Application of Motor Control/Motor Learning to Practice
1 Understand the concepts of motor control and motor learning theories.
2 Develop interventions for children with motor control deficits based on current motor control/motor learning research.
3 Compare and contrast intervention using motor control/motor learning approaches.
4 Describe components of motor control that influence movement, including postural control, balance, visual perception, and body awareness.
5 Define concepts of motor learning including transfer of learning, feedback, practice, sequencing and adapting tasks, modeling or demonstration, and mental rehearsal.
Typically-developing children move into and out of positions fluidly and with ease, exploring their worlds, learning about their bodies, and developing motor, cognitive, sensory, and social skills. They use their hands for feeding, dressing, bathing, play, and academics (Figure 9-1). They practice sitting, walking, jumping, and crawling. They play in a variety of positions and show variability in their movements. Conversely, children with motor control deficits have difficulty in such activities and may not have the same opportunities to explore their surroundings; they may take longer and often do not master movements. Because motor control is central to participation, occupational therapists are concerned with how to help children control movements so that they may engage in their occupations.
This chapter presents case examples to illustrate the principles of motor control and motor learning related to occupational therapy practice, beginning with a definition of motor control and an overview of past motor approaches. Next, dynamical systems theory and the components of movement, including postural control, balance, visual perception, and body awareness are explained to help readers understand the complexity of movement. A definition of related motor learning and a review of related key concepts, including practice, feedback, modeling or demonstration, and mental rehearsal, also are provided.
Case Studies 9-1 through 9-3 illustrate the diversity of motor control deficits found in children. Motor control deficits interfere with activities of daily living, self-care, social participation, play, and academics (Figure 9-2). The following section presents an overview of motor control and a review of the motor control approaches that led to the development of dynamical systems theory.
MOTOR CONTROL: OVERVIEW AND DEFINITION
Motor control is defined as the “ability to regulate or direct the mechanisms essential to movement” (p. 4).108 Motor control refers to how the central nervous system organizes movement, how we quantify movement, and the nature of movement. Researchers interested in motor control examine the mechanisms, strategies, and development of movement, as well as causes of motor dysfunction. Occupational therapy practitioners use this knowledge to design effective intervention so that children with motor control deficits may participate in their desired occupations.
Movement deficits occur in numerous conditions including cerebral palsy, developmental coordination disorder (DCD), pervasive developmental disorder, Down syndrome, sensory integration disorders, and acquired brain injury. Historically, intervention strategies used by practitioners varied according to the etiology and nature of motor impairments.71,108 Traditionally, therapists have used bottom-up approaches, hypothesizing that if they treat the underlying causes of motor dysfunction, the child’s function will improve. Therefore, the goals of intervention included improving abnormal muscle tone, sensory dysfunction, weakness, and poor endurance. Bottom-up approaches include sensory integration intervention, neurodevelopmental treatment, strength training, and perceptual motor training.5,11,25 These interventions focus on decreasing the underlying deficit and improving performance.11,73 These motor control approaches support a hierarchical model of control—that is, the brain (central nervous system) controls movements. Case Study 9-4 illustrates a bottom-up approach.
Overall, bottom-up approaches have not been found to be effective in improving the occupations of children.60,66,71,77,78,92,111,112 Bottom-up approaches do not take into consideration the dynamical nature of movement or the multiple systems that interact with one another to produce movement. In contrast, dynamical systems theory was developed to describe how systems interact and how these interactions are responsible for motor performance.108,117
DYNAMICAL SYSTEMS THEORY
Dynamical systems theorists propose that movement derives from a variety of sources and takes place within a variety of contexts.108,117 This contemporary motor control theory assists therapists in framing evaluation and subsequent intervention to promote movement in children and youth with motor dysfunction. Dynamical systems theory suggests that movement is dependent on task characteristics and an interaction among cognitive, neuromusculoskeletal, sensory, perceptual, socio-emotional, and environmental systems (Figure 9-3). The interaction among systems is essential to predictive and adaptive control of movement; motor performance results from an interaction between adaptable and flexible systems. Dysfunction occurs when there is a lack of flexibility or adaptability of movements to accommodate task demands and environmental constraints.
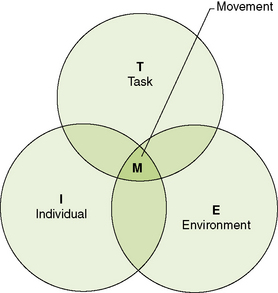
FIGURE 9-3 Dynamical systems theory. From Shumway-Cook, A., & Woollacott, M. H. [2007]. Motor control: translating research into clinical practice [3rd ed.]. Philadelphia: Lippincott Williams & Wilkins.
This lack of adaptability or flexibility is observed in children with motor impairments, who frequently move in limited or stereotypical ways—that is, they have a small repertoire of movements. For example, 3-year-old Sakina, who experienced motor planning deficits, had only one motor pattern for climbing onto a tricycle and could not get on the tricycle when it was turned at a different angle. Case Study 9-5 illustrates the complexity and dynamical nature of movement.
As depicted in this case, Teagan’s movement arises from interactions and organization among many systems and is not simply a matter of muscle tone and central nervous system functioning (as bottom-up approaches suggest). The occupational therapy practitioner simplified the task by using a tee-stand, instead of requesting that Teagan hit a moving target. Stationary tasks (e.g., ball placed on tee-stand) are more easily accomplished than dynamic tasks (e.g., hitting a moving target).
The difficulty of planning and executing movement may also be changed by altering the degrees of freedom required to accomplish a movement. Degrees of freedom are defined as possible planes of motion in the joints controlled by the musculoskeletal and central nervous system.9,108 Decreasing the degrees of freedom required for movement may result in more functional movement. Holding the bat close to the ball and hitting it while it is on the tee-stand require that Teagan control fewer planes of motion, thereby limiting the degrees of freedom for the movement when compared with hitting a moving ball.
Teagan may also learn to contract movements together (i.e., synergistically) to decrease the degrees of freedom. For example, synergistic movements (or coupling) occur when children reach for objects, because the elbow, wrist, and fingers tend to extend toward the object.109,113,121 Other synergistic patterns have been found with walking, tapping tasks, and throwing.18,142
Teagan may adopt movement tendencies or patterns in which he is comfortable, such as running with his arms close to his body. Dynamical systems theorists use the term attractor state to describe the tendency to stay in the patterns of the status quo.18 For example, a child may have the tendency to sit in a posterior pelvic tilt. This pattern may not be most efficient and may even prevent the child from achieving other milestones (e.g., such as reaching with ease). The therapist’s role is to identify the attractor state and help facilitate movement away from this state (i.e., perturbation), if it is not functional for the client. W-sitting (Figure 9-4) is a common attractor state children use to maintain stable sitting but is not recommended because it may dislocate hips and limit trunk strengthening. Facilitating a child away from an attractor state is often referred to as a perturbation—a force that alters the movement pattern. Perturbations can be used to help children move in different ways.
Dynamical systems theory integrates well with occupational therapy principles and can be used to facilitate intervention. Specifically, a child learns movement more easily and effectively if (1) the movement is taught as a whole (versus part); (2) the movement is performed in variable situations; (3) the child is allowed to actively problem-solve the actions required; and (4) the activity is meaningful to the child. Summarized next are findings from motor control literature on the non-linear dynamical systems concepts of whole learning, variability, problem-solving, and meaning, and their influence on occupational therapy practice.
Whole Learning
According to dynamical systems theory, many systems are involved and interact with each other to plan and execute movement.108 Therefore, engaging in the whole activity (occupation) targets and facilitates multiple systems and the interactions required for effective movement. Overall, learning the whole motor task is more effective and motivating than learning only a part of the movement.74,110
Children perform whole tasks more efficiently and with better coordination than when they are asked to perform only a part or component of the movement.35 Van der Weel and colleagues found that children with cerebral palsy used more supination when banging a drum than when simply exercising.124 Not only did children perform the task more efficiently, but they also engaged in the task for longer periods of time and activated more areas of the brain during the activity. In addition, functional magnetic resonance imaging (fMRI) studies indicate that more areas of the brain are activated when subjects engage in meaningful whole tasks versus parts of the tasks.62
Engaging in the whole activity or occupation requires children to use multiple systems and to respond to changes within and between systems. The ability to respond to this variability within systems is a hallmark of functional movement. Typically developing children, for example, use multiple strategies when moving, as opposed to children with DCD who have been found to exhibit limited variability and adaptability in their movement.71,104 Therefore, one goal of occupational therapy intervention is to promote variability and flexibility in movements.
Variability
Dynamical systems theorists propose that movement requires an ability to adapt to changes within and between systems; in other words, variability is central to functional movement. Variability is inherent in activity (e.g., reaching for different objects, environmental stimuli) as well as within and between systems (e.g., interactions between visual and sensory systems).
Movement occurs in a variety of settings and requires that children adapt to environmental changes (using visual and auditory systems) or internal changes (perceived through vestibular and proprioceptive systems) changes. For example, children may need to adjust movements in response to interpretations of visual input (e.g., the ball is coming fast versus slow); children may experience physiological changes (e.g., low energy) affecting movement patterns. The environment may pose changes (e.g., weather, terrain, other children). Functional movement, the goal of motor control intervention, requires that children possess a variety of motor skills.
Because variability is essential to functional movement, occupational therapists teach children to move in variable ways while engaging in occupations. Thus, the expectation of intervention is that the child perform movements in a variety of ways versus repeating and learning one pattern of movement. For example, requesting a child sit in a corner seat to repeatedly pick up a block and drop it into a stationary container requires no adaptability on the child’s part. The child is repeating the same motion. A better intervention session would include placing the blocks scattered on the floor and requiring the child reach in different directions (for different sized blocks) (Figure 9-5).
Performing movements in multiple ways requires that children problem-solve and self-correct. For example, to learn to build a sand castle, the child problem-solves his or her position in the sand and how to scoop and place the sand. Learning a new motor task is more likely to occur if this is a meaningful, socially engaging activity for the child. The child must position his or her body away from the structure and use adequate timing and force to make the castle of his choice. All children use problem-solving to develop and refine movement; therefore, problem-solving is an important part of motor control.
Problem-solving
Improved retention of motor skills occurs when children problem-solve and self-correct for motor errors.12,50,76,79,93 Children learn and retain motor skills more from intrinsically problem-solving a motor action than from receiving external feedback during an action (such as hand-over-hand assistance). Self-correcting enables children to rely on internal cues that indicate the effectiveness of movement and thereby help them adapt and modify movements in a variety of contexts.40,48
Therefore, therapists working to improve a child’s motor performance provide many opportunities for the child to actively solve motor problems by doing, rather than repetitive practicing of a part of the movement. Setting up the environment to facilitate physical, social, and cognitive tasks encourages the child to discover how to move, explore options, and self-correct movement errors beneficial to motor learning.
Not only do children benefit from problem-solving how to move, they also benefit from engaging in activities that they find meaningful. Participation in meaningful activities is central to occupational therapy practice and also improves the child’s motor control.
Meaning
Dynamical systems theory proposes that the interactions between systems (including the emotional system) influence movements. Occupational therapists have historically viewed the meaningfulness of activities as essential to practice and acknowledge the benefits of purposeful activity in motivating clients to perform.33,61,85,119 Kielhofner uses the term volition to describe one’s motivations, goals, desires, and belief in skill.61 A child’s participation in motor tasks is influenced by the extent to which he can identify his own interests and goals and believes he will be effective in those motor tasks. Illustrative of these concepts is that children are more motivated to engage in difficult motor skills if they find the activity important and fun and if they believe they can be successful.64
In addition, subjects participate for longer periods of time and perform more repetitions when activities are meaningful.110,141 Not only do subjects perform longer, but, in addition, the quality of movement improves when the activity has meaning to the child.41 Meaning may be determined by asking children directly using semi-structured interviews. Cohn, Miller, and Tickle-Degnen22 and O’Brien et al.86 found that children with motor deficits wanted to participate in “regular” activities with friends. These expressed interests suggest that practitioners promote meaningful physical activity (such as skiing, swimming, cycling, running, and skating) for children who have motor impairments.
To design effective motor control intervention, occupational therapists must acknowledge the meaning a child attaches to the activity by learning the child’s goals and desires.3,61,71 Meaning is derived from an individual’s experience and viewpoint; thus therapists involve the child in selecting and designing the activity.
DEVELOPMENT OF MOTOR CONTROL
The development of motor skills occurs in three stages—cognitive, associative, and autonomous—and involves an interaction among three processes (i.e., cognition, perception, and action).108 These stages and processes are considered dynamic in that they are constantly changing and interacting with each other in relation to the motor skill or performance requirements.
The cognitive stage refers to the skill acquisition stage. In this stage, the learner practices new movements, errors are common, and movements are inefficient and inconsistent. During this stage, learners need frequent repetition and feedback. Children learning to hold a spoon, for example, may need reminders to take little scoops of food, and to move the spoon to the mouth slowly.
The associative stage involves skill refinement, increased performance, decreased errors, and increased consistency and efficiency. During this stage the learner relates past experiences to the present, thereby “associating” movements (e.g., the child may realize that the last time he moved his hand too quickly, the food dropped off the spoon, so he reminds himself to slow down).
During the autonomous stage, the learner retains the skills and can perform the movement functionally. During this stage, skills are transferred easily to different settings and refined. For example, during this stage a child can feed himself or herself a variety of foods using a spoon and simultaneously carry on a conversation at the table.
Each stage of movement involves interactions among the processes of cognition, perception, and action.108 Cognition refers to intent or the child’s motivation to move, and also to the ability to plan the movement. Cognitive processes are used in decisions about how to use an object (e.g., throw versus catch).
Perception refers to how the individual receives and makes sense of a stimulus (visual, auditory, tactile, kinesthetic, vestibular, olfactory). Perception involves attributing meaning to sensory input. Perception refers to both peripheral sensory mechanisms and higher level processing that add interpretation and meaning to stimuli.108 For example, the child must be able to identify the object coming toward him or her or “feel” balance.
The process of action includes muscle contractions, patterns, and precision and nature of the movement (dynamic versus static). Research devoted to the action stage explores factors such as strength, ability to co-activate muscles groups, reaction time, and timing and sequencing, all contributors to movement.87,91,97
Each stage and process of movement involves a variety of factors that contribute to the motor performance. The following section provides an overview of factors that contribute to motor performance.
FACTORS AFFECTING MOTOR PERFORMANCE
A variety of factors are involved in producing motor skills and participation in occupations. After identifying the child’s desires and occupational goals, occupational therapists examine factors within a variety of systems (e.g., social-emotional, physical, sensory) to determine what may be interfering with or facilitating optimal movement.
Social-Emotional Factors
Emotion is a psychological state that may affect motor performance. Individuals are able to achieve motor challenges in which they attribute positive feelings.88,96,103 For example, athletes use the “power of positive thinking” to visualize achievement and subsequently exhibit improved motor performance as a result.81 Conversely, children may experience difficulty performing at their best when they are experiencing negative emotions (such as anxiety or fear). Children may perform less effectively if they are feeling pushed or judged; they may be afraid of failure. Children may want to perform an activity or skill and feel frustrated when they cannot. Watching the child’s expressions during therapy can provide cues to therapists about the degree of difficulty (Figure 9-6).
The practitioner’s therapeutic use of self can facilitate the child’s motor control. Pushing children too hard (e.g., to the point of tears) produces chaos versus self-organization and is not conducive to motor learning. A child who is crying is not actively problem-solving or ready to learn a new motor skill. Children learn movement best when they are challenged at a level at which success is achievable and they are emotionally ready to engage in problem-solving.
Physical Factors
While social-emotional factors are important for movement, physical limitations (and/or strengths) must be equally considered. Occupational therapy practitioners examine physical client factors using knowledge of biomechanics and kinesiology. The following section provides a brief overview of these client factors.
Range of motion is necessary for movement to occur. Impairments in range of motion may require children learn how to move differently (to compensate) or make adaptations in how activities are performed. Interventions are developed to help children increase range of motion to improve function. When examining range of motion, therapists also observe the physical appearance of the structures such as symmetry, physical anomalies, scar tissue, and stature. Not only is it important to evaluate these things, but also to consider how these areas affect movement. Occupational therapy intervention for physical anomalies often includes teaching children to compensate by performing activities in a different manner or providing adaptive equipment to help children perform occupations.
Muscle tone affects movement patterns and is considered in evaluation of motor performance. Muscle tone is defined as the resting state of the muscle. Typical muscle tone allows movement into and out of positions with ease. Children with hypertonicity exhibit increased muscle tone, resulting in limited movements; those with hypotonicity exhibit low muscle tone, which results in excessive range of movement but limited control over movement.
The goal of occupational therapy intervention is not to change the muscle tone, but rather to improve the child’s ability to perform occupations. This may be accomplished by providing children with assistive support, such as a supportive seat or an alternative tabletop (Figure 9-7). Case Study 9-6 illustrates how engaging the child in play and supporting an upright posture may improve muscle tone or, conversely, how despite abnormal muscle tone, a child can learn to move.
Strength limitations may interfere with motor performance. Strength is defined as the voluntary recruitment of muscle fibers. In strength training, the child repeats movements, often with added resistance or weight. Although it is possible to increase a child’s strength through exercise routines, engaging the child in play is more suitable to occupational therapy. Kaufman and Schilling reported changes in muscle strength, motor function and proprioceptive position in space in a young child with DCD after a strength training program.59 However, the authors did not examine how the program affected the child’s occupational performance.
RELATING DYNAMICAL SYSTEMS THEORY TO BALANCE
Because balance is an integral part of movement, occupational therapy practitioners frequently address balance issues in children. For example, children must possess adequate standing balance to dress and play. Children require adequate sitting balance for handwriting, feeding, and academic tasks. Balance involves the interaction of multiple systems (e.g., sensory, neuromuscular, skeletal, cognition, and environmental). How dynamical systems theory relates to balance is discussed next.
Balance: An Overview
For children to carry out skillful, coordinated, and effective movements, whether they are fine motor or gross motor actions, they must have an adequate foundation of balance and postural control. Children with poor posture and/or balance often exhibit limited motor skills, in part because the foundation for carrying out skillful movements is not well developed (e.g., posture is inappropriate and/or control of balance is poor or inconsistent).133,136 Frequently, it is the core muscles of the trunk and muscles of the lower extremity, along with the timing of activity in the muscles of the trunk and lower extremities, that contribute to the motor control issues observed in children who have difficulty carrying out both fine and gross motor tasks.13,94 Thus, it is important to have a rich understanding of the nature of the processes and developmental milestones associated with developing and maintaining balance.
To understand posture and balance and their intricate inter-relationships, it is important to define and describe these terms. Posture is defined as the alignment of body parts and involves the relationships among various segments of the body. The optimal alignment of body parts (e.g., posture) for standing is close to a straight line from the ankles through the hips, shoulders, and ears. In contrast with posture, balance has to do with overall body equilibrium or stability. Biomechanically, it is described as the maintenance of the center of mass over the base of support. Maintaining the center of mass over the base of support requires that the child equalize differences between two opposing forces: gravity, which is constantly pulling on the body and moving it out of alignment, and the internal force of muscular activity, which acts against gravity to maintain the body in its appropriate or desired alignment.133
Stability is required for movement and functional activities such as hand skills, feeding, dressing, bathing, and play. Stability and balance change as children modify their posture (e.g., the alignment of body parts). For example, if a child raises the arms over the head (as when reaching for a toy), the center of mass increases and stability diminishes, whereas if a child bends the knees, the center of mass decreases and stability increases. Generally, the higher the center of mass, the less stable balance is, and the lower the center of mass, the more stable the balance. Assuming different foot positions add to the effect by changing the child’s posture on the base of support. Standing with the feet in a tandem position narrows the base of support and thus decreases stability whereas standing with the feet shoulder width apart provides a wider base of support and increases stability in relation to standing with feet in tandem. Thus, when planning intervention, occupational therapy practitioners should keep in mind that it is more difficult for children to perform activities standing with one foot forward than with feet shoulder width apart. If a child then stands on the balls of the feet, this both raises the center of mass and reduces the base of support and decreases stability. These examples illustrate the subtle and intricate relationship between posture and balance. Both are controlled by the part of the sensory-motor systems referred to as the postural control system.133
The postural system maintains the body’s stability by maintaining (1) the body in a stationary position when necessary (e.g., static balance); (2) balance when changing from one discrete position to another (e.g., moving from supine to sitting or from sitting to standing); and (3) equilibrium while the body is in continuous motion (e.g., walking, running). Multiple physiological systems are involved in carrying out these highly interrelated functions and include the musculoskeletal, neuromuscular, and sensory systems (i.e., visual, vestibular, and proprioceptive or somatosensory).
To carry out these functions, the child must first detect the presence of instability—that is, any perturbation or disturbance to balance, must be detected and evaluated with regard to its potential for leading to a loss of balance (Figure 9-8) (Case Study 9-7). This is the job of the visual, vestibular, and proprioceptive systems. Generally, input from these systems is transmitted to the brain and a motor plan for correcting or adapting to the changes is developed. This motor plan is transmitted through the primary motor systems to the periphery to appropriate musculature. These muscle groups contract, moving the skeleton as dictated by the muscular activity, and balance is maintained or recovered.136
Sensory Organization and Control of Balance/Posture
To maintain balance, the child must be able to detect when balance has been challenged and equilibrium or stability is changing. The vestibular, proprioceptive, and visual systems work together to provide information to detect changes in postural stability, as discussed next.
Vestibular System
The vestibular system is a powerful source of information about orientation of the body, position of the head, and movement of the head. Children use vestibular information to understand where their head and body are in space.52,53 One set of sensory receptors in the inner ear signals the position of the head in relation to gravity (otoliths); another set helps to detect the speed and direction of body movement based in part on what is happening to the head (semicircular canals). The vestibular system provides critical input regarding head position, body orientation, balance, and equilibrium.2 It helps to detect and interpret the following:
Proprioceptive/Somatosensory Systems
The proprioceptive system contributes information critical to maintaining posture and balance. It provides information from the sensory receptors in the muscles (muscle spindle), tendons (Golgi tendon organs), and joints (joint receptors) throughout the body to the brain. Children use this proprioceptive information to detect body position, determine stability, and maintain posture and balance. The proprioceptive system conveys critical information about the position of the joints of the body and their relationship or alignment with each other, and gives children a sense of overall position of the body. The proprioceptive system also provides information about joint movement (e.g., changes in joint position), along with speed and direction of those changes/movements.23,56,107,133 Thus, the proprioceptive system helps children detect:
Visual System
The visual system also contributes to posture and balance control. Briefly, the visual system may be thought of as a monitoring system that tracks a variety of aspects of information integral to maintaining balance and postural control.29,47,90,107,115,133 For example, the visual system:
• Monitors the environment and provides information that addresses:
• What are the primary features of the environment?
• What is present in the environment (objects, people)?
• Are these objects/people moving or stationary?
• Where are the objects/people in the environment in relation to each other?
• Monitors the body and its movement in the environment and transmits information about:
• Self-motion: is the body stationary or moving?
• Speed and direction of body movement
• Verticality of the body: where is the head/body in relation to gravity?
• Monitors vestibular and proprioceptive input and indicates:
Intersensory Function
Many of the foregoing functions are intersensory functions because they involve synthesizing and integrating visual, proprioceptive and/or vestibular information in making decisions related to the stability of the body. It is well known that the sensory systems do not work in isolation of each other; rather they work in tandem and share information that is needed to detect instability and help correct that instability. Three conditions reveal how intersensory functions contribute to balance control: (1) redundancy of information, a condition in which all three sources of sensory information (visual, proprioceptive, and vestibular) are present and accurate; (2) removal or substitution of sensory information, a condition in which one or more of the three inputs is missing or degraded; and (3) sensory conflict, a condition in which input from any one of the three sensory systems is in conflict with other inputs (e.g., visual input may indicate that balance is unstable, whereas proprioceptive or vestibular information indicates that balance is stable).42,107,133,138
The redundancy condition is the most common condition in which children maintain balance; balance is generally well controlled in conditions where all three sources of sensory information are present and accurate. In many instances, one or more of these primary sensory inputs is not available or is inadequate, and in this case (removal or substitution of sensory information) the child must rely on other inputs to determine the nature or status of the equilibrium of the body. For example, children with visual impairments maintain balance based solely on inputs from the vestibular and proprioceptive systems. The third condition, sensory conflict, creates the greatest challenge to balance because the brain must determine which input is conflicting or erroneous and which is accurate, and then ignore or suppress the conflicting information. In this case, the child uses the remaining sources to judge the nature and degree of instability.133
Intersensory function and the effect of different sensory inputs on balance control can be measured by the amount of postural sway a child exhibits under different sensory conditions. To examine this, a child stands upright on a force platform and attempts to maintain balance under different combinations of sensory conditions (Figure 9-9):
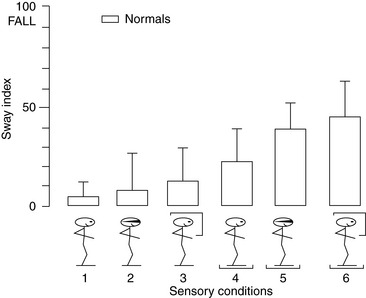
FIGURE 9-9 Sway and sensory conditions. 1 = visual, proprioceptive, and vestibular inputs all present and accurate; 2 = visual input is not available; 3 = conflicting visual information is present; 4 = ankle proprioception information is degraded; 5 = visual is not available and proprioceptive information is degraded; 6 = conflicting visual information is present, proprioceptive information is degraded. From Horak, F., Diener, H., & Nasher, L. [1990]. Postural strategies associated with somatosensory and vestibular loss, Experimental Brain Research, 82, 167–177.
2. No vision (proprioceptive/vestibular information present)
3. Conflicting visual information (proprioceptive/vestibular information present)
4. Conflicting/degraded proprioceptive information (visual/vestibular information present and accurate)
5. No vision and conflicting/degraded proprioceptive information (vestibular information accurate)
6. Conflicting visual information and conflicting/degraded proprioceptive information (vestibular information present and accurate)
In each of these conditions, changes in the amount of sway and/or in sway patterns can indicate deficits in a particular sensory system.107,133,139
When all three sensory inputs are available (Condition 1), sway is minimal; when visual input is removed (Condition 2), sway increases slightly suggesting that visual input is important in maintaining balance. It is interesting that in any condition when ankle proprioception is conflicting or degraded (e.g., Conditions 4, 5, 6) sway increases dramatically compared with when it is not degraded (e.g., Conditions 1, 2, 3). Sway is greatest when only vestibular information is present and “accurate” (Conditions 5, 6). The most difficult condition for maintaining balance is when ankle proprioception is degraded and visual input is conflicting and has to be suppressed. This type of condition may occur in children with hemiplegia who have limited sensation in the affected extremity (e.g., decreased ankle proprioception) and poor visual perceptual skills.
Motor Coordination Aspects of Posture/Balance Control
Once a child becomes posturally unstable, some correction for the disturbance to balance must take place quickly to avoid loss of balance. The response to instability and recovery of balance is a function of the motor control system and is referred to as the Motor Coordination component of balance control.
Corrective responses to disturbances of stability involve different levels of the motor control system. Some responses are “wired-in,” that is, they are reflexive or automatic and may involve lower levels of the nervous system (e.g., the stretch reflex, postural reflexes). Other responses may require higher-order analysis of visual, proprioceptive, and vestibular information and have been shown to involve supraspinal mechanisms, including the cortical regions. These latter responses include the postural synergies and integrative responses, both of which are adaptable or modifiable and are affected by practice and experience. These supraspinal responses or types of postural control include reactive responses (responses that occur after an instability or disturbance to balance have occurred) and anticipatory responses (responses planned before the occurrence of instability and designed to avoid instability). Presented next is a brief review of the postural reflexes, postural synergies, and integrative responses.16,17,82,83,122,136,140
Postural Reflexes
Children tend to develop postural reflexes in a predictable sequence: prone and supine positions to quadruped to standing. Postural reflexes act primarily to align the head with the body, keep the head in an upright position, and maintain equilibrium. There are three major categories of postural reflexes: attitudinal (also known as primitive), righting, and equilibrium and protective reflexes (Table 9-1). Attitudinal reflexes appear within the first year and are designed to align the head with the body (limbs) and the upper body with lower body. For example, when an infant changes his head position, the position of his limbs automatically shift (e.g., the symmetrical tonic neck and asymmetrical tonic neck reflexes). Most attitudinal reflexes are suppressed early in infancy but may reappear after injury or trauma to the brain.8,43,44,51,107,133
Righting reflexes are typically observed at about 3 months of age and persist to 6 months of age. When rotation is imposed on the body, the righting reflexes realign the segments of the body and bring the body into appropriate alignment. They are designed to align the head with gravity (keep the child’s head upright) and include, among others, the optical righting and labyrinthine righting reflexes. These two reflexes realign the head vertically when the body is displaced and are mediated, respectively, by the visual and vestibular systems.
The third category, equilibrium and protective reflexes, are present at about 6 months of age and persist throughout life to help the child remain upright. Equilibrium and protective reflexes are whole-body responses to instability. Shoves or pushes to the body or tilting of surfaces on which the child is standing or sitting will elicit these responses. These reflexes help children protect the body from injury during loss of balance; if some instability occurs that could lead to a fall, the child extends the appropriate set of limbs to protect the body. Children develop equilibrium reactions in supine and prone positions between 5 and 8 months of age and continue to develop equilibrium in more upright positions throughout early childhood.
Occupational therapy practitioners evaluate reflexes and reactions as an indication of the child’s neuromotor status, and the intervention emphasis is on improving postural stability and equilibrium to enhance the child’s occupational performance. Thus, therapists help children improve balance and equilibrium reactions for play, mobility, feeding, dressing, self-care, and school functions.
Postural Synergies
Postural synergies are an important part of posture and balance development. A synergy consists of a group of muscles acting as a single unit; it involves the “coupling” of muscle activation in a particular set of muscles. Postural synergies act to help correct for disturbances to balance or equilibrium, and although they are believed to be an inherent part of the motor system, they appear to be regulated at supraspinal levels. For this reason, postural synergies are often referred to as “long-loop” reflexes, indicating that they can be modified through practice and experience. Three major postural synergies—ankle, hip, and step—react to disturbances to equilibrium when the individual is in an upright stance. These are present as early as 2 years but continue to develop and undergo refinement until 7 to 10 years of age.
The ankle strategy involves the sequential contraction of the lower extremities in a disto-proximal direction (i.e., from the ankles up).83,84,107,133 The ankle strategy is usually activated when/if the child is standing on a firm surface that is wider than a foot (e.g., a large platform or a beam 6” or wider). Typically it is elicited when the child’s center of mass is displaced by a small amount (see Figure 9-9).
The hip strategy involves the sequential contraction of the muscles of the lower body in a proximo-distal direction (from the hips downward).82,83,107,133,140 The hip strategy is typically activated when/if the child is standing on a narrow or unstable/compliant surface. The strategy is elicited primarily with a fast, large perturbation to body stability (a quick but substantial jerk). This often occurs in young children when they attempt to walk a narrow (2′′) beam or stand on a balance board. When standing balance is perturbed in a backward direction, muscles on the anterior of the body contract in a consistent sequence (see Figure 9-9).
The third postural synergy is the step strategy; although this is elicited easily, the muscle activity involved is not well documented because this is a more complex strategy for regaining equilibrium.107 The step strategy typically occurs when or if the perturbation to balance is great enough to cause the center of mass to fall outside the base of support. This can be elicited under a variety of conditions, depending on the level of control of the child. In these instances, the response is a step/hop that serves to restore equilibrium. Children may use a variety of different combinations of strategies, depending on the task, individual, or circumstance.
Integrative Responses
Another set of responses often involved in responding to perturbations to balance are those referred to as integrative responses. These fall into the category of higher-order, conscious or voluntary responses that are thought to be anticipatory in nature. Integrative responses are preplanned and are designed to accommodate known or anticipated disturbances to balance. Integrative responses by definition involve intersensory functions, where the brain must either substitute one source of sensory information for another (e.g., when visual input is not available) or if there is a need to suppress erroneous incoming sensory information. Postural synergies can and do occur under such conditions as well.70,106,107,133 A common example of the use of integrative, anticipatory responses may be seen in the form of preplanning for possible changes in equilibrium when a child is asked to move through an obstacle course. In this case, the system must plan for maintaining balance control as the child moves through a series of obstacles that require the body move in a variety of positions and on, over, and/or around a number of stable and unstable objects.
Balance Control Issues in Children with Developmental Coordination Disorder
Children with DCD exhibit a variety of motor control disorders that include deficits in balance and postural control and other gross motor and fine motor eye-hand coordination skills that interfere with activities of daily living, school, feeding, and social participation.38,75,130,135 Examining the differences in balance and sensory processing between children with and without DCD may provide some insight into the motor coordination difficulties of children with DCD.
Vision and Proprioception
Children integrate and use information from visual, proprioceptive, and vestibular systems to control balance. Several studies indicate that children with DCD rely more heavily on visual input in controlling balance than typical children.128 It is possible that children with DCD who rely on vision to regulate balance may do so in part because of the inability to process and use proprioceptive input effectively.
Proprioceptive feedback is believed to play an important role in correcting for externally or internally induced errors in balance, as well as in modifying the speed and force of corrective actions. Effective processing of proprioceptive input is especially important in recognizing when one is becoming or close to becoming unstable. Children with DCD have more difficulty with this than typical children and thus lose control of balance more often. They also have difficulty in recovering balance after onset of instability. That is, when balance is lost or they become unstable, they cannot easily regain a stable state. Recovery of stability is also thought to be in large part a proprioceptive-related function.20
The brain may place greater weight on proprioceptive, visual, or vestibular inputs in regulating static balance. Inder and Sullivan reported that visual and vestibular functions in older children with DCD lagged behind those of their age-related peers.55 Based on performances on the Test of Visual-Perceptual Skills, it is clear that many children with DCD have less well-developed visual perception skills than typical children.120 Young children with DCD (4 to 6 years of age) have more difficulty regulating balance (e.g., they exhibit more sway) when proprioceptive input is degraded than when it is not.20 Children with DCD may rely more on proprioceptive input for balance control than typical children because of visual perception deficits. However, such deficits are not present in all of these children.37,95 They often have difficulty effectively integrating visual and proprioceptive information, a process important to maintaining and recovering control of balance.57,128
Overall evidence suggests that many children, including those with DCD, have deficits not in any one sensory system but in sensory organization (i.e., integration of visual, proprioceptive and/or vestibular inputs). For that reason, many young children, in particular children with DCD, tend to rely more on vision than proprioception for balance control. The child’s age certainly plays an important role in this integrative process because younger children do appear to have less well-developed integrative capacities than older children (10 years and older).87,135
Improving Balance: Intervention
Planning for and organizing a program of intervention activities to promote balance control is of critical importance to occupational therapists. Such planning and organization requires that therapists use as much information as possible about various aspects of balance so that tasks can be designed to provide a gradual, orderly, and sequential program of activities to promote and enrich the child’s ability to maintain stability. Therapists design tasks that are both varied and interesting to the child for whom the program is intended.
Occupational therapy practitioners help children perform a variety of daily living activities, play, and academic activities, all of which require balance. One perspective on how to approach analyzing and developing tasks to challenge balance in a systematic way is to consider the major ways in which the body and the environment can be structured to challenge different aspects of balance.134 These can be thought of as components of balance, which can be varied or combined in different ways to encourage adaptive balance control. By analyzing and facilitating components in an occupation-based intervention, the child can easily generalize new skills to his or her everyday natural environment. Components of balance may be grouped as primary or secondary, as described next.
Primary Components
Primary components involve aspects of balance that are integral to developing efficient balance control and consist of the following: body movement, use of vision, and external base of support. Therapists address these first in planning balance interventions.
Body Movement: An important component in any balance activity or task is whether the child is maintaining balance in a stationary position (static) or maintaining balance while the body is moving (dynamic). Because static and dynamic balance skills are important for effective stability in a wide variety of situations, and because they tend to be somewhat independent of each other, it is important to provide opportunities to develop control under conditions where the body remains stationary and where the body is moving or changing positions. Therefore, occupational therapy intervention to improve sitting balance may include sitting in one position and coloring (static) and sitting on an unstable surface (e.g., therapy ball) and playing catch (dynamic).
Use of Vision: Balance is almost always better when visual information is available than when it is not. Most experts agree that it is important to provide opportunities to practice balance under a variety of visual conditions; such practice also has the indirect benefit of providing opportunities to enhance the capacity to use vestibular and proprioceptive input regulating balance. Efforts to improve balance should include tasks where the child balances with vision, with vision occluded, as well as with varying kinds of distortion of visual information (e.g., blocking peripheral vision, wearing goggles, moving in lower levels of illumination). Occupational therapists can incorporate games with children, such as wearing various “funny” glasses.
External Base of Support: The nature of the external surface on which the child is asked to balance is an important part of developing effective balance control. Therapists structure the environment to challenge balance in a variety of ways. For example, the external base of support may be selected to include surfaces that range from:
Occupational therapy practitioners can use a wide range of combinations of different types of surfaces to provide interesting and relevant challenges that encourage improved balance control.
Secondary Components
Secondary components of balance are aspects of balance that can be used to add new and different challenges to balance control and include position of the body, internal base of support, and elevation.
Position of the Body: Examining the position of the body and/or the alignment of different parts or segments of the body provides another set of possibilities for challenging balance. Some common positions that challenge balance include upright position, trunk flexed forward, arms extended in front, hands on hips, arms overhead, and/or any combination of the foregoing. All of these have the effect of modifying the location of the center of mass (even though only slightly in many cases). Thus, occupational therapy practitioners modify the position in which the child balances to challenge stability and improve balance control whether the child is stationary or moving through space.
Internal Base of Support: The internal base of support is a component of balance that involves varying the nature and number of body parts used to maintain balance. Modifications in the internal base of support are an integral ingredient in challenging balance. Some examples of varying the internal base of support are activities requiring the child to balance on two feet or a single foot, knee and a hand, or one foot and a knee. Changing the internal base of support creates different demands on the balance system and in that way adds to the range of adaptations that the child must make. Occupational therapists can make this fun by incorporating different positions into play sessions or relay races (e.g., walk with right hand on left knee).
Elevation: A third and final secondary component important in challenging balance is that of elevation. This has to do with structuring the environment so that the element of height is added. Children tend to perceive a greater risk or challenge to balance with elevation than when they balance on the ground (e.g., non-elevated surface). Typical uses of elevation include balancing on large, very stable boxes of different heights (4″, 8″, 12″ high). Overall, the potential combinations of the foregoing components are almost endless and thus provide a guideline for developing interventions to promote improved balance as well as the child’s confidence in his or her ability to adapt to everyday balance challenges.
Occupational therapists may play climbing games with stacked heights on soft surfaces to promote balance. For example, encouraging children to walk on the blocks without falling into the “water” is a fun game that works on balance.
Examining Balance: Process Characteristics
When the goal is to improve balance for occupational performance, it is important to assess the nature and extent of the control exhibited in carrying out various balance tasks. Box 9-3 provides an assessment of balance. Figure 9-10 is a checklist that includes a series of process characteristics occupational therapists can observe as the child balances in various positions.134
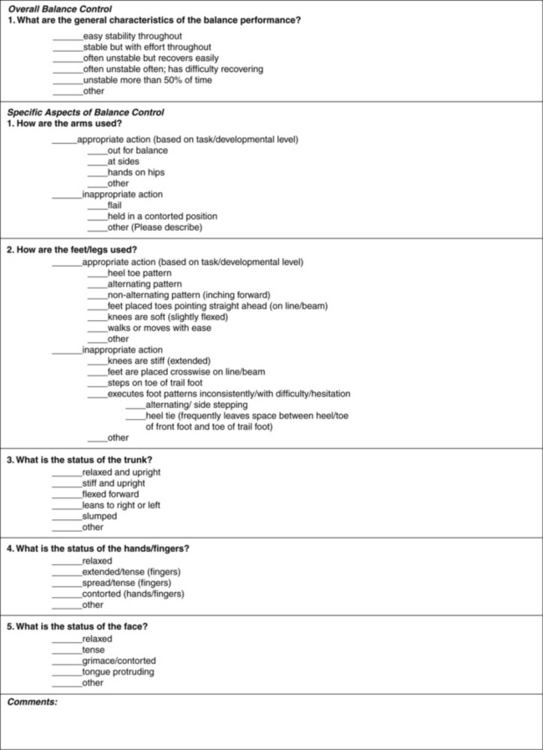
FIGURE 9-10 Williams’ checklist of process characteristics of balance performance.134
VISION, VISUAL PERCEPTION, AND MOTOR CONTROL
Visual perception refers to making sense and attributing meaning to what is seen. Depth perception, for example, refers to the ability to determine distance visually. This section defines the importance of visual perception on controlled movement and balance and explains the theoretical and practical aspects of visual perception related to balance and movement.
Perception and action are coupled in the sense that rapid and accurate perception of the visual components of the environment is intricately linked to the effective planning and execution of associated actions/movements. In general, children rely on vision and the processing of visual information for almost all interactions with the environment. For example the simple acts of reaching for an object on a table, walking down the street, using a computer, and writing a sentence within the boundaries of a defined space all require the ability to perceive and use visual information from the environment. To illustrate, the way a child prepares to reach for and grasp an object clearly differs for blind versus sighted children; a child with vision tends to reach directly toward the target object and automatically shapes the hand as it approaches the object to be grasped. This is accomplished by processing visual information that indicates the distance and direction of the object to be grasped (the transport phase) as well as the processing of the size, shape, and orientation of the object (the grasp phase). In contrast, a child without vision reaches less accurately toward the object to be grasped, and only when the object is touched is the hand shaped in an appropriate way for grasping.21,58,107,125,137,143
It is also clear that it is not by chance that children with motor dysfunctions frequently have perceptual difficulties or limitations.125 For example, the incidence of visual perception difficulties is significantly greater in children with DCD (poor motor coordination) than is the case for children without motor skill problems. In comparison with children with age-appropriate motor skill development, children with DCD also perform more poorly on visual perception tasks that involve judgments about form and space and exhibit deficits in the ability to retain visual information in short-term memory.105 In addition, children with DCD also have great difficulty coordinating eye movements needed to stabilize the focus on moving objects; in other words, they have difficulty synchronizing eye movements with the speed and direction of the path of a moving object.65
A Theoretical Perspective
Visual perception may be thought of as a process that involves the pick-up, processing, analysis/interpretation, and/or retrieval of visual information stored in the brain. Visual perception involves the capacity to discriminate among various visual stimuli and interpret or give meaning to those stimuli. In many ways, visual perception is a learned phenomenon; children learn to use the eyes, to attend to and fixate on visual stimuli, and to search these stimuli for information about the nature and meaning of what is being viewed.72,98,123,126,127 It also involves the capacity to track objects moving in the environment and move the eyes effectively in that process.
Children use information from the visual system, including visual structures and visual perception to understand the nature of the environment so they can respond to what they perceive and act on it.4,31,63,105,131 These components are described in Chapter 12.
Eye Movement Control
Eye movements may be helpful in identifying subgroups of children with movement or motor skill problems, particularly those with eye-hand coordination issues. Eye movements may act as a “window” to understanding general motor control processes; more specifically, they may serve as an early biological marker of motor control problems in children born prematurely and especially those with DCDs.
Tracking/Pursuit Movements: In typical development, von Hofsten and Rosander found that smooth pursuit or tracking of predictable targets (0.1-0.3 Hz sinusoidal motion) develops rapidly in the first 3 months of postnatal life.127 The tracking action was carried out predominantly by movement of the eyes, with some head motion. Other data indicate that tracking (pursuit)63 of slowly moving targets matures by age 7 but continues to improve into adolescence,102 whereas horizontal tracking of faster moving targets (12°/sec) takes longer to develop.1,102 Overall tracking skill appears early in development and continues to improve into adolescence.45 The long time course in acquiring skillful tracking movements may be due partly to incomplete maturation of the tracking/pursuit system and higher-level cognitive factors. For example, the ability to track a ball through space and judge its speed and direction is not fully developed until after 12 years of age.129 Early in development, the head and eyes tend to move together as a single unit in tracking moving objects; the separation of eye and head movement continues to be refined throughout early childhood.129
Langaas et al. studied differences between the tracking movements in children (5-7 years) with and without DCD.65 These workers examined (1) how closely the speed of eye movements matched the speed of target movement and (2) whether eye movements lag behind or ahead of target movement. Typical children tracked moving targets well and needed just a few quick saccades to get back on the target. Children with DCD consistently failed to match target velocity with eye movement speed and thus fell behind the target, suggesting that messages to the brain for making sensory decisions were slower or were incomplete. In addition, children with DCD had difficulty catching up to the target and had significantly more shifts away from the target than those noted in typical children. Thus children with DCD received less sensory input to the brain about the moving object and the surrounding environment. Visual acuity was within normal limits for all of the children and therefore did not account for the differences between children with and without DCD.
It is important to consider the effect that reduced ocular-motor control has on children’s perceptual development. For example, in children with DCD, the lack of effective tracking movements makes anticipatory judgments about speed and direction of moving targets difficult (i.e., they have difficulty judging when and where to go to catch an object). Many young children and those with DCD in particular have problems with catching or intercepting moving objects. The association between ocular-motor control and more general motor impairment has not been verified by research.34
Fixation/Search Movements: Infants develop the capacity to fixate on stationary objects with some degree of control within 4-5 days after birth and during the first two postnatal years. In terms of search processes (e.g., finding information in a picture) and determining the nature of the object or figure being viewed, refinement of this process undergoes important changes between 3 and 6 or 7 years. Whereas young children tend to be unsystematic and spend as much time fixating off target as they do on target (the time and number of fixations also varies widely), older children are more systematic and tend to use more rapid fixations of short duration that are directed to the salient parts of the stimulus being viewed (e.g., they follow the object’s contours). The important difference is that the patterns of fixation of the older child are adapted to fit the characteristics of the object/figure of interest, whereas the young child’s are not.127,129
Body Awareness and Motor Control
Several different terms are used in defining and discussing body awareness. Generally the development of the concept of the physical self involves at least three major components: body schema, body image, and body awareness. Figure 9-11 shows a schematic of the components of the concept of the physical self and the behavioral components specific to body awareness.
Body Schema
The body schema is the neural substrate for body awareness. It is present at birth, and as children grow and develop, this so-called diagram of the body (homunculus) in the sensory and motor areas of the brain is modified, in part, through the sensory-motor experiences (active movement, interaction with the environment, and the feedback derived from those interactions) the child undergoes. The child’s own body representations are processed in distinct regions of the intact brain. An example of the manifestation of the body schema may be seen in the phantom limb phenomenon. Children who have had a limb amputated often report that they “feel” both pain and sensation from the missing limb just as if it were physically present. Children who have cerebral palsy (hemiplegia) tend to ignore the affected limbs.
These clinical observations suggest that sensations received when the limb was intact are stored in the brain and when stimulated cause the child to experience feelings and sensations of the missing limbs. The general consensus is that the body schema becomes defined through sensory input from receptors in the skin, muscles, tendons, joints, and the vestibular system, which act to define the boundaries of the limb(s) in the body schema. These receptors are stimulated through body movement and through the actions of the child that are involved in interacting with persons and objects in the environment. The importance of body schema in motor control lies in its relation to motor planning (e.g., the planning of actions). Children develop body schema through active use of the body. Adequate planning of action is based, in part, on the fullness of the body schema. Theoretically, it is proposed that if information children receive and store in the brain in the form of the body schema is incomplete, imprecise, or simply unavailable, children will have difficulty planning or adequately preparing specific plans for action or movement.
Body Image
Body image refers to the image one has of oneself as a physical entity; it includes the perception that one has of the body’s physical or structural characteristics (e.g., am I short, tall, heavy, lean?) and of one’s physical performance abilities. By its nature, body image has an important emotional component that evolves as the child compares himself or herself to others in the environment in terms of both physical and motor performance characteristics. Integral to the development of an adequate body image is the input from significant others who interact with the child and provide feedback (verbal and nonverbal) about the importance and uniqueness of the child. Clearly, the nature of the interactions between the child and the family, teachers, peers, and others is an important element in the development of a positive self-image.6,15,36,67–69,94,99,118
An interesting aspect of the development of body image is seen in attempts by very young children (e.g., 30 months) to do things that the body size/shape simply will not allow; for example, they often try to fit themselves onto or into miniature toys that are clearly too small for them.27 This suggests that they are still developing body image in terms of the ability to accurately judge the physical characteristics of the body in relation to objects in the environment. Development of body image continues to evolve and be refined throughout early and later childhood, and into adolescence.
Body Awareness
A second component of the physical self-concept is body awareness; it is closely related to body schema in that it involves the conscious awareness of the location, position, and movement of the body and its parts, as well as the relationship between the body and the external environment. The importance of body awareness to motor control is seen in the many challenges that the young child, typical or atypical, faces in judging the characteristics of the body and of objects, people, and events in the surrounding environment. Children use the capacity to hold information about their own body in relation to other objects in the world as the foundation for developing effective plans for execution of movements necessary to achieve specific end goals. For example, the child uses body awareness when moving through obstacle courses, whether they be of natural origin or structured for specific purposes in a clinical setting or when manipulating objects of different sizes and shapes to learn about concepts such as spatial orientation; relationships among shape, size, and weight; and functional uses of objects.27,100,129
Body awareness is defined as the ability to visually discriminate, recognize, and identify labels for various aspects of the body’s physical and motor dimensions. Body awareness can be divided into internal (body-related) and external (environmental) aspects. Internal aspects involve the development and refined awareness of the body itself; external aspects are associated with development and awareness of the relationship of the body to the environment (external space), as well as the extension of select internal aspects of body awareness to external space. Internal aspects of body awareness tend to develop slightly in advance of external components.10,14,80,129 The internal and external aspects of body awareness and the relationships between the two are discussed next (see Figure 9-11).
Internal Aspects: As shown in Figure 9-11, there are five important behavioral indicators of the development of the internal aspects of body awareness.
Reflective self-awareness is manifested, in part, in young children’s ability to recognize themselves in the mirror, to refer to themselves by name, and to point to themselves referentially.15,68,80 Visual self-recognition exemplifies the emergence of the objective self and of body awareness. The development of this aspect of body awareness begins with the toddler’s discrimination of his own real-time limb movements as different from those of other toddlers when viewing paired videos or watching himself and another child in a mirror. Recognition of the movements of the limbs is an early form of the differentiation of the body (self) from the external environment (space). This recognition also serves as the perceptual/perceptual-motor foundation for later development of refined self-awareness and in particular the acquisition of conceptual knowledge about the body.6,99 This reflective self and body awareness typically are present in 2-year-olds. The significance of the awareness of the body’s movements is that it involves a kind of visual-kinesthetic-motor matching that is integral to effective planning and execution of actions.67 For example, children develop self-awareness as they begin to feed themselves and understand where their mouth is in relation to their body.
Laterality refers to the awareness that the body has two sides, that the body is separate from space, and that the limbs on each side of the body can move independently of each other. Initially the infant has only a crude awareness of the distinctness of the body as separate from space.129 Early in development, the infant does not distinguish between the two sides and often moves the two arms/hands and two legs together as a single unit. Gradually, the child begins to be “aware” that the limbs on either side of the body can be used independently of one another. Although at this early stage, the infant does not have “verbal labels” for any aspect of the body, he or she “knows” what is and what is not the body. Much of the defining of the body’s dimensions is derived from feedback from the movement of the body itself. Awareness that the body has two sides is an important part of the development of the perception of other internal aspects of the body and provides the foundation for the acquisition of directionality.
Therapists assess laterality clinically, using a series of both individual and coupled arm and leg movements (child lies in supine and moves various individual and combinations of arm and leg movements as requested by the clinician). The coupled arm/leg movements include both ipsilateral and contralateral (e.g., right arm/right leg versus right arm/left leg). Laterality is established when the child can discriminate and coordinate various individual and combinations of movements of the ipsilateral and contralateral sides of the body. Clearly, then laterality involves both sensory (awareness of limbs) and motor (coordination/control of movements) systems. Children need to develop a sense of laterality (i.e., understand the body has two sides) to move in a coordinated fashion. Awareness of both sides of the body is observed in movements required for feeding, dressing, bathing, play, and academics. Therefore, occupational therapy practitioners facilitate mastery of laterality to help children function in a variety of daily life skills (Figure 9-12).

FIGURE 9-12 Laterality refers to developing an understanding of both sides of the body and having a preferred side for tasks. Craft activities can be used to help children develop a sense of laterality.
Sensory dominance develops as the child becomes aware of his or her body and its parts and its separateness from space. Sensory dominance helps to further define the body, especially the two sides of the body. It manifests in the development of the preferential use of one side of the body. Most children have a well-defined preferred hand and foot by the age of 6 years.130 Occasionally, children as young as 4 years of age have established a hand preference; however most do not. The two categories of sensory dominance are mixed and pure. Pure dominance refers to the preferential use of the eye, hand, and foot on the same side of the body; mixed dominance involves the situation in which the preferred limbs and eye are on opposite sides of the body—that is the child may be right-handed, right-eyed, and left-footed. A large percentage of the adult population has mixed dominance (about 95%).
Hand dominance appears to be associated with cerebral dominance; approximately 90% of the population is right-handed and left cerebral dominant. The left cerebral hemisphere houses the major motor and speech control centers and regulates the actions of the right side of the body. The remaining 10% of the population has been reported to be either right cerebral dominant or have dual dominance. Interestingly, some of these individuals are right-handed, whereas others are left-handed. Handedness also appears to have a familial component. Clearly, mechanisms underlying sensory dominance, in particular handedness, are complex and not well understood.
The period from 4 to 8 years is an important period in the development of hand, eye, and foot preference. By 6 years of age, 81% of children have established a preferred hand, 73% have a preferred eye, and 94% have a preferred foot. Eye preference appears, in general, to be more variable than hand or foot preference. Foot preference is interesting in that there may be two types of foot preference: a preferred balance/strength foot and a preferred skill foot (Figure 9-13). This is most evident in comparing balance times on the right and left feet and examining the skill in kicking a ball. For example, balance is typically better on the side of the preferred foot. Although many children kick using the right foot, these children often have better balance on the left foot. In this case the left foot is considered the “balance foot” and the right foot, the “skill foot.” This makes sense in terms of differentiating the role of each foot in skills such as kicking.129
Body part identification develops at different rates in children and depends, in part, on the experiences of the child and the emphasis placed on language and the learning of the names of body parts. Knowing verbal labels for different body parts further solidifies the distinctness of the body and its parts.129 At 2 years, children can often identify some major body parts (e.g., nose, eyes, ears); by 3 years, they are aware of such parts as head, hand, and foot. By 5 years, a majority of children (55%) know more remote body parts (e.g., thumb, eyebrows) and at 6 to 7 years, 70% to 88% of children can name both major and minor parts of the body consistently (e.g., elbows, wrists, heels, shoulders, hips). At 8 or 9 years, it is rare that a child fails to verbally label all body parts, major or remote (95%). Children recognize verbal labels of body parts (e.g., show me your hand; point to your ankles) slightly earlier than that of attaching verbal labels to those same body parts.
Identifying right and left body parts is the next step in defining the body. This step in the development of body awareness adds to the distinction of the two sides of the body and to the body parts on those distinct sides. Language and spatial awareness are important elements in acquiring the capacity to identify right and left on the body. Developmentally, consistency in naming right and left sides of the body has a linear relationship with age.129 Young children (up to 5 years of age) typically have little concept of right and left; thus, 5-year-olds typically guess right and left on the body. A majority of 6-year-olds (70+%) are consistent in accurately and spontaneously identifying right and left on the body. This capacity continues to evolve so that by the age of 8 to 9 years, 90% to 94% of children have mastered this aspect of body awareness and readily label right and left parts of the body.
Children tend to master body awareness in the following order: (1) hand dominance, (2) body part identification, and (3) right-left discrimination. Overall, the internal aspects of body awareness tend to overlap in development and are loosely sequenced. Children need to develop internal body awareness, including reflective self-awareness, laterality, sensory dominance, body part identification, and right-left discrimination to be aware of their body to effectively move throughout the environment. For example, children with DCD frequently have difficulty “sensing” or “feeling” where their limbs are without looking at them. They may not possess an internal awareness of their body. This interferes with smooth and coordinated movement.
External Aspects: Children must also develop external awareness, including directionality and spatial awareness, to move their body through the environment. External aspects of body awareness are an extension or outgrowth of internal aspects and involve relating the body to space and to objects and other people in space.
Directionality refers to the child’s ability to identify right/left and other dimensions (e.g., top/bottom, front/back, beside) on objects or other persons. Some hypothesize that children project or extend the concepts of right/left and other spatial dimensions of the body onto objects in space. Because the environment has variant spatial references, children appear to use their reflection in the mirror, to refer to themselves by name, and to point to themselves or their own bodies to reference directionality. Thus, knowledge about the body is expanded to objects and persons in space. Most work has focused on directionality defined as identifying right/left on objects and other people.129 Mastery of directionality, in this case, is described as the ability to consistently and accurately identify right and left on another person and to understand the tenuousness of right and left on objects and how this varies with regard to their position (in relation to the object). Identification of other dimensions of objects is thought to be based on knowledge gained via experiences the child has had using language to describe dimensions of the body. Developmentally, with regard to right-left identification, approximately half of 6-to 7-year-olds have mastered directionality (50-52%); not until 9 years of age do a majority of children consistently and spontaneously identify right and left on another person.
Spatial awareness is the other major component of the external aspects of body awareness. This discussion focuses on two aspects of spatial awareness: awareness of the body in relation to objects in space and awareness of relationships between or among objects.99,129 These aspects of body awareness rely heavily on language and the conceptual meaning of the so-called “spatial” words. The former involves relating objects to the body and the body to objects using language. A sample activity might involve the child holding an object (e.g., a doll) and the clinician asking the child to “put the doll behind you,” and “put the doll in front of you,” “put the doll on your right side,” “place the doll on your right foot.” Object-to-child relationships involve the child’s identifying where the object is in relation to himself or herself. By placing a red ball to the right of the child and a blue balloon to the left of the child, and asking the child “where is the red ball/where is the blue balloon,” one can examine the child’s understanding of this relationship.
Object-to-object relationships are more complex and involve identifying where one object is in relation to (an)other object(s). Children 9 to 10 years of age are able to spontaneously identify relationships among objects. For example, place two objects (e.g., a key and a coin) on a table, one in front of the other and one to the right of the other and ask the child the following: “Which object is in front?” “Which object is to the right?” Development of body-object and object-object relationships overlap. Children typically develop these two aspects of spatial awareness as follows: placement of objects in front or back of self; identification of front and back of objects; placement of a standard object in front and back of an object with distinct features (e.g., a doll); placement of an object to one’s own side and to the side of an object with distinct features (e.g., a doll). Development of optimal spatial awareness (including awareness of relationships between or among objects, as well as the relationship between the body and objects in the environment) is integral to adequate planning and carrying out skillful movements. If spatial awareness is lacking or underdeveloped, the child often has difficulty moving and interacting skillfully with the surrounding environment because the child cannot accurately judge these subtle but important relationships between the body and the environment. Spatial awareness is a critical aspect of the movement planning and execution process.
INFLUENCE OF NON-MOTOR FACTORS
Dynamical systems theory suggests that motor control is the result of interactions between many systems, including the environment. These factors include the physical, social, psychological, institutional, and societal influences that may affect occupational performance.3
The physical environment consists of the surroundings, surface (e.g., flat, inclined, smooth, rough, hilly), and setting (inside, outside, city, country) and influences motor demands. Playing tee-ball on a competitive team differs from playing at home with parents. Playing on a rocky surface versus soft grass changes movement and balance requirements. Therapists examine the physical environment to determine the movement required.
The social system is part of the environment and influences movement requirements as well. For example, different motor skill requirements exist for a 10-year-old boy who is eating at home with one parent on a quiet afternoon and for another boy who must feed himself in the busy cafeteria at school with three friends. While the child is in the cafeteria, he wants to interact with his peers, increasing the motor demands for self-feeding. Now the child must try to socialize and feed himself (quickly so he can get to recess), realizing his friends will notice if he spills. Social participation is important to children, and, consequently, the influence of this system must be considered. For example, some children may not want adaptive equipment or special considerations in the classroom that make them “look different” than their peers.
The effect of psychological factors on movement must also be considered.19,88 Attention, concentration, and motivation to perform movements are necessary for motor learning.26,32 The ability to imagine or think through movement (e.g., mental practice) increases motor performance. Children who are motivated to perform or succeed in motor challenges are able to achieve skills more quickly and with better quality than those who do not.41,54,124
Institutional factors include those aspects of the institution or setting that hinder or facilitate movement. For example, institutions may have policies requiring children participate in physical activity. These institutional policies make it possible for children to participate. Requiring children to go outside for recess, for example, is an institutional policy that promotes activity.
Finally, societal influences may influence movement. For example, in the United States, active children are viewed as healthy and thus activities in which children move are expected. For this society, movement (e.g., on the playground, in the backyard) is valued and viewed as important for the child’s development. The environment plays a major role in children’s learning of motor skills and thus must be considered in designing intervention strategies to teach children movement.
MOTOR LEARNING
Motor learning refers to the acquisition or modification of motor skills. Motor learning literature explores transfer of learning, sequencing, and adapting tasks, type and amount of practice, error-based learning, timing, and type of feedback and mental rehearsal. These concepts provide useful information on techniques involved in the teaching-learning process of movement. Being knowledgeable and aware of the teaching-learning process enables therapists to incorporate motor learning principles into practice so that children learn and retain motor function for their daily lives (Box 9-4).
Transfer of Learning
Transfer of learning, or generalization, refers to applying learning to new situations. The goal of occupational therapy intervention is that the child transfer learning performed in the clinic or intervention setting to the natural context. For example, after working on maneuvering a new wheelchair through an obstacle course at the clinic with ease, the therapist hopes the child will be able to maneuver the wheelchair through the school hallway.
Children are best able to transfer motor skills when they have practiced the motor skill within the natural context or in the “real world” situation. Therefore, the best way to help the child be successful in maneuvering the wheelchair through the school hallway is to practice in that setting. The occupational therapist may need to start by teaching some basic wheelchair skills to the child, practice in the hallway after school hours (to decrease obstacles) and work up to maneuvering the wheelchair during class change. Research suggests that children transfer the task more quickly with this intervention strategy than with practicing in a clinic setting only.24,114
Transfer of learning occurs more easily when the motor task is performed during a functional activity or actual occupation, scheduled at its natural time and place, and in the real context.24,32,41,89 In addition, motor skills with similar components are more likely to transfer. For example, a child who has just successfully learned to throw a ball would more easily learn to throw a bean bag at a target.
Sequencing and Adapting Tasks
Grading and adapting motor tasks so that children are successful constitute part of the occupational therapy process (Table 9-2). Generally, discrete tasks are easier to accomplish than continuous tasks. Tasks involving uni-manual movements are often learned or mastered before bi-manual movements.133 Skills manipulating stationary objects develop before skills with moving objects.
“Closed tasks are those in which the environment is stationary during task performance” (p. 407),108 whereas open tasks are ones in which the environment is changing or in motion and involve some inter-trial variability. Closed tasks are generally simpler for most children to accomplish.
Therapists also consider the cognitive demands of activities; children complete simple motor tasks that have fewer cognitive requirements more easily. Tasks with fewer steps are accomplished more readily than those with multiple steps (e.g., throwing at a target is easier than picking up a ball from the container, moving to the starting line, and then throwing at a target). Children acquire tasks that require less precision (e.g., scribbling will be easier than coloring within the lines) more easily than those that require more precision. When sequencing and adapting activities for children, therapists consider the amount of direction required; movement requiring less direction is easier to learn than those requiring multiple directions.
The structure of the environment plays an important role in the nature and complexity of the demands of the activity. For example, environments with variability and extraneous stimuli (e.g., other children) are more challenging and thus more difficult for children because they must continually adapt and adjust.
Practice Levels and Types
Practice is an essential feature of occupational therapy intervention. A considerable amount of research has been conducted on the use of practice to improve or develop motor skills.49,89,114
Massed practice (also known as blocked) is defined as practice in which the period performing the movement is greater than the rest period. This type of practice works best during the cognitive stage, as the subject is just beginning to learn the movements. An example of blocked practice may include working on grasp pattern and release by asking a child to pick up 10 blocks and put them all in a container before taking a break and then repeating the game again.
Distributed practice is defined as practice in which rest between trials is greater than the time of the trial and is most useful during the associative stage (Figure 9-14). A clinical example of distributed practice includes asking the child to pick up bean bags placed on the floor while engaged in a game of swinging. In this scenario, the child is still practicing grasp and release, but the child is also working on postural control and processing vestibular input. Therefore, the child grasps and releases a few bean bags, has a rest while swinging in which he must work on other aspects of skill, and then returns to grasp and release.

FIGURE 9-14 Distributed practice. A, Child begins to learn to swing with feet close to the ground and with frequent rests. B, As the child develops, she is able to swing with her feet off the ground, with few rests.
Variable or random practice is most effective during the autonomous stage. Variable practice requires that learners repeat the same patterns but make small changes as necessary (Figure 9-15). This type of practice increases the ability to adapt and generalize learning. In general, short frequent practice is better than longer, less frequent practice because it decreases fatigue and increases reinforcement.132 For example, a child is doing random practice when working on grasp and release as he or she engages in a variety of play activities during the intervention. This type of practice is most closely related to the actual occupation. The child must pick up and release toys as the play requires. The child must pick up a variety of objects: small blocks, large swings, light toys, and heavy scooter boards.

FIGURE 9-15 Variable practice. The child ties her shoes right before she goes outside to play. She is able to tie different sneakers and often she sits on the floor to complete the task.
Mental practice includes performing the skill in the imagination, without any action involved. It may consist of role playing, watching a video, or imagining. Mental practice is effective in teaching motor skills and re-training the timing and coordination of muscle group activity.26,28,30,46,88,96,116 Much of the research on mental practice is conducted on athletes trying to maximize their performance.81,88,103 However, the techniques used may be beneficial to children with motor difficulties. See Research Note 9-1 for a description of a study on mental practice in children. Taktek and colleagues found performance (in throwing a ball) obtained with mental imagery combined with physical practice was equal during the retention phase, but superior during the transfer of learning phase.116 The researchers examined visual and kinesthetic imagery in young children and found that they were both effective in children as young as 8 years. Imagery techniques are relatively simple and have been shown to work with children as young as 6 years of age. Many theorists suggest it is effective because it requires cognitive processes and helps children problem-solve motor solutions.30,46
Driskell and colleagues provide some specific feedback that may assist therapists using mental practice in clinical settings.30 They suggest that practitioners using mental practice consider the type of task, duration of mental practice, and time between practice and performance for retention. Tasks in which the child may have had some experience may be easier to imagine. However, the child may be able to imagine movements after observing them on a video or seeing someone else perform them. Therapists should be cautious not to incorporate a too-long mental practice because this may be difficult for children and result in a lack of motivation. Finally, therapists should incorporate actual performance shortly after the mental practice for the best retention. Techniques of watching a video, pointing out components of the movement, or simply reviewing mentally how the movement will look in combination with physical practice may provide improved motor learning.
Error-Based Learning
Children learn movement by making errors or mistakes and self-correcting.7,39,114 Therefore, clinicians must sometimes allow the challenge to exceed the capacity of the child so that he or she is given the opportunity to make errors, correct them (if possible), and learn from the experience. Children with disabilities must learn to adapt to new, different, or unexpected situations. In the past, therapists typically have been hesitant to allow children to learn through making errors. However, making errors in controlled settings allows children to resolve problems and is important for facilitating their motor skill learning. Encouraging children to explore, adjust movements, and evaluate their responses and reactions helps them learn and refine motor skills.
Feedback
Intrinsic feedback, which allows the child to self-correct, is most effective for sustaining motor performance and should be the goal of intervention sessions. Intrinsic feedback may be elicited through discovery, a situation in which the therapist sets up the environment and the child is allowed to explore and discover, make errors, and consequently learn new ways of moving.
Children may require extrinsic feedback in the early stages of motor skill development. Extrinsic feedback consists of providing verbal cueing or physical guidance. Demonstrative feedback refers to modeling or imitating movements. Demonstrative feedback is best if it is provided before the child actually practices the movement, as well as throughout early stages of skill acquisition. It should not be given with verbal commentary, because that decreases the child’s attention to the movement.24,114
Knowledge of Performance
Feedback to improve movement is most helpful when it is specific and clear. Knowledge of performance helps children understand how they performed the desired movement. Knowledge of performance is helpful in refining and adjusting motor skills and therefore is useful after the child has established basic skills. Therapists may provide descriptive feedback to the child about performance of a specific task such as writing, such as “you held the pencil between thumb and fingers and pressed lightly” or therapists may provide prescriptive feedback, such as “next time, press a little more.”
Knowledge of Results
Feedback related to the desired outcome helps children understand movement. Providing this knowledge is most effective when specific information on the movement’s goal is stated. Thus, “each button is lined up with its buttonhole” is preferred over “good job.” Knowledge of results is motivating and encourages children to continue; it is most helpful when learning new motor tasks.
Verbal Feedback
Verbal praise and reinforcement are useful in motivating clients and changing behaviors but may be overused in clinical settings. Allowing children to make their own assessments of their performance is beneficial and will increase their sense of efficacy.114 Verbal feedback is best if provided immediately after completion of the task. Using one to three brief cue words that can be repeated easily by the performer is best. Knowledge of correct performance motivates a child to continue practicing, so such reinforcement may be used frequently. Positive feedback with specific cues improves performance such as “you pressed firmly with the pencil!”
APPLICATION OF MOTOR CONTROL/LEARNING THEORY IN OCCUPATIONAL THERAPY PRACTICE
Case Study 9-8 illustrates how therapists may apply current motor control/motor learning principles to practice. Specifically, this example applies dynamical systems theory from an occupational therapy perspective to intervention of a child’s motor deficits.
SUMMARY
This chapter defined motor control and motor learning and presented case examples to illustrate how to apply current research to occupational therapy practice with children and youth. Also defined was dynamical systems theory, and the components of movement, including postural control, balance, visual perception, and body awareness were described. An overview of motor learning concepts of practice, feedback, modeling or demonstration, and mental practice was provided. A final case example illustrated the application of motor control/motor learning principles to occupational therapy practice.
REFERENCES
1. Accardo, P., Pensiero, S., Da Pozzo, S., Perissutti, P. Characteristics of horizontal smooth pursuit eye movements to sinusoidal stimulation in children of primary school age. Vision Research. 1995;35:539–548.
2. Allum, J., Honegger, F., Schicks, H. The influence of a bilateral vestibular deficit on postural synergies. Journal of Vestibular Research. 1994;4:49–70.
3. American Occupational Therapy Association. Occupational therapy practice framework: Domain & process. Bethesda, MD: AOTA, Inc, 2008.
4. Aslin, R., Ciuffreda, K. Eye movements in preschool children. Science. 1983;222:75–78.
5. Ayres, A.J. Sensory integration and learning disorders. Los Angeles: Western Psychological Services, 1972.
6. Bahrick, L. Intermodal origins of self-perception. In: Rochat P., ed. The self in infancy: Theory & research. Amsterdam: Elsevier; 1995:349–374.
7. Banks, R., Rodger, S., Polatajko, H. Mastering handwriting: How children with developmental coordination disorder succeed with CO-OP. OTJR: Occupation, Participation and Health. 2008;28(3):100–109.
8. Barnes, M., Crutchfield, C. Reflex and vestibular aspects of motor control, motor development and motor learning. Atlanta: Stokesville, 1990.
9. Bernstein, N. The coordination and regulation of movements. London: Pergamon, 1967.
10. Bertoldi, A.L.S., Ladewig, E., Israel, V.L. Influence of selectivity of attention on the development of body awareness in children with motor deficiencies. Revista Brasileira de Fisioterapia. 2007;11:319–324.
11. Bobath, B. Motor development, its effect on general development and application to the treatment of cerebral palsy. Physiotherapy. 1971;57:526–532.
12. Bouffard, M., Wall, A.E. A problem-solving approach to movement skill acquisition: Implications for special populations. In: Reid G., ed. Problems in movement control. Amsterdam: Elsevier Science; 1990:107–131.
13. Brenière, Y., Bril, B. Development of postural control of gravity forces in children during the first 5 years of walking. Experimental Brain Research. 1998;121:255–262.
14. Brownwell, C., Zerwas, S. So Big”: The development of body self awareness in toddlers. Child Development. 2007;78:1426–1440.
15. Bullock, M., Lutkenhaus, P. Who am I? Self-understanding in toddlers. Merrill Palmer Quarterly. 1990;36:217–238.
16. Burtner, P., Qualls, C., Woollacott, M. Muscle activation characteristics of stance balance control in children with spastic cerebral palsy. Gait & Posture. 1998;8:163–174.
17. Burtner, P., Woollacott, M., Qualls, C. Stance balance control with orthoses in a select group of children with and without spasticity. Developmental Medicine and Child Neurology. 1999;41:748–757.
18. Carson, R.G., Goodman, D., Kelso, J.A.S., Elliott, D. Phase transitions and critical fluctuations in rhythmic coordination of ipsilateral hand and foot. Journal of Motor Behavior. 1995;27:211–224.
19. Chen, Y., Yang, T. Effect of task goals on the reaching patterns of children with cerebral palsy. Journal of Motor Behavior. 2007;39:317–324.
20. Cherng, R.J., Hsu, Y.W., Chen, Y.J., Chen, J.Y. Standing balance of children with developmental coordination disorder under altered sensory conditions. Human Movement Science. 2007;26:913–926.
21. Clarke, J., Whitall, J. Perception-action coupling in children with developmental coordination disorder. Journal of Sport and Exercise Psychology. 2003;25:9.
22. Cohn, E., Miller, L.J., Tickle-Degnen, L. Parental hopes for therapy outcomes: Children with sensory modulation disorders. American Journal of Occupational Therapy. 2000;54:36–43.
23. Coleman, R., Piek, J., Livesey, D. A longitudinal study of motor ability and kinaesthetic acuity in young children at risk of developmental coordination disorder. Human Movement Science. 2001;20:95–110.
24. Correa, V., Poulson, C., Salzberg, C. Training and generalization of reach-grasp behavior in blind, retarded young children. Journal of Applied Behavior Analysis. 1984;17:57–69.
25. Davidson, T., Williams, B. Occupational therapy for children with developmental coordination disorder: A study of the effectiveness of a combined sensory integration and perceptual-motor intervention. British Journal of Occupational Therapy. 2000;63:495–499.
26. Deecke, L. Planning, preparation, execution, and imagery of volitional action. Cognitive Brain Research. 1996;3:59–64.
27. DeLoache, J., Uttal, D., Rosengren, K. Scale errors offer evidence for a perception-action dissociation early in life. Science. 2004;304:1027–1029.
28. Denis, M. Visual imagery and the use of mental practice in the development of motor skills. Canadian Journal of Applied Sport Sciences. 1985;10:4S–16S.
29. Diener, H., Dichgans, J., Guschlbauer, B., Bacher, M. Role of visual and static vestibular influences on dynamic posture control. Human Neurobiology. 1986;5:105–113.
30. Driskell, J.E., Cooper, C., Moran, A. Does imagery practice enhance performance? Journal of Applied Psychology. 1994;79:481–492.
31. Dutton, G., Saaed, A., Fahad, B., Fraser, R., McDaid, G., McDade, J., et al. Association of binocular lower visual field impairment, impaired simultaneous perception, disordered visually guided motion and inaccurate saccades in children with cerebral visual dysfunction—a retrospective observational study. Eye. 2004;18:27–34.
32. Emanuel, M., Jarus, T., Bart, O. Effect of focus of attention and age on motor acquisition, retention, and transfer: A randomized trial. Physical Therapy. 2008;88:251–260.
33. Fisher, A.G. Uniting practice and theory in an occupational framework. American Journal of Occupational Therapy. 1998;52:509–521.
34. Freedman, E.G., Sparks, D.L. Coordination of the eyes and head: Movement kinematics. Experimental Brain Research. 2000;131:22–32.
35. French, K.E., Thomas, J.R. The relation of knowledge development to children’s basketball performance. Journal of Sport Psychology. 1987;9:15–32.
36. Gardner, R., Sorter, R., Friedman, B. Developmental changes in children’s body images. Journal of Social Behavior and Personality. 1997;12:1019–1036.
37. Geuze, R.H. Static balance and developmental coordination disorder. Human Movement Science. 2003;22:527–548.
38. Geuze, R.H., Jongmans, M.J., Schoemaker, M.M., Smits-Engelsman, B.C. Clinical and research diagnostic criteria for developmental coordination disorder: A review and discussion. Human Movement Science. 2001;20:7–47.
39. Gilner, J.A. Purposeful activity in motor learning theory: An event approach to motor skill acquisition. American Journal of Occupational Therapy. 1985;39:28–34.
40. Goodgold-Edwards, S.A., Cermak, S.A. Integrating motor control and motor leaning concepts with neuropsychological perspectives on apraxia and developmental dyspraxia. American Journal of Occupational Therapy. 1990;44:431–439.
41. Gordon, A., Schneider, J., Chinnan, A., Charles, J. Efficacy of a hand-arm bimanual intensive therapy (HABIT) in children with hemiplegic cerebral palsy: A randomized control trial. Developmental Medicine and Child Neurology. 2007;49:830–839.
42. Grove, C.R., Lazarus, J.A. Impaired re-weighting of sensory feedback for maintenance of postural control in children with developmental coordination disorder. Human Movement Science. 2007;26:457–476.
43. Hadders-Algra, M., Brogren, E., Forssberg, H. Ontogeny of postural adjustments during sitting in infancy: Variation, selection, and modulation. Journal of Physiology. 1996;493:273–288.
44. Hadders-Algra, M., Brogren, E., Forssberg, H. Development of postural control-differences between ventral and dorsal muscles. Neuroscience and Biobehavioral Reviews. 1998;22:501–506.
45. Haishi, K., Kokubun, M. Developmental trends in pursuit eye movements among preschool children. Perceptual and Motor Skills. 1995;81:1131–1137.
46. Hall, C.R. Individual differences in mental practice and imagery of motor skill performance. Canadian Journal of Applied Science. 1985;10:17S–21S.
47. Hatzitaki, V., Zisi, V., Kollias, I., Kioumourtzoglou, E. Perceptual-motor contributions to static and dynamic balance control in children. Journal of Motor Behavior. 2002;34:161–170.
48. Hay, J., Missiuna, C. Motor proficiency in children reporting low levels of participation in physical activity. Canadian Journal of Occupational Therapy. 1998;65:64–71.
49. Hebert, E., Landin, D., Solmon, M. Practice schedule effects on the performance and learning of low and high skilled students: an applied study. Research Quarterly for Exercise and Sport. 1996;67:52–58.
50. Henderson, S., Sugden, D. Movement Assessment Battery for Children. Kent, England: Psychological Corporation, 1992.
51. Hirshfeld, H., Forssberg, H. Epigenetic development of postural responses for sitting during infancy. Experimental Brain Research. 1994;97:528–540.
52. Horak, F., Diener, H., Nashner, L. Postural strategies associated with somatosensory and vestibular loss. Experimental Brain Research. 1990;82:167–177.
53. Horak, F., Jones-Rycewicz, C., Black, F., Shumway-Cook, A. Effects of vestibular rehabilitation on dizziness and imbalance. Otolaryngology Head and Neck Surgery. 1992;106:175–180.
54. Hseih, C.L., Nelson, D.L., Smith, D.A., Petersen, C.Q. A comparison of performance in added-purpose occupations and rote exercise for dynamic standing balance in persons with hemiplegia. American Journal of Occupational Therapy. 1996;50:10–16.
55. Inder, J.M., Sullivan, S.M. Motor and postural response profiles of four children with developmental coordination disorder. Pediatric Physical Therapy. 2005;17:18–29.
56. Ingles, J., Horak, F., Shupert, C., Rycewicz, C. The importance of somatosensory information in triggering and scaling automatic postural responses in humans. Experimental Brain Research. 1994;101:159–164.
57. Jung-Potter, J.O., Kim, S.J., Metcalfe, J.S., Horn, C., Wilms-Floet, A., McMenamin, S., et al. Somatosensory-motor coupling in children with Developmental Coordination Disorder. Banff, Alberta: Paper presented at the Fifth Biennial Workshop on Children with DCD, 2002.
58. Kagerer, F., Bo, J., Contreras-Vidal, J. Visuomotor adaptation in children with developmental coordination disorder. Motor Control. 2004;8:450–560.
59. Kaufman, L.B., Schilling, D.L. Implementation of a strength training program for a 5 year-old child with poor body awareness and developmental coordination disorder. Physical Therapy. 2007;87:455–467.
60. Kielhofner, G. Conceptual foundations of occupational therapy, 3rd ed. Philadelphia: FA Davis, 2004.
61. Kielhofner, G. Model of human occupation: Theory and application, 4th ed. Philadelphia: FA Davis, 2008.
62. Klingberg, T., Forssberg, H., Westerberg, H. Increased brain activity in frontal and parietal cortex underlies the development of visuospatial working memory capacity during childhood. Journal of Cognitive Neuroscience. 2002;14:1–10.
63. Kowler, A., Martins, J. Eye movements in preschool children. Science. 1982;215:997–999.
64. Kramer, J.M. Using a participatory action approach to identify habits and routines to support self-advocacy. OTJR: Occupation, Participation and Health. 2007;27:84S–85S.
65. Langaas, T., Mon-Williams, M., Wann, J., Pascal, E., Thompson, C. Eye movements, prematurity and developmental coordination disorder. Vision Research. 1998;38:1817–1826.
66. Law, M., Russell, D., Pollock, N., Rosenbaum, P., Walter, S., King, G. A comparison of intensive neurodevelopmental therapy plus casting and a regular occupational therapy program for children with cerebral palsy. Developmental Medicine & Child Neurology. 1997;39:664–670.
67. Lewis, M., Brooks-Gunn, J. Social cognition and the acquisition of self. New York: Plenum, 1979.
68. Lewis, M., Ramsay, D. Development of self recognition, personal pronoun use, and pretend play during the 2nd year. Child Development. 2004;75:1821–1831.
69. Lowes, J., Tiggemann, M. Body dissatisfaction, dieting awareness and the impact of parental influence in young children. British Journal of Health Psychology. 2003;8:135–147.
70. Malouin, F., Richards, C. Preparatory adjustments during gait initiation in 4–6-year-old children. Gait & Posture. 2000;11:239–253.
71. Mandich, A.D., Polatajko, H.J., Macnab, J.J., Miller, L.T. Treatment of children with developmental coordination disorder: What is the evidence? Physical and Occupational Therapy in Pediatrics. 2001;20:51–58.
72. Martineau, J., Cochin, S. Visual perception in children: Human, animal and virtual movement activates different cortical areas. International Journal of Psychophysiology. 2007;51:37–44.
73. Mathiowetz, V., Bass-Haugen, J. Motor behavior research: Implications for therapeutic approaches to central nervous system dysfunction. American Journal of Occupational Therapy. 1994;48:733–745.
74. Miller, L., Nelson, D.L. Dual-purpose activity versus single-purpose activity in terms of duration on task, exertion level, and affect. Occupational Therapy in Mental Health. 1987;7:55–67.
75. Missiuna, C. Motor skill acquisition in children with developmental coordination disorder. Adapted Physical Activity Quarterly. 1994;11:214–235.
76. Missiuna, C., Mandich, A., Integrating motor learning theories into practice. Cermak S., Larkin D., eds. Developmental coordination disorder, 2002:221–233. [Delmar].
77. Missiuna, C., Rivard, L., Bartlett, D. Exploring assessment tools and the target of intervention for children with developmental coordination disorder. Physical and Occupational Therapy in Pediatrics. 2006;26:71–89.
78. Miyahara, M. A meta-analysis of intervention studies on children with developmental coordination disorder. Corpus, Psyche & Societas. 1996;3:11–18.
79. Miyahara, M., Wafer, A. Clinical intervention for children with developmental coordination disorder: A multiple case study. Adapted Physical Activity Quarterly. 2004;21:281–300.
80. Moore, C., Mealiea, J., Garon, N., Povinelli, D. The development of body self-awareness. Infancy. 2007;11:157–174.
81. Murphy, S.M. Imagery interventions in sport. Medicine and Science in Sports and Exercise. 1994;26:486–494.
82. Nararro, A., Fukujima, M., Fontes, S., Matas, S., Prado, G. Balance and motor coordination are not fully developed in 7 year old blind children. Auquivos de Neuro-Psiquiatria. 2004;62:654–657.
83. Nashner, L. Sensory, neuromuscular, and biomechanical contributions to humanbalance. In: Duncan P., ed. Balance proceedings of the APTA forum. Alexandria, VA: American Physical Therapy Association, 1990.
84. Nashner, L., Shumway-Cook, A., Marin, O. Stance posture control in select groups of children with cerebral palsy: Deficits in sensory organization and muscular coordination. Experimental Brain Research. 1983;49:393–409.
85. Nelson, D.L. Occupation: Form and performance. American Journal of Occupational Therapy. 1988;42:633–641.
86. O’Brien, J., Bergeron, A., Duprey, H., Olver, C., St. Onge, H. Children with disabilities and their parents’ views of occupational participation needs. Occupational Therapy in Health Care. 2009;25:1–17.
87. O’Brien, J., Williams, H., Bundy, A., Lyons, J., Mittal, A. Mechanisms that underlie coordination in children with developmental coordination disorder. Journal of Motor Behavior. 2008;40:43–61.
88. Page, S., Sime, W., Nordell, K. The effects of imagery on female college swimmers’ perceptions of anxiety. The Sport Psychologist. 1999;13:458–469.
89. Painter, M., Inman, K., Vincent, W. Contextual interference effects: I. the acquisition and retention of motor tasks by individuals with mild mental handicaps. Adapted Physical Activity Quarterly. 1994;11:383–395.
90. Patla, A. Understanding the roles of vision in the control of human locomotion. Gait & Posture. 1997;5:54–69.
91. Piek, J., Skinner, R. Timing and force control during a sequential tapping task in children with and without motor coordination problems. Journal of International Neuropsychological Society. 1999;5:320–329.
92. Polatajko, H.J., Kaplan, B.J., Wilson, B.N. Sensory integration treatment for children with learning disabilities: Its status 20 years later. Occupational Therapy Journal of Research. 1992;12:323–341.
93. Polatajko, H., Mandich, A., Miller, L., Macnab, J. Cognitive orientation to daily occupational performance (CO-OP): Part II—the evidence. Physical & Occupational Therapy in Pediatrics. 2001;20:83–106.
94. Polivy, J., Herman, C.P. Etiology of binge eating: Psychological mechanisms. In: Fairburn C.G., Wilson G.T., eds. Binge eating: Nature, assessment and treatment. New York: Guilford Press; 1993:50–76.
95. Przysucha, E.P., Taylor, M.J. Control of stance and developmental coordination disorder: The role of visual information. Adapted Physical Activity Quarterly. 2004;21:19–33.
96. Rathunde, K. Toward a psychology of optimal human functioning: What positive psychology can learn from the ‘experiential turns’ of James, Dewey, and Maslow. The Journal of Humanistic Psychology. 2001;41:135–153.
97. Raynor, A. Strength, power, and coactivation in children with developmental coordination disorder. Developmental Medicine and Child Neurology. 2001;43:676–684.
98. Rizzolatti, G., Fadiga, L., Gallese, V., Fogassi, L. Premotor cortex and the recognition of motor actions. Cognition and Brain. 1996;3:131–141.
99. Rochat, P. Early objectification of the self. In: Rochat P., ed. The self in infancy: Theory and research. Amsterdam: Elsevier; 1995:53–71.
100. Rochat, P. Self perception and action in infancy. Experimental Brain Research. 1998;123:102–109.
101. Rood, M. Neurophysiological mechanisms utilized in the treatment of neuromuscular dysfunction. American Journal of Occupational Therapy. 1956;10:220–224.
102. Ross, R., Radant, A., Hommer, D. A development study of smooth pursuit eye movements in normal children from 7 to 15 years of age. Journal of American Academy of Child and Adolescent. 1993;32:783–791.
103. Ryan, E.D., Simons, J. Efficacy of mental imagery in enhancing mental rehearsal of motor skills. Journal of Sports Psychology. 1982;4:41–51.
104. Schoemaker, M.M., Niemeijer, A.S., Reynders, K., Smits-Engelsman, B.C. Effectiveness of neuromotor task training for children with developmental coordination disorder: A pilot study. Neural Plasticity. 2003;10:153–163.
105. Schoemaker, M.M., van der Wees, M., Flapper, B., Verheij-Jansen, N., Scholten-Jaegers, S., Geuze, R.H. Perceptual skills of children with developmental coordination disorder. Human Movement Science. 2001;20:111–133.
106. Shaefer, S., Krampe, R., Lindenberger, U., Baites, P. Age differences between children and young adults in the dynamics of dual-task prioritization: Body (balance) versus mind (mind). Developmental Psychology. 2008;44:747–757.
107. Shumway-Cook, A., Woollacott, M. Motor control: Theory and practical applications, 2nd ed. Philadelphia: Lippincott Williams & Wilkins, 2001.
108. Shumway-Cook, A., Woollacott, M. Motor control: Theory and practical applications, 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2007.
109. Steenbergen, B., Gordon, A.M. Activity limitation in hemiplegic cerebral palsy: Evidence for disorders in motor planning. Developmental Medicine and Child Neurology. 2006;48:780–783.
110. Steinbeck, T. Purposeful activity and performance. American Journal of Occupational Therapy. 1986;40:529–534.
111. Steultjens, E.M.J., Dekker, J., Bouter, L.M., Leemrijse, C.J., van den Ende, C.H.M. Evidence of the efficacy of occupation therapy in different conditions: An overview of systematic reviews. Clinical Rehabilitation. 2005;19:247–254.
112. Sugden, D., Dunford, C. Intervention and the role of theory, empiricism and experience in children with motor impairment. Disability & Rehabilitation. 2007;29:3–11.
113. Sugden, D., Utley, A. Interlimb coupling in children with hemiplegic cerebral palsy. Developmental Medicine and Child Neurology. 1995;37:293–309.
114. Sullivan, K., Kantuk, S., Burtner, P. Motor learning in children: Feedback effects on skill acquisition. Physical Therapy. 2008;88:720–732.
115. Sundermier, L., Woollacott, M., Jensen, J., Moore, S. Postural sensitivity to visual flow in aging adults with and without balance problems. Journal of Gerontology. 1996;51:M45–M52.
116. Taktek, K., Zinsser, N., St.-John, B. Visual versus kinesthetic mental imagery: Efficacy for the retention and transfer of a closed motor skill in young children. Canadian Journal of Experimental Psychology. 2008;62:174–187.
117. Thelen, E., Kelso, J., Kelso, J.S., Fogel, A. Self-organizing systems and infant motor development. Developmental Review. 1987;7:39–65.
118. Truby, H., Paxton, S. Development of the children’s body image scale. British Journal of Clinical Psychology. 2002;41:185–204.
129. Trombly, C.A. Occupation: Purposefulness and meaningfulness as therapeutic mechanisms. 1995 Eleanor Clarke Slagle Lecture. American Journal of Occupational Therapy. 1995;49:960–972.
120. Tsai, C.L., Wu, S.K., Huan, C.H. Static balance in children with developmental coordination disorder. Journal of Human Movement. 2008;27:142–153.
121. Utley, A., Sugden, D. Interlimb coupling in children with hemiplegic cerebral palsy during reaching and grasping at speed. Developmental Medicine and Child Neurology. 1998;40:396–404.
122. Vaillant, J., Vuillerme, N., Janvery, A., Louis, F., Braujou, R., Juvin, R., et al. Effect of manipulation of the feet and ankles on postural control in elderly adults. Brain Research Bulletin. 2008;75:18–22.
123. Vandenbussche, E. Deficits of visual perception in children with cerebral visual impairment due to early brain damage. Perception. 2000;29:6.
124. Van der Weel, F.R., Van der Meer, A.L., Lee, D.N. Effect of task on movement control in cerebral palsy: Implications for assessment and therapy. Developmental Medicine & Child Neurology. 1991;33:419–426.
125. Van Waelvelde, H., De Weerdt, W., De Cock, P., Janssens, L., Feys, H., Smits Engelsman, B.C.M. Parameterization of movement execution in children with developmental coordination disorder. Brain and Cognition. 2006;60:20–31.
126. Visser, T., Boden, C., Giaschi, D. Children with dyslexia: Evidence for visual attention deficits in perception of rapid sequences of objects. Vision Research. 2004;44:2521–2535.
127. von Hofsten, C., Rosander, K. The development of gaze control and predictive tracking in young infants. Vision Research. 1996;36:81–96.
128. Wann, J.P., Mon-Williams, M., Rushton, K. Postural control and co-ordination disorders: The swinging room revisited. Human Movement Science. 1998;17:491–513.
129. Williams, H. Perceptual and motor development. Englewood Cliffs, NJ: Prentice-Hall, 1983.
130. Williams, H., Motor control in children with developmental coordination disorder. Cermak S.A., Larkin D., eds. Developmental coordination disorder, 2002:117–137. [Delmar].
131. Williams, H. A working model of visual perception: A manual for developing visual perception behaviors in children. Columbia, SC: University of South Carolina Press, 2005.
132. Williams, H. Motor control. In: Solomon J., O’Brien J., eds. Pediatric skills for occupational therapy assistants. 2nd ed. St. Louis: Mosby; 2006:461–480.
133. Williams, H. Balance control: A smart text. Columbia, SC: University of South Carolina Press, 2007.
134. Williams, H. Perceptual-motor development evaluation protocols: Process characteristics of balance. Columbia, SC: University of South Carolina Press, 2007.
135. Williams, H., Fisher, J., Tritschler, K. Descriptive analysis of static postural control in 4, 6, and 8 year old normal and motorically awkward children. American Journal of Physical Medicine. 1983;62:12–26.
136. Williams, H., Ho, L. Balance and postural control across the lifespan. In: Dewey D., Tupper D., eds. Developmental motor disorders: A neurological perspective. New York: Guilford Press; 2004:211–236.
137. Wilmut, K., Wann, J.P., Brown, J.H. Problems in the coupling of eye and hand in the sequential movements of children with Developmental Coordination Disorder. Child Care, Health & Development. 2006;32:665–678.
138. Woollacott, M., Burtner, P., Jensen, J., Jasiewicz, J., Roncesvalles, N., Sveistrup, H. Development of postural responses during standing in healthy children and in children with spastic diplegia. Neuroscience Biobehavioral Review. 1998;22:583–589.
139. Woollacott, M., Shumway-Cooke, A. Changes in posture control across the life span: A systems approach. Physical Therapy. 1990;70:799–807.
140. Woollacott, M., Sveistrup, H. Changes in the sequencing and timing of muscle response coordination associated with developmental transitions in balance abilities. Human Movement Science. 1992;11:23–36.
141. Yoder, R., Nelson, D., Smith, D. Added purpose versus rote exercise in female nursing home residents. American Journal of Occupational Therapy. 1989;43:581–586.
142. Zanone, P.G., Kelso, J.A.S., The coordination dynamics of learning: Theoretical structure and experimental agenda. Swinnen S.P., Heuer H., Massion J., Casaer P., eds. Interlimb coordination: Neural, dynamical, and cognitive constraints. Academic Press: San Diego, CA, 1994:461–490.
143. Zoia, S., Castiello, U., Blason, L., Scabar, A. Reaching in children with and without developmental coordination disorder under normal and perturbed vision. Developmental Neuropsychology. 2005;27:257–273.

 CASE STUDY 9-1
CASE STUDY 9-1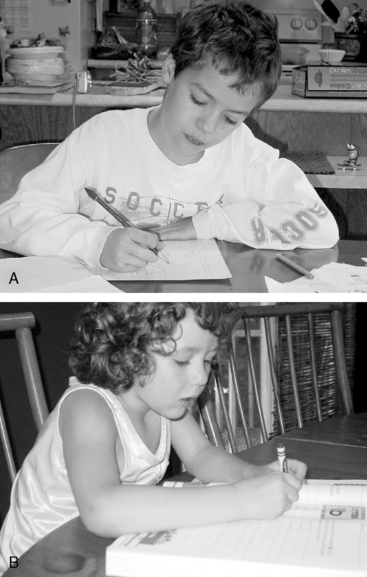

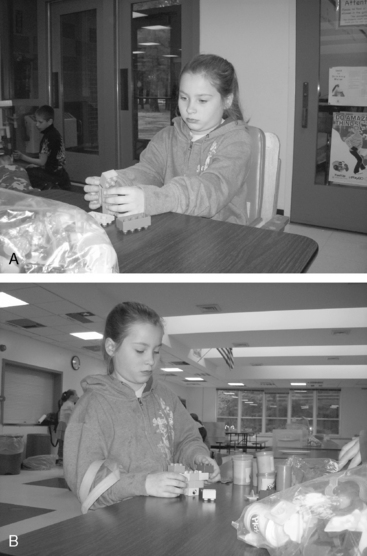


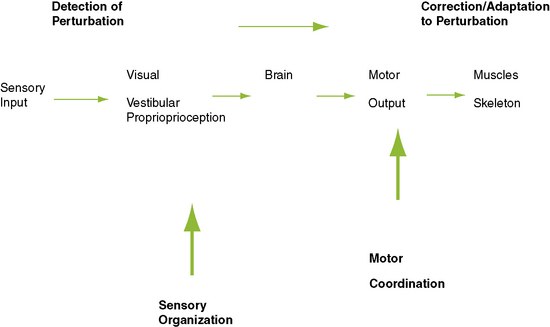
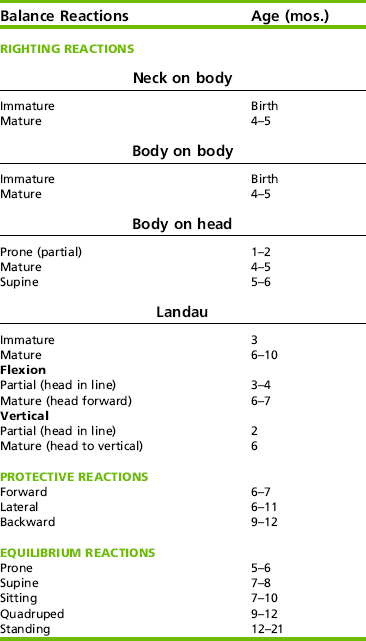


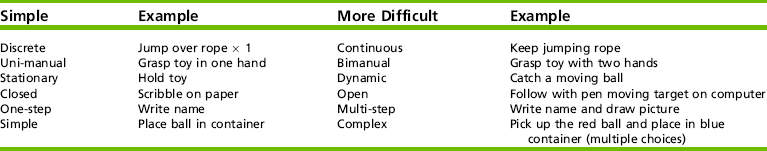
 RESEARCH NOTE 9-1
RESEARCH NOTE 9-1