Interpretation of Periodontal Disease
After completion of this chapter, the student will be able to do the following:
• Define the key terms associated with interpreting periodontal disease
• Describe the healthy periodontium
• Briefly describe periodontal disease
• Discuss the importance of the clinical examination and interpretation of dental images in the diagnosis of periodontal disease
• Describe the limitations of dental images in the detection of periodontal disease
• Describe the type of dental images that should be used to document periodontal disease and the preferred exposure technique
• State the difference between horizontal bone loss and vertical bone loss
• State the difference between localized bone loss and generalized bone loss
• State the differences among mild, moderate, and severe bone loss
• List each of the four American Dental Association (ADA) case types and describe the corresponding appearance on dental images
• Recognize each of the four ADA case types on dental images
• List two predisposing factors for periodontal disease
• Recognize and describe the appearance of calculus on dental images
Dental images play an integral role in the assessment of periodontal disease. An examination of dental images is essential for diagnostic purposes because it enables the dental professional to obtain vital information about supporting bone, as this information cannot be obtained clinically. Detailed information about periodontal disease is beyond the scope of this text. The purpose of this chapter is to introduce the dental radiographer to the description and detection of periodontal disease. The interpretation of periodontal disease, with an emphasis on a description of bone loss, ADA case types, and identification of predisposing factors, is also presented.
Description of the Periodontium
The term periodontium refers to tissues that invest and support teeth, such as the gingiva and alveolar bone. As described in Chapter 27, the normal anatomic landmarks of alveolar bone include the lamina dura, alveolar crest, and periodontal ligament space. The appearance of healthy alveolar bone on a dental image can be described as follows:
Lamina dura: In health, the lamina dura of teeth appears as a dense radiopaque line around the roots (Figure 34-1).

FIGURE 34-1 Healthy alveolar crest, normal lamina dura, and periodontal ligament space on a periapical image. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
Alveolar crest: The normal healthy alveolar crest is located approximately 1.5 to 2.0 mm apical to the cemento-enamel junctions (CEJs) of adjacent teeth (see Figure 34-1). The shape and density of the alveolar crest vary between the anterior and posterior regions of the mouth. In the anterior regions, the alveolar crest appears pointed and sharp and is normally very radiopaque (Figure 34-2). In the posterior regions, the alveolar crest appears flat, smooth, and parallel to a line between adjacent CEJs (Figure 34-3). The alveolar crest in the posterior regions appears slightly less radiopaque than that in the anterior regions.
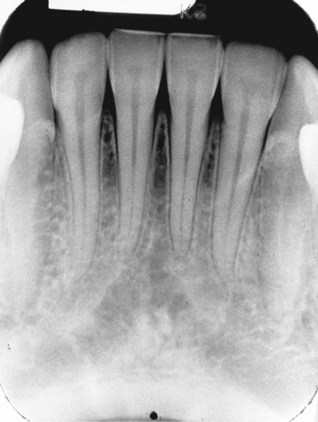
FIGURE 34-2 Healthy alveolar crest in the anterior region that appears pointed and highly radiopaque. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)

FIGURE 34-3 Healthy alveolar crest in the posterior region that appears flat, smooth, and radiopaque. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
Periodontal ligament space: The normal periodontal ligament space appears as a thin radiolucent line between the root of the tooth and the lamina dura. In health, the periodontal ligament space is continuous around the root structure and is of uniform thickness (see Figure 34-1).
Description of Periodontal Disease
The term periodontal literally means “around a tooth.” Periodontal disease refers to a group of diseases that affect the tissues around teeth. Periodontal disease may range from a superficial inflammation of the gingiva to the destruction of supporting bone and the periodontal ligament. With periodontal disease, the gingiva exhibits varying degrees of inflammation. Gingival tissues affected by periodontal disease may not appear stippled, pink, and firm. Instead, the gingiva may appear swollen, red, and bleeding, and formation of soft tissue pockets is seen.
On a dental image, the appearance of alveolar bone affected by periodontal disease differs from that of healthy alveolar bone. With periodontal disease, the alveolar crest is no longer located 1.5 to 2.0 mm apical to the CEJs and no longer appears radiopaque. Instead, the alveolar crest appears indistinct, and bone loss is seen. Periodontal disease may result in severe destruction of bone and loss of teeth.
Detection of Periodontal Disease
To detect periodontal disease, both clinical examinations and interpretation of dental images are necessary. Dental images must be used in conjunction with a clinical examination. In general, what is seen clinically cannot be evaluated on dental images, and what is viewed on dental images cannot be evaluated clinically. Clinical examination provides information about soft tissues, while dental images permit evaluation of bone.
Clinical Examination
Clinical examination must be performed by the dentist and dental hygienist and should include an evaluation of soft tissues (gingiva) for signs of inflammation (e.g., redness, bleeding, swelling, pus). A thorough clinical assessment must include periodontal probing. Whenever clinical evidence of periodontal disease is present, images must be obtained in order to get maximum diagnostic information.
Dental Image Examination
Dental images, along with clinical examination, enable the dental professional to determine the extent of periodontal disease. Dental images provide an overview of the amount of bone present and indicate the pattern, distribution, and severity of bone loss resulting from periodontal disease. In addition, dental images enable the dental professional to document periodontal disease at specific points in time.
The periapical image is recommended for the evaluation of periodontal disease. The paralleling technique is the preferred periapical exposure method for the demonstration of the anatomic features of periodontal disease. With the paralleling technique, the height of crestal bone is accurately recorded in relation to the tooth root. If the bisecting technique is used to expose periapical images, a dimensional distortion of bone results due to vertical angulation. Therefore, periapical images using the bisecting technique may show more or less bone loss than actually present (Figures 34-4 and 34-5).

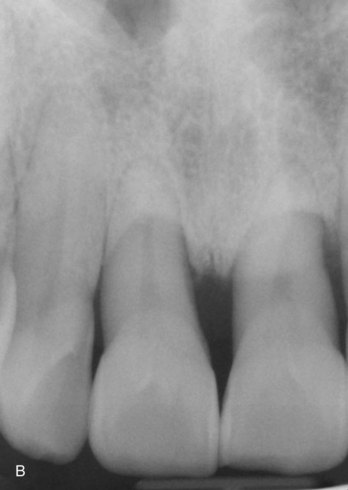
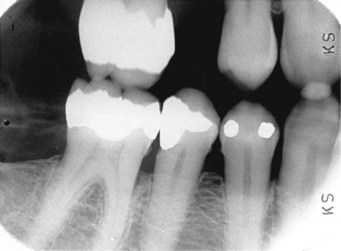
FIGURE 34-4 Bisecting technique distorting the level of bone present seen on an image because of the vertical angulation used. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)

FIGURE 34-5 Paralleling technique used to examine the same area seen in Figure 34-4. Note the difference in bone level. With the paralleling technique, the height of crestal bone is accurately recorded in relation to the tooth root. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
The horizontal bite-wing image alone should not be used to document moderate to severe periodontal disease. This image has limited use in the detection of periodontal disease; severe interproximal bone loss cannot be adequately visualized on horizontal bite-wing images.
The vertical bite-wing image can be used to examine bone levels and is best used for post-treatment and follow-up purposes. The panoramic image has little diagnostic value in the identification of periodontal disease and is not recommended to demonstrate the anatomic features of this condition.
Dental images alone cannot be used to diagnose periodontal disease because of limitations in detecting and diagnosing the condition; images must be used in conjunction with a thorough clinical examination. For example, dental images do not provide information about the condition of soft tissues or the early bony changes seen in periodontal disease. Because dental images record two-dimensional images of three-dimensional structures, certain areas of teeth and bone are difficult, if not impossible, to examine in this manner. Buccal and lingual areas are particularly difficult to evaluate. For example, bone loss in the furcation area—the area between the roots of multirooted teeth—may not be detected on a dental image because of the superimposition of buccal and lingual bone.
Interpretation of Periodontal Disease on Dental Images
The dental radiographer must be familiar with the appearance of periodontal disease. All images should be evaluated for bone loss and examined for other predisposing factors that may contribute to periodontal disease.
Bone Loss
A dental image allows the dental professional to view the amount of bone remaining rather than the amount of bone lost. However, in documenting bone levels, the amount of bone loss that has occurred is recorded rather than the amount of bone that remains. The amount of bone loss can be estimated as the difference between the physiologic bone level and the height of remaining bone (Figure 34-6). Bone loss can be described in terms of the pattern, distribution, and severity of loss.
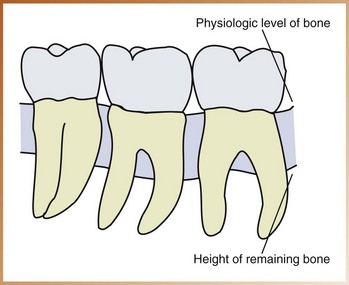
FIGURE 34-6 Bone loss estimated as the difference between the physiologic level of bone and the height of the remaining bone. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
Pattern
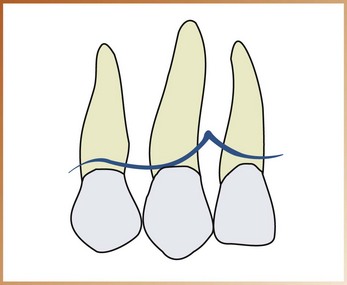
The pattern of bone loss viewed on a dental image can be described as horizontal or vertical. The CEJs of adjacent teeth can be used as a plane of reference in determining the pattern of bone loss present. With horizontal bone loss, the bone loss occurs in a plane parallel to the CEJs of adjacent teeth (Figures 34-7 and 34-8). With vertical bone loss (also known as angular bone loss), the bone loss does not occur in a plane parallel to the CEJs of adjacent teeth (Figures 34-9 and 34-10).
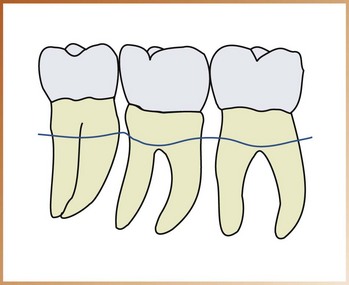
FIGURE 34-7 Horizontal bone loss, which occurs in a plane parallel to the cemento-enamel junctions (CEJs) of adjacent teeth. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
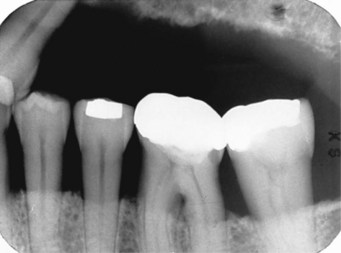
FIGURE 34-8 Horizontal bone loss. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
Distribution
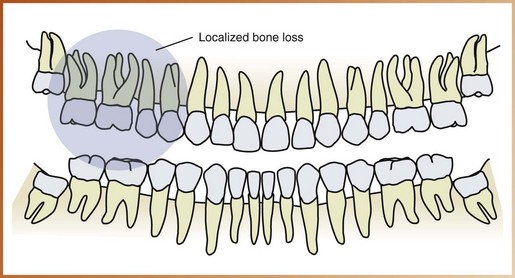
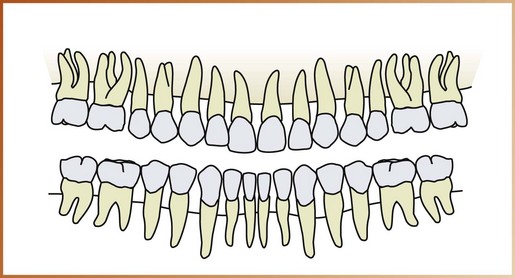
The distribution of bone loss seen on a dental image can be described as localized or generalized, depending on the areas involved. Localized bone loss occurs in isolated areas, with less than 30% of the sites involved (Figure 34-11). Generalized bone loss occurs evenly throughout the dental arches, with more than 30% of the sites involved (Figure 34-12).
Severity
Bone loss viewed on a dental image can be classified as slight, moderate, or severe. The severity of bone loss is measured by the clinical attachment loss (CAL). The CAL is a measurement of the distance in millimeters from the CEJ to the base of the sulcus or periodontal pocket; CAL is measured by the calibrated periodontal probe. (Note: Clinical conditions, such as recession or gingival overgrowth, must be considered when determining CAL.) The severity of bone loss can be defined as follows:
Classification of Periodontal Disease
Classification systems are routinely used to provide a framework to study clinical findings and for the treatment of disease. The classification system for periodontal disease was revised in 1999 (Armitage, 1999). More clinical information regarding disease categories, including gingival disease, age-related terminology, and the pathogenesis of periodontal disease, was highlighted in this latest classification system.
Dental images can be used in the classification of periodontal disease. On the basis of the amount of bone loss, periodontal disease can be classified as follows: the American Dental Association (ADA) Case Type I (gingivitis), ADA Case Type II (mild or slight periodontitis), ADA Case Type III (moderate periodontitis), or ADA Case Type IV (advanced or severe periodontitis). Each disease type has a specific appearance. Dental images can also be used to detect the contributing factors for periodontal disease, such as calculus and defective restorations.
ADA Case Type I
No bone loss is associated with type I disease (gingivitis); therefore, no change in bone is seen on the dental image. The crestal lamina dura is present, and the alveolar crest is approximately 1 to 2 mm apical to the CEJ. Clinically, bleeding may or may not be present. Only the gingival tissues are affected by the inflammatory process in ADA Case Type I.
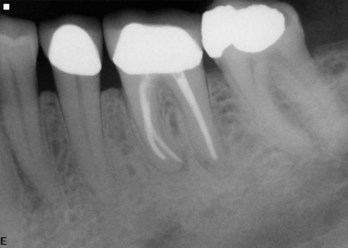
ADA Case Type II
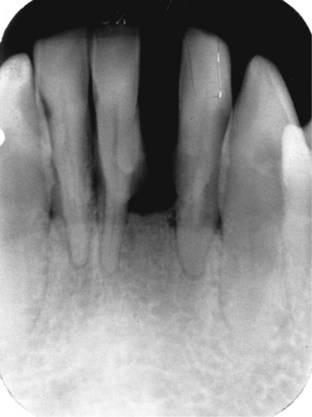
The bone loss associated with type II disease (mild or slight periodontitis) is mild crestal changes (Figures 34-13 to 34-15). The lamina dura becomes unclear and fuzzy and no longer appears to be a continuous radiopaque line. Horizontal bone loss is seen more often in type II disease, with the alveolar bone level approximately 3 to 4 mm apical to the CEJ. Clinically, bleeding may occur on probing, pocket depths resulting from attachment loss as well as localized areas of recession may be evident.
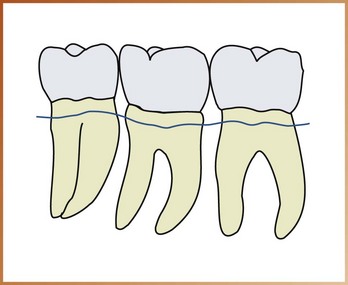
FIGURE 34-13 Mild bone loss. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
ADA Case Type III
Horizontal or vertical bone loss may be present in type III disease; the distribution of the bone loss may be localized or generalized (Figures 34-16 to 34-19). The alveolar bone level is approximately 4 to 6 mm apical to the CEJs of adjacent teeth. Furcation involvement, or the extension of periodontal disease between the roots of multirooted teeth, may also be seen in type III disease. When bone in the furcation area is destroyed, a radiolucent area is evident on the dental image (Figure 34-20). Clinically, pocket depths and attachment loss up to 6 mm are evident. Recession, furcation involvement areas, and slight mobility may also be present.

FIGURE 34-16 ADA Case Type III. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
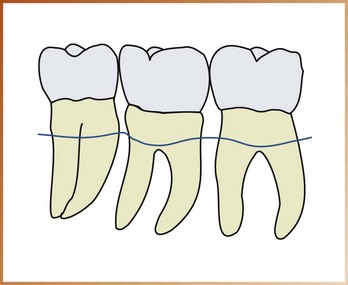
FIGURE 34-17 Moderate bone loss. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)

FIGURE 34-18 ADA Case Type III. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
ADA Case Type IV
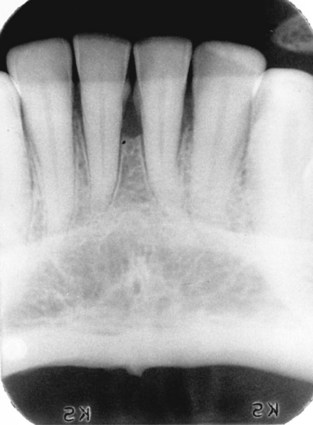
The bone loss associated with type IV disease (advanced or severe periodontitis) indicates further progression of the disease and is considered severe (Figures 34-21 to 34-23). The pattern of bone loss may be horizontal or vertical, and the alveolar bone level is 6 mm or greater from the CEJ. Furcation involvement is readily viewed on posterior images. Clinically, pocket depths and attachment loss are greater than 6 mm, and furcation involvement and mobility are more severe.
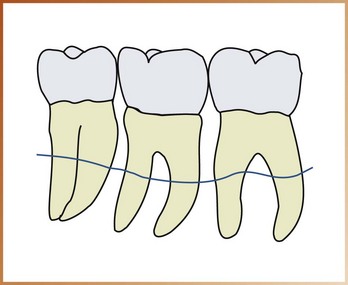
FIGURE 34-21 Severe bone loss. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
Predisposing Factors
The effects of certain medications, tobacco use, and various medical conditions are all considered risk factors for periodontal disease. A number of other factors may predispose the patient or contribute to periodontal disease. The identification, detection, and elimination of local irritants are important in the management and treatment of periodontal disease. Dental images play a major role in the detection of local irritants such as calculus and defective restorations.
Calculus
Calculus is a stonelike concretion that forms on the crowns and roots of teeth due to the calcification of bacterial plaque. Calculus acts as a contributing or predisposing factor to periodontal disease. Calculus appears radiopaque (white or light) on a dental image (Figure 34-24). Although calculus may have a variety of appearances on dental images, it most often appears as pointed or irregular radiopaque projections extending from proximal root surfaces (Figure 34-25). Calculus may also appear as a ringlike radiopacity encircling the cervical portion of a tooth (Figure 34-26), a nodular radiopaque projection (Figure 34-27), or a smooth radiopacity on a root surface (Figure 34-28).

FIGURE 34-24 Subgingival calculus that appears as irregular radiopaque projections in the maxillary anterior region. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
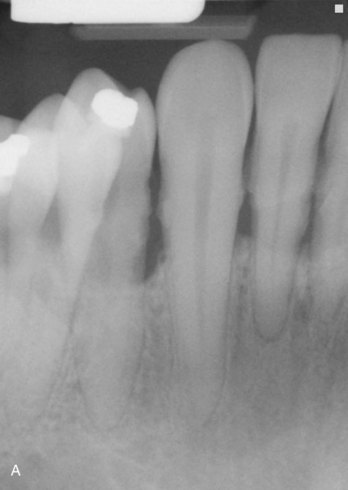

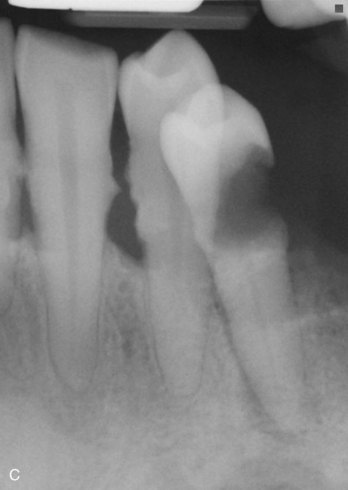
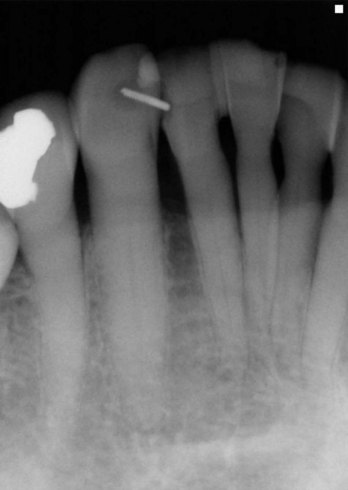
FIGURE 34-25 A–C, Calculus that appears as sharp, pointed radiopacities along the surfaces of mandibular anterior teeth. (Courtesy Timothy W. Godsey, DDS, MS, and Liliana Gandini, DMD, Chapel Hill, NC.)
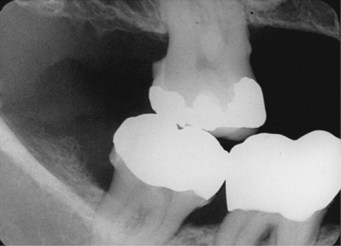
FIGURE 34-26 Calculus appearing as a ring-like radiopacity around the cervical region of a tooth. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
Defective Restorations
Faulty dental restorations act as potential food traps and lead to the accumulation of food debris and bacterial deposits. Defective restorations act as contributing factors to periodontal disease and can be detected both clinically and on dental images. Dental images allow the dental professional to identify restorations with open or loose contacts, poor contours uneven marginal ridges, overhangs, and inadequate margins, all of which may contribute to periodontal disease (Figures 34-29 to 34-35).
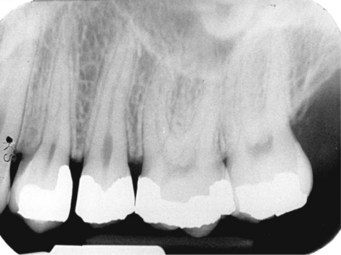
FIGURE 34-29 Open contact between maxillary premolars. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)

FIGURE 34-30 Poorly contoured crowns on maxillary and mandibular first molars. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)

FIGURE 34-31 A poorly contoured stainless steel crown causing bone loss on a mandibular first molar.
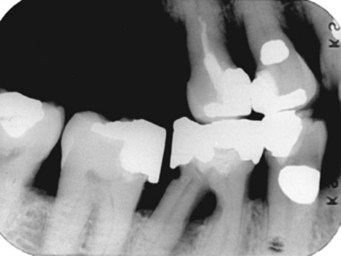
FIGURE 34-32 Uneven marginal ridges, open contacts, overhangs, and poorly contoured restorations on a bite-wing image. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)

FIGURE 34-33 Amalgam overhang on the mesial surface of the mandibular first molar. (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
Summary
• The term periodontal disease refers to a group of diseases that affect the tissues around teeth.
• Thorough clinical and dental image examinations are necessary to detect, diagnose, and evaluate periodontal disease. Clinical examination provides information about soft tissues, and the dental image examination provides information about supporting bone.
• Dental images can be used to document periodontal disease and determine the success or failure of periodontal therapy.
• Interpretation of periodontal disease on dental images should include an evaluation of alveolar bone; bony changes can be described in terms of pattern (horizontal or vertical), distribution (localized or generalized), and severity (slight, moderate, or severe).
• Dental images can be used in the classification of periodontal disease. On the basis of the amount of bone loss, periodontal disease can be classified as ADA Case Type I (gingivitis), Case Type II (mild/slight periodontitis), Case Type III (moderate periodontitis), and Case Type IV (advanced/severe periodontitis).
• Dental images can also be used to detect local irritants, including calculus and defective restorations, that contribute to periodontal disease.
American Academy of Periodontology. Treatment of plaque-induced gingivitis, chronic periodontitis and other clinical conditions. J Periodontol. 2001;72:1790–1800.
Armitage, GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4:1–6.
Frommer, HH, Savage-Stabulas, JJ, Caries and periodontal disease. Radiology for the dental professional, ed 9, St. Louis, Mosby, 2011.
Haring, JI, Lind, LJ. Periodontal disease. In: Radiographic interpretation for the dental hygienist. Philadelphia: Saunders; 1993.
Miles, DA, Van Dis, ML, Jensen, CW, Williamson, GF, Basics of interpretation: normal versus abnormal and common radiographic presentation of lesions. Radiographic imaging for the dental team, ed 4, Philadelphia, Saunders, 2009.
Newman, MG, Takei, H, Carranza, FA, Classification of diseases and conditions affecting the periodontium. Carranza’s clinical periodontology, ed 10, Philadelphia, Saunders, 2006.
White, SC, Pharoah, MJ, Periodontal diseases. Oral radiology: principles of interpretation, ed 6, St. Louis, Mosby, 2009.
Identification
For questions 1 to 5, identify the pattern of bone loss, severity of bone loss, and ADA Case Type (I to IV) represented by each dental image in Figures 34-36 to 34-40.

FIGURE 34-36 (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
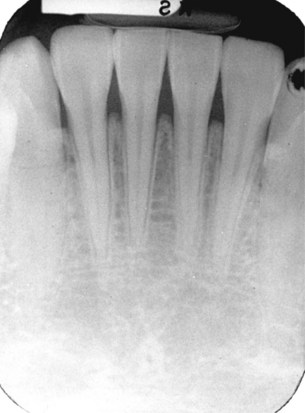
FIGURE 34-37 (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)

FIGURE 34-38 (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)

FIGURE 34-39 (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
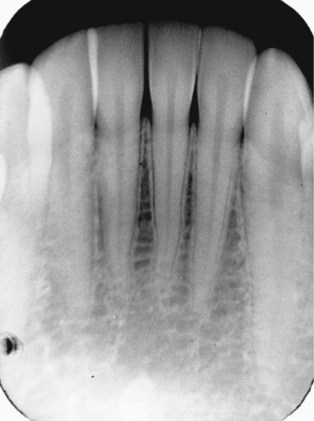
FIGURE 34-40 (From Haring JI, Lind LJ: Radiographic interpretation for the dental hygienist, Philadelphia, 1993, Saunders.)
Matching
For questions 6 to 9, match each of the ADA case types with the appropriate dental image description.
Fill in the Blank
10. A term that refers to tissues that invest and support teeth.
11. A term that means “around a tooth.”
12. A term that refers to the area between the roots of multirooted teeth.
13. The image of choice for the evaluation of periodontal disease.
14. The preferred method of exposure for receptors documenting periodontal disease.
15. The term that describes bone loss that occurs in a plane parallel to the CEJs of adjacent teeth.
16. The term that describes bone loss that does not occur in a plane parallel to the CEJs of adjacent teeth.
17. The term that describes a group of diseases that affect the tissues found around teeth.
18. The term that describes bone loss that occurs in isolated areas.
19. The term that describes bone loss that occurs evenly throughout the arches.
20. The term that describes a stonelike concretion that forms on the crowns and roots of teeth as a result of the calcification of plaque.