Chapter 116Lameness in the Dressage Horse
The Sport
Dressage is the ultimate athletic challenge in equestrian sports because it combines balance, suppleness, and power in a unique gravity-defying manner. A good horse gives the impression of athletic elegance and expressive animation. The gaits are described using terms such as balance, suppleness, and hindlimb activity. The first demand is that the horse be completely obedient, going wherever the rider wants and carrying out movements at his or her request. In doing so the horse has to rely on its rider, trust the rider, and accept the rider as its superior. The key to the training and development of a dressage horse from the lowest levels to International Grand Prix is gymnastic exercises, with the aim of strengthening the muscles and thereby avoiding injury to joints and tendons associated with an increased workload.
The Fédération Equestre Internationale (FEI) dressage rules state that the object of dressage is the harmonious development of the physique and ability of the horse. Through the levels of dressage training, the center of gravity of the horse and rider is placed further caudally, achieved by increasing the degree of flexion and loading of the hindlimbs, while at the same time freeing the front end of the horse to create a more airborne, uphill set of movements. This can be obtained only by increasing the power of the hindlimbs, by synchrony in movement between the forelimbs and the hindlimbs, and through the freedom of movement of the back.
In the German equestrian literature the following terms describe the aims of the correctly trained dressage horse:
Dressage is an international sport, although it always has had its main center of excellence in Northern Europe, most particularly Germany, but in later years also in Holland, Denmark, and Sweden. More recently, teams from Spain, the United Kingdom, and the United States have started to challenge for medal positions in international competitions. Dressage developed from the military institutes and only in the twentieth century became a truly civilian sport. Even up to the time of the Second World War, military officers participated at all the major dressage games.
In Europe the competitive sport has been divided into three levels: L, M, and S. L covers novice level (novice and elementary); M covers medium and advanced medium; and S covers Prix St Georges, Intermediare I and II, Grand Prix, and Grand Prix Special. The movements required at each of these levels reflect the horse’s degree of collection, with the L classes expressing balance and freedom of movement, M classes requiring more collection and lateral movements, and S classes demanding ultimate collection to enable movements of maximum collection and suspension, such as piaffe, passage (Figure 116-1), and canter pirouettes (Figure 116-2). However, even the most skilled rider or trainer has difficulty selecting the right horses, because many promising young horses with excellent gaits fail to learn passage and piaffe, probably because of our insufficient knowledge of the biokinematics of collection.1
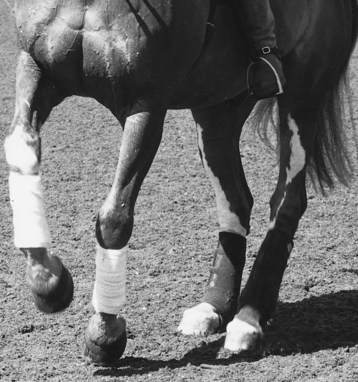
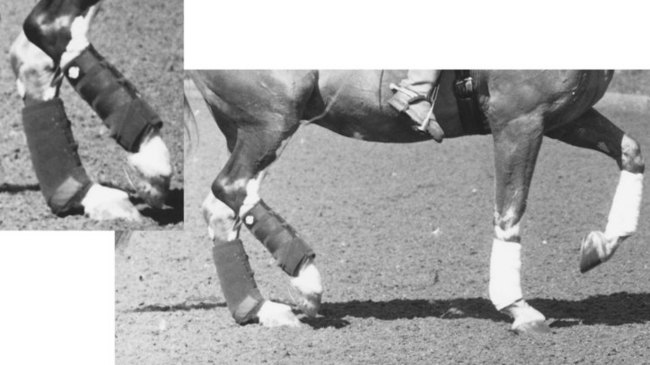
Fig. 116-2 Canter pirouette to the left. The horse intermittently takes all weight on the hindlimbs, resulting in extension of the metatarsophalangeal joints and great strain on the suspensory apparatus.
Lateral movements apply specific, unique strains to different structures within the skeleton. In shoulder-in, half-pass, renvers, and travers the horse is bent evenly in its neck and body but moves on more than two tracks. In shoulder-in, the horse moves on three tracks (1, outside hindlimb; 2, inside hindlimb and outside forelimb; and 3, inside forelimb) with the body at an ideal angle of 30 degrees to the direction of movement. In travers (quarters-in) and renvers (head to the wall) the horse moves on four tracks. These movements create an unusual strain on the horse’s back and pelvis and an additional twisting movement on the appendicular joints.
The increased engagement of the hindlimbs developed through collected work allows for greater storage of elastic strain energy in the hock joints and pelvis, which, via the increased lifting of the forehand, allows for high-energy movements such as medium and extended trot. The term cadence is associated closely with working through the back and self-carriage and requires complete freedom without which movements will be inferior. Self-carriage reflects a level of training in which the horse has learned to balance itself and its rider and additionally has developed its musculature to allow movement with greater range of freedom. This process takes time, and it is not unusual to see a degree of hindlimb gait irregularity in 4-year-old horses in the early part of training; normally this is a reflection of lack of balance and will improve with training and time.
Anlehnung (contact with the bit) is an important concept to understand, requiring the horse to move freely forward with impulsion, to take and accept the bit, and to react to it without resistance. The FEI rules require the horse to work on the bit—that is, with the front of the head positioned in, or slightly in front of, the vertical plane. In recent years the tendency has been toward training dressage horses in an over-bent fashion, with the horse’s forehead behind the vertical plane, in its extreme form referred to as rollkur. This is said to be a requirement for developing the trapezius and rhomboidius as well as other muscles of the shoulder and withers region and thus enabling a greater lift of the forehand via the shoulder girdle. Although this method of training contradicts the FEI requirement for the horse’s forehead to be in a vertical plane, top riders are able to place the horse’s head in virtually any position according to what is required. There has been considerable debate about rollkur being a forced and unnatural position; however, to date there is no scientific evidence to suggest that it is in any way detrimental to physical well-being, assuming that it is performed well. Moreover, some of the most successful dressage horses are trained using rollkur as part of the regular work program. However, as with any method of training, it is important that the horse be allowed regular stretching and rest periods to avoid muscular fatigue, which may predispose to injury.
“Contact with the bit” and “working on the bit” are terms that are frequently misunderstood. The horse must move with energy and impulsion and work through the back to enable correct contact with the bit. Stiffness in the back often results in poor and incorrect bit contact. Increased bit lathering as an indication of improved bit function is frequently seen after successful treatment of back pain. Misinterpretation of the role of the bit leads to restriction of the horse by the hands, which inevitably results in loss of action and gait irregularities. Thus inappropriate riding and training can potentially produce clinical problems.
The Dressage Horse
Most dressage horses competing internationally are Warmbloods (WBLs) with a high proportion of Thoroughbred (TB) breeding. Dressage horses today combine the elegance and athleticism of the TBs with the power and trainable mind of the WBLs, which have been selected for many generations for these traits. Few pure TBs reach international standard dressage. The TB has been bred to run fast or show courage jumping obstacles cross-country, which are not of great value when the rider requires complete obedience to perform movements that go as much upward and sideways as forward. Most TBs also lack the strength and quality in all three paces compared with the WBLs, in particular the walk and the trot. Most TBs do not show the same degree of natural engagement of the hindlimbs typical of many WBLs. Many of the greatest TB sires in postwar European dressage breeding (Der Löwe, Velten, and Pik As) have been neither particularly physically impressive nor equipped with more than an average trot. Previously TB stallions in WBL breeding were required to have a minimum general handicap to ensure that they had been physically and mentally strong enough to stand up to training and race consistently and reasonably successfully. Spanish horses have increased in popularity, often being easier to train than WBLs, readily learning and executing piaffe and passage, but lacking the expression and animation of the gaits of the most successful WBLs. Lipizzaner horses are rather similar and are used by the Spanish Riding School in Vienna, but are rarely used as competition horses. Mares, geldings, and stallions are used; stallions may combine competition work with breeding (usually by artificial insemination).
A dressage horse must be naturally well balanced. The head and neck must be set sufficiently high to facilitate working uphill and for easy contact with the bit to be made. The shape of the withers region is important, so that the saddle sits easily in the correct position. The dressage rider spends a lot of time sitting in the saddle in sitting trot; therefore correct weight distribution is critical.
Most dressage horses are broken at 3 or 4 years of age and begin competing in young horse classes at 5 years of age. Medium classes are reached by the age of 7 and many future Grand Prix dressage horses do a small tour at the age of 8 and 9. Once a dressage horse has reached Grand Prix level, the training predominantly involves repetition of movements, maintaining suppleness, and increasing physical power. Thus dressage horses rarely succumb to acute stress-induced traumatic injuries but are more likely to succumb to repetitive, accumulative subclinical injuries that may surface at irregular intervals. This means that with correct training and management, dressage horses can continue to compete at the highest level at an advanced age, often as old as 15 to 20 years. Many of the Lipizzaner stallions at the Spanish Riding School in Vienna are touring and performing adequately after 20 years of age.
A true link between conformation and soundness is difficult to establish, because what creates an outstanding dressage horse in terms of conformation does not necessarily create a particularly sound dressage horse, and vice versa. However, in a study of 4-year-old Swedish WBL horses, highly significant correlations were found between conformation and movement and between conformation and orthopedic health, whereas no correlation was found between the overall conformation score and competition performance.2 A series of elite dressage horses had larger hock joint angles and more sloping shoulders than more average horses, whereas good forelimb movements were characterized by a large range of flexion of the elbow and carpal joints during the second half of the swing phase. This is what previously has been referred to incorrectly as shoulder freedom. It is important that a young horse naturally places the hindlimbs well underneath itself, because the approach angle does not seem to be influenced by training.1
Wear-and-tear lesions frequently occur because of a less-than-ideal joint and limb angulation, but many other factors influence the durability of the horse, including genetic predisposition and management conditions before skeletal maturity. The main requirement must be the ability of the horse to balance itself at all paces, because imbalance and asynchrony in movement apply unusual strains on many structures. Holmström found that a large positive diagonal advanced placement (the time difference between the hindlimb and contralateral forelimb contacting the ground) correlates with high trot scores and suggests this as being an important indicator of the horse’s natural balance.1 The positive diagonal advanced placement does not change with more collection and therefore may become a useful selection criterion. Holmström also found that a group of selected elite horses with high gait scores had significantly larger stride duration, increased hind stance phase duration, and greater diagonal advanced placement than a group of horses with low gait scores.1 It should be noted, however, that advanced diagonal placement results in a single hindlimb bearing all the horse’s weight, with increased extension of the metatarsophalangeal joint and thus increased strain on the suspensory apparatus. Medium and extended trots result in greater extension of the fetlock joints compared with working and collected trots, thus stressing the suspensory apparatus. Many talented young horses that are professionally produced for sale by auction are worked in a much bigger trot than a true working trot, which also results in high loads on the suspensory apparatus, predisposing to injury in all four limbs.
Training Surfaces
Dressage horses are trained predominantly on artificial surfaces with a high degree of cushion, providing a consistency in the training surface not paralleled in other equestrian sports. All dressage competitions in mainland Europe take place on artificial surfaces, and only in England does dressage at the lower levels (L) still take place on grass. A multitude of artificial surfaces have been developed over the last 20 years. Most are based on silica sand mixed with a variety of rubber and polyvinyl chloride material, together with a binding and dust-limiting agent such as Vaseline, which ensures that such surfaces remain dust- and frost-free down to at least −5° C. This standardization of working and competition surfaces unquestionably plays a huge role in the low occurrence of many acute orthopedic problems in the dressage horse. Some trainers, however, consider constant working of repetitive movements on ideal surfaces likely to soften the limb structures and therefore recommend that the horses occasionally be jumped or hacked on less ideal surfaces to provide a stimulus for joint, tendon, and ligament adaptation and generally improve proprioception. We believe that working on a variety of surfaces and “cross training” are helpful for maintaining both musculoskeletal soundness and a correct mental attitude.
Arena maintenance is paramount for a good surface. An effective drainage system through central and perimeter drains is also absolutely essential. Dead corners of deep sand predispose horses to momentary loss of balance and may predispose to the development of lameness. Any sudden change of surface integrity also predisposes horses to lameness. Young horses in particular work more easily and confidently on firmer modern artificial surfaces, where they can obtain a more confident grip and are less likely to fatigue. In a recent questionnaire-based study of British dressage horses the effect of arena surfaces on both lameness and undesirable gait traits such as tripping or slipping was investigated.3 The results indicated that wax-coated and sand and rubber surfaces were associated with less detrimental surface properties than sand, sand and PVC, woodchip, or grass. Woodchip was most strongly associated with the detrimental characteristic of slipping, and sand with tripping. Findings indicated that any arena surface should have a base, and limestone was recommended, with crushed concrete best avoided. In a related study, work on sand-based arena surfaces resulted in a 1.36 times greater likelihood of having lameness in the previous 2 years compared with other surfaces.4 However, very regular work on sand appeared to have a protective effect. Regular work on an outside arena resulted in a 0.61 times reduced risk of lameness compared with horses worked in indoor arenas. Deep, patchy, or uneven going under normal conditions and patchy, boggy, or deep surfaces in wet conditions increased the risk of lameness.
Tack
The horse must be comfortable in its tack if it is going to work optimally. Dressage saddles are designed to position the rider with a deep seat and with an extended leg position. The surface area over which the weight is distributed must be as large as possible, to avoid focal pressure points. The use of gel pads and layers of numnahs (saddle pads) is not a substitute for good saddle fit. The saddle must fit the horse and the rider and must position the rider in appropriate balance. The fit must be assessed with and without a rider. The shape of the horse’s back musculature may change as the horse develops muscular strength and power; therefore a previously well-fitting saddle may become constricting. It should also be remembered that the withers and back may expand during a training session, sometimes effectively rendering the saddle too small.
Acceptance of the bit is crucial in a dressage horse. Horses vary considerably in the shape of the mouth and the sensitivity of the corners of the lips, bars, and tongue. Great variation also exists in the thickness of the tongue among horses. A slight crack in the corner of the mouth, caused by an inappropriate bit, can cause major problems with proper acceptance of the bit and the horse’s willingness to work straight. At S level, horses have to compete wearing a double bridle—that is, the mouth has to accommodate both bradoon (snaffle) and curb bits. These vary greatly in shape and design, and selection of the most appropriate can be critical.
Lameness Examination
Examining a lame dressage horse does not differ in any great detail from examining any other equine athlete. However, examination frequently requires spending more time observing the horse being ridden, because many dressage horses reproduce the perceived problem, often no more than a resistance, only when ridden and sometimes only during certain movements. This, however, does not mean that the horse should not be examined in hand, including walking and trotting on a straight line and lunging on hard, nonslip surfaces (such as gravel) and on softer artificial surfaces. Not only does lunging on tarmac or concrete carry the risk of the horse slipping, with potentially disastrous consequences, but also in most horses such lunging alters the gait so much that it has little value in a lameness examination of an extravagantly moving dressage horse. Leading the horse on a circle at a trot also tends to alter the horse’s stride. The horse does not have the freedom to move its neck and instead will set its head on the leader’s hand. Many big moving exuberant dressage horses are a safety hazard either to trot in hand or to lunge and lameness is easily masked, especially if low grade. The use of sedatives such as romifidine or detomidine can be helpful, although it is an art to select the most appropriate dose. Repeated sedation may be required to permit accurate interpretation of the response to nerve blocks.
In many horses the usual rider has to be available to reproduce the described problem, if lameness is not overt. However, one should remember that just as bad riders create lameness, so good riders may hide lameness. The latter may take place completely unintentionally and may involve no more than a corrective change of point of balance of the rider through a corner, but enough that for a long time the problem may not be observable from the ground. Most veterinarians who are not competent riders are not experienced fully to appreciate the subtle differences in high-quality dressage horses, and attempting to ride the horse to better appreciate the problem may create an embarrassing situation. They are better advised to spend more time observing the horse from the ground. However, one of the authors (SJD) who is an experienced rider often finds it hugely valuable to ride a horse to be able to better understand the feel of subtle problems.
The veterinarian should not just focus on the limbs when watching the horse ridden. It is important to observe changes such as a change in lathering of the mouth, audible change in the rhythm of the stride, or even absence of teeth grinding or grunting after a particular diagnostic test. The position of the head and neck, the suppleness of movement through the back, the balance of the horse, and its ability to engage the hindlimbs in downward transitions are all important features.
For many horses the veterinarian relies heavily on the perceived observations of the rider during the lameness examination; this may involve the appreciation of subtle changes of gait, or even just an impression of a stronger rhythm or less heavy contact on the bit after a peripheral nerve block. Many riders feel through their own body if the horse is working crookedly, that is, not straight and not in complete balance, and will be able to tell the clinician if this feeling has been altered by any of the diagnostic tests.
In many horses, alternating between lunging and ridden work is useful, often going back to lunging with full tack after the horse has been ridden to see a possible difference in the gait from being ridden. Generally, horses with back pain appear worse while ridden than when lunged, with a loss of freedom and athleticism.
A useful test is to ask the rider to deliberately ride on the wrong diagonal, that is, to sit to the trot in the saddle when the inside forelimb is bearing weight. Horses with forelimb or hindlimb lameness and horses with back pain may alter the gait when the weight-bearing diagonal (of the horse) is changed. The difference in the horse’s outline and attitude when changing between sitting and rising trot also may add valuable information.
It can be helpful to see the horse ridden in two 10-m–diameter circles in a figure eight. A low-grade hindlimb lameness may be highlighted as the horse changes direction, characterized by loss of rhythm and fluidity of movement, swinging the hindquarters outward, and a tendency for the inside hindlimb to cross in under the body during protraction. Careful observation of downward transitions from trot to walk may reveal that the horse does not “sit down” properly behind but stays somewhat croup high and takes slightly shortened steps behind. Low-grade unilateral hindlimb lameness may manifest only in certain movements, such as canter pirouette to the side of the lame limb. The horse may be unable to maintain the three-time canter rhythm and may try to jump out of the movement. The horse may find flying changes in canter difficult in the change toward the side of the lame limb—that is, a horse with right hindlimb lameness may perform flying changes from right to left without difficulty but perform less well from left to right, becoming croup high and/or changing late behind. Half-pass away from the lame limb may be less good—that is, a horse with right hindlimb lameness may find half-pass to the left more difficult than to the right.
In some horses lameness is created by the rider. This most commonly occurs with amateur riders who misunderstand the principles of obtaining an outline and riding the horse forward into a contact with the bit. Overrestriction by the hands, with inadequate impulsion, can create gait irregularities. Lower-level trainers are sometimes unable to appreciate these problems and may themselves be unable to work the horse better. Using a good professional rider who is not the horse’s trainer to work the horse during the examination is therefore preferable. Determining definitively whether the problem is one of riding or of training or a reflection of a genuine lameness may require observing the horse over several days. A rider who sits consistently crookedly can create back pain and loss of hindlimb rhythm and symmetry. Some dressage horses are exuberant and expressive movers and also strong-willed characters that may refuse to go forward properly if ridden by an enthusiastic but less competent amateur rider, especially if the rider is somewhat apprehensive and inclined to be overrestrictive. Nappy (resistant) behavior and unwillingness to work may reflect a pain-related problem, but not necessarily so.
One should remember that not all horses are athletes. Many owners tend to think that all horses can learn to do dressage. Veterinarians must in certain situations be prepared to offer the opinion that the particular horse has too many shortcomings physically or psychologically to be able to perform advanced dressage. A veterinarian may be able to help a horse overcome a specific problem but cannot provide missing athleticism.
The veterinarian should not forget to check the obvious. The horse may be apprehensive about taking the bit, may take irregular steps, or may be reluctant to bend properly. Wolf teeth frequently are blamed for reluctance to accept the bit properly and for irregularities in gait. Provided that a wolf tooth is immediately in front of the first upper cheek tooth and is not mobile, the tooth rarely is associated with pain.
Horses with a short poll and a relatively large mandible have difficulty in acquiring the correct degree of neck flexion. In these horses it is also important to check that airflow is not impaired. Restricted airflow is not necessarily accompanied by an audibly abnormal inspiratory and/or expiratory noise.
If a diagnosis cannot be made because clinical signs are too subtle, or if it is difficult to determine whether the clinical problem is pain related, working the horse while treating it with antiinflammatory medication (2 to 4 g phenylbutazone per day orally [PO]) for 2 to 3 weeks may be useful. If lameness returns once the medication has been withdrawn, the performance problem can be attributed to pain. The lameness also may be worse, making further investigation easier. If the horse appears to have a low-grade bilateral problem, starting by blocking one limb (forelimb or hindlimb) to see if a contralateral limb lameness immediately becomes obvious can be useful. Blocking both limbs simultaneously and then reassessing the overall freedom of movement and balance may also be of enormous value.
Diagnostic Analgesia
In principle, no differences exist between dressage horses and other equine athletes with regard to diagnostic analgesia. However, the horse’s response should be assessed both when ridden and when trotted in hand. Because only minor irregularities in gait are often the point of investigation in lame dressage horses, it is particularly important that the conditions, including the surface, the person handling the horse, and the tempo with which the horse is lunged remain consistent throughout the lameness investigation. Starting the investigation on one surface only to change surface halfway through the nerve blocks should therefore be avoided. Indoor arenas obviously are of great assistance in terms of providing a consistent working surface in severe weather conditions.
Although the sequence of the nerve blocks in theory should be the same in all equine athletes, known common lameness sites in dressage horses often make focusing on these areas possible in order to save time and to avoid an unnecessary number of injection sites and undesirable number of clipped sites. If clipping is essential, many riders prefer that the entire limb (and contralateral limb) be clipped symmetrically rather than producing many small clipped sites in one limb.
Imaging Considerations
Imaging of a lame dressage horse is no different from imaging any other equine athlete. However, the frequent lack of overt lameness in a submaximally performing dressage horse often necessitates the use of every possible diagnostic modality available. This is particularly true for evaluation of the neck and the back, both of which are important structures for balance and coordination. These are areas in which diagnostic analgesia is less easy than in the limbs but is nonetheless important.
Radiographic evaluation of the thoracolumbar region requires fixed or semimobile radiographic equipment. Use of a Dodger-T aluminum wedge to attenuate the primary x-ray beam facilitates acquisition of high-quality images of the dorsal spinous processes.5
Diagnostic ultrasonography of the thoracolumbar and pelvic regions is also useful, used transcutaneously or per rectum to image the supraspinous ligament and epaxial musculature, the synovial articulations (facet joints), and the ventral aspects of the lumbosacral and sacroiliac joints.6 An ability to obtain high-quality images of the suspensory ligament is crucial, but according to the shape of the proximal aspect of the hindlimbs this may or may not be possible. In some horses magnetic resonance imaging (MRI) may be required for accurate diagnosis.
Nuclear scintigraphic evaluation can be particularly helpful in evaluating the thoracolumbar and pelvic regions. However, a study in clinically normal WBL riding horses showed that mild increased radiopharmaceutical uptake (IRU) in the summits of the dorsal spinous processes may be seen. Thus, as with all imaging techniques, great scientific integrity is demanded to distinguish between normal variations and pathological lesions, and results must be correlated carefully with clinical observations and with other imaging modalities.
Computerized thermographic image analysis has been reported as being helpful but in our experience is often misleading, and it is no longer used routinely.
Ten Most Common Lameness Conditions in Dressage Horses
The conditions are listed not necessarily in strictly decreasing order of importance or frequency.
In our experience many of these conditions can cause overt unilateral lameness. However, bilateral conditions may be less easily recognized and the horse may be presented for investigation because of an insidious onset of progressive unwillingness to work or loss of quality of paces. In-depth investigation of such horses often reveals the presence of lameness in three or four limbs, with or without thoracolumbar or sacroiliac joint region pain.
Proximal Suspensory Desmitis: Hindlimbs
Probably the most important cause of lameness in dressage horses working at medium and advanced levels is proximal suspensory desmitis (PSD), although a recent study showed that nonelite dressage horses were also at high risk.7 The carrying capacity of the hindlimbs is increased with increased collection required for more advanced work, and movements such as piaffe, passage, and canter pirouettes (see Figure 116-2) place great strain on the hindlimb suspensory apparatus. Advanced diagonal placement, a gait characteristic of some excellent moving horses, increases stance duration and also results in the horse bearing weight on a single hindlimb, both of which may contribute to repetitive overload. Suspensory desmitis is believed to be caused by an accumulation of repetitive strains within the suspensory ligament (SL) and its proximal origin. The observation that some horses develop PSD in all four limbs suggests that some horses may have some genetic predisposition to injury.
Detection of PSD is often delayed because of its bilateral nature, which often means that overt hindlimb lameness is not present or immediately noticed by the rider. The condition may be manifested as a loss of performance, increased stiffness, change in contact with the bit, or resistances, if bilateral. If unilateral, problems may arise with specific movements such as canter pirouette or flying changes. In our experience dressage horses tolerate hindlimb PSD less well than show jumpers or event horses, probably because the temperament of the horses is different and the enjoyment of jumping can override low-grade pain.
Accurate diagnostic nerve blocks therefore are required to reveal lameness. When no obvious lameness is present, lameness may be created subsequently in the contralateral hindlimb by diagnostic analgesia of either of the hindlimbs. A negative response can be misleading, and it is often necessary to block both hindlimbs simultaneously, after which there may be a substantial improvement in gait. Direct palpation of the region often fails to indicate a problem because of the deep location of the proximal aspect of the SL. The clinical diagnosis is confirmed by positive subtarsal analgesia (of the deep branch of the lateral plantar nerve), together with negative intraarticular analgesia of the tarsometatarsal (TMT) joint. In some horses PSD and distal hock joint pain occur together and additional intraarticular analgesia of the TMT joint is required for complete resolution of lameness. In other horses, especially those with lesions involving the most proximal aspect of the SL, a tibial nerve block is required to abolish lameness. In some horses, usually those with bilateral PSD, there is coexistent sacroiliac region pain. There may be substantial clinical improvement after bilateral subtarsal nerve blocks, but the quality of the paces, especially canter, and the balance of the horse may not be normal. Further improvement is seen after infiltration of local anesthetic solution around the sacroiliac joint regions. In some young horses, often those that have been professionally produced and sold through public auction in continental Europe, that have developed problems within the first few months of purchase, resolution of hindlimb lameness may reveal a forelimb lameness, often bilateral, also the result of PSD.
Extensive ultrasonographic and radiological changes often reflect a chronic and long-standing problem. Ultrasonographic images may reveal enlargement of the proximal aspect of the SL in both transverse and longitudinal planes, with areas of reduced echogenicity, most often involving one or both of the dorsal quadrants of the ligament. However, in other horses ultrasonographic abnormalities may be much more subtle; areas of increased echogenicity may reflect chronic fibrosis. Radiological diagnosis requires high-quality radiographs of the proximal metatarsal region; dorsoplantar and lateromedial images are the most useful. Irregularity of the proximal plantar cortex of the third metatarsal bone (MtIII) may occur in the region of the origin of the SL, with a varying degree of endosteal new bone resulting in increased radiopacity of the trabecular bone over a distance of up to 5 cm. On dorsoplantar images this may be seen as a centrally or laterally positioned area of increased radiopacity within the trabecular metaphysis of the MtIII. One should remember, however, that such radiological changes may be present in an asymptomatic horse because of previous problems (either subclinically or clinically manifested), leading to the risk of a false-positive diagnosis. Diagnosis should never be based only on radiological evaluation.
Occasionally, nuclear scintigraphy can be useful in horses with early desmitis in which no radiological changes are present and subtle, equivocal abnormalities are detected with ultrasonography. IRU may occur in the proximoplantar aspect of the MtIII in bone phase (delayed) images. Pool phase (soft tissue) images are rather insensitive, and not all horses have associated IRU in the proximal plantar metatarsal region. Thus a negative bone scan does not preclude PSD. Moderate-to-intense IRU usually reflects entheseous reaction. MRI may be required for definitive diagnosis.
Treatment of this condition is often frustrating because of the chronic nature of the problem at the time of its detection. However, in well-conformed young horses with recent onset of clinical signs, rest may be all that is required, with a careful progressive resumption of work after approximately 3 months. Corrective trimming to restore foot balance is important; shoeing using egg bar shoes provides some support in horses with hyperextension of the fetlock joint. In horses with chronic injuries prolonged rest (3 to 6 months) often provides a disappointing response, and a controlled exercise program may be more successful. Periligamentous, subfascial injection of hyaluronan plus a corticosteroid (e.g., 40 mg of methylprednisolone acetate or 10 mg of triamcinolone acetonide) is now used frequently and is believed to provide an initial reduction in inflammation to enable a reasonably pain-free walking program to be initiated. This frequently is continued for as long as 12 weeks before slow, balanced trotting on a good surface is initiated.
The ultrasonographic appearance of the SL often changes little, even in horses that are returned successfully to full training. Egg bar shoes are often removed when normal training is initiated, because many riders believe that they provide too much breaking action on ground impact of the hindlimbs. The likelihood of recurrence of PSD is high, and special care should be taken not to overwork the horse on deep or holding surfaces or to change suddenly to a different surface. Modification of the training program is often required, particularly in terms of avoiding a fatiguing training session in deep or loose surfaces. Medium and extended paces should be avoided as far as possible during training.
Some horses have chronic lameness that fails to respond to therapy. Some horses with mild or moderate ultrasonographic lesions respond to serial shock wave therapy or radial pressure wave therapy, initially using three treatments at 2-week intervals. There is often substantial improvement in lameness and ultrasonographic appearance of the ligament. Further treatments can be given if required.
Ultrasound-guided injection of core lesions with platelet-rich plasma (PRP) has recently shown encouraging results. Neurectomy of the deep branch of the lateral plantar nerve, with or without fasciotomy, has a role in horses that fail to respond to medical management or in horses with a long-term history of suboptimal performance. Concurrent medication of the tarsometatarsal joint is required for complete resolution of lameness in some horses. The presence of a straight hock conformation or hyperextension of the hind fetlock is a poor prognostic indicator.
In view of the relatively common occurrence of PSD becoming apparent in young horses soon after purchase after preparation for sale by auction, one of the authors (SJD) recommends a 3-month period of rest after purchase and then introduction of a graduated work program to try to prevent PSD becoming clinically apparent.
Proximal Suspensory Desmitis: Forelimbs
Forelimb PSD is seen more often than hindlimb PSD in younger horses and may result from hyperextension of the carpus in extravagantly moving horses, in particular horses volunteering extended trot. PSD often results from the horse working on less than ideal surfaces. Lameness is often unilateral and acute in onset but is sometimes bilateral. Most sound horses resent firm manual squeezing of the body of the SL but the proximal region of the SL is difficult to access by palpation; therefore local analgesic techniques are required to verify the source of pain.
In horses with peracute PSD, slight swelling in the proximal metacarpal region may occur, but this often resolves within 24 hours. The horse may react to firm pressure applied over the proximal aspect of the SL. Lameness may be transient unless the horse is worked again. In these horses, the veterinarian relies on a history of acute-onset lameness that is usually worse with the affected limb on the outside of a circle. However this is not pathognomonic for PSD. Lameness is often easier to feel (by a rider) than to see from the ground. In some horses lameness is never apparent either in hand or on the lunge but is only seen ridden, incongruously with the lame limb on the inside of a circle. The appearance of lameness may be influenced by the diagonal on which the rider sits.
Lameness may be worse after palmar (abaxial sesamoid) nerve blocks, probably because the horse loses some proprioceptive information from the foot and therefore is less able to protect the loading of the suspensory apparatus. Some improvement is often seen after perineural analgesia of the palmar and palmar metacarpal nerves at the junction of the proximal two thirds and distal one third of the metacarpal region, either because of proximal diffusion of local anesthetic solution or the presence of pain in the more distal aspects of the suspensory apparatus. Lameness is usually substantially improved or resolved by blocking the lateral palmar nerve or the palmar metacarpal nerves at subcarpal level. However, in some horses an ulnar nerve block is required. Because of the close proximity of the middle carpal joint capsule, horses with a positive response to subcarpal analgesia should later be evaluated with intraarticular analgesia of the middle carpal joint to exclude articular pain from the carpus.
Radiography is frequently of little or no value in dressage horses with forelimb PSD. Ultrasonography is required to confirm the diagnosis. Use of a virtual convex array transducer and/or acquisition of images obtained while the limb is flexed may be required to identify abaxial lesions. Because subtle lesions may be present and may be a reflection of a previous pathological condition (possibly subclinical), high-quality ultrasonographic images of both limbs are required for comparison, together with knowledge of normal variations. Lesions vary from subtle enlargement of the proximal aspect of the SL with normal echogenicity to large areas of reduced echogenicity. In some young horses no ultrasonographic abnormalities have been detected, but MRI has confirmed the presence of PSD.
Rest, often for 12 to 16 weeks, together with a controlled, ascending walking program (in hand, using a horse walker, or ridden) is the treatment of choice. Careful trimming to restore foot balance is crucial. Intralesional injection using 2 mL of a polysulfated glycosaminoglycan (PSGAG) or PRP may also be tried.
The prognosis is good in horses with early PSD, provided that the horse is managed carefully subsequently, avoiding the medium or extended trot in training. In horses with chronic PSD the risk of recurrence is moderately high. Shock wave therapy has been useful in treating some of these horses. In others injection of mesenchymal stem cells or desmoplasty has produced a successful outcome. In some horses the ultrasonographic appearance may not change substantially, despite a favorable clinical response to treatment, leading to later risk of a false-positive diagnosis in an asymptomatic horse.
Desmitis of the Suspensory Ligament Branches: Forelimbs and Hindlimbs
Desmitis of a branch of the SL is often acute in onset and results in palpable enlargement of the suspensory branch and often moderate lameness. Occasionally, both medial and lateral branches are involved in a hindlimb. The branch is painful to palpation. Diagnosis is confirmed by ultrasonography. Enlargement of the branch is often accompanied by periligamentous fibrosis characterized by subcutaneous echogenic material. There is often a central (sometimes eccentric) hypoechogenic or anechogenic core lesion. The interface between the ligament branch and the proximal sesamoid bone (PSB) may be disrupted. This is best seen on longitudinal images and merits a more guarded prognosis. If both branches in a hindlimb are involved, echogenic material may be visible between the branches. The PSBs may or may not show radiological evidence of enthesopathy, with parallel linear opacities extending from the palmar or abaxial margin. Dystrophic mineralization within the SL branch is occasionally seen on ultrasonographic and radiographic images.
Treatment is prolonged rest (4 to 6 months) with a slow return to exercise. Intralesional injections using 1 mL of a PSGAG may be tried but generally have met with disappointing results. Counterirritation (pin firing) has been tried on horses with old, indurated lesions associated with chronic lameness, but again generally with disappointing results. Some horses have responded to intralesional treatment with β-aminopropionitrile fumarate. Encouraging results also have been obtained recently with shock wave therapy (three treatments at 2-week intervals), combined with a controlled walking exercise program for 3 to 4 months. However, the presence of extensive periligamentous fibrosis is a poor prognostic indicator.
The risk of recurrence is high. Any predisposing causes such as limb deviations or lateromedial imbalance of the feet should be corrected or at least adjusted.
Synovitis or Osteoarthritis of the Distal Interphalangeal Joint
Pain arising from the distal interphalangeal (DIP) joint is a frequent diagnosis in all sports horses. The unique anatomical position of the DIP joint, with the forces distributed on it through the rigidity of the hoof capsule and the forward thrust of the deep digital flexor tendon (DDFT) and the navicular bone during weight bearing and limb protraction, are likely to be contributory factors. Lateral-to-medial imbalance of the foot also contributes to the joint trauma in many horses.
The diagnosis is made by comparing the response to intraarticular analgesia with that of (minimal volume, 0.5 mL per branch) perineural analgesia of the palmar digital and palmar (abaxial sesamoid) nerves as well as intrasynovial analgesia of the navicular bursa. The interpretation of the response to intraarticular analgesia is not black and white, and the clinician must learn to build up a picture of a composite, often complicated distal forelimb lameness. Recent studies have confirmed that intraarticular analgesia of the DIP joint is not specific and can influence pain associated with the navicular bone, distal phalanx, DDFT, and even subsolar tissues. A rapid (within 5 minutes) positive response to a small volume (maximum of 6 mL) of local anesthetic solution may be a good indicator of the possible response to subsequent intraarticular medication. A good response to subsequent treatment requires at least 75% clinical improvement after intraarticular analgesia, together with absence of relevant radiological changes involving the DIP joint or the navicular bone.
Radiological changes usually involve the extensor process of the distal phalanx and the dorsoproximal margin of the navicular bone. One should remember that considerable variation exists in the shape and size of the extensor process between limbs and within sound horses. Minor modeling changes may not be of clinical significance. Small, mineralized fragments proximal to the extensor process may be seen incidentally. Large fragments may require surgical removal to prevent secondary osteoarthritis (OA).
Intraarticular medication using a number of individual drugs or a combination of drugs has given encouraging results, although results vary among clinicians and populations of horses. Horses with recent onset of usually unilateral lameness with palpable distention of the DIP joint capsule may respond favorably to 10 mg of triamcinolone acetonide or up to 40 mg of methylprednisolone acetate, combined with a short period of controlled walking exercise (e.g., 2 weeks on a horse walker) followed by 2 weeks of ridden walking. Injection with hyaluronan probably will provide a similar response in such horses. However, in horses with more chronic lameness, the response to corticosteroids is less favorable, and the most successful long-term results have been seen after a triple series of intraarticular injections of a PSGAG.8 PSGAGs received some negative press after a research study in North America in 1989 suggested that PSGAGs have a potentiating effect on a subinfectious dose of Staphylococcus aureus in a joint. Subsequently, this preparation has been used sparingly intraarticularly and in many horses only in combination with intraarticular amikacin. We have not seen any negative reaction (inflammatory or infectious) to numerous intraarticular injections of PSGAGs and do not use systemic or intraarticular antibiotics. Strict asepsis and a skillful technique are essential. Because of its distal location in the limb, we recommend that DIP joints always be bandaged for at least 24 hours after injection. Eighty-two percent of dressage horses returned to soundness after PSGAG medication of the DIP joint, compared with 65% in a similar-sized group of horses competing in cross-country jumping.8 In most horses the initial triple injection proved adequate, and additional injections in horses successfully treated using this technique were rarely needed.
Autologous conditioned serum containing interleukin-1 receptor antagonist protein (IRAP) has proved beneficial for management of horses with DIP joint or navicular bursa pain.
Corrective shoeing by improving the foot-pastern axis and reestablishment of correct hoof balance should always be combined with intraarticular medication, but changes should be performed slowly. Heart bar shoes often are used for an initial 3- to 6-month period.
Desmitis of the Accessory Ligament of the Deep Digital Flexor Tendon: Forelimbs
Desmitis of the accessory ligament of the DDFT (ALDDFT) frequently occurs as an acute injury associated with sudden onset of lameness and palpable inflammation (heat and swelling) in the proximal one third or one half of the metacarpal region. Overextension of the carpus caused by imbalance in young horses or resulting from imperfect working surfaces is often believed to be a contributory cause.
The diagnosis is confirmed by ultrasonography in both transverse and longitudinal planes. There is often substantial enlargement of the ALDDFT, together with loss of definition of the margins and areas of reduced echogenicity. A definite, hypoechogenic core lesion is recognized infrequently.
Horses with desmitis of the ALDDFT respond better to a controlled ascending walking exercise program than to complete box rest. Controlled walking for 3 to 6 months often is required in horses with severe desmitis, despite the initial lameness often resolving considerably sooner. The risk of recurrence is moderately high. Local invasive treatment of desmitis of the ALDDFT seldom has been rewarding, although some horses have responded favorably to treatment with β-aminopropionitrile fumarate and more recently with PRP.
Desmitis of the Accessory Ligament of the Deep Digital Flexor Tendon: Hindlimbs
Desmitis of the proximal aspect of the ALDDFT of hindlimbs results in acute-onset lameness usually associated with soft tissue swelling in the proximoplantar aspect of the metatarsal region. Diagnosis is confirmed by ultrasonographic examination; it is important to examine the limb from the plantaromedial aspect; otherwise, lesions may be missed (see Figure 71-3).
Osteoarthritis of the Centrodistal and Tarsometatarsal Joints
Lameness or poor performance (e.g., inability to collect in order to perform piaffe or passage) associated with pain arising from the centrodistal (CD) or TMT joints occurs frequently in dressage horses. Likewise, a horse with an outstanding freedom of movement in the trot may have an unexplainably poor canter associated with distal hock joint pain. In collected paces there is increased tarsal loading and joint compression,9 which may predispose to tarsal injury in dressage horses. The pattern of subchondral bone thickness in the distal tarsal bones reflecting loading pathways is different in elite performance horses compared with general-purpose horses.10 This may be related to circling and other specific movements, and potentially predisposes to pathological change.
A poor correlation exists between the clinical signs, including response to intraarticular analgesia of the TMT and CD joints, and the radiological appearance of these joints. Many dressage horses have confirmed pain from the joints but have fairly equivocal, if any, radiological changes. One should remember that the degree of joint collapse and osseous ankylosis always is underestimated from radiographs because of the curvilinear nature of the joints and the low radiodensity of immature bone bridging the joint centrally. Nuclear scintigraphy may be a sensitive indicator of increased bone modeling in the absence of radiological abnormalities or in horses with equivocal changes and also can be helpful in horses with subtle lameness, when the response to local analgesic techniques is difficult to interpret. Alternatively, diagnostic medication with intraarticular corticosteroids may be helpful.
Pain is often bilateral, and the presenting problem is often shortening of the hindlimb stride and an inability to collect, rather than overt lameness. An advanced horse may show irregularities of rhythm in piaffe and passage. Clinical signs mimicking back pain, rather than overt lameness, may be present.
Most horses respond to intraarticular analgesia of the TMT and CD joints, although occasionally a better response is seen after fibular and tibial nerve blocks or after treatment of the joints. Intraarticular analgesia of the TMT joint and the response to subtarsal analgesia should be compared. In horses with advanced radiological changes, false-negative responses to intraarticular analgesia may occur.
Horses with few or no radiological changes may respond satisfactorily to intraarticular medication with a corticosteroid (e.g., up to 40 mg of methylprednisolone acetate or 10 mg of triamcinolone acetonide), IRAP, or 1 mL of a PSGAG if lameness is of longer duration. Medical treatment often is combined with a program of controlled walking exercise for 2 to 4 weeks (pending response to treatment), together with alterations of the shoeing. Horses that tend to plait or swing the affected limb axially during protraction may benefit from a lateral extension shoe, which may help to normalize posture and hindlimb gait pattern with an additional effect on secondary back pain.
Repeated medication of the joint(s) may be required at monthly or quarterly intervals. A longer response may be achieved by combined use of corticosteroids and hyaluronan.
Additional PSGAG medication given intramuscularly on a weekly basis (500 mg/mL, 7 times 5 mL) may be beneficial. Tiludronate infusion has given poor results. Glucosamines and chondroitin sulfate given orally on a daily basis are often administered, but clinical efficacy remains largely unproven.
If substantial radiological changes are present, the joint is changed irreversibly, and the horse fails to respond to repeated intraarticular medication, fusion of the joints by surgery or by intraarticular injection of sodium monoiodoacetate or ethyl alcohol can be considered, but the prognosis for high-level dressage is guarded.
Synovitis of the Middle Carpal Joint
Lameness associated with pain in the middle carpal joint has been seen in many dressage horses, in particular young horses that still may be struggling to establish balance and synchronicity in all paces with the additional weight of the rider. Lameness is often mild and most frequently unilateral, being most noticeable when the limb is on the outside of a 10-m diameter circle. Intermittent hyperextension of the carpus, often on a tight circle, is believed to be involved.
If the response to analgesia of the middle carpal joint is positive, the proximal SL should be examined by ultrasonography to preclude injury.
Usually, no radiological or ultrasonographic changes are present involving the middle carpal joint. Arthroscopy of the middle carpal joint sometimes reveals damage to one (most frequently the medial) or both of the palmar intercarpal ligaments, which show edema, petechial hemorrhage, and fraying of superficial fibers.
Most horses respond well to intraarticular medication using a triple series of 1 to 2 mL of a PSGAG given 8 days apart, or treatment with short-acting corticosteroids combined with hyaluronan. Six to 8 weeks of ridden walk or on a horse walker should be followed by a modified training program for at least another 3 months.
Synovitis or Osteoarthritis of the Metatarsophalangeal and Metacarpophalangeal (Fetlock) Joints
Fetlock joint disease is not a common problem in dressage horses and certainly does not seem to be as common in this type of equestrian sport as in others. The absence of galloping across often firm and irregular surfaces associated with cross-country jumping is a likely explanation.
The diagnosis is confirmed by palpation and intraarticular analgesia. In the absence of radiological changes, intraarticular medication using a corticosteroid (e.g., 10 mg of triamcinolone acetonide), together with 2 mL hyaluronan in horses with synovitis, or 1 mL of PSGAG in horses with more long-standing OA, frequently has proved successful. IRAP treatment has also proven successful. Generally the response to medication is good and the likelihood of recurrence is low in the forelimbs. The response is poorer in hindlimbs. Horses with radiological abnormalities consistent with OA warrant a more guarded prognosis.
Palmar or Plantar Annular Ligament Desmitis
Desmitis of the palmar (plantar) annular ligament (PAL) occurs more commonly in forelimbs than in hindlimbs and usually results in acute-onset lameness. The PAL has localized heat and is palpably enlarged, with pain elicited by firm pressure. Mild distention of the digital flexor tendon sheath (DFTS) may occur. Diagnosis is confirmed by ultrasonography. The PAL is thickened, with a diffuse reduction in echogenicity or focal hypoechogenic areas. Horses with acute desmitis usually respond well to box rest and controlled walking exercise for 3 months. In the acute phase, nonsteroidal antiinflammatory drugs (e.g., phenylbutazone 2 g bid PO for 5 days) are beneficial. If associated with a degree of synovitis of the DFTS, intrasynovial treatment of the DFTS with a corticosteroid may assist in resolution of lameness.
Radial pressure wave treatment has also proven a useful alternative to surgery. Tenoscopic resection of the ligament is reserved for horses not responding to conservative management.
Tenosynovitis of the Digital Flexor Tendon Sheath
Tenosynovitis of the DFTS often results in sudden-onset lameness associated with distention. Some horses have long-standing distention of the DFTS without lameness (windgalls), especially in the hindlimbs, but subsequently develop clinically important tenosynovitis. Constriction of the DFTS by the PAL may be apparent. Lameness may vary from mild to severe and usually is accentuated by distal limb flexion. If distention of the DFTS is acute in onset, then local analgesia is usually unnecessary. However, if distention of the DFTS has been present for some time, then the source of pain should be confirmed by local analgesia. Intrathecal analgesia of the DFTS usually results in substantial improvement in lameness but often does not alleviate it fully. Perineural analgesia of the palmar or plantar (midcannon) and palmar metacarpal or plantar metatarsal nerves usually eliminates lameness. Improvement sometimes is seen after perineural analgesia of the palmar nerves at the level of the PSBs. Excluding the metacarpophalangeal joint as a potential source of pain by intraarticular analgesia may be necessary.
Ultrasonographic examination should be performed in the metacarpal and pastern regions. Usually an abnormal amount of fluid within the DFTS allows better visibility of the normal synovial plicae extending from the medial and lateral margins of the DDFT in the distal metacarpal region and the synovial fold on the palmar aspect of the DDFT in the pastern region. These should not be mistaken for adhesions or tears of the DDFT. In horses with chronic tenosynovitis, the DFTS wall may be thickened, with echogenic bands within the DFTS representing adhesions. Ultrasonography frequently underestimates adhesion formation. The superficial digital flexor tendon (SDFT) and DDFT should be inspected carefully, because tenosynovitis may be secondary to a primary pathological tendon condition. Lesions of the DDFT occur more commonly, either as ill-defined core lesions or marginal tears, most frequently of the lateral margin. The latter can be difficult to detect by ultrasonography. Enlargement of the cross-sectional area of the tendon compared with the contralateral limb suggests a lesion, which may be confirmed only by tenoscopic evaluation of the sheath. Mineralization within the DDFT warrants a guarded prognosis. Horses with early tenosynovitis without adhesions or detectable lesion of the DDFT respond well to intrasynovial administration of a corticosteroid (e.g., 10 mg of triamcinolone acetonide) or 2 mL of hyaluronan, together with a pressure bandage and box rest with handwalking for 4 to 6 weeks. Horses with small core lesions of the DDFT may respond satisfactorily to conservative management, but those with large core lesions have a more guarded prognosis. However, ultrasound-guided injection of cultured mesenchymal stem cells has yielded encouraging results in a small number of horses.
If the horse fails to respond adequately to medical therapy, then surgical exploration is warranted. Tenoscopic evaluation should be performed to evaluate the extent of adhesion formation and to detect longitudinal tears in the medial or lateral margins of the DDFT, which may extend proximally under the manica flexoria. Resection of intrasynovial adhesions and lavage, with or without resection of the PAL, may resolve the problem. Horses with lesions of the DDFT that may be debrided warrant a more guarded prognosis. Surgery is frequently followed by intrasynovial injection of 2 mL of hyaluronan, repeated 4 to 6 weeks later to reduce inflammation and to try to prevent adhesions from reforming.
The response to surgery depends on the chronicity of the problem, the amount of intrasynovial adhesions, and the presence of lesions of the DDFT. Horses with lesions involving the forelimbs appear to have a better prognosis than those involving the hindlimbs. Surgery is accompanied by 8 to 12 weeks of absence from training, although controlled walking in hand or on a horse walker is essential to try to stretch any adhesions that reform.
Proximal Palmar Cortical Stress Fracture of the Third Metacarpal Bone
Proximal palmar cortical stress fracture of the third metacarpal bone (McIII) occasionally is seen in dressage horses, especially young horses, with an acute onset of moderate-to-severe lameness. Hyperextension of the carpus, imbalance, and limb asynchrony in immature horses are believed to be contributing factors.
The diagnosis is sometimes suspected when pain is induced by digital pressure on the palmaroproximal aspect of the McIII. When the horse trots on a firm surface, the lameness tends to increase the farther the horse trots. If the horse turns and then trots again, lameness appears to be improved and then increases again. Lameness usually is improved substantially by perineural analgesia of the palmar metacarpal nerves in the subcarpal region. If the fracture extends into the carpometacarpal joint, improvement also may be seen after intraarticular analgesia of the middle carpal joint.
On radiographs a fracture may be recognized on a dorsopalmar image as a linear radiolucent line, usually in the medial aspect of the McIII and extending up to 8 cm, possibly with surrounding increased radiopacity. In some horses a fracture line cannot be seen, although increased radiopacity is present. In some horses no radiological abnormality is identified. In these horses, the diagnosis is confirmed by nuclear scintigraphy, with focal intense IRU in the proximal palmar aspect of the McIII. Alternatively, MRI can be used but is generally unnecessary.
Treatment is complete box rest for 6 weeks, followed by 6 weeks of controlled walking exercise. The prognosis is good, and the likelihood of recurrence low.
Thoracolumbar and Sacroiliac Pain
Thoracolumbar and sacroiliac region pain are frequent causes of reduced performance in dressage horses. In a questionnaire survey concerning British dressage horses, so-called back pain occurred in 25% of horses in a 2-year period.4 However, in a high proportion of horses lameness was subsequently identified. It is therefore important to appreciate that the appearance of back stiffness and recognition of back pain may reflect an underlying lameness, which is sometimes subclinical. Although caudal thoracic back muscle soreness may be secondary to primary hindlimb lameness, primary back pain does occur commonly and is usually not associated with overt lameness, although poor hindlimb impulsion or intermittent hindlimb gait irregularity can be seen. Sacroiliac joint region pain often develops secondarily to hindlimb PSD. The horse may have a history of unwillingness to perform certain movements, stiffness, loss of impulsion and cadence, loss of action, or being less easy to work in a correct outline. Sometimes bucking or other nappy (resistant) behavior remain the only clinical observations. The horse usually moves better on the lunge than when being ridden. The most common causes of back pain include the following:
Definitive diagnosis of the cause of back pain can be a diagnostic challenge. It may be helpful to work in conjunction with a skilled physiotherapist or chiropractor. Liaison with an experienced high-quality saddle fitter may also be valuable. Obvious causes such as ill-fitting saddle or the position of the rider should be eliminated first before proceeding with more sophisticated diagnostic tests such as radiography, ultrasonography, nuclear scintigraphy, and thermography. If back muscle tension or spasm is obvious, assessing the response to treatment using physiotherapy (e.g., manipulation and therapeutic ultrasound) or antiinflammatory medication may be worthwhile before further investigation.
Thermography provides pictorial images of the surface temperature of the body, which gives a physiological identification of changes in tissue perfusion or sympathetic neuromuscular dysfunction. Thermography is a useful tool to demonstrate to an owner the effect of a poorly fitting saddle or the rider sitting crookedly and also may be useful in identifying acute superficial ligament or muscle injuries.
Nuclear scintigraphy may be more sensitive than radiology for detecting lesions in the thoracolumbar or sacroiliac regions, but radiology potentially gives more structural information, such as the proximity of the dorsal spinous processes. It is important to verify the clinical significance of any lesions identified by infiltration of local anesthetic solution whenever possible. If dorsal spinous processes are extremely crowded, injecting between them may not be possible, but injecting around them (20 to 50 mL of mepivacaine) usually results in substantial improvement within 15 minutes of injection, although this may confirm “back pain” rather than pain specifically arising from impinging dorsal spinous processes.
Ultrasound guidance is necessary for infiltration around synovial articulations.
Treatment is aimed at removing any predisposing factor and control of pain. Local infiltration with corticosteroids (e.g., methylprednisolone acetate combined with mepivacaine) or Sarapin is successful in some horses. If pain associated with impinging dorsal spinous processes fails to be controlled by medical management, surgical treatment should be considered. Infiltration of corticosteroids, Sarapin, or a sclerosing agent, P2G (Martindale Pharmaceuticals, Romford, Essex, United Kingdom), around the sacroiliac joints produces clinical improvement in some horses with pain associated with these joints. Acupuncture can be a useful adjunctive therapy for pain management. The daily work pattern and training methods used by the rider and trainer should also be reviewed for successful long-term management. Regular lunge work in a Pessoa may be of benefit. Exercises to increase core muscle strength are important. Slow warm-up in a pace that the horse finds easy is also valuable.