments are found close to the operative field of periodontal and implant surgery sites. These spaces contain loose connective tissue but can be easily distended by hemorrhage, inflammatory fluid, and infection.
Surgical invasion of these areas may result in dangerous hemorrhage (intraoperative) or infections (postoperative) and should be carefully avoided. Some of these spaces are briefly described here. For further information, the reader is referred to other sources.2,11,20,21
The canine fossa contains varying amounts of connective tissue and fat and is bounded superiorly by the quadratus labii superioris muscle, anteriorly by the orbicularis oris, and posteriorly by the buccinator. Infection of this area results in swelling of the upper lip, obliterating the nasolabial fold, and of the upper and lower eyelids, closing the eye.
The buccal space is located between the buccinator and the masseter muscles. Infection of this area results in swelling of the cheek but may extend to the temporal space or the submandibular space, with which the buccal space communicates.
The mental, or mentalis, space is located in the region of the mental symphysis, where the mental muscle, depressor muscle of the lower lip, and depressor muscle of the corner of the mouth are attached. Infection of this area results in large swelling of the chin, extending downward.
The masticator space contains the masseter muscle, pterygoid muscles, tendon of insertion of the temporalis muscle, and mandibular ramus and posterior part of the body of the mandible. Infection of this area results in swelling of the face and severe trismus and pain. If the abscess occupies the deepest part of this compartment, facial swelling may not be obvious, but the patient may complain of pain and trismus. Patients may also have difficulty and discomfort when moving the tongue and swallowing.
The sublingual space is located below the oral mucosa in the anterior part of the floor of the mouth. It contains the sublingual gland and its excretory duct, the submandibular or Wharton’s duct, and is traversed by the lingual nerve and vessels and hypoglossal nerve (Figure 53-22). Its boundaries are the geniohyoid and genioglossus muscles medially and the lingual surface of the mandible and below by the mylohyoid muscle laterally and anteriorly (Figure 53-23). Infection of this area raises the floor of the mouth and displaces the tongue, resulting in pain and difficulty in swallowing but little facial swelling.
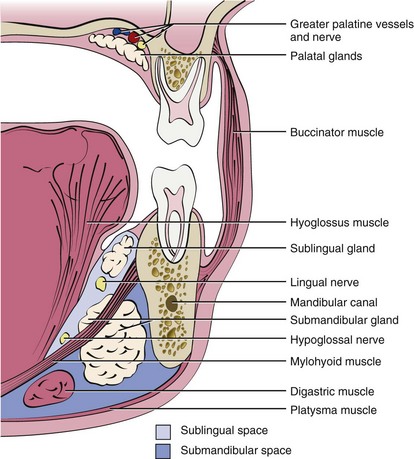
Figure 53-22 Diagram of a frontal section of the human head at the level of the first molars, depicting the most important structures in relation to periodontal surgery. Note the location of the sublingual space, submandibular space, and greater palatine nerve and vessels.
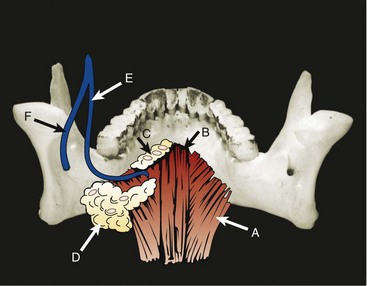
Figure 53-23 Posterior view of mandible, showing the attachment of the mylohyoid muscles (A); geniohyoid muscles (B); sublingual gland (C); submandibular gland (D), which extends below and also to some extent above the mylohyoid muscle; and sublingual (E) and inferior alveolar (F) nerves.
The submental space is found between the mylohyoid muscle superiorly and the platysma inferiorly. It is bounded laterally by the mandible and posteriorly by the hyoid bone. It is traversed by the anterior belly of the digastric muscle. Infections of this area arise from the region of the mandibular anterior teeth and result in swelling of the submental region; infections become more dangerous as they proceed posteriorly.
The submandibular space is found external to the sublingual space, below the mylohyoid and hyoglossus muscles (see Figures 53-22 and 53-23). This space contains the submandibular gland, which extends partially above the mylohyoid muscle, thus communicating with the sublingual space, and numerous lymph nodes. Infections of this area originate in the molar or premolar area and result in swelling that obliterates the submandibular line and in pain when swallowing. Ludwig’s angina is a severe form of infection of the submandibular space that may extend to the sublingual and submental spaces. It results in hardening of the floor of the mouth and may lead to asphyxiation from edema of the neck and glottis. Although the bacteriology of these infections has not been completely determined, they are presumed to be mixed infections with an important anaerobic component.1,17
![]() Science Transfer
Science Transfer
Consideration of the surgical anatomy serves as a basis for surgical procedures involving periodontal tissues and implants. Damage to nerves, such as the mental nerve, the mandibular nerve, and the lingual nerve, can be avoided with proper technique and treatment planning that should include three-dimensional radiographs when these structures are likely to be within the vicinity of surgical approaches. Penetration of the mandibular lingual bony plate during implant placement can cause hemorrhage into the sublingual and submandibular spaces, with possible life-threatening elevation of the tissues and respiratory obstruction. Infection spreading into these regions is also dangerous, and clinicians must be aware of these anatomic implications. Inadvertent surgical incision of major blood vessels, such as the greater palatine artery and the middle and posterior superior alveolar artery, can be avoided by knowledge of their anatomic positioning.
1 Bartlett JG, Gorbach SL. Anaerobic infections of the head and neck. Otolaryngol Clin North Am. 1976;9:655-678.
2 Clarke MA, Bueltmann KW. Anatomical considerations in periodontal surgery. J Periodontol. 1971;42:610-625.
3 De Andrade E, Otomo-Corgel J, Pucher J, Ranganath KA, St George NJr. The intraosseous course of the mandibular incisive nerve in the mandibular symphysis. Int J Periodontics Restorative Dent. 2001;21:591-597.
4 Dixon AD. Anatomy for students of dentistry. New York: Churchill Livingstone; 1986.
5 Driscoll CF. Bifid mandibular canal. Oral Surg Oral Med Oral Pathol. 1990;70:807.
6 DuBrul EL. Sicher and DuBrul’s oral anatomy. St. Louis: Ishiyaku EuroAmerica; 1988.
7 Elian N, Wallace S, Cho SC, Jalbout ZN, Froum S. Distribution of the maxillary artery as it relates to sinus floor augmentation. Int J Oral Maxillofac Implants. 2005;20:784-787.
8 Ella B, Noble Rda C, Lauverjat Y, Sedarat C, Zwetyenga N, Siberchicot F, Caix P. Septa within the sinus: effect on elevation of the sinus floor. Br J Oral Maxillofac Surg. 2008;46:464-467.
9 Ella B, Sedarat C, Noble Rda C, Normand E, Lauverjat Y, Siberchicot F, Caix P, Zwetyenga N. Vascular connections of the lateral wall of the sinus: surgical effect in sinus augmentation. Int J Oral Maxillofac Implants. 2008;23:1047-1052.
10 Greenstein G, Tarnow D. The mental foramen and nerve: clinical and anatomical factors related to dental implant placement: a literature review. J Periodontol. 2006;77:1933-1943.
11 Gregg JM. Surgical Anatomy. St. Louis: Mosby; 1980.
12 Jovanovic SA, Nevins M. Bone formation utilizing titanium-reinforced barrier membranes. Int J Periodontics Restorative Dent. 1995;15:56.
13 Kasabah S, Slezak R, Simunek A, Krug J, Lecaro MC. Evaluation of the accuracy of panoramic radiograph in the definition of maxillary sinus septa. Acta Medica (Hradec Kralove). 2002;45:173-175.
14 Kiesselbach JE, Chamberlain JG. Clinical and anatomic observations on the relationship of the lingual nerve to the mandibular third molar region. J Oral Maxillofac Surg. 1984;42:565-567.
15 Krennmair G, Ulm C, Lugmayr H. Maxillary sinus septa: incidence, morphology and clinical implications. J Craniomaxillofac Surg. 1997;25:261-265.
16 Krennmair G, Ulm CW, Lugmayr H, Solar P. The incidence, location, and height of maxillary sinus septa in the edentulous and dentate maxilla. J Oral Maxillofac Surg. 1999;57:667-671. discussion 671-662
17 Mulligan MR. Ear, nose, throat, and head and neck infections. San Diego: Academic Press; 1989.
18 Neiva RF, Gapski R, Wang HL. Morphometric analysis of implant-related anatomy in Caucasian skulls. J Periodontol. 2004;75:1061-1067.
19 Solar P, Geyerhofer U, Traxler H, Windisch A, Ulm C, Watzek G. Blood supply to the maxillary sinus relevant to sinus floor elevation procedures. Clin Oral Implants Res. 1999;10:34-44.
20 Spilka CJ. Pathways of dental infections. J Oral Surg. 1966;24:111-124.
21 Topazian RG, Goldberg MH, Hupp JR. Oral and Maxillofacial Infections. Philadelphia: W. B. Saunders; 2002.
22 Uchida Y, Noguchi N, Goto M, Yamashita Y, Hanihara T, Takamori H, Sato I, Kawai T, Yosue T. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region: a second attempt introducing cone beam computed tomography. J Oral Maxillofac Surg. 2009;67:744-750.
23 Uchida Y, Yamashita Y, Goto M, Hanihara T. Measurement of anterior loop length for the mandibular canal and diameter of the mandibular incisive canal to avoid nerve damage when installing endosseous implants in the interforaminal region. J Oral Maxillofac Surg. 2007;65:1772-1779.
24 van den Bergh JP, ten Bruggenkate CM, Disch FJ, Tuinzing DB. Anatomical aspects of sinus floor elevations. Clin Oral Implants Res. 2000;11:256-265.
25 Velasquez-Plata D, Hovey LR, Peach CC, Alder ME. Maxillary sinus septa: a 3-dimensional computerized tomographic scan analysis. Int J Oral Maxillofac Implants. 2002;17:854-860.