Pain Management
• Discuss common misconceptions about pain.
• Describe the physiology of pain.
• Identify components of the pain experience.
• Explain how the physiology of pain relates to selecting interventions for pain relief.
• Describe the components of pain assessment.
• Be able to perform an assessment of a patient experiencing pain.
• Explain how cultural factors influence the pain experience.
• Describe guidelines for selecting and individualizing pain interventions.
• Explain various pharmacological approaches to treating pain.
• Describe applications for use of nonpharmacological pain interventions.
• Discuss nursing implications for administering analgesics.
http://evolve.elsevier.com/Potter/fundamentals/
Everyone eventually experiences some type or degree of pain. Although it is the most common reason that people seek health care, pain is not well understood. A person in pain feels distress or suffering and seeks relief. As the nurse you cannot see or feel the patient’s pain. It is purely subjective. No two people experience pain in the same way, and no two painful events create identical responses or feelings in a person. The International Association for the Study of Pain (IASP) defines pain as “an unpleasant, subjective sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage” (IASP, 2010).
Congress declared 2000 to 2010 the Decade of Pain Control and Research, yet pain continues to be a leading public health problem in the United States. Providing pain relief is a basic human right and is in the Pain Care Bill of Rights (APF, 2007). According to the American Bar Association (2009), pain management is a basic right of people who are seriously ill. Nurses are legally and ethically responsible for managing pain and relieving suffering.
When caring for patients in pain, consider the nurse-patient relationship, patient advocacy, patient empowerment, compassion, and respect (Vaartio et al., 2009). Caring for patients in pain requires recognition that pain can and should be relieved. Effective communication among the patient, family, and professional caregivers is essential to achieve adequate pain management. You show respect for a patient in pain when you accept McCaffery’s classic definition: “Pain is whatever the experiencing person says it is, existing whenever he says it does” (Pasero and McCaffery, 2011). Effective pain management improves quality of life; reduces physical discomfort; promotes earlier mobilization and return to previous activity levels; results in fewer hospital and clinic visits; and decreases hospital lengths of stay, resulting in lower health care costs.
Scientific Knowledge Base
The pain experience is complex, involving physical, emotional, and cognitive components. Pain is subjective and highly individualized. Its stimulus is physical and/or mental in nature. Pain uses a person’s energy. It interferes with personal relationships and influences the meaning of life. You cannot measure it objectively. Only the patient knows whether pain is present and how the experience feels. It is not the responsibility of patients to prove that they are in pain; it is a nurse’s responsibility to accept their report (APS, 2003).
Physiology of Pain
There are four physiological processes of nociceptive (normal) pain: transduction, transmission, perception, and modulation (Pasero and McCaffery, 2011). A patient in pain cannot discriminate among the processes. Understanding each process helps you recognize factors that cause pain, symptoms that accompany it, and the rationale for selected therapies.
Thermal, chemical, or mechanical stimuli usually cause pain. Transduction converts energy produced by these stimuli into electrical energy Transduction begins in the periphery when a pain-producing stimulus sends an impulse across a sensory peripheral pain nerve fiber (nociceptor), initiating an action potential. Once transduction is complete, transmission of the pain impulse begins.
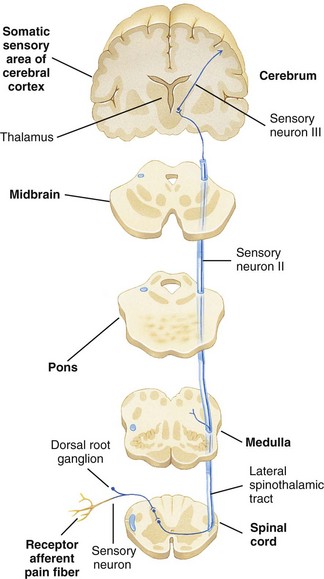
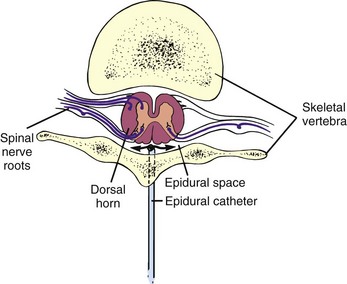
Cellular damage caused by thermal, mechanical, or chemical stimuli results in the release of excitatory neurotransmitters such as prostaglandins, bradykinin, substance P, and histamine (Box 43-1). These pain-sensitizing substances surround the pain fibers in the extracellular fluid, creating an “inflammatory soup,” spreading the pain message and causing an inflammatory response (Pasero and McCaffery, 2011). The pain stimulus enters the spinal cord via the dorsal horn and travels one of several routes until ending within the gray matter of the spinal cord. At the dorsal horn substance P is released, causing a synaptic transmission from the afferent (sensory) peripheral nerve to spinothalamic tract nerves, which cross to the opposite side (Pasero and McCaffery, 2011) (Fig. 43-1).
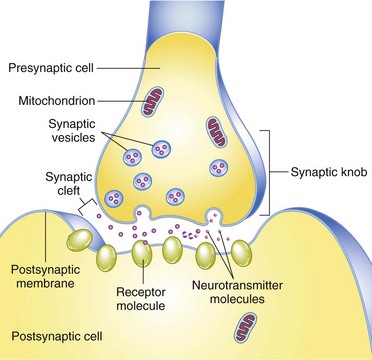
FIG. 43-1 Chemical synapses involve transmitter chemicals (neurotransmitters) that signal postsynaptic cells. (From Patton KT, Thibodeau GA: Anatomy & physiology, ed 7, St Louis, 2010, Mosby.)
Nerve impulses resulting from the painful stimulus travel along afferent (sensory) peripheral nerve fibers. Two types of peripheral nerve fibers conduct painful stimuli: the fast, myelinated A-delta fibers and the very small, slow, unmyelinated C fibers. The A fibers send sharp, localized, and distinct sensations that specify the source of the pain and detect its intensity. The C fibers relay impulses that are poorly localized, burning, and persistent. For example, after stepping on a nail, a person initially feels a sharp, localized pain, which is a result of A-fiber transmission. Within a few seconds the pain becomes more diffuse and widespread, until the whole foot hurts because of C-fiber innervations (Pasero and McCaffery, 2011).
Along the spinothalamic tract, pain impulses travel up the spinal cord (Fig. 43-2). After the pain impulse ascends the spinal cord, the thalamus transmits information to higher centers in the brain, including the reticular formation, limbic system, somatosensory cortex, and association cortex. Once a pain stimulus reaches the cerebral cortex, the brain interprets the quality of the pain and processes information from past experience, knowledge, and cultural associations in the perception of the pain (Pasero and McCaffery, 2011). Perception is the point at which a person is aware of pain. The somatosensory cortex identifies the location and intensity of pain, whereas the association cortex, primarily the limbic system, determines how a person feels about it. There is no single pain center.
As a person becomes aware of pain, a complex reaction occurs. Psychological and cognitive factors interact with neurophysiological ones in the perception of pain. Perception gives awareness and meaning to pain, resulting in a reaction. The reaction to pain includes the physiological and behavioral responses that occur after an individual perceives pain (Pasero and McCaffery, 2011).
Once the brain perceives pain, there is a release of inhibitory neurotransmitters (see Box 43-1) such as endogenous opioids, serotonin, norepinephrine, and gamma aminobutyric acid (GABA), which work to hinder the transmission of pain and help produce an analgesic effect (Pasero and McCaffery, 2011). This inhibition of the pain impulse is the fourth and last phase of the nociceptive process known as modulation (Pasero and McCaffery, 2011).
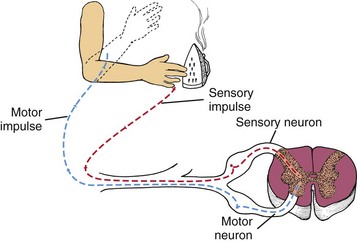
A protective reflex response also occurs with pain reception (Fig. 43-3). A-delta fibers send sensory impulses to the spinal cord, where they synapse with spinal motor neurons. The motor impulses travel via a reflex arc along efferent (motor) nerve fibers back to a peripheral muscle near the site of stimulation, thus bypassing the brain. Contraction of the muscle leads to a protective withdrawal from the source of pain. For example, when you accidentally touch a hot iron, you feel a burning sensation, but your hand also reflexively withdraws from the surface of the iron.
Gate-Control Theory of Pain
Melzack and Wall’s gate-control theory (1965) first suggested that pain has emotional and cognitive components in addition to a physical sensation. According to this theory, gating mechanisms located along the central nervous system regulate or even block pain impulses. Pain impulses pass through when a gate is open and are blocked when a gate is closed. Closing the gate is the basis for nonpharmacological pain-relief interventions. You gain a useful conceptual framework for pain management by understanding the physiological, emotional, and cognitive influences on the gates. For example, factors such as stress and exercise increase the release of endorphins, often raising an individual’s pain threshold (the point at which a person feels pain). Because the amount of circulating substances varies with every individual, the response to pain varies.
Physiological Responses
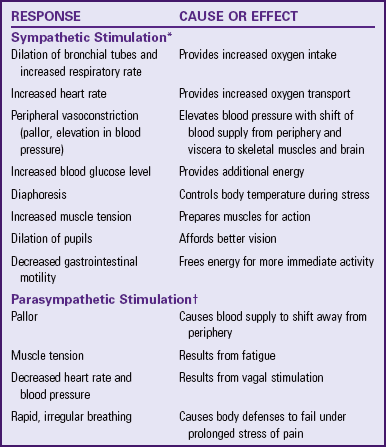
As pain impulses ascend the spinal cord toward the brainstem and thalamus, the stress response stimulates the autonomic nervous system. Pain of low to moderate intensity and superficial pain elicit the fight-or-flight reaction of the general adaptation syndrome (see Chapter 37). Stimulation of the sympathetic branch of the autonomic nervous system results in physiological responses (Table 43-1). Continuous, severe, or deep pain typically involving the visceral organs (e.g., with a myocardial infarction or colic from gallbladder or renal stones) activates the parasympathetic nervous system. Sustained physiological responses to pain sometimes seriously harm individuals. Except in cases of severe traumatic pain, which causes a person to go into shock, most people adapt to their pain, and their physical signs return to normal. Thus patients in pain do not always have changes in their vital signs. Changes in vital signs more often indicate problems other than pain.
Behavioral Responses
If left untreated or unrelieved, pain significantly alters quality of life. It usually interferes with every aspect of a person’s life, which supports why effective pain management is essential. It threatens physical and psychological well-being. Some patients choose not to report pain if they believe that it inconveniences others or if it signals loss of self-control, and some endure severe pain without assistance. Encourage your patients to accept pain-relieving measures so they remain active and continue to maintain daily activities. In contrast, other patients seek relief before pain occurs, having learned that prevention is easier than treatment. A patient’s ability to tolerate pain significantly influences your perceptions of the degree of the patient’s discomfort. Patients who have a low pain tolerance (level of pain a person is willing to accept) are sometimes inaccurately perceived as complainers. Teach patients the importance of reporting their pain sooner rather than later.
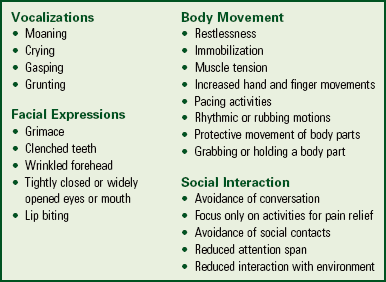
Body movements and facial expressions indicating pain include clenched teeth, holding the painful area, bent posture, and grimacing. Some patients cry or moan, are restless, or make frequent requests of a nurse. You soon learn to recognize patterns of behavior that reflect pain. This becomes especially important in patients who are unable to report their pain such as the cognitively impaired. However, lack of pain expression does not indicate that the patient is not experiencing pain (Pasero and McCaffery, 2011).
Types of Pain
Pain is categorized by duration (acute or chronic) or pathological condition (e.g., cancer or neuropathic).
Acute/Transient Pain
Acute pain is protective, has an identifiable cause, is of short duration, and has limited tissue damage and emotional response. It eventually resolves, with or without treatment, after an injured area heals. Because acute pain has a predictable ending (healing) and an identifiable cause, health team members are usually willing to treat it aggressively. Unrelieved acute pain can progress to chronic pain (Kehlet et al., 2006).
Acute pain seriously threatens a patient’s recovery by resulting in prolonged hospitalization, increased risks of complications from immobility (see Chapter 47), and delayed rehabilitation. Physical and psychological progress is delayed as long as acute pain persists because a patient focuses all energy on pain relief. Efforts aimed at teaching and motivating the patient toward self-care are often hampered until the pain is successfully managed. Complete pain relief is not always achievable, but reducing pain to a tolerable level is realistic. Thus a primary nursing goal is to provide pain relief that allows patients to participate in their recovery.
Chronic/Persistent Noncancer Pain
Unlike acute pain, chronic pain is not protective and thus serves no purpose. Chronic pain lasts longer than 6 months and is constant or recurring with a mild-to-severe intensity (Ackley and Ladwig, 2011). It does not always have an identifiable cause and leads to great personal suffering. Examples of chronic noncancer pain include arthritis, low back pain, myofascial pain, headache, and peripheral neuropathy. Chronic pain is usually non–life threatening. Sometimes an injured area healed long ago, yet the pain is ongoing and does not respond to treatment.
The possible unknown cause of chronic pain, combined with the unrelenting nature and uncertainty of its duration, frustrates a patient, frequently leading to psychological depression and even suicide. Chronic pain is a major cause of psychological and physical disability, leading to problems such as job loss, inability to perform simple daily activities, sexual dysfunction, and social isolation.
The person with chronic noncancer pain often does not show obvious symptoms and does not adapt to the pain. Rather, he or she seems to suffer more with time because of physical and mental exhaustion. Associated symptoms of chronic pain include fatigue, insomnia, anorexia, weight loss, apathy, hopelessness, and anger. Chronic pain creates the uncertainty of how one will feel from day to day. If there is no objective evidence to confirm the existence of pain, the “burden of proof” lies with the patient (Shaw, 2006). Health care workers are usually less willing to treat chronic noncancer pain with opioids, although a policy statement supports the use of opioids for it (Chou et al., 2009). In addition, the American Society of Anesthesiologists (2010) developed “Practice Guidelines for Chronic Pain Management,” which includes the use of opioids. Often a person with chronic pain who consults with numerous health care providers is labeled a drug seeker, when he or she is actually seeking adequate pain relief. This situation is called pseudoaddiction. Nurses need to discourage patients from having multiple health care providers for treating pain and refer them to pain specialists. Pain centers offer a holistic approach to chronic pain using both nonpharmacological and pharmacological strategies for pain management (Pasero and McCaffery, 2011).
Chronic Episodic Pain
Pain that occurs sporadically over an extended period of time is episodic pain. Pain episodes last for hours, days, or weeks. Examples are migraine headaches and pain related to sickle cell disease (Gruener and Lande, 2006).
Cancer Pain
Not all patients with cancer experience pain. For those who do, as many as 90% are able to have their pain managed with relatively simple means (Lehne, 2010). Some patients with cancer experience acute and/or chronic pain. The pain is nociceptive and/or neuropathic. Cancer pain is usually caused by tumor progression and related pathological processes, invasive procedures, toxicities of treatment, infection, and physical limitations. A patient senses pain at the actual site of the tumor or distant to the site, called referred pain. Assess reports of new pain by a patient with existing pain. Although the treatment of cancer pain has improved, undertreatment of cancer pain continues. Approximately 70% to 90% of patients with advanced cancer experience pain. Sixty percent of them report moderate-to-severe pain (Maxwell et al., 2005).
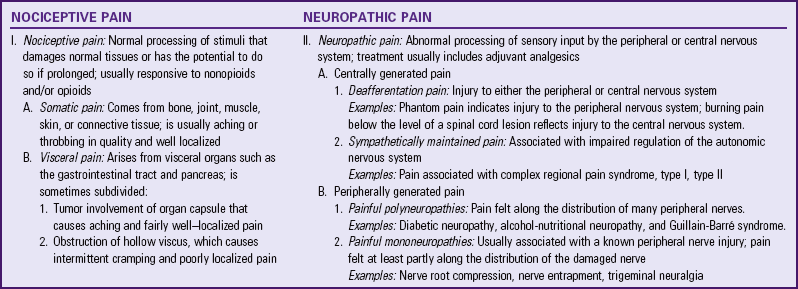
Pain by Inferred Pathological Process
Identifying the cause of pain is the first step in successful treatment. Nociceptive pain includes somatic (musculoskeletal) and visceral (internal organ) pain. Neuropathic pain arises from abnormal or damaged pain nerves (Table 43-2). Each of these pathological processes has distinct pain characteristics. The pain assessment section discusses these further.
Idiopathic Pain
Idiopathic pain is chronic pain in the absence of an identifiable physical or psychological cause or pain perceived as excessive for the extent of an organic pathological condition. An example of idiopathic pain is complex regional pain syndrome (CRPS). Research is needed to better identify the causes of idiopathic pain, thus leading to a more effective treatment (Pasero and McCaffery, 2011).
Nursing Knowledge Base
Nursing knowledge of pain mechanisms and interventions continues to grow through nursing research. This section explores factors that influence the pain experience.
Knowledge, Attitudes, and Beliefs
Attitudes of nurses and other health care providers affect pain management. The traditional medical model of illness generates attitudes about pain. This model suggests that physical problems result from physical causes. Thus pain is a physical response to organic dysfunction. When there is no obvious source of pain (e.g., the patient with chronic low back pain or neuropathies), health care providers sometimes stereotype pain sufferers as malingerers, complainers, or difficult patients.
Studies of nurses’ attitudes regarding pain management show that a nurse’s personal opinion about a patient’s report of pain affects pain assessment and titration of opioid doses. The amount of analgesia administered varies based on whether a patient is grimacing or smiling during the nurse’s assessment (Pasero and McCaffery, 2011). Nurses with more than 6 years of work experience, higher job motivation, and perceived higher levels of pain-care skills in themselves often use more patient advocacy skills in providing pain management for patients (Vaartio et al., 2009).
Nurses’ assumptions about patients in pain seriously limit their ability to offer pain relief. Biases based on culture, education, and experience influence everyone. Too often nurses allow misconceptions about pain (Box 43-2) to affect their willingness to intervene. Some nurses avoid acknowledging a patient’s pain because of their own fear and denial. They do not believe a patient’s report of pain if he or she does not look in pain. You are entitled to your personal beliefs; however, you must accept a patient’s report of pain and act according to professional guidelines, standards, position statements, policies and procedures, and evidence-based research findings (Pasero and McCaffery, 2011).
To help a patient gain pain relief, view the experience through the patient’s eyes. Acknowledging personal prejudices or misconceptions helps you address patient problems more professionally. When you become an active, knowledgeable observer of a patient in pain, you more objectively analyze the pain experience. The patient makes the diagnosis that pain is present, and you apply interventions that ultimately give relief.
Factors Influencing Pain
Pain is a complex process, involving physiological, social, spiritual, psychological, and cultural influences. Thus each individual’s pain experience is different. Consider all factors that affect the patient in pain to ensure a holistic approach to the assessment and care of the patient.
Physiological Factors
Age: Age influences pain, particularly in infants and older adults. Developmental differences found between these age-groups influence how children and older adults react to pain. Young children have trouble understanding pain and the procedures that cause it. If they have not developed full vocabularies, they have difficulty verbally describing and expressing pain to parents or caregivers. Toddlers and preschoolers are unable to recall explanations about pain or associate it with experiences that occur in various situations. With these developmental considerations in mind, you need to adapt approaches for assessing a child’s pain, including what to ask and the behaviors to observe, and how to prepare a child for a painful medical procedure.
Pain is not an inevitable part of aging. However, older adults have a greater likelihood of developing pathological conditions, which are accompanied by pain. Serious impairment of functional status often accompanies pain in older patients. Pain potentially reduces mobility, activities of daily living (ADLs), social activities, and activity tolerance. The presence of pain in an older adult requires aggressive assessment, diagnosis, and management (Box 43-3).
The ability of older patients to interpret pain is complicated. They often suffer from multiple diseases with vague symptoms that affect similar parts of the body. You need to make detailed assessments when there is more than one source of pain. Different diseases sometimes cause similar symptoms. For example, chest pain does not always indicate a heart attack; it also is a symptom of arthritis of the spine or an abdominal disorder. When older adults experience cognitive impairment and confusion, they have difficulty recalling pain experiences and providing detailed explanations of their pain (Pasero and McCaffery, 2011). You need to address misconceptions about pain management in the very young and in older adults before intervening for a patient (Tables 43-3 and 43-4).
TABLE 43-3
| MISCONCEPTION | CORRECTION |
| Infants cannot feel pain. | Infants have the anatomical and functional requirements for pain processing by mid-to-late gestation. |
| Infants are less sensitive to pain than older children and adults. | Term neonates have the same sensitivity to pain as older infants and children. Preterm neonates have a greater sensitivity to pain than term neonates or older children. |
| Infants cannot express pain. | Although infants cannot verbalize pain, they respond with behavioral cues and physiological indicators that are observable. |
| Infants must learn about pain from previous painful experiences. | Pain requires no prior experience; infants do not need to learn it from earlier painful experience. It occurs with the first insult. |
| You cannot accurately assess pain in infants. | You use behavioral cues (e.g., facial expressions, cry, body movements) and physiological indicators of pain (e.g., changes in vital signs) to reliably and validly assess pain in infants. |
| You cannot safely give analgesics and anesthetics to infants and neonates because of their immature capacity to metabolize and eliminate drugs and their sensitivity to opioid-induced respiratory depression. | Infants are very sensitive to drugs. Response to drugs is often intense and prolonged. Absorption is faster than expected. Dosages of drugs excreted by the kidneys need to be reduced (Lehne, 2010). Prescribers carefully select the medication, dosage, administration route, and time. Nurses monitor frequently for desired and undesired effects. Nurses also follow medication orders to titrate and wean medications to minimize adverse effects. |
TABLE 43-4
Misconceptions About Pain in Older Adults
| MISCONCEPTION | CORRECTION |
| Pain is a natural outcome of growing old. | Older adults are at greater risk (as much as twofold) than younger adults for many painful conditions; however, pain is not an inevitable result of aging. |
| Pain perception, or sensitivity, decreases with age. | This assumption is unsafe. Although there is evidence that emotional suffering specifically related to pain is possibly less in older than in younger patients, no scientific basis exists for the claim that a decrease in perception of pain occurs with age or that age dulls sensitivity to pain. |
| If the older patient does not report pain, he or she does not have pain. | Older patients commonly underreport pain. Reasons include expecting to have pain with increasing age; not wanting to alarm loved ones; being fearful of losing their independence; not wanting to distract, anger, or bother caregivers; and believing that caregivers know they have pain and are doing all they can to relieve it. The absence of a report of pain does not mean the absence of pain. |
| If an older patient appears to be occupied, asleep, or otherwise distracted from pain, he or she does not have pain. | Older patients often believe that it is unacceptable to show pain and have learned to use a variety of ways to cope with it (e.g., many patients use distraction successfully for short periods of time). Sleeping is sometimes a coping strategy; alternately, it indicates exhaustion, not pain relief. Do not make assumptions about the presence or absence of pain solely on the basis of a patient’s behavior. |
| The potential side effects of opioids make them too dangerous to use to relieve pain in older adults. | Opioids are safe to use in older adults with moderate-to-severe pain (Arnstein, 2010). Although the opioid-naive older adult is usually more sensitive to opioids, this does not justify withholding their use in pain management. Slow titration prevents potentially dangerous opioid-induced side effects. Regular, frequent monitoring and assessment of a patient’s response are necessary. Adjust dose and interval between doses when you detect side effects. If necessary, administer an opioid antagonist drug to reverse clinically significant respiratory depression. |
| Patients with Alzheimer’s disease and other cognitive impairments do not feel pain, and their reports of pain are most likely invalid. | No evidence exists that cognitively impaired older adults experience less pain or that their reports of pain are less valid than those of individuals with intact cognitive function (Herr, 2010). Patients with dementia or other deficits of cognition most likely suffer significant unrelieved pain and discomfort. Assessment of pain in these patients is challenging but possible. The best approach is to accept a patient’s report of pain and treat it as you would treat it in an individual with intact cognitive function. |
| Older patients report more pain as they age. | Even though older patients experience a higher incidence of painful conditions such as arthritis, osteoporosis, peripheral vascular disease, and cancer than younger patients, studies show that they underreport pain. Many older adults grew up valuing the ability to “grin and bear it” (Pasero and McCaffery, 2011). |
Fatigue: Fatigue heightens the perception of pain and decreases coping abilities. If it occurs along with sleeplessness, the perception of pain is even greater. Pain is often experienced less after a restful sleep than at the end of a long day.
Genes: Research on healthy human subjects suggests that genetic information passed on by parents possibly increases or decreases the person’s sensitivity to pain and determines pain threshold or pain tolerance. A study of twins by Kato et al. (2006) suggested modest genetic influence in the development of chronic widespread pain without significant differences experienced between men and women.
Neurological Function: A patient’s neurological function influences the pain experience. Any factor that interrupts or influences normal pain reception or perception (e.g., spinal cord injury, peripheral neuropathy, or neurological disease) affects the patient’s awareness of and response to pain. Some pharmacological agents (analgesics, sedatives, and anesthetics) influence pain perception and response and thus require close monitoring.
Social Factors
Attention: The degree to which a patient focuses attention on pain influences pain perception. Increased attention is associated with increased pain, whereas distraction is associated with a diminished pain response. This concept is one that nurses apply in various pain-relief interventions such as relaxation, guided imagery, and massage. By focusing patients’ attention and concentration on other stimuli, their perception of pain declines (see Chapter 32).
Previous Experience: Each person learns from painful experiences. Prior experience does not mean that a person accepts pain more easily in the future. Previous frequent episodes of pain without relief or bouts of severe pain cause anxiety or fear. In contrast, if a person repeatedly experiences the same type of pain that was relieved successfully in the past, the patient finds it easier to interpret the pain sensation. As a result, the patient is better prepared to take necessary actions to relieve the pain.
When a patient has no experience with a painful condition, the first perception of it often impairs the ability to cope. For example, after abdominal surgery it is common for patients to experience severe incisional pain for several days. Unless a patient knows this is a common occurrence following surgery, the onset of pain seems like a serious complication. Rather than participate actively in postoperative breathing exercises (see Chapter 50), the patient lies immobile in bed and breathes shallowly because of fear that something is not right. In the anticipatory phase of the pain experience, you need to prepare a patient with a clear explanation of the type of pain to expect and methods to reduce it. This usually results in a reduced perception of pain.
Family and Social Support: People in pain often depend on family members or close friends for support, assistance, or protection. Although pain still exists, the presence of family or friends can often make the pain experience less stressful. The presence of parents is especially important for children experiencing pain.
Spiritual Factors: Spirituality stretches beyond religion and includes an active searching for meaning to situations in which one finds oneself. Spiritual questions include “Why has this happened to me?” “Why am I suffering?” Spiritual pain goes beyond what we can see. “Why has God done this to me?” “Is this suffering teaching me something?” Other spiritual concerns include loss of independence and becoming a burden to family (Otis-Green et al., 2002). Consider making a referral to pastoral care for patients in pain. Recall that pain is an experience that has physical and emotional components. Thus providing interventions designed to treat both aspects is essential for the best possible pain management (see Chapter 35).
Psychological Factors
Anxiety: A person perceives pain differently if it suggests a threat, loss, punishment, or challenge. For example, a woman in labor perceives pain differently than a woman with a history of cancer who is experiencing a new pain and fearing recurrence. In addition, the degree and quality of pain perceived by a patient influences the meaning of pain. The relationship between pain and anxiety is complex. Anxiety often increases the perception of pain, and pain causes feelings of anxiety. It is difficult to separate the two sensations.
Critically ill or injured patients who perceive a lack of control over their environment and care have high anxiety levels. This anxiety leads to serious pain-management problems. Pharmacological and nonpharmacological approaches to the management of anxiety are appropriate; however, anxiolytic medications are not a substitute for analgesia (Pasero and McCaffery, 2011).
Coping Style: Coping style influences the ability to deal with pain. Persons with internal loci of control perceive themselves as having control over events in their life and the outcomes such as pain. In contrast, persons with external loci of control perceive that other factors in their life such as nurses are responsible for the outcome of events. Patient-controlled analgesia (PCA) uses this concept. Patients who self-administer small doses of intravenous (IV) pain medication using PCA during an acute episode successfully achieve pain control more quickly than those who rely on nurses to administer intermittent doses of pain medications.
You need to understand patients’ coping resources during painful experiences. Use resources such as communicating with a supportive family, being active, or praying, in your plan of care to support patients and offer a degree of pain relief (see Chapter 37).
Cultural Factors
The meaning that a person associates with pain affects the experience of pain and how one adapts to it. This is often closely associated with a person’s cultural background. Cultural beliefs and values affect how individuals cope with pain. Individuals learn what is expected and accepted by their culture, including how to react to pain. Health care providers often mistakenly assume that everyone responds to pain in the same way. Different meanings and attitudes are associated with pain across various cultural groups. An understanding of the cultural meaning of pain helps you design culturally sensitive care for people with pain (Pasero and McCaffery, 2011).
Culture affects pain expression. Some cultures believe that it is natural to be demonstrative about pain. Others tend to be more introverted. In addition, it is also important to know to what extent a member of a particular culture has assimilated into American society. For example, if several generations of a Hispanic patient’s family have lived in the United States, the influence of the Spanish culture may be limited, whereas newly immigrated patients still embrace their cultural norms.
As a nurse, explore the impact of cultural differences on a patient’s pain experience and make adjustments to the plan of care (Box 43-4). Work with the patient and family to facilitate communication about the assessment and management of pain. Find a culturally appropriate assessment tool and communicate use of that tool to other health care providers.
Critical Thinking
Successful critical thinking requires a synthesis of knowledge, experience, information gathered from patients, critical thinking attitudes, and intellectual and professional standards. To make clinical judgments, you anticipate the information you need, analyze the data, and make decisions regarding patient care. A patient’s condition or situation is always changing. During assessment consider all critical thinking elements that lead to appropriate nursing diagnoses.
Knowledge of pain physiology and the many factors that influence pain help you manage a patient’s pain. Previous experience in caring for patients with pain sharpens your assessment skills and ability to choose effective therapies. Critical thinking attitudes and intellectual standards ensure the aggressive assessment, creative planning, and thorough evaluation needed to obtain an acceptable level of patient pain relief. Successful pain management does not necessarily mean pain elimination but rather attainment of a mutually agreed-on pain-relief goal that allows patients to control their pain instead of the pain controlling them.
Nursing Process
Apply the nursing process and use a critical thinking approach in your care of patients. The nursing process provides a clinical decision-making approach for you to develop and implement an individualized plan of care.
Nurses approach pain management systematically to understand and treat a patient’s pain. Successful management of pain depends on establishing a relationship of trust among health care providers, patient, and family. Pain management extends beyond pain relief, encompassing the patient’s quality of life and ability to work productively, enjoy recreation, and function normally in the family and society.
The American Nurses Association (ANA) (2005) upholds that pain assessment and management is within the scope of every nurse’s practice. Thus the ANA offers a certification examination in pain management to staff nurses (http://www.aspmn.org/certification). Several clinical guidelines are available for managing pain in specific disorders. Guidelines are available through the American Pain Society (APS) on the management of pain in the primary care setting; sickle cell pain; cancer pain in adults and children; and pain in osteoarthritis, rheumatoid arthritis, and juvenile chronic arthritis. Sigma Theta Tau International offers guidelines for the older adult on their website (www.geriatricpain.org). In addition, the National Guidelines Clearinghouse (www.guideline.gov) posts a variety of pain-management guidelines, including ones on acute, chronic, spinal, chest, low back, cancer, and pancreatic pain.
Assessment
During the assessment process, thoroughly assess each patient and critically analyze findings to ensure that you make patient-centered clinical decisions required for safe nursing care.
Through the Patient’s Eyes
Many people view pain as a part of life. Some patients experience it for hours or days before seeking health care assistance. They often expect and even accept a certain amount of pain while being hospitalized. Asking patients about their tolerable pain level is the first step in helping them regain control. Assessing previous pain experiences and effective home interventions provides a foundation on which you can build. Patients expect nurses to accept their reports of pain and be prompt in meeting their pain needs.
When assessing pain, be sensitive to the level of discomfort and determine what level will allow your patient to function. For example, when caring for a patient with pain, you ask, “What level of pain will allow you to walk down the hall?” The patient answers that walking is possible when pain is at a level of 2 on a scale of 0 to 10, with 0 being no pain and 10 being worst pain imaginable. You then focus efforts on decreasing the pain to that level. If pain is acute or severe, it is unlikely that the patient is able to provide a detailed description of the entire experience. During an episode of acute pain you primarily assess its location, severity, and quality. Collect a more detailed acute pain assessment when the patient is more comfortable (Box 43-5). For patients with chronic pain, a thorough pain assessment includes affective, cognitive, behavioral, spiritual, and social dimensions. In the home care setting family members assess pain. Using the ABCs of pain management is an effective way to manage pain (Box 43-6).
Because pain is not static but dynamic, you monitor it on a regular basis along with other vital signs. Some institutions treat pain as the fifth vital sign. Pain assessment is not simply a number. Relying solely on a number is unsafe (Vila et al., 2005). Although pain assessment is a nursing function, nursing assistive personnel (NAP) also screen for pain (Schulman-Green et al., 2005). NAP have the responsibility to inform the nurse immediately when a patient is having pain so the nurse is able to confirm the assessment and begin appropriate treatment.
The ability to establish a nursing diagnosis, decide on appropriate interventions, and evaluate the patient’s response (outcomes) to interventions depends on the fundamental activity of a factual, timely, accurate pain assessment (Fig. 43-4). The core of this complex activity is the exploration of the pain experience through the eyes of the patient. Nurses use a variety of tools to assess nociceptive pain and neuropathic pain (Jensen et al., 2006). The goal in using these tools is to identify how much pain exists without interfering with patient function, not to identify how much pain the patient tolerates.
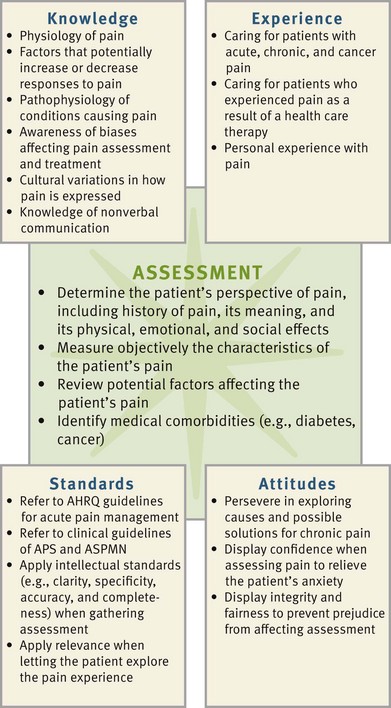
FIG. 43-4 Critical thinking model for pain assessment. AHRQ, Agency for Healthcare Research and Quality; ANA, American Nurses Association; ASPMN, American Society for Pain Management Nursing.
The Agency for Healthcare Research and Quality (AHRQ) established specific guidelines for assessing patients with acute and cancer pain. The focus is on planning successful pain-management interventions before a patient has pain. Because it involves a collaborative approach, the AHRQ pain treatment flow chart (Fig. 43-5) offers a useful conceptual approach to the control of acute pain. Patients need to understand that informed reporting of pain is valuable and necessary if the health care team is to manage it effectively.
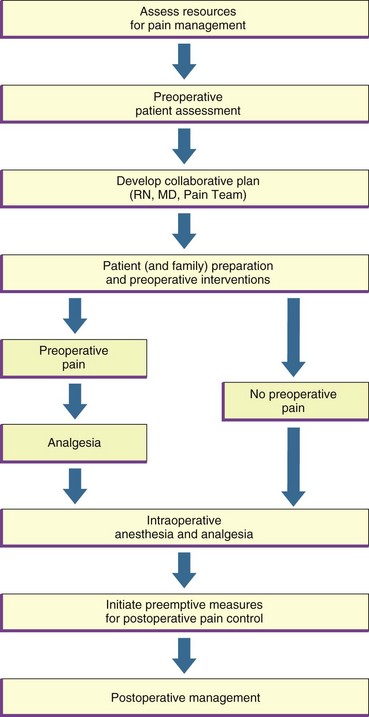
FIG. 43-5 Pain treatment flow chart: preoperative and intraoperative phases. MD, Medical doctor; RN, registered nurse. (From Agency for Health Care Policy and Research, Acute Pain Management Guideline Panel: Acute pain management: operative or medical procedures and trauma, Clinical Practice Guideline, AHCPR Pub No. 92-0032, Rockville, Md, 1992, Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services; and Jacox A et al: Management of cancer pain, Clinical Practice Guideline No. 9, AHCPR Pub No. 94-0592, Rockville, Md, 1994, Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services.)
Always be aware of possible errors in pain assessment (Box 43-7). Using the right tools and methods helps you avoid errors and ensures that you choose the right pain interventions. Failure of clinicians to assess a patient’s pain, accept the findings, and treat the report of pain is a common cause of unrelieved pain and suffering (Hughes, 2008).
Patient’s Expression of Pain
A patient’s self-report of pain is the single most reliable indicator of its existence and intensity (APS, 2003; Pasero and McCaffery, 2011). Pain is individualistic. Many patients fail to report or discuss discomfort. At the same time many nurses believe that patients report pain if they have it. If patients sense that you doubt that pain exists, they share little information about their pain experience or minimize their report. You need to establish a caring therapeutic relationship that allows for open communication. Simple measures such as sitting when talking to patients about pain lets them know that you are sincerely concerned about their pain.
Patients unable to communicate effectively often require special attention during assessment. Children, people who are developmentally delayed, patients who are psychotic, the critically ill, patients with dementia, and patients who do not speak English all require different approaches. Herr et al. (2006a, 2006b) examined various pain behavior assessment tools used with patients who were cognitively impaired. Although no one tool had sufficient reliability and validity, there are clinical practice recommendations (Box 43-8). However, you need to understand that “the number obtained when using a pain-behavior scale is a pain-behavior score, not a pain-intensity rating” (Pasero and McCaffery, 2005). These tools identify the presence of pain but do not determine its intensity.
Patients with cognitive impairments often require simple assessment approaches involving close observation of behavior changes, especially with movement. Patients who are critically ill and have a clouded sensorium or the presence of nasogastric tubes or artificial airways require you to ask specific questions that they can answer with a nod of the head or by writing out a response. If the patient speaks a different language, pain assessment is difficult. An interpreter is often necessary (Pasero and McCaffery, 2011).
Characteristics of Pain
Assessment of common characteristics of pain helps you form an understanding of the type of pain, its pattern, and the types of interventions that bring relief. Use of instruments to quantify the extent and degree of pain depends on a patient being cognitively alert enough to be able to understand your instructions.
Onset and Duration: Ask questions to determine the onset, duration, and sequence of pain. When did it begin? How long has it lasted? Does it occur at the same time each day? How often does it recur?
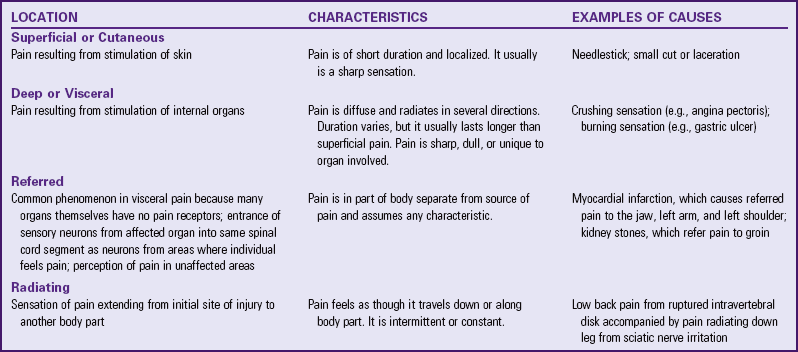
Location: To assess pain location, ask the patient to describe or point to all areas of discomfort. Do not assume that your patient’s pain always occurs in the same location. When describing pain location, use anatomical landmarks and descriptive terminology. The statement “Pain is localized in the upper right abdominal quadrant” is more specific than “The patient states the pain is in the abdomen.” Pain classified by location is superficial or cutaneous, deep or visceral, referred, or radiating (Table 43-5).
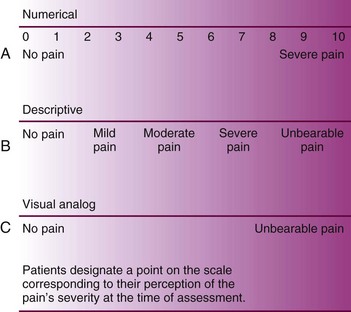
Intensity: One of the most subjective and therefore most useful characteristics for reporting pain is its severity or intensity. Nurses use a variety of pain scales to help patients communicate their pain intensity. Examples of pain intensity scales include the verbal descriptor scale (VDS), the numerical rating scale (NRS), and the visual analogue scale (VAS) (Fig. 43-6). When using the NRS, a report of 0 to 3 indicates mild pain; 4 to 6, moderate pain; and 7 to 10, severe pain, considered a pain emergency (Miaskowski, 2005). These scales work best when assessing pain intensity before and after therapeutic interventions. Many of them are available in several languages to aid nurses when an interpreter is not present (Pasero and McCaffery, 2011). In addition to the current pain level, also ask patients to rate their average pain and the worst pain they have had over the past 24 hours.
Although different patients prefer different pain scales, it is important for you to select and consistently use the same scale with a specific patient. Do not use a pain scale to compare the pain of one patient to that of another.
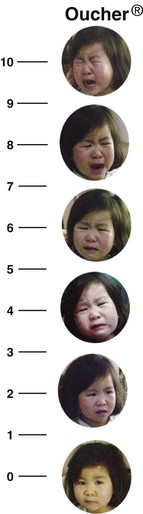
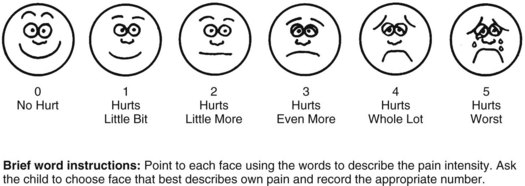
Assessing pain intensity in children requires special techniques. Children’s verbal statements are most important (Hockenberry and Wilson, 2011). Young children do not always know what the word pain means; therefore assessment requires you to use words such as owie, boo-boo, or hurt. Some unique tools are available to measure pain intensity in children. The “Oucher” (Beyer et al., 1992) uses photographs of the face of a child (in increasing levels of discomfort) to cue children into understanding pain and its severity. A child points to a face on the tool, thus simplifying the task of describing the pain. There are ethnic versions of the tool (Fig. 43-7). The FACES scale (Wong and Baker, 1988) assesses pain in verbal children (Fig. 43-8). The scale consists of six cartoon faces ranging from a smiling face (“no hurt”) to increasingly less happy faces; to a final sad, tearful face (“hurts worst”). Children as young as 3 years of age use the scale. Nurses use a variety of other tools to assess pain in neonates, infants, nonverbal toddlers, and children with cognitive impairments.
Quality: Because there is no common or specific pain vocabulary in general use, the words patients choose to describe pain vary. Patients of American descent often use hurt and ache to describe their pain, reserving the word pain for severe discomfort. Always use words other than pain to obtain an accurate report. For example, you say, “Tell me what your discomfort feels like.” The patient likely describes the pain as crushing, throbbing, sharp, or dull. Although a list of descriptive terms is available, it is more accurate to have patients describe the pain in their own words whenever possible.
There is some consistency in the way people describe certain types of pain. The pain associated with a myocardial infarction is often described as crushing or viselike; whereas the pain of a surgical incision is often described as dull, aching, and throbbing, indicating nociceptive pain. Neuropathic pain is usually burning, shooting, or electric-like (Williams, 2006). When a patient’s descriptions fit the pattern forming in the assessment, you then make a clearer analysis of the nature and type of pain. This leads to more appropriate pain management because you treat nociceptive and neuropathic pain differently.
Pain Pattern: Various factors affect the pattern of pain. It helps to assess specific events or conditions that precipitate or aggravate pain. Ask the patient to describe activities that cause pain such as physical movement or food. Also ask him or her to demonstrate actions that cause a painful response such as coughing or turning a certain way. For example, with a ruptured intravertebral disk the low back pain usually radiates down the leg to the foot, and bending over or lifting objects aggravates it. Asking the patient if there is a particular time of day that the pain is worse or if the pain is intermittent, constant, or a combination helps you plan interventions to prevent it from occurring or worsening.
Relief Measures: It is useful to know whether a patient has an effective way of relieving pain such as changing position, using ritualistic behavior (pacing, rocking, or rubbing), eating, meditating, praying, or applying heat or cold to the painful site. The patient’s methods are ones you can use for treatment. Patients gain trust when they know you are willing to try their relief measures. They also gain a sense of control over the pain instead of the pain controlling them. Assessment of relieving factors includes identification of all the patient’s health care providers (e.g., internist, orthopedist, acupuncturist, chiropractor, or dentist).
Contributing Symptoms: Some symptoms (depression, anxiety, fatigue, sedation, anorexia, sleep disruption, spiritual distress, and guilt) cause worsening of pain. You need to assess for these associated symptoms and evaluate their effects on the patient’s pain perception. Reporting and treating associated symptoms contributes to successful pain management.
Effects of Pain on the Patient: Pain alters a person’s lifestyle and affects psychological well-being. Chronic/persistent pain causes suffering, loss of control, loneliness, disabilities, exhaustion, and impaired quality of life. By recognizing the effects that pain has on patients, you better understand the patient’s experience and provide the best pain management. When a patient is in pain, you need to conduct a focused physical and neurological examination and observe for nonverbal responses to pain (e.g., “grimacing, rigid body posture, limping, frowning, or crying”) (Pasero and McCaffery, 2011). Examine the painful area to see if palpation or manipulation of the site increases pain.
Behavioral Effects: When a patient has pain, assess verbalization, vocal response, facial and body movements, and social interaction. A verbal report of pain is a vital part of assessment. You need to be willing to listen and understand. Many patients are unable to communicate their pain. An infant or a patient who is unconscious, disoriented or confused, aphasic or who speaks a foreign language is unable to explain the pain experience. In these cases it is especially important for you to be alert for behaviors that indicate pain (Box 43-9).
The nonverbal expression of pain either supports or contradicts other information about it. If a woman in labor reports that her labor pains are occurring more frequently and if she begins to massage her abdomen more often, this confirms her report. If a patient reports severe abdominal pain but continues to grasp the chest, a more detailed assessment is necessary.
Influence on Activities of Daily Living: Patients who live with daily pain are less able to participate in routine activities, which results in physical deconditioning. Assessment of these changes reveals the extent of the patient’s disability and adjustments necessary to help patients participate in self-care. Your primary goal as a nurse is to improve patient function.
Ask the patient whether pain interferes with sleep. Some patients experience difficulty in falling asleep and/or staying asleep. The pain awakens the patient during the night and makes it hard to fall back to sleep. Consider giving medications or trying nonpharmacological interventions to promote sleep (see Chapter 42). Do not use medications that promote sleep as a substitute for pain relief.
Depending on the location of the pain, some patients have difficulty independently performing ADLs. For example, some pain restricts mobility to the point at which the patient is no longer able to bathe in a bathtub. Patients with severe arthritis find it painful to grasp eating utensils or lower themselves to a toilet seat. Assess the patient’s need for assistance with self-care activities and collaborate with members of the health care team (e.g., physical and occupational therapy). Also consider the need for family members or friends to assist patients with basic hygiene.
Pain sometimes impairs the ability to maintain normal sexual relations. Include in your assessment the extent to which pain affects the patient’s sexual activity. It also helps to learn whether a patient is physically unable to participate or if pain reduces the desire for sexual intercourse.
Pain threatens a person’s ability to work. The more physical activity required in a job, the greater the risk of discomfort when the pain is associated with movement. Pain related to emotional stress increases in individuals whose jobs involve stressful decision making. Assess the work that patients do and their abilities to function in their jobs. Assess the daily chores of homemakers in the same manner as the duties involved in jobs outside the home. Also assess whether it is necessary for patients to stop activity occasionally because of pain, and then help them select ways to minimize or control it so they are able to remain productive.
Include an assessment of the effect of pain on social activities. Some pain is so debilitating that the patient becomes too exhausted to socialize. Identify the patient’s normal social activities, the extent to which activities have been disrupted, and the desire to participate in these activities.
Nursing Diagnosis
You make an accurate diagnosis only after you have performed a complete assessment. The development of an accurate nursing diagnosis for a patient in pain results from thorough data collection and analysis (Box 43-10). Careful assessment reveals the presence or potential for pain. In addition, examine the patient’s history for recent procedures or preexisting painful conditions.
The nursing diagnosis focuses on the specific nature of the pain to identify the most useful types of interventions for alleviating it and improving the patient’s function. Acute pain related to physical trauma and acute pain related to natural childbirth processes require very different nursing interventions. Accurate identification of related factors is necessary in choosing appropriate nursing interventions. For example, interventions for acute pain related to physical trauma require pharmacological intervention, whereas acute pain related to natural childbirth processes is sometimes managed more appropriately with nonpharmacological interventions such as controlled breathing techniques.
Your assessment often directs you to diagnoses other than that of acute or chronic pain. The extent to which pain affects a patient’s function and general state of health determines whether other nursing diagnoses are relevant. For example, your assessment reveals that a patient has pain of the hands and shoulders as a result of crippling arthritis for over 3 years. As a result the patient is unable to remove or fasten necessary items of clothing. The nursing diagnoses for this patient are dressing/grooming self-care deficit and chronic pain. The diagnosis of self-care deficit requires involvement by members of the interdisciplinary health care team to provide the patient with assistive devices for performing self-care. Examples of other diagnoses that are applicable to patients experiencing pain include the following:
Planning
During the planning step of the nursing process, you synthesize information from multiple resources. Critical thinking ensures that the patient’s plan of care (see the Nursing Care Plan) integrates all that you know about the individual patient and key critical thinking elements (Fig. 43-9, p. 978). Professional standards are especially important to consider when you develop a plan of care. These standards establish evidence-based guidelines for selecting effective nursing interventions. Professional standards of care regarding pain management are available as agency policies or through professional organizations such as the American Society for Pain Management Nursing (ASPMN).
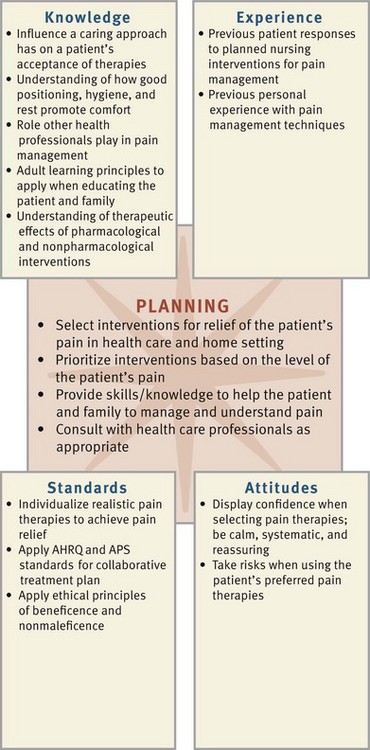
FIG. 43-9 Critical thinking model for pain management planning. AHRQ, Agency for Healthcare Research and Quality; APS, American Pain Society.
Another effective method for planning care is a concept map. Patients who are in pain frequently have interrelated problems. As one problem gets worse, other aspects of a patient’s level of health also change. The concept map helps you determine how the nursing diagnoses are interrelated with one another and linked to the patient’s medical diagnosis. Using the example here, as you plan care for the patient with rheumatoid arthritis, note the relationships among acute pain, impaired physical mobility, dressing and feeding self-care deficit, and fatigue (Fig. 43-10). Identifying these relationships helps you develop a holistic and patient-centered plan of care.
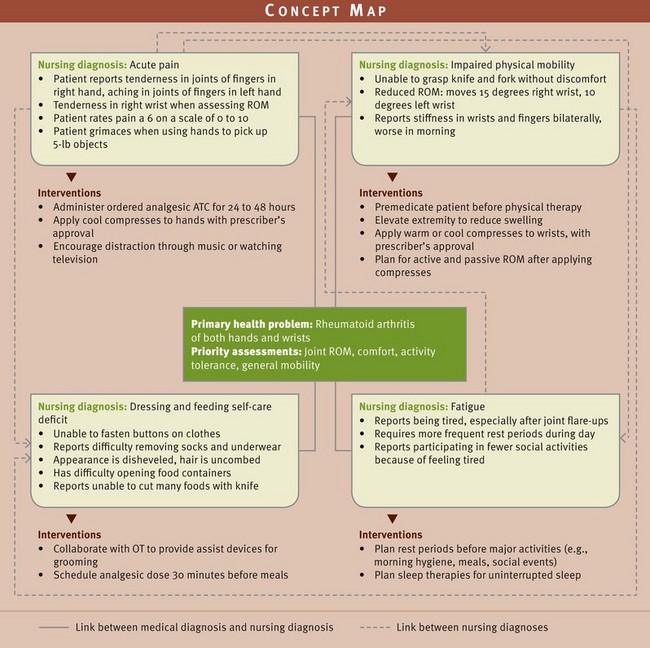
FIG. 43-10 Concept map for Mrs. Mays. ATC, Around the clock; OT, occupational therapist; ROM, range of motion.
Goals and Outcomes
When managing pain, goals of care promote a patient’s optimal function. Determine, along with the patient, what the pain has prevented the patient from doing. Then decide on a mutually acceptable level of pain that allows return of function. An indication of the success of the plan is determined through attainment of goals and outcomes. For example, for the goal “the patient will achieve a satisfactory level of pain relief within 24 hours,” the following are possible outcomes:
Setting Priorities
When setting priorities in pain management, consider the type of pain the patient is experiencing and the effect that it has on various body functions. Work with the patient to select interventions that are appropriate. For example, if an analgesic relieves acute pain, center your attention on how the pain is affecting your patient’s activity, appetite, and sleep. In contrast, when a patient’s pain continues to be severe, preventing you from implementing other interventions, immediate pain relief is the obvious priority. Your priorities change as a patient’s pain experience changes.
Teamwork and Collaboration
A comprehensive plan includes a variety of resources for pain control. Resources available include advanced practice nurses, doctors of pharmacology (PharmDs), physical therapists, occupational therapists, and clergy. An oncology or pain clinical nurse specialist is very familiar with pharmacological and nonpharmacological interventions that are most effective for chronic/persistent pain. PharmDs are knowledgeable about pharmacological treatments of pain. Physical therapists plan exercises that strengthen muscle groups and lessen pain in affected areas. Occupational therapists devise splints to support painful body parts. Clergy members help patients focus on spiritual health. It is important to involve the family in the plan of care because they often administer care in the home after discharge. If the pain-management plan is not successful in achieving the identified pain relief goal, talk with the patient’s health care provider about revising it. Consultation with a pain expert is sometimes necessary.
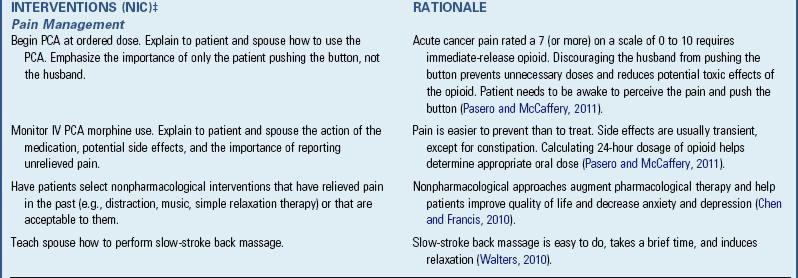
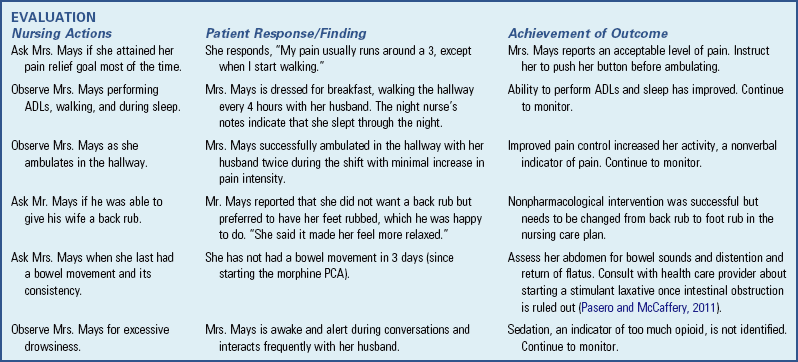
Implementation
Pain therapy requires an individualized approach, perhaps more so than any other patient problem. The nurse, patient, and frequently the family are partners in pain management. Nurses administer and monitor interventions ordered by health care providers for pain relief in addition to complementary pain-relief measures. Usually you try the least invasive or safest therapy first along with previously used successful patient remedies. If there is a question about a medical therapy, consult with the health care provider.
Health Promotion
Patients are better prepared to handle almost any situation when they understand it. The experience of pain is no exception. However, patients with moderate-to-severe pain are not always able to participate in the decision-making process until the pain is controlled at an acceptable level. Once you accomplish this, you are able to begin teaching.
Because pain affects physical and mental functioning, holistic health approaches are important interventions for maintaining wellness. Holistic health is an ongoing state of wellness that involves taking care of the physical self, expressing emotions appropriately and effectively, using the mind constructively, being creatively involved with others, and becoming aware of higher levels of consciousness (American Holistic Health Association, 2007). The concept of holistic health parallels the values of nursing in maintaining the integrity of the whole person.
Patients actively participate in their own well-being whenever possible. Common holistic health approaches include wellness education, regular exercise, rest, attention to good hygiene practices and nutrition, and management of interpersonal relationships. When a person develops pain, you can offer nonpharmacological and pharmacological strategies. Several of the nonpharmacological interventions are nurse initiated.
Nonpharmacological Pain-Relief Interventions: A number of nonpharmacological interventions lessen pain; however, they are to be used with, and not in place of, pharmacological measures (Gruener and Lande, 2006; Hughes, 2008). Nonpharmacological interventions include cognitive-behavioral and physical approaches. Cognitive-behavioral interventions change patients’ perceptions of pain, alter pain behavior, and provide patients with a greater sense of control. Distraction, prayer, relaxation, guided imagery, music, and biofeedback are examples. Physical approaches aim to provide pain relief, correct physical dysfunction, alter physiological responses, and reduce fears associated with pain-related immobility. Chiropractic therapy and acupuncture/acupressure therapy are examples (see Chapter 32). Complementary and alternative medicine (CAM) therapies such as therapeutic touch also help to alleviate pain in some patients. The Agency for Health Care Policy and Research guidelines for acute pain management (AHCPR, 1992) cite nonpharmacological interventions to be appropriate for patients who meet the following criteria:
• Find such interventions appealing
• Possibly benefit from avoiding or reducing drug therapy
• Are likely to experience and need to cope with a prolonged interval of postoperative pain
• Have incomplete pain relief after use of pharmacological interventions
Relaxation and Guided Imagery: Relaxation and guided imagery allow patients to alter affective-motivational and cognitive pain perception. Relaxation is mental and physical freedom from tension or stress that provides individuals a sense of self-control. You use relaxation techniques at any phase of health or illness. Physiological and behavioral changes associated with relaxation include the following: decreased pulse, blood pressure, and respirations; heightened awareness; decreased oxygen consumption; a sense of peace; and decreased muscle tension and metabolic rate. Relaxation techniques include meditation, yoga, Zen, guided imagery, and progressive relaxation exercises (see Chapter 32). For effective relaxation, teach techniques only when a patient is not distracted by acute discomfort. Sometimes you need to use a combination of these techniques to achieve optimal pain relief. With practice the patient performs relaxation exercises independently.
Distraction: The reticular activating system inhibits painful stimuli if a person receives sufficient or excessive sensory input. With sufficient sensory stimuli, a person ignores or becomes unaware of pain. Persons who are bored or in isolation have only their pain to think about and thus perceive it more acutely. Distraction directs a patient’s attention to something other than pain and thus reduces awareness of it. One disadvantage of distraction is that, if it works, health care providers or family members question the existence or severity of the pain. Distraction works best for short, intense pain lasting a few minutes such as during an invasive procedure or while waiting for an analgesic to work. Use activities enjoyed by the patient as distractions (e.g., singing, praying, listening to music, humor or laughter therapy, playing games).
Music: Music treats acute or chronic pain, stress, anxiety, and depression (Allred et al., 2010). It diverts a person’s attention away from the pain and creates a relaxation response. Music therapy uses all kinds of music. It is important to let patients select the type of music they prefer. Music produces an altered state of consciousness through sound, silence, space, and time. Therapeutic sessions usually last 20 to 30 minutes (Hughes, 2008). Patients use earphones to enhance their concentration on the music. This allows patients to adjust the volume of the music without interrupting other patients or staff. Evidence shows that music decreases the use of analgesics in some postoperative patients (Engwall and Duppils, 2009).
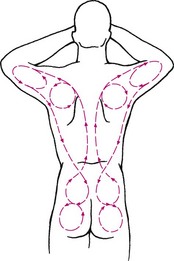
Cutaneous Stimulation: Stimulation of the skin helps relieve pain. A massage, warm bath, ice bag, and transcutaneous electrical nerve stimulation (TENS) stimulate the skin to reduce pain perception (Pain Management Center Staff, 2002). How cutaneous stimulation works is unclear. One suggestion is that it causes release of endorphins, thus blocking the transmission of painful stimuli. The gate-control theory suggests that cutaneous stimulation activates larger, faster-transmitting A-beta sensory nerve fibers. This closes the gate, thus decreasing pain transmission through small-diameter C fibers (Melzack and Wall, 1965).
Cutaneous stimulation gives patients and families some control over pain symptoms and treatment in the home. Using it properly helps to reduce muscle tension, resulting in less pain. When using cutaneous stimulation, eliminate sources of environmental noise, help the patient to assume a comfortable position, and explain the purpose of the therapy. Do not use it directly on sensitive skin areas (e.g., burns, bruises, skin rashes, inflammation, and underlying bone fractures).
Massage is effective for producing physical and mental relaxation, reducing pain, and enhancing the effectiveness of pain medication. Massaging the back, shoulders, hands, and/or feet for 3 to 5 minutes relaxes muscles and promotes sleep and comfort. Cutshall et al. (2010) reported a significant decrease in pain, anxiety, and tension in patients with cardiac problems who received a 20-minute massage. In older adults slow back massage and a 20-minute hand massage improved pain, anxiety, tension, and insomnia (Harris and Richards, 2010). Massages communicate caring and are easy for family members or other health care personnel to learn (Box 43-11).
Cold and heat applications (see Chapter 48) relieve pain and promote healing. The selection of heat versus cold interventions varies with patients’ conditions (McCarberg and O’Connor, 2004). For example, moist heat helps to relieve the pain from a tension headache, and cold applications reduce the acute pain from inflamed joints. When using any form of heat or cold application, instruct the patient to avoid injury to the skin by checking the temperature and not applying cold or heat directly to the skin. Especially at risk are patients with spinal cord or other neurological disorders, older adults, and patients who are confused.
Cold therapies are particularly effective for pain relief. Ice massage involves the use of a large ice cube or a small paper cup filled with water and frozen (water rises out of the cup as it freezes to create a smooth surface of ice for massage). A nurse or the patient applies the ice with firm pressure to the skin, which is covered with a lightweight cloth. Then you use a slow, steady, circular massage over the area. You apply cold near the pain site, on the opposite side of the body corresponding to the pain site, or on a site located between the brain and the pain site. Each patient responds differently to the site of application. Application near the actual site of pain tends to work best. A patient feels cold, burning, and aching sensations and numbness. When numbness occurs, remove the ice for usually 5 to 10 minutes. Cold is effective for tooth or mouth pain when you place the ice on the web of the hand between the thumb and index finger. This point on the hand is an acupressure point that influences nerve pathways to the face and head. Cold applications are also effective before invasive needle punctures.
Heat application is more effective for some patients. You use heating pads, warm compresses, or commercial pillows that are warmed in the microwave. Teach patients to check the temperature of the compress and not to lie on the heating element, because burning can occur.
Another form of cutaneous stimulation is transcutaneous electrical nerve stimulation (TENS), involving stimulation of the skin with a mild electrical current passed through external electrodes (Melzack and Wall, 2003). The therapy requires an order from a health care provider. The TENS unit consists of a battery-powered transmitter, lead wires, and electrodes. Place the electrodes directly over or near the site of pain. Remove any hair or skin preparations before attaching the electrodes. The patient turns the transmitter on when feeling pain. This creates a buzzing or tingling sensation. The patient adjusts the intensity and quality of skin stimulation and applies the tingling sensation until pain relief occurs. TENS is effective for postsurgical and procedural pain control.
Herbals: Many patients use herbals such as echinacea, ginseng, ginkgo biloba, and garlic supplements despite a lack of evidence supporting their use in pain relief (Wirth et al., 2005). Herbals often interact with prescribed analgesics; thus ask patients to report all substances they take to relieve pain (Yoon and Schaffer, 2006) (see Chapter 32).
Reducing Pain Perception: One simple way to promote comfort is to remove or prevent painful stimuli (Box 43-12). This is especially important for patients who are immobilized or have difficulty expressing themselves. For example, your patient becomes constipated and has abdominal distention and cramping. As the nurse you intervene to ensure that the normal elimination process continues: increasing fluids, ambulating the patient, and/or requesting stool softeners or laxatives. Another example involves reducing pain perception in the way you perform procedures. Always consider the patient’s condition, aspects of the procedure that are uncomfortable, and techniques to avoid causing pain. In a patient with severe arthritic knee pain who has severe discomfort during any extreme flexion of the knee, take precautions before walking the patient to the bathroom. Use an elevated toilet seat to allow the patient to sit and rise with minimal discomfort.
Acute Care
Acute Pain Management: Nurses often care for patients who have acute pain resulting from invasive procedures (e.g., surgery) or trauma. The AHCPR established a pain treatment flow chart in 1992 that is still used today (Fig. 43-11) for treatment of postoperative pain and pain from medical procedures and trauma. This systematic approach ensures quick caregiver response to patient discomfort. The key to success is ongoing evaluation of interventions: Does the patient feel relief? Are there any unacceptable side effects from the medications? It is the responsibility of the health care team to collaborate to find the combination of therapy that works best for a patient.
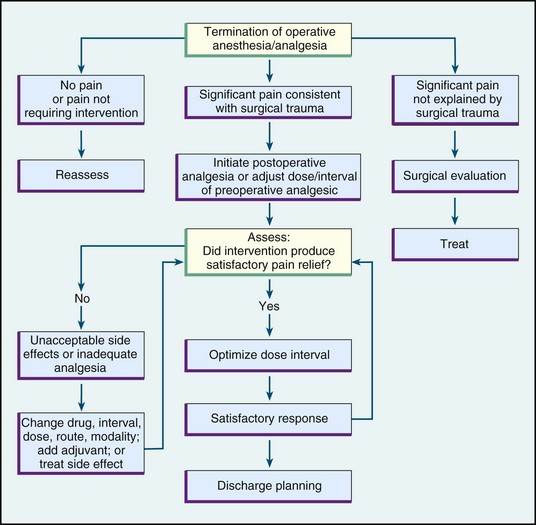
FIG. 43-11 Pain treatment flow chart: postoperative phase. (From Agency for Health Care Policy and Research, Acute Pain Management Guideline Panel: Acute pain management: operative or medical procedures and trauma, Clinical Practice Guideline, AHCPR Pub No. 92-0032, Rockville, Md, 1992, Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services.)
Pharmacological Pain-Relief Interventions: Many pharmacological agents are available to provide pain relief. A nurse’s judgment in the use and management of analgesics helps ensure the best pain relief possible. Unfortunately the ideal analgesic has yet to be developed.
Analgesics: Analgesics are the most common and effective method of pain relief. However, health care providers and nurses still tend to undertreat patients because of incorrect drug information, concerns about addiction, anxiety over errors in using opioid analgesics, and administration of excessive medication. You need to understand the drugs available for pain relief and their pharmacological effects.
There are three types of analgesics: (1) nonopioids, including acetaminophen and nonsteroidal antiinflammatory drugs (NSAIDs); (2) opioids (traditionally called narcotics); and (3) adjuvants, a variety of medications that enhance analgesics or have analgesic properties that were originally unknown (Pasero and McCaffery, 2011).
Acetaminophen (Tylenol) is considered one of the most tolerated and safest analgesics available. It has no antiinflammatory effects, and its action is unknown. Its major adverse effect is hepatotoxicity. It is in a variety of over-the-counter (OTC) cold, flu, and allergy remedies. The maximum 24-hour dose is 4 g (the same dose limitation for aspirin). It is often combined with opioids (e.g., Percocet [oxycodone], Vicodin [hydrocodone], Lortab [hydrocodone], and Ultracet [tramadol]) because it reduces the dose of opioid needed to achieve successful pain control. You treat overdoses of acetaminophen with acetylcysteine (Mucomyst) (Pasero and McCaffery, 2011).
Nonselective NSAIDs such as aspirin and ibuprofen provide relief for mild-to-moderate acute intermittent pain such as the pain associated with a headache or muscle strain. Treatment of mild-to-moderate postoperative pain begins with an NSAID unless contraindicated (Pasero and McCaffery, 2011). NSAIDs most likely inhibit the synthesis of prostaglandins (Lehne, 2010) and thus inhibit cellular responses to inflammation. Most NSAIDs act on peripheral nerve receptors to reduce transmission of pain stimuli and inflammation. Unlike opioids, NSAIDs do not depress the central nervous system, nor do they interfere with bowel or bladder function (Pasero and McCaffery, 2011). However, chronic NSAID use in the older patient is not recommended because it is associated with more frequent adverse effects (gastrointestinal bleeding and renal insufficiency). Mild-to-moderate musculoskeletal pain in older adults is effectively managed with the acetaminophen (AGS, 2002; Pasero and McCaffery, 2011). Some patients with asthma or an allergy to aspirin are also allergic to other NSAIDs (Kaufman, 2010). Some NSAIDs are available over-the-counter (OTC); thus advise patients to discuss the use of OTC NSAIDs to manage pain with their health care provider (D’Arcy, 2006).
Current evidence shows nonselective NSAIDs are safe when taken for short periods. Some patients who took selective COX-2 inhibitors for longer periods experienced heart attacks and strokes; thus Celebrex is the only selective COX-2 inhibitor currently available. The rest are no longer available on the market. Celebrex is not to be used in patients with a sulfa allergy.
Opioid or opioid-like analgesics are generally prescribed for moderate-to-severe pain. These analgesics act on higher centers of the brain and spinal cord by binding with opiate receptors to modify perceptions of pain. A rare adverse effect of opioids in opioid-naive patients is respiratory depression. Respiratory depression is only clinically significant if there is a decrease in the rate and depth of respirations from the patient’s baseline assessment (Pasero and McCaffery, 2011). Patients who are breathing deeply rarely have clinical respiratory depression. Sedation, another adverse effect of opioids, always occurs before respiratory depression. Thus closely monitor for sedation in opioid-naive patients (Pasero and McCaffery, 2011).
If a patient experiences respiratory depression, administer naloxone (Narcan) (0.4 mg diluted with 9 mL saline) intravenous push (IVP) at a rate of 0.5 mL every 2 minutes until the respiratory rate is greater than 8 breaths/min with good depth. Administering naloxone faster than recommended possibly causes severe pain and serious complications (Pasero and McCaffery, 2011). Reassess patients who receive naloxone every 15 minutes for 2 hours following drug administration because its duration is less than that of the opioid and respiratory depression sometimes returns.
Additional adverse effects of opioids include nausea, vomiting, constipation, itching, urinary retention, myoclonus, and altered mental processes (Ersek et al., 2004). Except for constipation, these side effects usually stop once a patient receives an opioid around the clock (ATC) for 4 to 10 days. Consider patients to be opioid naive until this point and opioid tolerant after about a week of ATC opioid dosing.
One way to maximize pain relief while potentially decreasing drug use is to administer analgesics on an ATC rather than a prn basis. The American Pain Society (APS, 2003) supports ATC administration if pain is anticipated for the majority of the day.
According to the American Geriatrics Society (AGS, 2002), opioids are probably not used enough with older persons. The AGS suggests a “start-low” (dose) and “go-slow” (upward dose titration) philosophy. Furthermore, do not use meperidine in older adults (AGS, 2002; Pasero and McCaffery, 2011). Meperidine (Demerol) is not recommended as an analgesic at any age because of its toxic metabolite, normeperidine, which causes seizures (APS, 2003; Pasero and McCaffery, 2011).
The proper use of analgesics requires careful assessment and critical thinking in the application of pharmacological principles and logic (Box 43-13). A person’s response to an analgesic is highly individualized. If the pain is caused by inflammation, an NSAID is sometimes as effective as, or more effective than, an opioid. An orally administered analgesic usually has a longer onset and duration of action than an injectable form. In addition, controlled- or extended-release opioid formulations (morphine [MS Contin, Kadian, Avinza], oxycodone [OxyContin], and methadone) are available for administration every 8 to 12 hours ATC; they are not ordered prn.
You need to know the comparative potencies of analgesics in oral and injectable form. In addition, know the route of administration most effective for a patient so controlled, sustained pain relief is achieved. If nurses on succeeding shifts choose different routes for the same dose, the patient does not receive the same level of analgesia; and pain control will be poor. Equianalgesic charts (i.e., charts converting one opioid to another or parenteral forms of opioids [e.g., morphine to hydromorphone] to oral forms ([or vice versa]) are available on most nursing units or by contacting pharmacy staff.
Before administering opioids, it is important to consider a patient’s situation, including current treatments, diseases/conditions, and/or organ (kidneys/liver) function. Opioid doses often need to be adjusted up or down according to patient circumstances. Situations requiring special considerations include breastfeeding mothers, patients on dialysis, those with neurological or respiratory conditions, and patients with recent abdominal surgery.
The Joint Commission requires health care agencies to have range-order policies in place to guide nurses in selecting the most appropriate dose of a medication. “Range orders are medication orders in which the dose varies over a prescribed range depending on the situation or the patient’s status” (Manworren, 2006). An example is “Administer 5 to 10 mg morphine sulfate IVP for acute pain.” Such an order is dangerous when there are no clinical guidelines to use for selecting the exact dose. Range orders give nurses the flexibility needed to treat patients’ pain in a timely way while allowing for differences in patient response to pain and analgesia. Safe and effective range orders consider the patient’s age, pain intensity, and co-morbidities; avoid frequency ranges; and prescribe a maximum dose that is at least two times but not more than four times the minimum dose in the range (Pasero et al., 2007; ASPMN, 2004).
Adjuvants are drugs originally developed to treat conditions other than pain but also have analgesic properties. For example, tricyclic antidepressants (e.g., nortriptyline [Pamelor]), anticonvulsants (e.g., gabapentin [Neurontin]), and infusional lidocaine successfully treat neuropathic pain. Corticosteroids relieve pain associated with inflammation and bone metastasis. Other examples of adjuvants are bisphosphonates and calcitonin given for bone pain (Pasero and McCaffery, 2011).
Sedatives, antianxiety agents, and muscle relaxants have no analgesic effect; however, they often cause drowsiness and impaired coordination, judgment, and mental alertness and contribute to respiratory depression. It is important to avoid attributing these adverse effects solely to opioids.
Patient-Controlled Analgesia: When patients depend on nurses for prn analgesia, an erratic cycle of alternating pain and analgesia often occurs. The patient feels pain and asks for medication, but you must first assess the patient and then prepare the medication. Under this circumstance analgesia finally occurs in about an hour, but pain relief may last only 30 minutes. Gradually the patient again feels discomfort, and the cycle begins again. The patient is constantly going in and out of analgesic therapeutic range.
A drug delivery system called patient-controlled analgesia (PCA) is a safe method for pain management that many patients prefer (Skill 43-1 on pp. 990-992). It is a drug delivery system that allows patients to self-administer opioids (morphine, hydromorphone, and fentanyl) with minimal risk of overdose. The goal is to maintain a constant plasma level of analgesic to avoid the problems of prn dosing. Systemic PCA traditionally involves IV or subcutaneous drug administration; however, a controlled analgesia device for oral medications, Medication on Demand (MOD), is now available. This device allows patients access to their own oral prn mediations, including opioids and other analgesics, antiemetics, and anxiolytics, at the bedside (Avancen, 2006).
PCA infusion pumps are portable and computerized and contain a chamber for a syringe or bag that delivers a small, preset dose of opioid (Fig. 43-12). To receive a demand dose, the patient pushes a button attached to the PCA device. Systems are designed to deliver a specified number of doses every 1 to 4 hours (depending on the pump settings) given every 5 to 15 minutes (programmable) to avoid overdoses (APS, 2003). Most pumps have locked safety systems that prevent tampering by patients or family members and are generally safe to be managed in the home. For patients with cancer pain, a low-dose continuous infusion (basal rate) of 0.5 to 1 mg/hr is sometimes programmed to deliver a steady dose of continuous medication (Pasero and McCaffery, 2011).

FIG. 43-12 Patient-controlled analgesia pump with cassette. (Courtesy of Smiths Medical ASD, Inc, St Paul, Minn.)
There are many benefits to PCA use. The patient gains control over pain, and pain relief does not depend on nurse availability. Patients also have access to medication when they need it. This decreases anxiety and leads to decreased medication use. Small doses of medications are delivered at short intervals, stabilizing serum drug concentrations for sustained pain relief.
Patient preparation and teaching is critical to the safe and effective use of PCA devices (Box 43-14). Patients need to understand PCA and be physically able to locate and press the button to deliver the dose. Be sure to instruct family members not to “push the button” for the patient. Use Authorized Agent Controlled Analgesia (AACA) guidelines to authorize a family member or nurse to administer the analgesic, when appropriate (Wuhrman et al., 2006).
Check the IV line and PCA device per institutional policy to ensure proper functioning. Even though patients control administration of analgesics, diligence of the nurse is needed to prevent errors related to programmable PCA devices. In opioid-naive patients, do not increase demand or basal dose and shorten the interval time simultaneously because this increases the risk for oversedation and respiratory depression. Document drug dosages and track medication wastes according to agency policy (Pasero and McCaffery, 2011). PCA basal doses are not recommended for opioid-naive patients following surgery because of the possibility for respiratory depression.
Perineural Local Anesthetic Infusion: You are able to manage pain for a variety of inpatient and outpatient adult and pediatric surgical procedures with perineural infusion pumps (e.g., Breg and On-Q). An unsutured catheter from a surgical wound placed near a nerve or groups of nerves connects to a pump containing a local anesthetic (bupivacaine or ropivacaine). You set the pump on demand or continuous mode, and it is usually left in place for 48 hours. Patients learn how to discontinue the pump at home and bring the catheter to their next health care provider visit. Some patients still need oral analgesics, but perineural infusions often reduce the total dosage (Pasero, 2004).
Topical Analgesics: Topical analgesics such as ELA-Max/LMX and eutectic mixture of local anesthetics (EMLA) are available for children. Apply EMLA via a disk or thick cream to the skin 30 to 60 minutes before minor procedures (e.g., IV start, IM injection) or anesthetic infiltration of soft tissue. Do not place EMLA around the eyes, the tympanic membrane, or over large skin surfaces.
The Lidoderm patch is a topical analgesic effective for cutaneous neuropathic pain in adults. You place three patches, cut to size, on and around the pain site using a 12-hour on, 12-hour off schedule to avoid lidocaine toxicity. Other topical analgesics include ketoprofen patch and capsaicin lotion (Pasero and McCaffery, 2011).
Local and Regional Anesthetics: Local anesthesia is the local infiltration of an anesthetic medication to induce loss of sensation to a body part. Health care providers often use local anesthesia during brief surgical procedures such as removal of a skin lesion or suturing a wound by applying local anesthetics topically on skin and mucous membranes or by injecting them subcutaneously or intradermally to anesthetize a body part. The drugs produce temporary loss of sensation by inhibiting nerve conduction. Local anesthetics also block motor and autonomic functions, depending on the amount used and the location and depth of an injection. Smaller sensory nerve fibers are more sensitive to local anesthetics than are large motor fibers. As a result, the patient loses sensation before losing motor function, and conversely, motor activity returns before sensation.
Local anesthetics cause side effects, depending on their absorption into the circulation. Itching or burning of the skin or a localized rash is common after topical applications. Application to vascular mucous membranes increases the chance of systemic effects such as a change in heart rate.
Regional anesthesia is the injection of a local anesthetic to block a group of sensory nerve fibers. Tissues are anesthetized layer by layer as the surgeon or anesthesia provider introduces the agent into deeper structures of the body. Kinds of regional anesthesia include epidural anesthesia, pudendal blocks, and spinal anesthesia. Epidural analgesia is common for the treatment of acute postoperative pain, labor and delivery pain, and chronic cancer pain (Chumbley and Thomas, 2010). It permits control or reduction of severe pain and reduces the patient’s overall opioid requirement, thus minimizing adverse effects. Epidural analgesia is short or long term, depending on a patient’s condition and life expectancy.
The health care provider administers epidural analgesia into the spinal epidural space (Fig. 43-13) by inserting a blunt-tip needle into the level of the vertebral interspace nearest to the area requiring analgesia. The health care provider advances the catheter into the epidural space, removes the needle, and secures the remainder of the catheter with a dressing. Ensure the catheter is taped securely along the back of the patient. If the catheter is temporary, it is connected to tubing positioned along the spine and over the patient’s shoulder. The end of the catheter is then placed on the patient’s chest for the nurse’s access. Nurse anesthetists, anesthesiologists, and nurses control epidural analgesia, depending on agency policy. Some patients control their demand dose, known as patient-controlled epidural analgesia (PCEA) (Pasero and McCaffery, 2011).
Nursing Implications: You maintain responsibility for providing emotional support to patients receiving local or regional anesthesia by explaining the insertion technique and warning patients that they will temporarily lose sensory function within minutes of injection. In the case of regional anesthesia, motor and autonomic (bowel and bladder control) function are also quickly lost. It is common for patients to fear paralysis because epidural and spinal injections come close to the spinal cord. To reassure the patient, explain that numbness, tingling, and coldness are common. Catheter insertion is painful unless the health care provider numbs the injection site. Prepare patients for such discomfort. Before a patient receives an analgesic, check for allergies. Also check to be sure that the drugs (morphine [Duramorph] and fentanyl [Sublimaze]) administered via the epidural catheter are free of potentially neurotoxic substances such as preservatives and additives. Assess vital signs to monitor systemic effects.
After administration of a local anesthetic, protect the patient from injury until full sensory and motor function return. Patients are at risk for injuring the anesthetized body part without knowing it. For example, after an injection into a joint, warn the patient to avoid using the joint until function returns. For patients with topical anesthesia, avoid applying heat or cold to numb areas. After spinal anesthesia the patient stays in bed until sensory and motor function return. Assist the patient the first time he or she tries to get out of bed.
When managing epidural infusions, connect the catheter to an infusion pump, a port, or reservoir or cap it off for bolus injections. To reduce the risk of accidental epidural injection of drugs intended for IV use, clearly label the catheter epidural catheter. Always administer continuous infusions through electronic infusion devices for proper control. Because of the catheter location, use surgical asepsis to prevent a serious and potentially fatal infection. Notify a patient’s health care provider immediately of any signs or symptoms of infection or pain at the insertion site. Thorough hygiene is necessary during nursing procedures to keep the catheter system clean and dry.
Nursing implications for managing epidural analgesia are numerous (Table 43-6). Do not administer supplemental doses of opioids or sedative/hypnotics because of possible additive central nervous system adverse effects. Monitoring for effects of medications differs, depending on whether infusions are intermittent or continuous. Complications of epidural opioid use include nausea and vomiting, urinary retention, constipation, respiratory depression, and pruritus (Lehne, 2010). When patients receive epidural analgesia, you monitor them as often as every 15 minutes, including assessment of vital signs, respiratory effort, and skin color. Once stabilized, monitoring occurs every hour (refer to agency policy).
The patient needs to receive thorough education about epidural analgesia in terms of the action of the medication and its advantages and disadvantages. Instruct patients about the potential for side effects and to notify you or their health care provider if side effects develop. If the patient requires long-term epidural use, the health care provider tunnels a permanent catheter through the skin. The catheter exits at the patient’s side. Teach a patient on long-term therapy how to safely administer home infusions with minimal ongoing nursing intervention.
Invasive Interventions for Pain Relief: When severe pain persists despite medical treatment, invasive interventions available for consideration include intrathecal implantable pumps or injections, spinal cord stimulators, deep brain stimulation, neuroablative procedures (cordotomy, rhizotomy, thalamotomy), trigger point injections, radiofrequency ablation, cryoablation, intradiscal electrothermal (IDET) annuloplasty, vertebroplasty, and intraspinal medications (opioids, steroids, local anesthetics, alpha agonists). It is not acceptable to tell a patient with severe unrelieved pain that there is “nothing more we can do for you.” Refer patients with pain unresponsive to medications to a pain expert.
Procedure Pain Management: The Thunder Project II (Puntillo et al., 2001) identified several procedures causing pain in critical care patients: turning, wound drain removal, tracheal suctioning, femoral catheter removal, placement of a central line, and changing of nonburn wound dressings.
Premedicating patients before painful procedures allows patients to cooperate more fully and reduces the experience of pain. The American Society of Anesthesiologists practice guidelines (2004) recommend premedicating patients before surgery as part of a multimodal analgesic pain management program.
Chronic Noncancer and Cancer Pain Management: Cancer pain is either chronic or acute. The AHCPR published clinical practice guidelines for cancer pain management in 1994 that continue to be a reference today (Lehne, 2010). The guidelines support comprehensive and aggressive treatment of cancer pain, including many options for pain relief (Fig. 43-14). The best choice of treatment often changes as the patient’s condition and the characteristics of pain change. You can use nonpharmacological interventions with pharmacological interventions.
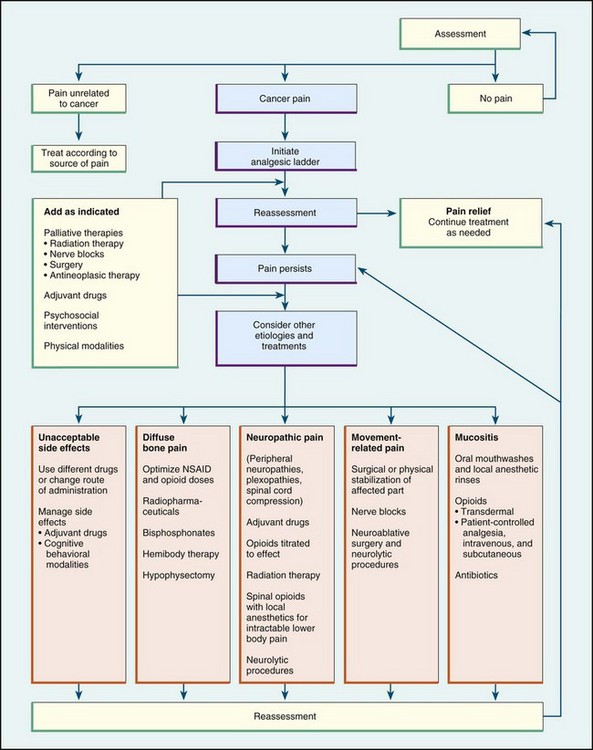
FIG. 43-14 Flow chart: continuing pain management in patients with cancer. NSAID, Nonsteroidal antiinflammatory drug. (From Jacox A et al: Management of cancer pain, Clinical Practice Guideline No. 9, AHCPR Pub No. 94-0592, Rockville, Md, 1994, Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services.)
Various medications and routes of administration provide relief for patients with cancer pain. Long-acting or controlled-release medications are very successful in managing all types of chronic pain. These controlled-released medications (e.g., morphine [MS Contin, Roxanol SR], and oxycodone [OxyContin]) relieve pain for 8 to 12 hours. A 72-hour fentanyl patch is also available. You can manage most chronic pain by using oral or patch medications. Do not use the intramuscular route for controlling pain because the injection is painful and there is inconsistent, erratic drug absorption (Pasero and McCaffery, 2011).
Estimates of addiction in patients with persistent pain range from 6% to 10% (Pasero and McCaffery, 2011). Patients with persistent pain requiring prolonged opioid administration sometimes develop an opioid tolerance. As a result, patients require higher doses of opioids to attain pain relief. The higher opioid dose is not lethal because patients also develop a tolerance to respiratory depression.
It is necessary to give patients with chronic pain required analgesics on a regular basis. Prescribing analgesics on a prn basis for chronic pain is ineffective and causes more suffering. The patient with chronic pain needs to take an analgesic ATC, even when the pain subsides. Regular administration maintains therapeutic drug blood levels for ongoing pain control.
Administering analgesics to treat chronic pain requires applying principles different from those used to treat acute pain. The World Health Organization (Pasero and McCaffery, 2011) recommends a three-step approach to managing cancer pain (Fig. 43-15). Therapy begins with using NSAIDs and/or adjuvants and progresses to strong opioids if pain persists. Side effects of opioids such as nausea and constipation are treated aggressively so patients are able to continue using them. Patients usually become tolerant to their side effects, with the exception of constipation. Routinely administer stimulant laxatives, not simple stool softeners, to prevent and treat constipation.
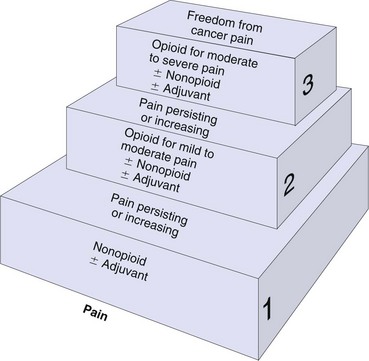
FIG. 43-15 WHO analgesic ladder is a three-step approach in treating cancer pain, accessed 9/27/10 from http://www.who.int/cancer/palliative/painladder/en/.
Transdermal fentanyl, which is 100 times more potent than morphine, is available at predetermined doses that provide analgesia for 48 to 72 hours. The transdermal route is useful when patients are unable to take drugs orally. Fentanyl patches are only used with patients who are opioid tolerant. Patients find this system easy to use because it allows for continuous opioid administration without needles or pumps. Self-adhesive patches release the medication slowly over time, achieving effective analgesia. Transdermal fentanyl is not for adult patients who weigh less than 100 pounds (too little subcutaneous tissue for absorption) or who are hyperthermic (increases drug absorption). Do not place heating pads over the patch and never cut it. To dispose of the patch, fold in half, adhesive side onto itself, and flush down the toilet (Pasero and McCaffery, 2011).
A transmucosal fentanyl “unit” now exists to treat breakthrough pain (Box 43-15) in opioid-tolerant patients. Breakthrough pain is a transient flare of moderate-to-severe pain superimposed on continuous or persistent pain. Swab the fentanyl unit in the mouth over the buccal mucosa and gums. The unit remains intact to dissolve in the mouth, not chewed. Allow to absorb over a 15-minute period, delaying swallowing as long as possible. Use no more than two units per breakthrough pain episode. If the patient’s pain is not relieved after two units, notify the patient’s health care provider (Pasero and McCaffery, 2011).
Administer analgesics rectally when patients are unable to swallow, have nausea or vomiting, or are near death. This route is contraindicated for patients with diarrhea or cancerous lesions involving the anus or rectum. Morphine, hydromorphone, and oxymorphone are available in suppositories (Pasero and McCaffery, 2011).
Some patients use PCA devices to treat severe cancer pain in the home or acute care setting. PCA devices provide improved, uniform pain control with fewer peaks and valleys in plasma concentration, more effective drug action, and lower drug dosages overall. Patients who usually benefit from continuous infusions include those with severe pain for whom oral and injectable medications provide minimal relief, those with severe nausea and vomiting, and those unable to swallow oral medications.
When a patient first receives continuous-drip opioids, the IV access needs to be patent and without complications (see Chapter 41). A central-line catheter such as a Groshong or Hickman catheter, an implanted venous access port, or a peripherally inserted central catheter is usually best for long-term IV infusion. When IV access is poor, the subcutaneous route with a concentrated dose is possible. When infusions begin, monitor the patient very closely for the first hour and then according to agency policy. Patients who are placed on continuous analgesic infusions are opioid tolerant; thus respiratory depression is rare.
Barriers to Effective Pain Management: Barriers to effective pain management are complex, involving the patient, health care provider, and health care system (Box 43-16). Some health care providers require opioid agreements and random urine testing from patients who need long-term opioid therapy. However, evidence of the effectiveness of agreements is lacking, and there are ethical concerns about using them for all patients who require long-term opioid therapy (Arnold et al., 2006). This raises the question as to whether agreements protect patients or health care providers.
Patients and health care providers often do not understand the differences between physical dependence, addiction, and drug tolerance (Box 43-17). Experiencing a physical dependency does not imply addiction, and drug tolerance in and of itself is not the same as addiction. That is not to say that addiction does not occur or that true addicts should not be treated for pain. “Patients with addictive disease and pain have the right to be treated with dignity, respect, and the same quality of pain assessment and management as all other patients” (ASPMN Position Statement, 2002). Nurses and health care providers need to avoid labeling patients as drug seeking because this term is poorly defined and can cause bias and prejudice. If you are concerned that a patient is abusing opioids, voice your concerns to the patient and notify the patient’s health care provider, explaining the reasons for your concern.
Follow recommendations for the management of acute pain in patients dependent on opioids who are not necessarily addicted (Mehta and Langford, 2006). A study of patients who had addictions and pain revealed that they did not feel respected by nurses who cared for them (Morgan, 2006). These patients used presentation (try to be nice and thank the nurse) and self-management strategies (do not get angry or make waves) to obtain pain relief.
Placebos: Placebos are medications or procedures that produce positive or negative effects in patients. These effects are not related to the specific physical or chemical properties of the placebo. Professional organizations discourage their use to treat pain. It is considered unethical and deceitful to administer them. Placebo use jeopardizes the trust between patients and their caregivers. If a placebo is ordered, you must question the order. Many health care agencies have policies that limit the use of placebos to research only (Pasero and McCaffery, 2011).
Restorative and Continuing Care
Pain Clinics, Palliative Care, and Hospices: Health professionals recognize pain as a significant health problem. Growth of pain centers, palliative care departments, and hospices designed to manage pain and suffering has increased. The Commission on Accreditation of Rehabilitation Facilities (CARF) accredits chronic pain treatment programs and sets standards for chronic pain management. A comprehensive pain center treats persons on an inpatient or outpatient basis. Staff members representing all health care disciplines (e.g., nursing, medicine, physical therapy, pastoral care, and dietetics) work with patients to find the most effective pain-relief measures. A comprehensive clinic provides not only diverse therapy but also research into new treatments and training for professionals.
Many hospitals have palliative-care departments to help patients and their family members successfully manage their diseases (Morrison et al., 2005). The goal of palliative care is to learn to live life fully with an incurable condition (see Chapter 36). Patients and their family members need ongoing assistance in managing their pain at home. A National Patient Safety Goal (TJC, 2011) recommends standardizing communication when a patient transfers into, out of, and within the medical system. Teaching pain management during discharge and ensuring continuation of pain management after discharge is essential.
Hospices are programs that care for patients at the end of life (see Chapter 36). The emphasis is on quality of life over quantity (Douglass et al., 2004). Hospice helps terminally ill patients continue to live at home or in a health care setting in comfort and privacy. Pain control is a priority for hospices. Under the guidance of hospice nurses, families learn to monitor patients’ symptoms and become the primary caregivers. Some hospice patients become hospitalized, such as in the event of a brief acute care crisis or family problem.
Hospice programs help nurses overcome their fears of contributing to a patient’s death when administering large doses of opioids. The American Nurses Association supports aggressive treatment of pain and suffering even if it hastens a patient’s death (Fowler, 2010). Recent research suggests that moderate opioid dose increases in patients who are terminally ill do not hasten death (Bengoechea et al., 2010). The disease, not the opioid, is killing the patient.
Evaluation
Evaluate patients’ perceptions of the effectiveness of interventions used to relieve pain. Patients help decide the best times to attempt pain treatments. Essentially they are the best judge of whether a pain-relief intervention works. Often the family is another valuable resource, particularly in the case of a patient with pain who is not able to express discomfort. Also ask patients about tolerance to therapy and the overall amount of relief obtained. If patients state that an intervention is not helpful or even aggravates the discomfort, stop it immediately and seek an alternative. Time and patience are necessary to maximize the effectiveness of pain management. Educate the patient about what to expect. Reassure the patient that you will check back frequently to assess for changes in pain level. Continually assess whether the character of the patient’s pain changes and whether individual interventions are effective.
Patient Outcomes
Evaluation of pain is one of many nursing responsibilities that require effective critical thinking (Fig. 43-16). A patient’s behavioral responses to pain-relief interventions are not always obvious. Evaluating the effectiveness of a pain intervention requires you to evaluate the patient’s pain after an appropriate period of time. For instance, oral medications usually peak in about 1 hour; whereas IVP medications peak in 15 to 30 minutes. Ask the patient if the medication alleviated the pain when it was peaking. Do not expect the patient to volunteer the information. Evaluate psychological and physiological responses to pain (e.g., “Does your pain ever cause you to get depressed or angry?”).
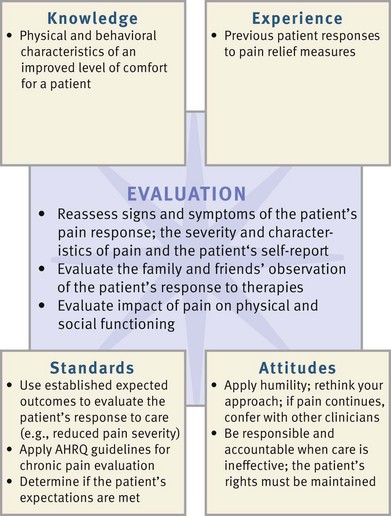
FIG. 43-16 Critical thinking model for pain-management evaluation. AHRQ, Agency for Healthcare Research and Quality.
If you evaluate that a patient continues to have discomfort after an intervention, try a different approach. For example, if an analgesic provides only partial relief, add relaxation exercises or guided-imagery exercises. You also consult with the patient’s health care provider about increasing the dose, decreasing the interval between doses, or trying different analgesics. If patient outcomes are not met, ask the patient:
• What is your current pain level?
• How far away is your pain level from your goal?
• What side effects are you experiencing from your pain medication?
• Describe limitations in function you are experiencing related to uncontrolled pain.
• How is your pain limiting or altering your rest and sleep?
Effective communication of your assessment of a patient’s pain and the response to intervention is facilitated by accurate and thorough documentation. This communication needs to happen from nurse to nurse, shift to shift, and nurse to other health care providers. It is your professional responsibility as the nurse caring for the patient to report the effectiveness of interventions for managing the patient’s pain and evaluation of patient care goals and outcomes. A variety of tools such as a pain flow sheet or diary help centralize information about pain management. The patient expects you to be sensitive to his or her pain and to be attentive in attempts to manage that pain. Effectively communicating with colleagues (Box 43-18) helps you achieve optimal pain relief for patients.
Safety Guidelines for Nursing Skills
Ensuring patient safety is an essential role of the professional nurse. To ensure patient safety, communicate clearly with members of the health care team, assess and incorporate the patient’s priorities of care and preferences, and use the best evidence when making decisions about your patient’s care. When performing the skills in this chapter, remember the following points to ensure safe, individualized patient care.
• The patient is the only person who should press the button to administer the pain medication when using PCA.
• Monitor the patient for signs and symptoms of oversedation and respiratory depression.
Skill 43-1: Patient-Controlled Analgesia ![]()
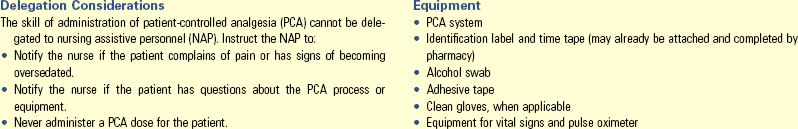
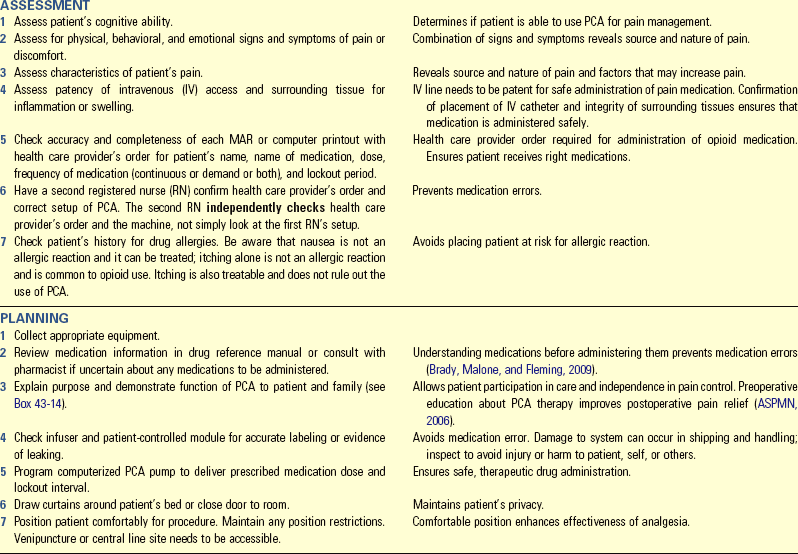
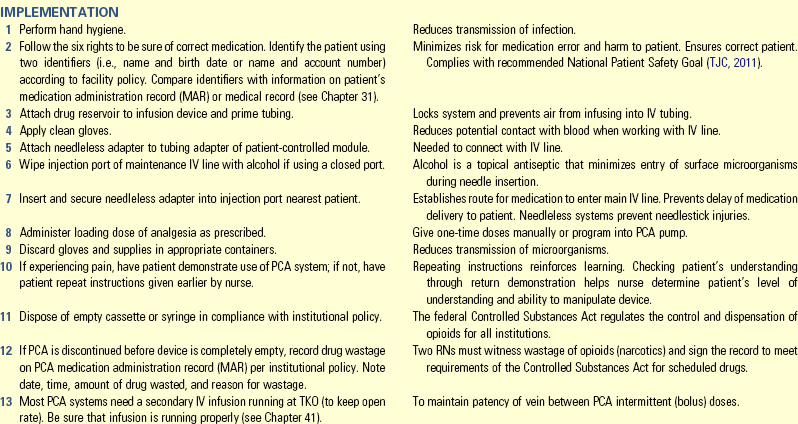
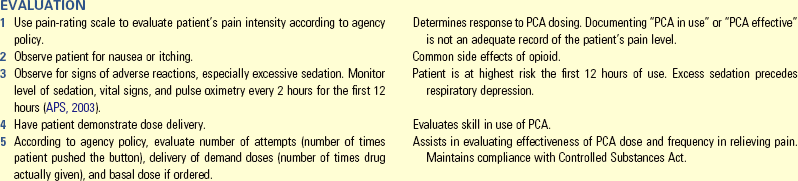
Unexpected Outcomes and Related Interventions:
1. Patient verbalizes continued or worsening discomfort or displays nonverbal behaviors indicative of pain, suggesting that underlying condition has changed or patient is undermedicated.
• Perform complete pain assessment.
• Inspect IV site for possible catheter occlusion or infiltration.
2. Patient is not readily arousable.
• Stop PCA, elevate head of bed unless contraindicated, and assess vital signs. Do not leave the patient’s bedside.
3. Patient unable to manipulate PCA device to maintain pain control.
• Consult with health care provider regarding alternative medication route.
• Discuss with health care provider possible basal (continuous) dose.
• Assess patient support system for significant other who can responsibly manipulate PCA device (ASPMN, 2006).
Key Points
• Pain is a purely subjective physical and psychosocial experience.
• Misconceptions about pain often result in doubt about the degree of the patient’s suffering and unwillingness to provide relief.
• Knowledge of the nociceptive pain processes of the pain experience—transmission, transduction, perception, and modulation—provides guidelines for selecting pain-relief measures.
• An interaction of psychological and cognitive factors affects pain perception.
• A person’s cultural background influences the meaning of pain and how it is expressed.
• It is common for older patients not to report pain.
• Patients who are in chronic pain are unlikely to show behavioral changes.
• The difference between acute and chronic pain involves the concept of harm. Acute pain is protective, thus preventing harm; chronic pain is no longer protective.
• Do not collect an in-depth pain history when the patient is experiencing severe discomfort.
• Pain causes physical signs and symptoms similar to those of other diseases.
• Individualize pain interventions by collaborating closely with the patient, using assessment findings, and trying a variety of interventions.
• Eliminating sources of painful stimuli is a basic nursing measure for promoting comfort.
• Using a regular schedule around-the-clock (ATC) for analgesic administration is more effective than an as-needed schedule in pain control.
• Sedation is an adverse effect of opioids that always precedes respiratory depression (which is rare).
• A PCA device gives patients pain control with low risk of overdose.
• While caring for a patient who receives local anesthesia, protect him or her from injury.
• Nursing implications for administering epidural analgesia include preventing infection and monitoring closely for respiratory depression.
• Addiction rarely occurs in patients who take opioids to relieve pain.
• The goal of pain management is to anticipate and prevent pain rather than treat it.
• Pain evaluation includes measuring the changing character of pain, the patient’s response to interventions, and the patient’s perceptions of the effectiveness of a therapy.
Clinical Application Questions
Preparing for Clinical Practice
After three doses (0.5 mg each) of morphine from the patient-controlled analgesia (PCA) device, Mrs. Mays started vomiting and stated that she was feeling “out of her head.” She rated her chest pain as 3 on a scale of 0 to 10. She is breathing comfortably on 2 L of nasal cannula oxygen, and her lung sounds are clear to auscultation. Her husband is very concerned and anxious about his wife and wants the morphine stopped so she will not become “addicted.”
1. Do you think Mrs. Mays is allergic to morphine? Support your answer.
2. What do you need to tell Mr. and Mrs. Mays about the adverse effects of morphine?
3. Which interventions do you need to complete before consulting the health care provider?
![]() Answers to Clinical Application Questions can be found on the Evolve website.
Answers to Clinical Application Questions can be found on the Evolve website.
Are You Ready to Test Your Nursing Knowledge?
1. Which of the following signs or symptoms in an opioid-naive patient is of greatest concern to the nurse when assessing the patient 1 hour after administering an opioid?
2. A health care provider writes the following order for an opioid-naive patient who returned from the operating room following a total hip replacement. “Fentanyl patch 100 mcg, change every 3 days.” Based on this order, the nurse takes the following action:
1. Calls the health care provider, and questions the order
2. Applies the patch the third postoperative day
3. Applies the patch as soon as the patient reports pain
4. Places the patch as close to the hip dressing as possible
3. A patient is being discharged home on an around-the-clock (ATC) opioid for chronic back pain. Because of this order, the nurse anticipates an order for which class of medication?
4. A new medical resident writes an order for OxyContin SR 10 mg PO q12 hours prn. Which part of the order does the nurse question?
5. The nurse notices that a patient has received oxycodone/acetaminophen (Percocet) (5/325), two tablets PO every 3 hours for the past 3 days. What concerns the nurse the most?
6. A patient with chronic low back pain who took an opioid around-the-clock (ATC) for the past year decided to abruptly stop the medication for fear of addiction. He is now experiencing shaking chills, abdominal cramps, and joint pain. The nurse recognizes that this patient is experiencing symptoms of:
7. After having received 0.2 mg of naloxone (Narcan) intravenous push (IVP), a patient’s respiratory rate and depth are within normal limits. The nurse now plans to implement the following action:
1. Discontinue all ordered opioids
2. Close the room door to allow the patient to recover
3. Administer the remaining naloxone over 4 minutes
4. Assess patient’s vital signs every 15 minutes for 2 hours
8. Which one of the following instructions is crucial for the nurse to give to both family members and the patient who is about to be started on a patient-controlled analgesia (PCA) of morphine?
1. Only the patient should push the button.
2. Do not use the PCA until the pain is severe.
9. A patient with a history of a stroke that left her confused and unable to communicate returns from interventional radiology following placement of a gastrostomy tube. The health care provider’s order reads as follows: “Vicodin 1 tab, per tube, q4 hours, prn.” Which action by the nurse is most appropriate?
1. No action is required by the nurse because the order is appropriate.
2. Request to have the ordered changed to ATC for the first 48 hours.
3. Ask for a change of medication to meperidine (Demerol) 50 mg IVP, q3 hours, prn.
4. Begin the Vicodin when the patient shows nonverbal symptoms of pain.
10. A patient returning to the nursing unit after knee surgery is verbalizing pain at the surgical site. The nurse’s first action is to:
1. Call the patient’s health care provider.
2. Administer pain medication as ordered.
11. The patient rates his pain as a 6 on a scale of 0 to 10, with 0 being no pain and 10 being the worst pain. The patient’s wife says that he can’t be in that much pain since he has been sleeping for 30 minutes. Which is the most accurate resource for assessing the pain?
1. The patient’s wife is the best resource for determining the level of pain since she has been with him continually for the entire day.
2. The patient’s report of pain is the best method for assessing the pain.
3. The patient’s health care provider has the best knowledge of the level of pain that the patient that should be experiencing.
12. When using ice massage for pain relief, which of the following are correct? (Select all that apply.)
1. Apply ice using firm pressure over skin.
2. Apply ice until numbness occurs and remove the ice for 5 to 10 minutes.
3. Apply ice until numbness occurs and discontinue application.
13. When teaching a patient about transcutaneous electrical nerve stimulation (TENS), which information do you include?
1. TENS works by causing distraction.
2. TENS therapy does not require a health care provider’s order.
3. TENS requires an electrical source for use.
4. TENS electrodes are applied near or directly on the site of pain.
14. While caring for a patient with cancer pain, the nurse knows that the World Health Organization (WHO) analgesic ladder recommends:
1. Transitioning use of adjuvants with nonsteroidal antiinflammatory drugs (NSAIDs) to opioids.
2. Using acetaminophen for refractory pain.
3. Limiting the use of opioids because of the likelihood of side effects.
4. Avoiding total sedation, regardless of how severe the pain is.
15. A postoperative patient is currently asleep. Therefore the nurse knows that:
Answers: 1. 2; 2. 1; 3. 2; 4. 2; 5. 3; 6. 4; 7. 4; 8. 1; 9. 2; 10. 4; 11. 2; 12. 1, 2; 13. 4; 14. 1; 15. 1.
References
Ackley, B, Ladwig, G. Nursing diagnosis handbook, ed 9. St Louis: Mosby; 2011.
Agency for Health Care Policy and Research, Acute Pain Management Guideline Panel (AHCPR), Acute pain management: operative or medical procedures and trauma. Clinical Practice Guideline, AHCPR Pub No. 92-0032. Rockville, Md: Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services; 1992.
American Bar Association, Legal guide for the seriously ill 2009. http://apps.americanbar.org/abanet/media/release/news_release.cfm?releaseid=849 [Accessed October 10, 2011].
American Geriatrics Society (AGS). The management of persistent pain in older persons. J Am Geriatr Soc. 2002;50(S6):205.
American Holistic Health Association. Wellness from within: the first step. Anaheim, Calif: The Association; 2007.
American Nurses Association (ANA). Pain management nursing: scope and standards of practice. Silver Spring, Md: The Association; 2005.
American Pain Foundation (APF), Pain care bill of rights 2007. http://www.painfoundation.org/ [Accessed September 25, 2010].
American Pain Society (APS). Principles of analgesic use in the treatment of acute and cancer pain, ed 5. Glenview, Ill: The Society; 2003.
American Pain Society (APS), Definitions related to the use of opioids for the treatment of pain. Glenview, Ill: The Society; 2011. www.ampainsoc.org/advocacy/opioids2.htm
American Society of Anesthesiologists (ASA). Practice guidelines for acute pain management in the perioperative setting. Anesthesiology. 2004;100:1573.
American Society of Anesthesiologists (ASA). Practice guidelines for chronic pain management. Anesthesiology. 2010;112:1.
American Society for Pain Management Nursing (ASPMN), Position statement on pain management in patients with addictive disease. Pensacola, Fla. 2002. http://www.asmpn.org/Organization/documents/AddictiveDisease.pdf
American Society for Pain Management Nursing (ASPMN), Position statement on the use of “as needed” range orders for opioid analgesics in the management of acute pain. Pensacola, Fla. 2004. http://www.asmpn.org/pdfs/As%20Needed%20Range%20Orders.pdf/
American Society for Pain Management Nursing (ASPMN). Patient-controlled analgesia: authorized agent controlled analgesia, a position statement. Pain Manag Nurs. 2006;7(4):134.
Arnold, R, et al. Opioid contracts in chronic nonmalignant pain management: objectives and uncertainties. Am J Med. 2006;119(4):292.
Arnstein, P. Balancing analgesic efficacy with safety concerns in the older adult. Pain Manage Nurs. 2010;11(2):S11.
Avancen, Medication on demand 2006. http://www.avancen.com [Accessed November 26, 2011].
Chou, R, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113.
Chumbley, G, Thomas, S. Care of the patient receiving epidural analgesia. Nurs Standard. 2010;25(9):35.
D’Arcy, Y. Hot topics in pain management: using NSAIDs safely. Nursing. 2006;35(2):22.
Douglass, AB, et al. Principles of palliative care medicine. I. Patient assessment. Adv Stud Med. 2004;4(1):15.
Ersek, M, et al. The cognitive effects of opioids. Pain Manag Nurs. 2004;5(2):75.
Fowler, MDM. Guide to the code of ethics for nurses. Silver Spring, Md: American Nurses Association; 2010.
Gruener, D, Lande, S. Pain control in the primary care setting. Glenview, Ill: American Pain Society; 2006.
Herr, K, et al. Pain assessment in the nonverbal patient: position statement with clinical practice recommendations. Pain Manag Nurs. 2006;7(2):44.
Herr, K, et al. Tools for assessment of pain in nonverbal older adults with dementia: a state-of-the-science review. J Pain Symptom Manage. 2006;31(2):170.
Herr, K. Pain in the older adult: an imperative across all health care settings. Pain Manage Nurs. 2010;11(2):S1.
Hockenberry, MJ, Wilson, D. Wong’s nursing care of infants and children, ed 9. St Louis: Mosby; 2011.
prepared with support from the Robert Wood Johnson Foundation. AHRQ Publication No. 08-0043. Hughes RG, ed. Patient safety and quality: an evidence-based handbook for nurses. Rockville, Md: Agency for Healthcare Research and Quality, March 2008.
International Association for the Study of Pain (IASP), Pain terms 2010. http://www.iasp-pain.org/AM/Template.cfm?Section=Pain_Definitions&Template=/CM/HTMLDisplay.cfm&ContentID=1728#Pain [Accessed September 10, 2010].
Kaufman, G. Basic pharmacology of nonopioid analgesics. Nurs Standard. 2010;24(30):55.
Kehlet, H, et al. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367(9522):1618.
Lehne, R. Pharmacology for nursing care, ed 7. Philadelphia: Saunders; 2010.
Manworren, R. A call to action to protect range orders. Am J Nurs. 2006;106(7):65.
Maxwell, T, et al. Palliative and end-of-life pain management: self-directed learning module. Pensacola, Fla: American Society for Pain Management Nursing; 2005.
McCarberg, B, O’Connor, A. A new look at heat treatment for pain disorders, part I. APS Bulletin. 2004;14(6):4.
Mehta, V, Langford, R. Acute pain management for opioid dependent patients. Anaesthesia. 2006;61(3):269.
Melzack, R, Wall, PD. Pain mechanisms: a new theory. Science. 1965;150:971.
Melzack, R, Wall, D. Handbook of pain management. London: Churchill Livingstone; 2003.
Miaskowski, C. The next step to improving cancer pain management. Pain Manag Nurs. 2005;6(1):1.
Morrison, R, et al. The growth of palliative care programs in United States hospitals. J Palliat Med. 2005;8(6):1127.
Otis-Green, S, et al. An integrated psychosocial model for cancer pain management. Cancer Pract. 2002;10(S1):58.
Pain Management Center Staff. When your pain flares up: easy, proven techniques for managing chronic pain. Minneapolis: Fairview Press; 2002.
Pasero, C. Perineural local anesthetic infusion. Am J Nurs. 2004;104(7):89.
Pasero, C, McCaffery, M. No self-report means no pain-intensity rating. Am J Nurs. 2005;205(10):50.
Pasero, C, McCaffery, M. Pain assessment and pharmacologic management. St Louis: Mosby; 2011.
Pasero, C, et al. Pain control: IV opioid range orders for acute pain management. Am J Nurs. 2007;107(2):52.
Schulman-Green, D, et al. Unlicensed staff members’ experiences with patients’ pain on an inpatient oncology unit: implications for redesigning the care delivery system. Cancer Nurs. 2005;28(5):340.
Shaw, S. Nursing and supporting patients with chronic pain. Nurs Stand. 2006;20(19):60.
The Joint Commission (TJC), 2011 National Patient Safety Goals (NPSG) 2011. http://jointcommission.org/Patient/Safety/NationalPatient/SafetyGoals/ [Accessed January 31, 2011].
Vila, H, et al. The efficacy and safety of pain management before and after implementation of hospital-wide pain management standards: is patient safety compromised by treatment based solely on numerical pain ratings? Anesth Analg. 2005;101(2):474.
Williams, H. Assessing, diagnosing and managing neuropathic pain. Nurs Times. 2006;102(16):22.
Wirth, J, et al. Use of herbal therapies to relieve pain: a review of efficacy and adverse effects. Pain Manag Nurs. 2005;6(4):145.
Wong, DL, Baker, CM. Pain in children: comparison of assessment scales. Oklahoma Nurse. 1988;33(1):8.
Wuhrman, E, et al, Authorized and unauthorized (“PCA by PROXY”) dosing of analgesic infusion pumps 2006. http://www.aspmn.org/organization/documents/PCAbyProxy-final-ew_004.pdf [Accessed October 10, 2011].
Yoon, S, Schaffer, S. Herbal, prescribed, and over-the-counter drug use in older women: prevalence of drug interactions. Geriatr Nurs. 2006;27(2):118.
Research References
Allred, K, et al. The effect of music on postoperative pain and anxiety. Pain Manage Nurs. 2010;11(1):15.
Bengoechea, I, et al. Opioid use at the end of life and survival in a hospital at home unit. J Palliat Med. 2010;13(9):1079.
Beyer, JE, et al. The creation, validation, and continuing development of the Oucher: a measure of pain intensity in children. J Pediatr Nurs. 1992;7(5):335.
Brady, A, Malone, A, Fleming, S. A literature review of the individual and systems factors that contribute to medication errors in nursing practice. J Nurs Manage. 2009;17(6):679.
Chen, Y, Francis, A. Relaxation and imagery for chronic, nonmalignant pain: effects on pain symptoms, quality of life, and mental health. Pain Manage Nurs. 2010;11(3):159.
Cutshall, SM, et al. Effect of massage therapy on pain, anxiety, and tension in cardiac surgical patients: a pilot study. Complement Ther Clin Pract. 2010;16(2):92.
Engwall, M, Duppils, GS. Music as a nursing intervention for postoperative pain: a systematic review. J PeriAnesth Nurs. 2009;24(6):370.
Harris, M, Richards, KC. The physiological and psychological effects of slow-stroke back massage and hand massage on relaxation in older people. J Clin Nurs. 2010;19(7-8):917.
Herr, K, Titler, M. Acute pain assessment and pharmacological management practices for the older adult with a hip fracture: review of ED trends. J Emerg Nurs. 2009;35(4):312.
Jensen, M, et al. The validity of the neuropathic pain scale for assessing diabetic neuropathic pain in a clinical trial. Clin J Pain. 2006;22(1):97.
Juarez, P, et al. Comparison of two pain scales for the assessment of pain in the ventilated adult patient. Dimens Crit Care Nurs. 2010;29(6):307.
Kato, K, et al. Importance of genetic influences on chronic widespread pain. Arthritis Rheum. 2006;54:1682.
Morgan, B. Knowing how to play the game: hospitalized substance abusers’ strategies for obtaining pain relief. Pain Manag Nurs. 2006;7(1):31.
Puntillo, K, et al. Patients’ perceptions and responses to procedural pain: results from Thunder Project II. Am J Crit Care. 2001;10(4):238.
Vaartio, H, et al. Nursing advocacy in procedural pain care. Nurs Ethics. 2009;16(3):340.
Walters, SJ. Massage and cancer: practice guidelines. J Aust Traditional Med Soc. 2010;16(3):141.