Chapter 118Lameness in Endurance Horses
Evolution of Endurance
Modern endurance is the most rapidly evolving equine sport. It has its roots in the long distance races of the ancient Bedouin across the desert. Later British and American cavalry used endurance tests as part of their military training, and nineteenth century Austrians had a Vienna to Budapest ride. Despite this long history, organized endurance riding is a young sport. The first modern endurance ride, the 100-mile (160-km) Tevis Cup from Nevada to California, has been run every year since 1955. The Tom Quilty Gold Cup, a prestigious 100-mile endurance race named for its founder, was established in 1966 and is held every year in a different part of Australia. The oldest endurance organization, the American Endurance Ride Conference, has been in existence only since 1972. Since 1984, all international endurance competitions have been held under the auspices of the Fédération Équestre Internationale (FEI). The Endurance World Championships are held every 2 years in a different host country, and endurance is now the fastest growing FEI sport. More countries participate in international endurance championships than in the international championships of any other FEI discipline.
Description of the Sport
The FEI Rules for Endurance describe the sport as a test of “the competitor’s ability to safely manage the stamina and fitness of the horse over an endurance course in a competition against the track, the distance, the climate, the terrain and the clock.” It is the clock, however, that determines the winner because the winner is the competitor who completes the course in the shortest time and passes the final veterinary inspection and forensic testing. As the sport of endurance has grown, it has come under intense scrutiny with regard to equine welfare. In addition, there is a great deal of debate within the endurance community as to whether the more media- and spectator-friendly events favoring increasing speeds over shorter distances (120 km) are preferable to the more traditional sport of slower speeds over longer distances and more challenging terrain. In March 2008, an Endurance World Forum was held in Paris to discuss these and other concerns, and a task force was appointed to revamp current rules governing the sport. The new rules went into effect in 2009; the current championship distance remains unchanged at 160 km (100 miles). The 2008 Endurance World Championships in Malaysia marked the first time that this event was internationally televised.
Each country has its own National Federation, and national competitions may be run under national rules. All international and championship competitions are run under FEI rules, and there are rigorous qualification requirements that must be met to participate. Concours de Raid d’Endurance International (CEI) competitions are divided into 4-star (championship level) through 1-star (low-level) events, depending on the distance covered and age requirements of the horse. Horses must be at least 5 years of age to compete in qualifying events, with age requirements increasing through the star rating. Horses must be at least 8 years of age to compete in championships and CEI 4-star competitions.
Veterinary Controls
Veterinary controls are an integral part of endurance events, and horses must undergo and pass an initial veterinary inspection and subsequent inspections after each phase of the competition. The total distance of the ride is divided into segments of 20 to 40 km, usually laid out in a cloverleaf pattern with a central Vet Gate area. After riding each section, the competitor must pass the Vet Gate or veterinary checkpoint, where panels of veterinarians evaluate horses for lameness and metabolic criteria. The heart rate must be at or less than 64 beats per minute (bpm) within 20 minutes of arrival from the course to each Vet Gate and within 30 minutes of arrival to the final inspection after crossing the finish line. FEI rules allow the Veterinary Commission the latitude to lower the heart rate criterion if extreme weather conditions are deemed severe enough to warrant it.
The time is taken when the competitor comes in off the course into the crewing area. The competitor has 20 minutes in which to “clock in” to the Vet Gate, or the horse will be eliminated on a time penalty. Heart rate decreases to less than 64 bpm within 1 to 3 minutes of arrival in most elite endurance horses. The time is recorded again when the horse enters the Vet Gate. There is a mandatory hold time after each phase of the competition, which begins from the time of entry into the Vet Gate. Therefore speed of entry into the Vet Gate is a critical opportunity to gain time. If the horse’s heart rate is higher than 64 bpm on initial inspection he is “spun” or required to go out of the Vet Gate and return for a reinspection when the heart rate meets the 64-bpm criterion. A horse is permitted one reinspection within the 20-minute time limit at the Vet Gates, but no second chance to meet the heart rate requirement is permitted at the finish. Intensive crewing (rapid cooling with copious amounts of ice water) is common at high-level competitions, and top-level horses generally come in off the course, have saddles removed, are cooled, have the heart rates checked, and go directly into the Vet Gate. Most championship venues have instituted digital heart rate monitors on which the heart rate for each horse is publically displayed at the end of the trotting lane. A second heart rate is measured by direct auscultation 1 minute after the commencement of a 40-meter trot, and the difference between the first and second heart rates is calculated. This is known as the cardiac recovery index (CRI) or Ridgway Test, after Dr. Kerry Ridgway. Although not a criterion for elimination in and of itself, a positive CRI, in which the second heart rate is elevated more than several beats above the first one, is an indication that the horse merits further evaluation. Other metabolic parameters, such as mucous membrane color, capillary refill time, skin turgor, and auscultable intestinal borborygmi, are checked and recorded. The presence of any saddle sores, girth rubs, or bitting lesions is also noted. A heart rate above the maximum allowed, injury, or “consistently apparent” lameness are grounds for elimination. Synchronous diaphragmatic flutter is a common condition in endurance horses and may be grounds for elimination if other metabolic abnormalities are concurrently present. Time-keeping systems for arrival from and departure to the course are automated at high-level events, with riders presenting a digitized “slash card” at timing checkpoints. After passing the veterinary examination, the horse is returned to the crewing area, where it is fed, groomed, and watered before called to return to the course. The horse is not permitted to leave the exit gate until the hold time for each phase is completed. A computerized record of the competitor position, exit time, time taken for the horse to present, and average speed is available at each Vet Gate and at the finish. Endurance horses are not permitted to compete on performance-enhancing medication, and medication control programs are in place to test for substances that are not permitted, in accordance with FEI rules for all equestrian disciplines.
Although national competitions may use the same veterinarians for control and treatment, FEI competitions require separate veterinarians dedicated to each. There are specific requirements regarding the number of commission and treatment veterinarians per number of competitors according to the star rating of the competition. Typically, a horse that is eliminated by a control (Commission) veterinarian for a lameness or metabolic problem is referred to the treatment veterinarian for further evaluation. If the treatment veterinarian deems that treatment is prudent, it is provided at a field clinic at the ride site, or in some cases the horse is transported to a local referral veterinary clinic or to its home stable for treatment. Team veterinarians are usually so busy with other competitors that have not been eliminated that they are happy to have the assistance of the treatment veterinarian. However, it is important that treatment and team veterinarians closely liaise with one another to provide the best possible care. Ride site clinics at large venues or championships offer sophisticated treatment (e.g., blood analysis, fluid therapy, digital radiography, ultrasonography, electrocardiography, endoscopy), and only those horses that require continued care, further diagnostics, or surgical treatment are referred.
Top-level international modern endurance is an extreme sport. Competitors and experienced endurance veterinarians recognize that proactive provision of postcompetition fluid therapy is beneficial in rapidly returning the horse to normal hydration and homeostasis. In my opinion, fluid therapy should not be withheld in an effort to reduce “treatment rates,” and competitors whose horses receive fluid therapy to optimize recovery should not be penalized.
Type of Horse
Most endurance rides are open to horses of any breed, but horses of Arabian extraction are most popularly used for endurance riding because they have light build and stamina for long distance rides. Larger, heavier framed horses are less able to sustain the speed required over the distances traveled. Endurance horses, compared with other athletic horses, tend to be small and light, although in the past 10 years there has been a trend toward taller more robust Anglo-Arab types. Like human marathon runners, good endurance horses tend to be ectomorphs, but speed, cardiac recovery capacity (the ability to rapidly decrease the heart rate after a fast gallop over long distances), and conformation that is likely to withstand the pressure of the demands to which endurance horses are subjected are currently the most sought-after qualities.
Training Methods and Competition Speeds
Training methods differ considerably among trainers, but most would agree that it takes 2 to 3 years of training to make a good endurance horse. Training distance and frequency depend largely on individual circumstances (terrain, weather, availability of pasture, or turn-out paddocks), but most regularly competing endurance horses are ridden 6 days a week. A typical program might include daily rides of 10 to 20 km, with weekly or 10-day interval 30- to 80-km rides. Horses are ridden at a walk, trot, and canter, with the proportion of the time spent at each gait varying considerably. Horses being prepared for a 100- to 160-km ride will usually perform a 60- to 80-km training ride on at least two occasions before competition. New qualification requirements mandate that horses complete successive rides at lesser distances before being permitted to compete at the next increased distance level. Overtraining of endurance horses tends to be more of a problem than undertraining, particularly by novice trainers.
Endurance competition has rapidly evolved from amateur operations where the same person owned, trained, and rode the same horse for many years, competing for pleasure, with small prizes in kind, to large stables with numerous horses run by professional trainers competing for international recognition, luxury automobiles, and hundreds of thousands of dollars in prize money. The value of a horse winning or running successfully in a prestigious international competition increases exponentially. Speeds at high-profile rides over mountainous terrain have not substantially changed, but as the sport has continued to develop, speeds of competition over flat terrain have increased dramatically. Essentially, at the highest levels the sport has changed from endurance riding to endurance racing. The winner of the 2008 World Championship in Malaysia averaged 18 km/h (5 m/sec) for 160 km, at night, in a torrential downpour, and with high humidity. A world record time for 160 km of 6 hours, 28 minutes, 28 seconds riding time was set in January 2008. Although the total average speed for all phases was 24.71 km/h (6.86 m/sec), the final 19-km loop was covered at an average speed of 30.29 km/h (8.41 m/sec). It must be borne in mind that as an average over 19 km, actual speeds for short bursts can be substantially higher. As winning speeds at the classic 160-km distance have increased, speeds at the shorter 120-km and 100-km distance have increased even more. In these races, average speeds for some phases reach more than 36 km/h (10 m/sec), which is the equivalent of an “open gallop.” It is not unusual to have flying finishes with fractions of seconds separating finishing places. Ten years ago this would have been unheard of. Opinions differ as to whether this is desirable progress, but from a veterinary standpoint, at rides where speeds are increasing, it means that we are beginning to see more flat-racing types of musculoskeletal injuries, as well as serious metabolic abnormalities. Although water is available on the course every 5 to 8 km, riders competing at distances less than 160 km rarely stop on the course to water their horses. The horses are watered when they come into the crewing area.
Course Terrain
Endurance horses compete and train over some of the most highly variable terrain of any sports horses, including rocky mountains, through creeks, across sandy deserts, along tarmac, gravel, or dirt roads, and across grassy fields, depending on where the ride is held. Course terrain clearly has a bearing on the type of injury, generally in a straightforward way. Stone-bruised feet and painful joints are more common when horses are worked on hard, rocky ground, whereas ligament and tendon injuries are more often observed in horses worked on soft or sandy ground. Downhill grades, if slippery or taken at speed, tend to produce a plethora of dorsal carpal injuries as a result of falls. A relatively recent innovation is the grading and harrowing of long stretches of the course, much like a racetrack without the cushion. Many large endurance stables now train horses on racetracks. This has resulted in an increase in racing-type fractures and superficial digital flexor tendon (SDFT) injuries.
Lameness and Conformation
Lameness in endurance horses can be divided into three categories involving (1) ligaments or tendons, (2) muscle, or (3) joints, bones, or feet. Lameness affecting endurance horses can also be separated into transient problems that may be cause for elimination on the day of competition but then resolve and more persistent problems that are likely to be recurrent. In the relatively recent past, many endurance horses competed over an 8- to 10-year period, and horses with the most glaring conformation defects tended to weed themselves out by attrition. Developments in the sport, most notably increases in speeds of competition, have paralleled the shortening of the competitive life of top-level endurance horses by several years. Astute veterinary advisors make a concerted effort to avoid young horses with flat, asymmetrical, or contracted feet, major angular limb deformities, offset cannon bones, and long, slack, or short, upright pasterns because these may contribute to later unsoundness problems.1 Although poorly conformed horses may be successful in the short term or at less-demanding levels of competition, it is an exceptional poorly conformed horse that stays sound and is successful over the time that it takes to reach championship level.2 Flaws that are not extreme may be present without compromising the overall function of the horse but are preferentially avoided when possible. Horses with toe-in conformation appear to be more likely to develop splint exostoses that may impinge on the suspensory ligament (SL), causing desmitis, and horses with recurrent suspensory desmitis are ultimately unsuitable for endurance.
The Lameness Examination and Proceeding without a Diagnosis
A lameness examination in any horse is most easily and efficiently performed when the lameness is visible, and the endurance horse is no exception. It is usually not possible to make a specific diagnosis if a horse is not lame at the time of examination. Endurance horses are problematic because often a mild transient lameness that resulted in elimination from competition may not be visible the next day or even later the same day, although many horses have painful superficial digital flexor tendons (SDFTs) and SLs after a race. Low-grade, inconsistent, nonspecific lameness that cannot be localized is a frustratingly common scenario faced by veterinarians charged with keeping endurance horses sound. When possible, watching the horse trot while lame, application of hoof testers, noting the presence of any palpable abnormalities, and response to flexion or other manipulative tests help to narrow the possible causes. Diagnostic analgesia, adhering to the principle of starting at the bottom and working upward, is the standard most useful means of localizing the source of pain causing lameness when no palpable abnormalities are present. Sometimes, despite a careful and complete lameness examination, diagnostic analgesia, and ancillary diagnostic aids such as radiography, ultrasonography, scintigraphy, and even magnetic resonance imaging (MRI), a specific diagnosis cannot be reached. Some horses never “block out.” A careful neurological examination should then be performed because subtle neurological deficits may mimic or produce lameness. In other horses, pain causing lameness can be isolated to a specific region, but no lesion can be found. Like other athletic horses, endurance horses may have subtle gait abnormalities emanating from numerous areas, all contributing to suboptimal performance but difficult to identify individually. The advent of MRI has elucidated some previously elusive conditions of the distal aspect of the limb, especially in the proximal palmar metacarpal region and the foot.
Horses with pain causing lameness localized using diagnostic analgesia or clinical examination to a specific region in which there are no detectable radiological or ultrasonographic lesions should be reexamined by the most appropriate conventional imaging modality after 2 to 4 weeks or should undergo scintigraphic or MRI examination if warranted by the degree of lameness present. Stress fractures are particularly notorious for not being detectable on the first radiological examination and being readily apparent later. However, stress fractures are usually detectable using scintigraphy or MRI. If the lameness has resolved and no lesion is detected on a recheck examination, it is reasonable to return the horse to light training. If lameness recurs, the lameness examination should be repeated.
Although “full-body” scintigraphy is ideally avoided, it is sometimes beneficial in horses that have an acute lameness that cannot be specifically localized. We have recognized the propensity for stress fractures to turn into catastrophic fractures; therefore obtaining a specific diagnosis is increasingly important. It should be borne in mind that the percentage of positive scintigraphic findings is higher for horses with acute, severe lameness than in those with chronic, low-grade lameness. Sometimes, despite every attempt at imaging and reimaging, the clinician is still left with a lame horse and no diagnosis. When this point is reached, a prolonged rest period (8 to 12 months) may be helpful.
Common Causes of Lameness in Endurance Horses
The principal cause of lameness is proximal palmar metacarpal pain,1-4 but the other top 10 causes of lameness in endurance horses tend to vary somewhat in ranking from season to season. Although the problems listed here are the most frequently encountered, not only is the ranking variable, but also pathology in the proximal palmar metacarpal region and in the fetlock can be divided into subcategories that may overlap and are difficult to separate. The advent of the availability of sophisticated imaging techniques, especially MRI, has made it more difficult to write a list of the 10 most common causes of lameness in endurance horses because of the ability to recognize to a greater degree the interrelatedness of the anatomical structures involved. In addition, some injuries appear to be part of a spectrum or continuum that progresses through phases with time. Bearing this in mind, the following are the lameness problems seen most commonly:
Proximal Palmar Metacarpal Pain
The leading cause of chronic or recurrent lameness in endurance horses, regardless of terrain, is pain in the proximal palmar metacarpal region. Proximal suspensory desmitis (PSD) is often the primary problem. Pain associated with the lesions of the palmar aspect of the third metacarpal bone (McIII) or less commonly pain associated with the second (McII) or the fourth (McIV) metacarpal bones, or the interosseous ligaments between the McII and McIII and the McIV and McIII may contribute to lameness. Injury to the proximal metatarsal region of the hindlimb also occurs but is less common.
Proximal Suspensory Desmitis
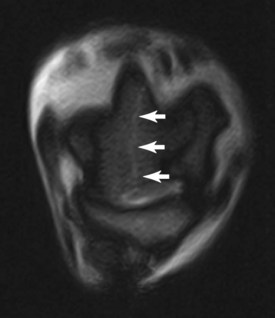
Desmitis of the SL typically develops in the later stages of a race when the horse becomes fatigued but may occur in the earlier stages of a race in an unfit horse or a horse that has had previous SL injury. It is also a common training injury. Lameness caused by PSD may be sudden in onset and severe or be more insidious in onset. Often, there is little or no detectable swelling, but careful palpation may elicit a painful response. However, many horses resent palpation of the proximal aspect of the SL and will give a false-positive response to even the most gentle and careful palpation. Horses with forelimb PSD are usually positive to distal limb flexion. Diagnostic analgesia is critical to definitively localize pain to the proximal palmar metacarpal region. The proximal palmar metacarpal region may be desensitized by (1) blocking the deep branch of the lateral palmar nerve laterally at the edge of the accessoriometacarpal ligament distal to the accessory carpal bone and the medial palmar nerve (high two-point or Wheat block, after Dr. John D. Wheat), (2) direct infiltration, (3) performing a high palmar and palmar metacarpal nerve block (“high four-point”), or (4) blocking the lateral palmar nerve in the longitudinal groove on the medial aspect of the accessory carpal bone.5 The first and last techniques have the advantage of avoiding inadvertent penetration of the distal palmar outpouchings of the carpometacarpal joint and the last technique avoids penetration of the carpal canal. Although lameness in endurance horses is seldom localized to the carpus, carpometacarpal joint pathology is increasingly recognized. When a high index of suspicion of proximal palmar metacarpal pain exists but the horse does not improve with one of the blocks, the block should be repeated, or one of the others should be tried because there may be some variability in response. Ultrasonographic examination of the SL is generally performed if diagnostic analgesia has localized the source of the pain causing lameness to this area. Ultrasonography is a less precise imaging modality than MRI, but it is more accessible and readily available to a general practitioner and remains a highly useful technique. PSD is characterized by loss of echogenicity of the dorsal-most fibers immediately distal to the carpometacarpal joint. Symmetry is important in determining whether acute SL injury has occurred, and the further distally the fiber loss extends (from zone 1 into zone 2), the worse the injury.6 Both forelimbs should be compared. Often, bilateral change is present, but the clinically affected side appears less echogenic (Figure 118-1). Examination of the limb in flexion with the digital flexor tendons and accessory ligament of the deep digital flexor tendon (DDFT) pushed aside can allow more complete evaluation of the medial and lateral lobes of the suspensory origin. If the pain causing lameness has been localized to the proximal palmar metacarpal region but the ultrasonographic appearance of the SL is within normal limits, there are several possible explanations: (1) inflammation of the ligament may exist without accompanying structural change; (2) abnormalities may be present in the ligament that are not detectable with ultrasonography7; and (3) there is pathology of other structures. It should be noted that most horses that have undergone any strenuous work will have some degree of ultrasonographic change (e.g., loss of echogenicity, fiber malalignment) in the proximal aspect of the SL6; the challenge is determining its clinical significance. Therefore combining the use of diagnostic analgesia and ultrasonographic comparison between limbs can be helpful in determining the relevance of a lesion. However, it is frustrating that there appears to be little correlation between ultrasonographic appearance of the SL, response to analgesia, ability to return to training, and incidence of recurrent lameness. MRI has revealed that this may be either because of SL damage that is present but undetectable using ultrasonography or injury of other structures.
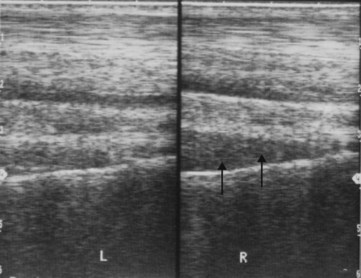
Fig. 118-1 Longitudinal ultrasonographic images of the palmar metacarpal soft tissues. The left forelimb is on the left. There is marked loss of echogenicity and disruption of the fiber pattern in the proximal aspect of the right suspensory ligament (arrows). Some loss of echogenicity is also seen in the proximal aspect of the nonlame left forelimb.
Initial management of horses with PSD regardless of whether ultrasonographic changes are present is aimed at reducing inflammation. Combination therapy using systemic corticosteroids (a single injection of intramuscular [IM] triamcinolone acetate, 0.03 mg/kg), rest, a 7- to 14-day course of nonsteroidal antiinflammatory drugs (NSAIDs), and local therapy (e.g., ice, cold hydrotherapy, poulticing, and bandaging) is beneficial. Lameness in some horses with transient soreness and pain on palpation resolves without further problems. Infiltration along the axial borders of the McII and the McIV with corticosteroids is sometimes helpful to reduce acute proximal SL inflammation in the short term and may enable a horse to compete successfully if no structural abnormalities are present. The short-term benefit must be weighed against the risk of enabling the horse to compete and sustain further damage. It is critical to rule out stress fractures in the proximal aspect of the McIII before infiltrating corticosteroids to minimize the risk of complete fracture. Correct foot balance is critical because a poorly balanced foot may contribute to SL strain. Weekly extracorporeal shock wave therapy (ESWT) for 3 to 5 weeks is used to reduce pain after the initial inflammatory period. Newer treatment modalities used with increasing frequency are intraligamentous injection of platelet-rich plasma, autologous stem cells derived from fat or bone marrow, and matrix derived from the urinary bladder of pigs (ACell Vet, ACell, Inc., Columbia, Maryland, United States). Although healing time is not shortened, these treatments may increase the quality of healing and decrease reinjury rate.8 Surgical splitting of the proximal aspect of the SL and osteostixis of the proximal aspect of the McIII or the third metatarsal bone (MtIII) was described in three dressage horses in which conservative management had failed and in which there was entheseous new bone on the McIII or the MtIII.9 This was reportedly successful. Fasciotomy is a technique used by some clinicians who treat other types of sports horses. I do not have enough experience with either technique to comment on their potential value in endurance horses. To accurately evaluate efficacy of various treatments, we must continue to define more precisely which structures have been injured. In general, I have had the most consistent success in endurance horses using initial antiinflammatory treatment, ESWT, rest, ensuring good foot balance, and a controlled rehabilitation and exercise program.
The horse should be restricted to handwalking until no lameness is apparent at a trot in hand on a hard surface without the benefit of systemic NSAIDs. The horse may then be gradually reintroduced to work if no structural abnormalities in the SL were identified. However, ultrasonographic examination should be repeated to confirm that no clinically significant structural change is present because the appearance of fiber damage observed ultrasonographically can lag behind the clinical perception of pain. Training may progress gradually if the lameness does not recur. If substantial structural change is present in the SL, if other ligamentous or osseous pathology has been identified, or if the lameness is persistent or recurrent, strenuous work should be avoided for at least 8 to 12 months. Although other sports horses may be able to return to training sooner, elite endurance horses are not able to quickly recover and require a considerably longer period. PSD is particularly treacherous to a horse’s career because, initially, a horse often responds to a short period of rest, but the horse then becomes lame again when increased exercise is attempted. This scenario may happen repeatedly after short rest periods.
Much of the recommended rehabilitation program for horses with tendon or ligament injury depends on the horse’s temperament and the amount of help and facilities available, but the best success is achieved with a controlled and gradual increase in exercise over 8 to 12 months. This may include turnout in a single-horse small paddock not much bigger than a stall; treadmill, handwalking, or walking machine exercise; and walking under tack. The bottom line has never changed: horses working in high-speed, strenuous athletic disciplines that sustain substantial damage to the SL (or SDFT) need 8 to 12 months of rest. The reason conventional wisdom becomes conventional is that it has withstood the test of time. Horses that sustain severe PSD may take 18 months to return to full training and will always be at increased risk of reinjury.
Stress Pathology of the Proximal Palmar Aspect of the Third Metacarpal Bone
Stress pathology of the proximal palmar aspect of the McIII includes avulsion and stress fractures, as well as more subtle bone and ligamentous change. Some avulsion fractures associated with the origin of the SL can be identified using radiology or ultrasonography; others not identifiable using these imaging modalities are apparent using scintigraphy (Figure 118-2). MRI has enabled the recognition of fractures, prefracture pathology, and other changes occurring in the proximal palmar metacarpal and metatarsal regions unapparent using other imaging techniques. Avulsion fractures are part of an array of proximal palmar metacarpal pathology that includes palmar cortical and endosteal abnormalities, enthesophyte formation at the origin of the SL, severe palmar McIII so-called “bone bruising” characterized by increased signal intensity in fat-suppressed MR images, and stress fractures or linear defects within the cortex consistent with linear incomplete cortical fractures.3,7 Some proximal metacarpal fractures originate at the carpometacarpal joint surface; others originate from avulsion fractures that propagate distally.10 Incomplete fractures can be difficult to diagnose; one horse with bilateral proximal palmar McIII cortical fractures that extended into the diaphysis displayed a crouching stance, giving the appearance of a primary hindlimb lameness.10 The crouched stance in this horse and unusual gait occurs in horses with other bilateral forelimb fractures and is often confused with hindlimb pain (Editors). Horses with incomplete fractures should be box-rested for 30 to 60 days and confined alone in a small paddock or handwalked for an additional 60 days before resuming exercise. If unrecognized, there is a substantial risk that incomplete cortical fractures may propagate to become complete, with disastrous consequences (Figure 118-3).
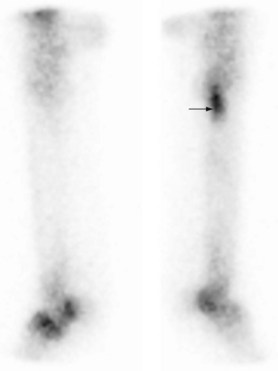
Fig. 118-2 Lateral bone phase scintigraphic images of the left and right forelimbs. There is intense focal increased radiopharmaceutical uptake (IRU) in the proximopalmar aspect of the right third metacarpal bone (McIII) (arrow) at the origin of the suspensory ligament. Note also IRU in the proximal aspect of the proximal phalanx of the left forelimb and IRU of the distal aspects of the McIII in both forelimbs.
Pathology Associated with the Second and Fourth Metacarpal Bones
Periostitis or exostosis of the McII and the McIV (splints) is much less common than other injuries in the proximal palmar metacarpal region and is included because of the close anatomical relationship to other structures in the region. It may be a minor problem necessitating a 2- to 4-week break from training, but abnormalities of the McII and the McIV may be associated with pathology of adjoining structures. Abnormalities identified with MRI include interosseous ligament pathology and reactive synostoses between the McII or the McIV and the McIII. This may be seen in association with injuries of the palmar cortex of the McIII and/or the SL, and the clinical significance of some of these findings is still undetermined. Loss of separation between either the McII or the McIV and the medial and lateral lobes of the SL with subsequent soft tissue apposition and adhesion formation may also occur and be of clinical significance. Radiological examination of an enlargement of the McII or the McIV should be performed to rule out a fracture. Ice, cold hydrotherapy, dimethyl sulfoxide (DMSO) gel, NSAIDs, and bandaging are used to reduce inflammation during the inflammatory period. Cryotherapy can also be used to reduce inflammation and will sometimes enable horses with reactive splint exostoses to continue in training and competition. Most uncomplicated splints resolve with time and treatment, although a nonpainful enlargement remains. If the exostosis continues to enlarge or if the area remains painful, training should be discontinued to avoid impingement on and damage to the SL. Sometimes SL damage occurs before recognition of the problem, and affected horses require a longer rest period. Fractures of the distal aspect of the McII or the McIV should be surgically removed, and horses should be given rest. Horses with splint exostoses that appear reactive or large enough to impinge on the SL may also be surgical candidates, although opinions differ. Horses undergoing distal splint ostectomy because of a fracture have a better prognosis than those receiving ostectomy because of exostosis.1 It may be that once SL damage has occurred, the window of opportunity for surgical intervention without adhesion formation is past. Any associated injury to the SL is the limiting factor in how quickly and how successfully horses with splint exostoses can be returned to work.
Foot Problems
Problems with the feet are a frequent cause of elimination from endurance competitions, as well as being a common cause of chronic or recurrent pain. Foot problems occur in both forelimbs and hindlimbs but are more regularly seen in the forelimb. Many lameness eliminations related to the feet are transient in nature: bruising or a dislodged shoe. The importance of a properly trimmed, well-balanced, well-shod foot cannot be overemphasized, and a good farrier is an integral part of a successful endurance team. Because endurance horses train and compete over very long distances, foot balance has a huge impact on the support structures of the limb. Trimming and shoeing with a long toe and low heel can lead to direct heel trauma, as well as increased strain on the SL and digital flexor tendons. Good medial-to-lateral balance is vital to avoid problems with collateral ligaments of the distal limb joints and the collateral sesamoidean and distal sesamoidean impar ligaments. Farriers who are accustomed to working with horses that wear keg shoes may be impatient with the requirements of endurance horses, which can sometimes require a more innovative and time-consuming approach aimed at providing the foot with increased protection and support. Many, if not most, endurance horses are shod with full pads for the day of a race, which are later removed. Silicon gel is often used for this purpose.
Sole bruises occur frequently in horses traveling over hard ground. Horses show a bilateral lameness manifest as a shortened, choppy gait. Application of hoof testers around the solar margins of the foot elicits a painful response. Lameness is often more pronounced in one limb. Diagnostic analgesia of the foot in which the lameness is most noticeable may then result in contralateral limb lameness. Sole bruising may be accompanied by increased radiopharmaceutical uptake (IRU) in the distal phalanx and changes indicative of distal laminar and bone inflammation on MRI (“pedal osteitis”).11 Radiological abnormalities include loss of bone opacity at the margins of the distal phalanx and increased size and number of vascular channels, resulting in a ragged appearance. Lateromedial radiographic images may reveal modeling at the distal aspect of the distal phalanx, sometimes described as a “ski jump” appearance. Management is aimed at protecting the solar margins and reducing concussion. Wide-webbed, seated-out shoes, full pads, or rim pads can be used to accomplish these goals. Distal interphalangeal (DIP) joint synovitis may occur concurrently and is treated by intraarticular medication (hyaluronan and corticosteroid combinations). Sore feet often occur in conjunction with distal hock joint and back pain and may be the inciting cause. Each area must be addressed individually, as well as the horse as a whole, for treatment to be successful.
Palmar foot pain is less common in Arabian and Arabian crossbreeds than in larger breeds, but it does occur and can be an important cause of lameness. As more MRI examinations are performed, abnormalities in the navicular region are identified with increasing frequency. Injuries identified in endurance horses with lameness abolished using palmar digital analgesia have included so-called “edema” of the navicular bone (i.e., increased signal intensity in the spongiosa in fat-suppressed images); distal border irregularities of the navicular bone; lesions of the DDFT from the level of the navicular bone to its insertion, with increased signal intensity in the palmar aspect of the navicular bone in fat-suppressed images; adhesions between the DDFT and the navicular bone; and disruption of the collateral sesamoidean ligament and its attachment to the dorsolateral aspects of the middle phalanx.
Endurance horses frequently exhibit inflammation of the coronary band (“coronitis”) in the first 24 hours after competition. It may be focal (usually dorsal) or all the way around and is usually painful on palpation. Separation of the hoof wall from the coronary band may occur, and there may be oozing of serum from the coronary band. This is sometimes, but not always, accompanied by a bounding digital pulse. Interestingly, as alarming as this is, these horses do not usually progress to typical laminitis. The outer layer of hoof wall may peel away from the coronary band, but the horse is not lame, and there is no rotation or sinking of the distal phalanx. The episode is marked by bruising and a distinct defect in the hoof wall that usually grows out without further incident.1,3
Endurance horses are also subject to laminitis that may be traumatic or metabolic in origin. Clinical signs become apparent 24 to 72 hours after competition. The severity may range from frightening, but mild, to disastrous. Horses without rotation or sinking are generally able to return to endurance competition. Horses with the worst outcomes often show few prodromal clinical signs. Proactive measures aimed at preventing laminitis should be considered in all high-risk horses after competition (those that are severely hemoconcentrated, exhausted, or have rhabdomyolysis, ileus, or diarrhea) because it is not possible to predict which horses will or will not have a satisfactory outcome. Continuously standing all four feet of the horse in an ice water slurry or water at 1° C up to the level of the carpus has proved to prevent onset of laminar damage12,13 but will not halt laminitis that is already occurring.13 Any horse that begins to shift weight or show any signs of discomfort after competition should certainly be treated, but by the time these signs are apparent, progression of the disease may be well underway. Flunixin meglumine (0.25 mg/kg intravenous [IV], thrice daily), phenylbutazone (2.2 to 4.4 mg/kg twice daily), acepromazine (0.0 25 mg/kg IM four times daily), pentoxifylline (7.5 mg/kg orally [PO] thrice daily) (Editors Note: Also see comments on page 373), and DMSO (1 g/kg IV diluted to 10% solution once or twice daily) are routinely used in various combinations, with the caveat that the horse should receive fluid therapy before administration of NSAIDs or acepromazine. Sole and frog pressure are also provided.
Metacarpophalangeal and Metatarsophalangeal Osteoarthritis, Capsulitis, Synovitis, and Periarticular Pathology
Osteoarthritis (OA) of the metacarpophalangeal (MCP) and metatarsophalangeal (MTP) joints and periarticular pathology is related to the ongoing nature of degenerative processes, chronic wear and tear associated with training and competing, and the fact that endurance horses may compete for several years. OA of the MCP or the MTP joints may occur with or without joint effusion and may be unilateral or bilateral, but is most often bilateral. OA is far more common in the MCP joints but also occurs in the hindlimbs. There is usually pain on flexion, and the joint often has a decreased range of motion and thickening of the joint capsule; acute or chronic synovitis may be present. Radiological changes may be subtle, such as narrowing of the joint space, or may consist of more obvious periarticular osteophyte or enthesophyte formation and joint modeling. Hypertrophy of the dorsal synovial pads with associated bone lysis at the proximal aspect of the sagittal ridge of the McIII is common, and osteochondral fractures may occur. Radiological changes do not always correlate with clinical significance; therefore diagnostic intraarticular or perineural (low palmar and palmar metacarpal) analgesia is used to confirm the site of pain. MRI findings may include effusion of the MCP joint with dorsal soft tissue accumulation and chronic, fibrotic synovial tissue and associated dorsal proximal plica formation. Lesions of the distal sesamoidean ligaments may contribute to periarticular pain. Using MRI a diagnosis of medial oblique sesamoidean desmitis is more common than lateral oblique desmitis. Acute, traumatic synovitis or capsulitis of the MCP joints may occur occasionally, but in general long-term management of chronic OA is the more common scenario, and management is similar to that in any other athletic horse. Local therapy (e.g., ice, cold hydrotherapy, poultice, and sweats), intramuscular glycosaminoglycans, intravenous hyaluronan, and judicious use of intraarticular hyaluronan and corticosteroids are beneficial. Repeated intraarticular corticosteroid injections may lead to a reduced response. Interleukin-1 receptor antagonist protein therapy may have long-term benefit, but most team and stable veterinarians preparing for a big race tend to continue to use intraarticular corticosteroid–hyaluronan combinations because the effects are more predictable. Withdrawal periods must be borne in mind. Horses with markedly hypertrophied dorsal synovial pads and osteochondral fragments usually require surgery.
Stress Pathology of the Distal Aspect of the Third Metacarpal or Third Metatarsal Bone
Repetitive overloading injury of bone can lead to athletically induced fractures. Most fractures in endurance horses propagate from the MCP or the MTP joints, and lateral condylar fractures of the McIII are the most common type.14 This is consistent with reported common fracture locations in Thoroughbred racehorses.15,16 MRI has proved to be a valuable tool in early identification of stress pathology that is not visible radiologically. Identified abnormalities include asymmetry in trabecular architecture between the medial and lateral condyles of the McIII and the MtIII, and superficial palmar or plantar fissure lines at the articular surface. Alteration in structure of the articular surface and osteochondral and some subchondral irregularities associated with the medial and lateral condyles of the McIII and the MtIII are likely to be a reflection of traumatic or degenerative cartilage and underlying bone damage, increasing potential for fracture at these sites.16-21 Bone trauma (so-called “bruising”) and, more commonly, chronic subchondral bone modeling of the distal aspect of the McIII or the MtIII of mature horses are recognized causes of pain, but may not increase risk of fracture formation.11,20,21 When pathological changes thought to increase the risk of fracture formation are identified, it is clearly prudent that the horse not continue training. However, it is not always clear what changes are pathological and increase fracture risk and what changes may reflect adaptive response to training. There is increasing evidence to support that many fractures in athletic horses occur not as isolated instances of a “bad step” but as a progression of pathological changes and stress remodeling over time, ultimately resulting in bone failure.15-19
Condylar fractures of the McIII or the MtIII may be complete or incomplete, displaced or nondisplaced, and may or may not be associated with joint effusion. Nondisplaced fractures are not always readily diagnosed but should be considered high on the list of differential diagnoses in an acutely lame endurance horse. The importance of careful physical examination and diagnostic imaging cannot be overemphasized because nondisplaced fractures risk becoming displaced if undiagnosed and sufficient confinement, support, and repair or stabilization are not provided. Many nondisplaced fractures are not diagnosed until several days after the occurrence of the injury and may require special imaging techniques. The presence of “moderate injury of the suspensory apparatus” increased the risk of condylar fracture in Thoroughbred racehorses.22 Given the high prevalence of PSD in endurance horses and the increasing numbers of condylar fractures identified, it is tempting to think that there may also be an association in endurance horses, and evaluation of risk factors for fracture in endurance horses is in progress.3
An unusual fracture type seen with increasing frequency in mature endurance horses is a transverse compression fracture of the distal metaphysis of the McIII at the residual physis (Figure 118-4). Horses with compression fractures of the distal aspect of the McIII have pain on palpation in the lateral condylar region and are usually suspected to have lateral condylar fractures, although no joint effusion is present. I have observed one horse with bilateral nondisplaced compression fractures, which had unilateral forelimb lameness. Horses with unilateral or bilateral nondisplaced fractures respond well to conservative management. One 7-year-old horse with no previous history of lameness pulled up grade 4 of 5 lame after a 40-km qualifying ride and had a transverse compression fracture with displacement of the distal epiphysis of the McIII.

Fig. 118-4 Dorsopalmar radiographic image of a metacarpophalangeal joint, obtained with a horizontal x-ray beam so that the proximal sesamoid bones are superimposed over the epiphysis of the third metacarpal bone, distal to the physis. Lateral is to the right. There is a transverse compression fracture of the distal aspect of the third metacarpal bone at the residual physeal scar characterized by increased radiopacity of the physis (black arrows) and a small step incongruity laterally (white arrow).
Diagnosis in horses with bilateral fractures of the McIII or MtIII is challenging. Two horses with bilateral forelimb condylar fractures were reluctant to move and had a stance similar to horses with acute laminitis, rocked back onto the hindlimbs. Another horse with bilateral hindlimb lateral condylar fractures and a concurrent hindlimb sagittal fracture of the proximal phalanx appeared to have unilateral hindlimb lameness (on the side with the proximal phalangeal fracture) and was reluctant to move. On initial examination at the ride venue there was a palpable condylar fracture. After the limb with the obvious fracture was splinted and analgesics had been administered, the horse walked reasonably comfortably. Subsequently swelling developed over the lateral condyle of the MtIII of the contralateral limb, and radiography revealed bilateral fractures, with a complete, displaced, comminuted lateral condylar fracture in the less lame contralateral limb.10 It must be recognized that bilateral fractures do occur but may not be obvious. However, if a horse has an unusual stance or is reluctant or unable to move, radiographs of both limbs should be obtained to rule out fractures of the proximal phalanx and the distal and proximal aspects of the McIII or the MtIII. It should be standard practice to obtain radiographs of the contralateral limb before placing a horse under general anesthesia for surgery.
Superficial Digital Flexor Tendonitis
Superficial digital flexor (SDF) tendonitis may be acute or chronic, low grade or severe. Acute ruptures or partial ruptures occur occasionally during competition. Although more common in forelimbs, SDFT injury also occurs in hindlimbs. Initial management is directed at trying to reduce swelling and inflammation and to relieve pain. Ice, bandaging, and NSAIDs are used to this effect. Dehydrated horses should not be treated with NSAIDs until they are rehydrated. Horses that sustain a rupture or partial rupture of the SDFT have a poor prognosis for return to endurance competition.
Horses with less severe damage to the SDFT can be more challenging to diagnose and manage. Training injuries, wherein the SDFT may be warm and tender on palpation, occur relatively frequently. Lameness is often not apparent. The initial unremarkable ultrasonographic appearance may belie underlying structural damage, which is not yet visible. A second examination should be performed 7 to 10 days later because the ultrasonographic appearance is often worse at that time than it is initially. Horses with transient heat and tenderness but no swelling or fiber damage can usually be safely returned to training within 2 to 4 weeks after the resolution of clinical signs. If the tendon is enlarged or if fiber separation has occurred, a substantially longer absence from training and competition is required.
Endurance horses that sustain tendon injuries in training or competition are managed similarly to any athletic horse. A one-time dose of intramuscular triamcinolone acetonide (0.03 mg/kg), local application of ice for the first few days, cold hydrotherapy, bandaging, poulticing, and NSAIDs for 2 to 3 weeks are beneficial in reducing initial inflammation. Surgical splitting of those tendons with central core lesions, autogenous liquid bone marrow injection of split SDFTs, and intralesional stem cell, platelet-rich plasma, or ACell injection may be beneficial, but whether these therapies are more beneficial than rest alone is uncertain. Endurance horses with SDF tendonitis have traditionally had a better prognosis for return to competition than horses that race over short distances at higher speeds. Prognosis may be less encouraging in the future as speeds of endurance competitions increase.
Paravertebral and Gluteal Myalgia
Paravertebral myalgia is related to repetitive stress over long distances and is exacerbated by a fatigued, unbalanced rider. Unbalanced movement of the horse contributes to muscle fatigue and often occurs as a result of the horse altering his gait to protect weaknesses. Unfortunately, concomitant diminished rider capability occurs in horses experiencing muscle fatigue. Horses ridden by fit, experienced riders are less subject to battering of the paravertebral muscles than those ridden by novices or poorly balanced riders. FEI rides require that a minimum weight of 75 kg be carried. A fit, competent rider is able to adjust his or her weight distribution to help a tiring horse, but a horse ridden by a less capable rider may be better off with the dead weight of a lead pad.
A horse that has strained or injured the paravertebral muscles appears stiff or rigid rather than lame, and instead of flexing and extending the spine normally when palpated, the horse tends to stiffen, squat, or crouch. It may be difficult or impossible to differentiate muscle pain from pain emanating from vertebral articular facets or dorsal spinous processes. Paravertebral myalgia can occur from a gait change induced by sore feet or sore hocks. Treatment consists of removing the inciting cause when possible and reducing inflammation. Most horses respond to 2 weeks of reduced exercise in conjunction with NSAIDs and pulsed muscle massage. Injection of the paravertebral muscles with an antiinflammatory agent can also be beneficial. The longissimus dorsi muscles are injected bilaterally, approximately 3 cm lateral to the dorsal midline, at five to six sites approximately 5 cm apart using a 22-gauge 1.5-inch needle, from the midthoracic area moving caudally, with 2 mL/injection site of an aqueous solution of soluble salts of the volatile bases from Sarraceniaceae (Sarapin, High Chemical Company, Levittown, Pennsylvania, United States) alone or mixed equally with estrone sulfate (50 mg).
Inflammation of the gluteal muscles also occurs with relative frequency in horses subjected to strenuous work over long distances. The horse exhibits stiffening and shortening of stride; pressure on the superficial and middle gluteal muscles produces a painful response; and the horse may crouch down or move away during palpation. Swelling or asymmetry may be apparent in the acute stages, with elevation of serum muscle enzyme concentrations. Severe inflammation of the gluteal muscles and accompanying rhabdomyolysis are serious problems that are discussed in the metabolic abnormalities section (see page 1147). NSAIDs must never be administered to a horse with acute gluteal muscle inflammation unless it can be ascertained that hydration and renal function are not compromised. Endurance horses with mild gluteal muscle inflammation usually respond to NSAID therapy, pulsed muscle massage to alleviate muscle pain and spasm, and a short (2 to 3 weeks) rest period. Gluteal soreness may occur in conjunction with forelimb lameness because horses may alter the hindlimb gait to avoid interference. The primary lameness must be managed to hasten resolution of gluteal muscle inflammation.
Osteoarthritis of the Distal Hock Joints
OA of the distal tarsal joints usually affects both the tarsometatarsal (TMT) and centrodistal joints and is often bilateral, with one limb usually more affected than the other. Joint effusion is not palpable, but occasionally during joint injection of the TMT joints one gets the impression that there is increased pressure and volume of synovial fluid. Affected horses are positive to hindlimb flexion and show variable sensitivity to the Churchill test. Radiological abnormalities include joint space narrowing and osteophyte formation but do not always correlate with clinical signs. If the clinical picture is one of distal hock joint pain, intraarticular medication is usually administered; a positive response is empirical evidence of a correct diagnosis. This approach obviates the need to go back after a positive response to intraarticular anesthesia to administer intraarticular medication. Distal hock joint pain frequently occurs concurrently with paravertebral muscle pain and sore front feet: the “terrible triad.” This is likely to be a result of a horse with sore front feet altering his gait in such a way as to cause strain in the paravertebral muscles and hocks. The best results are obtained when all three problems are treated simultaneously; otherwise, the pain in one area and gait alteration and soreness in another become a never-ending and ever-enlarging cycle.
If pain is localized to the tarsus but radiological findings are negative, consideration should be given to the possibility of less common causes. I have evaluated two endurance horses with nondisplaced parasagittal fractures of the talus. Pain was localized to the tarsocrural joint using diagnostic analgesia. In both horses there was IRU, and a clear fracture line was visible with MRI (Figure 118-5). MRI examination has been useful to diagnose incomplete fracture of the third tarsal bone and evidence of bone repetitive overloading injury in the talus, central, and third tarsal bones. Curb, inflammation of the long plantar ligament, or SDFT distal to the calcaneus may also be a cause of pain in the tarsal area but is usually identified by local pain and swelling.
Desmitis of the Suspensory Body and Branches
Desmitis of the suspensory body and branches is more obvious than PSD because there is usually palpable swelling. It most frequently occurs as acute, often severe, traumatic injury during training or competition. Low-grade, chronic desmitis often precedes acute onset of lameness. Ultrasonographic examination of the SL body and branches is easier to interpret than ultrasonography of the proximal aspect of the SL. Initial and long-term management is essentially the same as for horses with PSD. Suspensory desmitis often occurs in conjunction with pathology of the fetlock joint, which must be managed simultaneously.
Other Bone Injury
It is clear that most common fractures result from accumulated microdamage,15-20 but inconsistent, unpredictable surfaces may cause increased and uneven loads on the structural integrity of bone.23 Horses that get loose or run off over uneven ground or variable surfaces (sand to tarmac) may sustain unusual fractures. The presence of preexisting stress pathology increases this risk. Veterinarians working at endurance rides should be prepared to deal with emergency fracture management. A Kimzey splint over a suitable bandage is the most convenient and effective means of stabilizing a lower limb fracture or disruption of the suspensory apparatus. “Ski-boot” splints are equally effective but are more difficult to fit and apply correctly. Additional splint materials for stabilization of upper limb fractures, such as polyvinylchloride pipe cut into circumferential thirds and to appropriate lengths or a Kimzey splint with a proximal extension, should also be available.
While fractures of the distal aspect of the McIII or the MtIII are most common, the second most common fracture in endurance horses involves the proximal phalanx, and, importantly, horses often have acute lameness with limb instability from displaced fractures.14 Sagittal fractures are the most common followed by those that are comminuted. Proximal phalangeal fractures also occur in the dorsal plane and the dorsal and sagittal planes combined. Numerous radiographic views are essential to elucidate fracture configuration.
Less common fractures include radial, humeral, and scapular stress fractures diagnosed scintigraphically. A horse with a complete humeral fracture had no initial swelling or crepitus, but the limb could be abducted to an abnormal degree, and the presence of a fracture was confirmed radiologically. Other less common fractures of the distal phalanx (type V), proximal sesamoid bone (apical), middle phalanx (abaxial palmar eminence fracture), third trochanter of the femur, and pelvis (ilium and ischium) are occasionally seen.
Exertional Myopathy
Exertional myopathy, rhabdomyolysis, or myositis in endurance horses is not so much a lameness problem, but it is part of a larger picture of fatigue and metabolic abnormalities. It manifests as stiffening and shortening of the stride in all four limbs and may be accompanied by trembling and profuse sweating. It usually occurs either in the very early or very late stages of a ride. Severely affected horses often have pronounced swelling, hardening, or asymmetry of the gluteal muscles. Fluid therapy (0.9% sodium chloride) is the mainstay of treatment, and horses with severe myopathy may require large volumes (40 to 80 L) of fluids. Horses with myoglobinuria ideally should urinate normal-colored urine before administration of flunixin meglumine (0.55 to 1.1 mg/kg or 250 to 500 mg/450-kg horse). When in doubt as to the status of renal function, it is better to give the lower dose and repeat if necessary. Blood urea nitrogen and creatinine concentrations should be monitored, if possible. Portable, relatively inexpensive, user-friendly blood analyzers now make it possible to monitor renal function indicators and muscle enzymes, as well as electrolytes and packed cell volume. Methocarbamol (5 to 25 mg/kg IV) is helpful in many horses. DMSO (1 g/kg IV in a 10% to 20% solution) may also be beneficial. Dantrolene is not generally used because it is not available in an intravenous form, is expensive and not well absorbed when administered orally at recommended dosages, and is ideally given before exercise to be most effective. Horses that have suffered a clinical episode of exertional myopathy or myositis should not be returned to training until muscle enzyme concentrations return to normal values, bearing in mind that what is normal for a particular endurance horse may be higher than published ranges for other types of horses. Some endurance horses in regular training that show no clinical signs of myositis may have resting aspartate transaminase (AST) and creatine kinase (CK) values that commonly reach the range of 1000 U/L to 40,000 U/L or higher after a race or long training ride.3 Resting CK and AST values, as well as those after races or long rides, for individual horses must be known to determine whether elevated muscle enzyme concentrations are a result of new muscle damage causing lameness or the reason for subclinical poor performance.
Metabolic Problems
Avoidance, diagnosis, and management of metabolic problems are some of the many controversial topics currently faced by the sport of endurance. Veterinarians experienced in the sport of endurance racing believe that fatigued, metabolically compromised horses are at increased risk of developing musculoskeletal injury. The highly competitive nature of the sport has led to a large number of horses with metabolic abnormalities. Although veterinarians are now more adept at recognizing subtle signs of exhaustion and often treat horses proactively, a substantial number of horses still have serious problems. The “exhausted horse syndrome” described many years ago24 is still very much in evidence today. Exhausted horses undergo massive but poorly understood fluid and electrolyte shifts that lead to multiple organ system compromise. Initially, there is persistent elevation of the heart rate, a prolonged capillary refill time, and profound ileus that do not respond as anticipated to fluid therapy, electrolyte supplementation, or analgesics. Synchronous diaphragmatic flutter may be present. Horses with ileus and signs of abdominal pain should be checked for the presence of gastric distention by passing a nasogastric tube. Small intestinal volvulus after endurance competition is a recognized phenomenon,2,25 and horses with gastric reflux that do not respond to analgesics should be referred. A number of horses with small intestinal volvulus have experienced intractable pain and required intravenous general anesthesia for transport. Although dangerous, use of this technique has resulted in successful outcomes in horses that otherwise would not have survived.2 Two horses transported under intravenous general anesthesia that subsequently underwent small intestinal resection and anastomosis successfully returned to race the following season.
It cannot be overemphasized that exhausted, hypovolemic, or dehydrated horses or those with severe myositis must not be treated with NSAIDs until they are adequately reperfused. To do so risks renal failure, and these horses are already at high risk for renal failure as a result of hemodynamically mediated vasoconstriction. Vasoconstriction may contribute to subsequent renal ischemia that is exacerbated by NSAID-mediated inhibition of prostaglandin synthesis. If severe lameness or myositis is present, many veterinarians are lured into treating immediately with phenylbutazone or flunixin meglumine. This temptation must be resisted. Lame horses, even those with fractures and without overt evidence of metabolic compromise, should receive fluid therapy before NSAID administration. Horses with acute tendon or ligament injuries should have the affected limb placed in ice, and those with fractures should have appropriate external coaptation applied. Endurance horses should receive at least 10 L, and preferably 15 to 20 L, of intravenous 0.9% sodium chloride (or other available isotonic fluid) to restore renal perfusion before NSAID administration. This volume represents approximately half of the required fluid replacement volume for a moderately hypovolemic horse. Treatment of moderate hypovolemia, the decrease in circulating plasma volume responsible for clinical signs of tachycardia and prolonged capillary refill time, and dehydration (excessive loss of water from the body tissues) generally requires a minimum of 50 mL/kg of crystalloid fluids to replace deficits (20 L in a 400-kg horse). Horses with severe hypovolemia require large-volume replacement (60 to 90 mL/kg). The endpoint for fluid therapy is based on the response to treatment, which is closely monitored.
High-volume fluid replacement is by far the most effective treatment for horses suffering from severe hypovolemia that have collapsed or are on the verge of collapse. Two intravenous catheters should be placed; 14- or 12-gauge catheters are adequate if fluids can be delivered under pressure, and 10-gauge catheters are more difficult to place and usually require a cutdown. It is important that catheters are 140 mm (5.5 inches) long and are sutured in place to prevent dislodgement and extravasation of fluid. Aseptic technique is imperative to avoid the unwelcome complication of infectious thrombophlebitis. Horses with profound hypoglycemia may collapse, be reluctant to move, or exhibit a “sawhorse” stance and respond well to administration of 50 to 100 mL of 50% dextrose diluted in 3- or 5-L bags of saline, repeated as needed. Prednisolone sodium succinate (2.2 mg/kg IV or 1 g/450-kg horse; Solu-Delta-Cortef, Pfizer Inc., New York, New York, United States) can be helpful in stabilizing horses that have collapsed or are showing neurological signs, but it should be borne in mind that exhausted, hypovolemic, or dehydrated horses are also at risk for subsequent pleuropneumonia and laminitis, and large doses of corticosteroids may increase this risk. Profound leukopenia may precede the onset of pleuropneumonia, and appropriate antibiotic therapy should be instituted in leukopenic horses. It is wise to recheck the white blood cell count and creatinine levels of distressed horses the day after the race, even if they have been previously treated because endurance horses may be immunosuppressed or azotemic following competition. Laminitis may strike several days following postrace exhaustion. Prophylaxis for laminitis should be instituted in horses that are depressed, inappetent, leukopenic, or febrile.
Synchronous Diaphragmatic Flutter
Synchronous diaphragmatic flutter, or “thumps,” a condition in which the phrenic nerve is stimulated by atrial depolarization, causing contraction of the diaphragm and consequent “thumping” of the flank in time with the heartbeat, has traditionally been considered a sign of serious electrolyte imbalance, most commonly hypocalcemic, hypochloremic metabolic alkalosis.25 In my experience, blood levels of total or ionized calcium are often normal, and the presence and degree of alkalosis are variable. Measured electrolyte values may not reflect total body stores, and there is no convenient way to simultaneously measure chloride and ionized calcium. Many horses with thumps have no other identifiable abnormalities, and rest, food, and water may be all the treatment required. Before 2009, FEI rules dictated that horses be eliminated for thumps, but now disqualification is left to the discretion of the Commission Veterinarians. Most Commission Veterinarians require that horses with thumps be reexamined; if the condition is still present after the horse has been rested, fed, and watered, the horse is usually eliminated. Unfortunately, most horses with thumps take longer to resolve the condition than the limited time period given in which to represent, even if other metabolic abnormalities are not present. Horses eliminated from competition may be completely normal, and Commission Veterinarians may be in a bit of a conundrum: they do not wish to send a potentially compromised horse back out onto the course, nor do they wish to eliminate a competitor that is capable of safely completing. One must not lose sight of the forest for the trees, and it is essential to look at the overall picture.
Horses with thumps accompanied by serious metabolic abnormalities usually respond to intravenous calcium supplementation (100 to 300 mL of 20% to 23% calcium borogluconate diluted in 3 or 5 L of saline given over 15 to 20 minutes, to effect). It has been proposed that horses prone to thumps be fed a low-calcium diet before competition to enable more efficient mobilization of calcium from bone reserves during periods of stress.26 Although making physiological sense, this strategy has not been successful. Unfortunately, some horses appear to have a low threshold for development of thumps and are likely unsuitable for endurance use.
Prevention of Metabolic Problems
Many, if not most, metabolic problems could be avoided by the use of common sense, but in the heat of competition common sense is one of the first things lost. Although both horse and rider get tired, an astute rider is able to determine when the horse has had enough. The horse should be stopped if it is not eating and drinking at rest stops, is reluctant to move forward, or is stumbling.
Misuse of electrolyte replacement preparations is common, and concentrated electrolyte preparations that are force-fed may be detrimental if the horse does not drink. They increase the tonicity of the gastrointestinal lumen, cause fluid influx, and contribute to dehydration. Poorly formulated electrolyte preparations full of sugar cause hyperglycemia and a subsequent insulin-mediated hypoglycemic crash. Hay fed to a well-hydrated horse acts like a sponge, or water reservoir, in the large intestine. Whereas in flat racehorses hay and water are often withheld before racing, endurance horses should be encouraged to eat hay and should have free access to water before competition so that they will have a fluid reserve available for absorption from the large intestine.
Now one compulsory recheck examination is required at one or more Vet Gates at all FEI rides. This recheck examination has been exceedingly useful in identifying horses that pass the initial veterinary examination but then deteriorate during the mandatory hold period. Without a “second look,” horses may return to the course and further worsen. Focusing on the overall safety of the horse by early identification of metabolic and lameness problems is paramount and is in the best interests of the horse. It is incumbent on those of us entrusted with the stewardship of these horses to ensure that we do our utmost to manage them wisely.