Chapter 95Osteopathic Treatment of the Axial Skeleton of the Horse
Osteopathy originated in the United States with a Kansas physician, Andrew Taylor Still. He envisaged a system of healing that placed emphasis on the structural integrity of the body as being vital to the well-being of the organism. As knowledge of physiology and anatomy advanced, a concept evolved of the nervous system as an information network constantly changing and adapting in response to sensory information from the body and the environment. This knowledge allows a move away from the idea of pathological dysfunction as the only cause of illness to a concept of physiological (or somatic) dysfunction.1 To use a computer analogy, the body may suffer from software failure (physiological malfunction) and hardware failure (pathological malfunction). To extend the analogy, osteopathy may be thought of as a form of reprogramming.
Chiropractic treatment evolved at around the same time as osteopathy and is similar but subtly different. The differences are largely philosophical; both forms of treatment rely on mobilization of joints. Chiropractors in equine practice tend to look primarily for positional changes associated with skeletal dysfunction. Treatment is directed principally at restoring joint mobility, with manipulation directed to the local site of dysfunction.
The osteopathic approach considers local tissue dysfunction as the direct result of trauma or the breakdown of compensatory mechanisms consequent to past trauma. The diagnostic approach is based on identifying patterns of dysfunction, with minimal reliance on positional factors and emphasis on the interactions of the entire spine. Treatment is aimed not only at restoring local function but also at identifying and removing factors that predispose to acute relapse. Therefore treatment frequently involves tissues distant to the perceived area of local dysfunction.
Neurophysiological Basis of Osteopathy
It is not uncommon in clinical practice to encounter horses that exhibit musculoskeletal signs for which no pathological cause can be established. The osteopathic philosophy accommodates these horses with the concept of somatic dysfunction. This concept is fundamental to osteopathy and describes a disturbance in the neurological networks that affects the function of the body (software failure). In other words, somewhere in the course of entering information from the environment and body, processing the information in the central nervous system, and then generating a motor response, something has gone wrong. Clinically this presents as a horse with signs such as stiffness, loss of performance, poor coordination, or gait abnormality for which no pathological process can be identified. Osteopathic treatment is directed at changing the signals to the neural network to modify the way sensory information is processed and thus to correct the motor response generated in the central nervous system.
To explore this concept, it is necessary to appreciate aspects of neurological activity not only under normal circumstances and as part of the protective response to injury, but also when long-term and inappropriate changes occur that adversely affect function of the body.
Normal Neurophysiology
In a normal horse, sensory and motor systems work together to achieve optimum function.
Sensory Component
The peripheral sensory system has two categories of neurons that provide information to the central nervous system. The division is made based on fiber size. The fast, low-threshold large fibers carry the sensation of touch and proprioception, and the high-threshold small fiber system (C and Aδ fibers) conveys potentially painful nociceptive and temperature modalities. In the spinal cord, these neurons synapse on interneurons where the first stage in information processing occurs. How the signals from the periphery are modified and sent onward to cortical areas for interpretation relies in part on the balance between large fiber input and small fiber nociceptor activity. This balance forms the basis of the pain gate theory where small fiber input, which may potentially be decoded as pain, can be held in check by large fiber activity. Under normal circumstances, much of the nociceptive input is screened out at the spinal cord level and never progresses to register as a painful sensation.
The sensory information will initiate and/or modify activity of the motor system.
Motor Component
The basic motor pattern is one of mutual inhibition of flexor and extensor neurons,2 providing a balance between agonist and antagonist muscles. To refine the movements, proprioceptive information is sent constantly from muscle spindles and joint receptors back to the spinal cord. As sensory nerves enter the spinal cord, they send off sprays of ascending and descending collateral fibers, which synapse on interneurons that have connections within the spinal cord segment, with other spinal segments up and down the cord, and with tract cells up to the brainstem. The result is a network of neurons processing information from the body and environment. These generate flexible patterns of motor activity (sometimes referred to as central pattern generators [CPGs]). Thus a pattern of nerve activity is generated where the primary function is to move a limb, but simultaneously vital secondary functions are engendered—for example, changing the tone in the central musculature to counteract the changing load on the axial skeleton.
CPGs can cause many different routine patterns by virtue of the number and variety of interconnections, whose characteristics are determined by cellular and synaptic connections of the neurons. These patterns develop over time by a process of repetition and learning. Thus the inconsistent swing of a learner golfer becomes a confident, automatic swing after many hours of repetitive practice. This involves a process of chemical changes within a neuron and new synaptic connections with other neurons, which speed up or “fast track” a particular response and result in a consistent and reproducible pattern of motor activity.
Response to Injury
In response to injury, a number of events occur, which involve not only the sensory and motor pathways but also the autonomic system. A painful stimulus is conveyed from the periphery along small caliber nociceptors to the spinal cord. If the stimulus is of sufficient intensity, it will pass on to the brain to register pain. It will stimulate motor neurons in the ventral horn, resulting in paravertebral and peripheral muscle spasm,3 and stimulate sympathetic activity in the lateral horn, causing reduced blood flow to the skin.4 These neurophysiological changes represent a protective response against further injury and will, in the short term, affect the function of the body.
Once these defensive measures are activated, a control mechanism exists at the level of the spinal cord to modify this activity to prevent constant discomfort. Mediated by the large fiber system input of discriminatory touch and proprioception and by descending inhibitory cortical activity, the pain gate can be closed to painful stimuli. This can be demonstrated by rubbing an injured area to ease pain. It is the balance between large and small fiber stimulation and higher center input that determines the activity of the interneurons and therefore sensory, motor, and autonomic responses.
In the short term, these responses are protective. If they persist, however, changes occur in the activity of the neuronal network that results in altered pain states and impaired function.
Altered Neurophysiology
It is tempting to consider the reactions of the neurons to injury as hard wired, with a certain level of stimulus giving a corresponding magnitude of response. In fact, these neuronal networks are plastic, and the sensitivity of neurons to stimuli can be altered at any point in the pathway. In some circumstances, this process of sensitization or facilitation, as it is sometimes called, can be useful, for example, patterns of motor neuron firing during the acquisition of a new skill. However, when pain circuits are involved, a lower firing threshold may result in neurophysiological changes that affect function of the body long after the original injury has resolved. This is the basis of the somatic dysfunction concept that encompasses distortion in sensory, motor, and autonomic activity in the absence of any obvious pathology.
Sensory Effects
A lowered threshold for firing may occur at any point in the sensory system extending from peripheral receptors through to the spinal cord and brain. In response to injury, nociceptor nerve endings produce neurochemicals such as substance P.5 Combined with other inflammatory mediators such as prostaglandins and serotonin, the firing threshold is lowered, and the intensity at which the nociceptors will fire is increased. This local sensitization is generally responsive to treatment with antiinflammatory medication.
If nociceptor activity is intense or prolonged, changes can occur in the chemistry and structure of the interneurons of the spinal cord.6 These can be traced 3 to 7 days after only 45 minutes of moderate nociceptive stimulation.7 These changes lower the threshold for interneuron firing in a process called facilitation or “wind-up.” They become supersensitive to afferent input and internal network activity within the spinal cord and will activate a pain circuit at an inappropriately low level of nociceptive input. This is the mechanism underlying hyperesthesia.
A further stage in this central sensitization of interneuron pools is the development of allodynia, where even an innocuous stimulus such as a light touch results in a pain response. The clinical manifestation may be a “cold-backed” horse or one with sensitivity around the poll. Furthermore, the central pain pathways may be driven without any peripheral input at all. In experiments when afferent activity was blocked by sectioning the dorsal (sensory) root, a sensation of pain accompanied by autonomic and motor responses may still be present, driven by the output of the sensitized interneurons. This means that pain persists long after the original injury has resolved. Even when pain is no longer felt, the neuronal pool remains sensitive, and relatively low levels of nociceptive activity will produce a pain response inappropriate to the magnitude of the stimulus. This may account for horses with recurrent injuries that occur with minimal physical provocation.
Another characteristic of central sensitization is the development of antidromic activity in the sensory nerves. Although under normal circumstances a sensory neuron is stimulated at the periphery and transmits a signal back toward the spinal cord, it is in fact capable of firing from the center outward to the receptor, in what is termed the dorsal root reflex.8 On reaching the periphery, depolarization of the nerve endings has the same effect as depolarization as a result of a noxious stimulus from an injury. Proinflammatory neurochemicals are released from the nerve into the surrounding area and trigger an inflammatory cascade. This centrally driven inflammatory response may explain those cases of intermittent limb swellings and dysfunction for which no pathological cause can be identified.6
Alongside the deleterious effects of persistent sensory changes, there are motor and autonomic effects that will affect neuromusculoskeletal function.
Motor Effects
Part of the response to injury is contraction of muscle, which protects the area from further harm. In the short term, this is a helpful emergency measure. However, persistent muscular changes are not desirable. There are a number of biomechanical, neurophysiological, and biochemical consequences arising from a muscle that remains in a contracted state.
From a biomechanical perspective, muscle spasm causes asymmetry of and restriction in joint movement. This not only has a local effect but also causes adaptation of movement by other parts to accommodate this loss of function. These distant sites may themselves become symptomatic in the long term.
On a neurophysiological level, persistent contraction reduces joint movement and results in length changes in muscle fibers. This diminishes the amount of large fiber input from muscle spindles and joint receptors into central interneuron pools and shifts the balance in favor of small fiber nociceptor activity and stimulation of pain circuits.
The other consequence of reducing information from proprioceptors is that it impairs the ability of the central processing centers to map the position of the body in space. This is of particular importance in the cranial cervical spine, where the greatest concentration of proprioceptors is found9 and which is a vulnerable area when a horse falls. Joint stiffness and muscle contraction in this area following an injury will alter feedback from this level. This affects the ability of motor pattern generators throughout the spinal cord to modify activity in response to alterations in body position and may produce changes ranging from subtle gait disorders to ataxia. Clinically there may be no obvious signs, but it will affect the horse’s potential and leave it more susceptible to acute injury.
Biochemical effects of muscle spasm influence factors that regulate the number of sarcomeres, which are the building blocks of muscle mass. Although stimulation of muscle by motor neurons is an important ingredient in muscle development, another clinically significant factor is stretch of the muscle fibers.10 Stretch results in the production of a substance referred to as mechano–growth factor, which stimulates development of muscle mass. Lack of movement through an area may be responsible for the loss of topline and underdeveloped quarters often seen in a stiff horse.
Autonomic Effects
Alongside the sensory and motor effects that are characteristic in somatic dysfunction, altered autonomic patterns are also generated.
Thermography can be useful to detect this aspect of somatic dysfunction. In a “normal” horse, a reproducible thermographic pattern is observed, reflecting cutaneous blood flow.11 Where facilitated segments exist, sympathetic activity in the lateral horn reduces surface blood flow, giving distinctive segmental cooling. In addition to local segmental changes, the pattern may be disrupted throughout the length of the spine, giving a visual record of changes in autonomic nerve output.10
Clinical Implications for Altered Neurophysiology
These mechanisms may explain some of the nonspecific lameness and back pain that tend to be recurrent. A diagnosis based on pathological condition of tissue (demonstrated by radiographic and scintigraphic examinations or by diagnostic analgesia) is not possible because the abnormality results from physiological changes in the motor, sensory, and autonomic patterns generated by the facilitated neuronal segment. Gait disturbance may be observed, and muscle spasm, joint stiffness, and tissue texture changes may be appreciated by palpation and passive motion testing.
Effects of Osteopathic Treatment
The concept of somatic dysfunction means that if an injury is treated exclusively at the periphery but central sensitization has occurred, then treatment may be ineffective or the benefits may be short lived.
On a neurophysiological level, osteopathy seeks to reduce this central sensitization of the facilitated segment by increasing large fiber signaling into the central nervous system. This shifts the balance of input away from small fiber nociceptive traffic, thereby closing the pain gate and inhibiting pain circuits. This has the effect not only of reducing discomfort but also of increasing movement, improving proprioception, encouraging muscle development, and promoting nutrition to the musculoskeletal system.
In practical terms, most techniques are directed toward restoring movement to stiff joints to optimize maintenance of postural position and functioning of the body. Local musculature is relaxed and mobility improved, which is associated with an increase of mechanoreceptor activity carried by the large fiber system into the interneuron pool. The treatment may take a number of forms, including soft tissue techniques, articulatory techniques, and mobilization and functional techniques.
Soft tissue and articulatory techniques stretch the skin, fascia, and muscles to improve pliability of and nutrition to the periarticular tissues and also to allow the joints to move in a full range. These techniques include massage and repetitive flexion and extension of restricted joints.
Mobilization techniques involve taking a joint with poor mobility to the point of maximum resistance (the restrictive barrier) and pushing through this barrier with a short-amplitude, high-velocity thrust. This causes relaxation of the muscles and improved mobility resulting from a sudden increase in large fiber input from mechanoreceptor activity, which resets the balance of inputs into the spinal cord and reduces central sensitization.
A successful approach in horses with long-standing, complex injuries is the use of functional techniques. This uses the concepts of ease and bind. A normal joint reaches a point (usually at the middle of its range of movement) where tension on the capsular ligaments and the overlying muscles is minimal. This is the point of ease, where a joint tends to rest naturally. Any movement away from the point increases tension or bind. This information is used by the central nervous system to monitor joint position and to generate an appropriate pattern of motor activity. Where the normal relationships between the joint structures have been disturbed, this point of ease is offset, and afferent information from that joint is changed. New reference points become imposed on the established networks, and the joint is less able to perform appropriately or to coordinate movement with other joints.
This new abnormal point of ease may be detected clinically by testing each range of movement (flexion/extension, side bending, rotation, translocation, and traction/compression). With the joint held in the position of ease, tension is minimal, and therefore afferent input into the spinal cord is minimal. This appears to reduce conflicting information entering the network and allows the old pattern to reassert itself. The old pattern is preferred by the system because over time neuronal connections have been created that fire more readily to generate this original learned response. This form of treatment relies on the osteopath establishing and maintaining one or, more commonly, several joints at the point of ease until the original central pattern generators can reassert influence over the newly acquired patterns. This is a learned skill on the part of the osteopath and requires considerable tactile sensitivity and skill to adjust the tissues as the neurological patterns are modified. Among injured horses is a clinically challenging subgroup of 4- to 6-year-old horses that develop clinical signs as work becomes more demanding, rather than as a response to direct trauma. In these horses, it is tempting to conjecture that some form of perinatal injury may have occurred that has prevented the normal patterns from developing. These horses frequently undergo more treatment and require more careful rehabilitation than other horses.
Details of osteopathic techniques are beyond the scope of this chapter, but the reader is referred to an excellent textbook.11
Diagnosis and Case Selection for Osteopathic Treatment
Diagnosis should involve selection of horses with a somatic dysfunction and exclusion of horses with a pathological condition. Initially a conventional veterinary lameness examination should be performed. If the examination indicates a change in quality of movement rather than lameness, or if lameness is centered in the axial skeleton and no pathological process can be demonstrated readily (e.g., by radiological or scintigraphic evaluation), then the likelihood of a somatic dysfunction as the cause of lameness should be considered. Somatic dysfunction alters the way a horse moves and so may contribute to pathological change (e.g., synovitis in an overloaded joint). Once a primary pathological condition has been excluded, the process of making an osteopathic diagnosis can proceed. This diagnosis is based on somatic dysfunction, that is, how the component parts of the horse work together as a whole and how different areas of dysfunction or stiffness may contribute toward the problem.
An accurate case history is essential and should include the type of work the horse is expected to do and the level it is expected to attain. The history also highlights past injuries and illnesses and may reveal idiosyncrasies in behavior or movement that, although noticed by the owner, have not interfered with performance sufficiently to be a cause for concern. When considering the history, these subtle disturbances in motor function may, in retrospect, have been early signs of the coming crisis.
Examination begins by assessing muscle development and distribution of weight through all limbs in the standing horse. The horse should stand naturally with all cannon bones vertical and not shift weight constantly between limbs. Muscle development should be symmetrical, and the areas of muscle should be consistently developed throughout the horse. Areas of poor development over the top of the back, neck, or quarters should be noted. Similarly, uneven development or hypertrophy may be substantial. In particular, hypertrophy of the pectoral muscles may indicate that forward propulsion of the horse depends unduly on the forelimbs because of poor hindlimb function. Hypertrophy of the muscle over the atlas and axis frequently accompanies restricted joint movement at this level. Foot placement, shape, and shoe wear are also important for locating areas of dysfunction. When assessing feet, however, it is necessary to differentiate between change caused by altered limb movement and problems caused by poor farriery.
Movement at a walk is more revealing than at the trot, when the horse tends to fix the neck and back to guard against pain. Observation gives an impression of how the horse moves as a whole and indicates which areas are functioning poorly. Balance and fluidity of movement from head to tail are as important as stride length, foot placement, and frank lameness. How the horse copes with long and short turns indicates problems with lateral flexibility. In particular, when the horse is turned short, the head and neck should flex evenly in the direction of the turn, and the hindlimbs should be crossed as the quarters move around. All limbs should be moved with easy flowing strides, showing consistent stride length and straight limb flight. The feet should be placed easily, and in particular the hind feet should not dig into the ground when placed. Limb movement that appears heavy, stiff, inconsistent, or mechanical should alert the observer to potential problems. Excessive head and neck movement in time with the limbs is also abnormal. Substantial lateral movement of the pelvis, often associated with patches of worn hair under the back of the saddle, indicates reduced movement in the lumbosacral spine. The pelvis and tail being carried to one side also indicates uneven tone in the spinal musculature. Uneven height between the tubera coxae also should alert the clinician to potential problems.
The transition from walk to trot can be revealing, and any tendency to raise the head or skip in the transition indicates problems, probably in the region of the cervicothoracic junction. Assessing individual joint movements is useful, but it requires considerable skill and powers of observation. Running the hands down the paravertebral muscles from the occiput to the tail may reveal areas of muscle hypertrophy or spasm, and most importantly tissue texture can be felt. Moving the joints through the relevant ranges of motion identifies those that are stiff.
Diagnosis requires consideration of past injuries, the way the horse moves overall, and identification of dysfunction in specific areas. Initially, the clinician may only be able to form a working hypothesis, which will be refined once treatment begins. Where problems have been present for some time, the horse will have developed altered patterns of posture and movement to work around poorly functioning areas. These alterations may occur at several levels because of the interconnections of the neural networks. Ascertaining what is the site of the primary injury and what are secondary changes may be difficult.
Infrared Thermographic Imaging
Thermographic examination in the horse has proved to be an invaluable tool to confirm somatic dysfunction.12 It is important to realize that areas of cooling are more important in diagnosing sympathetic dystonia than are increased temperatures. Thermography is prone to artifactual results, and interpretation can be reliable only if image acquisition is carried out in a temperature-controlled environment (between 18 and 22° C) using an absolutely consistent technique.
The horse must be clean and dry because moisture absorbs infrared radiation and causes false readings. Hair length should be consistent because hair has an insulating effect, and horses that have clipped coats or rubs from rugs present difficulties in interpretation. Different coat colors may be of different hair length or density, which causes artifacts. When moulting, areas of different colored hair may moult at different times, again giving rise to artifactual results. Before performing a thermographic examination, horses should be acclimatized to the room temperature for as long as it takes for the surface temperature to remain stable. The time required depends on the difference in ambient temperature of the environments inside and outside the thermography room. The room should be free of drafts and direct sunlight.
In a normal horse, a reproducible thermographic pattern is observed, reflecting cutaneous blood flow.13 Where facilitated segments exist, sympathetic activity in the lateral horn reduces surface blood flow, giving distinctive segmental cooling. In addition to local changes, the pattern may be disrupted throughout the length of the spine, giving a visual record of changes in autonomic nerve output. Certain specific injuries give areas of increased blood flow and an increase in surface temperature. These injuries are usually around the head or in the lower limbs, where little or no overlying muscle is present.
In a normal horse, the surface temperature should be within 1.5° C over the neck and body of the horse and in the limbs proximal to the carpus and tarsus. The head and lower limbs are generally cooler. A useful guide when setting the thermographic factors is to assume the eye will be the hottest normal area and to set up the camera with this as the maximum temperature. Changes of 5 to 6° C are severe, so a temperature range of about 6° C is ideal. If the horse has parts of the coat clipped, then changes in the level of the window may be required to accommodate the clipped areas of the body. Particularly important is a dorsal view of the back, where a relatively warm dorsal midline stripe is seen, with the muscle on either side symmetrical and between 0.5 and 1° C cooler. When interpreting thermographs of the neck and back, changes of less than 1° C from the normal may be discounted. Changes in excess of 1° C usually indicate sympathetic dystonia, the importance of which must be interpreted in the light of information regarding clinical signs seen and the use to which the horse is put. It is likely that horses frequently suffer low-grade back pain or stiffness, which may not be of particular clinical significance if they live relatively sedentary or gymnastically undemanding existences (e.g., a racehorse or hunter performs satisfactorily with minor changes in the cranial aspect of the neck or thoracolumbar spine, which would cause unacceptable stiffness or gait modification in an event or dressage horse).
Figure 95-1, A to C (Color Plate 5), shows the thermographic appearance of a completely normal horse. One should bear in mind that few horses meet this degree of perfection, but they may still perform adequately at the required use. The most common area of the spine to show joint stiffness is the cranial aspect of the neck, with changes to the occipitoatlantal and atlantoaxial joints. This group of injuries results in a cold band running obliquely ventrally in the neck from about the level of the occiput (Figure 95-2; Color Plate 6). This band becomes narrower with time, and although a substantial temperature change is visible in the acute stage, over an initial period (probably about 2 years), the temperature change becomes less noticeable. Stiffness or injury farther caudal in the neck is accompanied by cooling of the surface temperature overlying the affected area (Figure 95-3; Color Plate 7). Because the nerve supply to the muscles of the shoulder arises from the caudal aspect of the neck, injuries to the spine between the shoulders are difficult to see thermographically, but a cold band running vertically down the back of the shoulder region (Figure 95-4, A; Color Plate 8, A), usually accompanied by cooling of the entire thoracic area and hindquarters, is an indicator of injury to the cervicothoracic area. Cooling of the hindquarters arising caudal to a diagonal band from the level of about the twelfth thoracic vertebra generally indicates injury at this level of the thoracic spine (Figure 95-4, B; Color Plate 8, B). Two other changes are of particular clinical significance. Any break in the normal dorsal stripe running along the midline of the back or substantial cooling on either side of this stripe indicates a change in sympathetic activity in that region (Figure 95-5; Color Plate 9). Second, cooling of the distal aspect of a limb may be clinically significant. If the ambient temperature decreases below about 15° C, normal physiological changes reduce blood flow in the distal aspect of the limbs to conserve body temperature. This causes cooling of the distal aspect of the limbs (distal to the carpus or tarsus, unilaterally or bilaterally), but such limbs should still show a surface temperature 5 to 6° C cooler than the trunk temperature. If severe injury has occurred at the base of the neck or in the lumbar region, then the temperature of the distal aspect of the limb may decrease to equal the ambient temperature. More detailed analysis of the thermographic changes seen is beyond the scope of this chapter.
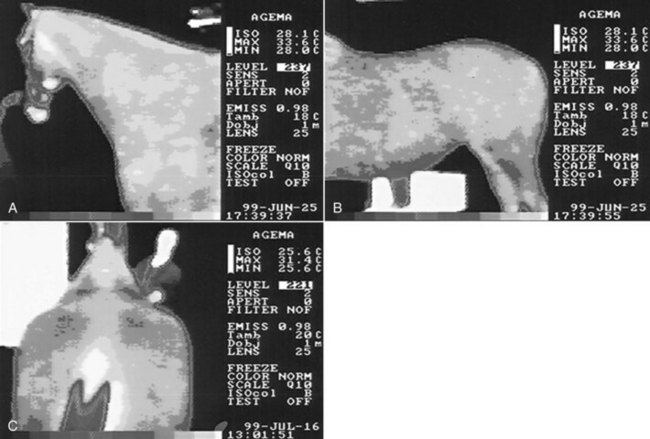
Fig. 95-1 Thermographs show the appearance of normal horses. The color scale represents 5.6° C using 10 colors; that is, each color represents about a 0.5° C change in temperature. The color bar under the image shows the colors used; those to the right side are the hottest, and those to the left are the coldest. White is above the top of the scale, and black is below the scale. A, Lateral image of the head, neck, and shoulder. B, Lateral image of the thorax, abdomen, and hindquarters. C, Oblique dorsal image from behind the horse looking toward its head and neck. Temperature variation is 1° C over the neck, trunk, and hindquarters. A warm midline dorsal stripe along the back extends from the withers to the base of the tail, with symmetrical muscle temperature on either side.

Fig. 95-2 Lateral image of the neck of horse with reduced mobility in the occipitoatlantal and atlantoaxial joints. A cool line runs obliquely from the region of the atlantoaxial joint caudally to the base of the neck and is 1.5° C cooler than the surrounding muscle, indicating an area of sympathetic dystonia.
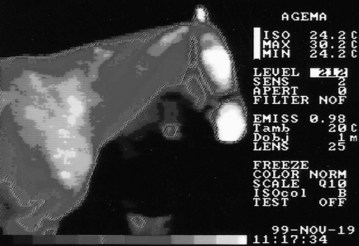
Fig. 95-3 Lateral image of the neck of horse with reduced mobility in the neck. There is clinically significant cooling from the occiput caudally to the level of the sixth and seventh cervical vertebrae, indicating a problem involving all joints in the neck.

Fig. 95-4 Lateral images of the thoracolumbar area of two horses, both showing substantial cooling in the musculature of the dorsal spine from the saddle region caudally. A, The vertical cranial boundary to the zone of cooling indicates that the injured area is in the region of the cervicothoracic junction, but the shoulder muscles overlying this area receive innervation from the lower neck, partly masking the muscles supplied by the upper thoracic area. B, The typical appearance of cooling in the muscle resulting from an injury to the region of the twelfth thoracic vertebra, with the cranial border of the region running obliquely ventrally and caudally. This horse has been clipped, but long hair left on the hindlimb produces an area 5° C cooler than the surface temperature of the thorax of the horse.

Fig. 95-5 Dorsal image of horse showing abnormal temperature patterns of the thoracolumbar spine. Note the complete loss of the normal central stripe, with substantial cooling indicating the presence of reduced mobility of the entire thoracolumbar spine and pelvis. The asymmetrical nature of the temperature pattern indicates the horse is likely to move with an asymmetrical gait, resulting from increased muscle tone on the left side of the body.
Treatment
Because of the vast number of interneural connections and the ramification of effects on the spinal cord, the entire spine must be considered as one interrelated structure, and treatment may have to be provided at several levels. Sedating the horse is useful because treatment requires identification of specific areas of stiffness or reduced movement. If the horse is sedated adequately, then the absence of conscious movement allows the osteopath to feel underlying deficiencies more easily. Sedation is particularly helpful when using functional techniques that monitor subtle changes in joint position. Osteopaths in the United Kingdom undergo a 4-year university course that includes considerable theory and practical training. The techniques used require considerable practical experience to be successful; therefore this chapter can only begin to outline treatment.
After the osteopath performs the static and moving examinations described earlier, he or she starts a physical examination, feeling the tone and physical character of the muscles and the extent of movement of the joints, usually starting at the head and working along the neck and back to the tail. It is necessary to try to determine which joints show restricted movement, which areas show abnormalities caused by primary injury, and which changes are secondary to the primary affected areas. Experience allows the osteopath to determine which area must be treated first. The areas showing somatic dysfunction tend to be interrelated and must be treated in a specific order if treatment is to be successful. Starting treatment on an area showing restricted movement secondary to another abnormal area is doomed to failure. However, treatment of a key area often results in dramatic relaxation throughout the spine. The basic techniques of treatment have already been outlined and rely on stimulating the activity of the large caliber fibers, thereby inhibiting the interneuron pool and blocking the small fiber (pain) signals. The results are effective in most horses, and once the neural activity returns to normal, the horse tends to maintain this state.
In a small number of horses the problem may be so ingrained and widespread that general anesthesia may be needed to facilitate assessment and treatment. The plane of anesthesia is light, and the horses are in good health; thus the risks of the procedure are minimal. Assessment of individual joint complexes can be made throughout the spine with the horse under general anesthesia. It is remarkable how often gross dysfunction of these complexes can be detected with the horse anesthetized, when they had previously been effectively concealed by the capacity of the body to set up compensatory mechanisms. Treatment is still based on the principles outlined above, but the horse is positioned on its back, allowing movements such as rotation of the thoracolumbar spine, which cannot be achieved in a standing horse. Using all limbs simultaneously is also possible, allowing functional techniques (outlined previously) to produce a massive large fiber input to the interneuron pool. This is done by moving each limb to its position of ease, and then holding the position until relaxation is felt. By moving the limbs to maintain the positions of ease, the sympathetic dystonia can be unwound gradually. This technique, used with the horse under general anesthesia, allows a potent but gentle treatment to be carried out. In a standing, conscious horse, techniques are necessarily limited and are most effective with relatively short-term injuries.
Results of Treatment
Pusey et al14 reported on a trial carried out over 4 years, treating horses with chronic dysfunction using osteopathic techniques. Eighty percent of treated horses returned to the previous use, performing at the same or a better level than before treatment, at least 12 months after the last treatment. As might be expected, the authors concluded that results were substantially better among the later horses because of increasing experience of treatment techniques.
Another study was made of horses that had been treated under general anesthesia, having failed to respond satisfactorily to treatment under sedation. Follow-up information was obtained at least 1 year after the treatment was finished. Thirty-five horses were treated. Twenty-four (71%) of these had maintained improvement and returned to the previous level of work: 11 at the previous level and 13 at a higher level than previously. Eight (24%) horses did not respond to treatment, and two horses deteriorated. One horse was not available for follow-up evaluation. The authors concluded that given that these horses had long-term intractable problems, this was a justifiable and useful treatment technique.
We hope this brief overview shows the potential for osteopathy in a complementary role, alongside veterinary science, in treating neuromusculoskeletal problems in the horse.