Sleep
• Explain the effect that the 24-hour sleep-wake cycle has on biological function.
• Discuss mechanisms that regulate sleep.
• Describe the stages of a normal sleep cycle.
• Explain the functions of sleep.
• Compare and contrast the sleep requirements of different age-groups.
• Identify factors that normally promote and disrupt sleep.
• Discuss characteristics of common sleep disorders.
• Conduct a sleep history for a patient.
• Identify nursing diagnoses appropriate for patients with sleep alterations.
• Identify nursing interventions designed to promote normal sleep cycles for patients of all ages.
http://evolve.elsevier.com/Potter/fundamentals/
Proper rest and sleep are as important to health as good nutrition and adequate exercise. Physical and emotional health depends on the ability to fulfill these basic human needs. Individuals need different amounts of sleep and rest. Without proper amounts, the ability to concentrate, make judgments, and participate in daily activities decreases; and irritability increases.
Identifying and treating patients’ sleep pattern disturbances are important goals. To help patients you need to understand the nature of sleep, the factors influencing it, and patients’ sleep habits. Patients require individualized approaches based on their personal habits, patterns of sleep, and the particular problem influencing sleep. Nursing interventions are often effective in resolving short- and long-term sleep disturbances.
Sleep provides healing and restoration (McCance et al., 2010). Achieving the best possible sleep quality is important for the promotion of good health and recovery from illness. Ill patients often require more sleep and rest than healthy patients. However, the nature of illness often prevents some patients from getting adequate rest and sleep. The environment of a hospital or long-term care facility and the activities of health care personnel make sleep difficult. Some patients have preexisting sleep disturbances; other patients develop sleep problems as a result of illness or hospitalization.
Scientific Knowledge Base
Sleep is a cyclical physiological process that alternates with longer periods of wakefulness. The sleep-wake cycle influences and regulates physiological function and behavioral responses.
Circadian Rhythms
People experience cyclical rhythms as part of their everyday lives. The most familiar rhythm is the 24-hour, day-night cycle known as the diurnal or circadian rhythm (derived from Latin: circa, “about,” and dies, “day”). The suprachiasmatic nucleus (SCN) nerve cells in the hypothalamus control the rhythm of the sleep-wake cycle and coordinate this cycle with other circadian rhythms (McCance et al., 2010). Circadian rhythms influence the pattern of major biological and behavioral functions. The predictable changing of body temperature, heart rate, blood pressure, hormone secretion, sensory acuity, and mood depend on the maintenance of the 24-hour circadian cycle (Van der Zee et al., 2009).
Factors such as light, temperature, social activities, and work routines affect circadian rhythms and daily sleep-wake cycles. All persons have biological clocks that synchronize their sleep cycles. This explains why some people fall asleep at 8 pm, whereas others go to bed at midnight or early in the morning. Different people also function best at different times of the day.
Hospitals or extended care facilities usually do not adapt care to an individual’s sleep-wake cycle preferences. Typical hospital routines interrupt sleep or prevent patients from falling asleep at their usual time. Poor quality of sleep results when a person’s sleep-wake cycle changes. Reversals in the sleep-wake cycle, such as when a person who is normally awake during the day falls asleep during the day, often indicate a serious illness.
The biological rhythm of sleep frequently becomes synchronized with other body functions. For example, changes in body temperature correlate with sleep patterns. Normally body temperature peaks in the afternoon, decreases gradually, and then drops sharply after a person falls asleep. When the sleep-wake cycle becomes disrupted (e.g., by working rotating shifts), other physiological functions usually change as well. For example, a new nurse who starts working the night shift experiences a decreased appetite and loses weight. Anxiety, restlessness, irritability, and impaired judgment are other common symptoms of sleep cycle disturbances. Failure to maintain an individual’s usual sleep-wake cycle negatively influences the patient’s overall health.
Sleep Regulation
Sleep involves a sequence of physiological states maintained by highly integrated central nervous system (CNS) activity. It is associated with changes in the peripheral nervous, endocrine, cardiovascular, respiratory, and muscular systems (McCance et al., 2010). Specific physiological responses and patterns of brain activity identify each sequence. Instruments such as the electroencephalogram (EEG), which measures electrical activity in the cerebral cortex; the electromyogram (EMG), which measures muscle tone; and the electrooculogram (EOG), which measures eye movements provide information about some structural physiological aspects of sleep.
The major sleep center in the body is the hypothalamus. It secretes hypocreatins (orexins) that promote wakefulness and rapid eye movement sleep. Prostaglandin D2, l-tryptophan, and growth factors control sleep (McCance et al., 2010).
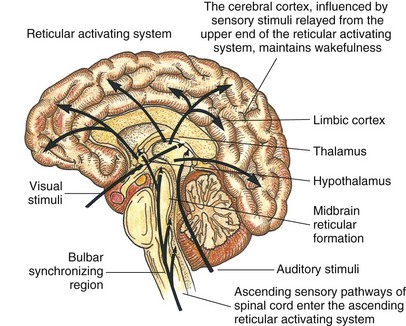
Researchers believe that the ascending reticular activating system (RAS) located in the upper brainstem contains special cells that maintain alertness and wakefulness. The RAS receives visual, auditory, pain, and tactile sensory stimuli. Activity from the cerebral cortex (e.g., emotions or thought processes) also stimulates the RAS. Arousal, wakefulness, and maintenance of consciousness result from neurons in the RAS releasing catecholamines such as norepinephrine (Izac, 2006).
Researchers hypothesize that the release of serotonin from specialized cells in the raphe nuclei sleep system of the pons and medulla produces sleep. This area of the brain is also called the bulbar synchronizing region (BSR). Whether a person remains awake or falls asleep depends on a balance of impulses received from higher centers (e.g., thoughts), peripheral sensory receptors (e.g., sound or light stimuli), and the limbic system (emotions) (Fig. 42-1). As people try to fall asleep, they close their eyes and assume relaxed positions. Stimuli to the RAS decline. If the room is dark and quiet, activation of the RAS further declines. At some point the BSR takes over, causing sleep.
Stages of Sleep
Current theory suggests that sleep is an active multiphase process. Different brain-wave, muscle, and eye activity is associated with different stages of sleep (Izac, 2006). Normal sleep involves two phases: nonrapid eye movement (NREM) sleep and rapid eye movement (REM) sleep (Box 42-1). During NREM a sleeper progresses through four stages during a typical 90-minute sleep cycle. The quality of sleep from stage 1 through stage 4 becomes increasingly deep. Lighter sleep is characteristic of stages 1 and 2, during which a person is more easily aroused. Stages 3 and 4 involve a deeper sleep, called slow-wave sleep. REM sleep is the phase at the end of each sleep cycle. Different factors promote or interfere with various stages of the sleep cycle.
Sleep Cycle
The normal sleep pattern for an adult begins with a presleep period during which the person is aware only of a gradually developing sleepiness. This period normally lasts 10 to 30 minutes; however, if a person has difficulty falling asleep, it lasts an hour or more.
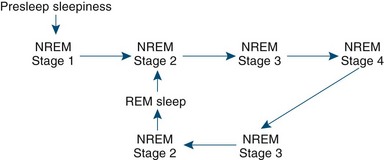
Once asleep, the person usually passes through four or five complete sleep cycles per night, each consisting of four stages of NREM sleep and a period of REM sleep (McCance et al., 2010). Each cycle lasts approximately 90 to 100 minutes. The cyclical pattern usually progresses from stage 1 through stage 4 of NREM, followed by a reversal from stages 4 to 3 to 2, ending with a period of REM sleep (Fig. 42-2). A person usually reaches REM sleep about 90 minutes into the sleep cycle. Seventy-five to eighty percent of sleep time is spent in NREM sleep.
With each successive cycle stages 3 and 4 shorten, and the period of REM lengthens. REM sleep lasts up to 60 minutes during the last sleep cycle. Not all people progress consistently through the stages of sleep. For example, a sleeper moves back and forth for short intervals between NREM stages 2, 3, and 4 before entering REM stage. The amount of time spent in each stage varies over the life span. Newborns and children spend more time in deep sleep. Sleep becomes more fragmented with aging, and a person spends more time in lighter stages (National Sleep Foundation, 2009). Shifts from stage to stage of sleep tend to accompany body movements. Shifts to light sleep or wakefulness tend to occur suddenly, whereas shifts to deep sleep tend to be gradual (Izac, 2006). The number of sleep cycles depends on the total amount of time that the person spends sleeping.
Functions of Sleep
The purpose of sleep remains unclear. It contributes to physiological and psychological restoration. NREM sleep contributes to body tissue restoration (McCance et al., 2010). During NREM sleep biological functions slow. A healthy adult’s normal heart rate throughout the day averages 70 to 80 beats/min or less if the individual is in excellent physical condition. However, during sleep the heart rate falls to 60 beats/min or less, which benefits cardiac function. Other biological functions decreased during sleep are respirations, blood pressure, and muscle tone (McCance et al., 2010).
The body needs sleep to routinely restore biological processes. During deep slow-wave (NREM stage 4) sleep, the body releases human growth hormone for the repair and renewal of epithelial and specialized cells such as brain cells (McCance et al., 2010). Protein synthesis and cell division for renewal of tissues such as the skin, bone marrow, gastric mucosa, or brain occur during rest and sleep. NREM sleep is especially important in children, who experience more stage 4 sleep.
Another theory about the purpose of sleep is that the body conserves energy during sleep. The skeletal muscles relax progressively, and the absence of muscular contraction preserves chemical energy for cellular processes. Lowering of the basal metabolic rate further conserves body energy supply (Izac, 2006).
REM sleep is necessary for brain tissue restoration and appears to be important for cognitive restoration. It is associated with changes in cerebral blood flow, increased cortical activity, increased oxygen consumption, and epinephrine release. This association assists with memory storage and learning (McCance et al., 2010).
The benefits of sleep on behavior often go unnoticed until a person develops a problem resulting from sleep deprivation. A loss of REM sleep leads to feelings of confusion and suspicion. Various body functions (e.g., mood, motor performance, memory, and equilibrium) are altered when prolonged sleep loss occurs (National Sleep Foundation, 2010a). Changes in the natural and cellular immune function also occur with moderate-to-severe sleep deprivation. Traffic, home, and work-related accidents caused by falling asleep cost billions of dollars a year in the United States because of lost productivity, health care costs, and accidents (Irwin et al., 2006).
Dreams
Although dreams occur during both NREM and REM sleep, the dreams of REM sleep are more vivid and elaborate; and some believe that they are functionally important to learning, memory processing, and adaptation to stress (Kryger et al., 2011). REM dreams progress in content throughout the night from dreams about current events to emotional dreams of childhood or the past. Personality influences the quality of dreams (e.g., a creative person has elaborate and complex dreams, whereas a depressed person dreams of helplessness).
Most people dream about immediate concerns such as an argument with a spouse or worries over work. Sometimes a person is unaware of fears represented in bizarre dreams. Clinical psychologists try to analyze the symbolic nature of dreams as part of a patient’s psychotherapy. The ability to describe a dream and interpret its significance sometimes helps resolve personal concerns or fears.
Another theory suggests that dreams erase certain fantasies or nonsensical memories. Because most people forget their dreams, few have dream recall or do not believe they dream at all. To remember a dream, a person has to consciously think about it on awakening. People who recall dreams vividly usually awake just after a period of REM sleep.
Physical Illness
Any illness that causes pain, physical discomfort, or mood problems such as anxiety or depression often results in sleep problems. People with such alterations frequently have trouble falling or staying asleep. Illnesses also force patients to sleep in unfamiliar positions. For example, it is difficult for a patient with an arm or leg in traction to rest comfortably.
Respiratory disease often interferes with sleep. Patients with chronic lung disease such as emphysema are short of breath and frequently cannot sleep without two or three pillows to raise their heads. Asthma, bronchitis, and allergic rhinitis alter the rhythm of breathing and disturb sleep. A person with a common cold has nasal congestion, sinus drainage, and a sore throat, which impair breathing and the ability to relax.
Connections between heart disease, sleep, and sleep disorders exist (Redeker, 2008). Sleep-related breathing disorders are linked to increased incidence of nocturnal angina (chest pain), increased heart rate, electrocardiogram changes, high blood pressure, and risk of heart diseases and stroke (McCance et al., 2010). Hypertension often causes early-morning awakening and fatigue. Hypothyroidism decreases stage 4 sleep, whereas hyperthyroidism causes persons to take more time to fall asleep. Research also identifies an increased risk of sudden cardiac death in the first hours after awakening.
Nocturia, or urination during the night, disrupts sleep and the sleep cycle. After repeated awakenings to urinate, returning to sleep is difficult, and the sleep cycle is not complete. This condition is most common in older people with reduced bladder tone or people with cardiac disease, diabetes, urethritis, or prostatic disease.
Many people experience restless legs syndrome (RLS), which occurs before sleep onset. More common in women, older people, and those with iron deficiency anemia, RLS symptoms include recurrent, rhythmical movements of the feet and legs. Patients feel an itching sensation deep in the muscles. Relief comes only from moving the legs, which prevents relaxation and subsequent sleep. RLS is sometimes a relatively benign condition, depending on how severely sleep is disrupted. Primary RLS is a CNS disorder. Researchers associate secondary RLS with lower levels of iron, pregnancy, and renal failure (Natarajan, 2010).
People with peptic ulcer disease often awaken in the middle of the night. Studies showing a relationship between gastric acid secretion and stages of sleep are conflicting. One consistent finding is that people with duodenal ulcers fail to suppress acid secretion in the first 2 hours of sleep (Kryger et al., 2011).
Sleep Disorders
Sleep disorders are conditions that, if untreated, generally cause disturbed nighttime sleep that results in one of three problems: insomnia, abnormal movements or sensation during sleep or when awakening at night, or excessive daytime sleepiness (Kryger et al., 2011). Many adults in the United States have significant sleep problems from inadequacies in either the quantity or quality of their nighttime sleep and experience hypersomnolence on a daily basis (National Sleep Foundation, 2010a). The American Academy of Sleep Medicine developed the International Classification of Sleep Disorders version 2 (ICSD-2), which classifies sleep disorders into eight major categories (Box 42-2).
The insomnias are disorders related to difficulty falling asleep. Individuals with sleep-related breathing disorders have disordered respirations during sleep. Hypersomnia not caused by sleep-related breathing disorders is a group of disorders that is not caused by disturbed circadian rhythms or nocturnal sleep. The circadian rhythm sleep disorders are caused by a misalignment between the timing of sleep and individual desires or the societal norm. The parasomnias are undesirable behaviors that occur usually during sleep. Sleep and wake disturbances are associated with many medical and psychiatric sleep disorders, including psychiatric, neurological, or other medical disorders. In sleep-related movement disorders the person experiences simple stereotyped movements that disturb sleep. The category of isolated symptoms, apparently normal variants, and unresolved issues includes sleep-related symptoms that fall between normal and abnormal sleep. The other sleep disorders category contains sleep problems that do not fit into other categories.
Sleep laboratory studies diagnose a sleep disorder. A polysomnogram involves the use of EEG, EMG, and EOG to monitor stages of sleep and wakefulness during nighttime sleep. The Multiple Sleep Latency Test (MSLT) provides objective information about sleepiness and selected aspects of sleep structure by measuring eye movements, muscle-tone changes, and brain electrical activity during at least four napping opportunities spread throughout the day. The MSLT takes 8 to 10 hours to complete. Patients wear an Actigraph device on the wrist to measure sleep-wake patterns over an extended period of time. Actigraphy data provide information about sleep time, sleep efficiency, number and duration of awakenings, and levels of activity and rest (Natale et al., 2009).
Insomnia
Insomnia is a symptom that patients experience when they have chronic difficulty falling asleep, frequent awakenings from sleep, and/or a short sleep or nonrestorative sleep (Kryger et al., 2011). It is the most common sleep-related complaint. People with insomnia experience excessive daytime sleepiness and insufficient sleep quantity and quality. However, frequently a patient gets more sleep than he or she realizes. Insomnia often signals an underlying physical or psychological disorder. It occurs more frequently in and is the most common sleep problem for women.
People experience transient insomnia as a result of situational stresses such as family, work, or school problems; jet lag; illness; or loss of a loved one. Insomnia sometimes recurs, but between episodes a patient is able to sleep well. However, a temporary case of insomnia caused by a stressful situation can lead to chronic difficulty in getting enough sleep, perhaps because of the worry and anxiety that develop about getting it.
Insomnia is often associated with poor sleep hygiene, or practices that a patient associates with sleep. If the condition continues, the fear of not being able to sleep is enough to cause wakefulness. During the day people with chronic insomnia feel sleepy, fatigued, depressed, and anxious. Treatment is symptomatic, including improved sleep hygiene measures, biofeedback, cognitive techniques, and relaxation techniques. Behavioral and cognitive therapies have few adverse effects and show evidence of sustained improvement in sleep over time (Babson et al., 2010).
Sleep Apnea
Sleep apnea is a disorder characterized by the lack of airflow through the nose and mouth for periods of 10 seconds or longer during sleep. There are three types of sleep apnea: central, obstructive, and mixed apnea. The most common form is obstructive sleep apnea (OSA). Research estimates that 2% to 4% of the adults in the United States meet the diagnostic criteria for OSA (Adult Obstructive Sleep Apnea Task Force, 2009). The two major risk factors for OSA are obesity and hypertension (Sheldon et al., 2009). Smoking, heart failure, type II diabetes, alcohol, and a positive family history of OSA also greatly increase the risk of developing the problem (Adult Obstructive Sleep Apnea Task Force, 2009). It occurs in up to 2% of middle-age women and up to 4% of middle-age men, with occurrence higher in the older-adult population and African Americans (Malhotra and Desai, 2010).
OSA occurs when muscles or structures of the oral cavity or throat relax during sleep. The upper airway becomes partially or completely blocked, diminishing nasal airflow (hypopnea) or stopping it (apnea) for as long as 30 seconds (Kryger et al., 2011). The person still attempts to breathe because chest and abdominal movement continue, which often results in loud snoring and snorting sounds. When breathing is partially or completely diminished, each successive diaphragmatic movement becomes stronger until the obstruction is relieved. Structural abnormalities such as a deviated septum, nasal polyps, certain jaw configurations, larger neck circumference, or enlarged tonsils predispose a patient to OSA (Pinto and Caple, 2010). The effort to breathe during sleep results in arousals from deep sleep often to the stage 2 cycle. In severe cases hundreds of hypopnea/apnea episodes occur every hour, resulting in severe interference with deep sleep.
Excessive daytime sleepiness (EDS) and fatigue are the most common complaints of people with OSA. Persons with severe OSA often report taking daytime naps and experience a disruption in their daily activities because of sleepiness (Adult Obstructive Sleep Apnea Task Force, 2009). Feelings of sleepiness are usually most intense on awakening, right before going to sleep, and about 12 hours after the midsleep period. EDS often results in impaired waking function, poor work or school performance, accidents while driving or using equipment, and behavioral or emotional problems.
Obstructive apnea causes a serious decline in arterial oxygen saturation level. Patients are at risk for cardiac dysrhythmias, right heart failure, pulmonary hypertension, angina attacks, stroke, and hypertension. Sleep apnea contributes to high blood pressure and increased risk for heart attack and stroke (National Sleep Foundation, 2010b).
Central sleep apnea (CSA) involves dysfunction in the respiratory control center of the brain. The impulse to breathe fails temporarily, and nasal airflow and chest wall movement cease. The oxygen saturation of the blood falls. The condition is common in patients with brainstem injury, muscular dystrophy, and encephalitis. Less than 10% of sleep apnea is predominantly central in origin. People with CSA tend to awaken during sleep and therefore complain of insomnia and EDS. Mild and intermittent snoring is also present.
Patients with sleep apnea rarely achieve deep sleep. In addition to complaints of EDS, sleep attacks, fatigue, morning headaches, irritability, depression, difficulty concentrating, and decreased sex drive are common (Kryger et al., 2011). OSA affects quality of life issues such as marital relationships and interactions within and outside the family and often is an embarrassment to a patient (Adult Obstructive Sleep Apnea Task Force, 2009). Treatment includes therapy for underlying cardiac or respiratory complications and emotional problems that occur as a result of the symptoms of this disorder.
Narcolepsy
Narcolepsy is a dysfunction of mechanisms that regulate sleep and wake states. Excessive daytime sleepiness is the most common complaint associated with this disorder. During the day a person suddenly feels an overwhelming wave of sleepiness and falls asleep; REM sleep occurs within 15 minutes of falling asleep. Cataplexy, or sudden muscle weakness during intense emotions such as anger, sadness, or laughter, occurs at any time during the day. If the cataplectic attack is severe, a patient loses voluntary muscle control and falls to the floor. A person with narcolepsy often has vivid dreams that occur as he or she is falling asleep. These dreams are difficult to distinguish from reality. Sleep paralysis, or the feeling of being unable to move or talk just before waking or falling asleep, is another symptom. Some studies show a genetic link for narcolepsy (Ahmed and Thorpy, 2010).
A person with narcolepsy falls asleep uncontrollably at inappropriate times. When individuals do not understand this disorder, a sleep attack is easily mistaken for laziness, lack of interest in activities, or drunkenness. Typically the symptoms first begin to appear in adolescence and are often confused with the EDS that commonly occurs in teens. Narcoleptic patients are treated with stimulants or wakefulness-promoting agents such as sodium oxybate, modafinil (Provigil) or armodafinil (Nuvigil) that only partially increase wakefulness and reduce sleep attacks. Patients also receive antidepressant medications that suppress cataplexy and the other REM-related symptoms. Brief daytime naps no longer than 20 minutes help reduce subjective feelings of sleepiness. Other management methods that help are following a regular exercise program, practicing good sleep habits, avoiding shifts in sleep, strategically timed daytime naps if possible, eating light meals high in protein, practicing deep breathing, chewing gum, and taking vitamins (Kryger et al., 2011). Patients with narcolepsy need to avoid factors that increase drowsiness (e.g., alcohol; heavy meals; exhausting activities; long-distance driving; and long periods of sitting in hot, stuffy rooms).
Sleep Deprivation
Sleep deprivation is a problem many patients experience as a result of dyssomnia. Causes include symptoms (e.g., fever, difficulty breathing, or pain) caused by illnesses, emotional stress, medications, environmental disturbances (e.g., frequent nursing care), and variability in the timing of sleep because of shift work. Physicians and nurses are particularly prone to sleep deprivation as a result of long work schedules and rotating shifts. Chronic sleep deprivation is associated with development of cardiovascular disease, weight gain, type II diabetes, poor memory, depression, and digestive problems (Ohlmann and O’Sullivan, 2009).
Hospitalization, especially in intensive care units (ICUs), makes patients particularly vulnerable to the extrinsic and circadian sleep disorders that cause the “ICU syndrome of sleep deprivation” (Fontana and Pittiglio, 2010). Constant environmental stimuli within the ICU such as strange noises from equipment, the frequent monitoring and care given by nurses, and ever-present lights confuse patients. Repeated environmental stimuli and the patient’s poor physical status lead to sleep deprivation (Fontana and Pittiglio, 2010).
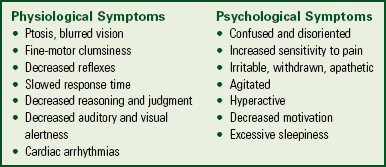
A person’s response to sleep deprivation is highly variable. Patients experience a variety of physiological and psychological symptoms (Box 42-3). The severity of symptoms is often related to the duration of sleep deprivation.
Parasomnias
The parasomnias are sleep problems that are more common in children than adults. Some have hypothesized that sudden infant death syndrome (SIDS) is thought to be related to apnea, hypoxia, and cardiac arrhythmias caused by abnormalities in the autonomic nervous system that are manifested during sleep (Kryger et al., 2011). Because of an association between the prone position and the occurrence of SIDS, the American Academy of Pediatrics recommends that parents place apparently healthy infants in the supine position during sleep (Koren et al., 2010).
Parasomnias that occur among older children include somnambulism (sleepwalking), night terrors, nightmares, nocturnal enuresis (bed-wetting), body rocking, and bruxism (teeth grinding). When adults have these problems, it often indicates more serious disorders. Specific treatment varies. However, in all cases it is important to support patients and maintain their safety.
Nursing Knowledge Base
When people are at rest, they usually feel mentally relaxed, free from anxiety, and physically calm. Rest does not imply inactivity, although everyone often thinks of it as settling down in a comfortable chair or lying in bed. When people are at rest, they are in a state of mental, physical, and spiritual activity that leaves them feeling refreshed, rejuvenated, and ready to resume the activities of the day. People have their own habits for obtaining rest and can find ways to adjust to new environments or conditions that affect the ability to rest. They rest by reading a book, practicing a relaxation exercise, listening to music, taking a long walk, or sitting quietly.
Illness and unfamiliar health care routines easily affect the usual rest and sleep patterns of people entering a hospital or other health care facility. Nurses frequently care for patients who are on bed rest to reduce physical and psychological demands on the body in a variety of health care settings. However, these people do not necessarily feel rested. Some still have emotional worries that prevent complete relaxation. For example, concern over physical limitations or a fear of being unable to return to their usual lifestyle causes such patients to feel stressed and unable to relax. You must always be aware of a patient’s need for rest. A lack of rest for long periods causes illness or worsening of existing illness.
Normal Sleep Requirements and Patterns
Sleep duration and quality vary among people of all age-groups. For example, one person feels adequately rested with 4 hours of sleep, whereas another requires 10 hours. Nurses play an important role in identifying treatable sleep-deprivation problems.
Neonates
The neonate up to the age of 3 months averages about 16 hours of sleep a day, sleeping almost constantly during the first week. The sleep cycle is generally 40 to 50 minutes with wakening occurring after one to two sleep cycles. Approximately 50% of this sleep is REM sleep, which stimulates the higher brain centers. This is essential for development because the neonate is not awake long enough for significant external stimulation.
Infants
Infants usually develop a nighttime pattern of sleep by 3 months of age. The infant normally takes several naps during the day but usually sleeps an average of 8 to 10 hours during the night for a total daily sleep time of 15 hours. About 30% of sleep time is in the REM cycle. Awakening commonly occurs early in the morning, although it is not unusual for an infant to awaken during the night.
Toddlers
By the age of 2 children usually sleep through the night and take daily naps. Total sleep averages 12 hours a day. After 3 years of age children often give up daytime naps (Hockenberry and Wilson, 2011). It is common for toddlers to awaken during the night. The percentage of REM sleep continues to fall. During this period toddlers may be unwilling to go to bed at night because they need autonomy or fear separation from their parents.
Preschoolers
On average a preschooler sleeps about 12 hours a night (about 20% is REM). By the age of 5 he or she rarely takes daytime naps except in cultures in which a siesta is the custom (Hockenberry and Wilson, 2011). The preschooler usually has difficulty relaxing or quieting down after long, active days and has bedtime fears, awakens during the night, or has nightmares. Partial awakening followed by normal return to sleep is frequent (Hockenberry and Wilson, 2011). In the awake period the child exhibits brief crying, walking around, unintelligible speech, sleepwalking, or bed-wetting.
School-Age Children
The amount of sleep needed varies during the school years. A 6-year-old averages 11 to 12 hours of sleep nightly, whereas an 11-year-old sleeps about 9 to 10 hours (Hockenberry and Wilson, 2011). The 6- or 7-year-old usually goes to bed with some encouragement or by doing quiet activities. The older child often resists sleeping because he or she is unaware of fatigue or has a need to be independent.
Adolescents
On average teenagers get about  hours of sleep per night. The typical adolescent is subject to a number of changes such as school demands, after-school social activities, and part-time jobs, which reduce the time spent sleeping (Noland et al., 2009). Shortened sleep time often results in EDS, which frequently leads to reduced performance in school, vulnerability to accidents, behavior and mood problems, and increased use of alcohol (Noland et al., 2009; Vallido et al., 2009).
hours of sleep per night. The typical adolescent is subject to a number of changes such as school demands, after-school social activities, and part-time jobs, which reduce the time spent sleeping (Noland et al., 2009). Shortened sleep time often results in EDS, which frequently leads to reduced performance in school, vulnerability to accidents, behavior and mood problems, and increased use of alcohol (Noland et al., 2009; Vallido et al., 2009).
Young Adults
Most young adults average 6 to  hours of sleep a night. Approximately 20% of sleep time is REM sleep, which remains consistent throughout life. It is common for the stresses of jobs, family relationships, and social activities to frequently lead to insomnia and the use of sleep medication. Daytime sleepiness contributes to an increased number of accidents, decreased productivity, and interpersonal problems in this age-group. Pregnancy increases the need for sleep and rest. Insomnia, periodic limb movements, RLS, and sleep-disordered breathing are common problems during the third trimester of pregnancy (Kryger et al., 2011).
hours of sleep a night. Approximately 20% of sleep time is REM sleep, which remains consistent throughout life. It is common for the stresses of jobs, family relationships, and social activities to frequently lead to insomnia and the use of sleep medication. Daytime sleepiness contributes to an increased number of accidents, decreased productivity, and interpersonal problems in this age-group. Pregnancy increases the need for sleep and rest. Insomnia, periodic limb movements, RLS, and sleep-disordered breathing are common problems during the third trimester of pregnancy (Kryger et al., 2011).
Middle Adults
During middle adulthood the total time spent sleeping at night begins to decline. The amount of stage 4 sleep begins to fall, a decline that continues with advancing age. Insomnia is particularly common, probably because of the changes and stresses of middle age. Anxiety, depression, or certain physical illnesses cause sleep disturbances. Women experiencing menopausal symptoms often experience insomnia.
Older Adults
Complaints of sleeping difficulties increase with age. More than 50% of older adults report sleep problems (Neikrug and Ancoli-Israel, 2010). Older adults experience weakening, desynchronized circadian rhythms that alter the sleep-wake cycle (Neikrug and Ancoli-Israel, 2010). Episodes of REM sleep tend to shorten. There is a progressive decrease in stages 3 and 4 NREM sleep; some older adults have almost no stage 4, or deep sleep. An older adult awakens more often during the night, and it takes more time for him or her to fall asleep. The tendency to nap seems to increase progressively with age because of the frequent awakenings experienced at night.
The presence of chronic illness often results in sleep disturbances for the older adult. For example, an older adult with arthritis frequently has difficulty sleeping because of painful joints. Changes in sleep pattern are often caused by changes in the CNS that affect the regulation of sleep. Sensory impairment reduces an older person’s sensitivity to time cues that maintain circadian rhythms.
Factors Influencing Sleep
A number of factors affect the quantity and quality of sleep. Often a single factor is not the only cause for a sleep problem. Physiological, psychological, and environmental factors frequently alter the quality and quantity of sleep.
Drugs and Substances
Sleepiness, insomnia, and fatigue often result as a direct effect of commonly prescribed medications (Box 42-4). These medications alter sleep and weaken daytime alertness, which is problematic (Kryger et al., 2011). Medications prescribed for sleep often cause more problems than benefits. Older adults take a variety of drugs to control or treat chronic illness, and the combined effects of their drugs often seriously disrupt sleep. Some substances such as l-tryptophan, a natural protein found in foods such as milk, cheese, and meats, promote sleep.
Lifestyle
A person’s daily routine influences sleep patterns. An individual working a rotating shift (e.g., 2 weeks of days followed by a week of nights) often has difficulty adjusting to the altered sleep schedule. For example, the body’s internal clock is set at 11 pm, but the work schedule forces sleep at 9 am instead. The individual is able to sleep only 3 or 4 hours because his or her body clock perceives that it is time to be awake and active. Difficulties maintaining alertness during work time result in decreased and even hazardous performance. After several weeks of working a night shift, a person’s biological clock usually does adjust. Other alterations in routines that disrupt sleep patterns include performing unaccustomed heavy work, engaging in late-night social activities, and changing evening mealtime.
Usual Sleep Patterns
In the past century the amount of sleep obtained nightly by U.S. citizens has decreased to about 6.7 hours per night, causing many Americans to be sleep deprived and experience excessive sleepiness during the day (Ohlmann and O’Sullivan, 2009). Sleepiness becomes pathological when it occurs at times when individuals need or want to be awake. People who experience temporary sleep deprivation as a result of an active social evening or lengthened work schedule usually feel sleepy the next day. However, they are able to overcome these feelings even though they have difficulty performing tasks and remaining attentive. Chronic lack of sleep is much more serious and causes serious alterations in the ability to perform daily functions. Sleepiness tends to be most difficult to overcome during sedentary (inactive) tasks such as driving. There is an increased risk of motor vehicle accidents if an individual drives after less than 7 hours of sleep (Heaton et al., 2009).
Emotional Stress
Worry over personal problems or a situation frequently disrupts sleep. Emotional stress causes a person to be tense and often leads to frustration when sleep does not occur. Stress also causes a person to try too hard to fall asleep, to awaken frequently during the sleep cycle, or to oversleep. Continued stress causes poor sleep habits.
Older patients frequently experience losses that lead to emotional stress such as retirement, physical impairment, or the death of a loved one. Older adults and other individuals who experience depressive mood problems experience delays in falling asleep, earlier appearance of REM sleep, frequent or early awakening, feelings of sleeping poorly, and daytime sleepiness (National Sleep Foundation, 2010c).
Environment
The physical environment in which a person sleeps significantly influences the ability to fall and remain sleep. Good ventilation is essential for restful sleep. The size, firmness, and position of the bed affect the quality of sleep. If a person usually sleeps with another individual, sleeping alone often causes wakefulness. On the other hand, sleeping with a restless or snoring bed partner disrupts sleep.
In hospitals and other inpatient facilities noise creates a problem for patients. Noise in hospitals is usually new or strange and often loud. Thus patients wake easily. This problem is greatest the first night of hospitalization, when patients often experience increased total wake time, increased awakenings, and decreased REM sleep and total sleep time. People-induced noises (e.g., nursing activities) are sources of increased sound levels. ICUs are sources of high noise levels because of staff, monitor alarms, and equipment. Close proximity of patients, noise from confused and ill patients, ringing alarm systems and telephones, and disturbances caused by emergencies make the environment unpleasant. Noise causes increased agitation; delayed healing; impaired immune function; and increased blood pressure, heart rate, and stress (Dennis et al., 2010).
Light levels affect the ability to fall asleep. Some patients prefer a dark room, whereas others such as children or older adults prefer keeping a soft light on during sleep. Patients also have trouble sleeping because of the room temperature. A room that is too warm or too cold often causes a patient to become restless.
Exercise and Fatigue
A person who is moderately fatigued usually achieves restful sleep, especially if the fatigue is the result of enjoyable work or exercise. Exercising 2 hours or more before bedtime allows the body to cool down and maintain a state of fatigue that promotes relaxation. However, excess fatigue resulting from exhausting or stressful work makes falling asleep difficult. This is often seen in grade-school children and adolescents who keep stressful, long schedules because of school, social activities, and work.
Food and Caloric Intake
Following good eating habits is important for proper sleep. Eating a large, heavy, and/or spicy meal at night often results in indigestion that interferes with sleep. Caffeine, alcohol, and nicotine consumed in the evening produce insomnia. Coffee, tea, cola, and chocolate contain caffeine and xanthines that cause sleeplessness. Thus drastically reducing or avoiding these substances can improve sleep. Some food allergies cause insomnia. A milk allergy sometimes causes nighttime waking and crying or colic in infants.
Weight loss or gain influences sleep patterns. Weight gain contributes to OSA because of increased size of the soft tissue structures in the upper airway (Kryger et al., 2011). Weight loss causes insomnia and decreased amounts of sleep (Benca and Schneck, 2005). Certain sleep disorders are the result of the semi-starvation diets popular in a weight-conscious society.
Critical Thinking
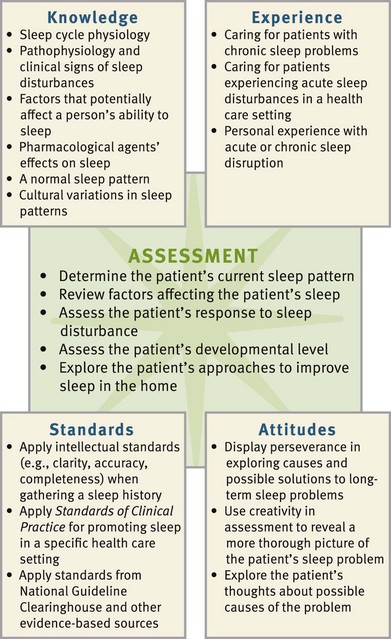
Successful critical thinking requires a synthesis of knowledge, including information gathered from patients, experience, critical thinking attitudes, and intellectual and professional standards. Clinical judgments require you to anticipate the information necessary, analyze the data, and make decisions regarding patient care. You adapt critical thinking to the changing needs of the patient. During assessment (Fig. 42-3) consider all elements to make appropriate nursing diagnoses.
In the case of sleep, integrate knowledge from nursing and disciplines such as pharmacology and psychology. Personal experience with a sleep problem and experience with patients prepares you to know effective forms of sleep therapies. You use critical thinking attitudes such as perseverance, confidence, and discipline to complete a comprehensive assessment and develop a plan of care to provide successful management of the sleep problem. Professional standards such as the Nursing Scope and Standards of Practice (American Nurses Association, 2010), Clinical Guidelines for the Evaluation and Management of Chronic Insomnia (National Guideline Clearinghouse, 2008) and “Excessive Sleepiness” in Evidence-based Geriatrics Nursing Protocols for Best Practice (Chasens et al., 2008) provide valuable guidelines to assess and address the needs of patients with sleep disorders.
Nursing Process
Apply the nursing process and use a critical thinking approach in the care of patients. The nursing process provides a clinical decision-making approach for you to develop and implement an individualized plan of care.
Assessment
During the assessment process, thoroughly assess each patient and critically analyze findings to ensure that you make patient-centered clinical decisions required for safe nursing care.
Through the Patient’s Eyes
Assess patients’ sleep patterns by using a nursing history to gather information about factors that usually influence sleep. Sleep is a subjective experience. Only the patient is able to report whether or not it is sufficient and restful. If the patient is satisfied with the quantity and quality of sleep received, you consider it normal, and the nursing history is brief. If a patient admits to or suspects a sleep problem, you need a detailed history and assessment. If a patient has an obvious sleep problem, consider asking if his or her sleep partner can be approached for further assessment data.
A poor night’s sleep for a patient often starts a vicious cycle of anticipatory anxiety. The patient fears that sleep will again be disturbed while trying harder and harder to sleep. Use a skilled and caring approach to assess the patient’s sleep needs. A caring nurse individualizes care for each patient. Always ask patients what they expect regarding sleep. This includes asking about the interventions that they currently use and how successful they are. It is important to understand patients’ expectations regarding their sleep pattern. When patients ask for assistance because of sleep disturbances, they typically expect a nurse to respond promptly to help them improve the quantity and quality of their sleep.
Sleep Assessment
Most persons are able to provide a reasonably accurate estimate of their sleep patterns, particularly if any changes have occurred. Aim your assessment at understanding the characteristics of the patient’s sleep problem and usual sleep habits so you incorporate ways for promoting sleep into nursing care. For example, if the nursing history reveals that a patient always reads before falling asleep, it makes sense to offer reading material at bedtime.
Sources for Sleep Assessment: Usually patients are the best resource for describing sleep problems and how they are a change from their usual sleep and waking patterns. Often the patient knows the cause for sleep problems such as a noisy environment or worry over a relationship.
In addition, bed partners are able to provide information about patients’ sleep patterns that help reveal the nature of certain sleep disorders. For example, partners of patients with sleep apnea often complain that the patient’s snoring disturbs their sleep. Often the partners must sleep in different beds or rooms to obtain adequate sleep. Ask bed partners (if the patient agrees) whether patients have breathing pauses during sleep and how frequently the apneic attacks occur. Some partners mention becoming fearful when patients apparently stop breathing for periods.
When caring for children, seek information about sleep patterns from parents or guardians because they are usually a reliable source of information. Hunger, excessive warmth, and separation anxiety often contribute to an infant’s difficulty going to sleep or frequent awakenings during the night. Parents of infants need to keep a 24-hour log of their infant’s waking and sleeping behavior for several days to determine the cause of the problem. They also need to describe the infant’s eating pattern and sleeping environment because these influence sleeping behavior. Older children often are able to relate fears or worries that inhibit their ability to fall asleep. If children frequently awaken in the middle of bad dreams, parents are able to identify the problem but perhaps do not understand the meaning of the dreams. Ask parents to describe the typical behavior patterns that foster or impair sleep. For example, excessive stimulation from active play or visiting friends predictably impairs sleep. With chronic sleep problems, parents need to relate the duration of the problem, its progression, and children’s responses.
Tools for Sleep Assessment: Two effective subjective measures of sleep are the Epworth Sleepiness Scale and the Pittsburgh Sleep Quality Index. The Epworth Sleepiness Scale evaluates the severity of EDS (Chasens et al., 2008). The Pittsburgh Sleep Quality Index assesses sleep quality and sleep patterns (Smyth, 2008). Another effective, brief method for assessing sleep quality is the use of a visual analogue scale (Lashley, 2004). Draw a straight horizontal line 100 mm (4 inches) long. Opposing statements such as “best night’s sleep” and “worst night’s sleep” are at opposite ends of the line. Ask patients to place a mark on the horizontal line at the point corresponding to their perceptions of the previous night’s sleep. Measuring the distances of the mark along the line in millimeters offers a numerical value for satisfaction with sleep. Use the scale repeatedly to show change over time. Such a scale is useful to assess an individual patient, not to compare patients.
Another brief subjective method to assess sleep is a numeric scale with a 0-to-10 sleep rating (Lashley, 2004). Ask individuals to separately rate the quantity and quality of their sleep on the scale. Instruct them to indicate with a number between 0 and 10 their sleep quantity and then their quality of sleep, with 0 being the worst sleep and 10 being the best.
Sleep History
When a patient reports having adequate sleep, a sleep history is usually brief. A determination of usual bedtime, normal bedtime rituals, preferred environment for sleeping, and what time the patient usually rises gives you information for planning care conducive to sleep. When suspecting a sleep problem, assess the quality and characteristics of sleep in greater depth by asking the patient to describe the problem. This includes recent changes in sleep pattern, sleep symptoms experienced during waking hours, use of sleep and other prescribed or over-the-counter medications, diet and intake of substances such as caffeine or alcohol that influence sleep, and recent life events that have affected the patient’s mental and emotional status.
Description of Sleeping Problems: Conduct a more detailed history when a patient has a sleep problem. This ensures that you provide appropriate therapeutic care. Open-ended questions help a patient describe a problem more fully. A general description of the problem followed by more focused questions usually reveals specific characteristics that are useful in planning therapies. To begin, you need to understand the nature of the sleep problem, its signs and symptoms, its onset and duration, its severity, any predisposing factors or causes, and the overall effect on the patient. Ask specific questions related to the sleep problem (Box 42-5).
Proper questioning helps to determine the type of sleep disturbance and the nature of the problem. Box 42-6 gives examples of additional questions for you to ask a patient when you suspect specific sleep disorders. The questions assist in selecting specific sleep therapies and the best time for implementation.
As an adjunct to the sleep history, have the patient and bed partner keep a sleep-wake log for 1 to 4 weeks (Cuellar et al., 2007). The patient completes the sleep-wake log daily to provide information on day-to-day variations in sleep-wake patterns over extended periods. Entries in the log often include 24-hour information about various waking and sleeping health behaviors such as physical activities, mealtimes, type and amount of intake (alcohol and caffeine), time and length of daytime naps, evening and bedtime routines, the time the patient tries to fall asleep, nighttime awakenings, and the time of morning awakening. A partner helps record the estimated times the patient falls asleep or awakens. Although the log is helpful, the patient needs to be motivated to participate in its completion.
Usual Sleep Pattern: Normal sleep is difficult to define because individuals vary in their perception of adequate quantity and quality of sleep. However, it is important to have patients describe their usual sleep pattern to determine the significance of the changes caused by a sleep disorder. Knowing a patient’s usual, preferred sleep pattern allows you to try to match sleeping conditions in a health care setting with those in the home. Ask the following questions to determine a patient’s sleep pattern:
1. What time do you usually get in bed each night?
2. How much time does it usually take to fall asleep? Do you do anything special to help you fall asleep?
3. How many times do you awaken during the night? Why?
Compare patient data with their pattern before the sleep problem or with the predominant pattern usually found for other patients of the same age. On the basis of this comparison, you begin to assess for identifiable patterns such as insomnia.
Patients with sleep problems frequently show patterns drastically different from their usual one, or sometimes the change is relatively minor. Hospitalized patients usually need or want more sleep as a result of illness. However, some require less sleep because they are less active. Some patients who are ill think that it is important to try to sleep more than usual, eventually making sleeping difficult.
Physical and Psychological Illness: Determine whether the patient has any preexisting health problems that interfere with sleep. A history of psychiatric problems also makes a difference. For example, a patient who is living with bipolar disorder sleeps more when depressed than when manic. A patient who is depressed often experiences an inadequate amount of fragmented sleep. Chronic diseases such as chronic obstructive pulmonary disease and painful disorders such as arthritis interfere with sleep. Also assess the patient’s medication history, including a description of over-the-counter and prescribed drugs. If a patient takes medications to aid sleep, gather information about the type and amount of medication and frequency used. Also assess the patient’s daily caffeine intake.
If the patient has recently had surgery, expect him or her to experience some sleep disturbance. Patients usually awaken frequently during the first night after surgery and receive little deep or REM sleep. Depending on the type of surgery, it takes several days to months for a normal sleep cycle to return.
Current Life Events: In your assessment learn if the patient is experiencing any changes in lifestyle that disrupt sleep. A person’s occupation often offers a clue to the nature of the sleep problem. Changes in job responsibilities, rotating shifts, or long hours contribute to a sleep disturbance. Questions about social activities, recent travel, or mealtime schedules help clarify the assessment.
Emotional and Mental Status: A patient’s emotions and mental status affect the ability to sleep. For example, if a patient is experiencing anxiety, emotional stress related to illness, or situational crises such as loss of job or a loved one, he or she often experiences insomnia. When a sleep disturbance is related to an emotional problem, the key is to treat the primary problem; its resolution often improves sleep (Ramakrishnan and Scheid, 2007). Patients with mental illnesses may need mild sedation for adequate rest. Assess the effectiveness of any medication and its effect on daytime function.
Bedtime Routines: Ask patients what they do to prepare for sleep. For example, some patients drink a glass of milk, take a sleeping pill, eat a snack, or watch television. Assess habits that are beneficial compared with those that disturb sleep. For example, watching television promotes sleep for one person, whereas it stimulates another to stay awake. Sometimes pointing out that a particular habit is interfering with sleep helps patients find ways to change or eliminate habits that are disrupting sleep.
Pay special attention to a child’s bedtime rituals. For example, the parents need to report whether it is necessary to read a bedtime story, rock the child to sleep, or engage in quiet play. Some young children need a special blanket or stuffed animal when going to sleep.
Bedtime Environment: During assessment ask the patient to describe preferred bedroom conditions, including preferences for lighting in the room, music or television in the background, or needing to have the door open versus closed. In addition, some children need the company of a parent to fall asleep. In a health care environment environmental distractions such as a roommate’s television, an electronic monitor in the hallway, a noisy nurses’ station, or another patient who cries out at night often interfere with sleep. Identify factors to reduce or control the environment.
Behaviors of Sleep Deprivation: Some patients are unaware of how their sleep problems are affecting their behavior. Observe for behaviors such as irritability, disorientation (similar to a drunken state), frequent yawning, and slurred speech. If sleep deprivation has lasted a long time, psychotic behavior such as delusions and paranoia sometimes develop. For example, a patient reports seeing strange objects or colors in the room, or he or she acts afraid when the nurse enters the room.
Nursing Diagnosis
Review your assessment data, looking for clusters of data that include defining characteristics for a sleep pattern disturbance or other health problem. If you identify a sleep problem, specify the condition, such as insomnia or sleep deprivation. By specifying the sleep disturbance diagnosis, you are able to design more effective interventions. For example, you choose different therapies for patients with insomnia who are unable to fall asleep than for those with sleep deprivation. Box 42-7 demonstrates how to use nursing assessment activities to identify and cluster defining characteristics to make an accurate nursing diagnosis.
Assessment also identifies the related factor or probable cause of a sleep disturbance such as a noisy environment or a high intake of caffeinated beverages in the evening. These causes become the focus of interventions for minimizing or eliminating the problem. For example, if a patient is experiencing insomnia as a result of a noisy health care environment, offer some basic recommendations for helping sleep such as controlling the noise of hospital equipment, reducing interruptions, or keeping doors closed. If the insomnia is related to worry over a threatened marital separation, introduce coping strategies and create an environment for sleep. If you incorrectly define the probable cause or related factors, the patient does not benefit from care.
Sleep problems affect patients in other ways. For example, you find that a patient with sleep apnea has problems with a spouse who is tired and frustrated over the patient’s snoring. In addition, the spouse is concerned that the patient is breathing improperly and thus is in danger. The nursing diagnosis of compromised family coping indicates that you need to provide support to the patient and spouse so they understand sleep apnea and obtain the medical treatment needed. Examples of nursing diagnoses for patients with sleep problems include the following:
Planning
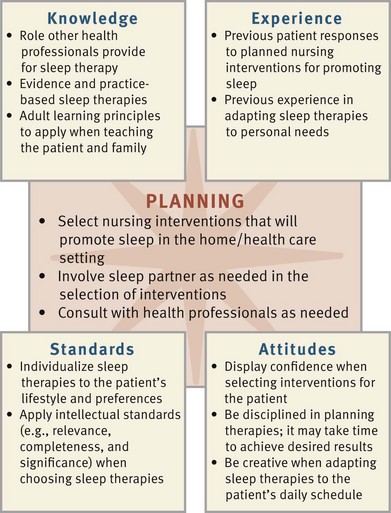
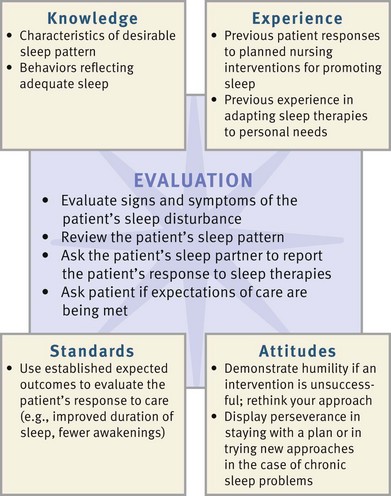
During planning you again synthesize information from multiple resources to develop an individualized plan of care (Fig. 42-4) (see the Nursing Care Plan). Professional standards are especially important to consider in developing a care plan. These standards often offer evidence-based guidelines for effective nursing interventions. For example, the Evidence-based Geriatrics Protocol for Best Practice (Chasens et al., 2008) titled “Excessive Sleepiness” recommends individualized nursing interventions that maintain and support an older adult’s normal sleep pattern and bedtime ritual. It is important for a plan of care for sleep promotion to include strategies appropriate to the patient’s sleep routines, living environment, and lifestyle.
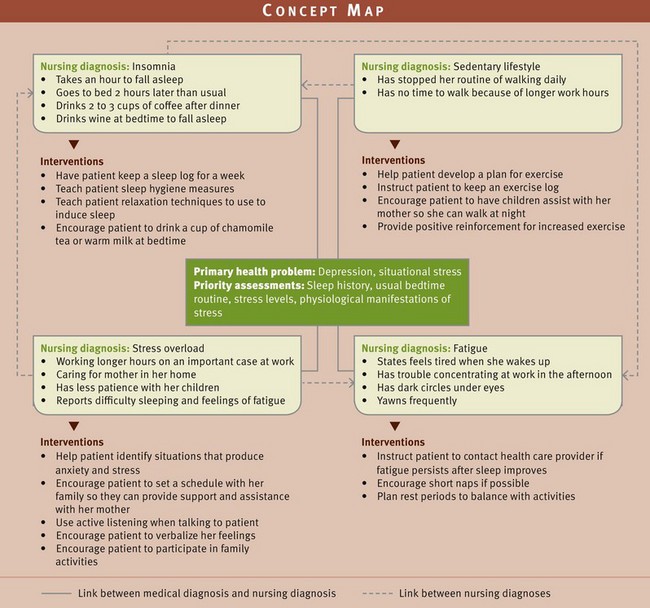
As you plan care for a patient with sleep disturbances, creation of a concept map is another method for developing holistic patient-centered care (Fig. 42-5 on p. 953). Create the map after identifying relevant nursing diagnoses from the assessment database. In this example the nursing diagnoses are linked to the patient’s medical diagnosis of depression and situational stress. The concept map shows the relationships among the nursing diagnoses insomnia, stress overload, sedentary lifestyle, and readiness for enhanced sleep. This approach to planning care helps the nurse recognize relationships among planned interventions. For this patient, interventions and successful outcomes for one nursing diagnosis affect the resolution of another nursing diagnosis.
When developing goals and outcomes, it is important for a nurse and patient to collaborate. As a result, you are more likely to set realistic goals and measurable outcomes with your patients. An effective plan includes outcomes established over a realistic time frame that focus on the goal of improving the quantity and quality of sleep in the home. Often family members are very helpful in contributing to the plan. A sleep-promotion plan frequently requires many weeks to accomplish. The following is an example of a goal with patient outcomes:
Goal: The patient will control environmental sources disrupting sleep within 1 month.
• Patient will identify factors in the immediate home environment that disrupt sleep in 2 weeks.
• Patient will report having a discussion with family members about environmental barriers to sleep in 2 weeks.
• Patient will report changes made in the bedroom to promote sleep within 4 weeks.
• Patient will report having fewer than two awakenings per night within 4 weeks.
Setting Priorities
Work with patients to establish priority outcomes and interventions. Frequently sleep disturbances are the result of other health problems. For example, when physical symptoms are interfering with sleep, managing the symptoms is your first priority. After symptoms are relieved, focus on sleep therapies. Patients are a helpful resource in determining which interventions hold priority. For example, once patients understand the factors that disrupt sleep, they make choices about the types of changes they would like to make in their lifestyle or sleeping environment.
Teamwork and Collaboration
Partner closely with the patient and sleep partner to ensure that any therapies such as a change in the sleep schedule or changes to the bedroom environment are realistic and achievable. In a health care setting plan treatments or routines so the patient is able to rest. For example, in the ICU use available electronic monitors to track trends in vital signs without awakening a patient each hour. Other staff members need to be aware of the care plan so they can cluster activities at certain times to reduce awakenings. In a nursing home the focus of the plan involves better planning of rest periods around the activities of the other residents. Roommates often have very different schedules.
When patients have chronic sleep problems, the initial referral for a patient is often to a comprehensive sleep center for assessment of the problem. The nature of the sleep disturbance then determines whether referrals to additional health care providers are necessary. For example, if a sleep problem is related to a situational crisis or emotional problem, refer the patient to a mental health clinical nurse specialist or clinical psychologist for counseling. If the nurse works in an inpatient setting and the patient needs a referral for continued care after discharge, offering information about the sleep problem is useful to the home care nurse. The success of sleep therapy depends on an approach that fits the patient’s lifestyle and the nature of the sleep disorder.
Implementation
Nursing interventions designed to improve the quality of a person’s rest and sleep are largely focused on health promotion. Patients need adequate sleep and rest to maintain active and productive lifestyles. During times of illness, rest and sleep promotion are important for recovery. Nursing care in an acute, restorative, or continuing care setting differs from that provided in a patient’s home. The primary differences are in the environment and the nurse’s ability to support normal rest and sleep habits. A patient’s age also influences the types of therapies that are most effective. Box 42-8 provides principles for promoting sleep in older patients.
Health Promotion
In community health and home settings help patients develop behaviors conducive to rest and relaxation. To develop good sleep habits at home, patients and their bed partners need to learn techniques that promote sleep and conditions that interfere with it (Kryger et al., 2011) (Box 42-9 on p. 954). Parents also learn how to promote good sleep habits for their children. Patients benefit most from instructions based on information about their homes and lifestyles such as which type of activities promotes sleep in a night-shift worker or how to make the home environment more conducive to sleep. They will more likely apply information that is useful and valued.
Environmental Controls: All patients require a sleeping environment with a comfortable room temperature and proper ventilation, minimal sources of noise, a comfortable bed, and proper lighting (National Heart, Lung, and Blood Institute, 2009). Children and adults vary more in regard to comfortable room temperature. Instruct parents to position cribs away from open windows or drafts and to cover the infant with a light, warm blanket. Older adults often require extra blankets or covers.
Eliminate distracting noise so the bedroom is as quiet as possible. In the home the television, telephone, or the intermittent chiming of a clock often disrupts a patient’s sleep. Involve the family in identifying approaches for reducing noise in the home, especially if there are several family members, all with different sleep schedules. It is also important to remember that some patients sleep with familiar inside noises such as the hum of a fan. Commercial products that produce a soothing noise such as ocean waves or rainfall create a soothing environment for sleep.
A bed and mattress need to provide support and comfortable firmness. Bed boards placed under mattresses add support. Sometimes extra pillows are important to help a person position comfortably in bed. The position of the bed in the room also makes a difference for some patients.
Patients vary in regard to the amount of light that they prefer at night. Infants and older adults sleep best in softly lit rooms. Light should not shine directly on their eyes. Small table lamps prevent total darkness. For older adults light reduces the chance of confusion and prevents falls when walking to the bathroom. If streetlights shine through windows or when patients nap during the day, heavy shades, drapes, or slatted blinds are helpful.
Promoting Bedtime Routines: Bedtime routines relax patients in preparation for sleep (Bulechek, Butcher, and Dochterman, 2008). It is always important for persons to go to sleep when they feel fatigued or sleepy. Going to bed while fully awake and thinking about other things often causes insomnia and interferes with the bed as a stimulus for sleep. Newborns and infants sleep through so much of the day that a specific routine is hardly necessary. However, quiet activities such as holding them snugly in blankets, singing or talking softly, and gentle rocking help infants fall asleep.
A bedtime routine (e.g., same hour for bedtime, snack, or quiet activity) used consistently helps young children avoid delaying sleep. Parents need to reinforce patterns of preparing for bedtime. Quiet activities such as reading stories, coloring, allowing children to sit in a parent’s lap while listening to music or listening to a prayer are routines that are often associated with preparing for bed.
Adults need to avoid excessive mental stimulation just before bedtime. Reading a light novel, watching an enjoyable television program, or listening to music helps a person relax. Relaxation exercises such as slow, deep breathing for 1 or 2 minutes relieve tension and prepare the body for rest (see Chapter 43). Guided imagery and praying also promote sleep for some patients.
At home discourage patients from trying to finish office work or resolve family problems before bedtime. The bedroom is not a place to work, and patients need to always associate it with sleep. Working toward a consistent time for sleep and awakening helps most patients gain a healthy sleep pattern and strengthens the rhythm of the sleep-wake cycle.
Promoting Safety: For any patient prone to confusion or falls, safety is critical. A small night-light helps a patient orient to the room environment before going to the bathroom. Beds set lower to the floor lessen the chance of a person falling when first standing. Instruct patients to remove clutter and throw rugs from the path used to walk from the bed to the bathroom. If a patient needs assistance in ambulating from a bed to the bathroom, place a small bell at the bedside to call family members. Sleepwalkers are unaware of their surroundings and are slow to react, increasing the risk of falls. Do not startle sleepwalkers but instead gently awaken them and lead them back to bed.
Infants’ beds need to be safe. To reduce the chance of suffocation, do not place pillows, stuffed toys, or the ends of loose blankets in cribs. Loose-fitting plastic mattress covers are dangerous because infants pull them over their faces and suffocate. Parents need to place an infant on his or her back to prevent suffocation.
Promoting Comfort: People fall asleep only after feeling comfortable and relaxed (Bulechek, Butcher, and Dochterman, 2008). Minor irritants often keep patients awake. Soft cotton nightclothes keep infants or small children warm and comfortable. Instruct patients to wear loose-fitting nightwear. An extra blanket is sometimes all that is necessary to prevent a person from feeling chilled and being unable to fall asleep. Patients need to void before retiring so they are not kept awake by a full bladder.
Establishing Periods of Rest and Sleep: In the home it helps to encourage patients to stay physically active during the day so they are more likely to sleep at night. Increasing daytime activity lessens problems with falling asleep. In a home setting you will frequently care for patients with chronic debilitating disease. The nursing care plan includes having patients set aside afternoons for rest to promote optimal health. Help adjust medication schedules, instruct patients to regularly void before rest periods, and suggest silencing the telephone ringer so rest periods are uninterrupted.
Stress Reduction: The inability to sleep because of emotional stress also makes a person feel irritable and tense. When patients are emotionally upset, encourage them to try not to force sleep. Otherwise insomnia frequently develops, and soon bedtime is associated with the inability to relax. Encourage a patient who has difficulty falling asleep to get up and pursue a relaxing activity such as sewing or reading rather than staying in bed and thinking about sleep.
Preschoolers have bedtime fears (fear of the dark or strange noises), awaken during the night, or have nightmares. After nightmares the parent enters the child’s room immediately and talks to him or her briefly about fears to provide a cooling-down period. One approach is to comfort children and leave them in their own beds so their fears are not used as excuses to delay bedtime. Keeping a light on in the room also helps some children. Cultural tradition causes families to approach sleep practices differently (Box 42-10). Always respect those that differ from traditional recommendations.
Bedtime Snacks: Some people enjoy bedtime snacks, whereas others cannot sleep after eating. A dairy product such as warm milk or cocoa that contains l-tryptophan is often helpful in promoting sleep. A full meal before bedtime often causes gastrointestinal upset and interferes with the ability to fall asleep.
Warn patients against drinking or eating foods with caffeine before bedtime. Coffee, tea, colas, and chocolate act as stimulants, causing a person to stay awake or to awaken throughout the night. Caffeinated foods and liquids and alcohol act as diuretics and cause a person to awaken in the night to void (National Heart, Lung, & Blood Institute, 2009).
Infants require special measures to minimize nighttime awakenings for feeding. It is common for children to need middle-of-the-night bottle-feeding or breastfeeding. Hockenberry and Wilson (2011) recommend offering the last feeding as late as possible. Tell parents not to give infants bottles in bed.
Pharmacological Approaches: Melatonin is a neurohormone produced in the brain that helps control circadian rhythms and promote sleep (Kryger et al., 2011). It is a popular nutritional supplement that is found to be helpful in improving sleep efficiency and decreasing nighttime awakenings (Pandi-Perumal et al., 2007).The recommended dose is 0.3 to 1 mg taken 2 hours before bedtime. Older adults who have decreased levels of melatonin find it beneficial as a sleep aid (Kryger et al., 2011). Short-term use of melatonin has been found to be safe, with mild side effects of nausea, headache, and dizziness being infrequent (Larzelere et al., 2010). Ramelton (Rozerem), a melatonin receptor agonist, is well tolerated and appears to be effective in improving sleep (Morin et al., 2007).
Several other herbal products assist in sleep. Valerian is effective in mild insomnia and RLS. It effects release of neurotransmitters and produces very mild sedation (Cuellar and Ratcliffe, 2009). Kava helps promote sleep in patients with anxiety. It needs to be used cautiously because of its potential toxic effects on the liver (Larzelere et al., 2010). Chamomile, an herbal tea, has a mild sedative effect that may be beneficial in promoting sleep (Moquin et al., 2009). Caution patients about the dosage and use of herbal compounds because the U.S. Food and Drug Administration (FDA) does not regulate them. Herbal compounds may interact with prescribed medication, and patients need to avoid using these together (Meiner, 2011).
The use of nonprescription sleeping medications is not advisable. Patients need to learn the risks of such drugs. Over the long term these drugs lead to further sleep disruption, even when they initially seemed to be effective. Caution older adults about using over-the-counter antihistamines because of their long duration of action, which can cause confusion, constipation, urinary retention, and increased risk of falls (Passarella and Duong, 2008). Help patients use behavioral and proper sleep hygiene measures to establish sleep patterns that do not require the use of drugs.
Acute Care
Patients in acute care settings have their normal rest and sleep routine disrupted, which generally leads to sleep problems. In this setting nursing interventions focus on controlling factors in the environment that disrupt sleep, relieving physiological or psychological disruptions to sleep, and providing for uninterrupted rest and sleep periods for the patient. “Excessive Sleepiness” in the Evidence-based Geriatric Nursing Protocols for Best Practice is based on the principle that nurses need to individualize an effective strategy based on patient needs and that sleep medications are a last-resort intervention (Chasens et al., 2008).
Environmental Controls: In a hospital the nurse controls the environment in several ways (Box 42-11). Close the curtains between patients in semiprivate rooms. Dim lights on a hospital nursing unit at night. One of the biggest problems for patients in the hospital is noise. Important ways to reduce noise are to conduct conversations and reports in a private area away from patient rooms and keep necessary conversations to a minimum, especially at night (Gardner et al., 2009). Additional ways to control noise in the hospital are listed in Box 42-12.
Promoting Comfort: Compared with beds at home, hospital beds are often harder and of a different height, length, or width. Keeping them clean and dry and in a comfortable position helps patients relax. Some patients suffer painful illnesses requiring special comfort measures such as application of dry or moist heat, use of supportive dressings or splints, and proper positioning before retiring (Fig. 42-6).
Establishing Periods of Rest and Sleep: In a hospital or extended care setting it is difficult to provide patients with the time needed to rest and sleep. The most effective treatment for sleep disturbances is elimination or correction of factors that disrupt the sleep pattern. You need to plan care to avoid awakening patients for nonessential tasks. Do this by scheduling assessments, treatments, procedures, and routines for times when patients are awake. For example, if a patient’s physical condition has been stable, avoid awakening him or her to check vital signs. Allowing patients to determine the timing and methods of delivery of basic care measures promotes rest. Do not give baths and routine hygiene measures during the night for nursing convenience. Draw blood samples at a time when the patient is awake. Unless maintaining the therapeutic blood level of a drug is essential, give medications during waking hours. Work with the radiology department and other support services to schedule diagnostic studies and therapies at intervals that allow patients time for rest. Always try to provide the patient with 2 to 3 hours of uninterrupted sleep during the night.
When the patient’s condition demands more frequent monitoring, plan activities to allow extended rest periods. A nurse instructs assistive personnel in the coordination of patient care to reduce patient disturbances. This means planning activities so the patient has as long as an hour or more to rest quietly rather than having a nurse or other personnel return to the room every few minutes. For example, if a patient needs frequent dressing changes, is receiving intravenous therapy, and has drainage tubes from several sites, do not make a separate trip into the room to check each problem. Instead use a single visit to perform all three tasks. Become the patient’s advocate for promoting optimal sleep. This means becoming a gatekeeper by postponing or rescheduling visits by family, asking consultants to reschedule visits, or questioning the frequency of certain procedures.
Promoting Safety: Patients with OSA are at risk for complications while in the hospital. Surgery and anesthesia disrupt normal sleep patterns. After surgery patients reach deep levels of REM sleep. This deep sleep causes muscle relaxation that leads to OSA (Hwang et al., 2008). Patients with OSA who are given opioid analgesics after surgery have an increased risk of developing airway obstruction because the medications suppress normal arousal mechanisms (Hwang et al., 2008). These patients often need ventilator support in the postoperative period because of the increased risk of respiratory complications. Monitor the patient’s airway, respiratory rate, depth, and breath sounds frequently after surgery.
Recommend lifestyle changes to patients with OSA that include sleep hygiene, alcohol moderation, smoking cessation, and a weight-loss program (Freedman, 2010). Teach the patient to elevate the head of the bed and use a side or prone position for sleep. Use pillows to prevent a supine position (Lamm et al., 2008; Pinto and Caple, 2010).
One of the most effective therapies is use of a nasal continuous positive airway pressure (CPAP) device at night, which requires a patient to wear a mask over the nose. A mask delivers room air at a high pressure (Fig. 42-7). The air pressure prevents airway collapse. The CPAP device is portable and effective particularly for obstructive apnea. Another treatment option is the use of an oral appliance. These appliances advance the mandible or tongue to relieve pharyngeal obstruction (Wickwire and Collop, 2010). In cases of severe sleep apnea the tonsils, uvula, or portions of the soft palate are surgically removed. The success of surgical procedures to correct OSA varies.
Stress Reduction: Patients who are hospitalized for extensive diagnostic testing often have difficulty resting or sleeping because of uncertainty about the state of their health. Giving patients control over their health care minimizes uncertainty and anxiety. Providing information about the purpose of procedures and routines and answering questions give patients the peace of mind needed to rest or fall asleep. A nurse on the night shift needs to take time to sit and talk with patients unable to sleep. This helps to determine the factors keeping patients awake. Back rubs also help patients relax more thoroughly. If a sedative is indicated, confer with the patient’s health care provider to be sure that the lowest dose is used initially. Discontinuing a sedative as soon as possible prevents a dependence that seriously disrupts the normal sleep cycle. Older adults’ metabolism of drugs is slow, making them more vulnerable to the side effects of sedatives, hypnotics, antianxiety drugs, or analgesics.
Restorative or Continuing Care
The nursing interventions implemented in the acute care setting are also used in the restorative or continuing care environment. Controlling the environment, especially noise; establishing periods of rest and sleep; and promoting comfort are important considerations. Nursing interventions related to stress reduction and controlling physiological disturbances are also implemented in these settings. Helping a patient achieve restful sleep in this environment sometimes takes time.
Promoting Comfort: Providing for personal hygiene improves a patient’s sense of comfort. A warm bath or shower before bedtime is relaxing. Offer patients restricted to bed the opportunity to void and wash their face and hands. Toothbrushing and care of dentures also help to prepare patients for sleep. Position patients to support their dependent body parts and protect pressure points. Offer a back or hand massage to aid in muscle relaxation just before a patient goes to sleep (Harris and Richards, 2010) (see Chapter 43).
Controlling Physiological Disturbances: As a nurse you will learn to control symptoms of physical illness that disrupt sleep. For example, a patient with respiratory abnormalities sleeps with two pillows or in a semi-sitting position to ease the effort to breathe. He or she benefits from taking prescribed bronchodilators before sleep to prevent airway obstruction. A patient with a hiatal hernia also needs special care. After meals he or she often experiences a burning sensation as a result of gastric reflux. To prevent sleep disturbances have the patient eat a small meal several hours before bedtime and sleep in a semi-sitting position. Patients with pain, nausea, or other recurrent symptoms receive any symptom-relieving medication timed so the drug takes effect at bedtime. Remove or change any irritants against the patient’s skin such as moist dressings or drainage tubes.
Pharmacological Approaches: The liberal use of drugs to manage insomnia is quite common in American culture. CNS stimulants such as amphetamines, caffeine, nicotine, terbutaline, theophylline, and modafinil need to be used sparingly and under medical management (Lehne, 2010). In addition, withdrawal from CNS depressants such as alcohol, barbiturates, tricyclic antidepressants (amitriptyline, imipramine, and doxepin), and triazolam causes insomnia. You need to manage these carefully.
Medications that induce sleep are called hypnotics. Sedatives are medications that produce a calming or soothing effect (Lehne, 2010). A patient who takes sleep medications needs to know about their proper use and their risks and possible side effects. Long-term use of antianxiety, sedative, or hypnotic agents disrupts sleep and leads to more serious problems. The FDA requires that the product labels of all sleep medications contain safety information related to the potential adverse effects of severe allergic reactions; severe facial swelling; and complex sleep behaviors such as sleep-driving, making phone calls, and preparing and eating food while asleep (USFDA, 2010).
Benzodiazepines and nonbenzodiazepines are common classifications of drugs used to treat sleep problems. The nonbenzodiazepines have become the treatment of choice for insomnia because of improved efficacy and safety of use (Neubauer, 2009). Experts recommend a low dose of a short-acting medication such as zolpidem (Ambien) for short-term use (no longer than 2 to 3 weeks) (Cramwell-Bruce, 2007). These drugs cause fewer problems with dependence and abuse and fewer rebound insomnia and hangover effects than benzodiazepines (Passarella and Duong, 2008).
The benzodiazepines cause relaxation, antianxiety, and hypnotic effects by facilitating the action of neurons in the CNS that suppress responsiveness to stimulation, thereby decreasing levels of arousal (Lehne, 2010). Short-acting benzodiazepines (e.g. oxazepam, lorazepam, or temazepam) at the lowest possible dose are recommended. Initial doses are small; and increments are added gradually, based on patient response, for a limited time. Warn patients not to take more than the prescribed dose, especially if the medication seems to become less effective after initial use. The use of benzodiazepines in older adults is potentially dangerous because of the tendency of the drugs to remain active in the body for a longer time. As a result, they also cause respiratory depression; next-day sedation; amnesia; rebound insomnia; and impaired motor functioning and coordination, which leads to increased risk of falls (Cramwell-Bruce, 2007; Neubauer, 2009). If older patients who were recently continent, ambulatory, and alert become incontinent or confused and/or demonstrate impaired mobility, the use of benzodiazepines needs to be considered as a possible cause.
Use benzodiazepines cautiously with children under 12 years of age. These medications are contraindicated in infants less than 6 months. Pregnant patients need to avoid them because their use is associated with risk of congenital anomalies. Nursing mothers do not receive the drugs because they are excreted in breast milk.
Regular use of any sleep medication often leads to tolerance and withdrawal. Rebound insomnia is a problem after stopping the medication. Immediately administering a sleeping medication when a hospitalized patient complains of being unable to sleep does the patient more harm than good. Consider alternative approaches to promote sleep. Routine monitoring of patient response to sleeping medications is important.
Evaluation
With regard to problems with sleep, the patient is the source for evaluating outcomes. Each patient has a unique need for sleep and rest. The patient is the only one who knows if sleep problems are improved and which interventions or therapies are most successful in promoting sleep (Fig. 42-8). To evaluate the effectiveness of nursing interventions, make comparisons with baseline assessment data to evaluate if sleep has improved. It is important to ask the patient if his or her sleep needs have been met. For example, ask the patient, “Are you feeling more rested?”; “Can you tell me if you feel we have done all we can to help improve your sleep?”; or “What interventions have been most effective in helping you sleep?” If expectations have not been met, you need to spend more time trying to understand the patient’s needs and preferences. Working closely with the patient and bed partner enables you to redefine expectations that can be met realistically within the limits of the patient’s condition and treatment.
Patient Outcomes
Determine whether expected outcomes have been met. Use evaluative measures shortly after a therapy has been tried (e.g., observing whether a patient falls asleep after reducing noise and darkening a room). Use other evaluative measures after a patient awakens from sleep (e.g., asking a patient to describe the number of awakenings during the previous night). The patient and bed partner usually provide accurate evaluative information. Over longer periods use assessment tools such as the visual analogue or sleep-rating scale to determine whether sleep has progressively improved or changed.
Also evaluate the level of understanding that patients or family members gain after receiving instruction in sleep habits. You measure compliance with these practices during a home visit, when you are able to observe the environment. When expected outcomes are not met, revise the nursing measures or expected outcomes based on the patient’s needs or preferences. When outcomes are not met, ask questions such as:
• Are you able to fall asleep within 20 minutes of getting in bed?
• Describe how well you sleep when you exercise.
If a nurse has successfully developed a good relationship with a patient and a therapeutic plan of care, subtle behaviors often indicate the level of the patient’s satisfaction. Note the absence of signs of sleep problems such as lethargy or frequent yawning or position changes in the patient. You are effective in promoting rest and sleep if the patient’s goals and expectations are met.
Key Points
• Sleep provides physiological and psychological restoration.
• The 24-hour sleep-wake cycle is a circadian rhythm that influences physiological function and behavior.
• The control and regulation of sleep depends on a balance among regulators within the CNS.
• During a typical night’s sleep a person passes through four to five complete sleep cycles. Each sleep cycle contains three NREM stages of sleep and a period of REM sleep.
• The most common type of sleep disorder is insomnia.
• The hectic pace of a person’s lifestyle, emotional and psychological stress, and alcohol ingestion frequently disrupt the sleep pattern.
• If a patient’s sleep is adequate, assess his or her usual bedtime, normal bedtime ritual, preferred environment for sleeping, and usual preferred rising time.
• When a patient has a sleep problem, conduct a complete sleep history. Diagnosing sleep problems depends on identifying factors that impair sleep.
• When planning interventions to promote sleep, considers the usual characteristics of the patient’s home environment and normal lifestyle.
• A regular bedtime routine of relaxing activities prepares a person physically and mentally for sleep.
• An environment with a darkened room, reduced noise, comfortable bed, and good ventilation promotes sleep.
• Important nursing interventions for promoting sleep in the hospitalized patient are establishing periods for uninterrupted sleep and rest and controlling noise levels.
• Pain or other disease symptom control is essential to promoting the ability to sleep.
• Long-term use of sleeping pills often leads to difficulty initiating and maintaining sleep.
Clinical Application Questions
Preparing for Clinical Practice
Julie returns to the neighborhood health clinic with her husband, David, for a follow-up visit. She tells you that since she started her sleep hygiene plan she feels more rested but is still having some problems sleeping because of her husband’s loud snoring. Besides Julie’s report of David’s snoring, you note that he is overweight.
1. Based on Julie’s report of David’s snoring, which additional assessment data should you gather from David?
2. Based on David’s reported symptoms, what problem do you suspect he might have? What recommendations do you give David to improve his sleeping?
3. Julie and David tell you that they are concerned about their 6-year-old daughter. She just started school and is having sleep problems. List at least four interventions for Julie and David to use to improve their daughter’s sleep patterns.
![]() Answers to Clinical Application Questions can be found on the Evolve website.
Answers to Clinical Application Questions can be found on the Evolve website.
Are You Ready to Test Your Nursing Knowledge?
1. The nurse is gathering a sleep history from a patient who is being evaluated for obstructive sleep apnea. Which common symptoms does the patient most likely report? (Select all that apply.)
2. The nurse incorporates which priority nursing intervention into a plan of care to promote sleep for a hospitalized patient?
1. Have patient follow hospital routines
2. Avoid awakening patient for nonessential tasks
3. Older adults are cautioned about the long-term use of sedatives and hypnotics because these medications can:
1. Cause headaches and nausea.
2. Be expensive and difficult to obtain.
4. The nurse is providing health teaching for a patient using herbal compounds such as melatonin for sleep. Which points need to be included? (Select all that apply.)
1. Can cause urinary retention
2. Should not be used indefinitely
3. May cause diarrhea and anxiety
4. May interfere with prescribed medications
5. Can lead to further sleep problems over time
6. Are not regulated by the U.S. Food and Drug Administration (FDA)
5. The patient reports vivid dreaming to the nurse. Through understanding of the sleep cycle, the nurse recognizes that vivid dreaming occurs during which sleep phase?
6. The nurse teaches a patient taking a benzodiazepine that this group of medications causes which symptom of a sleep problem?
7. Which intervention is appropriate to include on a care plan for improving sleep in the older adult?
1. Decrease fluids 2 to 4 hours before sleep
2. Exercise in the evening to increase fatigue
8. Which statement made by a mother being discharged to home with her newborn infant indicates a need for further teaching?
1. “I won’t put the baby to bed with a bottle.”
2. “For the first few weeks we’re putting the cradle in our room.”
3. “My grandmother told me that babies sleep better on their stomachs.”
4. “I know I’ll have to get up during the night to feed the baby when he wakes up.”
9. The nurse is developing a plan of care for a patient experiencing narcolepsy. Which intervention is appropriate to include on the plan?
1. Instruct the patient to increase carbohydrates in the diet
2. Have patient limit fluid intake 2 hours before bedtime
3. Preserve energy by limiting exercise to morning hours
4. Encourage patient to take one or two 20-minute naps during the day
10. Which nursing measure best promotes sleep in a school-age child?
11. Which action by the nursing assistant at bedtime requires the nurse to intervene?
12. Which statement made by the patient indicates a need for further teaching on sleep hygiene?
1. “I’m going to do my exercises before I eat dinner.”
2. “I’ll have a glass of wine at bedtime to relax.”
3. “I set my alarm to get up at the same time every morning.”
13. Which statement made by an older adult best demonstrates understanding of taking a sleep medication?
1. “I’ll take the sleep medicine for 4 or 5 weeks until my sleep problems disappear.”
2. “Sleep medicines won’t cause any sleep problems once I stop taking them.”
3. “I’ll talk to my health care provider before I use an over-the-counter sleep medication.”
4. “I’ll contact my health care provider if I feel extreme sleepy in the mornings.”
14. The school nurse is teaching health-promoting behaviors that improve sleep to a group of high school students. Which points should be included in the education? (Select all that apply.)
2. Go to sleep each night whenever you feel tired.
3. Turn off your cell phone at bedtime.
15. The nurse is taking a sleep history from a patient. Which statement made by the patient needs further follow-up?
Answers: 1. 1, 3, 5; 2. 2; 3. 4; 4. 2, 4, 6; 5. 1; 6. 3; 7. 1; 8. 3; 9. 4; 10. 4; 11. 4; 12. 2; 13. 3; 14. 1, 3, 4; 15. 1.
References
Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263.
Ahmed, I, Thorpy, M. Clinical features, diagnosis and treatment of narcolepsy. Clin Chest Med. 2010;31(2):371.
American Academy of Breastfeeding Medical Protocol Committee (AABMPC). ABM clinical protocol #6: guideline on co-sleeping and breastfeeding. Breastfeeding Med. 2008;3(1):38.
American Nurses Association. Nursing scope and standards of practice. Washington, DC: The Association; 2010.
Andrews, MM, Boyle, JS. Transcultural concepts in nursing care, ed 5. Philadelphia: Lippincott; 2008.
Babson, KA, et al. Cognitive behavioral therapy for sleep disorders. Psych Clin North Am. 2010;33(3):629.
Benca, RM, Schneck, CH. Sleep and eating disorders. In Kruger MH, et al, eds.: Principles and practice of sleep medicine, ed 4, St Louis: Saunders, 2005.
Bulechek, GM, Butcher, HK, Dochterman, JM. Nursing interventions classification (NIC), ed 5. St Louis: Mosby; 2008.
Chasens, ER, et al. Excessive sleepiness. In Capezuti E, et al, eds.: Evidence-based geriatric nursing protocols for best practice, ed 3, New York: Springer, 2008.
Cramwell-Bruce, LA. Hypnotic sedative drugs. Medsurg Nurs. 2007;16(3):198.
Cuellar, NG, et al. Assessment and treatment of sleep disorders in the elderly. Geriatr Nurs. 2007;28(4):254.
Ebersole, P, et al. Toward healthy aging: human needs and nursing response, ed 7. St Louis: Mosby; 2008.
Freedman, N. Treatment of obstructive sleep apnea. Clin Chest Med. 2010;31:187.
Getter, LT, McKenna, JJ. Never sleep with baby? Or keep me close but keep me safe; eliminating inappropriate “safe infant sleep” rhetoric in the United States. Curr Pediatr Rev. 2010;6(1):71.
Giger, JN, Davidhizar, RE. Transcultural nursing: assessment and intervention, ed 5. St Louis: Mosby; 2008.
Heaton, K, et al. Sleep and motor vehicle crashes. J Emerg Nurs. 2009;35(4):363.
Hockenberry, MJ, Wilson, D. Wong’s nursing care of infants and children, ed 9. St Louis: Mosby; 2011.
Hwang, D, et al. Association of sleep-disordered breathing with post-operative complications. CHEST. 2008;133(5):1128.
Izac, SM. Basic anatomy and physiology of sleep. Am J Electroneurodiagnostic Technol. 2006;46:18.
Kryger, MH, et al. Principles and practice of sleep medicine, ed 5. St Louis: Saunders; 2011.
Lamm, J, et al. Obtaining a thorough sleep history and routinely screening for obstructive sleep apnea. J Am Acad Nurs Pract. 2008;20:225.
Larzelere, MM, et al. Complementary and alternative medicine usage for behavioral health indicators. Prim Care Clin Office Pract. 2010;37(2):213.
Lashley, F. Measuring sleep. In Frank-Stromborg M, Olsen SJ, eds.: Instruments for clinical-healthcare research, ed 3, Boston: Jones & Bartlett, 2004.
Lehne, RA. Pharmacology for nurses, ed 7. St Louis: Mosby; 2010.
Malhotra, RK, Desai, AK. Healthy brain aging: what has sleep got to do with it? Clin Geriatr Med. 2010;26:45.
McCance KL, et al, eds. Pathophysiology: the biologic basis for disease in adults and children, ed 6, St Louis: Mosby, 2010.
Meiner, SE. Gerontologic nursing, ed 4. St Louis: Mosby; 2011.
Moquin, B, et al. Complementary and alternative medicine. Geriatr Nurs. 2009;30(3):196.
Morin, AK, et al. Therapeutic options for sleep-maintenance and sleep-onset insomnia. Pharmacotherapy. 2007;27(1):89.
Natarajan, R. Review of periodic limb movement and restless leg syndrome. J Postgrad Med. 2010;56(2):157.
National Guideline Clearinghouse, Clinical guideline for the evaluation and management of chronic insomnia in adults. NCG7396. 2008. http://www.guideline.gov/content.aspx?id=15089 [Accessed October 10, 2011].
National Heart, Lung, and Blood Institute, How is insomnia treated? 2009. http://www.nhlbi.nih.gov/health/health-topics/topics/inso/treatment.html [Accessed December 10, 2011].
National Sleep Foundation, Aging and sleep. Washington, DC. 2009. http://www.sleepfoundation.org/article/sleep-topics/aging-and-sleep [Accessed October 10, 2011].
National Sleep Foundation. The ABCs of ZZZs [Brochure]. Washington, DC: The Foundation; 2010.
National Sleep Foundation, Apnea and sleep. Washington, DC. 2010. http://www.sleepfoundation.org/article/sleep-topics/sleep-apnea-and-sleep [Accessed October 10, 2011].
National Sleep Foundation, Depression and sleep 2010. http://www.sleepfoundation.org/article/sleep-topics/depression-and-sleep [Accessed October 10, 2011].
Neikrug, AB, Ancoli-Israel, S. Sleep disorders in the older adult—a mini review. Gerontology. 2010;56:181.
Neubauer, DN. Current and new thinking in the management of comorbid insomnia. Am J Manag Care. 2009;15(1):S24.
Ohlmann, KK, O’Sullivan, MI. The costs of short sleep. AAOHN J. 2009;57(9):381.
Pandi-Perumal, SR, et al. Role of melatonin system in the control of sleep. CNS Drugs 2007. 2007;21(12):995.
Passarella, S, Duong, M. Diagnosis and treatment of insomnia. Am J Health Syst Pharmacol. 2008;65:927.
Pinto, S, Caple, C. Obstructive sleep apnea in adults. CINAHL Information Systems. 2010. [April 23].
Ramakrishnan, K, Scheid, DC. Treatment options for insomnia. Am Fam Physician. 2007;76(4):517.
Redeker, N. Sleep disturbance in people with heart failure: implications for self-care. J Cardiovasc Nurs. 2008;23(3):231.
Reeve, K, Bailes, B. Insomnia in adults: etiology and management. J Nurs Pract. 2010;6(1):53.
Smyth, CA. Evaluating sleep quality in older adult. Am J Nurs. 2008;108(5):42.
Touhy, TA, Jett, KF. Ebersole and Hess’ gerontological nursing healthy aging, ed 3. St Louis: Mosby; 2010.
Townsend-Roccichelli, J, et al. Managing sleep disorders in the elderly. Nurse Pract. 2010;35(5):30.
US Food and Drug Administration, Side effects of sleep drugs 2010. http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm107757.htm [Accessed October 10, 2011].
Van der Zee, EA, et al. The neurobiology of circadian rhythms. Curr Opinion Pulmonary Med. 2009;15:534.
Wickwire, EM, Collop, NA. Insomnia and sleep-related breathing disorders. CHEST. 2010;137(6):1449.
Research References
Cuellar, NG, Ratcliffe, SJ. Does valerian improve sleepiness and symptom severity in people with restless legs syndrome? Alt Ther Health Med. 2009;15(2):22.
Dennis, CM, et al. Benefits of quiet time for neurointensive care patients. J Neurosci Nurs. 2010;42(4):217.
Fontana, CJ, Pittiglio, LI. Sleep deprivation among critical care patients. Crit Care Nurs Q. 2010;33(1):75.
Gardner, G, et al. Creating a therapeutic environment: a non-randomized controlled trial of a quiet time intervention for patients in acute care. Int J Nurs Stud. 2009;46:778.
Harris, M, Richards, KC. The physiological and psychological effect of slow-stroke back massage and hand massage on relaxation in older people. J Clin Nurs. 2010;19:197.
Irwin, MR, et al. Comparative meta-analysis of behavioral interventions for insomnia and their efficacy in middle-aged adults and in older adults 55+ years of age. Health Psych. 2006;25(1):3.
Koren, A, et al. Parental information and behaviors and provider practices related to tummy time and back to sleep. J Pediatr Health Care. 2010;24(4):222.
Lahr, MAB, et al. Maternal-infant bed sharing: risk factors for bedsharing in a population-based survey of new mothers and implications for SIDS risk reduction. Matern Chld Health J. 2007;11(3):277.
LaReau, R, et al. Examining the feasibility of implementing specific nursing interventions to promote sleep in hospitalized elderly patients. Geriatr Nurs. 2008;29(3):197.
Natale, V, et al. Actigraphy in the assessment of insomnia: a quantitative approach. Sleep. 2009;32(6):767.
Noland, H, et al. Adolescents’ sleep behaviors and perceptions of sleep. J School Health. 2009;79(5):224.
Richardson, A, et al. Development and implementation of a noise reduction intervention programme: a pre- and postaudit of three hospital wards. J Clin Nurs. 2009;18:3316.
Sheldon, A, et al. Nursing assessment of obstructive sleep apnea in hospitalized adults: a review of risk factors and screening tools. Contemp Nurse. 2009;34(1):19.
Sobralske, MC, Gruber, ME. Risks and benefits of parent/child bed sharing. J Am Acad Nurs Pract. 2009;21:474.
Vallido, T, et al. Sleep in adolescence: a review of issues for nursing practice. J Clin Nurs. 2009;18:1819.