Maternal and Fetal Nutrition
• Explain recommended maternal weight gain during pregnancy.
• Compare the recommended level of intake of energy sources, protein, and key vitamins and minerals during pregnancy and lactation.
• Give examples of the food sources that provide the nutrients required for optimal maternal nutrition during pregnancy and lactation.
• Examine the role of nutritional supplements during pregnancy.
• List five nutritional risk factors during pregnancy.
• Compare the dietary needs of adolescent and mature pregnant women.
• Analyze examples of eating patterns of women from two different ethnic or cultural backgrounds, and identify potential dietary problems.
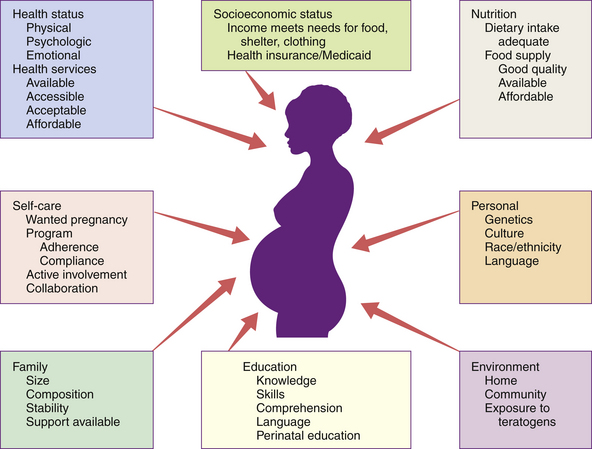
Nutrition is one of many factors that influence the outcome of pregnancy (Fig. 14-1). However, maternal nutritional status is an especially significant factor, both because it is potentially alterable and because good nutrition before and during pregnancy is an important preventive measure for a variety of problems. These problems include birth of low-birth-weight (LBW; birth weight of 2500 g or less) and preterm infants. Evidence is growing that a mother’s nutrition and lifestyle affect the long-term health of her children (Gardiner, Nelson, Shellhaas, Dunlop, Long, Andrist, & Jack, 2008). Thus the importance of good nutrition must be emphasized to all women of childbearing potential. Key components of nutrition care during the preconception period and pregnancy include:
• Nutrition assessment that includes appropriate weight for height and adequacy and quality of dietary intake and habits
• Diagnosis of nutrition-related problems or risk factors such as diabetes, phenylketonuria (PKU), and obesity
• Intervention based on an individual’s dietary goals and plan to promote appropriate weight gain, ingestion of a variety of foods, appropriate use of dietary supplements, and physical activity
• Evaluation as an integral part of the nursing care provided to women during the preconception period and pregnancy, with referral to a nutritionist or dietitian as necessary (Gardiner et al.)
Nutrient Needs Before Conception
The first trimester of pregnancy is crucial in terms of embryonic and fetal organ development. A healthful diet before conception is the best way to ensure that adequate nutrients are available for the developing fetus. Folate or folic acid intake is of particular concern in the periconception period. Folate is the form in which this vitamin is found naturally in foods, and folic acid is the form used in fortification of grain products and other foods and in vitamin supplements. Neural tube defects, or failures in closure of the neural tube, are more common in infants of women with poor folic acid intake. Proper closure of the neural tube is required for normal formation of the spinal cord, and the neural tube begins to close within the first month of gestation, often before the woman realizes that she is pregnant. It is estimated that the incidence of neural tube defects could be decreased 50% to 70% if all women had an adequate folate intake during the periconception period (National Center on Birth Defects and Developmental Disabilities, 2010; Wolff, Witkop, Miller, & Syed, 2009). All women capable of becoming pregnant are advised to consume 0.4 mg (400 mcg) of folic acid daily in fortified foods (ready-to-eat cereals and enriched grain products) or supplements, in addition to a diet rich in folate-containing foods: green leafy vegetables, whole grains, and fruits (Box 14-1) (Otten, Hellwig, & Meyers, 2006).
Maternal as well as fetal risks in pregnancy are increased when the mother is significantly underweight or overweight when pregnancy begins. Ideally all women would achieve their desirable body weights before conception.
Nutrient Needs During Pregnancy
Nutrient needs are determined, at least in part, by the stage of gestation, in that the amount of fetal growth varies during the different stages of pregnancy. During the first trimester the synthesis of fetal tissues places relatively few demands on maternal nutrition; therefore, during the first trimester, when the embryo or fetus is very small, the needs are only slightly greater than those before pregnancy. In contrast, the last trimester is a period of noticeable fetal growth, when most of the fetal stores of energy and minerals are deposited. Therefore, as fetal growth progresses during the second and third trimesters, the pregnant woman’s need for some nutrients increases greatly. Factors that contribute to the increase in nutrient needs include the following:
• The uterine-placental-fetal unit
• Maternal blood volume and constituents: During pregnancy the total blood volume increases by about 40% to 50% over the nonpregnant state.
• Maternal mammary development
• Metabolic needs: Basal metabolic rates, when expressed as kilocalories (kcal) per minute, are approximately 20% higher in pregnant women than in nonpregnant women. This increase includes the energy cost for tissue synthesis.
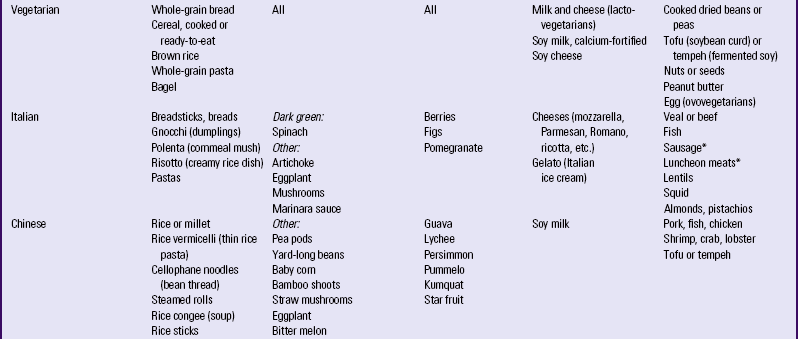
Dietary reference intakes (DRI)s (www.nap.edu) have been established for the people of the United States and Canada, and are updated regularly. The DRIs include recommendations for daily nutritional intakes that meet the needs of almost all (97% to 98%) of the healthy members of the population. They are divided into age, sex, and life-stage categories (e.g., infancy, pregnancy, and lactation), and they can be used as goals in planning individuals’ diets (Table 14-1).
TABLE 14-1
RECOMMENDATIONS FOR DAILY INTAKES OF SELECTED NUTRIENTS DURING PREGNANCY AND LACTATION
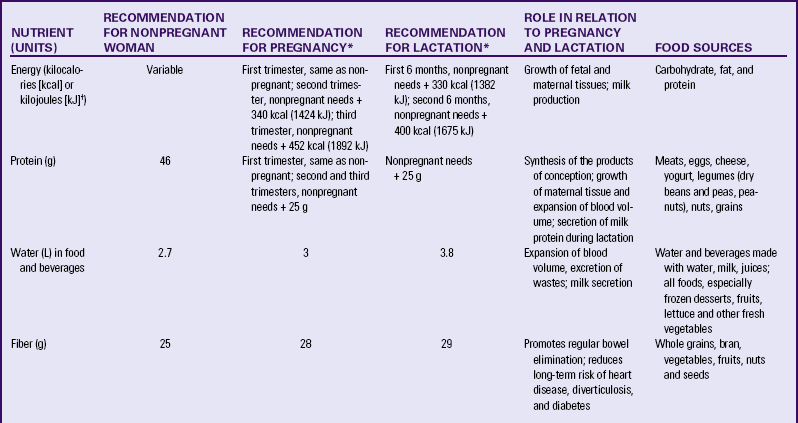
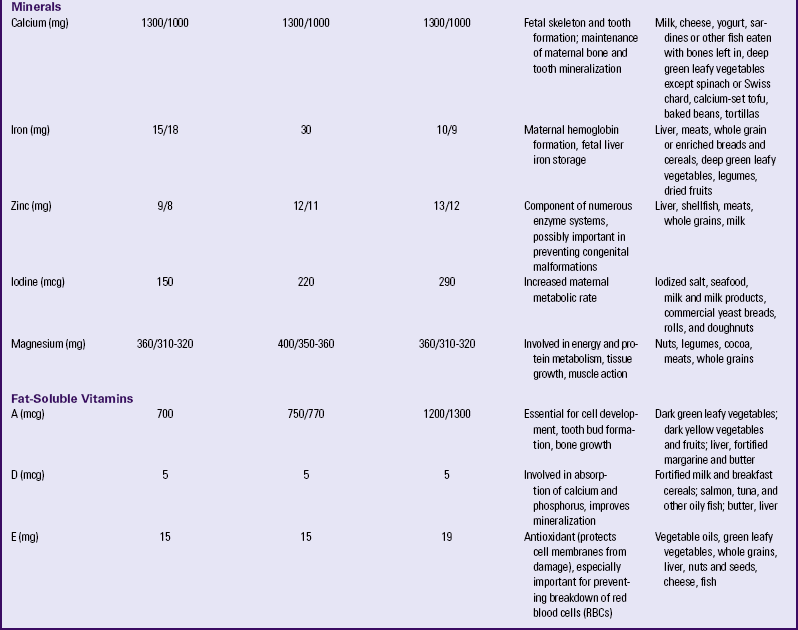
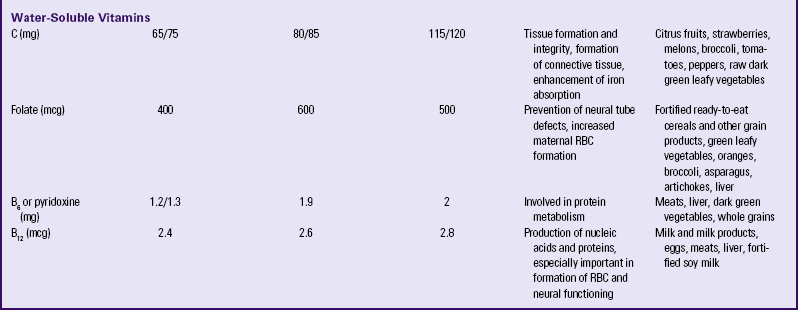
∗When two values appear, separated by a diagonal slash, the first is for females younger than 19 years, and the second is for those 19 to 50 years of age.
†The international metric unit of energy measurement is the joule (J). 1 kcal = 4.184 kJ.
Source: Institute of Medicine. (2005). Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. Washington, DC: National Academies Press; Institute of Medicine. (2006). Dietary reference intakes: The essential guide. Washington, DC: National Academies Press; Institute of Medicine. (2004). Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Washington, DC: National Academies Press.
Energy Needs
Energy (kilocalories [kcal]) needs are met by carbohydrate, fat, and protein in the diet. No specific recommendations exist for the amount of carbohydrate and fat in the diet of the pregnant woman, but the intake of these nutrients should be adequate to support the recommended weight gain. Although protein can be used to supply energy, its primary role is to provide amino acids for the synthesis of new tissues (see discussion later in chapter). Longitudinal assessment of weight gain during pregnancy is the best way to determine whether the kcal intake is adequate; very underweight or active women may require more than the recommended increase in kcal to sustain the desired rate of weight gain.
Weight Gain
The desirable weight gain during pregnancy varies among women. The primary factor to consider in making a weight gain recommendation is the appropriateness of the prepregnancy weight for the woman’s height, that is, whether the woman’s weight was normal before pregnancy or whether she was underweight or overweight. Whenever possible the woman should achieve a weight in the normal range for her height before pregnancy. Maternal and fetal risks in pregnancy are increased when the mother is significantly underweight or overweight before pregnancy and when weight gain during pregnancy is either too low or too high. Severely underweight women are more likely to have preterm labor and to give birth to LBW infants. Both normal-weight and underweight women with inadequate weight gain have an increased risk of giving birth to an infant with intrauterine growth restriction (IUGR). Greater-than-expected weight gain during pregnancy may occur for many reasons, including multiple gestation, edema, gestational hypertension, and overeating. When obesity is present (either preexisting obesity or obesity that develops during pregnancy), there is an increased likelihood of macrosomia and fetopelvic disproportion; operative vaginal birth; emergency cesarean birth; postpartum hemorrhage; wound, genital tract, or urinary tract infection; birth trauma; and late fetal death (Bhattacharya, Campbell, Liston, & Bhattacharya, 2007; Khashan & Kenny, 2009; Viswanathan, Siega-Riz, Moos, Deierlein, Mumford, Knaack, et al., 2008). Obese women are more likely than normal-weight women to have preeclampsia and gestational diabetes.
A commonly used method of evaluating the appropriateness of weight for height is the body mass index (BMI), which is calculated by the following formula:
in which the weight is in kilograms and height is in meters. Thus for a woman who weighed 81 kg before pregnancy and is 1.68 m tall:
Prepregnant BMI can be classified into the following categories: less than 18.5, underweight; 18.5 to 24.9, normal; 25 to 29.9, overweight; and 30 or greater, obese (Institute of Medicine [IOM], 2009). A tool for estimating the BMI without the need for calculation can be found at www.nhlbi.nih.gov/guidelines/obesity/bmi_tbl.pdf.
At the first health care visit the pregnant woman should be helped to establish a weight gain goal for pregnancy that is suited to her prepregnancy weight. Progress toward this goal should be monitored at each visit.
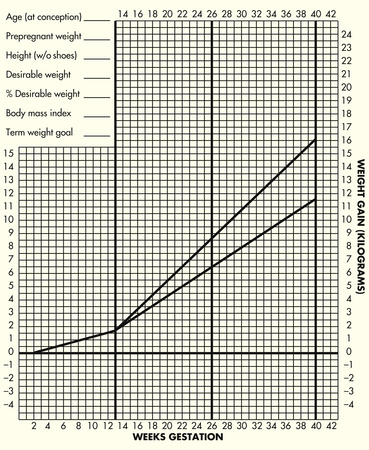
For women with single fetuses, current recommendations are that women with normal BMI should gain 11.5 to 16 kg (25 to 35 lb) during pregnancy (Fig. 14-2). Box 14-2 lists recommended weight gain for pregnancies with single fetuses, twin gestations and multifetal (more than 2) gestations for women who are normal weight, underweight and overweight.
Pattern of Weight Gain
The optimal rate of weight gain depends on the stage of pregnancy. During the first and second trimesters, growth takes place primarily in maternal tissues, and during the third trimester, growth occurs primarily in fetal tissues. During the first trimester of singleton pregnancy, the average total weight gain is only 1 to 2 kg. Thereafter the recommended weight gain increases to approximately 0.5 kg per week for an underweight woman and 0.4 kg per week for a woman of normal weight (see Fig. 14-2). The recommended weekly weight gain for overweight women during the second and third trimesters is 0.3 kg, and for obese women, 0.2 kg.
The recommended energy (kcal) intake corresponds to the recommended pattern of gain (see Table 14-1). There is no increment for the first trimester; an additional 340 and 452 kcal per day over the prepregnant intake is recommended during the second and third trimesters, respectively. These recommendations are most appropriate for singleton pregnancy and may need to be adjusted in multiple gestation. The amount of food providing the needed increase in energy intake is not large. The 340 additional kcal needed during the second trimester can be provided by one additional serving from each of the following groups: milk, yogurt, or cheese (all skim milk products); fruits; vegetables; and bread, cereal, rice, or pasta.
The reasons for an inadequate weight gain (less than 1 kg per month for normal-weight women or less than 0.5 kg per month for obese women during the last two trimesters) or excessive weight gain (more than 3 kg per month) should be thoroughly evaluated. Possible reasons for deviations from the expected rate of weight gain, besides inadequate or excessive dietary intake, include measurement or recording errors and differences in the weight of clothing or the time of day. An exceptionally high gain is likely to result from the accumulation of fluids, and a gain of more than 3 kg in a month, especially after the twentieth week of gestation, often indicates the development of preeclampsia.
Hazards of Restricting Adequate Weight Gain
An obsession with thinness and dieting pervades the North American culture. Figure-conscious women may find it difficult to make the transition from guarding against weight gain before pregnancy to valuing weight gain during pregnancy. In counseling these women the nurse can emphasize the positive effects of good nutrition as well as the adverse effects of maternal malnutrition (manifested by poor weight gain) on infant growth and development. This counseling includes information on the components of weight gain during pregnancy (Table 14-2) and the amount of this weight that will be lost after the birth. Because lactation can help to reduce maternal energy stores gradually, this also provides an opportunity to promote breastfeeding.
TABLE 14-2
TISSUES CONTRIBUTING TO MATERNAL WEIGHT GAIN AT 40 WEEKS OF GESTATION
| TISSUE | KILOGRAMS | POUNDS |
| Fetus | 3.2-3.9 | 7-8.5 |
| Placenta | 0.9-1.1 | 2-2.5 |
| Amniotic fluid | 0.9 | 2 |
| Increase in uterine tissue | 0.9 | 2 |
| Breast tissue | 0.5-1.8 | 1-4 |
| Increased blood volume | 1.8-2.3 | 4-5 |
| Increased tissue fluid | 1.4-2.3 | 3-5 |
| Increased stores (fat) | 1.8-2.7 | 4-6 |
In the United States 20% of women who give birth are obese (Paul, 2008). Pregnancy is not a time for a weight reduction
diet. Even overweight or obese pregnant women need to gain at least enough weight to equal the weight of the products of conception (fetus, placenta, and amniotic fluid). If they limit their energy intake to prevent weight gain, they also may excessively limit their intake of important nutrients. Moreover, dietary restriction results in the catabolism of fat stores, which in turn augments the production of ketones. The long-term effects of mild ketonemia during pregnancy are not known, but ketonuria is associated with the occurrence of preterm labor. It should be stressed to obese women, and all pregnant women for that matter, that the quality of the weight gain is important, with emphasis placed on the consumption of nutrient-dense foods and the avoidance of empty-calorie foods.
Excessive Weight Gain
Weight gain is important, but pregnancy is not an excuse for uncontrolled dietary indulgence. The old saying that the pregnant woman is “eating for two” should not be interpreted to mean that the food intake should be doubled. Instead the woman should place an emphasis on the quality of her food intake as she considers her needs and those of her fetus. Excessive weight gained during pregnancy may be difficult to lose after pregnancy, thus contributing to chronic overweight or obesity, an etiologic factor in a host of chronic diseases, including hypertension, diabetes mellitus, and arteriosclerotic heart disease. The woman who gains 18 kg or more is especially at risk (Box 14-3). Food energy intake and particularly intake of fat is likely to be high among pregnant women, especially low-income women.
Protein
Protein, with its essential constituent nitrogen, is the nutritional element basic to growth. An adequate protein intake is essential to meet increasing demands in pregnancy. These demands arise from the rapid growth of the fetus; enlargement of the uterus and its supporting structures, the mammary glands, and the placenta; increase in the maternal circulating blood volume and the subsequent demand for increased amounts of plasma protein to maintain colloidal osmotic pressure; and formation of amniotic fluid.
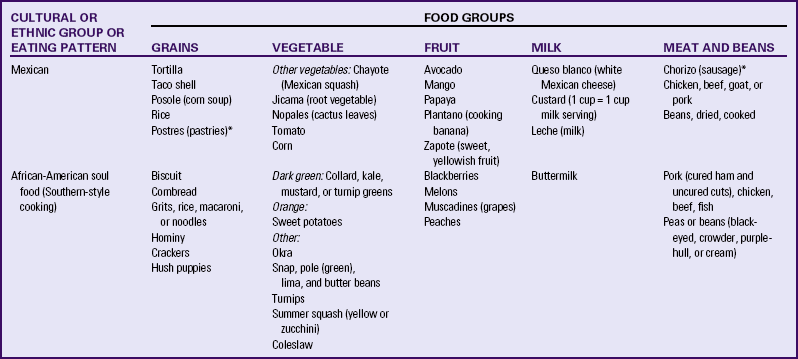
Milk, meat, eggs, and cheese are complete protein foods with a high biologic value. Legumes (dried beans and peas), whole grains, and nuts also are valuable sources of protein. In addition, these protein-rich foods are a source of other nutrients such as calcium, iron, and B vitamins; plant sources of protein often provide needed dietary fiber. The recommended daily food plan (Table 14-3) is a guide to the amounts of these foods that would supply the quantities of protein needed. The recommendations provide for only a modest increase in protein intake (25 g daily) over the prepregnant levels in adult women. Protein intake in many people in the United States is relatively high, and thus many women may not need to increase their protein intake at all during pregnancy. Three servings of milk, yogurt, or cheese (four for adolescents) and two servings (5 to 6 oz [140 to 168 g]) of meat, poultry, or fish would supply most of the recommended protein for a pregnant woman. Additional protein would be provided by vegetables and breads, cereals, rice, or pasta. Pregnant adolescents, women from impoverished backgrounds, and women adhering to unusual diets, such as a macrobiotic (highly restricted vegetarian) diet, are those whose protein intake is most likely to be inadequate. High-protein supplements are not recommended because they have been associated with an increased incidence of preterm births.
TABLE 14-3
DAILY FOOD GUIDE FOR PREGNANCY AND LACTATION
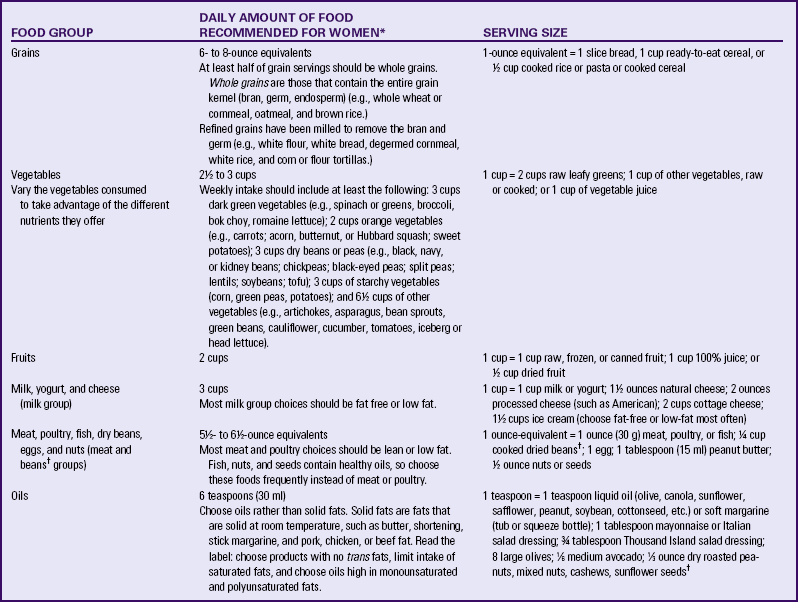
∗These are approximate amounts, based on a relatively sedentary lifestyle, and should be individualized. Intake may have to be increased for women with a more active lifestyle or multiple gestation, those who are underweight before pregnancy, or those exhibiting poor gestational weight gain. Needs during lactation may also be greater than these recommendations.
†Beans are also part of the vegetable group; avocados are also part of the fruit group, and nuts and seeds are part of the meat and beans group.
Pregnant and nursing women should be especially careful when choosing fish to select those that are low in mercury.
Fluids
Essential during the exchange of nutrients and waste products across cell membranes, water is the main substance of cells, blood, lymph, amniotic fluid, and other vital body fluids. It also aids in maintaining body temperature. A good fluid intake promotes regular bowel function, which is sometimes a problem during pregnancy. The recommended daily intake is about 8 to 10 glasses (2.3 L) of fluid. Water, milk, and decaffeinated tea are good sources. Foods in the diet should supply an additional 700 mL or more of fluid. Dehydration may increase the risk of cramping, contractions, and preterm labor.
The safety of caffeine use in pregnancy is an important issue. Some investigators (e.g., Weng, Odouli, & Li, 2008) but not others (e.g., Pollack, Louis, Sundaram, & Lum, 2010) have found that women who consume more than 200 mg of caffeine daily (equivalent to about 12 oz of coffee) may be at increased risk of miscarriage. There are also data suggesting that excess caffeine intake may contribute to IUGR. A recent review found that there is insufficient evidence to determine whether caffeine has any effect on pregnancy outcome (Jahanfar & Sharifah, 2009). Although the evidence about caffeine is far from conclusive, the March of Dimes recommends a daily intake of no more than 200 mg of caffeine (March of Dimes, 2008). Caffeine is found not only in coffee but also in tea, some soft drinks, and chocolate (Table 14-4).
TABLE 14-4
CAFFEINE CONTENT OF COMMON BEVERAGES AND FOODS
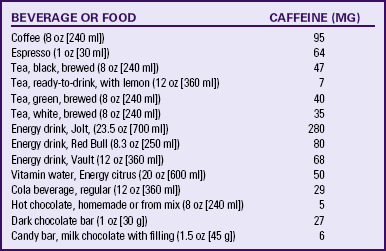
Source: U.S. Department of Agriculture, Agricultural Research Service. (2009). USDA National Nutrient Database for Standard Reference, Release 22. Nutrient Data Laboratory Home Page. Available at www.ars.usda.gov/ba/bhnrc/ndl. Accessed August 18, 2010; Chin, J., Merves, M., Goldberger, B., Sampson-Cone, A., & Cone, E. (2008). Caffeine content of brewed teas. Journal of Analytical Toxicology, 32(8), 702-704; Reissig, C., Strain, E., & Griffiths, R. (2009). Caffeinated energy drinks—A growing problem. Drug and Alcohol Dependence, 99(1-3), 1-10.
Aspartame (NutraSweet, Equal), acesulfame potassium (Sunett), and sucralose (Splenda), artificial sweeteners commonly used in low- or no-calorie beverages and low-calorie food products, have not been found to have adverse effects on the normal mother and fetus and are therefore approved by the U.S. Food and Drug Administration (FDA) for use during pregnancy. Aspartame, which contains phenylalanine, should be avoided by the pregnant woman with PKU, however (Box 14-4). Stevia (stevioside) is a sweetener sold as a dietary supplement; no acceptable daily intake has been established for stevia.
Minerals and Vitamins
In general, the nutrient needs of pregnant women, with perhaps the exception of folate and iron, can be met through dietary sources. Counseling about the need for a varied diet rich in vitamins and minerals should be a part of the early prenatal care of every pregnant woman and should be reinforced throughout pregnancy. However, it has been suggested that taking a micronutrient supplement (including vitamins and trace minerals) before and during pregnancy reduces the risk of congenital defects, LBW, and preterm birth, as well as preeclampsia (Scholl, 2008). There is no conclusive evidence to support this suggestion, but further research is needed on maternal and fetal benefits of micronutrient supplementation (Peña-Rosas & Viteri, 2009). Supplements are especially advisable for women with known nutritional risk factors (Box 14-5). It is important that the pregnant woman understand that the use of a vitamin-mineral supplement does not lessen the need to consume a nutritious, well-balanced diet.
Iron
Iron is needed to allow transfer of adequate iron to the fetus and to permit expansion of the maternal RBC mass. During pregnancy, plasma volume increases more than RBC mass, with the difference between plasma and RBCs being greatest during the second trimester. The relative excess of plasma causes a modest decrease in the hemoglobin concentration and hematocrit, known as physiologic anemia of pregnancy. This is a normal adaptation during pregnancy.
However, poor iron status, which can result in iron deficiency anemia, is relatively common among women in the childbearing years. Iron deficiency (not necessarily anemia) is estimated to affect approximately 10% of nonpregnant women in the childbearing years in the United States. Anemic women are poorly prepared to tolerate hemorrhage at the time of birth. In addition, women who have iron deficiency anemia during early pregnancy are at increased risk of preterm birth. Iron deficiency during the third trimester apparently does not carry the same risk. In the United States, anemia is most common among adolescents, African-American women, and women of lower socioeconomic status.
A supplement of 30 mg of ferrous iron daily, starting by 12 weeks of gestation, helps ensure an adequate iron intake. Iron supplements may be poorly tolerated during the nausea prevalent in the first trimester, and starting the supplement after this point may improve tolerance. If maternal iron deficiency anemia is present (preferably diagnosed by measurement of serum ferritin, a storage form of iron), increased iron dosages (60 to 120 mg daily) may be required. See the Teaching for Self-Management box regarding iron supplementation. Even when a woman is taking an iron supplement, however, she also should include good food sources of iron in her daily diet (see Table 14-1).
Calcium
There is no increase in the DRI of calcium during pregnancy and lactation, in comparison to the recommendation for the nonpregnant woman (see Table 14-1). The DRI (1000 mg daily for women 19 years and older and 1300 mg for those younger than 19 years) appears to provide sufficient calcium for fetal bone and tooth development to proceed while maintaining maternal bone mass. Milk and yogurt are especially rich
sources of calcium, providing approximately 300 mg per cup (240 m1). Nevertheless, many women do not consume these foods or do not consume adequate amounts to provide the recommended intakes of calcium. One problem that can interfere with milk consumption is lactose intolerance, the inability to digest milk sugar (lactose) because of the lack of the enzyme lactase in the small intestine. It is relatively common in adults, particularly African-Americans, Asians, Native Americans, and Inuits (Alaska Natives). Milk consumption may cause abdominal cramping, bloating, and diarrhea in such people, although many lactose-intolerant individuals can tolerate small amounts of milk without symptoms. Yogurt, sweet acidophilus milk, buttermilk, cheese, chocolate milk, and cocoa may be tolerated even when fresh fluid milk is not. Commercial lactase supplements (e.g., Lactaid) are widely available to consume with milk, and many supermarkets stock lactase-treated milk. The lactase in these products hydrolyzes, or digests, the lactose in the milk, making it possible for lactose-intolerant people to drink milk.
In some cultures it is uncommon for adults to drink milk. For example, Puerto Rican and other Hispanic people may use it only as an additive in coffee. Pregnant women from these cultures may need to consume nondairy sources of calcium (Box 14-6). If calcium intake appears low and the woman does not change her diet habits despite counseling, a supplement containing 600 mg of elemental calcium may be needed daily. Calcium supplements also may be recommended when a pregnant woman has leg cramps that are caused by an imbalance in the calcium-phosphorus ratio. Bone meal is not recommended as a calcium supplement because it may contain lead.
Other Minerals and Electrolytes
Magnesium: Diets of women in the childbearing years are likely to be low in magnesium, and as many as half of pregnant and lactating women may have inadequate intakes (IOM, 2006). Adolescents and low-income women are especially at risk. Dairy products, nuts, whole grains, and green leafy vegetables are good sources of magnesium.
Sodium: During pregnancy the need for sodium increases slightly, primarily because the body water is expanding (e.g., the expanding blood volume). Sodium is essential for maintaining body water balance. In the past, dietary sodium was routinely restricted in an effort to control the peripheral edema that commonly occurs during pregnancy. It is now recognized, however, that moderate peripheral edema is normal in pregnancy, occurring as a response to the fluid-retaining effects of elevated levels of estrogen. Sodium is not routinely restricted in pregnancy, and restriction has not proved effective in reducing the rates of preeclampsia. Severe sodium restriction also may make it difficult for pregnant women to achieve an adequate diet. Grain, milk, and meat products, which are good sources of the nutrients needed during pregnancy, are significant sources of sodium. Additionally, sodium restriction may stress the adrenal glands and kidneys as they attempt to retain adequate sodium. In general, sodium restriction is necessary only if the woman has a medical condition such as renal or liver failure or hypertension that warrants such a restriction.
On the other hand, excessive sodium intake is unwarranted because it may contribute to development of hypertension in salt-sensitive individuals. An adequate sodium intake for pregnant and lactating women, as well as nonpregnant women in the childbearing years, is estimated to be 1.5 g/day, with a recommended upper limit of intake of 2.3 g/day (Otten et al., 2006). Table salt (sodium chloride) is the richest source of sodium, with approximately 2.3 g sodium contained in 1 teaspoon (6 g) of salt. Most canned foods contain added salt, unless the label states otherwise. Large amounts of sodium also are found in many processed foods, including meats (e.g., smoked or cured meats, cold cuts, and corned beef), frozen entrees and meals, baked goods, mixes for casseroles or grain products, soups, and condiments. Products low in nutritive value and excessively high in sodium include pretzels, potato and other chips (except salt-free), pickles, catsup, prepared mustard, steak and Worcestershire sauces, some soft drinks, and bouillon. A moderate sodium intake can usually be achieved by salting food lightly during cooking, adding no additional salt at the table, and avoiding low-nutrient, high-sodium foods.
Potassium: Diets including adequate intakes of potassium are associated with reduced risk of hypertension. Potassium has been identified as one of the nutrients most likely to be lacking in the diets of women of childbearing age (IOM, 2006). A diet including 8 to 10 servings of unprocessed fruits and vegetables daily, along with moderate amounts of low-fat meats and dairy products, has been effective in reducing sodium intake while providing adequate amounts of potassium.
Zinc: Zinc is a constituent of numerous enzymes involved in major metabolic pathways. Zinc deficiency is associated with malformations of the central nervous system in infants. When large amounts of iron and folic acid are consumed, the absorption of zinc is inhibited, and the serum zinc levels are reduced as a result. Because iron and folic acid supplements are commonly prescribed during pregnancy, pregnant women should be encouraged to consume good sources of zinc daily (see Table 14-1). Women with anemia who receive high-dose iron supplements also need supplements of zinc and copper.
Fluoride: There is no evidence that prenatal fluoride supplementation reduces the child’s likelihood of tooth decay during the preschool years. No increase in fluoride intake over the nonpregnant DRI is currently recommended during pregnancy (Otten et al., 2006).
Fat-Soluble Vitamins
The fat-soluble vitamins include vitamins A, D, E, and K. These are of special concern during pregnancy because vitamin E intake is among the nutrients most likely to be lacking in the diets of women of childbearing age, and intake of vitamins A and D is also low in the diets of some women (IOM, 2006). Fat-soluble vitamins are stored in the body tissues; in the event of prolonged overdoses, these vitamins can reach toxic levels. Because of the high potential for toxicity, pregnant women are advised to take fat-soluble vitamin supplements only as prescribed. Toxicity from dietary sources is very unlikely, however.
Vitamin E is needed for protection against oxidative stress, and pregnancy is associated with increased oxidative stress. Indeed, oxidative stress has been proposed as an explanation for the etiology of preeclampsia, although supplementation with vitamin E has not been effective in reducing rates of preeclampsia (Villar, Purwar, Merialdi, Zavaleta, Thi Nhu Ngoc, Anthony, et al., 2009). Vegetable oils and nuts are especially good sources of vitamin E, and whole grains and leafy green vegetables are moderate sources.
Adequate intake of vitamin A is needed so that sufficient amounts of the vitamin can be stored in the fetus; however, a well-chosen diet including adequate amounts of deep yellow and deep green vegetables and fruits such as leafy greens, broccoli, carrots, cantaloupe, and apricots provides sufficient amounts of carotenes that can be converted in the body to vitamin A. Congenital malformations have occurred in infants of mothers who took excessive amounts of preformed vitamin A (from supplements) during pregnancy, and thus supplements are not recommended routinely for pregnant women.
Vitamin A analogs (e.g., isotretinoin [Accutane]), which are prescribed for the treatment of cystic acne, when used during early pregnancy have been associated with an increased incidence of congenital defects, as well as an increased risk of miscarriage. Topical agents such as tretinoin (Retin-A) do not appear to enter the circulation in substantial amounts, but their safety in pregnancy has not been confirmed.
Vitamin D plays an important role in the absorption and metabolism of calcium. The main food sources of this vitamin are enriched or fortified foods such as milk and ready-to-eat cereals. Vitamin D also is produced in the skin by the action of ultraviolet light (in sunlight). A severe deficiency may lead to neonatal hypocalcemia and tetany, as well as to hypoplasia of the tooth enamel. Women with lactose intolerance and those who do not include milk in their diet for any reason are at risk for vitamin D deficiency. Other risk factors for deficiency are dark skin, with African-American women being at high risk of deficiency; habitual use of clothing that covers most of the skin (e.g., Muslim women with extensive body covering); and living in northern latitudes where sunlight exposure is limited, especially during the winter. Use of recommended amounts of sunscreen with a sun protection factor (SPF) rating of 15 or greater reduces skin vitamin D production by as much as 99%, thus bringing about a need for regular intake of fortified foods or a supplement.
Water-Soluble Vitamins
Body stores of water-soluble vitamins are much smaller than those of fat-soluble vitamins, and the water-soluble vitamins, in contrast to the fat-soluble ones, are readily excreted in the urine. Therefore, good sources of these vitamins must be consumed frequently, and toxicity with overdose is less likely than it is in people taking fat-soluble vitamins.
Folate/Folic Acid: Because of the increase in RBC production during pregnancy, as well as the nutritional requirements of the rapidly growing cells in the fetus and placenta, pregnant women should consume about 50% more folate than nonpregnant women, or about 0.6 mg (600 mcg) daily. In the United States, all enriched grain products (which include most white breads, flour, and pasta) must contain folic acid at a level of 1.4 mg/kg flour. This level of fortification is designed to supply approximately 0.1 mg folic acid daily in the average American diet and has significantly increased folic acid consumption in the population as a whole. All women of childbearing potential need careful counseling about including good sources of folate in their diets (see Box 14-1). Supplemental folic acid is usually prescribed to ensure that intake is adequate. Women who have borne a child with a neural tube defect are advised to consume 4 mg of folic acid daily, and a supplement is required for them to achieve this level of intake.
Pyridoxine: Pyridoxine, or vitamin B6, is involved in protein metabolism. Although levels of a pyridoxine-containing enzyme have been reported to be low in women with preeclampsia, there is no evidence that supplementation prevents or eradicates the condition. Pyridoxine has been effective in reducing the nausea and vomiting of early pregnancy in some trials (Festin, 2007).
Vitamin C: Vitamin C, or ascorbic acid, plays an important role in tissue formation and enhances the absorption of iron. The vitamin C needs of most women are readily met by a diet that includes at least one or two daily servings of citrus fruit or juice or another good source of the vitamin (see Table 14-1), but women who smoke need more.
Other Nutritional Issues During Pregnancy
Pica, which is the practice of consuming nonfood substances (e.g., clay, soil, and laundry starch) or excessive amounts of foodstuffs low in nutritional value (e.g., ice or freezer frost, baking powder or soda, and cornstarch), often is influenced by the woman’s cultural background (Fig. 14-3). In the United States it appears to be most common among African-American and Hispanic women, women from rural areas, and women with a family history of pica. In some U.S. studies pica has been reported in almost 40% of pregnant women, although it appears less common in homogeneous societies such as Denmark (Mikkelsen, Andersen, & Olsen, 2006). One problem with pica is that regular and heavy consumption of low-nutrient products may cause more nutritious foods to be displaced from the diet. As an example, cornstarch ingestion is popular among African-American women. It is a source of “empty” calories; half a cup (64 g) provides 240 kcal (57 kJ) but almost no vitamins, minerals, or protein. Overuse of cornstarch can contribute to development of gestational diabetes. In addition, the pica items consumed may interfere with the absorption of nutrients, especially minerals (Stokes, 2006). Women who practice pica have been found to have lower hemoglobin levels than do those who do not practice pica.

FIG. 14-3 Nonfood substances consumed in pica: red clay from Georgia, Nzu from East Nigeria, baking powder, cornstarch, baking soda, laundry starch, and ice. Some individuals practice poly-pica, consuming more than one of these or other nonfood substances. (Courtesy Shannon Perry, Phoenix, AZ.)
Moreover, there is a risk that nonfood items will be contaminated with heavy metals or other toxic substances. Among Mexican-American women, consumption of tierra includes both soil and pulverized Mexican pottery. Lead contamination of soils and soil-based products has caused high levels of lead in pregnant women and their newborns (Mills, 2007). Regular household use of Mexican pottery in cooking or serving food or ingestion of ground pottery must be included in interviews or questionnaires regarding nutritional intake of pregnant women. The possibility of pica must be considered when pregnant women are found to be anemic, and the nurse should provide counseling about the health risks associated with pica.
The existence of pica, as well as details of the types and amounts of products ingested, is likely to be discovered only by the sensitive interviewer who has developed a relationship of trust with the woman. It has been proposed that pica and food cravings (i.e., the urge to have ice cream, pickles, or pizza, for example) during pregnancy are caused by an innate drive to consume nutrients missing from the diet. However, research has not supported this hypothesis.
Adolescent Pregnancy Needs
Many adolescent females have diets that provide less than the recommended intakes of key nutrients, including calcium and iron. Pregnant adolescents and their infants are at increased risk of complications during pregnancy and parturition. Growth of the pelvis is delayed in comparison to growth in stature, and this helps to explain why cephalopelvic disproportion and other mechanical problems associated with labor are common among young adolescents. Competition between the growing adolescent and the fetus for nutrients also may contribute to some of the poor outcomes apparent in teen pregnancies. Recommended weight gain goals are not different from those of adult women. BMI is calculated as for adult women (IOM, 2009), rather than by using the adolescent BMI growth charts available from the Centers for Disease Control and Prevention (www.cdc.gov). Adolescent females that have given birth have greater percentages of total fat and visceral fat (associated with the metabolic syndrome and cardiovascular disease) than those that have never given birth (Gunderson, Striegel-Moore, Schreiber, Hudes, Biro, Daniels, et al., 2009); thus the adolescent mother needs careful teaching regarding nutritional intake and physical activity to control body weight in the postpartum period.
Efforts to improve the nutritional health of pregnant adolescents focus on improving the nutrition knowledge, meal planning, and food preparation and selection skills of young women; promoting access to prenatal care; developing nutrition interventions and educational programs that are effective with adolescents; and striving to understand the factors that create barriers to change in the adolescent population.
Preeclampsia
There has been speculation that the poor intake of various nutrients might contribute to development of preeclampsia, but there is no definitive evidence. At present, a diet adequate in the recommended nutrients (see Table 14-1), along with use of a supplement that provides micronutrients both before and during pregnancy, appears to be the best means of reducing the risk of preeclampsia (Scholl, 2008).
Physical Activity During Pregnancy
Moderate exercise during pregnancy yields numerous benefits, including improving muscle tone, potentially shortening the course of labor, and promoting a sense of well-being. Two nutritional concepts are especially important for women who choose to exercise during pregnancy. First, a liberal amount of fluid should be consumed before, during, and after exercise, because dehydration can trigger premature labor. Second, the calorie intake should be sufficient to meet the increased needs of pregnancy and the demands of exercise.
Nutrient Needs During Lactation
Nutritional needs during lactation are similar in many ways to those during pregnancy. Needs for energy (calories), protein, calcium, iodine, zinc, the B vitamins (thiamine, riboflavin, niacin, pyridoxine, and vitamin B12), and vitamin C remain greater than nonpregnant needs. The recommendations for some of these (e.g., vitamin C, zinc, and protein) are slightly to moderately higher than those during pregnancy (see Table 14-1). This allowance covers the amount of the nutrient released in the milk, as well as needs of the mother for tissue maintenance. In the case of iron and folic acid, the recommendation during lactation is lower than that during pregnancy. Both of these nutrients are essential for RBC formation and thus for maintaining the increase in the blood volume that occurs during pregnancy. With the decrease in maternal blood volume to nonpregnant levels after birth, maternal iron and folic acid needs also decrease. Many lactating women have a delay in the return of menses, which also conserves blood cells and reduces iron and folic acid needs. It is especially important that the calcium intake be adequate; if it is not, a supplement of 600 mg of calcium per day may be needed.
The recommended energy intake is an increase of 330 kcal per day for the first 6 months above the woman’s nonpregnant daily requirement. It becomes difficult to obtain adequate nutrients for the maintenance of lactation if total intake is less than 1800 kcal. Because of the deposition of energy stores, the woman who has gained the optimal amount of weight during pregnancy is heavier after birth than at the beginning of pregnancy. As a result of the caloric demands of lactation, however, the lactating mother usually has a gradual but steady weight loss. Most women rapidly lose several kilograms during the first month after birth, whether they breastfeed or not. After the first month the average loss during lactation is 0.5 to 1 kg per month, and a woman who is overweight may be able to lose up to 2 kg without decreasing her milk supply.
Fluid intake also must be adequate to maintain milk production, but the mother’s level of thirst is the best guide to the right amount. There is no need to consume more fluids than those needed to satisfy thirst.
Smoking, alcohol consumption, and excessive caffeine intake should be avoided during lactation. Smoking not only may impair milk production but also exposes the infant to the risk of passive smoking. It is speculated that the infant’s psychomotor development may be affected by maternal alcohol use, and alcohol use may impair the milk-ejection reflex (Mennella & Pepino, 2008). Caffeine intake can lead to a reduced iron concentration in milk and consequently contribute to the development of anemia in the infant. The caffeine concentration in milk is only approximately 1% of the mother’s plasma level, but caffeine levels build up in the infant. Breastfed infants of mothers who drink large amounts of coffee or caffeine-containing soft drinks may be unusually active and wakeful.
Care Management
During pregnancy nutrition plays a key role in achieving an optimal outcome for the mother and her unborn baby. The motivation to learn about nutrition is usually greater during pregnancy because parents strive to “do what’s right for the baby.” Optimal nutrition cannot eliminate all the problems that may arise during pregnancy, but it does establish a good foundation for supporting the needs of the mother and her unborn baby (see the Nursing Process box).
Diet History
Assessment is based on a diet history (a description of the woman’s usual food and beverage intake and factors affecting her nutritional status, such as medications being taken and the adequacy of income to allow her to purchase the necessary foods) obtained from an interview and review of the woman’s health records, physical examination, and laboratory results. Ideally a nutritional assessment is performed before conception so that any recommended changes in diet, lifestyle, and weight can be accomplished before the woman becomes pregnant.
Obstetric and Gynecologic Effects on Nutrition
Nutritional reserves may be depleted in the multiparous woman or in the one who has had frequent pregnancies (especially three pregnancies within 2 years). A history of preterm birth or birth of an LBW or small-for-gestational-age (SGA) infant may indicate inadequate dietary intake. Birth of a large-for-gestational-age (LGA) infant often indicates the existence of maternal diabetes mellitus. Previous contraceptive methods also may affect reproductive health. Increased menstrual blood loss often occurs during the first 3 to 6 months after placement of an intrauterine contraceptive device; consequently the user may have low iron stores or even iron deficiency anemia. Oral contraceptive agents conversely are associated with decreased menstrual losses and increased iron stores; however, oral contraceptives may interfere with folic acid metabolism. The woman with polycystic ovary syndrome (PCOS) is likely to be
obese and insulin resistant and is prone to development of gestational diabetes (Racho & Teede, 2010).
& Teede, 2010).
Health History
Chronic maternal illnesses such as diabetes mellitus, renal disease, liver disease, cystic fibrosis or other malabsorptive disorders, seizure disorders and the use of anticonvulsant agents, hypertension, and PKU may affect a woman’s nutritional status and dietary needs. In women with illnesses that have resulted in nutritional deficits or that require dietary treatment (e.g., diabetes mellitus or PKU), it is extremely important for nutritional care to be started and for the condition to be optimally controlled before conception. The registered dietitian can provide in-depth counseling for the woman who requires medical nutrition therapy during pregnancy and lactation.
Usual Maternal Diet
The woman’s usual food and beverage intake, the adequacy of her income and other resources to meet her nutritional needs, any dietary modifications, food allergies and intolerances, and all medications and nutrition supplements being taken, as well as pica practice and cultural dietary requirements, should be ascertained. In addition, the presence and severity of nutrition-related discomforts of pregnancy such as morning sickness, constipation, and pyrosis (heartburn) should be determined. The nurse should be alert to any evidence of eating disorders such as anorexia nervosa, bulimia, and frequent and rigorous dieting before or during pregnancy.
The effect of food allergies and intolerances on nutritional status ranges from very important to almost nil. Lactose intolerance is of special concern in pregnant and lactating women because no other food group equals milk and milk products in terms of calcium content. If a woman has lactose intolerance, the interviewer should explore her intake of other calcium sources (see Box 14-6).
The assessment must include an evaluation of the woman’s financial resources and her knowledge of sound dietary practices. The quality of the diet improves with increasing socioeconomic status and educational level. Poor women may not have access to adequate refrigeration and cooking facilities and may find it difficult to obtain adequate nutritious food. Food-borne illnesses may cause adverse effects in pregnancy, and the woman’s understanding of safe food handling practices (cleansing hands, food preparation surfaces, and utensils frequently; avoiding contact between raw meat, fish, or poultry and other foods that will not be cooked before consumption; storing foods properly; and cooking foods to a safe temperature) should be assessed.
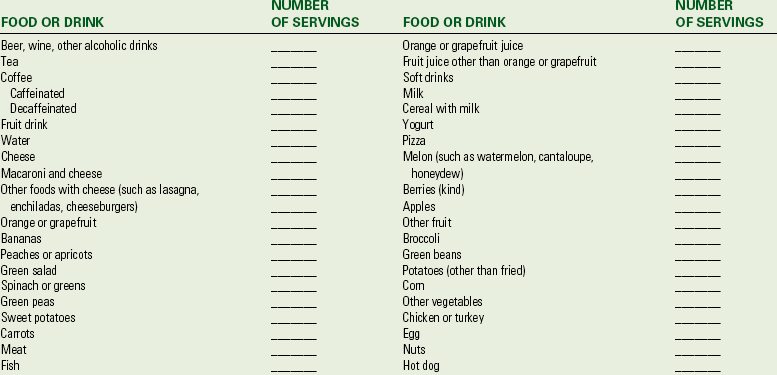
Box 14-7 provides a simple tool for obtaining diet history information. When potential problems are identified, they should be followed up with a careful interview.
Physical Examination
Anthropometric measurements provide short- and long-term information on a woman’s nutritional status and are thus essential to the assessment. At a minimum, the woman’s height and weight must be determined at the time of her first prenatal visit, and her weight should be measured at every subsequent visit (see earlier discussion of BMI).
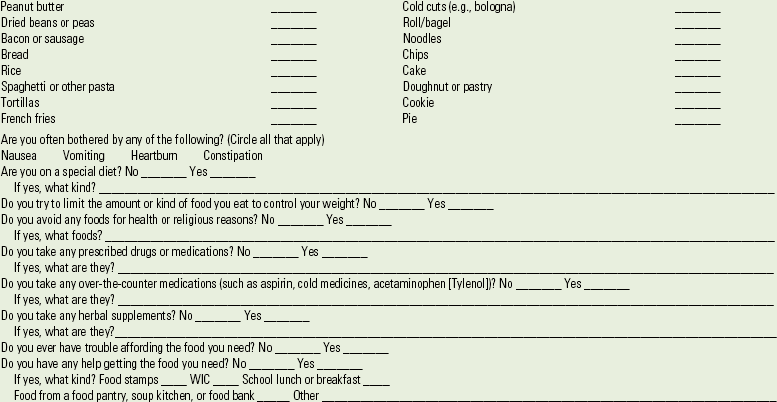
A careful physical examination can reveal objective signs of malnutrition (Table 14-5). It is important to note, however, that some of these signs are nonspecific, and the physiologic changes of pregnancy may complicate the interpretation of physical findings. For example, lower-extremity edema often occurs when caloric and protein deficiencies are present, but it also may be a normal finding in the third trimester. The interpretation of physical findings is made easier by a thorough health history and by laboratory testing, if indicated.
Laboratory Testing
The only nutrition-related laboratory test necessary for most pregnant women is a hematocrit or hemoglobin measurement to screen for the presence of anemia. Because of the physiologic anemia of pregnancy, the reference values for hemoglobin and hematocrit must be adjusted during pregnancy. The lower limit of the normal range for hemoglobin during pregnancy is 11 g/dl in the first and third trimesters and 10.5 g/dl in the second trimester (compared with 12 g/dl in the nonpregnant state). The lower limit of the normal range for hematocrit is 33% during the first and third trimesters and 32% in the second trimester (compared with 36% in the nonpregnant state) (Cunningham, Leveno, Bloom, Hauth, Rouse, & Spong, 2010; Pagana, & Pagana, 2009). Cutoff values for anemia are higher in women who smoke or live at high altitudes, because the decreased oxygen-carrying capacity of their RBCs causes them to produce more RBCs than other women.
A woman’s history or physical findings may indicate the need for additional testing, such as a complete blood cell count with a differential to identify megaloblastic or macrocytic anemia and the measurement of levels of specific vitamins or minerals believed to be lacking in the diet.
Client Education
For many women with uncomplicated pregnancies, the nurse can serve as the primary source of nutrition education. The registered dietitian, who has specialized training in diet evaluation and planning, nutritional needs during illness, and ethnic and cultural food patterns, as well as in translating nutrient needs into food patterns, frequently serves as a consultant. Pregnant women with serious nutritional problems, those with intervening illnesses such as diabetes (either preexisting or gestational), and any others requiring in-depth nutrition counseling should be referred to the dietitian. The nurse, dietitian, physician, and nurse-midwife collaborate in helping the woman achieve nutrition-related expected outcomes. Nutritional care and teaching generally involve (1) acquainting the woman with the nutritional needs during pregnancy and the characteristics of an adequate diet, if necessary; (2) helping her to individualize her diet so that she achieves an adequate intake while conforming to her personal, cultural, financial, and health circumstances; (3) acquainting her with strategies for coping with the nutrition-related discomforts of pregnancy; (4) helping her use nutrition supplements appropriately; and (5) consulting with and making referrals to other professionals or services as indicated. Two programs that provide nutrition services are the food stamp program and the Special Supplemental Program for Women, Infants, and Children (WIC), which provides vouchers for selected foods to pregnant and lactating women, as well as infants and children at nutritional risk (see the Nursing Care Plan).
Adequate Dietary Intake
Nutrition teaching can take place in a one-on-one interview or in a group setting. In either case, teaching should emphasize the importance of choosing a varied diet composed of readily available foods (rather than specialized diet supplements). Good nutrition practices (and the avoidance of poor practices such as smoking and alcohol or drug use) are essential content for prenatal classes designed for women in early pregnancy.
MyPyramid (www.mypyramid.gov) can be used as a guide to making daily food choices during pregnancy and lactation, just
as it is during other stages of the life cycle. Additional individualized information and resources for professionals are available from the website. The importance of consuming adequate amounts from the milk, yogurt, and cheese group must be emphasized, especially for adolescents and women younger than 25 years who are still actively adding calcium to their skeletons; adolescents need at least three to four servings from the milk group daily.
Pregnancy: The pregnant woman must understand what an adequate weight gain during pregnancy means, recognize the reasons for its importance, and be able to evaluate her own gain in terms of the desirable pattern. Many women, particularly those who have worked hard to control their weight before pregnancy, may find it difficult to understand the reason the weight gain goal is so high when a newborn is so small. The nurse can explain that the maternal weight gain consists of increments in the weight of many tissues, not just the growing fetus (see Table 14-2).
Dietary overindulgence, conversely, which may result in excessive fat stores that persist after giving birth, should be discouraged. Nevertheless, it is best not to focus unduly on weight gain, which can result in feelings of stress and guilt in the woman who does not achieve the preferred pattern of gain. Teaching regarding weight gain during pregnancy is summarized in Box 14-2.
Postpartum: An important goal of postpartum nutrition is for the woman to lose the weight gained during pregnancy. Retention of this weight can contribute to overweight/obesity and the development of later health problems including metabolic syndrome, cardiovascular disease, and diabetes.
The need for a varied diet consisting of a representation of foods from all the food groups continues throughout lactation. The lactating woman should be advised to consume at least 1800 kcal daily, and she should receive counseling if her diet appears to be inadequate in any nutrients. Special attention should be given to her zinc, vitamin B6, and folic acid
intake because the recommendations for these remain higher than those for nonpregnant women (see Table 14-1). Sufficient calcium is needed to allow for both milk formation and maintenance of maternal bone mass. It may be difficult for lactating women to consume enough of these nutrients without careful diet planning.
Obese women and normal-weight women who gain more than the recommended amount of weight during pregnancy are less likely to breastfeed than normal-weight women with appropriate weight gain (Viswanathan et al., 2008). Obese women who do choose to breastfeed have a statistically shorter period of lactation than normal-weight women (Viswanathan et al.). The woman who does not breastfeed can lose weight gradually if she consumes a balanced diet that provides slightly less than her daily energy expenditure, although overweight and obese women with excessive weight gain during pregnancy have an increased likelihood of failing to return to their prepregnancy weights (Siega-Riz, Viswanathan, Moos, Deierlein, Mumford, Knach, et al., 2009). A reasonable weight loss goal for nonlactating women is 0.5 to 0.9 kg per week; a loss of 1 kg per month is recommended for most lactating women. Those at risk for obesity and overweight need follow-up to ensure that they know how to make wise food choices, primarily from fruits, vegetables, whole grains, lean meats, and low-fat dairy products. An hour of moderately vigorous physical activity (walking, jogging, swimming, cycling, aerobic dance, etc.) most days of the week will improve the ability of the woman to lose weight gradually and maintain the weight loss.
Daily Food Guide and Menu Planning
The daily food plan (see Table 14-3) can be used as a guide for educating the woman about nutritional needs during pregnancy and lactation. This food plan is general enough to be used by women from a wide variety of cultures, including those who follow a vegetarian diet. One of the more helpful teaching strategies is to help the woman plan daily menus that follow the food plan and are affordable, are realistic in terms of preparation time, and are compatible with personal preferences and cultural practices. Information regarding cultural food patterns is provided later in this chapter.
Medical Nutrition Therapy
During pregnancy and lactation, the food plan for women receiving special medical nutrition therapy may have to be modified. The registered dietitian can instruct these women about their diets and assist them in meal planning. However, the nurse should understand the basic principles of the diet and be able to reinforce the teaching.
The nurse should be especially aware of the dietary modifications necessary for women with diabetes mellitus (gestational or preexisting) because this disease is relatively common and because fetal morbidity and mortality occur more often in pregnancies complicated by hyperglycemia or hypoglycemia. Every effort should be made to maintain blood glucose levels in the normal range throughout pregnancy. The food plan of the woman with diabetes usually includes four to six meals and snacks daily, with the daily carbohydrate intake distributed fairly evenly among the meals and snacks. The complex carbohydrates—fibers and starches—should be well represented in the diet. To maintain strict control of the blood glucose level, the pregnant woman with diabetes usually must monitor her own blood glucose daily (American Diabetes Association, 2006). The nurse must therefore teach the woman how to monitor her own blood glucose level, unless she has already been doing this before pregnancy (see Chapter 29).
Counseling About Iron Supplementation: The nutritional supplement most commonly needed during pregnancy is iron; however, a variety of dietary factors can affect the completeness of absorption of an iron supplement. The Teaching for Self-Management box summarizes important points regarding iron supplementation.
Coping with Nutrition-Related Discomforts of Pregnancy
The most common nutrition-related discomforts of pregnancy are nausea and vomiting or “morning sickness,” constipation, and pyrosis.
Nausea and Vomiting: Nausea and vomiting of pregnancy (NVP) are most common during the first trimester. Most of the time NVP causes only mild to moderate problems nutritionally, although it may be a source of substantial discomfort. Antiemetic medications, vitamin B6, ginger, or P6 acupressure may be effective in reducing the severity of symptoms, although the evidence supporting them is not strong (ACOG, 2004; Holst, Wright, Haavik, & Nordeng, 2009; Ozgoli, Goli, & Simbar, 2009).
The dose of ginger tested is a total of 1 g daily, and there is no evidence that larger doses are safe or more effective than the 1-g dose (Holst et al.).![]() The pregnant woman may find the suggestions in Box 14-8 helpful in alleviating NVP.
The pregnant woman may find the suggestions in Box 14-8 helpful in alleviating NVP.
Hyperemesis gravidarum, or severe and persistent vomiting causing weight loss, dehydration, and electrolyte abnormalities, occurs in up to approximately 1% of pregnant women. (See Chapter 29 for further discussion.)
Constipation: Improved bowel function generally results from increasing the intake of fiber (e.g., bran and whole-grain products, popcorn, and raw or lightly cooked vegetables) in the diet, because fiber helps to create a bulky stool that stimulates intestinal peristalsis. The recommendation for fiber intake in pregnancy is 28 g daily. An adequate fluid intake (at least 50 ml/kg/day) helps to hydrate the fiber and increase the bulk of the stool. Making a habit of participating in physical activity that uses large muscle groups (walking, swimming, water aerobics) also helps to stimulate bowel motility.
Pyrosis: Pyrosis, or heartburn, is usually caused by the reflux of gastric contents into the esophagus. This condition can be minimized by the consumption of small, frequent meals, rather than two or three larger meals daily. Because fluids further distend the stomach they should not be consumed with foods. The woman needs to be sure to drink adequate amounts between meals, however. Avoiding spicy foods may help alleviate the problem. Lying down immediately after eating and wearing clothing that is tight across the abdomen can contribute to the problem of reflux.
Cultural Influences
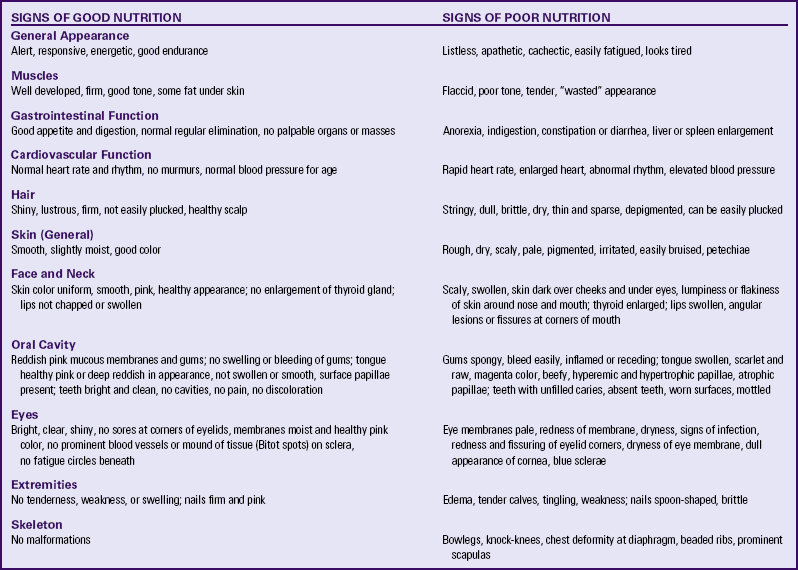
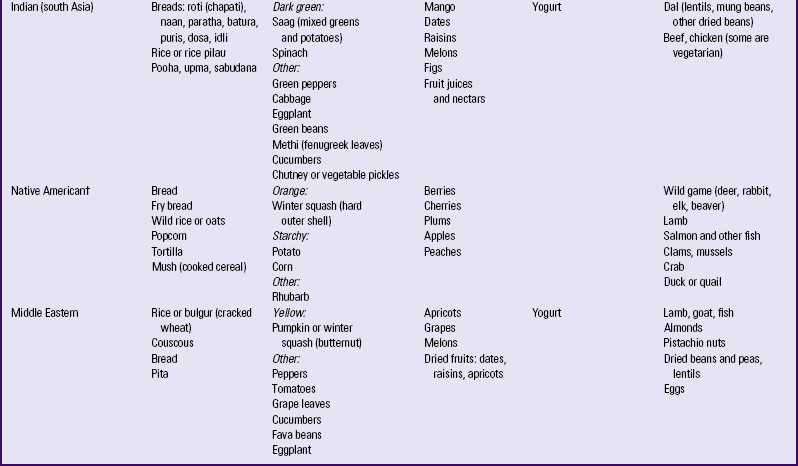
Consideration of a woman’s cultural food preferences enhances communication, providing a greater opportunity for compliance with the agreed-on pattern of intake. Women in most cultures are encouraged to eat a diet typical for them. The nurse needs to be aware of what constitutes a typical diet for different cultural or ethnic groups; however, within one cultural group, several variations may occur. Thus careful exploration of individual preferences is needed. Although ethnic and cultural food beliefs may seem at first glance to conflict with the dietary instruction provided by physicians, nurses, and dietitians, it is often possible for the empathic health care provider to identify cultural beliefs that are congruent with the modern understanding of pregnancy and fetal development. Many cultural food practices have some merit, or the culture would not have survived. Food cravings during pregnancy are considered normal by many cultures, but the kinds of cravings often are culturally specific. In most cultures women crave acceptable foods, such as chicken, fish, and greens among African-Americans. Cultural influences on food intake usually lessen as the woman and her family become more integrated into the dominant culture. Nutritional beliefs and the practices of selected cultural groups are summarized in Table 14-6.
Vegetarian Diets
Vegetarian diets represent another cultural effect on nutritional status. Foods basic to almost all vegetarian diets are vegetables, fruits, legumes, nuts, seeds, and grains, but with many variations. Lacto-vegetarians include milk products. Another type of vegetarian, lacto-ovovegetarians, consumes eggs and dairy products in addition to plant products. Vegans, or total vegetarians consume only plant products. All of these types of vegetarian diets, if they are well planned, can be nutritionally adequate for pregnant and lactating women (Craig & Mangels, 2009). Because vitamin B12 is found only in foods of animal origin, the vegan diet may be low in vitamin B12. As a result, vegans should consume vitamin B12-fortified foods such as fortified soy milk two or three times a day or take a supplement. Vitamin B12 deficiency can result in megaloblastic anemia, glossitis (inflamed red tongue), and neurologic deficits in the mother. Infants born to affected mothers are likely to have megaloblastic anemia and to exhibit neurodevelopmental delays. The diet should be carefully planned to include adequate minerals. Iron and zinc may not be as well absorbed from plant foods as they are from meats, and calcium intake can be low if milk products are avoided. Plant proteins tend to be “incomplete” in that they lack one or more amino acids required for growth and the maintenance of body tissues. However, the daily consumption of a variety of different plant proteins—grains, dried beans and peas, nuts, and seeds—can provide all of the essential amino acids.
KEY POINTS
• A woman’s nutritional status before, during, and after pregnancy contributes, to a significant degree, to her well-being and that of her developing fetus and newborn.
• Many physiologic changes occurring during pregnancy influence the need for additional nutrients and the efficiency with which the body uses them.
• Both the total maternal weight gain and the pattern of weight gain are important determinants of the outcome of pregnancy.
• The appropriateness of the mother’s prepregnancy weight for height (BMI) is a major determinant of her recommended weight gain during pregnancy.
• Nutritional risk factors include adolescent pregnancy; bizarre or faddish food habits; abuse of nicotine, alcohol, or drugs; a low or high weight for height; and frequent pregnancies.
• Iron supplementation is usually recommended routinely during pregnancy, even though there is some controversy regarding its beneficial effects on successful outcome of pregnancy. Other supplements may be recommended when nutritional risk factors are present.
• The nurse and the woman are influenced by cultural and personal values and beliefs during nutrition counseling.
• Pregnancy complications that may be nutrition related include anemia, gestational hypertension, gestational diabetes, and IUGR.
• Dietary adaptation can be effective for some of the common discomforts of pregnancy, including nausea and vomiting, constipation, and heartburn.
![]() Audio Chapter Summaries Access an audio summary of the Key Points on
Audio Chapter Summaries Access an audio summary of the Key Points on ![]()


 cups of orange juice with calcium added
cups of orange juice with calcium added