Evaluation and Interventions to Develop Hand Skills
1 Describe the typical development of hand skills in children.
2 Identify factors that contribute to typical or atypical development of hand skills.
3 Explain the implications of hand skill problems for children’s occupational performance, particularly in the areas of play, activities of daily living, and school performance.
4 Describe typical problems with children’s development of hand skills.
5 Identify evaluation tools and methods useful in assessing hand skills in children.
6 Describe intervention approaches and strategies to assist children in improving or compensating for problems with hand skills.
Hand skills are critical to interaction with the environment. The hands allow action through human contact and contact with objects. Hands are the “tools” most often used to accomplish work and play and to perform activities of daily living. The child who has a disability affecting hand skills has less opportunity to take in sensory information from the environment and to experience the effect of his or her actions on the world.
COMPONENTS OF HAND SKILLS
Effective use of the hands to engage in a variety of occupations depends on a complex interaction of hand skills, postural mechanisms, cognition, and visual perception. The term visual-motor integration refers to the interaction of visual skills, visual-perceptual skills, and motor skills. The term hand skills is used interchangeably with the terms fine motor coordination, fine motor skills, and dexterity. Because this chapter refers only to skills of the hands that are needed to attain and manipulate objects, the more specific term hand skills is used.
Although most therapists assume that the development of hand skills depends on adequate postural functions and sufficient visual-perceptual and cognitive development, these areas are not discussed in detail in this chapter. Hand skills are patterns that normally rely on both tactile-proprioceptive and visual information for accuracy. However, the child can accomplish these skills without visual feedback if somatosensory functions provide adequate information. The patterns include reach, grasp, carry, and voluntary release, as well as the more complex skills of in-hand manipulation and bilateral hand use. These patterns can be defined briefly as follows:
• Reach: extension and movement of the arm for grasping or placing objects
• Grasp: attainment of an object with the hand
• Carry: transportation of a hand-held object from one place to another
• Voluntary release: intentional letting go of a hand-held object at a specific time and place
• In-hand manipulation: adjustment of an object in the hand after grasp
• Bilateral hand use: use of two hands together to accomplish an activity
In the following discussion, the term hand-arm refers to the interactive movement and stabilization of different parts of the hand and arm to accomplish a fine motor task.
Visual skills constitute the use of extra-ocular muscles to direct eye movements. These skills include the ability to visually fix on a stationary object and the smooth, accurate tracking of a moving target. Visual-perceptual skills involve the recognition, discrimination, and processing of sensory information through the eyes and related central nervous system (CNS) structures. Visual-perceptual skills include the identification of shapes, colors, and other qualities; the orientation of objects or shapes in space; and the relationship of objects or shapes to one another and to the environment (see Chapter 12).
CONTRIBUTIONS OF CONTEXTUAL FACTORS TO HAND SKILLS
For occupational therapists, knowledge of context factors is critical for understanding, evaluating, and providing intervention for hand skill problems. Social and cultural factors, in particular, are likely to play important roles in the acquisition and use of various hand skills. Social factors that can affect the development of hand skills include socioeconomic status and gender and role expectations. Both cultural social factors are less likely to affect the development of more basic hand skills but may have a greater influence on skills needed for complex manipulation of objects and tool use. For example, children who live in conditions of poverty may not have the exposure to writing utensils, scissors, and other materials common to children from middle-class environments.
The objects that are important to the child’s cultural group influence the development of object manipulation. Because tools that are important in one culture may not be available in another, children may not have the opportunity to develop some tool-specific skills. For example, eating utensils vary from chopsticks to forks and spoons. Scissors use may be important for school performance in some cultures but not in others.
In addition, the age at which children are expected to achieve skill in object manipulation can vary. Safety concerns influence parents in some cultural groups to delay introduction of a knife to their child, whereas parents in other cultural groups encourage independence in knife use. Some cultures introduce children to the use of writing materials before 1 year of age. Other cultures do not provide children with these materials until they can be expected to adhere to requirements such as using them only on paper (rather than on the wall or on clothing).
Culture also influences the perception of children’s need for manipulative materials. Linked to this is the cultural group’s view of the importance of play. Play materials that provide opportunities for the development of manipulative skills (e.g., building sets, beads, puzzles, table games) are highly valued in some cultural groups, whereas in other groups, play with gross motor objects (e.g., balls, riding toys) or play with animals is more valued. Some cultural groups do not view children’s play as important; therefore, few play materials of any type are available.
Although the types of activities encouraged can promote the development of specific skills, acquisition of the basic hand skills of reach, grasp, release, and manipulation does not rely on the availability of any particular materials; rather, it relies on reasonable exposure to a variety of materials with the opportunity to handle them. Verdonck and Henneberg studied differences in performance on the Box and Block Test of Manual Dexterity in two groups of South African children between 6 and 17 years of age.140 They found that children from the middle-class urban area performed significantly better than those from the poor rural area. Yim, Cho, and Lee found that school-aged Korean children had somewhat less strength in palmar and lateral pinch than that measured in Western children.153
CONTRIBUTIONS OF BODY FUNCTIONS TO HAND SKILLS
Body functions related to performance play a critical role in the development of hand skills. Although therapists usually give motor issues the most attention, many dimensions of development significantly influence effective hand use, including the child’s visual skills, somatosensory functions, sensory integration, visual perception, cognition and, as discussed above, social factors and culture. As children mature, they begin to coordinate visual skills with hand skills effectively, and later they combine hand-eye coordination with visual-perceptual skills.3
Visual Skills
Visual skills play a major role in the development of hand function.10,77,142 Vision is particularly important for learning new motor skills. At about 4 months of age, infants begin to move their hands under visual control as they reach for an object and make differentiated finger movements. The visuomotor development required for accurate reach matures by approximately 6 months of age. The infant’s visual-motor coordination continues to refine, and by 9 months of age, the infant guides his or her hand movements using visual-somatosensory integration (i.e., these sensory inputs are combined and compared as the infant anticipates and plans movement). Vision is also important as the infant learns new fine motor skills or when an activity requires highly precise and accurate movements (e.g., stringing small beads or putting together a puzzle).
Somatosensory Functions
The relationship between somatosensory functions of the hands and hand skills is strong. Good hand skills are associated with intact somatosensory functioning; however, intact somatosensory functioning does not necessarily yield good hand skills. Huang, Gillespie, and Kuo found that adults with normal hand function had significant benefit from feedback that included both visual and haptic information to ensure consistency and rhythm while manipulating an object.74
The role of somatosensory information and feedback is critical to development in many areas of children’s hand skills, particularly those involving isolated movements of the fingers and thumb. Typical infants develop the ability to match haptic perception (knowledge of objects gathered by means of active touch) of some three-dimensional objects with visual perception within the first 6 months of life. Bushnell and Boudreau reported that children as young as 2.5 years of age can identify common objects by touch alone and that children 5 years of age demonstrate good haptic recognition of unfamiliar objects.16 Many aspects of haptic perception, such as identification of three-dimensional common objects and perception of spatial orientation, are well developed by 6 years of age. The adolescent has fully developed the refinement of haptic perception and the ability to discriminate all aspects of object characteristics through touch.132
The fingertips gather precise information about many types of object qualities. Children with impaired control of finger movement have limited access to somatosensory information, and/or the impaired control of finger movement may reflect their difficulties in perceiving and using sensory information. Initiating and sustaining grasp force requires tactile and proprioceptive input and integration.60,64,78 The ability to hold objects in the hand (i.e., without dropping them) is related primarily to intact somatosensory functioning.62 Gordon and Duff also noted that tactile information is critical for anticipating the amount of force needed to grasp and lift an object.64 Apparently a minimum amount of tactile awareness, as measured by two-point discrimination, is needed for functional development of these fine motor skills.
Somatosensory functioning is difficult to study in children, particularly in young children and those with disabilities. In testing, the performance of these children varies from one session to another, which further complicates the assessment process. Given that the link between somatosensory functioning and hand skills is a strong one, further investigation of the relationship between tactile functioning and various hand skills will support the development of new intervention approaches for these children.
Sensory Integration
The types of sensory integration problems most likely to influence hand use are sensory registration problems, tactile hypersensitivity, poor tactile discrimination, and dyspraxia. Children with poor sensory registration engage in few activities involving hand skills. The child with tactile hypersensitivity is likely to avoid contact with certain materials, thus limiting exposure to various objects. Motor-planning deficits and clumsiness are associated with poor tactile and proprioceptive functioning. Praxis problems based on poor tactile and proprioceptive processing are referred to as somatodyspraxia.4 Children with cerebral palsy can have sensory integration problems in addition to motor problems. Evidence of motor planning problems has been identified in children with cerebral palsy130 as well as in children with other motor problems.
Visual Perception and Cognition
Perceptual development and cognitive development are difficult to isolate from each other, particularly as they relate to object-handling skills in children; for this reason, these areas are addressed together here. The development of hand skills allows for more complex interaction with objects, and perceptual and cognitive development allows the child to know the possibilities available for object use and interactions. Hand use and cognitive development seem to be particularly linked in infancy and very early childhood.35
The child’s perception of object characteristics, movement speed required, and power needed affects his or her ability to effectively control objects.44 The child acquires knowledge about objects through object manipulation. Early manual exploratory behavior plays an important role in the development of visual-spatial skills and learning about the environment.34
During the first 6 months, the infant uses visual and tactile perception to guide fine motor development and begins to develop an awareness of object placement in space. In the second half of the first year, the infant adjusts the actions of the hand in response to object characteristics, such as size, shape, and surface qualities.28 Ruff, McCarton, Kurtzber, and Vaughan emphasized the importance of object manipulation in infants between 6 and 12 months of age for learning object characteristics, because this learning was believed to be important for concept and language development.119 Infants demonstrate their perceptual and cognitive skills when reaching for objects. By 9 to 10 months of age, infants adapt their arm positions to horizontal versus vertical object presentations and shape their hands appropriately for convex and concave objects.
During the second year, infants learn to relate objects to one another with more accuracy and purpose. Before 18 months of age, infants modify their movement approach in anticipation of the weight of the object.16,28
Rao discussed the interaction of cognition and hand skill development.114 Like perceptual development, cognitive development influences and is supported by the development of hand skills. For example, changes in attentional control and the development of problem-solving strategies are seen in the gradual improvement in infants’ ability to handle two objects simultaneously. Without this development in cognition, bilateral skills would not be possible. The infant must be able to attend to two objects simultaneously to be able to bang objects together, stabilize an object with one hand while manipulating with the other, and manipulate two or more objects simultaneously. Because attention and planning demands are greater for two-handed activities than for one-handed activities, bilateral skill development lags behind unilateral skill development.16,28
Skeletal Integrity
The integrity of the hand’s joint and bone structures is an important consideration in hand function. Children with congenital hand anomalies may be missing one or more digits, a condition that significantly affects the variety of possible prehension patterns. Refined finger movements and in-hand manipulation skills may also be limited or absent. Severe congenital anomalies can affect bilateral hand use. Involvement of the thumb has a more significant effect on acquisition and use of hand skills than impairment of any other digit.
Joint range of motion (ROM) has a significant effect on the positioning of the arm for hand use and on reaching and carrying skills. Effective hand function also depends on adequate mobilization of distal muscle groups that control palmar arches. Limitations in range can occur as a result of abnormal joint structure, muscle weakness, or joint inflammation. Any of the problems that reduce range of motion are likely to affect a child’s ability to grasp larger objects or to flatten the hand to stabilize materials.
Muscle Function
Aspects of muscle functions include muscle power (strength), muscle tone, and muscle endurance. Sufficient strength is necessary to initiate all types of grasp patterns and to maintain these patterns during lifting and carrying. Children’s grasp strength gradually increases through the preschool years,88,89 the elementary school years,153 and adolescence.93,126 This increase allows them to engage in activities with objects of increasing weight and to use greater resistance. Children with poor strength may be unable to initiate the finger extension or the thumb opposition pattern necessary before grasp. They also may not have the flexor control to hold a grasp pattern. Many children with diminished strength are unable to use patterns that rely on the intrinsic muscles for control and therefore are unable to use thumb opposition or metacarpophalangeal (MCP) joint flexion with interphalangeal (IP) joint extension. Children with fair strength may be able to initiate a grasp pattern but may be unable to lift an object against gravity while maintaining the grasp. Endurance during an activity can be a problem for children with mildly diminished strength, particularly in situations in which they must use a sustained grasp pattern or hold an object against resistance (e.g., during eating with utensils, coloring, handwriting, and scissors activities).
Tone in muscle groups affects the stability of parts of the arms and hands during activities and the types of movements possible. Damage to the CNS may cause tonal abnormalities, which can affect joint ROM and, in general, decrease speed of movement. Increased tone results in loss of ROM, whereas decreased tone results in exaggerated joint ROM and decreased stability. Children with fluctuating tone typically have full ROM but can maintain joint stability only at the extreme end of a joint position (full flexion or full extension). In addition, movements are less controlled and often are random or unrelated to the task.
GENERAL DEVELOPMENTAL CONSIDERATIONS
Developmental principles are further described in Chapter 3. Overall, hand skill development has a very long course, continuing through adolescence for many skills.33,65 This long course of development mirrors other aspects of development and reflects the complexity of hand skills in expressing an understanding of objects and what they can be used to accomplish.
Two principles with particular application to hand skill development are the development of movement patterns from mass to specific and of motor control from proximal to distal. Two additional principles are discussed in this section: specifically, that mature movement patterns are characterized by integrated stability and mobility and that involuntary movement patterns precede associated movements that develop into isolated, voluntary movement and coordinated action.
The mass-to-specific principle of development means that less-differentiated movement patterns precede discrete, highly specialized skills. For example, the infant uses all fingers in early grasping and later uses only the specific number of fingers needed for object contact.
The proximal-to-distal principle means that development initially occurs proximally (in the head and trunk) and gradually progresses toward the distal parts of the body (hands and feet). Clinicians have interpreted this relationship to mean that improvement in postural control results in improvement in hand skills and/or that intervention should be sequential, proceeding from proximal to distal control. However, several clinical research studies24,146 and some authors105,106 have questioned this principle. The clinical studies have yielded weak correlations between postural or proximal control and hand function (approximately r = 0.20 to 0.35). Case-Smith and colleagues stated that “the correlations between the proximal and distal motor functions would be markedly higher if proximal motor control was necessary for the development of distal motor skill” (p. 661).24 The relationship between proximal and distal control is a functional or biomechanical one in which postural control is necessary for placement of the hand in space and support of the hand during its execution of skills. These workers emphasized that “therapists should not assume that proximal control is a necessary precursor to fine motor skill; they should, however, assume that treating proximal weakness may affect distal function” (p. 661).24 However, the degree of proximal control does not necessarily determine the child’s degree of distal control.
Pehoski106 used work by Lawrence and Kuypers87 to explain why distal control is not directly linked to proximal control. Two motor systems are used in upper extremity control. One system is responsible for postural control and proximal control, including integrated body-limb and body-head movements. This system comprises primarily the ventromedial brainstem pathways that synapse primarily with interneurons to trunk and proximal muscles. In contrast, the corticospinal track system originates in the primary motor cortex, and its fibers directly synapse with the motoneurons for hand muscles. The latter system allows for isolated finger movements, which are needed for a precise pincer grasp and fine manipulation.106 Thus development of upper extremity skills and hand skills occurs as a result of proximal and distal control mechanisms, rather than proximal to distal mechanism.
Refined movements also depend on the ability to combine patterns of stability and mobility effectively. The child must develop the ability to stabilize the trunk effectively and maintain it in an upright position without relying on the frequent use of one or both arms to maintain balance. In addition, the child sequentially develops patterns of stability and mobility in the scapulohumeral, elbow, and wrist joints; this permits arm use independent of, but effectively used with, trunk movement. Eventually the ability to use stability and mobility in the hand emerges.
For normal functioning, joints must be able to stabilize at any point in the normal range of movement and to move within small, medium-sized, or large segments of range. During most arm-hand activities (e.g., grasp and manipulation of objects), the proximal joints are stable while the fingers are moving. However, in carrying, the distal joints are stable while the arm is moving. In mature handwriting, the elbow, forearm, and wrist joints are relatively stable and the shoulder and finger joints are mobile.
An important sequence in the development of motor control is the use of straight movement patterns before the emergence of controlled rotation patterns. For example, the infant first develops controlled stability and mobility in basic flexion and extension of the shoulder, elbow, and wrist. This is followed by control of internal and external rotation of the shoulder and pronation and supination of the forearm.
In typical development the infant gradually learns to use both sides of the body together in effective ways and to use each side of the body independently of the other. Initially the infant uses his or her arms in asymmetrical patterns that are not coordinated. Movements of one arm often elicit reflexive, nonpurposeful reactions in the other arm. Gradually the infant develops the ability to move the two arms together in the same pattern. As skilled use of symmetrical hand and arm patterns is refined, the infant begins to use the two arms independently of one another for different parts of an activity. For example, one hand stabilizes an object while the other hand manipulates it. Overflow and associated movements gradually decrease to allow separate but coordinated action of the two hands.
DEVELOPMENT OF HAND SKILLS
As in all areas of occupational therapy, the therapist must supplement academic study of hand skill development and treatment with observations of typical infants and children and of children with differences in development. Imitating each of the normal and abnormal movements and patterns described in the following text also helps clarify the descriptions provided.
Reach and Carry
Rosblad stated that “in a reaching movement, the goal is to transport the hand to the target, with precision in both time and space” (p. 81).117 Thus the development of reaching is described in terms of the changes that take place in the control and speed of the hand’s movement toward the object and the preparation of the hand for grasp.
Within the first several days of life, the neonate shows visual regard of objects close to him or her and activation of the arms in response to objects.141 Over the next few months the arms become more active and the infant swipes or bats at objects with the arm abducted at the shoulder. Reach with an extended arm is likely to occur between approximately 12 and 22 weeks of age.136 Objects are rarely grasped and then only by accident. If grasped, they are released at random, generally in association with arm movements.
Gradually a midline orientation of the hands develops. Initially the hands are held close to the body. Soon, with an increased desire for visual regard of the hands and greater proximal arm stability, the child holds the hands further away to view them. This pattern precedes the onset of symmetric bilateral reaching, which usually occurs first in the supine and then in the sitting position. At this stage, the child initiates reach with humeral abduction, partial shoulder internal rotation, forearm pronation, and full finger extension.
As the infant shows increasing dissociation of the two body sides during movement, unilateral reaching begins. Abduction and internal rotation of the shoulder are less prominent in reach. The hand opens in preparation for grasping the object and is usually more open than necessary for the size of the object.
As scapular control and trunk stability mature, the infant begins to use shoulder flexion, slight external rotation, full elbow extension, forearm supination, and slight wrist extension during reaching. Active supination of the forearm is not seen until some external rotation is used to stabilize the humerus. In addition, well-controlled elbow extension evolves as the rotation elements are developing. Mature reach is usually seen with sustained trunk extension and a slight rotation of the trunk toward the object of interest. Over the next few years, the child refines this unilateral reaching pattern, increasing the accuracy of arm placement and the grading of finger extension as appropriate to the size of the object (Figure 10-1), as well as the timing of the various movement elements. To study the evolution of reaching behaviors after its primary development, Schneiberg, Sveistrup, McFadyen, McKinley, and Levin compared reaching behavior in typical 4- to 11-year-olds with that of adults.121 Developmental changes during this period include decreased trunk movement when objects are within arm’s length, enhanced smoothness, and decreased variability. With increasing age, arm movements were straighter and reaching patterns were more consistent.121 The quality of reach with grasp continues to mature until approximately 12 years of age, at which time the child prepares the hand with the optimal hand opening for the object size at the initiation of reach.84 Before this age the child needs to use visual monitoring for accuracy in hand opening during reach.
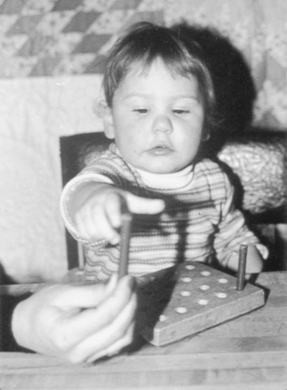
FIGURE 10-1 This typically developing child demonstrates reach with trunk rotation, full elbow extension, slight forearm rotation, and wrist stability, yet some degree of excess finger extension before grasp. (Courtesy Ed Exner, Greensburg, PA.)
Carrying (“moving” and “lifting”) involves a smooth combination of body movements accompanied by stabilization of an object in the hand. When carrying involves objects used in most occupational activities, small ranges of movements are used and adjusted in accordance with the demands of the activity. Co-contraction in the more distal joints of the wrist and hand often is present. The child must be able to hold the forearm stable while in any degree of rotation, and he or she must be able to modify the forearm and wrist positions during the carry so that the object remains in an optimal position. Similarly, the child must be able to use shoulder rotation movements simultaneously with shoulder flexion and abduction so that appropriate object orientation is maintained.
Grasp Patterns
Napier proposed two basic terms to describe hand movements: prehensile and nonprehensile.103 Nonprehensile movements involve pushing or lifting an object with the fingers or the entire hand. In contrast, prehensile movements involve grasp of an object and may be subdivided according to the purpose of the grasp: precision or power. Precision grasps involve opposition of the thumb to fingertips. Power grasps involve the use of the entire hand. In a power grasp, the thumb is held flexed or abducted to other fingers, depending on control requirements.
In most cases the activity and the object’s characteristics determine the grasp pattern used. Small objects are generally held in a precision grasp, primarily because of the large amount of sensory feedback available through the fingertips and the control used to move them. Medium objects can be held with either pattern, and large objects are held with a power grasp. Napier noted a frequent interplay between precision and power handling of different objects based on the activity demands.103
Weiss and Flatt described a slightly different method of classification.144 Grasps with no thumb opposition include hook grasp, power grasp, and lateral pinch. Patterns that use thumb opposition include tip and palmar pinches. The palmar pinch category is divided into standard, spherical, cylindrical, and disk grasps.
The hook grasp is used when strength of grasp must be maintained to carry objects. For this grasp, the transverse metacarpal arch is essentially flat, the fingers are adducted with flexion at the IP joints, and flexion or extension occurs at the MCP joints (Figure 10-2, A).144 The thumb can be flexed over the fingers if additional power is needed. Observation of this pattern provides an indication of the child’s ability to sustain wrist extension during finger flexion.


FIGURE 10-2 A, Hook grasp used to carry a child’s art case. B, Power grasp with the right hand, used in cutting bread. (Courtesy Kanji Takeno, Towson University, Towson, MD.)
In contrast, the power grasp often is used to control tools or other objects. Oblique object placement in the hand, flexion of the ulnar fingers, less flexion with the radial fingers, and thumb extension and adduction facilitate precision handling with this grasp (e.g., for brushing the hair). Thus the child stabilizes the object with the ulnar side of the hand and controls the object for position and use with the radial side of the hand (Figure 10-2, B).144 Observation of this pattern allows for assessment of the degree of radial-ulnar dissociation in the hand that the child can use and his or her control of thumb adduction with extension.
Lateral pinch is used to exert power on or with a small object. Partial thumb adduction, MCP flexion, and slight IP flexion are characteristics of this pattern. Although the index finger is slightly flexed, it is more extended than the other fingers. The pad of the thumb is placed against the radial side of the index finger at or near the distal interphalangeal (DIP) joint (Figure 10-3). This pattern involves controlling the index finger while adducting and flexing the thumb.
There are two types of standard pinches. Opposition of the thumb to the index finger pad describes only the pad-to-pad, two-point pinch124 or pincer grasp (Figure 10-4, A).57 Opposition of the thumb simultaneously to the index and middle finger pads, which provides increased stability of prehension, describes the three-point pinch124 or three-jaw chuck grasp (Figure 10-4, B). In both cases, the thumb forms an oval or a modified oval shape with the fingers. In addition, the forearm is slightly supinated, which frees the thumb and radial fingers from contact with the surface and allows for an optimal view of the object. Observation of this pattern allows for assessment of the child’s ability to control objects with the radial finger pads while controlling thumb opposition.

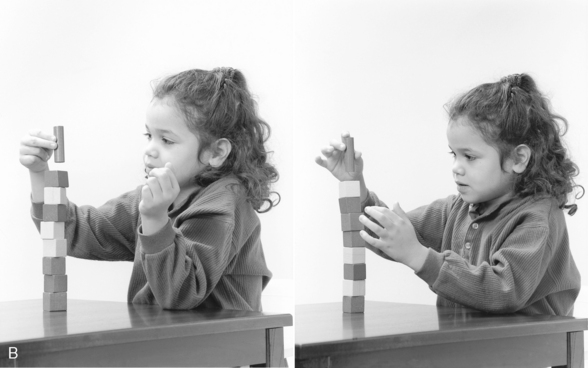
FIGURE 10-4 A, Pincer grasp, used to place “food” for the “climbing polar bears.” B, This child uses variations of a three-jaw chuck grasp with her right hand, depending on task demands. (Courtesy Kanji Takeno, Towson University, Towson, MD.)
Opposition of the thumb tip and the tip of the index finger, forming a circle, describes a tip pinch (Figure 10-5). All joints of the index finger and thumb are partly flexed. This pinch pattern is used to obtain small objects. Observation of this grasp provides information about the child’s ability to dissociate the two sides of the hand and to use the tips of the index finger and thumb. Edwards, Buckland, and McCoy-Powlen further explain and illustrate the development of grasping patterns.38
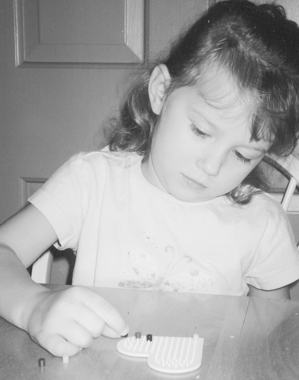
FIGURE 10-5 Tip pinch with the right hand, used to complete a bead craft project. Normal radial grasps, such as the tip pinch, are accompanied by slight forearm supination.
Differences in hand posture characterize the other palmar grasps. Significant wrist extension, finger abduction, and some degree of flexion at the MCP and IP joints describe the spherical grasp (Figure 10-6). Stability of the longitudinal arch is necessary to use this pattern to grasp large objects. The hypothenar eminence lifts to assist the cupping of the hand for control of the object.144 Observation of this grasp pattern suggests the child’s ability to balance control of the intrinsic and extrinsic hand muscles.
In the cylindrical grasp, the transverse arch is flattened to allow the fingers to hold against the object. The fingers are only slightly abducted, and IP and MCP joint flexion is graded according to the size of the object. When additional force is required, more of the palmar surface of the hand contacts the object (Figure 10-7).144 Observation of this pattern allows for assessment of palmar arch control during handling of a relatively large object.

FIGURE 10-7 This child uses a cylindrical grasp with his left hand and a disk grasp with his right hand to open a jar. Note the grading of finger abduction with the left hand to provide adequate stability to the jar.
A disk grasp incorporates finger abduction that is graded according to the size of the object held, hyperextension of the MCP joints, and flexion of the IP joints (see Figure 10-7).144 The wrist is more flexed when objects are larger, and only the pads of the fingers contact the object. The amount of thumb extension also increases with object size. The transverse metacarpal arch is flattened in this prehension pattern. This pattern involves dissociation of flexion and extension movements and use of a combination of wrist flexion with MCP extension and IP flexion.
Sequential Development of Grasp Patterns
Several developmental trends affect the particular type of grasp pattern an infant is able to use at any time. The sequences listed in Box 10-1 are different ways to reflect the progressions in grasp; these sequences interact and overlap. The infant’s growing interest in objects, desire to attain them, and desire to explore them and relate them to other objects influence these motor sequences. Haptic development and visual-perceptual development contribute to the infant’s ability to shape the hand appropriately for the object and to approach the object with optimal orientation of the arm and hand.
Another aspect of motor development that contributes to the infant’s use of increasingly mature and more varied patterns is the ability to effect internal stability throughout upper extremity movement, forearm supination, and thumb opposition. Thumb activity and control are necessary to allow for patterns other than palmar grasp. The ability to stabilize the wrist in a slightly extended position is important for grasp patterns that use distal (fingertip) control. Slight forearm supination is important because it positions the hand so that the thumb and radial fingers are free for active object exploration, and it allows the infant to view fingers and thumb during grasp.73
A typical sequence can be seen during the infant’s first 6 months. Initially the infant appears to have no voluntary hand use. The hands alternately open and close in response to various sensory stimuli. Gradually the traction response and grasp reflex decrease, and a voluntary palmar grasp begins to emerge (Figure 10-8). By approximately 6 months the infant progresses to being able to use a radial palmar grasp. Case-Smith, Bigsby, and Clutter found a marked increase in grasp skill between 4 and 5 months of age.23 They noted less change between 5 and 6 months of age.
The second 6 months is a key period for the development of hand skills. The ability to grasp a variety of objects increases significantly between 6 and 9 months of age. During this time, grasp patterns with active thumb use emerge. Crude raking of a tiny object is present by about 7 months of age, and by 9 months of age the infant is able to hold a tiny object between the finger surface and the thumb. By 8 to 9 months of age, the infant holds a larger object between the thumb and the radial fingers (Figure 10-9) and readily varies the grasping pattern according to the shape of the object. Case-Smith et al. noted a particularly dramatic increase in skill between 8 and 9 months of age.23 However, at this time intrinsic muscle control is not effective because the infant does not use grasp with MCP flexion and IP extension. Between 9 and 12 months of age, refinement occurs in the ability to use thumb and finger pad control for tiny and small objects. More precise preparation of the fingers before initiation of grasp, more inhibition of the ulnar fingers, and slight wrist extension and forearm supination are characteristics of this refinement.
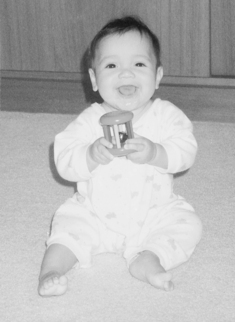
FIGURE 10-9 This baby uses a radial-digital grasp with both hands to hold a toy for shaking and mouthing.
After 1 year of age, further refinement occurs in grasp patterns that were seen earlier, and more sophisticated patterns emerge. Between 12 and 15 months of age, the infant’s ability to hold crackers, cookies, and other flat objects identifies an increasing control of the intrinsic muscles. Although studies are limited in terms of grasp development for patterns other than the pincer grasp, between 18 months and 3 years of age, most children with typical development acquire the ability to use a disk grasp, a cylindrical grasp, and a spherical grasp with control. Control of a power grasp continues to develop through the preschool years. The pattern for a lateral pinch may be present by 3 years of age, but children generally do not use this pattern with power until later in the preschool years. Overall grasp patterns for a variety of objects are well developed by 5 years of age, but those involving tools may continue to mature into the early school years.
In addition to quality of grasp, strength of grasp continues to increase throughout childhood. Lee-Valkow et al. reported on the development of grip and pinch strength in typical preschool-age children.88 These workers noted significant increases in strength for palmar grip, key (lateral) pinch, and tripod (three-point) pinch for children between 3 and 4 years of age and 4 and 5 years of age. The increase in strength was greater between 4 and 5 years than between 3 and 4 years in both preferred and nonpreferred hands. Yim et al. found increases in grip, lateral pinch, palmar pinch, and tip pinch across the age range in 7- to 12-year-old Korean children; they also reported significant differences in grip strength between boys and girls in each age group for both right and left hands.153 They noted that right-handed girls were stronger than left-handed girls in grip and lateral pinch with both hands. In a study of isometric strength of the index finger, Smits-Engelsman, Wilson, Westenberg, and Duysens found that isometric force increased gradually during the 5- to 10-year-old age span, reflecting corticospinal system maturation.127 Compared with 10- to 12-year-olds, adults exhibited greater use of alternative strategies for selecting and monitoring force needed in an activity.
In-Hand Manipulation Skills
In-hand manipulation includes five basic types of patterns: finger-to-palm translation, palm-to-finger translation, shift, simple rotation, and complex rotation.47 All skills require the ability to control the arches of the palm (Figure 10-10). Long, Conrad, Hall, and Furler described translation as a linear movement of the object from the palm to the fingers or from the fingers to the palm; the object stays in constant contact with the thumb and fingers during this pattern.90 The fingers and thumb maintain grasp but move into and out of MCP and IP flexion and extension. In contrast, Exner described the pattern of finger-to-palm translation as grasping the object with the pads of the fingers and thumb and moving it into the palm.47 The finger pad grasp is released so that the object rests in the palm of the open hand or is held in a palmar grasp at the conclusion of the pattern. The object moves in a linear direction in the hand, and the fingers move from an extended position to a more flexed position during the translation. An example of this skill is picking up a coin with the fingers and thumb and moving it into the palm of the hand.



FIGURE 10-10 A,The child shows the ability to keep the palm in a cupped position to hold several stones for a game. The forearm is in almost full supination. B, Palm-to-finger translation with stabilization is initiated for one of the stones while the other stones are retained in the palm. The translation movement produced by the fingers is accompanied by forearm rotation into midposition. C, Palm-to-finger translation with stabilization is completed for one stone. The other stones are retained in the hand by flexion of the ulnar fingers. The forearm moves toward pronation to assist with placement of the stone on the game board.
Palm-to-finger translation is the reverse of finger-to-palm translation.47 However, palm-to-finger translation requires isolated control of the thumb and use of a pattern beginning with finger flexion and moving toward finger extension (see Figure 10-10). This pattern is more difficult for the child to execute than finger-to-palm translation. An example of this skill is moving a coin from the palm of the hand to the finger pads before placing the coin in a vending machine.
Shift involves linear movement of the object on the finger surface to allow for repositioning of the object on the pads of the fingers.47 In this pattern the fingers move just slightly at the MCP and IP joints, and the thumb typically remains opposed or adducted with MCP and IP extension throughout the shift. The object usually is held solely on the radial side of the hand. Examples of this skill are separating two pieces of paper, moving a coin from a position against the volar aspect of the DIP joints to a position closer to the fingertips (e.g., so that the coin can be easily inserted into the slot of a vending machine), and adjusting a pen or pencil after grasp so that the fingers are positioned close to the writing end of the tool. This skill is used frequently in dressing tasks such as buttoning, fastening snaps, lacing shoes, and putting a belt through belt loops.
The two patterns of rotation are simple rotation and complex rotation. Simple rotation involves the turning or rolling of an object held at the finger pads approximately 90° or less.47 The fingers act as a unit (little or no differentiation of action is shown among them), and the thumb is in an opposed position. Examples of simple rotation are unscrewing a small bottle cap, reorienting a puzzle piece in the hand by turning it slightly before placing it in the puzzle, and picking up a small peg and rotating it from a horizontal to a vertical position for insertion into a pegboard.
Complex rotation involves the rotation of an object 180 to 360° once or repetitively.47 During complex rotation the fingers and thumb alternate in producing the movement, and the fingers typically move independently of one another. An object may be moved end over end, such as in turning a coin or a peg over or in turning a pencil over to use the eraser.
In-hand manipulation skills can occur with only one object in the hand or with two or more objects in the hand. For example, a child typically unscrews a bottle lid with no other objects in his or her hand. In-hand manipulation skills also are used when the child is holding other objects in the hand. For example, a child may have two or more pieces of cereal in his or her hand but brings only one piece out to the finger pads before placing it in the mouth (see Figure 10-10). The term with stabilization refers to the use of an in-hand manipulation skill while other objects are stabilized in the hand. Therefore picking up multiple pieces of cereal involves palm-to-finger translation with stabilization, whereas unscrewing the bottle lid is simple rotation. In-hand manipulation skills with stabilization are generally more difficult to perform than the same skill without the simultaneous stabilization of other objects in the hand.
Developmental Considerations
Motor skill prerequisites for in-hand manipulation include the following43:
• Movement into and stability in various degrees of supination
• Opposed grasp with thumb opposition and object contact with the finger surface (not in the palm)
• Isolated thumb and radial finger movement
• Control of the transverse metacarpal arch
Children who are unable to use in-hand manipulation skills are likely to substitute other patterns. Substitution patterns are part of the typical strategies used in acquiring in-hand manipulation skills; however, their use does not necessarily represent abnormal fine motor control. Typical patterns a child uses when he or she shows very limited in-hand manipulation are (1) changing of hands (putting the object in the other hand for use) and (2) transferring from hand to hand (moving the object from one hand to the other and back to the hand that held it first). The child uses these patterns after the initial grasp when he or she realizes that the object in the hand needs to be repositioned for use but that the object cannot readily be adjusted in that hand. For example, a child picks up a crayon or marker with the right hand but is unable to shift it to place the fingers near the writing end; therefore, he or she grasps the object with the left hand and then transfers it back to the right hand with the fingers appropriately positioned. Some children preplan for this by picking up the crayon with the nonpreferred hand and changing it to the preferred hand.
Therapists observe several skills in children who are beginning to use in-hand manipulation skills or are preparing for the use of these skills. Infants typically engage in bilateral manipulation of objects by moving an object between the two hands. As the child moves the object between the hands, he or she turns and repositions it within the hands. Children use this strategy, called a hand assist, to substitute for palm-to-finger translation or rotation. In this case the object does not leave the hand that grasped it initially, but the other hand helps with repositioning of the object. Sometimes children use other surfaces or other parts of the body to provide support for the manipulation. Children commonly use assist strategies for shift and complex rotation.
Ongoing research is directed toward determining a sequence for the development of in-hand manipulation skills.45,107,108 Based on these research studies, the following developmental sequence has emerged. By approximately 12 to 15 months of age, infants use finger-to-palm translation to pick up and “hide” small pieces of food in their hands. By 2 to 2.5 years of age, children use palm-to-finger translation and simple rotation with some objects. Complex rotation skills are observed in children at 2.5 to 3 years of age, although this age group often has difficulty with them. By 4 years of age, children consistently use complex rotation without using an external support.107 Children between 3.5 and 5.5 years of age develop skills in rotating a marker (regardless of its initial orientation) and shifting it into optimal position for coloring and writing.45,75 Shift typically is evident but inconsistent in children 3 and 3.5 years old.45
After 3 years of age the child uses in-hand manipulation skills with greater proficiency and consistency. Dropping of objects during in-hand manipulation tasks decreases through the preschool years.108 Lee-Valkov et al. reported data on preschool-age children’s object manipulation speed, as gathered with the Functional Dexterity test (using a pegboard with short pegs approximately 1 inch in diameter).88 The test was administered to both hands, and scoring was based on the amount of time needed to rotate and place 16 pegs, accounting for use of substitution patterns or for dropping. Speed in performing the test improved yearly, with improvement in time to completion of approximately 7 to 8 seconds each year.
By 6 years of age, children develop the ability to use a variety of in-hand manipulation skills with stabilization.45,108 Between 6 and 7 years of age, children more consistently use combinations of in-hand manipulation skills that must be used in an activity (e.g., palm-to-finger translation with stabilization followed by complex rotation with stabilization). A recent study by Pont, Wallen, Bundy, and Case-Smith illustrates the challenges of measuring in-hand manipulation skills in children between the ages of 5 and 6 years, including the variability in performance that still seems to be present at that age.111
Ongoing research by Exner and colleagues suggests that children continue to refine in-hand manipulation skills up to approximately 9 to 10 years of age and continue to develop speed of skill use through 12 years of age. Yim et al. used the Nine-Hole Pegboard test to evaluate dexterity skills (complex rotation skills) in Korean children without disabilities between the ages of 7 and 12 years.153 In comparing their data for 12-year-olds with data for adults obtained by Kellor, Rost, Silberberg, Iversen, and Cummings,79 they found that the girls’ mean time scores were approximately the same as those for the youngest adults, but that the 12-year-old boys’ mean time scores were slightly lower. The difference may reflect a cultural difference or possibly the continuing development of object manipulation speed during adolescence.
The ability to use a skill with one type of object is not always associated with an ability to use the skill with another size or shape of object. For example, the child may be able to use simple rotation to turn a small peg but may not be able to use simple rotation to orient a crayon for coloring. In general, small objects (e.g., smaller-diameter crayons) are easier for children to manipulate than slightly larger objects (e.g., larger-diameter crayons) or tiny objects. Tiny objects require precise fingertip control, whereas medium-sized and larger objects require control with more fingers.
In addition to object characteristics, other factors can contribute to a child’s use of in-hand manipulation skills; such factors include the cognitive-perceptual demands of the activity, the child’s interest in the manipulative materials or the activity, processing tactile-proprioceptive information, visual acuity, and the child’s motor-planning skills. Problems in any of these areas can affect development of in-hand manipulation skills. Data collected by Lee-Valkov et al. suggest that dexterity in typical preschool children is not significantly correlated with grip or pinch strength.88 However, it should be noted that typical children were likely to have grip and pinch strength generally within normal limits. Markedly diminished strength could have a negative effect on in-hand manipulation skills.
Voluntary Release
Voluntary release, like grasp, depends on control of arm and finger movements. To place an object for release, the arm must move into position accurately and then stabilize as the fingers and thumb extend. Gordon, Lewis, Eliasson, and Duff refer to the two components of voluntary release as replacement and release.63
Initially the infant does not voluntarily release an object; objects either drop involuntarily from the hand or must be forcibly removed from the hand. As the infant’s nondiscriminative responses to tactile and proprioceptive stimuli decrease and visual control and cognitive development increase, volitional control of release emerges. With increases in the mouthing of objects and bringing of both hands to midline and playing with them there, the infant begins to transfer objects from one hand to another. Initially the child stabilizes the object in the mouth during transfers or pulls it out of one hand with the other. Soon the infant begins to freely transfer the object from one hand to another. The receiving hand stabilizes the object, and the releasing hand is fully opened.
By 9 months of age, the infant begins to release objects without stabilizing then with the other hand. The arm is fairly extended during release. The infant exhibits increasing humeral control as he or she moves the arm to drop objects in different locations. The next step is the development of elbow stability in various positions, and the infant begins to release with the elbow in some degree of flexion. The child may stabilize the arm or hand on the surface during release. At about 1 year of age, the child can release objects with shoulder, elbow, and wrist stability; however, the MCP joints remain unstable during this pattern, therefore the infant continues to show excess finger extension (Figure 10-11, A). Gradually the child develops the ability to release objects into smaller containers (Figure 10-11, B) and to stack blocks (Figure 10-11, C). The release pattern is refined over the next few years until the child can release small objects with graded extension of the fingers, indicating control over the intrinsic hand muscles. These skills also illustrate the integration of perceptual, cognitive, and sensory skills with motor skills. For example, Eliasson and Gordon reported that typical children between 7 and 13 years of age demonstrate the ability to effectively modulate a decrease in force used to grasp a lighter object and a heavier object to allow for appropriate timing in voluntary release.43
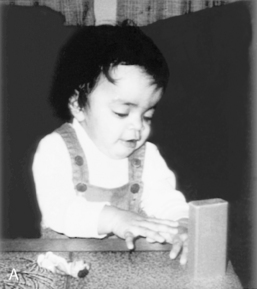

FIGURE 10-11 A, Full finger extension and some wrist movement occur with voluntary release. Note the visual regard of the object being released. B, The child’s shoulder, elbow, and wrist are stable, and less finger extension occurs with release. The child visually monitors release of the object into a small container. C, Stability of the shoulder, elbow, forearm, wrist, and fingers combines with perceptual development to promote accurate placement of objects. This 5-year-old is able to use forearm supination to midposition with controlled finger extension. In this challenging task, only slight overextension of the fingers occurs. (B, Courtesy Kennedy Krieger Institute, Baltimore.)
Bilateral Hand Use
As discussed previously, the normal infant progresses from asymmetry to symmetry to differentiated asymmetrical movements, which are used in bilateral hand activities. Asymmetry is a characteristic of movement patterns until almost 3 months of age. Symmetric patterns predominate between 3 and 10 months of age, when bilateral reach, grasp, and mouthing of the hands and objects are primary activities. Control of these movements originates proximally at the shoulders, allowing the hands to engage at midline. By 9 to 10 months of age, the infant can hold one object in each hand and bang them together (see Figure 10-9). This ability to hold an object in each hand at the same time is critical for further bilateral skill development. By 10 months of age, bimanual action is well differentiated, with one hand grasping the object and the other manipulating parts of it.50 More complex bilateral skills depend on this ability.
Bimanual activity emerges first as reciprocal or alternating hand movements, then as simultaneous hand movements. By 17 to 18 months of age, infants frequently use role-differentiated strategies (i.e., one hand stabilizes or holds the materials and the other manipulates or activates them).113 For these skills to emerge, the infant must be able to dissociate the two sides of the body and begin to use the two hands simultaneously for different functions. Effective stabilization of materials also depends on adequate shoulder, elbow, and wrist stability.
Between 18 and 24 months of age, the child begins to develop skills that are precursors to simultaneous manipulation. Bilateral skill refinement depends heavily on continuing development of reach, grasp, release, and in-hand manipulation skills. Skills in visual-perceptual, cognitive, and motor areas become more integrated, leading to the child’s effective use of motor planning for task performance. The child demonstrates simultaneous manipulation at 2 to 3 years of age. The mature stage of bilateral hand use, which is the ability to use opposing hand and arm movements for highly differentiated activities (e.g., cutting with scissors), begins to emerge at about 2.5 years of age. The child applies and refines the patterns from each stage of bilateral hand use in a variety of activities throughout childhood.
Once a child is able to differentially use the two hands, the task becomes more significant in eliciting the particular strategy to be used to accomplish a task than the particular motor action. For example, Kunde and Weigelt explored the challenge presented by different types of bilateral manipulative tasks.85 They found that when the goal of a manipulative task was to orient two objects similarly, speed and efficiency were better even if arm-hand movements needed to differ to accomplish the task than when objects were to be oriented differently but the movement of the two hands was the same. This supports the concept that the goal of a motor action is more important in selecting a movement strategy than is the ease of the motor action itself.
Ball-Throwing Skills
Ball-throwing skills reflect the child’s ability to use voluntary release skills. In throwing a small ball, the child must sequence and time movements throughout the entire upper extremity. The child must bring the arm into a starting position, then prepare for projection of the ball into space by moving the trunk with the scapulohumeral joint, stabilizing the shoulder while beginning to extend the elbow, stabilizing the elbow while moving the wrist from extension to a neutral position, and simultaneously forcefully extending the fingers and thumb.
Children progress through a series of skill levels before they can smoothly sequence these movements and project the ball to the desired location. By 2 years of age, the child should be able to throw a ball forward and maintain balance so that his or her body does not also move forward.123 At this age the child uses extensor movements to fling the ball but is unable to sustain shoulder flexion during the toss.55 The child can dissociate trunk and arm movement but cannot dissociate humeral and forearm movements. By 2.5 to 3 years of age, the child can aim the ball toward a target and project the ball approximately 3 feet forward. This ability to control the direction of the ball to some degree implies that the child can control the humerus so that the elbow is in front of the shoulder when the ball is released. Thus the shoulder has sufficient stability to support controlled elbow and finger movement. By 3.5 years of age, the child is able to throw the ball 5 to 7 feet toward a target with little deviation from a straight line.55 To accomplish this accuracy, the child positions his or her elbow in front of the shoulder before the ball is released.
Further refinement of ball-throwing skills continues over the next few years. Distance and accuracy improve as the child gains scapulohumeral control, the ability to sustain the humerus above the shoulder, and the ability to control the timing of elbow, wrist, and finger extension. Thus at approximately 5 years of age, the child is able to use an overhand throw to hit a target 5 feet away fairly consistently. Children between 6 and 7 years of age are able to hit a target 12 feet away by using an overhand throw.55 Underhand throws to contact a target are also possible in children 5 years of age or older. This skill requires the ability to move the humerus into flexion while sustaining full external rotation.
Tool Use
Connolly and Dalgleish defined a tool as “a device for working on something … tools serve as extensions of the limbs and enhance the efficiency with which skills are performed” (p. 895).26 They defined tool use as “a purposeful, goal-directed form of complex object manipulation that involves the manipulation of the tool to change the position, condition or action of another object” (p. 895).26 Tool-use skills are more complex than other hand skills, because the child must use a tool, rather than the hand, to act on objects.
The development of skill in using tools is critical to a variety of self-care, play and leisure, and school and work tasks. Skills in tool use for eating and play typically begin to emerge during the second year, after the child has mastered the basic skills of reach, grasp, and release. The skills emerge concurrently with in-hand manipulation skills, which are necessary for the progression of tool use skills beyond grasp and release proficiency. In-hand manipulation skills allow the tool to be adjusted in the hand after it has been grasped.
A key factor in the acquisition of tool-use skills is the high degree of interaction of these skills and cognitive development. Connolly and Dalgleish emphasized that an individual needs to know both what he or she wants to do (the intentional aspect of the task) and how he or she can accomplish it (the operational aspect of the task).26 Both of these elements require development of the child’s cognitive skills and operational aspects of the child’s motor skills.
As with any new skill, when the child is developing tool use, the therapist sees inconsistencies in the child (even in the same session). The therapist is likely to record multiple strategies for children who are beginning to use a particular skill. Thus “inconsistency” in the strategy used to perform a skill should be considered an important stage in the skill-acquisition process. As skill acquisition progresses, practice allows the skill to progress from being performed with a high level of attention to being performed at a more automatic level. With such practice, performance becomes faster, more accurate, and smoother. Practice typically is necessary for a skill to become functional for execution in daily life tasks.
Researchers have studied the acquisition of children’s skills in the use of three tools: drawing and writing, scissoring, and eating. Of these, most of the research has focused on drawing and writing tool use (see Chapter 19 for a description of this type of tool use).
Schneck and Battaglia described the development of scissors skills in young children.120 This skill emerges when the child first learns to place his or her fingers in the holes and to open and close the scissors. Early cutting is actually snipping, a process of closing the scissors on the paper with no movement of the paper and with no ability to repetitively open and close the scissors while flexing the shoulder and extending the elbow to move across the paper. Three-year-old children may use a pronated forearm position or a forearm-in-midposition placement,120 or they may alternate between the two forearm positions. By 4 years of age, children typically hold both forearms in midposition for the cutting activity.
The Peabody Developmental Motor Scales has established the following typical sequence for scissors skills55:
• By 2 years of age, children can snip with scissors.
• By 2.5 years of age, most children can cut across a 6-inch piece of paper.
• By 3 to 3.5 years of age, they can cut on a line that is 6 inches long.
More complex cutting skills develop between 6 and 7 years of age. Other factors the therapist should consider when assessing a child’s skill in cutting include the width of the line to cut on, the size of the paper, the size of the design to be cut, and the complexity of the design.
The child’s grasp on the scissors changes over time. The thumb position in one hole remains consistent, but the finger positions change according to the child’s level of maturation and the type of scissors used.120 In a mature grasp, which may not be achieved until after 6 years of age, the child has the middle finger in the lower hole of the handle, the ulnar two fingers flexed (inside or outside the lower hole, depending on its size), and the index finger positioned to stabilize the lower part of the scissors.102,120
The general ages at which a child learns to use various utensils in eating are as follows: a spoon by 18 months of age, a fork by 2.5 years of age, and a knife by 6 years of age.70 However, documentation regarding how these skills are acquired and how various components of movement interact to produce skill is limited. Connolly and Dalgleish conducted a longitudinal study on development of spoon use skills in infants between 11 and 23 months of age.26 They analyzed videotapes of the infants’ grasp patterns on the spoon; the placement of the spoon in the hand; movements used in filling the spoon, bringing it to the mouth, clearing the spoon, and taking it out of the mouth; and visual monitoring of the pattern, timing, and use of the nonpreferred hand in the eating process. They found that the mean number of grasp patterns decreased between 11 and 17 months of age and that most infants 17 months of age or older showed a clear hand preference for eating. The infants used 10 different grasp patterns, but none of them used an adult pattern. The most commonly used pattern was a transverse palmar grasp with all four fingers flexed around the handle of the spoon. In the next two most commonly used patterns, the spoon handle was held within the fingers rather than in the palm. The 17- to 23-month-old infants used some degree of index finger extension to hold and orient the spoon. The infants became increasingly efficient in spoon use during this period, and exhibited improved visual monitoring of the process.
Another component in the development of tool use in children is the role of the assisting hand. In handwriting and coloring, the assisting hand plays an important role in stabilizing the paper. However, in using scissors and eating, the assisting hand is likely to be much more active. In cutting, this hand must hold the paper and orient it through rotation by moving in the same or the opposite direction as the hand with the scissors. In eating, the child’s assisting hand may be involved in a variety of activities, depending on the child’s age and the utensils used. Connolly and Dalgleish found that infants between 18 and 23 months of age showed significantly more involvement of the assisting hand in stabilizing a dish during spoon feeding than did infants between 12 and 17 months of age.26 Learning to use a knife entails the child learning to stabilize food with a fork in one hand while using a knife for spreading or cutting.
Hand Preference
Hand preference, previously referred to more frequently as hand dominance, is a complex concept. In typical children hand preference evolves over a long period of time and gradually becomes more consistent, as do other expressions of motor functioning. Fagard and Lochman studied young children between the ages of 6 months and 48 months with a variety of tasks involving hand use.51 Greater variability was actually noted for less complex grasp activities. Activities and objects that elicited manipulative strategies were more likely to result in more consistent use of one hand for manipulation and the other for stabilization. Inconsistent use of one hand in a precision grasp task was noted in almost 20% of the infants under 12 months, but in none of the 2.5- to 3-year-old children, whereas about 60% of the children in this age group (and in the infants 6 to 24 months of age) were inconsistent in hand used for a simple grasp task. When one hand needed to be used as a stabilizer and one as a manipulator, 65% or more of the children over 18 months used the right hand as the manipulator. Inconsistency was noted in some children in the 2.5- to 3-year-old group but not in the 4-year-old group. Overall, Fagard and Lochman noted that the right hand was used more frequently than the left hand by infants and young children in every age group, even when it was not used consistently (on 80% or more of the trials).51
Hand preference continues to develop until at least 8 years of age, as illustrated in a study of a reaching activity that involved crossing the midline of the body. Carlier, Doyen, and Lamard found that with increasing age, children used the preferred hand with greater frequency to pick up cards in various locations, including crossing the midline with the preferred hand.18 As with other areas of hand skill development, some degree of variability and inconsistency is the typical pattern for infants and young children. It is worrisome and atypical when infants (less than 7 months) consistently use one hand, and these infants should be further evaluated for possible neurologic impairment.
RELATIONSHIP OF HAND SKILLS TO CHILDREN’S OCCUPATIONS
Hand skills are vital to the child’s interaction with the environment. Engagement in most occupations requires object handling, almost all of which is accomplished with the hands.
Play
Although infants engage with people and objects through their visual and auditory senses, these are distant senses and do not readily bring the infant key information, which can be gained only through touch. Ruff described object handling with visual exploration as essential for an infant to learn object properties.118 The interaction of touching and looking helps enhance the infant’s ability to integrate sensory information and to learn that objects remain the same regardless of visual orientation. Typically this object handling in infants is called play because it is purposeful and done with pleasure.
With increasing age, until at least the early school years, a great deal of play depends on competence in fine motor skills. These skills are reflected in the child’s interest in activities such as cutting with scissors, dressing and undressing dolls, putting puzzles together, constructing with various types of building materials and model sets, participating in sand play, completing craft projects, and engaging in imaginary play with objects. Playing video games and using computers also require fine motor control. Some children may pursue play and leisure activities through organized groups such as the Girl Scouts or Boy Scouts and 4-H clubs, which tend to have projects requiring manual skills as a key component of their programs.
Activities of Daily Living
Activities of daily living also depend on the child’s ability to use all types of hand skills. According to Henderson, the specific skills needed for skill development in this area are “(1) finger manipulation and grip ability, (2) the use of two hands in a complementary fashion, (3) the ability to use the hands in varied positions with and without vision, (4) the execution of increasingly complex action sequences, and (5) the development of automaticity” (p. 213).70 Case-Smith found that in-hand manipulation speed, grasp strength, motor accuracy, and tool handling were each significantly positively correlated with self-care skills in preschool-age children receiving occupational therapy services.21
Dressing skills involve complex grasp patterns and in-hand manipulation skills in the use of fasteners, but the ability to use all types of bilateral skills and a variety of grasp patterns is useful for putting on and removing shirts, shoes, socks, and pants. The ability to put on jewelry relies on the ability to use delicate grasp patterns and in-hand manipulation.
Bathing, showering, and other personal hygiene skills depend on the child’s increasing fine motor skills in handling slippery objects (e.g., soap). In addition, these skills are likely to be needed when an individual is in a standing position, such as when putting toothpaste on a toothbrush (Figure 10-12), brushing the teeth, shaving, or applying makeup. A high level of skill in tool use is needed for complex hygiene activities such as shaving, applying makeup, using tweezers, cutting nails, and styling hair (applying barrettes or rubber bands and using a curling iron, a brush, and a hair dryer).
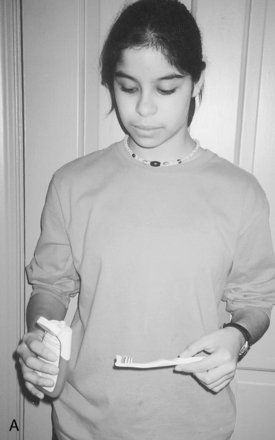
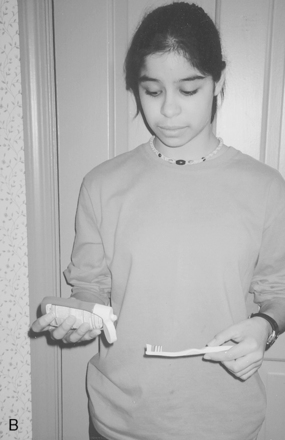
FIGURE 10-12 A, Different grasp patterns are used in preparation for putting toothpaste on a toothbrush. The child uses just-right force to stabilize the toothbrush with a modified power grasp (with supination to midposition) while using a cylindrical grasp on the toothpaste container. B, The child has used forearm supination and the in-hand manipulation skill of simple rotation to position the toothpaste container for application of the toothpaste to the toothbrush.
Eating skills rely on refinement of the ability to use forearm control with a variety of grasp patterns and tools. The ability to use both hands together effectively is necessary for spreading and cutting with a knife, opening all types of containers, pouring liquids, and preparing food. In-hand manipulation skills are used to adjust eating utensils within the hand (Figure 10-13) and finger foods in the hand, to handle a napkin, and to manipulate the opening of packaged food and utensils.
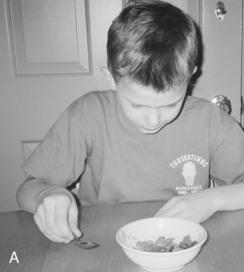
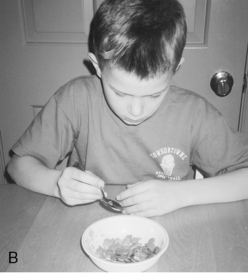
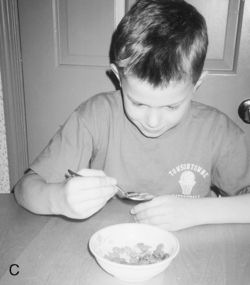
FIGURE 10-13 A, The child grasps the spoon from the table surface with a radial-digital grasp. The forearm is slightly supinated. B, He uses the in-hand manipulation skill of complex rotation to move the handle of the spoon from the palmar surface of his hand toward the web space between the index finger and thumb. Isolation and differentiation of the index finger and thumb are needed to produce this rotation. Forearm movement toward midposition assists. C, The child completes spoon positioning in his hand by moving the spoon so that the end of the handle is stabilized in the web space. Additional flexion of the metacarpophalangeal (MCP) joints of the fingers while extension of the interphalangeal (IP) joints is sustained assists with optimal positioning for eating.
In their studies of school-age children with developmental coordination disorder (DCD), Summers, Dawne, and Dewey133 and Missiuna, Moll, King, King, and Law99 illustrate the impact of hand skills on activities of daily living. Typically developing children 8 years of age and older are highly independent in an array of skills that rely on hand skill as well as postural control. In contrast, children with DCD demonstrated delayed development in dressing, personal hygiene, toileting, and independent eating skills. Older children who had DCD performed similarly to younger typical children. Parents provided cues, assistance, and substitutions for many of the needed skills far longer for their children with DCD than did parents of typically developing children.99,133
School Functions
Independent functioning in the school environment requires effective fine motor skills. The preschool classroom provides children with a variety of manipulative activities, including the use of crayons, scissors, small building materials, and puzzles, as well as simple cooking and art projects. During kindergarten and the early elementary school years, children use fine motor skills most of the school day. McHale and Cermak found that 45 to 55% of the school day for first and second grade children is spent in fine motor activities. Fourth grade children spend approximately 30% of their school day participating in fine motor tasks.94 The primary fine motor activities in all of these grades are paper-pencil tasks. Any writing activity includes preparing one’s paper, using an eraser, and getting writing tools in and out of a box. Other typical fine motor activities in children’s classrooms include cutting with scissors, folding paper, using paste and tape, carrying out simple science projects, assuming responsibility for managing one’s own snack and lunch items, and organizing and maintaining one’s desk. Children also need computer skills in most elementary classrooms.
Older children and adolescents need fine motor skills for science projects, vocational courses (e.g., woodworking, metal shop, and home economics), art classes, music classes (other than vocal music), managing a high volume of written work and notebooks, keyboarding, and maintaining a locker. Greater speed (e.g., in writing and keyboarding) and greater strength (e.g., for physical education and vocational courses) are required. Adolescents should be able to demonstrate consistent hand skills that they can execute quickly in a variety of situations.
GENERAL MOTOR PROBLEMS THAT AFFECT HAND SKILLS
Children with a wide variety of types of disabilities are likely to have difficulty with hand function. These disabilities include cerebral palsy,52,66 DCD,92 attention deficit–hyperactivity disorder (ADHD),115 and mental retardation and epilepsy.9 As Mandich et al. noted, “Incompetence in everyday activities [has] serious negative effects for the children” (p. 583).92
Regardless of the nature of a specific disability, the affected child is likely to have impaired hand skills. Impairment of basic hand function (reach, grasp, carry, and release) in early childhood precludes emergence of more advanced hand skill and bilateral hand use. This section presents problems that may be observed as major or minor in any child with hand skill difficulties.
One of the more common problems is inadequate isolation of movements. Children who demonstrate significant problems in this area tend to use total patterns of flexion or extension throughout the upper extremities, and they are unable to combine wrist extension with finger flexion or elbow flexion with finger extension. Similarly, the child may be unable to perform differentiated motions with each arm and hand. More subtle problems may be seen in children who have difficulty isolating wrist and finger movements.
Another common problem is poorly graded movement, which may refer to movements not effectively graded in terms of range or strength. Eliasson and Gordon use the term poor force scaling to refer to difficulties in appropriately adjusting the force needed for grasp or release.43 When joint stability in the hand or proximal to the hand is not effective, the child may be unable to hold the elbow in approximately 90° of flexion and the wrist in neutral position during a grasp activity. Thus, when initiating the grasp, the child may overflex the fingers in an attempt to obtain the object before the arm posture is lost. Another common pattern is difficulty shaping the hand in accordance with the object’s properties prior to grasp.83
Children with poorly graded movements lack the ability to use the middle ranges of movement effectively; instead, during attempts at hand use they hold one or more joints in a locked position of full flexion or full extension (Figure 10-14, A). Typical patterns that children use to increase their stability include internal rotation of the shoulder, elbow extension, and hyperextension and/or abduction of the MCP joints (Figure 10-14, B). Problems with grading of movement are typically associated with tactile sensory problems, abnormal tone, and/or muscle weakness. The child with sensory problems has difficulty perceiving and evaluating feedback and therefore cannot accurately plan the extent of movements or force needed for a task. Gordon and Duff found that “spasticity may limit the ability to finely grade the fingertip force to the object’s properties” (p. 590).64


FIGURE 10-14 A, This child, who has involuntary movement, demonstrates the attempt to find stability by locking her left elbow with the arm in extension and by elevating her right shoulder during hand use. She also has difficulty isolating upper extremity movements and using the two hands together at midline. B, During voluntary release this child shows overextension and increased abduction of the fingers, with hyperextension at the MCP joints of the ulnar fingers. He also shows adduction of the thumb rather than slight abduction. (A, Courtesy Kennedy Krieger Institute, Baltimore, MD.)
Insufficient force may interfere with grasp control. Problems with force have been noted in children with developmental coordination disorder148 and in children with cerebral palsy.64 Difficulties with regulation of force may be due to poor tactile discrimination and/or spasticity.64 Muscle weakness has also been suggested as a problem for individuals with cerebral palsy31; weakness could contribute significantly to insufficient force.
Poor timing of movements can also be a problem. Improper timing of muscle contractions leads to the use of movements that are too fast or too slow for the intended purpose. Movements that are too fast also tend to be poorly graded. Eliasson and Gordon describe difficulties in children with spastic hemiplegic cerebral palsy relative to the timing of “transitions between phases [and] sequential generation of forces” (p. 228) as needed for grasp and release of objects.43 During voluntary release, children with increased tone are likely to place an object very quickly and then have slowed movement of the fingers away from the object.43 Similarly, Kuhtz-Buschbeck et al. documented that children with traumatic brain injury also had impaired reaction times and slower movements when performing a task involving the combination of reach and grasp.83 Wilson et al. similarly reported difficulties with timing of movements in children with DCD.148 Tone problems or muscle weakness are often the underlying factors in movement that is too slow. Poor coordination of agonistic and antagonistic muscles and poor tactile discrimination are likely to be key factors in impaired timing of actions.43 Speed and accuracy demands, particularly when these skills are required to place an object on an unstable surface, lead to increased difficulty with motor timing and regulation of force.63 Instability at joints can contribute to disordered sequences of hand and arm movements. For example, wrist extension may not be combined with the reach for an object but instead may occur after the grasp.
Another common motor problem is limited variety of movement patterns—a restricted repertoire often associated with biomechanical or neurologic issues affecting movement range and/or coordination. Other children may have marked variability in movement patterns83 that result in substantial inefficiency of movement.
A fifth type of problem that affects hand function is a disorder in bilateral integration of movements. Some children are unable to bring both hands to midline effectively or to maintain the use of both hands at midline long enough to accomplish a task. Other children can hold objects symmetrically at midline but are unable to dissociate arm movements; they therefore have difficulty with activities that require reciprocal or simultaneous bilateral hand use.
Many children have difficulty with hand use because of limitations in trunk movement and control. CNS dysfunction or generalized muscle weakness can impair development or effective use of equilibrium reactions. Therefore the child may use one or both arms for support in maintaining sitting or standing positions. This significantly limits bilateral hand use and may limit the development of fine motor skills in the hand that the child most often uses for support.
Children with trunk instability or abnormal posture have difficulty with smooth, accurate placement of the hand and arm being used for a fine motor task. When the trunk is postured in flexion, functional ROM in the arm is limited (Figure 10-15). Conversely, arching of the trunk is accompanied by hyperextension of the humerus. The latter pattern typically causes one of three patterns of shoulder and elbow positioning: external rotation with elbow flexion, neutral rotation with elbow flexion, or internal rotation with elbow extension. Posturing in any of these arm patterns affects the development of hand skills. Similarly, lateral trunk flexion causes the child to lean to one side and thus affects the child’s ability to use the arm on the flexed side.
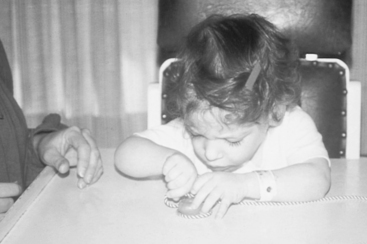
FIGURE 10-15 Poor trunk stability affects the upper extremity range of motion that this child can use. Note the right forearm pronation and wrist flexion. The child is unable to use a three-jaw chuck, or pincer, grasp effectively on the materials. However, she demonstrates awareness of the need to use both hands in this manipulative activity and good visual monitoring of the materials. (Courtesy Kennedy Krieger Institute, Baltimore, MD.)
The problems discussed in this section can contribute to the child’s use of compensatory patterns of movement. In an effort to increase function, the child seeks another pattern to substitute for movements impaired by the primary problem. For example, the child with weakness or instability may learn to use lateral trunk flexion to increase the height of the opposite arm during reach, or a child with increased tone may compensate for limited finger extension by using a wrist tenodesis (flexion) action. Although these patterns are functional for certain tasks, continued use of compensatory movements may hinder the development of higher level skills.
OTHER FACTORS THAT AFFECT HAND SKILLS IN CHILDREN WITH DISABILITIES
Somatosensory problems can produce significant problems with hand function, even when motor control is good,106 and poor hand skills can contribute to the child obtaining a limited amount of somatosensory information. Children with poor tactile discrimination receive less feedback about how their fingers move together and independently of one another. In addition, poor tactile discrimination has been found to be associated with difficulty anticipating the force needed in grasp, modulating the force needed for grasp, and transitioning from grasp to lift.64
Children with cerebral palsy are very likely to have tactile discrimination problems as well as motor control problems. Several studies of tactile dysfunction in children with cerebral palsy were conducted in the 1950s and 1960s. These studies verified the presence of a variety of tactile discrimination problems in the hands of a high percentage of children with this disorder.80,101,139 Recent studies of children with spastic hemiplegia have resulted in similar findings. Cooper, Majnemer, Rosenblatt, and Birnbaum found that eight of the nine children with spastic hemiplegia whom they tested had bilateral sensory deficits.27 Yekutiel, Jariwala, and Stretch found that 51% of the 55 children with cerebral palsy whom they tested had sensory deficits on two-point discrimination and/or stereognosis.152 In a study of 25 children with spastic hemiplegia, Krumlinde-Sundholm and Eliasson found that 18 had impairment of the hemiplegic hand in two-point discrimination at 3 mm and more than half had difficulty with two-point discrimination at 7 mm.83 For approximately one third of these children, tactile problems were noted in all five tests of tactile discrimination in the hemiplegic hand. A marked difference in stereognosis was seen between testing with common objects (11 children showed impairment) and testing with flat shapes (24 showed impairment). Arnould, Penta, and Thonnard also found deficits in stereognosis, proprioception, and perception of touch pressure in a large sample (approximately 100) of school-age and young adolescent children with cerebral palsy.2 Some researchers have found that children with hemiplegia have deficits in the less (or non) involved upper extremity as well as the hemiplegic hand.27
Although some researchers note that the degree of tactile problems is not always associated with the degree of motor impairment,2,27 Krumlinde-Sundholm and Eliasson found strong relationships between impairment in sensation and dexterity in the more impaired hand of children with spastic hemiplegia (i.e., r = 0.60 to 0.71).82 They noted that bilateral hand skills were less associated with the level of tactile discrimination. Differences in these study findings may be associated with differences in tactile testing methodologies and sample sizes. Children with cerebral palsy tend to need more trials than nondisabled children to match tactile and proprioceptive information with force for grasp and lift of objects.39
The use of sensory information about objects to plan movements also appears to be impaired in children with cerebral palsy, thus affecting their skill in object handling. In their study of children with cerebral palsy, Gordon et al. found that when children used their hand with motor impairment they did not effectively plan initiation of grasp with well-controlled finger spacing for the object (“anticipatory control”) relative to object weight, despite experience with the objects in the task.61 Of interest, however, is that when grasping objects with the other hand, they appeared to reflect knowledge of object weight that was learned by grasping with the involved hand. Thus, Gordon et al. stated that “the findings suggest that the impaired anticipatory control may be due to an inability to integrate the sensory information with the motor command in the involved hand… and that intact sensory information alone is not enough for anticipatory control, but instead it must be integrated with motor-related information” (p. 590).61
Children with milder problems also are at risk for somatosensory problems that affect hand skills. Case-Smith studied the relationship between both tactile hypersensitivity and tactile discrimination and in-hand manipulation skills in 50 children between 4 and 6 years of age.19 In this sample, which included 80% typical children, those having problems with either tactile defensiveness or decreased tactile discrimination showed no significant problems with performing the in-hand manipulation tasks presented. However, those who had both tactile discrimination problems and hypersensitivity had difficulty performing the in-hand manipulation tasks that were timed. Their performances were significantly less efficient than those of the children in the other groups.
Strategies and plans of action rely on knowledge of object properties that probably is gained through tactile and proprioceptive information. Children with DCD appear to have tactile problems, because they have difficulty with feed-forward strategies127 and with planning for intentional actions that depend on the anticipation of force and timing.148 Similarly Smyth and Mason found proprioception problems in a variety of tasks in children with DCD.128
Learned Nonuse Phenomenon in Children with Hemiplegia
Sterr, Freivogel, and Schmalohr conducted a study to assess available use in the more involved arm-hand of a sample of 21 children, adolescents, and young adults with hemiplegia.131 Their research was based on several other studies with adults with learned nonuse as a result of strokes. They found that “the learned nonuse model predicts that even if the residual movement capacities of the hemiparetic arm should allow the person to carry out activities of daily living … that arm is not, in fact, used in the real-life situation” (p. 1727).131 The difference between these individuals’ available movement skills and the use of them in spontaneous situations was significant. The authors concluded that the limited use of the hemiplegic arm appeared to be due to learned nonuse.
Hand Skill Problems in Children and Adolescents with Various Developmental Difficulties
Children with a wide variety of developmental problems show significant difficulties in hand skills. Common developmental conditions that are reported to result in hand skill or fine motor problems include visual impairment/blindness, ADHD, autism spectrum disorders (ASD), and DCD.
Hand skill problems that reflect motor coordination difficulties have been identified in children with ASD58,116,146 and with ADHD.54,58,116 In a number of studies, the problems with motor coordination have been particularly linked to either the inattentive type of ADHD54 or the combined type (both inattention and hyperactivity)115; less correlation has been documented with children who have ADHD-hyperactive type alone. Overall, problems with hand skills have been documented in these diagnostic categories in both large- and small-scale studies across a variety of ages of children, with a variety of test instruments. These problems have been corroborated by parent and teacher reports and reflect evidence for persistent coordination difficulties beyond childhood.54
A study by Meyer and Sagvolden clarified the types of hand skill problems that may be noted in children with ADHD.99 They compared typical South African children with a similar sample of children with ADHD relative to their skills in performing three fine motor tasks involving tool use, object manipulation, and finger tapping. Although the two groups did not differ on the repetitive tapping item, the children with ADHD were significantly slower and less accurate in performance on the more complex items involving object control. Children at the younger ages (6 to 9 years versus 10 to 13 years) appeared to have greater differences in the object manipulation task relative to their typical age-peers, but this may have been due to a ceiling effect on the measure used. The authors concluded that the combination of speed with demand for eye-hand coordination is very difficult for children with both hyperactivity and inattentiveness.
In clinical practice children with autism may be assumed to either not have specific hand skills problems112 or have hand skill problems due to sensory avoidance of certain textures or materials or due to a limited repertoire of interests, which may interfere with the range and type of object manipulation activities. Some toddlers with autism have poorer fine motor skills than gross motor skills, but others may have similar performance in the two areas or poorer gross motor skills; all had at least some delay in motor skills.112 Within the area of fine motor skills, the most common pattern identified was a delay in visual-motor integration and handling of objects.
In recent years, significant attention has been given to documenting the characteristics of children with developmental coordination disorder and to attempting to determine similarities and differences in the fine motor difficulties these children have relative to children with ASD150 and ADHD.115 Flapper, Houwen, and Schoemaker found that approximately 60% of a sample of children with DCD had attention deficit disorders.53 In a subset of 12 of the children they studied, the children differed significantly from typical children on the manual dexterity section of the Movement Assessment for Children, with 9 of the children having notable fine motor problems and 2 others having borderline performance. Their problems were reflected in increased errors and slower speed of performance. Piek et al. noted that attention difficulties may cause motor performance to be more variable, whereas difficulties with motor skill interfered with performance speed.110 One of the difficulties with motor skill may be related to poor control of force and torque using the finger tips.104 The component of rotation/movement was more impaired in 7-, 9-, and 11-year-old children than was the component of pressure alone. Overall the typical 7-year-old children and the 9-year-olds with DCD had similar scores on the torque measure, while the force measure showed about a 1-year delay. The authors note that “impairments of torque control in children with DCD may result in a greater challenge in daily manipulative tasks” (p. 45)104 because of the number of different digits that need to be controlled with relative force.
Differences in Developmental Trends between Children with and without Disabilities
Although information about normal development of hand skills can be useful to therapists in understanding difficulties with functioning and/or in guiding intervention planning, therapists also need to recognize that normal developmental sequences may not apply to children with some types of disabilities. For example, in a longitudinal study by Hanna et al., hand function in children with cerebral palsy generally improved in early childhood and then began to decline.66 They found somewhat different patterns of development with children who had mild, moderate, and severe impairments and for children with hemiplegic cerebral palsy and with quadriplegic cerebral palsy. Hand skills increased more slowly in children with greater degrees of motor impairment. In general, the children with quadriplegic cerebral palsy showed more decrease in quality of functioning over time than did the children with hemiplegia. Overall the highest quality of functioning was found at the average age of 46 months, and the highest scores on the PDMS Fine Motor Scale were achieved at approximately 5 years of age.
Eliasson et al. also found a longer course of development of hand skills, but did not identify deterioration in the skills they tested over time.42 The children with cerebral palsy in their study were initially tested when they were between 6 and 8 years of age and retested 13 years later, assessing their hand skill dexterity and their ability to time finger movements for grasp and use a direct approach for grasp of objects. Overall they became faster in object manipulation both as measured on a standardized test and on a task involving grasp and lift. Thus, the children demonstrated increases in motor skill, including greater speed and increased consistency in movement, but appeared to have a longer course of development than in typical children (Research Note 10-1). The differences in findings between Hanna et al.66 and Eliasson et al.42 may be related to use of different measures of hand function as well as different samples of children and may be influenced by intervention.
Similarly, it should be noted that individuals with DCD and other hand skill problems may continue to improve in performance over time, but problems with coordination persist that affect interactions with peers and have a negative impact on the children’s emotional well-being.99 The time demands associated with slower performance or inability to accomplish tasks can make it extremely difficult or impossible to effectively engage in academic work.99 Such problems with hand skill use for complex tasks are reported to persist at least through adolescence.54
EVALUATION OF HAND SKILLS IN CHILDREN
The occupational therapist evaluates a child’s hand skills when the evidence is sufficient to suggest that problems with performance of occupational skills are at least partly attributable to the child’s problems with hand skills. A hand skill evaluation should not be performed simply to obtain information about the child’s fine motor skills. The therapist first must have evidence suggesting that the child has a problem in at least one area of occupational performance. Parents, teachers, and the child often are the best sources of information about difficulties with participation in the family and the community, and this information can be obtained through the development of an occupational profile. See Chapter 7 for additional information on how to obtain an occupational profile.
Screening for Hand Skill Problems
When a problem with occupational performance has been identified, the therapist needs to continue gathering information on the child’s performance of specific daily life activities. As part of this process, the therapist determines whether it is reasonable to carry out a full evaluation of fine motor and hand skill performance. This information must include data about the child’s age and general information about motor skills, cognitive and perceptual skills, sensory processing, social situation and skills, and emotional functioning, as well as contexts that affect the child. The therapist can obtain screening information from parents, teachers, the child, and other professionals or from reports of other professionals.
Observation of the skills noted in Table 10-1 can help determine what standardized test and further analysis should be pursued. These observations about the child’s quality of hand skills can supplement a standardized test. Some skills are inappropriate for younger children; an “X” designates the age group for which any activity may be used. When a skill emerges within a particular age group, ages are listed rather than an “X.” For block stacking, the number represents the number of blocks a child in that age group should be able to stack. The therapist can vary the materials used for some of the items so that he or she can assess many of these skills during mealtime, dressing, hygiene, or play activity. For all categories, except Bilateral Skills and Tool Use, the therapist should ask the child to perform the activities with both the right hand and with the left hand. Evaluation of both hands is important, because subtle difficulties may not be readily apparent. For example, Gordon, Lewis, Eliasson, and Duff found mild problems in the timing of voluntary release components in the noninvolved hand of children with hemiplegia.63
TABLE 10-1
Screening Activities for Hand Skills
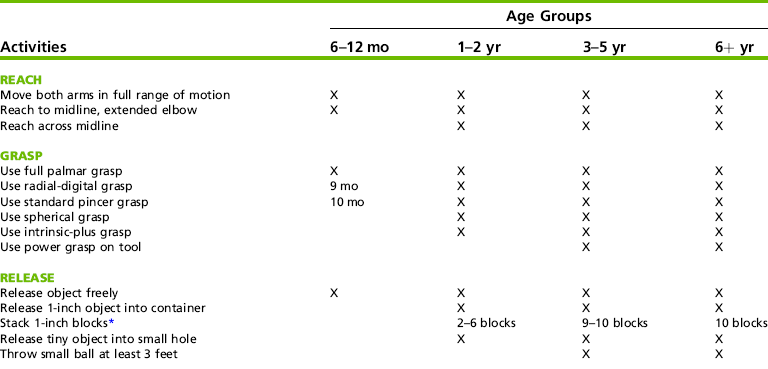
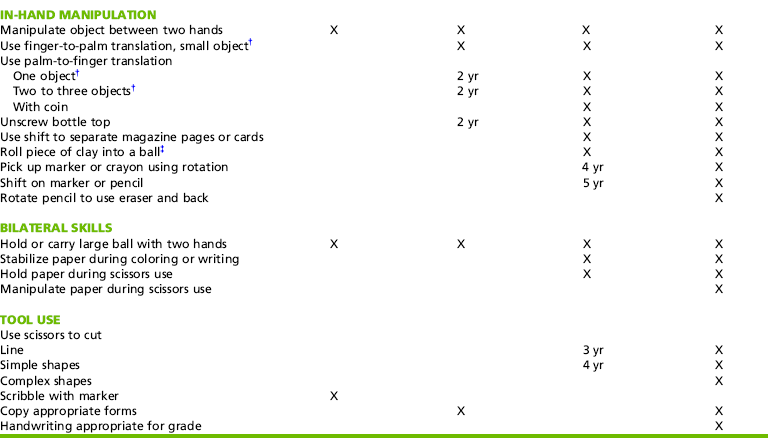
*Block stacking allows for assessment of arm stability in space, spatial orientation of the objects, and controlled finger extension. Voluntary release of objects other than blocks may be used. Screening should include placement of objects when arm is not supported and placement that requires precision.
†An object that is not flat should be used, such as small pieces of cereal (appropriate for children younger than 3 years or those who still mouth objects), small beads, or small pegs.
‡A piece of clay approximately 1/4 inch thick and 1 inch in diameter is placed in the palm of the child’s hand. The child is asked to form the clay into a ball without using the other hand or the table surface. Palm-to-finger translation, finger-to-palm translation, simple rotation, and sometimes complex rotation may be observed.
Evaluation Content
A child with occupational performance problems who shows difficulties on screening for hand skills should be further evaluated so that the characteristics of the problem and the situations in which the child’s performance is optimal can be carefully delineated. When determining the child’s performance in the area of hand skills and potential reasons for any problems, the occupational therapist often uses a variety of standardized and nonstandardized assessments. All children should receive an assessment of hand skills in activities such as dressing, eating, hygiene skills, school activities, and play activities. Completion of a parent interview is helpful in determining persistent concerns and priorities. Wilson, Kaplan, Crawford, Campbell, and Dewey have developed a Developmental Coordination Disorder Questionnaire for parents.147
Analysis of the identified hand skills problem involves administration of specific assessments or scales that define the basis of the problem and the extent of the impairment. A sample analysis of an occupational performance problem in the area of constructive play that is at least partly caused by hand skill difficulties is presented in Box 10-2. In this example the therapist has identified two main performance problems: lack of ability to manipulate materials after grasp and breakage of materials being handled (“manipulates” and “calibrates”1). The therapist then attempts to determine how sensory functions, neuromusculoskeletal and movement-related functions, and mental functions contribute to this performance limitation. Muscle and movement functions associated with this problem may include difficulties with wrist and MCP joint stability, limited midrange movement control, lack of isolated finger movement, and excessive use of flexion. Based on evaluation findings and the therapist’s frames of reference, specific impairments are identified.
The following outline presents examples of tools and methods used in comprehensive evaluation to assess the underlying impairments associated with hand skill difficulties and delays.
1. Measurement of active and passive ROM (especially important for children who have weakness or increased muscle tone)
3. Evaluation of tactile functioning using standard assessment of tactile discrimination or two-point discrimination and finger identification with vision occluded
4. Assessment of postural alignment and postural stability, including stability and mobility of the hand
5. Administration of a standardized general developmental test that includes a fine motor section for young children (see Appendix 7-A)
• Hawaii Early Learning Profile (HELP)
• Bayley Scales of Infant and Toddler Development (3rd Ed.): Motor Scale
6. Administration of a developmental motor test
7. Administration of a test of fine motor skills for older children and adolescents
• Movement Assessment Battery for Children
• The Melbourne Assessment of Unilateral Upper Limb Function
8. Classification of manual skills to document outcomes
9. Administration of a visual-motor integration test
10. Assessment of hand skills in prevocational or work tasks (important for adolescents)
GUIDELINES FOR INTERVENTION
Several factors affect the types of goals developed in the area of hand skills and in other areas of the child’s functioning: the child’s occupational performance problems, the contexts in which the skills are needed, the types of problems in the hand skill area, the therapist’s frame of reference, and the setting in which services are to be provided. For some children, developmental sequences of skills influence the selection of goals, but for the child with a motor disability, other factors will affect the goals established and the strategies selected for intervention. These factors include the types of occupational performance skills the child needs, the complexity and severity of the child’s problems, and the human and nonhuman resources available to support the intervention program.
A child’s goals generally are developed through a process of child/adolescent, family, and professional collaboration. The Perceived Efficacy and Goal Setting System100 is helpful in setting goals with children who are functioning at approximately the 6- to 9-year-old level.
Overall, the therapist must be realistic in the number and types of goals to recommend relative to other goals for the child. In addition, the therapist must consider hand skill goals that are feasible for the child to accomplish. Such goals may be limited for children with severe disabilities. In all cases the therapist must link hand skill goals to the child’s ability to engage in occupational activities more effectively. For some children the most appropriate focus of intervention is the development of skills in using adaptive equipment and strategies for accomplishing skills needed in activities of daily living. For children who show readiness to develop better quality or more complex hand skills, intervention can focus on acquisition of these skills. Factors to consider in planning intervention for hand skills problems are discussed in the following sections.
Considering Roles of the Occupational Therapy Assistant and Others in Intervention
Clearly the occupational therapist has a key role in evaluation, goal setting, and intervention planning for a child or adolescent with hand skill problems that are affecting functioning in daily life skills. However, others have a significant role as well. Typically not only is a parent/caregiver and/or a teacher involved in noting concerns relative to hand skills, but the child or adolescent, parent/caregiver, and other professionals need to identify their roles relative to intervention. In addition to parents/caregivers, teachers often have a key role. In fact, in some schools, the occupational therapist has predominantly a consultant role and the teacher is the primary interventionist.8 However, although teachers indicate a high level of receptivity to input and recommendations from the occupational therapist in helping children with hand skill difficulties, they may have limited knowledge of the role of the occupational therapist76 and/or want a higher level of input than periodic consultation for these children.8
In general, teachers and parents/caregivers can be provided with specific activities (classroom or games or selected tasks that work well within daily living skills) that allow for repetition of skills that the child or adolescent is able to show with simple cuing or with particular materials. Thus, it is preferable for the occupational therapist to provide activities that allow for practice of skills, but not to expect these individuals to determine how to vary or adapt an activity to elicit a better response from the child or adolescent.
The occupational therapist and the occupational therapy assistant can be an excellent team in providing both direct and consultative intervention in the area of hand skills. When a child has complex problems and/or is highly inconsistent in performance, intervention by the occupational therapist who is continually assessing and modifying the intervention strategies is generally preferable. When a child has less variability or when the child is ready to make incremental gains in motor skills or to use motor skills within graded functional activities, often the occupational therapy assistant can provide highly appropriate intervention with grading of activities in response to changes in child performance.
Sequencing of Intervention Sessions
When the therapist provides direct services to improve hand and arm function, he or she usually carries out in the following sequence:
• Promoting isolated arm and hand movements, such as external rotation, supination, and wrist extension
• Enhancing reach, grasp, carry, and release skills
• Enhancing in-hand manipulation skills
• Facilitating bilateral hand use skills
• Generalizing skills (integration of hand skills into functional activities)
Not all children need all the steps in this sequence. In addition, intervention for all areas is rarely done in one session.
Preparation for Hand Skill Development
Many children require preparation of the total body in each treatment session before the therapist can begin intervention for specific hand skill problems. In addition to intervention to improve motor function, the therapist should pay specific attention to the child’s sensory functioning. The therapist can provide tactile and proprioceptive input to the arms and hands to enhance sensory awareness and discrimination. Lotion, toys, the child’s own clothing or, preferably, active movements of the child’s hands, with or without assistance, can provide stimuli. Children have greater tactile sensitivity when performing an activity that involves active touching rather than being touched.67 The therapist should also encourage visual awareness of the hands with tactile and proprioceptive input.
Positioning the Child
In selecting the positioning of the therapist and the child for fine motor intervention, the therapist must consider the optimal position for eliciting the particular skills desired in that child and the position in which the child will use the skills. When these positions are different, the therapist must consider whether to use only one position at this time and introduce the other position later or to use both positions concurrently. For example, the child may be able to bring both hands to midline and to reach with the greatest elbow extension in the side-lying position. However, for functional use the child may need to be able to contact a switch on a surface while in an adapted sitting position. In an intervention session the therapist initially may work with the child in the side-lying position, then move to a supported sitting position to help the child generalize the skills to a functional position. Eventually the therapist may work with the child primarily in a supported sitting position. The therapist almost always needs to specifically address carryover of skills across positions with the child, often through activities developed collaboratively with the parents or the teacher.
The therapist can use certain body positions to elicit specific hand skills. The supine position is effective for working with children on arm movements and visual regard of the hands during movement. The prone position on the forearms is appropriate for addressing shoulder stability and co-contraction in 90-degree elbow flexion, dissociation of the two sides of the body during weight bearing on one arm while manipulating with the other, gross bilateral manipulation of objects, and visual regard of the hands. Side-lying can be an effective position for encouraging unilateral arm movement to bat at an object and for hand-to-hand play. Visual regard of the hands and objects is difficult to address in the side-lying position.
Sitting at a table is often the position in which children are most likely to use fine motor skills. For optimal hand use, children need a stable chair with adequate foot support. Even young children without motor disabilities benefit from sitting in furniture that fits appropriately. Smith-Zuzovsky and Exner found that typical young children had significantly better in-hand manipulation skills when seated in chairs and at a table fitted to them (Figure 10-16) than when seated in chairs and at a table that were slightly too large.125 These workers suggest that appropriately fitted furniture may enhance hand function by means of its effect on proximal stability and/or by allowing the child to focus more on the manipulative tasks and less on postural readjustments. A study by Wingrat and Exner supported the theory that classroom chair size affects posture and attention.149 They found that typical young children’s sitting posture and on-task classroom behaviors were enhanced when they were in chairs appropriate to their size compared with their performance when seated in standard but slightly too large classroom chairs.

FIGURE 10-16 This child is seated at a table that is an appropriate height for tabletop activities. She can effectively place her arms on the surface without elevating her shoulders. Arm support on the surface, elbow flexion, and handing her the candles in a vertical position rather than having her grasp them from a table surface encourages the child’s use of forearm supination and fingertip control during grasp and placement of the candles on the clay birthday cake. (Courtesy Kanji Takeno, Towson University.)
For children with disabilities, seated positioning for hand function activities requires specific attention. The therapist should not expect a child who cannot yet sit independently to work on sitting stability while working on hand skills. Such children need adaptations for sitting (e.g., lateral supports and chest straps) when working on hand skills. A tray or table surface should be a work surface rather than a support surface. The table or tray should be only slightly above elbow height, because a lower table promotes use of body flexion and a higher surface promotes use of abduction and internal rotation of the arms. The therapist also may provide activities with the child sitting on the floor or in a chair without a table, particularly when working on reaching skills or gross bilateral skills. Enhancement of hand function based on body position was illustrated in the study by Savalsbergh and colleagues. Their study of ball catching in 9- and 10-year-old children illustrated the significantly greater difficulty exhibited by less skilled children when they were standing than when they were sitting. Children who had good catching skills were not affected by the change in body position, thus illustrating their ability to combine a greater postural challenge with timed arm-hand movements.
For children with mild to moderate motor involvement, standing may be an appropriate position for treatment of some hand skills. Many daily living skills that rely on hand skills are most commonly done while standing, such as brushing the teeth, zipping and buttoning clothing, shaving, applying makeup, and cooking. For children who have substantial difficulties with standing, the therapist should use this position only after the child has mastered the skills in a sitting position.
Improving Postural Tone and Control
The child with increased tone throughout the body may need overall inhibition of tone before participating in hand skill activities. Slow rotary movements using small ranges of motion between internal and external shoulder rotation and between forearm pronation and supination can help inhibit tone. Upper extremity weight bearing is particularly useful as a treatment technique for improving postural control and improving stability in the scapulohumeral area. The therapist can also use upper extremity weight bearing to encourage the child to maintain elbow co-contraction and some degree of wrist extension while engaging in slight weight shifting.12,32 The therapist provides proprioceptive input during weight bearing. For most children the primary focus is on helping the child increase overall stability rather than concentrating on achieving full elbow, wrist, or finger extension. The therapist can carry out weight-bearing activities with the child in the prone position on the forearms, the prone position on extended arms, the side-sitting position, or the long-sitting position, depending on the child’s skill level.12
For the child who has tightness in wrist flexion, a position of upper extremity weight bearing on hands with the arms extended often is difficult, if not impossible, to achieve. The most appropriate positions for these children to use for weight bearing include prone on the forearms and side-lying. The therapist can help the child position the wrists in neutral position, and some therapists use splints during weight bearing to assist with wrist and hand positioning.81
Finger flexion is permitted during weight bearing as long as the thumb is not in an abnormal position. If the child’s thumb is tightly adducted and flexed, the therapist should use handling techniques before weight bearing. The therapist can use his or her own hand to provide firm pressure over the first metacarpal joint and relax the child’s hand through slow, small, rotary, and flexion-extension movements. Children with mildly and moderately increased tone often can work toward maintaining full finger extension during weight bearing.
Using a multiple-baseline single-subject design, Barnes found that children with cerebral palsy demonstrated increased use of wrist extension and finger extension after upper extremity weight bearing.5–7 The weight bearing increased wrist extension during these activities but did not affect grasp and voluntary release quality and skill. Kinghorn and Roberts, who conducted a single-subject study of weight bearing with splinting for a child with cerebral palsy, did not find significant changes in objective measures of tone, positioning, or function.81 However, family members reported improved functioning.
Improving Muscle Strength
Interventions to increase strength may improve skilled hand use in children with certain disabilities. Focus on strength needs to be addressed carefully in children with tone problems, because a primary focus on strength would diminish focus on coordination, which seems to be the primary problem in these children. Damiano and Abel reported on the use of strength training to support functioning in children with cerebral palsy.31 They researched strengthening for walking and found that the children they assessed had marked muscle weakness. With a controlled program of strengthening, the children’s strength improved, as did the quality of some components of walking. However, caution is required in applying these results to hand skills, because strengthening programs to enhance arm and hand function of children with cerebral palsy have not yet been researched.
In another study that focused on strengthening, Weaver, Gardner, Triolo, and Betz used neuromuscular electrical stimulation (NMES) with toddlers who had arthrogryposis that significantly affected their arm and finger strength and movement.143 The NMES resulted in several positive changes in functions of the fingers, including greater ROM at the various finger joints. Associated changes in the developmental level of the children’s grasp patterns occurred as well, resulting in the use of a more radial and distal grasp rather than an ulnar-palmar pattern. The authors suggest that NMES may be a positive addition to other interventions for this population.
Development of Hand Skills
The interventions described in this section apply and integrate four models of practice or frames of reference: neurodevelopmental treatment, developmental, motor learning, and biomechanical. Neurodevelopmental treatment frame of reference focuses on understanding and improving the child’s impairments in postural tone, postural control, and stability and mobility.122 The intervention activities focus on providing adequate support and helping the child develop dissociated and coordinated patterns of movement. Developmental theories give us a frame of reference to describe the sequences of skills that children develop (e.g., the progression from palmer grasp to a pincer grasp pattern). This frame of reference suggests that tasks should be presented in a sequential order and that children achieve increasingly more difficult skills in a specific developmental sequence.
When therapists use motor learning theory, they focus on how the child learns specific motor skills. The occupational therapist assists the child in acquiring motor skills through structure and feedback and provides him or her with structured practice to refine the skills. The therapist selects a specific type of practice and feedback based on the child’s level of performance and response to intervention. Sullivan, Kantak, and Burtner presented a clear example of research with children based on motor learning theory.132 In their study, different frequencies of feedback were provided during a task involving arm movements. The authors found that children use feedback in a manner different from that of adults and require longer periods of practice. Chapter 9 provides additional description of motor learning theory.
The biomechanical frame of reference is used primarily to assess and provide intervention activities that improve a child’s range of motion, strength, or endurance. Biomechanical approaches focus on postural alignment, joint stability and relationships, and musculoskeletal problems. Biomechanics helps the therapist understand the principles involved in tenodesis grasping patterns and the relationship of intrinsic and extrinsic muscle control for grasp and in-hand manipulation patterns.
When addressing hand skill development in children, the therapist must select activities that are interesting and appropriately challenging to the child. To support skill development, the therapist must be able to repeat these activities. Eliasson stated specifically that “practice or repetition is an important part of the learning process” (p. 50).40 She defines learning as evidenced through “relatively consistent performance and retention of the task” (p. 50).40 Therefore, eating activities and toys and games with many pieces can be particularly useful and enjoyable. Engaging in play while addressing hand skills can have important benefits, including motivating the child to engage in activities repeatedly and building his or her play repertoire.29,137 Recent research suggests that the use of cognitive strategies to encourage awareness of elements of task performance may be helpful for enhancing the performance of children with developmental coordination disorders (Research Note 10-2).17,98 Eliasson provides an excellent summary of a wide range of approaches to hand skill interventions for children with cerebral palsy, citing key research references as a basis for each of the approaches.
Promoting Isolated Arm and Hand Movements
The therapist may choose to address specific movements in the upper extremity apart from specific hand skills. For example, the therapist may assist the child in using elbow flexion-extension, supination-pronation, or wrist flexion-extension movements before integrating these movements into reaching, grasping, or releasing patterns. Helping children generalize the movement patterns they have practiced and learned into a functional activity is an important aspect of motor learning theory. Such an approach is most successful with children who can follow verbal instructions and participate actively in working on specific hand skills. The therapist can use games or songs to practice the use of these movements. The therapist needs to emphasize specific movements and, in the same treatment session, use them in a functional context.
Supination control is one of the areas of greatest difficulty for children with disabilities, particularly those with tone problems. Abnormal posturing at the trunk, shoulder, elbow, or wrist often compensates for difficulties in initiating or sustaining forearm supination. Supination is easiest to use when the elbow is fully flexed and most difficult to use with full elbow extension. The therapist therefore can use activities that position the elbow in greater than 90° of flexion to facilitate supination. Examples of such activities include finger feeding, holding a kaleidoscope, and putting lotion on the face.
If the child can initiate supination but has poor control of this pattern, he or she can benefit from activities with the elbow held in 90° of supination with the forearm stabilized on a surface and an object presented vertically (see Figure 10-16). Gradually the therapist moves materials to encourage the child to use more elbow extension while maintaining the supinated position. Children with more severe involvement may be able to achieve only about 30° of supination, the minimum amount needed to handle materials on a table effectively. The therapist should encourage children with less motor impairment to obtain and use at least 90° of supination to accomplish functional activities such as drinking, eating with utensils, or turning a doorknob. Supination is critical for successful, smooth use of in-hand manipulation skills. In these activities it also is helpful to facilitate supination in the nonpreferred arm so that that hand can stabilize materials more effectively.
Enhancement of Reach and Carry Skills
Problems: Children with neuromotor disabilities exhibit typical problems in reach that limit range and control. Examples of problems in reach are:
• Use of abduction and internal rotation to initiate reach
• Use of shoulder elevation and lateral trunk flexion to increase the height of the arm for reaching and carrying
• Inability to coordinate the degree of hand opening or the hand position with the timing of the reach
• Difficulty maintaining an upright body posture when reaching or carrying forward or across the midline
Goals: Presented next are examples of goals the therapist can use for children with a variety of levels of disability. The goals are in approximate order of difficulty, although difficulty using any one pattern can vary with the individual child. All of the goals are associated with increasing the child’s independence in morning hygiene skills. Some children may attain more limited independence in morning hygiene activities. Sample applications of the specific objects that could be the focus of the goals are indicated in parentheses. The goals are that the child will:
1. Maintain visual regard of the (soap, faucet handle, comb) while making hand contact
2. Bring the hand into contact with hygiene items (soap, toothpaste, towel) presented in various planes
3. Attain and carry hygiene items needed (soap, toothpaste, toothbrush, comb) located near the body but in various planes while sustaining sufficient finger extension to allow for grasp
4. Pick up objects (a towel, a large plate or pan) presented at midline by reaching with both hands together (forearm may be pronated)
5. Attain and carry large objects (e.g., a towel) in a variety of locations using both hands and incorporating appropriate forearm positioning
6. Attain and carry hygiene items (toothbrush, toothpaste, shampoo bottle, safety razor) using appropriate hand positioning for grasp combined with a mature reaching pattern
7. Pick up and place items (toothbrush, washcloth, makeup items) in various locations on a bathroom sink or counter, crossing the midline with an erect trunk posture and humeral external rotation, elbow extension, and forearm supination to midposition
8. Attain items from all levels in a cabinet or closet (including reaching above the head) with control
Intervention Strategies: When the child initiates little movement or is unable to open the hand during arm movement, the primary focus of intervention is on controlled initiation of arm movements. This includes using various types of arm movements and being able to place and hold the arm to allow for contact with objects. This type of reaching goal is a priority for children with extremely limited movement control or strength and those with a degenerative disease process that results in skill regression. These movements are important for contact with others, and the child can use them to activate switches for toys and electronic equipment.
To facilitate arm movements and contact with objects, the therapist must identify the best position to promote postural stability and visual regard. The most commonly used position is sitting, with attention given to head and trunk control, visual regard, and visual tracking. However, the therapist also can use the supine and side-lying positions effectively.
Children with severe motor involvement need toys and materials that are easy to activate and that have no “failure” elements. Such items include play foam, beans, rice, musical toys activated by light touch, and soap bubbles. The therapist usually can obtain the best results through proximal handling at the shoulders and upper arms while assisting the child with movements of either or both arms. The emphasis initially is on general arm movement, then on hand and arm placement, and finally on finger extension during arm movement as a precursor for reach with grasp.
When children are able to contact objects with some control, the therapist should introduce structured activities to assist the child in using elements of a more mature reaching pattern. Gradually these elements are combined to promote a smooth, direct reach. The therapist needs to determine the placement of objects in relation to the child’s body so that the child can use the best reaching pattern possible. From that position the therapist can begin to vary object placement and orientation. For example, because presentation of objects at shoulder height often results in the child reaching with internal rotation and elbow flexion, initial presentation of objects at a level below the child’s shoulder may facilitate the use of shoulder flexion and neutral rotation. Gradually the therapist can raise objects higher as the child develops more control. The therapist can use activities that require lateral reaching with shoulder abduction and slight external rotation before encouraging reaching with shoulder flexion. Box 10-3 includes a sequence of promoting reach and grasp while encouraging use of shoulder flexion or neutral or external rotation at the shoulder and elbow extension.
The therapist should also encourage the child to reach behind his or her body, combining humeral hyperextension with controlled internal rotation and various elbow positions. Many children have difficulty with this posterior reaching pattern, which is required in dressing and other daily living skills. Some children can use neutral to slight external shoulder rotation in combination with humeral flexion if the therapist provides them with a minimal amount of handling at the humerus or elbow and appropriate object orientation (Figure 10-17). However, if such handling techniques are required for a child to use a mature reaching pattern, the therapist should present objects somewhat to the side or in front of the shoulder initially and then gradually toward the midline. To encourage reaching that incorporates neutral to slight external rotation of the shoulder and forearm supination, the therapist should orient the objects vertically. Horizontal orientation of an object encourages the use of forearm pronation.

FIGURE 10-17 Facilitation is provided to prompt use of slight humeral external rotation and forearm supination. The object is held vertically to assist this reaching pattern. A lotto card game is used to engage the child and allow for repetition of the pattern. (Courtesy Kanji Takeno, Towson University.)
To carry an object, the child must be able to vary all joint positions in the arm while sustaining grasp. Generally the child maintains wrist extension with sustained finger flexion when carrying or lifting an object to place it. The therapist should be especially attentive to the child’s use of compensatory trunk movements and to difficulty dissociating arm and trunk movements. If these are present, the child may need intervention to improve sustained trunk control in the midline and trunk rotation with arm movements. The use of adapted equipment to support the trunk in a symmetric, erect posture is helpful for many children. The therapist also may need to stabilize the shoulder to prevent scapular elevation.
The therapist can use facilitation of arm movements in a manner similar to that described for reaching to encourage carrying patterns of shoulder rotation, graded elbow movements, and forearm supination. Most children with increased tone or stability problems have more difficulty carrying small or thin objects. Use of objects that are larger in diameter, such as those adapted with built-up handles, can promote wrist extension and management of objects during carrying.
Children with muscle weakness can more effectively reach and carry objects when they can use a table or tray surface at or slightly above elbow height. The therapist can use mobile arm suspension systems to support and assist the child who has muscle strength rated as fair-minus or less.
The therapist should provide objects that have high color contrast or bright, solid colors to children with visual impairment. In cases of severe visual impairment, objects can combine both auditory stimuli and varied textures. If the child has not developed the ability to search for objects, the therapist should provide materials in a confined space or tied to strings so that the child can easily retrieve them when they are dropped.

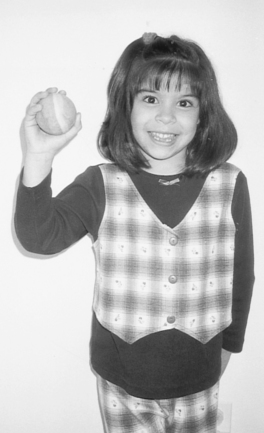

 RESEARCH NOTE 10-1
RESEARCH NOTE 10-1