Chapter 120The Western Performance Horse
 The Cutting Horse
The Cutting Horse
Jerry B. Black and Robin M. Dabareiner
Description and History of the Sport
The cutting horse was born of necessity long ago on the open grass plains of West Texas. This was the era of Western history that included big cattle drives from the open ranges of ranches such as Burnett and the 6666 Ranch, Waggoner Ranch, the Pitchfork Ranch, and the Matador Ranch to Dodge City, Kansas. Cutting horses enabled big country ranches, where no barbed-wire fences existed, the only means of working vast herds of cattle. In those days the task of the horse was simple, at least by definition. Guided by the rider, the cutting horse entered a herd of cattle quietly and deliberately. A single cow was cut, or separated, from the herd. The natural instinct of the cow is to return to the safety of the rest of the herd. The cutting horse, through breeding and training, controlled the cow with a series of moves and countermoves. The speed, agility, balance, and quickness of the cutting horse kept the cow from the herd, where other cowboys would hold the cut. The horse and rider would reenter the herd again and again, cutting cattle out until the work was done. Only the top hands earned the right to ride the best horses of the remuda (herd), the cutting horses.
The unique skills of the cutting horse were a great source of pride to the frontier cowboy. This often led to impromptu or jackpot cuttings on the open range or, from about 1900, in outdoor pens of the large ranches. From this love of the cutting horse, as well as the subsequent competition to determine who had the best horse, came the roots of cutting as we know it today. The first cutting horse contest for money was held at the 1898 Cowboy Reunion in Haskell, Texas. Twelve cutting horses competed for a purse of $150. From this start, regular events occurred on ranches of the Southwest and at the Fort Worth Stockyards. Rules and prizes varied greatly, but the ability of the cutting horse to separate a single cow from the herd always was and continues to be the goal of the competition. From these roots the National Cutting Horse Association was formed in 1946 during the Fort Worth Exposition and Fat Stock Show. The stated purpose of the organization was to standardize the rules and judging of competition and to preserve the tradition and history of the cutting horse with the ranching and livestock industry.
Today competitions approved by the National Cutting Horse Association occur throughout the United States and Canada. In addition, many association members from other countries, such as Australia, are conducting competitions outside North America. The format of these competitions and other Western performance horse disciplines, such as reining, presents a unique challenge to the equine veterinarian.
Training
Training of the cutting horse begins at 2 years of age. Usually 60 to 90 days are spent in basic training before the horse is introduced to cattle. This generally is accomplished by turning one cow into a round pen that is 38 to 54 m in diameter. The horse is taught to mirror the movements of the cow as the cow moves around the perimeter of the arena. This process of training a cutting horse is repetitive and is done several days a week for months. The object of training is for the horse to develop an ability to perform identical movements with the cow. Simply put, when the cow stops or stops and turns, the horse does the same maneuver. This type of training is accomplished by asking the horse to stop with the aid of a bridle and turning the horse to move with the cow. The key to training is a complete and balanced stop. With time, a stop ultimately is followed by the instinctive ability of the horse to “read” the movement of the cow and to turn in the direction the cow is going. Because this ability to watch a cow and respond to its movement is instinctive to the working stock horse, breeding is of the utmost importance. Without this genetic instinct a horse simply does not respond to the movement of a cow and does not initiate a stop or turn as necessary to continue to track the cow. A good cutting horse trainer knows in a relatively short period if a young horse has the instinct and athletic ability to be a successful cutting horse. A finished cutting horse must perform the necessary moves to keep a cow in proper position away from the herd, without any hand cues from the rider, relying on instinct alone to read the movement of the cow. Reining the horse is permitted only to make the cut of a single cow out of the herd. After the cut is successfully made, the reins are placed in a relaxed position on the horse’s neck, and only leg cues are permitted from the rider during the actual working time. The ability of a horse to contain an individual cow provides the excitement of competition in cutting.
Training of a cutting horse prospect that has shown good potential continues when it is a 3-year-old, preparing it for the first major competitions, the futurities. The futurity is the first of the horse’s aged event competitions that continue for 4 years. No horse can compete in aged events beyond 6 years of age. Aged events consist of two elimination go-rounds, followed by the semifinal and the final competition. Substantial musculoskeletal stress is placed on these athletic performance horses, with multiday competitions over a short period. In addition, the horses usually are practiced with cattle daily, including the day of competition, to sharpen performance skills. Competition in these aged events is heavy, with the major shows having more than 500 entries in a single age division. Purses in this type of event can exceed a total of $1 million. The nature of this aged event competition, with large purses in numerous events over a 4-year period, has caused the cutting horse economy to grow rapidly during the past several years. Select yearling and training sales are conducted annually that are beginning to parallel the racing industry in financial return on sales. This has contributed to the current popularity and resurgence of breeding of cutting and Western stock horses, which in turn will ensure the preservation of the tradition and heritage that this horse played in the history of the great Old West.
Lameness Examination
The increasing popularity of the cutting and reining horse for show and performance is occurring nationally and internationally. Sales of this type of horse have increased to Europe, South America, and other countries. In North America, the revival of interest stems primarily from excellent programs instituted by associations such as the National Cutting Horse Association and the National Reining Horse Association. These associations encourage owner participation at an amateur level in cutting and reining events. This type of performance horse creates a new diagnostic and treatment challenge for attending veterinarians, partially because of the rigid training schedules necessary for 3- to 6-year-old horses to compete in futurities and aged events.
Hindlimb lameness presents one of the more interesting diagnostic challenges to an equine clinician. The lameness is often difficult to diagnose and even more difficult to manage. A systematic approach must be developed to achieve an accurate diagnosis consistently. The veterinarian must use a routine that is repeated with each horse and must allow sufficient time to complete a thorough examination. Western stock horses may be difficult to evaluate while being led. These horses usually are not taught to lunge and are often difficult to trot in hand. A 10- to 15-m round pen with firm footing has proved to be beneficial for evaluating lameness.
Diagnosis and Management of Specific Lameness
Hindlimb lameness is more common than forelimb lameness in cutting horses. Mixed lameness with swinging and supporting components is common in hindlimbs, especially in upper limb lamenesses such as those involving the hock, stifle, and hip or sacroiliac region. Hindlimb lameness may be associated with two sources of pain: for example, chronic hock lameness and secondary lumbar and gluteal myositis. This section focuses on selected hindlimb lamenesses of the hock, stifle, and thoracolumbar regions.
Selected Lameness of the Tarsus
Osteoarthritis of the Distal Tarsal Joints (Distal Hock Joint Pain)
Osteoarthritis (OA) of the distal tarsal joints is seen most commonly in horses that have repeated, excessive compression and rotation of the hocks at high speed, and a high incidence occurs in young working cow horses and in cutting and reining futurity prospects, reflecting the demanding training schedules of 5 to 6 days a week at 2 and 3 years of age. Sickle hocks, cow hocks, and narrow hocks also may predispose horses to lameness. OA also may develop secondary to partial collapse of the central and third tarsal bones, and affected horses often develop lameness within the first year after birth. In one author’s practice (JBB), routine survey radiology of the tarsus in 20, 2-year-old cutting horse prospects before training began revealed evidence of OA in 11 (55%).
Clinical signs include reduced height of the foot flight arc, resulting in abnormal toe wear, and a shortened cranial phase of stride. Hard work increases the degree of lameness, although most horses are lame and stiff when first taken out of the box stall and improve to some degree during the initial warm-up. Trotting in a circle increases the degree of lameness. Gait alteration or lameness may be observed with the affected limb on the inside or outside of a circle. Cutting, reining, and stock horses are reluctant to stop properly. Upper limb flexion often increases the degree of lameness. Palpation of the distal medial aspect of the hock may reveal an exostosis and soft tissue thickening. Deep palpation of the area can cause a painful withdrawal response. Thoracolumbar pain is present in about 50% of horses.
Diagnosis is based on a positive response to intraarticular analgesia and radiology. Radiological abnormalities are often only seen in a dorsolateral-plantaromedial image in 2- to 4-year-old cutting horses, findings that differ from those seen in other young sports horses.
Therapy varies depending on the degree of lameness. Rest is generally not helpful in horses with advanced OA, and obtaining trainer compliance if the lameness is subtle is difficult. Training usually is continued with the help of nonsteroidal antiinflammatory drugs (NSAIDs), such as phenylbutazone (2 g daily or 1.5 g twice daily) and intraarticularly administered antiinflammatory drugs. Shoeing changes include removing excessive toe, squaring the toe of the shoe, and extending both branches of the shoe for more heel support. Half-round shoes help aid breakover in some horses with cow-hocked or sickle-hocked conformation. Changes in training schedules include more paddock or free-choice exercise and longer warm-up periods before training. Training in deep surfaces, overtraining, or conditioning in circles should be avoided. Varying the gait frequently during training and conditioning helps the horse to stay more comfortable.
Intraarticular medication is used to keep chronically lame horses in competition. A combination of methylprednisolone acetate (40 mg) and hyaluronan (10 to 20 mg) is injected separately into the centrodistal (distal intertarsal) and tarsometatarsal joints in horses with advanced OA. The veterinarian should not rely on communication between the two joints. If good results are achieved, these injections are repeated as necessary every 12 to 16 weeks. Horses with early OA respond favorably to intraarticular treatment with hyaluronan (20 mg of Hylartin-V, Pfizer Inc., New York, New York, United States) and triamcinolone acetonide (3 to 6 mg). Intravenous injections of hyaluronan (Legend [Bayer HealthCare LLC, Animal Health Division, Shawnee Mission, Kansas, United States]; 40 mg in 7-day intervals, series of three) or intramuscular injections of polysulfated glycosaminoglycan (PSGAG; 500 mg of Adequan [Luitpold Animal Health, Shirley, New York, United States] intramuscularly [IM] in 5-day intervals, series of four to eight) are used frequently as concurrent therapy. Combinations of intermediate-acting corticosteroids and hyaluronan administered intraarticularly have been used in horses that are lame immediately before leaving for circuit shows or important multiday competitions, such as cutting horse, snaffle bit, and reining horse futurities.
Therapeutic levels of NSAIDs may be necessary during competition if allowed by the breed, performance, or state drug regulations governing the event. Phenylbutazone (2 g daily or 1.5 g twice daily) is usually effective. However, many stock horse trainers believe that this drug tends to dull the mouth and sides of the horse, thus limiting bit and spur response. Other NSAIDs that are effective include flunixin meglumine (Banamine [Intervet/Schering-Plough Animal Health, Roseland, New Jersey, United States]; 1 mg/kg daily) or ketoprofen (Ketofen [Pfizer Inc.]; 2 mg/kg daily). Horses vary in response to the therapeutic effects of each NSAID. If one drug is not effective, a different one should be assessed. Tiludronate and interleukin-1 receptor antagonist protein (IRAP) have recently been introduced, but long-term follow-up results are not known. Tiludronate is administered as a single intravenous infusion. IRAP is injected three to five times at 1- to 2-week intervals. Focused extracorporeal shock wave therapy is used in horses refractory to intraarticular medication.
Surgery has been an important adjunct to OA therapy in horses requiring repeated intraarticular injections or continual therapy with NSAIDs. Horses with mild to moderate radiological changes but normal joint spaces respond favorably to cunean tenectomy. Horses with substantial intraarticular changes and joint space collapse are treated best surgically with a combination of cunean tenectomy and arthrodesis (fenestration) of the affected joint or joints using a 3.2-mm drill bit and creating three to four tracts. The horse is returned to work as soon as possible after surgery to encourage ankylosis. Handwalking is begun the day after surgery, and light riding at a walk may begin 2 to 3 weeks later. Light riding exercise continues for another 3 weeks, and full training begins 45 to 60 days postoperatively if the horse is reasonably comfortable. Phenylbutazone, 2 g once daily as needed, is used initially if obvious lameness persists. Most horses show almost immediate improvement after surgery. This improvement may be caused partially by the release of intraosseous pressure after the fenestration procedure, plus cessation of the rotational effect of the cunean tendon on the distal aspect of the tarsus. Radiological evidence of ankylosis occurs over a prolonged period, even up to 1 year postsurgery. Soundness does not seem to be related to radiological evidence of ankylosis.
Prognosis varies depending on the degree of OA, the number of joints involved, and the type of competition in which the horse is engaged. Surgery offers the best prognosis for horses with chronic lameness. It is possible that chemical fusion with ethyl alcohol may offer a shorter convalescent time.
Arthrosis of the Tarsocrural Joint
Distention of the tarsocrural joint capsule is usually the result of osteochondrosis or trauma. Osteochondrosis lesions occur on the cranial aspect of the intermediate ridge of the tibia, the trochlear ridges of the talus, and the lateral or medial malleoli of the tibia. Trauma is related to quick turns, hard stops, loss of balance, and poor footing. Faulty conformation, such as overly straight angulation of hock and stifle joints, may be a predisposing factor.
Distention of the tarsocrural joint capsule is observed most easily on the dorsomedial aspect of the hock, but swelling also occurs in the plantar pouches, laterally or medially. The horse may have pain on palpation. A proximal limb (hock) flexion test may or may not be positive, depending on the degree of joint capsule distention and synovitis. Radiographic examination is essential to determine the cause and should be repeated after 10 to 14 days if initial radiographs are normal.
Horses with osteochondrosis are treated surgically. Horses with traumatic distention of the tarsocrural joint are treated by intraarticular injection of intermediate-acting corticosteroids and hyaluronan, two or three times, 14 to 21 days apart. Intraarticular injections often are followed by hyaluronan (40 mg) administered intravenously weekly for 3 weeks. All injected hocks are bandaged concurrently to help reduce joint effusion. Pressage elastic contour bandages (Jupiter Veterinary Products, Harrisburg, Pennsylvania, United States) provide adequate pressure and are easy to maintain. The horse is given rest for 3 to 6 weeks.
Exploratory or diagnostic arthroscopy is justified in any horse that does not respond to conservative therapy, permitting identification of subtle osteochondrosis lesions not detectable radiologically and soft tissue injuries, as well as providing joint lavage.
The prognosis is good if treatment is initiated early and if all fragments and debris are removed soon after the synovitis is recognized in horses with osteochondrosis lesions or severe trauma. If conformation is the predisposing cause, the prognosis is poor.
Selected Lameness of the Stifle
The stifle is a large, complex joint composed of two articulations: the femorotibial and femoropatellar joints. One author’s experience (JBB) has been that during arthroscopy of the femorotibial joint, despite high intraarticular fluid pressure, obvious distention of the femoropatellar joint capsule does not occur. Thus little or no distention of the femoropatellar joint capsule occurs in association with disease of the femorotibial joint. When performing intraarticular analgesia of the stifle, all three compartments should be injected separately.
Osteochondrosis
Osteochondrosis of the trochlear ridges of the femur is seen commonly in young horses. Clinical signs include distention of the femoropatellar joint capsule and varying degrees of lameness, depending on the amount of joint surface involved. Diagnosis is confirmed radiologically. Arthroscopic surgery is the treatment of choice to debride all diseased cartilage and bone and to remove all free-floating bone and cartilage. Aftercare consists of 45 to 60 days of stall rest, followed by an equal amount of stall and paddock confinement. Training generally resumes 3 to 6 months postoperatively. Intraarticularly administered hyaluronan (20 mg) followed by intramuscularly administered PSGAGs (500 mg in 5-day intervals, series of four to eight) 2 to 3 weeks after surgery has helped to reduce postoperative synovitis.
Subchondral Bone Cysts
Subchondral bone cysts of the medial condyle of the femur are the most frequently recognized bony lesions of the stifle in one author’s (JBB) practice. Affected horses are lame at the walk or trot in one or both hindlimbs. The degree of lameness varies greatly among horses. Some horses are subtly lame, requiring riding or repeated flexion to produce a recognizable lameness. Others have acute, severe lameness and are unwilling to trot. Moderately lame horses tend to swing the toe medially during protraction. This contrasts with horses with painful conditions of the femoropatellar joint or patellar ligaments, with which the horse often carries the stifle out or abducts the limb. Lameness may be more obvious with the affected limb on the inside of a circle.
Subtle distention of the femorotibial joint capsule may be palpated between the medial patellar and medial collateral ligaments. Some horses resent deep digital pressure over the medial femoral condylar region.
Diagnosis of subchondral bone cysts is based on clinical signs and response to intraarticular analgesia using 30 mL of mepivacaine and radiology. Conservative treatment for the most part yields only temporary improvement in the lameness and is used only when a performance horse needs to compete for the remainder of the season or when finances prohibit surgical intervention. Conservative treatment consists of intraarticular injections of hyaluronan, with or without corticosteroids such as betamethasone or triamcinolone acetonide. Intramuscularly administered PSGAGs, given in a series of four to eight injections at 5-day intervals, are also used. Many trainers report a pronounced effect about 24 hours after administration of PSGAGs. Therapeutic levels of systemic NSAIDs may be also necessary during multiday competitions. Owners should be informed that continued training and competition over an extended period might lead to secondary OA.
There are several treatment options, but the treatment of choice in our experience is curettage and fenestration of the subchondral bone cyst. Before 1988, this procedure was done through an arthrotomy incision. Although the surgery was successful in most horses, wound dehiscence and prolonged hospitalization were of great concern. Currently the surgery is performed by arthroscopy, with the horse placed in dorsal recumbency and the limb in flexion. This position provides adequate visibility and good access to the cystic lesion via an instrument portal. Postoperative hospitalization is minimal, and to date no postoperative complications have been seen. The horse is confined for 60 days after surgery. Handwalking for 10 minutes daily is allowed during confinement. Free-choice exercise for an additional 2 to 4 months is allowed. Training usually resumes 6 months postoperatively or earlier, if the horse is sound. Surgical success is about 50% to 60%. Most of these horses return to a competitive level of performance, if given adequate rest. Recently arthroscopic injection of corticosteroids into the fibrous tissue of subchondral cystic lesions has been described.1 A retrospective study examined 52 horses with subchondral cystic lesions in the medial femoral condyle that were injected with arthroscopic guidance with a reported success rate of 77%. Preexisting osteophytes had a negative impact on outcome. This seems like a viable first option for treatment, and if unsuccessful then surgical debridement and fenestration can be performed.
Upward Fixation of the Patella
Partial or complete upward fixation of the patella is a common cause of stifle pain, which can eventually produce articular changes of the patella. Upward fixation of the patella can occur in any type of body conformation and hindlimb angulation and may be related to the anatomical formation and depth of the notch on the proximal aspect of the medial trochlea of the distal aspect of the femur. Lack of condition and loss of condition are contributory factors. Poor coordination between extensor and flexor groups of the stifle and lack of quadriceps development may explain why upward fixation is seen in young horses at the beginning of training. One of us (JBB) examined two horses in which upward fixation of the patella was secondary to a subchondral bone cyst in the medial femoral condyle. Upward fixation may have been caused by alteration of gait and foot placement because of pain in the medial femorotibial joint. Upward fixation resolved after arthroscopic treatment of the subchondral bone cyst. The duration of locking varies from an almost instantaneous release, with only slight backward jerk evident, to a complete locking that can last for hours and may require surgical release.
Diagnosis is based on clinical signs. Often, although no obvious upward fixation occurs in extension, the limb snaps with an audible click while in an extended position. Occasionally, pushing the patella over the top of the trochlear ridge when the limb is in extension can produce the locking. Clinical signs often are exacerbated if the horse is walked down a steep slope. The diagnosis is sometimes based almost entirely on the owner’s or trainer’s description of the condition.
Treatment should remain conservative when possible. If complete upward fixation has occurred for any period, the femoropatellar joint usually has effusion. Treatment should be aimed initially toward reducing inflammation and resting the tissues involved. The usual treatment schedule includes administration of systemic corticosteroids (20 mg of dexamethasone [Azium, Intervet/Schering-Plough Animal Health] IM daily) for 1 to 3 days, followed by 3 to 5 days of NSAIDs (2 g of phenylbutazone twice daily). Handwalking for 5 to 10 minutes is allowed if no further upward fixation occurs, but no free-choice exercise is allowed. Excessive toe is removed, and wedged shoes or wedge pad and flat shoes are used if the heel is low. Half-round shoes allow the horse to break over in its most comfortable and natural position.
Once the initial inflammation has subsided, a conditioning program is started. Long warm-up periods are essential. Thirty minutes of walking and trotting, followed by an increasing amount of extended trotting on the straightaway are recommended. Once the horse becomes conditioned, trotting in the hills is prescribed, where possible. The concept of conditioning is to improve quadriceps development and tone and to improve overall coordination. Horses that are underweight should be fed to gain weight and to improve the overall body condition and the condition of the muscles involved in movement of the stifle.
Horses that do not respond to conservative treatment may require an internal blister, medial patellar desmotomy, or medial patellar desmoplasty. Internal blister is accomplished by local infiltration of 2% iodine in peanut or almond oil injected directly into the body of the medial patellar ligament. Care must be taken to avoid the accidental penetration and injection of the femoropatellar joint with the counterirritant solution. If this is unsuccessful, splitting the medial patellar ligament is a viable option. This can be performed in either a standing sedated horse or under intravenous anesthesia. The area over the medial patellar ligament is clipped and scrubbed, and a number 15-scalpel blade or 14-gauge needle is inserted at 1-cm intervals and used to scarify the ligament perpendicular to the longitudinal axis of the limb. The thought is that by creating inflammation and scar tissue, the ligament will tighten, thereby preventing upward fixation of the patella. This treatment has been very successful in one of our hands (RMD). Medial patellar desmotomy should be reserved as a last form of therapy because the postoperative complications include fragmentation of the distal aspect of the patella, soft tissue fibrosis, and mechanical alteration of gait.
Femorotibial Joint Pain
Subtle soft tissue injuries may occur in the femorotibial joint, resulting in low-grade lameness that is most evident when the horse trots in circles. Such injuries often occur as training is increased. A typical example is a young cutting horse that is being worked hard on cattle before a futurity. The horse has a shortened cranial phase of stride and lowered foot flight, causing toe drag. Results of hindlimb flexion tests are generally negative. Mild distention of the medial femorotibial joint capsule may be palpable. Diagnosis is based on clinical signs, response to intraarticular analgesia of the femorotibial joint, and the absence of radiological abnormalities.
Treatment comprises intraarticular medication with hyaluronan and corticosteroids such as triamcinolone acetonide (6 mg), plus intramuscularly administered PSGAGs. Systemic NSAIDs are given in decreasing doses over 10 to 14 days. All trailers and calks are removed from shoes. A wedge pad may be added with an egg bar shoe or extended branch shoe, depending on the amount of heel support needed.
Training is resumed after 14 to 21 days of rest. Long warm-up periods and extended straightaway trotting are recommended to condition the muscles of the upper hindlimb.
Prognosis is good if a consistent training schedule is maintained. Horses with irregular training schedules and frequent periods of several days off between exercise sessions tend to have recurrent problems.
Thoracolumbar Injuries
Thoracolumbar Myositis
Soft tissue injuries of the thoracolumbar region produce back soreness and are common injuries in a working stock horse. Thoracolumbar myositis may coexist with hindlimb lameness, such as distal hock OA, or may be a primary traumatic lesion, frequently caused by the extraordinary forces of rotation and propulsion placed on the hindlimbs. Other factors include rigid training and competition schedules such as the fall futurities for 3-year-olds that result in an overworked young horse.
Local myositis involving the muscles of the thoracolumbar and pelvic region can have a profound effect on the performance of a stock horse. A cutting horse has three basic components to work: the stop, turn, and ability to track a cow in mirror image across the arena at high speed. Localized back pain results in decreased performance in all of these, without obvious lameness. The trainer perceives that the horse is simply not trying. Consequently, a horse with back pain is forced to try even harder and soon falls into the overworked category.
Clinical signs of thoracolumbar myositis include pain to palpation of the affected muscle groups and associated spinous processes, obvious discomfort during saddling or mounting, subtle bilateral or unilateral hindlimb lameness, unwillingness to stop in form, and overall lack of performance. Flexion tests are seldom positive, unless the back problem coexists with distal hock joint pain. One may reasonably believe that arthrosis of vertebral articulations in the lumbar and lumbosacral region exists in some horses. However, because of the depth and mass of the muscles involved, distinguishing the exact pathological condition or even the exact site of the injury is impossible.
Therapy is aimed at reducing inflammation and controlling the associated muscle pain and spasms. Prolonged rest periods from training always are indicated but in reality are difficult to achieve because of the rigid schedule of preparation for competition. For example, an average futurity horse being prepared for the National Cutting Horse Association futurity in December of its 3-year-old year accumulates a $20,000 to $24,000 debt in training and entry fees alone before competition. Convincing an owner and trainer that a horse should be allowed to rest immediately before the futurity is difficult, if appropriate therapy has even a remote chance of being effective.
The systemic use of skeletal muscle relaxants such as methocarbamol (10 mg/kg orally [PO] twice daily for 5 to 10 days) has been effective in treating cutting horses with generalized back pain. Dexamethasone (10 mg PO twice daily for 3 to 4 days) is indicated in horses with acute pain. Horses with chronic back pain may be treated successfully during competition with a single dose of triamcinolone acetonide (12 to 16 mg IM) and methocarbamol administered orally. NSAIDs generally have not been effective unless the back pain is secondary or coexists with distal hock joint pain. Care must be taken to comply with any medication rules.
Specific localized pain may be treated successfully by local injection of methylprednisolone acetate (200 to 400 mg) and Sarapin (50 mL; High Chemical Company, Levittown, Pennsylvania, United States). Treatment is repeated every 10 to 14 days until pain subsides.
Other management considerations are important for recovery. Horses with low, underslung heels of the hind feet should be shod using raised heels. Evaluation of the fit of the saddle, type of pad, and specific pressure points when ridden should be considered. Other modalities of therapy, such as pulsed electromagnetic field and therapeutic ultrasound, have been useful in keeping a horse in competition. Long warm-up periods without the rider for 30 to 45 minutes by ponying (leading from another horse) at a walk and trot always are indicated. The trainer must be cautioned that overwork and severe fatigue must be avoided at all times.
Sacroiliac Region Pain
Strain and subluxation of the sacroiliac joint are not uncommon in working stock horses because of twisting and rotation of the back and pelvis during work. This rotation is complicated by the weight of tack and the rider, who is attempting to maintain balance and remain stationary on top of the horse during sudden hard stops, turns, and bursts of speed.
Many of the clinical signs observed in horses with thoracolumbar myositis are also common in those with sacroiliac region pain because the epaxial muscles go into spasm to provide stability to the traumatized sacroiliac joint. However, bilateral or unilateral lameness with stiffness and alteration of gait usually are associated with sacroiliac region pain. Protrusion of the tubera sacrale may be evident when the horse is walking away from the observer. Flexion of the contralateral limb for 2 minutes may result in elevation of the tuber sacrale, hip hike, and stiffness of the affected limb. Digital palpation adjacent to the tuber sacrale and over the gluteal regions usually elicits pain. Local infiltration of local anesthetic solution may result in improvement, but rarely are clinical signs fully alleviated.
Deep intramuscular injections of methylprednisolone acetate (400 mg) and Sarapin (50 mL) into the region of the sacroiliac joint have been effective in treatment. Disposable needles at least 10 cm long are necessary to reach the affected area. Strict aseptic technique must be followed. Injections usually are repeated after 2 to 3 weeks. Concurrent systemic therapy with NSAIDs is beneficial. Horses must have rest, and 2 to 6 months out of training is often necessary, with strict stall confinement for the first 30 to 45 days.
Proper therapy and management of injuries to the thoracolumbar and sacroiliac regions generally are rewarding if initiated early in the course of the disease. Horses with chronic recurrent problems usually can be managed to allow some level of competition.
 The Roping Horse
The Roping Horse
Team Roping Horse
Description of the Sport
A unique handicapping system implemented in the early 1990s has contributed to team roping becoming a rapidly growing equestrian sport. Team roping began as a rodeo event many years ago, evolving from the everyday work of cowboys on ranches. If a cow needed to be treated on the open range, the only method of restraint was to secure the head and heel of the animal, or to team rope it. The cowboys soon began wagering among themselves to see which team of a header and heeler could accomplish this feat in the shortest time. Currently nearly 1 million people compete in team roping competitions in North America.
Because of the large number of participants, team roping has become of great economic importance. Many team roping organizations exist nationally, but the most prestigious is the United States Team Roping Championships. The numbering or handicapping system of the team ropers was begun by the United States Team Roping Championships and has become standard. A number, from 1 to 9, with 9 being the highest level of ability, is assigned to each of the team ropers. This number is based on various factors, including ability, previous prize earnings, experience, age, and physical handicaps.
The roping categories also are assigned a numerical value that cannot be exceeded by the total handicap numbers of the two participating ropers. The highest level of roping is the open roping, which is open to any roper but usually is entered by professional ropers (numbered 9), allowing the world champions to compete together. The lowest number is a true beginner, who would be a number 1 or 2. This handicap system allows the lower-level ropers to compete as a team with the world champions and to level the playing field of competition at all levels. The entry fees of the participants usually generate the purse money in a jackpot fashion. A portion of the entry fee is held out by the producer of the roping to pay for the arena, the cattle, and advertising, and the rest of the fee is placed in the purse money to be divided among the winners.
Dally team roping is a timed event involving five basic elements: the header, the heading horse, the heeler, the heeling horse, and the steer. The steers that are used for the team roping event are usually horned cattle called Corriente cattle, often from Mexico. Other types of cattle used are longhorns or other native homed breeds ranging in weight from 170 to 320 kg.
A typical run in dally team roping begins with a steer contained in a chute at the end of an arena. The heading box is to the left of the chute, and the heeling box is to the right of the chute. When the header calls for the steer, or asks that the steer be released from the chute, the chute gate is opened and the steer is allowed a head start called the score. If the header leaves the heading box before the steer crosses the score line, or reaches the predetermined head start, then the team is issued a penalty of 10 seconds. The timing of the run is begun when the steer crosses the score line.
When cued by the riders, the horses leave the roping box much as a racehorse leaves the starting gate to attain maximum speed as quickly as possible. As the header approaches the steer with the heading horse running at full speed, the horse is trained to rate off, or to slow up slightly, once the horse reaches the hip of the steer, to position the steer properly so that the header may rope the steer. Team roping has three legal head catches: both horns (a clean horn catch), a half head (one horn and the nose of the steer), or a neck. All other catches are considered illegal, and the team is given a no time.
After the header successfully catches the head of the steer and dallies (wraps in a full circle) the rope around the saddle horn, the heading horse drops its hindquarters and slows somewhat as it sets the steer and brings the steer’s head around to the left. As the steer’s body progresses to the left, the heading horse also is turned to the left and is moved out in front of the steer to allow the header to pull it across the arena at about a 90-degree angle to the original direction of travel, maintaining a constant slower speed, thus allowing the heeler to get into position to rope the hindlegs of the steer.
As the header sets and turns the steer, the heeler turns left following the steer and positions just behind and slightly to the left of the steer as it is taken across the arena. As the heeling horse follows the steer in this position, maintaining a constant speed equal to that of the header and steer, the heeler properly times his swing and then releases the heel rope, placing the loop under the steer and ropes the hindlegs of the steer. If only one hindleg is caught, then the team is issued a 5-second penalty. As the slack is taken out of the heel loop and as the dally is made on the saddle horn, the heeling horse is signaled to drop its hindquarters and come to an abrupt stop.
As the heading horse progresses away from the heeler with the steer still in tow, the ropes come tight, and when tight, the heading horse is cued to spin around to the right while maintaining a tight rope to face the steer. When the facing is complete, the rope is tight and in a straight line from the saddle horn of the header to the head of the steer and is tight from the hind feet of the steer to the saddle horn of the heeler, and then the flagman signals the end of the run and the time is taken.
The roping can be accomplished by experts in 6 to 7 seconds but requires thousands of hours of practice to achieve this and to minimize the danger to all the participants. Runs recorded in the range of 3.4 to 3.6 seconds have been made by the World Champion–caliber team ropers.
Conformation
The horses, predominately geldings, used in team roping are usually American Quarter Horses (QHs), preferred because of exceptional athletic ability, quick acceleration over short distances, and a good mind. Other breeds are rarely used. The head horse must be larger and faster than the heel horse. Head horses typically weigh 545 to 590 kg and are heavily muscled to tow the steer across the arena. The heel horse is smaller and quicker with more cow sense than the head horse. Horses that are trained for cutting but no longer are competing often make good heel horses because of size and cow sense. Team ropers prefer a mature, experienced horse, and so horses are usually over the age of 10 years, and many top ropers have horses in the mid to late teens. Therefore repetitive injuries are common, but because horses often have had several owners, a complete medical history is rarely available. In a recent retrospective study looking at lameness and poor performance in horses used solely for team roping, horses used for heading were significantly heavier (median weight, 545 kg; range, 473 to 603 kg) and older (median age, 12 years) than heeling horses (median weight, 490 kg; range, 441 to 545 kg; median age, 9.5 years).1
Training
The training of heading and heeling horses involves thousands of team roping runs and many thousands of miles of hauling. The horse must anticipate every variable of a team roping run, so that rider intervention is unnecessary. This allows the roper to focus on nothing but the speed of the run, which is an important factor contributing to injury. The current high demand for a finished team roping horse has greatly increased the value of these horses, and because replacement is difficult, veterinary advice is now sought more often.
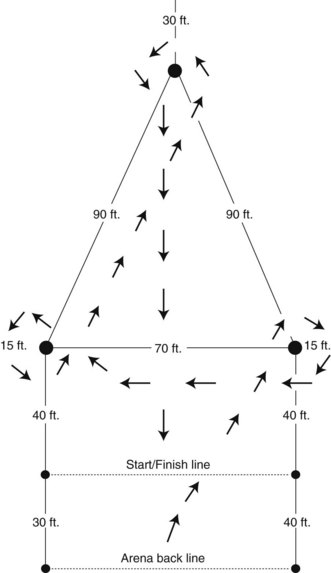
Historical Data and Decreased Performance
It is imperative for a clinician to know whether a team roping horse is used primarily as a heading or heeling horse. In addition, a thorough description of the owner’s complaint of a change in or decreased performance provides valuable insight into the underlying problem, bearing in mind that often in the early stages little or no lameness may be present. Eighty-nine of 118 (75%) team roping horses had a history of lameness, and 29 (25%) had an owner complaint of decreased or altered performance.1 The type of performance change differed between horses used for heading or heeling (Figures 120-1 and 120-2).
Lameness Examination
Team roping horses experience many of the same problems as any of the Western performance horses. In the heading horse, the right forelimb is placed under tremendous force after the steer is roped and just before turning 90 degrees. The right forelimb is placed cranially and laterally to decelerate and brace against its forward motion and the weight of the steer, thus placing tremendous strain on this limb (see Figure 120-1). A study reported that horses used for heading had significantly more right forelimb lameness (72%) than heeling horses (43%).1 The heading horse also had significantly more bilateral forelimb lameness (25%) compared with the heeling horse (9%).1 Heeling horses that did not turn properly into the steer after it switched directions often had left forelimb lameness.1 The distal tarsal joints are loaded with the rider’s weight, the horse’s weight, the deceleration of the full-speed forward motion, and the weight of the steer as primarily rotational forces. This occurs as the horse is asked to set and get under the steer and pull the steer’s weight forward across the arena. After a successful catch by the heeler, the heading horse must face or spin around to the right while the hocks and distal hindlimbs are loaded as described, and do so with the addition of a backward motion to maintain tightness of the rope. Although more forelimb versus hindlimb musculoskeletal problems were observed in horses used for heading, distal hock joint pain and osteoarthritis (OA) were the most common problems observed in the hindlimbs.
The heeling horse often has a similar history, with problems in the heeling box, not making the corner properly as the steer is set and turned, or nickering and bouncing out of the stop at the completion of a run while maximal tension is on the ropes. Clinical examination often reveals pain on palpation of the caudal lumbar area, the gluteal muscles, and over the point of both hips. This pain often is accompanied by the owner complaint that the horse is sore in the kidneys. If only the distal tarsal joints are involved, effusion usually is not detectable, but the horse may be reluctant to allow palpation of the medial aspect of the tarsus, as if anticipating pain. The dorsomedial distal aspect of the tarsus may be enlarged. High-quality radiographic examination of the hocks is essential. Intraarticular analgesia is often ineffective because the horse has developed performance problems in response to the pain experienced during every run, and the pain is anticipated, even though the area has been blocked. Thus horses become intractable in the roping box because they dread the pain that they will experience during the run. However, horses often respond well to intraarticular therapy when they realize, after several runs, that the pain has been lessened or stopped. The most common musculoskeletal problems causing lameness in horses used for heeling were (1) left forelimb palmar foot pain, (2) distal tarsal joint OA, (3) palmar foot pain and distal tarsal joint pain, (4) left forelimb pastern joint OA, and (5) hindlimb fetlock OA.
Diagnosis and Management of Specific Lameness
Palmar Foot Pain
Given the usual QH conformation of large body size and small feet or short, upright pastern conformation, navicular disease and injuries to structures within the palmar aspect of the foot are common. Right forelimb or bilateral palmar foot pain and left forelimb palmar foot pain were the most common problems identified in heading and heeling horses, respectively. Palmar foot pain results in a slowly progressive lameness, often bilateral, and horses may initially respond to intraarticular medication of the distal interphalangeal (DIP) joint, NSAIDs, and corrective shoeing. Soft tissue injuries of the palmar aspect of the foot (e.g., injury of the distal sesamoidean impar ligament [DSIL], a collateral ligament of the DIP joint, or the deep digital flexor tendon [DDFT] in the region of the navicular bone) are also common in heading horses and usually are acute, occurring during a roping event. Lameness is improved by perineural analgesia of the palmar digital nerves or intraarticular analgesia of the DIP joint. Often no radiological abnormality is apparent. Diagnosis of the specific structure injured can usually only be determined by magnetic resonance imaging (MRI).
The diagnosis of palmar foot pain is not complicated, but determining which structure is damaged can be challenging. Diagnosis is based on a combination of historical data and the response to perineural and intraarticular analgesia, high-quality radiographs, and possibly advanced diagnostic techniques such as nuclear scintigraphy, computed tomography, or MRI. Severity and duration of the lameness, the horse’s activity, potential owner compliance, and the experience of the owner’s farrier should be considered when determining therapy. The horse’s hoof wall quality, conformation, environment, and occupation all affect treatment.
A thorough musculoskeletal examination should include palpation of the digital pulse amplitudes and assessing the hoof capsule for increased heat. In 97% of 23 horses with palmar foot pain there was increased digital pulse amplitude in the most severely affected limb. Hoof tester evaluation can be beneficial in determining pain location. Pain involving the navicular area is identified by application of intermittent hoof tester pressure over the middle third of the frog, which results in persistent nonfatigable reflex withdrawal of the hoof from the examiner. However, false-negative results may occur, especially during periods of dry weather when the horse’s feet are excessively hard or in horses with thick soles and hard frogs. It is important to assess whether the withdrawal reflex is resulting from real pain and not a whimsical reaction by the horse. The results from both front feet should be compared. Horses with an injury of the DSIL or the insertion of the DDFT seem particularly sore with hoof tester pressure near the junction of the middle and dorsal thirds of the frog. Horses with underrun heels, bruised heels, or damaged laminae in the heel area often have more pain over the affected heel. It is important, if possible, to differentiate peripheral versus central hoof pain with a thorough hoof tester examination.
Many of the middle-aged roping horses diagnosed with palmar foot pain have moderate to severe radiological lesions of the navicular bone. My initial treatment involves correcting any existing hoof imbalance. I apply a 2-degree wedge pad or wedge shoe, which decreases the pressure on the navicular area by about 25%. If the horse’s foot was imbalanced and/or poorly shod, then correcting these problems combined with systemic NSAID therapy (phenylbutazone 1 g twice daily for 10 days) and rest may temporarily resolve the lameness. If the owner cannot rest the horse or the feet are properly shod, then I medicate the DIP joint using a combination of 9 mg of triamcinolone acetonide, 10 to 20 mg of hyaluronan, and 125 mg of amikacin.2 Postinjection care involves 4 to 5 days of no roping and NSAID therapy (phenylbutazone 2 g daily for 5 days). Approximately 60% of horses respond to DIP joint medication and, depending on severity of disease and level of work, will remain sound for 4 to 6 months. If the horse does not respond to DIP joint medication, then I medicate the navicular bursa with 10 mg of hyaluronan and 9 mg of triamcinolone acetonide, or if a severe bony lesion exists, I use 20 mg of methylprednisolone acetate plus 125 mg of amikacin. I reserve navicular bursa medication only for those not responding to DIP medication and known not to have an acute soft tissue injury (e.g., a DDFT lesion). Horses with chronic collateral sesamoidean ligament pathology, identified by the presence of a spur on the proximomedial or proximolateral aspects of the navicular bone, usually do not respond to DIP joint medication but do respond to treatment of the navicular bursa. I caution the owner that navicular bursa injections are invasive and may lead to subsequent DDFT pathology and/or rupture. Palmar digital neurectomy is the last resort in treating horses with palmar foot pain because of its short-lived results (average 2 years of soundness) and numerous complications, such as severe infection, DDFT rupture, and DIP joint subluxation.
Soft Tissue Injuries
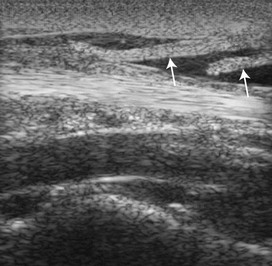
Ligament or tendon injury occurred in about 15% of heading horses, especially in the right forelimb, and in about 10% of heeling horses, usually in the left forelimb.1 The structure affected varied, but the suspensory apparatus, the accessory ligament of the DDFT, DDFT, superficial digital flexor tendon (SDFT), and the distal sesamoidean ligaments were all involved. These injuries usually cause lameness of varying degrees, and diagnosis by clinical examination is straightforward. Ultrasonography should be used to confirm the diagnosis. Distal sesamoidean ligament injury may be more difficult to diagnose but often results in acute, moderate to severe lameness (grade 2 to 3 of 5) after a run, associated with pain on palpation of the palmar aspect of the pastern. Perineural analgesia of the palmar digital nerves may improve the lameness, but analgesia of the palmar nerves at the base of the proximal sesamoid bones is needed for complete soundness. Fractures of the middle phalanx are also common; therefore the horse should be examined by radiography and ultrasonography. Ultrasonographic evidence of enlargement or reduction in echogenicity in the straight (SSL) or oblique sesamoidean ligaments (OSL) is diagnostic (Figure 120-3). Radiological examination is usually negative if lameness is acute; however, chronic injury is often associated with entheseous new bone on the palmar aspect of the proximal phalanx or on the proximopalmar aspect of the middle phalanx associated with OSL or SSL injury, respectively.
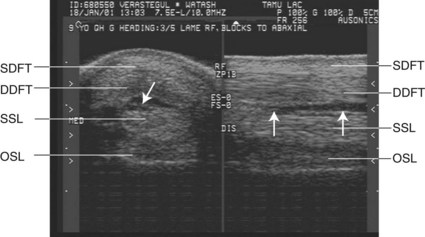
Fig. 120-3 Transverse (left) and longitudinal (right) ultrasonographic images of the midpastern region of the right forelimb of a head horse. There is a hypoechogenic lesion in the straight sesamoidean ligament (arrows) (SSL). SDFT, Superficial digital flexor tendon; DDFT, deep digital flexor tendon; OSL, oblique sesamoidean ligament.
In hindlimbs, deep digital flexor tendonitis, tenosynovitis of the digital flexor tendon sheath, and proximal suspensory desmitis (PSD) are common, especially in the left hindlimb of head horses. When turning to face the steer, the head horse turns 180 degrees at fast speeds, putting a rotational torque on the distal aspect of the left hindlimb (Figure 120-4).

Fig. 120-4 A head horse (right) turns to face the heeler at the end of the run. Note the strain placed on the left hindlimb.
The management of roping horses with these soft tissue injuries varies with which structure is affected and severity of the lesion, although the initial treatment is similar. The first 2 weeks consist of daily ice therapy for 20 minutes two to three times per day, NSAIDS (phenylbutazone 1 g twice daily for 7 days), stall rest with 10 minutes of handwalking, and a support bandage. This is followed by a variable period of stall rest with 15 to 20 minutes of daily handwalking. When the horse is sound and there is 80% resolution of any lesion seen using ultrasonography, a controlled exercise program is initiated to strengthen the affected structure (Box 120-1).
BOX 120-1 Exercise Regimen after Mild Injuries to Forelimb Suspensory Ligament or Accessory Ligament of the Deep Digital Flexor Tendon
| Weeks 1-2 | The horse is given stall rest or a small run (6 × 10 m) with support bandage on the limb, ice therapy, and nonsteroidal antiinflammatory drugs. |
| Weeks 2-6 | Length of time depends on severity of the lesion and structure affected. Horses are rechecked and ultrasonographic examination is performed at 3-month intervals until the horse is sound and the lesion is 75% to 80% healed. The horse is handwalked 10 minutes daily. |
| Weeks 6-8 | Confinement is continued with 15 minutes of handwalking twice daily. |
| Weeks 9-12 | Confinement is continued with 30 minutes of handwalking daily. |
| Weeks 13-16 | If horse is sound at the trot, then confinement is continued, but the horse is walked under saddle or is ponied 15 minutes a day plus 5 minutes of trotting. Five minutes of walking and trotting are added every third day. The horse is reexamined by ultrasonography before returning to roping activity. |
The horse remains confined until the controlled exercise program is completed. Lameness and ultrasonographic examinations are repeated before the horse returns to roping activity or turnout.
Distal Hock Joint Pain
OA of the distal hock joints is common, and heeling horses seem especially at risk. Most respond well to intraarticular medication of the centrodistal and tarsometatarsal joints. Middle-aged horses with moderate or severe OA are treated with 40 mg of methylprednisolone acetate and 125 mg of amikacin per joint. Younger horses or horses with mild to no radiological lesions are treated as above except 10 mg of hyaluronan is added to each joint. Postinjection care is 7 to 10 days off before returning to roping. The toes are squared on the hindlimbs to ease breakover and decrease torque on these joints.
Back and Pelvic Region Pain
Injury to the back and pelvic area is seen, especially in heading horses. Strain or tearing of the sacroiliac ligaments or epaxial musculature can occur. Radiographic evaluation is difficult and often unrewarding, but ultrasonographic examination may reveal longissimus lumborum and gluteal muscle tearing and can be used to evaluate the sacroiliac area. Lameness predisposing to back pain must be eliminated. Rest combined with topical heat (hot towels) and dimethyl sulfoxide or diclofenac (Surpass, IDEXX Pharmaceuticals, Inc., Greensboro, North Carolina, United States) helps many horses, but often months of rest are needed before the pain is eliminated. Treating the painful areas with local injections hastens the recovery time. I prefer a combination of 5 mL of methylprednisolone acetate, 5 mL of Sarapin, and 5 mL of prednisolone diluted with 30 mL of mepivacaine and then depositing 3 to 5 mL in several sites around the painful muscle or ligament. The horse is given 2 to 3 weeks of light riding, with no roping activity, and then is reevaluated by ultrasonography. Most horses return to roping activity within 4 weeks from the time of injury.
Obviously all team roping horses are also susceptible to any of the same injury problems that other equine athletes experience. Most of these injuries produce overt lameness, and diagnosis is usually straightforward.
Shoeing Considerations
Because roping horses are often middle-aged, are used frequently, and commonly have palmar foot pain, maintenance of proper hoof balance is critical in keeping these horses sound. Long toes and collapsed heels are common. The heels grow too far forward and are left unsupported and thus are at risk of abnormal concussion. We recommend trimming the heel back to the widest part of the frog and setting the shoe further back on the foot; thus the heels of the shoe end at the widest aspect of the frog. Care must be taken to fit the front shoes properly so that little of the medial side of the shoe is exposed because head horses have a tendency to grab this portion of the shoe and pull off a shoe, especially the left front shoe. Easing the breakover of the limb can be accomplished by rockering the shoe. A rim shoe or steel natural balance shoe provides good traction and allows an easier breakover by the rounded and rockered toe region of the shoe construction. The natural balance shoe has a wider web than a normal shoe and is beneficial for horses with sore feet acquired from performing on harder ground. If trimming alone cannot establish a correct hoof-pastern angle, a 1- to 2-degree wedge pad is recommended. We prefer a cutout pad because a full pad often traps moisture and can lead to thrush. Care must be taken to avoid pad pressure over the central region of the frog in horses with navicular pain.
In horses with deep digital flexor tendonitis, we recommend applying a 2- to 3-degree wedge pad for the initial 4 to 5 months of rest to decrease tension on the DDFT. The wedge is reduced gradually over three shoe resets, once the horse is sound. In horses with distal hock joint pain, we try to ease breakover of the hind feet by squaring the toes or by setting the shoe back under the toe 0.3 cm. Avoiding any type of trailer or extension on the rear shoes is also preferable, especially for a heading horse, because this can aggravate pain associated with distal hock OA.
Calf Roping and Breakaway Roping Horses
Description of the Sport
Calf roping originated on ranches of the Old West when sick calves were roped and tied down for medical treatment. Success in calf roping depends on the teamwork between a cowboy and a horse. After the calf is given a head start (like a scoreline in team roping), horse and rider chase the calf, and as the rider ropes the calf, the rider dismounts and runs to the calf. As the rider dismounts, the horse must sit back on its hind end and come to a sudden stop, which takes the slack out of the rope and stops the running calf. This allows the cowboy to catch the calf and throw the calf to the ground, termed flanking the calf. Once on the ground, the cowboy ties three of the calf’s legs together with a pigging string. The horse is trained to “work the rope” as the cowboy ties the calf, meaning to back up if needed to keep the rope tight, thus keeping the calf still for the rider to tie. When the cowboy completes his tie, he throws his hands up in the air as a signal to the judge that his run is complete. The calf must stay tied for 6 seconds. A 10-second penalty is added if the calf roper breaks the barrier at the beginning of the run. An 8- to 9-second run is considered good, and Jeff Chapman of Athens, Texas set the arena record in 1997 when he roped and tied a calf in 6.8 seconds.
Breakaway roping is similar to calf roping except the participants are women and children and the rider does not dismount and tie the calf. Instead, the calf is given a similar score or head start, and the horse and rider chase the calf and rope it around the neck. The rope used for breakaway roping has a quick-release device on it so that when the rope becomes tight, it snaps open and the calf runs free. After the calf is roped, the horse stops abruptly, the rope tightens and breaks away, and time is called. The rider remains on horseback. A typical breakaway time is 3.0 to 4.0 seconds.
Conformation
QHs are used for calf roping and must be athletic and well trained. Because the rider must dismount during calf roping, calf horses are usually not tall, often 14.2 or 14.3 hands high. Calf horses also have wide-base and muscular frontquarters and hindquarters. Many ropers believe that the performance demands on a calf horse are greater than those of a team roping horse.
Historical Data and Poor Performance
Calf roping and breakaway roping horses often show an alteration in performance before an observable lameness. There are no scientific studies specifically evaluating calf and breakaway roping horses. However, anecdotally the most common owner complaint is that a calf horse quits “working the rope,” that is, after the calf is roped, the horse does not want to back up and keep tension on the rope for the rider to catch and tie the calf. This is usually associated with hindlimb lameness. Another common complaint is that the horse ducks to the right or left after the calf is roped instead of stopping in a straight line. If the horse ducks to the right, this is usually because of left-sided pain that the horse is trying to avoid. A horse that will not run hard to the calf usually has front foot pain.
Diagnosis and Management of Specific Lameness
Calf horses have lameness similar to that of team roping horses with a few exceptions. Hindlimb lameness is more common in horses used for calf roping. OA of the distal hock joints is the most common problem, but stifle lameness also occurs frequently, such as collateral ligament or meniscal injury. However, diagnosis is usually not possible until after bony changes are seen radiologically, months after the initial injury. Bony reaction at the proximal medial aspect of the tibia is diagnostic. With rest, NSAIDs, and intraarticular medications, these horses often can return to roping, but at a lower level, perhaps as a calf roping horse for a child or beginner. Hindlimb proximal suspensory desmitis, traumatic fetlock OA, and fractures of the proximal sesamoid bones and middle phalanx are common. The most common forelimb lameness is palmar foot pain, often resulting from improper shoeing.
Shoeing Considerations
The same shoeing considerations are used for balance and protection of the navicular region in the forelimbs as described for team roping horses. Rim shoes or half round shoes are commonly worn on the front feet. In the hindlimbs if the toes of the feet are too short, so that the horse has a broken forward hoof-pastern axis, then the hind toe digs deep into the ground and the limb stops abruptly, causing sudden torque on the distal aspect of the limb. Having more toe length and a shoe that fits full with the heel branches of the shoe extending to the heel bulbs is preferable, so that the horse slides as it stops. This not only protects the heel bulbs from the ground surface, but it also puts less strain on the distal aspect of the limb. Horses used for calf roping often wear skid boots, protective leg gear aimed at minimizing friction between the ground surface and the plantar aspect of the hindlimb fetlock joints, because the horse skids to a stop.
 The Reined Cow Horse
The Reined Cow Horse
Van E. Snow*
The National Reined Cow Horse Association was initiated in 1949 as the California Reined Cow Horse Association and changed its name in 1970. The purpose of the association is to preserve the training traditions of the vaqueros, the horsemen of early California, who trained their horses for ranch work. As a result of selective breeding and refined training techniques, reined cow horses today are able to achieve more with livestock than was ever thought possible.
The National Reined Cow Horse Association held its first Snaffle Bit Futurity in 1970 in Sacramento, California. Bobby Ingersoll, a renowned cow horse trainer, had the idea to showcase the best all-around cow horses in the world. The competition involves showing the horse in three different disciplines: herd work (cutting), rein work, and cow work (working a cow down a fence). In the Snaffle Bit Futurity, the top 20 horses from the first round of competition come back and do another round over 2 days, starting again with even scores. The sport of reined cow horse has evolved from 1970, when 27 horses competed for $3900, to now when hundreds of horses compete at their annual futurity for nearly $1 million.
The professionals compete on numerous horses in four divisions: snaffle bit, hackamore, two rein, and bridle. Competition consists of numerous levels, including professional, nonprofessional, amateur, and limited open. An auction is held each year at the reined cow horse futurity at which horses that range from 1 to 12 years of age and breeding stock horses are available for sale.
Affiliate groups of the National Reined Cow Horse Association are organized in Canada, Germany, Belgium, and Australia, and a strong interest in the group exists in most of Europe and in South and Central America. No restrictions exist as to the breeds allowed to compete in the futurities. Numerically the American Quarter Horse dominates, but Paint horses often compete successfully, and an Appaloosa has won.
The competition requires that a horse be accomplished in its ability to run, stop, turn, and “read” and control a cow. These horses also must have a high level of endurance. These qualifications do not necessarily dictate a particular body type, but a reined cow horse tends to be a taller, leaner horse than a cutting horse. Stallions, mares, and geldings compete equally, as do all genders and age groups of riders.
Reined cow horses typically begin training when they are less than 2 years old and start to compete at 3 years of age. They have about 20 months to learn all of the events and to become conditioned well enough to withstand the rigors of competition. This requires that the training surface, shoeing, and judgment of the trainer be optimal throughout the 20-month period.
Most trainers have become knowledgeable in the prevention and the early detection of lameness. Musculoskeletal evaluations are done quarterly on the futurity prospects, beginning in the fall of the 2-year-old year. These evaluations include a complete lameness evaluation, including flexion tests. At this time, good baseline information on each horse is established, and future insidious problems can be detected before they become unmanageable. In the past, it was commonplace for a trainer to blame himself or herself or the horse’s attitude for not being able to accomplish a certain task, when in fact low-grade lameness was developing. The trainer would continue to train the horse, and often a serious lameness would develop. For a trainer to suspect a subtle lameness and to have the horse evaluated is much more common now. Lameness detected at this point is usually manageable.
A reined cow horse continues to compete beyond 3 years of age. As 4-year-olds, they can continue in the snaffle bit or begin in the hackamore or bridle class. The 5-year-olds are shown in the hackamore or bridle class, and the 6-year-olds compete in the bridle class. Hackamore and bridle horses compete in the reining and cow work divisions, but they do not do herd work. The intention is to finish a horse’s education by the time the horse is 6 years old.
Training Surfaces
The training surface has a strong influence on lameness in terms of incidence, degree of severity, and type of injury. In general, an arena or round pen is best constructed as follows: the original ground is graded to a 1.5% grade from one corner to the other and is compacted to 95%. A 15-cm thickness of base material such as limestone rock dust is then added, watered, and compacted to 95%. The type of base used is dictated by what is available in the area, but it should be smaller-sized particles (not small rocks) that have interlocking edges. A 1.5% grade should be maintained. Sand is then added to the top of the base to a thickness of at least 5 cm and not more than 12 cm in the arena, and from 10 to 15 cm in a round pen. Adding the sand at the minimum levels first and then adding more later if necessary is recommended. In general, less injury occurs with thinner layers of sand, but performance may be enhanced with thicker layers of sand. Fine beach sand is the best because it has low abrasive characteristics and is light. These qualities are important because the sand gets between the skin and protective boots and also comes in direct contact with the back of the pasterns and fetlocks. If the sand is coarse and abrasive, it damages the skin and causes lameness. The density of the sand is important because a horse has to push the sand during sliding stops, and if the sand is too heavy, it causes injury and destroys the horse’s confidence.
Water content of the training surface is also an important consideration. In general, applying water a few hours before use is a good idea, so that the water is distributed evenly. If the training surface is too deep with sand or if the base is not consistent, I see more soft tissue injuries such as tendonitis, suspensory injuries, curbs, and sprained backs. If the training surface is too hard, I tend to see bone injuries such as osteitis of the distal phalanx, navicular syndrome, sesamoiditis, or fractured proximal sesamoid bones.
The Relationship of Training to Lameness
The types of injuries commonly seen tend to vary as the training progresses. The young 2-year-olds have hoof and sole problems during the initial breaking process, before they are shod, associated with an increased digital pulse amplitude and sensitivity to hoof testers. Subchondral bone cysts in the medial femoral condyle and osteochondrosis of the fetlock may manifest at this time. Chip fractures, present but unnoticed when the horse was a foal or yearling, may become clinically apparent when ridden work starts.
The work during the latter half of training for a 2-year-old involves more speed and collection, and low-grade lamenesses may develop that later become persistent problems. These lamenesses include suspensory desmitis, navicular syndrome, and hock and stifle pain. The 3-year-old year involves even more collection, cow work at speed, and harder stops. We generally see a continuation of the 2-year-old problems, if they are not managed well, and also more acute injuries to soft tissue and chip fractures of the fetlock and carpus.
Conformation and Lameness
Conformation has an effect on the development of lameness, but I believe that conformation often is overemphasized. The component of conformation that has the biggest effect on soundness is body conformation and the degree of balance in motion. I have seen many horses whose conformation was not impressive when viewed at a standstill but were impressive when evaluated in motion. Balance in motion is that somewhat immeasurable quality that gives one the impression that the horse could jump, stop, turn, or do almost anything on any given stride without effort. In my experience, these horses remain sound while performing to an exceptional level, whereas horses that have less balance suffer more frequent injury. Although static conformation related to lameness is important and should be evaluated, in my opinion, conformation in motion is equally important.
The most common conformation problems that I see are toed in and toed out. These problems predispose the horse to lameness but are present to some degree in nearly all horses. Most often these conformational abnormalities are associated with injury to the suspensory ligament (SL) and also can be associated with injury to the collateral ligaments of the digit. I try to manage these conformation faults before they cause injury to the horse by trimming and shoeing. A horse that toes out initially contacts the ground with the outside toe quarter with improper trimming. The hoof then slides along the ground and begins to rotate the toe out. The inside heel bulb then makes contact with the ground, and the hoof rotation stops. However, this rotational force continues up the limb and places unnatural strain on the soft tissues below the carpus and eventually causes damage. I recommend removing more wall from the hoof at the point of contact and beveling the toe so that breakover is accomplished easily over a wide area. My goal is to get the entire hoof to contact the ground evenly and eliminate the rotational force. Horses that toe in generally contact the ground at the inside toe quarter. Horses with this problem need more hoof removed from the inside toe, the goal being to cause the foot to land flat.
Lameness Evaluation
I begin the lameness examination by obtaining as complete a history as possible. I establish the duration of lameness; any change in lameness, if the horse has been rested or kept in work; any response to treatment; alteration in lameness with work; when the horse was last trimmed and shod; any changes in footing, type of work, or shoeing; if lameness was associated with turnout or work; if the horse has received any intramuscular injections; if the horse kicks the paddock or stall; if the horse is turned out with others; if the horse stumbles; any known trauma; whether the lameness occurred insidiously or suddenly; and if the horse stands normally. Generally, the best history is obtained from the grooms and trainer, although some owners can provide information.
I watch the horse at the walk, trot, and canter, loose in a 9-m round pen, and on firm footing on a 2% slope. The degree of lameness often is amplified when the horse is loose, on hard ground, and allowed to work on a slight slope. Some lameness characteristics are best seen at a slow trot and some at an extended trot. The round pen enables one to evaluate the horse’s ability to hold leads. Detecting low-grade ataxia is also easier when the horse works free, especially during downward transitions.
Lameness may be manifest in how a horse does a sliding stop; lameness may be accentuated after several sliding stops from a canter. A horse may slide stronger on one hindlimb than the other. The complaint is often made that a horse is not stopping as well as previously, although lameness is not noticed. A horse may begin a sliding stop normally but then pick up the painful limb halfway through the stop and replace it. The stop is not held evenly. The stop becomes normal if pain is removed by local analgesia.
Another common situation occurs when a horse is cutting a cow; the horse runs off at one end or does not come back with the cow as strongly at one end. The hindlimb farthest from the cow before the weak turn is generally the lame limb. If this horse is asked to do rollbacks in a round pen, the horse is much weaker when it reverses direction one way. Generally, the hindlimb on the outside of the circle after the weak rollback is the lame limb.
Competition is now so great that the difference between winning and losing is sometimes a matter of which horse feels the best. Performance diminishes before outright lameness is noted. Hindlimb lameness is particularly common in reined cow horses because of hock or stifle pain or proximal suspensory desmitis.
Flexion tests include flexion of the digit in all limbs and carpal, hock, and stifle flexions. Notes are made on the results and whether the horse resented flexion. The digit is flexed in an oblique plane (applying medial and lateral torque), and any resentment or decreased elasticity is noted.
All the soft tissue structures are palpated, and any enlargements and sensitivity are noted. Hoof testers always are applied to the front feet, as well as to the hind feet of horses with hindlimb lameness. Any lameness or weakness is classified in degrees (grade 1 to 5); by the limb involved; by weight bearing or non–weight bearing or mixed status; by the effect of walking in a circle or on a straight line, on an incline or decline; by flexion tests; and by the effects of prolonged digital pressure over sensitive areas.
If lameness is serious enough possibly to be caused by fracture, radiography is performed first; otherwise, diagnostic analgesia is used to establish the source of pain. Intraarticular analgesia is more specific than regional analgesia, which can be done at a later time if necessary; therefore I often start with intraarticular blocks, especially in forelimbs. I rely on the flexion tests to direct the start point. If flexion of the distal limb is normal but carpal flexion is positive, I usually use perineural analgesia of the proximal palmar metacarpal and palmar nerves (high four-point). If lameness persists, I perform intraarticular analgesia of the carpus. If flexion of the distal limb is positive, I perform intraarticular analgesia of the distal interphalangeal (DIP) joint first and then proceed to the pastern and fetlock joints if necessary to eliminate the pain causing lameness. If intraarticular analgesia is not helpful and the flexion test is still positive, I perform perineural analgesia of the palmar digital nerves, followed by the digital nerves at the base of the proximal sesamoid bones (PSBs) and later a “low four-point block.” Knowing whether the problem is articular is useful because horses with articular problems are often more amenable to treatment.
For intraarticular analgesia I do a three-step povidone-iodine (Betadine, Purdue Products L.P., Stamford, Connecticut, United States) and alcohol skin preparation and use sterile gloves. I place a subcutaneous bleb of local anesthetic solution before injection and combine local anesthetic solution with gentamicin sulfate (40 mg).
In a hindlimb I usually use perineural analgesia proximal to the fetlock, local infiltration around the region of the origin of the SL, intraarticular analgesia of the centrodistal and tarsometatarsal joints separately, and intraarticular analgesia of the femoropatellar and medial femorotibial joints. The lateral femorotibial compartment rarely is involved. If the response to a low four-point block is positive but the response to plantar nerve blocks at the base of the PSBs is negative, intraarticular analgesia of the metatarsophalangeal joint is performed the following day.
Imaging Considerations
Once the region of pain is localized, the area is examined using radiography and ultrasonography to identify the exact structure that has been damaged and to assess the degree of damage. The more specific I can be at this point, the more reliable the prognosis and treatment are. If the diagnosis is not specific, scintigraphy often is used. Generally, a differential diagnosis list is generated based on the physical examination. Developing a therapeutic plan based on a tentative or vague diagnosis is a mistake. Nearly all diagnoses are tentative until the pain has been localized as specifically as possible through the use of diagnostic analgesia and appropriate imaging.
Proceeding without a Diagnosis
Sometimes the site of pain causing lameness cannot be discovered, even after all the joints and nerves have been blocked and a complete scintigraphic examination has been performed. I then treat the horse for myofascial pain with drugs or chiropractic therapy. If the horse responds to these therapies, then this is indirect evidence of the cause. Another possible cause is equine protozoal myelitis (EPM). Horses with EPM may show chronic lameness without other neurological signs.
Lameness and Shoeing Considerations
Proper foot balance is critical to resolving all lameness problems successfully. The foot should be trimmed to land evenly. Any medial-to-lateral imbalance should be removed by trimming. If the point of contact is the lateral toe quarter, then enough of the lateral wall should be removed so the foot lands flat. The foot should be trimmed or a wedge used to achieve a hoof angle that is the same as the pastern angle (about 55 degrees in forelimbs and 57 degrees in hindlimbs). A square-toed shoe that has a wide bevel, which extends from the medial to lateral toe nail holes, commonly is recommended and is useful. The shoe should be set back so the dorsopalmar axis is shortened. The heels are trimmed so the shoe comes in contact with the wall at the widest section of the frog. These specifications are designed to remove rotational forces up the limb that occur in horses with medial-to-lateral imbalances, to provide mechanical advantage to the palmar/plantar aspect of the limb that occurs in horses with a long toe and low heel, and to reduce concussion to the digit that occurs in horses with the two-phase foot impact associated with foot imbalance.
An egg bar shoe is used for horses with moderate to severe tendonitis, suspensory desmitis, or an apical PSB fracture. A reverse shoe is used sometimes for horses with navicular syndrome, ringbone, sesamoiditis, suspensory desmitis, tendonitis, constricted palmar/plantar annular ligament, carpitis, and tarsitis. Horses with bruising in the sole are shod with soft dental acrylic pads. Horses with heel and quarter cracks are managed with egg bar shoes.
Treatment of Lameness
Suspensory Desmitis
For horses with suspensory desmitis, it is important to optimize foot balance as previously described. Corrective shoeing is designed to minimize any further physical damage and therefore prevent further pain and inflammation. Other treatments provide short-term results and are aimed at reducing the existing inflammation.
Horses with minor to moderate fiber disruption are treated with perilesional injections of Sarapin and corticosteroids. If the lesion is proximal, a sterile skin preparation is recommended, with the addition of gentamicin sulfate (40 mg) in case the carpometacarpal joint is entered inadvertently. The drugs are injected under the loose tissue between the SL and the accessory ligament of the deep digital flexor tendon. Middle carpal joint pain may occur concurrently and is treated using intraarticularly administered corticosteroids, provided that no radiological abnormalities are apparent. Physical therapy in the form of electrical stimulus modalities or low-level light laser therapy is started 3 days after injection and continued as needed through the intended competition. Magnets of 600 to 1200 G placed over the site have been used successfully and are kept in place for 60 days and then as needed for soundness.
The lesion is monitored monthly using ultrasonography. If conservative treatment fails, extracorporeal shock wave therapy (ESWT) is used and administered with the horse under general anesthesia. Up to four treatments have been used, combined with rest for 60 to 90 days.
Centrodistal and Tarsometatarsal Joint Pain
Intraarticular injection of corticosteroids is effective at relieving pain and inflammation in the centrodistal and tarsometatarsal joints. Horses are allowed to rest for at least 10 days after injection, and then work gradually is increased as soundness dictates. The systemic use of hyaluronan and acetylglucosamine is helpful for maintenance. Orally administered chondroitin sulfate and glucosamine products also have been useful. If medication is ineffective, joint drilling or forage to induce joint ankylosis, or periarticular ESWT can be used effectively.
Navicular Syndrome
Navicular syndrome is diagnosed based on a positive response to palmar digital analgesia and analgesia of the DIP joint, radiography, and scintigraphy. Radiology can be misleading, and in my opinion scintigraphy is the most reliable method of diagnosis. Corrective shoeing is essential. Isoxsuprine hydrochloride (600 mg) is given orally once daily for 60 days. Aspirin (15 g) also is given orally once daily for 60 days. If this combination provides relief, it is continued for another 60 days or until the horse finishes the futurity season. Injection of the DIP joint with corticosteroids, or a combination of corticosteroid and hyaluronan, often provides temporary relief (about 30 days).
If a horse fails to respond to corrective shoeing and medications, ESWT is indicated and has been effective, except in horses with entheseous new bone at the attachment of the collateral sesamoidean ligaments. Palmar digital neurectomy is used as a last resort.
Traumatic Hoof Injuries
Horses with bruises and cracks in the hooves respond well to egg bar shoes with soft dental acrylic pads or metal pads. A horse with a quarter crack is treated by trimming the wall palmar/plantar to the defect, so that no contact is made with the shoe, that is, floating the heel. The air gap is up to 6 mm deep and is reopened daily using a hacksaw blade to relieve pressure between the hoof wall and the shoe until the defect has grown out. If the crack is moving and bleeding, a copper patch is attached to the wall with screws to span the defect and therefore stabilize it.
Superficial Digital Flexor Tendonitis
Ultrasonography is used to characterize size and position of the lesion in horses with superficial digital flexor tendonitis. If a lesion is small, the owner or trainer usually decides to continue preparing for the futurity. It is important to try to determine the circumstances that caused the lesion to develop to eliminate further damage. Possible causes for tendonitis include poor hoof balance, deep footing, fatigue, speed, overexertion from working a difficult cow, uncontrolled exercise (turnout), interference from hindlimbs, tight bandages, poorly fitting support boots, and hanging a leg on a hot walker, tie rope, or fence.
Therapy for tendonitis involves depositing corticosteroids in the loose subcutaneous tissue in the proximity of the lesion. The leg is wrapped in a gelocast for 3 days and then is treated with ice and laser or electrical stimulus therapy. The horse is walked in hand or under saddle for 15 minutes twice daily for 7 days. Training then is resumed. The leg is maintained in a support wrap continuously. Shoeing, good footing, and conservative training are critical to the healing process.
Stifle Pain
If no abnormalities are detected in the stifle radiologically, the affected joints are treated with intraarticularly administered corticosteroids and hyaluronan. The horse is prescribed weekly injections of systemic acetylglucosamine, which continue through the futurity. Subsequent intraarticular injections are not performed sooner than 6 months and preferably not at all.
If radiological evidence of osteochondrosis of the trochlear ridges of the femur exists, the same therapy is effective. The prognosis for horses with subchondral bone cysts of the medial femoral condyle is dismal, and I do not recommend that these horses continue training to be futurity horses.
Metatarsophalangeal Joint Pain
Metatarsophalangeal joint pain may be caused by traumatic osteoarthritis, fracture of a PSB, sesamoiditis, fragments detached from the proximoplantar aspect of the proximal phalanx, or periarticular soft tissue injury. If no radiological lesions are present, the horse is treated with intraarticularly administered betamethasone and hyaluronan, followed by 10 days of rest. Systemic glucosamine is given every 2 weeks as maintenance therapy. Orally administered glucosamine and chondroitin sulfate also seem to be useful in managing metatarsophalangeal joint pain. Shoeing imbalances must be corrected concurrently.
Sesamoiditis
The foot must be properly balanced to treat sesamoiditis. Egg bar shoes with a square toe and a wide roll or bevel are used. The shoe is set back to minimize the leverage on the palmar/plantar aspects of the fetlock. The hoof angle is optimal when it matches the pastern angle. Isoxsuprine hydrochloride (600 mg) and aspirin (15 g) are given orally once daily for 60 to 90 days. Electromagnetic energy is applied to the affected region every other day for 3 months and thereafter as needed for soundness. The amount of training is dictated by the degree of soundness.
Distal Interphalangeal Joint Pain
The foot must be properly balanced to treat reined cow horses with DIP joint pain. Soft dental acrylic pour-in–type pads and shock-absorbing rim pads can be helpful. Intraarticular injection of a corticosteroid and hyaluronan is followed by the systemic use of acetylglucosamine and hyaluronan. It is imperative that training is continued on a soft surface.
Osteitis of the Distal Phalanx
Soft dental acrylic pour-in–type pads and shock-absorbing rim pads are used to treat horses with osteitis of the distal phalanx. The horse is treated with isoxsuprine hydrochloride (600 mg), aspirin (15 g), and phenylbutazone (2 g) given orally once daily for 60 days and then as needed for soundness. Training must be done in soft footing to reduce concussion to the foot. ESWT has recently been introduced to manage horses with osteitis of the distal phalanx. The Editors question whether shock waves can penetrate the hoof capsule, or whether they have adequate depth of penetration if administered via the heel bulbs.
 Barrel-Racing Horses
Barrel-Racing Horses
Barrel racing began in 1948 when a group of Texas ranch women started riding horses around a cloverleaf pattern of barrels and the fastest horse around the course was the winner. Barrel racing has evolved into a multimillion-dollar industry called the Women’s Professional Rodeo Association (WPRA). From this original organization many other barrel racing associations, which host numerous futurities for horses 4 or 5 years of age or younger and derbies for older horses, have arisen.1-5 Now (from the WPRA website) “WPRA barrel racers compete for millions of dollars each year, culminating in twelve circuit finals rodeos held throughout the country, the Dodge National Circuit Finals Rodeo held in Pocatello, Idaho in April, and the Wrangler National Finals Rodeo held in Las Vegas each December.” The major competitions are divided into rodeo, futurities, derbies, open jackpots, and professional levels. Futurities and derbies are classified by age of the horse. Open competitions are open to any horse or rider and are highly competitive. Within the open jackpots, a new classification of barrel racing has developed, termed a 3D or 4D competition, which includes a handicapping system that allows less experienced horses or riders to compete with seasoned horses and riders.
Barrel racing is a timed event with the clock beginning when a predetermined line is crossed. Three barrels (55-gallon steel drums) are positioned in a triangle or cloverleaf (Figure 120-5). The contestant must turn the left or right barrel first (most choose to turn the right-hand barrel first) in a manner that the path always crosses. The distance covered for the pattern varies with the size of the arena, but generally the distance from the starting line to the first barrel is 14 to 18 m. The distance between the first and second barrel is 21 to 27 m and between the second and third barrel is 27 to 32 m. The horses must start at the alleyway or entrance to the arena, run at full speed to the first barrel, slow down and complete a 360-degree turn around the barrel, speed up and run to the second barrel, turn 360 degrees, head to the third barrel, turn 360 degrees, and then sprint to the finish line. The fastest time to complete the pattern varies with distance of the pattern and arena size, but a good run for a large arena pattern is 15 to 16 seconds. An electric eye timing system usually is used, and times are recorded in hundredths of a second. If a rider hits a barrel and tips it over, a 5-second penalty is imposed. If the horse and rider fail to negotiate the pattern correctly, they are disqualified. The arena is often leveled after each horse.
Conformation
Horses are predominately American Quarter Horses (QHs) and Appendix horses (QH and Thoroughbred [TB] crosses), but occasionally TB, Paint, or Arabian horses are seen. Speed, quick acceleration, and agility to slow down quickly to turn the barrel are essential. Many barrel horses have QH racehorse pedigrees. Some prefer stockbred horses, which usually have a calmer personality. Geldings are preferred. Horses usually range from 14.3 to 15.1 hands. Barrel horses are not usually as muscular and wide based as calf roping horses. They usually have long, leaner muscle mass that provides the speed and flexibility needed to perform the 360-degree turns. In a recent retrospective study evaluating musculoskeletal problems in 118 horses used solely for barrel racing, the median age was 9 years (range, 3 to 19 years), median weight was 509 kg (range, 409 to 611 kg), and 73% were geldings and 27% were mares.6
Training
Futurity competitions are popular because of the amount of prize money, and training usually starts at 2 years of age. Futurity horses often have short careers because of the pressure to perform at a high level of competition at only 4 to 5 years of age, resulting in advanced osteoarthritis (OA), often in the distal tarsal joints. Successful futurity horses seldom have long-term careers because of behavioral problems or performance-limiting injuries.
Horses that are 5 years of age or older, started slowly, and are allowed to mature before performing in serious competition may compete professionally for 5 years.2 The average age of a professional barrel horse is 10 to 15 years. Horses may compete in 50 to 100 rodeos per year and spend much time traveling. An experienced barrel horse is trained by practicing turns but rarely uses the barrels because the horse learns to anticipate the pattern and tires of it. Many professional horses are ponied (led from another horse) or are ridden just enough to keep them fit for competition, but they are never really worked unless competing.
Older, semiretired horses that are well trained to the barrel pattern, but not fast enough for upper-level competition, may be used for a child or beginner. These horses do make repetitive barrel pattern runs in a practice pen for the rider to learn and often have use-related injuries, requiring much maintenance therapy to withstand the number of practice runs needed to teach a beginner.
Historical Data and Poor Performance
Barrel racing is the one equine discipline that most riders train and ride their own horses. Unlike roping events where many variables exist (e.g., cow selection and partners), there are few variations in the barrel horse pattern or run. Size of arena and ground surface may affect the speed of the run, but the barrel pattern is constant, and most riders know what time to expect from their horse for a given arena size. Therefore more barrel horses are examined because of a change or decrease in performance (40%) compared with roping horses (about 25%), rather than overt lameness. In a recent study, 45% of barrel horses that had an owner complaint of running past or wide around the first (right) barrel had a right forelimb musculoskeletal problem.6 Unilateral or bilateral forelimb foot pain or subclinical epistaxis was observed in horses that had a recent decrease in speed. Horses that were reluctant to turn to the left had either a left forelimb or hindlimb musculoskeletal problem.
Other musculoskeletal problems depend on the horse’s age and level of competition. A young futurity barrel horse may run up the fence, that is, the horse does not turn around the barrel but runs past it up the arena, or it may refuse to enter the arena. No lameness may be detectable, and the veterinarian has to determine whether the young horse is mentally stressed and showing behavioral problems or is responding to pain. Several options are presented to the owner to help determine whether the horse is responding to pain or it is a result of overtraining. One option is to administer phenylbutazone (2.2 mg/kg daily for 2 weeks and then 1.1 mg/kg daily for 2 weeks) for 30 days and to keep the horse in barrel race training. If the horse returns to normal performance, then it is concluded that the horse is most likely experiencing pain. If the problem does not resolve, then I try to address any behavioral problems. If problems persist, I often suggest giving the horse a 3- to 6-month break from barrel racing and have the horse work cattle or perform other less intense activities. A second option is to increase the workload and try to establish whether lameness can be identified and then located with diagnostic analgesia, but few owners select this option. Older, experienced horses usually have pain-related problems.
Most barrel racers train their own horses, and the quality of training is inconsistent, and performance changes may be induced by the rider. Determining which barrel is the problem barrel is helpful. An owner may complain that the horse will not stay in the ground for the first barrel but works fine for the second and third barrels. The horse may perform well for the first barrel but does not make a good turn around the second barrel. The first barrel (usually going to the right) is the hardest barrel and most often a problem because the horse is running at full speed when it reaches the barrel and must slow quickly to make the 360-degree turn. When the horse is turning the barrel, the inside forelimb and hindlimb appear to be under the greatest pressure (Figure 120-6). If the owner complains that the horse is swinging wide or pulling away from the first barrel, the horse does not want to turn to the right and is probably trying to avoid right hindlimb or right forelimb pain.

Fig. 120-6 A barrel horse turning a barrel. Note the pressure on the inside hindlimb. This horse is on the backside of the barrel coming out of the turn and is in correct position. At this point in the barrel turn, a horse with hindlimb pain becomes uncollected and swings wide around the barrel.
The teeth are always evaluated to eliminate bitting problems as a cause of performance changes.
Lameness Examination
A barrel horse does not run at top speed over long distances like flat racehorses; therefore fatigue-type injuries like superficial digital flexor tendonitis or fetlock and carpal chip fractures are seen less commonly than in racehorses. Some of the common injuries seen in barrel horses are attributed to the twisting and turning motion of the horse at high speeds (see Figure 120-6).
In a recent study, the most common musculoskeletal problem observed in horses used solely for barrel racing was (1) forelimb foot pain (33%), with the right front more often affected; (2) OA of the distal tarsal joints (15%); (3) suspensory branch desmitis or tendon injury (14%); (4) a combination of foot pain and distal tarsal pain (12%); and (5) medial femorotibial joint pain (10%).6
If an obvious lameness is not detected when trotting the horse in a straight line or large circle, the horse is trotted in hand in a small circle (1.5- to 3-m radius), mimicking the barrel turn, which will exacerbate the lameness. This may be the only time the horse shows lameness.
Diagnosis and Management of Specific Lameness
QHs and Appendix QHs make up most of the barrel horses. Sore feet, navicular area pain, and palmar foot pain are the most frequent causes of forelimb lameness, with poor hoof conformation and farriery and hard arena surfaces being predisposing factors. Diagnosis and management are similar to those described for the team roping horse.
Distal hock OA is the second most common musculoskeletal problem and most common hindlimb problem most resulting in reduced performance or lameness. Diagnosis is based on intraarticular analgesia, radiology, response to treatment, and sometimes nuclear scintigraphy. The centrodistal and tarsometatarsal joints are treated using methylprednisolone acetate (40 to 60 mg/joint) or triamcinolone acetonide (6 mg/joint) alone or in combination with hyaluronan (10 mg/joint) plus 125 mg of amikacin. Ideally the horse should have 7 to 10 days of turnout or light exercise before returning to barrel racing, but often the competition schedule does not allow this. Response to treatment may take up to 3 weeks. If the horse does not respond to treatment, we reevaluate the horse for lameness.
Hindlimb proximal suspensory desmitis (PSD) and suspensory branch desmitis are common in older, seasoned horses and can be career-ending injuries. Deep sand in arenas may contribute to the high incidence. Moderate lameness (grade 2 to 3 of 5) often is exacerbated by upper limb flexion. The horse usually has no swelling or minimal swelling and no heat and pain for proximal suspensory body lesions, but these will be seen in horses with suspensory branch desmitis. Local analgesia is essential to verify the source of pain. Radiology of the proximal metatarsal area is often negative, although if the condition is chronic, endosteal reaction or entheseous new bone may be present, seen as increased radiopacity. Ultrasonographic examination may reveal an enlarged and hypoechogenic SL, but some horses have no detectable structural abnormalities. The latter are treated by local infiltration of triamcinolone acetonide (9 to 12 mg) and reduced work. With acute, mild PSD, horses often return to work in 2 to 4 weeks. I also recommend confining the horse to a small area to avoid further damage from excessive uncontrolled exercise. If ultrasonographic abnormalities are detected, the horse is confined to a small area (12- × 30-foot [3.7 × 9.1 m] run) with no riding for 60 to 90 days before reexamination. Complete healing often takes 6 to 12 months, and some horses never return to full athletic function. After the initial 2 weeks of ice therapy, rest, nonsteroidal antiinflammatory drugs, and support bandages, the horse is reevaluated. If the lesion is extensive or severe (type 2 or greater on a scale of 0 to 4), then novel tissue healing therapies such as platelet-rich plasma (PRP) or stem cells are injected into the lesion under ultrasonographic guidance to enhance quality of ligament fiber repair. I have had more experience with PRP and prefer it to stem cell therapy, but both may be beneficial in ligament healing. Hindlimb PSD can be difficult to treat because of the constricting thick fascia surrounding it. If the horse is not sound after 4 to 6 months (depending on severity of lesion) of confinement, then I have had good success performing a fasciotomy and neurectomy of the deep branch of the lateral plantar nerve. Postsurgery care consists of 60 days of stall rest with 20 minutes of daily handwalking and 60 days of controlled exercise program before returning to barrel racing or turnout activity.
PSD is also common in forelimbs. Deep arenas and long toes and low heels are predisposing factors. The prognosis for barrel racing horses with forelimb PSD is good, with most horses responding well to rest and controlled exercise for 3 to 4 months. Tendon protection boots are recommended.
Medial femorotibial joint pain also frequently occurs and is treated in a similar manner as described above for cutting horses (see page 1167). If the lameness is recurrent after several intraarticular injections, diagnostic arthroscopy is recommended. Metacarpophalangeal joint synovitis results in mild lameness (grade 1 to 2 of 5) that is exacerbated by fetlock flexion. The horse often strongly resists fetlock flexion. Lameness and response to fetlock flexion are eliminated by intraarticular analgesia. Radiology is usually negative. The horse is treated with intraarticularly administered triamcinolone acetonide (6 mg) and hyaluronan (20 mg). The problem may or may not recur. If recurrence is frequent, diagnostic arthroscopy is recommended.
Many times horses have undergone several types of alternative therapies (e.g., equipment changes, acupuncture, chiropractic, and herbal therapy) in an attempt to correct the perceived problems before being checked by a veterinarian. Often, for some inexplicable reason, an accurate diagnosis and conventional medical therapy are sought only after failure of these other treatments. Many owners rely on diagnosis from a fellow competitor and request treatment that was successful in another horse. This makes client communication difficult.
Shoeing Considerations
Traction, especially in the deep and often muddy arenas in which horses compete, is critical. A rim shoe is used most commonly on all feet, with one rim higher than the other to provide added traction. A rounded toe provides easier breakover than a normal flat steel shoe. Hind shoes may have square toes.
Recently the natural balance shoe has gained popularity as owners are becoming more aware of good farriery principles and are trying to correct long-toe, low-heel problems. The natural balance shoe is available in steel or aluminum. Steel construction is preferred because of the added weight, which provides better traction than an aluminum shoe. The natural balance shoe has a rockered toe that eases breakover of the forelimb and is built with a wider web than a normal shoe, which benefits a sore-footed horse competing on hard surfaces.
Other Considerations
Exercise-induced pulmonary hemorrhage is common in barrel horses. The owner may complain that the horse has lost a step or has become slower. If a musculoskeletal reason for the performance change cannot be determined, a respiratory evaluation is indicated. Obvious bleeding from the nostrils rarely is seen, but endoscopic examination within 30 minutes of the barrel race often reveals tracheal hemorrhage. Presently no drug testing or rules prevent drug administration for competition. Most horses receive phenylbutazone or flunixin meglumine 4 to 6 hours before competition and furosemide (4 to 8 mL/horse).
 The European Western Performance Horse
The European Western Performance Horse
The Western performance horse sports have developed in Europe, especially in Germany and Italy, since the mid-1980s, with reining and cutting the most popular sports. Most horses are American Quarter Horses (QHs) and are traditionally broken at 18 months of age. The intense training needed to show 3-year-olds in the futurity competitions results in many horses not competing at 4 years of age because of behavioral or lameness problems. In an attempt to reduce injuries, there has been a move to shift bigger purses to 4-year-olds. In addition, the Fédération Équestre Internationale (FEI) has recently acknowledged reining as an official discipline, and only horses 6 years of age or older can compete under FEI rules. This is slowly changing the European approach to training of reining QHs.
There is zero tolerance of any drugs in competing horses, and antidoping testing takes place at most official shows in Europe for both professional and nonprofessional classes. This influences the treatment strategies that can be used for lameness. The strict medication rules also influence advice given concerning purchase of horses with preexisting lameness problems. Increasing attention is being paid to welfare, and strict rules govern which bits and harness are acceptable. Excessive use of spurs or whips may result in suspension of the rider. Common procedures like hair clipping around a horse’s nose and ears are not recommended when competing in Germany.
Lameness of the Foot
Common causes of foot pain include subsolar abscessation, solar bruising, osteoarthritis (OA) of the distal interphalangeal (DIP) joint, osteitis or fracture of a palmar process of the distal phalanx, and navicular syndrome. Oblique radiographic images of the palmar (plantar) processes of the distal phalanx and a palmaroproximal-palmarodistal oblique image of the navicular bone are particularly valuable.
Poor foot conformation is often an important predisposing factor for the development of foot pain. The foot is often upright with overgrown angles of the wall and heel, flattening of the sole at the toe, and an underdeveloped frog. Bar shoes exacerbate high heel conformation because they prevent the heel bulbs from sinking into the ground; the bar of the shoe concentrates loading and reaction forces from the ground in the bars and underlying structures inducing palmar foot pain.
In such horses trimming of the bars and wall at the heel increases the length of the loading plane, thus distributing ground reaction forces over a wider area. If the horse works on soft ground, reaction forces on the palmar aspect of the foot can be reduced by applying aluminum shoes with thinned and beveled heels; if the horse works on harder ground, a complete pad must be inserted between the shoe and the foot, and the shoe must be well concaved on the inner surface to prevent direct pressure to the sole through the pad itself. Shearing forces at the toe can be decreased by moving the breakover point back with a rolled-toe shoe.
Most of the top-level reining QHs are now shod with premade aluminum shoes beveled along the entire outer surface (Figure 120-7; Colleoni/Zaffi design, Farrier Product Distribution, Shelbyville, Kentucky, United States). These are available in either an open or bar type. The beveled outer surface helps the foot to breakover in most of the demanding figures (like spins or roll backs) that produce marked oblique and twisting forces on the distal aspect of the limb. A rocker toe shoe or squared toe is used less frequently because it can restrict the length of the stride.
Fig. 120-7 A typical shoe used in reining horses is made of aluminum and is beveled along the entire outer surface to reduce torsional forces associated with sudden turns and spins.
Treatment of reining horses with navicular syndrome during the show season is challenging because of the long detection times of most commonly used drugs either for local injection or for oral use. Horses with navicular syndrome often have long toe and underrun heel conformation. Treatment involves restoration of a more correct hoof-pastern axis and use of an egg bar or bar shoe to increase the loading area of the foot. A bar shoe also prevents the heel from sinking into the ground and reduces tension on the deep digital flexor tendon. Tendon lesions usually occur toward the insertion. Some are detectable ultrasonographically, but magnetic resonance imaging (MRI) is superior for diagnosis.
The hind feet are subject to enormous loading and twisting forces when horses perform quick stops or when spinning or doing a roll back. Reining horses are shod behind with sliding plates (sliders), which are usually kept long at the heels. A long-heeled shoe concentrates load at the angle of the heel and can create resistance to turning.
Lameness of the Hock
Lameness associated with tarsocrural joint is infrequent; however, many veterinarians still inject all three compartments of the hock routinely, thus increasing chances of articular reaction and infection.
OA of the distal hock joints is common. In 2-year-olds there is a high prevalence of partial collapse of the central and third tarsal bones with secondary OA. This is usually accompanied by a camped-under, sickle-hocked, or cow-hocked conformation of one or both hindlimbs.
I use a hock torsion test to try to differentiate pain arising from the centrodistal or tarsometatarsal joints. With the hock in a semiflexed position, I apply a medial to lateral rotational force on the longitudinal axis of proximal aspect of the third metatarsal bone. If the horse reacts quickly or tries to kick, this indicates centrodistal joint pain, whereas if the reaction is slower and the horse gradually lifts and abducts the limb, the test suggests tarsometatarsal joint pain. The hock torsion test is not the “Churchill test.” When performing the torsion test there must be neither direct compression on the medial aspect of the hock nor any compression of the suspensory ligament (SL).
Treatment of horses with OA of the distal hock joints is by intraarticular administration of corticosteroids and sodium hyaluronan. Care must be taken with withdrawal times for horses competing under FEI rules. Horses refractory to intraarticular medication are treated by surgical (drilling) or chemical (sodium monoiodoacetate or ethyl alcohol) arthrodesis. Arthrodesis is most effective in 2-year-olds.
Tenosynovitis of the long digital extensor tendon sheath on the dorsolateral aspect of the tarsus may result in a shortened cranial phase of the hindlimb stride. Ultrasonographic examination of the sheath may reveal tendon lesions and extensive tenosynovial adhesions (Figure 120-8). Treatment involves intrathecal injection of corticosteroids. If chronic, tenoscopic debridement of adhesions and partial retinacular release are indicated.
Superficial Digital Flexor Tendonitis
Acute superficial digital flexor tendonitis is a common cause of lameness in 2-year-old reining and cutting horses. Chronic injuries are seen in older horses that have not received proper treatment of acute lesions. Two groups of horses are predisposed to superficial digital flexor tendon (SDFT) injury: (1) young thin-legged Appaloosas, Paints, and QHs with conformation defects such as tied in below the knee, offset knees, and calf knees; and (2) well-built 3-year-old QHs intensely trained, especially working on spins in preparation for the futurity.
Lesions almost invariably affect the most lateral or medial border of the SDFT, usually extending for 3 to 5 cm in the middle or distal third of the metacarpal region, and are seen as diffuse areas of reduced echogenicity (Figure 120-9). Extreme uneven loading of the medial or lateral side of SDFT occurs while the horse is spinning or performing rapid turn backs. To reduce leverage and shearing forces acting on a hoof’s quarters in the breakover phase of the spin, top-level reining QHs are currently shod with aluminum shoes beveled along the entire outer surface (see Figure 120-7).
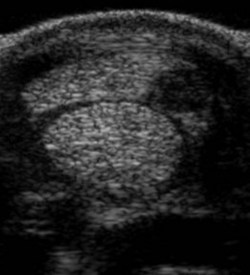
Fig. 120-9 Transverse ultrasonographic image of the distal metacarpal region of a 3-year-old Quarter Horse filly in full training. Medial is to the left. There is an acute anechogenic lesion of the lateral aspect of the superficial digital flexor tendon, which is swollen.
Treatment of horses with acute tendon lesions is aimed at reducing inflammation and edema with rest, cold packs, poultice, stall bandage, oral nonsteroidal antiinflammatory drugs followed by peritendonous injection of low doses of short-acting corticosteroids mixed with antiedema drugs. Intralesional, ultrasound-guided injection of platelet rich plasma (PRP) is performed 10 to 14 days after injury. For acute SDFT lesions in reining or cutting QHs, it is recommended that the horse should not return to full athletic function until at least 8 months after injury.
Lameness of the Stifle
Stifle pain is caused by subchondral bone cysts in the medial femoral condyle, traumatic OA, medial collateral ligament injury, osteochondrosis of the femoral trochleas, and fragmentation of the distal aspect of the patella in horses that underwent previous medial patellar desmotomy.
Digital radiography has enhanced the ability to detect subtle alteration in shape of the joint surface of the medial femoral condyle and early changes of subchondral bone opacity in early stages of the disease.
Intraarticular therapy should avoid use of the depot form of corticosteroids because it has been associated with rapid progression of OA and persistent lameness associated with the medial femorotibial joint in reining and cutting QHs. Surgical management of horses with medial femoral condyle cysts using arthroscopically guided injections of methylprednisolone acetate into the cyst lining or curettage results in a 50% to 60% chance for return of the horse to previous level of competition. Rest for 6 to 8 months is mandatory.
Suspensory Desmitis
Proximal suspensory desmitis (PSD) and desmitis of the branches of the SL are common. PSD affects young reining and cutting QHs in early or advanced training. Lameness is usually intermittent and can vary in intensity from grade 1 to 3 of 5, depending on workload; the horse is lamer with the affected limb on the outside of the circle. Lameness is abolished with analgesia of the lateral palmar nerve. Subtle ultrasonographic changes can be difficult to identify, and comparison with the contralateral limb is useful. Radiology is useful for identification of increased opacity in the proximal aspect of the third metacarpal/metatarsal bone.
Treatment of horses with PSD is based on rest, intralesional injection of PRP, shock wave therapy, radiotherapy/hyperthermia (INDIBA, Sant Cugat del Vallés, Barcelona, Spain). Corrective shoeing comprises an open aluminum shoe wide at the toe and thinned and beveled at the heels. A horse with an uncomplicated PSD lesion requires 90 days of convalescence. The presence of increased bone opacity at the origin of the SL is a poor prognostic indicator, with many horses remaining chronically lame.
Desmitis of a branch of the SL is frequently induced by medial-to-lateral foot imbalance; the wall is lower on the lateral side, and this induces more tensile stress on the lateral branch of the SL. Affected horses often have an offset knee or carpus valgus/fetlock varus and toe-in conformation.
Ultrasonographic examination often reveals hypoechogenic lesions of the most axial part of the branch. Therapy consists of periligamentous injection of corticosteroids and antiedema drugs and intraarticular treatment of the fetlock joint. Horses with chronic branch desmitis are treated with shock wave therapy, hyperthermia, controlled exercise, and repeated local application of working blisters. Shoeing correction involves the use of an open aluminum shoe with wider web on the side of the injured SL branch and balancing the foot.
Lameness of the Fetlock Joint
Osteochondrosis is frequent in front and hind fetlock joints. Most lesions in the dorsal aspect of the joint involve the sagittal ridge of the third metacarpal (McIII) or metatarsal (MtIII) bones, whereas lesions of the palmar (plantar) aspect originate from palmar (plantar) processes of the proximal phalanx.
OA of the fetlock joint is frequently accompanied by insertional desmitis of the SL branches or desmitis of the SL body at the level of its bifurcation. Both the fetlock joint and the SL must be treated for a successful outcome. Chronic synovitis may result in supracondylar lysis in 2-year-old QHs. Scintigraphy can be useful for identification of increased radiopharmaceutical uptake in the palmar aspect of the condyles of the third metacarpal bone, reflecting bone trauma in horses with no detectable radiological abnormality.
Western performance horses with early fetlock joint OA are managed using serial intraarticular injections with sodium hyaluronan, polysulfated glycosaminoglycans or interleukin-1 receptor antagonist protein (autologous conditioned serum). The prognosis is good. However, if there is thinning of articular cartilage and subchondral bone sclerosis or the presence of cystic lesions in the distal aspect of the condyles of the third metacarpal or metatarsal bones, the prognosis is poor, irrespective of medical or surgical treatment.
Lameness of the Carpus
Faulty conformation of the carpi is often present, especially offset knees. Lesions of the carpus include OA of the antebrachiocarpal and middle carpal joints, self-induced trauma of either the accessory carpal bone or the dorsal aspect of the carpus incurred during hard spinning, tenosynovitis of the carpal sheath, chip fractures of the radial or third carpal bones, increased radiopacity (sclerosis) of the radial facet of the third carpal bone, or sagittal fracture.
Sclerosis and sagittal fracture of the third carpal bone are the result of shearing forces caused by uneven loading of the medial aspect of the third carpal bone produced by repeated spinning and galloping in small circles.
Exostosis of the Second or Fourth Metacarpal/Metatarsal Bones (Splints)
Medial splints are common in 2-year-old reining and cutting QHs, frequently associated with a carpus valgus or offset knee conformation; lateral splints are less common but are occasionally seen in horses with an offset third metacarpal bone and base-narrow conformation.
Splints usually produce transient lameness, but horses with chronic lameness can be managed by freeze firing to reduce local pain and lameness. Shin splints—bony swelling on the proximal dorsomedial aspect of the McIII—are occasionally seen in very hard-stopping horses. The swelling is caused by periosteal and endosteal reaction to microfractures produced by repeated compression cycles of the dorsal cortex of the MtIII. Treatment is rest and handwalking for 30 to 45 days and freeze firing to reduce swelling and pain.
Curb
Curb is seen in 2-year-old QHs that have a sickle-hocked/cow-hocked conformation as a result of partial collapse of cuboidal hock bones. Ultrasonographic examination helps to determine which tendonous or ligamentous structure is involved and to decide the appropriate treatment.
Fracture of the Plantar Process of the Middle Phalanx
A fracture of the medial plantar process of the middle phalanx is the result of an avulsion caused by extreme pulling of the distal enthesis of the insertion of the SDFT during a stop. The tension in the medial branch of the SDFT may be the result of the wide stance of the hindlimbs that some horses adopt during the last phase of a sliding stop.
Shoeing should aim to correct horses that stop too wide by an inward rotation of the shoe or by applying medial heel extensions (trailers). Surgical management of horses with this middle phalangeal fracture by internal fixation with compression screws has had disappointing results. Prognosis is also poor following digital neurectomy and prolonged rest. Arthrodesis of the proximal interphalangeal joint might be a better choice.