Physiology of the skin
The skin is a metabolically active organ with vital functions (Table 1), including the protection and homeostasis of the body.
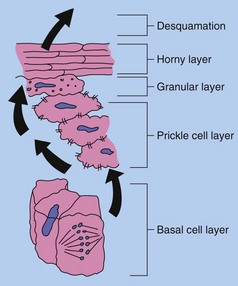
Keratinocyte maturation
The differentiation of basal cells into dead, but functionally important, corneocytes is a unique feature of the skin. The horny layer is important in preventing all manner of agents from entering the skin, including micro-organisms, water and particulate matter. Antimicrobial peptides of the defensin and cathelicidin classes, present on the epidermal surface, have bactericidal activity. The epidermis also prevents the body’s fluids from getting out.
Epidermal cells undergo the following sequence during keratinocyte maturation (Fig. 1):
1. Undifferentiated cells in the basal layer and the layer immediately above divide continuously. Half of these cells remain in place, and half progress upwards and differentiate.
2. In the prickle cell layer, cells change from being columnar to polygonal. Differentiating keratinocytes synthesize keratins, which aggregate to form tonofilaments. The desmosomes connecting keratinocytes are composed of the structural molecules cadherins, desmogleins and desmocollins. Desmosomes distribute structural stresses throughout the epidermis and maintain a distance of 20 nm between adjacent cells.
3. In the granular layer, enzymes induce degradation of nuclei and organelles. Keratohyalin granules containing filaggrin mature the keratin and provide an amorphous protein matrix for the tonofilaments. Membrane-coating granules attach to the cell membrane and release an impervious lipid-containing cement, which contributes to cell adhesion and to the horny layer barrier.
4. In the horny layer, the dead, flattened corneocytes have developed thickened cornified envelopes containing involucrin that encase a matrix of keratin macrofibres aligned by filaggrin. The strong disulphide bonds of the keratin provide strength to the stratum corneum, but the layer is also flexible and can absorb up to three times its own weight in water. However, if it dries out (i.e. water content falls below 10%), pliability fails.
5. The corneocytes are eventually shed from the skin surface after degradation of the lamellated lipid and loss of desmosomal intercellular connections.
Rate of maturation
Kinetic studies show that, on average, the dividing basal cells replicate every 200–400 h. The resultant differentiating cells in normal skin take 52–75 days to be shed from the stratum corneum. The epidermal transit time is considerably reduced in keratinization disorders such as psoriasis.
Hair growth
In most mammals, hair or fur plays an essential role in survival, especially in the conservation of heat; this is not the case in ‘nude’ humans. Scalp hair in humans does function as a protection against the cancer-inducing effects of ultraviolet (UV) radiation; it also protects against minor injury. However, the main role of hair in human society is as an organ of sexual attraction, and therein lies its importance to the cosmetics industry.
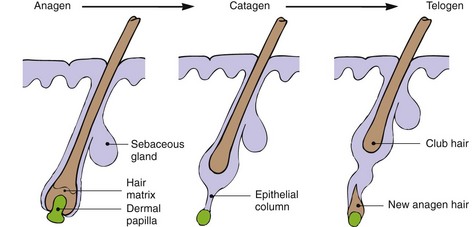
The rate of hair growth differs depending on the site. For example, eyebrow hair grows faster and has a shorter anagen (see below) than scalp hair. On average, there are about 100 000 hairs on the scalp, and the normal rate of growth is 0.4 mm/24 h. Hair growth is cyclical, with three phases, and is randomized for individual hairs, although synchronization does occur during pregnancy. The three phases of hair development (Fig. 2) are anagen, catagen and telogen.
1. Anagen is the growing phase. For scalp hair, this lasts from 3 to 7 years but, for eyebrow hair, it lasts only 4 months. At any one time, 80–90% of scalp hairs are in anagen, and about 50–100 scalp follicles switch to catagen per day.
2. Catagen is the resting phase and lasts 3–4 weeks. Hair protein synthesis stops, and the follicle retreats towards the surface. At any one time, 10–20% of scalp hairs are in catagen.
3. Telogen is the shedding phase, distinguished by the presence of hairs with a short club root. Each day, 50–100 scalp hairs are shed, with less than 1% of hairs being in telogen at any one time.
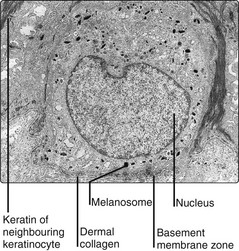
Melanocyte function
Melanocytes (located in the basal layer) produce the pigment melanin in elongated, membrane-bound organelles known as melanosomes (Fig. 3). These are packaged into granules, which are moved down dendritic processes and transferred by phagocytosis to adjacent keratinocytes. Melanin granules form a protective cap over the outer part of keratinocyte nuclei in the inner layers of the epidermis. In the stratum corneum, they are uniformly distributed to form a UV-absorbing blanket, which reduces the amount of radiation penetrating the skin. Thickening of the epidermis also blocks UV.
UV radiation – mainly the wavelengths of 290–320 nm (UVB) – darkens the skin first by immediate photo-oxidation of preformed melanin and second, over a period of days, by stimulating melanocytes to produce more melanin. UV radiation also induces keratinocyte proliferation, resulting in thickening of the epidermis.
Variations in racial pigmentation result not from differences in melanocyte numbers, but in the number and size of melanosomes produced. Gene polymorphisms in red-haired people cause impaired melanocyte-stimulating hormone signalling to the MC1-receptor, which leads to reduced levels of melanocyte eumelanin (brown/black) and therefore predominantly red phaeomelanin (p. 8).
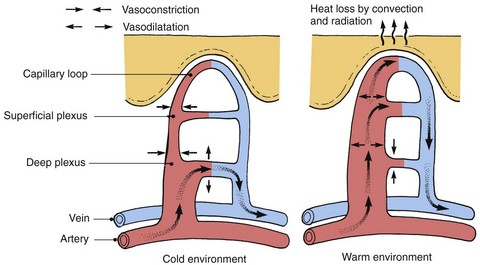
Thermoregulation
The maintenance of a near-constant body core temperature of 37°C is a great advantage to humans, allowing a constancy to many biochemical reactions that would otherwise fluctuate widely with temperature changes. Thermoregulation depends on several factors, including metabolism and exercise, but the skin plays an important part in control through the evaporation of sweat and by direct heat loss from the surface.
Blood flow
Skin temperature is highly responsive to skin blood flow. Dilatation or contraction of the dermal blood vessels results in vast changes in blood flow, which can vary from 1 to 100 mL/min per 100 g of skin for the fingers and forearms. Arteriovenous anastomoses under the control of the sympathetic nervous system shunt blood to the superficial venous plexuses (Fig. 4), affecting skin temperature. Local factors, both chemical and physical, can also have an effect.
Sweat
The production of sweat cools the skin through evaporation. The minimum insensible perspiration per day is 0.5 L. Maximum daily secretion is 10 L, with a maximum output of about 2 L/h. Men sweat more than women.
Watery isotonic sweat, produced in the sweat gland, is modified in the excretory portion of the duct so that the fluid delivered to the skin surface has:
 a low concentration of Na+ (30–70 mEq/L) and Cl− (30–70 mEq/L)
a low concentration of Na+ (30–70 mEq/L) and Cl− (30–70 mEq/L)
 a high concentration of K+ (up to 5 mEq/L), lactate (4–40 mEq/L), urea, ammonia and some amino acids.
a high concentration of K+ (up to 5 mEq/L), lactate (4–40 mEq/L), urea, ammonia and some amino acids.
Only small quantities of toxic substances are lost.
Sweating may also occur in response to emotion and after eating spicy food. In addition to thermoregulation, sweat also helps to maintain the hydration of the horny layer and improves grip on the palms and soles.
Physiology