CHAPTER 6 The Dental Hygiene Care Environment
The dental hygiene care environment is the physical setting that contains equipment and instruments where the dental hygienist delivers professional oral care. This chapter identifies the structural components of a conventional treatment area (operatory), the equipment and powered instruments the dental hygienist uses and maintains, and legal and ethical issues associated with equipment maintenance.
SETTINGS
Private Practice
Floor Plan
A private practice maintains treatment areas for dental units, radiographic equipment, general structural fixtures, a radiograph processing area, an instrument processing area, a laboratory, supply storage, a business office, a reception area, and a restroom. Some offices also have staff and private consultation rooms.
Dental Hygiene Treatment Area
Stools and Chairs
The treatment area, where professional oral care is provided, contains stools, the dental chair, the dental unit, and equipment (Figure 6-1). The operator stool can be adjusted for seat height and back support with controls located under the seat cushion (Figure 6-2). Ergonomic stools contain extended armrests to support forearms. The dental assistant stool, taller than an operator stool, differs in function and usually has a bar to support the feet and a torso support bar that allows the dental assistant to lean forward over the patient (Figure 6-3). The dental chair, a reclining elongated lounge, has arm supports and is adjustable by switch, touch pad, or foot control for height, head rest, swivel, and tilt. Coverings on dental stools and chairs are durable and easily cleaned and disinfected (Figure 6-4).
The Dental Unit
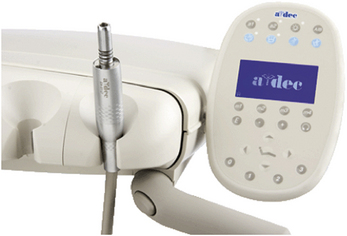
The dental unit contains the delivery system and a dental light. The delivery system, attached to a bracket table, moveable arm, or mobile cart, typically contains the air-water syringe, the high-speed and low-speed handpiece tubing, and a radiograph view box. The dental light can be mounted on a ceiling track or on a pole attached to the dental unit. Electrical power, light, and water are controlled by switch or rheostat (foot control); most units have separate power and water switches independent of each other. Some delivery systems have touch pads mounted on the bracket or instrument table that operate the components of the system (Figures 6-5 and 6-6). There are a number of variations in design for a bracket or instrument table, which can hold instruments and the components of the delivery system for the clinician and dental assistant.
Additional mounted tubing on the delivery system arm may include an ultrasonic or sonic scaler, an air polishing hand-piece, a fiberoptic light, a composite curing light, a laser, and/or an intraoral camera. Usually these devices are activated by switch or rheostat. Mounted on the delivery arm could be a monitor for a computer to display electronic client records. These pieces of equipment could be mounted in front of the clinician for a 9 o'clock seating position or behind the client's head for a 12 o'clock delivery system and a seating position for the clinician behind the client's head (Figures 6-7 and 6-8).
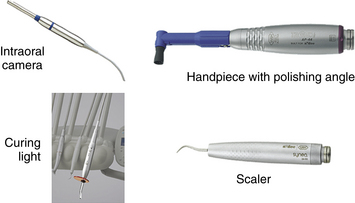
Figure 6-7 Examples of mounted equipment in a dental delivery system.
(Courtesy A-dec, Inc, Newberg, Oregon.)
High-volume evacuation (HVE) and low-volume evacuation (LVE) tubing or suction lines facilitate client rinsing and maintain visibility and oral fluid control during care. Adapters and devices are available for suction lines that accommodate narrow and wide suction tip inserts and saliva ejectors. Dental units have a separate water bottle supply (closed water system) for the unit (Figure 6-9) or a facility-wide water treatment system. In either case, daily treatments such as iodine tablets for water bottles or suction line chemical treatments are necessary to prevent biofilm formation in the water tubing or lines. Antiretraction valves on the water lines prevent the backflow of contaminated water into the water lines of the unit.
Radiographic Equipment
Radiographic equipment consists of a wall-mounted control panel with an on-off switch, an indicator light, exposure settings, an x-ray tube mounted on a long moveable arm with an open cylinder or rectangular position-indicating device (PID) at the end, and a wall-mounted exposure button (Figure 6-10). The lead apron with a thyroid collar is worn by patients during x-ray exposure; it is hung on hooks or a bar located in the treatment area. The radiograph view box may be mounted on the delivery system, wall, or counter (Figure 6-11).

Figure 6-10 A dental unit x-ray tube.
(Courtesy Practiceworks Systems, LLC, the exclusive maker of Kodak Dental Systems, Atlanta, Georgia.)

Figure 6-11 Radiograph view box.
(Courtesy Dentsply Rinn, a division of Dentsply International, Elgin, Illinois.)
Digital radiographic technology uses the same x-ray tube as conventional methods; however, a charged photoreceptor sensor, the size of #0 or #2 film, is used in lieu of a conventional film packet. Digital radiographic images can be viewed on a computer screen, stored, transmitted electronically, or printed (Figure 6-12).

Figure 6-12 Digital radiographic sensors.
(Courtesy Dentsply Rinn, a division of Dentsply International, Elgin, Illinois.)
Panoramic radiography produces a film of the maxillary and mandibular jaws. Some treatment areas may be large enough to house the panoramic x-ray machine; some facilities have separate rooms for this machine.
Structural Fixtures
Most treatment areas have storage cabinets, a sink, paper towel dispensers, and alcohol hand rub and antibacterial soap dispensers with manual, foot, or laser controls. Infection-control standards mandate an emergency eye wash station attached to the faucet of a sink in the facility. A biohazard sharps container to collect contaminated needles and sharp objects is in the treatment area to help prevent needle stick exposures during disposal. This counter can also hold the client's dental chart, models, or other reference materials during treatment. The walls and flooring in the treatment area are functional, easily cleaned and sturdy. Draperies, carpeting, and delicate furnishings are not appropriate in treatment areas because they hold contaminants and are difficult to disinfect.
A compressor provides compressed air to run the dental handpieces and suction. Because of its size and noise production, the compressor may be housed in a mechanical room with other devices such as circuit breakers, fuse box, central suction, water heater, and heating and air conditioning units.
Darkroom or Radiograph Processing Area
A film processing area houses automatic dental radiographic film processing units that provide standardized processing of films using premixed solutions, automated time and temperature exposure, and rinsing and drying of films. In addition to overhead lighting in the room, an outside warning light prevents accidental entry into the darkroom while films are being processed (Figure 6-13).
Instrument Recirculation Area (see Chapter 7 on Infection Control)
The instrument recirculation area is where contaminated instruments are processed for reuse. Contaminated instruments must be carried to this area in a covered container or cassette. The area should have a clearly demarcated entrance point to bring in contaminated instruments and an exit point for the sterile instruments. Demarcated areas prevent the accidental exposure of sterile instruments and people to blood and bodily fluids from contaminated instruments. This well-ventilated area contains the ultrasonic instrument cleaning device, dry heat, steam-pressure or chemical-pressure and/or flash sterilizer, products used in preparing instruments for sterilization, and a container with a high-level liquid chemical instrument disinfectant. Another biohazard trash and sharps container is located in the contaminated section of the processing area or isolated area.
Sterilized instruments are stored in wrapped preset trays or cassettes away from the contaminated processing area. Following manufacturer's directions for all equipment is necessary so that procedures are implemented consistently to ensure the optimum performance of the equipment. Cleaning and disinfection supplies may be stored in this area.
Dental Laboratory
The dental laboratory is used for pouring impressions and trimming study models and the storing of impression trays, rubber bowls, alginate, spatulas, dental plaster, dental stone, tray formers, and a model vibrator to eliminate air bubbles in the models. A model trimmer, used to trim the excess plaster or stone from the study models, a sink, and a water source with temperature controls are standard dental laboratory features.
Many treatment facilities finish (final stage of polishing or fabrication) crowns or bridges, adjust dental appliances, or fabricate mouth guards, night guards, or custom whitening trays. To accomplish these tasks, a model articulator, dental lathe, a lathe hood, a vacuum machine to shape acrylic, shears and nippers, and a dental engine with a laboratory handpiece are needed, along with air and gas outlets, gas torch, alcohol or Bunsen burners, casting ovens, waxing units to make templates, base plates, waxing spatulas, copings, and waxed patterns for casting procedures. In some facilities, preparation of impressions or prostheses for transmittal to a commercial laboratory takes place in the laboratory. This is usually an area where dust, byproducts from procedures, and noises are present. Whenever possible, the dental laboratory is accessible to the treatment areas but out of sight and hearing range of patients.
Equipment Maintenance
Delivery of high-quality dental care requires equipment maintenance; regular cleaning of the dental unit's traps, filters, and lines prevents biofilm contamination and disease transmission. Dental equipment suppliers publish information on the use and maintenance of their products, which should be followed. If these documents are not available, most manufacturers publish maintenance information on their websites.
Business Area
Generally located near the entrance of the facility, the business area, with computer terminals, phones, and an intraoffice communication system, is where the client records, appointment schedules, and office supplies are maintained. The complexity of this area depends on the size and needs of the practice. Adjacent is a reception area in which clients can relax before their appointments.
Dental Hygiene Care Facility (College Setting)
In a college setting, dental hygiene students encounter most of the structural fixtures, equipment, and instruments of a private practice. Most campus clinical settings have simulator labs where an automated manikin complete with a dentoform or typodont (replica of the oral cavity) and delivery system allow students to practice, media equipment to view and record instruction from professors, and computers to store and access information electronically (Figure 6-14).
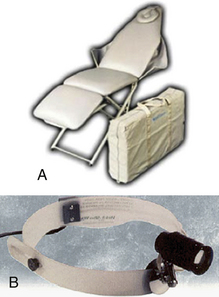
Hospital Setting
As part of a specialized oral surgical team, dental hygienists provide therapeutic services to cognitively challenged and medically complex individuals. In acute and chronic care settings, dental hygienists may provide bedside care to patients too ill to be transported to the dental clinic. Care for persons who are home-bound, bedridden, or wheelchair-bound requires the clinician to use hand-activated methods of instrumentation or portable dental equipment (Figures 6-15 and 6-16).
Mobile Dental Facility
Some community health agencies and private foundations own fully equipped mobile dental vans for providing preventive and therapeutic services to underserved populations (Figure 6-17). Fully equipped train cars travel on the existing rail systems, bringing high-quality oral care to underserved areas. An example of this type of mobile dental facility is the Smile Train.
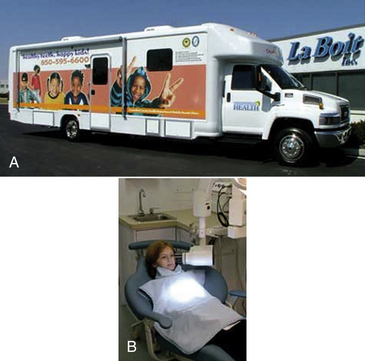
Figure 6-17 A, Mobile dental van. B, Treatment area.
(Courtesy La Boit, Inc, Gahanna, Ohio, www.laboit.com.)
CLIENT EDUCATION TIPS
LEGAL, ETHICAL, AND SAFETY ISSUES
KEY CONCEPTS
 A dental hygiene care environment is the physical setting in which professional care is delivered; defined areas are designed for the delivery and support of professional care. The environment may be stationary or mobilized to place-bound or underserved populations.
A dental hygiene care environment is the physical setting in which professional care is delivered; defined areas are designed for the delivery and support of professional care. The environment may be stationary or mobilized to place-bound or underserved populations. The treatment area is where professional oral care is delivered; it includes specially designed chairs for the client, the clinician, and the assistant; bracket tables; delivery systems; dental light; sink; an x-ray machine; an ultrasonic or sonic scaler; an intraoral camera; and a computer monitor.
The treatment area is where professional oral care is delivered; it includes specially designed chairs for the client, the clinician, and the assistant; bracket tables; delivery systems; dental light; sink; an x-ray machine; an ultrasonic or sonic scaler; an intraoral camera; and a computer monitor. Additional space for instrument and film processing is created in separate rooms or in clearly designated areas.
Additional space for instrument and film processing is created in separate rooms or in clearly designated areas. High-quality professional care may be delivered in private practices, college campus care facilities, hospitals, research facilities, community clinics, mobile vehicles, elementary schools, long-term care facilities, military bases, penal institutions, and private homes.
High-quality professional care may be delivered in private practices, college campus care facilities, hospitals, research facilities, community clinics, mobile vehicles, elementary schools, long-term care facilities, military bases, penal institutions, and private homes. The dental hygienist is responsible for learning effective, safe usage practices for the equipment, supplies, and instruments used in the delivery of care.
The dental hygienist is responsible for learning effective, safe usage practices for the equipment, supplies, and instruments used in the delivery of care.Bird D.L., Robinson D.S. Torres and Ehrlich modern dental assisting, ed 9. St Louis: Saunders; 2009.
Finkbeiner B., Finkbeiner C. Practice management for the dental team, ed 6. St Louis: Mosby; 2006.
Finkbeiner B., Johnson C. Mosby's comprehensive review of dental assisting. St Louis: Mosby; 1997.
Kohn W.G., Collins A.S., Cleveland J.L., et al. Guidelines for infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003;52(RR-17):1.
Visit the  website at http://evolve.elsevier.com/Darby/Hygiene for competency forms, suggested readings, glossary, and related websites..
website at http://evolve.elsevier.com/Darby/Hygiene for competency forms, suggested readings, glossary, and related websites..