Enhancement of Grasp Skills
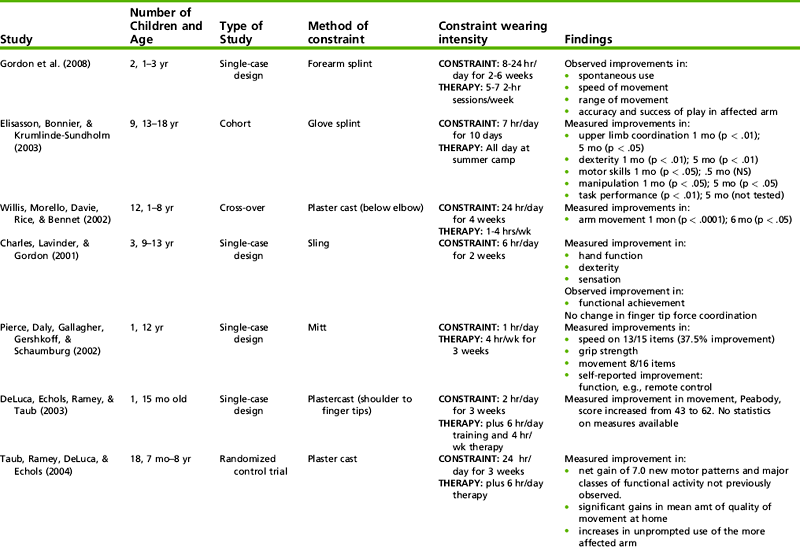
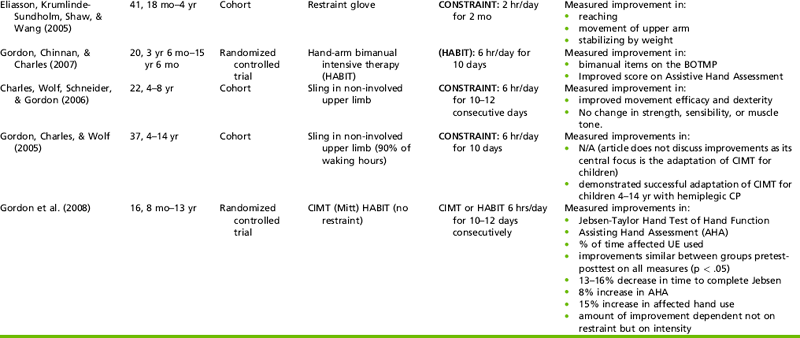
Problems: The following are problems in the development of effective grasp, some of which are illustrated in Figure 10-18:

FIGURE 10-18 When this child combines reach with grasp, he demonstrates significant difficulties with effective hand positioning. Note the slight wrist flexion, the thumb adduction with IP joint extension, and the finger MCP joint hyperextension with IP flexion that he uses in an attempt to achieve stability with this grasp. The arm positioning in abduction and internal rotation (not shown) contribute to use of this grasp pattern.
• Fisting or finger flexion that prevents hand opening
• Wrist flexion (often with ulnar deviation) in combination with finger extension
• Excessive forearm pronation, which interferes with the use of radial finger grasp patterns
• Thumb adduction in grasps that should use opposition, often with MCP or IP flexion
• Inability to use thumb abduction and adduction with MCP and IP extension
• Inability to initiate or sustain thumb opposition
• Inability to use grasp patterns that involve control of the intrinsic finger muscles
• Inability to vary grasp in accordance with object characteristics and activity demands
Goals: Presented next are examples of goals that can be used for children with a variety of levels of disability. The goals are in approximate order of difficulty, although difficulty using any one pattern can vary with the individual child. Some children may develop grasp only up to one of the lower levels identified here, whereas others may be able to attain the higher level skills. To illustrate how the goals associated with grasp may be integrated with occupations of the child or adolescent, sample occupations (in parentheses) are identified for each grasp. The goals are that the child will:
1. (Put on clothing, pick up a towel, play a game with large game pieces) using a sustained grasp with the arm in a variety of positions.
2. (Hold hard finger foods, pick up clothing, play with a car set) using a finger surface grasp on a variety of objects.
3. (Eat finger foods, use manipulative objects in math activities, play a game with small pieces, do a puzzle) using a finger pad grasp with thumb opposition on small objects.
4. (Prepare a meal, perform dressing tasks, perform hygiene tasks) using an opposed thumb and fingertip grasp pattern in accordance with object shapes and characteristics.
5. (Use a key to open a door, build with construction toys) using an effective lateral pinch grasp pattern.
6. (Handle computer materials such as paper and disks and file papers in folders; eat a cracker or sandwich) using finger pads to hold thin, flat objects.
7. (Brush the teeth, use a knife, comb the hair, and use a safety razor) using a power grasp.
Intervention Strategies: For children with delays and functional difficulties in grasp, the therapist needs to match preparation techniques, such as positioning, handling, or strengthening, to the child’s problem. Some children fist their hands or refuse to grasp objects because of tactile hypersensitivity, which also can influence the ability to maintain grasp. If this problem is present, grading tactile input from well tolerated to more difficult to tolerate is helpful. Initially, the child best tolerates firm objects with smooth surfaces and contours.
Tactile discrimination problems can contribute to grasp problems. Poor discrimination can affect dynamic use of grasp patterns and regulation of pressure in grasp. Problems with regulating pressure are seen as the child either holding objects with excessive force or dropping objects. Most children benefit from graded sensory input and attention to sensory discrimination as part of the intervention for grasp skills. Having the child actively explore the sizes, shapes, and textures of objects can precede emphasis on grasp in a treatment session.
In planning intervention that addresses grasp problems, the therapist, when selecting objects, should keep in mind the child’s interests, sensory needs, and motor skills. Properties to consider include the size, shape, color, weight, and texture of objects.
Children with Severe Disabilities: Children with severe disabilities need to develop an effective palmar grasp and, if possible, grasp patterns using the finger surface. If possible, the therapist should stress the abilities to initiate grasp and sustain grasp with the arm in a variety of positions. If the child is unable to open the hand readily for grasp, the therapist may explore whether changing the child’s body position would be helpful. The side-lying position may reduce stress on overall body posture and may make it possible for the child to open the hand more easily. In supported sitting, the child may find opening the hand easier if the therapist places an object below the seat of the chair and lateral to the child’s body. Boehme described other handling techniques that may assist the child with hand opening.12 The therapist should follow these techniques with movement of the open hand across objects and surfaces as a way of increasing the child’s sustained hand opening and object interaction.
For the child who can independently open the hand but who shows wrist flexion with grasp, the therapist can emphasize wrist extension with grasp by positioning objects above the table surface or at chest height. Once the child can sustain wrist extension, the therapist can assist or encourage him or her to move the arm while maintaining grasp of an object. Sample activities using this skill include using a small stick to hit a suspended balloon or to break soap bubbles blown by the therapist, touching pictures on a wall or mirror with a stick, or holding onto clothing items while they are pulled up or down.
The child with a severe disability can wear a splint or other orthotic device during treatment and at other times of the day. Splinting techniques that may be useful in supporting hand function during treatment are described later in this chapter. Burtner et al. found that dynamic splints had a significant positive effect on grip over a static splint or no splint in a study that compared children with spastic cerebral palsy and typical children.15 Of note was a finding of compensatory movements at the shoulder when these children wore a static splint during grasp activities.15
In addition to the above strategies, many children need adaptations of materials to support their performance of activities at home, school, and play. Use of standard materials may not be possible. Built-up handles that accommodate a palmar grasp pattern and larger objects, such as game pieces and blocks, may be used instead of smaller ones. Adapted page turners for books, switches for toys, and computer adaptations may be necessary to give the child some independence in play and school activities.
Children with Moderate Disabilities: Children with moderate disabilities are able to grasp but have difficulty with functional use of a variety of grasp patterns. They have problems in forearm control, wrist extension, thumb opposition, and control of the MCP and IP joints (see Figure 10-18). Grasp may be initiated with wrist flexion. Grasp goals for these children usually are designed to address the use of opposed grasp patterns and grasp patterns in which the hand effectively accommodates to objects.
The occupational therapist selects specific object shapes, sizes, and textures to develop opposed grasp patterns. The therapist selects activities that are age appropriate, interesting, and meaningful to the child and have elements the child can repeat. Games and imaginary play materials can provide opportunities for repetitive presentation of objects to the child. The child can use opposed grasps with medium-sized, small, and tiny objects. Children often can demonstrate better thumb and finger control with small or medium-sized objects that have well-defined edges. Tiny objects require too much precision, such that the child often resorts to a more primitive grasping pattern. In fact, skill in using a pincer grasp usually is less critical for the child’s functional performance of daily life tasks than skill in using and varying a three-finger opposed grasp pattern. Once the child begins to acquire an opposed grasp pattern, the therapist can vary the objects by size, shape, texture, and weight.
The research findings of Case-Smith et al. support the clinical observation that object characteristics are important in eliciting specific grasp patterns, particularly when these patterns are emerging.25 To help the child develop an opposed grasp pattern, the therapist can begin working on grasp alone rather than reach and grasp. The child’s arm should be well stabilized when objects are presented. Having the wrist in a neutral or slightly extended position is critical; if appropriate, the therapist can stabilize the volar surface of the child’s forearm on the table surface and give support over the dorsum of the forearm. The therapist should present objects in line with the shoulder and not at midline, because midline positioning has a tendency to encourage the use of pronation. With objects presented in line with the shoulder, neutral rotation of the humerus is encouraged (versus internal rotation) and slight forearm supination is likely to occur. The therapist holds the object with the fingers and presents the object directly to the child’s fingers (Figure 10-19, A). After grasp, the child carries the object to a nearby container or surface. Practice of this strategy for grasp, carry, and release using a variety of objects is needed for the child to integrate this skill.


FIGURE 10-19 A, The child shows the ability to use a controlled radial-digital grasp pattern with the wrist in a neutral position, thumb opposition, and appropriate finger flexion when he is not asked to combine reach with grasp. Note that the therapist’s presentation of the object helps ensure that the child will grasp the object with his fingertips. Her grasp also ensures that the object remains stable while the child initiates the grasp pattern. B, The child practices grasping from the therapist’s hand. His arm is stabilized on his leg during this grasp. The therapist’s hand provides some degree of stability to prevent the object from moving during initiation of grasp.
Once the child is able to use this pattern well, the therapist can move to the next skill level. At this level the therapist places the object in his or her cupped hand (just under the child’s hand and in line with the child’s shoulder), so that the object is stable, and asks the child to grasp the object (Figure 10-19, B). When the therapist uses this strategy, the child needs to use more internal stability of the arm and some degree of prepositioning of the fingers before grasp.
As the child develops skill in grasping from the therapist’s hand, the therapist can begin to place an object on the table surface. As at the prior two levels, the object is in line with the child’s shoulder, not at midline. The therapist may need to stabilize the object or place it on a nonskid surface for the child who does not have sufficient arm stability to grasp without unintentionally moving the object.
After the child is able to grasp from the table surface with the object in line with the shoulder, the therapist can begin to move the object further away on the table surface, above the table surface, and closer to midline. In this way the therapist is structuring activities to combine reach with grasp. This requires the child to stabilize the arm in space while controlling finger movements. The therapist may use a variety of these object placements in a therapy session to elicit the child’s best skills. Different object placements may be needed with various sizes and shapes of objects.
Using principles of motor learning theory, the therapist systematically varies object placement and the size and weight of objects during intervention activities. Varying the input enables the child to develop more adaptable, flexible skills that can be generalized to a variety of situations. Duff and Gordon noted that 7- to 14-year-old children with hemiplegic cerebral palsy were able to demonstrate anticipatory control (i.e., the ability to adjust the force needed to lift an object) with novel objects, given the ability to practice these grasp-lift patterns.37 Their findings suggest that these children can develop an awareness of the object properties and the adjustment in force needed by practicing grasping and lifting objects of similar size but different weights. In addition, this ability can be achieved through practice of several grasp-lift repetitions with objects that have the same weight followed by repetitions with objects that have a different weight, or the weights of the objects can be varied randomly in a practice session.37 The therapist can assess the type of repetition that seems to have the most positive effect for a particular child. Further study is needed to determine children’s retention of these skills over time. Gordon, Charles, and Steenbergen also found that children with cerebral palsy improved in their adjustment of the force necessary to lift an object via experiences with the opposite hand.60 They were able to anticipate the force after using either the involved hand or the noninvolved hand. Thus, therapists should consider presenting objects for grasp to both hands, even if one is more impaired—and thus receiving more focus in therapy.
Children with Mild Disabilities: Children with mild disabilities typically have difficulty with small ranges of movement in supination and wrist extension. Sustained control with the intrinsic muscles of the hand may be difficult for these children to achieve. Fingertip control in grasp often is poor, as is the ability to control the palmar arches and to achieve radial-ulnar dissociation of movements within the hand. Some children substitute use of the middle finger for the index finger in attempting a pincer grasp (Figure 10-20); typical children may use this pattern occasionally, but children with tone problems (high or low) tend to use it frequently because of instability with the index finger and/or difficulty controlling the thumb in true opposition. Thus the thumb aligns more directly with the middle finger. This pattern can be functional for activities with tiny objects, but if the index finger cannot be used effectively with the middle finger, stable three-jaw chuck grasp patterns are not available for the child.

FIGURE 10-20 The child uses a substitution for a standard pincer grasp or tip pinch. Note that with slight adduction of the thumb, the pad of the thumb is more aligned with the middle finger than the index finger. The index finger is slightly too flexed to participate in the grasp.
Goals for grasp skills for these children usually focus on the use of a variety of grasp patterns, with accommodation of the grasp pattern to the object characteristics. These patterns include use of an effective pincer grasp and lateral pinch grasp pattern; use of a grasp with MCP flexion and IP extension to hold thin, flat objects; and/or use of a power grasp on a variety of tools in daily living tasks. The standard and lateral pinch patterns and the grasp for thin, flat objects require wrist stability and use of the intrinsic muscles.
The therapist can use a variety of treatment strategies with children who are working on these skills, including verbal cueing and structuring of activities to elicit intrinsic muscle activity. Sample activities include holding all fingers in adduction and extension while rolling out clay, using finger abduction to stretch rubber bands placed around two or more fingers, playing finger games that require isolation and small ranges of finger movements, holding or hiding objects in a cupped hand, and squeezing clay or other objects between the pad of the thumb and the pads of one or more fingers.
Development of a power grasp relies on the development of radial-ulnar dissociation and the ability to extend the index finger and thumb during ulnar finger flexion. Emphasis on radial-ulnar dissociation in the hand and on grasp with MCP flexion and IP extension is helpful as a precursor to the power grasp pattern. To address radial-ulnar dissociation, the therapist structures activities in which the child holds two objects in one hand and releases one at a time; holds an object in the ulnar side of the hand with the ring and little fingers while grasping and releasing with the radial fingers and thumb; and engages in activities that develop finger-to-palm translation with stabilization skills. In addressing the power grasp in functional activities, the therapist carefully selects the type of tool the child handles. Tools that have a narrow surface for index finger contact are particularly difficult for children to control. The therapist can use verbal cues, stickers, or dots on the handles of the tools to encourage appropriate finger placement. The child may need built-up handles to facilitate performance initially.
Enhancement of Voluntary Release Skills
Problems: Therapists usually combine treatment for voluntary release problems with intervention for grasp. Children who have difficulty releasing objects may exhibit the following:
• Fisting and tight finger flexion
• Difficulty with sustained arm position during object placement and release
• Difficulty combining wrist extension with finger extension
• Inability to use slight forearm supination to allow for release in small areas or near other objects and with visual monitoring of the placement
• Overextension of the fingers in release, limiting control of specific object placement
In their study of 7- to 13-year-old children with hemiplegic cerebral palsy, Eliasson and Gordon reported specific difficulties with both the placement phase and the release phase of object voluntary release.43 The children’s replacement “is abrupt,” they said, “and their force coordination is impaired, resulting in a prolonged and uncoordinated release of the grasp” (p. 232).43
Goals: Presented next are examples of goals the therapist can use for children with a variety of levels of disability. These goals specifically define the size of an area in which the child can release the object (e.g., into a container with a 4-inch opening) or the height of a surface on which the child can release the object (e.g., a stack of six cubes). The following goals incorporate these commonly used measures of voluntary release skill. The goals are in approximate order of difficulty, although difficulty using any one pattern can vary with the individual child. The therapist should integrate these goals with the child’s functional goals. The goals are that the child will:
1. Release objects into a container placed on the floor (e.g., pick up toys to put away [hard objects may be easier to use than soft objects]).
2. Release objects into a container placed on a table surface with the container at arm’s length from the child’s body to encourage wrist extension with finger extension (e.g., put objects into and take them out of a container).
3. Release objects into a container at the midline while using wrist extension (e.g., put pens and pencils into a basket after a group activity).
4. Release tiny objects into a container with a small opening (e.g., put nails or screws into a container after a project or put beads into a container for a beaded art project).
5. Place objects within 1 inch of other objects without making other objects move or fall (e.g., place game board pieces during a game, set the table with utensils).
6. Release unstable, lightweight objects while keeping them in an upright position (e.g., place objects on a desk at school and paper cups on the lunch table).
7. Release objects without visual monitoring (e.g., put a toothbrush into a container, pencils into a container, paper on a desk).
Intervention Strategies: Intervention focuses on one or more of the following areas, depending on the child’s problems: hand opening for object release, arm placement and stability for release, and accuracy of object placement. Releasing patterns correlate with grasping patterns. A child who uses a palmar grasp will use full finger extension to release the object. A child who uses a pincer grasp can use voluntary release with good control of the intrinsic muscles as balanced with the extrinsic muscles.
When the child shows excessive finger flexion (fisting), initial treatment for voluntary hand opening focuses on the child’s ability to move the arm while maintaining some finger extension. Splinting may be helpful in supporting the child’s wrist or facilitating increased wrist and finger extension. In children with fisting, asking the child to place the object into a container increases the child’s fisting. Some children have success releasing to the side of their body because movement away from the midline decreases the pronation-flexion posturing, thus increasing the hand fisting.
If the child can accomplish this level of voluntary release, he or she can attempt release of large and medium-sized objects into a container with a large opening that is placed on the floor. For some children, transfer of objects from hand to hand is a reasonable strategy for encouraging release with object stabilization.
Children who can voluntarily open their hands but who use tenodesis patterns may benefit from intervention to increase voluntary finger extension while maintaining the wrist in a neutral position. For some children, structured activities and handling are effective; other children benefit from wearing a dorsal wrist splint. A therapist can have the child wear a splint during part of the therapy session and encourage finger extension through a variety of activities, including voluntary release. The child can practice similar activities after splint removal.
Children who use wrist flexion with voluntary release may benefit from structured activities in which a container for objects is placed slightly lateral to the child’s midline and at a sufficient distance from the child’s body that the child needs to extend the elbow (Figure 10-21). This level of control is similar to that of an infant who releases objects with the arm held in a total extension pattern. Over time, the therapist can move the target containers closer to the child’s body, requiring gradually increasing elbow flexion with wrist extension for release of objects. Sometimes the therapist can facilitate this pattern if he or she sets the containers at an angle. Once the child can release medium-sized objects into a container at the midline while maintaining wrist extension to at least a neutral position, the therapist can reduce the size of the container opening.

FIGURE 10-21 Positioning materials to elicit elbow extension during release encourages the child’s use of wrist extension. (Courtesy Kanji Takeno, Towson University.)
Children with overextension of the fingers during voluntary release may benefit from activities described previously that address the development of intrinsic muscle control. They also may need intervention to improve somatosensory awareness of their hands. Activities for these children often incorporate the use of lightweight materials and objects that vary in size and stability. Verbal cueing of the child to attend to object and hand placement and graded activities to facilitate increasing accuracy and visual monitoring of materials are often helpful. Also, Gordon et al. observed that tasks that required increased accuracy (including object placement on a relatively unstable surface) could be used to encourage children with hemiplegia to slow their movements.65 Instruction was helpful to the children in encouraging faster movements.63 On the basis of findings from their studies, these researchers suggested that different speeds be used during voluntary release activities and that “practicing release tasks with the noninvolved hand first or practicing with bimanual tasks may enhance performance and should be studied” (p. 247).63 In addition, the work of Eliasson and Gordon suggests that repetition of object release in which the object’s weight remains constant over a number of trials allows children with hemiplegic cerebral palsy to learn to adjust the release of grasp.43 These findings provide support for the use of activities for voluntary release in which repetition and timing can be adjusted. Games of various types are often very effective for this purpose and are selected for the child’s cognitive level as well as the motor level.
Enhancement of In-Hand Manipulation Skills
Problems: Children who have difficulty with in-hand manipulation skills drop objects, use surfaces for support during manipulation, or are slow in the execution of skills.45 Case-Smith found empirical support for these problems in her study of children with and without fine motor delays.20 These problems are associated with tactile problems.19 Praxis and motor control problems, particularly of the intrinsic muscles, also may be a major cause of limited in-hand manipulation skill development. Attentional and cognitive problems contribute to these problems in some children. Problems that limit in-hand manipulation include the following:
Goals: Presented next are examples of goals the therapist can use for children with a variety of levels of in-hand manipulation skill. The goals are in approximate order of difficulty, although difficulty using any one pattern can vary with the individual child. The activities, including additional examples in parentheses, require specific in-hand manipulation skills. The goals are that the child will:
1. Move coins (move finger foods) into the palm of the hand by demonstrating finger-to-palm translation.
2. Move several coins (move pieces of finger foods) into the palm of one hand by using finger-to-palm translation with stabilization skills.
3. Adjust coins for placement into a bank (adjust playing cards for a game) using shift skills.
4. Adjust eating utensils (adjust a toothbrush while cleaning the teeth) using simple rotation skills.
5. Eat small finger foods (setup/clean up a game board) using palm-to-finger translation (and palm-to-finger translation with stabilization).
6. Play with a building set (put caps onto markers) using simple rotation with stabilization skills.
7. Erase with a pencil (handle containers or lids) using complex rotation skills.
Intervention Strategies: The therapist’s assessment of the causes of the child’s problems and the therapist’s determination of the child’s potential for acquiring specific in-hand manipulation skills influence intervention goals and strategies. Many children with moderate and severe disabilities who lack the necessary prerequisite skills cannot develop in-hand manipulation skills. Children with mild disabilities usually can develop at least lower level in-hand manipulation skills.
Specific activity suggestions are given in Box 10-4. Suggestions for strategies therapists can use with children with different levels of skills are discussed next. Exner provides additional information on treatment of in-hand manipulation skills.48
Children with No In-Hand Manipulation Skills: The therapist may encourage the child with no in-hand manipulation skills or only finger-to-palm translation to manipulate objects between the two hands and use support surfaces to assist in object manipulation. Use of these strategies can help the child begin to move the fingers actively over object surfaces. The therapist can use objects such as cubes that have pictures on all sides, kaleidoscopes, and textured toys. When the child can effectively move the fingers over objects, the therapist can introduce finger-to-palm translation activities in the context of “hiding the object” games using various objects. Finger isolation games can be useful, and the therapist should incorporate the thumb into these activities. The child should be assisted in developing and functionally using a variety of grasp patterns, including those that combine flexion at the MCP joints with extension at the IP joints. The therapist can use tactile discrimination and proprioception activities to enhance awareness of fingers and areas of the palm of the hand.
Children with Beginning In-Hand Manipulation Skills: Children who can use finger-to-palm translation and beginning simple rotation, or shift, or palm-to-finger translation skills can work on refining these skills, expanding their repertoire of skills used without stabilization, and beginning their ability to stabilize objects in the ulnar side of the hand while manipulating with the radial fingers.
Object selection for in-hand manipulation skills with these children is important. Objects that do not roll and that are small (not tiny) are often the easiest for the child to handle. Examples are dice-sized cubes, nickels, game pieces, and other small toys. With larger objects, the child must involve all fingers in the manipulation and must use more hand expansion; therefore, these objects are more difficult for the child to handle. With tiny objects, the child must have excellent tactile discrimination and fingertip control, which also makes these objects more difficult to handle than small objects.
The therapist structures the presentation of objects to assist the child in using a particular in-hand manipulation skill and often cues the child in the use of the skill. In a study of preschool children without disabilities who had emerging in-hand manipulation skills, Exner found that use of verbal cues or demonstration of skills had a positive effect on the children’s scores (as a group).46 However, children with lower scores showed more improvement with cues than children with higher scores. These findings suggest that verbal cueing may be an important component of intervention for in-hand manipulation skills. The Cognitive Orientation to Occupational Performance (CO-OP) approach encourages the therapist to provide verbal cues and the child to select his or her own goals and strategies and to talk his or her way through an activity as a method of increasing coordination and motor planning.
In addressing palm-to-finger translation, the therapist first places the object on the middle phalanx of the child’s index finger. When the child is able to move the object from this position out to the pads of the fingers, the therapist places the object on the volar surface of the proximal phalanx of the index finger. Later the therapist places the object in the palm of the child’s hand to promote thumb isolation and control to move the object.
The therapist can structure simple rotation skills by placing the object in the child’s hand (in a radial grasp pattern) and asking the child to turn it upright (Figure 10-22). Pegs and peglike objects (e.g., candles and objects that look like little people) can be helpful in developing these skills.
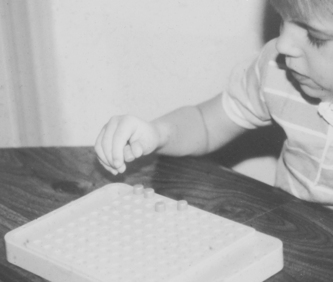
FIGURE 10-22 The peg has been placed in the child’s hand upside down to encourage rotation prior to placement in the game board.
Finger-to-palm translation with stabilization is the one skill with stabilization that is likely to be feasible for these children. This child often can facilitate this skill during finger-feeding activities and in play with coins. The therapist first encourages the child to hold one object in the hand while picking up and hiding another. After the child can manage two objects, the therapist can progress to using three or more objects.
Children with Basic In-Hand Manipulation Skills: For children with basic in-hand manipulation skills, the therapist emphasizes the development of complex rotation skills (Figure 10-23) and the use of stabilization with the other skills. The therapist introduces small and medium-sized objects and emphasizes use of the skills in a variety of functional activities, including dressing, hygiene, and school tasks. The child practices combinations of skills, such as finger-to-palm translation, palm-to-finger translation, and simple rotation. The therapist also can stress speed of skill use by timing skills and reporting the speed to the child. Children who are working at this level of skill typically respond well to verbal cueing for strategies to use in performing skills and to feedback about the effectiveness and speed of their skills. Eliasson, Bonnier, and Krumlinde-Sundholm studied the impact of practice of shift skills with a pen by adolescents who have cerebral palsy.41 Eight of the nine adolescents showed improvements in use of this skill after a 2-week period of daily practice and retention of the skill 5 months later by five of the adolescents. Three adolescents had some loss of skill at the 5-month time period; however, none returned to their original performance level. The only adolescent to show no change with intervention had a 0 score (of 8) on the initial assessment, but three other children with initial performance at this level did show improvement in in-hand manipulation skills.

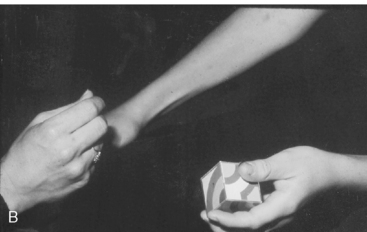
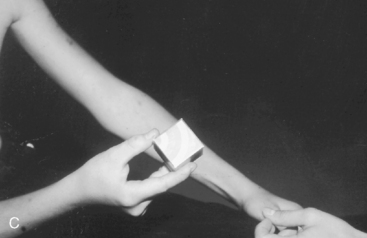
FIGURE 10-23 A, The child is forming a picture with a set of puzzle blocks. He is encouraged to find the side of the block that fits the design being constructed. The therapist has placed the correct side of the block against the palm of his hand so that he must use complex rotation to find it. B, Prior to using the in-hand manipulation skill of complex rotation, the child must use palm-to-finger translation to move the block toward the distal finger surface. In that process the block begins to be turned. C, Having identified the correct side, the child shifts the object out to the pads of the fingers prior to placement with the other blocks.
Facilitation of Bilateral Hand Use Skills
Problems: Difficulties with bilateral hand use result from a combination of problems, of which motor factors are only one component. Some children with significant cognitive delays cannot attend to two objects simultaneously; therefore, reciprocal hand use or stabilization with one hand combined with object handling by the other hand is challenging and may not be possible. Children may exhibit deficits in integration of the two body sides, and some children have impaired sensation with a lack of attention to one body side. Lack of bilateral motor experience, as with hemiplegia or after brachial plexus injuries, can cause children to approach all tasks in a one-handed manner. Other problems may include the following:
Goals: Presented next are examples of goals the therapist can use for children with a variety of levels of disability. These goals fit the categories of gross symmetrical bilateral skills, stabilizing or manipulating with one hand while manipulating with the other hand, and bilateral simultaneous manipulation. The goals are listed in increasing level of difficulty, consistent with a developmental approach. This progression in skills may not be appropriate for children with significant weakness or motor problems on one body side. The goals are that the child will:
1. Push large objects using both hands together.
2. Lift and carry large objects using both hands.
3. Lift and carry medium-sized objects using both hands.
4. Color (write), demonstrating the ability to stabilize. materials on a table surface with one open hand while the other hand manipulates materials.
5. Hold the handle of a small pan while pretending to cook (hold the edge of a puzzle box while putting pieces away, hold the handle of a small bucket while filling with water), demonstrating the ability to stabilize materials using a palmar grasp while the other hand manipulates materials.
6. Hold a cup while pouring liquid into it (hold a slice of bread while spreading butter on it, hold a marker box while putting the markers away), demonstrating the ability to stabilize materials using a variety of grasp patterns while the other hand manipulates materials (Figure 10-24, A).

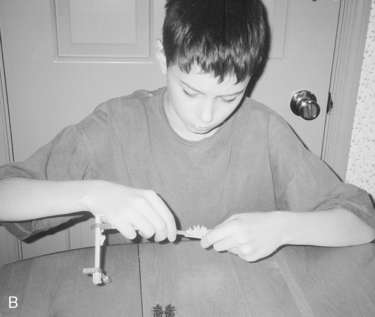
FIGURE 10-24 A, This child shows the bilateral skill of stabilizing with a refined grasp with her left hand while placing a penny in the bank with her right hand. Note the appropriate use of force in holding both objects. B, Bilateral manipulation occurs with both hands in this construction activity. The child uses modifications of the power grasp with different forearm positions on the right and left while connecting two parts of the toy.
7. Button (tie shoes, fix hair, complete a mechanical project), demonstrating the ability to manipulate objects with both hands simultaneously (Figure 10-24, B).
Treatment goals vary depending on the severity of the child’s disability and the level of skills the child is expected to acquire. The therapist must consider the child’s need and potential for gross symmetrical hand use, stabilizing with one hand while manipulating with the other, and bilateral simultaneous manipulation.
Children with Severe Disabilities: Intervention for the child with significantly increased tone or marked asymmetry focuses on promoting the child’s ability to stabilize materials with the more involved hand while manipulating with the more proficient hand. Activities that require stabilization with grasp are often easier for these children than are symmetrical bilateral skills or stabilization without grasp. However, the child can accomplish stabilization without grasp as long as he or she can use the hand in a fisted position with the wrist in neutral to slight extension. Activities that elicit symmetrical bilateral hand use can increase awareness of one arm to increase movement and/or control of that arm. Simultaneous bilateral manipulation skills usually are inappropriate for these children unless the therapist can use adaptations.
Special handling techniques can promote the child’s ability to stabilize objects while manipulating them or to use gross bilateral skills. The therapist can sit behind the child and stabilize both shoulders to help the child bring and keep both hands at the midline. The therapist should also encourage trunk rotation so that the child can cross the midline effectively.
Toys and materials selected for bilateral activities must require both hands to be used, particularly in the early phases of treatment. Initially the child may be more successful with gross bilateral skills if he or she can sustain grasp and keep the forearms pronated, such as in holding a stick horizontally to hit a balloon. Expecting bilateral hand use to occur with the forearms in supination to midposition may be far too difficult for the child.
For the child who is working on stabilizing with one hand while manipulating with the other, presenting objects on a slippery surface may require the child to use one hand as a stabilizer. Objects that have handles are useful when the therapist is working on stabilization with grasp. Activities that are simple for the manipulating hand can allow the child to focus on the role of the stabilizing hand. Usually the therapist places materials for bilateral skill development at the midline. However, the therapist and the child should explore other positions if midline positioning is not optimal.
If a child cannot successfully stabilize materials and does not show potential for this skill in the near future, the therapist should consider adaptations. Nonskid surfaces and other devices can assist in stabilization of materials for table activities.
Children with Moderate Disabilities: Intervention for children with low tone or some degree of involuntary movement can approximate the normal sequence of bilateral hand skill development. Therapy initially focuses on improving symmetry and stability and proceeds through developing the child’s skills in stabilizing with and without grasp. Children at this skill level may benefit from working on a slightly unstable surface to prompt spontaneous stabilization of materials during manipulation. The child may need adaptations for certain highly demanding activities (e.g., handwriting) in which one hand must be an effective stabilizer. Generally, simultaneous bilateral manipulation is not feasible for these children.
Children with Mild Disabilities: Children with mild disabilities may require further refinement of gross symmetrical bilateral skills and stabilizing with one hand while manipulating with the other. These children can also develop or improve their simultaneous bilateral manipulation skills. To enhance development of simultaneous bilateral manipulation skills, the therapist carefully selects, grades, and structures a variety of activities that elicit these skills. The therapist may also use functional activities of daily living to facilitate development of these skills.
Children with Muscle Weakness: Children with muscle weakness can often manage simultaneous manipulation activities well because little hand strength and movement of the arms against gravity are required. These children often need assistance or adaptations to develop the ability to stabilize materials with one hand because this demands more strength in the stabilizing arm. The child may be able to accomplish gross symmetrical bilateral skills only on table surfaces that provide arm support.