Contraception and Abortion
• Compare various methods of contraception.
• Identify the advantages and disadvantages of commonly used methods of contraception.
• Explain the common nursing interventions that facilitate contraceptive use.
• Examine the various ethical, legal, cultural, and religious considerations of contraception.
• Describe the techniques used for medical and surgical interruption of pregnancy.
• Discuss the various ethical and legal considerations of elective abortion.
Contraception
Contraception is the intentional prevention of pregnancy during sexual intercourse. Birth control is the device and/or practice to decrease the risk of conceiving, or bearing, offspring. Family planning is the conscious decision on when to conceive, or to avoid pregnancy, throughout the reproductive years. With the wide assortment of birth control options available, it is possible for a woman to use several different contraceptive methods at various stages throughout her fertile years. Nurses interact with the woman to compare and contrast available options, reliability, relative cost, protection from sexually transmitted infections (STIs), the individual’s comfort level, and the partner’s willingness to use a particular birth control method. Those who practice contraception may still be at risk for pregnancy simply because their choice of birth control method is not perfect or is used inconsistently or incorrectly. Providing adequate instruction about how to use a contraceptive method, when to use a backup method, and when to use emergency contraception can decrease the chance of unintended pregnancy (Stewart, Trussell, & Van Look, 2007).
Care Management
A multidisciplinary approach may assist a woman in choosing and correctly using an appropriate contraceptive method. Nurses, nurse-midwives, nurse practitioners, and other advanced practice nurses as well as physicians have the knowledge and expertise to assist a woman in making decisions about contraception that will satisfy the woman’s personal, social, cultural, and interpersonal needs.
Family, friends, media, partner or partners, religious affiliation, and health care professionals influence a woman’s perception of contraceptive choices. These external influences form a woman’s unique view. The nurse assists in supporting the woman’s decision based on the individual’s situation (see Nursing Process box).
Informed consent is a vital component in the education of the client concerning contraception or sterilization. The nurse often has the responsibility of documenting information provided and the understanding of that information by the client. The acronym BRAIDED may be useful (see Legal Tip).
To foster a safe environment for consultation, a private setting should be provided in which the client can feel free to be open. Distractions should be minimized, and samples of birth control devices for interactive teaching should be available. The nurse counters myths with facts, clarifies misinformation, and fills in gaps of knowledge. The ideal contraceptive should be safe, easily available, economical, acceptable, simple to use, and promptly reversible. Although no method may ever achieve all these objectives, new contraceptive technologies are being developed (Blithe, 2008; Practice Committee of the American Society for Reproductive Medicine, 2008; Yranski & Gamache, 2008).
Contraceptive effectiveness varies from couple to couple (Box 8-1) and depends on the properties of the method and the characteristics of the user (Kost, Singh, Vaughan, Trussell, & Bankole, 2008). Contraceptive failure rate refers to the percentage of contraceptive users expected to have an unplanned pregnancy during the first year, even when they use a method consistently and correctly. Failure rates decrease over time, either because a user gains experience and uses a method more appropriately or because the less effective users stop using the method.
Methods of Contraception
The following discussion of contraceptive methods provides the nurse with information needed for client teaching. After implementing the appropriate teaching for contraceptive use, the nurse supervises return demonstrations and practice to assess client understanding (Fig. 8-1). The woman is given written instructions; if she has difficulty understanding the written instructions, she (and her partner, if available) is offered graphic material and a telephone number to call as necessary, or is offered an opportunity to return for further instruction (see Nursing Care Plan).

FIG. 8-1 Nurse counseling woman about contraceptive methods. (Courtesy Dee Lowdermilk, Chapel Hill, NC.)
Coitus Interruptus
Coitus interruptus (withdrawal) involves the male partner withdrawing the penis from the woman’s vagina before he ejaculates. Although coitus interruptus is one of the least effective methods of contraception, it is a good choice for couples who do not have another contraceptive available (Kowal, 2007). Effectiveness is similar to barrier methods and depends on the man’s ability to withdraw his penis before ejaculation. The percentage of women who will experience an unintended pregnancy within the first year of typical use (failure rate) of withdrawal is about 27% (Trussell, 2007). Coitus interruptus does not protect against STIs or human immunodeficiency virus (HIV) infection.
Fertility Awareness Methods (Natural Family Planning)
Fertility awareness methods (FAMs) of contraception, also known as periodic abstinence or natural family planning, depend on identifying the beginning and end of the fertile period of the menstrual cycle. These methods provide contraception by relying on avoidance of intercourse during fertile periods. Natural family planning methods are the only contraceptive practices acceptable to the Roman Catholic Church. When women who want to use FAMs are educated about the menstrual cycle, three phases are identified:
1. Infertile phase: before ovulation
2. Fertile phase: about 5 to 7 days around the middle of the cycle, including several days before and during ovulation and the day afterward
The human ovum can be fertilized no later than 12 to 24 hours after ovulation (Cunningham, Leveno, Bloom, Hauth, Rouse, & Spong, 2010; Hatcher, 2007). Motile sperm have been recovered from the uterus and the oviducts as long as 60 hours after coitus, but their ability to fertilize the ovum probably lasts no longer than 24 to 48 hours. One problem with FAMs is that the exact time of ovulation cannot be predicted accurately, and couples may find it difficult to exercise restraint for several days before and after ovulation. In addition, women with irregular menstrual periods have the greatest risk of failure with FAMs.
Although ovulation can be unpredictable in many women, teaching the woman about how she can directly observe her fertility patterns is an empowering tool. There are nearly a dozen categories of FAMs. To prevent pregnancy, each one uses a combination of charts, records, calculations, tools, observations, and either abstinence or barrier methods of birth control during the fertile period in the menstrual cycle (Jennings & Arevalo, 2007). The charts and calculations associated with these methods can also be used to increase the likelihood of detecting the optimal timing of intercourse to achieve conception. Signs and symptoms of fertility awareness most commonly used with abstinence are menstrual bleeding, cervical mucus, and basal body temperature (see later discussions) (Jennings & Arevalo).
Advantages of these methods include low to no cost, absence of chemicals and hormones, and lack of alteration in the menstrual flow pattern. Disadvantages of FAMs include adherence to strict record-keeping, unintentional interference from external influences that may alter the woman’s core body temperature and vaginal secretions, decreased effectiveness in women with irregular cycles (particularly adolescents who have not established regular ovulatory patterns), decreased spontaneity of coitus, and attending possibly time-consuming training sessions by qualified instructors (Jennings & Arevalo, 2007) (Box 8-2). The typical failure rate for most FAMs is 25% during the first year of use (Trussell, 2007). FAMs do not protect against STIs or HIV infection.
FAMs involve several techniques to identify fertile days. The following discussion includes the most common techniques as well as some promising techniques for the future.
Calendar Rhythm Method: Practice of the calendar rhythm method is based on the number of days in each cycle, counting from the first day of menses. With this method the fertile period is determined after accurately recording the lengths of menstrual cycles for at least 6 months. The beginning of the fertile period is estimated by subtracting 18 days from the length of the shortest cycle. The end of the fertile period is determined by subtracting 11 days from the length of the longest cycle (Jennings & Arevalo, 2007). If the shortest cycle is 24 days and the longest is 30 days, application of the formula to calculate the fertile period is as follows:
To avoid conception the couple would abstain during the fertile period— days 6 through 19. If the woman has very regular cycles of 28 days each, the formula indicates the fertile days to be as follows:
To avoid pregnancy the couple abstains from day 10 through 17 because ovulation occurs on day 14 plus or minus 2 days. A major drawback of the calendar method is that one is trying to predict future events with past data. The unpredictability of the menstrual cycle also is not taken into consideration. The calendar rhythm method is most useful as an adjunct to the basal body temperature or the cervical mucus method.
Standard Days Method: The Standard Days Method (SDM) is essentially a modified form of the calendar rhythm method that has a “fixed” number of days of fertility for each cycle—that is, days 8 to 19 (Germano & Jennings, 2006). A CycleBeads necklace—a color-coded string of beads—can be purchased as a concrete tool to track fertility (Fig. 8-2). Day 1 of the menstrual flow is counted as the first day to begin the counting. Women who use this device are taught to avoid unprotected intercourse on days 8 to 19 (white beads on CycleBeads necklace). Although this method is useful to women whose cycles are 26 to 32 days long, it is unreliable for those who have longer or shorter cycles. The typical failure rate for the SDM is 12% during the first year of use (Jennings & Arevalo, 2007).

FIG. 8-2 CycleBeads. Red bead marks the first day of the menstrual cycle. White beads mark days that are likely to be fertile days; therefore, unprotected intercourse should be avoided. Brown beads are days when pregnancy is unlikely and unprotected intercourse is permitted. (Courtesy Dee Lowdermilk, Chapel Hill, NC.)
TwoDay Method: The TwoDay Method is based on the monitoring and recording of cervical secretions (Germano & Jennings, 2006). Each day the woman asks herself, (1) “Did I note secretions today?” and (2) “Did I note secretions yesterday?” If the answer to either is yes, she should avoid coitus or use a backup method of birth control. If the answer to both questions is no, her probability of getting pregnant is very low. After 2 days without secretions, the woman may resume unprotected intercourse. The TwoDay Method appears to be simpler to teach, learn, and use than other natural methods. Results suggest that the method can be an effective alternative for low literacy populations or for programs that find current natural family planning methods too time consuming or otherwise not feasible to incorporate into their services. Early studies have found the typical failure rate of the TwoDay Method to be 14% (Germano & Jennings).
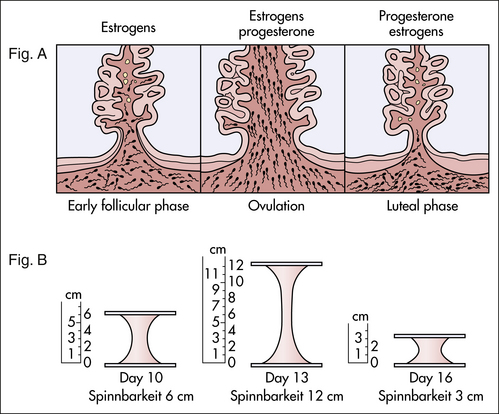
Ovulation Method: The cervical mucus ovulation-detection method (also called the Billings method and the Creighton model ovulation method) requires that the woman recognize and interpret the cyclic changes in the amount and consistency of cervical mucus that characterize her own unique pattern of changes (see Teaching for Self-Management box: Cervical Mucus Characteristics). The cervical mucus that accompanies ovulation is necessary for viability and motility of sperm. It alters the pH environment, neutralizing the acidity, to be more compatible for sperm survival. Without adequate cervical mucus, coitus does not result in conception. Women check quantity and character of mucus on the vulva or introitus with fingers or tissue paper each day for several months to learn the cycle. To ensure an accurate assessment of changes, the cervical mucus should be free from semen, contraceptive gels or foams, and blood or discharge from vaginal infections for at least one full cycle. Other factors that create difficulty in identifying mucus changes include douches and vaginal deodorants, being in the sexually aroused state (which thins the mucus), and taking medications such as antihistamines (which dry up the mucus). Intercourse is considered safe without restriction beginning the fourth day after the last day of wet, clear, slippery mucus (postovulation) (Jennings & Arevalo, 2007).
Some women may find this method unacceptable if they are uncomfortable touching their genitals. Whether or not the individual wants to use this method for contraception, it is to the woman’s advantage to learn to recognize mucus characteristics at ovulation. Self-evaluation of cervical mucus can be highly accurate and can be useful diagnostically for any of the following purposes:
Basal Body Temperature Method: The basal body temperature (BBT) is the lowest body temperature of a healthy person, taken immediately after waking and before getting out of bed. The BBT usually varies from 36.2° to 36.3° C during menses and for about 5 to 7 days afterward (Fig. 8-3). At about the time of ovulation, a slight decrease in temperature (approximately 0.5° C) may occur in some women, but others may have no decrease at all. After ovulation, in concert with the increasing progesterone levels of the early luteal phase of the cycle, the BBT increases slightly (approximately 0.2° to 0.5° C) (World Health Organization Department of Reproductive Health & Research [WHO/RHR] and Johns Hopkins Bloomberg School of Public Health/Center for Communication Programs [CCP], 2007). The temperature remains on an elevated plateau until 2 to 4 days before menstruation, and then it decreases to the low levels recorded during the previous cycle, unless pregnancy has occurred and the temperature remains elevated. If ovulation fails to occur, the pattern of lower body temperature continues throughout the cycle.
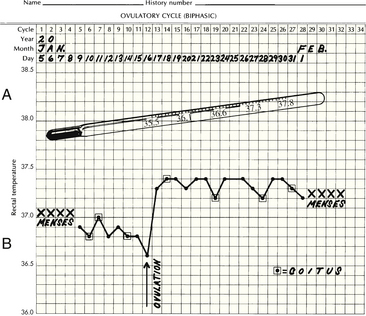
FIG. 8-3 A, Special thermometer for recording basal body temperature, marked in tenths to enable person to read more easily. B, Basal temperature record shows drop and sharp rise at time of ovulation. Biphasic curve indicates ovulatory cycle.
To use this method, the fertile period is defined as the day of first temperature drop, or first elevation through 3 consecutive days of elevated temperature. Abstinence begins the first day of menstrual bleeding and lasts through 3 consecutive days of sustained temperature rise (at least 0.2° C) (Jennings & Arevalo, 2007; WHO/RHR & CCP, 2007). The decrease and subsequent increase in temperature are referred to as the thermal shift. When the entire month’s temperatures are recorded on a graph, the pattern described is more apparent. It is more difficult to perceive day-to-day variations without the entire picture. Infection, fatigue, less than 3 hours sleep per night, awakening late, and anxiety may cause temperature fluctuations, altering the expected pattern. If a new BBT thermometer is purchased, this fact is noted on the chart because the readings may vary slightly. Jet lag, alcohol and antipyretic medications taken the evening before, or sleeping in a heated waterbed also must be noted on the chart because each affects the BBT. Therefore, the BBT alone is not a reliable method of predicting ovulation.
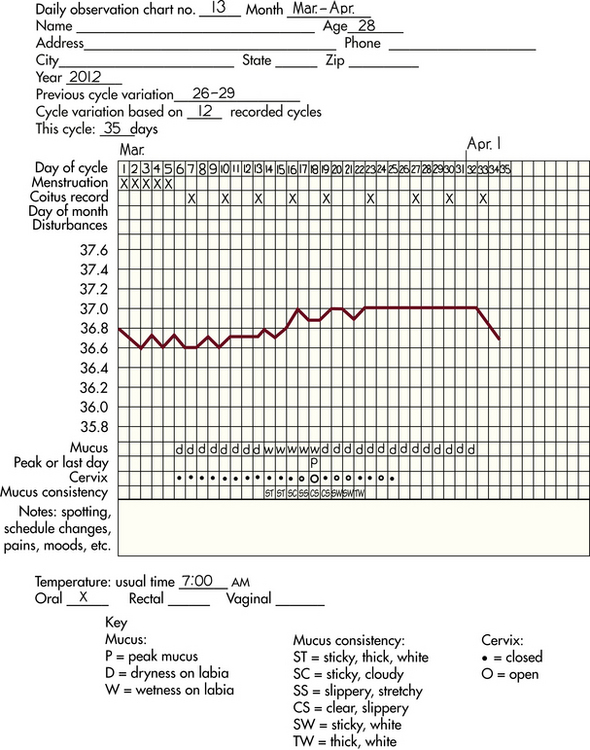
Symptothermal Method: The symptothermal method is a tool for the woman to gain fertility awareness as she tracks the physiologic and psychologic symptoms that mark the phases of her cycle. This method combines at least two methods, usually cervical mucus changes with BBT, in addition to heightened awareness of secondary, cycle phase–related symptoms (Pallone & Bergus, 2009). Secondary symptoms may include increased libido, midcycle spotting, mittelschmerz, pelvic fullness or tenderness, and vulvar fullness. The woman is taught to palpate her cervix to assess for changes in texture, position, and dilation that indicate ovulation. During the preovulatory and ovulatory periods, the cervix softens, opens, rises in the vagina, and is more moist. During the postovulatory period the cervix drops, becomes firm, and closes. The woman notes days on which coitus, changes in routine, and illness have occurred (Fig. 8-4). Calendar calculations and cervical mucus changes are used to estimate the onset of the fertile period; changes in cervical mucus or the BBT are used to estimate its end.
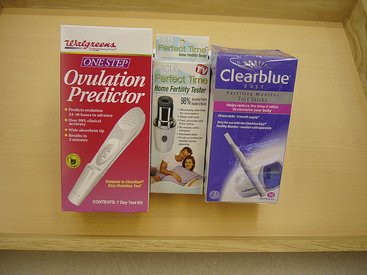
Home Predictor Test Kits for Ovulation: All of the preceding methods discussed are indicative of but do not prove the occurrence and exact timing of ovulation. The urine predictor test for ovulation is a major addition to the NFP and fertility-awareness methods to help women who want to plan the time of their pregnancies and those who are trying to conceive (Fig. 8-5). The urine predictor test for ovulation detects the sudden surge of luteinizing hormone (LH) that occurs approximately 12 to 24 hours before ovulation. Unlike BBT, the test is not affected by illness, emotional upset, or physical activity. For home use, a test kit contains sufficient material for several days of testing during each cycle. A positive response indicative of an LH surge is noted by an easy-to-read color change. Directions for use of urine predictor test kits vary with the manufacturer. Saliva predictor tests for ovulation use dried, nonfoamy saliva as a tool to show fertility patterns. More research is needed to determine the efficacy of use of these tests for pregnancy prevention.
The Marquette Model: The Marquette Model (MM) is a natural family planning method that was developed through the Marquette University College of Nursing Institute for Natural Family Planning (Fehring, Schneider, & Barron, 2008). The MM uses cervical monitoring along with the ClearPlan Easy Fertility Monitor. The ClearPlan monitor is a handheld device that uses test strips to measure urinary metabolites of estrogen and LH. The monitor provides the user with “low,” “high,” and “peak” fertility readings. The MM incorporates the use of the monitor as an aid to learning NFP and fertility awareness. The MM is currently being tested at different sites in the United States for its effectiveness in helping couples avoid pregnancy. One study has shown a typical use failure rate of 10.6% (Fehring et al.).
Spermicides and Barrier Methods
Barrier contraceptives have gained in popularity, not only as a contraceptive method but also as a protective measure against the spread of STIs, such as human papillomavirus (HPV) and herpes simplex virus (HSV). Some male condoms and female vaginal methods provide a physical barrier to several STIs, and some male condoms provide protection against HIV (Cates & Raymond, 2007; Warner & Steiner, 2007). Spermicides serve as chemical barriers against the sperm.
Spermicides: Spermicides, such as nonoxynol-9 (N-9), work by reducing the sperm’s mobility; the chemicals attack the sperm flagella and body, thereby preventing the sperm from reaching the cervical os. N-9, the most commonly used spermicidal chemical in the United States, is a surfactant that destroys the sperm cell membrane; however, data suggest that frequent use (more than two times a day) of N-9, or use as a lubricant during anal intercourse, can disrupt the mucosa, which could increase the transmission of HIV (Cates & Raymond, 2007). Women with high risk behaviors that increase their likelihood of contracting HIV and other STIs are advised to avoid the use of spermicidal products containing N-9, including those lubricated condoms, diaphragms, and cervical caps to which N-9 is added (Centers for Disease Control and Prevention [CDC], Workowski, & Berman, 2006).
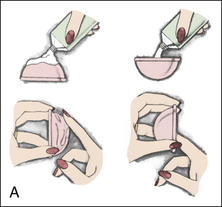
Intravaginal spermicides are marketed and sold without a prescription as foams, tablets, suppositories, creams, films, and gels (Fig. 8-6). Preloaded single-dose applicators small enough to be carried in a small purse are available. Effectiveness of spermicides depends on consistent and accurate use. Clients should be cautioned against misunderstanding terms: contraceptive gel differs from fruit jelly, and cosmetics or hair products containing the nonspermicidal forms of nonoxynol are not adequate substitutes. The spermicide should be inserted high into the vagina so that it makes contact with the cervix. Some spermicide should be inserted at least 15 minutes before, and no longer than 1 hour before, sexual intercourse. Spermicide must be reapplied before each additional act of intercourse, even if a barrier method is used. Studies have shown varying effectiveness rates for spermicidal use alone. Typical failure rate for spermicide use alone is about 29% (Trussell, 2007).
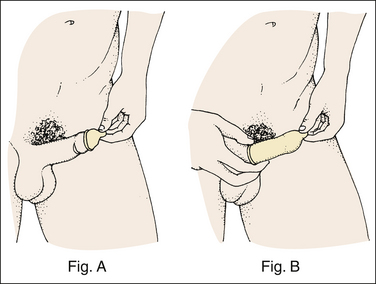
Condoms: The male condom is a thin, stretchable sheath that covers the penis before genital, oral, or anal contact and is removed when the penis is withdrawn from the partner’s orifice after ejaculation (Fig. 8-7, A). Condoms are made of latex rubber, polyurethane (strong, thin plastic), or natural membranes (animal tissue). In addition to providing a physical barrier for sperm, nonspermicidal latex condoms also provide a barrier for STIs (particularly gonorrhea, chlamydia, and trichomoniasis) and HIV transmission. Condoms lubricated with N-9 are not recommended for preventing STIs or HIV (CDC et al., 2006). Latex condoms will break down with oil-based lubricants and should be used only with water-based or silicone lubricants (Warner & Steiner, 2007). Because of the growing number of people with latex allergies, condom manufacturers have begun using polyurethane, which is thinner and stronger than latex. Research is being conducted to determine the effectiveness of polyurethane condoms to protect against STIs and HIV.
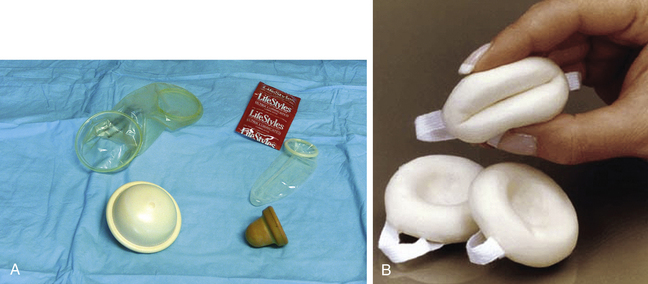
FIG. 8-7 A, Mechanical barriers. From the top left corner, clockwise: female condom, male condom, cervical cap, diaphragm. B, Contraceptive sponge. (A, Courtesy Dee Lowdermilk, Chapel Hill, NC; B, courtesy Allendale Pharmaceuticals, Inc., Allendale, NJ.)
A small percentage of condoms are made from lamb cecum (natural skin). Natural skin condoms do not provide the same protection against STIs and HIV infection as latex condoms. Natural skin condoms contain small pores that could allow passage of viruses such as hepatitis B, HSV, and HIV.
A functional difference in condom shape is the presence or absence of a sperm-reservoir tip. To enhance vaginal stimulation, some condoms are contoured and rippled or have ribbed or roughened surfaces. Thinner construction increases heat transmission and sensitivity; a variety of colors and flavors increase condoms’ acceptability and attractiveness (Warner & Steiner, 2007). A wet jelly or dry powder lubricates some condoms. Condoms must be discarded after each single use. They are available without a prescription. The typical failure rate in the first year of male condom use is 15% (Trussell, 2007). To prevent unintended pregnancy and the spread of STIs, it is essential that condoms be used consistently and correctly. Instructions, such as those listed in Box 8-3, can be used for client teaching.
The female condom is a lubricated vaginal sheath made of polyurethane and has flexible rings at both ends (see Fig. 8-7, A). The closed end of the pouch is inserted into the vagina and is anchored around the cervix, and the open ring covers the labia. Women whose partner will not wear a male condom can use this as a protective mechanical barrier. Rewetting drops or oil or water-based lubricants can be used to help decrease the distracting noise that is produced while penile thrusting occurs. The female condom is available in one size, is intended for single use only, and is sold over the counter. Male condoms should not be used concurrently because the friction from both sheaths can increase the likelihood of either or both tearing (Cates & Raymond, 2007). The typical failure rate in the first year of female condom use is 21% (Trussell, 2007).
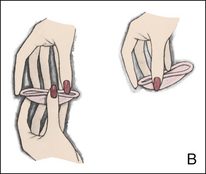
Diaphragms: The contraceptive diaphragm is a shallow dome-shaped latex or silicone device with a flexible rim that covers the cervix (see Fig. 8-7, A). There are four types of diaphragms: coil spring, arcing spring, flat spring, and wide seal rim. Available in many sizes, the diaphragm should be the largest size the woman can wear without her being aware of its presence. The typical failure rate of the diaphragm combined with spermicide is 16% in the first year of use (Trussell, 2007). Effectiveness of the diaphragm is less when used without spermicide. Women at high risk for HIV should avoid use of N-9 spermicides with the diaphragm (Cates & Raymond, 2007).
The woman is informed that she needs an annual gynecologic examination to assess the fit of the diaphragm. The device should be inspected before every use, replaced every 2 years, and may have to be refitted for a 20% weight fluctuation, after any abdominal or pelvic surgery, and after every pregnancy (WHO/RHR & CCP, 2007). Because various types of diaphragms are on the market, the nurse should use the package insert for teaching a woman how to use and care for the diaphragm (see Teaching for Self-Management box: Use and Care of the Diaphragm).
Disadvantages of diaphragm use include the reluctance of some women to insert and remove the diaphragm. Although it can be inserted up to 6 hours before intercourse, a cold diaphragm and a cold gel temporarily reduce vaginal response to sexual stimulation if insertion of the diaphragm occurs immediately before intercourse. Some women or couples object to the messiness of the spermicide. These annoyances of diaphragm use, along with failure to insert the device once foreplay has begun, are the most common reasons for failures of this method. Side effects may include irritation of tissues related to contact with spermicides. The diaphragm is not a good option for women with poor vaginal muscle tone or recurrent urinary tract infections. For proper placement the diaphragm must rest behind the pubic symphysis and completely cover the cervix. To decrease the chance of exerting urethral pressure, the woman should be reminded to empty her bladder before diaphragm insertion and immediately after intercourse. Diaphragms are contraindicated for women with pelvic relaxation (uterine prolapse) or a large cystocele. Women with a latex allergy should not use latex diaphragms.
Toxic shock syndrome (TSS), although reported in very small numbers, can occur in association with the use of the contraceptive diaphragm and cervical caps (Cates & Raymond, 2007). The nurse should instruct the woman about ways to reduce her risk for TSS. These measures include prompt removal 6 to 8 hours after intercourse, not using the diaphragm or cervical caps during menses, and learning and watching for danger signs of TSS.
Cervical Caps: Three types of cervical caps are available; two come in varying sizes and one is one-size-fits-all. They are made of rubber or latex-free silicone and have soft domes and firm brims (see Fig. 8-7, A). The cap fits snugly around the base of the cervix close to the junction of the cervix and vaginal fornices. It is recommended that the cap remain in place no less than 6 hours and not more than 48 hours at a time. It is left in place at least 6 hours after the last act of intercourse. The seal provides a physical barrier to sperm: spermicide inside the cap adds a chemical barrier. The extended period of wear may be an added convenience for women.
Instructions for the actual insertion and use of the cervical cap closely resemble the instructions for the use of the contraceptive diaphragm. Some of the differences are that the cervical cap can be inserted hours before sexual intercourse without a need for additional spermicide later, no additional spermicide is required for repeated acts of intercourse when the cap is used, and the cervical cap requires less spermicide than the diaphragm when initially inserted. The angle of the uterus, the vaginal muscle tone, and the shape of the cervix may interfere with the cervical cap’s ease of fitting and use. Correct fitting requires time, effort, and skill from both the woman and the
clinician. The woman must check the cap’s position before and after each act of intercourse (see Teaching for Self-Management box).
Because of the potential risk of TSS associated with the use of the cervical cap, another form of birth control is recommended for use during menstrual bleeding and up to at least 6 weeks postpartum. The cap should be refitted after any gynecologic surgery or birth and after major weight losses or gains. Otherwise the size should be checked at least once a year.
Women who are not good candidates for wearing the cervical cap include those with abnormal Papanicolaou (Pap) test results, those who cannot be fitted properly with the existing cap sizes, those who find the insertion and removal of the device too difficult, those with a history of TSS, those with vaginal or cervical infections, and those who experience allergic responses to the latex cap or spermicide. Failure rates the first year of use are 16% in nulliparous and 32% in multiparous women (WHO/RHR & CCP, 2007).
Contraceptive Sponge: The vaginal sponge is a small, round polyurethane sponge that contains N-9 spermicide (see previous discussion of N-9) (see Fig. 8-7, B). It is designed to fit over the cervix (one size fits all). The side that is placed next to the cervix is concave for better fit. The opposite side has a woven polyester loop to be used for removal of the sponge.
The sponge must be moistened with water before it is inserted. It provides protection for up to 24 hours and for repeated instances of sexual intercourse. The sponge should be left in place for at least 6 hours after the last act of intercourse. Wearing it longer than 24 to 30 hours may put the woman at risk for TSS (Cates & Raymond, 2007). The typical failure rate in the first year of use is 32% for parous women and 16% for nulliparous women (Trussell, 2007).
Hormonal Methods
More than 30 different hormonal contraceptive formulations are available in the United States today. General classes are described in Table 8-1. Because of the wide variety of preparations available, the woman and the nurse must read the package insert for information about specific products prescribed. Formulations include combined estrogen-progestin medications and progestational agents. The formulations are administered orally, transdermally, vaginally, by implantation, by injection, or by intrauterine insertion.
TABLE 8-1
| COMPOSITION | ROUTE OF ADMINISTRATION | DURATION OF EFFECT |
| Combination estrogen and progestin (synthetic estrogens and progestins in varying doses and formulations) | Oral | 24 hours; extended cycle—12 weeks |
| Transdermal | 7 days | |
| Vaginal ring insertion | 3 weeks | |
| Progestin only: | ||
| Norethindrone, norgestrel | Oral | 24 hours |
| Medroxyprogesterone acetate | Intramuscular injection; subcutaneous injection | 3 months |
| Progestin, etonogestrel | Subdermal implant | Up to 3 years |
| Levonorgestrel | Intrauterine device | Up to 5 years |
Combined Estrogen-Progestin Contraceptives:
Oral Contraceptives: The normal menstrual cycle is maintained by a feedback mechanism. Follicle-stimulating hormone (FSH) and LH are secreted in response to fluctuating levels of ovarian estrogen and progesterone. Regular ingestion of combined oral contraceptive pills (COCs) suppresses the action of the hypothalamus and anterior pituitary, leading to insufficient secretion of FSH and LH; therefore, follicles do not mature, and ovulation is inhibited.
Other contraceptive effects are induced by the combined steroids. Maturation of the endometrium is altered, making it a less favorable site for implantation. COCs also have a direct effect on the endometrium, so that from 1 to 4 days after the last COC is taken, the endometrium sloughs and bleeds as a result of hormone withdrawal. The withdrawal bleeding is usually less profuse than that of normal menstruation and may last only 2 to 3 days. Some women have no bleeding at all. The cervical mucus remains thick from the effect of the progestin (Nelson, 2007).
Cervical mucus under the effect of progesterone does not provide as suitable an environment for sperm penetration as does the thin, watery mucus at ovulation. The possible effect, if any, of altered tubal and uterine motility induced by COCs is not clear.
Monophasic pills provide fixed dosages of estrogen and progestin. Multiphasic pills (e.g., biphasic and triphasic oral contraceptives) alter the amount of progestin and sometimes the amount of estrogen within each cycle. These preparations reduce the total dosage of hormones in a single cycle without sacrificing contraceptive efficacy (Nelson, 2007). To maintain adequate hormonal levels for contraception and enhance compliance, COCs should be taken at the same time each day.
Advantages: Because taking the pill does not relate directly to the sexual act, its acceptability may be increased. Improvement in sexual response may occur once the possibility of pregnancy is not an issue. For some women it is convenient to know when to expect the next menstrual flow.
Evidence of noncontraceptive benefits of oral contraceptives is based on studies of high-dose pills (50 mg estrogen). Few data exist on noncontraceptive benefits of low-dose oral contraceptives (less than 35 mg estrogen) (Nelson, 2007). The noncontraceptive health benefits of COCs include decreased menstrual blood loss and decreased iron deficiency anemia, regulation of menorrhagia and irregular cycles, and reduced incidence of dysmenorrhea and premenstrual syndrome (PMS). Oral contraceptives also offer protection against endometrial cancer and ovarian cancer, reduce the incidence of benign breast disease, improve acne, protect against the development of functional ovarian cysts and salpingitis, and decrease the risk of ectopic pregnancy. Oral contraceptives are considered a safe option for nonsmoking women until menopause. Perimenopausal women can benefit from regular bleeding cycles, a regular hormonal pattern, and the noncontraceptive health benefits of oral contraceptives (Nelson).
A pelvic examination and Pap smear are not necessary before initiating COCs (WHO/RHR & CCP, 2007). If STI screening is indicated, a urine-based test can be used for some infections (e.g. chlamydia, gonorrhea); others will require a pelvic examination and cultures of vaginal or cervical secretions or blood tests (Planned Parenthood, 2010). Most health care providers assess the woman 3 months after beginning COCs to detect any complications.
Use of oral hormonal contraceptives is initiated on one of the first days of the menstrual cycle (day 1 of the cycle is the first day of menses) or after childbirth or abortion. With a “Sunday start,” women begin taking pills on the first Sunday after the start of their menstrual period. If contraceptives are to be started at any time other than during normal menses, or within 3 weeks after birth, miscarriage, or induced abortion, another method of contraception should be used throughout the first week to avoid the risk of pregnancy (Nelson, 2007). Taken exactly as directed, oral contraceptives prevent ovulation, and pregnancy cannot occur; the overall effectiveness rate is almost 100%. Almost all failures (i.e., pregnancy occurs) are caused by omission of one or more pills during the regimen. The typical failure rate of COCs due to omission is 8% (Trussell, 2007).
Disadvantages and Side Effects: Since hormonal contraceptives have come into use, the amount of estrogen and progestational agent contained in each tablet has been reduced considerably. This is important because adverse effects are, to a degree, dose related.
Women must be screened for conditions that present absolute or relative contraindications to oral contraceptive use. Contraindications for COC use include a history of thromboembolic disorders, cerebrovascular or coronary artery disease, breast cancer, gallbladder disease, estrogen-dependent tumors, pregnancy, impaired liver function, liver tumor, lactation less than 6 weeks postpartum, smoking if older than 35 years, headaches with focal neurologic symptoms, surgery with prolonged immobilization or any surgery on the legs, hypertension (140/90 mm Hg), and diabetes mellitus (of more than 20 years’ duration) with vascular disease (Nelson, 2007; WHO/RHR & CCP, 2007).
Certain side effects of COCs are attributable to estrogen, progestin, or both. Serious adverse effects documented with high doses of estrogen and progesterone include stroke, myocardial infarction, thromboembolism, hypertension, gallbladder disease, and liver tumors (Nelson, 2007). Common side effects of estrogen excess include nausea, breast tenderness, fluid retention, and chloasma. Side effects of estrogen deficiency include early spotting (days 1 to 14), hypomenorrhea, nervousness, and atrophic vaginitis leading to painful intercourse (dyspareunia). Side effects of progestin excess include increased appetite, tiredness, depression, breast tenderness, vaginal yeast infection, oily skin and scalp, hirsutism, and postpill amenorrhea. Side effects of progestin deficiency include late spotting and breakthrough bleeding (days 15 to 21), heavy flow with clots, and decreased breast size. One of the most common side effects of combined COCs is bleeding irregularities (Nelson).
In the presence of side effects, especially those that are bothersome to a woman, a different product, a different drug content, or another method of contraception may be required. The “right” product for a woman contains the lowest dose of hormones that prevents ovulation and that has the fewest and least harmful side effects. There is no way to predict the right dosage for any particular woman. Issues to consider in prescribing oral contraceptives include history of oral contraceptive use, side effects during past use, menstrual history, and drug interactions (Nelson, 2007).
Large prospective studies have not shown a relationship between use of oral contraceptives available and diabetes or glucose intolerance (Nelson, 2007). The risks and benefits should be assessed before prescribing oral contraceptives for women who have diabetes with vascular problems.
The effectiveness of oral contraceptives can be negatively influenced when the following medications are taken simultaneously (Nelson, 2007; WHO/RHR & CCP, 2007):
• Anticonvulsants: barbiturates, oxcarbazepine, phenytoin, phenobarbital, felbamate, carbamazepine, primidone, and topiramate
• Systemic antifungals: griseofulvin
No strong pharmacokinetic evidence exists that shows a relation between broad-spectrum antibiotic use and altered hormonal levels among oral contraceptive users, although potential antibiotic interaction can occur. Studies on the incidence of breast cancer in COC users have not found a significant increase of breast cancer in women who use COCs (Nelson, 2007).
After discontinuing oral contraception, return to fertility usually happens quickly, but fertility rates are slightly lower the first 3 to 12 months after discontinuation (Nelson, 2007). Many women ovulate the next month after stopping oral contraceptives. Women who discontinue oral contraception for a planned pregnancy commonly ask whether they should wait before attempting to conceive. Studies indicate that these infants have no greater chance of being born with any type of birth defect than do infants born to women in the general population, even if conception occurred in the first month after the medication was discontinued. Little evidence suggests that oral contraceptives cause postpill amenorrhea. Amenorrhea after oral contraceptive use is probably related to the woman’s menstrual cycle before taking the pill (Nelson).
Nursing Considerations: Many different preparations of oral hormonal contraceptives are available. The nurse reviews the prescribing information in the package insert with the woman. Because of the wide variations, each woman must be clear about the unique dosage regimen for the preparation prescribed for her. Directions for care after missing one or two tablets also vary (Fig. 8-8).
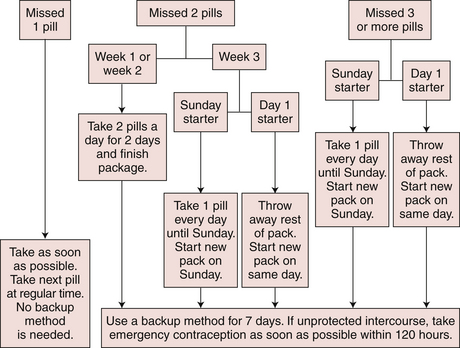
FIG. 8-8 Flowchart for missed active contraceptive pills, 2010. (Courtesy Patsy Huff, PharmD, Chapel Hill, NC.)
Withdrawal bleeding tends to be short and scanty when some combination pills are taken. A woman may see no fresh blood at all. A drop of blood or a brown smudge on a tampon or the underwear counts as a menstrual period.
Only about 68% of women who start taking oral contraceptives are still taking them after 1 year (Trussell, 2007). All women choosing to use oral contraceptives should be provided with a second method of birth control and be instructed in and comfortable with this backup method. Most women stop taking oral contraceptives for nonmedical reasons.
The nurse also reviews the signs of potential complications associated with the use of oral contraceptives (see Signs of Potential Complications box: Oral Contraceptives). Oral contraceptives do not protect a woman against STIs or HIV. A barrier method such as condoms and spermicide should be used for protection.
Oral Contraceptive 91-Day Regimen: Some women prefer to take COCs in 3-month cycles and have fewer menstrual periods. Levonorgestrel/ethinyl estradiol (Seasonale), U.S. Food and Drug Administration (FDA)– approved for extended cycle use, contains both estrogen and progestin and is taken in
3-month cycles of 12 weeks of active pills followed by 1 week of inactive pills. Menstrual periods occur during the thirteenth week of the cycle. There is no protection from sexually transmitted infections, and risks are similar to COCs. Other monophasic COCs may be prescribed for extended cycle use and must be taken on a daily schedule, regardless of the frequency of intercourse. Because users will have fewer menstrual flows, they should consider the possibility of pregnancy if they do not experience their thirteenth-week flows (Nelson, 2007; WHO/RHR & CCP, 2007).
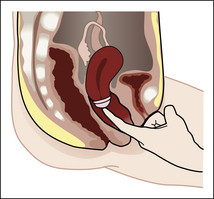
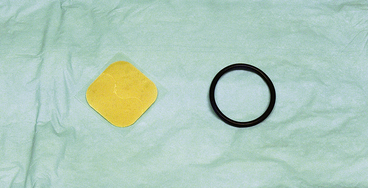
Transdermal Contraceptive System: Available by prescription only, the contraceptive transdermal patch delivers continuous levels of norelgestromin (progesterone) and ethinyl estradiol. The patch can be applied to intact skin of the upper outer arm, the upper torso (front and back, excluding the breasts), the lower abdomen, or the buttocks (Fig. 8-9). Application is on the same day once a week for 3 weeks, followed by a week without the patch. Withdrawal bleeding occurs during the “no-patch” week. Mechanism of action, efficacy, contraindications, skin reactions, and side effects are similar to those of COCs. The typical failure rate during the first year of use is less than 8% in women weighing less than 198 pounds (Trussell, 2007).
Vaginal Contraceptive Ring: Available only with a prescription, the vaginal contraceptive ring is a flexible ring (made of ethylene vinyl acetate copolymer) worn in the vagina to deliver continuous levels of etonorgestrel (progesterone) and ethinyl estradiol (see Fig. 8-9). One vaginal ring is worn for 3 weeks, followed by a week without the ring. The ring is inserted by the woman and does not have to be fitted. Some wearers may experience vaginitis, leukorrhea, and vaginal discomfort (Nanda, 2007). Withdrawal bleeding occurs during the “no-ring” week. If the woman or partner notices discomfort during coitus, the ring can be removed from the vagina, but only up to 3 hours to still be effective when reinserted. Mechanism of action, efficacy, contraindications, and side effects are similar to those of COCs. The typical failure rate of the vaginal contraceptive ring is reportedly less than 8% during the first year of use (Trussell, 2007).
Progestin-Only Contraceptives: Progestin-only methods impair fertility by inhibiting ovulation, thickening and decreasing the amount of cervical mucus, thinning the endometrium, and altering cilia in the uterine tubes (Raymond, 2007b).
Oral Progestins (Minipill): The failure rate of progestin-only pills for typical users is about 1% to 10% in the first year of use (WHO/RHR & CCP, 2007). Effectiveness is increased if minipills are taken correctly. Because minipills contain such a low dose of progestin, the minipill must be taken at the same time every day (Raymond, 2007b). Users often complain of irregular vaginal bleeding.
Injectable Progestins: Depot medroxyprogesterone acetate (DMPA or Depo-Provera), 150 mg, is given intramuscularly in the deltoid or the gluteus maximus muscle. A 21- to 23-gauge needle, 2.5 to 4 cm long, should be used. DMPA should be initiated during the first 5 days of the menstrual cycle and administered every 11 to 13 weeks. A subcutaneous injection is also available (Practice Committee of the American Society for Reproductive Medicine, 2008).
Advantages of DMPA include a contraceptive effectiveness comparable to that of perfect use of COCs, long-lasting effects, requirement of injections only four times a year, and the improbability of lactation being impaired. Side effects at the end of a year include decreased bone mineral density, weight gain, lipid changes, increased risk of venous thrombosis and thromboembolism, irregular vaginal spotting, decreased libido, and breast changes (Goldberg & Grimes, 2007). Other disadvantages include no protection against STIs (including HIV). Return to fertility may be delayed as long as up to 18 months after discontinuing DMPA. The typical failure rate is 3% in the first year of use (Trussell, 2007).
Implantable Progestins: Contraceptive implants are one or more thin rods that contain progestin. The implants are inserted under the skin of the woman’s arm. A single-rod implant
(Implanon) that is effective for up to 3 years is the only implant available in the United States. Implants will prevent some, but not all, ovulatory cycles and will thicken cervical mucus. Other advantages include reversibility and long-term continuous contraception that is not related to frequency of coitus. Irregular menstrual bleeding is the most common side effect. Less common side effects include headaches, nervousness, nausea, skin changes, and vertigo. No STI protection is provided with the implant method, so condoms should be used for protection (Raymond, 2007a).
Emergency Contraception
Emergency contraception (EC) is available in more than 100 countries, and in about one third of these countries it is available without a prescription. In the United States, Plan B has been the only EC method available without a prescription and only in limited pharmacies and clinics in pharmacy access states (states where legislation has been passed to allow this practice)—Alaska, California, Hawaii, Maine, Massachusetts, New Hampshire, New Mexico, Vermont, and Washington. In 2009, the FDA approved Plan B for over-the-counter sale to women ages 17 and older without a prescription (FDA, 2009).
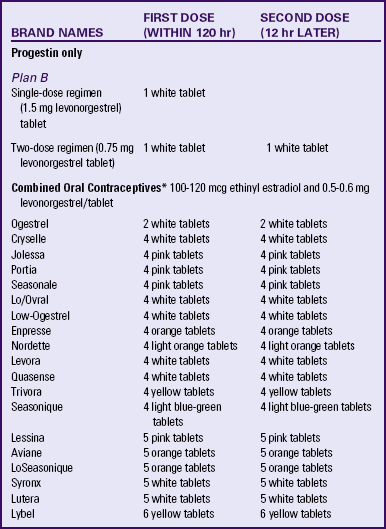
Plan B (levonorgestrel-only) is available in 1 or two dose regimens. Other options that the FDA has determined to be safe for emergency contraception include high doses of oral estrogen or COCs (ECPs) and insertion of a copper IUD (Stewart, Trussell & Van Look, 2007). These options will continue to be available by prescription only.
Emergency contraception should be taken by a woman as soon as possible but within 120 hours of unprotected intercourse, or birth control mishap (broken condom, dislodged ring or cervical cap, missed oral contraceptive pills, late for injection, and so on) to prevent unintended pregnancy (Stewart et al., 2007; WHO/RHR & CCP, 2007). If taken before ovulation, emergency contraception prevents ovulation by inhibiting follicular development. If taken after ovulation occurs, there is little effect on ovarian hormone production or the endometrium. Recommended oral medication regimens with ECPs are presented in Table 8-2. To minimize the side effect of nausea that occurs with high doses of estrogen and progestin, the woman can be advised to take an over-the-counter antiemetic 1 hour before each dose. Women with contraindications for estrogen use should use progestin-only emergency contraception. No medical contraindications for emergency contraception exist, except pregnancy and undiagnosed abnormal vaginal bleeding. If the woman does not begin menstruation within 21 days after taking the pills, she should be evaluated for pregnancy. Emergency contraception is ineffective if the woman is pregnant because the pills do not disturb an implanted pregnancy. Risk of pregnancy is reduced by as much as 75% (estrogen-progestin) and 89% (progestin only) if the woman takes ECPs (Stewart et al., 2007).
IUDs containing copper (see later discussion) provide another emergency contraception option. The IUD should be inserted within 5 days of unprotected intercourse (Stewart et al., 2007). This method is suggested only for women who wish to have the benefit of long-term contraception. The risk of pregnancy is reduced by as much as 99% with emergency insertion of the copper-releasing IUD.
Contraceptive counseling should be provided to all women requesting emergency contraception, including a discussion of modification of risky sexual behaviors to prevent STIs and unwanted pregnancy.
Intrauterine Devices
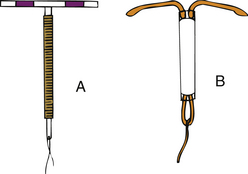
An IUD is a small T-shaped device with bendable arms for insertion through the cervix (Fig. 8-10). Once the trained health care provider inserts the IUD against the uterine fundus, the arms open near the fallopian tubes to maintain position of the device and to adversely affect the sperm motility and irritate the lining of the uterus. Two strings hang from the base of the stem through the cervix and protrude into the vagina for the woman to feel for assurance that the device has not been dislodged (Grimes, 2007). The woman should have had a negative pregnancy test, treatment for dysplasia if present, cervical cultures to rule out STIs, and a consent form signed before IUD insertion. Advantages to choosing this method of contraception include long-term protection from pregnancy and immediate return to fertility when removed. Disadvantages include increased risk of pelvic inflammatory disease (PID) shortly after placement, unintentional expulsion of the device, infection, and possible uterine perforation. IUDs offer no protection against HIV or other STIs. Therefore, women who are in mutually monogamous relationships are the best candidates for this device (see Evidence-Based Practice box).
There are two FDA-approved IUDs, the ParaGard Copper T 380A and the hormonal intrauterine system (Mirena). The ParaGard Copper T 380A is made of radiopaque polyethylene and fine solid copper and is approved for 10 years of use. The copper primarily serves as a spermicide and inflames the endometrium, preventing fertilization (Grimes, 2007). Sometimes women experience more bleeding and cramping within the first year after insertion, but nonsteroidal antiinflammatory drugs (NSAIDs) can be taken for pain relief. The typical failure rate in the first year of use of the copper IUD is less than 1% (Trussell, 2007).
The hormonal intrauterine system (Mirena) releases levonorgestrel from its vertical reservoir. Effective for up to 5 years, it impairs sperm motility, thickens cervical mucus, decreases the lining of the uterus, and has some anovulatory effects (Grimes, 2007). Uterine cramping and bleeding are usually decreased with this device, although irregular spotting are common in the first few months following insertion. The typical failure rate in the first year of use is less than 1% (Trussell, 2007).
Nursing Considerations: The woman should be taught to check for the presence of the IUD strings after menstruation to rule out expulsion of the device. If pregnancy occurs with the IUD in place, an ultrasound should confirm that it is not ectopic. Early removal of the IUD helps decrease the risk of spontaneous miscarriage or preterm labor. The woman should report any signs of flulike illness because this may indicate a septic miscarriage (Grimes, 2007). In some women who are allergic to copper, a rash develops, necessitating the removal of the copper-bearing IUD. Signs of potential complications to be taught to the woman are listed in the Signs of Potential Complications box.
Sterilization
Sterilization refers to surgical procedures intended to render a person infertile. Most procedures involve the occlusion of the passageways for the ova and sperm (Fig. 8-11). For the woman,
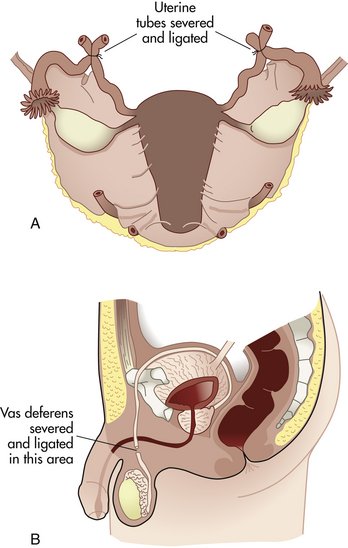
FIG. 8-11 Sterilization. A, Uterine tubes severed and ligated (tubal ligation). B, Sperm duct severed and ligated (vasectomy).
the oviducts (uterine tubes) are occluded; for the man, the sperm ducts (vas deferens) are occluded. Only surgical removal of the ovaries (oophorectomy) or uterus (hysterectomy) or both will result in absolute sterility for the woman. All other sterilization procedures have a small but definite failure rate; that is, pregnancy may result.
Female Sterilization: Female sterilization (bilateral tubal ligation [BTL]) may be done immediately after childbirth (within 24 to 48 hours), concomitant with induced abortion, or as an interval procedure (during any phase of the menstrual cycle). If sterilization is performed as an interval procedure, the health care provider must be certain that the woman is not pregnant. Half of all female sterilization procedures are performed immediately after a pregnancy (Pollack, Thomas, & Barone, 2007). Sterilization procedures can be safely done on an outpatient basis.
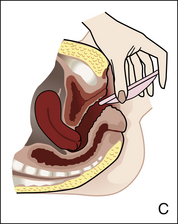
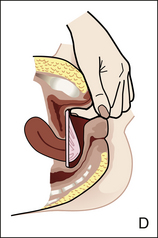
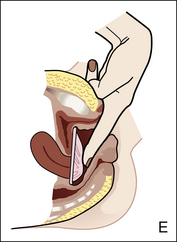
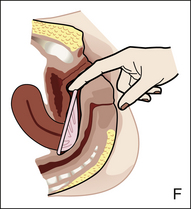
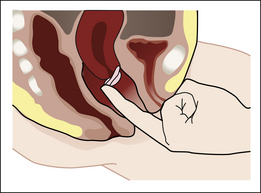
Tubal Occlusion: A laparoscopic approach or a minilaparotomy can be used for tubal ligation (Fig. 8-12), tubal electrocoagulation, or the application of bands or clips. Electrocoagulation and ligation are considered to be permanent methods. Use of the bands or clips has the theoretic advantage of possible removal and return of tubal patency.
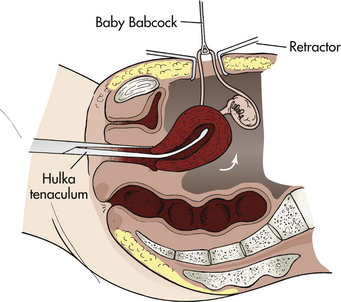
FIG. 8-12 Use of minilaparotomy to gain access to uterine tubes for occlusion procedures. Tenaculum is used to lift uterus (arrow) toward incision.
For the minilaparotomy, the woman is admitted the morning of surgery, having received nothing by mouth since midnight. Preoperative sedation is given. The procedure can be carried out with a local anesthetic, but a regional or general anesthetic also can be used. A small incision is made in the abdominal wall below the umbilicus. The woman may experience sensations of tugging, but no pain, and the operation is completed within 20 minutes. She may be discharged several hours later if she has recovered from anesthesia, or next day if done postpartum. Any abdominal discomfort usually can be controlled with a mild analgesic (e.g., acetaminophen). Within days the scar is almost invisible (see Teaching for Self-Management box: What to Expect After Tubal Ligation). As with any surgery, there is always a possibility of complications of anesthesia, infection, hemorrhage, and trauma to other organs.
Transcervical Sterilization: Still considered experimental, hysteroscopic techniques can be used to inject occlusion agents into the uterine tubes. One FDA-approved device is the Essure system, an interval sterilization method (not intended for the postpartum period). A trained health care professional inserts a small catheter holding the polyester fibers through the vagina and cervix and places the small metallic implants into each uterine tube. The device works by stimulating the woman’s own scar tissue formation to occlude the uterine tubes and prevent conception (Abbott, 2007). An advantage is that the nonhormonal form of contraception can be inserted during an office procedure without anesthesia. Analgesia is recommended to decrease mild to moderate discomfort associated with tubal spasm. Particularly convenient for obese women, or those with abdominal adhesions, the transcervical approach eliminates the need for abdominal surgery. Because the procedure is not immediately effective, it is essential that the woman and her partner use another form of contraception until tubal blockage is proven. It may take up to 3 months for tubal occlusion to fully occur, and success must be confirmed by hysterosalpingogram. Other disadvantages include expulsion and perforation. The typical failure rate during the first year of use of the Essure system is less than 1%. Long-term efficacy and safety rates are unknown (Hastings-Tolsma, Nodine, & Teal, 2006).
Tubal Reconstruction: Restoration of tubal continuity (reanastomosis) and function is technically feasible except after laparoscopic tubal electrocoagulation. Sterilization reversal, however, is costly, difficult (requiring microsurgery), and uncertain. The success rate varies with the extent of tubal destruction and removal. The risk of ectopic pregnancy after tubal reanastomosis is increased by 1% to 7% (Pollack et al., 2007).
Male Sterilization: Vasectomy is the sealing, tying, or cutting of a man’s vas deferens so that the sperm cannot travel from the testes to the penis (Pollack et al., 2007). It is considered the easiest and most commonly used operation for male sterilization. Vasectomy can be carried out with local anesthesia on an outpatient basis. Pain, bleeding, infection, and other postsurgical complications are considered the disadvantages to the surgical procedure. It is considered a permanent method of sterilization because reversal is generally unsuccessful.
Two methods are used for scrotal entry: conventional (scalpel incision) and no-scalpel (small puncture) vasectomy. The surgeon identifies and immobilizes the vas deferens through the scrotum. Then the vas is ligated or cauterized (see Fig. 8-11, B). Surgeons vary in their techniques to occlude the vas deferens: ligation with sutures, division, cautery, application of clips, excision of a segment of the vas, fascial interposition, or some combination of these methods (Pollack et al., 2007).
The man is instructed in self-care to promote a safe return to routine activities. To reduce swelling and relieve discomfort, ice packs are applied to the scrotum intermittently for a few hours after surgery. A scrotal support may be applied to decrease discomfort. Moderate inactivity for about 2 days is advisable because of local scrotal tenderness. The skin suture can be removed 5 to 7 days after surgery. Sexual intercourse may be resumed as desired; however, sterility is not immediate. Some sperm will remain in the proximal portions of the sperm ducts after vasectomy. One week to several months are required to clear the ducts of sperm; therefore, some form of contraception is needed until the sperm count in the ejaculate on two consecutive tests is down to zero (Pollack et al., 2007).
Vasectomy has no effect on potency (ability to achieve and maintain erection) or volume of ejaculate. Endocrine production of testosterone continues, so secondary sex characteristics are not affected. Sperm production continues, but sperm are unable to leave the epididymis and are lysed by the immune system. Men occasionally may develop a hematoma, infection, or epididymitis (Pollack et al., 2007). Less common are painful granulomas from accumulation of sperm.
Complications after bilateral vasectomy are uncommon and usually not serious. They include bleeding (usually external), suture reaction, and reaction to anesthetic agent. The failure rate for male sterilization is 0.15% (Trussell, 2007).
Tubal Reconstruction: Microsurgery to reanastomose (restoration of tubal continuity) the sperm ducts can be accomplished successfully in more than 90% of cases (i.e., sperm in the ejaculate); however, the fertility rate varies widely from 38% to 89% (Pollack et al., 2007). The rate of success decreases as the time since the procedure increases. The vasectomy may result in permanent changes in the testes that leave men unable to father children. The changes are those ordinarily seen only in older adults (e.g., interstitial fibrosis [scar tissue between the seminiferous tubules]). In some men, antibodies develop against their own sperm (autoimmunization). The role of antisperm antibodies in fertility after vasectomy reversal has not been completely determined. Additional research is needed to explore a possible link between vasectomy and prostate cancer.
Laws and Regulations: All states have strict regulations for informed consent. Many states permit voluntary sterilization of any mature, rational woman without reference to her marital or pregnancy status. Although the partner’s consent is not required by law, the man or woman is encouraged to discuss the situation with the partner, and health care providers may request the partner’s consent. Sterilization of minors or mentally incompetent individuals is restricted by most states and often requires the approval of a board of eugenicists or other court-appointed individuals (see Legal Tip).
Nursing Considerations: The nurse plays an important role in assisting people with decision making so all requirements for informed consent are met. The nurse also provides information about alternatives to sterilization, such as contraception. The nurse acts as a “sounding board” for people who are exploring the possibility of choosing sterilization and their feelings about and motivation for this choice. The nurse records this information, which may be the basis for referral to a family-planning clinic, a psychiatric social worker, or another professional health care provider.
Information must be given about what is entailed in various procedures, how much discomfort or pain can be expected, and what type of care is needed. Many individuals fear sterilization procedures because of the imagined effect on their sex life. They need reassurance concerning the hormonal and psychologic basis for sexual function and that uterine tube occlusion or vasectomy has no biologic sequelae in terms of sexual adequacy (Pollack et al., 2007). Preoperative care includes health assessment, which includes a psychologic assessment, physical examination, and laboratory tests. The nurse assists with the health assessment, answers questions, and confirms the client’s understanding of printed instructions (e.g., nothing by mouth after midnight). Ambivalence and extreme fear of the procedure are reported to the physician.
Postoperative care depends on the procedure performed (e.g., laparoscopy, laparotomy for tubal occlusion, or vasectomy). General care includes recovery after anesthesia, monitoring of vital signs and fluid and electrolyte balance (intake and output, laboratory values), prevention of or early identification and treatment for infection or hemorrhage, control of discomfort, and assessment of emotional response to the procedure and recovery.
Discharge planning depends on the type of procedure performed. In general, the client is given written instructions about observing for and reporting symptoms and signs of complications, the type of recovery to be expected, and the date and time for a follow-up appointment.
Breastfeeding: Lactational Amenorrhea Method
The lactational amenorrhea method (LAM) can be a highly effective, temporary method of birth control. It is more popular in underdeveloped countries and traditional societies, where breastfeeding is used to prolong birth intervals. The method has seen limited use in the United States since most American women do not establish breastfeeding patterns that provide maximum protection against pregnancy (Kennedy & Trussell, 2007).
When the infant suckles at the mother’s breast, a surge of prolactin hormone is released, which inhibits estrogen production and suppresses ovulation and the return of menses. LAM works best if the mother is exclusively or almost exclusively breastfeeding, if the woman has not had a menstrual flow since giving birth, and if the infant is younger than 6 months of age. Effectiveness is enhanced by frequent feedings at intervals of less than 4 hours during the day and no more than 6 hours during the night, long duration of each feeding, and no bottle supplementation or limited supplementation by spoon or cup. The woman should be counseled that disruption of the breastfeeding pattern or supplementation can increase the risk of pregnancy. The typical failure rate is 2% (Kennedy & Trussell, 2007; King, 2007).
Future Trends
Contraceptive options are more limited in the United States and Canada than in some other industrialized countries. Lack of funding for research, governmental regulations, conflicting values about contraception, and high costs of liability coverage for contraception have been cited as blocks to new and improved methods. Existing methods of contraception are being improved, however, and a variety of new methods are being developed.
Lower-dose COCs (15 mcg of ethinyl estradiol) are available in Europe. Female barrier methods (new female condoms, client-fitted diaphragms, and new vaginal sponges) are being tested. Vaginal delivery systems including progestin-only vaginal rings and progesterone daily suppositories are under investigation. Two new IUDs and spermicidal microbicides are being evaluated. Male hormonal methods are also being investigated, including hormonal injections (testosterone), gonadotropin-releasing hormone antagonists, antisperm compounds, immunologic methods, and contraceptive vaccines (Blithe, 2008; Gabelnick, Schwartz, & Darroch, 2007).
Induced Abortion
Induced abortion is the purposeful interruption of a pregnancy before 20 weeks of gestation. (Spontaneous abortion [miscarriage] is discussed in Chapter 28.) If the abortion is performed at the woman’s request, the term elective abortion is used; if performed for reasons of maternal or fetal health or disease, the term therapeutic abortion applies. Many factors contribute to a woman’s decision to have an abortion. Indications include (1) preservation of the life or health of the mother, (2) genetic disorders of the fetus, (3) rape or incest, and (4) the pregnant woman’s request. The control of birth, dealing as it does with human sexuality and the question of life and death, is one of the most emotional components of health care and has been the most controversial social issue in the last half of the 20th century and continues to be so today. Regulations exist to protect the mother from the complications of abortion.
Abortion is regulated in most countries, including the United States. Before 1970, legal abortion was not widely available in the United States. However, in January 1973, the U.S. Supreme Court set aside previous antiabortion laws and legalized abortion. This decision established a trimester approach to abortion. In the first trimester, abortion is permissible, the decision is between the woman and her health care provider, and a state has little right to interfere (Paul & Stewart, 2007). In the second trimester, abortion is left to the discretion of the individual states to regulate procedures as long as they are reasonably related to the woman’s health. In the third trimester, abortions may be limited or even prohibited by state regulation unless the restriction interferes with the life or health of the pregnant woman (Paul & Stewart).
In 1992, the U.S. Supreme Court made another landmark ruling, this time allowing states to restrict early abortion services as long as the restrictions did not place an “undue burden” on the woman’s ability to choose abortion. Since then many bills have been introduced to limit access and funds for women seeking abortion. In 2006, several states introduced bills to ban most abortions; the U.S. Supreme Court will again play a major role in deciding the future of abortions. Hospitals maintained by Roman Catholics and some of those maintained by strict fundamentalists forbid abortion (and often sterilization) despite legal challenges.
Incidence
The number of abortions performed in the United States in 2006 was 846,181 (Pazol, Gamble, Parker, Cook, Zane, & Hamdan, 2009). Most abortions are performed in the first trimester, with about 62% in the first 8 weeks after the last menstrual period. Only about 5% of abortions are performed after 16 weeks of gestation. Most women who are having an elective abortion are Caucasian, between the ages of 20 to 29 years, and unmarried (Pazol et al.). In 2006, an estimated 91,377 abortions were performed in Canada (Statistics Canada, 2010).
The Decision to Have an Abortion
A woman who is deciding whether to have an abortion is often ambivalent. She needs information and an opportunity to discuss her feelings about pregnancy, abortion, and the effect of either choice on her future. She needs to make her decision without feeling coerced (Levi, Simmonds, & Taylor, 2009).
Nurses and other health care providers often struggle with the same values and moral convictions as those of the pregnant woman. The conflicts and doubts of the nurse can be readily communicated to women who are already anxious and overly sensitive. Regardless of personal views on abortion, nurses who provide care to women seeking abortion have an ethical responsibility to counsel women about their options and to make appropriate referrals (Levi et al., 2009).
The Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN, 2009) continues to support a nurse’s right to choose to participate or not in abortion procedures in keeping with his or her “personal, moral, ethical, or religious beliefs.” AWHONN also advocates that “nurses have a professional obligation to inform their employers, at the time of employment, of any attitudes and beliefs that may interfere with essential job functions.”
Care Management
A thorough assessment is conducted through history, physical examination, and laboratory tests. The length of pregnancy and the condition of the woman must be determined to select the appropriate type of abortion procedure. An ultrasound examination should be performed before a second-trimester abortion is done. If the woman is Rh negative, she is a candidate for prophylaxis against Rh isoimmunization. She should receive Rho(D) immune globulin within 72 hours after the abortion if she is D negative and if Coombs’ test results are negative (if the woman is unsensitized or isoimmunization has not developed).
The woman’s understanding of alternatives, the types of abortions, and expected recovery are assessed. Misinformation and gaps in knowledge are identified and corrected. The record is reviewed for the signed informed consent, and the woman’s understanding is verified. General preoperative, operative, and postoperative assessments are performed.
Analysis of data leads to identification of the appropriate nursing diagnoses for the woman undergoing elective abortion. Potential nursing diagnoses are listed in Box 8-4.
Counseling about abortion includes help for the woman in identifying how she perceives the pregnancy, information about the choices available (i.e., having an abortion or carrying the pregnancy to term and then either keeping the infant or placing the baby for adoption), and information about the types of abortion procedures.
First-Trimester Abortion
Methods for performing early abortion (less than 9 weeks of gestation) include surgical (aspiration) and medical methods (mifepristone with misoprostol, and methotrexate with misoprostol).
Aspiration
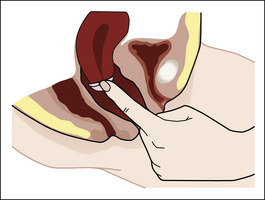
Aspiration (vacuum or suction curettage) is the most common procedure in the first trimester, with almost 88% of all procedures being performed by this method (Pazol et al., 2009). Aspiration abortion is usually performed under local anesthesia in the physician’s office, the clinic, or the hospital. The suction procedure for performing an early elective abortion (ideal time is 8 to 12 weeks since the last menstrual period) usually requires less than 5 minutes.
A bimanual examination is done before the procedure to assess uterine size and position. A speculum is inserted and the cervix is anesthetized with a local anesthetic agent. The cervix is dilated if necessary and a cannula connected to suction is inserted into the uterine cavity. The products of conception are evacuated from the uterus.
During the procedure the nurse or physician keeps the woman informed about what to expect next (e.g., menstrual-like cramping, sounds of the suction machine). The nurse assesses the woman’s vital signs. The aspirated uterine contents must be carefully inspected to ascertain whether all fetal parts and adequate placental tissue have been evacuated. After the abortion the woman rests on the table until she is ready to stand. She remains in the recovery area or waiting room for 1 to 3 hours for detection of excessive cramping or bleeding; then she is discharged.
Bleeding after the operation is normally about the equivalent of a heavy menstrual period, and cramps are rarely severe. Excessive vaginal bleeding and infection, such as endometritis or salpingitis, are the most common complications of elective abortion. Retained products of conception are the primary cause of vaginal bleeding. Evacuation of the uterus, uterine massage, and administration of oxytocin or methylergonovine (Methergine) or both may be necessary. Prophylactic antibiotics to decrease the risk of infection are commonly prescribed (Paul & Stewart, 2007). Postabortion pain may be relieved with NSAIDs such as ibuprofen.
Postabortion instructions differ among health care providers (e.g., tampons should not be used for at least 3 days or should be avoided for up to 3 weeks, and resumption of sexual intercourse may be permitted within 1 week or discouraged for 2 weeks). The woman may shower daily. Instruction is given to watch for excessive bleeding and other signs of complications and to avoid douches of any type.
The woman may expect her menstrual period to resume 4 to 6 weeks from the day of the procedure. Information about the birth control method the woman prefers is offered, if this has not been done previously during the counseling interview that usually precedes the decision to have an abortion. Some methods can be initiated immediately such as an IUD insertion. Hormonal methods may be started immediately or within a week (Paul & Stewart, 2007). The woman must be strongly encouraged to return for her follow-up visit so complications can be detected. A pregnancy test may also be performed at that time to determine whether the pregnancy was successfully terminated.
Medical Abortion
Early medical abortion has been popular in Canada and Europe for more than 15 years, but it is a relatively new procedure in the United States. Medical abortions are available for use in the United States for up to 9 weeks after the last menstrual period. Methotrexate, misoprostol, and mifepristone are the drugs used in the current regimens to induce early abortion. About 11% of all reported abortion procedures in 2006 were medical procedures (Pazol et al., 2009).
Methotrexate is a cytotoxic drug that causes early abortion by blocking folic acid in fetal cells so that they cannot divide. Misoprostol (Cytotec) is a prostaglandin analog that acts directly on the cervix to soften and dilate and on the uterine muscle to stimulate contractions. Mifepristone, formerly known as RU 486, was approved by the FDA in 2000. It works by binding to progesterone receptors and blocking the action of progesterone, which is necessary for maintaining pregnancy (Paul & Stewart, 2007).
Methotrexate and Misoprostol: There is no standard protocol, but methotrexate is given intramuscularly or orally (usually mixed with orange juice). Vaginal placement of misoprostol follows in 3 to 7 days. The woman returns for a follow-up visit in 1 week to confirm the abortion is complete. If not, the woman is offered an additional dose of misoprostol, or vacuum aspiration is performed (Paul & Stewart, 2007).
Mifepristone and Misoprostol: Mifepristone can be taken up to 7 weeks after the last menstrual period. The FDA-approved regimen is that the woman takes 600 mg of mifepristone orally; 48 hours later she returns to the office and takes 400 mcg of misoprostol orally (unless abortion has already occurred and been confirmed). Two weeks after the administration of mifepristone, the woman must return to the office for a clinical examination or ultrasound to confirm that the pregnancy has been terminated. In 1% to 5% of cases, the drugs do not work, and surgical abortion (aspiration) is needed (Paul & Stewart, 2007).
Research has demonstrated a more effective regimen that has fewer side effects. This regimen can be given up to 9 weeks after the last menstrual period and includes administration of 200 mg mifepristone orally followed by misoprostol 800 mcg vaginally in 24 to 48 hours. This vaginal insertion can be done at home by the woman. A follow-up visit is in 4 to 8 days (Paul & Stewart, 2007).
With any medical abortion regimen, the woman usually will experience bleeding and cramping. Side effects of the medications include nausea, vomiting, diarrhea, headache, dizziness, fever, and chills. These are attributed to misoprostol and usually subside in a few hours after administration (Paul & Stewart, 2007).
Second-Trimester Abortion
Second-trimester abortion is associated with more complications and costs than first-trimester abortions. Dilation and evacuation (D&E) accounts for almost all procedures performed in the United States. Induction of uterine contractions with hypertonic solutions (e.g., saline, urea) injected directly into the uterus and uterotonic agents (e.g., misoprostol, dinoprostone) account for only about 0.5% of all abortions (Pazol et al., 2009).
Dilation and Evacuation
D&E can be performed at any point up to 20 weeks of gestation although it is most commonly performed between 13 and 16 weeks of gestation (Paul & Stewart, 2007). The cervix requires more dilation because the products of conception are larger. Often, osmotic dilators (e.g., laminaria) are inserted several hours or several days before the procedure, or misoprostol can be applied to the cervix. The procedure is similar to vaginal aspiration except a larger cannula is used and other instruments may be needed to remove the fetus and placenta. Nursing care includes monitoring vital signs, providing emotional support, administering analgesics, and postoperative monitoring. Disadvantages of D&E may include possible long-term harmful effects to the cervix.
Nursing Considerations
The woman will need help exploring the meaning of the various alternatives and consequences to herself and her significant others. It is often difficult for a woman to express her true feelings (e.g., what having an abortion means to her now and how she may feel about her decision in the future and what support or regret her friends and peers may demonstrate). A calm, matter-of-fact approach on the part of the nurse can be helpful (e.g., “Yes, I know you are pregnant. I am here to help. Let’s talk about alternatives.”). Listening to what the woman has to say and encouraging her to speak are essential. Neutral responses such as “Oh,” “Uh-huh,” and “Umm,” and nonverbal encouragement such as nodding, maintaining eye contact, and use of touch are helpful in setting an open, accepting environment. Clarifying, restating, and reflecting statements, open-ended questions, and feedback are communication techniques that can be used to maintain a realistic focus on the situation and bring the woman’s problems into the open.
Information about alternatives to abortion such as referral to adoption agencies or to support services if the woman chooses to keep her baby should be provided. If a decision is made to have an abortion, the woman must be assured of continued support. Information about what is entailed in various procedures, how much discomfort or pain can be expected, and what type of care is needed must be given. A discussion of the various feelings including depression, guilt, regret, and relief that the woman might experience after the abortion is needed. Information about community resources for postabortion counseling may be needed (Paul & Stewart, 2007). If family or friends cannot be involved, scheduling time for nursing personnel to give the necessary support is an essential component of the care plan.
After an abortion, studies have indicated that most women report relief, but some have temporary distress or mixed emotions. A systematic review of the literature found no difference in the long-term mental health outcomes of women who had abortions and women who did not have abortions (Charles, Polis, Sridhara, & Blum, 2008). Because symptoms can vary among women who have had abortions, nurses must assess women for grief reactions and facilitate the grieving process through active listening and nonjudgmental support and care.
![]() Audio Chapter Summaries Access an audio summary of the Key Points on
Audio Chapter Summaries Access an audio summary of the Key Points on ![]()
KEY POINTS
• A variety of contraceptive methods are available with various effectiveness rates, advantages, and disadvantages.
• Women and their partners should choose the contraceptive method or methods best suited to them.
• Effective contraceptives are available through prescription and nonprescription sources.
• A variety of techniques are available to enhance the effectiveness of periodic abstinence in motivated couples who prefer this natural method.
• Hormonal contraception includes both precoital and postcoital prevention through various modalities and requires thorough client education.
• The barrier methods of diaphragm and cervical cap provide safe and effective contraception for women or couples motivated to use them consistently and correctly
• Intrauterine devices can provide long-term (5 to 10 years) protection.
• Emergency contraception should be taken as soon as possible after unprotected intercourse, but no later than 120 hours.
• Proper, concurrent use of spermicides and latex condoms provides protection against STIs.
• Tubal ligations and vasectomies are permanent sterilization methods used by increasing numbers of women and men.
• Induced abortion performed in the first trimester is safer than an abortion performed in the second trimester.
• The most common complications of induced abortion include infection, retained products of conception, and excessive vaginal bleeding.