Sensory Integration
1 Explain the neurobiological concepts that are basic to an individual’s sensory integrative function.
2 Explain the link between sensory input from the environment and the child’s adaptive response.
3 Describe the development of sensory integration from prenatal life through childhood.
4 Explain the clinical picture and hypothesized basis for problems in sensory modulation and sensory discrimination.
5 Describe atypical vestibular-bilateral functions and the types of behaviors that children with these problems often demonstrate.
6 Define developmental dyspraxia, and identify examples of behaviors that might be observed in a child with this problem.
7 Relate the Ayres Sensory Integration® (ASI) approach to childhood occupations and to the Occupational Therapy Practice Framework.
8 Discuss the evaluation of sensory integration within varying contexts such as home and school.
9 Identify and describe tests, interviews, and instruments used to evaluate sensory integration.
10 Describe ASI intervention and discuss the disadvantages and benefits of using such an intervention approach.
11 Explain some considerations for determining whether ASI may be an appropriate frame of reference for an individual child.
12 Describe specific skill training, group programming, and consultative interventions (such as activity or environmental modifications), including the benefits and limitations of using these approaches in conjunction with or instead of ASI intervention.
13 Identify the expected outcomes of an occupational therapy program using ASI intervention.
14 Discuss published research related to the effectiveness of ASI intervention.
15 Identify some of challenges when evaluating the effectiveness of ASI intervention.
The term sensory integration holds special meaning for occupational therapists. In some contexts it is used to refer to a particular way of viewing the neural organization of sensory information for functional behavior. In other situations this term refers to a clinical frame of reference for the assessment and treatment of people who have functional disorders in sensory processing. Both of these meanings originated in the work of A. Jean Ayres, an occupational therapist and psychologist whose brilliant clinical insights and original research revolutionized occupational therapy practice with children.
Ayres’ ideas ushered in a new way of looking at children and understanding many of the developmental, learning, and emotional problems that arise during childhood. Her innovative practice and groundbreaking research met a tremendous amount of resistance within the profession when introduced in the late 1960s and 1970s. Today, the treatment methods that she pioneered continue to be questioned and investigated, but there is little doubt that her perspective has had a profound influence on occupational therapy practice. The presence of sensory integration concepts in nearly all of the chapters of this book attests to the extent to which these ideas have affected the thinking of pediatric occupational therapists. Furthermore, the research base of the sensory integration approach to practice is extensive.
This chapter provides an in-depth orientation to this fascinating aspect of occupational therapy practice. The reader will gain a general sense of how sensory integration as a brain function is related to everyday occupations. Following is a description of how sensory integration is manifested in typically developing children and in relation to the daily life problems of children who experience difficulty with sensory integration. The history of research on sensory integration problems is reviewed to give the reader a perspective on how this field came into being, what the major constructs are, and how they have changed—and continue to change—over time. Sensory integration, as an intervention approach developed by Ayres, is now trademarked through the Franklin B. Baker/A. Jean Ayres Baker Trust as Ayres Sensory Integration® (ASI).130 According to the trademark document, ASI encompasses the theory, assessment methods, patterns of sensory integration and praxis problems, and intervention concepts, principles, and techniques developed by Ayres.129 In this chapter, ASI is described with respect to different types of sensory integration problems encountered by children, methods of clinical assessment, and characteristics of both direct and indirect modes of intervention, with emphasis on the principles of individual ASI intervention. Effectiveness research on individual ASI intervention is presented and case examples of children who have been helped by occupational therapists using an ASI approach are provided.
SENSORY INTEGRATION IN CHILD DEVELOPMENT
One of the most distinctive contributions that Ayres made to understanding child development was her focus on sensory processing, particularly with respect to the proximal senses (vestibular, tactile, and proprioceptive). From the sensory integration viewpoint, these senses are emphasized because they are primitive and primary; they dominate the child’s interactions with the world early in life. The distal senses of vision and hearing are critical and become increasingly more dominant as the child matures. Ayres believed, however, that the body-centered senses are a foundation on which complex occupations are scaffolded. Furthermore, when Ayres began her work, the vestibular, tactile, and proprioceptive senses were virtually ignored by scholars and clinicians who were interested in child development. She devoted her career to studying the roles that these previously forgotten senses play in development and in the genesis of developmental problems of children.
Ayres’ basic assumption was that brain function is a critical factor in human behavior.11 She reasoned, therefore, that knowledge of brain function and dysfunction would give her insight into child development and would help her understand the developmental problems of children. However, Ayres also had a pragmatic orientation that sprang from her professional background as an occupational therapist. She was concerned particularly with how brain functions affected the child’s ability to participate successfully in daily occupations. Consequently, her work represents a fusion of neurobiological insights with the practical, everyday concerns of human beings, particularly children and their families.
As Ayres developed her ideas about sensory integration, she used terms such as sensory integration, adaptive response, and praxis in ways that reflected her orientation. A glossary of terms that are commonly used within the framework of sensory integration theory is presented on the Evolve website. It may be helpful to the reader to refer to these definitions frequently while reading this chapter.
Ayres coined some of these terms, whereas other terms were drawn from the literature of other fields. When Ayres borrowed a term from another field, however, she imparted a particular meaning to it. For example, Ayres did not use the term sensory integration to refer solely to intricate synaptic connections within the brain, as neuroscientists typically do. Rather, she applied it to neural processes as they relate to functional behavior. Hence, her definition of sensory integration is the “organization of sensation for use” (p. 5).18 It is the inclusion of the final clause “for use” that is Ayres’s hallmark, because it ties sensory processing to the person’s occupation.5
Ayres introduced a new vocabulary of sensory integration theory and synthesized important concepts from the neurobiologic literature to organize her views of child development and dysfunction. Many of these ideas were first published in her classic book Sensory Integration and Learning Disorders.11 Later she wrote a book for parents, Sensory Integration and the Child,18,22 outlining the behavioral changes that can be observed in a child as sensory integration develops. Major points made in these books regarding neurobiologic concepts in relationship to development and the ontogeny of sensory integration are presented in the following section.
NEUROBIOLOGICALLY BASED CONCEPTS
Sensory Support for Development and Brain Function
Sensory input is necessary for optimal brain function. The brain is designed to constantly take in sensory information, and it malfunctions if deprived of it. Sensory deprivation experiments conducted in the 1950s and 1960s made it clear that without an adequate inflow of sensation, the brain generates its own input in the form of hallucinations and subsequently distorts incoming sensory stimuli.145 If adequate sensory stimulation is not available at critical periods in development, brain abnormalities and resulting behavioral disorders result.74,77,79 It is now well established that persistent, serious impairments in cognitive, social, and emotional functioning often result when infants and young children are institutionalized in environments that are impoverished with respect to availability of a wide range of sensory experiences, the presence of a nurturing caregiver, and opportunities for sensory-motor exploration.29,47,56,122
Ayres considered sensory input to be sensory nourishment for the brain, just as food is nourishment for the body.18 Wilbarger, a colleague of Ayres, built on this concept with the sensory diet, designed to provide individualized sensory experiences for the child with sensory integrative dysfunction.152 The therapeutic sensory diet provides an optimal combination of sensory-based activities at the appropriate intensities for a specific child. For most typically developing children, the sensory diet does not require conscious monitoring by caregivers. The environment continuously “feeds” the child a variety of nourishing sensations in the flow of everyday life.
As critical as input is to the developing brain, the mere provision of sensory stimulation is limited in value. Too much stimulation can generate stress that is detrimental to brain development and may reduce the person’s subsequent ability to cope with stress.72 To have an optimal effect on development, learning, and behavior, the sensory input must be actively organized and used by the child to act on and respond to the environment.
Adaptive Response
A child does not passively absorb whatever sensations come along. Rather the child actively selects the sensations most useful at the time and organizes them in a fashion that facilitates accomplishing goals. This is the process of sensory integration. When this process is going well, the child organizes a successful, goal-directed action on the environment, which is called an adaptive response. When a child makes an adaptive response, he or she successfully meets some challenge presented in the environment. The adaptive response is possible because the brain has been able to efficiently organize incoming sensory information, which then provides a basis for action (Figure 11-1).
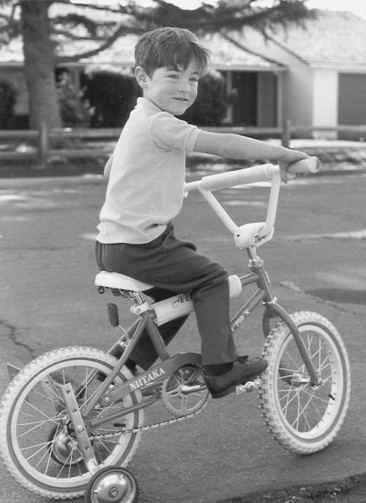
FIGURE 11-1 Adaptive responses help the child acquire skills such as riding a bicycle. Although training wheels reduce the challenge for this boy, his nervous system must integrate vestibular, proprioceptive, and visual information adequately for him to successfully steer the bicycle while it is moving. (Courtesy Shay McAtee.)
Adaptive responses are powerful forces that drive development forward. When a child makes an adaptive response that is more complex than any previously accomplished response, the brain attains a more organized state and its capacity for further sensory integration is enhanced. Thus, sensory integration leads to adaptive responses, which in turn result in sensory integration that is more efficient.
Ayres provides the example of learning to ride a bicycle to illustrate this process.18 The child must integrate sensations, particularly from the vestibular and proprioceptive systems, to learn how to balance on the bicycle. The senses must accurately and quickly detect when the child begins to fall. Eventually, perhaps after many trials of falling, the child integrates sensory information efficiently enough to make the appropriate weight shifts over the bicycle to maintain balance. This is an adaptive response, and once made, the child is able to balance more effectively on the next attempt to ride the bike. The child’s nervous system has changed, so the child is now more adept at bicycle riding.
In making adaptive responses, the child is an active doer, not a passive recipient. Adaptive responses come from within the child. No one can force a child to respond adaptively, although a situation may be set up that is likely to elicit adaptive responses from the child. For typically developing children and for most children with disabilities, there is an innate drive to develop sensory integration through adaptive responses. Ayres called this inner drive and speculated that it is generated primarily by the limbic system of the brain, a structure known to be critical in both motivation and memory.18 Ayres designed therapeutic activities and environments to engage the child’s inner drive (elicit adaptive responses) and, in so doing, advance sensory integrative development and the child’s occupational competence.
Neural Plasticity
It is thought that when a child makes an adaptive response, change occurs at a neuronal synaptic level. This change is a function of the brain’s neural plasticity. Plasticity is the ability of a structure and concomitant function to be changed gradually by its own ongoing activity.11 It is well established in the neuroscientific literature that when organisms are permitted to explore interesting environments, significant increases in dendritic branching, synaptic connections, synaptic efficiency, and size of brain tissue result.79 These changes are most dramatic in a young animal and probably represent a major mechanism of brain development,74 although it is clear that such manifestations of plasticity are characteristic of optimal brain functioning throughout the lifespan.27,55,88
Studies of the effects of enriched environments on animals indicate that the essential ingredient for positive brain changes is that the organism actively interacts with a meaningful and challenging environment.31,79 Passive exposure to sensory stimulation does not produce these same positive changes.55,59 It can be hypothesized from these findings that adaptive responses activate the brain’s neuroplastic capabilities. Furthermore, the brain’s plasticity makes it possible for an adaptive response to increase the efficiency of sensory integration at a neuronal level.
Central Nervous System Organization
Ayres looked to the organization of the central nervous system (CNS) for clues to how children organize and use sensory information and how sensory integration develops over time.11 At the time that she was developing her theory, hierarchic models of the CNS dominated thinking in the neurosciences.
Hierarchic models view the nervous system in terms of vertically arranged levels, with the spinal cord at the bottom, the cerebral hemispheres at the top, and the brainstem sandwiched in between. These levels are interdependent yet reflect a trend of ascending control and specialization. Thus, the cerebral cortex at the top of the hierarchy is highly specialized and analyzes precise details of sensory information. Ordinarily the cortex assumes a directive role over lower levels of the hierarchy. For example, the cortex may command lower centers to “ignore” certain stimuli deemed unimportant. This process is called descending inhibition and is critical in enabling higher brain functions to work efficiently.11 The lower levels of the CNS, however, have functions that are more diffuse and primitive, less specialized, and yet potentially more pervasive in influence compared with those of the higher levels. One of the important responsibilities of the lower levels is to filter and refine sensory information before relaying organized sensory messages upward to the cerebral cortex. Thus, cortical centers depend on lower centers for the receipt of essential, well-organized sensory information to analyze in preparation for the planning of action. According to hierarchic views, the higher levels of the CNS superimpose functions that are more sophisticated on the lower levels, but these do not replace the important lower level functions.11
Ayres believed that critical aspects of sensory integration are seated in the lower levels of the CNS, particularly the brainstem and thalamus.11 Most of the CNS processing of vestibular information occurs in the brainstem, and much somatosensory processing takes place there and in the thalamus. One of the basic tenets of Ayres’s theory is that, because of the dependence of higher CNS structures on lower structures, increased efficiency at the levels of the brainstem and thalamus enhance5 higher order functioning.11 This view varies from traditional neuropsychology and education models, which have tended to emphasize the direct study and remediation of high-level, cortically directed skills such as reading and writing. However, newer models of education have considered “readiness” for academics and the importance of other modes such as “kinesthetic” learning.60,141
In adopting a hierarchic view of the CNS, Ayres also assumed that the CNS develops hierarchically from bottom to top, with spinal and brainstem structures maturing before higher level centers.11 At the time that Ayres was developing her theory, this was somewhat speculative, although generally accepted by neuroscientists. In research conducted in more recent years, the use of positron electron tomography (PET) scans on infants has provided direct support for the notion that brain development proceeds in a bottom-to-top direction.48
The hierarchic approach to CNS functioning and development led Ayres to emphasize the more primitive vestibular and somatosensory systems in her work with young children. These systems mature early and are seated in the lower CNS centers (particularly the brainstem, cerebellum, and thalamus). Using the logic of hierarchy, Ayres reasoned that the refinement of primitive functions, such as postural control, balance, and tactile perception, provides a sensorimotor foundation for higher-order functions, such as academic ability, behavioral self-regulation, and complex motor skills (e.g., those required in sports). Thus, she viewed the developmental process as one in which primitive body-centered functions serve as building blocks upon which complex cognitive and social skills can be scaffolded. This view undergirds a basic premise of the therapy approach that she developed: enhancing lower-level functions related to the proximal senses might have a positive influence on higher-level functions.
On some points Ayres departed from a strictly hierarchic view of the CNS.11 For example, she noted that each level of the CNS can function as a self-contained sensory integration system. Therefore, the brainstem can independently direct some sensorimotor patterns without being directed by the higher level cortex. Furthermore, the sensory integrative process involves the brain working as a whole, not simply as a series of hierarchically controlled messages, as rigid hierarchic models might suggest. These ideas are more consistent with the view of some contemporary biologists that the brain is a heterarchic system. A heterarchy is a system in which different parts may assume the controlling role in different situations; control does not always flow in a top-down direction.135 Ayres was ahead of her time in suggesting that the brain does not operate exclusively as a hierarchy but has holistic characteristics. These heterarchic notions strengthened her view that functions considered primitive were worthy of serious consideration in therapy.
SENSORY INTEGRATIVE DEVELOPMENT AND CHILDHOOD OCCUPATIONS
Ayres believed that the first 7 years of life is a period of rapid development in sensory integration.18 She drew this conclusion not only from her many years of observing children, but also from research in which she gathered normative data on tests of sensory integration.11 By the time most children reach 7 or 8 years of age, their scores on standardized tests of sensory integrative capabilities reflect almost as much maturity as an adult’s.
Development, from a sensory integrative standpoint, occurs as the CNS organizes sensory information and adaptive responses with increasing degrees of complexity. Sensory integration, of course, enables adaptive responses to occur, which in turn promote the development of sensory integration and the emergence of occupational engagement and social participation.114,146 As this process unfolds in infancy, the developing child begins to attach meaning to the stream of sensations experienced. The child becomes increasingly adept at shifting attention to what he or she perceives as meaningful, tuning out that which is irrelevant to current needs and interests. As a result, the child can organize play behavior for increasing lengths of time and gains control in the regulation of emotions.
Inner drive leads the child to search for opportunities in the environment that are “just right challenges.” These are challenges that are not so complex that they overwhelm or induce failure, nor so simple that they are routine or uninteresting. The just right challenge is one that requires effort but is accomplishable. Because there is an element of challenge, a successful adaptive response engenders feelings of mastery and a sense of oneself as a competent being.
It is fascinating to watch this process unfold. Most children require no adult guidance or teaching to acquire basic developmental skills such as manipulating objects, sitting, walking, and climbing. Little, if any, step-by-step instruction is needed to learn daily occupations such as playing on playground equipment, dressing and feeding oneself, drawing and painting, and constructing with blocks. These achievements seem to just happen. They are the product of an active nervous system busily organizing sensory information and searching for challenges that bring forth more complex behaviors, all shaped within the context of a world saturated with sociocultural expectations and meanings.114
In this section, developmental hallmarks of sensory integration are identified and connected to the occupational achievements of childhood. The proximal senses dominate early infancy and continue to exert their influence in critical ways as the visual and auditory systems gain ascendancy. Although there is some variability across children in the sequence in which developmental achievements unfold during the first year of life, this variability becomes increasingly apparent after this first year. By kindergarten age, skills vary tremendously among children because of differences in environmental opportunities, familial and cultural influences, personal experiences, and genetic endowment. It is important to keep in mind that, throughout development, sensory integrative processes contribute to the child’s construction of his or her identity, but many other influences are powerful as well—the family and cultures that shape the child’s occupational routines, the interpretations given to the child’s behaviors by others, the child’s talents and abilities, and even chance events that carry special meaning to the child.114
Prenatal Period
The first known responses to sensory stimuli occur early in life, at approximately 5½ weeks after conception.78 These first responses are to tactile stimuli. Specifically, they involve reflexive avoidance reactions to a perioral stimulus (e.g., the embryo bends its head and upper trunk away from a light touch stimulus around the mouth). This is a primitive protective reaction. It is not until about 9 weeks’ gestational age that an approach response (moving of the head toward the chest) occurs,78 probably as a function of proprioception.
The first known responses to vestibular input in the form of the Moro reflex also appear at about 9 weeks after conception. The fetus continues to develop a repertoire of reflexes such as rooting, sucking, Babkin, grasp, flexor withdrawal, Galant, neck righting, Moro, and positive supporting in utero that are fairly well established by the time of birth. Thus, when the time comes to leave the uterus, the newborn is well equipped with the capacity to form a strong bond with a caregiver and to actively participate in the critical occupation of nursing. These innate capacities require rudimentary aspects of sensory integration that are built into the nervous system. However, even in this earliest period of development, environmental influences, such as maternal stress, can have a significant impact on the quality of sensory integrative development. For example, Schneider and her colleagues found that infant rhesus monkeys born to mothers who had experienced stress in early pregnancy had signs of diminished responses to vestibular input, such as impaired righting responses, weak muscle tone, and attenuated postrotary nystagmus.138,139
Neonatal Period
Touch, smell, and movement sensations are particularly important to the newborn infant, who uses these to maintain contact with a caregiver through nursing, nuzzling, and cuddling. Tactile sensations, especially, are critical in establishing a primary attachment relationship with a caregiver and fostering feelings of security in the infant. This is just the beginning of the important role that the tactile system plays in a person’s emotional life because it is directly involved in making physical contact with others (Figure 11-2). Proprioception is also critical in the mother–infant relationship, enabling the infant to mold to the adult caregiver’s body in a cuddly manner. The phasic movements of the infant’s limbs generate additional proprioceptive inputs. Together, all of these tactile and proprioceptive inputs set the stage for the eventual development of body scheme (the brain’s map of the body and how its parts interrelate).
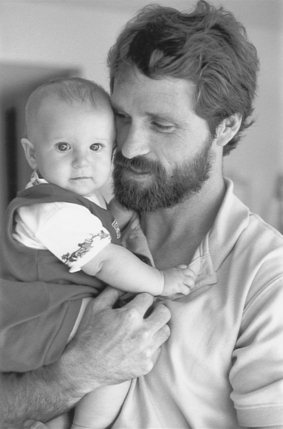
FIGURE 11-2 Tactile sensations play a critical role in generating feelings of security and comfort in the infant and are influential in emotional development and social relationships throughout the lifespan. (Courtesy Shay McAtee.)
The vestibular system is fully functional at birth, although refinement of its sensory integrative functions, particularly its integration with visual and proprioceptive systems, continues through childhood. Of all the sensory systems, the vestibular system is the first to mature.98 Most caregivers who use rocking and carrying to soothe and calm the infant instinctively appreciate the influence of vestibular stimuli on the infant’s arousal level. Ayres pointed out that sensations such as these, which make a child contented and organized, tend to be integrating for the child’s nervous system.18
Experiences that activate the vestibular sense have other integrating effects on the infant as well. Being lifted into an upright position against the caregiver’s shoulder is known to increase alertness and visual pursuit.70 While being held in such a position, the young infant’s vestibular system detects the pull of gravity and begins to stimulate the neck muscles to raise the head off the caregiver’s shoulder. This adaptive response reaches full maturation within 6 months. In the first month of life, head righting may be minimal and intermittent with much wobbling, but it will gradually stabilize and become firmly established as the baby assumes different positions (first when the baby lies in a prone position and later in the supine position).
The visual and auditory systems of the newborn are immature. The newborn orients to some visual and auditory inputs and is particularly interested in human faces and voices, although meaning is not yet attached to these sensations. Visually the infant is attracted to high-contrast stimuli, such as black-and-white designs, and the range of visual acuity for most stimuli is limited to approximately 10 inches. The infant’s visual acuity and responsiveness to visual patterns expand dramatically over the first few months of life.98 During this time the infant begins to use eye contact to relate to the caregiver, further strengthening the bond between them.
Stimulation in each of the sensory systems potentially affects the infant’s state of arousal. The infant’s capacity to behaviorally adapt to changing sensations is another important aspect of sensory integrative development—the development of self-regulation. It is relatively easy to overstimulate young infants, for example, with changes in water temperature, changes in body position, or an increase in auditory or visual stimuli.136 However, as sensory integration develops, the older child is better able to self-regulate his or her responses to changing stimuli by initiating behaviors that will be calming and soothing (such as thumb sucking or cuddling with a favorite blanket) or exciting and energizing (such as jumping or singing).124 This process of self-regulation begins in the neonatal period and develops throughout early childhood.
First 6 Months
By 4 to 6 months of age, a shift occurs in the infant’s behavioral organization. The sensory systems have matured to the extent that the baby has much greater awareness and interest in the world, and developing vestibular-proprioceptive-visual connections provide the beginnings of postural control. During the first half of the first year, the infant begins to show a strong inner drive to rise up against gravity (Figure 11-3), and this drive is evident in much of the baby’s spontaneous play. Body positions during the first 6 months characteristically involve the prone position, with gradually increasing extension from the neck down through the trunk as the arms gradually bear more weight to help push the chest off the floor. By 6 months of age, many infants spend a great deal of time in the prone position with full active trunk extension, and most are able to sit independently, at least if propped with their own hands. These body positions usually are the infant’s preferred positions for play and are reflect the maturing of the lateral vestibulospinal tract. Head control is well established by 6 months of age and provides a stable base for control of eye muscles. This, of course, reflects the growing integration of vestibular, proprioceptive, and visual systems, which becomes increasingly important in providing a stable visual field as the baby becomes mobile.

FIGURE 11-3 Strong inner drive to master gravity is evident in this infant’s efforts to lift his head and shoulders off the floor. This is an early form of the prone extension posture. (Courtesy Shay McAtee.)
Somatosensory achievements at this time are particularly evident in the infant’s hands. The infant uses tactile and proprioceptive sensations to grasp objects, albeit with primitive grasps. Touch and visual information are integrated as the baby begins to reach for and wave or bang objects. The infant has a strong inner drive to play with the hands by bringing them to midline while watching and touching them. Connections between the tactile and visual systems pave the way for later hand–eye coordination skills. Midline hand play is a significant milestone in the integration of sensations from the two sides of the body.
By now, neonatal reflexes no longer dominate behavior; the baby is beginning to exercise voluntary control over movements during play. The earliest episodes of motor planning occur as the infant works to produce novel actions. This becomes evident as the infant handles objects and begins to initiate transitions from one body position to another, as in rolling from prone position to supine. Although reflexes play a role in such actions (such as grasp and neck righting reflexes), the infant’s actions have a goal-directed, volitional quality and are not stereotypically reflex bound. The emergence of intentionality is a marker of the beginning of occupational engagement.
Second 6 Months
Another major transition occurs during the latter half of the first year. Infants become mobile in their environments, and by the first birthday they can willfully move from one place to another, many walking while others creep or crawl. These locomotor skills are the product of the many adaptive responses that have gone before, resulting in increasingly more sophisticated integration of somatosensory, vestibular, and visual inputs.
As the infant explores the environment, greater opportunities are generated for integrating a variety of complex sensations, particularly those responsible for developing body scheme and spatial perception. The child learns about environmental space and about the body’s relationship to external space through sensorimotor experiences.
During the second 6 months after birth, tactile perception becomes further refined and plays a critical role in the child’s developing hand skills. The infant relies on precise tactile feedback in developing a fine pincer grasp, which is used to pick up small objects. Proprioceptive information is also an important influence in developing manipulative skills, and now the baby experiments with objects using a variety of actions. These somatosensory-based adaptive responses contribute to development of motor planning ability. Further development of midline skills is also apparent as the baby easily transfers objects from one hand to the other and may occasionally cross the midline while holding an object.
Through the first year, auditory processing plays a significant role in the infant’s awareness of environment, especially the social environment. Auditory information is integrated with tactile and proprioceptive sensations in and around the mouth as the infant vocalizes. The fruits of this process begin to blossom in the latter half of this first year, when the infant begins to experiment with creating the sounds of the language used by caregivers. Vocalizations such as consonant–vowel repetitions (“baba” and “mamama”) are common. Parents often attach meaning to these infant vocalizations and strongly encourage them, thus leading the infant also to attach meaning to these sounds. By their first birthday, many infants have a small vocabulary of words or wordlike sounds that they use meaningfully to communicate desires to caregivers.
Another major landmark toward the end of the first year is beginning independence in self-feeding. This complex achievement requires refined somatosensory processing of information from the lips, the jaw, and inside the mouth to guide oral movements in the chewing and swallowing of food. Taste and smell sensations are also integral to this process, but self-feeding involves more than the mouth. All of the acquired sensory integrative milestones involving hand–eye coordination are important to self-feeding. The infant at this period of life uses the fingers directly to feed him or herself and to explore the textures of foods. At this stage, use of a utensil such as a spoon is not very functional and is messy because motor planning skills have not progressed to the point that the child can manipulate the utensil successfully. However, many infants begin to demonstrate a drive to use the spoon in self-feeding by the end of the first year. For many contemporary American infants, use of a spoon is the first real experience in using a tool (Figure 11-4).

FIGURE 11-4 Because somatosensory processing and visual-motor coordination strongly influence self-feeding skills, sensory integration is an important contributor to the development of dining, a fundamental occupation. (Courtesy Shay McAtee.)
The occupation of dining, then, begins to emerge in infancy as sensory integrative abilities mature, allowing the child to engage in self-feeding. As an occupation, dining in its fullest sense goes far beyond the physical, sensorimotor act of feeding. Dining usually takes place within a social context, whether at a family dinner at home or in a formal restaurant, so social standards for acceptable behavior and etiquette become increasingly important as the child develops. Furthermore, partaking in a meal and sharing certain types of food gradually come to take on powerful symbolic meanings. The sensory integrative underpinnings of the dining experience influence how the child experiences mealtimes and how others view the child as a dining partner, thus playing a role in shaping the social and symbolic aspects of this vitally important occupation.
Second Year
As the child moves into the second year, the basic vestibular-proprioceptive-visual connections that were laid down earlier continue to refine, resulting in growing finesse in balance and fluidity of dynamic postural control. Discrimination and localization of tactile sensations also become much more precise, allowing for further refinement of fine motor skills.
Increasingly complex somatosensory processing contributes to the continuing development of body scheme. Ayres hypothesized that as body scheme becomes more sophisticated, so does motor planning ability.11 This is because the child draws on knowledge of how the body works to program novel actions (Figure 11-5). Throughout the second year, the typically developing toddler experiments with many variations in body movements. Imitation of the actions of others contributes further to the child’s movement repertoire. In experiencing new actions, the child generates new sensory experiences, thus building an elaborate base of information from which to plan future actions.

FIGURE 11-5 As motor planning develops during the second year of life, the infant experiments with a variety of body movements and learns how to transition easily from one position to another. These experiences are thought to reflect the development of body scheme. (Courtesy Shay McAtee.)
While motor planning ability becomes increasingly more complex in the second year, another aspect of praxis, ideation, begins to emerge. Ideation is the ability to conceptualize what to do in a given situation. Ideation is made possible by the cognitive ability to use symbols, first expressed gesturally and then vocally during the second year of life.35 Symbolic functioning enables the child to engage in pretend actions and to imagine doing actions, even actions that the child has never before done. By the end of the second year, the toddler can join several pretend actions in a play sequence.102 Furthermore, the 2-year-old child demonstrates that he or she has a plan before performing an action sequence, either through a verbal announcement or through a search for a needed object.102 Thus, a surge in practic development occurs in the second year as the child generates many new ideas for actions and begins to plan actions in a systematic sequence.
The burgeoning of praxis abilities plays an important role in the development of self-concept. Infant psychiatrist Daniel Stern suggests that the sense of an integrated core self begins in infancy as an outcome of the volition and the proprioceptive feedback involved in motor planning.147 The consequences of the child’s voluntary, planned actions add to the developing sense of self as an active agent in the world. As praxis takes giant leaps during the second year, so does this sense of self as an agent of power. The child feels in command of his or her own life when sensory integration allows the child to move freely and effectively through the world.18
Third through Seventh Years
The child’s competencies in the sensorimotor realm mature in the third through seventh years of life, which Ayres considered a crucial period for sensory integration because of the brain’s receptiveness to sensations and its capacity for organizing them at this time.18 This is the period when sensorimotor functions become consolidated as a foundation for higher intellectual abilities. Although further sensory integrative development can and usually does occur beyond the eighth birthday, the changes that take place are likely to be more limited than those that occurred earlier.
In the third through seventh years, children have strong inner drives to produce adaptive responses that not only meet complicated sensorimotor demands but also sometimes require interfacing with peers. The challenges posed by children’s games and play activities attest to this complexity. In the visual-motor realm, sophistication develops through involvement in crafts, drawing and painting, constructional play with blocks and other building toys, and video games (Figure 11-6). Children are driven to explore playground equipment by swinging, sliding, climbing, jumping, riding, pushing, pulling, and pumping. Toward the end of this period they enthusiastically grapple with the motor-planning challenges posed by games such as jump rope, jacks, marbles, and hopscotch. It is also during this period that children become expert with cultural tools such as scissors, pencils, zippers, buttons, forks and knives, pails, shovels, brooms, and rakes (Figure 11-7). Many children begin to participate in occupations that present sensorimotor challenges for years to come, such as soccer, softball, karate, gymnastics, playing a musical instrument, and ballet. Furthermore, children develop the ability to organize their behavior into more complex sequences over longer time frames. This makes it possible for them to become more autonomous in orchestrating daily routines, such as getting ready for school in the morning, completing homework and other school projects, and performing household chores.

FIGURE 11-6 Adaptive responses involved in this activity require precise tactile feedback and sophisticated praxis. During activities such as this one, the preschooler becomes adept at handling tools and objects that are encountered in daily occupations throughout life. (Courtesy Shay McAtee.)
FIGURE 11-7 By the time a child reaches school age, sensory integrative capacities are almost mature. The child now can devote full attention to the demands of academic tasks because basic sensorimotor functions, such as maintaining an upright posture and guiding hand movements while holding a tool, have become automatic. (Courtesy Shay McAtee.)
As children participate in these occupations, they must frequently anticipate how to move in relation to changing environmental events by accurately timing and sequencing their actions.39 This is particularly challenging in sports when peers, with their often unpredictable moves, are involved. Their bodies are challenged to maintain balance through dynamic changes in body position. In fine motor tasks, children must efficiently coordinate visual with somatosensory information to guide eye and hand movements with accuracy and precision while maintaining a stable postural base.
Children meet these challenges with varying degrees of success. Some are more talented than others with respect to sensory integrative abilities, but most children eventually achieve a degree of competency that allows them to fully participate in the daily occupations that they are expected to do and wish to do at home, in school, and in the community. Furthermore, most children experience feelings of satisfaction and self-efficacy as they master occupations that depend heavily on sensory integration.
WHEN PROBLEMS IN SENSORY INTEGRATION OCCUR
Unfortunately, not every child experiences competency in sensory integration. When some aspect of sensory integration does not function efficiently, the child may experience stress in the course of everyday occupations because processes that should be automatic or accurate are not. It may be stressful, for example, to simply maintain balance when sitting in a chair, to get dressed in the morning before school, to attempt to play jump rope, or to eat lunch in a socially acceptable manner. The child is aware of these difficulties and becomes frustrated by frequent failure when confronted with ordinary tasks that come easily for other children. Many children with sensory integrative problems develop a tendency to avoid or reject simple sensory or motor challenges, responding with refusals or tantrums when pushed to perform. If this becomes a long-term pattern of behavior, the child may miss important experiences, such as playing games with peers, which are critical in building feelings of competency, mastering a wide repertoire of useful skills, and developing flexible social strategies. Thus, the capacity to participate fully in the occupations that the child wants to do and needs to do is compromised.
Often behavioral, social, academic, or motor coordination concerns are cited when a child with a sensory integrative dysfunction is referred for occupational therapy. The occupational therapist needs to evaluate whether a sensory processing problem may underlie these concerns. The therapist then must decide on a course of action to help the child move toward the goal of greater success and satisfaction in doing meaningful occupations. These challenges to the therapist—to identify a problem that may be hidden and to figure out how to best help the child—were the challenges to which Ayres devoted most of her career.
As mentioned previously, Ayres turned to the neurobiologic literature to give her insight into understanding children’s learning and behavior problems. Ayres also took on the responsibility of conducting research to develop her theory of sensory integration. In doing so, she produced a diagnostic system for clinical evaluation of children through the use of standardized tests. She also conducted research that was designed to evaluate the effectiveness of her treatment methods. After each study, Ayres returned to her theory to revise and refine it in light of research findings. While she was doing this, she maintained a private practice; thus, she had many years of firsthand, clinically based experience on which to ground her theoretical work.
The following sections examine the research that Ayres conducted to identify different types of sensory integrative dysfunction in children. The general categories of sensory integrative problems that concern clinicians today, based on research findings and clinical experience, are discussed. The field of sensory integration continues to be a dynamic field that changes as research generates new findings and as experiences of clinicians generate new ways of interpreting those findings.
RESEARCH BASE FOR SENSORY INTEGRATIVE PROBLEMS
Throughout her professional career, Ayres was guided by her keen observation skills and her search to reach a deeper understanding of the clinical problems that she encountered in practice. To begin answering the questions that arose as she worked with children, Ayres initiated the process of developing standardized tests of sensory integration during the 1960s. She originally developed these tests solely as research tools to aid in theory development. At the time, she was working with children with learning disabilities, many of whom she suspected had covert difficulties processing sensory information, and she sought to uncover the nature of whatever sensory integrative difficulties might exist. It was after her initial efforts at research using her tests that other therapists asked to have access to the tests, instigating their publication by Western Psychological Services.
The first group of tests Ayres created was published as the Southern California Sensory Integration Tests (SCSIT).12 These were later revised and renamed the Sensory Integration and Praxis Tests (SIPT).21 Normative data were collected on a regional scale for the SCSIT and on a national scale for the SIPT. The tests were designed to measure aspects of visual, tactile, kinesthetic, and vestibular sensory processing as well as motor planning abilities.
Using first the SCSIT and later the SIPT with samples of children, Ayres used a statistical procedure called factor analysis to develop a typology of sensory integrative function and dysfunction. Tables 11-1 and 11-2 summarize results of her factor analytic studies, along with results of several studies conducted by other researchers. In factor analysis, sets of test scores are grouped according to their associations with one another. The resulting groups of associated test scores are called factors. Ayres interpreted the factors that emerged from her studies as representative of neural substrates underlying learning and behavior in children. For example, in her 1965 study, Ayres found that the tactile tests correlated highly with the motor planning tests, forming a factor.5 She hypothesized that there is an ability called motor planning that depends on somatosensory processing and influences one’s interactions with the physical world. Apraxia is the term she used to identify a disorder in this ability. In her later work, she subsumed the notion of motor planning under the construct of praxis and replaced the term apraxia with dyspraxia when referring to children.
TABLE 11-1
Purpose, Methods, Results, and Contributions of Studies of Sensory Integrative Patterns
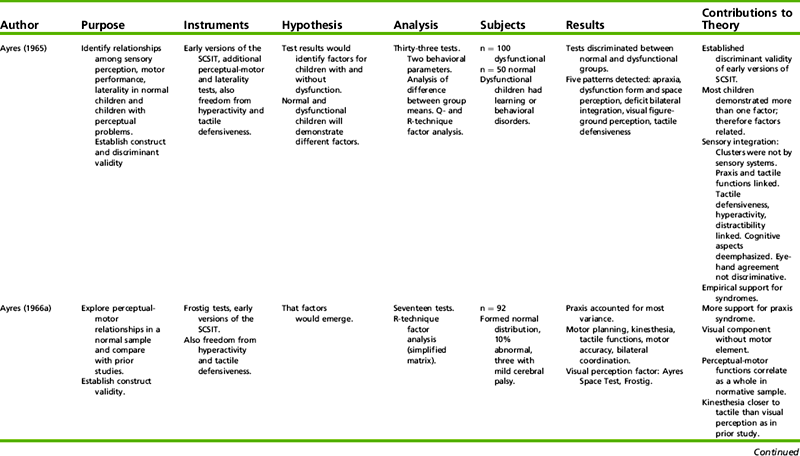
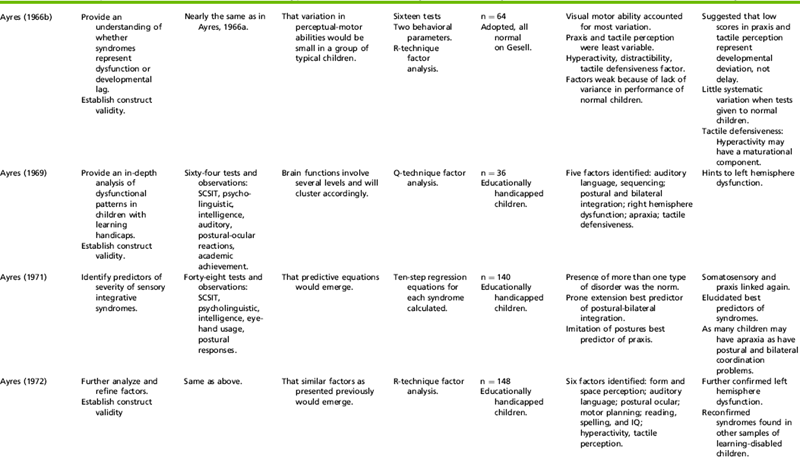
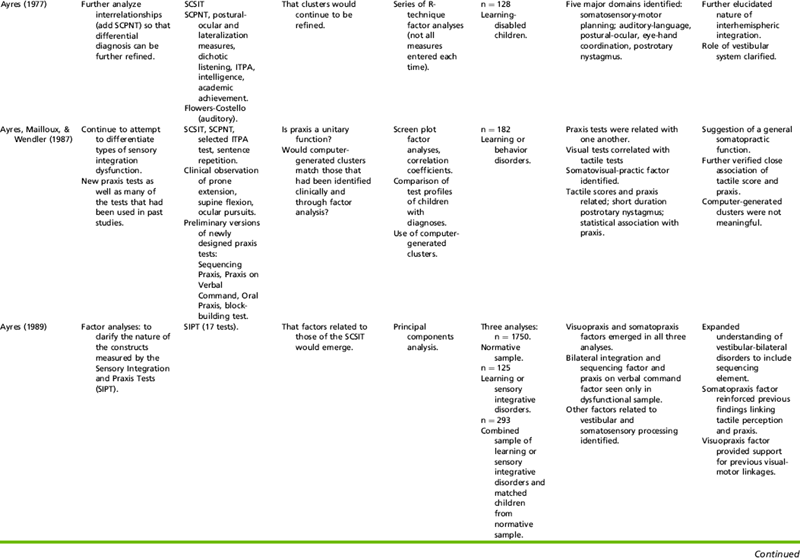
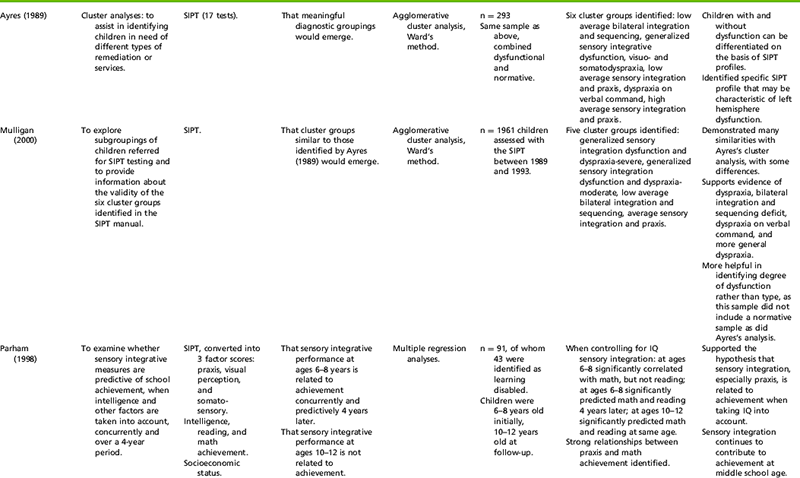
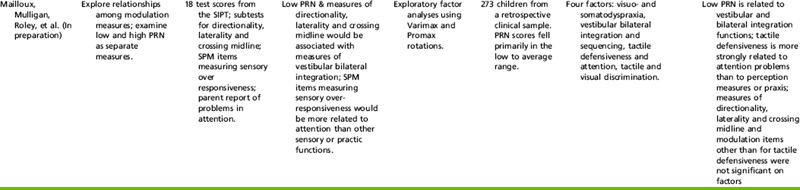
CFA, Confirmatory factor analysis; ITPA, Illinois Test of Psycholinguistic Abilities; SCPNT, Southern California Postrotary Nystagmus Test; SCSIT, Southern California Sensory Integration Test; SIPT, Sensory Integration and Praxis Tests; SEM, structural equation modeling.
Ayres, A. J. (1965). Patterns of perceptual-motor dysfunction in children: a factor analytic study. Perceptual and Motor Skills, 20, 335-368. Ayres, A. J. (1966a). Interrelationships among perceptual-motor functions in children. American Journal of Occupational Therapy, 20, 68-71. Ayres, A. J. (1966b). Interrelations among perceptual-motor abilities in a group of normal children. American Journal of Occupational Therapy, 20, 288-292. Ayres, A. J. (1969). Deficits in sensory integration in educationally handicapped children. Journal of Learning Disabilities, 2(3), 44-52. Ayres, A. J. (1971). Characteristics of types of sensory integrative dysfunction. American Journal of Occupational Therapy, 25, 329-334. Ayres, A. J. (1972). Types of sensory integrative dysfunction among disabled learners. American Journal of Occupational Therapy, 26, 13-18. Ayres, A. J. (1977). Cluster analyses of measures of sensory integration. American of Journal of Occupational Therapy, 31, 362-366. Ayres, A. J., Mailloux, Z., & Wendler, C.L.W. (1987). Development apraxia: is it a unitary function Occupational Therapy Journal of Research, 7, 93-110. Ayres, A. J. (1989). Sensory Integration and Praxis Tests manual. Los Angeles: Western Psychological Services. Mailloux, Z., Mulligan, S., & Roley, S. S., et al. (2009). Verification and clarification of patterns of sensory integrative dysfunction (manuscript in progress). Mulligan, S. (2000). Cluster analysis of scores of children on the Sensory Integration and Praxis tests. Occupational Therapy Journal of Research, 20, 256-270. Parham, L. D. (1998). The relationship of sensory integrative development to achievement in elementary students: Four-year longitudinal patterns. Occupational Therapy Journal of Research, 18, 105-127.
TABLE 11-2
Factors and Clusters Identified in Research
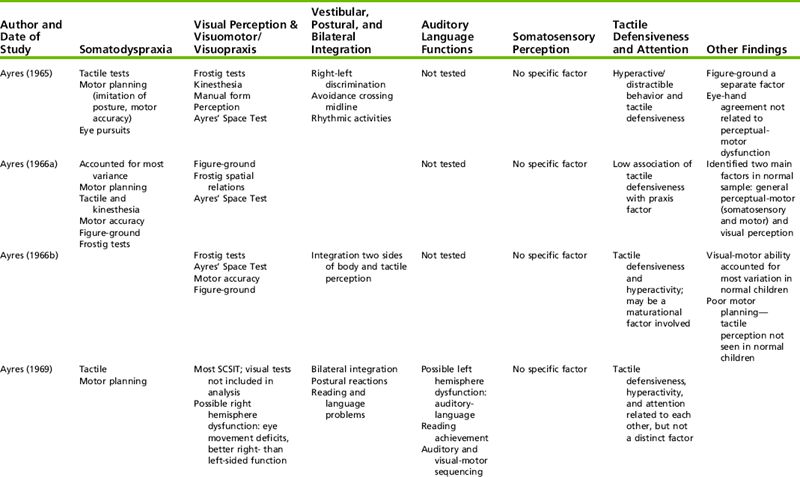
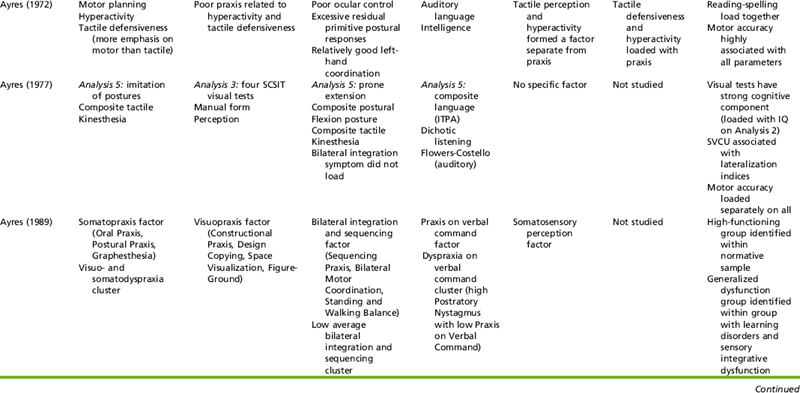
ITPA, Illinois Test of Psycholinguistic Abilities; SCSIT, Southern California Sensory Integration Test; SVCU, Space Visualization Contralateral Use.
Ayres, A.J. (1965). Patterns of perceptual-motor dysfunction in children: A factor analytic study. Perceptual and Motor Skills, 20, 335-368. Ayres, A.J. (1966a). Interrelationships among perceptual-motor functions in children. American Journal of Occupational Therapy, 20, 68-71. Ayres, A.J. (1966b). Interrelations among perceptual-motor abilities in a group of normal children. American Journal of Occupational Therapy, 20, 288-292. Ayres, A.J. (1969). Deficits in sensory integration in educationally handicapped children. Journal of Learning Disabilities, 2(3), 44-52. Ayres, A.J. (1972). Types of sensory integrative dysfunction among disabled learners. American Journal of Occupational Therapy, 26, 13-18. Ayres, A.J. (1977). Cluster analyses of measures of sensory integration. American Journal of Occupational Therapy, 31, 362-366. Ayres, A.J. (1989). Sensory Integration and Praxis Tests manual. Los Angeles: Western Psychological Services. Mailloux, Z., Mulligan, Smith, Roley (in prep).Mulligan, S. (1998). Patterns of sensory integration dysfunction: A confirmatory factor analysis. American Journal of Occupational Therapy, 52, 819-828. Mulligan, S. (2000). Cluster analysis of scores of children on the Sensory Integration and Praxis tests. Occupational Therapy Journal of Research, 20, 256-270.
In her last set of analyses with the SIPT, just before her death in 1988, Ayres used both factor analysis and another statistical technique called cluster analysis, which groups together children with similar SIPT profiles (see Table 11-1). This approach was used to further carve out diagnostic groupings of children that might be useful clinically. Today, consideration of both factor analysis and cluster groupings is a critical component in the interpretation of a child’s SIPT scores.
Through the years as Ayres conducted her studies with different groups of children, she continually revisited her theory, bringing along new hypotheses based on new research results. Of particular interest were the patterns that recurred despite being generated from different samples of children. Among the most consistent findings was that children who had been identified as having learning or developmental problems often displayed difficulties in more than one sensory system. Ayres interpreted this finding in light of the neurobiologic literature on intersensory integration, which indicates that the sensory systems tend to function synergistically with each other rather than in isolation.11 Thus, the idea of intersensory integration as critical to human function became one of the major tenets of sensory integration theory.
Another finding, which emerged in early studies and in later SIPT studies, was that some patterns of scores were seen only in groups of children who had been identified as having disorders. In other words, some factors were not evident in typically developing children at any age. This led to the proposal that the sensory integrative problems associated with these particular patterns were representative of neural dysfunction rather than developmental lag.
Yet another recurrent pattern was a relationship between tactile perception and praxis scores. This association appeared repeatedly in her studies and led Ayres to theorize that the tactile system contributes importantly to the development of efficient practic functions. The robustness of this finding across many studies influenced Ayres to emphasize the relationship between the tactile system and praxis, a relationship that has become a cornerstone of sensory integration theory.
Throughout her research, several patterns emerged that Ayres suspected were related to a discrete involvement of cortical rather than brainstem or intersensory dysfunction. Ayres came to view these types of problems as different than those classified as sensory integrative disorders and less likely to be responsive to the treatment techniques that she was developing. An example is the association of low Praxis on Verbal Command scores with high postrotary nystagmus scores. Praxis on Verbal Command is the only test on the SIPT with a strong language comprehension component. Postrotary nystagmus is a test that may reflect cortical dysfunction if scores are extremely high. In this example, it is hypothesized that an underlying cortical dysfunction, possibly involving the left hemisphere (where language centers are located), is responsible for the pattern of scores. Ayres did not view this particular pattern as a sensory integrative dysfunction, although it might be detected by her tests.
In spite of small sample sizes, Ayres found similar factors across multiple studies (see Tables 11-1 and 11-2). Many of these findings were replicated by Mulligan (1998) in a confirmatory factor analytic study of more than 10,000 children. Mailloux, Mulligan, Smith Roley, et al. found a very close replication of the same factors identified by Ayres.96 In a study of children with suspected sensory integrative problems, factors emerged that reflected associations among (1) visual and tactile perception with praxis, (2) vestibular and proprioceptive processing with bilateral functions, (3) attention and tactile defensiveness, and (4) visual and tactile discrimination. The robustness of some of these findings across many studies strengthens the hypothesis that they reflect underlying patterns of function.
Ayres conducted her factor and cluster analyses to shed light on the types of sensory integrative dysfunctions that children experience, yet she did not view the resulting typologies as specific diagnostic labels to pin on individual children. Rather, the typologies were seen as general patterns exhibited time after time by groups of children who were struggling in school or with some other aspect of behavior or development. They provide the therapist with relevant information to consider when conducting clinical assessments. They do not provide prefabricated slots in which to fit children. Ultimately, the important job of interpreting an individual child’s pattern of scores in relation to his or her unique life situation lies in the purview of the therapist’s judgment, using research, training, and experience to guide decision making.
SENSORY INTEGRATIVE PROBLEMS
The results of research, combined with the experiences of clinicians and the work of scholars in the field, have generated many different ways of conceptualizing sensory integrative problems over the past 30 years. The complexity of this domain can be daunting for the novice therapist, but is also a reflection of the growth in knowledge in this field. The terms sensory integrative disorder, sensory integrative dysfunction, and sensory integrative problems do not refer to one specific type of difficulty but describe a heterogeneous group of problems that are thought to reflect subtle neural differences involving multisensory and motor systems.
Most discussions of sensory integrative problems assume normal sensory receptor function. In other words, sensory integrative problems involve central, rather than peripheral, sensory functions. This assumption has been supported in several well-designed studies. For instance, Parush, Sohmer, Steinberg, and Kaitz found that the somatosensory-evoked potentials of children with attention deficit–hyperactivity disorder (ADHD) differ from those of typically developing children with respect to indicators of central tactile processing but not peripheral receptor responses.119 Many of the children with ADHD in this study were also identified as having tactile defensiveness, a sensory integrative problem. In another study, researchers found that children with learning disabilities, compared with nondisabled children, had impaired postural responses involving central integration of vestibular, proprioceptive, and visual inputs, whereas measures of peripheral receptor functions were normal.142 Thus, when sensory integrative problems involving the vestibular system are discussed, these problems are generally thought to be based within CNS structures and pathways (i.e., the vestibular nuclei and its connections) rather than the vestibular receptors (i.e., the semicircular canals, utricle, or saccule).159 In this chapter, the discussions of sensory integrative problems assume that peripheral function is normal.
As noted previously, different conceptualizations of sensory integrative problems have been generated over the years. Although perfect consensus on how to categorize these problems does not exist, clearly there are recurring themes across authors. Distinct but overlapping taxonomies of sensory integrative problems include, for example, those of Bundy and Murray39 and Kimball.81 Bundy and Murray presented a taxonomic model that depicts sensory integrative dysfunction as manifested in two major ways: poor sensory modulation and poor praxis.39 Miller, Anzalone, Lane, Cermak, and Osten proposed a nosology of Sensory Processing Disorders (SPD) that includes three main types of disorder: sensory modulation disorder, sensory-based motor disorder, and sensory discrimination disorder.105 Subtypes within their category of sensory modulation disorder are overresponsivity, underresponsivity, and sensory seeking. Subtypes within their sensory-based motor disorder category include postural disorders and dyspraxia.
For the purposes of this chapter, sensory integrative problems are divided into four general categories:
1. Sensory modulation problems
2. Poor sensory discrimination and perception
These four categories are used here because they are consistent with the research data available at this time. Although variations were reported across studies, these patterns emerged in research on different samples of children over many decades. This research indicated that the patterns are interrelated and often coexist in individual children. When planning intervention, occupational therapists need to carefully analyze assessment data to discern whether one or more specific patterns of sensory integration problems seem to be affecting an individual child’s participation in activities. Each of the main categories of sensory integration problems is presented in the next section.
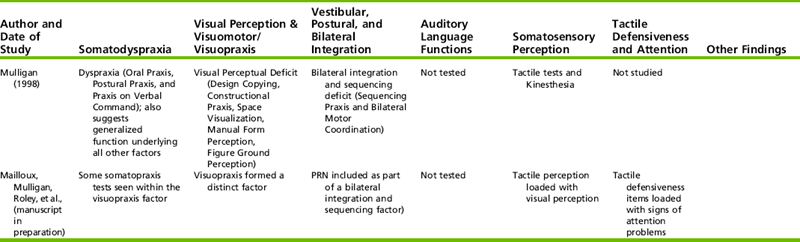
Sensory Modulation Problems
Modulation refers to CNS regulation of its own activity.18 The term sensory modulation refers to the tendency to generate responses that are appropriately graded in relation to incoming sensory stimuli, rather than underreacting or overreacting to them. Cermak45 and Royeen131 hypothesized that there is a continuum of sensory responsivity, with hyporesponsivity at one end and hyperresponsivity at the other. An optimal level of arousal and orientation lies in the center of the continuum (Figure 11-8). This is where most activity falls for most individuals, although everyone experiences fluctuations across this continuum of sensory responsivity in the course of a day. In the continuum model, dysfunction is indicated when the fluctuations within an individual are extreme or when an individual tends to function primarily at one extreme of the continuum or the other. The individual who tends to function at the extremely underresponsive end of the continuum may fail to notice sensory stimuli that would elicit the attention of most people. This characteristic often is identified as a problem in sensory registration. At a less severe degree of underresponsiveness, the individual notices sensory stimuli, but is slow to respond or seems to crave intense sensory input. At the opposite extreme of the continuum is the overresponsive individual with sensory defensiveness. This person is overwhelmed and overstressed by ordinary sensory stimuli.
FIGURE 11-8 Continuum of sensory responsivity and orientation. Modified from Royeen, C. B., & Lane, S. J. [1991]. Tactile processing and sensory defensiveness. In A. G. Fisher, E. A. Murray, & A. C. Bundy [Eds.], Sensory integration: Theory and practice. Philadelphia: F.A. Davis.
Originally, Ayres thought of sensory registration problems as different in nature from sensory modulation problems such as tactile defensiveness.18 Soon after she introduced the concept of sensory registration, however, other experts in the field of sensory integration suggested that sensory registration and tactile defensiveness might be related through common underlying neural functions.66,134 This idea contributed to the continuum model. Experts soon found that this simple continuum model did not adequately address the complexity of child behaviors, however. For example, Royeen and Lane hypothesized that the relationship between underresponsiveness and overresponsiveness may be circular instead of linear, because a child who is extremely defensive may be overloaded to the point of shutting down and becoming underresponsive.134 Previously, we have criticized the continuum model as overly simplistic because sensory modulation very likely is influenced by the individual’s history of personal experiences and interpretation of the situation, as well as interactions among multiple neural systems.117 Furthermore, individuals who are unusually underresponsive to input from one sensory system may tend to be overresponsive in another system. For example, a child may be overresponsive to touch, but at the same time be underresponsive to vestibular sensations. The continuum model does not account for this phenomenon.
Dunn presented a conceptual model that takes into account the potential roles of various neural processes in generating patterns of underresponsiveness and overresponsiveness (Figure 11-9).61,63 In her model, four main patterns represent individual differences in sensory responding: low registration, sensation seeking, sensitivity to stimuli, and sensation avoiding. Dunn hypothesized these patterns emerge from individual differences in the neural processes of habituation, sensitization, threshold, and maintenance of homeostasis. The person who falls in the low-registration quadrant of the model is underresponsive due to a high threshold for reactivity and therefore needs to have a high level of intensity in environmental stimuli in order to notice and attend. The person who falls in the sensation-seeking quadrant is also considered underresponsive with a high threshold but expresses this behaviorally by actively seeking out intense sensory input. The sensory sensitivity and sensation-avoiding quadrants represent overresponsive patterns. Individuals who fall in the sensory sensitivity quadrant have heightened awareness of, and are distracted by, sensory stimuli due to a low threshold, but they tend to passively cope with these sensations. In contrast, those who are sensation-avoiding not only have heightened awareness of sensory stimuli but actively attempt to avoid the ordinary sensations that they experience as noxious. One of the most important contributions of this model is that it can be used to consider what kinds of work and play or leisure environments present an optimal match for an individual’s sensory modulation characteristics.63
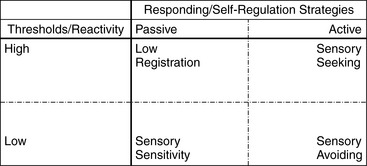
FIGURE 11-9 Dunn’s Model of Sensory Processing. Adapted from Dunn, W. [1997]. The impact of sensory processing abilities on the daily lives of young children and families: A conceptual model. Infants and Young Children, 9[4] 23-25.
In another model that addresses the complexity of sensory modulation, Miller, Reisman, McIntosh, and Simon differentiate between physiologic and behavioral elements of what they call sensory modulation disorders (SMDs).107 Their ecologic model includes both external and internal dimensions affecting sensory modulation (Figure 11-10). External dimensions identified are culture, environment, relationships, and tasks, whereas internal dimensions are sensory processing, emotion, and attention. The external dimensions highlight the importance of context, whereas the internal dimensions focus on enduring differences among individuals. In this model, external and internal dimensions are interlinked through multidirectional, rather than linear, relationships and must be viewed together to design interventions for children with SMDs.
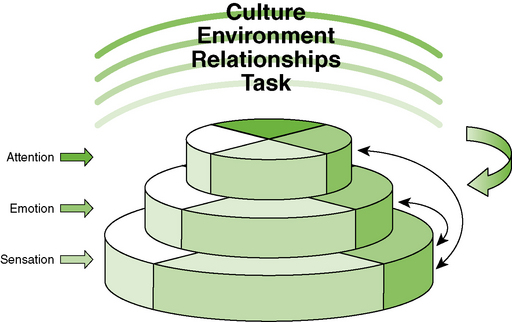
FIGURE 11-10 Miller et al.’s (2001) Ecological Model of Sensory Modulation. Light shading, underresponsivity; medium shading, normal responsivity (a match between the external and internal dimensions); dark shading, overresponsivity; darkest shading, lability, severe overresponsivity alternating with severe underresponsivity. The Ecological Model of Sensory Modulation. Note. From Roley, S. S., Blanch, E. I., Scharr, R. C. (2001). Understanding the nature of sensory integration with diverse populations (p. 61). Austin, TX: PRO-ED. Copyright 2001 by PRO-ED, Inc., Reprinted with permission.
These models of sensory modulation help us to organize the complex information relevant to understanding children with difficulties in overresponding or underresponding to sensory information in everyday situations. Many unanswered questions about modulation remain. For example, some research indicates that many children frequently demonstrate behavioral characteristics of both underresponding and overresponding, often within the same sensory system.86 This may be particularly the case for children with autism.87,148 Existing models do not yet do an adequate job of explaining these phenomena. Nevertheless, these models are important because they provide a foundation upon which research programs can be built to explicate the complex issues that are involved. Today, research on patterns of sensory modulation and their manifestations in everyday activities is an area of focused investigation in occupational therapy.28,67,107 In addition, the relationship between physiologic measures and patterns of behavior that characterize sensory modulation problems continues to be explored—for example, through studies of brain electrical activity57 and autonomic responses106,137 to sensory input.
Although there remains much to learn about sensory modulation, a general consensus exists among sensory integration experts regarding the behaviors that characterize different kinds of sensory modulation difficulties. These behaviors are described next.
Sensory Registration Problems
As noted previously in this chapter, sensory integration is the “organization of sensory input for use” (p. 184).18 However, before sensory information can be used functionally, it must be registered within the CNS. When the CNS is working well, it knows when to “pay attention” to a stimulus and when to “ignore" it. Most of the time, this process occurs automatically and efficiently. For example, a student may not be aware of the noise of traffic outside the window of a classroom while listening to a lecture, instead focusing attention on the sound of the lecturer’s words. In this situation, the student registers the auditory stimuli generated by the lecturer but not the stimuli generated by the traffic. The process of sensory registration is critical in enabling efficient function so that people pay attention to those stimuli that enable them to accomplish desired goals. Simultaneously, if the process is working well, energy is not wasted attending to irrelevant sensory information.
Traditionally, occupational therapists, beginning with Ayres,18 have used the term sensory registration problem to refer to the difficulties of the person who frequently fails to attend to or register relevant environmental stimuli. This kind of problem is often seen in individuals with autism, but it may also be seen in other individuals with developmental problems. When a sensory registration problem is present, the child often seems oblivious to touch, pain, movement, taste, smells, sights, or sounds. Usually more than one sensory system is involved, but for some children one system may be particularly affected. Sometimes the same child who does not register relevant stimuli may be overfocused on irrelevant stimuli; this is commonly seen with autism. It is also common for children with severe developmental problems, such as autism, to lack sensory registration in some situations but react with extreme sensory defensiveness in other situations.
Safety concerns are frequently an important issue among children with sensory registration problems. For example, the child who does not register pain sensations has not learned that certain actions naturally lead to negative consequences, such as pain, and therefore may not withdraw adequately from dangerous situations. Instead of avoiding situations likely to result in pain, the child may repeatedly engage in activities that may be injurious, such as jumping from a dangerous height onto a hard surface or touching a hot object. Other children with sensory registration problems may not register noxious tastes and smells that warn of hazards. Similarly, sights and sounds such as sirens, flashing lights, firm voice commands, and hand signals or signs that are meant to warn of perils go unheeded if not registered. This can be a life-endangering problem in some circumstances (e.g., when a child steps in front of a moving car).
A sensory registration problem interferes with the child’s ability to attach meaning to an activity or situation. Consequently, in severe cases, the child lacks the inner drive that compels most children to master ordinary childhood occupations (e.g., the child who is generally unmotivated to engage in play activities or to practice skills). Therefore the long-term effects on the child’s development can be profound.
Sensation-Seeking Behavior
Some children register sensations, but may be “underresponsive” to the incoming stimuli. These children seem to seek intense stimulation in the sensory modalities that are affected. The child who is hyporesponsive to vestibular stimuli may seek large quantities of intense stimulation when introduced to suspended equipment in a clinic setting. This child registers the vestibular sensations and usually shows signs of pleasure from the sensations, but the input does not affect the nervous system to the extent that it does for most other children. The underresponsive child may not become dizzy or show the expected autonomic responses to stimulation that is so intense it would be overwhelming for most peers. This is called hyporesponsivity because it refers to the underlying mode of sensory processing rather than to observable motor behavior. Although the child may appear to be active motorically, the child is not reacting to intense vestibular stimuli to the degree that most children do. In everyday settings, these children often appear to be restless, motorically driven, and thrill seeking.
Some children seem to seek greater than average amounts of proprioceptive input. Typically these children often seek active resistance to muscles, deep touch pressure stimulation, or joint compression and traction (e.g., by stomping instead of walking; intentionally falling or bumping into objects, including other people; or pushing against large objects). They may tend to use strong ballistic movements such as throwing objects forcefully. Some of these children may not seem to register the positions of body parts unless intense proprioceptive stimulation is present.
Some children who seek large amounts of proprioceptive input demonstrate signs of tactile defensiveness or gravitational insecurity. Because proprioception is thought to have an inhibitory effect on tactile and vestibular sensations, these children may be seeking increased proprioceptive input in order to help themselves modulate the overwhelming touch and movement sensations that they often experience.
The behaviors generated by sensation-seeking children may be disruptive or inappropriate in social situations. Safety issues frequently are of paramount concern, and often these children are labeled as having social or behavioral problems. A challenge for the occupational therapist working with these children may be to identify strategies by which they can receive the high levels of stimulation that they seek without being socially disruptive, inappropriate, or dangerous to themselves or others.
Overresponsiveness
At the opposite end of the sensory modulation continuum are problems associated with overresponsiveness, sometimes called hyperresponsivity or sensory defensiveness. The child who is overresponsive is overwhelmed by ordinary sensory input and reacts defensively to it, often with strong negative emotion and activation of the sympathetic nervous system. This condition may occur as a general response to all types of sensory input, or it may be specific to one or a few sensory systems.
The term sensory defensiveness was first introduced by Knickerbocker84 and later used by Wilbarger and Wilbarger152 to describe sensory modulation disorders involving multisensory systems. Sensory modulation problems include overreactions to touch, movement, sounds, odors, and tastes, any of which may create discomfort, avoidance, distractibility, and anxiety. Most of the research-based and clinical knowledge regarding overresponsiveness is related to the tactile and vestibular systems.
Tactile Defensiveness: Tactile defensiveness involves a tendency to overreact to ordinary touch sensations.4,11,18 It is one of the most commonly observed sensory integrative disorders involving sensory modulation. Individuals with tactile defensiveness experience irritation and discomfort from sensations that most people do not find bothersome. Light touch sensations are especially likely to be disturbing. Common irritants include certain textures of clothing, grass or sand against bare skin, glue or paint on the skin, the light brush of another person passing by, the sensations generated when having one’s hair or teeth brushed, and certain textures of food. Common responses to such irritants include anxiety, distractibility, restlessness, anger, throwing a tantrum, aggression, fear, and emotional distress.
Common self-care activities such as dressing, bathing, grooming, and eating are often affected by tactile defensiveness. Classroom activities such as finger painting, sand and water play, and crafts may be avoided. Social situations involving close proximity to others, such as playing near other children or standing in line, tend to be uncomfortable and may be disturbing enough to lead to emotional outbursts. Thus, ordinary daily routines can become traumatic for children with tactile defensiveness and for their parents. Teachers and friends are likely to misinterpret the child with tactile defensiveness as being rejecting, aggressive, or simply negative.
It is difficult for individuals with tactile defensiveness to cope with the fact that others do not share their discomforts and may actually enjoy situations that they find so upsetting. For a child with this disorder, who may not be able to verbalize or even recognize the problem, the accompanying feelings of anxiety and frustration can be overwhelming and the influence on functional behavior is likely to be significant.
An occupational therapist working with a child who is tactually defensive must become aware of the specific kinds of tactile input that are aversive and the kinds that are tolerated well by that particular child. Usually light touch stimuli are aversive, especially when they occur in the most sensitive body areas such as the face, abdomen, and palmar surfaces of the upper and lower extremities. Generally, tactile stimuli that are actively self-applied by the child are tolerated much better than stimuli that are passively received, as when being touched by another person. Tactile stimuli may be especially threatening if the child cannot see the source of the touch. Most individuals with tactile defensiveness feel comfortable with deep touch stimuli and may experience relief from irritating stimuli when deep pressure is applied over the involved skin areas.
Knowledge of these characteristics of tactile defensiveness helps the occupational therapist identify strategies that help the child and others who interact with the child to cope with this condition. For example, the occupational therapist may recommend to the teacher that if the child needs to be touched, it should be done with firm pressure in the child’s view, rather than with a light touch from behind the child.
Gravitational Insecurity: Gravitational insecurity is a form of overresponsiveness to vestibular sensations, particularly sensations from the otolith organs, which detect linear movement through space and the pull of gravity.18 Children with this problem have an insecure relationship to gravity characterized by excessive fear during ordinary movement activities. The gravitationally insecure child is overwhelmed by changes in head position and movement, especially when moving backward or upward through space. Fear of heights, even those involving only slight distances from the ground, is a common problem associated with this condition.
Children who display gravitational insecurity often show signs of inordinate fear, anxiety, or avoidance in relation to stairs, escalators or elevators, moving or high pieces of playground equipment, and uneven or unpredictable surfaces. Some children are so insecure that only a small change from one surface to another, as when stepping off the curb or from the sidewalk to the grass, is enough to send them into a state of high anxiety or panic.
Common reactions of children with gravitational insecurity include extreme fearfulness during low-intensity movement or when anticipating movement and avoidance of tilting the head in different planes (especially backward). They tend to move slowly and carefully, and they may refuse to participate in many gross motor activities. When they do engage in movement activities such as swinging, many of these children refuse to lift their feet off the ground. When threatened by simple motor activities, they may try to gain as much contact with the ground as possible or they may tightly clutch a nearby adult for security. These children often have signs of poor proprioception in addition to the vestibular overresponsiveness. May-Benson and Koomar developed a Gravitational Insecurity (GI) Assessment and found that scores on this standardized tool, which involves activities such as performing a backward roll and stepping off a chair with eyes closed, significantly discriminated between children with gravitational insecurity and typical children.101
Playground and park activities are often difficult for children with gravitational insecurity, as are other common childhood activities such as bicycle riding, ice skating, roller skating, skateboarding, skiing, and hiking. Ability to play with peers and to explore the environment is therefore significantly affected. Functioning in the community may also be affected when the child needs to use escalators, stairs, and elevators.
A distinction may be made between gravitational insecurity and a similar condition called postural insecurity. Postural insecurity was the term Ayres originally used to refer to all children with fears related to movement. Later, however, she hypothesized that some children moved slowly and displayed fears of movement not because of a hyperresponsivity to vestibular input but because they lacked adequate motor control to perform many activities without falling. The fears of these children, then, seemed to be based on a learned, realistic appraisal of their motor limitations. The term posturally insecure is used to refer to these children.
Often it is difficult to discern whether a child’s anxiety is based on sensory overresponsivity or limited motor control because these two conditions can, and often do, coexist in the same child. Sometimes, however, the distinction is clear. Children with mild spastic diplegia, for example, commonly have postural but not gravitational insecurity. These children typically (and appropriately) react with anxiety when faced with a minimal climbing task; however, they may show pleasure at receiving vestibular stimulation, including having the head radically tilted in different planes so long as they are securely held and do not have to rely on their own motor skills to maintain a safe position.
Overresponsiveness in Other Sensory Modalities: Hyperresponsivities in other sensory systems can also have a significant influence on a person’s life. For example, overreactions to sounds, odors, and tastes are often problematic for children with heightened sensitivities. These types of problems, like overresponsiveness to touch and movement, may create discomfort, avoidance, distractibility, and anxiety. Most people interpret the raucous sounds found at birthday parties, parades, playgrounds, and carnivals as happy sounds, but these can be overwhelming to a child with auditory defensiveness. A visually busy and unfamiliar environment may evoke an unusual degree of anxiety in a child with visual defensiveness. Similarly, the variety of tastes and odors encountered in some environments may be disturbing to a child with overresponsivity in these systems.
Sensory Discrimination and Perception Problems
Sensory discrimination and perception allow for refined organization and interpretation of sensory stimuli. Some types of sensory integrative disorders involve inefficient or inaccurate organization of sensory information (e.g., difficulty differentiating one stimulus from another or difficulty perceiving the spatial or temporal relationships among stimuli). A classic example involving the visual system is that of the older child with a learning disability who persists in confusing a b with a d. A child with an auditory discrimination problem may be unable to distinguish between the sounds of the words doll and tall. A child with a tactile perception problem may not be able to distinguish between a square block and a hexagonal block using touch only, without visual cues.
Some children with perceptual problems have no difficulty with sensory modulation. However, modulation problems often coexist with perceptual problems. It makes sense that these two types of problems are associated. A child who often does not register stimuli probably has a deficit in perceptual skills because of a lack of experience interacting with sensory information. Conversely, the child who has sensory defensiveness may exert a lot of energy trying to avoid certain sensory experiences. Defensive reactions may make it difficult to attend to the detailed features of a stimulus and thereby may impede perception.
Discrimination or perception problems can occur in any sensory system. They are best detected by standardized tests, except in the case of proprioception, which is difficult to measure in a standardized manner. Discrimination or perception problems can occur in any sensory system. They are best detected by standardized tests, except in the case of proprioception, which is difficult to measure in a standardized manner. Although most factor analytic studies of the SIPT test scores revealed patterns that linked sensory perception with motor functions, certain patterns reflected specific sensory perception factors (e.g., a visual form and space perception factor or a tactile perception factor, as well as a somatosensory perception factor). Professionals in many fields, such as neuropsychology, special education, and speech language pathology, are trained to evaluate perceptual problems, and their focus usually is on the visual and auditory systems. In contrast, occupational therapists are unique in their understanding of the functional relevance of lesser known areas of sensory perception such as tactile, kinesthetic, and vestibular sensory processing.
Tactile Discrimination and Perception Problems
Poor tactile perception is one of the most common sensory integrative disorders. Children with this disorder have difficulty interpreting tactile stimuli in a precise and efficient manner. For example, they may have difficulty localizing precisely where an object has brushed against them or using stereognosis to manipulate an object that is out of sight. Fine motor skills are likely to suffer when a tactile perception problem is present, especially if tactile defensiveness is also present.44
As discussed previously, the tactile system is a critical modality for learning during infancy and early childhood. Tactile exploration using the hands and mouth is particularly important. If tactile perception is vague or inaccurate, the child is at a disadvantage in learning about the different properties of objects and substances. It may be difficult for a child with such problems to develop the manipulative skills needed to efficiently perform tasks such as connecting pieces of constructional toys, fastening buttons or snaps, braiding hair, or playing marbles. Inadequate tactile perception also interferes with the feedback that is normally used to precisely guide motor tasks such as writing with a pencil, manipulating a spoon, or holding a piece of paper with one hand while cutting with the other.
Tactile perception is associated with visual perception24; thus, it is fairly common to see children with problems in both of these sensory systems. Not surprisingly, these children tend to have concomitant problems with hand–eye coordination. A discrete somatosensory perception factor emerged as a pattern in analyses of the SIPT,21 but a more striking finding in the factor analytic studies of sensory integration tests over many decades was the link between tactile perception and motor planning, which recurred in many different studies.5–7,9,10,16,24,111 These findings led Ayres to hypothesize that tactile perception is an important contributor to the ability to plan actions. She speculated that the tactile system is responsible for the development of body scheme, which then becomes an important foundation for praxis.
Ordinarily, tactile perception operates at such an automatic level that, when it is impaired, compensation strategies take a great deal of energy. An example of this is that of the child who cannot make the subtle manipulations needed to fasten a button without looking at it. Because this child needs to use compensatory visual guidance, the task of buttoning, which is usually performed rapidly and automatically, becomes tedious, tiring, and frustrating. The necessity of using such compensatory strategies throughout the day tends to interrupt the child’s ability to focus on the more complex conceptual and social elements of tasks and situations.
Proprioception Problems
Another type of perceptual problem involves proprioception, which arises from the muscles and joints to inform the brain about the position of body parts. This is a difficult area to research because direct standardized measures of proprioception are not available. However, the experience of many master clinicians suggests that many children have serious difficulties interpreting proprioceptive information.
Children who do not receive reliable information about body position often appear clumsy, distracted, and awkward. As with poor tactile perception, these children must often rely on visual cues or other cognitive strategies (e.g., use of verbalizations) to perform simple aspects of tasks, such as staying in a chair or using a fork correctly. Other common attributes of children with poor proprioception include using too much or too little force in activities such as writing, clapping, marching, or typing. Breaking toys, bumping into others, and misjudging personal space are other consequences of poor proprioception that which have strong social implications.
Many children thought to have proprioception problems seek firm pressure to their skin or joint compression and traction. These sensation-seeking behaviors may be an attempt to gain additional feedback about body position, or they may reflect a concomitant hyporesponsiveness to tactile and proprioceptive sensations. In any case, if these behaviors are done in socially inappropriate ways or at inopportune times, such as leaning on another child during circle time or hanging from a doorway at school, the child’s behavior may be misinterpreted as being willfully disruptive.
Visual Perception Problems
Visual perception is an important factor in the competent performance of many constructional play activities and fine motor tasks. Early factor analyses of sensory integration test scores revealed a form and space perception factor. Tests are available to measure figure-ground perception, spatial orientation, depth perception, and visual closure, to name just a few of the many aspects of visual perception that have been of concern to professionals in many disciplines.
Problems with visual perception are commonly seen in children with sensory integrative disorders, particularly when poor tactile perception or dyspraxia is present.21,24 Whereas some children have only a specific visual perception problem without any other sign of a sensory integrative dysfunction, many others have difficulties in visual perceptual abilities as a component of broader sensory integration difficulties. Henderson, Pehoski, and Murray point out the many relationships between visual spatial abilities and functions such as grasp, balance, locomotion, construction, and cognition.73 As these authors note, low scores on tests of visual perception can occur for a variety of reasons and in some cases will represent a problem that therapists would not view as reflective of a sensory integrative issue.
A sensory integrative treatment approach, as described later in this chapter, may be appropriate for the child who demonstrates visual perception problems along with other indicators of sensory integrative difficulties, such as poor tactile perception or praxis. A sensory integration approach may not be appropriate for children who show discrete visual perceptual problems. When other sensory integration issues are not present or have been resolved with intervention, the occupational therapist may choose to work with the child using another treatment approach, such as visual perception training, use of compensatory strategies, or skill training in specific activities.
Other Perceptual Problems
Many other dimensions of perception and sensory discrimination exist. For example, perception of movement through space involves the integration of vestibular, proprioceptive, and visual integration and may be affected in children with vestibular-proprioceptive problems. Auditory perception is an important function that may, when impaired, contribute to sensory integrative disorders in some children. Central auditory processing disorders recently have received increasing attention in the literature, and some authors have suggested that more attention should be given to the role of the auditory system in the sensory integration literature.41 However, since so much of the function of the auditory system is related to the functions of hearing, speech, and language, this area of study in sensory integration may be most appropriately pursued in collaboration with speech–language pathologists and audiologists. Although auditory perception problems are not usually considered to be a type of sensory integrative dysfunction when seen in isolation, difficulties with auditory perception and language development often coexist with signs of sensory integrative dysfunction. The relationship between these processes warrants further research.
Vestibular-Proprioceptive Problems
In her research, Ayres identified a pattern of problems thought to reflect inefficient central vestibular processing. Clinical signs related to this type of problem involve the motor functions that are outcomes of vestibular processing, such as poor equilibrium reactions and low muscle tone, particularly of the extensor muscles, which are strongly influenced by the vestibular system. These disorders are assessed using informal and formal clinical observations and standardized test scores.
Different names have been applied to vestibular processing problems at different points in time because of the changing patterns of research findings. In her early factor analytic studies, Ayres identified a linkage between postural-ocular mechanisms and integration of the two sides of the body. Clinically, she called the related dysfunction a disorder in postural and bilateral integration, and she noted that it often occurred in children with learning disabilities, especially those with reading disorders.11 Additional problems commonly seen in this disorder include low muscle tone, immature righting and equilibrium reactions, poor right-left discrimination, and lack of clearly defined hand dominance.
Later in the 1970s, Ayres included the Southern California Postrotary Nystagmus Test (SCPNT) in her research as a more specific measure of vestibular processing.14 This test continues to be used and is part of the SIPT. Based on analysis of SCPNT scores, Ayres identified a vestibular processing component to the postural and bilateral integration (PBI) disorder.17 At this point she replaced the old PBI concept with the term vestibular-bilateral integration (VBI) disorder. One of the main characteristics of this problem was depressed postrotary nystagmus scores, suggesting inefficient central processing of vestibular input. Also characteristic were other signs of vestibular-related dysfunction, such as low muscle tone, postural-ocular deficits, and diminished balance and equilibrium reactions. In addition, poor bilateral coordination was implicated in VBI disorder.
Factor and cluster analyses using the SIPT led to further evolution of the concept of vestibular processing disorders. The SIPT studies identified a bilateral integration and sequencing (BIS) factor characterized by poor bilateral coordination and difficulty sequencing actions, which Ayres proposed was influenced primarily by vestibular functioning.21 Building on Ayres ideas, Fisher suggested that poor vestibular-proprioceptive processing is the basis for a type of sensory integrative dysfunction characterized by poor bilateral integration and sequencing.68 She used the term vestibular-proprioceptive to emphasize that these two sensory systems work so closely together that their functions are intertwined.
In addition, Fisher introduced an interesting new concept in relation to the BIS pattern: the notion of projected action sequences.68 To perform a projected action sequence, the child anticipates how to move as his or her spatial relationship to the environment changes, as when running to kick a ball or catching a moving ball. Fisher suggested that difficulty with projected action sequences is related to poor vestibular-proprioceptive processing, and, furthermore, that such deficits are a form of motor planning disorder. Thus, Fisher proposed a formal link between vestibular processing and praxis through the production of bilateral and sequenced movements.
Following Fisher’s work, other experts recently addressed the BIS pattern as a mild form of praxis disorder that generally is associated with vestibular-proprioceptive difficulties and characterized by problems with bilateral coordination as well as anticipatory actions.39,85,125 These authors also acknowledged that there may be a subset of children with BIS problems who do not have sensory integrative difficulties, in much the same way that children with isolated visual or auditory perception problems are not thought to have a sensory integration disorder.
Despite the variety of ways that have been used to describe vestibular-proprioceptive problems, certain classic clinical signs are common to all. In general, many children with these problems do not have a severe level of dysfunction, so the problem is easy to overlook. These children often exhibit poor equilibrium reactions, lower than average muscle tone (particularly in extensor muscles), poor postural stability, a tendency toward slouching, and difficulty in keeping the head upright. Inefficiency of the vestibularocular pathways may adversely affect function in directing head and eye movements while moving, as when watching a rolling soccer ball while running to kick it. Impaired balance and equilibrium reactions are likely to affect competence in performing activities such as bicycle riding, roller-skating, skiing, and playing games like hopscotch. Poor bilateral integration interferes with these activities as well. In addition, poor bilateral integration makes activities such as cutting with scissors, buttoning a shirt, or doing jumping jacks especially challenging. Bilateral integration difficulties are sometimes manifested in delays in body midline skill development, such as hand preference, spontaneous crossing of the body midline, and right-left discrimination. Neural connections between the vestibular centers in the brainstem and the reticular activating system also put children with vestibular processing disorders at risk for problems with attention, organization of behavior, communication, and modulation of arousal.
Praxis Problems
Praxis is the ability to conceptualize, plan, and execute a nonhabitual motor act.18 Problems with praxis are often referred to as dyspraxia. When the term dyspraxia is used in regard to children, it usually refers to a condition characterized by difficulty with praxis that cannot be explained by a medical diagnosis or developmental disability and that occurs despite ordinary environmental opportunities for motor experiences. When Ayres originally wrote about dyspraxia, she used the term developmental apraxia.11 However, because the term apraxia is often associated with brain damage in adults, she later replaced this term with developmental dyspraxia.18,20 The prefix developmental implies that the condition emerges in early childhood development and is not the result of traumatic injury.
As noted previously, Ayres was struck with the relationship between tactile perception and praxis that emerged in study after study. She hypothesized that good tactile perception contributes to development of an accurate and precise body scheme, which serves as a reservoir of knowledge to be drawn on in planning new actions. Her interest in praxis appeared to grow over time, as is evident in the number of praxis tests included in the SIPT as opposed to the older SCSIT. When Ayres discussed praxis in relation to her SIPT studies, she introduced the idea that praxis problems may be manifested in different forms, not all of which are sensory integrative in nature.21 She coined the term somatopraxis to refer to the aspect of praxis that is sensory integrative in origin and grounded in somatosensory processing. At the same time she introduced the term somatodyspraxia to refer to a sensory integrative deficit that involves poor praxis and impaired tactile and proprioceptive processing. By definition, somatodyspraxia involves a disorder in tactile discrimination and perception. Cermak noted that not all children with developmental dyspraxia demonstrate poor tactile perception.47 The term somatodyspraxia applies only to those who do.
The child with somatodyspraxia typically appears clumsy and awkward. Novel motor activities are performed with great difficulty and often result in failure. Transitioning from one body position to another or sequencing and timing the actions involved in a motor task may pose a great challenge. These children typically have difficulty relating their bodies to physical objects in environmental space. They often have difficulty accurately imitating actions of others. Directionality of movement may be disturbed, resulting in unintentional breakage of toys when the child forcefully pushes an object that should be pulled. Many of these children have difficulties with oral praxis, which may affect eating skills or speech articulation.
Some children with dyspraxia have problems with ideation (i.e., they have difficulty generating ideas of what to do in a novel situation). When asked to simply play, without being given specific directions, these children may not initiate any activity or they may initiate activity that is habitual and limited or seems to lack a goal. Typical responses may include are to wander aimlessly; to perform simple repetitive actions such as patting or pushing objects around; to randomly pile up objects with no apparent plan; or for the more sophisticated child, to wait to observe others doing an activity and then imitate them rather than initiating an activity independently. May-Benson expanded on the role of ideation in praxis, highlighting the role of language and the social environment and reviewing the neuroanatomic foundations for this important function.99
For children with dyspraxia, skills that most children attain rather easily can be excessively challenging (e.g., donning a sweater, feeding oneself with utensils, writing the alphabet, jumping rope, completing a puzzle). These skills can be mastered only with high motivation on the part of the child, coupled with a great deal of practice, far more than most children require. Participation in sports is often embarrassing and frustrating, and organization of schoolwork may be a problem of particular concern. Children who have somatodyspraxia and are aware of their deficits often avoid difficult motor challenges and may attempt to gain control over such situations by assuming a directing or controlling role over others.
Praxis is best evaluated using the SIPT, which is sensitive to difficulties in this area. However, parent interview and informal observations provide critical pieces in the assessment process. These are essential in evaluating ideation because currently available standardized tests on large normative samples are extremely limited in their measurement of this aspect of praxis. The new Test of Ideational Praxis is promising as a standardized, objective means for assessing ideation.100
Secondary Problems Related to Sensory Integrative Difficulties
As already shown, sensory integration difficulties often impose some limitation on the quality of the child’s participation in occupations that he or she wants or needs to do as a member of a family, classroom, or community. How others respond to the child’s struggles may have a powerful effect on the child’s developing competence. In addition, the child’s willingness to grapple with challenging experiences will influence his or her occupational life over the years.114 Unfortunately, a number of secondary problems often arise in conjunction with sensory integration problems. These secondary problems may actually have a more powerful impact on the child’s life outcomes than the original sensory integration difficulty. In some cases, what started out as a minor sensory integration difficulty can become magnified into a major barrier to life satisfaction. Following is an explanation of several of these indirect, but significant, influences on the child and family.
First, sensory integrative dysfunction is an “invisible” disability (i.e., not directly and easily detected by the casual observer) that is easily misinterpreted. Sensory integrative disorders can fluctuate in severity from one time to another within the same child. Moreover, the severity of dysfunction and the ways in which dysfunction is expressed vary tremendously from one individual to another. This variability makes it difficult to predict which situations cause problems for a particular child, how much discomfort results, and when distress is likely to occur. Parents and teachers of children with these disorders often find the unpredictability of the child’s behavior to be frustrating and difficult to understand. As a result, sensory integrative problems are frequently misinterpreted as purely behavioral or psychological issues. Consequently, the child may be punished or responded to inappropriately, which may lead to chronic feelings of hopelessness as the child develops a self-view as bad or incapable.
A second indirect effect of sensory integrative dysfunction on the child’s life is its negative influence on skill development secondary to limited participation in childhood occupations. The child who avoids finger painting because of tactile defensiveness or who rarely attempts climbing on the jungle gym because of dyspraxia misses more than these singular experiences. The child also misses experiences that hone underlying functions such as tactile discrimination, hand strength and dexterity, shoulder stability, balance and equilibrium, hand-eye coordination, bilateral coordination, ideation, and motor planning. If the child misses a substantial amount of such experiences over time, the gap between the child’s sensorimotor skills and the skills of peers may grow.
In addition to interference with the development of sensorimotor functions, interactions important to the development of communication and social skills may not occur. Thus, some children with sensory integrative disorders may lack the ability to play successfully with peers partly because they have not been able to participate fully in the play occupations in which sensory, motor, cognitive, and social skills emerge and develop. The fear, anxiety, or discomfort that accompanies many everyday situations is also likely to work against the expression of the child’s inner drive toward growth-inducing experiences. Therefore lack of experience and diminished drive to participate compound the direct effects of a sensory integrative disorder. Consequently, the development of competence in many domains of development may be seriously compromised.
A third indirect effect of sensory integrative problems is the undermining of self-esteem and self-confidence over time. Children with sensory integrative problems are often aware of their struggles with commonplace tasks, so it is natural for them to react with frustration. Frustration is likely to mount as the child observes peers mastering these same tasks effortlessly. Chronic frustration can negatively affect and detract from the child’s feelings of self-efficacy. Instead, the child may develop feelings of helplessness. This leads to further limitations in the child’s experiences because the child becomes less likely to attempt challenging activities.
ASSESSMENT OF SENSORY INTEGRATIVE FUNCTIONS
Assessment of sensory integration, like all other areas addressed in occupational therapy, requires a multifaceted approach because of the need to understand presenting problems, not only in relation to the individual who is being assessed but also with respect to the family and environments in which that individual participates. Assessment by the occupational therapist begins with a general exploration of the occupations of the child and family, focusing on their concerns and hopes in relation to the child’s strengths and challenges in routine activities. A variety of tools are needed to help the therapist detect problems in sensory integration, to understand the nature and scope of these difficulties, and to decide whether intervention should be recommended. Assessment tools employed by occupational therapists using a sensory integration perspective include interviews and questionnaires, informal and formal observations, standardized tests, and consideration of services and resources available to and appropriate for the family. Roley127 provided an excellent discussion of how this process of assessment is consistent with the guidelines laid out in the Occupational Therapy Practice Framework.1
Interviews and Questionnaires
The need for an occupational therapy assessment of sensory integration usually arises when a parent, teacher, physician, or other person who knows the child notices problems that the child is experiencing that are not easily explained by other conditions or considerations. The referral source, family members, and others who work with the child may all be valuable sources of information through interview or questionnaire (Figure 11-11). This initial phase of evaluation identifies the presenting problems, or main concerns, about the child and begins the process of determining whether sensory integration difficulties might account for the concerns about the child.

FIGURE 11-11 Because parents know their child better than anyone else, they are invaluable sources of information to the therapist, especially in beginning phases of the assessment process. Courtesy Shay McAtee.
The initial interview with the parent, teacher, or other referral source provides an opportunity for the therapist to gather important information about signs of sensory integration problems that may be present. For example, the teacher may report that the child is always fighting while standing in line and cannot seem to stay seated during reading circle time. Further questioning by the therapist may disclose signs of tactile defensiveness that might explain the child’s behavior but were not considered by the teacher, who is unfamiliar with this condition. A parent may be able to provide critical information about the child’s development, which may be helpful in identifying early signs of sensory integrative dysfunction. For instance, parents may have noticed that specific tasks, such as cutting with scissors or pedaling a tricycle, were especially difficult for the child. Since difficulty coordinating the two sides of the body is common when vestibular processing difficulties are present, this type of information can inform the therapist about additional observations and tests needed. Another important role of the interview is to uncover alternative explanations of the child’s difficulties that may rule out sensory integration problems, such as when a recent emotional crisis (e.g., a divorce or death) coincides with the onset of problems. Miller and Summers provided examples of the kinds of questions to ask in a parent interview.108
Questionnaires, checklists, and histories given by caregivers and other adults who know the child well are other means for gathering information that aid in identifying presenting problems, estimating how long they have been a concern, and clarifying the priorities of the family. One such instrument is a sensory history or similar questionnaire. Originally developed by Ayres as an unpublished questionnaire, this type of instrument asks parents questions regarding specific child behaviors indicative of sensory integrative dysfunction, and parents respond by rating the child using a Likert-style scale. These types of questionnaires were subsequently developed using normative samples to produce reliable and valid scores. The Sensory Profile62 and the Sensory Processing Measure (SPM)116 are two sensory questionnaires used extensively in pediatric occupational therapy. The Sensory Profile is available in versions for parents of infants and toddlers64 and of children in early and middle childhood,62 as well as for self-reports of adolescents and adults.36 Additionally, a Sensory Profile School Companion is available for teacher report of child behavior at school.65 The SPM has two forms, Home115 and Main Classroom,109 that are standardized on the same sample of 5- to 12-year-old children and can furnish a score that aids the therapist in discerning whether a child’s sensory issues are manifested differently in the contexts of home versus school. In addition, the SPM contains separate rating scales for school personnel other than the main teacher, such as art teacher, music teacher, or bus driver.
An additional way to gather information in the initial phases of assessment is through review of records, including previous reports from other professionals as well as educational and medical histories. It is useful to talk with the child directly when possible. Royeen and Fortune developed a child questionnaire for the assessment of tactile defensiveness, called the Touch Inventory for Elementary School–Aged Children (TIE).133,134 Children with sufficient verbal skills to discuss their own abilities, perceptions, and difficulties can sometimes provide invaluable insight into their condition through such a questionnaire-based interview. The Alert Program, a group intervention program for older children and adults, includes a self-assessment of sensory preferences that can be adapted for assessment of younger children to help them identify and communicate their characteristic sensory responses.154
The information garnered through the initial interview process is used to decide whether further assessment is warranted and, if so, which evaluation procedures are most appropriate. This information is also critical in interpreting the final pool of information gathered through assessment and in prioritizing goals for the child in light of the main concerns of the family.
Informal and Formal Observations of the Child
Direct observation of the child is essential to the evaluation of sensory integration. Informal observations, clinical observations, and standardized testing are commonly used.
Informal Observations
Informal observation of the child in natural settings, such as a classroom, playground, or home, is informative and helpful whenever feasible. Informal observation will influence the conclusion as to whether a sensory integrative disorder is present and will, perhaps more importantly, indicate how the child’s difficulties are interfering with daily occupations. For example, an experienced therapist can often detect signs of poor body awareness by observing the child at school. Such signs may include exerting too much pressure on a pencil, standing too close to classmates in line, poor foot placement when climbing on a jungle gym, or sitting in an ineffective position in a chair while doing class assignments. Teachers may not necessarily report these behaviors to the therapist if they perceive them as typical signs of inattentiveness or clumsiness.
Informal observation of the child in the clinical setting can also be useful in showing how the child responds to situations that are novel or unpredictable. A child with dyspraxia may have a great deal of difficulty problem-solving how to mount an unfamiliar climbing structure in the clinic, even though performance is adequate on similar tasks at home or at school, where the child has practiced them. The novelty of the clinical therapy room elicits responses from children that may be diagnostically relevant. For children with good ideation and sensory processing abilities, the endless opportunities afforded by sensory integration equipment in the clinic can be exhilarating. For the child with a disorder like dyspraxia, the same environment may be confusing, puzzling, or frustrating. A child with gravitational insecurity may be terrified by the prospect of equipment that moves, whereas a child with autism may be distressed by the clinic environment because of its unpredictability and discrepancy from familiar settings. Parham has provided some guidelines for organizing informal observations in the clinic, with special attention to issues related to praxis.113 Although her suggestions are focused on the assessment of preschoolers, they can also be applied to older children and may be particularly helpful in evaluating older children who are unable to cooperate with standardized testing. Roley128 and Windsor, Roley, and Szklut158 provide additional guidelines for assessing praxis through informal observations.
Clinical Observations
Formal observations that are highly structured and similar to test items are often used in an occupational therapy assessment of sensory integration. Usually referred to as clinical observations, these typically involve a set of specific procedures that allow the therapist to observe signs of nervous system integrity that are associated with sensory integrative functioning. Ayres included measures of such formal observations in her factor analytic studies, along with standardized tests.5–9,13,16 She also developed a set of clinical observations that she used in clinical practice. These unpublished, nonstandardized evaluation tools were intended to supplement standardized test scores and subsequently were revised, expanded upon, and studied by many other therapists over the years.32,38,157 Examples of some of the most commonly used clinical observations are presented in Box 11-1.
One of the difficulties in using clinical observations as an assessment tool is that often the administration and scoring criteria have not been standardized. This means that they are administered using different procedures from one clinician to another. Furthermore, most of them lack normative data to aid in interpretation of the scores obtained. Some, but not all, clinical observations are supported by research using standardized administration to inform interpretation.71,91,100,101,157
Occupational therapists must rely on the information from these studies, as well as their personal expertise and judgment, to interpret the results of clinical observations. Without the requisite data in hand, occupational therapists are cautioned to avoid overinterpretation of clinical observations in light of the lack of standardized procedures and inadequate information regarding expected performance across age, gender, and other demographically related groups.
Most clinical observations address motor functions that may be strongly affected by conditions other than sensory integration problems. Therefore, the therapist must use sound clinical reasoning with advanced knowledge of sensory integration theory in order to appropriately interpret these observations.
Standardized Testing
Occupational therapists frequently use standardized tests to evaluate sensory integration. Although several tests are available that contribute incidental information regarding sensory integrative functions, the SIPT protocol is the only set of standardized tests designed specifically for in-depth evaluation of sensory integration. The SIPT evolved from a series of tests that Ayres developed in the 1960s3,4,6,7,18 and later published as the SCSIT12 and the SCPNT.14 The standardization process used in the development of the SIPT was rigorous, involving normative data on approximately 2000 children in North America and extensive reliability and validity studies.21 Its 17 tests measure tactile, vestibular, and proprioceptive sensory processing; form and space perception and visuomotor coordination; bilateral integration and sequencing abilities; and praxis.25 A list of the 17 tests and the functions measured by each is presented in Table 11-3.
TABLE 11-3
Functions Measured by the Sensory Integration and Praxis Tests
| Function | Description |
| Space visualization | Motor-free visual space perception; mental manipulation of objects |
| Figure-ground perception | Motor-free visual perception of figures on a rival background |
| Manual form perception | Identification of block held in hand with visual counterpart or with block held in other hand |
| Kinesthesia | Somatic perception of hand and arm position and movement |
| Finger identification | Tactile perception of individual fingers |
| Graphesthesia | Tactile perception and practic replication of designs |
| Localization of tactile stimuli | Tactile perception of specific stimulus applied to arm or hand |
| Praxis on verbal command | Ability to motor-plan body postures on the basis of verbal directions without visual cures |
| Design copying | Visuopractic ability to copy simple and complex two-dimensional designs, and the manner or approach one uses to copy designs |
| Constructional praxis | Ability to relate objects to each other in three-dimensional space |
| Postural praxis | Ability to plan and execute body movements and positions |
| Oral praxis | Ability to plan and execute lip, tongue, and jaw movements |
| Sequencing praxis | Ability to repeat a series of hand and finger movements |
| Bilateral motor coordination | Ability to move both hands and both feet in a smooth and integrated pattern |
| Standing and walking balance | Static and dynamic balance on one or both feet with eyes opened and closed |
| Motor accuracy | Hand-eye coordination and control of movement |
| Postrotary nystagmus | Central nervous system processing of vestibular input assessed through observation of the duration and integrity of a vestibulo-ocular reflex |
From Mailloux, Z. (1990). An overview of the Sensory Integration and Praxis Tests. American Journal of Occupational Therapy, 44, 589-594.
The SIPT protocol requires about 1½ to 2 hours to administer and another 30 to 45 minutes to score. Raw scores may be translated into standard scores by the therapist using a computer diskette available from the publisher. Alternatively, raw scores may be sent to the publisher, Western Psychological Services, for an analysis using the normative data. After normative scores are obtained, the therapist critically examines them to determine if patterns of sensory integrative dysfunction are evident. Not only are patterns of test scores scrutinized, but also the therapist’s observations of child behavior during testing are considered in interpreting test scores. Finally, test scores and test behaviors are integrated with all other sources of information from the assessment in reaching a conclusion regarding the status of sensory integrative functioning.
Like all standardized tests, the SIPT protocol is administered with adherence to standardized procedures (Figure 11-12). Specialized training is required for administration and interpretation. This tool is a complex set of tests and, unlike most published tests, cannot be self-taught by simply reading the manual. In addition to formal training for the SIPT, it is strongly recommended that therapists practice administration of the tests with children who do not have any known problems and with children who have recognized difficulties. With this experience and training, the therapist can administer the tests in a manner that produces reliable scores while allowing for observation of behaviors that provide additional information about the child’s sensory integration and praxis abilities.
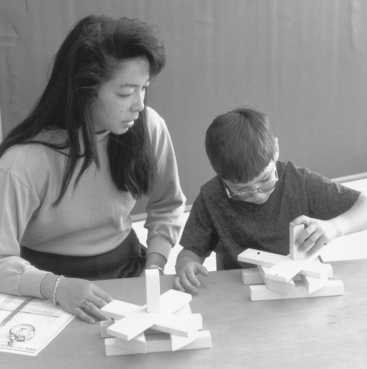
FIGURE 11-12 The Constructional Praxis Test is 1 of 17 tests of the Sensory Integration and Praxis Tests (SIPT). The SIPT must be administered individually with strict adherence to standardized procedures. Courtesy Shay McAtee.
Other pediatric tests include items or subtests from which inferences regarding sensory integration may be drawn. For example, the Miller Function & Participation Scales includes tests of praxis, visual-motor integration, figure–ground perception, and some vestibular functions.104 A number of tests, such as the Bruininks-Oseretsky Test of Motor Proficiency, (BOT-2),37 measure aspects of fine and gross motor skills (such as bilateral coordination) that are related to sensory integrative functions. Other tests, such as the Developmental Test of Visual Motor Integration,30 provide specific information related to visual-perceptual and perceptual-motor skills.
Some tests geared toward the broader evaluation of occupation, such as the School Function Assessment (SFA)54 or the Social Participation Scale of the SPM,116 are useful for identifying the extent to which sensory integrative disorders may be affecting the child’s participation in occupations within specific settings. For the child with suspected sensory integrative problems, tests such as the SFA are most effectively used along with specific measures of sensory integration. When combined, these tests identify the functional problems to target in intervention and the reasons for the child’s difficulties.
Consideration of Available Services and Resources
In addition to the information that is gathered about the child, an occupational therapy assessment of sensory integration takes into consideration the services and resources that are available to the child and family. Information regarding the type of services that the child is currently receiving, how he or she is responding to these services, and what services, programs, and resources are available to the child need careful consideration in light of the purpose and findings of the evaluation before recommendations can be formulated. For example, an occupational therapist may be asked to provide a reevaluation of a child who has been receiving occupational therapy for several years. If the child continues to demonstrate significant sensory integrative problems and has shown a diminishing response to treatment using a sensory integration approach, the recommendations would be different from those for a child no longer showed evidence of a significant sensory integrative problem.
Similarly, a child who lives in an area where no occupational therapists are qualified to provide sensory integration intervention needs a different program recommendation from that for a child who has easy access to this type of service. Understanding family aspirations and values, as well as resources, such as funding, transportation, time, and caregivers, is also critical in identifying the types of services that will be most helpful to the child and family. These issues are as important to the assessment process as the child factors that are addressed in a sensory integration evaluation.
Interpretation of Assessment Findings
Once all of the information from interviews, questionnaires, informal and formal observations, standardized tests, and consideration of available services and resources has been collected, the occupational therapist must integrate and interpret these data to reach meaningful conclusions and appropriate recommendations for the individual child. Conclusions and recommendations are framed with an overriding consideration of the occupations of the child and family and the contexts that influence occupational engagement.1,127 Burke, Schaaf, and Hall advocate the strategy of creating a narrative, or story, to form an integrated understanding of the child and family in order to focus assessment and intervention planning on issues that are most meaningful and important to them.40 In using such a future-oriented, top-down approach, the therapist not only generates a picture of the child and family in the present, but also imagines how changes might unfold over the next few years.114 Therapists use research as well as training and experience to formulate conclusions and recommendations. (See Research Note 11-1 for an example of research that can inform interpretation of how assessment data relate to a child’s academic functioning in school.)
One of the important steps in interpretation of assessment findings is to evaluate whether a sensory integrative problem may contribute to the occupational challenges of the child. To do this, data are classified into categories that either support or refute the presence of particular types of sensory integrative problems. After a detailed analysis of the constellation of assessment findings, a hypothesis is generated as to whether a sensory integrative problem appears to be present and, if so, what type it appears to be.
As in any aspect of occupational therapy, it is critical to relate the assessment findings to the presenting problems and initial concerns of the family or referral source. For example, an assessment may uncover signs of tactile defensiveness in a child described by the parents as destructive and impulsive. The evaluating therapist explains how tactile defensiveness may be related to the child’s behavior problems. Because sensory integrative problems are not always recognized and understood, the therapist includes an explanation of how the assessment findings are linked to the daily life experiences and occupations of the child and family.94
If an assessment leads to a recommendation for intervention, it generally includes an estimate of the duration of time that the child should receive therapy, some indication of prognosis, and a statement regarding expected areas of change. The anticipated gains can be further clarified through the establishment of specific goals and objectives. Writing and explaining goals will provide the occupational therapist with an opportunity to illuminate the ways in which the identified sensory integration issues intersect with the presenting problems and desired functional outcomes.94 Regardless of the types of goals that are written, goals are established in a manner that is culturally relevant for the family and considers the needs and wishes of the individual child.
The format in which goals are specified is often a function of the setting in which therapy is delivered. For example, a school district may include certain types of goals as part of an individualized education plan, whereas a hospital setting may require medically related outcomes. Goal attainment scaling is a specific method for writing goals that are individualized and then quantified to allow for comparison of outcomes across a large group of children.95 In this process, individualized goals are carefully placed on a standard scale that allows for quantitative comparison of changes across dissimilar outcomes (e.g., the amount of change in pumping a swing in comparison with the amount of change in tolerance of food textures). Although this method was developed for outcomes research, it may be useful in documenting intervention effectiveness across a large group of children for purposes of program evaluation.
 RESEARCH NOTE 11-1
RESEARCH NOTE 11-1