CHAPTER 5 Major and Minor Connectors
Components of a typical removable partial denture are illustrated in Figure 5-1.

Figure 5-1 A, Framework for mandibular removable partial denture with the following components: 1, lingual bar major connector; 2a, minor connector by which the resin denture base will be attached; 2b, minor connector, proximal plate, which is part of clasp assembly; 2c, minor connector used to connect rests to major connectors; 3, occlusal rests; 4, direct retainer arm, which is part of the total clasp assembly; 5, stabilizing or reciprocal components of clasp assembly (includes minor connectors); and 6, an indirect retainer consisting of a minor connector and an occlusal rest. B, Maxillary removable partial denture with resin denture bases supporting artificial posterior teeth. Bases are attached to metal framework by ladderlike minor connectors similar to those seen in 2a. C, Mandibular bilateral distal extension removable partial denture with resin denture bases supporting artificial posterior teeth.
When a prosthesis that can be removed from the mouth is used, the prosthesis must extend to both sides of the arch. This enables transfer of functional forces of occlusion from the denture base to all supporting teeth and tissues within an arch for optimum stability. It is through this cross-arch tooth contact, which occurs at some distance from the functional force, that optimum resistance can be achieved. This is most effectively accomplished when a rigid major connector joins the portion of the prosthesis receiving the function to selected regions throughout the arch.
The chief functions of a major connector include unification of the major parts of the prosthesis, distribution of the applied force throughout the arch to selected teeth and tissue, and minimization of torque to the teeth. A properly designed rigid major connector effectively distributes forces throughout the arch and acts to reduce the load to any one area while effectively controlling prosthesis movement.
The principle of leverage is connected with this component part. A rigid major connector will limit movement possibilities by acting as a counteracting lever. This phenomenon is referred to as cross-arch stability. Cross-arch stability becomes more important in situations associated with high potential for greater prosthesis movement (e.g., distal extensions).
In this chapter, major and minor connectors are considered separately as to their function, location, and design criteria. Other components are presented in designated chapters.
Role of Major Connectors in Control of Prosthesis Movement
A major connector is the component of the partial denture that connects the parts of the prosthesis located on one side of the arch with those on the opposite side. It is that unit of the partial denture to which all other parts are directly or indirectly attached. This component also provides cross-arch stability to help resist displacement by functional stresses.
The major connector may be compared with the frame of an automobile or with the foundation of a building. It is through the major connector that other components of the partial denture become unified and effective. If the major connector is flexible, the ineffectiveness of connected components jeopardizes the supporting oral structures and can be a detriment to the comfort of the patient. Failure of the major connector to provide rigidity may be manifest by traumatic damage to periodontal support of the abutment teeth, injury to residual ridges, or impingement of underlying tissue. It is the dentist’s responsibility to ensure that appropriate design and fabrication of the major connector are accomplished.
Location
Major connectors should be designed and located with the following guidelines in mind:
Appropriate relief beneath the major connector avoids the need for its adjustment after tissue damage has occurred. In addition to being time consuming, grinding to provide relief from impingement may seriously weaken the major connector, which can result in flexibility or possibly fracture. Major connectors should be carefully designed for proper shape, thickness, and location. Alteration of these dimensions by grinding can only be detrimental. Relief is covered at the end of this chapter and is expanded in Chapter 11.
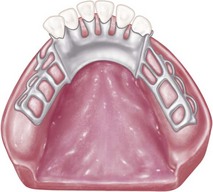
Margins of major connectors adjacent to gingival tissue should be located far enough from the tissue to avoid any possible impingement. To accomplish this, it is recommended that the superior border of a lingual bar connector be located a minimum of 4 mm below the gingival margin(s) (Figure 5-2). At the inferior border of the lingual bar connector, the limiting factor is the height of the moving tissue in the floor of the mouth. Because the connector must have sufficient width and bulk to provide rigidity, a linguoplate is commonly used when space is insufficient for a lingual bar.
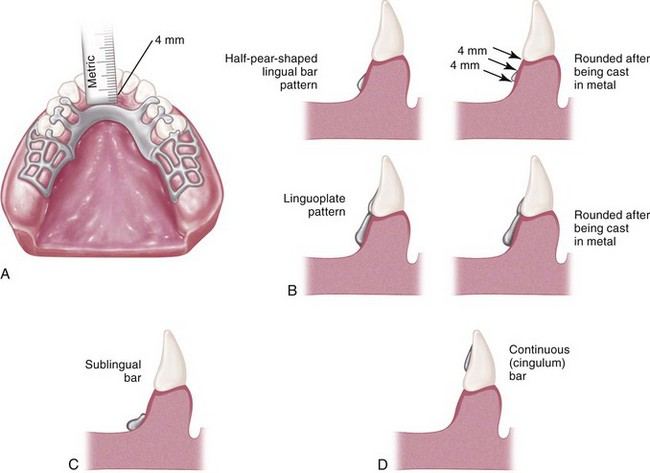
Figure 5-2 A, Lingual bar major connector should be located at least 4 mm inferior to gingival margins and farther if possible. The vertical height of a finished lingual bar should be at least 4 mm for strength and rigidity. If less than 8 mm exists between gingival margins and the movable floor of the mouth, a linguoplate (B), a sublingual bar (C), or a continuous bar (D) is preferred as a major connector. Relief is provided for soft tissue under all portions of the mandibular major connector and at any location where the framework crosses the marginal gingiva. The inferior border of mandibular major connectors should be gently rounded after being cast to eliminate a sharp edge.
In the maxillary arch, because no moving tissue is present in the palate as in the floor of the mouth, the borders of the major connector may be placed well away from gingival tissue. Structurally, the tissue covering the palate is well suited for placement of the connector because of the presence of firm submucosal connective tissue and an adequate, deep blood supply. However, when soft tissue covering the midline of the palate is less displaceable than the tissue covering the residual ridge, varying amounts of relief under the connectors must be provided to avoid impingement of tissue. The amount of relief required is directly proportional to the difference in displaceability of the tissue covering the midline of the palate and the tissue covering the residual ridges. The gingival tissue, on the other hand, must have an unrestricted superficial blood supply to remain healthy. To accomplish this, it is recommended that the borders of the palatal connector be placed a minimum of 6 mm away from and parallel to the gingival margins. Minor connectors that must cross gingival tissue should do so abruptly, joining the major connector at nearly a right angle (Figure 5-3). In this way, maximum freedom is ensured for gingival tissue.
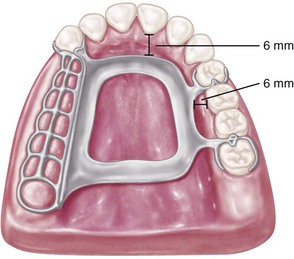
Figure 5-3 Palatal major connector should be located at least 6 mm away from gingival margins and parallel to their mean curvature. All adjoining minor connectors should cross gingival tissues abruptly and should join major connectors at nearly a right angle.
Except for a palatal torus or a prominent median palatal suture area, palatal connectors ordinarily require no relief. Intimate contact between the connector and the supporting tissue adds much to the support, stability, and retention of the denture. Except for gingival areas, intimacy of contact elsewhere in the palate is not detrimental to the health of the tissue if rests are provided on abutment teeth to prevent tissue-ward movement.
An anterior palatal strap or the anterior border of a palatal plate also should be located as far as possible posteriorly to avoid interference with the tongue in the area of the rugae. It should be uniformly thin and its anterior border should be located to follow the contours between the crests of the rugae. The anterior borders of such palatal major connectors therefore will be irregular in outline as they follow the contours between the rugae. The tongue may then pass from one ruga prominence to another without encountering the border of the connector. When the connector border must cross a ruga crest, this should be done abruptly, while avoiding the crest as much as possible. The posterior limitation of a maxillary major connector should be just anterior to the vibrating line. A useful rule applied to major connectors and throughout partial denture design is to try to avoid adding any part of the denture framework to an already convex surface.
Characteristics of major connectors that contribute to the maintenance of health of the oral environment and the well-being of the patient may be listed as shown in Box 5-1.
Mandibular Major Connectors
The six types of mandibular major connectors include the following:
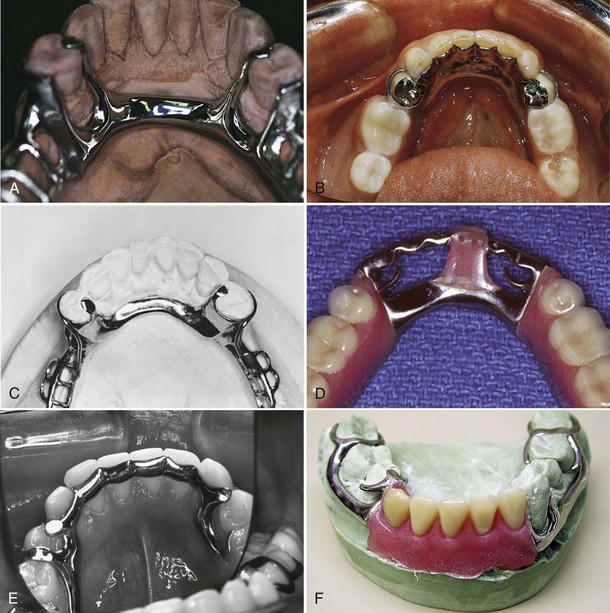
Figure 5-4 Mandibular major connectors. A, Lingual bar. B, Linguoplate. C, Sublingual bar. D, Lingual bar with continuous bar (cingulum bar). E, Cingulum bar. F, Labial bar.
The lingual bar and the linguoplate are by far the most common major connectors used in mandibular removable partial dentures.
Lingual Bar
The basic form of a mandibular major connector is a half-pear shape, located above moving tissue but as far below the gingival tissue as possible. It is usually made of reinforced, 6-gauge, half-pear–shaped wax or a similar plastic pattern (Figure 5-5).
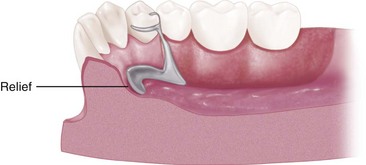
Figure 5-5 Sagittal section showing half-pear shape of lingual bar. A taper of the superior border of the bar to the soft tissues above will minimize interference with the tongue and will be more acceptable to the patient than would a dissimilar contour. Tissue relief is necessary to protect the soft tissue of the floor of the mouth.
The major connector must be contoured so that it does not present sharp margins to the tongue and cause irritation or annoyance by an angular form. The superior border of a lingual bar connector should be tapered toward the gingival tissue superiorly, with its greatest bulk at the inferior border, resulting in a contour that has a half-pear shape. Lingual bar patterns, both wax and plastic, are made in this conventional shape. However, the inferior border of the lingual bar should be slightly rounded when the framework is polished. A rounded border will not impinge on the lingual tissue when the denture bases rotate inferiorly under occlusal loads. Frequently, additional bulk is necessary to provide rigidity, particularly when the bar is long or when a less rigid alloy is used. This is accomplished by lining the ready-made form underneath with a sheet of 24-gauge casting wax rather than altering the original half-pear shape.
The inferior border of a lingual mandibular major connector must be located so that it does not impinge on the tissue in the floor of the mouth because it changes elevations during the normal activities of mastication, swallowing, speaking, licking the lips, and so forth. Yet at the same time, it seems logical to locate the inferior border of these connectors as far inferiorly as possible to avoid interference with the resting tongue and trapping of food substances when they are introduced into the mouth. In addition, the more inferiorly a lingual bar can be located, the farther the superior border of the bar can be placed from the lingual gingival crevices of adjacent teeth, thereby avoiding impingement on the gingival tissue.
At least two clinically acceptable methods may be used to determine the relative height of the floor of the mouth and locate the inferior border of a lingual mandibular major connector. The first method is to measure the height of the floor of the mouth in relation to the lingual gingival margins of adjacent teeth with a periodontal probe (Figure 5-6). When these measurements are taken, the tip of the patient’s tongue should just lightly touch the vermilion border of the upper lip. Recording of these measurements permits their transfer to both diagnostic and master casts, thus ensuring a rather advantageous location of the inferior border of the major connector. The second method is to use an individualized impression tray for which lingual borders are 3 mm short of the elevated floor of the mouth, and then to use an impression material that will permit the impression to be accurately molded as the patient licks the lips. The inferior border of the planned major connector can then be located at the height of the lingual sulcus of the cast resulting from such an impression. Of the two methods, we have found measuring the height of the floor of the mouth to be less variable and more clinically acceptable.
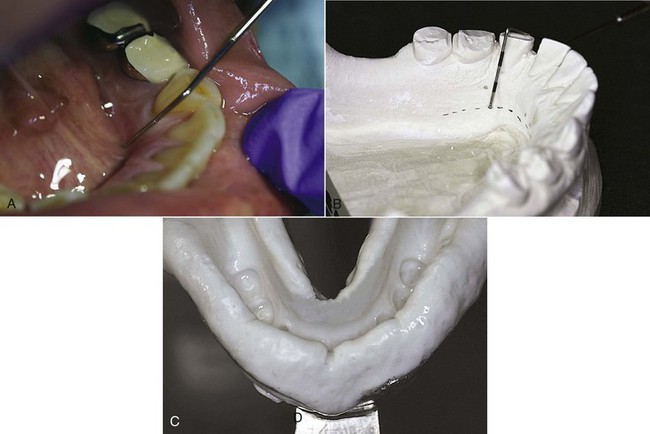
Figure 5-6 A, Height of floor of the mouth (tongue elevated) in relation to lingual gingival sulci measured with a periodontal probe. B, Recorded measurements are transferred to a diagnostic cast and then to a master cast after mouth preparations are completed. The line connecting marks indicates the location of the inferior border of the major connector. If periodontal surgery is performed, the line on the cast can be related to incisal edges of teeth and the measurements recorded for subsequent use. C, Impression made with functional movement of the tongue to demonstrate maximum shortening of the floor of the mouth. This allows visualization of the anatomic feature that establishes the inferior extent of a major connector. If a stock tray causes impingement on this functional position, an individualized or custom tray may be used for the same purpose.
Linguoplate
If the rectangular space is bounded by the lingual bar, the anterior tooth contacts, and the cingula, and the bordering minor connectors are filled in, a linguoplate results (Figure 5-7).

Figure 5-7 View of mandibular Class I design with contoured linguoplate. Linguoplate is made as thin as possible and should follow the lingual contours of the teeth contacted. Doing so will often result in a scalloped superior margin. In this example, the straight superior margin can be bulky at the cingulum region, causing tongue discomfort.
A linguoplate should be made as thin as is technically feasible and should be contoured to follow the contours of the teeth and the embrasures (Figure 5-8). The patient should be aware of as little added bulk and as few altered contours as possible. The upper border should follow the natural curvature of the supracingular surfaces of the teeth and should not be located above the middle third of the lingual surface, except to cover interproximal spaces to the contact points. The half-pear shape of a lingual bar should still form the inferior border that provides the greatest bulk and rigidity. All gingival crevices and deep embrasures must be blocked out parallel to the path of placement to avoid gingival irritation and any wedging effect between the teeth. In many instances, judicious recontouring of the lingual proximal surfaces of overlapped anterior teeth permits closer adaptation of the linguoplate major connector, eliminating otherwise deep interproximal embrasures to be covered (Figure 5-9).

Figure 5-8 Apron of linguoplate (tissue side) is closely adapted to the teeth extending into nonundercut interproximal embrasures, resulting in a scalloped form. When well adapted, this form will benefit from some anterior teeth acting together to help resist horizontal rotational tendencies of the prosthesis, especially if the posterior ridge form does not resist such movement.
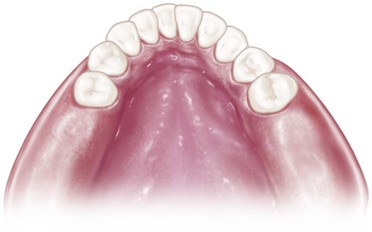
Figure 5-9 If a linguoplate major connector was indicated for this patient with overlapped anterior teeth, judicious recontouring of the lingual proximal surfaces of right lateral, right central, and left lateral incisors would eliminate excessive undercuts and permit closer adaptation of the lingual apron of the major connector.
The linguoplate does not in itself serve as an indirect retainer. When indirect retention is required, definite rests must be provided for this purpose. Both the linguoplate and the cingulum bar ideally should have a terminal rest at each end, regardless of the need for indirect retention. However, when indirect retainers are necessary, these rests may also serve as terminal rests for the linguoplate or continuous bar.
Because no component part of a removable partial denture should be added arbitrarily, each component should be added to serve a definite purpose. Indications for the use of a linguoplate may be listed as follows:
The same reasons for use of a linguoplate anteriorly apply to its use elsewhere in the mandibular arch. If a lingual bar alone is to be used anteriorly, there is no reason to add an apron elsewhere. However, when auxiliary splinting is used for stabilization of the remaining teeth or for horizontal stabilization of the prosthesis, or for both, small rectangular spaces sometimes remain. Tissue response to such small spaces is better when they are bridged with an apron than when they are left open. Generally, the apron is used to avoid gingival irritation or entrapment of food debris or to cover generously relieved areas that would be irritating to the tongue (Figure 5-10).
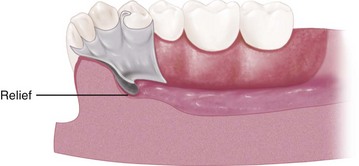
Figure 5-10 Sagittal section through the linguoplate demonstrating a basic half-pear–shaped inferior border with the metallic apron extending superiorly. Extension of linguoplate to the height of contour on the premolar was accomplished to enclose a rather large triangular interproximal space inferior to the contact point between the canine and premolar. Such spaces may often be bridged to eliminate obvious food traps. Relief is provided for soft tissue under all portions of the mandibular major connector and at any location where the framework crosses the marginal gingiva.
Sometimes a dentist is faced with a clinical situation wherein a linguoplate is indicated as the major connector of choice even though the anterior teeth are quite spaced and the patient strenuously objects to metal showing through the spaces. The linguoplate can then be constructed so that the metal will not appreciably show through the spaced anterior teeth (Figure 5-11). The rigidity of the major connector is not greatly altered. However, such a design may be as much of a food trap as the continuous bar type of major connector.
Design of Mandibular Major Connectors
The following systematic approach to the design of a mandibular lingual bar and linguoplate major connectors can be readily used with diagnostic casts after the diagnostic data are considered and related to the basic principles of major connector design:
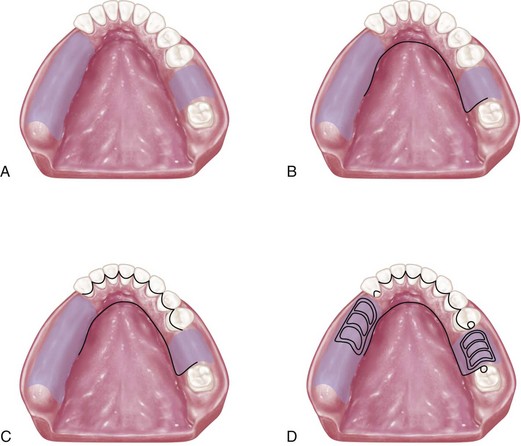
Figure 5-12 Sequence of design considerations for a mandibular major connector. A, Diagnostic cast with basal seat areas outlined. B, Inferior border of the major connector is outlined. Location of the inferior border was determined as suggested in Figure 5-6 and extends to the mesial of the mandibular right molar. C, Superior border of the major connector is outlined. Limited space for the lingual bar requires use of the linguoplate major connector. Linguoplate requires that rest seats be used on canines and the first premolar for positive support. D, Rest seat areas on the posterior teeth are outlined, and minor connectors for retention of resin denture bases are sketched.
Sublingual Bar
A modification of the lingual bar that has been demonstrated to be useful when the height of the floor of the mouth does not allow placement of the superior border of the bar at least 4 mm below the free gingival margin is the sublingual bar. The bar shape remains essentially the same as that of a lingual bar, but placement is inferior and posterior to the usual placement of a lingual bar, lying over and parallel to the anterior floor of the mouth. It is generally accepted that a sublingual bar can be used in lieu of a lingual plate if the lingual frenum does not interfere, or in the presence of an anterior lingual undercut that would require considerable blockout for a conventional lingual bar. Contraindications include interfering lingual tori, high attachment of a lingual frenum, and interference with elevation of the floor of the mouth during functional movements.
Cingulum Bar (Continuous Bar)
When a linguoplate is the major connector of choice, but the axial alignment of the anterior teeth is such that excessive blockout of interproximal undercuts must be made, a cingulum bar may be considered. A cingulum bar located on or slightly above the cingula of the anterior teeth may be added to the lingual bar or can be used independently (Figure 5-13). In addition, when wide diastemata exist between the lower anterior teeth, a continuous bar retainer may be more esthetically acceptable than a linguoplate.
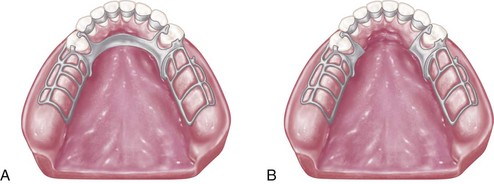
Figure 5-13 A, Lingual bar and cingulum bar (continuous bar) major connector. Upper portion of this major connector is located on the cingula of anterior teeth. The requirement of positive support by rest seats, at least as far anteriorly as the canines, is critical. Note that the superior border of the lingual bar portion is often placed objectionably close to the gingival margins if sufficient bulk for rigidity is to be obtained. This type of major connector easily traps food and is often more objectionable to patients than a linguoplate. B, Cingulum bar (continuous bar) major connector. Although this design may reduce the possibility of food entrapment, it may not provide adequate rigidity.
Labial Bar
Fortunately, in only a few situations does extreme lingual inclination of the remaining lower premolar and incisor teeth prevent the use of a lingual bar major connector. With the use of conservative mouth preparations in the form of recontouring and blockout, a lingual major connector can almost always be used. Lingually inclined teeth sometimes may have to be reshaped by means of crowns. Although the use of a labial major connector may be necessary in rare instances, this should be avoided by resorting to necessary mouth preparations rather than by accepting a condition that is otherwise correctable (Figure 5-14). The same applies to the use of a labial bar when a mandibular torus interferes with placement of a lingual bar. Unless surgery is definitely contraindicated, interfering mandibular tori should be removed so that the use of a labial bar connector may be avoided.
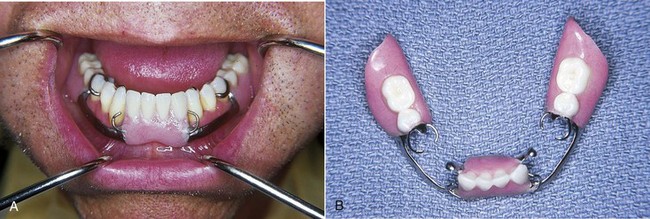
Figure 5-14 A, Lingual inclination of patient’s canines and premolars precludes use of the lingual bar. B, Labial bar major connector was used in treatment. Retention was obtained on terminal abutments. Support and stabilization were gained by using rests, minor connectors arising from the labial bar, and well-fitting denture bases.
A modification to the linguoplate is the hinged continuous labial bar. This concept is incorporated in the Swing-Lock* design, which consists of a labial or buccal bar that is connected to the major connector by a hinge at one end and a latch at the other end (Figure 5-15).

Figure 5-15 The hinge for this continuous labial bar connector is located buccal and distal to the remaining dentition (area of tooth #21). The latching mechanism is opposite to the hinge, adjacent to tooth #28. In this location, it will be housed within the buccal flange of the denture.
Support is provided by multiple rests on the remaining natural teeth. Stabilization and reciprocation are provided by a linguoplate that contacts the remaining teeth and are supplemented by the labial bar with its retentive struts. Retention is provided by a bar type of retentive clasp with arms projecting from the labial or buccal bar and contacting the infrabulge areas on the labial surfaces of the teeth.
Use of the Swing-Lock concept would seem primarily indicated when the following conditions are present:

Figure 5-16 Absence of the mandibular canine requires that all remaining anterior teeth be used for stabilization and retention of the replacement restoration. The Swing-Lock concept can be used to ensure that all remaining teeth share in stabilization and retention of the prosthesis.
Obvious contraindications to the use of this hinged labial bar concept are apparent. The most obvious is poor oral hygiene or lack of motivation for plaque control by the patient. Other contraindications include the presence of a shallow buccal or labial vestibule or a high frenal attachment. Any of these factors would prevent the proper placement of components of the Swing-Lock partial denture.
Maxillary Major Connectors
Six basic types of maxillary major connectors are considered:
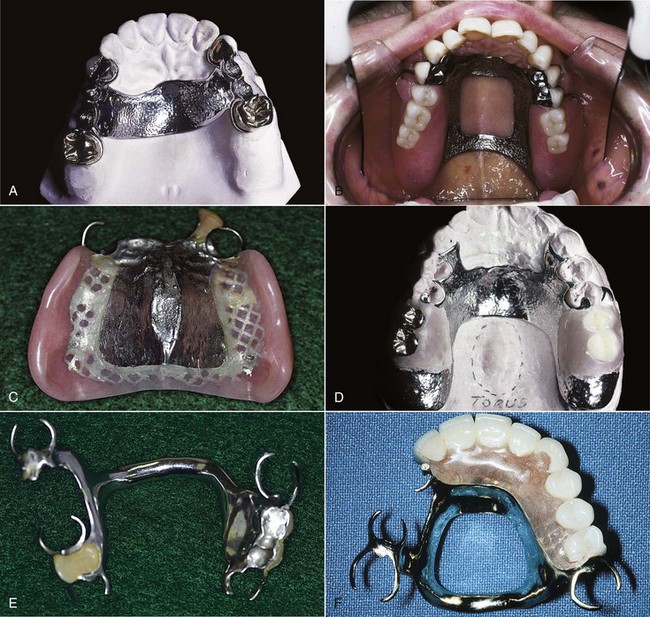
Figure 5-17 Maxillary major connectors: A, Single palatal strap. B, Anterior-posterior palatal strap. C, Palatal plate. D, U-shaped. E, Single palatal bar. F, Anterior-posterior palatal bars.
Whenever it is necessary for the palatal connector to make contact with the teeth for reasons of support, definite tooth support must be provided. This is best accomplished by establishing definite rest seats on the predetermined abutment teeth. These should be located far enough above the gingival attachment to provide for bridging of the gingival crevice with blockout. At the same time, they should be low enough on the tooth to avoid unfavorable leverage and low enough on the maxillary incisors and canine teeth to avoid incisal interference of the opposing dentition.
Major connector components resting on unprepared inclined tooth surfaces can lead to slippage of the denture or to orthodontic movement of the tooth, or to both. In either situation, settling into gingival tissue is inevitable. In the absence of the required vertical support provided by rests, the health of the surrounding tissue is usually impaired. Similarly, interproximal projections of the major connector that rest on the gingival third of the tooth and on gingival tissues that are structurally unable to render support may be traumatized. To prevent these sequelae, one should support the major connector with definite rests on the teeth, provide adequate gingival relief, and/or locate the connector far enough away from the gingival margin to avoid any possible restriction of blood supply and entrapment of food debris. All gingival crossings should be abrupt and at right angles to the major connector. Creating a sharp, angular form on any portion of a palatal connector should be avoided, and all borders should be tapered toward the tissue.
Single Palatal Strap
Bilateral tooth-supported prostheses, even those with short edentulous spaces, are effectively connected with a single, broad palatal strap connector, particularly when the edentulous areas are located posteriorly (Figure 5-18). Such a connector can be made rigid without objectionable bulk and interference with the tongue, provided the cast framework material is distributed in three planes. Suitable rigidity, without excessive bulk, may be obtained for a single palatal strap by the laboratory technician by casting a 22-gauge matte plastic pattern.
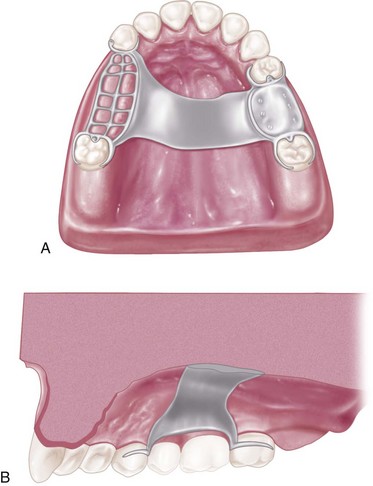
Figure 5-18 A, This single palatal strap–type major connector is better suited for the restoration of short-span tooth-supported bilateral edentulous areas. It may also be used in tooth-supported unilateral edentulous situations with provision for cross-arch attachment by extracoronal retainers or internal attachments. Width of the palatal strap should be confined within the boundaries of supporting rests. B, Sagittal section. Midportion of the major connector demonstrates slight elevation to provide rigidity. Such thickness of the major connector does not appreciably alter palatal contours.
For reasons of torque and leverage, a single palatal strap major connector should not be used to connect anterior replacements with distal extension bases. To be rigid enough to resist torque and to provide adequate vertical support and horizontal stabilization, a single palatal strap would have to be objectionably bulky. When placed anteriorly, this bulk would become even more objectionable to the patient because it could interfere with speech.
Combination Anterior and Posterior Palatal Strap–type Connector
Structurally, this is a rigid palatal major connector. The anterior and posterior palatal strap combination may be used in almost any maxillary partial denture design (Figure 5-19).

Figure 5-19 Anterior-posterior palatal strap–type major connector. The anterior component is a flat strap located as far posteriorly as possible to avoid rugae coverage and tongue interference. The anterior border of this strap should be located just posterior to a rugae crest or in the valley between two crests. The posterior strap is thin, a minimum of 8 mm wide, and located as far posteriorly as possible, yet entirely on the hard palate. It should be located at right angles to midline rather than diagonally.
A posterior palatal strap should be flat and a minimum of 8 mm wide. Posterior palatal connectors should be located as far posterior as possible to avoid interference with the tongue but anterior to the line of flexure formed by the junction of the hard and soft palates. The only condition that prevents their use is an inoperable maxillary torus that extends posterior to the soft palate. In this situation, a broad, U-shaped major connector may be used, as described elsewhere in this chapter.
The strength of this major connector design lies in the fact that the anterior and posterior components are joined together by longitudinal connectors on either side, which form a square or rectangular frame. Each component braces the others against possible torque and flexure. Flexure is practically nonexistent in such a design.
The anterior connector may be extended anteriorly to support anterior tooth replacements. In this form, a U-shaped connector is made rigid by the horizontal strap that has been added posteriorly. If a maxillary torus exists, it may be encircled by this type of major strap-type connector without reduced rigidity.
The combination anterior-posterior connector design may be used with any Kennedy class of partially edentulous arch. It is used most frequently in Classes II and IV, whereas the single wide palatal strap is used more frequently in Class III situations. The palatal plate–type or complete coverage connector, described in this chapter, is used most frequently in Class I situations for reasons to be explained subsequently. All maxillary major connectors should cross the midline at a right angle rather than on a diagonal. It has been suggested that the tongue will accept symmetrically placed components far more readily than those placed without regard for symmetry.
Palatal Plate–type Connector
For lack of better terminology, the words palatal plate are used to designate any thin, broad, contoured palatal coverage used as a maxillary major connector and covering one half or more of the hard palate (Figure 5-20). Anatomic replica palatal castings have uniform thickness and strength by reason of their corrugated contours. Through the use of electrolytic polishing, uniformity of thickness can be maintained, and the anatomic contours of the palate will be faithfully reproduced in the finished denture.

Figure 5-20 Palatal major connector covering two thirds of the palate. The anterior border follows valleys between rugae and does not extend anteriorly to indirect retainers on the first premolars. The posterior border is located at the junction of the hard and soft palates but does not extend onto the soft palate. In the bilateral distal extension situation illustrated, indirect retainers are a must to aid in resisting horizontal rotation of the restoration. Note that provisions have been made for a butt-type joint joining the denture bases and framework as the denture base on each side passes through the pterygomaxillary notch.
The anatomic replica palatal major connector has several potential advantages:
The palatal plate may be used in any one of three ways. It may be used as a plate of varying width that covers the area between two or more edentulous areas, as a complete or partial cast plate that extends posterior to the junction of the hard and soft palates (Figures 5-21 and 5-22), or in the form of an anterior palatal connector with a provision for extending an acrylic resin denture base in a posterior direction (Figure 5-23).

Figure 5-21 Palatal plate major connector for a Class I, modification 1 removable partial denture. The posterior border lies on the immovable hard palate and crosses the midline at a right angle. Total contact provides excellent support.

Figure 5-22 Complete coverage palatal major connector. The posterior border terminates at the junction of the hard and soft palates. The anterior portion, in the form of the palatal linguoplate, is supported by positive lingual rest seats on canines. The location of finishing lines is most important in this type of major connector. Anteroposteriorly, they should be parallel to a line along the center of the ridge crest and located just lingual to an imaginary line contacting the lingual surfaces of missing natural teeth. Alteration of the natural palatal contour should be anticipated with its attendant detrimental effects on speech if these contours are not followed.
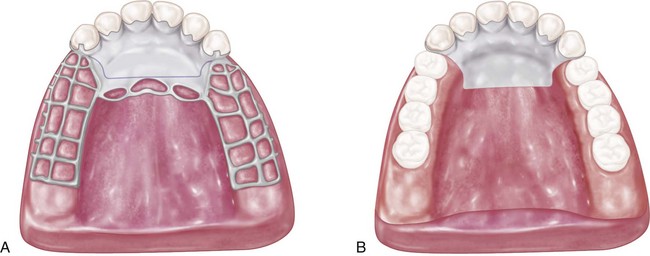
Figure 5-23 A, Maxillary major connector in the form of a palatal linguoplate with provisions for attaching the full-coverage resin denture base. B, Completed removable partial denture with resin base. The palatal linguoplate is supported by rests occupying lingual rest seats prepared in cast restorations on canines. This type of removable partial denture is particularly applicable when (1) residual ridges have undergone extreme vertical resorption, and (2) terminal abutments have suffered some bone loss and splinting cannot be accomplished.
The palatal plate should be located anterior to the posterior palatal seal area. The maxillary complete denture’s typical posterior palatal seal is not necessary with a maxillary partial denture’s palatal plate because of the accuracy and stability of the cast metal.
When the last remaining abutment tooth on either side of a Class I arch is the canine or first premolar tooth, complete palatal coverage is strongly advised, especially when the residual ridges have undergone excessive vertical resorption. This may be accomplished in one of two ways. One method is to use a complete cast plate that extends to the junction of the hard and soft palates (see Figure 5-22). The other method is to use a cast major connector anteriorly, with retention posteriorly, for the attachment of an acrylic-resin denture base that extends posterior to the anatomic landmarks previously described (see Figure 5-23).
Despite increased costs, the advantages of a cast palate make it preferable to an acrylic-resin palate. However, the latter method may be used satisfactorily when relining is anticipated or cost is a factor. The complete palatal plate is not a connector that has received universal use. It has, however, become accepted as a satisfactory palatal connector for many maxillary partial dentures. In all circumstances, the portion contacting the teeth must have positive support from adequate rest seats. The dentist should be familiar with its use and, at the same time, with its limitations, so that it may be used intelligently and to fullest advantage.
Design of Maxillary Major Connectors
In 1953, Blatterfein described a systematic approach to designing maxillary major connectors. His method involves five basic steps and is certainly applicable to most maxillary removable partial denture situations. When using a diagnostic cast and knowledge of the relative displaceability of the palatal tissue, including that covering the median palatal raphe, he recommends the following basic steps:
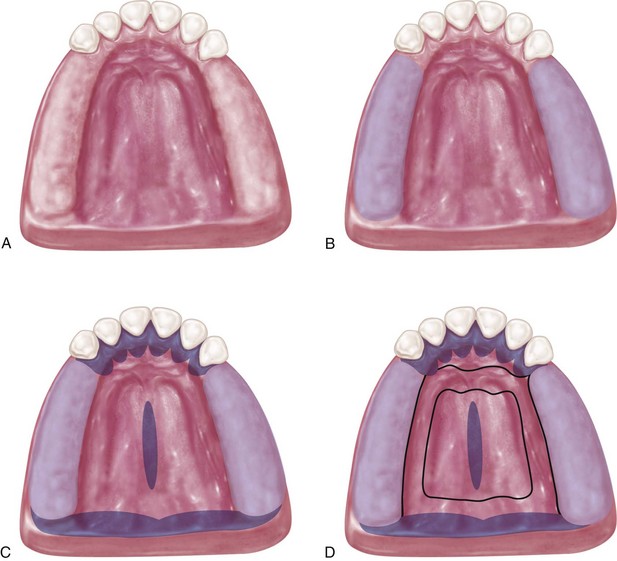
Figure 5-24 A, Diagnostic cast of partially edentulous maxillary arch. B, The palatal extent of the denture base areas are located 2 mm from the palatal surface of the posterior teeth. C, Nonbearing areas outlined in black, which include lingual soft tissue within 5 to 6 mm of teeth, an unyielding median palatal raphe area, and the soft palate. The space bounded by bearing and nonbearing area outlines is available for placement of the major connector. D, The major connector selected will be rigid and noninterfering with the tongue and will cover a minimum of the palate.
Indications for the use of complete palatal coverage have been previously discussed in this chapter. Although many variations in palatal major connectors have been noted, a thorough comprehension of all factors that influence their design will lead to the best design for each patient.
U-shaped Palatal Connector
From both the patient’s standpoint and a mechanical standpoint, the U-shaped palatal connector is the least desirable of maxillary major connectors. It should never be used arbitrarily. When a large inoperable palatal torus exists, and occasionally when several anterior teeth are to be replaced, the U-shaped palatal connector may have to be used (Figure 5-25). In most instances, however, other designs will serve more effectively.
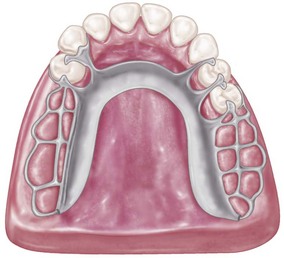
Figure 5-25 U-shaped palatal connector is probably the least rigid type of maxillary major connector and should be used only when a large inoperable palatal torus prevents the use of palatal coverage or combination anterior-posterior palatal strap–type designed framework.
The following are the principal objections to use of the U-shaped connector:
Many maxillary partial dentures have failed for no other reason than the flexibility of a U-shaped major connector (Figure 5-26). To be rigid, the U-shaped palatal connector must have bulk where the tongue needs freedom the most—the rugae area. Without sufficient bulk, the U-shaped design leads to increased flexibility and movement at the open ends. In distal extension partial dentures, when tooth support posterior to the edentulous area is nonexistent, movement is particularly noticeable and is traumatic to the residual ridge. No matter how well the extension base is supported or how harmonious the occlusion, without a rigid major connector the residual ridge suffers.

Figure 5-26 Removable partial denture design that uses an objectionable U-shaped palatal major connector. Such a connector lacks necessary rigidity, places bulk where it is most objectionable to the patient, and impinges on gingival tissue lingual to remaining teeth.
The wider the coverage of a U-shaped major connector, the more it resembles a palatal plate–type connector with its several advantages. But when used as a narrow U design, the necessary rigidity is usually lacking. A U-shaped connector may be made more rigid with multiple tooth support through definite rests. A common error in the design of a U-shaped connector, however, is its proximity to, or actual contact with, gingival tissue. The principle that the borders of major connectors should be supported by rests in prepared rest seats or should be located well away from gingival tissue has been stated previously. Most U-shaped connectors fail to do either, with resulting gingival irritation and periodontal damage to the tissue adjacent to remaining teeth.
Single Palatal Bar
To differentiate between a palatal bar and a palatal strap, a palatal connector component less than 8 mm in width is referred to as a bar in this textbook. The single palatal bar is perhaps the most widely used and yet the least logical of all palatal major connectors. It is difficult to say whether the bar or the U-shaped palatal connector is the more objectionable of palatal connectors.
For a single palatal bar to have the necessary rigidity for cross-arch distribution of stress, it must have concentrated bulk, which, unfortunately, is all too often ignored. For a single palatal bar to be effective, it must be rigid enough to provide support and cross-arch stabilization and must be centrally located between the halves of the denture. Mechanically, this practice may be sound enough. However, from the standpoint of patient comfort and alteration of palatal contours, it is highly objectionable.
A partial denture made with a single palatal bar is often too thin and flexible or too bulky and objectionable to the patient’s tongue. The decision to use a single palatal bar instead of a strap should be based on the size of the denture-bearing areas that are connected and on whether a single connector located between them would be rigid without objectionable bulk.
Combination Anterior and Posterior Palatal Bar–type Connectors
Structurally, this combination of major connectors exhibits many of the same disadvantages as the single palatal bar (Figure 5-27). To be sufficiently rigid and to provide needed support and stability, these connectors could be too bulky and could interfere with tongue function.
Beading of the Maxillary Cast
Beading is a term used to denote the scribing of a shallow groove on the maxillary master cast outlining the palatal major connector exclusive of rugae areas (Figure 5-28). The purposes of beading are as follows:

Figure 5-28 Framework design on master cast before preparation for duplication in refractory investment. A shallow groove (0.5 mm) has been scribed on the outline of anterior and posterior borders of the major connector. The anterior outline follows the valleys of rugae. Beading is readily accomplished with a cleoid carver. A slightly rounded groove is preferred to a V-shaped groove.

Figure 5-29 A, Refractory cast. Note the definitive outline of the major connector indicated by beading lines that were transferred in duplicating the master cast. B, The wax pattern for the major connector is accurately executed by following the beading lines. The major connector is confined to previously scribed beading.

Figure 5-30 Cast and framework showing metal margin produced by the 0.5-mm beading line scribed on the cast. Such a margin is easily finished in the lab and provides intimate tissue contact, preventing food from easily dislodging the prosthesis. Care should be exercised in adapting such a beaded margin to noncompressible tissue, such as the median palatal raphe.
Beading is readily accomplished by using an appropriate instrument, such as a cleoid carver. Care must be exercised to create a groove not in excess of 0.5 mm in width or depth (Figure 5-31).
Minor Connectors
Minor connectors are those components that serve as the connecting link between the major connector or the base of a removable partial denture and the other components of the prosthesis, such as the clasp assembly, indirect retainers, occlusal rests, or cingulum rests. In many instances, a minor connector may be continuous with some other part of the denture. For example, an occlusal rest at one end of a linguoplate is actually the terminus of a minor connector, even though that minor connector is continuous with the linguoplate. Similarly the portion of a partial denture framework that supports the clasp and the occlusal rest is a minor connector, which joins the major connector with the clasp proper. Those portions of a removable partial denture framework that retain the denture bases are also minor connectors.
Functions
In addition to joining denture parts, the minor connector serves two other purposes.
Form and Location
Like the major connector, the minor connector must have sufficient bulk to be rigid; otherwise the transfer of functional stresses to the supporting teeth and tissue will not be effective. At the same time, the bulk of the minor connector should not be objectionable.
A minor connector that contacts the axial surface of an abutment should not be located on a convex surface. Instead it should be located in an embrasure (Figure 5-32), where it will be least noticeable to the tongue. It should conform to the interdental embrasure, passing vertically from the major connector so that the gingival crossing is abrupt and covers as little of the gingival tissue as possible. It should be thickest toward the lingual surface, tapering toward the contact area (Figure 5-33).

Figure 5-32 In an embrasure space, the minor connector is tapered to the tooth to avoid bulk and to accommodate the tongue.
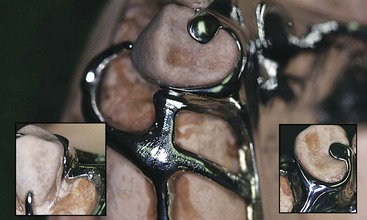
Figure 5-33 The minor connector that contacts the guiding plane is part of a clasp assembly. It can be separate from the other parts, or, as in this case, it can be connected to the lingual stabilizing portion of the clasp assembly. The proximal plate minor connector contact is about one-half the distance between tips of adjacent buccal and lingual cusps of the abutment tooth, and it extends gingivally, contacting an area of the abutment from the marginal ridge to two-thirds the length of the enamel crown. Viewed from above, it is triangular, the apex of the triangle being located buccally and the base of the triangle being located lingually. Less interference with the arrangement of the adjacent artificial tooth is encountered with minor connectors so shaped.
The deepest part of the interdental embrasure should have been blocked out to avoid interference during placement and removal, and to avoid any wedging effect on the contacted teeth.
A modification of the conventional removable partial denture minor connector has been proposed. This application was suggested to be limited to the maxillary arch, with the minor connector located in the center of the lingual surface of the maxillary abutment tooth.
It is suggested that this modification reduces the amount of gingival tissue coverage, provides enhanced guidance for the partial denture during insertion and removal, and increases stabilization against horizontal and rotational forces. However, because of its location, such a design variation could encroach on the tongue space and create a greater potential space for food entrapment. The proposed variation should be used with careful application.
When a minor connector contacts tooth surfaces on either side of the embrasure in which it lies, it should be tapered to the teeth. This avoids sharp angles, which could hinder tongue movement, and eliminates spaces that could trap food (Figure 5-34).
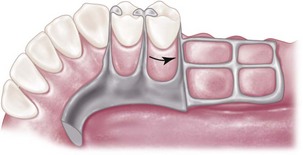
Figure 5-34 Finishing line at the junction of the ladderlike minor connector and the major connector blends smoothly into the minor connector contacting the distal guiding plane on the second premolar. The framework is feathered toward tissue anterior to the finishing line to avoid as much bulk in this area as possible without compromising the strength of the butt-type joint.
It is a minor connector that contacts the guiding plane surfaces of the abutment teeth, whether as a connected part of a direct retainer assembly or as a separate entity (see Figure 5-33). Here the minor connector must be wide enough that the guiding plane can be used to fullest advantage. When it gives rise to a clasp arm, the connector should be tapered to the tooth below the origin of the clasp. If no clasp arm is formed (as when a bar clasp arm originates elsewhere), the connector should be tapered to a knife-edge the full length of its buccal aspect.
When an artificial tooth will be placed against a proximal minor connector, the minor connector’s greatest bulk should be toward the lingual aspect of the abutment tooth. This way sufficient bulk is ensured with the least interference with placement of the artificial tooth. Ideally the artificial tooth should contact the abutment tooth with only a thin layer of metal intervening buccally. Lingually the bulk of the minor connector should lie in the interdental embrasure—the same as between two natural teeth.
As was stated previously, those portions of a denture framework by which acrylic-resin denture bases are attached are minor connectors. This type of minor connector should be so designed that it will be completely embedded within the denture base.
The junctions of these mandibular minor connectors with the major connectors should be strong butt-type joints but without appreciable bulk (see Figure 5-34). Angles formed at the junctions of the connectors should not be greater than 90 degrees, thus ensuring the most advantageous and the strongest mechanical connection between the acrylic-resin denture base and the major connector.
An open latticework or ladder type of design is preferable and is conveniently made by using preformed 12-gauge half-round and 18-gauge round wax strips. The minor connector for the mandibular distal extension base should extend posteriorly about two-thirds the length of the edentulous ridge and should have elements on both lingual and buccal surfaces. Such an arrangement not only will add strength to the denture base but may minimize distortion of the cured base from its inherent strains caused by processing. The minor connector must be planned with care so that it will not interfere with the arrangement of artificial teeth (Figure 5-35).

Figure 5-35 The minor connector for attaching the resin denture base should be designed so that denture tooth placement is not compromised. The minor connector design should not include a main lattice strut at the ridge crest or in a desired tooth location.
A means to attach acrylic-resin individualized trays to the mandibular framework when a corrected impression is planned must be arranged when the framework pattern is being developed. Three nailhead minor connectors fabricated as part of the denture base minor connector serve this purpose well. Unless some similar arrangement is made, the resin trays may become detached or loosened during impression-making procedures. Minor connectors for maxillary distal extension denture bases should extend the entire length of the residual ridge and should be of a ladderlike and loop design (Figure 5-36).
Tissue Stops
Tissue stops are integral parts of minor connectors designed for retention of acrylic-resin bases. They provide stability to the framework during the stages of transfer and processing. They are particularly useful in preventing distortion of the framework during acrylic-resin processing procedures. Tissue stops can engage buccal and lingual slopes of the residual ridge for stability (Figure 5-37).
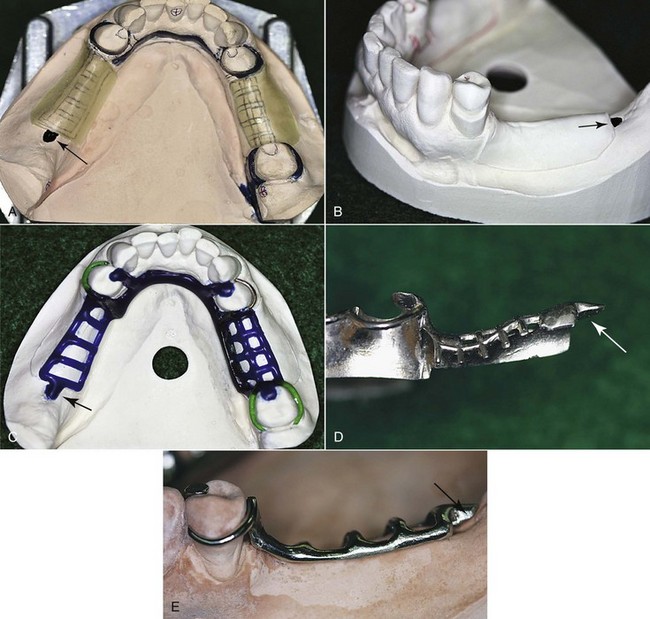
Figure 5-37 A, Arrow points to location of the tissue stop. B, Master cast partially prepared for duplication in refractory investment. Posterior to relief wax, at the distal of the residual ridge (arrow), a tissue stop will be waxed. C, Wax tissue stop placed distal to relief (arrow). After casting, this will result in tissue stop contact of the framework. D, Tissue stop seen from labial position. E, Framework on cast shows tissue contact posterior to the minor connector with planned relief. Arrow points to the created tissue stop.
Altered cast impression procedures often necessitate that tissue stops be augmented subsequent to the development of the altered cast. This can be readily accomplished with the addition of autopolymerizing acrylic resin (Figure 5-38).
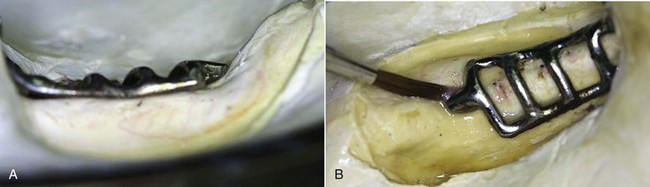
Figure 5-38 A, Lower half of the flask in which the distal extension denture was invested. Note that the terminal portion of the minor connector (original tissue stop) is elevated from the residual ridge. The framework was developed on cast, with the residual ridge recorded in its anatomic form. The residual ridge was later recorded in its functional form by a corrected impression, thus the elevated tissue stop. B, Autopolymerizing resin is painted on between the tissue stop and the ridge to maintain the position of the minor connector during packing and processing procedures for a resin denture base.
Another integral part of the minor connector designed to retain the acrylic-resin denture base is similar to a tissue stop but serves a different purpose. It is located distal to the terminal abutment and is a continuation of the minor connector contacting the guiding plane. Its purpose is to establish a definitive finishing index tissue stop for the acrylic-resin base after processing (Figure 5-39).
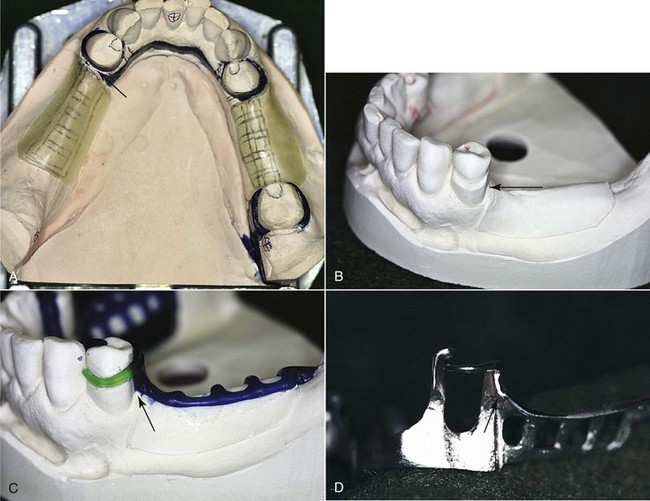
Figure 5-39 Finishing index tissue stop. A, Designed to facilitate finishing of the denture base resin at the region of the terminal abutment. Note the space at the anterior region of wax relief. Framework will be waxed to fill this space and provide positive tissue contact. B, Refractory cast shows space distal to the abutment. C, Wax pattern filling space for future tissue index contact. D, Framework index tissue stop anterior to relief beneath the minor connector of the distal extension base and posterior to the primary abutment.
Finishing Lines
The finishing line junction with the major connector should take the form of an angle not greater than 90 degrees, therefore being somewhat undercut (Figure 5-40). Of course the medial extent of the minor connector depends on the lateral extent of the major palatal connector. Too little attention is given to this finishing line location in many instances. If the finishing line is located too far medially, the natural contour of the palate will be altered by the thickness of the junction and the acrylic resin supporting the artificial teeth (Figure 5-41). If, on the other hand, the finishing line is located too far buccally, it will be most difficult to create a natural contour of the acrylic resin on the lingual surface of the artificial teeth. The location of the finishing line at the junction of the major and minor connectors should be based on restoration of the natural palatal shape, with consideration given to the location of the replacement teeth.
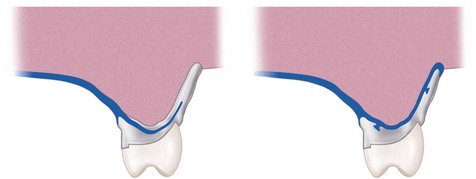
Figure 5-40 Frontal sections through lingual finishing lines of palatal major connectors. The right image is through the full cast metal base major connector; the left image is through the resin denture base. In both situations, the location of finishing lines minimizes the bulk of resin attaching the artificial teeth. Palatal contours are restored, enhancing speech and contributing to a natural feeling for the patient.
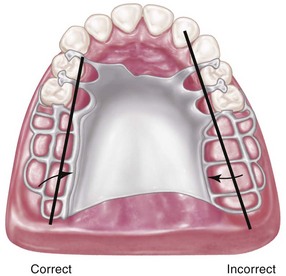
Figure 5-41 Junction of the major connector and the minor connector at palatal finishing lines should be located 2 mm medial from an imaginary line that would contact the lingual surfaces of missing posterior teeth. The finish line on the right is too far toward midline of the palate. The natural contours of the palate will be altered.
Equal consideration must be given to the junction of minor connectors and bar-type direct retainer arms. These junctions are 90-degree butt-type joints and should follow the guidelines for base contour and clasp length.
Reaction of Tissue to Metallic Coverage
The reaction of tissue to coverage by the metallic components of a removable partial denture has been the subject of significant controversy, particularly in regions of marginal gingiva and broad areas of tissue contact. These tissue reactions can result from pressure caused by lack of support, lack of adequate hygiene measures, and prolonged contact through continual use of a prosthesis.
Pressure occurs at regions where relief over gingival crossings and other areas of contact with tissue that are incapable of supporting the prosthesis is inadequate. Impingement will likewise occur if the denture settles because of loss of tooth and/or tissue support. This may be caused by failure of the rest areas resulting from improper design, caries involvement, fracture of the rest itself, or intrusion of abutment teeth under occlusal loading. It is important to maintain adequate relief and support from both teeth and tissue. Settling of the denture caused by loss of tissue support may also produce pressure elsewhere in the arch, such as beneath major connectors. Settling of a prosthesis must be prevented or corrected if it has occurred. Excessive pressure must be avoided whenever oral tissue must be covered or crossed by elements of the partial denture.
Lack of adequate hygiene measures can result in tissue reactions caused by an accumulation of food debris and bacteria. Coverage of oral tissue with partial dentures that are not kept clean irritates those tissues because of an accumulation of irritating factors. This has led to misinterpretation of the effects of tissue coverage by prosthetic restorations. An additional hygiene concern is related to the problem of maintaining cleanliness of the tissue surface of the prosthesis.
The first two causes of untoward tissue reaction can be accentuated the longer a prosthesis is worn. It is apparent that mucous membranes cannot tolerate this constant contact with a prosthesis without resultant inflammation and breakdown of the epithelial barrier. Some patients become so accustomed to wearing a removable restoration that they neglect to remove it often enough to give the tissue any respite from constant contact. This is frequently true when anterior teeth are replaced by the partial denture and the individual does not allow the prosthesis to be out of the mouth at any time except in the privacy of the bathroom during toothbrushing. Living tissues should not be covered all the time, or changes in those tissues will occur. Partial dentures should be removed for several hours each day so that the effects of tissue contact can subside and the tissue can return to a normal state.
Clinical experience with the use of linguoplates and complete metallic palatal coverage has shown conclusively that when factors of pressure, cleanliness, and time are controlled, tissue coverage is not in itself detrimental to the health of oral tissue.
Major Connectors in Review
Mandibular Lingual Bar
Indications for Use: The lingual bar should be used for mandibular removable partial dentures when sufficient space exists between the slightly elevated alveolar lingual sulcus and the lingual gingival tissue.
Characteristics and Location: (1) Half-pear shaped with bulkiest portion inferiorly located. (2) Superior border tapered to soft tissue. (3) Superior border located at least 4 mm inferior to gingival margins and farther if possible. (4) Inferior border located at the ascertained height of the alveolar lingual sulcus when the patient’s tongue is slightly elevated.
Blockout and Relief of Master Cast: (1) All tissue undercuts parallel to the path of placement. (2) An additional thickness of 32-gauge sheet wax when the lingual surface of the alveolar ridge is undercut or parallel to the path of placement (see Figures 11-23 and 11-24). (3) No relief is necessary when the lingual surface of the alveolar ridge slopes inferiorly and posteriorly. (4) One thickness of baseplate wax over basal seat areas (to elevate minor connectors for attaching acrylic-resin denture bases).
Waxing Specifications: (1) Six-gauge, half-pear–shaped wax form reinforced by 22- to 24-gauge sheet wax or similar plastic pattern adapted to the design width. (2) Long bar requires more bulk than short bar; however, cross-sectional shape is unchanged.
Finishing Lines: Butt-type joint(s) with minor connector(s) for retention of denture base(s).
Mandibular Linguoplate
Indications for Use: (1) When the alveolar lingual sulcus so closely approximates the lingual gingival crevices that adequate width for a rigid lingual bar does not exist. (2) In those instances in which the residual ridges in Class I arch have undergone such vertical resorption that they will offer only minimal resistance to horizontal rotations of the denture through its bases. (3) For using periodontally weakened teeth in group function to furnish support to the prosthesis and to help resist horizontal (off-vertical) rotation of the distal extension type of denture. (4) When the future replacement of one or more incisor teeth will be facilitated by the addition of retention loops to an existing linguoplate.
Characteristics and Location: (1) Half-pear shaped with bulkiest portion inferiorly located. (2) Thin metal apron extending superiorly to contact cingula of anterior teeth and lingual surfaces of involved posterior teeth at their height of contour. (3) Apron extended interproximally to the height of contact points (i.e., closing interproximal spaces). (4) Scalloped contour of apron as dictated by interproximal blockout. (5) Superior border finished to continuous plane with contacted teeth. (6) Inferior border at the ascertained height of the alveolar lingual sulcus when the patient’s tongue is slightly elevated.
Blockout and Relief of Master Cast: (1) All involved undercuts of contacted teeth parallel to the path of placement. (2) All involved gingival crevices. (3) Lingual surfaces of alveolar ridge and basal seat areas the same as for a lingual bar.
Waxing Specifications: (1) Inferior border: 6-gauge, half-pear–shaped wax form reinforced with 24-gauge sheet wax or similar plastic pattern. (2) Apron: 24-gauge sheet wax.
Finishing Lines: Butt-type joint(s) with minor connector(s) for retention of denture base(s).
Mandibular Sublingual Bar
Indications for Use: The sublingual bar should be used for mandibular removable partial dentures when the height of the floor of the mouth in relation to the free gingival margins will be less than 6 mm. It also may be indicated whenever it is desirable to keep the free gingival margins of the remaining anterior teeth exposed and depth of the floor of the mouth is inadequate to place a lingual bar.
Contraindications for Use: Remaining natural anterior teeth severely tilted toward the lingual.
Characteristics and Location: The sublingual bar is essentially the same half-pear shape as a lingual bar, except that the bulkiest portion is located to the lingual and the tapered portion is toward the labial. The superior border of the bar should be at least 3 mm from the free gingival margin of the teeth. The inferior border is located at the height of the alveolar lingual sulcus when the patient’s tongue is slightly elevated. This necessitates a functional impression of the lingual vestibule to accurately register the height of the vestibule.
Blockout and Relief of Master Cast: (1) All tissue undercuts parallel to path of placement. (2) An additional thickness of 32-gauge sheet wax when the lingual surface of the alveolar ridge is undercut or parallel to the path of placement. (3) One thickness of baseplate wax over basal seat areas (to elevate minor connectors for attaching acrylic-resin denture bases).
Waxing Specifications: (1) Six-gauge, half-pear–shaped wax form reinforced by 22- to 24-gauge sheet wax or similar plastic pattern adapted to design width. (2) Long bar bulkier than short bar; however, cross-sectional shape unchanged.
Finishing Lines: Butt-type joint(s) with minor connector(s) for retention of denture base(s).
Mandibular Lingual Bar With Continuous Bar (Cingulum Bar)
Indications for Use: (1) When a linguoplate is otherwise indicated but the axial alignment of anterior teeth is such that excessive blockout of interproximal undercuts would be required. (2) When wide diastemata exist between mandibular anterior teeth and a linguoplate would objectionably display metal in a frontal view.
Characteristics and Location: (1) Conventionally shaped and located same as lingual bar major connector component when possible. (2) Thin, narrow (3 mm) metal strap located on cingula of anterior teeth, scalloped to follow interproximal embrasures with inferior and superior borders tapered to tooth surfaces. (3) Originates bilaterally from incisal, lingual, or occlusal rests of adjacent principal abutments.
Blockout and Relief of Master Cast: (1) Lingual surfaces of alveolar ridge and basal seat areas same as for lingual bar. (2) No relief for continuous bar except blockout of interproximal spaces parallel to path of placement.
Waxing Specifications: (1) Lingual bar major connector component waxed and shaped same as lingual bar. (2) Continuous bar pattern formed by adapting two strips (3 mm wide) of 28-gauge sheet wax, one at a time, over the cingula and into interproximal embrasures.
Finishing Lines: Butt-type joint(s) with minor connector(s) for retention of denture base(s).
Mandibular Continuous Bar (Cingulum Bar)
Indications for Use: When a lingual plate or sublingual bar is otherwise indicated but the axial alignment of the anterior teeth is such that excessive blockout of interproximal undercuts would be required.
Contraindications for Use: (1) Anterior teeth severely tilted to the lingual. (2) When wide diastemata that exist between the mandibular anterior teeth and the cingulum bar would objectionably display metal in a frontal view.
Characteristics and Location: (1) Thin, narrow (3 mm) metal strap located on cingula of anterior teeth, scalloped to follow interproximal embrasures with inferior and superior borders tapered to tooth surfaces. (2) Originates bilaterally from incisal, lingual, or occlusal rests of adjacent principal abutments.
Blockout and Relief of Master Cast: No relief for cingulum bar except blockout of interproximal spaces parallel to the path of placement.
Waxing Specifications: Cingulum bar pattern formed by adapting two strips (3 mm wide) of 28-gauge sheet wax, one at a time, over the cingula and into interproximal embrasures.
Finishing Lines: Butt-type joint(s) with minor connector(s) for retention of denture base(s).
Mandibular Labial Bar
Indications for Use: (1) When lingual inclinations of remaining mandibular premolar and incisor teeth cannot be corrected, preventing placement of a conventional lingual bar connector. (2) When severe lingual tori cannot be removed and prevent the use of a lingual bar or lingual plate major connector. (3) When severe and abrupt lingual tissue undercuts make it impractical to use a lingual bar or a lingual plate major connector.
Characteristics and Location: (1) Half-pear shaped with bulkiest portion inferiorly located on the labial and buccal aspects of the mandible. (2) Superior border tapered to soft tissue. (3) Superior border located at least 4 mm inferior to labial and buccal gingival margins and farther if possible. (4) Inferior border located in the labial-buccal vestibule at the juncture of attached (immobile) and unattached (mobile) mucosae.
Blockout and Relief of Master Cast: (1) All tissue undercuts parallel to path of placement, plus an additional thickness of 32-gauge sheet wax when the labial surface is undercut or parallel to the path of placement. (2) No relief necessary when the labial surface of the alveolar ridge slopes inferiorly to the labial or buccal. (3) Basal seat areas same as for lingual bar major connector.
Waxing Specifications: (1) Six-gauge, half-pear–shaped wax form reinforced with 22- to 24-gauge sheet wax or similar plastic pattern. (2) Long bar necessitates more bulk than short bar; however, cross-sectional shape unchanged. (3) Minor connectors joined with occlusal or other superior components by a labial or buccal approach. (4) Minor connectors for base attachment joined by a labial or buccal approach.
Finishing Lines: Butt-type joint(s) with minor connector(s) for retention of denture base(s).
Single Palatal Strap–type Major Connector
Indications for Use: Bilateral edentulous spaces of short span in a tooth-supported restoration.
Characteristics and Location: (1) Anatomic replica form. (2) Anterior border follows the valleys between rugae as nearly as possible at right angles to median suture line. (3) Posterior border at right angle to median suture line. (4) Strap should be 8 mm wide or approximately as wide as the combined width of a maxillary premolar and first molar. (5) Confined within an area bounded by the four principal rests.
Blockout and Relief of Master Cast: (1) Usually none required except slight relief of elevated medial palatal raphe or any exostosis crossed by the connector. (2) One thickness of baseplate wax over basal seat areas (to elevate minor connectors for attaching acrylic-resin denture bases).
Beading: (See Figures 5-37 to 5-40.)
Waxing Specifications: Anatomic replica pattern equivalent to 22- to 24-gauge wax, depending on arch width.
Finishing Lines: (1) Undercut and slightly elevated. (2) No farther than 2 mm medial from an imaginary line contacting lingual surfaces of principal abutments and teeth to be replaced. (3) Follow curvature of arch.
Single Broad Palatal Major Connector
Indications for Use: (1) Class I partially edentulous arches with residual ridges that have undergone little vertical resorption and will lend excellent support. (2) V- or U-shaped palates. (3) Strong abutments (single or made so by splinting). (4) More teeth in arch than six remaining anterior teeth. (5) Direct retention not a problem. (6) No interfering tori.
Characteristics and Location: (1) Anatomic replica form. (2) Anterior border following valleys of rugae as near right angle to median suture line as possible and not extending anterior to occlusal rests or indirect retainers. (3) Posterior border located at junction of hard and soft palate but not extended onto soft palate; at right angle to the median suture line; extended to pterygomaxillary notches.
Blockout and Relief of Master Cast: (1) Usually none required except relief of elevated median palatal raphe or any small exostoses covered by the connector. (2) One thickness of baseplate wax over basal seat areas (to elevate minor connectors for attaching acrylic-resin denture bases).
Beading: (See Figures 5-37 to 5-40.)
Waxing Specifications: Anatomic replica pattern equivalent to 24-gauge sheet wax thickness.
Finishing Lines: (1) Provision for butt-type joint at pterygomaxillary notches. (2) Undercut and slightly elevated. (3) No farther than 2 mm medial from an imaginary line contacting the lingual surfaces of the missing natural teeth. (4) Following curvature of arch.
Anterior-Posterior Strap–type Major Connector
Indications for Use: (1) Class I and II arches in which excellent abutment and residual ridge support exists, and direct retention can be made adequate without the need for indirect retention. (2) Long edentulous spans in Class II, modification 1 arches. (3) Class IV arches in which anterior teeth must be replaced with a removable partial denture. (4) Inoperable palatal tori that do not extend posteriorly to the junction of the hard and soft palates.
Characteristics and Location: (1) Parallelogram shaped and open in center portion. (2) Relatively broad (8 to 10 mm) anterior and posterior palatal straps. (3) Lateral palatal straps (7 to 9 mm) narrow and parallel to curve of arch; minimum of 6 mm from gingival crevices of remaining teeth. (4) Anterior palatal strap: anterior border not placed farther anteriorly than anterior rests and never closer than 6 mm to lingual gingival crevices; follows the valleys of the rugae at right angles to the median palatal suture. Posterior border, if in rugae area, follows valleys of rugae at right angles to the median palatal suture. (5) Posterior palatal connector: posterior border located at junction of hard and soft palates and at right angles to median palatal suture and extended to hamular notch area(s) on distal extension side(s). (6) Anatomic replica or matte surface.
Blockout and Relief of Master Cast: (1) Usually none required except slight relief of elevated median palatal raphe where anterior or posterior straps cross the palate. (2) One thickness of baseplate wax over basal seat areas (to elevate minor connectors for attaching acrylic-resin denture bases).
Beading: (See Figures 5-37 to 5-40.)
Waxing Specifications: (1) Anatomic replica patterns or matte surface forms of 22-gauge thickness. (2) Posterior palatal component: a strap of 22-gauge thickness, 8 to 10 mm wide (a half-oval form of approximately 6-gauge thickness and width) may also be used.
Finishing Lines: Same as for single broad palatal major connector.
Complete Palatal Coverage Major Connector
Indications for Use: (1) In most situations in which only some or all anterior teeth remain. (2) Class II arch with a large posterior modification space and some missing anterior teeth. (3) Class I arch with one to four premolars and some or all anterior teeth remaining, when abutment support is poor and cannot otherwise be enhanced; residual ridges have undergone extreme vertical resorption; direct retention is difficult to obtain. (4) In the absence of a pedunculated torus.
Characteristics and Location: (1) Anatomic replica form for full palatal metal casting supported anteriorly by positive rest seats. (2) Palatal linguoplate supported anteriorly and designed for attachment of acrylic-resin extension posteriorly. (3) Contacts all or almost all of the teeth remaining in the arch. (4) Posterior border: terminates at the junction of the hard and soft palates; extended to hamular notch area(s) on distal extension side(s); at a right angle to median suture line.
Blockout and Relief of Master Cast: (1) Usually none required except relief of elevated median palatal raphe or any small palatal exostosis. (2) One thickness of baseplate wax over basal seat areas (to elevate minor connectors for attaching acrylic-resin denture bases).
Beading: (See Figures 5-37 to 5-40.)
Waxing Specifications: (1) Anatomic replica pattern equivalent to 22- to 24-gauge sheet wax thickness. (2) Acrylic-resin extension from linguoplate the same as for a complete denture.
Finishing Lines: As illustrated here and previously discussed.
U-Shaped Palatal Major Connector
This connector should be used only in those situations in which inoperable tori extend to the posterior limit of the hard palate.
The U-shaped palatal major connector is the least favorable design of all palatal major connectors because it lacks the rigidity of other types of connectors. When it must be used, indirect retainers must support any portion of the connector that extends anteriorly from the principal occlusal rests. Anterior border areas of this type of connector must be kept at least 6 mm away from adjacent teeth. If for any reason the anterior border must contact the remaining teeth, the connector must again be supported by rests placed in properly prepared rest seats. It should never be supported even temporarily by inclined lingual surfaces of anterior teeth.
Waxing specifications, finishing lines, and so forth, are the same as for full palatal castings or other previously discussed similar major connectors.