Chapter 115Lameness in the Show Hunter and Show Jumper
Historical Perspective
Show jumping and related competitions have origins in hunting sport and military tradition. The show hunter, most popular in North America, has evolved from the traditions of fox and stag hunting. These horses were expected to provide fast, safe, and athletic passage for the rider, and considerable pride was taken in being well mounted and having the horse admired. Today in the show ring these horses are judged for beauty, athletic ability, manners, and way of going. Jumping style is important and must be coupled with consistent performance.
Some competitions encourage the development of a young horse to a higher level of training, others award a mature horse for outstanding performance, and others separate amateur and professional riders. Horses often are selected based on suitability for a particular division of competition.
The modern show jumper has many of its origins with military traditions. Many cavalry officers were by necessity highly skilled and accomplished horsemen. Thus when the era of the modern Olympics began, the equestrian competitors were military men. With the mechanization of the military and the replacement of the cavalry with motorized transport, the private sector became more involved in Olympic show jumping. Many of the early civilian competitors were retired military men. Show jumping has become increasingly more popular, and many talented riders have emerged on the national and international scenes. Since the 1960s many women have entered this sport, once dominated by men.
Structure of the Sport
Show jumping combines athletic effort of the horse and rider. The scoring process is objective, with the winner jumping the course with the fewest rails knocked down and, in the jump off, in the fastest time. Heights of fences range from 1 m at novice level to 1.7 m for advanced competitions. The course should be completed within an allowed time, and some competitions are considered as speed classes in which jumping and time faults are combined. As the jumps get bigger, the potential for injury increases, and many conditions develop from repetitive strain. Many of the fences are set at distances to each other so that the horse must adjust stride length to fit in the appropriate number of strides. A good horse must have explosive power and great athleticism, combined with carefulness—a desire not to hit fences. Contrary to many equine sports, similar numbers of mares and geldings or stallions compete (Figure 115-1).

Fig. 115-1 A Grand Prix show jumper jumping a large oxer at Spruce Meadows, Calgary, Canada, a venue with one of the most lucrative prize structures worldwide. Note the symmetrical position of each of the forelimbs and hindlimbs. Asymmetry may reflect an underlying pain-related problem. The horse is jumping squarely across the fence; jumping obliquely may reflect hindlimb pain and uneven propulsion.
Some older horses compete at levels of competition lower than they have reached to be schoolmasters for less experienced riders. These older horses may experience unique problems related to age and use. Today show jumping is a highly diverse and competitive sport enjoyed all over the world from beginner level to the level of the Olympic Games. At the top level the sport is entirely professional, with horses changing hands for huge prices and with large amounts of prize money available, putting pressure on the veterinarian to keep horses sound. Competition continues throughout the year, with outdoor shows during the summer months and indoor shows during the winter, so horses potentially get few breaks.
Characteristics of the Jumping Sports Horse
Many breeds are capable of show jumping and related activities and include Thoroughbreds (TBs), European Warmbloods, TB-Warmblood crosses, and American Quarter Horses and related crosses. The European Warmbloods most often are represented by the Hanoverian, Holsteiner, Trakehner, Dutch Warmblood, Selle Français, Swedish Warmblood, and Irish crossbred breeds. Breeding in continental Europe has become highly specialized and has developed in part through financial support from state governments. Most modern day top-level show jumpers are naturally well-balanced, good-moving athletes. Various pony breeds, such as the Welsh crosses, are used for children (see Chapter 126).
Current preferences are for lighter and taller horses, with moderate muscling. This body type is associated with greater speed and agility, which are assets to a modern show jumper. This body type also benefits hunters because these horses have graceful movement, with good extension and natural balance. Larger horses, if not excessively heavy, are at an advantage for show jumping because of greater stride length and overall strength and power. The TB long has been preferred by American trainers for the hunter ring; however, in recent years Warmblood breeds have gained favor because of a calmer nature and better manners.
Horses often start competing at 4 years of age, reach peak ability at 9 to 12 years of age, and may continue to compete until 18 to 20 years of age.
Training
Training of the hunter and jumper emphasizes using the hindquarters for engagement and collection, which places more weight and stress on the hindlimbs as they are brought forward and under the rider during locomotion. Such a posture is somewhat unnatural for the horse, whose normal inclination is to distribute weight over the forehand. These stresses may contribute to or accelerate the development of problems of the thoracolumbar and pelvic regions, and ligaments and joints of the hindlimbs. Early in the training of a young horse, lameness often reflects musculotendonous problems and relates to lack of adaptation to work.
When training over fences begins, new loads on the hindlimbs occur that place more stress on soft tissues and joints. Stresses on the forelimbs also are increased because they are involved in takeoff and landing. The forelimbs are involved in setting up the jump and aiding in the directional change from horizontal to vertical. On landing the forelimbs receive considerable impact loads and absorb the entire weight of the horse. Increased load places more stress on the foot, distal limb joints, and the soft tissues of the forelimbs.
Horses must learn to adjust stride length by shortening or lengthening the stride, to jump from a line perpendicular to a fence or at an angle, to turn quickly, to change leading legs in canter, and to jump from variable speeds of approach. Unwillingness to change leads or always favoring one lead when landing after a fence may indicate a problem (see Chapter 97). Much of the basic flat work training is similar to dressage.
Many lameness conditions encountered early in a horse’s training begin as subtle performance-limiting problems, progress relatively slowly, and may disappear with further conditioning. However, excessive training leads to the development of important problems such as chronic muscle soreness, fatigue, joint inflammation, and behavioral changes. Slow, steady work with a gradual buildup in exercise intensity and duration results in fewer joint and soft tissue problems later.
Training and Competition Surfaces
Training, warm-up, and competition surfaces play a substantial role in the development of lameness in a jumper. Soft, deep footing requires much more effort by the horse and is responsible for early fatigue of muscles, tendons, and ligaments. Injuries include gluteal muscle strain and spasm, suspensory desmitis, desmitis of the accessory ligament of the deep digital flexor tendon (ALDDFT), and superficial digital flexor (SDF) tendonitis as well as inflammation of or trauma to any of the soft tissue structures in the hoof, pastern, and metacarpal and metatarsal regions. Sandy soils contribute to the development of hoof wall problems. Hard surfaces may result in bone- and joint-related injuries, as well as distal limb and foot problems such as subsolar bruising, distal interphalangeal (DIP) joint synovitis, and osteoarthritis (OA) of the proximal interphalangeal (PIP) and DIP joints.
Formerly most high level outdoor competitions in Europe took place on grass, but there is an increasing trend for some of the higher-level competitions to take place on all-weather surfaces. The nature of the footing depends highly on the weather and can vary extremely. To enhance traction, screw-in studs often are used in the front and hind shoes. Studs may be used in the medial and lateral branches of the shoe or just the lateral branch to reduce risk of interference injuries. If studs are used in only one branch of the shoe, this immediately creates mediolateral imbalance and the potential for abnormal torque. Studs also alter the dorsopalmar balance, especially if the ground is firm. Horses that flex the carpi excessively during jumping may have to wear a girth guard to protect the sternal region from self-inflicted injuries. If a horse is jumping on firm going, studs concentrate the forces of impact and can predispose the horse to deep-seated bruising of the foot. There is a tendency in horses with poor-quality horn for the hoof wall to break in the region where studs are placed. In some circumstances studs may halt the normal slide of a foot on landing and thereby predispose to injury.
Excessive work, such as long period of lunging a hunter to calm it down, prolonged competitive efforts, and long show schedules of repeated competitions play a role in the development of many injuries in hunters and jumpers.
Conformation and Lameness
Conformational abnormalities of the foot predispose horses to lameness. An underrun heel, long toe, and a broken hoof-pastern axis frequently contribute to palmar foot pain and DIP joint synovitis. Horses with improper medial-to-lateral hoof balance may develop a sheared heel, crushed bar, and chronic foot pain. Base-wide or base-narrow forelimb conformation may contribute to injuries to the suspensory ligament (SL), its branches, and the distal sesamoidean ligaments.
Toe-in or toe-out forelimb conformation may predispose horses to PIP and metacarpophalangeal joint problems. Short, more upright pasterns predispose horses to navicular disease and DIP joint and PIP joint synovitis or OA. These horses are often straight through the shoulder as well and lack the stride and extension necessary for jumping. Long, more sloping pasterns sometimes are associated with sesamoiditis and soft tissue injuries to the distal aspect of the limb.
Over-at-the-knee conformation may predispose horses to SL strain and should be avoided in selecting a jumper. Offset-knee conformation predisposes a jumper to medial splint problems. However, attention always should be paid to subclinical contralateral hindlimb lameness in a mature horse that develops an acutely painful medial splint bone. Subtle angular limb deformities are rarely a problem, provided proper attention is paid to shoeing and hoof balance.
Extremely sickle-hocked conformation is associated with weak hindlimbs and places more stress on the plantar tarsal soft tissues and the centrodistal and tarsometatarsal joints. A straighter hock is actually more desirable, but an overly straight hock may predispose to SL strain and distal hock joint pain, especially in association with an extended fetlock and long pastern conformation.
Horses that are extremely straight through the stifle are poor jumping prospects and have a high incidence of instability and upward fixation of the patella. A more angular stifle gives the horse a longer, more powerful stride and is thought to provide more strength for jumping.
A long, sloping hip and croup are desirable characteristics in a jumping horse, providing strength and power. Horses with a flat croup often suffer from thoracolumbar and sacroiliac pain. Asymmetry of the tubera sacrale and tubera coxae can be seen in the absence of lameness and may reflect previous trauma. An experienced rider usually can manage these horses.
Horses with excessively base-wide or base-narrow hindlimb conformation place abnormal stress on the feet and joints. Base-wide horses may have an increased incidence of hock problems, whereas base-narrow horses may have more stifle problems.
Shoeing Considerations
Many lameness problems are a direct result of improper trimming and shoeing. Neglected feet are frequently a source of lameness, and a poorly shod foot also may contribute to lameness by forcing the horse to transfer abnormal and excessive stresses to other parts of the limb or to other limbs. Many of the Warmblood breeds have relatively tall, narrow upright feet, which are predisposed to the development of thrush and sheared heels. Others have wide flat feet that can be carelessly shod into a broken back hoof-pastern axis with an underrun heel and abnormal orientation of the distal phalanx. Studs in the shoes may create foot imbalance and may increase the severity of interference injuries. A good cooperative relationship with an experienced farrier is an essential element in lameness prevention and management. This can be a problem for top-level competition horses that are constantly moving from show to show and are being trimmed and reshod by different people with varying ability. The time of shoeing relative to the day of competition is important because trimming may alter biomechanical forces. To avoid increased stresses on the soft tissue structures within the hoof capsule, it is suggested that the horse be shod within a maximum of 4 weeks from competition. In Europe we consider 7 to 15 days to be the optimum interval between shoeing and competition (PHB, SJD).
Lameness Examination
Before a horse is examined because of a suspected lameness problem, several factors should be considered. If the horse is currently competing, will any diagnostic tests or treatment have an effect on the horse’s ability to continue competition? Knowledge of the competition rules and drug use guidelines are essential. Has the horse recently competed? Has a change in exercise intensity or duration been made? Does the horse have a new trainer? When was the horse last shod? If the horse has been competing away from home, it is important to determine if another veterinary surgeon already has examined and treated the horse, and if so with what.
The lameness examination should begin as the horse is walked from the stall or paddock to the examination room or area, because movements such as a small circle to reverse its direction may offer clues as to which limb or limbs may be affected. It is not uncommon for there to be concurrent lameness in more than one limb. Careful observation and palpation of the joints of each limb as well as the neck and back are performed while the horse is held quietly. Passive flexion tests and evaluation of the lateral movements of the head, neck, and back are performed.
A dynamic examination should be performed beginning with an observation of the horse at the walk in a straight line, in small circles, and in a figure eight. The horse should next be examined at the trot in hand on a firm, level surface. Lunging on firm footing in small circles in both directions should be performed, as this often exacerbates subtle lameness, especially if involving the foot.
It is sometimes necessary to see the horse ridden to determine which limb is lame. The rider may also be asked to change the diagonal at the trot and figure eight to increase the load on a specific limb when it is on either the inside or the outside of the circle.
Examinations performed after strenuous exercise or after competition may be useful; more subtle lameness may then be more obvious. It should also be noted and recommended that the veterinarian observe the “way” or “style” the horse trains and jumps. Defects in the horse’s position and way of jumping that would have otherwise gone unnoticed may be observed during a routine physical or lameness examination. Watching videos of the horse may also allow the practitioner to see abnormalities of the horse’s balance or gaits when in motion. Knowing what is “normal” may also help the practitioner detect early or subtle changes in movement before an obvious lameness is manifest.
Proximal and distal limb flexion tests should be performed on all limbs. The method and duration of flexion are a matter of personal preference but should be consistent and interpreted with care, bearing in mind that joints and soft tissue structures may be stressed simultaneously. It has become common practice for top-level competition horses to be examined periodically throughout the year to try to detect early warning signs of impending problems. A positive response to flexion is often followed by treating the stressed joint(s). The true value of this practice is difficult to determine objectively.
Once the lame limb(s) has been identified, the limb is carefully reexamined. Hoof tester response should also be assessed. An obvious source of pain may be identified, but perineural or intraarticular analgesia often is required to localize the source(s) of pain. Results are sometimes confusing and always should be related to the clinical examination.
Aseptic preparation is essential for intrasynovial injections to minimize the risk of infection. Two authors (RPB, CBM) also administer gentamicin intravenously before entering any synovial space. The conditions of the work area and the temperament of the horse being examined influence which analgesic technique to use. Intrasynovial analgesia may be delayed or not performed if no clean, dry place is available for safe injection. Although intraarticular analgesia is considered to be more specific than perineural analgesia, it may influence periarticular pain. In some instances regional or intraarticular analgesia may not be safely performed without first tranquilizing the horse. This may interfere with the lameness examination, especially if the lameness is low grade. Lameness is reassessed after the effects of sedation have worn off. Alternatively the horse is sedated, the suspected joint is treated with the appropriate drug(s), and the horse is reevaluated in a few days. The treatment is therefore substituted for intraarticular analgesia. In situations in which subtle lameness makes interpretation of nerve blocks difficult, in those horses with multiple-limb lameness, in horses that are difficult or dangerous, or when comprehensive blocking fails to localize the lameness, other techniques such as nuclear scintigraphy should be considered.
When horses are competing regularly, especially away from home, owners, riders, trainers, and peers often put pressure on the veterinarian to treat the horse based on an index of clinical suspicion rather than on a complete lameness evaluation including local analgesia. Although this can be successful and a positive response to treatment clearly indicates a correct diagnosis, one must bear in mind that some injuries do require rest for the best long-term outcome. A merely transient response to treatment or a lack of response warrants further investigation of the lameness, and this routinely should include local analgesic techniques.
Imaging Considerations
Only after successfully localizing the source of pain causing lameness or after an extensive physical examination has provided the veterinarian with a reasonable indication of the problem should the examination progress to diagnostic imaging, including radiography, ultrasonography, and, if indicated, nuclear scintigraphy, computed tomography, or magnetic resonance imaging (MRI). Routine techniques are used, with no special images. High-quality diagnostic imaging is related directly to the veterinarian’s success as a diagnostician. The routine use of both ultrasonography and radiography is strongly encouraged, as soft tissue structures are commonly involved in injuries of the bone and joints. The complete extent of the injury may be identified; the presence of a soft tissue component may influence both the treatment options and the prognosis. Frequent ultrasonographic examinations make a practitioner more confident in correctly recognizing an abnormality.
Failure to Make a Diagnosis
Every veterinarian, no matter how astute as a lameness diagnostician, eventually will be confused or unsure or simply have no idea as to why a particular horse is lame, and consultation with associates or referral to other experts should be considered. Just as a good relationship with a farrier is paramount to the successful management of many foot-related problems, good relationships with other veterinarians are necessary and may be helpful when one is faced with a difficult or confusing lameness. The veterinarian must be honest and open about the horse with the owners and trainers; inclusion of other professionals in the case or referral for advanced imaging may ultimately lead to both an accurate diagnosis and enhancement of the veterinarian’s relationship with the client if handled well. Reexamination at a later date also may be beneficial. Some bone lesions may take a few weeks to become visible radiologically, so the veterinarian should consider reimaging if the pain causing lameness has been localized to a specific area.
The use of many medications for a “shotgun” approach to treatment may be a veterinarian’s only hope when all diagnostic methods are either unrewarding or not available and if previously attempted “trial therapies” have failed. Such medications include but are not limited to nonsteroidal antiinflammatory drugs (NSAIDs), doxycycline, tiludronate, intramuscular polysulfated glycosaminoglycans (PSGAGs), intravenous hyaluronan, and oral nutraceuticals.
Treatment
In recent years the trend has been toward much more aggressive treatment, with many different treatment modalities often being combined to manage a single condition. Although in some circumstances this can be justified, it does mean that the veterinarian is often not sure which treatment really is effective. More targeted treatment based on a precise diagnosis actually may be equally effective. A thorough understanding of the overall “pain map” of the horse can lead to a confident approach to treatments even in the absence of objective data from the lameness examination. The pain map essentially represents the postulated sites of pain causing poor performance based on an assessment of a detailed history of performance; the results of palpation including the response to stimulation of acupuncture points; evaluation of the horse moving in hand, on the lunge, and ridden, both when work is first initiated and later in the work program; and the response to flexion tests and chiropractic assessment of joint mobility, sometimes combined with assessment of the response to local analgesic techniques (TRO).
Ten Most Common Lameness Problems of Show Hunters and Show Jumpers
Many of these problems are interrelated, and more than one problem may occur simultaneously. We have attempted to list these in relative order of frequency; however, this is not intended to imply that one is more serious than another.
Diagnosis and Management of Common Causes of Lameness
Foot Pain
Foot Soreness
The most common site of forelimb lameness and overall lameness in a hunter or jumper is the foot. The horse naturally supports 60% to 65% of its body weight over the forelimbs, and impact forces during jumping dramatically increase load and structural stresses in tissues within the hoof capsule. This may be exacerbated by training regimens that do not focus on improving strength from behind and therefore the overall balance of the horse.
The manner in which a horse is shod has tremendous importance in the development of hoof- and foot-related problems. A long toe and underrun heel are common hoof conformational defects and frequently contribute to heel pain because of hoof wall separation or bruising in the heel, quarter, and bar areas. The heel itself may be excessively long and collapsed inward, and the horse actually may be bearing weight on the outer wall. This often results in sensitivity to hoof tester pressure applied to each heel bulb and when the heel bulbs are squeezed together. A flattened and chronically bruised heel and bar area (corns) may be seen after removal of the shoe.
Lameness is often improved by analgesia of the palmar digital nerves. Lateromedial radiographic images of the foot may reveal that the distal phalanx is abnormally oriented, in extreme situations so that the palmarmost aspect of the bone is lower (more distal) than the toe (so-called “negative palmar angle”). The so-called “negative palmar angle” appears to occur more commonly in the United States than in Europe. The solar margins of the distal phalanges may be irregular. In horses with chronic lameness, deep digital flexor (DDF) tendonitis and distal sesamoidean impar desmitis may contribute to pain associated with an underrun heel. However, these soft tissue injuries have been documented using MRI in show jumpers with both poor and good foot conformation (SJD).
Some horses with underrun heels and poor angulation of the distal phalanges do not respond well to shoeing. Removing the shoes, trimming back the abnormal heel wall, and placing the foot in a support bandage are recommended. One author’s (RPB) preference is to fashion a cushion support for the palmar aspect of the hoof using a two-part putty elastomer material (EDSS, Equine Distal Support System, Penrose, Colorado, United States). Using the sulci of the frog for support is believed to suspend the heel and promote the new growth to be more vertical in its orientation. This process, however, requires a long-term commitment by the owner and trainer, because new heel growth may take up to 6 months to be sufficient for the reapplication of shoes. One author floats the heel using a  rim pad and either a heart bar shoe or a pour-in pad in an effort to keep the horses in work and competition (CBM).
rim pad and either a heart bar shoe or a pour-in pad in an effort to keep the horses in work and competition (CBM).
Attention should be paid to the role of training and overall management of the horse, specifically as it relates to hindlimb strength and comfort.
Subsolar Bruising
Horses with subsolar bruising often respond well initially to Epsom salt poultices or cooked linseed hoof packs and NSAIDs (e.g., phenylbutazone) followed by corrective shoeing. Rasping excessive toe from the solar surface proximally up the dorsal wall to create a 45-degree angle with the ground surface and application of a shoe fitted full at the heel may be of benefit by removing resistance to breakover. Ideal breakover is located between two points; the first is located by extending a line distally along the dorsal surface of the distal phalanx to the bearing surface, and the other by drawing a perpendicular line from the dorsal distal aspect of the distal phalanx to the bearing surface. Egg bar shoes may be required to gain adequate heel support. Shoes such as the EDSS natural balance shoe (Equine Digital Support System), with the web behind and squared off at the toe, also improve breakover and reduce stress in the palmar portion of the foot. We do not recommend the long-term application of plastic wedge pads or egg bar shoes because they actually may contribute to further crushing of the heel and promote the heel bulbs to slide forward and grow horizontally. Leather pads may be helpful in some horses if sole pain is present and sole protection is desired. In horses with a chronic problem, long-term use of aspirin (60 g once daily or 20 g bid for 5 days) may be helpful. Hoof growth supplements containing biotin and methionine also may be of benefit, and we recommend feeding of biotin (100 mg to 1 g for 3 to 12 months, either alone or combined with zinc, cysteine, and dl-methionine daily) to promote hoof wall growth. Careful attention should be paid to the condition of the gastric mucosa with long-term NSAID use in show horses, because gastric ulceration may occur or worsen. Concurrent administration of acid pump inhibitors such as omeprazole should be considered.
Extreme sensitivity to hoof testers may be evident along the periphery of the sole at the level of the distal phalanx. Such pain may be associated with bruising, solar margin fractures, laminar inflammation or inflammation of the distal phalanx caused by chronic concussion from hard ground, or excessive sole pressure from the shoe. These conditions may be more common in North America (with its harder and dryer footing) than in Europe. Radiology is necessary for diagnosis of solar margin fractures of the distal phalanx. Shoeing should be directed at reducing local pressure on the affected areas and improving the overall hoof balance. Egg bar shoes and rim pads are often effective, but soft sole pours that provide extra cushion and shock absorption also help. Two-part putty elastomer is thought to benefit by providing support and lift from the sulci of the frog. Care should be taken with a pour or putty elastomer to avoid overfilling, causing excessive sole pressure.
Subsolar Abscess
Subsolar abscesses occur commonly and result from shoe nails improperly applied, poor environmental conditions, a shoe moving slightly, and poor hoof structure. Onset of clinical signs may be rapid, such as immediately after a show, or may occur within the first several days after shoeing. The additional trauma of jumping exacerbates the condition, leading the rider or trainer to suspect trauma or serious injury. Warmth in the hoof wall, increased digital pulse amplitudes, and focal, extreme sensitivity to hoof tester application are usually diagnostic, provided that the hoof horn is not excessively hard. Perineural analgesia is rarely necessary to confirm the suspected diagnosis and also may be confusing, because not all horses respond positively. After blocking and trotting the horse to reassess lameness, reexamination of the solar surface of the foot may reveal purulent drainage from the area of suspicion. Treatment is directed toward liberal opening of the solar surface of the foot at the point of maximum sensitivity to establish adequate drainage. If drainage is not established, bandaging the foot with hyperosmotic agents such as products containing magnesium sulfate (Epsom salts) is recommended. Twice daily soaking of the foot with a hot, supersaturated solution of Epsom salts with the bandage left on is also recommended for 3 to 5 days. Once drainage has been established, the foot is bandaged in a similar fashion, and NSAIDs also may be administered to reduce the inflammation. Antibiotics rarely are indicated but are sometimes used if soft tissue swelling occurs above the coronary band.
Navicular Disease
Navicular disease may initially be misdiagnosed as inflammation of the DIP joint. It is also likely that navicular disease is overdiagnosed in horses with simple heel pain. The diagnosis of navicular disease carries the stigma of a permanent and disabling lameness and is upsetting to the horse owner and trainer. Therefore the veterinarian should make an exhaustive effort to rule out all other possible sources for the pain causing lameness before making the diagnosis.
Lameness in horses with navicular disease usually is characterized by a slow, insidious onset. Early signs include shortening of the stride length, tripping, toe stabbing, and an intermittent unilateral lameness, although the lameness is almost always bilateral. Show horses are often more lame the day after a competition. Some horses with no previous lameness history become suddenly lame and are often refractory to standard therapies. Recent experience using MRI suggests that a proportion of horses that were previously thought to have navicular disease have primary lesions of the deep digital flexor tendon (DDFT) within the hoof capsule (SJD). Some horses with navicular disease also have an acute-onset unilateral lameness. The response to hoof testers varies, and often the horse shows only resentment when the heel bulbs are squeezed together. The wedge test may accentuate lameness; however, a positive response is not pathognomonic for the disease. Lameness may be increased after distal limb flexion, but the response is nonspecific. Lameness is almost always eliminated by palmar digital nerve blocks, and a previously undetected lameness often appears in the contralateral limb. Analgesia of the DIP joint or the navicular bursa often improves or abolishes the lameness.
Interpretation of the radiological appearance of the navicular bone is not easy; many horses with navicular bone pain have no detectable radiological abnormality. Radiolucent cystlike lesions in the body of the bone, large lollypop-shaped radiolucent areas on the distal border of the bone, increased thickness of the flexor cortex, and enthesophyte formation on the proximal and distal borders of the bone should be considered clinically significant.
Nuclear scintigraphy may be useful in horses that appear normal radiologically. The solar image is most useful and may reveal increased radiopharmaceutical uptake (IRU) in the navicular bone, reflecting abnormal bone metabolism. Lateral pool phase images may also be useful for highlighting horses that may have DDF tendonitis within the hoof capsule.
Ultrasonographic examination of the navicular bone and its associated soft tissue structures through the window of the frog may be useful, especially if MRI is not an option. It potentially allows assessment of the palmar aspect of the navicular bone, and the DDFT and the distal sesamoidean impar ligament and the insertions on the distal phalanx. MRI is useful for the diagnosis of various forms of navicular disease, identifying bone abnormalities not visible radiologically (Figure 115-2) and associated soft tissue injuries.

Fig. 115-2 Transverse T1-weighted gradient echo magnetic resonance image of a foot. Medial is to the left. There is increased signal intensity in the flexor cortex of the navicular bone medial to the sagittal ridge (arrow), dorsal to which signal intensity in the spongiosa is also increased, bounded dorsally by a rim of reduced signal intensity. There is dorsal irregularity of the deep digital flexor tendon in the same sagittal plane as the navicular bone defect (arrowhead).
Therapy for navicular disease includes pain management and corrective shoeing. Clients should be advised that this disease rarely is cured and requires a long-term commitment to its management. Horses with chronic, refractory lameness may require neurectomy.
Trimming and shoeing should be directed toward facilitating breakover, providing support to the palmar aspect of the foot, and in some horses elevating the heel to reduce tension in the DDFT. A full fitted egg bar shoe with a rockered toe or the EDSS natural balance shoe may be useful. The forward edge of the shoe should be set back from the toe and the branches fitted full at the heel. Leather wedge pads have been used to elevate the heel; however, the foot should be monitored closely to prevent crushing of the heel. A commercially available aluminum wedge-shaped shoe also may be used to provide heel elevation. It should also be noted that horses with palmar foot pain associated with injury to the DDFT often demonstrate improvement in lameness when shoes are removed.
Medical management includes the use of NSAIDs, isoxsuprine, pentoxifylline, tiludronate, and aspirin; intraarticular injection of the DIP joint and intrathecal injection of the navicular bursa with corticosteroids and hyaluronan; and rest. Many of these therapies, usually in combination, have proved successful in short-term management of this condition, and we generally would recommend the least-invasive therapies first. The degenerative nature of this disease, however, ultimately usually results in the failure of any treatment, and palmar digital neurectomy may be considered. Surgical case selection is important, and consideration should be given to the overall condition of the horse and its level of performance. This procedure is not allowed for horses competing under Fédération Equestre Internationale (FEI) rules. Horses with evidence of DDF tendonitis and PIP or DIP joint OA are not considered good candidates because of the possibility of rupture of the DDFT or exacerbation of OA. Some horses may experience temporary pain relief from the application of a chemical nerve block using a mixture of corticosteroids, ammonium sulfate, and Sarapin locally injected at the level of the palmar digital nerves. This procedure may work well initially, only to gradually lose its effectiveness.
Shock wave therapy recently has been introduced as a noninvasive therapeutic option for pain management in horses with navicular disease. Several investigators have reported good results, but differences in equipment and protocols require further investigation. Positive results may be short-lived.
Sheared Heel
Sheared heel can be a serious problem in hunters and jumpers. Lameness is often insidious in onset, or a critical point of instability may be reached, producing a more acute lameness. Subtle conformational abnormalities and poor hoof balance likely contribute to this condition. The medial heel bulb often is displaced proximally, with the remainder of the foot splayed laterally. When viewed from the solar surface of the foot, the lateral half of the foot is larger and flared compared with the medial half. The medial heel bulb may be painful to hoof testers, and the heel bulbs may be manipulated independently. Analgesia of the medial palmar digital nerve frequently improves lameness, but usually it is necessary to desensitize both heel bulbs before the horse appears sound. Many horses demonstrate radiological abnormalities of the medial palmar process of the distal phalanx, such as roughening or demineralization of the margin of the bone, presumably because of chronic trauma and inflammation. The therapeutic goal is to stabilize the heel bulbs and reduce pressure on the driven up or proximally displaced bulb. Stabilization most often is accomplished best by improving balance and breakover so that the foot lands flatly and relieving the affected heel from excessive loading during weight bearing. In a jumper an egg bar shoe with or without a pour-in pad to stabilize the heel is usually satisfactory. Horses with more severely affected feet may benefit from a heart bar, diagonal bar, or G-bar shoe. A rim pad with the portion to lie beneath the affected heel cut away may float the heel enough to allow that side to descend into a more normal position. Six to 9 months of persistent treatment are required before a more stable heel structure is established.
Distal Interphalangeal Joint Synovitis and Osteoarthritis
Inflammation of the DIP joint is common in jumping horses and usually results in subtle lameness that is frequently bilateral. Palpable joint effusion may or may not be present. Many horses, but not all, respond positively to a distal limb flexion test. Forelimbs are most commonly affected, but the hindlimbs also may be involved. The horse may have a reduction in stride length, and lameness is most obvious when the horse circles on firm footing. The rider or trainer may complain of a reduction in jumping performance, such as a reluctance to leave the ground and landing in a heap. Very hard surfaces for training or competition and surfaces that are too soft, irregular, and unstable may be predisposing factors. Soft footing, although not seemingly likely to contribute to excessive concussion, produces torsional forces on the DIP joint that strain the periarticular soft tissues. An underrun heel, long-toe conformation is probably the single most important contributing factor. The horse often shows a painful response to hoof testers with pressure applied from either heel to the opposite side of the frog and from the center of the frog to the dorsal hoof wall. Lameness usually is improved with analgesia of the palmar digital nerves and eliminated with palmar (abaxial sesamoid) nerve blocks or intraarticular analgesia of the DIP joint.
Radiological changes may be absent or subtle; however, in horses with more chronic or severe disease, active periosteal bone may be present on the dorsal aspect of the middle phalanx, and modeling of the extensor process of the distal phalanx may occur. With chronic, severe OA of the DIP joint there may be subchondral radiolucent areas in the distal phalanx consistent with collapse of the joint. Prominent radiolucent areas representing synovial invaginations may be present on the distal border of the navicular bone. Ultrasonographic examination of the collateral ligaments should be performed.
Nuclear scintigraphy is useful to rule out bone involvement. An area of IRU in the synovial structures of the joint may be visible in pool phase studies. Differentiating the palmar pouch of the DIP joint from the navicular bursa is difficult, and both structures may be involved in horses with severe lameness.
MRI has proven extremely useful in identifying abnormalities in and around the DIP joint including osseous trauma of the distal aspect of the middle phalanx (Figure 115-3). However, osseous trauma of the middle phalanx can occur alone, without DIP joint pain.
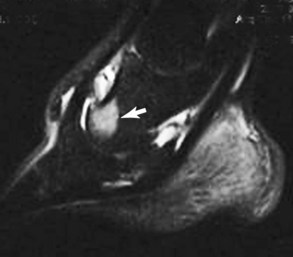
Fig. 115-3 Parasagittal fat suppressed short tau inversion recovery (STIR) magnetic resonance image of the phalanges. There is a well-demarcated region of increased signal intensity on the distal dorsal aspect of the middle phalanx (arrow), reflecting bone trauma. This was associated with reduced signal intensity in T1-weighted images.
Therapy for horses with DIP joint synovitis depends on the severity of the lameness and the horse’s competition schedule. Proper trimming and shoeing as for palmar foot pain with attention to the medial-to-lateral hoof balance is essential. The use of NSAIDs is common. Peripheral vasodilating agents such as isoxsuprine are of questionable value, although higher-than-standard doses appear to be clinically effective.
Intraarticular injection of high-molecular-weight hyaluronan and corticosteroids (triamcinolone acetonide or betamethasone) with proper shoeing and an appropriate amount of rest usually yields the best results. Occasionally, repeated injections are necessary after 4 to 6 weeks; however, injections repeated more frequently than once every 3 months should be avoided and should prompt a thorough review of the shoeing and hoof balance. Nutraceuticals and parenterally administered chondroprotective agents (PSGAGs) may be beneficial. Interleukin-1 receptor antagonist protein (IRAP) is helpful in managing recurrent inflammation in the DIP joint. A series of three or four injections given 7 to 10 days apart often is effective at relieving lameness associated with chronic synovitis.
Other primary sources of pain causing forelimb overload should be investigated.
Collateral Ligament Injury of the Distal Interphalangeal Joint
Some horses with synovitis of the DIP joint that are unresponsive to therapy should be evaluated for possible collateral ligament injury of the DIP and other anatomically related injuries. In a few horses, we (RDM, SJD) have identified enlargement and disruption of the infrastructure of the collateral ligament ultrasonographically, sometimes with focal IRU at the site of insertion on the distal phalanx, occasionally extending into the ipsilateral palmar process (SJD, RPB). MRI must be considered the gold standard for imaging structures in this area. Horses with collateral ligament injury should be managed with corrective shoeing and rest. Work level is reduced substantially. Extracorporeal shock wave or therapeutic ultrasound therapy combined with prolonged rest (at least 6 to 9 months) may be effective. Palmar digital neurectomy has been an effective management tool in horses failing to respond to conservative management (SJD).
Distal Hock Joint Pain
Distal hock joint pain is the second most common reason for lameness in a hunter or jumper and is the most common hindlimb lameness. Conformational defects, developmental abnormalities, and the incredible torsional stresses placed on the distal hock joints during jumping are thought to contribute to lameness. A variety of subtle signs becomes manifest before the onset of clinical lameness. Often the trainer or rider complains of a loss in the horse’s stride length, poor impulsion, and a change in the horse’s jumping style. Many horses may develop a tendency to switch leads in front of a jump or may have difficulty jumping from a particular lead. The horse consistently may develop the tendency to jump to one corner of the obstacle, and wider jumps appear to require more effort than usual or even necessary.
Clinical examination often reveals sensitivity to palpation of the muscles of the lumbar area and shortened cranial phase of the stride. The upper limb flexion test may reveal resentment of flexion and may or may not have a positive result. Some horses are reluctant to move forward immediately into a trot after flexion and may canter away from the veterinarian. Other horses may demonstrate an overall loss of balance after proximal limb flexion, manifesting as an induced forelimb lameness (TRO). The Churchill test often has a positive result in horses with tarsometatarsal (TMT) joint pain, but the result may be negative with centrodistal (CD) joint pain. Some horses with proximal suspensory desmitis (PSD) also respond positively to both proximal limb flexion and the Churchill test (RPB, RDM). Tarsocrural effusion may or may not be present. We (RPB, RDM) rarely perform regional perineural analgesia of the fibular and tibial nerves, because we consider the procedure difficult to interpret and somewhat dangerous to perform. Intraarticular analgesia of the CD and the TMT joints is preferred. However, a negative response to intraarticular analgesia does not preclude CD and TMT joint pain, and using fibular and tibial nerve blocks to identify some horses with distal hock joint pain may be essential. With practice this is a highly reliable and safe technique (SJD). With subtle hindlimb lameness or complaints of poor performance and no apparent lameness, it may be necessary for the horse to be ridden and for the rider to interpret the results of the block. The veterinarian should allow this with only the most experienced and talented riders.
Radiological changes vary from none to severe, with what may appear as total radiological evidence of joint fusion. Radiological changes do not necessarily correlate to the degree of lameness, but extensive radiolucent regions are often associated with moderate lameness. Osteochondral fragments on the cranial aspect of the intermediate ridge of the tibia, or at the distal aspect of the medial trochlea of the talus in a mature athlete in the absence of lameness, are usually an incidental finding of little if any clinical significance. However, fragments on the cranial aspect of the intermediate ridge of the tibia are occasionally associated with OA of the tarsocrural joint. The severity of the degenerative changes may be similar in the CD and the TMT joints; however, the TMT joint often has less severe abnormalities. The reason for this is unclear.
Nuclear scintigraphy can be helpful and reveals IRU in the distal aspect of the tarsus. Occasionally, small, focal, moderate-to-intense areas of IRU may reflect focal areas of loss of joint space, bone trauma, or tearing of interosseous ligamentous attachments.
It has been generally accepted that radiological evidence of distal joint(s) fusion is desirable, because the suggestion is that once joint fusion has occurred, the inflammation and therefore the pain should disappear. This is an unfortunate myth. Surgical arthrodesis is a currently accepted treatment for horses with OA of the CD or TMT joints that have become refractory to routine therapies. We challenge this belief and have observed evidence to the contrary. Once arthrodesis has occurred, the normal function of the joint is lost. The distal joints are responsible for the dissipation of the twisting or torsional forces and shear stress in that area. With this capability gone, these forces are concentrated, and stress fracture of the central or the third tarsal bones may occur or OA of the talocalcaneal-centroquartal (proximal intertarsal) joint may develop (RPB, SJD).
Treatment of horses with distal hock joint pain varies. Intraarticular injections of corticosteroids (20 to 40 mg methylprednisolone acetate, up to 10 mg triamcinolone acetonide, or 5 to 7.5 mg betamethasone in each joint) and hyaluronan (2 mL per joint) is usually the first treatment, combined with NSAIDs, and is usually the best and most expeditious means of treatment. With radiological evidence of severe OA we use a long-acting corticosteroid alone. Treating horses with more mildly affected joints with a low corticosteroid dose in combination with hyaluronan may be chondroprotective and extend the useful life span of the joint. Combined therapies have grown popular because of the perception that they work better and the effects last longer. Most horses respond favorably, and the riders comment on how much better the horse performs. Many horses, especially those with demanding show schedules, have the hocks (and perhaps other joints also) routinely injected at intervals predetermined by the history of when the horse previously became unsound after previous injections. Maintenance treatment is performed about 1 month earlier. This reduces the risks of loss of performance, recurrent lameness, or development of a secondary problem. However, we strongly advocate that horses should undergo periodic clinical reappraisal to determine the current cause or causes of suboptimal performance or lameness. Recurrent apparent hock pain should lead to investigation of other causes of lameness such as caudal back pain and PSD.
Many horses also are treated with oral nutraceuticals, parenterally administered PSGAGs, and intravenously administered hyaluronan. These products are incorporated into a maintenance program designed to keep the horse comfortable and prolong the interval between intraarticular joint injections. Frequently the large size of these horses means that they are treated with twice the normal dose of PSGAGs. Horses often are treated with intramuscularly administered PSGAGs and intravenously administered hyaluronan the evening before competition. Occasionally, horses with joints unresponsive to corticosteroids and hyaluronan do respond to intraarticularly administered PSGAGs, with or without corticosteroids. Once the horse has been made more comfortable, an exercise program consistent in intensity and duration, emphasizing strengthening the hindquarters and abdominal muscles, improves performance. Shock wave therapy has been effective in controlling the pain associated with severe OA of the distal tarsal joints. In addition, intravenous tiludronate has proven beneficial in some horses. Shoeing is aimed at encouraging breakover in the center of the hoof by squaring the toe. Alternative therapies such as muscle massage and acupuncture are used commonly with traditional therapies.
Suspensory Desmitis
Injury to the SL is the most common soft tissue injury and certainly one of the most serious injuries of jumping horses. Early lesions may go unnoticed by even the most skilled horseman, because the rider or trainer is aware of only a vague problem that the horse warms out of fairly quickly. With bilateral hindlimb injury the rider may complain of loss of power. Exercise continues, and the injury eventually worsens to the point of causing enough damage to produce obvious lameness. With forelimb injury the lameness usually is more pronounced when the horse is trotted in a circle with the affected limb on the outside and also may be exacerbated in soft footing. With hindlimb injury lameness may be worse with the lame(r) limb on either the inside or the outside of a circle. Midbody and branch lesions are diagnosed easily by palpation; however, diagnosis of PSD is more challenging. The distal limb flexion test may be resented and substantially increase the lameness in horses with midbody and branch lesions, whereas carpal flexion and upper hindlimb flexion frequently accentuate lameness associated with PSD, which can cause confusion with hock pain. Perhaps injuries to the distal aspect of the branches and at the insertion onto the proximal sesamoid bones (PSBs) may lead to fetlock joint instability. Careful examination of the distal aspect of the ipsilateral splint bone should be performed in horses with chronic desmitis of the branches or distal aspect of the body. A high palmar metacarpal nerve block, direct infiltration of the SL origin, or analgesia of the lateral palmar nerve eliminates lameness in the forelimb. Analgesia of the proximal aspect of the hindlimb SL requires caution, because injury to both the veterinarian and the horse can occur. Analgesia is best performed with the horse restrained with a twitch and the leg positioned in the veterinarian’s lap as if the horse’s foot were being examined. Displacing the digital flexor tendons medially and isolating the SL for injection is thus easier. The SL is infiltrated with local anesthetic solution from the axial aspect of the lateral splint bone, fanning across the SL from lateral to medial. During injection, the local anesthetic solution should go in with considerable resistance if it is being deposited within the SL itself. Another technique involves having an assistant hold the limb in a similar fashion and making an injection medially 1.5 cm distal to the chestnut along the axial margin of the DDFT in a dorsolateral direction. Depositing 3 to 6 mL of local anesthetic solution within the SL can then be accomplished, usually with little objection by the horse. Alternatively, perineural analgesia of the deep branch of the lateral plantar nerve can easily and safely be performed with the limb bearing weight (SJD). With direct infiltration of the ligament, soundness should be almost immediate. Some risk exists of entering the distal palmar outpouchings of the carpometacarpal joint capsule using direct infiltration in the forelimb, causing potential diagnostic confusion; however, infiltration in the hindlimb inadvertently entering the tarsometatarsal joint is less likely. With hindlimb injury there may be associated pain in the sacroiliac joint region.
Ultrasonographic examination of the SL may reveal obvious lesions; however, finding minimal evidence of damage in horses with acute injuries is not uncommon. Recent nerve blocks may confuse interpretation, so ultrasonographic examination is best delayed for 1 to 2 days. Alternatively, ultrasonographic examination may precede nerve blocks. In our opinion, ultrasonographic imaging of the proximal SL in the hindlimb is difficult. The transducer should be placed on the plantaromedial aspect of the limb to get the best-quality images A cross-sectional area of greater than 1.5 cm2 suggests PSD, even in the absence of a focal or diffuse loss of echogenicity. Comparison with the contralateral hindlimb is essential.
Radiographic examination of the proximal aspect of the third metacarpal bone (McIII) or third metatarsal bone (MtIII) may demonstrate increased radiopacity with or without radiolucent defects in a dorsopalmar (dorsoplantar) image or subcortical increased radiopacity in lateromedial images. Incidental radiological changes can be seen in hindlimbs, especially in older horses.
Nuclear scintigraphy has proved useful in characterization and prognosis of some horses with PSD. The pool phase occasionally reveals pooling of radiopharmaceutical in the ligament. A characteristic pattern of IRU is present in the forelimbs and hindlimbs in the bone phase. The lateral image is most important in the forelimb because focal IRU is present on the proximopalmar aspect of the McIII if bone injury accompanies PSD. PSD occurs often without chronic changes in the palmar or plantar cortex of the McIII or the MtIII. Dorsal images of the forelimb are less sensitive than lateral images because the limb is farther away from the gamma camera. In hindlimbs lateral and plantar images have similar sensitivity. The veterinarian should not mistake for a lesion IRU in the proximolateral aspect of the metatarsal region in plantar images, which is a normal finding. Ultrasonographic abnormalities of the SL and abnormal scintigraphic images confirm injury to the bone at the origin of the SL, indicating a complex injury involving two tissue types and adversely affecting the prognosis. IRU in the proximal aspect of the McIII or the MtIII in the absence of detectable ultrasonographic abnormalities may reflect primary osseous injury, which can be confirmed using MRI. MRI has also been useful in the diagnosis of PSD when the condition is not evident ultrasonographically and for identification of concurrent osseous pathology.
Medical therapy for horses with suspensory desmitis varies. NSAIDs combined with rest and physical therapy have historically been considered the only option, and clients were advised that treatment could take 6 to 12 months. We recommend stall rest for 10 to 14 days after the injury, with twice daily handwalks in an effort to cool the ligament down. Recently, new therapies (adult bone marrow–derived stem cells, growth factors, platelet-rich plasma [PRP], pigs’ urinary bladder matrix [A-Cell]) have become available and show early promise; however, long-term follow-up on a large number of horses is required. After the injection the limb is kept bandaged for at least 2 weeks. Phenylbutazone is administered (2 g bid for 4 days and then 1 g bid for 10 days) after the injection. Walking under saddle then is commenced for 20 to 30 minutes once or twice daily for the next 30 days. Follow-up ultrasonographic examinations are performed after 30 days and every 30 to 60 days thereafter. The duration and intensity of exercise gradually are increased based on the ultrasonographic appearance of the SL and the clinical appearance of the horse. Trotting begins once the horse is sound. Some veterinarians in North America recommend an internal blister, using 2% iodine in almond oil infiltrated into the SL. Light exercise is continued immediately after this therapy, with a gradual return to full work. Shoeing should be improved if necessary. In horses with acute PSD with no substantial ultrasonographic changes, local injection of corticosteroids may decrease inflammation and eliminate pain. We use triamcinolone acetonide (12 to 18 mg), betamethasone (30 mg), or isoflupredone acetate. Sarapin (4 mL) also may be added. If there is IRU in the McIII or the MtIII, there is anecdotal evidence that tiludronate may be effective.
Recently a surgical procedure has been reported in which the tight fascia overlying the proximal aspect of a hindlimb SL is transected in order to reduce pressure or in this apparent compartment syndrome. Bone marrow aspirate collected from the sternum then is injected into the area of the injury in an effort to stimulate healing. Early results from this technique appear promising; however, further investigation and long-term follow-up information are needed. Neurectomy of the deep branch of the lateral plantar nerve together with fasciotomy have been used successfully for management of horses with hindlimb PSD, with approximately 70% of horses returning to long-term full athletic function (SJD). Osteostixis of the proximal plantar aspect of the MtIII may also help with some horses with chronic injuries with radiological abnormalities but is invasive and has yet to be shown effective in a large number of horses.
Shock wave therapy has been used successfully to treat suspensory desmitis of the origin, body, and branches, especially in horses with bone involvement at the origin. This technique provides profound analgesia and therefore may decrease or even eliminate the lameness.
Horses with larger lesions within the body of the SL or its branches may benefit from splitting alone. This appears to allow a more complete healing of core lesions, which otherwise may be slow to resolve.
Therapeutic ultrasound or infrared laser therapy may aid and reportedly speed healing, although evidence is mainly anecdotal.
Shoeing should be directed at supporting the toe and preventing it from sinking deeper into the ground surface than the heel on weight bearing. If this happens, the heel is elevated, the fetlock drops, and strain is applied to the suspensory apparatus. A shoe with a wide toe is commercially available and helps to prevent the toe from sinking.
Selection of the footing during the convalescent period and when work is resumed is vital, together with careful modification of the training program.
Back Pain
Back pain is common in jumpers, and although signs are recognized easily, the etiological diagnosis may be elusive and complex. The trainer or owner may perceive that a horse has back pain from many clinical signs including sensitivity to grooming and saddling, resistance to rider weight, overall body stiffness, poor performance, and pain on palpation of the muscles over the back. Careful examination of the horse under saddle and over fences and a good working relationship with professional riders can be of great help in interpreting and localizing the type of back pain. Many clinical signs are also common to other diseases or injuries and may be secondary to clinical or subclinical hindlimb lameness resulting in or from an altered gait. Primary back pain may be caused by muscle strain, impingement or overriding of the spinous processes, diskospondylosis, sacroiliac desmitis, supraspinous desmitis, OA of the synovial intervertebral articulations (facet joints), and sacroiliac joint pain.
The veterinarian should first attempt to rule out any lameness. Horses with distal hock joint, stifle, or gluteal muscle pain may swing the hindlimb outward away from the body or inward toward the midline in an attempt to reduce the degree of joint flexion required to advance the limb. Hindlimb lameness should be suspected in horses with simultaneous gluteal and back pain. Horses with bilateral hindlimb PSD may hold the back stiffly and mimic a horse with primary back pain. Chronic forelimb soreness, particularly involving the foot, also may contribute to cervical and/or thoracic pain because of an inverted way of jumping that somewhat protects the foot on landing. Teeth problems or neck pain also should be considered.
Severe back pain suggests a primary back problem. The horse may move with a shortened, stiff gait and appear to be flat or hollowed out in the back when ridden but appear much more comfortable when moving free in a paddock or on the lunge. Injection of local anesthetic solution into the painful areas of the back may change the horse’s movement.
Impinging Spinous Processes
Radiology of the thoracolumbar spinous processes may reveal impingement with increased radiopacity, bone proliferation, and radiolucent defects. Nuclear scintigraphy can be used to diagnose and support the diagnosis of spinous process impingement and osteitis, although false-negative results are sometimes obtained. Occasionally, areas of IRU are visible in the spinous processes without any radiological changes, and supraspinous ligament desmitis should be considered.
The treatment for impingement of the spinous processes or supraspinous desmitis is similar. NSAIDs and methocarbamol are prescribed routinely for a prolonged period. Sarapin and corticosteroids frequently are injected between and around the impinging spinous processes. The locations for injection are determined best by placing a radiodense marker on the top of the back during radiography and then identifying the affected vertebrae by clipping the hair. Mesotherapy may be useful: small doses of flumethasone, lignocaine, Traumeel (a homeopathic remedy), and normal saline are delivered intradermally with 0.4- to 0.6-cm 27-gauge needles on a multiport injection rack. Numerous rows of skin blebs are formed after the injections, and pain relief is almost immediate. Shock wave therapy is also helpful.
Muscle Injury and Pain
Acute muscle strain may be accompanied by spasm, which is evident as a firm, painful swelling. Palpation of the psoas and lumbar muscles can also be performed transrectally, and pressure may also be applied to the caudal and ventral sciatic nerve roots as well. Immediate application of ice and administration of NSAIDs such as phenylbutazone or naproxen are beneficial One author (RPB) also administers 20 to 40 mg of dexamethasone once daily for 2 days in horses with acute pain. Later, moist heat and therapeutic ultrasound reduce pain and inflammation. Local treatment with mesotherapy is useful when treating back muscle pain. Acupuncture has proved useful in managing horses with back pain no matter what the cause. Chiropractic manipulation may be of some benefit in relieving pain and muscle spasm. Pulsating magnetic field therapy is used routinely in show jumpers for the long-term management of back pain. Shock wave therapy has also been used successfully to treat and manage jumpers with back muscle pain.
Saddle fit always should be evaluated critically in a horse with chronic or recurrent back pain, and thermography may be helpful, together with advice available through most good saddle manufacturers.
Fracture of the Withers
Fracture of the withers is not uncommon if a horse flips over backward. The withers area may appear flat and is extremely painful to palpation. The horse plaits in front and holds the neck stiffly. Radiographs are diagnostic. Treatment is directed toward reducing pain and inflammation by applying ice and administering NSAIDs immediately after the injury. Bone sequestrae occasionally develop, and purulent drainage may appear weeks after the injury. However, most fractures are uncomplicated, and horses usually may be able to return to work after 6 to 12 months.
Sacroiliac Joint Pain
Sacroiliac strain is common in show jumpers. Many horses have chronic low-grade pain that never seems adversely to affect the ability to perform. With severe pain a horse may stand parked out (the hindlimbs are extended unusually) and rest one hindlimb. Unilateral lameness may develop, and the horse’s performance then is affected severely. The horse may experience pain on palpation around the lumbosacral region and directly over the tubera sacrale, but this is not specific. Exerting pressure on one of the tubera sacrale may reveal slight motion and even may be resented by the horse. The horse may offer considerable resistance when one of the hind feet is picked up and the limb is flexed high. Rocking the pelvis may cause the horse to grunt. Injection of local anesthetic solution deep into the muscles directed toward the sacroiliac articulations should be performed with caution because the horse may lose its ability to stand. Transrectal ultrasonographic examination may reveal irregular margins of the caudal aspect of the sacroiliac joint and may be useful to support a clinical diagnosis. Evaluation of the ventral sacral nerve roots and the lumbosacral joints may be useful. Nuclear scintigraphy may reveal little if any IRU in this region and is therefore unreliable, but with modern motion-correction software and improved image quality, useful information is acquired in some horses (SJD).
Rest and time are the most important factors influencing the outcome. Horses lame from acute sacroiliac strain may require at least 6 months to heal. Severely affected horses should be given stall rest for 30 days, followed by 2 to 3 months of controlled paddock rest. Light exercise then may begin, gradually increasing the intensity and duration of the work. In our experience, acupuncture has been extremely useful for pain management and the treatment of muscle spasm.
Horses with less severe injuries may be managed successfully by local injections of corticosteroids and Sarapin deep into the painful areas. These horses are able to continue to exercise and compete successfully. The procedure involves directing a 15- to 25-cm needle from a point just medial to one of the tubera sacrale along the inner surface of the ilium deep toward the sacroiliac articulation or using ultrasound guidance and approaching the sacroiliac joint from a cranial dorsal ipsilateral aspect and a caudal dorsal route to treat both sides of the horse. One author (RPB) prefers to use all three approaches on each side. A combination of corticosteroids and Sarapin is injected; however, some practitioners have reported good results with IRAP and bone marrow aspirate as well. Deep injections from either side of midline to the transverse processes of the caudal lumbar vertebrae also help. For 2 weeks after treatment, the rider is cautioned not to collect the horse or perform aggressive lateral movements. Proper and careful rehabilitation is paramount to avoiding recurrence of the problem. Horses with sacroiliac disease are more predisposed to injury when competing at indoor shows, performing high jumps with tight turns.
Injection of the acupuncture points on either side of or parallel to the sacrum with the same solution also may be performed. Chiropractic manipulation often is attempted in horses with sacroiliac injury. Although chiropractic has proved useful as a diagnostic tool and may be of benefit with mild sacroiliac strain, manipulation of the sacrum in horses with more severe injuries never replaces the need for prolonged rest. Pulsating magnetic field therapy, cold laser, and therapeutic ultrasound may be used for the long-term management of chronic sacroiliac problems.
Osteoarthritis of the Thoracolumbar Synovial Intervertebral (Facet) Joints
OA of the synovial intervertebral (facet) joints may be contributing to thoracolumbar region pain, and diagnosis is by radiography and ultrasonography. Ultrasound-guided periarticular injections through the fascia of the multifidus muscle may be of benefit. Careful and progressive warm-up exercises are important.
Fetlock Joint
Synovitis and Osteoarthritis
Metacarpophalangeal or metatarsophalangeal joint synovitis and OA are common in older horses with lengthy careers. Chronic capsulitis results in a thickened, prominent joint capsule with a dramatic decrease in the flexibility of the joint. At least a moderate amount of joint effusion occurs, but many sound horses may have chronic effusion, thickening of the joint capsule, and reduced range of motion. The source of pain is confirmed by a low four-point palmar or plantar nerve block or intraarticular analgesia.
Radiological examination may reveal osteophyte formation on the proximal aspects of the proximal phalanx and the PSBs and flattening of the sagittal ridge of the McIII or the MtIII. The McIII or the MtIII may have a scalloped appearance on the dorsal or palmar/plantar aspect in horses with advanced OA. Subchondral radiolucent areas may develop in the McIII or the MtIII or the proximal phalanx and may result from severe, focal trauma or end-stage OA. The prognosis for horses to return to athletic competition after the development of these lesions is considered poor. Acute fractures and small chips are uncommon in hunters and show jumpers. Small, round, smooth fragments on the proximodorsal aspect of the proximal phalanx are seen in forelimbs and hindlimbs. These fragments represent osteochondrosis and are rarely associated with lameness but occasionally may become unstable and require removal.
Nuclear scintigraphy may reveal mild-to-moderate IRU in the distal, dorsal aspect of the McIII or the MtIII, the proximodorsal aspect of the proximal phalanx, or both. In some horses flexed lateral images are required to separate the bones, especially if IRU in one area is so intense that identifying the adjacent structures is impossible.
In the absence of substantial radiological abnormalities, medical therapy should include NSAIDs, intraarticularly administered corticosteroids and hyaluronan, and orally and parenterally administered PSGAGs. Horses with chronic OA or those difficult to manage may benefit from regular treatment with IRAP. Physical therapies such as icing, cool water therapy, poultices, sweats, cold laser, therapeutic ultrasound, support wraps, and rest are also beneficial. Arthroscopic exploration of the metacarpophalangeal joint is indicated if the response to medical treatment is transient or poor. Clients should be advised that although the causal problem may be revealed, treatment may not be possible. Debridement of damaged cartilage and subsequent replacement with fibrocartilage may be curative; however, excessive erosion of the articular cartilage warrants a poor prognosis for continued jumping.
Therapeutic shoeing targeted at providing support to the palmar aspect of the foot, such as a wide-web shoe, may be of benefit (RDM, RPB). One author prefers an aluminum shoe with short branches, which decreases extension of the fetlock, especially when the horse is landing (PHB). Proper medial-to-lateral hoof balance is also important in reducing torque on the metacarpophalangeal joint.
Sesamoiditis
Sesamoiditis frequently is associated with chronic suspensory branch desmitis. Horses are variably lame and may warm out of the lameness. The distal limb flexion test usually is resented and results in increased lameness. The suspensory branches may be palpably thickened and painful. Intraarticular analgesia of the metacarpophalangeal or metatarsophalangeal joint may improve lameness but does not alleviate it. Lameness is abolished by a low four-point palmar/plantar nerve block.
Abnormal radiological findings include linear lucent zones or lytic areas within the body of the PSB. A generalized loss of bone opacity or proliferative, reactive bone also may be present on the abaxial margins in association with suspensory branch desmitis and insertional lesions of the SL and palmar/plantar annular ligament. We find proximodistal oblique images of the PSBs useful.
Nuclear scintigraphy is sensitive to inflammation in the PSBs, and IRU in the PSBs often is intense. A flexed lateral image helps to separate the PSBs from the McIII or the MtIII. Dorsal or plantar images are required to distinguish between the medial and lateral PSBs.
Treatment for horses with sesamoiditis includes rest, NSAIDs, and supportive shoeing similar to that prescribed for fetlock joint problems. Shock wave therapy may be helpful.
Stifle Joint Pain
Problems involving the stifle joint are common in show jumpers and frequently accompany problems in the tarsus. Joint effusion is present variably. Stifle pain may be primary and related to trauma, mechanical problems, developmental diseases, and OA, or it may be secondary to other lameness. Primary problems include OA, osteochondrosis, meniscal and cruciate ligament trauma, upward fixation or delayed release of the patella, and patellar desmitis. Signs may be subtle at first, with mild shortening of the stride or switching leads at the canter or gallop. Caudal back pain also may be present. The proximal or upper limb flexion test may or may not have a positive result, and the veterinarian should look closely for subtle gait changes such as a shortening of the cranial phase of the stride. Separation of stifle and tarsal pain may be accomplished by flexing the stifle with the hock slightly extended so that the metatarsal region is held behind the tail and perpendicular to the ground, with the tibia held parallel to the ground. The Churchill test also may help to separate hock from stifle pain. Cranial to caudal motion of the tibia relative to the femur during weight bearing (cruciate test) may produce a change in stride; however, it is not routinely performed and has been replaced by abducting and adducting the limb in an attempt to stress the stifle (RDM). However, intraarticular analgesia always is required to confirm the source of pain.
Horses with straight stifle conformation are predisposed to upward fixation and instability of the patella. Pain results from subsequent patellar ligament strain and synovitis. Although the limb may be observed to lock in extension, more frequently a slight hesitation in the advancement of the limb is noted. Femoropatellar effusion may be present.
Ultrasonographic examination of the patellar ligaments may reveal desmitis characterized by enlargement and a focal or diffuse hypoechogenic region. Horses with transient upward fixation of the patella benefit from NSAIDs and an increased exercise program designed to increase muscle tone in the quadriceps group, which stabilizes the patella. Failure to respond to these measures may justify a more aggressive procedure, such as local injection of 2% iodine in almond oil at the proximal aspect, middle portion, and insertions of all three patellar ligaments and into the muscle just proximal to the stifle. This procedure has proved effective in treating transient upward fixation of the patella and subtle soreness in the adjacent muscles. A “splitting” (desmoplasty) of the medial patellar ligament may be performed in horses with more severe upward fixation of the patella. This induces desmitis of the ligament and subsequent thickening. Anecdotal reports describe benefit from estrone sulfate, estradiol, and calcium channel blockers. Jumpers with primary patellar ligament injuries require rest.
Cranial Cruciate Ligament and Meniscal Injury
Trauma to the cranial cruciate ligament produces profound lameness. Intraarticular analgesia of the femorotibial joints may or may not abolish the lameness, and radiographs of the stifle may be normal in horses with an acute injury. With chronic injury new bone may be seen cranial to the intercondylar eminences, most obvious in a flexed lateromedial image. Injury to the medial meniscus is most common. Intraarticular analgesia of the femorotibial joint on the affected side usually produces improvement in the lameness. Radiographs may reveal osteophyte formation on the proximomedial aspect of the tibial plateau indicative of OA and a subjective decrease in the joint space width on the affected side.
Ultrasonographic examination of the stifle is routinely performed and enables assessment of parts of the medial and lateral menisci, the cranial meniscal ligaments, the articular surfaces of the medial and lateral condyles and trochlear ridges, the medial and lateral collateral ligaments, the patellar ligaments, and the tendons originating from the femur and tibia. The presence of joint effusion can also be assessed. Evaluation of the cranial cruciate ligament is challenging.
Osteochondrosis and Subchondral Bone Cysts
Osteochondrosis and subchondral bone cysts should be considered in a young Warmblood that has recently started training or increased its training intensity and has developed lameness localized to the stifle. Intraarticular analgesia usually at least partially eliminates the lameness. We recommend blocking all three joint spaces.
Radiographs are usually diagnostic. Arthroscopy may be indicated. Horses with subchondral bone cysts and other lesions in the medial femoral condyle usually have a poorer prognosis than those with osteochondrosis of the lateral trochlear ridge of the femur. We recommend radiography of the stifles as part of the routine radiographic study when a young Warmblood is examined for purchase.
Nuclear scintigraphy of the stifle in horses with osteochondrosis may reveal little if any IRU. Both caudal and lateral images should be obtained. IRU (to any degree) in the medial femoral condyle in a caudal image almost always is associated with a pathological condition (RPB).
Synovitis and Osteoarthritis
Mature horses may develop synovitis and OA of any one or a combination of the stifle joints. Often the femoropatellar and medial femorotibial joints are involved; however, lateral femorotibial OA may occur alone. Intraarticular analgesia of all three joints should be performed.
The diagnosis may or may not be confirmed radiologically. Osteophyte formation on the proximal medial aspect of the tibia is not uncommon. Nuclear scintigraphy may reveal mild-to-moderate IRU in the femoral condyle and the opposing surface of the tibia on the affected side in a caudal image. Ultrasonographic examination often reveals mild soft tissue inflammation and may be more sensitive than radiography for identification of periarticular osteophytes.
Intraarticular injection of corticosteroids and hyaluronan usually has favorable results. Each joint should be injected separately with double doses of a high-molecular-weight hyaluronan combined with methylprednisolone acetate (40 to 80 mg) or betamethasone (5 to 10 mg). In many horses treatment of the medial femorotibial joint alone is successful (RDM, SJD). NSAIDs, parenterally administered PSGAGs, and intravenously administered hyaluronan are also beneficial and may be used routinely with nutraceuticals as part of a maintenance program. Adequate rest also should be prescribed; however, strict stall confinement is usually not appropriate. Walking these horses under saddle for 30 minutes once or twice daily is preferred. Alternative therapies such as those described for distal tarsitis are also beneficial. Acupuncture commonly is used for managing horses with stifle pain. Recurrent synovitis of a stifle that has been injected repeatedly is suggestive of a more serious injury such as meniscal damage causing some degree of joint instability; therefore, prolonged rest or exploratory arthroscopy should be considered.
Pastern
The pastern region is subject to considerable stress in the jumping horse. OA of the PIP joint is not uncommon and often is associated with OA of the DIP joint. Horses with base-narrow or toe-in conformational defects are affected most frequently. Distal sesamoidean desmitis is also a common problem. Trainers complain that many horses with OA of the PIP joint start out stiff when training and feel much better after warming up, but eventually the lameness becomes persistent. With chronic injury comes obvious thickening in the distal aspect of the pastern. Palmar (abaxial sesamoid) nerve blocks normally eliminate the lameness, although a low palmar (four-point) block sometimes is required. Intraarticular analgesia of the PIP joint also usually produces soundness. The veterinarian must beware that a palmar digital nerve block may alleviate lameness associated with OA of the PIP joint because of proximal diffusion of the local anesthetic solution and the distal palmar extension of the joint capsule.
There is usually greater RU in the subchondral bone of the PIP joints of sound jumping horses relative to other joints. With OA the intensity of the IRU usually increases. We (RPB, RDM) therefore believe that subclinical OA of the PIP joint is common. Radiological changes in horses with OA of the PIP joint include osteophyte formation on the proximodorsal aspect of the middle phalanx. Subchondral osseous cystlike lesions in the proximal aspect of the middle phalanx may be associated with severe trauma or end-stage OA. Acquired osseous cystlike lesions usually are associated with focal, intense IRU.
Management of horses with OA of the PIP joint includes using NSAIDs, intraarticularly administered corticosteroids and hyaluronan, and orally and parenterally administered PSGAGs. The horse should be trimmed and shod to reduce resistance to breakover at the toe and to balance the foot to land as flatly as possible. Occasionally, wedge pads provide comfort by opening up the dorsal aspect of the joint space. Shock wave therapy has been of benefit to horses with advanced ringbone and may be combined with intraarticular injection. Horses with severe OA of the PIP joint may respond poorly to medical management, and arthrodesis may be required. Arthrodesis is often successful in the hindlimbs of jumping horses, but results are often unsatisfactory in forelimbs. Tibial neurectomy also has been used successfully.
Soft Tissue Injury
Injury to the distal sesamoidean ligaments may or may not be accompanied by obvious swelling or pain on palpation. The oblique sesamoidean ligaments are most commonly affected, but jumpers with this injury have a better prognosis than those with injuries to the straight sesamoidean ligament. Analgesia of the palmar (abaxial sesamoid) nerves usually eliminates the lameness. Ultrasonographic examination reveals focal or diffuse hypoechogenic regions in the affected ligament. Palmar or plantar displacement of the DDFT medially or laterally may be secondary to distal sesamoidean ligament injury. The veterinarian should image all structures carefully in the pastern, because several structures may be injured simultaneously. DDFT injuries are more common in the pastern than in the metacarpal region (Figure 115-4). Chronic strain at the insertion of the oblique sesamoidean ligaments may be evident radiologically as enthesophyte formation on the palmar or plantar lateral and medial borders of the proximal phalanx.
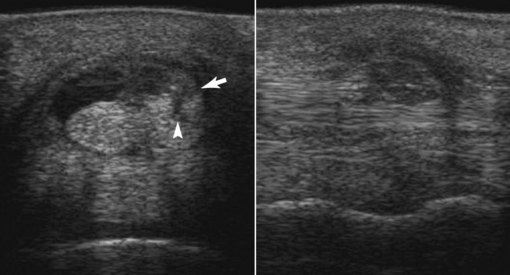
Fig. 115-4 Transverse (left) and longitudinal (right) ultrasonographic images of the palmar aspect of the pastern. Lateral is to the right and distal is to the right. There is an abnormal amount of fluid in the digital flexor tendon sheath. The lateral lobe of the deep digital flexor tendon (DDFT) is enlarged (arrow) with disruption of the palmar border and echogenic material palmar to this. There is a vertically orientated hypoechogenic defect extending across the lateral lobe of the DDFT seen in the transverse image (arrowhead).
Horses with strains and tears of the distal sesamoidean ligaments usually respond to supportive shoeing, NSAIDs, and rest. Horses with acutely torn ligaments may benefit from cast or splint application for about 1 month. Physical therapy such as therapeutic ultrasound may speed recovery. Shock wave therapy is routinely used to treat horses with injuries to the soft tissue structures in the palmar or plantar aspect of the pastern. Regenerative therapies such as those previously mentioned for the treatment of suspensory desmitis may also be of benefit. Injury to these ligaments usually requires 6 to 12 months for convalescence. Returning the horse to work too soon results in thickening and fibrosis of the pastern and prolonged lameness.
Croup and Hip Region Pain
Strain and inflammation of the gluteal muscles are common in jumping horses and sometimes result from an altered gait secondary to lameness elsewhere in the ipsilateral or contralateral hindlimb. Primary strain may occur in a horse during jumping, when a horse refuses a jump, or after a fall. Palpation of the gluteal muscles at the insertion on the greater trochanter and third trochanter of the femur and over the middle gluteal region reveals milder reactivity in horses with secondary strains and a much more severe response or resentment after a primary muscle injury. Upper limb flexion tests may be positive, especially if the gluteal soreness is secondary to lameness involving the hock or stifle. Ultrasonographic examination of the coxofemoral joint may rarely reveal increased fluid indicative of effusion, the result of synovitis or OA. Nuclear scintigraphy may support that diagnosis with IRU in dorsal or oblique images of the coxofemoral joint.
Treatment depends on the severity of the muscle injury or inflammation. Identification and appropriate treatment of the primary lower limb lameness, if present, may do much to reduce mild soreness in just a few days. Most horses with mild injury also respond well to NSAIDs, local application of moist heat, dimethyl sulfoxide, and therapeutic ultrasound. Methocarbamol (20 mg/kg orally bid) may be of benefit. Acupuncture treatments, and in horses with severe injuries local injection of corticosteroids mixed with Sarapin (mix Sarapin, prednisolone, and betamethasone in equal parts in a 12-mL syringe and inject 3 mL per site), provide pain relief. Injections are performed on either side of the spine into the sorest portions of the muscle at 5- to 8-cm intervals or at specific acupuncture sites. Injections may also be made around the region of the greater trochanter of the femur. Ultrasound-guided injection into the coxofemoral joint when synovitis or OA is suspected is recommended. Rest and a reduction in the intensity and duration of exercise also may help. Some horses may require total rest, with exercise limited to handwalking, for several weeks.
Superficial Digital Flexor Tendonitis, Tenosynovitis of the Digital Flexor Tendon Sheath, and Desmitis of the Accessory Ligament of the Deep Digital Flexor Tendon
Superficial Digital Flexor Tendonitis
Injury to the superficial digital flexor tendon (SDFT) in a hunter or jumper is far less common and severe than in a racehorse, probably because the horse is not trained at high speeds. Injuries are more likely to result from a misstep in deep footing rather than from muscle or tendon fatigue proceeding to failure, but low-grade injuries occur frequently in top-level horses from about 10 years of age. Recurrent injuries to the SDFT and ALDDFT may occur in association with foot pain, which changes the biomechanical stress on the digital flexor tendons (PHB). Spontaneous rupture of the SDFT also is seen in old (midteens) jumpers. Often no indication of any tendonitis is apparent before rupture. We also have seen several aged horses no longer in competition with spontaneous SDFT rupture. Geldings are overrepresented, and there may be an association between this severe trauma and hormonal imbalance.
The diagnosis of SDF tendonitis is normally not difficult, and unlike injury to the DDFT usually is not accompanied by substantial lameness, unless an acute injury occurs in the proximal metacarpal region. Lesions in the proximal metacarpal region may be a diagnostic challenge because of lack of swelling. Ultrasonographic evaluation is recommended to assess the severity, location, and extent of the injury. Several reexaminations are important to determine the rate of healing and predict the time to return the horse safely to competition.
The therapeutic goals for management of a hunter or jumper with an acutely injured digital flexor tendon are rapid reduction of the inflammatory response and elimination of edema. This is achieved with the administration of NSAIDs, low doses of corticosteroids, and diuretics. Ice, hydrotherapy, and support bandages also are used and applied as soon as possible, and often the trainer applies them before the veterinary examination. For horses with strains or injury without actual fiber tearing (type 1 or 2 lesions), peritendonous injection of corticosteroids or intralesional injection of hyaluronan may dramatically decrease the size of the tendon and produce favorable cosmetic results. The trainer must be advised not to exercise the horse and that total healing actually may be delayed slightly. After the injection the limb should be supported with a firm, modified Robert Jones bandage to prevent the return of any swelling. Tendon splitting has been indicated in horses with substantial core lesions (type 3 or 4 with a diameter greater than 0.5 cm). Ultrasound-guided intralesional injections of IRAP, PRP, or A-Cell may be of benefit for lesions of this type and severity. The benefit of a splitting is obtained with the multiple injections required to deliver an adequate volume of product. During the procedure the material is seen going into and coming out of the tendon and causing peritendonous or subcutaneous swelling. Perhaps this produces a “lavaging” effect and removes some of the blood, serum, and inflammatory mediators from the core lesion. It is one author’s opinion that this lavaging effect is actually beneficial and that larger volumes of fluid should be used when possible (RPB). Therapeutic ultrasound after the initial phase of healing (3 to 4 weeks after injury) encourages resolution of inflammation and promotes healing. Shock wave therapy is also sometimes recommended after the injection; there is debate about frequency and intensity of treatment.
Overall, the time required for digital flexor tendons to heal sufficiently so the horse may return to jumping depends on the severity of the injury and to some degree the location of the injury. Routine SDF tendonitis takes less time to heal than an injury to the SL at the same location. A mild injury takes 3 to 4 months and a severe injury takes about 12 months to heal. Monthly ultrasonographic examinations are used to determine the physical therapy schedule and the optimum time for the horse to return to jumping. Horses often can continue to compete despite active SDFT injuries, although the lesions may slowly get worse.
Tenosynovitis of the Digital Flexor Tendon Sheath
SDFT or DDFT injury within the digital flexor tendon sheath (DFTS) frequently is seen in jumpers at any age or level of competition (Figure 115-4). Tenosynovitis also occurs without tendon injury. SDF tendonitis may result in chronic tenosynovitis and often plagues older horses. Tenosynovitis is slightly more prevalent in hindlimbs, presumably because of the strain caused by the push-off in jumping. The DFTS may be warm and swollen. Digital pressure at the proximal and distal aspects of the DFTS usually is resented. Pressure applied directly over the palmar or plantar aspect of the fetlock also may cause pain. Results of a distal limb flexion test are usually positive. Moderate effusion is usually present in horses with an acute injury, but those with chronic injuries may have a thickened, fibrotic DFTS and much less fluid. The proximal aspect of the DFTS may show effusion, yet none may occur distally in the pastern. Lack of effusion likely results from a compartment syndrome with thickening of the DFTS synovium, the SDFT, and possibly the palmar/plantar annular ligament, thus preventing the flow of fluid distally past the PSBs. However, DDFT lesions in the pastern may be associated with distention of the DFTS localized to the pastern. DDFT lesions may be core injuries readily identified using ultrasonography or marginal tears more reliably diagnosed using tenoscopy (see Figure 115-4). Lameness may vary and may be evident only after flexion of the distal aspect of the limb. Intrathecal analgesia of the DFTS usually improves lameness. Ultrasonographic examination should include the fetlock and pastern regions and reveals increased fluid, allowing the tendons and a thickened synovium to be evaluated easily. The digital flexor tendons may appear to be normal.
Therapy for horses with tenosynovitis of the DFTS varies depending on the severity of the problem and the structures involved. Antiinflammatory therapy consisting of ice, cool water therapy, poultices, NSAIDs, and corticosteroids is effective in horses with mild primary injuries of the DFTS. In horses with more severe injuries, intrathecal injection of corticosteroids and hyaluronan is beneficial. Rest is essential. Horses with mild injuries may return to work in 1 to 2 weeks, but those with more severe injuries require more time. Good trimming and shoeing are beneficial. Transient response to treatment usually implies associated tendon injury. Horses with chronic, unresponsive tenosynovitis may require tenoscopic examination and possibly desmotomy of the palmar or plantar annular ligament.
Desmitis of the Accessory Ligament of the Deep Digital Flexor Tendons
Desmitis of the ALDDFT is a common problem, especially in older show jumpers, and often results in sudden onset of lameness after landing over a fence, with rapid development of localized swelling. In some horses there is only mild-to-moderate swelling below the carpus on the day after jumping, with minimal to no lameness. Ultrasonography is required to determine the location, severity, and extent of the injury and subsequently to monitor healing. Treatment is similar to that for SDF tendonitis, and rapid and aggressive use of systemic NSAIDS as well as local injection of corticosteroids to control early inflammation is important. A premature return to work may result in recurrent injury and ultimately adhesion formation between the ALDDFT and the SDFT. However, many horses with mild-to-moderate strains can be managed with shortened rest periods and aggressive antiinflammatory therapy. Once inflammation has been controlled, the horse can return to work and may handle a normal workload even without meaningful healing of the injury. This depends on the severity of the injury, in particular the proportion of the cross-sectional area of the ligament affected. As long as pain and swelling are controlled, lameness is controlled and the horse can perform in many instances even without a completely healed ligament (TRO). Shock wave therapy may be useful.
Cervical Osteoarthritis and Pain
Soreness in the cervical region can seriously affect a jumper’s performance. OA of the cervical facet joints is common but may not always cause clinical signs. Muscle strain in the cervical region can also occur. Neck pain may be evidenced by an unwillingness to flex the neck laterally or dorsoventrally, by being “hard” on one side of the mouth, or by an overt forelimb lameness, which first may appear as a reluctance to advance the limb. Enticing the horse with a carrot to stretch and flex from side to side may reveal an unwillingness or limited range of motion. There may be pain on palpation. Lameness related to neck pain may appear similar to primary forelimb pain, but it is not abolished using diagnostic analgesia of the lame limb. Shoulder pain may mimic cervical pain, but analgesia of the shoulder joint or bicipital bursa may improve the lameness.
Nuclear scintigraphy is a potential screening method (RPB), but greater radiopharmaceutical uptake is frequently normally seen in the caudal cervical facet joints compared with further cranially (SJD). Comparison of left and right lateral images is crucial (SJD). Lateral and oblique radiographic images are useful for identification of OA, bearing in mind that many horses with radiologically apparent lesions do not have clinical signs (SJD). Ultrasonography may yield additional information about joint effusion and joint capsule thickening.
Ultrasound-guided intraarticular injections of the facet joints can be used both diagnostically and therapeutically. One author (RPB) routinely injects the affected facet joints and those immediately cranial to and caudal to the suspected joint; however, it is also his experience that regional injection also produces a positive response. Methylprednisolone acetate, 20 mg, is injected as a 3-mL solution in sterile saline at each site.