CHAPTER 74 Esthetic Management of Difficult Cases (Minimally Invasive Approach)
In recent years, implant dentistry has been increasingly influenced by esthetic considerations. In addition to successful osseointegration, harmonious soft and hard tissues must surround the implant restorations so that they look natural and healthy. A major challenge in implant dentistry is that, in many instances, dental implants need to be placed in an esthetic zone in which there is extensive alveolar bone deficiency from tooth loss, dentoalveolar infection, or other pathology (Figure 74-1, A to C). Gingival morphology follows the shape of the underlying bone, and it is difficult to build esthetically acceptable gingiva in areas with deficient supporting bone. Furthermore, using conventional surgical approaches to accomplish the goal in a patient-friendly manner with minimal trauma and clinical predictability is an extremely demanding task.
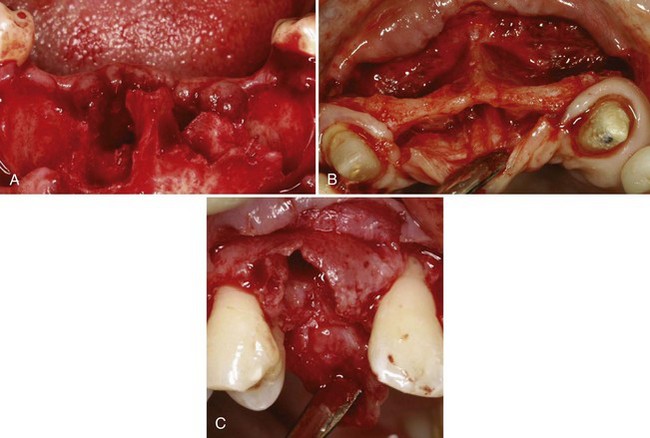
Figure 74-1 Implant sites in the anterior, esthetic zone with extensive bone loss. A, Anterior mandibular site showing extensive bone loss following extraction of hopelessly infected mandibular incisors. B, Extremely narrow (labial-palatal) ridge width in the anterior maxilla that was missing centrals and laterals for many years. C, Moderate bone loss associated with the extraction socket of a maxillary cuspid.
Treatment planning in a complex implant case today is often confusing because there are many different surgical and restorative approaches to solve the same problem. Many times these procedures seem to conflict. When considering the surgical placement of implants, clinicians must consider the approach (conventional two-stage approach versus a one-stage approach) and the timing of implant placement (immediate versus delayed or staged placement). For bone augmentation procedures, there is the more conventional approach of augmenting the ridge first and placing the implant(s) after healing, or the simultaneous implant placement with bone augmentation approach in which bone grafting is done at same time as implant placement. All of these approaches can provide a successful outcome if patient selection is appropriate and techniques are performed properly.9,22,24,32 However, depending on the situation, some of these techniques are more advantageous than others in achieving esthetic results with better predictably and less patient discomfort.
It is easy for a clinician to “dogmatically” choose one approach, usually choosing the one that he or she feels most comfortable with, and to treat all patients with the same approach. However, with heightened expectations of esthetics pushing the art and science of dentistry, it is necessary more than ever for clinicians to fully understand all the available options of treatment and decide appropriately which, where, when, and how to utilize these options for each patient.
An important recent clinical development in dental implant surgery is the concept of “minimally invasive” approaches to treatment. Specifically, there is a new drive toward minimally invasive implant placement. With advances in technologies, materials, and biologic sciences in dentistry, this approach to implant surgery is becoming more popular among clinicians and will most likely dominate the way dental implants will be placed in the near future.
Minimally invasive surgery in implant dentistry implies a surgical approach that minimizes the extent and number of surgeries while providing esthetics, predictability, and longevity with minimal surgical morbidity and discomfort to patients. The surgical approach most often required to achieve these goals for anterior implant therapy involves immediate implant placement, one-stage surgical approach, with or without flap, and simultaneous bone grafting. Furthermore, these surgical techniques need to be guided by a consistent surgical strategy that provides predictable esthetic results in implant dentistry. A minimally invasive approach to implant therapy in posterior sextants in which esthetics is not a major concern can be predictably achieved with the use of short wide implants.2,15,16,27
This chapter introduces surgical strategies that enhance the esthetic predictability in implant dentistry. The minimally invasive surgical approach to manage difficult esthetic and anatomically deficient cases is discussed with examples. The one-stage, immediate implant placement technique, which is the foundation of a patient-friendly approach to esthetic implant dentistry, is presented in detail. The thought processes involved in case selection, their scientific rationale, and proper techniques of soft and hard tissue management are described with cases.
Surgical Strategy for Predictable Esthetics
Observation of and adherence to the following surgical strategies enhance predictability and outcomes for esthetic dental implant surgeries with minimal discomfort to patients:
Determine the Level of Surgical Esthetic Goal
In dental implant therapy, it is important to determine from the onset the level of surgical esthetic goal. To determine the treatment needs, it is important to assess the patient’s esthetic expectations and to consider their age, medical condition, time constraints, and finances as well as the status of existing soft and hard tissue. The ability and experience of the clinician must also be factored into the determination.
The surgical esthetic goal can be ideal, acceptable, or compromised. An ideal surgical esthetic goal (Figure 74-2) implies an ideal, complete surgical reproduction of periimplant tissue around an implant restoration. An acceptable surgical esthetic goal (Figure 74-3) implies that the esthetics of the final implant restoration and the periimplant tissue is not ideal, but both the patient and the clinician accept it. Also, the hygiene and the long-term health of the restoration is not compromised. A compromised surgical esthetic goal (Figure 74-4) implies that the esthetic, hygiene, and long-term health of the implant is far below what is acceptable in today’s clinical standard.

Figure 74-2 Ideal surgical esthetic goal. Clinical photograph of an implant-supported crown replacing maxillary right cuspid in a 20-year-old female with a high smile line. Soft tissues are full and contours appear natural.

Figure 74-3 Acceptable surgical esthetic goal. Clinical photograph of implant-supported crowns replacing multiple missing maxillary anterior teeth in a 63-year-old female with a low smile line. Soft tissues are nearly full and contours appear fairly normal but not ideal.

Figure 74-4 Compromised surgical esthetic goal. Severe ridge deficiency resulted in long implant-supported fixed restoration and difficult oral hygiene access. Notice the pink porcelain used to mask the increased length of the crowns. Soft tissues are obviously compromised and completely lack any semblance of normal.
In general, more surgeries are required to achieve esthetic results that are close to ideal. The treatment time is usually much longer, and the cost is much higher. There is more surgical morbidity for the patient, and the ideal esthetic outcome remains illusive and often is not achieved.
Because of the logistic consequences of this decision, the level of the esthetic goal should be determined at the beginning of treatment so that the patient is well informed about treatment costs and time requirements. Many clinicians feel it is over-treatment to attempt ideal esthetics for all patients.
Visualize the Final Outcome
Once the level of the esthetic goal is determined, the next step is to visualize the final outcome. Determination of the vertical position of the implant, quantity and quality of the soft and hard tissue augmentation needed, components of the alveolar tissue that need to be preserved in surgery, and what surgical approach is most appropriate for the patient cannot be accomplished without first visualizing the final esthetics of the implant restoration(s) involved. In simple cases, the visualization can be done mentally or with the aid of computer graphic simulation. In more complex cases, a diagnostic wax-up may be necessary.38
Preserve Existing Tissues Important for Esthetics
Once what needs to be accomplished surgically is decided through visualization of the esthetics of the final restorations, the next step is determining what aspects of the soft and hard tissues need to be preserved for a predictable esthetic result. For example, if the initial vertical position of the interdental papilla is esthetically compatible with the image of the final restorations, it is prudent to preserve them rather than needing to rebuild them after they are lost. Knowing what needs to be preserved will help assist in choosing an appropriate surgical approach.
Always Overbuild Bone and Soft Tissue in Augmentation Surgeries
Many studies have shown that there is rapid labial and vertical bone loss after extractions,3,26,30 and immediate implant placement does not stop the resorption process.10,12,35 Furthermore, it has been demonstrated that soft and hard tissues grafted in augmentation procedures to enhance esthetics undergo extensive shrinkage within 3 to 6 months.1,36 Therefore the deficient ridge needs to be overbuilt by approximately 30% to 40% at the time of surgery to be esthetically sufficient after the expected primary and secondary tissue shrinkage.
Immediate Implant Placement for Predictability and Esthetics
Immediate implant placement in a one-stage approach, in which a healing abutment or provisional restoration is attached to the implant and remains exposed, provides more predictable preservation of the interproximal periimplant gingival tissue with less patient discomfort and treatment time.21,22 This approach to implant placement is the foundation of a minimally invasive approach to esthetic implant dentistry. However, as with any surgical technique, it takes learning and practice to perform it properly. The criteria and techniques for proper immediate implant placement have previously been established and reported with successful long-term outcomes.18,32
One of the more difficult aspects of immediate implant placement is positioning the implant with sufficient primary stability in an extraction socket, often without elevating a flap. The alveolar architecture in relation to the angle of the implant to be inserted; the presence or absence of a bone concavity apical to the extracted tooth; the amount of existing bone apical and palatal to the extraction socket, which can provide primary stability for the immediate implant; and the quality of the bone and soft tissues of the ridge should all be thoroughly evaluated clinically and radiographically before surgery.18,32 Many clinicians perform successful immediate implant placement without the aid of a three-dimensional scans (e.g., computed tomography [CT] or cone-beam CT [CBCT]). However, if the tooth involved is long and large or if there is an alveolar concavity or other anatomic variations, the use of a CT/CBCT scan is advised.
A major disadvantage of placing implants immediately in the changing alveolar bone of an extraction socket is that it may result in progressive recession of the gingival labial margin over the implant restoration.4,17 Therefore, when placing an immediate implant with one-stage surgical approach in an esthetic zone, a prudent strategy would be to improve the quality and quantity of labial gingival tissue, which seems to be vital for the stability of the labial gingival margin involving immediate implants.19,31 One of the most effective ways to keep the implanted socket from collapsing and improve the labial gingival biotype is to simultaneously fill the labial socket void with particulate bone and augment the labial gingival tissue with soft tissue.3,23,26,30,32
An effective bone and gingival tissue augmentation technique used with flapless immediate implant placement in a one-stage approach is the bone and crescent-shaped free gingival grafting technique.18 In this technique, the space between the inner surface of the labial bony wall and the labial surface of the implant is filled with slow-resorbing mineralized, freeze-dried particulate bone allograft (FDBA) or particulate xenograft to help preserve the horizontal dimension of the ridge (Figure 74-5, A). Then, a crescent-shaped soft tissue graft is harvested from the ipsilateral palate (Figure 74-5, B) and transplanted into the labial recipient site coronal to the particulate bone graft (Figure 74-5, C). To provide/maintain the blood supply to the donor tissue, it is important that the outer surface of the crescent graft fits with an intimate contact with the bleeding lamina propria of the labial gingiva. Proper suturing ensures good proximity and prevents the graft from being displaced coronally out of the recipient site (Figure 74-5, D).
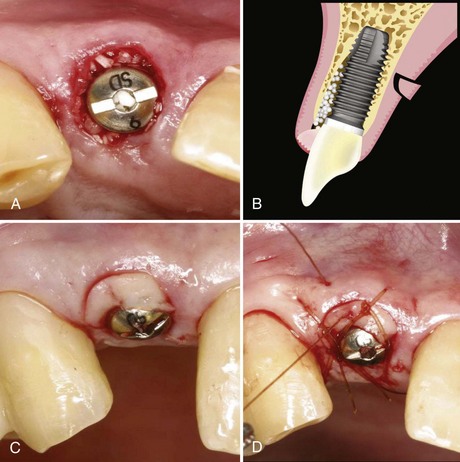
Figure 74-5 A, Bone graft material is lightly packed into the extraction socket gap between the labial wall and the implant surface. B, Diagram of crescent-shaped, free gingival graft tissue being harvested from the palate. C, Clinical photograph of crescent-shaped, free gingival graft tissue positioned over the bone graft to fit snuggly in the gap between the gingival wall and the implant surface. D, Crescent-shaped, free gingival graft is sutured in place using 5-0 gut sutures. The sutures pass through the gingival graft toward the labial gingival margin and are tied. Then, without cutting the ends, the suture is passed over the graft and tied to the palatal gingival tissue. Three sutures are needed to keep the graft in position.
The advantage of this approach to gingival augmentation is simplicity and minimal surgical morbidity. In addition to providing a sealed protection for the bone graft, it prevents resorption of the sensitive labial crestal bone. Preparation of the recipient site involves no surgical manipulation other than de-epithelialization as described. Gingival walls are completely intact with a full blood supply. The donor site wound is small (approximately 3 mm depth × 3 mm height at the widest point) with intact epithelium around the wound, which epithelializes within a week and causes minimal discomfort for the patient. Since each donor tissue graft is small, multiple grafts can be harvested from a single palate, so that multiple immediate implants can be augmented at same time. Furthermore, this gingival augmentation technique frequently improves an unfavorable initial gingival margin since the grafted gingival margin is always coronal to the existing gingival margin. This minimizes a need for other time-consuming techniques, such as orthodontic extrusion, or a delayed approach to implant placement when the initial gingival margin is not esthetic or ideal, as recommended by many authors.5,33
The risk-to-benefit ratio of the crescent grafting technique is favorable enough that if the graft does not survive, or if more than expected horizontal resorption of the ridge occurs, traditional techniques (e.g., subepithelial connective tissue graft) can be performed to augment the results. This is usually possible without refabrication of the implant restoration because the vertical height of the interdental papilla is sufficiently preserved with immediate implant placement in a one-stage approach.
Surgical Management of Difficult Cases (Minimally Invasive Approach)
The cause of the failure to satisfy the esthetic needs of a patient frequently starts with an inadequate examination of the soft and hard tissues surrounding the surgical site and the natural dentition. This can result in an incorrect diagnosis, which leads to incorrect treatment plan. The wrong treatment plan combined with selection of inappropriate surgical approaches or techniques can result in a disastrous esthetic outcome and unnecessary patient suffering. The first two case presentations describe the examination and thought processes involved in determining the diagnosis and treatment planning of complex anterior cases with extensive alveolar bone loss. The proper application of the surgical strategies and the minimally invasive techniques, previously described, are illustrated. The final case presentation illustrates the minimally invasive approach to posterior implant therapy with the use of short wide implants, in which esthetics is not the major concern.2,15,16,27
Components of Esthetic Examination
The patient’s chief complaint, esthetic zone, tooth positions, gingival form, osseous crest position, biotype, tooth shape, horizontal and vertical ridge deficiency, and occlusal status all play an important role in deriving an accurate esthetic treatment plan for the patient. Therefore developing the necessary skill and knowledge to examine and recognize problems of these components is an essential first step to clinical success.
Case Presentation 1
The first case presented is a simultaneous bone and soft tissue augmentation with multiple maxillary anterior immediate implants placed in a one-stage, flapless approach.
Patient Dental History and Chief Complaint
The patient is a 70-year-old female with severe mobility and discomfort of the maxillary four incisors. Except for a generalized feeling of weakness, she is healthy and does not have any medical contraindications for dental treatment. She presented with a desire to replace her maxillary incisors with dental implants, but she is very concerned about the physical discomfort she may experience from the implant surgery. She does not want to wear a removable prosthesis at all, not even for a short time. She is content with her present dental esthetics.
Examination and Diagnosis
The maxillary incisors exhibit moderate-to-severe periodontitis with 4 to 7 mm periodontal probing depths. They exhibit severe (2+) mobility with fremitus. The periodontal and restorative prognosis of these teeth is poor. She has an excessive overbite with evidence of moderate mandibular incisor wear, indicating possible parafunctional habits. Her incisors are slightly elongated, but the dentogingival symmetry is acceptable (Figure 74-6, A). The shape of the incisors is slightly triangular with sufficient interdental papilla volume and height. Interproximal gingival tissue is not swollen or edematous. Her gingival biotype appears to be on the thin side with slight marginal inflammation, and the position of the labial gingival margins is already high (i.e., maximal apical position). Any further recession will be unaesthetic.

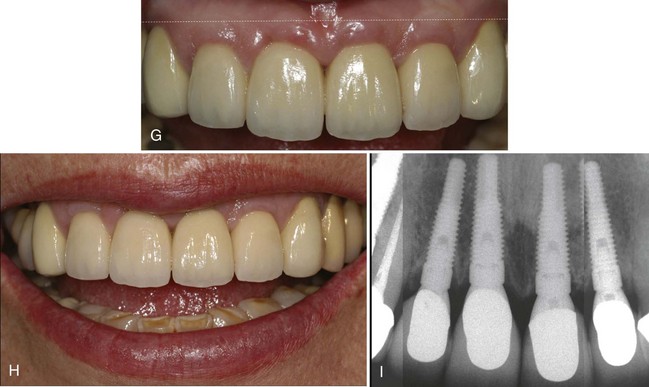
Figure 74-6 A, Clinical photograph of periodontally compromised maxillary anterior teeth with long clinical crowns. The presenting esthetic status is not ideal. However, the dentogingival symmetry is fair since the gingival margin is approximately the same for all incisors (cuspids, laterals, and centrals). B, Periapical radiographs of the maxillary anterior teeth reveal moderate to severe horizontal periodontal bone loss with vertical intrabony defects. C, Simple, atraumatic extraction of the maxillary incisors reveals sockets with unsupported interdental tissues. Note that there are no incisions or flap reflection, which has preserved the blood supply and integrity of the interdental soft tissues. D, Guide pins placed in prepared implant sites reveal good position within the extraction sockets achieving good primary stability from the palatal aspect of the socket. E, Implants with temporary abutments and crescent shaped, free gingival grafts (not yet sutured). F, Implant provisional abutments are prepared and provisional restorations are fabricated using conventional methods. G, One-year postloading results show nearly complete preservation of the interproximal papilla height and improved labial gingival biotype. Labial gingival margins are substantially coronal in position as compared to the initial levels. H, The final restorations have a more normal length offering the patient a much more youthful smile. Preexisting moderate to severe attrition is noted on the incisal edges of the mandibular anterior teeth. I, Periapical radiographs at 1 year of the implants with final restorations reveal good preservation of interproximal bone height with minimal saucerization. The platform-switched implant restorations likely contribute to the preservation of bone.
Radiographic evaluation demonstrates moderate-to-severe vertical and horizontal periodontal bone loss. The osseous crest position, in relation to the gingival margins, appears too apical to provide adequate gingival support (Figure 74-6, B). The restorative and periodontal status of the canines is healthy.
Treatment Objectives
Considering her age, reasonable esthetic expectation, concern for surgical morbidity, and a lack of willingness to wear a removable provisional prosthesis, the treatment objective for this patient would be to utilize a surgical approach that minimizes the extent and number of surgical procedures while providing predictability, longevity, and acceptable esthetics. Recommending orthodontic extrusion or multiple surgeries to achieve ideal esthetics on this patient would be considered an excessive treatment plan and would not provide any additional value or benefits for her.
Treatment Options
Considerations for extracting four maxillary incisors include the need to remove sound (porcelain-fused-to-metal) PFM crowns from the canines to replace them as part of a 6-unit fixed prosthesis. This option has questionable long-term functional and esthetic prognosis. Her dentition exhibits evidence of excessive overbite and parafunctional habit, which may have contributed to the alveolar bone loss of the incisors in the first place. The convex shape of the ridge and the lack of osseous support most likely result in substantial horizontal and vertical resorption of the edentulous ridge under the pontics of the fixed bridge, even with extraction socket grafting and ovate provisionalization. This will compromise the long-term esthetics.
Even if this patient can tolerate the temporary removable partial denture, which she said she could not, this option poses a considerable esthetic challenge. The ridge surrounding the extraction sockets will rapidly lose vertical and horizontal dimensional soon after the extractions.3 The loss of vertical height in the interproximal gingival areas creates an esthetic problem that is very difficult to correct. It often requires multiple surgeries that have a high incidence of surgical morbidity and rarely achieves the desired ideal esthetic result. This is especially true in a case like this in which there is extensive periodontal vertical and horizontal bone loss. The anticipated vertical ridge collapse after the extraction is substantial, even with bone grafting of the extraction sockets. More importantly, the need for multiple surgeries to achieve “acceptable” esthetic results for this patient may be too traumatic for her.
Extracting four maxillary incisors, immediately placing two implants, and replacing the teeth with a 4-unit provisional fixed partial denture supported by two implants is an acceptable but risky treatment option. Immediate provisionalization of the two immediately-placed implants with her occlusion and suspected parafunctional habit carries the risk of early excessive loading and implant failure. Additionally, it will be challenging to maintain the vertical and horizontal ridge dimensions in the edentulous area under the pontics. Most likely it will require additional soft tissue augmentation procedure(s) to achieve “acceptable” esthetics in the pontic area (i.e., missing central incisor area).
Extracting four maxillary incisors, immediately placing four implants in the sockets, and replacing the missing teeth with a 4-unit provisional fixed partial denture supported by four implants is another acceptable option. Splinting four provisionals together should provide sufficient resistance and protection to the implants from early excessive loading. Some clinicians do not recommend placing implants next to each other in the lateral and central incisor positions because they are often positioned too close and it is very difficult to create or maintain an interdental papilla that emulates an interdental papilla between an implant and a tooth or between two natural teeth.39 However, the more recent use of implants with a platform-switching design may change the spatial requirements for achieving an interdental papilla between implants. The bone between implants appears to be better protected, and as a result, the vertical height of the interproximal tissue may be better preserved.8,25 If procedures are carried out properly, this option can provide a long-term functional and esthetic result, with minimal discomfort to the patient.
Surgical Strategy for Predictable Esthetics
Because of the patient’s age and reasonable expectation, the level of the esthetic goal determined for this patient is not ideal but is acceptable. This level of esthetics can be predictably achieved in a minimally invasive, patient-friendly manner. By mentally visualizing the surgical and prosthetic goal, an acceptable esthetic outcome can be achieved for this patient if the existing heights of the interproximal gingival tissues can be maintained. Additionally, if the existing biotype and the level of the labial gingival margin can be overbuilt with hard and soft tissue augmentation, the final esthetic outcome is enhanced. If this can be accomplished with simultaneous implant placement, it minimizes the number of surgeries required. In this case, especially since the patient appears to have parafunctional habits, it is desirable to place more implants and use them to support the immediate provisionalization.
Considering all of these treatment options, the treatment that is most compatible with this patient’s surgical strategy for predictability, acceptable esthetics, and long-term results is treatment option 4, extraction of the incisors followed by immediate placement of four implants with an immediate provisional restoration supported by the implants.
Treatment Plan and Rationale
Four maxillary incisors are to be extracted, and four implants placed immediately in a one-stage approach with simultaneous bone and soft tissue grafting. The bone and crescent-shaped free-gingival grafting technique is used to overbuild labial gingival biotype.18 A tapered implant with platform-switching design is to be utilized. The tapered design has shown to promote primary stability in sockets, and the platform-switching design better maintains the interimplant bone.8,25 An immediate provisional restoration without centric contacts is attached to the implants.
Treatment Sequence
In complex treatment involving dental implants, the treatment plan must be sequenced and coordinated between the restorative dentist and the surgeon before starting the treatment. This is especially true when immediate provisionalization is planned. This will enhance success and help make the treatment more patient friendly.
Surgical Procedure
Once the patient is anesthetized, the incisors are extracted atraumatically, ensuring that gingival tissues, especially the interdental papilla are not damaged (Figure 74-6, C). The sockets are prepared to receive implants by removing the sulcular epithelium, and by completely and thoroughly removing all granulation tissue. Immediately placed implants must have complete primary stability at the time of placement. Proper vertical position, buccolingual position, and mesiodistal position, as well as buccolingual angulation, are all critical factors for a successful outcome. Implants in anterior sockets are prepared and placed toward the palate (Figure 74-6, D) to ensure sufficient labial bone thickness for labial margin stability.9 Once the provisional healing abutments are accurately seated (may require bone profiler), the labial void of the sockets are grafted with particulate bone and a crescent-shaped free gingival tissue graft is harvested and placed over the graft (Figure 74-6, E) as described previously and in the literature.18 Using this technique, all four teeth can be augmented in one surgery with minimal discomfort to the patient. Once the soft tissue crescent grafts are secured with sutures, the provisional abutments are prepared for provisional crowns. The provisional crowns (splinted) are fabricated using conventional methods (Figure 74-6, F). Contours of the provisional crowns may need to be modified as the healing and remodeling occurs. Impression taking for the final restoration is relatively easy because the provisional abutments placed at the time of surgery and modified during healing nicely shape the tissues for an optimal prosthetic emergence profile.
Results
The 1-year result shows nearly complete preservation of the interproximal papilla height, an improved labial biotype with labial gingival margins that are substantially coronal to the original gingival margin level (Figure 74-6, G). The final result is crowns with a more normal incisor length and a more youthful smile (Figure 74-6, H). There is some gingival irregularity noted, which appears to be a result of the soft tissue grafting. These areas could easily be smoothed with gingivoplasty, but the patient refused. Radiographs reveal preservation of interproximal bone with minimal saucerization around the implants with a platform-switch design (Figure 74-6, I).
After the surgical strategies described and utilizing minimally invasive surgical techniques, this 70-year-old patient received immediate implant-supported replacement of severely compromised maxillary incisors with an acceptable (or better) esthetic result and minimal treatment discomfort. With one surgery, including the extractions, she was provided with a fixed implant restoration on four implants. In the same surgery, the bone and soft tissue was augmented while preserving the interdental papilla. She experienced very little postoperative pain and was pleased with her new, more youthful-looking smile. The treatment time was only 6 months from extraction to final restoration. She was never without teeth and never wore a removable prosthesis. The improvement of the labial gingival margin was achieved without orthodontic extrusion or multiple surgeries.
Case Presentation 2
Case presentation 2 is a simultaneous extensive bone augmentation with multiple mandibular anterior immediate implants placed in a one-stage approach with labial flap reflection.
Dental History and Chief Complaint
The patient is a 41-year-old female with severe periodontal and endodontic infection affecting her mandibular anterior teeth. She is experiencing pain, halitosis, and a bad taste in her mouth. She is healthy and does not present with any medical contraindications for dental treatment. She is frustrated by her current dental condition because she recently replaced the crowns on the involved teeth. She understands the hopeless condition and would like to replace the teeth with dental implants, but she is apprehensive about the surgical procedure(s) and concerned the procedures will interfere with her busy schedule. She prefers a fixed provisional during the healing period if possible.
Examination and Diagnosis
The patient’s mandibular incisors exhibit severe periodontal and endodontic infections with periodontal pockets extending to the apex on several of her teeth. PFM crowns with overhanging margins are splinted together. The gingival tissue is swollen, erythematous, and heavy exudation is expressed from the gingival margins with palpation (Figure 74-7, A). She has a difficult time brushing because of the pain from the infection. Radiographic evaluation reveals severe generalized vertical and horizontal periodontal bone loss around the incisors with endodontic involvement. Existing endodontic treatment showed inadequate obturation and apical seal (Figure 74-7, B). These mandibular incisors have poor periodontal and endodontic prognosis. The remaining dentition is stable. She is not overtly concerned with esthetics, but desperately wants relief from pain, halitosis, and the bad taste in her mouth.

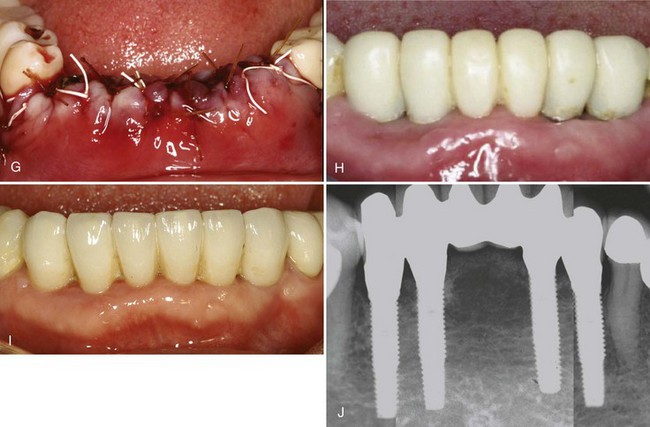
Figure 74-7 A, Splinted porcelain-fused-to-metal (PFM) crowns with overhanging margins on mandibular incisors that are infected. The gingival tissues are swollen with moderate to severe inflammation. B, Radiograph reveals severe generalized vertical and horizontal bone loss from periodontal and endodontic infections. C, Alveolar bone shows extensive destruction from periodontal and endodontic infections. D, With a surgical stent, the proposed implant sites are visualized and the surrounding bone is evaluated. E, Visualizing how the adjacent bone topography (socket walls) will contribute to bone formation around the implants, it is evident that even without grafting, most of the implant surface will become integrated with bone. F, Layers of resorbable collagen membrane cover the bone graft material. G, Full-thickness periosteal flaps are released, adapted around the healing abutments and sutured. H, Three months after surgery, the provisional restoration shows healing gingival tissues with sufficient ridge height and volume. I, Four year results show acceptable esthetic implant restorations in a stable ridge with a wide zone of keratinized, attached gingiva. J, Periapical radiographs at 4 years demonstrate good bone regeneration and maintenance with osseointegration of all implants.
Treatment Objectives
The immediate focus for this patient is to make her comfortable by eliminating the source of infection as soon as possible. However, considering her esthetic requirements, concern for surgical morbidity, and preference for a fixed provisional, an important treatment objective for this patient would be to identify a surgical approach that minimizes the extent and number of surgeries while providing predictability, longevity, and acceptable esthetics. Getting into a situation in which multiple extensive surgeries are necessary to achieve acceptable esthetics would be difficult for both the clinician and the patient.
Treatment Options
It is common to expect a loss of vertical height ranging from 5 to 10 mm after extraction of multiple mandibular incisors with severe bone loss. Surgical procedures used in an attempt to regain the vertical height of the ridge for acceptable esthetics in this region carry substantial risk and morbidity. Once the ridge collapses, any vertical ridge augmentation procedure requires extensive labial flap releasing to close over the grafting material and membrane. These large flaps often dehisce from the tension caused by the lower lip muscle movements and require more time to heal by secondary intention with potentially compromised outcome.
Even when flap closure is maintained, extensive labial flap releasing frequently results, obliterates the vestibular space, and creates mucogingival problems, which may require additional surgery to correct. The ridge augmentation procedure can be done on an incremental basis to minimize surgical complications, but the patient is subjected to multiple surgeries and prolonged treatment time. Distraction osteogenesis is an option to gain back the lost ridge height, but there are other problems associated with this approach, and it also requires multiple patient visits with extended use of a removable provisional prosthesis.11,20 However, the biggest disadvantage to this direction of treatment is that whichever ridge augmentation procedure is used to reconstruct the ridge, it is extremely difficult to gain back the vertical ridge height that was lost. The final esthetic result is usually disappointing.
There is risk of flap dehiscence during healing for the reason mentioned previously. Because of the postoperative swelling and ridge dimensional changes, maintaining the flap closure under a removable provisional prosthesis is difficult. Complete bone regeneration will take 6 to 10 months, depending on the type of bone grafting material used, and the total treatment time will be prolonged. Most often, multiple surgeries are required with several provisional modifications to obtain the desired esthetics. However, the biggest disadvantage of this treatment option is the inability to predictably reconstruct the lost vertical ridge height. The final esthetic result is typically disappointing, especially considering the enormous time and effort invested in treatment.
If implants are placed immediately using a two-stage approach (i.e. flap release with primary closure), there will be similar surgical risks and esthetic limitations as described for treatment option 2. However, this option has some advantages over treatment option 2. The implants placed at the time of extractions will function as tent poles to support the bone graft materials and membrane and will be osseointegrated and able to support a fixed provisional restoration in approximately 6 months. This will minimize the required time that the patient will have to endure a removable provisional prosthesis. If the implant-bone relationship is favorable enough to place the implants in a one-stage approach (i.e., the implant will be positioned in an intraosseous location or within the bony envelope and not supracrestal or outside the bony envelope), the surgical risks and morbidity will be less and an immediate fixed provisional restoration can be delivered at the time of the surgery. This treatment option more predictably preserves the vertical height of the ridge, and avoids the likelihood of severe ridge collapse following extractions. Only this treatment option offers a reasonable possibility of providing an esthetic implant restoration; it is accomplished with a minimal number of surgeries and less surgical risk.
Surgical Strategy for Predictable Esthetics
Because of the patient’s reasonable expectation, the level of the esthetic goal selected for this patient is not an ideal level but an acceptable level. This level of esthetics can be predictably achieved in a minimally invasive, patient-friendly manner. Mentally visualizing the final result with clinical and radiographic data, an acceptable esthetic outcome can be achieved for this patient if the existing heights of the lingual and interproximal bone can be preserved with grafting. If the implants can be placed immediately, they will assist in preserving the alveolar bone height by acting as tent poles to support the grafting material and membrane. The ridge will be overbuilt in anticipation of augmentation tissue/material shrinkage. If the implant-bone relationship is favorable, a one-stage approach can be utilized and an immediate fixed provisional restoration can be delivered at the time of surgery.
Considering all of these treatment options, the treatment that is most compatible with this patient’s surgical strategy for predictability, acceptable esthetics, and long-term results is treatment option 3, extraction of the mandibular incisors, immediate placement of implants (provided the implant-bone relationship is favorable), bone augmentation with particulate bone graft and barrier membrane, and immediate fixed provisional restoration supported by the implants. Again, provided the implant-bone relationship is favorable).
Treatment Plan and Rationale
To decrease the infectious process, alleviate symptoms, and improve tissue quality, initial therapy consisted of patient education, oral hygiene instructions with an ultrasoft toothbrush, chlorhexidine rinses, and 1 week of antibiotic therapy (e.g., Augmentin 500 mg, by mouth [PO], every 8 hours [q8h] × 7 days). Six mandibular incisors will be extracted using a labial full-thickness flap reflection to ensure complete removal of the granulation tissue and to visualize the bony architecture. If the implant-bone relationship is favorable for bone regeneration around the restoratively determined implant positions (canines and laterals), implants are immediately placed in a one-stage approach with simultaneous bone augmentation, which allows immediate provisionalization of these implants. Since the bone in the anterior mandible is dense, sufficient primary stability for immediate provisionalization can be easily achieved. If the bone architecture is unfavorable for a one-stage approach, the implants are placed in a two-stage approach with simultaneous bone grafting, barrier membrane, and primary flap closure. If a one-stage implant placement is achieved, the implant position is recorded (i.e., indexed) at the time of surgery for the purpose of laboratory provisional fabrication, and the provisionals are delivered within 1 to 2 weeks after surgery. The bulk of the surgical swelling should have subsided at that time. An Essex provisional is delivered at the time of surgery for temporary esthetic replacement of the missing teeth. The patient is in provisional restoration for 6 months to ensure implant integration and periimplant tissue stabilization. A final restoration can be fabricated and delivered at that time.
Treatment Sequence
Impressions are taken at the initial oral hygiene appointment and used to fabricate a surgical guide and an Essex provisional restoration.
During the surgical appointment, the anterior mandibular teeth are extracted, and the surgical treatments are carried out as outlined in the treatment plan. The Essex provisional is delivered, and patient is dismissed. If all goes as planned and implants are immediately placed in a one-stage approach, the fixed provisionals are delivered in 1 to 2 weeks. The fixed provisional restoration is replaced with the final restoration in approximately 6 months.
Surgical Procedure
Once the patient is anesthetized, the incisors are extracted with minimal damage to the delicate gingiva. The interdental papilla are severed at the crest, and a full-thickness labial flap is reflected. The flap is designed with divergent vertical incisions at the mesial line angles of the first premolars to facilitate surgical access and wound closure. A lingual full-thickness flap is reflected just enough to expose the crest of the lingual bony wall. Granulation tissue is thoroughly debrided to prepare the bone for implant placement and bone augmentation (Figure 74-7, C).
The initial impression of the extensive bony destruction observed after complete debridement suggests that immediate implant placement may not be possible and certainly immediate implant placement in a one-stage approach is doubtful. However, when the surgical guide is put in position, the bony architecture surrounding the proposed implant sites indicates a favorable implant-bone relationship (Figure 74-7, D) and a good potential for bone regeneration around the immediately placed implants, even in a one-stage approach. Mentally visualizing the final result again with the bone exposed confirms that an acceptable esthetic result can be achieved for this patient because the existing heights of the lingual and interproximal bone can be preserved with immediate implant placement and bone augmentation.
It has been documented in the literature and confirmed with clinical cases that if implant(s) are placed within the bony envelope of the ridge (i.e., in an intraosseous relationship with the surrounding bone), the bone regeneration potential around immediately placed implant(s) is favorable even when there is a labial dehiscence.40 Furthermore, when the implant head is positioned at or below the crest of bone in an intraosseous relationship to the surrounding bone and bone grafts are used with barrier membranes, bone will predictably fill to the top of the implant and integrate with the implant surface.34
Therefore the four implants are placed according to these principles, in the sites determined by the surgical guide. The apical-coronal position of the implant is partially dictated by the adjacent level of the bony wall, but care is taken to avoid placing them more than 4 mm below the anticipated labial gingival margin of the final restorations. The implants are placed as far lingual as reasonably possible to maximize the distance from the implant to the labial envelope of the residual ridge to enhance the likelihood of achieving an intraosseous relationship with the surrounding bone. Imagining how the adjacent bone topography (socket walls) contributes to bone formation around the implants, it is evident that even without grafting, most of the implant surfaces will become integrated with bone (Figure 74-7, E). Once a favorable potential for bone regeneration around the implants was ascertained, the decision to proceed with a one-stage implant placement approach was confirmed. Long implants (15 mm length) were placed to ensure sufficient primary stabilization that, when splinted together, would be capable of withstanding occlusal loads. A rapid setting registration material was used to register the implant position for provisional fabrication. Healing abutments (5 mm tall) were lightly secured to the implants for the initial postoperative healing phase.
For more complete bone regeneration around the implants and to overbuild the ridge dimensions, the site was augmented with particulated autogenous graft and mineralized allograft. A thin layer of particulated autogenous bone harvested from the ramus area was placed directly on the implant surfaces to enhance integration, and the allograft was layered to overbuild the ridge. Since only a small piece of the ramus bone was harvested, the donor surgical site was minimized and postoperative discomfort was minor. The grafted material was covered with two layers of resorbable collagen membrane (Bio-Gide, Osteohealth, Shirley, NY) to isolate and protect the graft material (Figure 74-7, F). The labial flap periosteum was adequately released to minimize flap tension during closure and healing. The flaps were adapted around the healing abutments and sutured with interrupted 4-0 chromic gut sutures (Figure 74-7, G). The mucogingival junction and the vestibular depth was not appreciably altered because it was not necessary to advance the flap significantly. The Essex provisional was delivered to the patient, making sure that the apical edges did not cut the sutures or impinge on the wound during the postoperative healing and probable swelling. The patient was dismissed with postoperative instructions.
Ten days after the surgery and after the postoperative swelling has mostly subsided, the lightly secured healing abutments were removed. The laboratory-fabricated provisionals were carefully placed; making sure to avoid tissue impingement. Provisional bridges should be sectioned before placing and rejoined after the placement on the implants. The joined contacts should be strong enough to avoid being separated during mastication. The patient should be seen on a monthly basis to enforce good oral hygiene and to evaluate tissue healing and provisional stability (Figure 74-7, H). The provisional restoration is replaced with a final restoration in approximately 6 months.
Results
The 4-year result demonstrates an acceptable esthetic implant restoration in a stable ridge with sufficient vertical height and horizontal volume. There is a wide zone of keratinized, attached gingiva (Figure 74-7, I). Periapical radiograph (4 years) indicates bone regeneration and maintenance at the top of the implants. All implants are stable and appear to be osseointegrated (Figure 74-7, J).
By following the surgical strategies described and utilizing minimally invasive techniques, this 41-year-old patient was provided with esthetic dental implant restoration with a minimal number of surgeries and treatment time. Her immediate complaints were addressed without the need for multiple extensive surgeries. She did experience some postoperative pain and swelling, but her entire treatment required only one surgery and the total treatment time was only 6 months from extractions to the final restoration. She was provided immediately with an Essex provisional restoration, which was replaced with a laboratory-fabricated fixed provisional restoration attached to the implants 10 days after surgery. She was comfortable throughout the duration of the treatment.
This surgery may appear very extensive and at first impression not minimally invasive. However, any treatment option other than this approach would most likely require multiple, more extensive surgeries with higher surgical morbidity and much longer treatment time. More critically, since it is difficult to reconstruct vertical ridge height after it is lost, the biggest disadvantage of the other treatment options is that the final esthetic result is more often than not disappointing. Therefore, even with the extensive bone loss observed in this case, immediate implant placement in a one-stage approach with simultaneous bone augmentation and immediate provisionalization is considered by many to be a minimally invasive and patient-friendly approach to providing esthetic dental implant therapy.
Case Presentation 3
Case presentation 3 illustrates the use of short wide-diameter implants to treat a severely resorbed mandibular posterior ridge.
Dental History and Chief Complaint
The patient is a 65-year-old female with a severely resorbed mandibular posterior ridge. She is frustrated with her partial denture and wants dental implants to give her better “chewing” ability. She does not present any medical contraindication for dental treatment, but she is anxious about extensive dental surgeries. The esthetic outcome is not a concern for her.
Examination and Diagnosis
The patient’s posterior ridge of the mandible shows extensive vertical ridge resorption with a narrow band of keratinized gingiva at the crest. The ridge height is near the floor of the mouth, with frenum and muscle pull on the buccal side (Figure 74-8, A). The radiographic vertical height of the ridge measured from the crest to the mandibular canal is approximately 7 mm (Figure 74-8, B). Clinical examination shows what appears to be a narrow ridge, but the horizontal width of the ridge measured at the bony crest with a caliper is approximately 8 mm. A three-dimensional scan (e.g., CT or CBCT) can confirm this finding. The typical anatomy of mandibular and maxillary posterior segments after severe vertical resorption cases often has sufficient ridge width for implant placement.
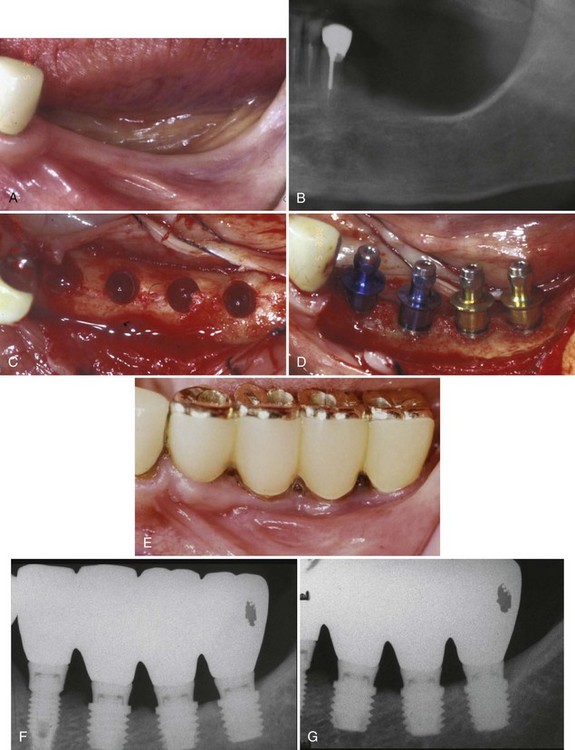
Figure 74-8 A, Severely resorbed ridge in the posterior mandible in a 65-year-old female. Examination reveals a narrow band of keratinized, attached gingiva at the ridge crest. B, Panoramic radiograph of patient in Figure 74-8, A, showing a limited vertical height of bone above the inferior alveolar nerve of approximately 7 mm. C, Clinical view of prepared implant osteotomy sites in the posterior mandible. Despite the severe vertical ridge resorption, most of the time there is sufficient ridge width in posterior sites to accommodate wide-diameter implants. D, One 4-mm diameter short (7 mm) implant and three 5-mm diameter short (5 mm) implants were placed with good initial stability. The bone width was adequate, and there were no implant thread exposures. E, The final implant restorations were fabricated with gold occlusal surfaces and splinted together. Adequate interproximal spaces were created for oral hygiene access. F, Periapical radiograph (13 months post-loading) reveals stable crestal bone height despite the long crown-to-implant ratio. G, Another follow-up periapical radiograph (30 months postloading) reveals continued stability of the crestal bone height. Platform-switched abutment/restorations, adequate biomechanical support, and careful occlusal design contributes to bone preservation and maintenance.
Treatment Objectives
Considering her concerns about surgical morbidity, the treatment objective would be to identify a surgical approach that minimizes the extent and number of surgeries while providing predictability and longevity. Attempting to reconstruct the vertical height of the deficient posterior ridge with multiple extensive surgeries would be difficult for both the clinician and the patient.
Treatment Options
Treatment Plan and Rationale
Since there is an 8-mm horizontal width and only a 7-mm vertical ridge height at the three distal implant sites, three 5-mm diameter × 5-mm long implants are placed. A 4-mm diameter × 7-mm long implants are placed in the most anterior site, since the ridge is narrower (≈6 mm) and taller (≈9 mm). These implants will be placed in a two-stage approach to accommodate the clinician’s preference, but with precise surgery, they could be placed in a one-stage approach. This surgery does not require special skills, and if the restorative treatment plan is properly executed, the use of short implants will provide predictability and longevity.2,15,16,27
Treatment Sequence
No special treatment sequencing is necessary. This procedure is facilitated, like all implant surgeries, by using a surgical stent and following a proper restorative treatment plan.
Surgical Procedure
Once the patient is anesthetized, a crestal incision is made, bisecting the existing band of crestal keratinized tissue. Buccal and lingual full-thickness flaps are reflected to clearly visualize the full width of the ridge. Sutures can be used to keep the flaps away from the surgical site. Properly spaced osteotomy sites are prepared to accommodate one 4-mm diameter and three 5-mm diameter implants (Figure 74-8, C). Implants are placed with very good primary stability and no bone dehiscence(s) (Figure 74-8, D). The flaps are closed with a combination of mattress and interrupted sutures. The exposure of the implants and the fabrication of the restorations are done 3 months after the implant placement. Since the esthetic is not the major concern for the patient, the clinician elected to use gold metal occlusal surfaced implant restorations (Figure 74-8, E). The restorations have a platform switching configuration to enhance crestal bone preservation, and they are splinted together with sufficient embrasure for proper oral hygiene.
Results
A periapical radiograph, taken 13 months after loading, shows a stable crestal bone level despite the long crown-to-implant ratio of the restorations (Figure 74-8, F). The implant abutments have platform-switching design, which has been shown to preserve crestal bone. A periapical radiograph, taken 30 months after loading, shows long-term crestal bone stability without further bone loss around the short wide-diameter implants (Figure 74-8, G).
This patient was provided with a very functional stable implant restoration in just 3 months using short wide-diameter implants. The other possible treatment options for this patient would have required multiple surgeries and would have increased the risk of surgical morbidities and complications. Treatment time would have been much longer and the results may have fallen short of the treatment goal. This case offers a sound example of how patients with extensive vertical bone loss in posterior regions can be treated using short wide-diameter implants with a minimally invasive, patient-friendly surgical approach, without sacrificing predictability and longevity.