Chapter 81Tendon Lacerations
Tendon lacerations are serious injuries in horses because of the loss of the biomechanical function of the tendon, the slow return of tendon strength, the immediate strenuous loading demanded by a horse, and the complications of scarring. Nonetheless, early diagnosis, wound management, limb support, and long-term surgical and medical management have resulted in a good prognosis for most horses with extensor tendon lacerations and a fair prognosis for most of those with flexor tendon lacerations.1,2 The extensor (dorsal) aspect of the limb is often damaged by wire or a sharp object over which the horse has jumped. The flexor (palmar or plantar) aspect of the limb may be traumatized by circumferential wire injuries, landing on a sharp object, or being struck. The latter may be self-inflicted or from another horse.
Diagnosis
Gross Appearance of the Wound
Any laceration over the dorsal or palmar/plantar surface of the limb distal to the stifle or elbow, especially across the dorsal aspect of the tarsus, distal dorsal aspect of the tarsus, dorsal metatarsal region, distal aspect of the radius, dorsal metacarpal region, and dorsal fetlock region may involve a tendon (Figure 81-1). Extensor tendons and the superficial digital flexor tendon (SDFT) are positioned directly under the skin; therefore minor-appearing wounds can transect these tendons completely. Direct visual inspection may reveal transected tendon fibers protruding from the wound. However, injuries sustained at the gallop may result in a skin wound removed from the site of tendon damage because of the movement of the skin during exercise. The position of the wound relative to synovial structures should be evaluated with care because concurrent synovial contamination or infection reduces the prognosis and necessitates specific emergency treatment.
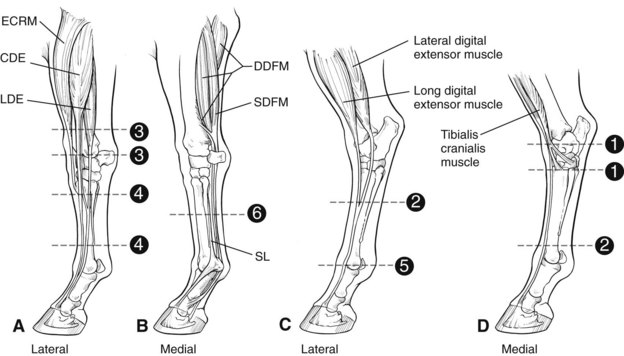
Fig. 81-1 Diagram illustrating common sites of tendon injury. A, Lateral forelimb. B, Medial forelimb. C, Lateral hindlimb. D, Medial hindlimb. 1, Dorsal tarsus; 2, dorsal metatarsal region; 3, distal radius; 4, dorsal metacarpal region; 5, dorsal fetlock region; 6, palmar metacarpal region; ECRM, extensor carpi radialis muscle; CDE, common digital extensor muscle; LDE, lateral digital extensor muscle; DDFM, deep digital flexor muscle; SDFM, superficial digital flexor muscle; SL, suspensory ligament.
(Adapted from Bertone AL: Tendon laceration in tendon and ligament injuries. Part II, Vet Clin North Am Equine Pract 11:293, 1995.)
Evaluation of Gait
Each tendon serves a biomechanical function. Complete severance of a tendon results in a posture or gait change, which may be pathognomonic for disruption of the tendon integrity.
Extensor Tendons
Transection of an extensor tendon below the carpus produces a reduced ability to extend the digit, which is detected as an exaggerated, rapid (uncontrolled) dorsal flip of the hoof at the walk. This subtle change is easiest to detect if the lateral and common (or long) digital extensor tendons are transected completely. Intermittently the horse knuckles at the fetlock joint and places the digit on the dorsal surface of the pastern and fetlock joint. The gait abnormality is more obvious in a hindlimb and with lacerations in close proximity to the fetlock. Remaining peritendonous fascial attachments provide some support in horses with more proximal injuries. Horses with extensor tendon lacerations bear weight fully in a normal posture, unless other aspects of the wound create lameness and pain.
Transection of extensor tendons proximal to the carpus and at, or just proximal to, the tarsus also commonly occurs. Proximal to the carpus, transection of the extensor carpi radialis and common digital extensor tendons is most frequent. Flexion of the carpus may cause pain. The tendon sheath is often involved.
Proximal or dorsal to the tarsus, transection of the long digital extensor, cranialis tibialis, and fibularis (peroneus) tertius tendons is most frequent. ![]() If the fibularis tertius is disrupted, the hock can be extended while the stifle is flexed, indicating loss of the reciprocal apparatus. The gastrocnemius tendon develops a characteristic wrinkle in this extended position (see Figure 80-2 and page 802). The degree of gait abnormality may be mild. Transection of all the extensor tendons over the tarsus still allows full weight bearing with the foot flat on the ground. A greater tarsal extension during the swing phase of the stride and intermittent knuckling of the digit can be detected.
If the fibularis tertius is disrupted, the hock can be extended while the stifle is flexed, indicating loss of the reciprocal apparatus. The gastrocnemius tendon develops a characteristic wrinkle in this extended position (see Figure 80-2 and page 802). The degree of gait abnormality may be mild. Transection of all the extensor tendons over the tarsus still allows full weight bearing with the foot flat on the ground. A greater tarsal extension during the swing phase of the stride and intermittent knuckling of the digit can be detected.
Digital Flexor Tendons
Transection of the digital flexor tendons below the carpus or tarsus produces pain on weight bearing and therefore lameness and gait abnormality. Transection of the SDFT is most common because it has the most superficial position of the two digital flexor tendons. The suspensory ligament (SL) is deep to the deep digital flexor tendon (DDFT) and is therefore least commonly injured with lacerations. A horse with complete transection of the SDFT may stand normally, or it may bear weight on the toe of the hoof to minimize movement of the tendon ends with fetlock joint extension. Complete transection of one branch of the SDFT in the pastern may not alter the stance during full load bearing. Administration of phenylbutazone for pain may eliminate lameness, and a gait abnormality may become hard to detect. The DDFT and SL support the fetlock joint together with the SDFT. Therefore slight hyperextension of the fetlock because of disruption of the SDFT may be difficult to detect unless the contralateral limb is picked up. The greater the number of structures transected, the less support to the fetlock and other distal joints and the greater the likelihood of vessel and nerve transection. Elevation of the toe is pathognomonic for transection of the DDFT.
Digital Palpation of the Wound
Digital palpation is a simple and direct way to determine the extent of damage to structures below the skin. Integrity of the tendons is readily determined by feel. Partial tears can be distinguished from complete tears, and this affects treatment (see Partial Tendon Lacerations section). The tendon ends are often palpable beneath the skin proximal and distal to the wound, but they may be removed from the wound if the injury was sustained while the horse was galloping. The muscular attachment to the proximal end pulls the proximal tendon end farther from the wound. The wound should be clipped around the edges and cleansed thoroughly with a dilute antiseptic solution such as chlorhexidine before exploration. Gross debris can be debrided manually from the wound. Sterile gloves should be worn for the digital exploration after the wound is clean. Digital palpation may reveal involvement of a tendon sheath or joint capsule; however, small tears of these synovial structures may not be palpable. Sterile preparation of the skin and injection of a balanced electrolyte solution into the synovial structure in question at a site distant from the wound may demonstrate communication if solution exits the wound. Synovial fluid also can be obtained and submitted for cytological evaluation. Hemorrhage or inflammation is usually present in the synovial fluid if a sheath has been penetrated. Mild inflammatory changes can be seen in synovial structures adjacent to tendon injuries, even if no actual communication with the wound occurs.
Ultrasonographic Evaluation
Ultrasonographic evaluation of the tendons can quantitate the degree of tendon damage, particularly in horses with partial tears. Ultrasonographic examination is not necessary for diagnosing complete tears and therefore is performed rarely. Ultrasonography may also be technically difficult in the region of a skin wound because air in the wound impairs transmission of ultrasound waves. A partial laceration of the SDFT may be associated with the development of longitudinal splits extending proximodistally as a result of altered shear stresses. Complete transection of a branch of the SDFT in the pastern region may result in a shift of position of the branch proximal to the transection toward the side of the intact branch.
Ultrasonographic evaluation can be useful during the healing phases of horses with partial or complete tendon lacerations.3 The amount of repair tissue should increase early in repair and then decrease as the tissue matures and gains strength. In digital flexor tendons, about 6 weeks are required for the tendon to gain the strength to support 450 kg, and the strength of the repair tissue is largely because of an increase in tissue mass. The repair tissue cross-sectional area is greater than the original tendon area, but the strength of that tissue per unit area is reduced.4 The quality of the repair tissue can be monitored with ultrasonography. Ultrasonographic examinations should show progressively increased homogeneity of echogenicity, reduction in the hypoechoic areas of damaged tendon or early immature repair tissue, and appearance of parallel arrangements of fibers.
Emergency Management
Treatment of Shock
Trauma is often severe in horses with lacerated tendons, particularly digital flexor tendons. Some horses may be trapped for hours in wire or entangled in equipment. Blood loss may be extensive if major arteries to the distal limbs have been transected. The loss of the function of a limb is painful and stressful. Initial management of these horses can be lifesaving. If possible, the horse should be caught and brought into a warm, clean area for examination and further treatment. If the horse has severe tachycardia (>100 beats/min) with pale mucous membranes and is reluctant to move, initial treatment should be performed on site. If the wound is still bleeding, a clean pressure bandage should be applied to stop the bleeding and provide some support to the limb. If the function of the limb is impaired mechanically, a splint should be applied over the bandage to minimize further damage with movement. Use of tranquilizers and sedatives should be kept to a minimum until the degree of blood loss and shock can be assessed and treated. Most sedatives are peripheral vasodilators and may produce substantial hypotension in a hypovolemic horse. Some horses may be in stress-induced shock from pain, with extreme catecholamine release. The effect of tranquilizers may be unpredictable and potentially can worsen the bleeding. Securing the horse in a familiar, warm, clean environment and stabilizing the injured limb may resolve the stress-related shock and allow assessment of hemorrhagic shock by evaluating peripheral pulse strength and quality, heart rate, and mucous membrane color. If hemorrhagic shock is severe, the most important treatment is intravenous fluid volume replacement, which can be in the form of high-volume isotonic fluids (20 to 60 L minimum per 450 kg of horse) or hypertonic saline (9% NaCl; 1 L per 450 kg of horse), followed by isotonic fluid replacement. Hypertonic fluid therapy can be effective for rapid expansion of the vascular space in hemorrhagic shock, but hypertonic solutions dehydrate the interstitium and induce a profound renal diuresis. Therefore it is critical that isotonic fluid therapy begins within 30 minutes to 1 hour after hypertonic fluid administration. Hypertonic fluid therapy is practical because of the convenience of the small volumes necessary and works well if the horse is referred or transported to a facility that has access for fluid administration.
Transportation
For transportation the injured limb should be placed toward the back of a trailer. The horse’s weight shifts to the front of a trailer during braking, which is often less controlled than acceleration. The horse’s head should not be tied tightly, so the head and neck can be used for balance. The limb should be supported with a padded pressure bandage and a splint for transport.
Medical Management
All horses with tendon lacerations need medical therapy, whether surgery to reappose tendon ends is elected or not. If tendon laceration, partial or complete, is diagnosed, a more thorough aseptic preparation of the wound should be performed. These procedures require sedation, restraint, and local or regional analgesia.
Wound Cleansing and Debridement
The hair should be clipped circumferentially from above the wound (to the estimated top of the bandage) and the entire limb distal to the wound. Drainage of serum and exudate from the wound is often voluminous, and removal of the hair makes subsequent cleaning of the limb easier and more thorough, thereby minimizing bacterial growth and contamination. A 10-minute scrub of the wound with an antiseptic solution should be performed. If bone and tendon are exposed, care must be taken to minimize trauma to these tissues. A minor sterile instrument pack may be helpful in trimming heavily contaminated tissues and lacerated tendon ends, as well as for removing hair and debris from deep in the wound. Lacerated tendons should be trimmed at the edges to remove traumatized tissue that is expected to become necrotic. Debridement of tendon ends should be most conservative in horses with digital flexor tendon lacerations, for which apposition of tendon ends with suture is recommended.
Systemic and Local Medications
Tetanus toxoid should be administered to any horse with a tendon laceration, and tetanus antitoxin should be given if no vaccination history exists. Because all wounds are contaminated at injury and compound wounds have extensive soft tissue injury, broad-spectrum antimicrobial drugs should be administered systemically for a minimum of 3 days. Metronidazole should be considered in horses with grossly contaminated distal extremity wounds. The duration of antimicrobial therapy may be longer in horses with heavily contaminated wounds, wounds healing by second intention, infected wounds, wounds involving a tendon sheath, or wounds with delayed treatment (>24 hours). Wound lavage should be copious, usually with a minimum of 5 L of a balanced electrolyte solution.
Surgical Treatment
Surgery in the form of wound closure is performed in most horses with open wounds involving tendons. Primary closure is preferred, if possible, to provide the best success of obtaining primary wound healing, minimal scar formation, and the fewest complications associated with the transected tendon. However, wounds that are heavily contaminated, older than 24 hours, or heavily traumatized should have a delayed closure (1- to 3-day delay) performed to reduce the contamination and necrotic debris before closure. The decision to close a wound older than 24 hours must be made based on the condition of the wound and surrounding structures. Wounds in horses that have been managed appropriately from the time of injury until surgery can be closed at any time, if tissue loss is minimal and infection is not present.
Extensor Tendons
Transected extensor tendons heal well without primary suturing of the tendon, even if a large gap has formed between the tendon ends. Serial ultrasonographic evaluations show fibrosis occurring between the tendon ends that eventually becomes more organized and regains the linear arrangement of collagen along the pattern of the original tendon. This fibrous tissue seems to provide a mechanical link between the tendon ends because extensor function of the digit returns in most horses. In our experience, a palpable thinning of the new tendon and an enlargement at the old tendon ends usually remains, even after 1 year.
Horses with lacerated extensor tendons have a good prognosis, with 73% of injured horses returning to athletic soundness and 18% to pasture soundness.2 In that study, 62% of the affected horses were treated with a three-layer cotton bandage, 23% with a splint and bandage, and 10% with fiberglass casts.
It is important that the horse is confined to box rest for at least 6 weeks so that lameness does not ensue. With lameness the hoof may be positioned on the toe, and the force of the digital flexor tendons maintains this position, particularly without the counterforce of the extensor tendon. Chronic flexor pull may result in permanent flexural deformity and lameness. If flexor dominance is noted, a splint or cast should be applied (see Chapter 86).
In our experience, the best cosmetic outcome, as well as chances of achieving primary wound closure, occurs with using a fiberglass cast for 3 to 6 weeks. The cast provides the most immobility to the limb and the lacerated tendon ends. Early fibrosis matures more quickly, without disruption of the early granulation tissue.
Digital Flexor Tendons
Horses with complete laceration of one or more digital flexor tendons are best treated with tendon suturing, wound closure, and postoperative immobilization for about 6 weeks. Digital flexor tendons support the weight of the horse on loading. Thus healing and return to full strength is a slow process, one that does not return to normal for at least 6 months. In studies investigating methods of tendon repair, immobilization of the limb in a cast without suturing produced a significantly weaker repair that resulted in the clinical sequela of a hyperextended fetlock joint.4,5 The amount of scar tissue filling the tendon gap was significantly less in this group compared with the sutured groups and was the reason for the reduced strength. Therefore suturing of digital flexor tendon injuries is recommended. Monofilament suture (nylon or polyglyconate) produced the greatest strength of repair compared with carbon fiber suture when placed in a double-locking loop pattern (nylon) or three-loop pulley pattern (polyglyconate) for apposition of tendon ends or for spanning tendon gaps.4-6 The limb should be cast for at least 6 weeks, with the fetlock joint in mild flexion, by building a heel support with casting tape or plaster to provide a level weight-bearing surface with the ground.
Repairs of flexor tendon lacerations above the hock (i.e., gastrocnemius tendon, DDFT, or SDFT) should follow the same principles, but the prognosis is decreased because of the greater difficulty in maintaining a full-limb cast, larger size of the tendons at this location, and greater biomechanical stresses to support the hock with weight bearing.
Partial Tendon Lacerations
Horses with partially transected tendons can be treated successfully without suturing but with wound closure and limb immobilization. Partial transection of digital flexor tendons usually involves the SDFT only or the axial margin (medial or lateral) of the SDFT and DDFT. If the limb is immobilized, the remaining fibers of tendon provide the stability for the torn tendon ends to remain in apposition and provide the strength to prevent further tendon tearing during healing. Anecdotally, if more than 75% of the SDFT is lacerated, tendon suturing may provide a reduced gap and faster healing and improve the repair. If the SDFT is completely transected along with a partial laceration of the DDFT, the SDFT should be treated with suturing as previously described and the DDFT left unsutured.
Lacerations in Tendon Sheaths
If a laceration enters a tendon sheath, then therapy is altered to include aggressive lavage of the sheath and wound, intrathecal administration of antibiotics, close monitoring of sheath fluid cytological condition, longer use of systemic antibiotics, and limb immobilization. If tissue loss is minimal, wounds entering tendon sheaths should be closed primarily. Primary closure and fiberglass cast application offer the best chance of early healing and minimize the potential for the complications of ascending infection, chronic drainage and fistulae formation, and fibrosis.
Convalescent Therapy
Shoeing
After removal of a cast or splint for horses with extensor tendon lacerations, a gradual return to full weight bearing is recommended. Shoeing recommendations are simple and include trimming or shoeing level, without toe extensions that may catch and produce knuckling. For horses with digital flexor tendon lacerations, an elevated and extended heel shoe can be applied and the heel lowered sequentially over the next 6 weeks to a flat position. For severe lacerations involving the DDFT, SDFT, or SL, an extended heel shoe may always be required for additional flexor support.7
Graduated Exercise
Horses with extensor tendon injuries have not been evaluated as closely during the healing process to assess tissue maturation and return of strength as those with digital flexor tendon injuries. Because the function of the extensor tendon is to extend the digit and not endure a load on weight bearing, return to full strength may occur sooner than for digital flexor tendons. Horses should remain in a box stall or a confined area during the wound healing phases and early fibroblastic repair phases of tendon healing (3 to 6 weeks). After this time, handwalking and controlled exercise such as swimming can begin to strengthen the tendon and improve gliding function. After 10 to 12 weeks of controlled exercise, and if no signs of knuckling or flexor dominance are present, gradual return to athletic use can begin.
Horses with digital flexor tendon lacerations require a more gradual convalescent period. After the first 6 weeks of immobilization, the next 6 weeks should be spent in confinement and regaining a normal foot posture and full weight bearing. Heel support shoes are applied during this time. After 12 weeks, handwalking can begin and gradually increase in frequency and duration over the next 3 to 6 weeks. Controlled exercise with walking, lunging, swimming, or ponying (leading from another horse) is preferred to turnout. Turnout can be given after the horse is sound at the walk and trot and ultrasonographic examination demonstrates extensive fibrosis and mature scar tissue. Heavy athletic use should not begin until 8 to 12 months after the injury.
Prognosis
Successful outcome (soundness) occurs in about 75% of horses with extensor tendon lacerations and up to 54% of horses with digital flexor tendon lacerations.1,2,8 The prognosis for horses with partial disruption of the SDFT, DDFT, or both is better than for those with complete lacerations.8 Long-term failures are attributable to continued pain from extensive adhesions, joint pain, other injury at the time of laceration, tendon sheath adhesions, tendon contracture, palmar (plantar) annular ligament constriction, reinjury, and failure of the repair to regain adequate strength to support the joint, leading to breakdown. Reinjury to a damaged tendon may occur during healing, but such a tendon can heal successfully, although convalescence is prolonged. In general the prognosis is better for pleasure riding horses than for sports horses, but especially with injuries involving the digital flexor tendons of a hindlimb, complete function may be restored. An association exists between lacerations of either or both the long and lateral digital extensor tendons in the proximal part of the metatarsal region and the subsequent development of stringhalt several months later.9