Chapter 9 The female urinary tract
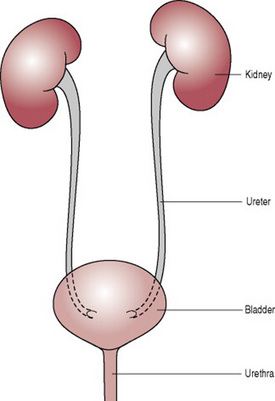
The principal function of the urinary system, together with other body systems, is to maintain homeostasis. One aspect of this function is to rid the body of waste products that accumulate because of cellular metabolism. The urinary tract begins with the kidneys, and continues as a passage for urine in the ureters, the bladder and the urethra.
The kidneys
The kidneys are a pair of bean-shaped excretory glands that have both endocrine and exocrine functions. They are about 10 cm long, 6.5 cm wide and 3 cm thick and weigh around 120 g. Although similar in shape, the left kidney is a longer and more slender organ than the right kidney. Congenital absence of one or both kidneys, known as unilateral or bilateral renal agenesis, can occur.
Functions
The kidneys extract soluble wastes from the blood and excrete excess water and minerals. They also prevent substances that are needed by the body from being lost and have a part to play in red cell production and the maintenance of blood pressure.
Position and relations
The kidneys are in the posterior of the abdominal cavity, one on either side of the spine. They extend approximately from vertebra T12 superiorly to L3 inferiorly and however, because of the contents of the abdominal cavity the right kidney is located slightly lower than the left kidney. The anterior and posterior surfaces of the kidneys are related to numerous structures some of which come into direct contact with the kidneys whereas others are separated by a layer of peritoneum (Drake et al 2005). An adrenal gland sits on top of each kidney.
Supports
The kidneys are maintained in position by a generous packing of perinephric fat and by the closeness of neighbouring organs, particularly parts of the gastrointestinal tract in front and the musculature of the posterior abdominal wall behind.
Structure
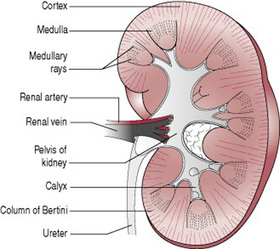
Each kidney has a smooth surface covered by a tough fibrous capsule. There is a concave side facing medially; on this medial aspect is an opening called the hilum from which the renal artery, renal vein, nerves, and lymphatics enter and leave the kidney (Fig. 9.1). Internally the hilum is continuous with the renal sinus.
Each kidney consists of an outer cortex and an inner medulla. The cortex sits directly beneath the kidney’s fibrous capsule. Below the cortex lies the medulla which is divided into pyramids. There are approximately 12 pyramids and they contain bundles of tubules leading from the cortex. The tubules create a lined appearance known as the medullary rays. The base of each pyramid is curved and the cortex arches over it projecting downwards between them forming columns of tissue known as the columns of Bertini. Each pyramid together with the associated overlying cortex forms a renal lobe. The tip of each pyramid, known as a papilla, empties into a calyx, and the calices empty into the renal pelvis. Urine is transmitted from the renal pelvis to the urinary bladder via the ureter.
The nephrons
When the tissue of a normal adult kidney is examined under the microscope the basic functional unit, the nephron, of which there are more than 1 million, can be seen.
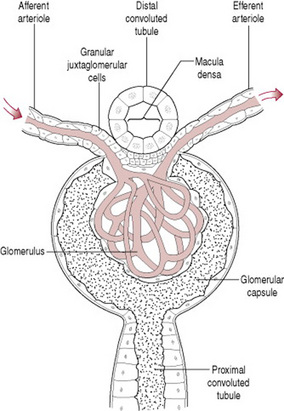
Each nephron starts at a knot of capillaries called a glomerulus (Fig. 9.2). It is fed by a branch of the renal artery, the afferent arteriole, and the blood is collected up again into the efferent arteriole. This is the only place in the body where an artery collects blood from capillaries. The pressure within the glomerulus is raised because the afferent arteriole has a wider bore than the efferent arteriole and this factor forces the filtrate out of the capillaries into the capsule. At this stage, any substance with a small molecular size will be filtered out.
Surrounding the glomerulus is a cup known as the glomerular capsule, into which fluid and solutes are exuded from the blood. The glomerulus and capsule together are known as the glomerular body (Fig. 9.2).
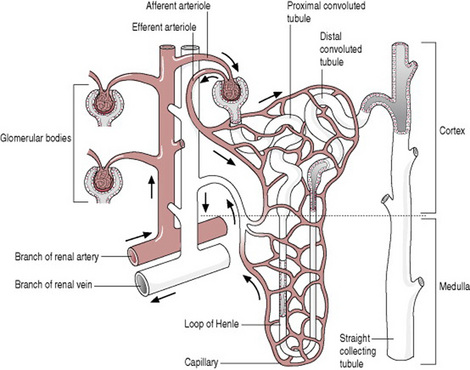
The cup of the capsule is attached to a tubule. The tubule initially winds and twists, then forms a straight loop that dips into the medulla, rising up into the cortex again to wind and turn before joining the straight collecting tubule, which receives urine from several nephrons. The first twisting portion of the nephron is the proximal convoluted tubule, the loop is termed the loop of Henle and the second twisting portion is the distal convoluted tubule. The whole nephron is about 3 cm in length (Fig. 9.3). The straight collecting tubule runs from the cortex to a medullary pyramid; it forms a medullary ray and receives urine from over 4000 nephrons along its length.
The distal convoluted tubule returns to pass alongside granular cells of the afferent arteriole and this part of the tubule is called the macula densa (Fig. 9.2). The two are known as the juxtaglomerular apparatus. The granular cells secrete renin whereas the macula densa cells monitor the sodium chloride concentration of fluid passing through.
Blood supply
The renal arteries are early branches of the descending abdominal aorta and divert about a quarter of the cardiac output into the kidneys. The artery enters at the renal hilum, sends numerous branches into the cortex and forms a glomerulus for each nephron. Blood is collected up and returned via the renal vein.
Lymphatic drainage
A rich supply of lymph vessels lies under the cortex and around the urine-bearing tubules. Lymph drains into large lymphatic ducts that emerge from the hilum and lead to the aortic lymph glands.
Nerve supply
The nerves of the kidney enter by the renal hilum and provide a sympathetic and parasympathetic nerve supply. Although small, there are about 15 in number.
Endocrine activity
The kidney secretes two hormones renin and erythropoietin. Renin is produced in the afferent arteriole and is secreted when the blood supply to the kidneys is reduced and in response to lowered sodium levels. It acts on angiotensinogen, which is present in the blood, to form angiotensin, which raises blood pressure and encourages sodium reabsorption. Erythropoietin stimulates the production of red blood cells.
Urine
The colour of urine ranges from a pale straw colour when very dilute to a dark brown colour when very concentrated. It should never be cloudy. In the newborn baby, it is almost clear. It has a recognizable smell, which in health is not unpleasant when freshly passed. An adult passes between one and 2 L of urine daily, depending on fluid intake.
The specific gravity of urine is 1.010–1.030. It is composed of 96% water, 2% urea and 2% other solutes. Urine is usually acid and contains no glucose or ketones, nor should it carry blood cells or bacteria. Women are susceptible to urinary tract infection but this is usually an ascending infection acquired via the urethra. A low bacterial count less than 100 000/mL is insignificant.
The production of urine
The production of urine takes place in three stages: filtration, reabsorption and secretion.
Filtration
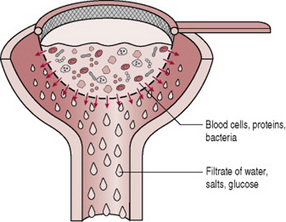
Filtration is the simple process of water and the substances dissolved in it being passed from the glomerulus into the glomerular capsule because of the raised intracapillary pressure. Blood components such as corpuscles and platelets as well as plasma proteins, which are large molecules, are kept in the blood vessel; water, salts and glucose escape through the filter as the filtrate (Fig. 9.4). A vast amount of fluid passes out in this way, about 2 mL per second or 120 mL per minute: 99% of this must be recovered, or the body would be totally drained of fluid within hours.
Reabsorption
The body selects from the filtrate the substances that it needs: water, salts and glucose. The posterior pituitary gland controls the reabsorption of water by producing antidiuretic hormone (ADH). If the body has lost fluid such as in sweating or if fluid intake has been low, more water is conserved and less urine passed, the urine appearing more concentrated. In the opposite circumstances, when the individual has consumed a lot of fluid and is sweating little, the urine is more copious and dilute. However, this is not always the case, for instance following the consumption of alcohol, urine flow increases because alcohol causes the acute inhibition of the release of ADH. The absence of ADH causes segments of the kidney’s tubule system to become impermeable to water, thus preventing it from being reabsorbed into the body (Epstein 1997). Newborn babies’ ability to concentrate and dilute their urine is poor and preterm infants even more so. For this reason they are unable to tolerate wide variations in their fluid intake.
Minerals are selected according to the body’s needs. The reabsorption of sodium is controlled by aldosterone, which is produced in the cortex of the suprarenal gland. The interaction of aldosterone and ADH maintains water and sodium balance. The pH of the blood must be controlled and if it is tending towards acidity then acids will be excreted. However, if the opposite pertains, alkaline urine will be produced. Often this is the result of an intake of an alkaline substance.
The ureters
The ureters are hollow muscular tubes; the upper end is funnel-shaped and merges into the pelvis of the kidney where urine is received from the renal tubules.
Structure
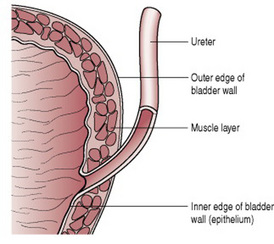
Each tube is about 3 mm in diameter and 25–30 cm long, running from the renal hilum to the posterior wall of the bladder (Fig. 9.5). They descend on the medial aspect of the psoas major muscle. At the pelvic brim, they descend along the side walls of the pelvis to the level of the ischial spines and then turn forwards to pass beside the uterine cervix and enter the bladder from behind passing through the bladder wall at an angle (Fig. 9.6).
Layers
The ureters are composed of three layers: a lining, a muscle layer and an outer coat. The lining is formed of transitional epithelium arranged in longitudinal folds. This type of epithelium consists of several layers of pear-shaped cells and makes an elastic and waterproof inner coat.
The muscular layer is arranged as an inner longitudinal layer, a middle circular layer and an outer longitudinal layer.
The outer coat is of fibrous connective tissue, which is continuous with the fibrous capsule of the kidney.
Blood supply
The upper part of the ureter is supplied similarly to the kidney. In its pelvic portion, it derives blood from the common iliac and internal iliac arteries and from the uterine and vesical arteries, according to its proximity to the different organs. Venous return is along corresponding veins.
The bladder
The bladder is a hollow, muscular, distensible pelvic organ which acts as a reservoir for the storage of urine until it is convenient for it to be voided.
Midwives need to be familiar with the anatomy and physiology of the bladder as pregnancy and childbirth can affect bladder control.
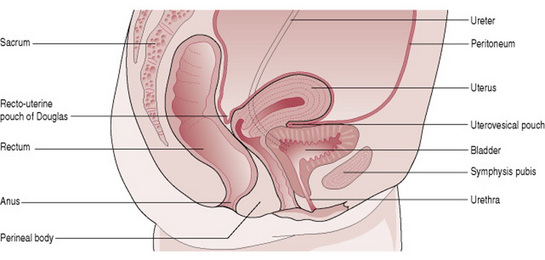
Position, shape and size
The empty bladder lies in the pelvic cavity with its base resting on the upper half of the vagina with its apex directed towards the symphysis pubis. However, as it fills with urine it rises up out of the pelvic cavity becoming an abdominal organ. It can be palpated above the symphysis pubis when full. During labour, the bladder is an abdominal organ as it is displaced by the descent of the fetus into the pelvic cavity.
When empty the bladder is described as being pyramidal, with its base being triangular. When it is full, it becomes more globular in shape as its walls are distended.
The empty bladder is of similar size to the uterus but when full of urine it becomes much larger. Its capacity is around 600 mL but it is capable of holding more, particularly under the influence of pregnancy hormones.
Relations (Fig. 9.7)
Supports
There are five ligaments attached to the bladder. Two lateral ligaments extend from the bladder to the side walls of the pelvis. Two pubovesical ligaments extend from the bladder neck anteriorly to the symphysis pubis with the bladder neck resting on the pubococcygeus muscle. A fibrous band called the urachus extends from the apex of the bladder to the umbilicus.
Structure
The base of the bladder is termed the trigone. It is situated at the back of the bladder, resting against the vagina. Its three angles are the exit of the urethra below and the two slit-like openings of the ureters above. The apex of the trigone is thus at its lowest point, which is also termed the neck (Fig. 9.8).
The anterior part of the bladder lies close to the symphysis pubis and is termed the apex of the bladder. From it, the urachus runs up the anterior abdominal wall to the umbilicus. In fetal life, this is the remains of the yolk sac but in the adult is simply a fibrous band.
Layers
The lining of the bladder, like that of the ureter, is formed of transitional epithelium, which helps to allow the distension of the bladder without losing its water-holding effect. The lining, except over the trigone, is thrown into rugae, which flatten out as the bladder expands and fills. The mucous membrane lining lies on a submucous layer of areolar tissue that carries blood and lymph vessels and nerves.
The epithelium over the trigone is smooth and firmly attached to the underlying muscle.
The musculature of the bladder consists chiefly of the large detrusor muscle whose function is to expel urine. This muscle has an inner longitudinal, a middle circular and an outer longitudinal layer. Around the neck of the bladder, the circular muscle is thickened to form the internal urethral sphincter. The general elasticity of the numerous muscle fibres around the bladder neck tend to keep the urethra closed (Standring et al 2004). In the trigone, the muscles are somewhat differently arranged. A band of muscle between the ureteric apertures forms the interureteric bar. The urethral dilator muscle lies in the ventral part of the bladder neck and the walls of the urethra; it is thought to be of significance in overcoming urethral resistance to micturition (Standring et al 2004).
The outer layer of the bladder is formed of visceral pelvic fascia, except on its superior surface, which is covered with peritoneum (Fig. 9.7).
Blood supply
The vesical arteries are the main suppliers of blood. A few small branches from the uterine and vaginal arteries also bring blood to the bladder. Venous return is through corresponding veins.
Nerve supply
The nerve supply is parasympathetic and sympathetic and comes via the Lee-Frankenhäuser pelvic plexus in the pouch of Douglas. The stimulation of sympathetic nerves causes the internal urethral sphincter to contract and the detrusor muscle to relax, whereas the parasympathetic nerve fibres cause the sphincter to relax and the bladder to empty.
The urethra
The final passage in the urinary tract is the urethra, which is 4 cm long in the female and consists of a narrow tube buried in the outer layers of the anterior vaginal wall. It runs from the neck of the bladder and opens into the vestibule of the vulva as the urethral meatus. During labour, the urethra becomes elongated as the bladder is drawn up into the abdomen; becoming as much as several centimetres longer.
Structure
The urethra forms the junction between the urinary tract and the external genitalia. The epithelium of its lining reflects this. The upper half is lined with transitional epithelium whereas the lower half is lined with squamous epithelium. The lumen is normally closed unless urine is passing down it or a catheter is in situ. When closed, it has small longitudinal folds. Small blind ducts called urethral crypts open into the urethra, of which the two largest are Skene’s ducts, which open just beside the urethral meatus. There is the possibility of them becoming infected with an organism such as the gonococcus.
The submucous coat of the urethra is composed of epithelium, which lies on a bed of vascular connective tissue.
The musculature is arranged as an inner longitudinal layer, continuous with the inner muscle fibres of the bladder, and an external circular layer. The inner muscle fibres help to open the internal urethral sphincter during micturition.
The outer layer of the urethra is continuous with the outer layer of the vagina and is formed of connective tissue.
At the lower end of the urethra, voluntary, striated muscle fibres form the so-called membranous sphincter of the urethra. This is not a true sphincter but it gives some voluntary control to the woman when she desires to resist the urge to urinate. The powerful levator ani muscles, which pass on either side of the uterus, also assist in controlling continence of urine.
Micturition
The bladder fills and then contracts as a reflex response. The internal sphincter opens by the action of Bell’s muscles (Fig. 9.8). If the urge is not resisted, the external sphincter relaxes and the bladder empties. This action, known as micturition, may be speeded by raising intra-abdominal pressure either to initiate the process or throughout voiding.
The urge to pass urine is felt when the bladder contains about 200–300 mL of urine, but also when psychological stimuli operate such as waking after sleep, arriving or leaving home, and from external stimuli such as the sound and feel of water and the feel of the toilet seat. Helpless laughter or paroxysmal coughing may also trigger a desire to empty the bladder. Micturition can be temporarily postponed but the full bladder becomes progressively more uncomfortable.
In newborn babies, there is no resistance to the spontaneous prompting of the bladder that it wishes to be emptied. The sphincters relax, the detrusor muscle contracts and urine is passed. After about 2 years a child learns to resist the urge to void and by adulthood it is taken for granted. Many women, particularly pregnant and parous women, have trouble in maintaining continence under the stress of coughing, laughing, sneezing and other factors that raise intra-abdominal pressure. Regular muscular exercise such as walking, swimming, running and pelvic floor exercises help to raise the tone of the voluntary muscles.
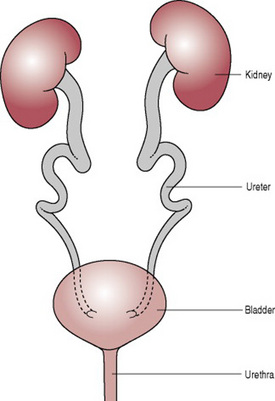
Changes to the urinary tract in pregnancy
In pregnancy, the enlarging uterus affects all the parts of the urinary tract (see Ch. 14) at various times with the hormones of pregnancy having an even greater influence than the mechanical effects. For instance, progesterone relaxes the walls of the ureters and allows dilatation and kinking (Fig. 9.9). In some women, this is quite marked and it tends to result in a slowing down or stasis of urinary flow, making infection a greater possibility. In addition, large amounts of urine are produced because in pregnancy, glomerular filtration is increased as it helps to eliminate the additional wastes created by maternal and fetal metabolism. In the first postpartum days, there is a rapid and sustained loss of sodium and a major diuresis occurs. A midwife will commonly observe a woman who has recently given birth voiding upwards of 1 L on a single occasion.
Drake RL, Wayne V, Mitchell ADM. Gray’s anatomy for students. Edinburgh: Churchill Livingstone, 2005;320-327.
Epstein M. Alcohol’s impact on kidney function. Alcohol Health & Research World, 21. 1997;1:84-93. Online. Available: http://pubs.niaaa.nih.gov/publications/arh21-1/84.pdf, 22nd April 2007
Standring S, Healy J, Johnson D, et al. Gray’s anatomy: the anatomical basis of clinical practice, 39th edn. New York: Churchill Livingstone, 2004.
Beischer NA, Mackay EV. Obstetrics and the newborn, 3rd edn. London: WBSaunders, 1997.
Chapter 38 in this book offers an account of changes in pregnancy with radiological/ultrasound illustrations, as well as addressing urinary tract problems associated with childbearing.
Coad J, Dunstall M. Anatomy and physiology for midwives, 2nd edn. Edinburgh: Churchill Livingstone, 2005.
Chapter 2 of this book gives a very accessible account of the urinary system and a number of examples of clinical applications. A stylized diagram of urine production may help the individual who learns best from visual representation.
Stables D, Rankin J. Physiology in childbearing with anatomy and related biosciences, 2nd edn. Edinburgh: Baillière Tindall, 2004.
This text offers a fuller account of the urinary system, including changes in pregnancy and a short account of the postnatal period.