11 Frequency-specific microcurrent in clinical practice
The history chapter describes how FSM was developed, the mechanisms chapter described how we think it has its effects, the treatment chapters describe how to use FSM to treat specific conditions and this chapter will describe how to integrate it into clinical thought and practice.
The pain management applications of FSM are easy to document and use but the implications and experience of using frequency patterns to change physical conditions in biological tissue are profound. The softening, warmth and relaxation response that occurs when the frequency is correct can be perceived to varying degrees by most practitioners. The ability to perceive the frequency response follows a bell-shaped curve in any given class of students at an FSM seminar. On one end of the curve are practitioners who are so sensitive that they become light-headed, euphoric, warm and wobbly. On the other end of the curve are those students who perceive nothing at all when different frequencies are used during the practicum sessions. And the bulk of the class has an experience that is someplace in between the two extremes.
The resonance response affects an arena of perception that most people do not normally attend to even though almost everyone probably has the capacity. It is as if we are born with auditory apparatus but live in a silent world until someone points out the sounds that can be heard. The same is true with the resonance response. We live in an environment filled with electromagnetic signals but most of them are not coherent and most are not noticed until the phenomenon is isolated and presented in an educational setting.
Using frequency-specific microcurrent in clinical practice creates a profound change in outcomes and expectations and ultimately requires a change in practice mechanics and patient flow to produce optimal results.
The diagnosis matters
Changes in patient history and physical examination
The change begins with the patient history and physical examination. In some medical settings the history may be simple and even perfunctory because the treatment options for a particular patient will be identical no matter how the patient arrived at his symptoms. FSM treatments are very specific and so the diagnosis must be equally specific. For example if the patient presents with “leg pain” and pain medication, such as non-steroidal anti-inflammatory medications or opiates are the only available treatment option then the mechanism of injury and the exact nature of the pain generators are not material. Pain medication is the only treatment option and correcting the source of the pain, while desirable, is not a consideration. But if the patient presents to an FSM practitioner with “leg pain” the diagnosis is the primary consideration because the treatment must be specific to the condition if it is to be successful.
What tissue is it? What is wrong with it?
The FSM practitioner asks, “What tissue is causing the pain? And what pathology in this tissue is making it a pain generator?”
“Leg pain” may come from dermatomal nerves originating in the low back and the history will include some mechanism of injury that includes forward flexion and perhaps rotation that would injure a disc. Flexion, including driving and sitting in a chair with slumped posture, will make the pain worse; extension may make the pain better. The pain will follow a dermatomal nerve pattern and will travel down the leg to the big toe or heel. The sensory examination will show hyperesthesia or numbness in dermatomal nerves. A “straight leg raise” may increase the pain in the leg or foot. The FSM treatment will be for the nerve and the disc.
Moderate to severe “leg pain” in a nerve root distribution may begin after some insignificant activity. The sensory exam may show nerve hypersensitivity but reflexes are normal, flexion doesn't increase the pain and the mechanism of injury (slight) does not match the severity of the pain (moderate to severe). The FSM treatment will be for shingles in the L2, L3, L4 or L5 dermatome.
“Leg pain” may also come from low back facet joints. The posterior joints create “leg pain” that usually goes down the back or front of the thigh to the knee and follows a scleratomal or joint referral pattern. The pain will be worse with sitting and with low back extension and may be better while lying supine with the knees up and the back flat. The pain will increase during the physical examination when the facet joints are compressed as the patient lies prone. The FSM treatment must address the facet joints and the psoas and lumbar paraspinal muscles if it is to be successful.
“Leg pain” may come solely from myofascial trigger points in the lumbar spine, gluteals or the leg muscles. It may have started after some overuse injury, from chronic postural strain, or trauma or a fall. The history may include some metabolic cause of myofascial trigger points such as hypothyroidism, significant emotional stressors or after use of lipid-lowering drugs. Statins have a considerable risk of causing muscle pain even after the patient has been taking them for some months and may be overlooked as a cause of pain because of the time lapse between initial medication use and the onset of symptoms. The whole class of lipid-lowering medication carries this risk which is minimized with the prescription because of the perceived benefit. The history points the way to this diagnosis and the FSM treatment must address the cause of trigger points in muscles in order to successfully resolve the pain.
“Leg pain” may also be due to referred pain from the sacroiliac, hip or knee joints. The history and physical examination will be specific and positive for dysfunction in those joints. FSM treatment and supportive therapies will be effective if specific to the local joint pathology.
The myofascial protocol calls for treating the nerve, then the muscle and then the spinal discs, facets and finally the peripheral joints. This protocol provides the context for treating all of the causations of “leg pain” mentioned above except shingles. The practitioner experienced in physical medicine who enjoys differential diagnosis may produce relief more quickly but anyone following the protocol will be able to provide a positive outcome in most patients treated.
This change in detail in the history, physical examination and diagnosis is achieved over time and assisted by the patient's response to treatment. Experience has shown that when the treatment is not effective either the patient is dehydrated or the diagnosis is incorrect. This positive response to treatment becomes apparent within a single 30-minute treatment session and the rapid feedback shortens the learning curve once the practitioner learns to trust the response.
Equipment
Applying frequency-specific microcurrent to a patient requires a two-channel microcurrent instrument that produces a ramped square wave, pulsed, direct current output that can be set to deliver between 20 and 600μamps. This is current in millionths of an amp and cannot be provided by a TENS unit even though most microcurrent devices are approved in the USA and other countries in the category of TENS. The machine must be able to run the current in either alternating or polarized positive mode. New injuries require a gentle waveslope and very chronic conditions require a sharp waveslope, so a variable waveslope is ideal. The two channels must be independent and capable of providing a different three-digit specific frequency accurately on each channel.
All of the research and experience in frequency-specific microcurrent has been performed with an analog two-channel microcurrent unit, the Precision Micro, manufactured by Precision Microcurrent, Inc. (Newberg, Oregon) and sold by Precision Distributing, Inc. (Vancouver, Washington). But there are numerous units available, digital or analog, which supply the same electronic parameters which should be capable of reproducing the results described in this text.

Figure 11.1 • The Precision Micro (Precision Microcurrent Inc., Newberg, OR, USA) shown here with leads attached to graphite gloves and cotton tipped probes attached to the front panel din plug, is an analog two-channel microcurrent device that produces frequencies accurate to three digits using a variable ramped square wave pulse train on each channel. The current varies between 10 and 600μamps and the frequencies and current can be set independently on each channel. The battery operated device delivers pulsed alternating or polarized positive or polarized negative DC current. Company standards require that the frequencies be accurate to 0.5 Hz. FSM research has been done using this unit but any microcurrent device may be used that provides the same current, polarization, wave shape and frequency parameters.
The reader is advised to evaluate units based on the required electronic parameters, availability, service policies and price.
Units such as the Precision Micro require someone to change the frequencies manually and are perfect for attended therapy in clinics specializing in physical medicine, pain management or physical therapy. But individualized hands-on treatment is not ideal for a busy practice setting in which similar conditions are treated in numerous patients and unattended treatments are preferred. The only units programmed with the frequency protocols described in this text are supplied by Precision Distributing. The HomeCare, AutoCarePlus, CustomCare and SportsCare are preprogrammed with some of the protocols described in this text but are not easily modified for treatments that must be customized during the session. The AutoCarePlus and SportsCare can hold on one frequency combination, skip a frequency, or go back to the last frequency used. These units are only sold to practitioners who have taken the FSM course because they include protocols for visceral and neurological conditions not covered in this text.

Figure 11.2 • The AutoCarePlus runs 83 frequency protocols by sequencing automatically through a list of programmed frequencies for each protocol. It has a manual mode that allows the unit to hold on a frequency combination, skip forward to the next frequency combination, and go back to the last frequency combination in the sequence or to customize but not store a frequency choice. This unit is regulated as a TENS device and cannot make any claims beyond that which could be made for a TENS device. The screen shows only initials that indicate the frequency sequences being delivered. This unit is only sold to practitioners who have completed the FSM Core seminar.
Precision Distributing has made available a small automated unit preprogrammed with only the protocols described in this text. The FSM PainCare will run these protocols for the average times described in the text and will have a manual mode that allows for some customization. It can be purchased by any practitioner whose practice scope or license includes the ability to purchase, use or prescribe electrical stimulation devices.
Conduction choices
There are a variety of conductive gloves for various electrical stimulation uses available through different providers. Silver-yarn knit gloves are stretchy and fit a wide range of hand sizes comfortably. They are difficult to clean in between patients but may be used with a PVC (vinyl, non-latex) glove over them for sanitary reasons because the PVC gloves conduct current when they are wet or stretched. The silver on the nylon mesh oxidizes when exposed to chlorine bleach or iodine cleansers and becomes non-conductive. The silver-yarn knit gloves are generally more expensive than the graphite gloves and can be found on the internet from various providers.
Graphite conductive gloves are sold by Precision Distributing. The graphite gloves cannot be left in the sun or exposed to chlorine bleach, iodine-based cleansers or UV light. They need to be kept free of oil in order to maintain conductivity and must be washed only with hot water and grain or ethyl alcohol such as vodka. They are considered a temporary electrode and are not warranted by the manufacturer because they are somewhat fragile and subject to damage by misuse. With good care they usually last one to two years but exposure to oil or bar soap can make them irreversibly non-conductive in minutes.
The graphite gloves have certain advantages that may make the extra care worthwhile. They are flexible and easy to wear and use for manual therapy, and appear to create what is probably a magnetic field associated with the circular electron path around the glove that has a subtle but distinct effect. For some reason, which possibly exists only in the author's imagination, the graphite gloves seem to provide an additional effect not found with adhesive electrode pads. It is left to the reader to decide based on personal experience. The graphite gloves must be wet with plain tap water to conduct current comfortably. The cart holding the machine should be equipped with a small water dish or spray bottle for moistening the gloves. If the gloves become dry the current will prickle and sting so it is best to moisten them before the patient has this unpleasant experience. The contact becomes “skittery” just before it begins to sting but it is best to moisten the gloves each time a frequency is changed.

Figure 11.5 • Latex or nitrile gloves are worn under the graphite glove to insulate the practitioner from the current flow. Two positive leads, one from channel A and one from channel B, are connected to the pin jacks cemented onto the cuff of one graphite conductive glove. Two negative leads, one from channel A and one from channel B, are connected to the pin jacks on the back of the other glove. The frequencies and current from both channels “cross” in the area between the gloves forming the required interferential field.

Figure 11.6 • The treatment room cart is set up with the machine, the latex or nitrile insulating gloves, a small dish of water that can be changed after each patient and a small spray bottle filled with water set up on the top shelf. Dip the fingers of the graphite glove in the water and then rub the hands together to distribute the water evenly over the glove surface.
The practitioner can also use “alligator clips” to attach the leads to a conductive fabric such as small hand towels, wash cloths, or even single-use paper towels wet with warm water. The graphite gloves can be wrapped inside a piece of wet fabric allowing the same option. When attached to the machine by alligator clips, the wet fabric becomes a long flexible conductive surface or electrode and can wrap around the neck or low back, lay along the length of the spine, wrap around a knee, ankle, elbow or wrist, hand or foot. Any sort of long flexible fabric or graphite electrode will be useful for treating regional pain or dermatomal nerve pain.
Alligator clips can be purchased inexpensively at any commercial electronic supply store. A high quality clip with minimal resistance is recommended to reduce current loss into the conductor. The machines are constant current generators and will increase the voltage as needed to overcome resistance and ensure that the current flowing to the patient is equivalent to what the device has been set to deliver. If the resistance in the conductive medium is too high the machine may reach its maximum voltage output before the desired current can be achieved. If this happens, and the resistance is too high, the machine will show less than 100% conductance on the current flow indicators. The practitioner can decrease the current until 100% of the current set can be conducted or change the conducting medium and re-hydrate the patient to improve conductivity.
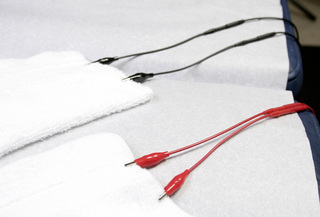
Figure 11.7 • The two positive leads from channel A and channel B are connected to two red alligator clips which are then attached to a moistened fabric contact such as a hand towel or face cloth to create a long flexible electrode. The two negative leads from channel A and channel B are connected to the two black alligator clips which are then attached to another moistened fabric or graphite contact to form a long flexible electrode. The two contacts should be positioned so the current and frequencies cross in the body area being treated and so that they do not touch each other.
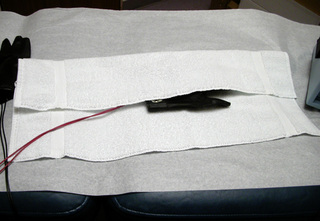
Figure 11.8 • The hand towel or any similar convenient fabric contact is first thoroughly wet with warm water, then wrung to eliminate excess moisture and folded lengthwise into thirds with the graphite glove in the middle. This arrangement converts the entire towel into one long electrode.
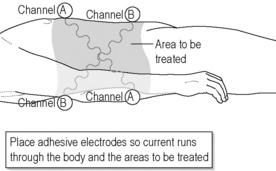
Adhesive electrode pads can be used to conduct the current and are available in a wide range of sizes and shapes. Sanitary considerations require that each patient have their own set of gel adhesive electrodes and that these electrodes be labeled and stored in the patient chart or in some central place in the clinic. Graphite electrodes adhered and moistened with conductive gel for each application are a little messier but less expensive to use because they can be used on indefinite numbers of patients. Some patients are sensitive to adhesives and the chemicals in the gels and this consideration may limit usefulness of this method for those patients. The adhesive pads must be arranged so that the current and frequencies from the two channels cross and intersect in three dimensions through the area being treated.
Regardless of the medium used to apply the current the practitioner needs to keep in mind the need to create an interferential field in the area to be treated where the current and frequencies from the two channels cross. The positive leads from both channels need to be positioned so that the current flows through the area being treated in three dimensions to the negative leads from both channels. The photographs provide illustration of the principle.
Setting up the treatment room
The ideal treatment room arrangement provides a variable height table that allows the practitioner to work with optimal body biomechanics during the treatment and allows the patient to be positioned comfortably no matter what their pain complaint may be. If patients are going to be treated with unattended current and protocols from automated units they may be treated while lying on tables or seated in reclining chairs as long as their position is supported and comfortable.
The equipment should be placed on the top shelf of a sturdy metal or plastic cart or trolley that has room for the machine plus a water spray bottle or small plastic dish for the water needed to keep the graphite gloves moist, and a box of the latex or nitrile gloves required to isolate the current from the practitioner. The frequency summary sheet may be laminated so it is waterproof and kept under the machine for easy access.
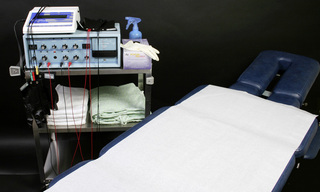
Figure 11.10 • The treatment table in this photograph (Hill Tables) has adjustable supports and cushioning for prone or supine patient positioning and is adjustable in height for practitioner comfort. Any table can be used that suits the practitioner's preference and allows for proper practitioner body mechanics during treatment. The cart is shown with two machines, the Precision Micro manual unit and an AutoCarePlus automated unit, the insulating gloves, the water spray bottle on the top shelf and gowns and spare dry towels on the second shelf. The practitioner sits on an adjustable height rolling stool for easy mobility and comfort.
If a flexible wet contact is going to be used for conducting current then the treatment room or some space nearby should be set up to make them available and convenient. A supply of dry hand towels or rolls or stacks of dry paper towels can be kept on the cart or on a shelf in the treatment room or nearby supply area as long as there is a warm water faucet and basin nearby in which to moisten them. Some practitioners keep a supply of hand towels wet and warm for the day's patients in an electric warmer like a “crock-pot”. Adjust the water temperature so there is no risk of scalding to either patients or employees. Using a microwave to warm a wet towel produces isolated hot spots which can burn a patient and is not recommended.
The bottom shelf or shelves of the cart can be used to store patient gowns, a supply of towels, a small soft blanket to use as a drape and bolsters or pillows used for patient positioning and comfort. The options for equipment and room set-up are virtually unlimited and depend on practitioner training and preference and the types of patients being treated. The details are left to the reader to explore and experience.
If the wet contacts are not disposable then some accommodation must be made for laundry management. Some clinics have a washer and dryer on site and find it most economical to do the laundry daily in-house. If a laundry service is used the added cost can be balanced against the convenience of having clean towels supplied once or twice a week. If disposable paper contacts are used then some consideration should be given to how to recycle the paper.
Patient hydration
In order for FSM to be effective the patient must be hydrated. For most patients this means drinking 1 to 2 quarts of water in the 3 to 4 hours prior to treatment. The boxed alert below appears in every treatment chapter and some version of it should be posted

Figure 11.11 • Hydration is so important to successful treatment that one creative practitioner, Vanessa Cayle, PT created this hydration poster and placed it on the waiting room and treatment room walls
(© Vanessa Cayle, reproduced with kind permission).
on the wall in the waiting room of every FSM practitioner. Hydrated patients require that the clinic have easy access to toilet facilities.
• The patient must be hydrated to benefit from microcurrent treatment.
• Hydrated means 1 to 2 quarts of water consumed in the 2 to 4 hours preceding treatment.
• Athletes and patients with more muscle mass seem to need more water than the average patient.
• The elderly tend to be chronically dehydrated and may need to hydrate for several days prior to treatment in addition to the water consumed on the day of treatment.
• DO NOT accept the statement, “I drink lots of water”.
• ASK “How much water, and in what form, did you drink today before you came in?”.
• Coffee, caffeinated tea, carbonated cola beverages do not count as water.
Patient flow
For some practitioners the 20–60-minute treatment time required for FSM therapy is compatible with appointment time slots already in use and, for some, scheduling will need to be adjusted to accommodate the longer appointments. If the practitioner cannot afford to spend 20–30 minutes of individual time with a patient, a clinical assistant can be trained to administer FSM treatment for the various conditions covered in this text. If a clinical assistant performs the treatment in one treatment room, the clinician is free to start a patient interview or close a patient appointment in additional rooms in 5–10-minute slots.
Once a patient has been assessed, the automated units allow unattended treatment for conditions that don't require manual therapy. The patient can be treated with unattended protocol for 30 minutes and then seen for manual therapy in the last 15 minutes by either the practitioner or a skilled assistant. If the space is available and the patient demand justifies it, the practitioner can expand the number of rooms and the number of clinical assistants almost indefinitely. Eight rooms and six clinical assistants seem to be the maximum workable in larger pain management or physical medicine practices and four rooms and two or three assistants is more easily managed.
The practitioner may open the appointment by taking the history, checking the pain diagram and visual analog pain score and asking about changes since the last treatment, and then conducting a quick physical examination or assessment. If a clinical assistant is to perform the FSM treatment, instructions would be given as to what protocols to run and in what order at this point, the practitioner would leave them to their work and move on to the next room. The patient in the next room is either ready for the practitioner to open the appointment or has already been treated by the assistant and is ready for the closing evaluation.
The patient should give a pain score report at the beginning and at the end of every treatment. It only takes a minute and it is invaluable for patient management and data collection to demonstrate efficacy of treatment for research, or for the patient or for a third party, such as an insurance company, that is paying for treatment. The patient should fill out a questionnaire that documents function instead of pain at regular intervals. If the pain remains the same but function improves that is a positive response to treatment and should be documented.
If the patient reports at the beginning of an appointment that the treatment isn't helping, a quick check of the post-treatment pain scores will show that the patient has been pain free at the end of the last four treatments and has returned with the pain score reduced from the previous incoming pain score at each of the last three treatments. So the pain returns at some point between treatments but to a lesser degree than was present before. The data helps to reassure the patient and helps the clinician to ask questions to discover the source of the patient's frustration.
In a different instance, the pain score data may make it clear that the patient is no longer making progress. The patient comes in at a 5/10 VAS and leaves at a 2/10 VAS with an identical pain diagram at each of the last six once-a-week appointments.
The data gives a starting point for the conversation about:
1. Treatment frequency: How soon does the pain return and would twice a week treatments instead of once a week treatments for a few weeks help make the response more lasting? What do time and finances allow?
2. Treatment goals: What does the patient want from treatment and is the pattern acceptable? After 12 years in chronic pain the patient may be thrilled with 4 days of a level 3–4/10 pain between treatments. Or perhaps the patient envisions a pain free life and is frustrated with the pattern of improvement and return. Treatment goals should be a collaborative decision making process. The patient is allowed to vote. Some fibromyalgia patients cannot envision a pain free life and devise a treatment schedule that leaves them in just enough pain so that they have what they need to navigate their emotional and social landscape.
3. Treatment program: Can the patient do the prescribed exercises or home treatments consistently or does the prescribed home program need to be modified? Are they prone to overdo prescribed home programs or do they tend to forget and do half of what is prescribed? The only way to find out is to have a judgment free conversation and then modify the prescription to suit the patient.
4. Treatment expectations: Is the present situation acceptable to the patient and what expectations do they have for treatment at this point? This progress report is much more easily done with data collected at the beginning and end of each treatment session. If the forms have a 10cm visual analog scale and a pain diagram at the top of the page and a place at the bottom of the page to record a verbal pain score, the data collection is quick and effortless and well worth adjusting the patient flow to acquire it.
Patient flow and scheduling will depend on the number of rooms available, the number of patients who need to be treated in an hour to meet clinic revenue needs and the complexity of patients being treated. This in turn will depend on the number of hours the clinician wants to work, the clinic reputation and the demographics of the clinic and the clientele. Patients with fibromyalgia associated with spine trauma occupy a treatment room and an automated unit for 60–90 minutes but only require supervision for 10–20 minutes of that time or perhaps manual therapy for specific regional complaints for up to 20 minutes. If treatment rooms are very
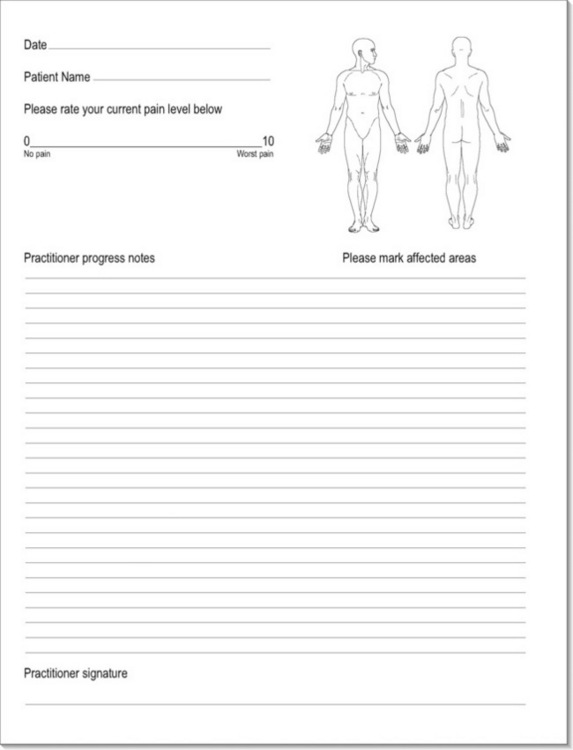
Figure 11.12 • This chart note sheet is an example of a simple form that can be used to document pain scores and a pain diagram at the beginning of each treatment. The pain diagram can help distinguish between different pain generators by providing pattern recognition for the practitioner before the history begins. This sample has blank lines for notes but any convenient format can be used depending on the practitioner's profession. If electronic chart notes are being used the patient should be given a sheet with a 10cm line and a body diagram to fill out at each visit.
limited then the practitioner may not wish to cultivate a clientele of fibromyalgia patients or may need to restrict their numbers. These patients can progress to treatment at home with a personal sized automated unit and shortened in-office appointments for regional pain treatment or metabolic rehabilitation within weeks, making them much more easily managed and very satisfying to treat.
Eventually the practitioner who decides to use FSM will personalize it and create the optimal combination of devices and equipment, frequency protocol references, adjunctive therapies, referral sources, patient flow and manual skills to make FSM useful and satisfying adjunct to practice. This text is only the beginning and the practitioner is encouraged to enjoy the personalization process.
Billing and charting
Every practitioner in every health care profession is required to keep chart notes that document the treatment delivered to patients. The chart notes provide a record of services performed during the therapeutic encounter that supports billing for the treatment provided. If the practitioner has a cash practice or works in an environment that does not include insurance billing, be grateful and skip to the next paragraph. To provide support for billing, the chart needs to document the complexity of the condition and the time spent with the patient. If the condition is complex and requires a longer visit, it is reimbursed at a higher rate but the complexity has to be reflected in the number or severity of diagnosis or documentation of the topics discussed and the amount of time spent in patient contact. Each profession is reimbursed at a different rate for the cognitive evaluation portion of the treatment. The chart needs to document what modalities were used and for how long. FSM treatments are billed as “attended electrical stimulation” in 15-minute time units for insurance reimbursement as if it were a TENS device because the device is classified as a TENS device by governmental regulatory agencies such as the FDA in the US or the TGA in Australia. It can be combined with manual therapy, trigger point therapy or proprioceptive neuro facilitation (PNF) and each of those modalities is billed as a separate service. Detailed advice on billing and coding is beyond the scope of this text and the practitioner should consult a professional in this area for more complete information.
Even if the practitioner does not bill insurance the chart notes serve as something akin to a laboratory notebook for the clinician's reference. If the clinician wants to know how the patient responded, the record of the treatment and the response should be in the chart notes in as much detail as possible so that a positive response can be reproduced and a negative response can be avoided.
For an FSM practitioner this means documenting the patient's condition, the frequency protocols used and the response. It may be a fine point, but for complete accuracy, the practitioner should simply list the frequencies used and not interpret the frequency action. When 13 / 396, 142 are used to “remove scar tissue between the nerve and fascia”, it may decrease pain with motion and increase range of motion but there is no way to say with complete certainty that the frequency combination is actually dissolving scar tissue between the nerve and fascia. It acts as if it is dissolving scar tissue but there is no way to prove that claim. It is far more accurate to report 20 degrees of flexion with pain before treatment, use of 13 / 396, 142 and then 40 degrees of pain free flexion after treatment with that frequency combination.
In modern practice the chart note is also a medical-legal document in the event of any unfortunate treatment outcome that might lead to a malpractice lawsuit. Risk management advice dispensed by malpractice insurance companies suggests that every patient encounter be recorded with the thought in mind that the practitioner may end up in court or before a review board. In addition to being good advice in general, this recommendation is another reason to avoid making claims in the chart notes about the effect of a given frequency. If 40 / 116, 480, 783, 157 are used on a red and swollen joint, it is easier to defend and more accurate to report that those frequencies reduced redness and swelling and increased range of motion by a certain amount than to say that the frequency reduced inflammation in the immune system, joint capsule, periosteum and cartilage. If asked in a legal setting what the frequency was used for the practitioner is not in the position of making an unsupportable claim. “The treatment reduced redness and swelling” is an observation by a trained and licensed professional. “The treatment reduced inflammation” is an entirely different statement which cannot be supported.
If the patient has any side effects from treatment such as a detox reaction, it is important to make note of the reaction along with the instructions given to prevent it or manage it. Any conversation or interaction regarding positive or negative effects of treatment should be recorded in as much detail as space and time allow.
Marketing
In general, the use of FSM to treat pain patients increases patient volume and clinic revenue even though it increases overheads by requiring the purchase of machines and consumables like adhesive electrode pads and towels. Detailed marketing advice is beyond the scope of this text because marketing is constrained by the individual practitioner's finances, personality and preferences and, in some cases, by statute and licensing board regulations.
Experience suggests that the ideal marketing tool is a satisfied pain free patient who tells everyone, including their friends, family, referring physician and fellow pain patients, about their positive outcome. Sending out preprinted thank you notes to referring physicians and a preprinted welcome card to new patients and having an incentive program for patients who refer new patients are simple inexpensive touches that can improve patient relations and increase patient flow.
The learning curve
Every new skill acquired has a certain learning curve. The practitioner usually starts at a place of “unconscious competence”, completely comfortable with a familiar skill set that produces desired outcomes and unaware of any effort required to use it. When any new skill is learned this equilibrium is upset.
The practitioner moves to a period of “conscious incompetence” in which he is not very skilled at the new technique and is aware of the lack of proficiency but is also enthusiastic enough about the rewards and the promise of improvement to keep practicing. This is the most uncomfortable part of learning any new skill and with luck, persistence, practice, good learning tools and rapid feedback it is brief. This portion of the FSM learning curve lasts about 3 months depending on how many patients are treated per day. The average practitioner needs to treat approximately 10–20 patients with similar complaints such as shoulder or low back pain or nerve pain to move through to the next phase.
The summary sheet that comes with this text provides the frequencies and summary protocols at a glance. This eliminates the need to memorize the frequencies and helps shorten the time to competence. It can be copied and laminated for durability and easy access. Learning the frequencies and the protocols can proceed from practice and repetition and may be almost effortless for some practitioners and may be a struggle for others. Some motivated and enthusiastic practitioners will memorize the numbers and protocols very quickly because they can and because they enjoy the process. Both approaches have advantages and which is chosen depends solely on practitioner preference. The photographs in the text and in the summary boxes may shorten the time required to become comfortable with the mechanics of placing electrodes on the patient for treating different conditions in different parts of the body but it is still a matter of trial and error and takes time, repetition and may involve some problem solving. The learning curve and acceptable solutions will be different for every practitioner and every patient.
If the practitioner survives the “conscious incompetence” phase and has the personality, intellect and tools to make it to the next phase, the rewards of “conscious competence” make the transition worthwhile. “Conscious competence” produces better outcomes with less effort because the practitioner knows what to do to produce an effective treatment even though it takes some conscious thought. In the case of acquiring skill in using FSM, making the correct diagnosis becomes easier; patient set-up requires little if any thought, and choice of the appropriate or optimal treatment protocol becomes more easily apparent. This phase is more comfortable and may last for months or years depending on the practitioner and the conditions being treated.
The conscious competence phase may be prolonged because the patients being referred for treatment tend to become more challenging over time. Every difficult patient who has been successfully treated seems to know six people just like themselves who also need care. Eventually the case load that seemed difficult at first looks easy by comparison and the practitioner develops improved diagnostic and treatment skills by continually treating more and more complex cases. This growth in skill set requires conscious effort and prolongs the conscious competence phase.
The practitioner moves almost imperceptibly into the next and final phase returning to “unconscious competence” having fully integrated the new skill set and using it to produce successful outcomes without thinking about the process. The average FSM practitioner requires perhaps a year or two to achieve this level of comfort.
Rapid feedback accelerates the learning curve
The rapid changes in tissue texture and pain provide immediate feedback during treatment and shorten the learning curve dramatically. If the practitioner has to wait hours, days or weeks to determine whether a specific application of the new skill has been successful, it takes longer to learn because the feedback that distinguishes between correct and incorrect choice of action is so delayed. The rapid feedback available with use of FSM shortens the learning curve once the practitioner learns to notice it and then learns to believe what can be felt. The occasional patient who experiences or reports positive response to treatment 24 hours after the treatment instead of noticing it immediately is the rare but disconcerting exception to this rule.
At first, when there are so many new things to notice and to attend to – doing a more detailed history and physical examination, operating the machine, positioning and setting up the patient for treatment, instructing an assistant, reading the frequency list, integrating the examination findings with the patient's palpation, deciding and then wondering about the diagnosis, to mention a few – the clinician has little time or attention to devote to noticing the tissue response. But, as some of these issues become routine there is more time and attention available to notice the response to treatment. There will be times when the response is so immediate and profound as to grab the attention but it may not be obvious in every case at first.
The profound change in state that occurs when the proper frequencies are used has been described as “disorienting” because it is unlike anything experienced with any other form of treatment in common use. One practitioner described his difficulty at the end of the first day of class with the statement, “Everything I thought I knew about muscles, or even matter, and how it works has just changed. It is disorienting.” It is almost impossible to describe the change in words because it is such a palpatory phenomenon and is akin to describing the sunrise to a blind person. The tissue simply rapidly profoundly changes state when it responds to the correct frequency.
Muscle tissue that is hard, tough, scarred, firm, rigid, “gnarly” or stiff begins to soften and within minutes feels “smooshy”, like pudding in a plastic sack. The areas of tissue that have not responded to that frequency or set of frequencies stands out amidst the smooshy tissue and can then be addressed with additional frequency choices. The residual firm tissue will respond and assume the pudding-like consistency when the appropriate frequency combination is applied and so on until the area being treated is comfortable and uniformly soft. It has to be experienced to be believed. Skeptics are forgiven in advance because there really is no reason to believe that this phenomenon is possible until it is experienced.
For the author there was one learning curve for noticing this softening as a palpatory change and a separate learning curve for believing that it had happened. There is a third and final learning curve in which this response is taken for granted and its presence or absence is used to determine the choice of treatment. Patience is recommended during this part of the FSM learning process as each phase may require weeks or months of experience. Thousands of patient treatments were required before the author fully appreciated this phenomenon.
Managing patients
FSM is one of few treatment modalities with a problem caused by the speed of positive outcomes. When a patient with chronic nerve pain or fibromyalgia from spine trauma has been in pain for more than 10 years and becomes virtually pain free in 90 minutes it is almost disorienting. There is an emotionally challenging dissonance between the pain the brain expects and the comfort the patient is currently experiencing.
In a very real sense, the patients literally do not know who they are if they are not in pain. Pain has limited and defined every aspect of life and function for years and now it is gone. Imagine and attempt to appreciate the challenge that presents itself to the patient. They have to change or reduce medication levels, rediscover their boundaries, learn what they can and cannot do now on almost a daily basis through rehabilitation until the recovery process is complete. They have to dare to be willing to hope that the pain relief and physical recovery will persist. They have to dare to hope again when the inevitable temporary setback occurs. They have to be willing to believe that recovery is possible. They have to be patient when recovery stalls and it becomes apparent that it will never be complete. The recovery process takes time but occurs faster with FSM than with almost any other treatment modality and the practitioner needs to learn how to support the patients emotionally and physiologically during this process. The learning curve is different for every practitioner and his or her patients in this situation. There is no way to give specific guidance on exactly what to do or how to do it during the recovery phase and it is only possible to advise the practitioner to prepare for its inevitable appearance.
When a regional pain patient with neck or shoulder pain, for example, achieves increased range of motion and reduction of pain in two to three treatments the challenge is less profound but still present. The compensations created by the body in response to the dysfunctional tissue are no longer necessary or appropriate. The patient will notice the compensations once the original problem is gone and may think that they are a new problem and become concerned.
Experience will make these “compensation events” predictable and the wise practitioner will learn to warn patients about this phenomenon before it happens. “We just increased the range of motion in your neck by 50% in 30 minutes and there is going to be some reaction someplace in your body to this change. I cannot tell you what the reaction will be or where it will be because it is different for everyone but I can guarantee that something somewhere will be different. It may be as simple as the fact that your upper back and shoulders will feel tighter in the areas we didn't treat. The neck moves farther and more easily and the shoulders and upper back are being asked to move in ways not possible for years so they will feel tighter. This is not a new problem; it is a response to an improvement and is very good news. Or, the response may be something as strange as low back pain or leg cramps. Whatever it is we will be able to treat it when it comes up.”
Patients may experience an increase in thirst during treatment or shortly after treatment. Increasing current flow and ATP energy production requires water molecules to form a contiguous semiconductor layer all throughout the body in the fascia. It could be that the brain senses this need and increases the desire for water. Whatever the cause, it is not uncommon for patients to report increased thirst during and after treatment and they should be encouraged most strongly to increase water intake.
Managing expectations and limitations
The last area of patient management is peculiar to the rapid responses seen with FSM treatment – management of expectations on the part of both the patient and the practitioner. Once the patient has experienced the effects of increased range of motion and decreased pain, stabilized ligaments, or elimination of nerve pain, improved cognitive function and emotional stability it is hard to imagine that anything is impossible.
It is difficult to describe the excitement and pleasure that accompany each successful treatment. Using FSM is fun and even veterans of 18 years in practice find renewed joy, delight and stimulation in producing the rapid results in routine patients. The joy becomes addictive and each success creates the expectation that the next success will be as easily achieved.
Eventually the practitioner will encounter a new patient, or a new condition in a patient successfully treated for some other condition in which the desired relief simply cannot be achieved. When this occurs during the early years of experience with FSM it is not as surprising as when it happens after several years of experience creating changes formerly thought to be impossible. After a few years using FSM the formerly impossible result becomes the expected outcome. The challenge is not the unsuccessful treatments; the challenge lies in the unrealistic expectations. No treatment is ever 100% successful.

Be realistic, expect a miracle
But be patient, the impossible takes slightly longer than the difficult
A phone call from a practitioner who was treating a patient with moderate Parkinson's disease brought this situation into stark relief. The practitioner described treating a patient with the characteristically rigid posture, difficulty walking, loss of fluid motion and tremor seen with moderate Parkinson's disease. She described her success in reversing these symptoms in a single 60-minute treatment allowing the patient to walk normally and move fluidly without tremor or rigidity. She asked in frustration what she was doing “wrong” because the improvements would only last 3 days. She lost sight of the fact that the improvements themselves, however temporary, were miraculous and it was the expectation of a permanent resolution that was unrealistic. She was not ever able to produce a permanent resolution in this patient but by managing her expectations she and the patient were both content with once a week treatments that restored function temporarily and improved his quality of life.
The frequencies cannot put tissue back that is not there. They can restore function, especially in neural tissue, reduce inflammation, dissolve scar tissue and restore secretions by providing a frequency pattern that apparently changes cellular function. But frequencies cannot put tissue back that is not there. There are some degrees of scarring that so damage the tissue it cannot be restored to its former state. The interactions between damaged and compensating tissues are so complex and so restricted that FSM seems to have little lasting impact on them. These failures are frustrating and humbling and often leave the practitioner wondering if there isn't some treatment protocol that could be devised if enough was known.
There are some emotional predispositions and psychological responses to early childhood trauma or pain that are so severe that nothing FSM can do will restore emotional peace and normal central pain processing. The dedicated curious practitioner can acquire additional skills, knowledge, tools or referral options in nutritional support, evaluation and biochemical manipulation of neurotransmitter levels, hypnosis, and different types of therapies helpful in modulating emotional responses. Navigating this process requires more thought and inventiveness than knowing how to spell and dose the newest anti-depressant medication. FSM is likely to be necessary but not sufficient to achieve success in these complicated patients. And sometimes nothing seems to help. The persistent practitioner with a hopeful or desperate patient may eventually find a solution if they search long enough.
These less than optimal responses keep the clinician humble. No matter how successful FSM has been in treating similar cases the clinician is advised to avoid making promises or being or appearing overconfident. As the practitioner's level of experience increases so usually does the degree of difficulty of patients being referred for treatment.
It is much easier to “under promise and over perform” by exceeding expectations than it is to come back from the disappointment of unrealistic expectations that have not been met. When a patient presents with nerve pain, it is much more prudent to allow that FSM has pretty good success in treating nerve pain and that a trial of treatment would be worthwhile.
And the final advice for the practitioner who will use FSM to treat more and more difficult patients is to “Participate fully in the process but don't get attached to the outcome.” Eventually there will be patients who cannot be helped for whatever reason. Pain patients invite compassion in the dedicated physician or practitioner of every profession who treats them. Participating fully in the process of discovering the pain generators, treating them appropriately, providing emotional and nutritional support and physical reconditioning is challenging and stimulating, creating hope and the vision of the opportunity for healing for the practitioner and the patient.
Frustration and despair await those who become attached to the outcomes. And frustration makes it easy to misdirect the blame from the failed treatment to the patient. Pain patients are routinely told that the pain is “all in their head” by frustrated physicians who do not understand or appreciate the diagnosis or have the tools to treat the pain. There is no way for anyone to know enough to help every chronic pain patient who walks in the door. And eventually, every FSM practitioner will have patients who cannot be helped. There is no one to blame.
If there is no attachment to the outcome, there is no frustration and no need to blame anyone or anything for the failure. If the therapeutic process is its own reward and the ego does not need the patient to recover for its own satisfaction then, in the end, compassion remains. The outcome is simply an outcome and compassion can help the patient manage when the outcome is not a cure.
The practitioner and the patient form a team that works for recovery. Healing is not something that the practitioner does to the patient. It is a collaborative effort between the patient and the practitioner with FSM as a third collaborator.
FSM beyond this text
Some patient responses will require frequencies and ways of thinking that are not within the scope of this text. For example, a patient who was injured in a severe auto accident 24 years previously was treated for neck and shoulder pain. Her cervical range of motion increased from pre-treatment flexion of 30 degrees to post-treatment flexion of 60 degrees and the neck and shoulder pain resolved. And then during the night after treatment the patient experienced lower leg and foot muscle cramps. The patient had been warned to expect some unpredictable reaction as a result of the increased range of motion in the neck and so called to report the painful leg cramps the next day.
What could possibly connect the neck with the calves and feet? It might have been pure coincidence but the timing of the leg cramps and a cursory knowledge of neurology made that an unlikely and remote possibility. The potential solution and how to arrive at it are obvious to those with more advanced training and experience in FSM.
There are frequencies for the spinal cord in Chapter 8 and for the dura in the FSM advanced course. The spinal cord contains sensory and motor tracks that carry signals between the brain and the muscles in the legs and feet, the dura covers the cord and they travel together through the neck inside the spinal column. When the neck moves, the cord and the dura have to slide through the spinal canal during the movement like a cable moving inside a piece of moving flexible conduit. If the neck has not moved to more than 30 degrees of flexion in 24 years, then the dura and the cord have not moved in 24 years and could be expected to become adhered to the canal during that time. Increasing range of motion in the neck from 30 degrees to 60 degrees in a 40-minute treatment after 24 years of restricted movement by working on the muscles, discs, and facet joints (but not the dura or the cord) would reasonably be expected to cause problems in the untreated tissue. The increased movement would tug on the adhesions between the cord and the dura and the dura and the canal, create traction in neural pathways in the cord and probably inflammation in tethered regions of the cord and dura. It would not be surprising if this inflammation led to leg cramps in this particular patient. At least this was the hypothesis formed when the patient called. There had to be a connection between the increased motion and the leg cramps and this seemed the most likely possibility.
The solution was to treat the cord and the dura to remove inflammation and adhesions while the patient flexed forward to move the cord and dura through a complete range of motion. Initially the patient could feel restrictions and pain in the spine and pain in the lower legs at 20 degrees of forward spinal flexion. Instructed to return to an upright position and then to try trunk flexion again after a few minutes with the frequencies running from neck to feet, her range increased by 10 degrees. After repeating this movement during 20 minutes of treatment to remove “inflammation and scar tissue” from the “cord and the dura” she gradually flexed further forward with each repetition until she was sitting with her chest on her thighs and her hands on the floor for the first time in 24 years. The pain and range of motion in her neck improved even more with this treatment and the leg cramps were never again a problem.
The ability to treat the condition helped to create the hypothesis and then test it. The response to treatment suggests that the dura and the cord became inflamed and adhered to each other because of the injuries to the disc created by the accident 24 years previously.
• “Inflammation leads to chronic inflammation leads to fibrosis, adhesions, hardening, and scarring.” This progression of pathology is universal and the ability to disrupt it by dissolving adhesions and removing inflammation in minutes using frequencies presents treatment possibilities not available through any other means.
The treatment possibilities change the diagnostic possibilities. It would never occur to most (non-FSM) practitioners to connect increased range of motion in the neck with leg cramps unless there was a way to treat the spinal cord and dura to remove the hypothesized inflammation that was causing the cramps and dissolve the hypothesized adhesions that were limiting range of motion. It is entirely possible that the adhesions would have dissolved in time due to the effects of increased motion but it was educational and revealing to double range of motion in the trunk and reduce the tone in the calf muscles in 20 minutes. The time frame in which the changes were created eliminates the possibility that anything other than the frequency-specific intervention was responsible for the change.
These more advanced frequencies and concepts are available to those who wish to move beyond this introductory text to the full FSM Core seminar course and then progress to the advanced frequencies and physical medicine or visceral medicine advanced course material.
The frequency response creates profound changes in physical tissue and gives us a glimpse of the energetic reality behind matter and physical appearance. The power for healing and pain relief inherent in the frequency response should be used with compassion, skill, humility and wisdom.