7 Upper Limb
Conceptual overview
GENERAL DESCRIPTION
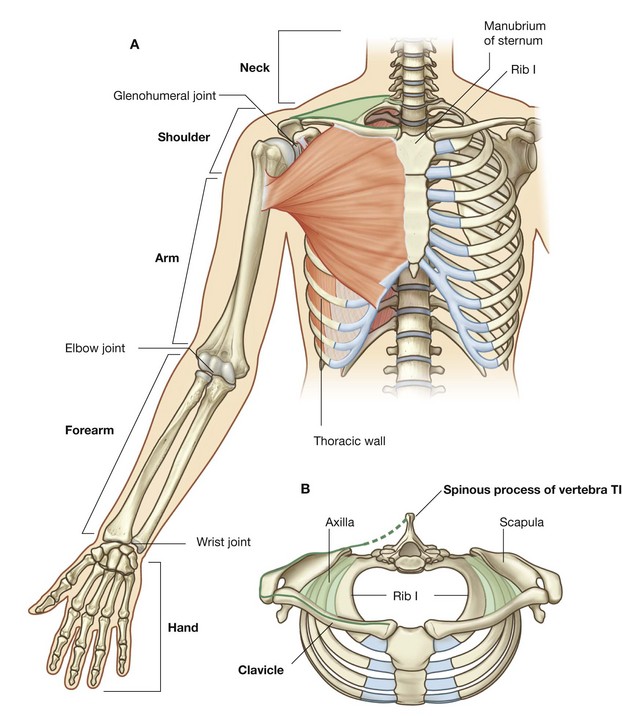
The upper limb is associated with the lateral aspect of the lower portion of the neck and with the thoracic wall. It is suspended from the trunk by muscles and a small skeletal articulation between the clavicle and the sternum—the sternoclavicular joint. Based on the position of its major joints and component bones, the upper limb is divided into shoulder, arm, forearm, and hand (Fig. 7.1A).
The shoulder is the area of upper limb attachment to the trunk (Fig. 7.1B).
The arm is the part of the upper limb between the shoulder and the elbow joint; the forearm is between the elbow joint and the wrist joint; and the hand is distal to the wrist joint.
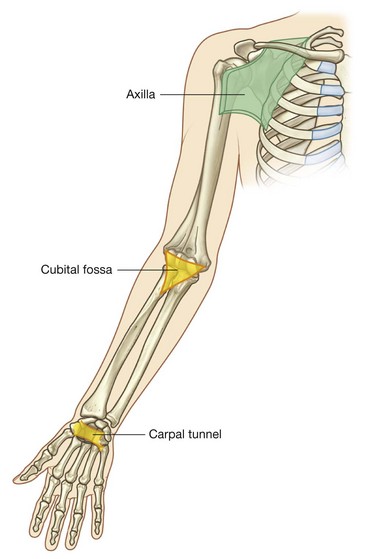
The axilla, cubital fossa, and carpal tunnel are significant areas of transition between the different parts of the limb (Fig. 7.2). Important structures pass through, or are related to, each of these areas.
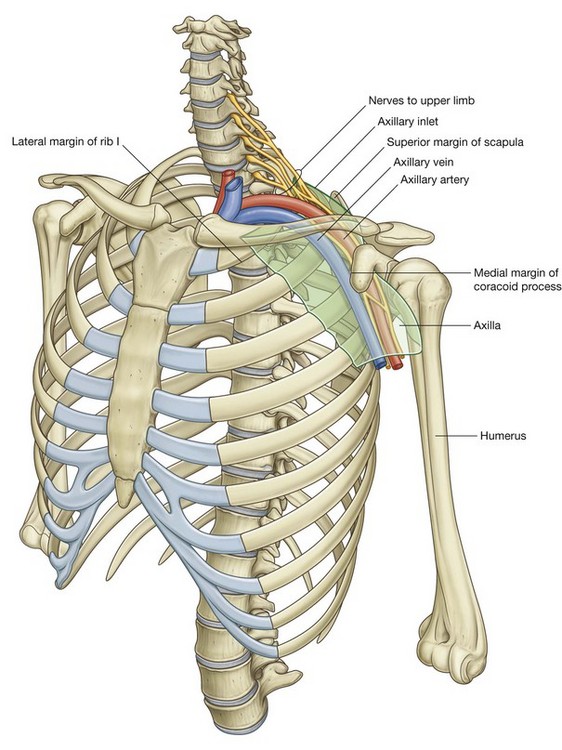
The axilla is an irregularly shaped pyramidal area formed by muscles and bones of the shoulder and the lateral surface of the thoracic wall. The apex or inlet opens directly into the lower portion of the neck. The skin of the armpit forms the floor. All major structures that pass between the neck and arm pass through the axilla.
The cubital fossa is a triangularly shaped depression formed by muscles anterior to the elbow joint. The major artery, the brachial artery, passing from the arm to the forearm passes through this fossa, as does one of the major nerves of the upper limb, the median nerve.
The carpal tunnel is the gateway to the palm of the hand. Its posterior, lateral, and medial walls form an arch, which is made up of small carpal bones in the proximal region of the hand. A thick band of connective tissue, the flexor retinaculum, spans the distance between each side of the arch and forms the anterior wall of the tunnel. The median nerve and all the long flexor tendons passing from the forearm to the digits of the hand pass through the carpal tunnel.
FUNCTIONS
Positioning the hand
Unlike the lower limb, which is used for support, stability, and locomotion, the upper limb is highly mobile for positioning the hand in space.
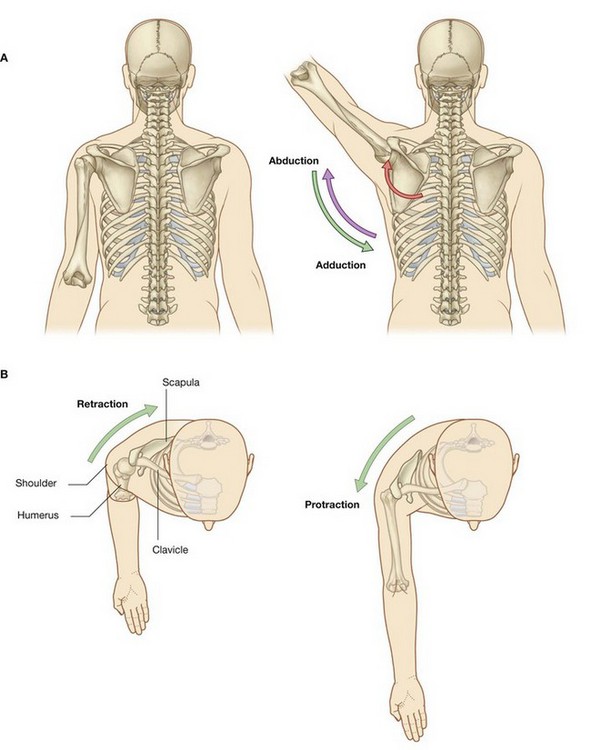
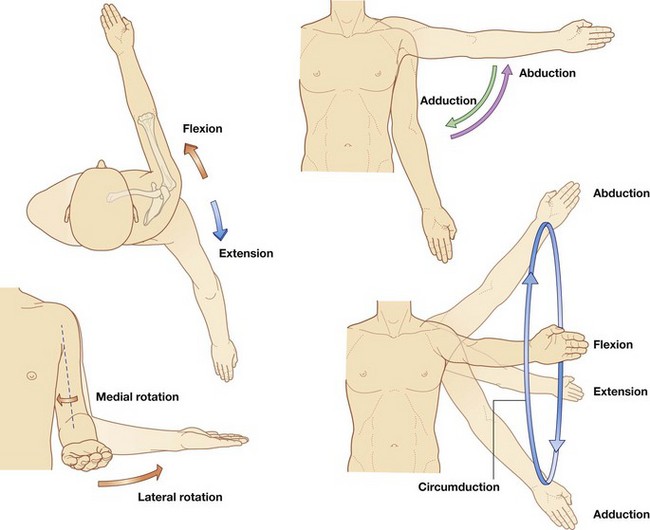
The shoulder is suspended from the trunk predominantly by muscles and can therefore be moved relative to the body. Sliding (protraction and retraction) and rotating the scapula on the thoracic wall changes the position of the glenohumeral joint (shoulder joint) and extends the reach of the hand (Fig. 7.3). The glenohumeral joint allows the arm to move around three axes with a wide range of motion. Movements of the arm at this joint are flexion, extension, abduction, adduction, medial rotation (internal rotation), lateral rotation (external rotation), and circumduction (Fig. 7.4).
The major movements at the elbow joint are flexion and extension of the forearm (Fig. 7.5A). At the other end of the forearm, the distal end of the lateral bone, the radius, can be flipped over the adjacent head of the medial bone, the ulna. Because the hand is articulated with the radius, it can be efficiently moved from a palm-anterior position to a palm-posterior position simply by crossing the distal end of the radius over the ulna (Fig. 7.5B). This movement, termed pronation, occurs solely in the forearm. Supination returns the hand to the anatomical position.
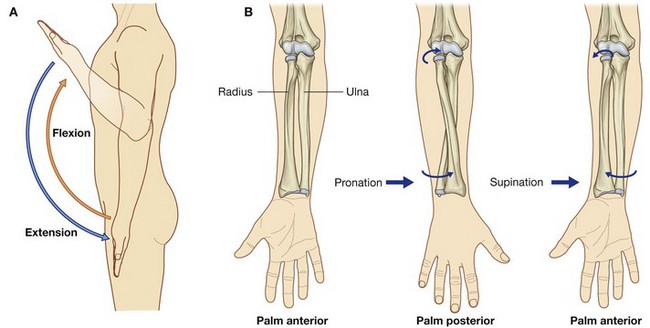
Fig. 7.5 Movements of the forearm. A. Flexion and extension at the elbow joint. B. Pronation and supination.
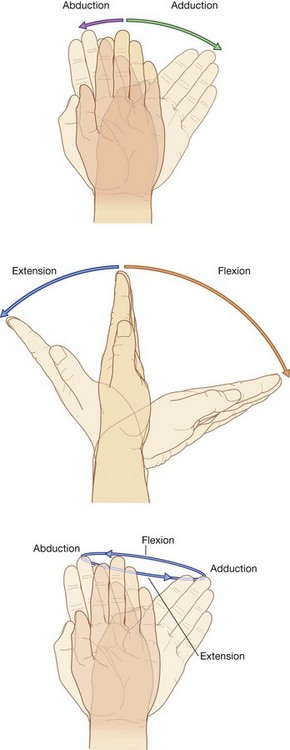
At the wrist joint, the hand can be abducted, adducted, flexed, extended, and circumducted (Fig. 7.6). These movements, combined with those of the shoulder, arm, and forearm, enable the hand to be placed in a wide range of positions relative to the body.
The hand as a mechanical tool
One of the major functions of the hand is to grip and manipulate objects. Gripping objects generally involves flexing the fingers against the thumb. Depending on the type of grip, muscles in the hand act to:
The hand as a sensory tool
The hand is used to discriminate between objects on the basis of touch. The pads on the palmar aspect of the fingers contain a high density of somatic sensory receptors. Also, the sensory cortex of the brain devoted to interpreting information from the hand, particularly from the thumb, is disproportionately large relative to that for many other regions of skin.
COMPONENT PARTS
Bones and joints
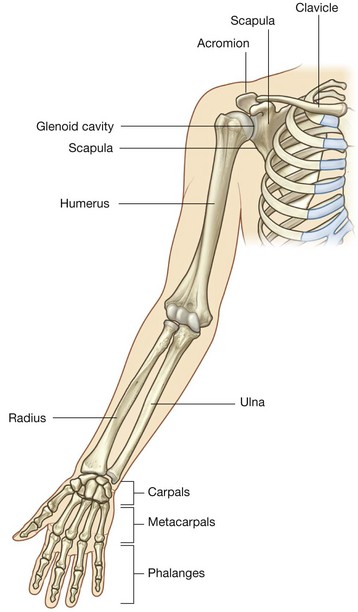
The bones of the shoulder consist of the scapula, clavicle, and proximal end of the humerus (Fig. 7.7).
The clavicle articulates medially with the manubrium of the sternum and laterally with the acromion of the scapula, which arches over the joint between the glenoid cavity of the scapula and the head of the humerus (the glenohumeral joint).
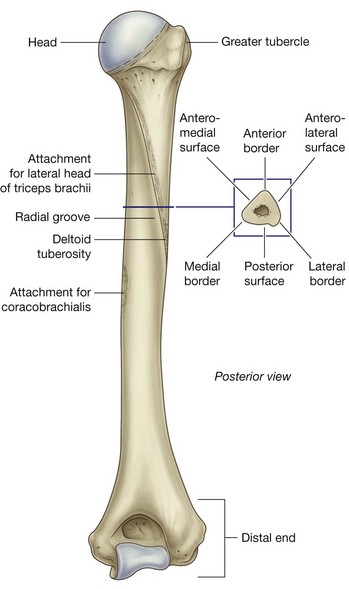
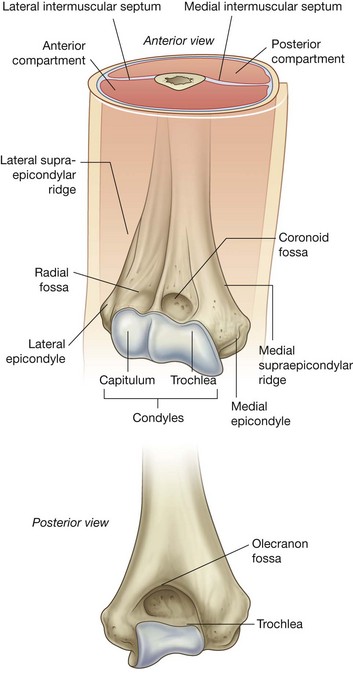
The humerus is the bone of the arm (Fig. 7.7). The distal end of the humerus articulates with the bones of the forearm at the elbow joint, which is a hinge joint that allows flexion and extension of the forearm.
The forearm contains two bones:
At the elbow joint, the proximal ends of the radius and ulna articulate with each other as well as with the humerus.
In addition to flexing and extending the forearm, the elbow joint allows the radius to spin on the humerus while sliding against the head of the ulna during pronation and supination of the hand.
The distal portions of the radius and the ulna also articulate with each other. This joint allows the end of the radius to flip from the lateral side to the medial side of the ulna during pronation of the hand.
The wrist joint is formed between the radius and carpal bones of the hand and between an articular disc, distal to the ulna, and carpal bones.
The bones of the hand consist of the carpal bones, the metacarpal bones, and the phalanges (Fig. 7.7).
The five digits in the hand are the thumb and the index, middle, ring, and little fingers.
Joints between the eight small carpal bones allow only limited amounts of movement; as a result, the bones work together as a unit.
The five metacarpal bones, one for each digit, are the primary skeletal foundation of the palm (Fig. 7.7).
The joint between the metacarpal bone of the thumb (metacarpal I) and one of the carpal bones allows greater mobility than the limited sliding movement that occurs at the carpometacarpal joints of the fingers.
Distally, the heads of metacarpals II to V (i.e., except that of the thumb) are interconnected by strong ligaments. Lack of this ligamentous connection between the metacarpal bones of the thumb and index finger together with the biaxial saddle joint between the metacarpal bone of the thumb and the carpus provide the thumb with greater freedom of movement than the other digits of the hand.
The bones of the digits are the phalanges (Fig. 7.7). The thumb has two phalanges, while each of the other digits has three.
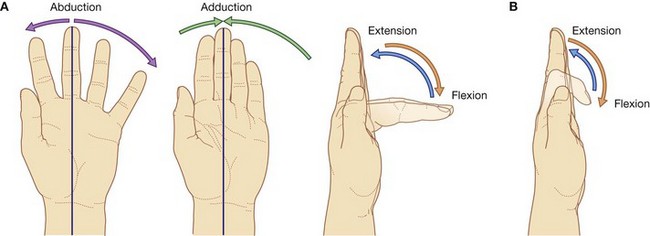
The metacarpophalangeal joints are biaxial condylar joints (ellipsoid joints) that allow abduction, adduction, flexion, extension, and circumduction (Fig. 7.8). Abduction and adduction of the fingers is defined in reference to an axis passing through the center of the middle finger in the anatomical position. The middle finger can therefore abduct both medially and laterally and adduct back to the central axis from either side. The interphalangeal joints are primarily hinge joints that allow only flexion and extension.
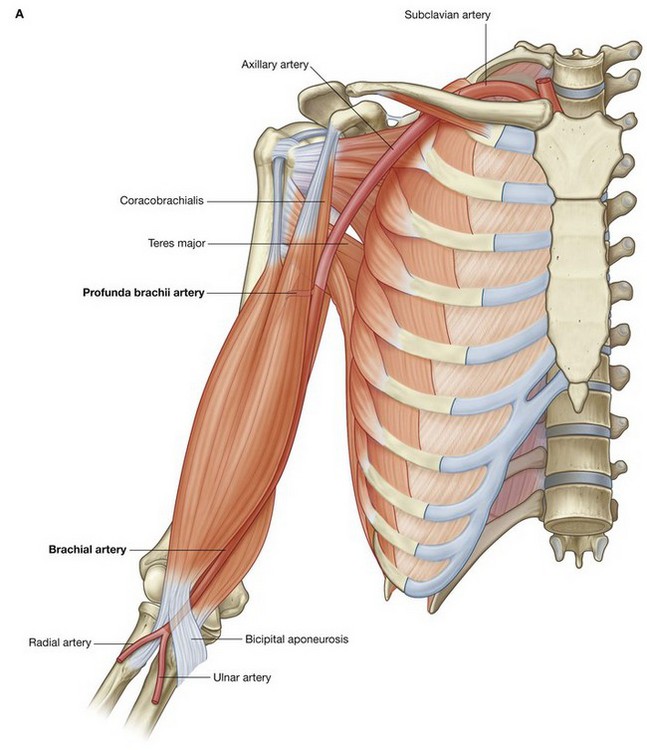
Muscles
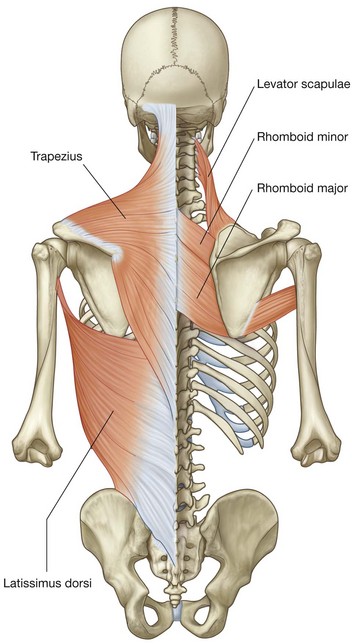
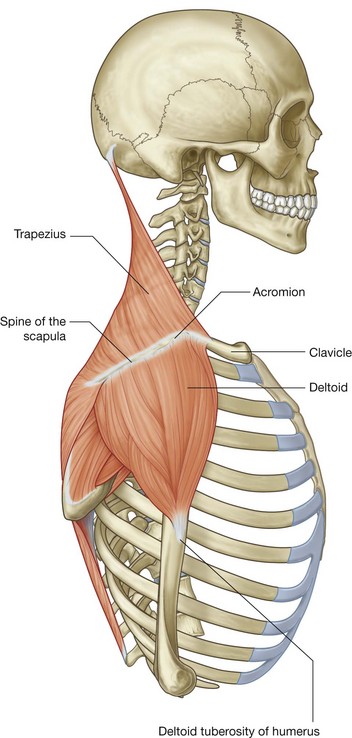
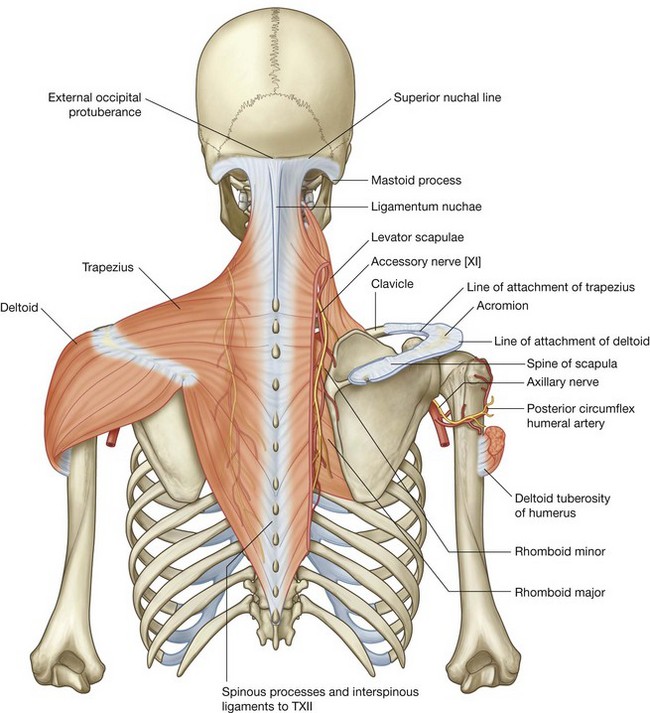
Some muscles of the shoulder, such as the trapezius, levator scapulae, and rhomboids, connect the scapula and clavicle to the trunk. Other muscles connect the clavicle, scapula, and body wall to the proximal end of the humerus. These include the pectoralis major, pectoralis minor, latissimus dorsi, teres major, and deltoid (Fig. 7.9A and B). The most important of these muscles are the four rotator cuff muscles—the subscapularis, supraspinatus, infraspinatus, and teres minor muscles—which connect the scapula to the humerus and provide support for the glenohumeral joint (Fig. 7.9C).
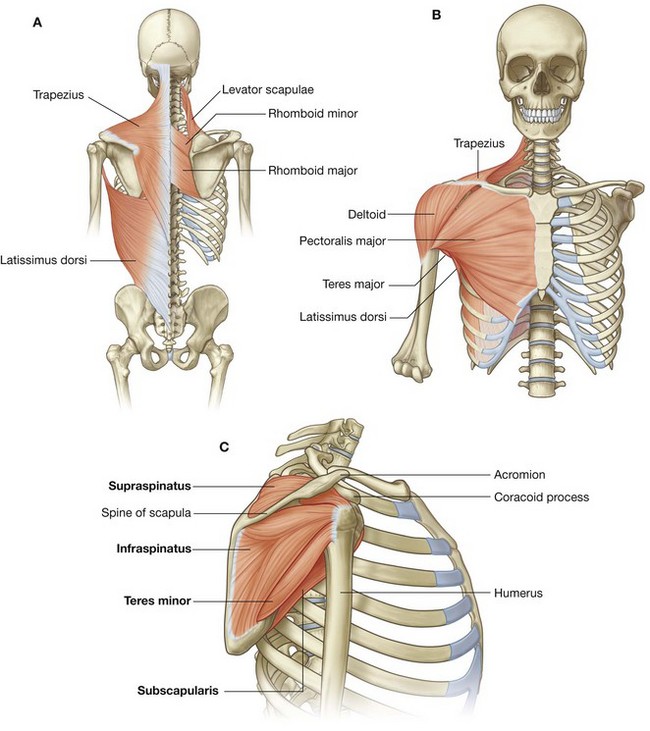
Fig. 7.9 Muscles of the shoulder. A. Posterior shoulder. B. Anterior shoulder. C. Rotator cuff muscles.
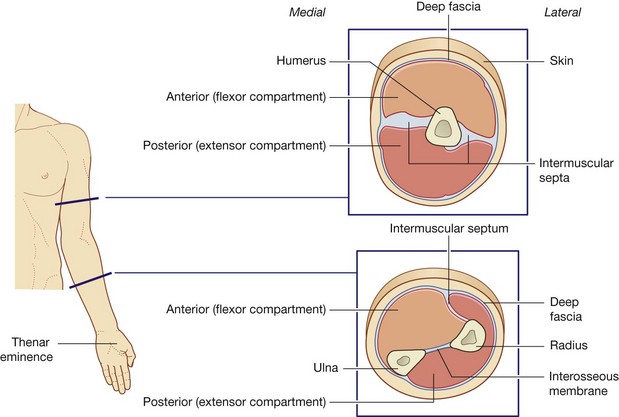
Muscles in the arm and forearm are separated into anterior (flexor) and posterior (extensor) compartments by layers of fascia, bones, and ligaments (Fig. 7.10).
The anterior compartment of the arm lies anteriorly in position and is separated from muscles of the posterior compartment by the humerus and by medial and lateral intermuscular septa. These intermuscular septa are continuous with the deep fascia enclosing the arm and attach to the sides of the humerus.
In the forearm, the anterior and posterior compartments are separated by a lateral intermuscular septum, the radius, the ulna, and an interosseous membrane, which joins adjacent sides of the radius and ulna (Fig. 7.10).
Muscles in the arm act mainly to move the forearm at the elbow joint, while those in the forearm function predominantly to move the hand at the wrist joint and the fingers and thumb.
Muscles found entirely in the hand, the intrinsic muscles, generate delicate movements of the digits of the hand and modify the forces produced by tendons coming into the fingers and thumb from the forearm. Included among the intrinsic muscles of the hand are three small thenar muscles, which form a soft tissue mound, called the thenar eminence, over the palmar aspect of metacarpal I. The thenar muscles allow the thumb to move freely relative to the other fingers.
RELATIONSHIP TO OTHER REGIONS
Neck
The upper limb is directly related to the neck. Lying on each side of the superior thoracic aperture at the base of the neck is an axillary inlet, which is formed by:
The major artery and vein of the upper limb pass between the thorax and the limb by passing over rib I and through the axillary inlet. Nerves, predominantly derived from the cervical portion of the spinal cord, also pass through the axillary inlet and the axilla to supply the upper limb.
Back and thoracic wall
Muscles that attach the bones of the shoulder to the trunk are associated with the back and the thoracic wall and include the trapezius, levator scapulae, rhomboid major, rhomboid minor, and latissimus dorsi (Fig. 7.12).
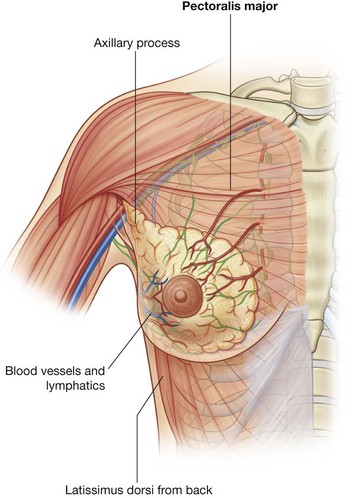
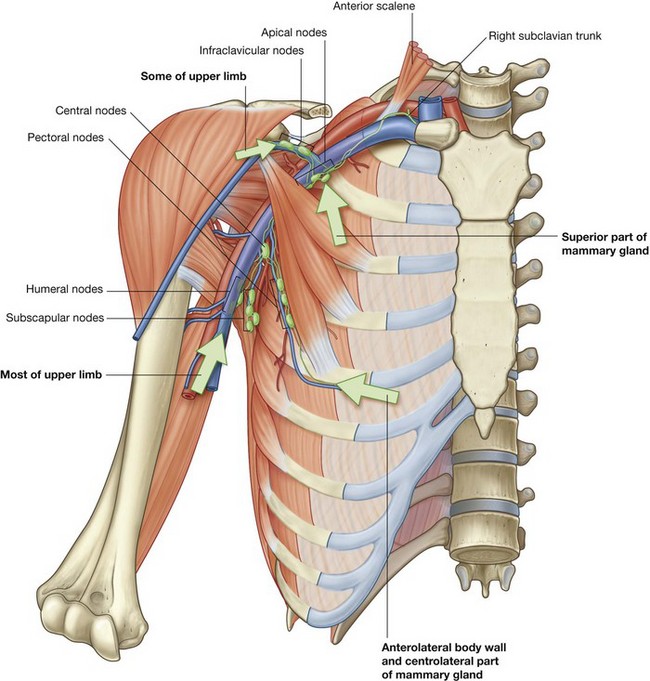
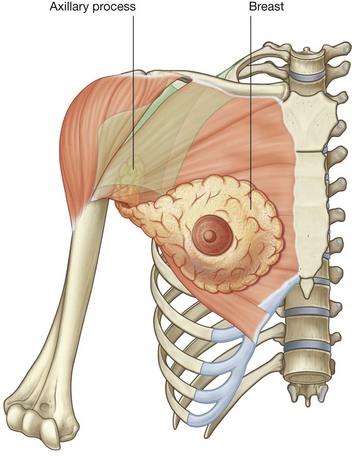
The breast on the anterior thoracic wall has a number of significant relationships with the axilla and upper limb. It overlies the pectoralis major muscle, which forms most of the anterior wall of the axilla and attaches the humerus to the chest wall (Fig. 7.13). Often, part of the breast known as the axillary process extends around the lateral margin of pectoralis major into the axilla.
Lymphatic drainage from lateral and superior parts of the breast is predominantly into lymph nodes in the axilla. Several arteries and veins that supply or drain the gland also originate from, or drain into, major axillary vessels.
KEY POINTS
Innervation by cervical and upper thoracic nerves
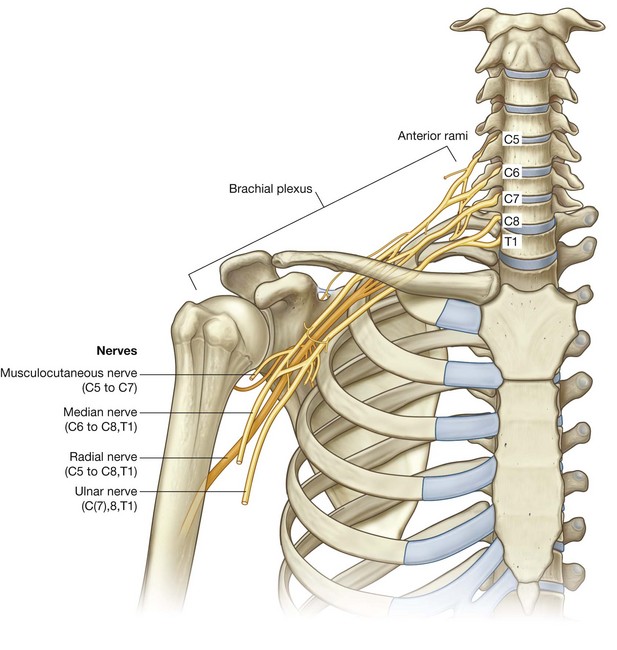
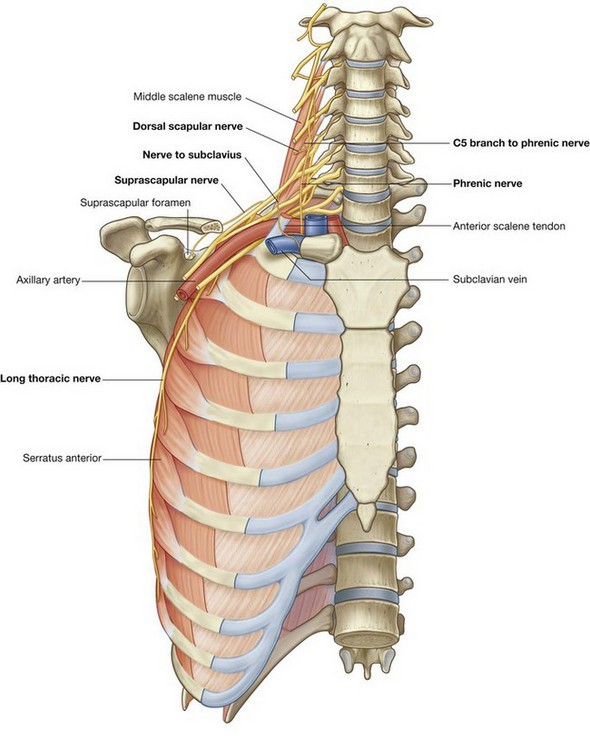
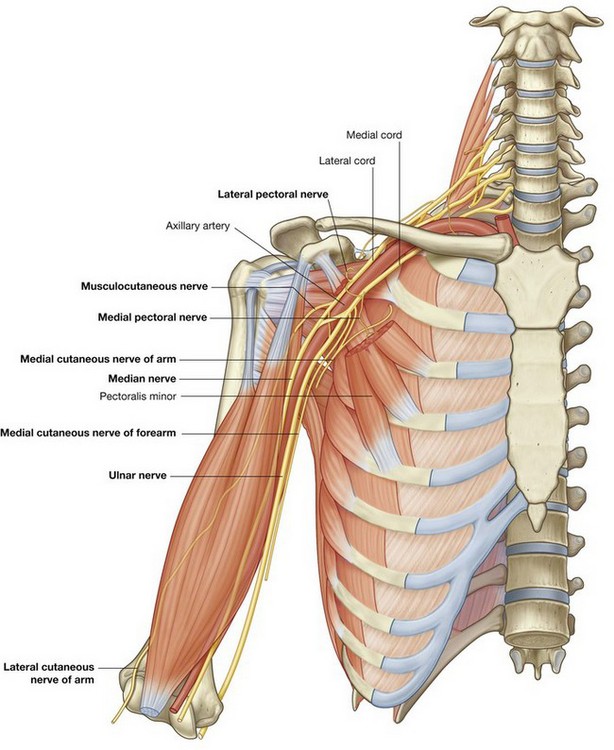
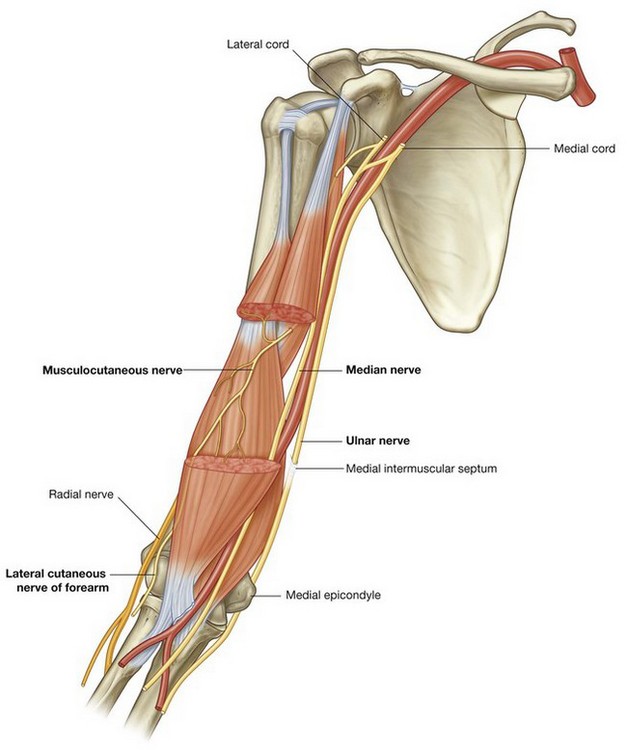
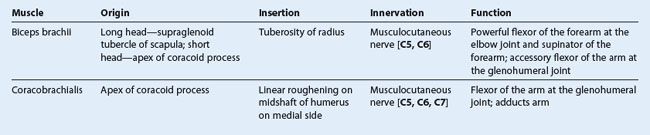
Innervation of the upper limb is by the brachial plexus, which is formed by the anterior rami of cervical spinal nerves C5 to C8, and T1 (Fig. 7.14). This plexus is initially formed in the neck and then continues through the axillary inlet into the axilla. Major nerves that ultimately innervate the arm, forearm, and hand originate from the brachial plexus in the axilla.
As a consequence of this innervation pattern, clinical testing of lower cervical and T1 nerves is carried out by examining dermatomes, myotomes, and tendon reflexes in the upper limb. Another consequence is that the clinical signs of problems related to lower cervical nerves—pain, pins and needles sensations or paresthesia, and muscle twitching—appear in the upper limb.
Dermatomes of the upper limb (Fig. 7.15A) are often tested for sensation. Areas where overlap of dermatomes is minimal include the:
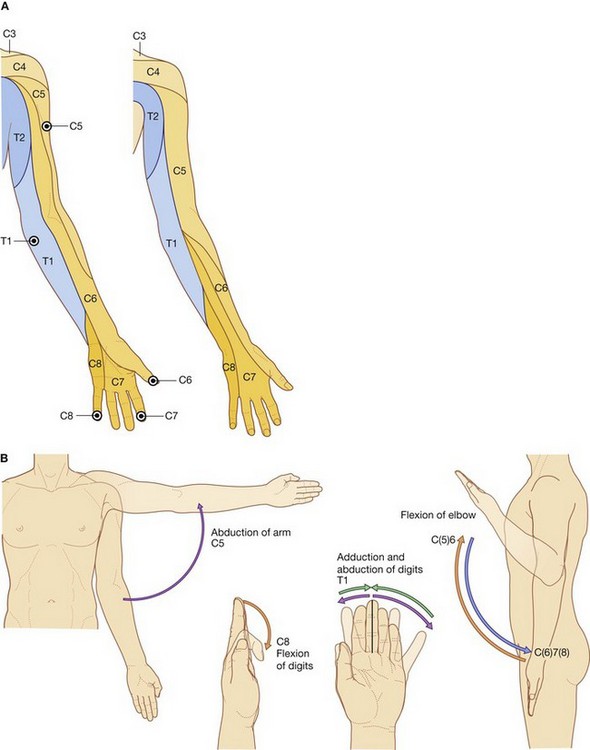
Fig. 7.15 Dermatomes and myotomes in the upper limb. A. Dermatomes. B. Movements produced by myotomes.
Selected joint movements are used to test myotomes (Fig. 7.15B):
In an unconscious patient, both somatic sensory and motor functions of spinal cord levels can be tested using tendon reflexes:
The major spinal cord level associated with innervation of the diaphragm, C4, is immediately above the spinal cord levels associated with the upper limb.
Evaluation of dermatomes and myotomes in the upper limb can provide important information about potential breathing problems that might develop as complications of damage to the spinal cord in regions just below the C4 spinal level.
Each of the major muscle compartments in the arm and forearm and each of the intrinsic muscles of the hand is innervated predominantly by one of the major nerves that originate from the brachial plexus in the axilla (Fig. 7.16A):
 the median nerve innervates the muscles in the anterior compartment of the forearm, with two exceptions—one flexor of the wrist (the flexor carpi ulnaris muscle) and part of one flexor of the fingers (the medial half of the flexor digitorum profundus muscle) are innervated by the ulnar nerve;
the median nerve innervates the muscles in the anterior compartment of the forearm, with two exceptions—one flexor of the wrist (the flexor carpi ulnaris muscle) and part of one flexor of the fingers (the medial half of the flexor digitorum profundus muscle) are innervated by the ulnar nerve; most intrinsic muscles of the hand are innervated by the ulnar nerve, except for the thenar muscles and two lateral lumbrical muscles, which are innervated by the median nerve;
most intrinsic muscles of the hand are innervated by the ulnar nerve, except for the thenar muscles and two lateral lumbrical muscles, which are innervated by the median nerve; all muscles in the posterior compartments of the arm and forearm are innervated by the radial nerve.
all muscles in the posterior compartments of the arm and forearm are innervated by the radial nerve.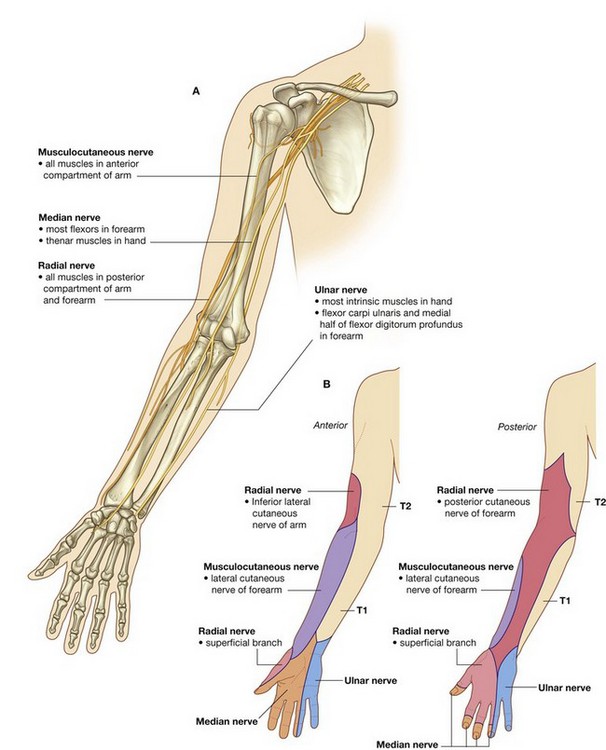
Fig. 7.16 Nerves of upper limb. A. Major nerves in the arm and forearm. B. Anterior and posterior areas of skin innervated by major peripheral nerves in the arm and forearm.
In addition to innervating major muscle groups, each of the major peripheral nerves originating from the brachial plexus carries somatic sensory information from patches of skin quite different from dermatomes (Fig. 7.16B). Sensation in these areas can be used to test for peripheral nerve lesions:
Nerves related to bone
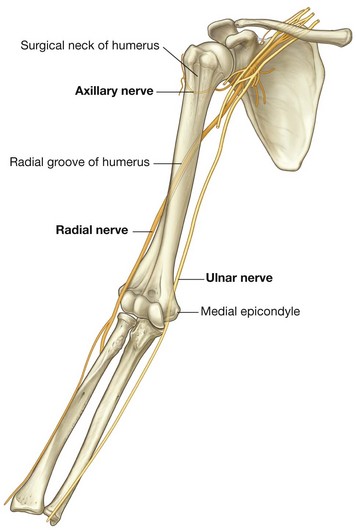
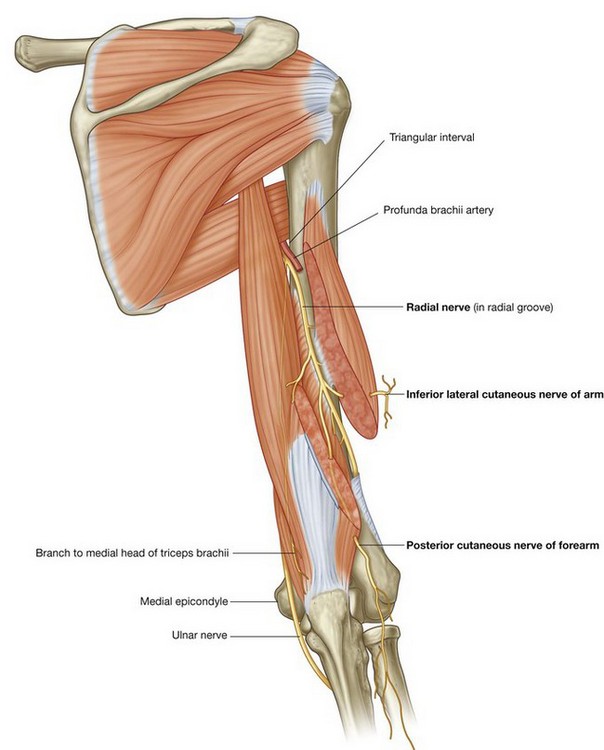
Three important nerves are directly related to parts of the humerus (Fig. 7.17):
 the axillary nerve, which supplies the deltoid muscle, a major abductor of the humerus at the glenohumeral joint, passes around the posterior aspect of the upper part of the humerus (the surgical neck);
the axillary nerve, which supplies the deltoid muscle, a major abductor of the humerus at the glenohumeral joint, passes around the posterior aspect of the upper part of the humerus (the surgical neck); the radial nerve, which supplies all of the extensor muscles of the upper limb, passes diagonally around the posterior surface of the middle of the humerus in the radial groove;
the radial nerve, which supplies all of the extensor muscles of the upper limb, passes diagonally around the posterior surface of the middle of the humerus in the radial groove; the ulnar nerve, which is ultimately destined for the hand, passes posteriorly to a bony protrusion, the medial epicondyle, on the medial side of the distal end of the humerus.
the ulnar nerve, which is ultimately destined for the hand, passes posteriorly to a bony protrusion, the medial epicondyle, on the medial side of the distal end of the humerus.Fractures of the humerus in any one of these three regions can endanger the related nerve.
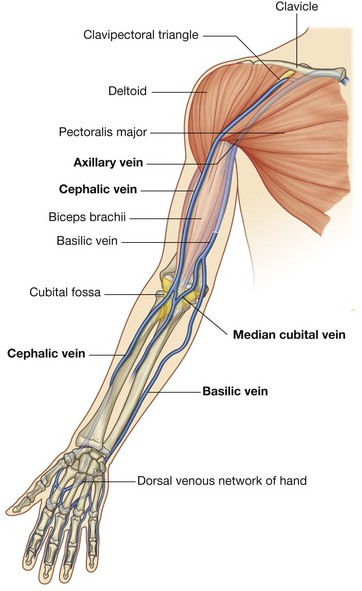
Superficial veins
Large veins embedded in the superficial fascia of the upper limb are often used to access a patient’s vascular system and to withdraw blood. The most significant of these veins are the cephalic, basilic, and median cubital veins (Fig. 7.18).
The cephalic and basilic veins originate from the dorsal venous network on the back of the hand.
The cephalic vein originates over the anatomical snuff box at the base of the thumb, passes laterally around the distal forearm to reach the anterolateral surface of the limb, and then continues proximally. It crosses the elbow, then passes up the arm into a triangular depression—the clavipectoral triangle (deltopectoral triangle)—between the pectoralis major muscle, deltoid muscle, and clavicle. In this depression, the vein passes into the axilla by penetrating deep fascia just inferior to the clavicle.
The basilic vein originates from the medial side of the dorsal venous network of the hand and passes proximally up the posteromedial surface of the forearm. It passes onto the anterior surface of the limb just inferior to the elbow and then continues proximally to penetrate deep fascia about midway up the arm.
At the elbow, the cephalic and basilic veins are connected by the median cubital vein, which crosses the roof of the cubital fossa.
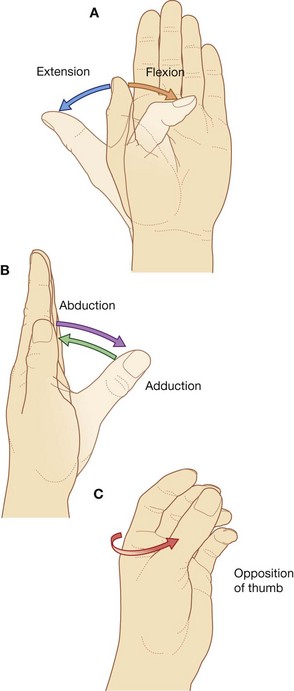
Orientation of the thumb
The thumb is positioned at right angles to the orientation of the index, middle, ring, and little fingers (Fig. 7.19). As a result, movements of the thumb occur at right angles to those of the other digits. For example, flexion brings the thumb across the palm, whereas abduction moves it away from the fingers at right angles to the palm.
Importantly, with the thumb positioned at right angles to the palm, only a slight rotation of metacarpal I on the wrist brings the pad of the thumb into a position directly facing the pads of the other fingers. This opposition of the thumb is essential for normal hand function.
Regional anatomy
SHOULDER
The shoulder is the region of upper limb attachment to the trunk.
The bone framework of the shoulder consists of:
The superficial muscles of the shoulder consist of the trapezius and deltoid muscles, which together form the smooth muscular contour over the lateral part of the shoulder. These muscles connect the scapula and clavicle to the trunk and to the arm, respectively.
Bones
Clavicle
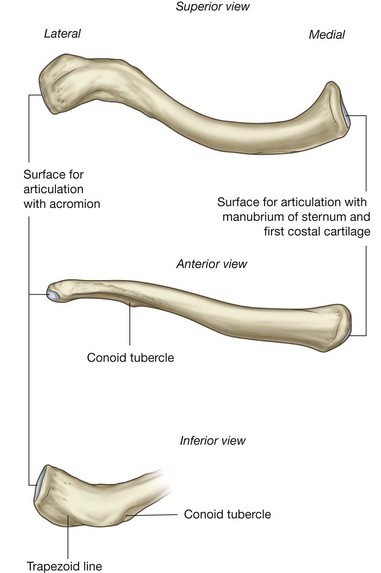
The clavicle is the only bony attachment between the trunk and the upper limb. It is palpable along its entire length and has a gentle S-shaped contour, with the forward-facing convex part medial and the forward-facing concave part lateral.
The acromial (lateral) end of the clavicle is flat, whereas the sternal (medial) end is more robust and somewhat quadrangular in shape (Fig. 7.20).
The acromial end of the clavicle has a small oval facet on its surface for articulation with a similar facet on the medial surface of the acromion of the scapula.
The sternal end has a much larger facet for articulation mainly with the manubrium of the sternum, and to a lesser extent, with the first costal cartilage.
The inferior surface of the lateral third of the clavicle possesses a distinct tuberosity consisting of a tubercle (the conoid tubercle) and lateral roughening (the trapezoid line), for attachment of the important coracoclavicular ligament.
In addition, the surfaces and margins of the clavicle are roughened by the attachment of muscles that connect the clavicle to the thorax, neck, and upper limb. The superior surface is smoother than the inferior surface.
Scapula
The scapula is a large, flat triangular bone with:
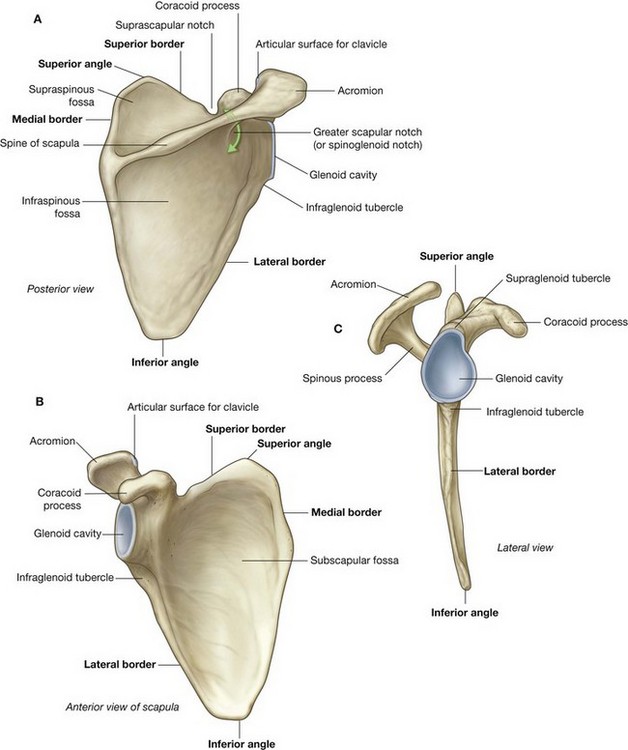
Fig. 7.21 Scapula. A. Posterior view of right scapula. B. Anterior view of costal surface. C. Lateral view.
The lateral angle of the scapula is marked by a shallow, somewhat comma-shaped glenoid cavity, which articulates with the head of the humerus to form the glenohumeral joint (Fig. 7.21B and 7.21C).
A large triangular-shaped roughening (the infraglenoid tubercle) inferior to the glenoid cavity is the site of attachment for the long head of the triceps brachii muscle.
A less distinct supraglenoid tubercle is located superior to the glenoid cavity and is the site of attachment for the long head of the biceps brachii muscle.
A prominent spine subdivides the posterior surface of the scapula into a small, superior supraspinous fossa and a much larger, inferior infraspinous fossa (Fig. 7.21A).
The acromion, which is an anterolateral projection of the spine, arches over the glenohumeral joint and articulates, via a small oval facet on its distal end, with the clavicle.
The region between the lateral angle of the scapula and the attachment of the spine to the posterior surface of the scapula is the greater scapular notch (spinoglenoid notch).
Unlike the posterior surface, the costal surface of the scapula is unremarkable, being characterized by a shallow concave subscapular fossa over much of its extent (Fig. 7.21B). The costal surface and margins provide for muscle attachment, and the costal surface, together with its related muscle (subscapularis), moves freely over the underlying thoracic wall.
The lateral border of the scapula is strong and thick for muscle attachment, whereas the medial border and much of the superior border is thin and sharp.
The superior border is marked on its lateral end by:
 the coracoid process, a hook-like structure that projects anterolaterally and is positioned directly inferior to the lateral part of the clavicle; and
the coracoid process, a hook-like structure that projects anterolaterally and is positioned directly inferior to the lateral part of the clavicle; andProximal humerus
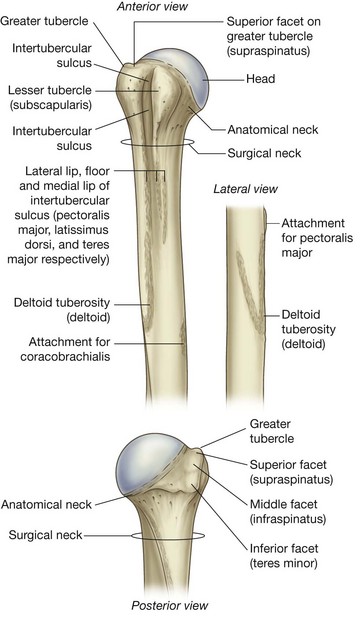
The proximal end of the humerus consists of the head, the anatomical neck, the greater and lesser tubercles, the surgical neck, and the superior half of the shaft of humerus (Fig. 7.22).
The head is half-spherical in shape and projects medially and somewhat superiorly to articulate with the much smaller glenoid cavity of the scapula.
The anatomical neck is very short and is formed by a narrow constriction immediately distal to the head. It lies between the head and the greater and lesser tubercles laterally, and between the head and the shaft more medially.
Greater and lesser tubercles
The greater and lesser tubercles are prominent landmarks on the proximal end of the humerus and serve as attachment sites for the four rotator cuff muscles of the glenohumeral joint.
The greater tubercle is lateral in position. Its superior surface and posterior surface are marked by three large smooth facets for muscle tendon attachment:
The lesser tubercle is anterior in position and its surface is marked by a large smooth impression for attachment of the subscapularis muscle.
A deep intertubercular sulcus (bicipital groove) separates the lesser and greater tubercles and continues inferiorly onto the proximal shaft of the humerus (Fig. 7.22). The tendon of the long head of the biceps brachii passes through this sulcus.
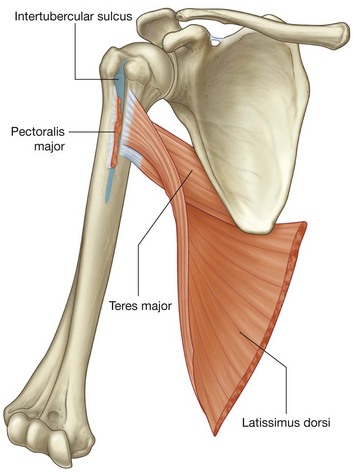
Roughenings on the lateral and medial lips and on the floor of the intertubercular sulcus mark sites for the attachment of the pectoralis major, teres major, and latissimus dorsi muscles, respectively.
The lateral lip of the intertubercular sulcus is continuous inferiorly with a large V-shaped deltoid tuberosity on the lateral surface of the humerus midway along its length (Fig. 7.22), which is where the deltoid muscle inserts onto the humerus.
In approximately the same position, but on the medial surface of the bone, there is a thin vertical roughening for attachment of the coracobrachialis muscle.
Surgical neck
One of the most important features of the proximal end of the humerus is the surgical neck (Fig. 7.22). This region is oriented in the horizontal plane between the expanded proximal part of the humerus (head, anatomical neck, and tubercles) and the narrower shaft. The axillary nerve and the posterior circumflex humeral artery, which pass into the deltoid region from the axilla, do so immediately posterior to the surgical neck. Because the surgical neck is weaker than more proximal regions of the bone, it is one of the sites where the humerus commonly fractures. The associated nerve (axillary) and artery (posterior circumflex humeral) can be damaged by fractures in this region.
In the clinic
Fracture of the proximal humerus
It is extremely rare for fractures to occur across the anatomical neck of the humerus because the obliquity of such a fracture would have to traverse the thickest region of bone. Typically fractures occur around the surgical neck of the humerus. Although the axillary nerve and posterior circumflex humeral artery may be damaged with this type of fracture, this rarely happens. It is important that the axillary nerve is tested before relocation to be sure that the injury has not damaged the nerve and that the treatment itself does not cause a neurological deficit.
Joints
The three joints in the shoulder complex are the sternoclavicular, acromioclavicular, and glenohumeral joints.
The sternoclavicular joint and the acromioclavicular joint link the two bones of the pectoral girdle to each other and to the trunk. The combined movements at these two joints enable the scapula to be positioned over a wide range on the thoracic wall, substantially increasing “reach” by the upper limb.
The glenohumeral joint (shoulder joint) is the articulation between the humerus of the arm and the scapula.
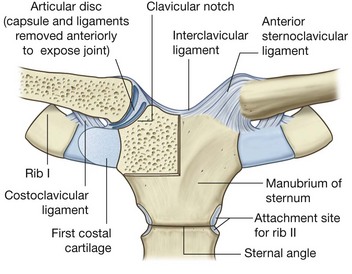
Sternoclavicular joint
The sternoclavicular joint occurs between the proximal end of the clavicle and the clavicular notch of the manubrium of sternum together with a small part of the first costal cartilage (Fig. 7.23). It is synovial and saddle-shaped. The articular cavity is completely separated into two compartments by an articular disc. The sternoclavicular joint allows movement of the clavicle, predominantly in the anteroposterior and vertical planes, although some rotation also occurs.
The sternoclavicular joint is surrounded by a joint capsule and is reinforced by four ligaments:
 the anterior and posterior sternoclavicular ligaments are anterior and posterior, respectively, to the joint;
the anterior and posterior sternoclavicular ligaments are anterior and posterior, respectively, to the joint;Acromioclavicular joint
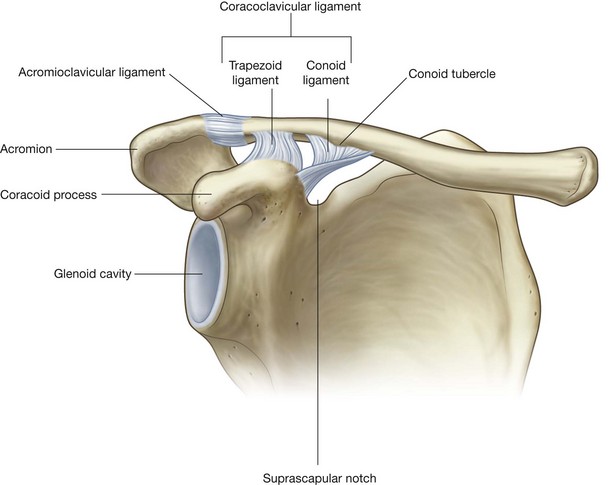
The acromioclavicular joint is a small synovial joint between an oval facet on the medial surface of the acromion and a similar facet on the acromial end of the clavicle (Fig. 7.24). It allows movement in the anteroposterior and vertical planes together with some axial rotation.
The acromioclavicular joint is surrounded by a joint capsule and is reinforced by:
 a small acromioclavicular ligament superior to the joint and passing between adjacent regions of the clavicle and acromion; and
a small acromioclavicular ligament superior to the joint and passing between adjacent regions of the clavicle and acromion; and a much larger coracoclavicular ligament, which is not directly related to the joint, but is an important strong accessory ligament, providing much of the weightbearing support for the upper limb on the clavicle and maintaining the position of the clavicle on the acromion—it spans the distance between the coracoid process of the scapula and the inferior surface of the acromial end of the clavicle and comprises an anterior trapezoid ligament (which attaches to the trapezoid line on the clavicle) and a posterior conoid ligament (which attaches to the related conoid tubercle).
a much larger coracoclavicular ligament, which is not directly related to the joint, but is an important strong accessory ligament, providing much of the weightbearing support for the upper limb on the clavicle and maintaining the position of the clavicle on the acromion—it spans the distance between the coracoid process of the scapula and the inferior surface of the acromial end of the clavicle and comprises an anterior trapezoid ligament (which attaches to the trapezoid line on the clavicle) and a posterior conoid ligament (which attaches to the related conoid tubercle).Glenohumeral joint
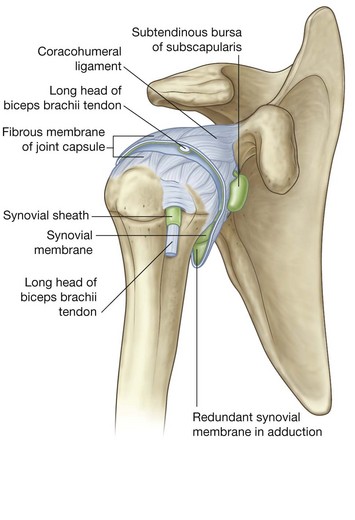
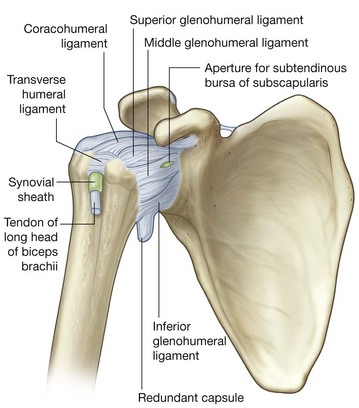
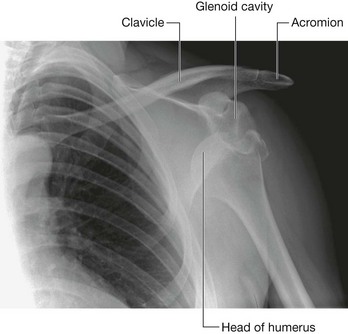
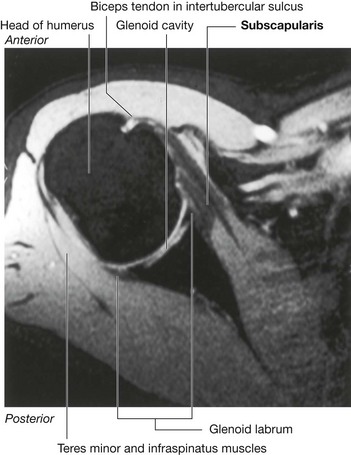
The glenohumeral joint is a synovial ball and socket articulation between the head of the humerus and the glenoid cavity of the scapula (Fig. 7.25). It is multi-axial with a wide range of movements provided at the cost of skeletal stability. Joint stability is provided, instead, by the rotator cuff muscles, the long head of the biceps brachii muscle, related bony processes, and extracapsular ligaments. Movements at the joint include flexion, extension, abduction, adduction, medial rotation, lateral rotation, and circumduction.
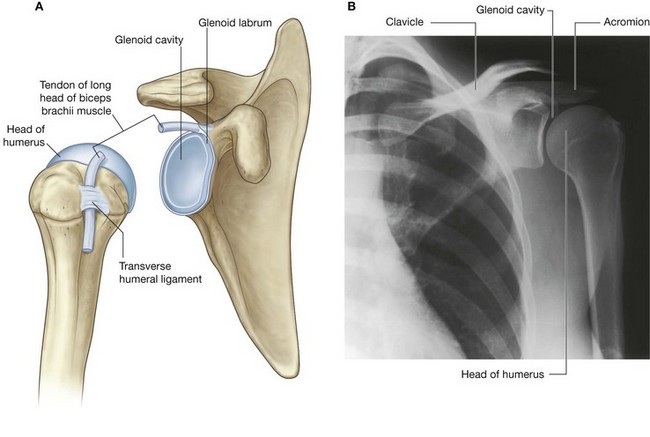
Fig. 7.25 Glenohumeral joint. A. Articular surfaces of right glenohumeral joint. B. Radiograph of a normal glenohumeral joint.
The articular surfaces of the glenohumeral joint are the large spherical head of the humerus and the small glenoid cavity of the scapula (Fig. 7.25). Each of the surfaces is covered by hyaline cartilage.
The glenoid cavity is deepened and expanded peripherally by a fibrocartilaginous collar (the glenoid labrum), which attaches to the margin of the fossa. Superiorly, this labrum is continuous with the tendon of the long head of the biceps brachii muscle, which attaches to the supraglenoid tubercle and passes through the articular cavity superior to the head of the humerus.
The synovial membrane attaches to the margins of the articular surfaces and lines the fibrous membrane of the joint capsule (Fig. 7.26). The synovial membrane is loose inferiorly. This redundant region of synovial membrane and related fibrous membrane accommodates abduction of the arm.
The synovial membrane protrudes through apertures in the fibrous membrane to form bursae, which lie between the tendons of surrounding muscles and the fibrous membrane. The most consistent of these is the subtendinous bursa of subscapularis, which lies between the subscapularis muscle and the fibrous membrane. The synovial membrane also folds around the tendon of the long head of the biceps brachii muscle in the joint and extends along the tendon as it passes into the intertubercular sulcus. All these synovial structures reduce friction between the tendons and adjacent joint capsule and bone.
In addition to bursae that communicate with the articular cavity through apertures in the fibrous membrane, other bursae are associated with the joint but are not connected to it. These occur:
 between the acromion (or deltoid muscle) and supraspinatus muscle (or joint capsule) (the subacromial or subdeltoid bursa);
between the acromion (or deltoid muscle) and supraspinatus muscle (or joint capsule) (the subacromial or subdeltoid bursa); in relationship to tendons of muscles around the joint (coracobrachialis, teres major, long head of triceps brachii, and latissimus dorsi muscles).
in relationship to tendons of muscles around the joint (coracobrachialis, teres major, long head of triceps brachii, and latissimus dorsi muscles).The fibrous membrane of the joint capsule attaches to the margin of the glenoid cavity, outside the attachment of the glenoid labrum and the long head of the biceps brachii muscle, and to the anatomical neck of the humerus (Fig. 7.27).
On the humerus, the medial attachment occurs more inferiorly than the neck and extends onto the shaft. In this region, the fibrous membrane is also loose or folded in the anatomical position. This redundant area of the fibrous membrane accommodates abduction of the arm.
Openings in the fibrous membrane provide continuity of the articular cavity with bursae that occur between the joint capsule and surrounding muscles and around the tendon of the long head of the biceps brachii muscle in the intertubercular sulcus.
The fibrous membrane of the joint capsule is thickened:
 anterosuperiorly in three locations to form superior, middle, and inferior glenohumeral ligaments, which pass from the superomedial margin of the glenoid cavity to the lesser tubercle and inferiorly related anatomical neck of the humerus (Fig. 7.27);
anterosuperiorly in three locations to form superior, middle, and inferior glenohumeral ligaments, which pass from the superomedial margin of the glenoid cavity to the lesser tubercle and inferiorly related anatomical neck of the humerus (Fig. 7.27); superiorly between the base of the coracoid process and the greater tubercle of the humerus (the coracohumeral ligament);
superiorly between the base of the coracoid process and the greater tubercle of the humerus (the coracohumeral ligament); between the greater and lesser tubercles of the humerus (transverse humeral ligament)—this holds the tendon of the long head of the biceps brachii muscle in the intertubercular sulcus (Fig. 7.27).
between the greater and lesser tubercles of the humerus (transverse humeral ligament)—this holds the tendon of the long head of the biceps brachii muscle in the intertubercular sulcus (Fig. 7.27).Joint stability is provided by surrounding muscle tendons and a skeletal arch formed superiorly by the coracoid process and acromion and the coraco-acromial ligament (Fig. 7.28).
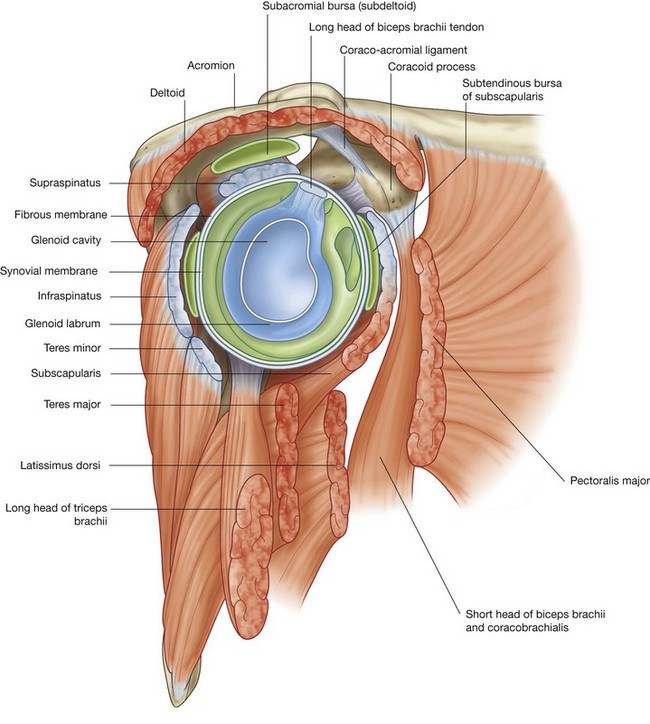
Fig. 7.28 Lateral view of right glenohumeral joint and surrounding muscles with proximal end of humerus removed.
Tendons of the rotator cuff muscles (the supraspinatus, infraspinatus, teres minor, and subscapularis muscles) blend with the joint capsule and form a musculotendinous collar that surrounds the posterior, superior, and anterior aspects of the glenohumeral joint (Figs. 7.28 and 7.29). This cuff of muscles stabilizes and holds the head of the humerus in the glenoid cavity of the scapula without compromising the arm’s flexibility and range of motion. The tendon of the long head of the biceps brachii muscle passes superiorly through the joint and restricts upward movement of the humeral head on the glenoid cavity.
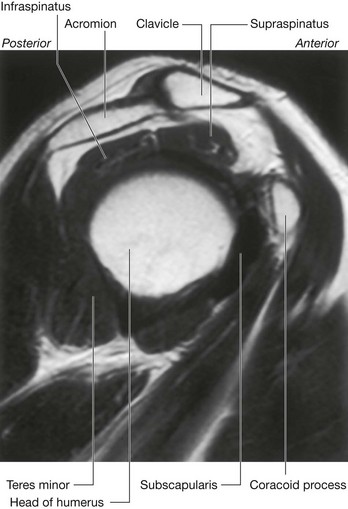
Fig. 7.29 Magnetic resonance image (T1-weighted) of a normal glenohumeral joint in the sagittal plane. Ant, anterior; Post., posterior.
Vascular supply to the glenohumeral joint is predominantly through branches of the anterior and posterior circumflex humeral and suprascapular arteries.
The glenohumeral joint is innervated by branches from the posterior cord of the brachial plexus, and from the suprascapular, axillary, and lateral pectoral nerves.
In the clinic
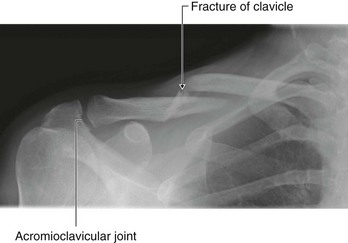
Fractures of the clavicle and dislocations of the acromioclavicular and sternoclavicular joints
The clavicle provides osseous continuity between the upper limb and thorax. Given its relative size and the potential forces that it transmits from the upper limb to the trunk, it is not surprising that it is often fractured. The typical site of fracture is the middle third (Fig. 7.30). The medial and lateral thirds are rarely fractured.
The acromial end of the clavicle tends to dislocate at the acromioclavicular joint with trauma (Fig. 7.31). The outer third of the clavicle is joined to the scapula by the conoid and trapezoid ligaments of the coracoclavicular ligament.

Fig. 7.31 Radiographs of acromioclavicular joints. A. Normal left acromioclavicular joint. B. Dislocated right acromioclavicular joint.
A minor injury tends to tear the fibrous joint capsule and ligaments of the acromioclavicular joint, resulting in acromioclavicular separation on a plain radiograph. More severe trauma will disrupt the conoid and trapezoid ligaments of the coracoclavicular ligament, which results in elevation and upward subluxation of the clavicle.
The typical injury at the medial end of the clavicle is an anterior or posterior dislocation of the sternoclavicular joint. Importantly, a posterior dislocation of the clavicle may impinge on the great vessels of the superior mediastinum and compress or disrupt them.
In the clinic
Dislocations of the glenohumeral joint
The glenohumeral joint is extremely mobile, providing a wide range of movement at the expense of stability. The relatively small bony glenoid cavity, supplemented by the less robust fibrocartilaginous glenoid labrum and the ligamentous support, make it susceptible to dislocation.
Anterior dislocation (Fig. 7.32) occurs most frequently and is usually associated with an isolated traumatic incident (clinically, all anterior dislocations are anteroinferior). In some cases, the anterior inferior glenoid labrum is torn with or without a small bony fragment. Once the joint capsule and cartilage are disrupted, the joint is susceptible to further (recurrent) dislocations. When an anteroinferior dislocation occurs, the axillary nerve may be injured by direct compression of the humeral head on the nerve inferiorly as it passes through the quadrangular space. Furthermore, the “lengthening” effect of the humerus may stretch the radial nerve, which is tightly bound within the radial groove, and produce a radial nerve paralysis. Occasionally, an anteroinferior dislocation is associated with a fracture, which may require surgical reduction.
Posterior dislocation is extremely rare; when seen, the clinician should focus on its cause, the most common being extremely vigorous muscle contractions, which may be associated with an epileptic seizure caused by electrocution.
In the clinic
Rotator cuff disorders
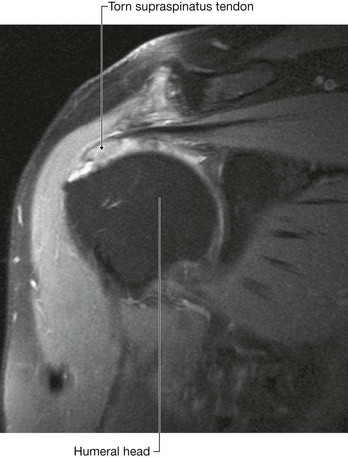
The two main disorders of the rotator cuff are impingement and tendinopathy. The muscle most commonly involved is supraspinatus as it passes beneath the acromion and the acromioclavicular ligament. This space, beneath which the supraspinatus tendon passes, is of fixed dimensions. Swelling of the supraspinatus muscle, excessive fluid within the subacromial/subdeltoid bursa, or subacromial bony spurs may produce significant impingement when the arm is abducted.
The blood supply to the supraspinatus tendon is relatively poor. Repeated trauma, in certain circumstances, makes the tendon susceptible to degenerative change, which may result in calcium deposition, producing extreme pain.
When the supraspinatus tendon has undergone significant degenerative change, it is further susceptible to trauma and partial- or full-thickness tears may develop (Fig. 7.33). These tears are most common in older patients and may result in considerable difficulty in carrying out normal activities of daily living such as combing hair. However, complete tears may be entirely unsymptomatic.
In the clinic
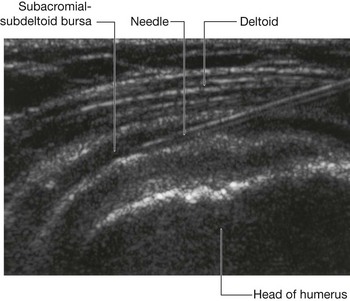
Inflammation of the subacromial (subdeltoid) bursa
Between the supraspinatus and deltoid muscles laterally and the acromion medially, there is a bursa referred to clinically as the subacromial or subdeltoid bursa. In patients who have injured their shoulder or who have supraspinatus tendinopathy, this bursa may become inflamed, making movements of the glenohumeral joint painful. These inflammatory changes may be treated by injection of a corticosteroid and local anesthetic agent (Fig. 7.34).
Muscles
The two most superficial muscles of the shoulder are the trapezius and deltoid muscles (Fig. 7.35 and Table 7.1). Together, they provide the characteristic contour of the shoulder:
Both the trapezius and deltoid are attached to opposing surfaces and margins of the spine of the scapula, acromion, and clavicle.
The scapula, acromion, and clavicle can be palpated between the attachments of trapezius and deltoid.
Deep to the trapezius the scapula is attached to the vertebral column by three muscles—the levator scapulae, rhomboid minor and rhomboid major. These three muscles work with the trapezius (and with muscles found anteriorly) to position the scapula on the trunk.
Trapezius
The trapezius muscle has an extensive origin from the axial skeleton, which includes sites on the skull and the vertebrae, from CI to TXII (Fig. 7.36). From CI to CVII, the muscle attaches to the vertebrae through the ligamentum nuchae. The muscle inserts onto the skeletal framework of the shoulder along the inner margins of a continuous U-shaped line of attachment oriented in the horizontal plane, with the bottom of the U directed laterally. Together, the left and right trapezius muscles form a diamond or trapezoid shape, from which the name is derived.
The trapezius muscle is a powerful elevator of the shoulder and also rotates the scapula to extend the reach superiorly.
Innervation of the trapezius muscle is by the accessory nerve [XI] and the anterior rami of cervical nerves C3 and C4 (Fig. 7.36). These nerves pass vertically along the deep surface of the muscle.
Deltoid
The deltoid muscle is large and triangular in shape, with its base attached to the scapula and clavicle and its apex attached to the humerus (Fig. 7.36). It originates along a continuous U-shaped line of attachment to the clavicle and the scapula, mirroring the adjacent insertion sites of the trapezius muscle. It inserts into the deltoid tuberosity on the lateral surface of the shaft of the humerus.
The major function of the deltoid muscle is abduction of the arm beyond the initial 15° accomplished by the supraspinatus muscle.
The deltoid muscle is innervated by the axillary nerve, which is a branch of the posterior cord of the brachial plexus. The axillary nerve and associated blood vessels (the posterior circumflex humeral artery and vein) enter the deltoid by passing posteriorly around the surgical neck of the humerus.
Levator scapulae
The levator scapulae originates from the transverse processes of CI to CIV vertebrae (Fig. 7.36). It descends laterally to attach to the posterior surface of the medial border of the scapula from the superior angle to the smooth triangular area of bone at the root of the spine.
The levator scapulae muscle is innervated by the dorsal scapular nerve and directly from C3 and C4 spinal nerves.
Rhomboid minor and major
The rhomboid minor and major muscles attach medially to the vertebral column and descend laterally to attach to the medial border of the scapula inferior to the levator scapulae muscle (Fig. 7.36).
The rhomboid minor originates from the lower end of the ligamentum nuchae and the spines of CVII and TI vertebrae. It inserts laterally into the smooth triangular area of bone at the root of the spine of the scapula on the posterior surface.
The rhomboid major originates from the spines of vertebrae TII to TV and from the intervening supraspinous ligaments. It descends laterally to insert along the posterior surface of the medial border of the scapula from the insertion of the rhomboid minor to the inferior angle.
The rhomboid muscles are innervated by the dorsal scapular nerve, which is a branch of the brachial plexus.
The rhomboid minor and major retract and elevate the scapula.
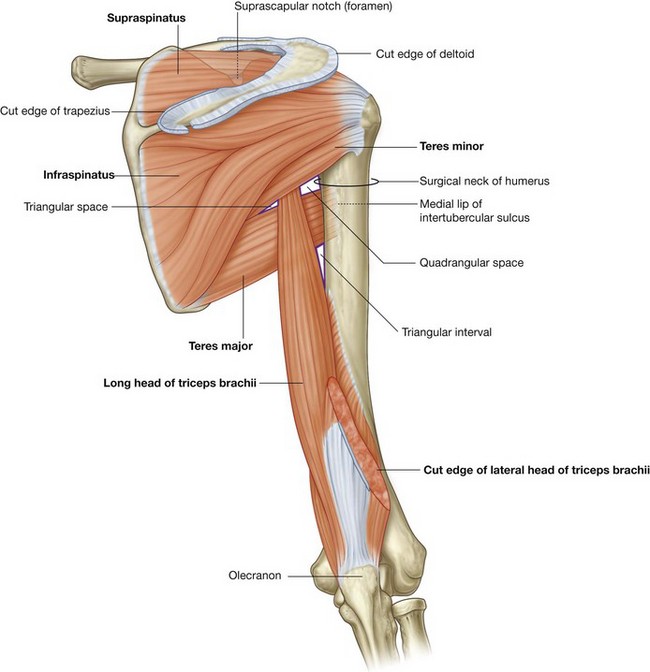
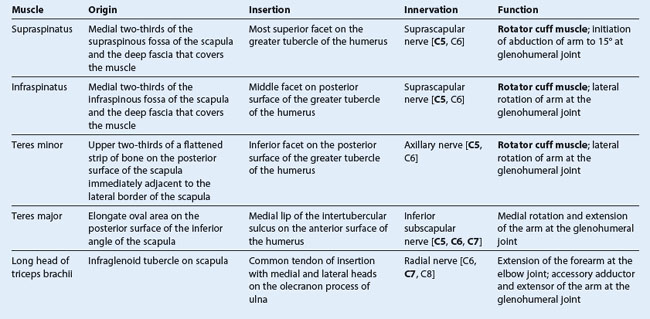
POSTERIOR SCAPULAR REGION
The posterior scapular region occupies the posterior aspect of the scapula and is located deep to the trapezius and deltoid muscles (Fig. 7.37 and Table 7.2). It contains four muscles, which pass between the scapula and proximal end of the humerus: the supraspinatus, infraspinatus, teres minor, and teres major muscles.
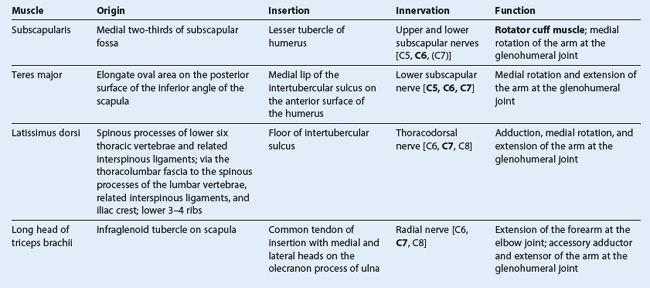
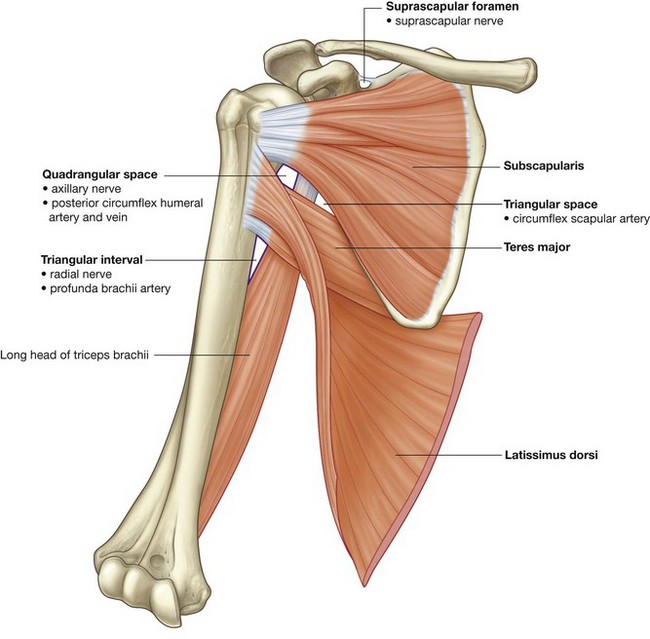
Table 7.2 Muscles of the posterior scapular region (spinal segments in bold are the major segments innervating the muscle)
The posterior scapular region also contains part of one additional muscle, the long head of the triceps brachii, which passes between the scapula and the proximal end of the forearm. This muscle, along with other muscles of the region and the humerus, participates in forming a number of spaces through which nerves and vessels enter and leave the region.
The supraspinatus, infraspinatus, and teres minor muscles are components of the rotator cuff, which stabilizes the glenohumeral joint.
Muscles
Supraspinatus and infraspinatus
The supraspinatus and infraspinatus muscles originate from two large fossae, one above and one below the spine, on the posterior surface of the scapula (Fig. 7.37). They form tendons that insert on the greater tubercle of the humerus.
 The tendon of the supraspinatus passes under the acromion, where it is separated from the bone by a subacromial bursa, passes over the glenohumeral joint, and inserts on the superior facet of the greater tubercle.
The tendon of the supraspinatus passes under the acromion, where it is separated from the bone by a subacromial bursa, passes over the glenohumeral joint, and inserts on the superior facet of the greater tubercle. The tendon of the infraspinatus passes posteriorly to the glenohumeral joint and inserts on the middle facet of the greater tubercle.
The tendon of the infraspinatus passes posteriorly to the glenohumeral joint and inserts on the middle facet of the greater tubercle.The supraspinatus initiates abduction of the arm. The infraspinatus laterally rotates the humerus.
Teres minor and teres major
The teres minor muscle is a cord-like muscle that originates from a flattened area of the scapula immediately adjacent to its lateral border below the infraglenoid tubercle (Fig. 7.37). Its tendon inserts on the inferior facet of the greater tubercle of the humerus. The teres minor laterally rotates the humerus and is a component of the rotator cuff.
The teres major muscle originates from a large oval region on the posterior surface of the inferior angle of the scapula (Fig. 7.37). This broad cord-like muscle passes superiorly and laterally and ends as a flat tendon that attaches to the medial lip of the intertubercular sulcus on the anterior surface of the humerus. The teres major medially rotates and extends the humerus.
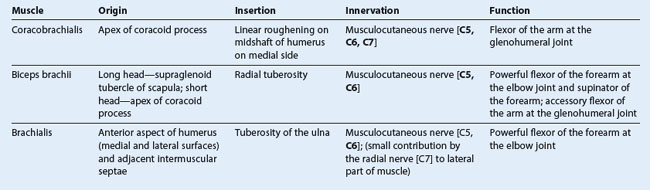
Long head of triceps brachii
The long head of triceps brachii muscle originates from the infraglenoid tubercle and passes somewhat vertically down the arm to insert, with the medial and lateral heads of this muscle, on the olecranon of the ulna (Fig. 7.37).
The triceps brachii is the primary extensor of the forearm at the elbow joint. Because the long head crosses the glenohumeral joint, it can also extend and adduct the humerus.
The importance of the triceps brachii in the posterior scapular region is that its vertical course between the teres minor and teres major, together with these muscles and the humerus, forms spaces through which nerves and vessels pass between regions.
Gateways to the posterior scapular region
Suprascapular foramen
The suprascapular foramen is the route through which structures pass between the base of the neck and the posterior scapular region (Fig. 7.37). It is formed by the suprascapular notch of the scapula and the superior transverse scapular (suprascapular) ligament, which converts the notch into a foramen.
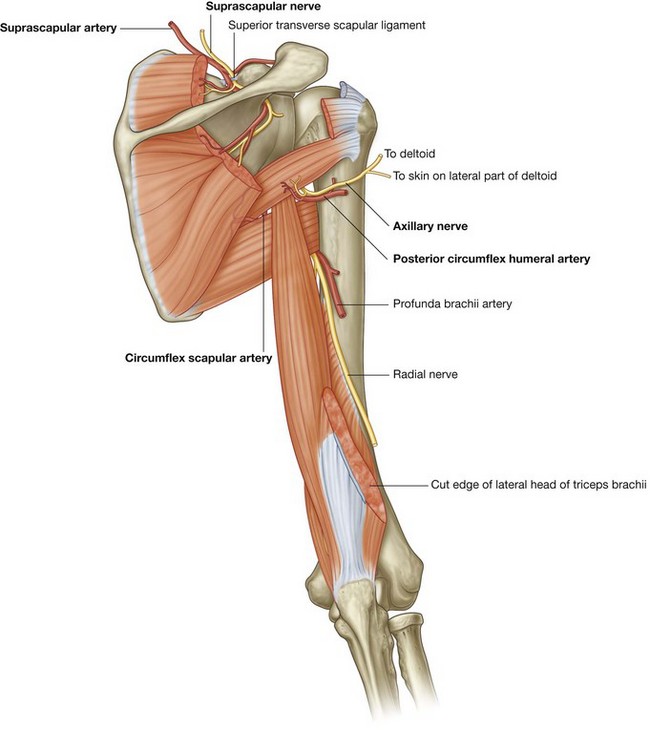
The suprascapular nerve passes through the suprascapular foramen; the suprascapular artery and the suprascapular vein follow the same course as the nerve, but normally pass immediately superior to the superior transverse scapular ligament and not through the foramen (Fig. 7.38).
Quadrangular space (from posterior)
The quadrangular space provides a passageway for nerves and vessels passing between more anterior regions (the axilla) and the posterior scapular region (Fig. 7.37). In the posterior scapular region, its boundaries are formed by:
The axillary nerve and the posterior circumflex humeral artery and vein pass through this space (Fig. 7.38).
In the clinic
Quadrangular space syndrome
Hypertrophy of the quadrangular space muscles or fibrosis of the muscle edges may impinge on the axillary nerve. Uncommonly, this produces weakness of the deltoid muscle. Typically it produces atrophy of the teres minor muscle, which may affect the control that the rotator cuff muscles exert upon shoulder movement.
Triangular space
The triangular space is an area of communication between the axilla and the posterior scapular region (Fig. 7.37). When viewed from the posterior scapular region, the triangular space is formed by:
The circumflex scapular artery and vein pass through this gap (Fig. 7.38).
Triangular interval
The triangular interval is formed by:
Because this space is below the inferior margin of the teres major, which defines the inferior boundary of the axilla, the triangular interval serves as a passageway between the anterior and posterior compartments of the arm and between the posterior compartment of the arm and the axilla. The radial nerve, the profunda brachii artery (deep artery of arm), and associated veins pass through it (Fig. 7.38).
Nerves
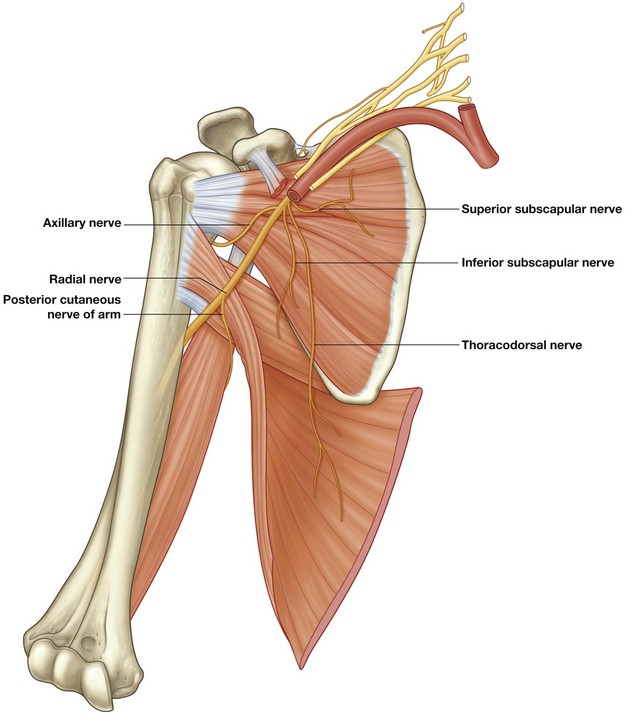
The two major nerves of the posterior scapular region are the suprascapular and axillary nerves, both of which originate from the brachial plexus in the axilla (Fig. 7.38).
Suprascapular nerve
The suprascapular nerve originates in the base of the neck from the superior trunk of the brachial plexus. It passes posterolaterally from its origin, through the suprascapular foramen to reach the posterior scapular region, where it lies in the plane between bone and muscle (Fig. 7.38).
It innervates the supraspinatus muscle, then passes through the greater scapular (spinoglenoid) notch, between the root of the spine of the scapula and the glenoid cavity, to terminate in and innervate the infraspinatus muscle.
Generally, the suprascapular nerve has no cutaneous branches.
Axillary nerve
The axillary nerve originates from the posterior cord of the brachial plexus. It exits the axilla by passing through the quadrangular space in the posterior wall of the axilla, and enters the posterior scapular region (Fig. 7.38). Together with the posterior circumflex humeral artery and vein, it is directly related to the posterior surface of the surgical neck of the humerus.
The axillary nerve innervates the deltoid and teres minor muscles. In addition, it has a cutaneous branch, the superior lateral cutaneous nerve of the arm, which carries general sensation from the skin over the inferior part of the deltoid muscle.
Arteries and veins
Three major arteries are found in the posterior scapular region: the suprascapular, posterior circumflex humeral, and circumflex scapular arteries. These arteries contribute to an interconnected vascular network around the scapula (Fig. 7.39).
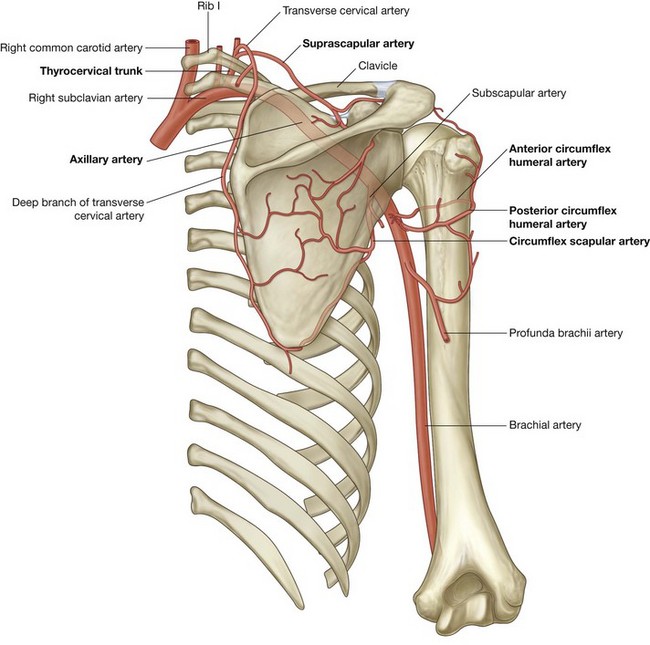
Suprascapular artery
The suprascapular artery originates in the base of the neck as a branch of the thyrocervical trunk, which in turn, is a major branch of the subclavian artery (Figs. 7.38 and 7.39). The vessel may also originate directly from the third part of the subclavian artery.
The suprascapular artery normally enters the posterior scapular region superior to the suprascapular foramen, whereas the nerve passes through the foramen. In the posterior scapular region, the vessel runs with the suprascapular nerve.
In addition to supplying the supraspinatus and infraspinatus muscles, the suprascapular artery contributes branches to numerous structures along its course.
Posterior circumflex humeral artery
The posterior circumflex humeral artery originates from the third part of the axillary artery in the axilla (Fig. 7.39).
The posterior circumflex humeral artery and axillary nerve leave the axilla through the quadrangular space in the posterior wall and enter the posterior scapular region. The vessel supplies the related muscles and the glenohumeral joint.
Circumflex scapular artery
The circumflex scapular artery is a branch of the subscapular artery that also originates from the third part of the axillary artery in the axilla (Fig. 7.39). The circumflex scapular artery leaves the axilla through the triangular space and enters the posterior scapular region, passes through the origin of the teres minor muscle and forms anastomotic connections with other arteries in the region.
AXILLA
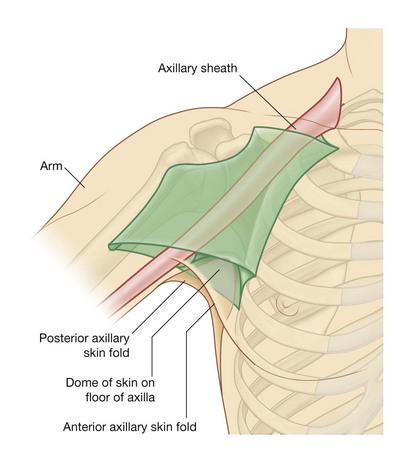
The axilla is the gateway to the upper limb, providing an area of transition between the neck and the arm (Fig. 7.40A). Formed by the clavicle, the scapula, the upper thoracic wall, the humerus, and related muscles, the axilla is an irregularly shaped pyramidal space with:
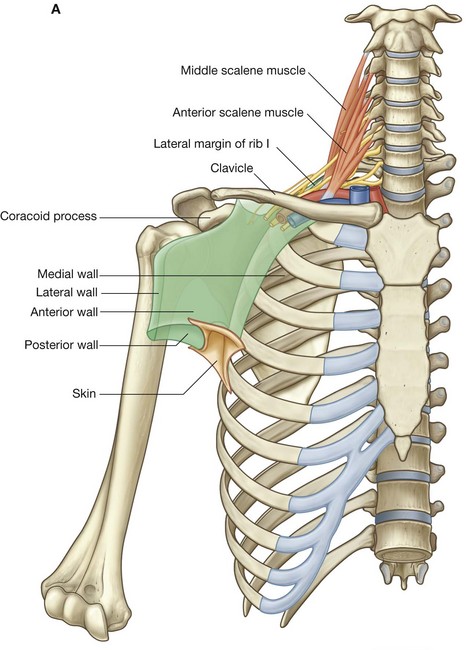
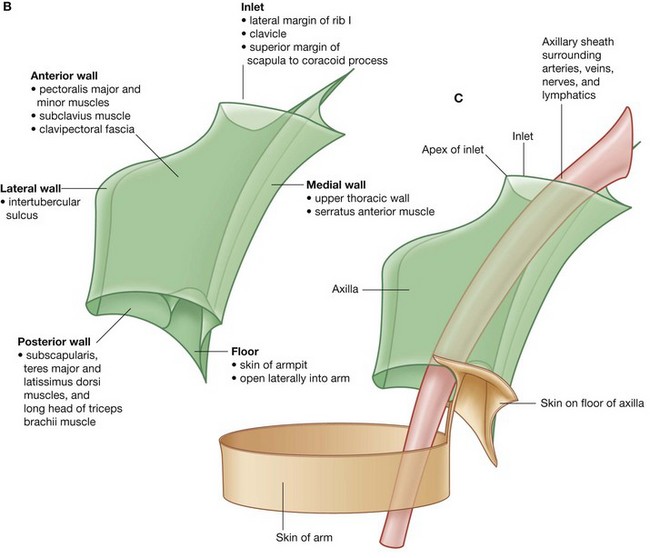
Fig. 7.40 Axilla. A. Walls and transition between neck and arm. B. Boundaries. C. Continuity with the arm.
The axillary inlet is continuous superiorly with the neck, and the lateral part of the floor opens into the arm.
All major structures passing into and out of the upper limb pass through the axilla (Fig. 7.40C). Apertures formed between muscles in the anterior and posterior walls enable structures to pass between the axilla and immediately adjacent regions (the posterior scapular, pectoral, and deltoid regions).
Axillary inlet
The axillary inlet is oriented in the horizontal plane and is somewhat triangular in shape, with its apex directed laterally (Fig. 7.40A and 7.40B). The margins of the inlet are completely formed by bone:
The apex of the triangularly shaped axillary inlet is lateral in position and is formed by the medial aspect of the coracoid process.
Major vessels and nerves pass between the neck and the axilla by crossing over the lateral border of rib I and through the axillary inlet (Fig. 7.40A).
The subclavian artery, the major blood vessel supplying the upper limb, becomes the axillary artery as it crosses the lateral margin of rib I and enters the axilla. Similarly, the axillary vein becomes the subclavian vein as it passes over the lateral margin of rib I and leaves the axilla to enter the neck.
At the axillary inlet, the axillary vein is anterior to the axillary artery, which, in turn, is anterior to the trunks of the brachial plexus.
The inferior trunk (lower trunk) of the brachial plexus lies directly on rib I in the neck, as does the subclavian artery and vein. As they pass over rib I, the vein and artery are separated by the insertion of the anterior scalene muscle (Fig. 7.40A).
Anterior wall
The anterior wall of the axilla is formed by the lateral part of the pectoralis major muscle, the underlying pectoralis minor and subclavius muscles, and the clavipectoral fascia (Table 7.3).
Table 7.3 Muscles of the anterior wall of the axilla (spinal segments in bold are the major segments innervating the muscle)
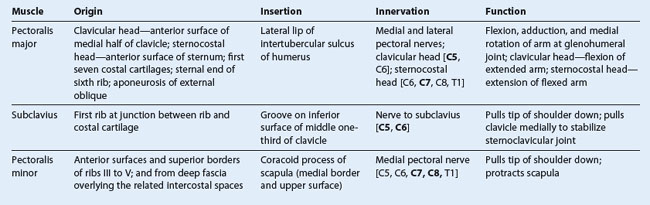
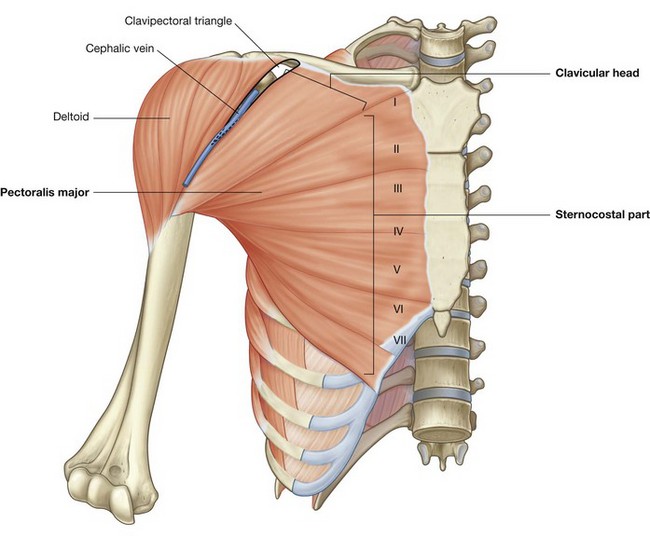
Pectoralis major
The pectoralis major muscle is the largest and most superficial muscle of the anterior wall (Fig. 7.41). Its inferior margin underlies the anterior axillary fold, which marks the anteroinferior border of the axilla. The muscle has two heads:
 the sternocostal head originates from the medial part of the anterior thoracic wall—often fibers from this head continue inferiorly and medially to attach to the anterior abdominal wall, forming an additional abdominal part of the muscle.
the sternocostal head originates from the medial part of the anterior thoracic wall—often fibers from this head continue inferiorly and medially to attach to the anterior abdominal wall, forming an additional abdominal part of the muscle.The muscle inserts into the lateral lip of the intertubercular sulcus of the humerus. The parts of the muscle that have a superior origin on the trunk insert lower and more anteriorly on the lateral lip of the intertubercular sulcus than the parts of the muscle that originate inferiorly.
Acting together, the two heads of the pectoralis major flex, adduct, and medially rotate the arm at the glenohumeral joint. The clavicular head flexes the arm from an extended position, whereas the sternocostal head extends the arm from a flexed position, particularly against resistance.
The pectoralis major is innervated by the lateral and medial pectoral nerves, which originate from the brachial plexus in the axilla.
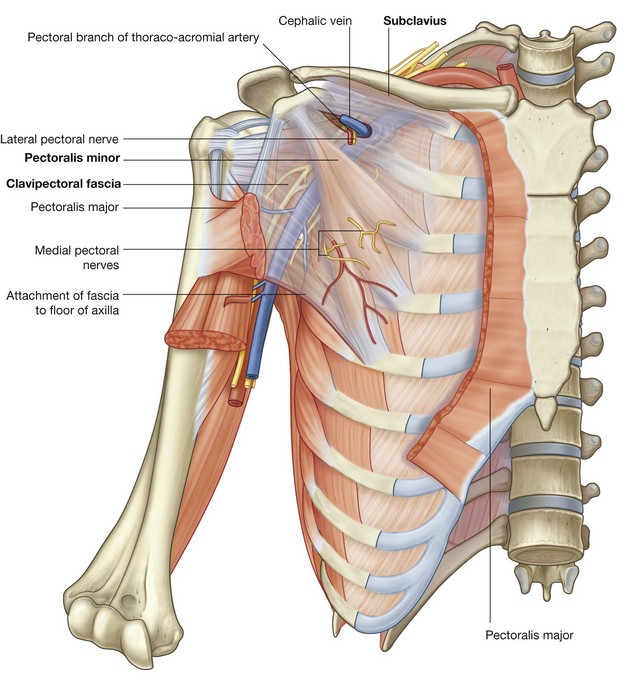
Subclavius
The subclavius muscle is a small muscle that lies deep to the pectoralis major muscle and passes between the clavicle and rib I (Fig. 7.42). It originates medially, as a tendon, from rib I at the junction between the rib and its costal cartilage. It passes laterally and superiorly to insert via a muscular attachment into an elongate shallow groove on the inferior surface of the middle third of the clavicle.
The function of the subclavius is not entirely clear, but it may act to pull the shoulder down by depressing the clavicle and may also stabilize the sternoclavicular joint by pulling the clavicle medially.
The subclavius muscle is innervated by a small branch from the superior trunk of the brachial plexus.
Pectoralis minor
The pectoralis minor muscle is a small triangular-shaped muscle that lies deep to the pectoralis major muscle and passes from the thoracic wall to the coracoid process of the scapula (Fig. 7.42). It originates as three muscular slips from the anterior surfaces and upper margins of ribs III to V and from the fascia overlying muscles of the related intercostal spaces. The muscle fibers pass superiorly and laterally to insert into the medial and upper aspects of the coracoid process.
The pectoralis minor muscle protracts the scapula (by pulling the scapula anteriorly on the thoracic wall) and depresses the lateral angle of the scapula.
The pectoralis minor is innervated by the medial pectoral nerve, which originates from the brachial plexus in the axilla.
Clavipectoral fascia
The clavipectoral fascia is a thick sheet of connective tissue that connects the clavicle to the floor of the axilla (Fig. 7.42). It encloses the subclavius and pectoralis minor muscles and spans the gap between them.
Structures travel between the axilla and the anterior wall of the axilla by passing through the clavipectoral fascia either between the pectoralis minor and subclavius muscles or inferior to the pectoralis minor muscle.
Important structures that pass between the subclavius and pectoralis minor muscles include the cephalic vein, the thoraco-acromial artery, and the lateral pectoral nerve.
The lateral thoracic artery leaves the axilla by passing through the fascia inferior to the pectoralis minor muscle.
The medial pectoral nerve leaves the axilla by penetrating directly through the pectoralis minor muscle to supply this muscle and to reach the pectoralis major muscle. Occasionally, branches of the medial pectoral nerve pass around the lower margin of the pectoralis minor to reach and innervate the overlying pectoralis major muscle.
Medial wall
The medial wall of the axilla consists of the upper thoracic wall (the ribs and related intercostal tissues) and the serratus anterior muscle (Fig. 7.43 and Table 7.4, and see Fig. 7.40).
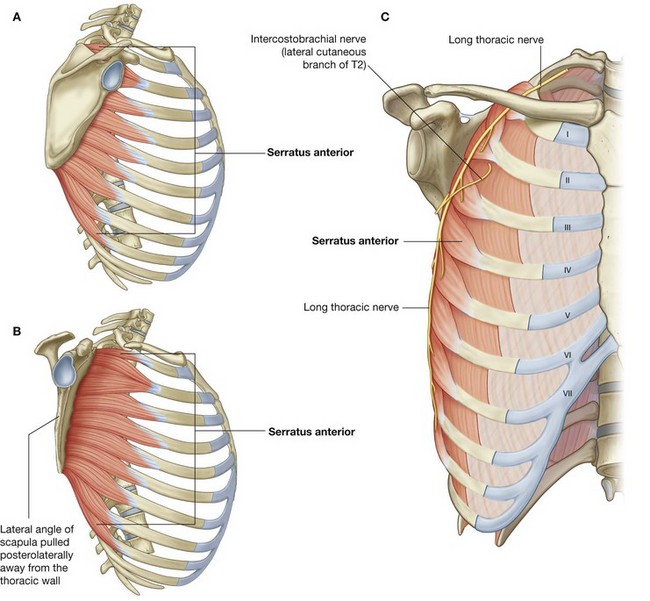
Fig. 7.43 Medial wall of the axilla. A. Lateral view. B. Lateral view with lateral angle of scapula retracted posteriorly. C. Anterior view.
Table 7.4 Muscles of the medial wall of the axilla (spinal segments in bold are the major segments innervating the muscle)
Serratus anterior
The serratus anterior muscle originates as a number of muscular slips from the lateral surfaces of ribs I to IX and the intervening deep fascia overlying the related intercostal spaces (Fig. 7.43). The muscle forms a flattened sheet, which passes posteriorly around the thoracic wall to insert primarily on the costal surface of the medial border of the scapula.
The serratus anterior pulls the scapula forward over the thoracic wall and facilitates scapular rotation. It also keeps the costal surface of the scapula closely opposed to the thoracic wall.
The serratus anterior is innervated by the long thoracic nerve, which is derived from the roots of the brachial plexus, passes through the axilla along the medial wall, and passes vertically down the serratus anterior muscle on its external surface, just deep to skin and superficial fascia.
Intercostobrachial nerve
The only major structure that passes directly through the medial wall and into the axilla is the intercostobrachial nerve (Fig. 7.43). This nerve is the lateral cutaneous branch of the second intercostal nerve (anterior ramus of T2). It communicates with a branch of the brachial plexus (the medial cutaneous nerve of the arm) in the axilla and supplies skin on the upper posteromedial side of the arm, which is part of the T2 dermatome.
In the clinic
Damage to the long thoracic nerve
Because the long thoracic nerve passes down the lateral thoracic wall on the external surface of the serratus anterior muscle, just deep to skin and subcutaneous fascia, it is vulnerable to damage. Loss of function of this muscle causes the medial border, and particularly the inferior angle, of the scapula to elevate away from the thoracic wall, resulting in characteristic “winging” of the scapula, on pushing forward with the arm. Furthermore, normal elevation at the arm is no longer possible.
Lateral wall
The lateral wall of the axilla is narrow and formed entirely by the intertubercular sulcus of the humerus (Fig. 7.44). The pectoralis major muscle of the anterior wall attaches to the lateral lip of the intertubercular sulcus. The latissimus dorsi and teres major muscles of the posterior wall attach to the floor and medial lip of the intertubercular sulcus, respectively (Table 7.5).
Posterior wall
The posterior wall of the axilla is complex (Fig. 7.45 and see Fig. 7.50). Its bone framework is formed by the costal surface of the scapula. Muscles of the wall are:
 the distal parts of the latissimus dorsi and teres major muscles (which pass into the wall from the back and posterior scapular region); and
the distal parts of the latissimus dorsi and teres major muscles (which pass into the wall from the back and posterior scapular region); and the proximal part of the long head of the triceps brachii muscle (which passes vertically down the wall and into the arm).
the proximal part of the long head of the triceps brachii muscle (which passes vertically down the wall and into the arm).Gaps between the muscles of the posterior wall form apertures through which structures pass between the axilla, posterior scapular region, and posterior compartment of the arm.
Subscapularis
The subscapularis muscle forms the largest component of the posterior wall of the axilla. It originates from, and fills, the subscapular fossa and inserts on the lesser tubercle of the humerus (Figs. 7.45 and 7.46). The tendon crosses immediately anterior to the joint capsule of the glenohumeral joint.
Together with three muscles of the posterior scapular region (the supraspinatus, infraspinatus, and teres minor muscles), the subscapularis is a member of the rotator cuff muscles, which stabilize the glenohumeral joint.
Subscapularis is innervated by branches of the brachial plexus (the superior and inferior subscapular nerves), which originate in the axilla.
Teres major and latissimus dorsi
The inferolateral aspect of the posterior wall of the axilla is formed by the terminal part of the teres major muscle and the tendon of the latissimus dorsi muscle (Fig. 7.45). These two structures lie under the posterior axillary fold, which marks the posteroinferior border of the axilla.
The flat tendon of the latissimus dorsi muscle curves around the inferior margin of the teres major muscle on the posterior wall to insert into the floor of the intertubercular sulcus of the humerus, anterior to and slightly above the most distal attachment of the teres major muscle to the medial lip of the intertubercular sulcus. As a consequence, the inferior margin of the teres major muscle defines the inferior limit of the axilla laterally.
The axillary artery becomes the brachial artery of the arm as it crosses the inferior margin of the teres major muscle.
Long head of the triceps brachii
The long head of the triceps brachii muscle passes vertically through the posterior wall of the axilla, and, together with surrounding muscles and adjacent bones, results in the formation of three apertures through which major structures pass through the posterior wall:
Gateways in the posterior wall
(See also “Gateways to the posterior scapular region” and Figs. 7.37 and 7.38, pp. 681–684.)
Quadrangular space
The quadrangular space provides a passageway for nerves and vessels passing between the axilla and the more posterior scapular and deltoid regions (Fig. 7.45). When viewed from anteriorly, its boundaries are formed by:
Passing through the quadrangular space are the axillary nerve and the posterior circumflex humeral artery and vein.
Triangular space
The triangular space is an area of communication between the axilla and the posterior scapular region (Fig. 7.45). When viewed from anteriorly, it is formed by:
The circumflex scapular artery and vein pass into this space.
Floor
The floor of the axilla is formed by fascia and a dome of skin that spans the distance between the inferior margins of the walls (Fig. 7.47 and see Fig. 7.40B). It is supported by the clavipectoral fascia. On a patient, the anterior axillary fold is more superior in position than is the posterior axillary fold.
Inferiorly, structures pass into and out of the axilla immediately lateral to the floor where the anterior and posterior walls of the axilla converge and where the axilla is continuous with the anterior compartment of the arm.
Contents of the axilla
Passing through the axilla are the major vessels, nerves, and lymphatics of the upper limb. The space also contains the proximal parts of two muscles of the arm, the axillary process of the breast, and collections of lymph nodes, which drain the upper limb and chest wall.
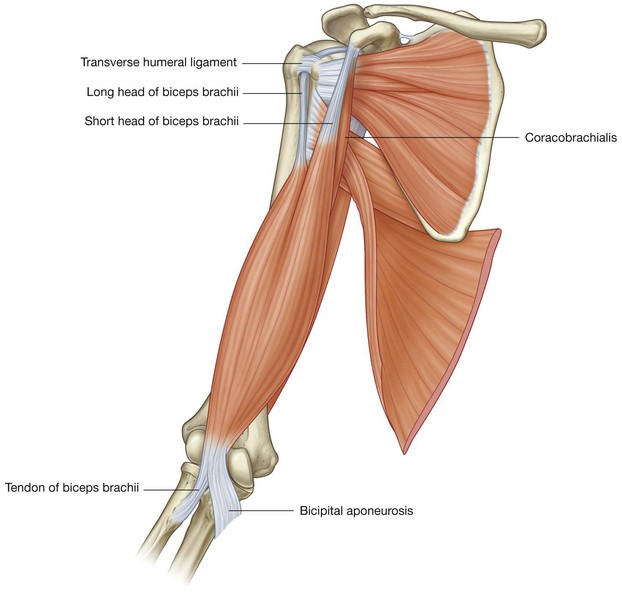
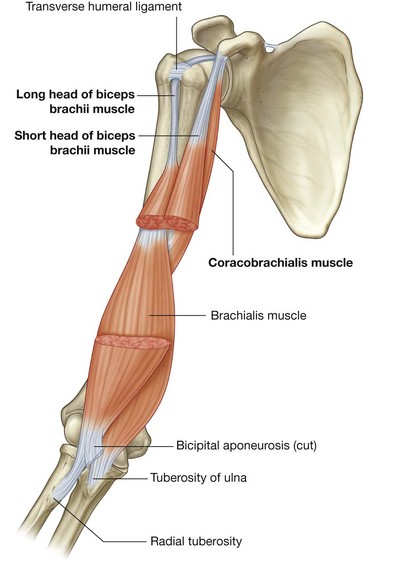
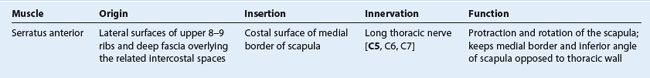
The proximal parts of the biceps brachii and coracobrachialis muscles pass through the axilla (Table 7.6).
Table 7.6 Muscles having parts that pass through the axilla (spinal segments in bold are the major segments innervating the muscle)
Biceps brachii
The biceps brachii muscle originates as two heads (Fig. 7.48):
 the short head originates from the apex of the coracoid process of the scapula and passes vertically through the axilla and into the arm where it joins the long head;
the short head originates from the apex of the coracoid process of the scapula and passes vertically through the axilla and into the arm where it joins the long head; the long head originates as a tendon from the supraglenoid tubercle of the scapula, passes over the head of the humerus deep to the joint capsule of the glenohumeral joint, and enters the intertubercular sulcus where it is held in position by a ligament, the transverse humeral ligament, which spans the distance between the greater and lesser tubercles; the tendon passes through the axilla in the intertubercular sulcus and forms a muscle belly in the proximal part of the arm.
the long head originates as a tendon from the supraglenoid tubercle of the scapula, passes over the head of the humerus deep to the joint capsule of the glenohumeral joint, and enters the intertubercular sulcus where it is held in position by a ligament, the transverse humeral ligament, which spans the distance between the greater and lesser tubercles; the tendon passes through the axilla in the intertubercular sulcus and forms a muscle belly in the proximal part of the arm.The long and short heads of the muscle join in distal regions of the arm and primarily insert as a single tendon into the radial tuberosity in the forearm.
The biceps brachii muscle is primarily a powerful flexor of the forearm at the elbow joint and a powerful supinator in the forearm. Because both heads originate from the scapula, the muscle also acts as an accessory flexor of the arm at the glenohumeral joint. In addition, the long head prevents superior movement of the humerus on the glenoid cavity.
The biceps brachii muscle is innervated by the musculocutaneous nerve.
Coracobrachialis
The coracobrachialis muscle, together with the short head of the biceps brachii muscle, originates from the apex of the coracoid process (Fig. 7.48). It passes vertically through the axilla to insert on a small linear roughening on the medial aspect of the humerus, approximately midshaft.
The coracobrachialis muscle flexes the arm at the glenohumeral joint.
In the axilla, the medial surface of the coracobrachialis muscle is pierced by the musculocutaneous nerve, which innervates and then passes through the muscle to enter the arm.
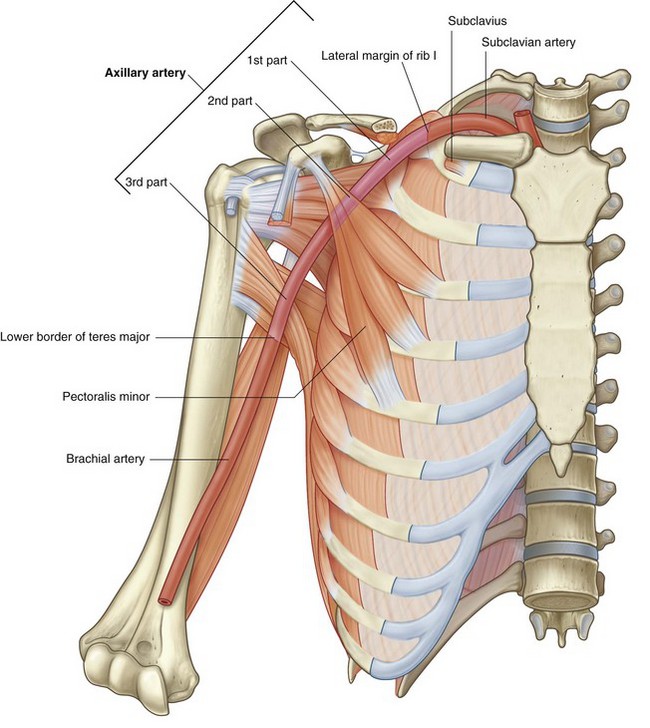
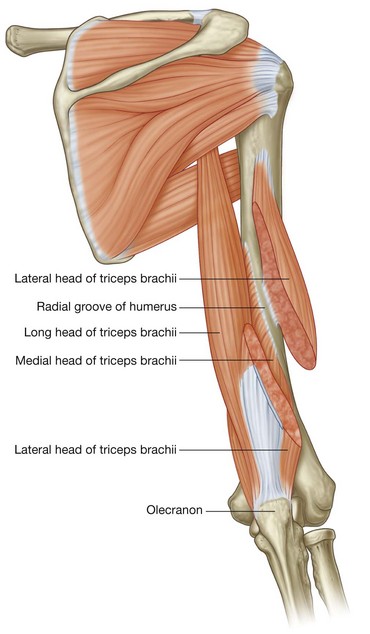
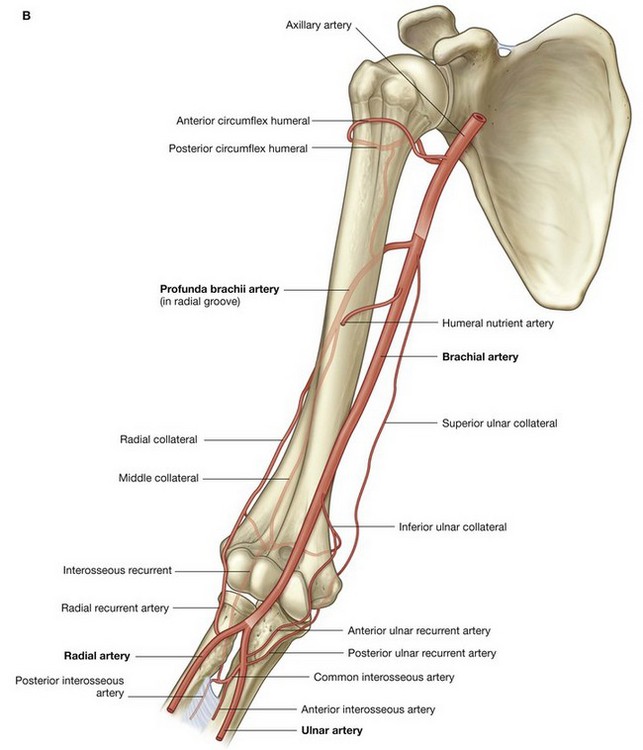
Axillary artery
The axillary artery supplies the walls of the axilla and related regions, and continues as the major blood supply to the more distal parts of the upper limb (Fig. 7.49).
The subclavian artery in the neck becomes the axillary artery at the lateral margin of rib I and passes through the axilla, becoming the brachial artery at the inferior margin of the teres major muscle.
The axillary artery is separated into three parts by the pectoralis minor muscle, which crosses anteriorly to the vessel (Fig. 7.49):
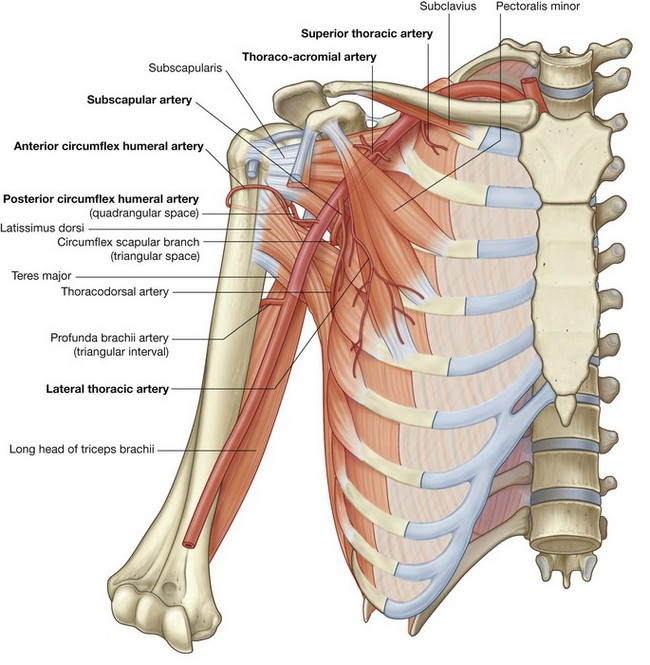
Generally, six branches arise from the axillary artery:
 two branches, the thoraco-acromial artery and the lateral thoracic artery, originate from the second part;
two branches, the thoraco-acromial artery and the lateral thoracic artery, originate from the second part; three branches, the subscapular artery, the anterior circumflex humeral artery, and the posterior circumflex humeral artery, originate from the third part (Fig. 7.50).
three branches, the subscapular artery, the anterior circumflex humeral artery, and the posterior circumflex humeral artery, originate from the third part (Fig. 7.50).Superior thoracic artery
The superior thoracic artery is small and originates from the anterior surface of the first part of the axillary artery (Fig. 7.50). It supplies upper regions of the medial and anterior axillary walls.
Thoraco-acromial artery
The thoraco-acromial artery is short and originates from the anterior surface of the second part of the axillary artery just posterior to the medial (superior) margin of the pectoralis minor muscle (Fig. 7.50). It curves around the superior margin of the muscle, penetrates the clavipectoral fascia, and immediately divides into four branches—the pectoral, deltoid, clavicular, and acromial branches, which supply the anterior axillary wall and related regions.
Additionally, the pectoral branch contributes vascular supply to the breast, and the deltoid branch passes into the clavipectoral triangle where it accompanies the cephalic vein and supplies adjacent structures (see Fig. 7.41).
Lateral thoracic artery
The lateral thoracic artery arises from the anterior surface of the second part of the axillary artery posterior to the lateral (inferior) margin of pectoralis minor (Fig. 7.50). It follows the margin of the muscle to the thoracic wall and supplies the medial and anterior walls of the axilla. In women, branches emerge from around the inferior margin of the pectoralis major muscle and contribute to the vascular supply of the breast.
Subscapular artery
The subscapular artery is the largest branch of the axillary artery and is the major blood supply to the posterior wall of the axilla (Fig. 7.50). It also contributes to the blood supply of the posterior scapular region.
The subscapular artery originates from the posterior surface of the third part of the axillary artery, follows the inferior margin of the subscapularis muscle for a short distance, then divides into its two terminal branches, the circumflex scapular artery and the thoracodorsal artery.
 The circumflex scapular artery passes through the triangular space between the subscapularis, teres major, and long head of the triceps muscles. Posteriorly, it passes inferior to, or pierces, the origin of the teres minor muscle to enter the infraspinous fossa. It anastomoses with the suprascapular artery and the deep branch (dorsal scapular artery) of the transverse cervical artery, thereby contributing to an anastomotic network of vessels around the scapula.
The circumflex scapular artery passes through the triangular space between the subscapularis, teres major, and long head of the triceps muscles. Posteriorly, it passes inferior to, or pierces, the origin of the teres minor muscle to enter the infraspinous fossa. It anastomoses with the suprascapular artery and the deep branch (dorsal scapular artery) of the transverse cervical artery, thereby contributing to an anastomotic network of vessels around the scapula.Anterior circumflex humeral artery
The anterior circumflex humeral artery is small compared to the posterior circumflex humeral artery, and originates from the lateral side of the third part of the axillary artery (Fig. 7.50). It passes anterior to the surgical neck of the humerus and anastomoses with the posterior circumflex humeral artery.
This anterior circumflex humeral artery supplies branches to surrounding tissues, which include the glenohumeral joint and the head of the humerus.
Posterior circumflex humeral artery
The posterior circumflex humeral artery originates from the lateral surface of the third part of the axillary artery immediately posterior to the origin of the anterior circumflex humeral artery (Fig. 7.50). With the axillary nerve, it leaves the axilla by passing through the quadrangular space between the teres major, teres minor, and the long head of the triceps brachii muscle and the surgical neck of the humerus.
The posterior circumflex humeral artery curves around the surgical neck of the humerus and supplies the surrounding muscles and the glenohumeral joint. It anastomoses with the anterior circumflex humeral artery, and with branches from the profunda brachii, suprascapular, and thoraco-acromial arteries.
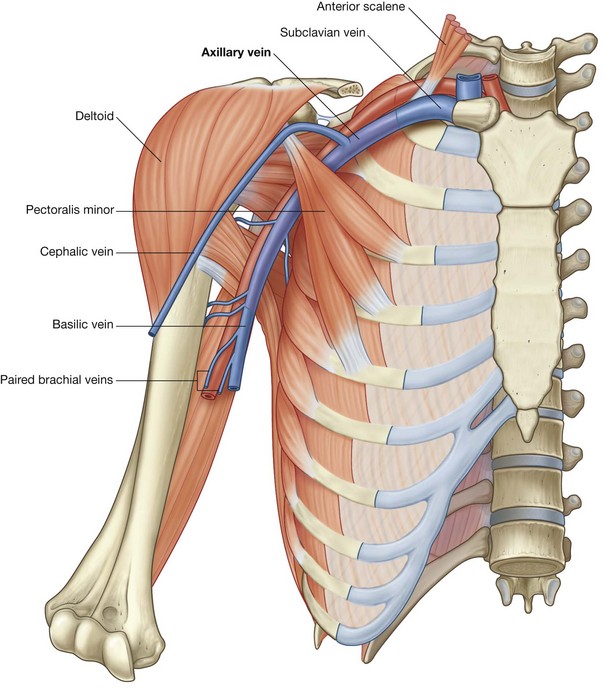
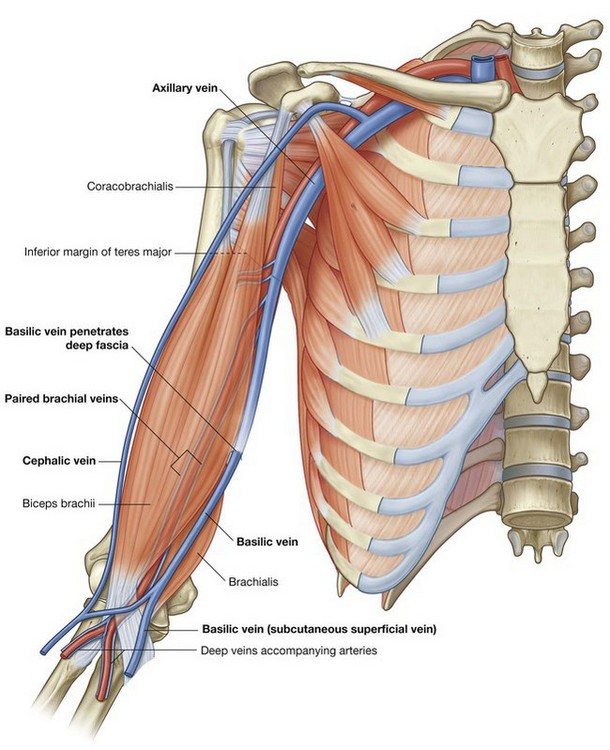
Axillary vein
The axillary vein begins at the lower margin of the teres major muscle and is the continuation of the basilic vein (Fig. 7.51), which is a superficial vein that drains the posteromedial surface of the hand and forearm and penetrates the deep fascia in the middle of the arm.
The axillary vein passes through the axilla medial and anterior to the axillary artery and becomes the subclavian vein as the vessel crosses the lateral border of rib I at the axillary inlet. Tributaries of the axillary vein generally follow the branches of the axillary artery. Other tributaries include brachial veins that follow the brachial artery, and the cephalic vein.
The cephalic vein is a superficial vein that drains the lateral and posterior parts of the hand, the forearm, and the arm. In the area of the shoulder, it passes into an inverted triangular cleft (the clavipectoral triangle) between the deltoid muscle, pectoralis major muscle, and the clavicle. In the superior part of the clavipectoral triangle, the cephalic vein passes deep to the clavicular head of the pectoralis major muscle and pierces the clavipectoral fascia to join the axillary vein. Many patients who are critically unwell have lost blood or fluid, which requires replacement. Access to a peripheral vein is necessary to replace the fluid. The typical sites for venous access are the cephalic vein adjacent to the anatomical snuffbox or the antecubital veins, which lie within the superficial tissues of the cubital fossa.
In the clinic
Imaging the blood supply to the upper limb
When there is clinical evidence of vascular compromise to the upper limb, or vessels are needed to form an arteriovenous fistula (which is necessary for renal dialysis), imaging is required to assess the vessels.
Ultrasound is a useful tool for carrying out a noninvasive assessment of the vessels of the upper limb from the third part of the subclavian artery to the deep and superficial palmar arteries. Blood flow can be quantified and anatomical variants can be noted.
Angiography is carried out in certain cases. The femoral artery is punctured below the inguinal ligament and a long catheter is placed through the iliac arteries and around the arch of the aorta to enter either the left subclavian artery or the brachiocephalic trunk and then the right subclavian artery. Radiopaque contrast agents are injected into the vessel and radiographs are obtained as the contrast agents pass first through the arteries, then the capillaries, and finally the veins.
In the clinic
Trauma to the arteries of the upper limb
The arterial supply to the upper limb is particularly susceptible to trauma in places where it is relatively fixed or in a subcutaneous position.
Fracture of rib I
As the subclavian artery passes out of the neck and into the axilla, it is fixed in position by the surrounding muscles to the superior surface of rib I. A rapid deceleration injury involving upper thoracic trauma may cause a first rib fracture, which may significantly compromise the distal part of the subclavian artery or the first part of the axillary artery. Fortunately, there are anastomotic connections between branches of the subclavian artery and the axillary artery, which form a network around the scapula and proximal end of the humerus; therefore, even with complete vessel transection, the arm is rarely rendered completely ischemic (ischemia is poor blood supply to an organ or a limb).
Anterior dislocation of the humeral head
Anterior dislocation of the humeral head may compress the axillary artery resulting in vessel occlusion. This is unlikely to render the upper limb completely ischemic, but it may be necessary to surgically reconstruct the axillary artery to obtain pain-free function. Importantly, the axillary artery is intimately related to the brachial plexus, which may be damaged at the time of anterior dislocation.
In the clinic
Subclavian pinch-off syndrome
There are a number of routes through which central venous access may be obtained. The “subclavian route” and the jugular routes are commonly used by clinicians. The subclavian route is a misnomer that remains the preferred term in clinical practice. In fact, most clinicians enter the first part of the axillary vein.
There are a number of patients that undergo catheterization of the subclavian vein/axillary vein. Entering the subclavian vein/axillary vein is a relatively straightforward technique. The clavicle is identified and a sharp needle is placed in the infraclavicular region aiming superomedially. When venous blood is aspirated, access has been obtained. This route is popular for long-term venous access, such as Hickman lines, and for shorter-term access where multiple-lumen catheters are inserted (e.g., intensive care unit). The subclavian vein/axillary vein is also the preferred site for insertion of pacemaker wires. There is, however, a preferred point of entry into the vein to prevent complications. The vein should be punctured in the midclavicular line or lateral to this line. The reason for this puncture site is the course of the vein and its relationship to other structures. The vein passes anterior to the artery, superior to the first rib and inferior to the clavicle as it courses through the thoracic inlet. Beneath the clavicle is situated the subclavius muscle. Should the puncture of the vein enter where the subclavius muscle is related to the axillary vein, the catheter or wire may become kinked at this point. Moreover, the constant contraction and relaxation of this muscle will induce fatigue in the line and wire, which may ultimately lead to fracture. A fractured pacemaker wire or a rupture in a chemotherapy catheter can have severe consequences for the patient.
Brachial plexus
The brachial plexus is a somatic plexus formed by the anterior rami of C5 to C8, and most of the anterior ramus of T1 (Fig. 7.52). It originates in the neck, passes laterally and inferiorly over rib I, and enters the axilla.
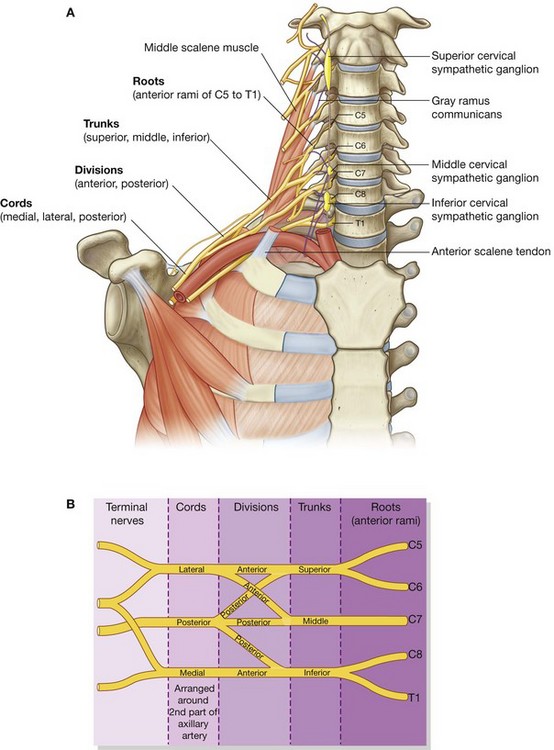
Fig. 7.52 Brachial plexus. A. Major components in the neck and axilla. B. Schematic showing parts of the brachial plexus.
The parts of the brachial plexus, from medial to lateral, are roots, trunks, divisions, and cords. All major nerves that innervate the upper limb originate from the brachial plexus, mostly from the cords. Proximal parts of the brachial plexus are posterior to the subclavian artery in the neck, while more distal regions of the plexus surround the axillary artery.
Roots
The roots of the brachial plexus are the anterior rami of C5 to C8, and most of T1. Close to their origin, the roots receive gray rami communicantes from the sympathetic trunk (Fig. 7.52). These carry postganglionic sympathetic fibers onto the roots for distribution to the periphery. The roots and trunks enter the posterior triangle of the neck by passing between the anterior scalene and middle scalene muscles and lie superior and posterior to the subclavian artery.
Trunks
The three trunks of the brachial plexus originate from the roots, pass laterally over rib I, and enter the axilla (Fig. 7.52):
The inferior trunk lies on rib I posterior to the subclavian artery; the middle and superior trunks are more superior in position.
Divisions
Each of the three trunks of the brachial plexus divides into an anterior and a posterior division (Fig. 7.52):
 the three anterior divisions form parts of the brachial plexus that ultimately give rise to peripheral nerves associated with the anterior compartments of the arm and forearm;
the three anterior divisions form parts of the brachial plexus that ultimately give rise to peripheral nerves associated with the anterior compartments of the arm and forearm; the three posterior divisions combine to form parts of the brachial plexus that give rise to nerves associated with the posterior compartments.
the three posterior divisions combine to form parts of the brachial plexus that give rise to nerves associated with the posterior compartments.No peripheral nerves originate directly from the divisions of the brachial plexus.
Cords
The three cords of the brachial plexus originate from the divisions and are related to the second part of the axillary artery (Fig. 7.52):
 the lateral cord results from the union of the anterior divisions of the upper and middle trunks and therefore has contributions from C5 to C7—it is positioned lateral to the second part of the axillary artery;
the lateral cord results from the union of the anterior divisions of the upper and middle trunks and therefore has contributions from C5 to C7—it is positioned lateral to the second part of the axillary artery; the medial cord is medial to the second part of the axillary artery and is the continuation of the anterior division of the inferior trunk—it contains contributions from C8 and T1;
the medial cord is medial to the second part of the axillary artery and is the continuation of the anterior division of the inferior trunk—it contains contributions from C8 and T1; the posterior cord occurs posterior to the second part of the axillary artery and originates as the union of all three posterior divisions—it contains contributions from all roots of the brachial plexus (C5 to T1).
the posterior cord occurs posterior to the second part of the axillary artery and originates as the union of all three posterior divisions—it contains contributions from all roots of the brachial plexus (C5 to T1).Most of the major peripheral nerves of the upper limb originate from the cords of the brachial plexus. Generally, nerves associated with the anterior compartments of the upper limb arise from the medial and lateral cords and nerves associated with the posterior compartments originate from the posterior cord.
Branches (Table 7.7)
Branches of the roots
In addition to small segmental branches from C5 to C8 to muscles of the neck and a contribution of C5 to the phrenic nerve, the roots of the brachial plexus give rise to the dorsal scapular and long thoracic nerves (Fig. 7.53).
Table 7.7 Branches of brachial plexus (brackets indicate that a spinal segment is a minor component of the nerve or is inconsistently present in the nerve)
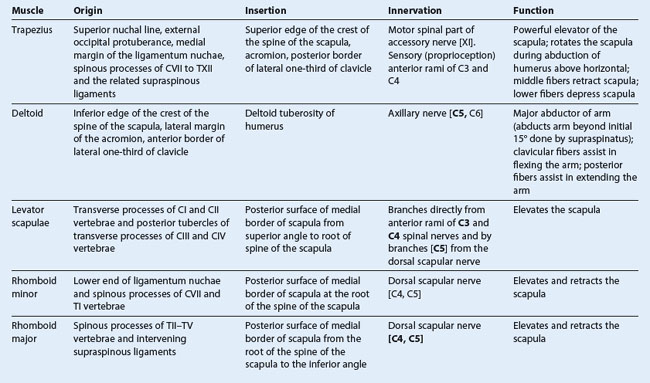
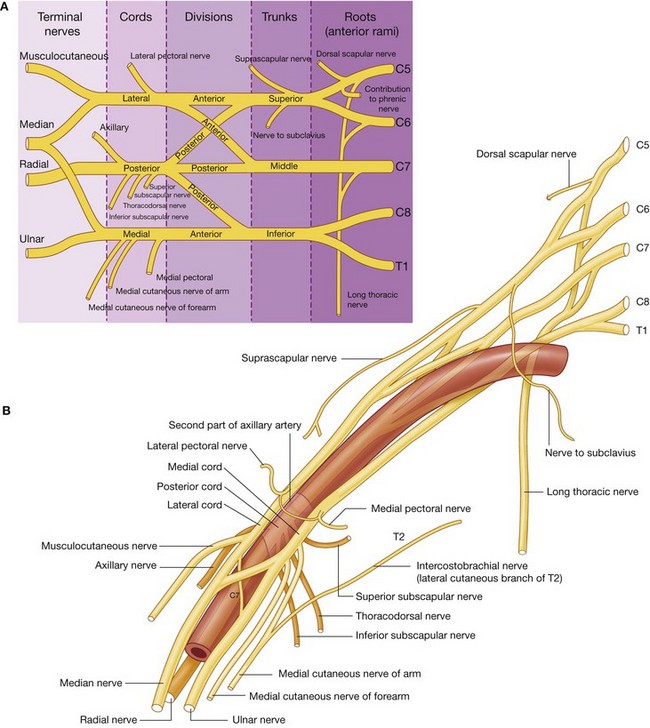
Fig. 7.53 Brachial plexus. A. Schematic showing branches of the brachial plexus. B. Relationships to the axillary artery.
 passes posteriorly, often piercing the middle scalene muscle in the neck, to reach and travel along the medial border of the scapula (Fig. 7.54); and
passes posteriorly, often piercing the middle scalene muscle in the neck, to reach and travel along the medial border of the scapula (Fig. 7.54); and passes vertically down the neck, through the axillary inlet, and down the medial wall of the axilla to supply the serratus anterior muscle (Fig. 7.54); and
passes vertically down the neck, through the axillary inlet, and down the medial wall of the axilla to supply the serratus anterior muscle (Fig. 7.54); andBranches of the trunks
The only branches from the trunks of the brachial plexus are two nerves that originate from the superior trunk (upper trunk): the suprascapular nerve and the nerve to the subclavius muscle (Fig. 7.53).
The suprascapular nerve (C5 and C6):
 passes laterally through the posterior triangle of the neck (Fig. 7.54) and through the suprascapular foramen to enter the posterior scapular region;
passes laterally through the posterior triangle of the neck (Fig. 7.54) and through the suprascapular foramen to enter the posterior scapular region; is accompanied in the lateral parts of the neck and in the posterior scapular region by the suprascapular artery.
is accompanied in the lateral parts of the neck and in the posterior scapular region by the suprascapular artery.The nerve to subclavius muscle (C5 and C6) is a small nerve that:
Branches of the lateral cord
Three nerves originate entirely or partly from the lateral cord (Fig. 7.53).
 The lateral pectoral nerve is the most proximal of the branches from the lateral cord. It passes anteriorly, together with the thoraco-acromial artery, to penetrate the clavipectoral fascia that spans the gap between the subclavius and pectoralis minor muscles (Fig. 7.55), and innervates the pectoralis major muscle.
The lateral pectoral nerve is the most proximal of the branches from the lateral cord. It passes anteriorly, together with the thoraco-acromial artery, to penetrate the clavipectoral fascia that spans the gap between the subclavius and pectoralis minor muscles (Fig. 7.55), and innervates the pectoralis major muscle. The musculocutaneous nerve is a large terminal branch of the lateral cord. It passes laterally to penetrate the coracobrachialis muscle and pass between the biceps brachii and brachialis muscles in the arm, and innervates all three flexor muscles in the anterior compartment of the arm, terminating as the lateral cutaneous nerve of forearm.
The musculocutaneous nerve is a large terminal branch of the lateral cord. It passes laterally to penetrate the coracobrachialis muscle and pass between the biceps brachii and brachialis muscles in the arm, and innervates all three flexor muscles in the anterior compartment of the arm, terminating as the lateral cutaneous nerve of forearm. The lateral root of median nerve is the largest terminal branch of the lateral cord and passes medially to join a similar branch from the medial cord to form the median nerve (Fig. 7.55).
The lateral root of median nerve is the largest terminal branch of the lateral cord and passes medially to join a similar branch from the medial cord to form the median nerve (Fig. 7.55).Branches of the medial cord
The medial cord has five branches (Fig. 7.55).
 The medial pectoral nerve is the most proximal branch. It receives a communicating branch from the lateral pectoral nerve and then passes anteriorly between the axillary artery and axillary vein. Branches of the nerve penetrate and supply the pectoralis minor muscle. Some of these branches pass through the muscle to reach and supply the pectoralis major muscle. Other branches occasionally pass around the inferior or lateral margin of the pectoralis minor muscle to reach the pectoralis major muscle.
The medial pectoral nerve is the most proximal branch. It receives a communicating branch from the lateral pectoral nerve and then passes anteriorly between the axillary artery and axillary vein. Branches of the nerve penetrate and supply the pectoralis minor muscle. Some of these branches pass through the muscle to reach and supply the pectoralis major muscle. Other branches occasionally pass around the inferior or lateral margin of the pectoralis minor muscle to reach the pectoralis major muscle. The medial cutaneous nerve of arm (medial brachial cutaneous nerve) passes through the axilla and into the arm where it penetrates deep fascia and supplies skin over the medial side of the distal third of the arm. In the axilla, the nerve communicates with the intercostobrachial nerve of T2. Fibers of the medial cutaneous nerve of arm innervate the upper part of the medial surface of the arm and floor of the axilla.
The medial cutaneous nerve of arm (medial brachial cutaneous nerve) passes through the axilla and into the arm where it penetrates deep fascia and supplies skin over the medial side of the distal third of the arm. In the axilla, the nerve communicates with the intercostobrachial nerve of T2. Fibers of the medial cutaneous nerve of arm innervate the upper part of the medial surface of the arm and floor of the axilla. The medial cutaneous nerve of forearm (medial antebrachial cutaneous nerve) originates just distal to the origin of the medial cutaneous nerve of arm. It passes out of the axilla and into the arm where it gives off a branch to the skin over the biceps brachii muscle, and then continues down the arm to penetrate the deep fascia with the basilic vein, continuing inferiorly to supply the skin over the anterior surface of the forearm. It innervates skin over the medial surface of the forearm down to the wrist.
The medial cutaneous nerve of forearm (medial antebrachial cutaneous nerve) originates just distal to the origin of the medial cutaneous nerve of arm. It passes out of the axilla and into the arm where it gives off a branch to the skin over the biceps brachii muscle, and then continues down the arm to penetrate the deep fascia with the basilic vein, continuing inferiorly to supply the skin over the anterior surface of the forearm. It innervates skin over the medial surface of the forearm down to the wrist. The medial root of median nerve passes laterally to join with a similar root from the lateral cord to form the median nerve anterior to the third part of the axillary artery.
The medial root of median nerve passes laterally to join with a similar root from the lateral cord to form the median nerve anterior to the third part of the axillary artery. The ulnar nerve is a large terminal branch of the medial cord (Fig. 7.55). However, near its origin, it often receives a communicating branch from the lateral root of the median nerve originating from the lateral cord and carrying fibers from C7. The ulnar nerve passes through the arm and forearm into the hand where it innervates all intrinsic muscles of the hand (except for the three thenar muscles and the two lateral lumbrical muscles). On passing through the forearm, branches of the ulnar nerve innervate the flexor carpi ulnaris muscle and the medial half of the flexor digitorum profundus muscle. The ulnar nerve innervates skin over the palmar surface of the little finger, medial half of the ring finger, and associated palm and wrist, and the skin over the dorsal surface of the medial part of the hand.
The ulnar nerve is a large terminal branch of the medial cord (Fig. 7.55). However, near its origin, it often receives a communicating branch from the lateral root of the median nerve originating from the lateral cord and carrying fibers from C7. The ulnar nerve passes through the arm and forearm into the hand where it innervates all intrinsic muscles of the hand (except for the three thenar muscles and the two lateral lumbrical muscles). On passing through the forearm, branches of the ulnar nerve innervate the flexor carpi ulnaris muscle and the medial half of the flexor digitorum profundus muscle. The ulnar nerve innervates skin over the palmar surface of the little finger, medial half of the ring finger, and associated palm and wrist, and the skin over the dorsal surface of the medial part of the hand.The median nerve is formed anterior to the third part of the axillary artery by the union of lateral and medial roots originating from the lateral and medial cords of the brachial plexus (Fig. 7.55). It passes into the arm anterior to the brachial artery, through the arm into the forearm where branches innervate most of the muscles in the anterior compartment of the forearm (except for the flexor carpi ulnaris muscle and the medial half of the flexor digitorum profundus muscle, which are innervated by the ulnar nerve).
The median nerve continues into the hand to innervate:
 the skin over the palmar surface of the lateral three and one-half digits and over the lateral side of the palm and middle of the wrist.
the skin over the palmar surface of the lateral three and one-half digits and over the lateral side of the palm and middle of the wrist.The musculocutaneous nerve, the lateral root of the median nerve, the median nerve, the medial root of the median nerve, and the ulnar nerve form an M over the third part of the axillary artery (Fig. 7.55). This feature, together with penetration of the coracobrachialis muscle by the musculocutaneous nerve, can be used to identify components of the brachial plexus in the axilla.
Branches of the posterior cord
Five nerves originate from the posterior cord of the brachial plexus:
All these nerves except the radial nerve innervate muscles associated with the posterior wall of the axilla; the radial nerve passes into the arm and forearm.
The superior subscapular nerve, the thoracodorsal, and the inferior subscapular nerves originate sequentially from the posterior cord and pass directly into muscles associated with the posterior axillary wall (Fig. 7.56). The superior subscapular nerve is short and passes into and supplies the subscapularis muscle. The thoracodorsal nerve is the longest of these three nerves and passes vertically along the posterior axillary wall. It penetrates and innervates the latissimus dorsi muscle. The inferior subscapular nerve also passes inferiorly along the posterior axillary wall and innervates the subscapularis and teres major muscles.
The axillary nerve originates from the posterior cord and passes inferiorly and laterally along the posterior wall to exit the axilla through the quadrangular space (Fig. 7.56). It passes posteriorly around the surgical neck of the humerus and innervates both the deltoid and teres minor muscles. A superior lateral cutaneous nerve of arm originates from the axillary nerve after passing through the quadrangular space and loops around the posterior margin of the deltoid muscle to innervate skin in that region. The axillary nerve is accompanied by the posterior circumflex humeral artery.
The radial nerve is the largest terminal branch of the posterior cord (Fig. 7.56). It passes out of the axilla and into the posterior compartment of the arm by passing through the triangular interval between the inferior border of the teres major muscle, the long head of the triceps brachii muscle, and the shaft of the humerus. It is accompanied through the triangular interval by the profunda brachii artery, which originates from the brachial artery in the anterior compartment of the arm. The radial nerve and its branches innervate:
 the skin on the posterior aspect of the arm and forearm, the lower lateral surface of the arm, and the dorsal lateral surface of the hand.
the skin on the posterior aspect of the arm and forearm, the lower lateral surface of the arm, and the dorsal lateral surface of the hand.The posterior cutaneous nerve of arm (posterior brachial cutaneous nerve) originates from the radial nerve in the axilla and innervates skin on the posterior surface of the arm.
In the clinic
Injuries to the brachial plexus
The brachial plexus is an extremely complex structure. When damaged, it requires meticulous clinical history taking and examination. Assessment of the individual nerve functions can be obtained by nerve conduction studies and electromyography, which assess the latency of muscle contraction when the nerve is artificially stimulated.
Brachial plexus injuries are usually the result of blunt trauma producing nerve avulsions and disruption. These injuries are usually devastating for the function of the upper limb and require many months of dedicated rehabilitation for even a small amount of function to return.
Spinal cord injuries in the cervical region and direct pulling injuries tend to affect the roots of the brachial plexus. Severe trauma to the first rib usually affects the trunks. The divisions and cords of the brachial plexus can be injured by dislocation of the glenohumeral joint.
Lymphatics
All lymphatics from the upper limb drain into lymph nodes in the axilla (Fig. 7.57).
In addition, axillary nodes receive drainage from an extensive area on the adjacent trunk, which includes regions of the upper back and shoulder, the lower neck, the chest, and the upper anterolateral abdominal wall. Axillary nodes also receive drainage from approximately 75% of the mammary gland.
The 20–30 axillary nodes are generally divided into five groups on the basis of location.
 Humeral (lateral) nodes posteromedial to the axillary vein receive most of the lymphatic drainage from the upper limb.
Humeral (lateral) nodes posteromedial to the axillary vein receive most of the lymphatic drainage from the upper limb. Pectoral (anterior) nodes occur along the inferior margin of the pectoralis minor muscle along the course of the lateral thoracic vessels and receive drainage from the abdominal wall, the chest, and the mammary gland.
Pectoral (anterior) nodes occur along the inferior margin of the pectoralis minor muscle along the course of the lateral thoracic vessels and receive drainage from the abdominal wall, the chest, and the mammary gland. Subscapular (posterior) nodes on the posterior axillary wall in association with the subscapular vessels drain the posterior axillary wall and receive lymphatics from the back, the shoulder, and the neck.
Subscapular (posterior) nodes on the posterior axillary wall in association with the subscapular vessels drain the posterior axillary wall and receive lymphatics from the back, the shoulder, and the neck. Central nodes are embedded in axillary fat and receive tributaries from humeral, subscapular, and pectoral groups of nodes.
Central nodes are embedded in axillary fat and receive tributaries from humeral, subscapular, and pectoral groups of nodes. Apical nodes are the most superior group of nodes in the axilla and drain all other groups of nodes in the region. In addition, they receive lymphatic vessels that accompany the cephalic vein as well as vessels that drain the superior region of the mammary gland.
Apical nodes are the most superior group of nodes in the axilla and drain all other groups of nodes in the region. In addition, they receive lymphatic vessels that accompany the cephalic vein as well as vessels that drain the superior region of the mammary gland.Efferent vessels from the apical group converge to form the subclavian trunk, which usually joins the venous system at the junction between the right subclavian vein and the right internal jugular vein in the neck. On the left, the subclavian trunk usually joins the thoracic duct in the base of the neck.
In the clinic
Breast cancer
Lymphatic drainage from the lateral part of the breast passes through nodes in the axilla. Significant disruption to the normal lymphatic drainage of the upper limb may occur if a mastectomy or a surgical axillary nodal clearance has been carried out for breast cancer. Furthermore, some patients have radiotherapy to the axilla to prevent the spread of metastatic disease, but a side effect of this is the destruction of the tiny lymphatics as well as the cancer cells.
If the lymphatic drainage of the upper limb is damaged, the arm may swell and pitting edema (lymphedema) may develop.
Axillary process of the mammary gland
Although the mammary gland is in superficial fascia overlying the thoracic wall, its superolateral region extends along the inferior margin of the pectoralis major muscle toward the axilla. In some cases, this may pass around the margin of the muscle to penetrate deep fascia and enter the axilla (Fig. 7.58). This axillary process rarely reaches as high as the apex of the axilla.
ARM
The arm is the region of the upper limb between the shoulder and the elbow (Fig. 7.59). The superior aspect of the arm communicates medially with the axilla. Inferiorly, a number of important structures pass between the arm and the forearm through the cubital fossa, which is positioned anterior to the elbow joint.
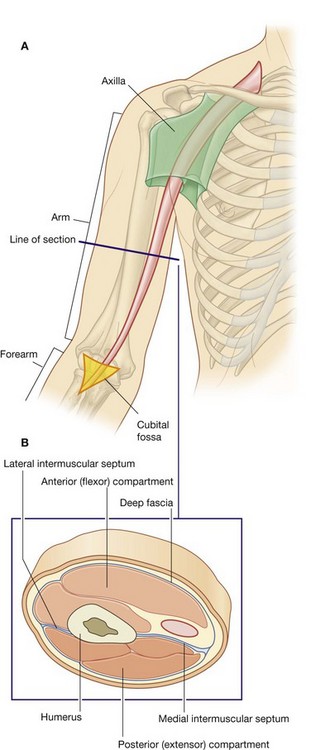
Fig. 7.59 Arm. A. Proximal and distal relationships. B. Transverse section through the middle of the arm.
The arm is divided into two compartments by medial and lateral intermuscular septa, which pass from each side of the humerus to the outer sleeve of deep fascia that surrounds the limb (Fig. 7.59).
The anterior compartment of the arm contains muscles that predominantly flex the elbow joint; the posterior compartment contains muscles that extend the joint. Major nerves and vessels supply and pass through each compartment.
Bones
The skeletal support for the arm is the humerus (Fig. 7.60). Most of the large muscles of the arm insert into the proximal ends of the two bones of the forearm, the radius and the ulna, and flex and extend the forearm at the elbow joint. In addition, the muscles predominantly situated in the forearm that move the hand originate at the distal end of the humerus.
Shaft and distal end of the humerus
In cross-section, the shaft of the humerus is somewhat triangular with:
The posterior surface of the humerus is marked on its superior aspect by a linear roughening for the attachment of the lateral head of the triceps brachii muscle, beginning just inferior to the surgical neck and passing diagonally across the bone to the deltoid tuberosity.
The middle part of the posterior surface and adjacent part of the anterolateral surface are marked by the shallow radial groove, which passes diagonally down the bone and parallel to the sloping posterior margin of the deltoid tuberosity. The radial nerve and the profunda brachii artery lie in this groove.
Approximately in the middle of the shaft, the medial border is marked by thin elongate roughening for the attachment of the coracobrachialis muscle.
Intermuscular septa, which separate the anterior compartment from the posterior compartment, attach to the medial and lateral borders (Fig. 7.61).
Distally, the bone becomes flattened, and these borders expand as the lateral supraepicondylar ridge (lateral supracondylar ridge) and the medial supraepicondylar ridge (medial supracondylar ridge). The lateral supraepicondylar ridge is more pronounced than the medial and is roughened for the attachment of muscles found in the posterior compartment of the forearm.
The distal end of the humerus, which is flattened in the anteroposterior plane, bears a condyle, two epicondyles, and three fossae, as follows (Fig. 7.61).
The condyle
The two articular parts of the condyle, the capitulum and the trochlea, articulate with the two bones of the forearm.
The capitulum articulates with the radius of the forearm. Lateral in position and hemispherical in shape, it projects anteriorly and somewhat inferiorly and is not visible when the humerus is viewed from the posterior aspect.
The trochlea articulates with the ulna of the forearm. It is pulley shaped and lies medial to the capitulum. Its medial edge is more pronounced than its lateral edge and, unlike the capitulum, it extends onto the posterior surface of the bone.
The two epicondyles
The two epicondyles lie adjacent, and somewhat superior, to the trochlea and capitulum (Fig. 7.61).
The medial epicondyle, a large bony protuberance, is the major palpable landmark on the medial side of the elbow, and projects medially from the distal end of the humerus. On its surface, it bears a large oval impression for the attachment of muscles in the anterior compartment of the forearm. The ulnar nerve passes from the arm into the forearm around the posterior surface of the medial epicondyle and can be palpated against the bone in this location.
The lateral epicondyle is much less pronounced than the medial epicondyle. It is lateral to the capitulum and has a large irregular impression for the attachment of muscles in the posterior compartment of the forearm.
The three fossae
Three fossae occur superior to the trochlea and capitulum on the distal end of the humerus (Fig. 7.61).
The radial fossa is the least distinct of the fossae and occurs immediately superior to the capitulum on the anterior surface of the humerus.
The coronoid fossa is adjacent to the radial fossa and is superior to the trochlea.
The largest of the fossae, the olecranon fossa, occurs immediately superior to the trochlea on the posterior surface of the distal end of the humerus.
These three fossae accommodate projections from the bones in the forearm during movements of the elbow joint.
Proximal end of the radius
The proximal end of the radius consists of a head, a neck, and the radial tuberosity (Fig. 7.62).
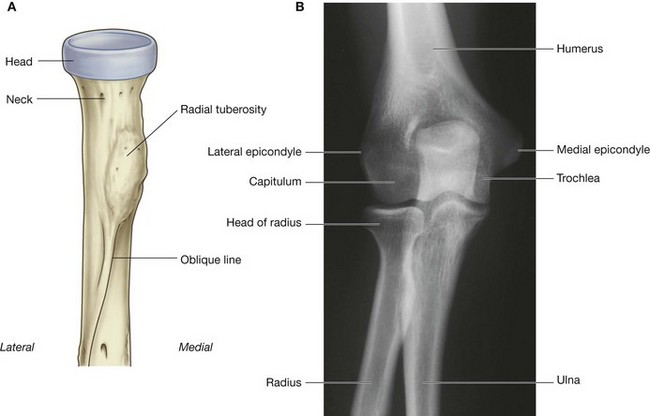
Fig. 7.62 A. Anterior view of the proximal end of the radius. B. Radiograph of the elbow joint (anterior–posterior view).
The head of the radius is a thick disc-shaped structure oriented in the horizontal plane. The circular superior surface is concave for articulation with the capitulum of the humerus. The thick margin of the disc is broad medially where it articulates with the radial notch on the proximal end of the ulna.
The neck of the radius is a short and narrow cylinder of bone between the expanded head and the radial tuberosity on the shaft.
The radial tuberosity is a large blunt projection on the medial surface of the radius immediately inferior to the neck. Much of its surface is roughened for the attachment of the biceps brachii tendon. The oblique line of the radius continues diagonally across the shaft of the bone from the inferior margin of the radial tuberosity.
Proximal end of the ulna
The proximal end of the ulna is much larger than the proximal end of the radius and consists of the olecranon, the coronoid process, the trochlear notch, the radial notch, and the tuberosity of ulna (Fig. 7.63).
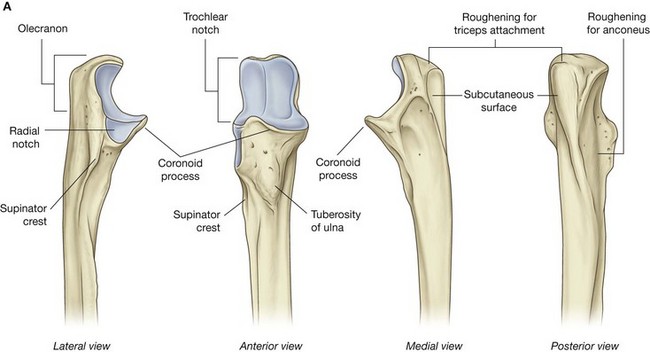
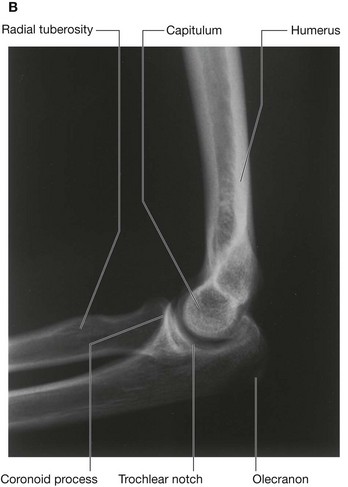
Fig. 7.63 A. Lateral, anterior, medial, and posterior views of the proximal end of the ulna. B. Radiograph of the elbow joint (lateral view).
The olecranon is a large projection of bone that extends proximally from the ulna. Its anterolateral surface is articular and contributes to the formation of the trochlear notch, which articulates with the trochlea of the humerus. The superior surface is marked by a large roughened impression for the attachment of the triceps brachii muscle.
The posterior surface is smooth, shaped somewhat triangularly, and can be palpated as the “tip of the elbow.”
The coronoid process projects anteriorly from the proximal end of the ulna (Fig. 7.63). Its superolateral surface is articular and participates, with the olecranon, in forming the trochlear notch. The lateral surface is marked by the radial notch for articulation with the head of the radius.
Just inferior to the radial notch is a fossa that allows the radial tuberosity to change position during pronation and supination. The posterior margin of this fossa is broadened to form the supinator crest. The anterior surface of the coronoid process is triangular, with the apex directed distally, and has a number of roughenings for muscle attachment. The largest of these roughenings, the tuberosity of ulna, is at the apex of the anterior surface and is the attachment site for the brachialis muscle.
Muscles
The anterior compartment of the arm contains three muscles—the coracobrachialis, brachialis, and biceps brachii muscles—which are innervated predominantly by the musculocutaneous nerve.
The posterior compartment contains one muscle—the triceps brachii muscle—which is innervated by the radial nerve.
Coracobrachialis
The coracobrachialis muscle extends from the tip of the coracoid process of the scapula to the medial side of the midshaft of the humerus (Fig. 7.64 and Table 7.8). It passes through the axilla and is penetrated and innervated by the musculocutaneous nerve.
Biceps brachii
The biceps brachii muscle has two heads:
 the short head of the muscle originates from the coracoid process in conjunction with the coracobrachialis;
the short head of the muscle originates from the coracoid process in conjunction with the coracobrachialis; the long head originates as a tendon from the supraglenoid tubercle of the scapula (Fig. 7.64 and Table 7.8).
the long head originates as a tendon from the supraglenoid tubercle of the scapula (Fig. 7.64 and Table 7.8).The tendon of the long head passes through the glenohumeral joint superior to the head of the humerus, then passes through the intertubercular sulcus and enters the arm. In the arm, the tendon joins with its muscle belly and, together with the muscle belly of the short head, overlies the brachialis muscle.
The long and short heads converge to form a single tendon, which inserts onto the radial tuberosity.
As the tendon enters the forearm, a flat sheet of connective tissue (the bicipital aponeurosis) fans out from the medial side of the tendon to blend with deep fascia covering the anterior compartment of the forearm.
The biceps brachii muscle is a powerful flexor of the forearm at the elbow joint; it is also the most powerful supinator of the forearm when the elbow joint is flexed. Because the two heads of the biceps brachii muscle cross the glenohumeral joint, the muscle can also flex the glenohumeral joint.
The biceps brachii muscle is innervated by the musculocutaneous nerve. A tap on the tendon of biceps brachii at the elbow is used to test predominantly spinal cord segment C6.
In the clinic
Rupture of biceps tendon
It is relatively unusual for muscles and their tendons to rupture in the upper limb; however, the tendon that most commonly ruptures is the tendon of the long head of the biceps brachii muscle. In isolation, this has relatively little effect on the upper limb, but it does produce a characteristic deformity—on flexing the elbow, there is an extremely prominent bulge of the muscle belly as its unrestrained fibers contract—the “Popeye” sign.
Brachialis
The brachialis muscle originates from the distal half of the anterior aspect of the humerus and from adjacent parts of the intermuscular septa, particularly on the medial side (Fig. 7.64 and Table 7.8). It lies beneath the biceps brachii muscle, is flattened dorsoventrally, and converges to form a tendon, which attaches to the tuberosity of the ulna.
The brachialis muscle flexes the forearm at the elbow joint.
Innervation of brachialis muscle is predominantly by the musculocutaneous nerve. A small component of the lateral part is innervated by the radial nerve.
Posterior compartment
The only muscle of the posterior compartment of the arm is the triceps brachii muscle (Fig. 7.65 and Table 7.9). The triceps brachii muscle has three heads:
 the medial head originates from the extensive area on the posterior surface of the shaft of the humerus inferior to the radial groove;
the medial head originates from the extensive area on the posterior surface of the shaft of the humerus inferior to the radial groove;Table 7.9 Muscle of the posterior compartment of the arm (spinal segments indicated in bold are the major segments innervating the muscle)
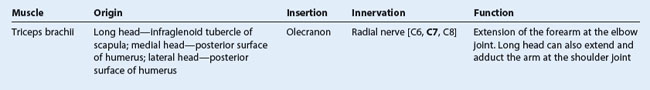
The three heads converge to form a large tendon, which inserts on the superior surface of the olecranon of the ulna.
The triceps brachii muscle extends the forearm at the elbow joint.
Arteries and veins
Brachial artery
The major artery of the arm, the brachial artery, is found in the anterior compartment (Fig. 7.66). Beginning as a continuation of the axillary artery at the lower border of the teres major muscle, it terminates just distal to the elbow joint where it divides into the radial and ulnar arteries.
In the proximal arm, the brachial artery lies on the medial side. In the distal arm, it moves laterally to assume a position midway between the lateral epicondyle and the medial epicondyle of the humerus. It crosses anteriorly to the elbow joint where it lies immediately medial to the tendon of the biceps brachii muscle. The brachial artery is palpable along its length. In proximal regions, the brachial artery can be compressed against the medial side of the humerus.
Branches of the brachial artery in the arm include those to adjacent muscles and two ulnar collateral vessels, which contribute to a network of arteries around the elbow joint. Additional branches are the profunda brachii artery and nutrient arteries to the humerus, which pass through a foramen in the anteromedial surface of the humeral shaft.
In the clinic
Blood pressure measurement
Blood pressure measurement is an extremely important physiologic parameter. High blood pressure (hypertension) requires treatment to prevent long-term complications such as stroke. Low blood pressure may be caused by extreme blood loss, widespread infection, or poor cardiac output (e.g., after myocardial infarction). Accurate measurement of blood pressure is essential.
Most clinicians use a sphygmomanometer and a stethoscope. The sphygmomanometer is a device that inflates a cuff around the midportion of the arm to compress the brachial artery against the humerus. The cuff is inflated so it exceeds the systolic blood pressure (greater than 120 mm Hg). The clinician places a stethoscope over the brachial artery in the cubital fossa and listens (auscultates) for the pulse. As the pressure in the arm cuff of the sphygmomanometer is reduced just below the level of the systolic blood pressure, the pulse becomes audible as a regular thumping sound. As the pressure in the sphygmomanometer continues to drop, the regular thumping sound becomes clearer. When the pressure in the sphygmomanometer is less than that of the diastolic blood pressure, the audible thumping sound becomes inaudible. Using the simple scale on the sphygmomanometer, the patient’s blood pressure can be determined. The normal range is 120/80 mm Hg (systolic blood pressure/diastolic blood pressure).
Profunda brachii artery
The profunda brachii artery, the largest branch of the brachial artery, passes into and supplies the posterior compartment of the arm (Fig. 7.66). It enters the posterior compartment with the radial nerve and together they pass through the triangular interval, which is formed by the shaft of the humerus, the inferior margin of the teres major muscle, and the lateral margin of the long head of the triceps muscle. They then pass along the radial groove on the posterior surface of the humerus deep to the lateral head of the triceps brachii muscle.
Branches of the profunda brachii artery supply adjacent muscles and anastomose with the posterior circumflex humeral artery. The artery terminates as two collateral vessels, which contribute to an anastomotic network of arteries around the elbow joint.
Veins
Paired brachial veins pass along the medial and lateral sides of the brachial artery, receiving tributaries that accompany branches of the artery (Fig. 7.67).
In addition to these deep veins, two large subcutaneous veins, the basilic vein and the cephalic vein, are located in the arm.
The basilic vein passes vertically in the distal half of the arm, penetrates deep fascia to assume a position medial to the brachial artery, and then becomes the axillary vein at the lower border of the teres major muscle. The brachial veins join the basilic, or axillary, vein.
The cephalic vein passes superiorly on the anterolateral aspect of the arm and through the anterior wall of the axilla to reach the axillary vein.
Nerves
Musculocutaneous nerve
The musculocutaneous nerve leaves the axilla and enters the arm by passing through the coracobrachialis muscle (Fig. 7.68). It passes diagonally down the arm in the plane between the biceps brachii and brachialis muscles. After giving rise to motor branches in the arm, it emerges laterally to the tendon of the biceps brachii muscle at the elbow, penetrates deep fascia, and continues as the lateral cutaneous nerve of forearm.
Median nerve
The median nerve enters the arm from the axilla at the inferior margin of the teres major muscle (Fig. 7.68). It passes vertically down the medial side of the arm in the anterior compartment and is related to the brachial artery throughout its course:
 in more distal regions, the median nerve crosses to the medial side of the brachial artery and lies anterior to the elbow joint.
in more distal regions, the median nerve crosses to the medial side of the brachial artery and lies anterior to the elbow joint.The median nerve has no major branches in the arm, but a branch to one of the muscles of the forearm, the pronator teres muscle, may originate from the nerve immediately proximal to the elbow joint.
In the clinic
Median nerve injury in the arm
In the arm and forearm the median nerve is usually not injured by trauma because of its relatively deep position. The commonest neurological problem associated with the median nerve is compression beneath the flexor retinaculum at the wrist (carpal tunnel syndrome).
On very rare occasions, a fibrous band may arise from the anterior aspect of the humerus beneath which the median nerve passes. This is an embryological remnant of the coracobrachialis muscle and is sometimes called the ligament of Struthers; occasionally, it may calcify. This band can compress the median nerve, resulting in weakness of the flexor muscles in the forearm and the thenar muscles. Nerve conduction studies will demonstrate the site of nerve compression.
Ulnar nerve
The ulnar nerve enters the arm with the median nerve and axillary artery (Fig. 7.68). It passes through proximal regions medial to the axillary artery. In the middle of the arm, the ulnar nerve penetrates the medial intermuscular septum and enters the posterior compartment where it lies anterior to the medial head of the triceps brachii muscle. It passes posterior to the medial epicondyle of the humerus and then into the anterior compartment of the forearm.
Radial nerve
The radial nerve originates from the posterior cord of the brachial plexus and enters the arm by crossing the inferior margin of the teres major muscle (Fig. 7.69). As it enters the arm, it lies posterior to the brachial artery. Accompanied by the profunda brachii artery, the radial nerve enters the posterior compartment of the arm by passing through the triangular interval.
As the radial nerve passes diagonally, from medial to lateral, through the posterior compartment, it lies in the radial groove directly on bone. On the lateral side of the arm, it passes anteriorly through the lateral intermuscular septum and enters the anterior compartment where it lies between the brachialis muscle and a muscle of the posterior compartment of the forearm—the brachioradialis muscle, which attaches to the lateral supraepicondylar ridge of the humerus. The radial nerve enters the forearm anterior to the lateral epicondyle of the humerus, just deep to the brachioradialis muscle.
In the arm, the radial nerve has muscular and cutaneous branches (Fig. 7.69).
 Muscular branches include those to the triceps brachii, brachioradialis, and extensor carpi radialis longus muscles. In addition, the radial nerve contributes to the innervation of the lateral part of the brachialis muscle. One of the branches to the medial head of the triceps brachii muscle arises before the radial nerve’s entrance into the posterior compartment and passes vertically down the arm in association with the ulnar nerve.
Muscular branches include those to the triceps brachii, brachioradialis, and extensor carpi radialis longus muscles. In addition, the radial nerve contributes to the innervation of the lateral part of the brachialis muscle. One of the branches to the medial head of the triceps brachii muscle arises before the radial nerve’s entrance into the posterior compartment and passes vertically down the arm in association with the ulnar nerve. Cutaneous branches of the radial nerve that originate in the posterior compartment of the arm are the inferior lateral cutaneous nerve of arm and the posterior cutaneous nerve of forearm, both of which penetrate through the lateral head of the triceps brachii muscle and the overlying deep fascia to become subcutaneous.
Cutaneous branches of the radial nerve that originate in the posterior compartment of the arm are the inferior lateral cutaneous nerve of arm and the posterior cutaneous nerve of forearm, both of which penetrate through the lateral head of the triceps brachii muscle and the overlying deep fascia to become subcutaneous.