CHAPTER 73 Advanced Implant Surgical Procedures
The high predictability of endosseous dental implants has led to routine use and an expectation for success. However, the ultimate success for any patient or any particular implant relies on several factors, the most important of which is the availability of bone. The loss of teeth, whether caused by disease or trauma, can result in severe deficiency of the alveolar bone. Horizontal bone deficiencies are managed quite predictably with localized bone augmentation procedures (see Chapter 72). However, vertical bone deficiencies are much more challenging. The edentulous posterior maxilla is challenging as the result of a general lack of bone volume and the omnipresent poor bone quality of the area; that is, posterior maxillary bone often consists of a thin cortical shell filled with sparse trabecular bone. Edentulous sites, in any anatomic location, that have suffered significant vertical alveolar bone loss are especially challenging to reconstruct.
This chapter reviews advanced surgical procedures used to treat the most challenging type of bone loss, which is a deficiency in vertical bone height. Maxillary sinus elevation and bone augmentation, vertical bone augmentation, and distraction osteogenesis are reviewed. The role of growth factors in bone augmentation procedures is also discussed.
Maxillary Sinus Elevation and Bone Augmentation
Rehabilitation of the edentulous posterior maxilla with endosseous dental implants often represents a clinical challenge because of insufficient bone volume resulting from pneumatization of the maxillary sinus along with resorption or loss of alveolar crestal bone. Before the utilization of bone augmentation procedures, patients with missing teeth and deficient bone in the posterior maxilla could only be rehabilitated with removable prostheses, short implants, or cantilevered restorations (i.e., supported by adjacent teeth or implants). Historically, the failure rate for implants in the posterior maxilla has been significantly higher than failure rates for implants in all other anatomic locations.16 Therefore procedures such as the maxillary sinus elevation and bone augmentation are needed to increase the amount of vertical bone height in the posterior maxilla for the placement of implants.
In 1980, Boyne and James3 first described a procedure to graft the maxillary sinus floor with autogenous marrow and bone for placing an implant (blade type). Access to the maxillary sinus was gained through a “Caldwell-Luc” procedure (i.e., an opening into the maxillary sinus created at the anterior-superior aspect). Since then, several other techniques have been described, including variations on the lateral window osteotomy and a variety of techniques to lift the sinus floor from a crestal approach.
Various bone graft materials have been used to augment the maxillary sinus. The 1996 Consensus Conference on Maxillary Sinus Bone Grafting reviewed available data and concluded that allografts, alloplasts, and xenografts, alone or in combination with autogenous bone, can be effective as bone substitute graft materials for sinus bone augmentation.17 More importantly, it was concluded that the sinus graft procedure with implant placement is a highly predictable and effective therapeutic modality for the rehabilitation of the posterior maxilla. Sinus floor elevation with bone augmentation of the maxillary sinus is now a well-accepted procedure used to increase bone volume in the posterior maxilla. Numerous reports have validated the safety and efficacy of this procedure.6,9,11 Implant success rates are equal to or better than that of implants placed in non-grafted maxillary bone (i.e., areas of the posterior maxilla with adequate height of existing native bone). Thus bone augmentation of the maxillary sinus is a viable option for the vertically deficient posterior maxilla in which the interocclusal dimension is normal or only moderately increased.
Indications and Contraindications
As with any therapeutic procedure, treatment success depends on appropriate patient selection, careful evaluation of the anatomy, identification and management of any pathology, sound surgical procedures, and appropriate postsurgical management. The primary indication for maxillary sinus elevation and bone augmentation, specific for the placement of endosseous dental implants, is an alveolar bone height in the posterior maxilla that is deficient (e.g., less than 7 mm of existing vertical bone height). Other factors that must be considered include the health of the patient, the condition of the remaining dentition, and the likelihood of a beneficial outcome. A thorough evaluation of the patient and the judgment of the clinician ultimately determines whether the procedure is indicated for any particular individual.
Contraindications to maxillary sinus elevation and bone augmentation are similar to contraindications for other surgical procedures, with the added consideration of the maxillary sinus (Box 73-1). Patients must be in good general health and free of diseases that affect the maxilla or maxillary sinus. Local factors that are considered contraindications to maxillary sinus elevation and bone augmentation include the presence of tumors, maxillary sinus infection, severe chronic sinusitis, scar or deformity of the sinus cavity from previous surgery, dental infection, severe allergic rhinitis, and chronic use of topical steroids. Systemic contraindications to treatment include radiation therapy, uncontrolled metabolic disease (e.g., diabetes), excessive tobacco use, drug or alcohol abuse, and psychologic or mental impairment.
Surgical Procedures for Sinus Elevation
The goal of sinus elevation and bone augmentation is to lift the schneiderian membrane from the floor of the sinus, raising it up into the sinus cavity to create a new, more superiorly located sinus floor with a space between it and the deficient alveolar ridge. The newly created space can then be filled with bone (or a suitable bone substitute material) to increase the total vertical height of bone in the posterior maxilla for the placement of endosseous implants.
The maxillary sinus bone augmentation procedure was first described in the 1960s by Boyne (unpublished oral presentations to United States [US] Navy Dental postgraduates, 1965–1968) and originally used as a preprosthetic surgical procedure for patients with large tuberosities and pneumatized sinuses.2 To reduce the size of the tuberosity without creating an oral-antral defect, bone was grafted into the sinus cavity to increase the volume of bone within the maxillary tuberosity. After a period of healing, the tuberosity was able to be reduced surgically from the alveolar ridge crest. As stated earlier, Boyne and James3 were the first to describe the use of the maxillary sinus bone-grafting procedure for placement of an implant (blade type) to retain a prosthesis. Greater use and further development of this procedure evolved along with the success of endosseous dental implants and the desire to replace missing posterior maxillary teeth with implant-retained restorations.
The techniques used for sinus elevation and bone augmentation are primarily differentiated by the anatomic location of the osteotomy used to gain access to the maxillary sinus. Specifically, four different anatomic locations have been described: (1) the superior lateral wall, or “Caldwell-Luc,” opening, which is located just anterior to the zygomatic arch; (2) the middle lateral wall opening, which is located midway between the alveolar ridge and the zygomatic arch; (3) the inferior lateral wall opening, which is located at the level of the alveolar ridge; and (4) the crestal osteotomy approach, which is an opening through the alveolar bone crest superiorly toward the floor of the sinus. At present, the most common procedures used for sinus elevation and bone augmentation are the lateral wall antrostomy (middle or inferior approach) and the crestal approach osteotomy.
Presurgical Evaluation of Maxillary Sinus
Presurgical evaluation of the maxillary sinus is primarily accomplished using radiographic examination techniques (Figure 73-1). Several observations about the anatomy can be made with a periapical or panoramic projection, but the internal anatomy is more accurately assessed with a three-dimensional scan, such as computed tomography (CT) or cone-beam CT (CBCT) scan. The maxillary sinus should be evaluated for any pathology, masses, or the presence of septa. If three-dimensional scans are available, the lateral wall should also be evaluated for the presence of medium or large intraosseous vascular channels (see Figure 53-15). Medium- to large-sized vessels occasionally traverse the lateral wall of the maxillary sinus, and identifying them is helpful in avoiding a bleeding problem during surgery (see Chapter 53).
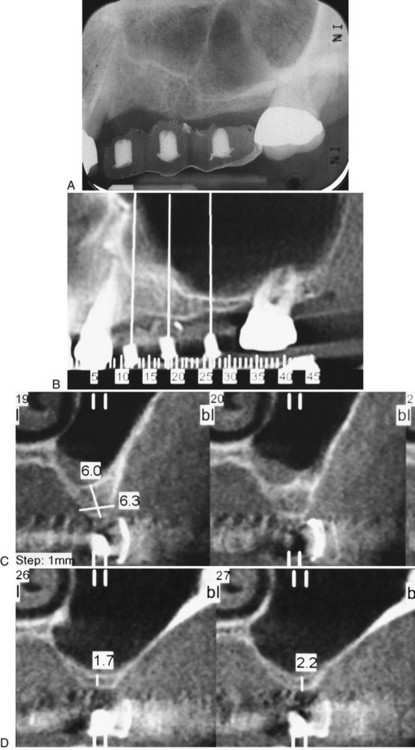
Figure 73-1 Presurgical evaluation of the maxillary sinus. A, Periapical radiograph. B, Panoramic projection from cone-beam scan. Note the presence of maxillary septa in the premolar region. C, Cross-sectional image in premolar region showing about 6 mm of bone height and presence of maxillary septa. D, Cross-sectional image in molar region showing about 2 mm of bone height.
Simultaneous Implant Placement
Simultaneous implant placement is possible with sinus elevation and bone augmentation procedures as long as the implant can be stabilized in the desired location with the existing native bone (Figure 73-2, online).
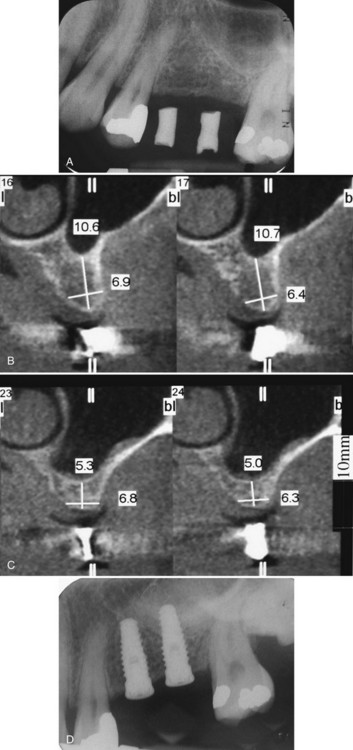
Figure 73-2 Simultaneous implant placement with maxillary sinus elevation and bone augmentation procedure. A, Preoperative periapical radiograph. B, Preoperative, cross-sectional image in premolar region demonstrating 10.6 mm of vertical bone height. C, Preoperative, cross-sectional image in molar region demonstrating 5.3 mm of vertical bone height. D, Postsurgical radiograph of graft and implants in place.
It has been suggested that a minimum of 5 mm of existing native bone in the alveolar crest is required for simultaneous implant placement. However, some clinicians claim that it is possible to place implants simultaneously with as little as 1 mm of remaining bone.22,42 The most important factor in determining whether implant(s) can be placed at the time of sinus bone augmentation is the ability to achieve implant stability in the existing bone rather than any measure of bone height. Factors that influence implant stability include bone height, bone quality, precision of osteotomy preparation, and the surgeon’s skill and experience. If inadequate native bone exists to place implants at the time of the bone augmentation procedure, they can be placed at a subsequent surgery after an appropriate healing period (Figure 73-3).
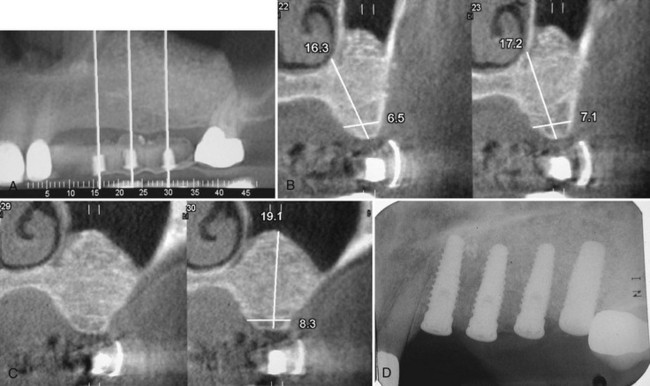
Figure 73-3 Staged implant placement after sinus elevation and bone augmentation procedure. Same patient as in Figure 73-1. See preoperative radiograph and preoperative cross-sectional images. A, Postsurgical panoramic view of bone-augmented maxillary sinus. The maxillary left cuspid has been extracted because of a vertical fracture. B, Postsurgical cross-sectional image in premolar region demonstrating more than 17-mm vertical bone height. C, Postsurgical cross-sectional image in molar region demonstrating 19.1-mm vertical bone height. D, Postsurgical radiograph of implants placed in the previously grafted maxillary sinus (and cuspid site).
Bone Graft Materials
Autogenous bone is often considered the “gold standard” for bone augmentation because of its osteoconductive, osteoinductive, and osteogenic properties.3 However, harvesting autogenous bone from intraoral or extraoral locations creates a second surgical site with additional morbidity. Numerous studies have demonstrated clinical success using many variations of bone graft materials and combinations.17
Several recent clinical studies and reports have attempted to evaluate the maxillary sinus augmentation procedures using a variety of bone-grafting materials, including autogenous bone from the iliac crest or oral cavity and bone substitutes such as freeze-dried demineralized bone, resorbable and nonresorbable hydroxyapatite, and xenografts. However, only a few studies have critically evaluated the long-term clinical outcome of this procedure, and most have used a small study population. Short- to long-term clinical studies of dental implants placed into grafted sinuses demonstrate an equivalent or higher survival rate as compared to implants placed in native maxillary bone (i.e., without the need of sinus augmentation).17 The results of these studies support the clinical predictability of maxillary sinus augmentation procedures for the rehabilitation of the edentulous posterior maxilla with implant-supported prostheses.
The use of bone-substitute graft materials can reduce the morbidity introduced by a second surgical site while maintaining equally good implant success rates.17 These materials form an osteoconductive scaffold for bone growth but do not have any osteoinductive properties. A possible exception is demineralized freeze-dried bone allograft (DFDBA). This material has demonstrated osteoinductive potential40 but has not proved to be particularly advantageous in the maxillary sinus bone augmentation.17,40 In fact, the bone volume gained with the use of DFDBA is less than that achieved with mineralized graft materials as a result of moderate postoperative shrinkage of DFDBA-grafted bone.
Crestal Osteotomy Technique
In cases with moderate bone height (e.g., 7 to 9 mm) that require limited sinus bone augmentation, a crestal approach to elevation may be desirable. The osteotome technique is a procedure that uses osteotomes (Figure 73-4, online) to compress bone (internally from the alveolar crest upward) against the floor of the sinus, ultimately leading to a controlled “inward fracture” of the sinus floor bone along with the schneiderian membrane, which should remain intact above the inward-fractured bone.
The osteotome sinus floor elevation (OSFE) technique was described by Summers.33,34 It is considered to be a “conservative” approach to sinus elevation, but it is also a “blind” technique because it does not allow the operator to visualize the schneiderian membrane during the osteotomy. For this reason, it is a technique-sensitive procedure as well (i.e., the operator must “feel” the bone fracture and the membrane elevation). Verification of success can only be observed with radiographs and visualization of the bone graft material in the sinus cavity.
Procedure
An osteotomy site is prepared with a series of drills (e.g., initial drills used for implant site preparation) to a depth that is approximately 1 to 2 mm from the floor of the maxillary sinus. Osteotomes are used to increase compressive forces gradually against the floor of the sinus by adding incremental quantities of graft material until the floor of the sinus fractures inward (Figure 73-5). After the controlled inward fracture of the maxillary sinus floor, bone graft materials continue to be slowly introduced, through the osteotomy site and into the maxillary sinus, which continues to elevate the membrane and thus allows a vertical expansion of the bone height in a localized area of the maxillary sinus. Once the sinus membrane is elevated with bone graft material to the desired height, the implant osteotomy can be completed, with a final drill used to finish preparation of the site, and an implant can be inserted. Multiple individual sites can be elevated and prepared simultaneously through separate osteotomy sites.
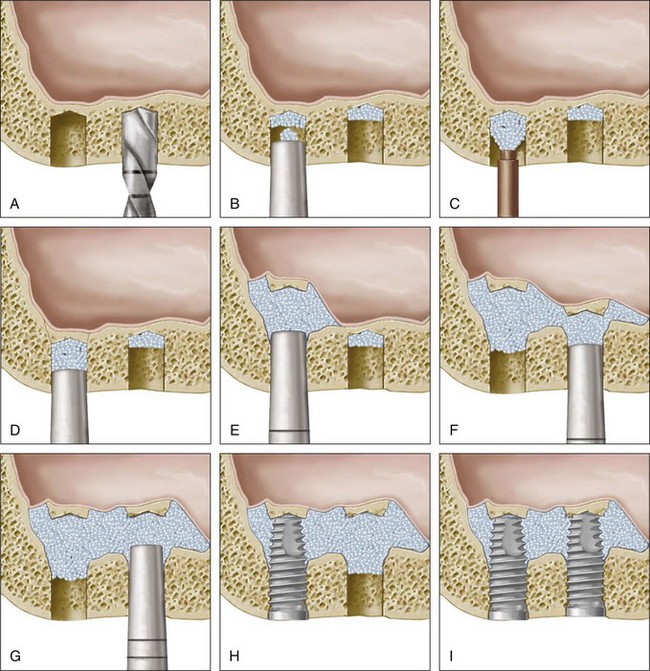
Figure 73-5 Illustration of the osteotome sinus floor elevation (OSFE) technique. A, Osteotomy prepared with drills to a depth that is near the maxillary sinus floor. B, Graft material introduced into osteotomy and condensed with osteotome. C, Additional bone graft material is added to the osteotomy. D, Bone graft continues to be condensed by osteotomes. E, This process is continued until floor of sinus is “fractured” up internally and the floor is lifted with the bone graft material. F, Continuation of process shown in E for second site. G, Bone graft material continues to be added gradually to both sites with osteotome condensation to elevate the schneiderian membrane away from the bone (maxillary sinus walls) until sufficient height and volume are created for the placement of implants. H, The coronal aspect of the osteotomy is carefully prepared for the placement of implants (instrumentation not shown) and the implant is placed. I, Final view of two implants placed in the grafted maxillary sinus using the OSFE technique.
Published reports of this technique have demonstrated increased bone height from 2 to 7 mm (average, 3.8 mm).37 Thus the crestal approach is a useful technique for increasing the vertical height of bone up to approximately 4 mm. If more vertical bone height is needed, the lateral wall osteotomy approach may be more advantageous. In addition to the usual precautions and contraindications for sinus elevation and bone augmentation procedures, the osteotome technique may be contraindicated for sinuses that have an acutely sloped floor or septa in the location of the planned osteotomy. An acutely sloped sinus floor will tend to deflect the osteotome in an undesirable direction rather than allowing the osteotome to penetrate into the sinus space, and the presence of septa makes it virtually impossible to fracture the sinus floor inward. Box 73-2 provides additional precautions and clinician comments on using the osteotome technique. Several new instruments and techniques have emerged that improve the ability to create a crestal approach osteotomy while avoiding trauma or injury to the schneiderian membrane. These instruments/techniques vary from drill systems to piezoelectric bone surgery. See Chapter 75 for a description of piezoelectric bone surgery.
BOX 73-2 Clinician Comments on Use of Osteotome Technique
Clinical Perspective 1
The osteotome procedure involves repeated tapping of osteotomes with a mallet to create the necessary pressure to fracture the floor of the maxillary sinus. This tapping can be bothersome to some individuals, especially those patients who are not sedated for the procedure. The tapping procedure tends to be more bothersome for patients with dense cortical bone and for those with loose trabecular bone. In fact, a specific postoperative complication, called benign paroxysmal positional vertigo (BPPV), has been associated with the osteotome sinus elevation technique. During the osteotomy preparation and sinus floor elevation, the trauma induced by percussion of the osteotome with the surgical hammer, along with hyperextension of the neck during the operation, can displace otoliths in the inner ear and induce BPPV (see Chapter 77).
Clinical Perspective 2
The osteotome technique requires that the osteotome be properly aligned in the direction of the long axis of the planned implant. Thus patients must be able to open wide enough to allow a direct insertion of the osteotome into the osteotomy site. Offset osteotomes are available that can facilitate the correct angulation (see Figure 73-4, B, online).
Lateral Window Technique
The lateral window technique is probably the most effective and efficient way to access the maxillary sinus and elevate the sinus floor. In this procedure, an opening into the maxillary sinus is created to elevate the schneiderian membrane and to place bone graft in the space immediately above the existing alveolar bone. The osteotomy can be prepared with a high-speed round diamond or a piezoelectric bone surgery device (see Chapter 75). Some clinicians prefer to cut the lateral window (outline cut through to the membrane) and use the impacted bony wall as the superior wall of the space created for bone grafting (Figure 73-6, A to C), and others prefer to eliminate the bony window entirely by reducing it to a paper-thin layer, which is easily removed (Figure 73-6, D to F). With the former technique, it is important to create a window that is small enough, relative to the mediolateral width of the maxillary sinus, to allow the “window” to be pushed completely into the sinus cavity. If the window cannot be inserted completely, it must be carefully separated from the membrane and removed. The bone removed from the lateral window osteotomy can be harvested and incorporated into the bone graft.
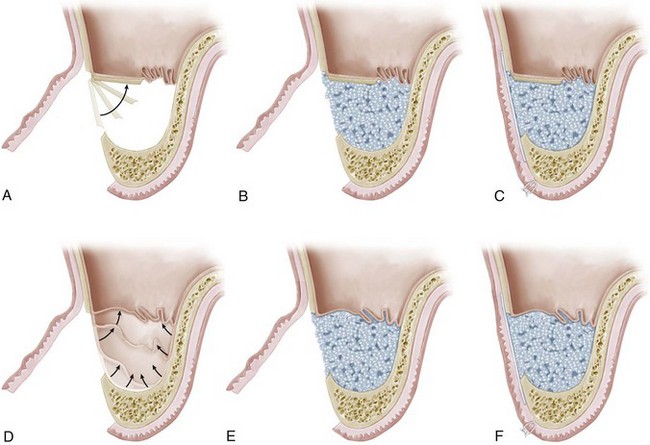
Figure 73-6 Illustrations showing two techniques for the lateral window procedure to access the maxillary sinus for bone augmentation. The first technique (A to C) preserves the bone of the lateral window elevating it up into the sinus cavity to create a new sinus floor. The second technique (D to F) completely removes the lateral window as part of the preparation. A, Lateral window is cut at the periphery of the access window, leaving the lateral bony wall in the center of the window intact. The bony window is then pushed inward to become the new, elevated sinus floor/superior wall of the grafted maxillary sinus space. B, Bone graft material is packed into the newly created space. C, A barrier membrane is placed over the lateral window and bone graft material. The full-thickness flap is sutured over the barrier membrane. D, Lateral window is removed entirely during the preparation of the osteotomy. The schneiderian membrane is elevated inward and upward to become the superior containment of the grafted maxillary sinus space without a superior bony wall. E, Bone graft material is packed into the newly created space. F, A barrier membrane is placed over the lateral window and bone graft material. The full-thickness flap is sutured over the barrier membrane.
Elevation of the schneiderian membrane is accomplished with hand instruments that are inserted along the internal aspect of the bony walls of the sinus (Figure 73-7, online).

Figure 73-7 Instruments used to elevate the schneiderian membrane through lateral window antrostomy. A, De Marco curettes. B, Gracey 13/14 curette. C, Universal curettes. D, Large spoon curettes. E, Medium-sized curved membrane elevators.
Great care is taken to avoid perforation of the membrane. Small instruments, such as the De Marco curette, are introduced along the inferior, anterior, posterior, and superior aspects of the prepared antrostomy window, gradually inserting further along the bone until the membrane begins to separate and lift away from the bone. Subsequently, larger instruments, such as the Gracey 13/14 curette, are gently introduced along the bone to continue lifting the membrane to the desired levels (height, width, and depth). Instruments must always be kept in contact with the bone surface while elevating the schneiderian membrane to avoid perforation. Regardless of whether implants are being placed simultaneously or not, it is useful to estimate the dimensions of the augmentation needed by inserting a surgical guide with holes or markers indicating the ideal location for planned implants. Once elevated, the space can be grafted with bone (autogenous, bone substitute, or a combination). If implants are being simultaneously placed, the implant osteotomy sites should be prepared, and implants placed after the medial, anterior, and posterior aspects are filled with bone, thereby supporting the schneiderian membrane up and away from the drills and implants. After implant placement, the remaining lateral aspect is packed with bone graft. Finally, the antrostomy and bone graft is covered with a barrier membrane (e.g., resorbable membrane) and the flap is sutured.
Risks and Complications
The maxillary sinus elevation and bone augmentation procedure is technique sensitive, requiring meticulous surgical skills. Risks and complications of the procedure include tearing or perforation of the schneiderian membrane, intraoperative/postoperative bleeding, postoperative infection, and loss of bone graft or implants (see Chapter 77).
The reported incidence of perforation or tearing of the schneiderian membrane varies greatly (up to 60%) and depends largely on the anatomy of the sinus and the skill and experience of the operator.19,23,28 The presence of septa in the maxillary sinus increases the likelihood of membrane perforation. If the perforation is small, it can often be managed with a resorbable barrier membrane placed over the opening, followed by careful packing of the bone augmentation material. If a perforation or tear is extensive (see Figure 77-18, A), it may be necessary to abort the procedure, close the wound, and attempt it again at a later date.
Infections have been reported in a small but significant number of cases (up to 10%) after maxillary sinus elevation and bone augmentation procedures.28 Prevention of infection is crucial for bone augmentation procedures. Surgery should always be performed using sterile technique. Patients should use a presurgical antimicrobial mouth rinse (e.g., chlorhexidine), and postoperative antibiotics should be prescribed.
Opening a window through the lateral wall is accomplished by completely cutting through the bone of the lateral wall up to the schneiderian membrane. The membrane is highly vascularized and may bleed significantly. However, a more serious bleeding problem can arise if an intraosseous artery is severed in the process. Bone wax and topical hemostatic agents must be available to manage such an urgent surgical complication. If a medium-to-large vascular channel is identified (with CT or CBCT scan) presurgically, it can usually be avoided.
Supracrestal/Vertical Bone Augmentation
Supracrestal or vertical bone augmentation presents one of the greatest challenges of bone regeneration in implant dentistry. This is primarily a result of the difficulty of the surgical procedure and its potential complications. Since vertical augmentation can be a very challenging procedure with a relatively high rate of complications, it is necessary to justify this particular treatment for each patient. The rate of complications associated with vertical bone augmentation procedures, including membrane exposure and/or postoperative infection, is reported to range from 12.5% to 17%.31,32,36 Alternative treatment options, albeit with limited outcomes, need to be considered. For example, regenerating a vertically deficient defect may not be necessary if (1) implants can be placed in adjacent sites, (2) short implants can be used, or (3) pink ceramic can be used to create an illusion of “normal” soft tissue anatomy.
Historic attempts to vertically increase alveolar bone height using modalities such as onlay bone grafting have failed. More recent treatment modalities developed for vertical bone growth include distraction osteogenesis and vertical guided bone regeneration (GBR). The techniques and evidence of success are presented.
Guided Bone Regeneration and Augmentation
The surgical technique of GBR for supracrestal regeneration was described in the 1990s.36 Both animal and human studies demonstrated successful vertical bone augmentation with histologic evidence.18,32 The available evidence describing and supporting the use of supracrestal GBR is limited. Some studies have evaluated the effect of space creation by a membrane alone, whereas others have used an autogenous bone graft to maintain space under the membrane. Animal (dog) studies demonstrated the ability to gain about 2.7 mm (0.4 to 4.0 mm) of vertical bone height around simultaneously placed implants.18 In one clinical study, 5 patients were treated with a supracrestal exposure of 3 to 7 mm (average of 4.67 mm) and showed a clinical bone gain of 0.5 to 4 mm (average of 2.97 mm) after 9 months.30 These studies suggest that supracrestal bone formation up to 3 mm is predictable using the GBR technique with a membrane–blood clot combination.
Simion et al32 and Jovanovic et al18 used a titanium-reinforced (TR) membrane for vertical bone regeneration around dental implants without the placement of supportive bone substrates. Instead, the space was filled with a blood clot facilitated by perforating the cortical bone surface or by injecting the space with venous blood. Supracrestal bone regeneration achieved was 3.3 mm32 and 1.82 mm in these studies, respectively.18,32 Recent studies showed that supracrestal bone formation is more predictable using a bone graft filler material placed under the TR membrane. Therefore, at present, advanced surgical GBR augmentation for vertical bone gain should be achieved with a nonresorbable TR membrane that is supported by a bone graft (Figure 73-8).
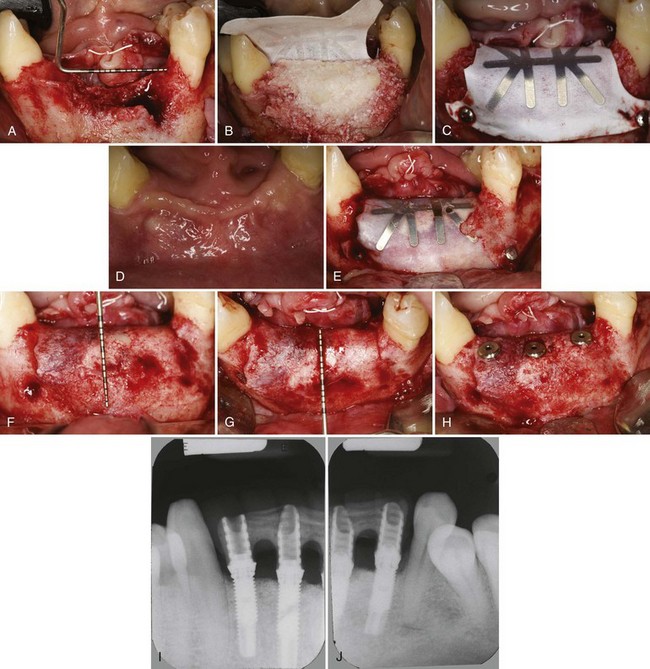
Figure 73-8 Representative case of a patient treated with supracrestal/vertical alveolar ridge bone augmentation (1 : 1 mixture of autogenous particulated bone and anorganic bovine bone mineral). A, Vertical defect in the anterior mandible. B, Buccal view of autogenous particulated bone mixed with anorganic bovine bone mineral. C, Guided tissue regeneration membrane/titanium-reinforced (GTRM-TR) membrane is fixed in place with titanium pins. D and E, Following 9 months of uneventful healing, the expanded polytetrafluoroethylene (ePTFE) membrane has maintained its position. F and G, At membrane removal the area demonstrates complete vertical bone gain. Note the excellent incorporation of both graft materials. H, Three regular platform implants are placed into ideal positions. I and J, Radiographs of implants restored in function. Note the appearance of good quality bone around all implants.
The long-term results of vertical GBR after 1 to 5 years of prosthetic loading were examined in a retrospective multicenter study evaluating 123 implants.30 Three treatment modalities (nonresorbable regenerative membranes in combination with blood clot only, DFDBA, or autogenous bone chips) were studied, and the results from this investigation revealed that vertical bone regeneration greater than 4 mm could only be achieved with the use of autogenous bone chips. These authors reported an overall success rate of 97.5%, leading them to conclude that vertically augmented bone using GBR techniques supports implant placement in a fashion similar to native, nonregenerated bone.
Urban et al39 used TR membranes with autogenous particulated bone for vertical bone augmentation before implant placement. The study included 35 patients with 36 vertical bone defects. Eighty-two implants were placed in a staged approach and a resorbable collagen membrane (Bio-Gide Resorbable Bilayer Membrane, Osteohealth, Shirley, NY) was placed over the newly formed crestal bone at the implant placement surgery to protect the graft from early resorption after removal of the expanded polytetrafluoroethylene (ePTFE) membrane. Implants were followed from 1 to 6 years after prosthetic loading.
Treatment groups included single and multiple tooth sites, as well as vertical defects in the posterior maxilla. Vertical bone augmentation of the posterior maxillary ridge was done simultaneously with sinus bone augmentation (Figure 73-9). At membrane removal, the mean vertical bone augmentation was 5.5 mm (±2.29 mm). The mean combined crestal remodeling was 1.01 mm (±0.57 mm) at 12 months, which remained stable through the 6-year follow-up period. There were no statistically significant differences between the treatment groups in mean marginal bone remodeling. The overall implant survival rate was 100% with a cumulative success rate of 94.7%.
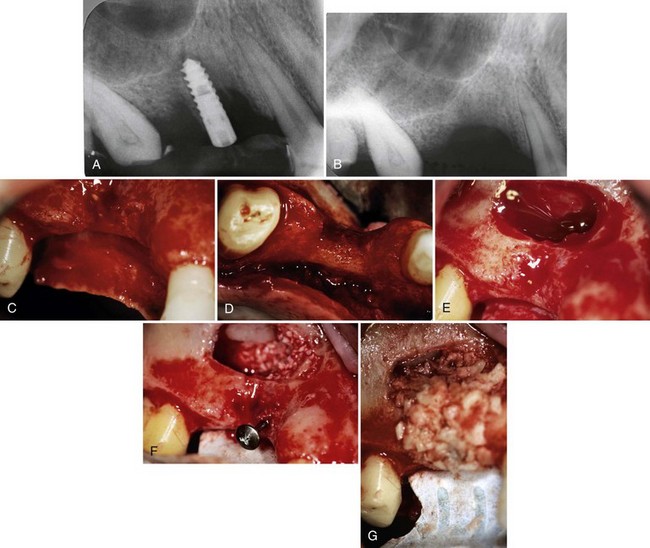
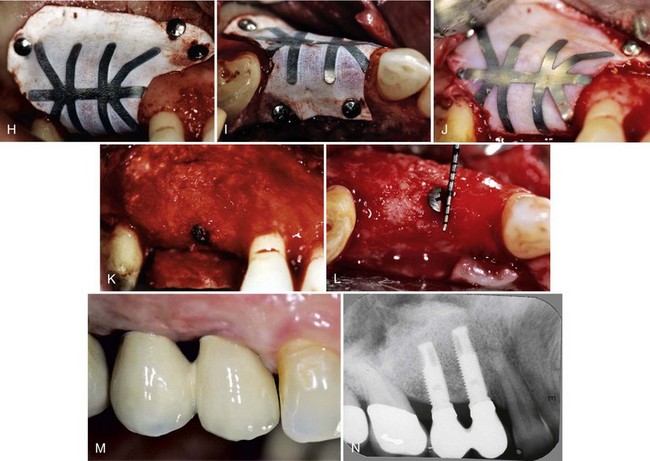
Figure 73-9 Simultaneous vertical ridge and sinus bone augmentation. Representative case requiring posterior maxillary vertical and sinus augmentation. A, Failing implant and severe periimplant bone defect on the right maxillary premolar area. B, Radiograph 3 months after implant removal demonstrates vertical deficiency and sinus proximity. C and D, Remote full thickness flap is elevated exposing the facial bone of the posterior maxillary region. Buccal and occlusal views of esthetically and functionally demanding vertical defect. E, The lateral window of the sinus is outlined and fractured inward. The schneiderian membrane is carefully elevated until the correct vertical height is reached. F and G, Anorganic bovine-derived bone mineral (ABBM) and autogenous bone was applied and packed to the subantral space of the elevated sinus. Guided tissue regeneration membrane/titanium-reinforced (GTRM-TR) membrane was fixated on the palatal bone and a titanium tenting screw is placed protruding to the desired vertical position. Autogenous particulated bone was applied to the vertical defect. H and I, Buccal and occlusal views of GTRM-TR membrane secured over the graft with titanium pins. J, After 9 months of uneventful healing, the GTRM-TR membrane has maintained its position. K and L, Buccal and occlusal views of the regenerated alveolar bone crest. M, The final reconstruction demonstrates a functional and esthetic outcome. N, Stable crestal bone around the implants after 6 years of loading.
The efficacy of a 1:1 mixture of anorganic bovine-derived bone mineral (ABBM)* (Bio-Oss, Geistlich Pharma AG, Wolhusen, Switzerland) and autogenous particulated bone graft using ePTFE membranes was evaluated histologically and histomorphometrically in 8 patients (10 ridge defects).29 After a healing period of 6 to 9 months, a mean vertical gain of 3.15 mm (SD ±1.12 mm) was achieved. The histologic analysis demonstrated new bone formation and ongoing remodeling of autogenous particulated bone and the ABBM particles. However, long-term results are not available to confirm the predictability of the procedure or implant success. More long-term studies are needed.
Distraction Osteogenesis
Distraction osteogenesis is a surgical technique that has been developed to increase vertical bone height in the deficient jaw site and contrasts with the more conventional method of bone grafting with or without membranes. Under the proper circumstances, most cells in bone can differentiate into osteogenic (or chondrogenic) cells needed for repair. Ilizarov popularized the concept of distraction osteogenesis in the 1980s by developing a protocol for “cutting” long bones and “stretching” them during the healing process.13-15
Based on experimental and clinical studies over 35 years, distraction osteogenesis can provide a surgeon with the ability to treat small bones in the hands and feet using external fixation devices. Recently, new intraoral devices for vertical bone growth of the alveolar process have been developed and successfully applied in preparation for the placement of dental implants. Other important advantages of distraction osteogenesis are that it may avoid the need for a second surgical site to harvest bone, and the newly created bone has native bone at the crest, which is thought to withstand forces better than regenerated bone.
One of the most significant disadvantages of the distraction osteogenesis procedure for intraoral application is the unidirectional limitation of current devices. The application of distraction osteogenesis for vertical bone growth has shown good predictability. However, limitations have been encountered in achieving horizontal bone growth with this method. Secondary bone grafting is frequently needed following vertical distraction osteogenesis, especially for the extremely resorbed (narrow) ridges. Consequently, distraction osteogenesis cannot be expected to solve vertical ridge defects without the use of additional augmentation procedures.
Growth Factors in Bone Augmentation
Current research is exploring the use of various growth factors to induce bone formation.5 These bone-inductive mediators are powerful modifiers of the healing process. Incorporation of osteoinductive mediators into bone graft material or other carriers can be applied to sites in conjunction with conventional bone augmentation procedures to enhance the outcome.
Most of the clinical techniques available to try and stimulate new bone growth at such sites utilize some type of bone replacement graft, including autograft, allograft, xenograft, or alloplast. These bone graft materials have both advantages and limitations. Consequently, attempts have been made to improve bone grafting by either using growth factors alone or growth factors combined with a bone replacement graft.1,26,27 The rationale is that bone formation can be further enhanced when a growth factor is used to stimulate osteoblast precursor or osteoblast cells and hence to push the bone formation/bone resorption balance in favor of bone formation.25
Bone Morphogenetic Proteins
Perhaps the most studied of all the osteoinductive growth factors are the bone morphogenetic proteins (BMPs), which belong to the transforming growth factor beta (TGF-β) superfamily. Of this family, recombinant human bone morphogenetic protein-2 (rhBMP-2) has shown significant signs of bone-enhancing potential.
One commercial bone growth factor product has been approved by the Food and Drug Administration (FDA) for use in the oral cavity to stimulate bone formation. As was noted in the use of growth factors for periodontal regeneration, the growth factor protein must be combined with a carrier to have activity and be used clinically. The commercially available bone growth product contains rhBMP-2 combined with a bovine type I collagen sponge. This product has been cleared for oral cavity use in both sinus lift augmentation therapy and for ridge augmentation in maxillary anterior extraction sites with bone loss.4,5,10,12,38
The BMPs are a group of related proteins that are found in the body and are important for skeletal development.7,8,43 Each of the proteins has relatively specific functions, and BMP-2 has been shown to have some of the strongest bone-producing activity. BMP-7 (also called osteogenic protein-1 [OP-1]) and BMP-3 (also known as osteogenin) have also been shown to stimulate bone formation. The BMPs were originally isolated from bovine bone by Marshall Urist.40 As a growth factor, the BMPs induce the differentiation of mesenchymal stem cells to become bone-producing osteoblast cells. Thus, unlike proliferation factors that increase the number of cells, the BMPs are differentiation factors that stimulate cells to produce bone tissue. Many carriers have been tested with the BMPs, but the binding and release kinetics using bovine type I collagen have proved to be the most useful clinically. BMP binds tightly to the collagen within minutes and has been shown to be released over time for 2 to 3 weeks at the defect site. The extended release kinetics likely allow the undifferentiated mesenchymal cells migrating into the wound site over time to be exposed to the growth factor. These BMPs have been extensively studied and have been shown to stimulate bone formation in many animal models and in humans under a variety of conditions and indications.41 In fact, the same product approved for use in the oral cavity had previously been approved by the FDA for use in single-level spine fusion procedures and in open tibial fractures in humans.
The BMPs have specific receptors on the surfaces of cells.24,35,44 Binding of the BMP causes dimerization of the receptor proteins, which in turn stimulates a cascade of events intracellularly involving a set of proteins called SMADs. The end result of the intracellular cascade is the activation of genetic activity and bone cell differentiation.
The preclinical results of using rhBMP-2 in animals with critical-sized defects have reported rapid new bone formation. The inductive capacity of rhBMP-2 was demonstrated by impregnating a polymer carrier and placing the substrate in critical-sized rat mandibular defects with or without a barrier membrane.20 The study evaluated 12- and 24-day healing times and showed a bony union of the defects for rhBMP-treated sites. The control sites were not closed at the same intervals.
The clinical results of using rhBMP-2 and collagen in patients are remarkable considering that only one bone differentiation agent is being delivered to the bone site and it is only delivered at the time of the surgical procedure. Relatively high doses of the protein are often used in some sites however, possibly as the result of the need to release effective doses at later times. Future research directions will likely focus on more targeted delivery of the bone growth factor at specified times during the wound healing process.
The use of growth factors for bone augmentation has the potential to completely eliminate the need of bone harvesting and any bone filler materials, and preliminary results are encouraging. However, the clinician must recognize that there is limited clinical information available on these new modalities, and no information on resorption of the regenerated bone, implant survival, or bone remodeling around implants. Further documentation from long-term, randomized, controlled clinical studies are necessary.
Autologous Platelet Concentration
In recent years, a new approach to enhance the vitality of bone grafts has been introduced by using platelet concentrate or platelet-rich plasma (PRP).21 PRP is an autologous source of platelet-derived growth factors and transforming growth factors that is obtained by sequestering and concentrating platelets by centrifugation. The patient’s own blood is withdrawn and separated into platelet-rich and platelet-poor components. The PRP is the important content, containing a high-level mixture of platelets and a concentration of growth factors. This PRP mixture is added to the autologous bone graft and has been shown to increase the quality of and reduce the time needed for bone regeneration. Clinical and experimental studies are scarce but suggest that this technique holds promise for large bone defects and bone defects with low osteogenic potential. Extrapolation to the possible effect of PRP on other bone-filler materials cannot be made at this time.
Conclusion
Bone augmentation and advanced implant surgery procedures allow clinicians to reconstruct vertical alveolar bone deficiencies and replace missing teeth with endosseous dental implants. As stated in Chapter 72, the predictable outcome of these procedures depends on several biologic principles that must be followed. Diagnosis, treatment planning, careful execution of the surgical treatment, postoperative follow-up, and appropriate implant loading are all important factors in achieving success. Sinus elevation and bone augmentation has become a widely used and predictable procedure to augment the deficient posterior maxilla (i.e., pneumatized maxillary sinus). Reconstruction of vertically deficient ridges remains a significant challenge despite the reported progress and success of new techniques.
![]() Science Transfer
Science Transfer
A variety of bone grafting techniques and materials are successful in creating sufficient bone volume in maxillary sinuses where insufficient bone was available to place implants. In cases in which there is 5 mm or more of bone height, the space for grafts can be completed by elevating the sinus membrane through the osteotomy created for implant placement. This can be accomplished with osteotomes or threaded elevators. In addition, there are special surgical instruments designed to release and lift the membrane through the apical end of the osteotomy so that grafts can be placed. In more advanced cases, a lateral window can be created to gain access for elevating the sinus membrane and for placing graft material.
Implants can be placed simultaneously with sinus grafting if sufficient bone is available to give initial stabilization of the implants. This generally requires at least 5 mm of bone height. In those cases in which stability of implants cannot be obtained, it is necessary to wait a minimum of 5 months for bone growth into the sinus graft before placing implants.
In deficient ridges, bone height can be increased by using special surgical procedures with bone grafts covered by titanium reinforced nonresorbable membranes. This can give an average of 3 to 4 mm gain but requires a meticulous management of flaps so that they are released and can be sutured with a watertight closure.
Distraction osteogenesis is used in cases where significant improvements in height of bone is needed. This is also a complex surgical procedure that requires highly skilled surgeons. As much as 7 or 8 mm of additional bone height can be obtained and once the initial distraction has occurred, there is a wait of at least 5 months before implant placement. These cases frequently require subsequent bone grafts to obtain sufficient width of the implant site.
Platelet-rich plasma can be used to supplement bone graft materials, however most cases are successfully treated using bone grafts alone. Recently, bone morphogenetic protein has become available for clinical use with a collagen carrier. This material has been successful in a number of applications including maxillary sinus grafts and regenerative surgery at the time of tooth extraction.
1 Boyan BD, Weesner TC, Lohmann CH, et al. Porcine fetal enamel matrix derivative enhances bone formation induced by demineralized freeze dried bone allograft in vivo. J Periodontol. 2000;71:1278-1286.
2 Boyne PJ. History of maxillary sinus grafting. In: Jensen Ole T, editor. The sinus bone graft. 2nd ed. Hanover Park, Illinois: Quintessence Publishing Co. Inc; 2006:3-12.
3 Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38:613-616.
4 Boyne PJ, Lilly LC, Marx RE, et al. De novo bone induction by recombinant human bone morphogenetic protein-2 (rhBMP-2) in maxillary sinus floor augmentation. J Oral Maxillofac Surg. 2005;63:1693-1707.
5 Boyne PJ, Marx RE, Nevins M, et al. A feasibility study evaluating rhBMP-2/absorbable collagen sponge for maxillary sinus floor augmentation. Int J Periodontics Restorative Dent. 1997;17:11-25.
6 Bruschi GB, Scipioni A, Calesini G, Bruschi E. Localized management of sinus floor with simultaneous implant placement: a clinical report. Int J Oral Maxillofac Implants. 1998;13:219-226.
7 Chen D, Zhao M, Mundy GR. Bone morphogenetic proteins. Growth Factors. 2004;22:233-241.
8 Cochran DL, Wozney JM. Biological mediators for periodontal regeneration. Periodontol 2000. 1999;19:40-58.
9 Del Fabbro M, Testori T, Francetti L, et al. Systematic review of survival rates for implants placed in the grafted maxillary sinus. Int J Periodontics Restorative Dent. 2004;24:565.
10 Fiorellini JP, Howell TH, Cochran D, et al. Randomized study evaluating recombinant human bone morphogenetic protein-2 for extraction socket augmentation. J Periodontol. 2005;76:605-613.
11 Geurs NC, Wang IC, Shulman LB, Jeffcoat MK. Retrospective radiographic analysis of sinus graft and implant placement procedures from the Academy of Osseointegration Consensus Conference on Sinus Grafts. Int J Periodontics Restorative Dent. 2001;21:517-523.
12 Howell TH, Fiorellini J, Jones A, et al. A feasibility study evaluating rhBMP-2/absorbable collagen sponge device for local alveolar ridge preservation or augmentation. Int J Periodontics Restorative Dent. 1997;17:124-139.
13 Ilizarov GA. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res. 1989:263-285.
14 Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989:249-281.
15 Ilizarov GA. Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res. 1990:8-26.
16 Jaffin RA, Berman CL. The excessive loss of Branemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991;62:2-4.
17 Jensen OT, Shulman LB, Block MS, Iacono VJ. Report of the Sinus Consensus Conference of 1996. Int J Oral Maxillofac Implants. 1998;13(Suppl):11-45.
18 Jovanovic SA, Schenk RK, Orsini M, Kenney EB. Supracrestal bone formation around dental implants: an experimental dog study. Int J Oral Maxillofac Implants. 1995;10:23-31.
19 Levin L, Herzberg R, Dolev E, Schwartz-Arad D. Smoking and complications of onlay bone grafts and sinus lift operations. Int J Oral Maxillofac Implants. 2004;19:369-373.
20 Linde A, Hedner E. Recombinant bone morphogenetic protein-2 enhances bone healing, guided by osteopromotive e-PTFE membranes: an experimental study in rats. Calcif Tissue Int. 1995;56:549-553.
21 Marx RE, Carlson ER, Eichstaedt RM, et al. Platelet-rich plasma: growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:638-646.
22 Peleg M, Mazor Z, Chaushu G, Garg AK. Sinus floor augmentation with simultaneous implant placement in the severely atrophic maxilla. J Periodontol. 1998;69:1397-1403.
23 Raghoebar GM, Batenburg RH, Timmenga NM, et al. Morbidity and complications of bone grafting of the floor of the maxillary sinus for the placement of endosseous implants. Mund Kiefer Gesichtschir. 1999;3(Suppl 1):S65-S69.
24 Rosen V. BMP and BMP inhibitors in bone. Ann N Y Acad Sci. 2006;1068:19-25.
25 Schwartz Z, Carnes DLJr, Pulliam R, et al. Porcine fetal enamel matrix derivative stimulates proliferation but not differentiation of pre-osteoblastic 2T9 cells, inhibits proliferation and stimulates differentiation of osteoblast-like MG63 cells, and increases proliferation and differentiation of normal human osteoblast NHOst cells. J Periodontol. 2000;71:1287-1296.
26 Schwartz Z, Mellonig JT, Carnes DLJr, et al. Ability of commercial demineralized freeze-dried bone allograft to induce new bone formation. J Periodontol. 1996;67:918-926.
27 Schwartz Z, Somers A, Mellonig JT, et al. Addition of human recombinant bone morphogenetic protein-2 to inactive commercial human demineralized freeze-dried bone allograft makes an effective composite bone inductive implant material. J Periodontol. 1998;69:1337-1345.
28 Schwartz-Arad D, Herzberg R, Dolev E. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol. 2004;75:511-516.
29 Simion M, Fontana F, Rasperini G, Maiorana C. Vertical ridge augmentation by expanded-polytetrafluoroethylene membrane and a combination of intraoral autogenous bone graft and deproteinized anorganic bovine bone (Bio Oss). Clin Oral Implants Res. 2007;18:620-629.
30 Simion M, Jovanovic SA, Tinti C, Benfenati SP. Long-term evaluation of osseointegrated implants inserted at the time or after vertical ridge augmentation. A retrospective study on 123 implants with 1-5 year follow-up. Clin Oral Implants Res. 2001;12:35-45.
31 Simion M, Jovanovic SA, Trisi P, et al. Vertical ridge augmentation around dental implants using a membrane technique and autogenous bone or allografts in humans. Int J Periodontics Restorative Dent. 1998;18:8-23.
32 Simion M, Trisi P, Piattelli A. Vertical ridge augmentation using a membrane technique associated with osseointegrated implants. Int J Periodontics Restorative Dent. 1994;14:496-511.
33 Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium. 1994;15:152. 154-156, 158 passim; quiz 162
34 Summers RB. Sinus floor elevation with osteotomes. J Esthet Dent. 1998;10:164-171.
35 ten Dijke P. Bone morphogenetic protein signal transduction in bone. Curr Med Res Opin. 2006;22(Suppl 1):S7-S11.
36 Tinti C, Parma-Benfenati S. Vertical ridge augmentation: surgical protocol and retrospective evaluation of 48 consecutively inserted implants. Int J Periodontics Restorative Dent. 1998;18:434-443.
37 Toffler M. Osteotome-mediated sinus floor elevation: a clinical report. Int J Oral Maxillofac Implants. 2004;19:266-273.
38 Triplett RG, Nevins M, Marx RE, et al. Pivotal, randomized, parallel evaluation of recombinant human bone morphogenetic protein-2/absorbable collagen sponge and autogenous bone graft for maxillary sinus floor augmentation. J Oral Maxillofac Surg. 2009;67:1947-1960.
39 Urban IA, Jovanovic SA, Lozada JL. Vertical ridge augmentation using guided bone regeneration (GBR) in three clinical scenarios prior to implant placement: a retrospective study of 35 patients 12 to 72 months after loading. Int J Oral Maxillofac Implants. 2009;24:502-510.
40 Urist MR. Bone: formation by autoinduction. Science. 1965;150:893-899.
41 Wikesjo UM, Huang YH, Polimeni G, Qahash M. Bone morphogenetic proteins: a realistic alternative to bone grafting for alveolar reconstruction. Oral Maxillofac Surg Clin North Am. 2007;19:535-551. vi-vii
42 Winter A, Pollack AS, Odrich RB. Placement of implants in the severly atrophic posterior maxilla using localized management of the sinus floor: a preliminary study. Int J Oral Maxillofac Implants. 2002;17:687.
43 Wozney JM. The bone morphogenetic protein family: multifunctional cellular regulators in the embryo and adult. Eur J Oral Sci. 1998;106(Suppl 1):160-166.
44 Wu X, Shi W, Cao X. Multiplicity of BMP signaling in skeletal development. Ann N Y Acad Sci. 2007;1116:29-49.
