8 Treating fibromyalgia associated with spine trauma
Fibromyalgia is a chronic pain condition associated with a complex of multi-system symptoms and has been characterized in recent years as a neuroendocrine disorder that includes characteristics of central pain sensitization and alterations in central hormonal function. There is no definitive laboratory test that will be positive in fibromyalgia and patients may or may not be diagnosed correctly.
55% of fibromyalgia patients report gradual onset of symptoms as middle aged adults. 55% could not recall a precipitating event. 24% report onset after some physical trauma such as an auto accident, fall or surgery. 14% report onset after some psychological stressor. Various studies report that up to 88% of fibromyalgia patients are female, 92–100% are Caucasian, average age at onset is 29–37 years old, average age at presentation is 34–53 years old (Moldofsky 1975).
Fibromyalgia patients have reduced levels of the branch chain amino acids, reduced serum levels of serotonin, epinephrine, norepinephrine and growth hormone and increased levels of substance P in the spinal fluid (Juhl 1998). Fibromyalgia is 13.3 times more common in patients following cervical injuries than it is in patients who have had lower extremity injuries. A study from Israel documented a 22% prevalence of fibromyalgia 1 year after auto accidents causing whiplash injuries in comparison with 1% prevalence after accidents involving leg fractures (Buskilla 1997).
Fibromyalgia patients process pain differently from normal patients. Patients with fibromyalgia have augmented central processing of nociceptive stimuli in comparison with pain-free controls. When measured by EEG, fibromyalgia patients have changes of greater amplitude on both sides of the brain in response to painful stimuli. Pain-free controls responded on only one side of the brain with smaller evoked potentials (Mountz 1995).
The nerves respond more strongly to painful stimuli and the response lasts longer than is normal. There was an increase in late nociceptive evoked somatosensory response in 10 FMS patients as compared to 10 controls (Bennett 1994). SPECT scanning of the brain of a patient with fibromyalgia shows reduced blood flow in the caudate nucleus of the thalamus, which is a site of central pain processing. Fibromyalgia patients have the characteristic pain of allodynia in which non-noxious stimuli such as light touch are processed as painful (Kandel 1985, Bennett 1999).
There is evidence that pain perception in fibromyalgia patients is different in quality from healthy patients; fibromyalgia patients are more sensitive to pain. In normal controls the pain threshold increases gradually between 80 and 160 pressure units and spikes dramatically at 160 units of pressure. Fibromyalgia patients show a linear increase in pain intensity with pressure intensity at every level from 80 to 200 units of pressure. Animal studies show this same pattern due to central sensitization and lowered firing threshold in the dorsal horn cells (Bendtsen 1998).
The most important thing you need to know about fibromyalgia is that it is curable. This chapter is intended to teach not only the frequency treatment protocols that are appropriate for treating fibromyalgia associated with spine trauma but also the conceptual framework for diagnosis and the adjunctive therapies that are necessary to help a patient to recover from fibromyalgia once the pain has been eliminated and to understand and address the cases in which recovery is elusive or difficult.
Eliminating the pain is only the first part of the recovery process. Returning the patient to full health is a challenging multidisciplinary project but has been done in enough cases to provide hope and therapeutic direction. The research shows that treatment must address the spinal cord, the pain processing centers in the brain and the neuroendocrine system. Clinical practice shows that treatment must reduce or eliminate pain as a way of reducing HPA stress and then rehabilitate the digestive system, the adrenals and the endocrine system.
Fibromyalgia diagnosis
Fibromyalgia (FMS) is a complex and still controversial diagnosis because it is a syndrome, a complex of symptoms forming a picture that must be diagnosed clinically. It cannot be diagnosed from an MRI, or by any imaging or blood test. There are more than 200 studies in the medical literature demonstrating neurologic and endocrine changes unique to fibromyalgia patients as compared to other chronic pain or depression patients. For the purposes of this chapter it will be assumed that the condition is real and can be diagnosed by a discerning, informed and educated clinician.
Patients are tested with an algometer to determine the point at which they report pain with pressure. The ACR criteria say that this threshold has to be reached at 4 pounds per square inch pressure or less. Using an algometer ensures that the testing is reproducible and will allow for repeat testing to document decreases in sensitivity as the patient improves. The report of full body pain, fatigue and non-restorative sleep lasting for more than 3 months fulfills the diagnostic criteria (Moldofsky 1975, Russell 1986).
What is not fibromyalgia
A careful history and laboratory blood work is required to ensure that the patient doesn't have one of the following conditions that cause symptoms similar to fibromyalgia. All too often a patient is mistakenly diagnosed with fibromyalgia (FMS) when the symptoms are instead caused by a treatable medical condition.
• Chronic fatigue: Fatigue, cognitive problems, pharyngitis, swollen lymph nodes, low grade fever, substance P not elevated. Epstein–Barr viral titers and antibodies may be elevated.
• Depression: Check neurotransmitter profile by testing urine or using a questionnaire. Sleep disturbance with early morning awakening differs from fibromyalgia sleep disturbance and the cognitive dysfunction is different. FMS responds to smaller doses of anti-depressants. Rule out major depression.
• Hypothyroidism: Early hypothyroidism shows diffuse myalgia and fatigue. Laboratory values will be abnormal particularly TSH, T3, T4 and anti-thyroid antibodies. Body temperature is low in hypothyroidism but normal in FMS. Constipation, dry skin, and brittle hair are not characteristic symptoms of FMS. TSH is notoriously unreliable as a precise indicator of thyroid function. All parameters have to be taken into consideration.
• Primary growth hormone deficiency and/or hypogonadism (low testosterone in a male): When the complaint is muscle aches, fatigue, depression, exercise intolerance especially in a 20–40-year-old male, growth hormone and testosterone deficiency must be ruled out before a diagnosis of FMS or depression can be made. The history in growth hormone or testosterone deficiency may include a head injury, trauma or viral infection.
• Sleep apnea: Sleep apnea can cause fatigue and muscle aches. FMS can result from the stress response to sleep deprivation but if the patient has apnea the FMS can be easily resolved by correcting the apnea. Sleep apnea is at potentially fatal condition and proper diagnosis is crucial. Excessive daytime sleepiness, weight gain, reports of snoring or frequent nocturnal awakening should be followed up with a sleep study and CPAP prescription to correct the problem.
• Inflammatory muscle disease: While the symptoms of body pain and sleep disturbance (due to pain) are similar to FMS, muscle enzymes and sed rate will be elevated in this condition and are normal in FMS.
• Lyme disease: Lyme is reaching epidemic proportions in the US and is characterized by rapid symptom onset, rash, joint aches, positive antibody tests and may respond to doxycycline. The CDC diagnostic criteria requires that five out of five antibody markers be present for a definitive diagnosis but clinicians treating the condition report that if the patient has the symptoms and history characteristic of Lyme disease and have two or three of the antibody markers treatment is justified and useful.
• Parkinson's: The patient will present with stiffness often interpreted as mildly painful but myofascial pain due to age related arthritis and sleep disturbance may confuse the picture. Patient may have tremor, loss of spontaneous movements and loss of facial expression.
• Polymyalgia rheumatica: Pain and stiffness in shoulders, trunk and pelvis usually found in patients over age 50 are characteristic. Sleep disturbance may be age related or due to pain. Sed rate will be elevated in PMR and is normal in FMS.
• Rheumatoid arthritis, lupus and systemic sclerosis: Fatigue and myalgia occur before articular symptoms and can be mistaken for FMS. RA factor, sed rate, ANA titer will be normal in FMS, abnormal in these conditions.
• Silicon breast implant reaction: History will include breast implants – even saline. Symptoms include dry eyes and mouth, painful joints. 70% have positive ANA. Symptoms can persist even after removal of the implant.
Before a patient is diagnosed with fibromyalgia the following blood work must have been ordered and values must be in the normal range: complete blood count (CBC), chemistry screen to evaluate liver and kidney function, sed rate, ANA titer, muscle enzymes, CRP, salivary or serum hormone levels including cortisol, progesterone, DHEA and testosterone, IgF1, TSH, T3, T4, anti-thyroid antibodies. A vestibular screening examination should be performed to rule out endolymphatic disorders.
If the patient reports symptom onset following spine trauma, a trial of treatment can be done to determine if the pain can be reduced. However the patient is entitled to more than one diagnosis and may have pain from fibromyalgia and one of the above conditions.
Different etiologies of fibromyalgia
In a clinical setting, fibromyalgia patients seem to sort into eight fairly clear although often overlapping etiologies. These are clinical distinctions based on patient histories and response to treatment developed during 12 years of treating hundreds of fibromyalgia and myofascial pain patients.
• Stress: One type of FMS seems to be associated with prolonged emotional or physical stress and physiologic sequelae of prolonged elevated cortisol

Figure 8.1 • The algometer allows delivery of a calibrated amount of pressure to assess pain sensitivity. The ACR criteria require that the patient report pain at 11 of 18 pressure points in response to 4 pounds per square inch pressure. There is also some mention of “the amount of pressure required to produce blanching of the examiner's thumb nail bed” which leaves room for considerable ambiguity. The algometer allows more precise and reproducible pressure.
and other stress hormones and the subsequent adrenal depletion (Maes 1998, Adler 1999). The section below describing the physiologic effects of severe prolonged stress explains the mechanism by which stress can create fibromyalgia (Dessein 1999).
• IgG food sensitivities: FMS can be associated with “leaky gut” and IgG food or environmental allergies. Mast cell overload from elevated IgG complexes causes the release of histamine causing “brain fog” and fatigue and stimulating class C pain fibers to create widespread aching.
• Toxicity: This etiology of FMS is associated with one-time acute or long-term chronic exposure to organic chemicals, heavy metals or pesticides that change nerve membrane firing characteristics creating generalized body pain, cognitive dysfunction and fatigue. Liver enzymes, especially GGT, may be elevated. GGT is so frequently positive that many labs no longer include it in a standard chemistry screen. It is the most sensitive marker for liver inflammation and must be ordered specifically. History questions regarding previous places of employment and residence, previous job descriptions such as hair dresser, landscape maintenance, printer, or painter will reveal exposures to organic chemicals (Baker 1997).
• Genetic: This type has a genetic link, seems to run in families and may be associated with food sensitivities, especially gluten, or may represent an increased need for enzyme substrate in the liver detoxification or serotonin pathways.

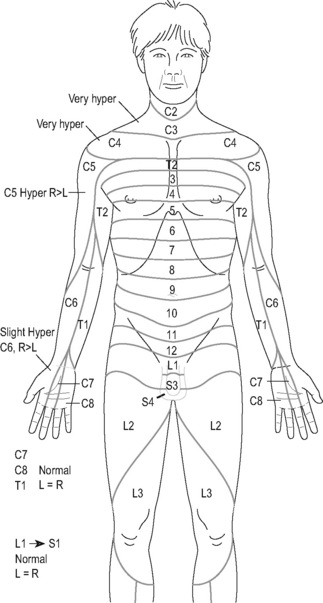
Figure 8.2 • When the tender points are evaluated with an algometer the number recorded on the diagram represents the number of pounds per square inch pressure that caused pain. Dating the record allows tender point evaluation to track progress.
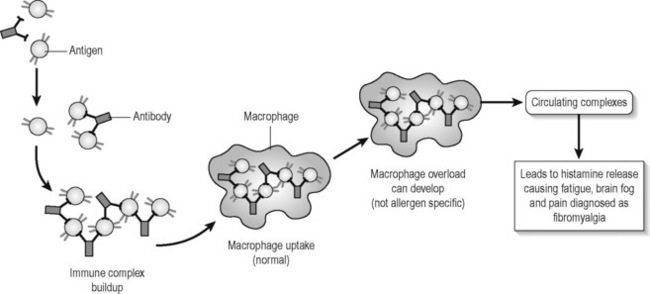
Figure 8.3 • When large numbers of IgG antigen–antibody complexes are ingested by macrophages histamine is released into circulation. Histamine stimulates class C pain fibers causing widespread diffuse aching and stimulates immune system responses leading to fatigue and cognitive dysfunction and a diagnosis of fibromyalgia.
• Viral: This type occurs after immunizations or viral illness. The symptoms may be from immune response to the virus or from nervous system response to the mercury preservatives in the immunizations.
• Vestibular injuries: This condition is not truly fibromyalgia but it is associated with the sleep disturbances and cognitive difficulties resulting from a vestibular injury or brain trauma. The sleep deprivation creates neuroendocrine stress eventually resulting in fibromyalgia. The patient will present with symptoms characteristic of FMS and the vestibular etiology has to be teased out during the history.
• Peri-menopause and trigger points: This type of FMS is associated with poorly managed menopause. Estrogen reductions cause sleep disturbance due to hot flashes and relative progesterone deficiency causes fatigue. Myofascial trigger points cause regional pain which can be in all four quadrants leading to central sensitization and a diagnosis of fibromyalgia. The solution for this etiology of fibromyalgia is proper hormone management and trigger point therapy using FSM (see Chapter 7) (McMakin 1998, 2004).
• Spine trauma: This type of fibromyalgia occurs after whiplash injuries, cervical or thoracic spine trauma, or after surgery and can be caused by any trauma that involves spinal flexion/rotation, spinal compression or ballistic segmental movement during a fall or impact (Bohlman 1979, Mendel 1989). The post-surgical cases are thought to occur when the neck is hyper-extended during intubation and constitute a cervical injury. Approximately 24–30% of fibromyalgia patients associate the onset of their condition with physical trauma although privately some clinicians have proposed the percentage to be closer to 50%. As a group they are the only FMS patients who complain specifically of pain in the hands and feet or describe their pain as burning.
All fibromyalgia patients, regardless of the etiology of their condition, have the same neuroendocrine and central sensitization features described in the fibromyalgia research but each etiology responds to different treatment strategies (Bennett 1999, Crofford 1998, Neeck & Reidel 1999). The model for the different types of fibromyalgia was developed when it was discovered that fibromyalgia could be successfully resolved when the treatment strategy addressed the specific cause or etiology of the pain or dysfunction.
Fibromyalgia associated with spinal trauma (cervical trauma fibromyalgia or CTF) represents a distinct etiology from fibromyalgia associated with other causes. The other types of fibromyalgia can be improved or cured without the use of FSM, although FSM helps accelerate the process. Fibromyalgia from spine trauma appears to respond only to FSM treatment and probably represents the 30% of non-responding fibromyalgia patients found in most fibromyalgia therapeutic studies.
Fibromyalgia from spine trauma – typical presentation and history
Treating fibromyalgia from spine trauma (CTF) is fairly easy; recognizing it can be more problematic because patients do not always associate their pain with the physical trauma but may attribute it to the emotional stress that accompanied the physical event. The patient who described her FMS as being due to the “emotional stress” of her divorce failed to recall falling off of a chair and hitting her head on the wall while painting the kitchen ceiling during her divorce until after treatment for CTF alleviated her pain and persistent questioning jogged her memory.
The pain diagram and symptom complaint describes aching burning midscapular pain, shoulder, neck, arm and hand pain that begins soon after the trauma and persists to varying degrees from the time of the injury to the date of presentation. Mid-scapular pain may represent referred pain from an injured cervical disc (Cloward 1959, Bogduk 1988). After some period of time, usually 1–6 months post-injury, the pain generalizes to the whole body, particularly down the thoracic and lumbar paraspinals, the gluteals and down both legs into the feet. The pain will be described as burning, aching, stabbing and sharp.
The patients generally rate the pain as varying between a 4 and a 9/10 on a visual analog scale. Most describe their hands and feet as feeling cold, burning or aching since the accident or injury. CTF patients have a characteristic affective response to the pain; it is particularly bothersome. Most have chronic headaches that can be quite severe. Many have been on narcotics, Neurontin or Lyrica for some time.
Imaging
MRI studies usually show a disc bulge or a contained herniation at C5–6 or C6–7 and less often at C4–5. In many cases the films have been read as normal by the original radiologist since degenerative changes and
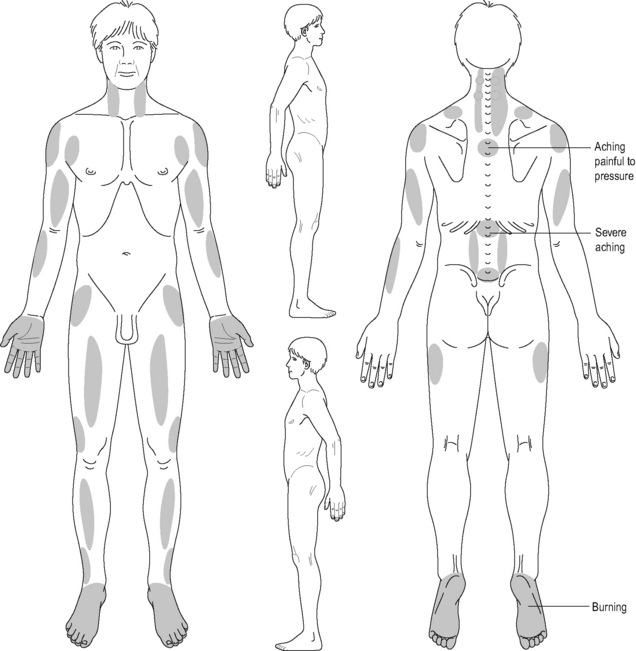
Figure 8.4 • The pain diagram for fibromyalgia associated with cervical spine trauma (CTF) differs from other fibromyalgia pain diagrams. As a group, CTF patients are the only fibromyalgia patients who describe their pain as burning and stabbing and report aching and burning in the hands and feet. This pain diagram is characteristic and predictive of a CTF diagnosis. It is virtually identical to pain diagrams characteristic of central pain except that central pain patients usually also report pain in the head and face (see Chapter 10).
small disc bulges are considered “normal” in a patient population. Many pain-free patients have disc bulges that do not produce symptoms. When the films were re-examined by a consulting radiologist specializing in spinal imaging the revised report described a central bulge or contained herniation.
The clinician is encouraged to review the films personally and not rely on the report when assessing fibromyalgia patients. The findings on the film must be correlated with the clinical assessment and physical examination as there is no way to tell from imaging alone whether a disc is causing symptoms.
Weight bearing flexion–extension MRI studies have recently become available in some facilities and will occasionally reveal a disc bulge that looks small in neutral but then extrudes in either flexion or extension causing spinal cord compression and myelopathic changes in the cord. The risk to the spinal cord requires a surgical referral for these patients.
Plain film x-rays cannot assess disc injuries but may reveal anterolisthesis or retrolisthesis near the abnormal segment. Flexion–extension lateral cervical spine x-rays may show increased translation, at the level of disc injury documented on the MRI.
In a very rare case the imaging may be completely normal but the mechanism of injury may involve force vectors that stretch the spinal cord and cause direct injuries to the spinal cord vasculature or neuronal tracts.

Figure 8.5 • This microscopic examination done at autopsy shows contained herniation and end plate fractures in a disc whose postmortem imaging was read as normal (reproduced with permission from Taylor & Twomey 1993). The patients in this study died from causes other than spine trauma during motor vehicle accidents.
Physical examination
The patellar reflex will be hyperactive, very brisk with a larger than normal amplitude. This is the hallmark diagnostic physical examination finding for fibromyalgia associated with spine trauma. In many cases, striking the patellar tendon on one side causes not only the hyperactive patellar reflex but also causes the adductors on the opposite leg to contract. In most cases the upper extremity and Achilles reflexes will be normal. Fibromyalgia that is not due to spinal trauma will demonstrate normal or even reduced patellar reflexes.
The sensory examination invariably shows hyperesthesia in one or more upper extremity dermatomes, usually C3, C4 or C5, and occasionally in a lower extremity dermatome.
Muscle strength will be normal in most cases. These patients are not generally surgical candidates although some may be. Cervical compression, performed by applying axial pressure to the spine by pressing on the top of the head, will produce neck pain and an increase in shoulder pain in most cases.
Measurement of the 18 ACR defined tender points by algometer show at least the required 11 out of 18 necessary for a fibromyalgia diagnosis unless the patient was on narcotic medication that reduced sensitivity. Many of these patients will report pain with as little as 1–2 pounds per square inch of pressure.
How spine trauma leads to fibromyalgia
How could cervical spine trauma cause fibromyalgia and central pain sensitization? Trauma creates cracks in the disc annulus or the cartilaginous end plate and exposes the spinal fluid and spinal cord to the material in the disc nucleus. The disc nucleus contains neurotoxic concentrations of phospholipase A2 (PLA2) shown to cause nerve destruction in dogs, pigs and rabbits. PLA2 has been shown to be so inflammatory and neuro-toxic that it destroys nearby nerves in a dose related response (McCarron 1987, Olmarker 1993, 1995, Ozaktay 1995, 1998, Cavanaugh 1997, Chen 1997, Marshall 1997).
The damage to the discs shown by Taylor & Twomey (1993) occurs in the postero-lateral portion of the disc which is directly adjacent to the antero-lateral portion of the spinal cord. The paleospinothalamic tract is the outermost of the two tracts in the lateral column of antero-lateral cord and carries diffuse deep pain information up the spine to the thalamus, caudate nucleus and the cortex (Lombard 1983). This tract is the one closest to the portion of the disc most likely to be damaged (Netter 1991).
The anatomic proximity of the cracks in the discs and endplates could expose this tract to very high neurotoxic levels of PLA2.
If inflammation progressed to create damage in the paleospinothalamic nerves it would effectively create a chemical deafferentation of the pain pathways in the spinal cord. Inflammatory chemicals reduce the firing of nerves and slow or stop nerve conduction.
Trauma can cause direct mechanical disruption of the antero-lateral pathways and the spinal cord leading to deafferentation of these axonal pathways according to Taylor & Twomey (1993). Deafferentation in the antero-lateral ascending pain pathways in the spinal cord would produce what is essentially thalamic or central pain. Disruption of pain pathways in the spinal cord leads to central pain:
“Central pain can arise not only from pathologic lesions in the thalamus but also from neurosurgical lesions placed anywhere along the nociceptive pathway from the spinal cord and brain stem to the thalamus and cortex. … The sensations are unpleasant and abnormal, often unlike anything the patients had ever felt before: spontaneous aching and shooting pain, numbness, cold, heaviness, burning and other unsettling sensations that even the most articulate patients find difficult to describe. Central pain is particularly distressing emotionally.”
Fibromyalgia patients with a cervical trauma etiology use exactly the same pain descriptors, word for word, as central or thalamic pain patients. Patients with fibromyalgia that is not caused by cervical trauma do not have the same severity, quality or location of pain that cervical trauma patients describe. Their pain is diffuse and achy but it lacks the disturbing affective neuropathic intensity seen in the cervical-trauma mediated fibromyalgia patients. Post-traumatic fibromyalgia patients are the only group who complain of aching in their hands and feet and the only group that responds to the treatment protocol for inflammation in the spinal cord.
Treating fibromyalgia associated with spine trauma
Medical science accepts as a given that fibromyalgia is an incurable condition and the randomized controlled studies done so far have had that view as a starting point. Controlled trials by their nature can study only one intervention as it affects one or more symptoms. Since fibromyalgia is a collection of multiple symptoms affecting numerous systems each affected by multiple influences, the possibility that any one intervention will produce remission of all symptoms or cure the condition is extremely remote, especially if one starts with the presumption that the condition is incurable. The clinical strategies that have created recovery for so many patients operate within a framework in which recovery, while not inevitable, is thought possible because it has been observed to be so (Teitelbaum 2001). It is left to the reader to decide which viewpoint is most productive.
The treatment protocol in this chapter was developed by trial and error in 1999 and found to be effective in eliminating pain in over 200 FMS patients with spinal trauma onset. Pain has been reduced from an average of 7.4/10 to 1.4/10 in every patient with hyperactive patellar reflexes, dermatomal hyperesthesia, a history of trauma and pain in the hands and feet. Reducing the pain is relatively easy; achieving recovery is more involved because of the neuroendocrine and metabolic disturbances (McMakin 2005).
Pain is only part of the fibromyalgia diagnosis and symptom picture. Once the pain can be alleviated the patient still has the metabolic abnormalities characteristic of fibromyalgia. The neuroendocrine dysfunction in fibromyalgia patients is almost as disabling as the pain and it may be associated with alterations in central hormone function, primarily mediated corticotrophin releasing hormone or corticotrophin releasing factor (CRF or CRH).
Neeck & Reidel (1999) proposed, and it seems a reasonable hypothesis, that the pain itself serves as a chronic stressor elevating CRH in the hypothalamus. CRH in turn modifies levels of LHRH (luteinizing hormone releasing hormone), TSH (thyroid stimulating hormone), and GHRH (growth hormone releasing hormone) centrally contributing to disruptions in circulating hormones. Progesterone, growth hormone, thyroid hormone levels and thyroid receptor sensitivity are all affected. Chronic moderate neuropathic pain would be sufficient to cause the elevations in CRH found in fibromyalgia and the alterations in central pain processing common to fibromyalgia patients (Bennett 1999).
By the time the patient has been in moderate to severe pain for 1–2 years the symptoms generalize to include the classic neuroendocrine abnormalities seen in fibromyalgia caused by any etiology (Crofford, Demitrack 1996, Crofford, Engleberg, Demitrack 1996, Crofford 1998, Neeck & Reidel 1999). Understanding the neuroendocrine abnormalities is helpful when diagnosing fibromyalgia but it becomes crucial when attempting to resolve or cure it.
Understanding stress and neuroendocrine dysfunction
The key problematic central neuroendocrine hormone in fibromyalgia is corticotrophin releasing hormone or corticotrophin releasing factor (CRF or CRH). The stress response has its own evolutionary survival logic. When the body comes under attack it does not respond differently if the level 8/10 pain is caused by a tiger dragging you into the woods or by a disc bulge causing full body neuropathic pain. Certain stress responses go into effect mediated primarily by CRF/CRH and cortisol to keep the body alive until the attack is over. CRF stimulates the adrenals to increase cortisol levels and it acts centrally to modulate central regulatory hormones.
All repair systems and long-term physiologic processes are put “on hold” until the threat either kills you or resolves (Sapolsky 1994). This survival strategy is perfect for short-term attacks by tigers but creates problems when the stress persists in the form of moderate to severe pain lasting years.
Stress and thyroid
CRF suppresses thyroid stimulating hormone (TSH) centrally (Neeck & Reidel 1999). Primitive survival logic dictates that the stress hormones are stimulating enough and additional thyroid hormone would be hyper-stimulatory. Elevated cortisol from the adrenal glands suppresses the peripheral conversion of the T4 storage form of thyroid hormone into the T3 active form of the hormone. Many fibromyalgia patients present as if they are clinically hypothyroid complaining of weight gain, constipation, dry skin, hair loss, fatigue and feeling cold. The patient becomes functionally hypothyroid because T4 cannot convert efficiently into T3 but TSH is almost always found to be in the normal or upper end of normal range when tested. TSH cannot rise in response to the relative peripheral insufficiency because it is suppressed centrally by CRF.
Stress and gonadal hormones
CRF suppresses FSH (follicle stimulating hormone) and LH (luteinizing hormone) centrally (Sapolsky 1994). The long-term projects of ovulation, sperm production, copulation and pregnancy are put on hold until the threat is gone. In women FSH and LH promote maturation of the corpus luteum and its increased production of progesterone to balance the estrogen produced by the ovaries during the post-ovulatory portion of the menstrual cycle. If production of progesterone by the corpus luteum is insufficient to balance estrogen the patient experiences the symptoms of premenstrual syndrome (PMS) caused by estrogen dominance. The patient complains of fatigue, irritability, water retention, sleep problems and emotional lability. These complaints are common to fibromyalgia patients.
Stress and growth hormone
CRF suppresses growth hormone releasing factor (GHRH) centrally interfering with growth hormone secretion (Bennett 1997). In an adult, growth hormone facilitates amino acid transport across the cell membrane to enhance tissue repair. Growth hormone in an adult is released during stage IV sleep and in a burst about 1 hour after vigorous exercise. Fibromyalgia patients do not experience stage IV sleep and they do not have the normal burst following exercise due to CRF suppression. Without adequate levels of growth hormone the normal exercises and activities of life and the minor tissue damage that follows are not easily repaired. This explains why fibromyalgia patients experience days or weeks of muscle pain after simple exercise or exertion.
Stress and the brain
CRF acts as a neurotransmitter and modifies cognitive processing to interfere with short-term memory and modulate long-term memory. In acute stress the only short-term information processing required is the answer to: “How do I get away from this tiger?” which leads the brain to focus on: “How did I get away from the tiger the last time?” Fibromyalgia patients complain of problems with short-term memory, processing and memory for details and sequencing of activities and information. And long-term memory is biased toward remembering unpleasant events and how they happened (Henley 2001).
Stress, digestion and IBS
Cortisol, chronic stress and sympathetic upregulation interfere with digestion. Digestive enzymes and stomach acid secretions are suppressed. Digesting meals is one of the short-term projects put on hold until the threat passes. Food can be digested tomorrow, if there is a tomorrow, but digestion is not as important as escape when the threat is present. If stomach acid secretions are suppressed, the stomach does not empty efficiently, leading to reflux of the semi-digested food and when it does empty the contents may not be as acidic as required for optimal digestion and absorption of minerals and protein.
The proper acidic pH of gastric contents creates the environment that supports proper bacterial flora in the intestines. Acid-loving bacteria decline and other bacteria proliferate in the more alkaline environment created by bicarbonate from the pancreas and relative decrease of acid. Intestinal bacteria help to digest food and create short-chain fatty acids that maintain intestinal health. If stomach acid and pancreatic digestive enzymes are both insufficient food may not be adequately digested or absorbed. Large undigested food particles may putrefy in the gut creating the local allergic responses and inflammation characteristic of irritable bowel syndrome commonly seen in fibromyalgia patients. Elevated cortisol levels cause thinning of the gut wall and when combined with inflammation caused by dysfunctional digestion, can contribute to the loss of gut membrane integrity sometimes called “leaky gut”. Larger food molecules could leak across the membrane and encounter the immune system, contributing to food sensitivities commonly seen in fibromyalgia patients (Guyton 1986, Sapolsky 1994, Galland 1997).
Stress and insulin resistance
The stress response shifts the body to a short-term glucose economy to ensure that there is enough glucose available to fuel the muscles required to run away from the tiger. Insulin sensitivity declines as the body attempts to keep glucose out of storage and into the blood and muscles where it is needed emergently. This, combined with the exercise intolerance caused by growth hormone deficiency, leads to weight gain, insulin resistance and all of their associated health risk factors (Henley 2001, Sapolsky 1994).
Pain reduction and stress reduction
The key to resolving fibromyalgia appears to be keeping the pain below a 4/10 VAS level. When the pain is consistently kept below a 4/10, the neuroendocrine disturbances seem to resolve within approximately 4 months. It is intriguing to watch this transition. The neuro-hormonal and digestive disturbances common to fibromyalgia begin to improve within several weeks and may even resolve with no other intervention beyond pain relief. Reducing pain reduces stress and reducing stress allows the neuroendocrine system to return to normal function.
It is possible to provide adrenal support with FSM, nutritional supplements and herbs, to provide neuroendocrine support for cognitive function and mood with neurotransmitter precursors and FSM, and to support digestive system recovery with FSM, digestive enzymes, nutritional supplements, herbs and appropriate gut bacteria.
But if time allows and the patient is healthy enough to achieve it, it is intriguing to watch the body normalize function on its own with no other intervention except continuous pain relief.
Treating fibromyalgia associated with spine trauma
• The patient must be hydrated to benefit from microcurrent treatment.
• Hydrated means 1 to 2 quarts of water consumed in the 2 to 4 hours preceding treatment.
• Athletes and patients with more muscle mass seem to need more water than the average patient.
• The elderly tend to be chronically dehydrated and may need to hydrate for several days prior to treatment in addition to the water consumed on the day of treatment.
• DO NOT accept the statement, “I drink lots of water”.
• ASK “How much water, and in what form, did you drink today before you came in?”.
• Coffee, caffeinated tea, carbonated cola beverages do not count as water.
Channel A: condition frequencies
The frequencies listed are thought to remove or neutralize the condition for which they are listed except for 81 and 49 / which are thought to increase secretions and vitality respectively
| 91 / | |
| 284 / | |
| 50 / | |
| 40 / | |
| 19 / | |
| 43, 46 / |
| 94 / | |
| 321 / | |
| 9 / | |
| 13 / | |
| 3 / | |
| 81 / | |
| 49 / |
Channel B: tissue frequencies
 This frequency appears to affect the spinal cord but not the dura. Treating the dura is beyond the scope of this introductory text and is covered in the FSM Advanced courses.
This frequency appears to affect the spinal cord but not the dura. Treating the dura is beyond the scope of this introductory text and is covered in the FSM Advanced courses. The midbrain frequency appears to address the anatomical structures in the center of the brain including the thalamus and hypothalamus. The thalamus is involved in the central pain amplification and central pain sensitization seen in fibromyalgia. In clinical applications, the use of this frequency on channel B combined with the frequency to reduce inflammation consistently reduces central pain and central pain amplification.
The midbrain frequency appears to address the anatomical structures in the center of the brain including the thalamus and hypothalamus. The thalamus is involved in the central pain amplification and central pain sensitization seen in fibromyalgia. In clinical applications, the use of this frequency on channel B combined with the frequency to reduce inflammation consistently reduces central pain and central pain amplification. All parts of the brain are affected by prolonged pain. The medulla frequency is thought to address the entire brainstem including the reticular activating system which alerts the brain to threat. The forebrain modifies judgment to consider the affects of pain and the hindbrain modifies movement and activity to avoid pain. All of these parts of the brain are affected by chronic pain and central pain sensitization. Reduction of central pain amplification appears to be most effective when all parts of the brain are treated.
All parts of the brain are affected by prolonged pain. The medulla frequency is thought to address the entire brainstem including the reticular activating system which alerts the brain to threat. The forebrain modifies judgment to consider the affects of pain and the hindbrain modifies movement and activity to avoid pain. All of these parts of the brain are affected by chronic pain and central pain sensitization. Reduction of central pain amplification appears to be most effective when all parts of the brain are treated.Treatment protocol
Prepare the cord for treatment
40, 50 / 10
Alternating current minimizes the chance of a side effect thought to be caused by restriction of spinal fluid flow around a disc bulge near the spinal cord. Alternating current doesn't reduce pain as effectively as polarized positive current but it doesn't seem to increase the rate of spinal fluid flow. Use at the first treatment and in every treatment in any patient with known cord or thecal sac encroachment.
19, 43, 46 / 10
Response to treatment can be slow if the patient has had multiple injections or surgeries or is taking narcotics. Over time it was found that using the frequencies to remove “anesthesia” and “opiates” in the spinal cord improved the rate of response to treatment. It is not known whether these frequencies actually affect opiate levels or tissue storage of anesthesia metabolites or if they just make the receptors more sensitive to the frequency effect. These frequencies do not increase pain so it is unlikely that they have any direct effect on drug levels. Use at the first treatment and any time patients are taking narcotics.
Reduce the pain
40 / 10
• Remove Inflammation / from the spinal cord.
• Current polarized positive +.
• Treatment time: approximately 60 minutes
• Patient supine – well supported.
• Place patient hands on the skin of the abdomen.
 Stay in the room with the patient during the first treatment for at least the first 20 minutes. If there is going to be an adverse reaction to polarized current it will happen in the first 10 minutes. Pain will begin to recede upwards from the feet and lower legs within 10–15 minutes. If asked for a pain level after 15 minutes of treatment, the patient will usually report that their “neck hurts” but if asked how their legs feel they will usually notice that the pain in the legs is reduced or absent.
Stay in the room with the patient during the first treatment for at least the first 20 minutes. If there is going to be an adverse reaction to polarized current it will happen in the first 10 minutes. Pain will begin to recede upwards from the feet and lower legs within 10–15 minutes. If asked for a pain level after 15 minutes of treatment, the patient will usually report that their “neck hurts” but if asked how their legs feel they will usually notice that the pain in the legs is reduced or absent. Pain reduction proceeds upwards from the feet and legs and the neck and shoulder pain is reduced last.
Pain reduction proceeds upwards from the feet and legs and the neck and shoulder pain is reduced last.Lead placement – Patient position
1. Patient should be supine with a bolster under the knees for low back comfort or seated in a recliner chair if one is available. The patient may be treated side lying if that is most comfortable but the head and torso must be well supported. The induced euphoria seen with this protocol during the first few treatments is profound and the patient must be in a well supported comfortable position. For subsequent in-office treatments and for treatments performed by the patient at home the patient may be in any comfortable position.
2. Wrap the glove attached to both positive leads in a warm wet hand towel and wrap the towel around the neck. The towel should be thoroughly wet and then firmly wrung out so it is not dripping.
3. Wrap the glove attached to both negative leads in a warm wet hand towel and wrap the towel around the feet.
4. The patient should be covered with a soft blanket from chin to toes to prevent chill as the towels cool off.
5. Place both of the patient's hands on the skin of the abdomen so the current flows through them during the treatment. This position improves the pain reduction in the arms and hands.

Figure 8.7 • The positive leads from channel A and channel B are attached to a warm wet fabric contact (hand towel) by alligator clips or by wrapping the graphite glove inside the towel that is folded lengthwise around the glove. The towel should be wet thoroughly and then wrung out so it is not dripping. Wrap the towel around the neck avoiding contact with the ears.
• Place adhesive electrode pads on hands and soles of the feet. Channel A positive leads must be on opposite hand from the foot with channel A negative leads.
• Current level: 100–300μamps. Use lower current levels for very small or debilitated patients. Use higher current levels for larger or very muscular

Figure 8.8 • The negative leads from channel A and channel B are attached to a warm wet fabric contact (hand towel) by alligator clips or by wrapping the graphite glove inside the towel that is folded lengthwise around the glove. The towel should be wet thoroughly and then wrung out so it is not dripping. Wrap the towel around both feet. If the patient is very large two towels can be joined by sliding one end into the other creating one longer contact out of the two towels.

Figure 8.9 • Position the patient comfortably in a supine position. Position a bolster under the knees so the spine is comfortably flat. The patient should be covered with a soft blanket from chin to toes to prevent chill as the towels cool and should be well supported on the table or in a reclining chair since patients become very relaxed and many will fall asleep.
patients. In general higher current levels reduce pain more quickly.
• Waveslope: Use a moderate to sharp waveslope for treating the spinal cord and fibromyalgia associated with spine trauma.

Figure 8.10 • When the patient is being treated at home or in a setting where use of towels is inconvenient adhesive electrode pads can be used on the hands and feet. Place the positive lead from channel A on the back of one hand and the negative lead from channel A on the top of the opposite foot. The photograph shows the patient seated for photographic convenience. The patient should be fully supported during treatments because many will fall asleep.
 Possible side effect – increased pain between the shoulder blades, headache
Possible side effect – increased pain between the shoulder blades, headache
Some patients will experience an increase of pain between the shoulder blades and develop a headache within 5 minutes of treatment with current polarized positive from neck to feet. It is speculated that this effect is due to an increase in the rate of spinal fluid flow that first increases pressure on the disc annulus causing referred pain in the mid-scapular area, as shown in Chapter 5 from Cloward (1959), and then causing a headache as the spinal fluid pressure builds up into the ventricles. Using alternating current and the frequencies to reduce inflammation and congestion in the cord at the beginning of the treatment minimizes the chance of this side effect occurring and it should be rare.

Figure 8.11 • Place the positive lead on one hand and the negative lead on the opposite foot. Larger pads conduct current more comfortably. If the pads become dry the current will sting or prickle and can be moistened with water.
Remedy: If mid-scapular pain and a headache occur despite the precautions built into the protocol, stop treating immediately and move the patient from supine to a sitting position. Place the negative leads on the floor under the feet and move the towel with the positive leads from the neck to the shoulders and change the current to alternating (±). Continue to run 40Hz and 10Hz using alternating current until the pain recedes. The entire treatment may be performed with alternating current but it takes more time to reduce the pain with alternating current.
Treating inflammation in the spinal cord has a curious effect on affect and cognitive function, especially in the first few treatments. Most, but not all, patients will experience an “induced euphoria” that is characteristic of this treatment. It is most pronounced while using 40 / 10 polarized positive and the practitioner may want to warn the patient that it is a normal effect as it begins. This is especially advisable for “type A” patients and for those who like to be in control of their surroundings.

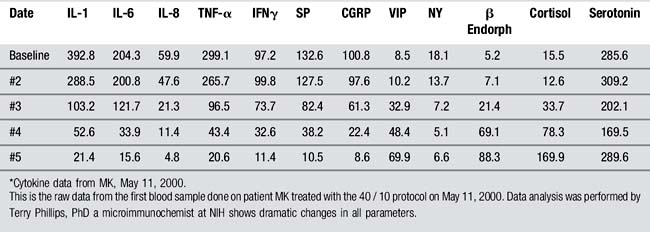
Figure 8.12 • Beta-endorphin, in the first patient measured by micro-immunochromatography prior to treatment, was 5.2 pg/ml. Beta endorphin quadrupled in 45 minutes to 21.4 pg/ml and reached 88.3 pg/ml in 90 minutes, increasing endorphin levels by 17 times during the treatment period and causing the patient to ask drowsily if the treatment was “legal”. The average endorphin levels published from six patients was 8.2 ± 2.5 increasing to 71.1 ± 9.3 pg/ml in a 90-minute period (P = 0.003).
Blood sample data shows endorphins increasing by 10 times in 90 minutes which quantified this response and provided a predictable timeline for its appearance. Endorphin levels double in the first 30 minutes in every patient for whom blood samples have been analyzed. The first sign will be a reduction in the rate of blinking, respiration and speech that starts within 10–15 minutes and corresponds to the reduction in lower extremity pain. Some patients fall asleep, all close their eyes and some become so “stoned” that they do not wish to or simply cannot speak. They can hear and should be reassured that the effect is normal and that it is temporary.
This dramatic effect usually appears at the 30–60-minute mark during the treatment as endorphin levels begin a very steep rise. This phenomenon will wear off as the other frequencies are used at the end of the treatment protocol. The patient will remain relaxed and should come to full function within an hour or so after treatment. Most patients are in full possession of their faculties by the time they are ready to leave the clinic.
PRECAUTION: The practitioner should take care to ensure that the patient is safe to drive.
The only side effect commonly encountered with this protocol is a sympathetic reaction that usually occurs 20–40 minutes into the treatment in about 10% of patients. The reaction is more likely to happen during the first few treatments and less likely with each successive treatment. The patient will become some combination of agitated, anxious, irritated, impatient or annoyed about something. As the pain and cytokines decline the blood chemistries show steep increases in cortisol and endorphins at about the same time that this reaction sets in and these changes in neuro-chemicals are assumed to be related to this phenomenon in some way.
The patient will not know that this reaction is caused by the treatment unless they have been warned about it and may ask to leave the room, stop the treatment, use the toilet or report feeling anxious about the time that has passed, the need to get home or make a phone call. It is wise to tell the patient at the beginning of the treatment that such a reaction is possible so the reaction will not concern or surprise them. The patient should be advised to inform the practitioner if any such symptoms occur.
If the patient has not been warned about this reaction before the treatment and it happens, the best approach seems to be to agree with whatever is concerning the patient and ask if they can delay responding to their urgent situation for just a few minutes. Patients have always agreed to this request. Change the frequencies to those used to quiet the sympathetics. Once the anxiety has passed, tell the patient that this reaction is not uncommon and explain the changes in brain chemistry responsible for it and ask the patient if they still need to do whatever it is that seemed so urgent a few minutes previously.
• Remedy: Change the frequency to 40 / 562.
• Reduce inflammation / in the sympathetics.
• Current polarized positive +.
Once the patient is calm, resume treatment with 40 / 10 polarized positive. If the patient becomes agitated again repeat use of 40 / 562 until the patient is calm again and then resume treatment with 40 / 10 until the pain is gone.
Sustain pain reduction
The body pain should be reduced to 0–2/10 at approximately 60 minutes but may require as long as 90 minutes on the first treatment.
The treatment does not change local joint pain but will only change the full body neuropathic pain. The body pain will be eliminated but the patient may still have local facet joint pain in the neck or low back.
The pain relief achieved with just 40/10 would last between 2 and 12 hours. The shock and disappointment when it returned motivated the clinicians to find ways to make the pain reduction more lasting.
13 / 10 – Polarized positive +
• Reduce scar tissue / in the cord.
• Current polarized positive +.
• Patient seated – Contacts at neck and feet. Once treatment eliminated the pain patients wanted the relief to last longer. Questioning revealed that when the pain was reduced and patients began to exercise and increase range of motion, the pain returned with movement. In an effort to make the pain reduction more lasting it was hypothesized that the chronic inflammation in the spinal cord had caused adhesions in the spinal cord and that removing them would increase exercise tolerance and range of motion. The hypothesis was confirmed when it was discovered that forward trunk flexion of 20 degrees would cause pain or pressure between the scapula and that treating the cord to remove scarring resolved this problem. This protocol makes the pain reduction more lasting.
• Move the cord during 13 / 10 – until range of motion is normal.
 Move the patient to a seated position with the positive leads glove in a warm wet towel that is wrapped around the neck and the negative leads glove wrapped in a warm wet towel placed under the feet.
Move the patient to a seated position with the positive leads glove in a warm wet towel that is wrapped around the neck and the negative leads glove wrapped in a warm wet towel placed under the feet. Have the patient flex the trunk, not the neck, forward slowly until some tension is felt in the mid back usually between the shoulder blades.
Have the patient flex the trunk, not the neck, forward slowly until some tension is felt in the mid back usually between the shoulder blades. Have the patient stop flexion and return to neutral upright position and wait 1 minute while 13 / 10 continues to run. It's a nice time to chat with the patient about their hobbies and grandchildren.
Have the patient stop flexion and return to neutral upright position and wait 1 minute while 13 / 10 continues to run. It's a nice time to chat with the patient about their hobbies and grandchildren. Have the patient flex forward again and there should be some increase in flexion. Stop movement at the first sign of tension or pressure in the mid back. This time the restriction should be felt lower down on the spine at about the T10 area. Return the patient to a neutral upright position and wait 1 to 2 minutes while 13 / 10 continues to run.
Have the patient flex forward again and there should be some increase in flexion. Stop movement at the first sign of tension or pressure in the mid back. This time the restriction should be felt lower down on the spine at about the T10 area. Return the patient to a neutral upright position and wait 1 to 2 minutes while 13 / 10 continues to run. Repeat this process until the patient can flex forward to between 70 and 90 degrees or to some range that is limited by the hips and not the spine.
Repeat this process until the patient can flex forward to between 70 and 90 degrees or to some range that is limited by the hips and not the spine. If a movement increases body pain switch the frequency back to 40 / 10 for 5 minutes or until the pain is reduced. Then return to the 13/ 10 process until range is acceptable.
If a movement increases body pain switch the frequency back to 40 / 10 for 5 minutes or until the pain is reduced. Then return to the 13/ 10 process until range is acceptable.• Use 3 / 10 if range of motion does not increase fully with 13 / 10.
• Reduce sclerosis / in the spinal cord.
• Some patients seem to respond better to 3 / 10 than they do 13 / 10. Use the same motion instructions and timing as described for 13 / 10.
Reduce central amplification
It is common for the patient to be strongly affected by the endorphin levels and to appear almost disoriented once the pain is near 0/10, especially as the range of motion increases. One patient commented that, “I feel as if I should be in pain but I am not.”
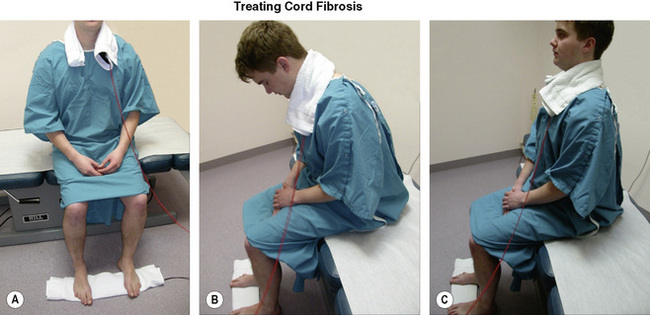
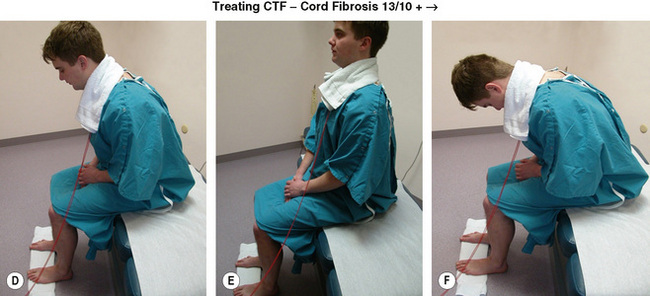
Figure 8.13 • A, B C: When the pain is reduced to 0–2/10, have the patient sit up on the edge of the table. With leads at the neck and feet – treat for adhesions in the cord with 13 / 10. Have the patient bend forward to the edge of pain or stiffness and then go back to neutral. Treat for 60 seconds with 13 / 10. D, E, F: Then have the patient flex the trunk forward again – the range will increase, then return to neutral. Each time the patient flexes forward to the edge of pain, the range should increase. Treat with 13 / 10 for 60 seconds then flex again. Treat for adhesions in the cord until forward flexion is normal and comfortable.
It was hypothesized that this disorientation was the result of central pain amplification that no longer had pain to amplify. The midbrain or thalamus shifts its function in fibromyalgia patients from pain suppression to pain amplification. When the pain is gone the amplification function has no object and the patient feels disoriented. Through trial and error, it was discovered that the protocols for central pain discussed in Chapter 10 would reduce or eliminate this feeling of disorientation.
40 / 89
• Reduce inflammation / in the midbrain.
• Current polarized positive +.
The patient can remain seated for this portion of the protocol with the contacts still at the neck and the feet as they were during the protocol to increase range of motion. Run 40 / 89 until the patient reports having it feel more normal to be out of pain. The shift in the patient's affect can be easily observed. The dazed look clears and the eyes become more focused.

CAUTION: DO NOT run this protocol unless the patient appears disoriented by being pain free. If the patient does NOT have central amplification and the midbrain is performing its normal function of pain suppression, using frequencies to reduce the activity of the midbrain reduces central pain suppression and may cause pain to increase temporarily.
• The 40 / 89 protocol is only effective for central pain amplification.
• Do not use 40 / 89 for other types of pain.
• Do not use 40 / 89 before pain has been reduced to a 1–2/10 VAS by using 40 / 10.
• If use of 40 / 89 increases pain, switch back to 40 / 10 until the pain is reduced or use 81 / 89 for 1 to 2 minutes or until pain is reduced.
40 / 94, 90, 84 Polarized positive + – 1–2 minutes each
• Reduce inflammation / in the medulla, the forebrain and the hindbrain.
• Current polarized positive +.
All parts of the brain are affected by prolonged pain. The medulla frequency is thought to address the entire brainstem including the reticular activating system which alerts the brain to threat. The forebrain modifies judgment to consider the affects of pain and the hindbrain modifies movement and activity to avoid pain. All of these parts of the brain are affected by chronic pain and central pain sensitization. Reduction of central pain amplification appears to be most effective when all parts of the brain are treated.
Address residual neuropathic pain
40, 284, 13 / 396
• Reduce Inflammation / in the nerves.
• Current Polarized positive +.
• Positive contacts at the neck – negative contacts at the hands may be needed to reduce arm pain.
• If patient has developed neuropathic irritation at L3 – place positive leads at low back and negative leads on the thighs.
If the patient does not or cannot place the hands on the abdomen during the treatment the arm pain may not be optimally reduced and may require specific treatment for the cervical dermatomal nerves with 40 / 396. This protocol usually eliminates the arm pain within 10 minutes. See Chapter 3 for details on treating neuropathic pain.
Making recovery possible

The most important thing you need to know about fibromyalgia is that it is curable. Not in every case or in every patient but it can be cured often enough that a cure should be the ultimate goal of therapy.
Practicalities
The long treatment times for this protocol are not possible for most practitioners and it is financially unfeasible for a clinician to spend 90 minutes with one patient. This treatment protocol requires a space for the patient but the patient does not require the clinician to be present after the first 15 minutes as long as the patient has been warned about the possible agitation side effect. The rewards and satisfaction that come with being able to help someone with this condition to become pain free make the time invested well worthwhile.
Treatment interval
There have not been any properly diagnosed patients to date in whom this treatment protocol has not produced pain relief. Patients will finish the treatment with pain levels between 0/10 and 3/10 on a VAS scale regardless of their incoming pain or chronicity.
The patient must be warned that the pain relief is temporary. The pain will return at a reduced level within 2 hours up to 2 weeks following the initial treatment. It is important to tell the patient that the pain relief is temporary: “When the pain comes back it will not be as bad as it was before but you will mind it more because it was gone for a while. There are two parts to pain. One is ‘how much it hurts’ and the other is ‘how much you mind it or how bothersome it is’. The pain will be less intense but you will mind it more.”
It is also important to tell the patient that if the treatment was effective the first time it will always be effective. “If it worked the first time there will never be a time when it doesn't work and it is OK if you don't believe it.” Most patients with fibromyalgia from spine trauma have been in pain for so long and have been disappointed so may times that it is important to give them permission to be skeptical. Central sensitization is still an issue to some extent, even after 40 / 89 has improved the situation. Being out of pain is entirely foreign to the patient and it is going to take time for them to begin to trust that pain relief is possible and even longer for them to expect it as the norm. Repeated in-office treatment is important so that the practitioner can monitor and support the patient through this transition from pain patient to recovering patient.
Second treatment: The second treatment should be scheduled for 1–2 days after the first treatment so that the patient is treated a second time before the pain has had time to return to baseline pretreatment levels. The same procedure should be followed as in the first treatment and the same frequencies should be used. The “concussion protocol” discussed in Chapter 10 should be used once the pain has been reduced.
Follow-up
Subsequent treatments should be scheduled twice or three times a week. It is ideal if the patient's personal finances allow the purchase of a unit for home treatment. The HomeCare (Precision Distributing, Vancouver, Washington) is a preprogrammed automated microcurrent unit that provides the basic 40 / 10 protocol described above by sequencing automatically through the frequency sequences. If a patient has benefited from in-office care the HomeCare will provide the same pain relief and give the patient control of their pain.
The primary requirement for recovery from fibromyalgia is that the patient must keep the pain below a 4/10 level at all times for up to 16 weeks. For some patients this is a matter of four to six in-office treatments in 6 weeks. The neuropathic pain disappears and doesn't return but this is not the norm. Some patients need repeated treatments and using a HomeCare unit is often necessary to achieve this goal, especially if the patient cannot afford two or three in-office treatments per week. Any device can be used that provides microcurrent and delivers 40Hz on channel A and 10Hz on channel B.
It would be convenient if every patient benefited from the same adjunctive therapies for the neuroendocrine and digestive dysfunctions but this is not the case. The same treatment protocol will produce pain relief in every patient and keeping the pain below a 4/10 is the primary requirement for recovery but reducing full body neuropathic pain is only a part of the recovery process. The practitioner will need every skill, experience, intuition and technique acquired in training and practice to produce recovery. Every patient treated to date with the 40 / 10 protocol has had pain relief but only 58% have recovered.
Orthopedic issues
Once the pain and pain amplification are reduced the patient becomes the same as any other orthopedic patient of a similar age discussed in the previous chapters. The injured disc that caused the cord inflammation must be repaired to prevent reoccurrence. If the disc has been separated from the end plate it may never recover and ongoing treatment or even surgery may be required especially if the segment is hypermobile.
Each patient will have unique combinations of orthopedic complaints that must be addressed. Every fibromyalgia patient has myofascial trigger points that will need to be treated. Facet joints, discs, muscles and extremity joints may all need treatment and reconditioning exercises if the patient is to recover full function. The reader is referred to FSM protocols in the preceding chapters for these conditions and to any of the many texts available in the area of spinal and physical rehabilitation. Some patients may require facet joint injections, epidural injections, spinal stabilization exercises and general reconditioning in order to recover.
Regardless of the orthopedic pain generators, if the neuropathic pain can be kept below a 4 / 10 the neuroendocrine system will right itself and the patient can recover from fibromyalgia.
Medication management and withdrawal
Medication management and withdrawal must be addressed if the patient is to achieve recovery.
Opiates and narcotics
Once the FSM protocol has reduced the pain, a patient taking narcotics is automatically over-medicated. Narcotic side effects which were not previously a problem may become problematic in some patients. It is essential that the patient begin reducing narcotic dosages within days or at most a week after the second successful treatment. The patient should trust through experience that the treatment will relieve pain predictably before they are asked to begin reducing pain medication. It is essential that patients taking high doses of opiates not stop their medication abruptly; narcotics withdrawal symptoms are stressful, unpleasant and can be dangerous.
Comprehensive medication management and withdrawal recommendations are beyond the scope of this text. In general, experience suggests that narcotics should be reduced first and that withdrawal should be gradual and adjusted to patient tolerance. FSM will manage the neuropathic cord mediated pain so that the patient doesn't require opiates for pain control but FSM doesn't help withdrawal symptoms. Patients should be warned against abrupt discontinuance of long-standing narcotic medication without medical supervision. It is prudent and completely acceptable to continue to take narcotics simply in order to avoid withdrawal symptoms. Patients may experience a range of withdrawal symptoms including but not limited to increased body pain and flu-like aching, sinus and nasal congestion, emotional agitation or depression, nausea and chills. The patient should continue to treat with FSM at home or in the office to keep the body pain down while physician supervised medication withdrawal is accomplished during the weeks or months required.
Narcotic addiction becomes apparent when the patient stops using FSM at home or in the office, even though it reduces the pain, because taking the medication is easier or provides some comfort beyond pain relief. These cases account for some of the failures of FSM therapy in fibromyalgia recovery. To date, no patient using a fentanyl patch has persisted from pain free to full recovery. Frank conversation, counseling and drug rehabilitation have all been used successfully in a few cases but it is a challenging situation and success depends entirely on the patient's self awareness, motivation and personal support system.
It is important that common sense guide this process. Not every patient on narcotics is addicted or needs to be withdrawn. The case that comes to mind is the 76-year-old patient who had nerve damage in her left foot creating complex regional pain syndrome (CRPS) some 40 years previously. After years on various medications, she had been successfully managed on low dose methadone for 15 years and suffered no side effects from the drug even though her pain was still a 7/10 while taking it. When she became pain free and was able to walk she discontinued the methadone overnight because she felt it was wrong to take it if she had no pain. It caused significant withdrawal reactions. The patient had to be reassured that the practitioner had no judgment about her use of methadone and that it was completely acceptable for her to stay on a lowered dose of medication if only to avoid the stress of withdrawal at her age.
Anti-depressants
Anti-depressants are often used in chronic pain patients to help increase serotonin levels and modulate central sensitization or they may be used because clinicians have found them useful empirically or because the prescribing clinician feels that chronic pain problems are really caused by depression. For whatever reason they have been prescribed, many chronic pain patients will be taking one or more anti-depressants. Once the pain has been reduced, anti-depressants keep the patient from feeling pain but they also blunt all types of emotions. Patients don't feel bad when taking anti-depressants but in general they don't feel anything. Obviously if the patient had a problem with primary depression prior to the onset of pain then an appropriate psychiatric consultation should be performed before modifying anti-depressant medications. Depending on which medication or medications have been prescribed withdrawal may require weeks or months with careful monitoring and gradual reduction. Most but not all patients feel “more like themselves” when they have discontinued anti-depressant medication. Some patients feel best when they remain on a low dose. It is a completely individual response.
Other classes of medications that have been prescribed for various neuroendocrine or digestive symptoms may be withdrawn by the prescribing physician in collaboration with the patient as tolerated. Once the pain has been reduced the perpetuating factor for neuroendocrine and digestive complaints has been eliminated. In general the medications required previously to manage these symptoms will no longer be necessary. But it may take both the physician and the patient some weeks to recognize and act on this. Medication side effects should be evaluated and may become more prominent as the condition improves and the medication has fewer symptoms to control.
Digestive reconditioning
Digestion begins to improve on its own within a few weeks of pain reduction. The changes to digestion brought on by stress begin to resolve but occasionally direct therapeutic intervention will be helpful. This is a cursory review and practitioners are advised to explore the full range of information available on this topic (Galland 1997).
Digestive enzymes and hydrochloric acid are reduced by the stress response. Professional grade nutritional supplements containing digestive enzymes and hydrochloric acid taken just before the meal will help make digestion more comfortable. Proton pump inhibitors being taken for reflux or stomach bloating reduce stomach acid and should be discontinued. Once stomach acid and enzymes return to normal, digestion will improve and reflux should resolve.
Bacterial flora in the gut helps digest food and creates short chain fatty acids that repair the gut wall. The balance of beneficial bacteria and Candida maintained by proper digestive system pH and enzyme function is disrupted by stress. Replacement flora and suppression of excess Candida may help the gut recover more quickly.
Food allergy testing may help identify food intolerances and avoiding dietary allergens can help both the gut and the patient to recover more quickly. Serum allergy testing is more accurate and useful than skin testing which only identifies IgE reactions. Most food intolerances are IgG delayed sensitivities.
FSM can be used to reduce inflammation in the gut and to treat irritable bowel, leaky gut and constipation. These protocols are taught in the FSM Core seminar.
Adrenal rehabilitation
The adrenal glands which produce cortisol among other essential hormones can become depleted after years of sustained stress. Most professional grade nutritional companies provide supplements to assist with adrenal recovery. Some patients who are very depleted and exhausted may benefit from a low dose prescription adrenal replacement such as Cortef (Jeffries 1996).
Pain and stress disturb the normal diurnal rhythm in which we are awake and lively in the morning and quiet and ready for sleep after dark. Fibromyalgia patients are routinely exhausted in the morning and do not begin to feel awake until evening. As the pain and stress decline the normal diurnal rhythm begins to return. Nutritional supplements and herbs to quiet the adrenals may be used in the late afternoon and early evening. Supplements such as licorice root, vitamin B5, and vitamin C and combination supplements for adrenal support may be used in the morning. In the author's experience, glandular supplements or stimulants have never been successful in the long run (Henley 2001).
FSM protocols for adrenal support used in the morning increase salivary cortisol temporarily and seem to enhance adrenal recovery overall. FSM protocols to quiet adrenals may be helpful in quieting the adrenals, restoring diurnal rhythm and improving sleep. These protocols are included in the FSM Core seminar and are beyond the scope of this basic text.
Adrenal function will improve as the pain and stress remain reduced but adrenal rehabilitation may take a few years.
Neurotransmitter reconditioning
If patients are not on anti-depressants and the practitioner has or can acquire knowledge of how to measure, monitor and manipulate neurotransmitters using diet, exercise and selected amino acid and herbal supplements recovery can be enhanced. Neurotransmitters affect mood, sleep and cognitive function.
Physical reconditioning
Once the pain remains below a 4/10 for 2 weeks, on average, the neuroendocrine system begins to right itself. Patients start sleeping better, digesting their food better and begin to see a return of normal diurnal rhythm. They may comment that they are now tired earlier at night and awaken more rested in the morning. Patients begin to tolerate more exercise and may even crave it suggesting that the reduction in pain may lead to a reduction in CRF leading to a corresponding increase in growth hormone. Walking, swimming and gradual reconditioning are the safest way to begin physical rehabilitation and reconditioning. Resistance training should be undertaken gradually if at all, under supervision if possible and only to tolerance. Any activity that causes an increase in symptoms should be avoided. Over head lifting should be avoided because it stresses and compressed the cervical discs. If at all possible a specific program of spinal stabilization should be undertaken to strengthen the muscles in the neck and support and repair the injured disc. The physical reconditioning process may take several months and depending on the patient's age and length of illness may take up to a few years.
Psychological reconditioning
Prior to their first treatment many patients have finally accepted what they have been told by authority figures in white coats and support groups on the internet, “You will be in pain for the rest of your life. Fibromyalgia cannot be cured but you can learn to live with it.” The greatest challenge most patients face when body pain is reduced from a 7/10 to a 0/10 during the first 90-minute treatment is the existential crisis that occurs when they need to answer the question, “Who am I if I am not in pain?” or “Who am I if I am not a pain patient”.
This more than medication management and withdrawal, more than neuroendocrine recovery or reconditioning is the single most common source of treatment failures. Think about it. Who you are, who you think yourself to be, is by and large determined by what you do in our culture. If your activities and lifestyle have been defined by doctor's appointments and pain-limited activities for years and you have now been pain free for 2 weeks, “Who am I now?” is a reasonable question.
Some patients experience unexpected emotions that surprise them such as resentment, anger or grief. Why did I have to suffer? Why didn't I find you sooner? What if it doesn't last? Why couldn't the other doctors help me? I am so sorry my family had to suffer along with me.
Some patients, especially those with a history of early childhood abuse or trauma and those raised in emotionally abusive environments, have internalized the abuse. They have a subconscious belief that they deserve to suffer, that life will always be difficult and painful. Studies show that their neuroendocrine system over reacts to threat and pain. The same stressor will produce a much stronger stress response in an adult abused as a child than it will in an adult raised in a non-abusive environment. Because the response is unconscious, the patient doesn't know that there is another way to be. It can be challenging to present this concept to the patient because it seems so personal. It is important that they not feel as if they have done anything “wrong.”
Telling the story of the research done with baby mice may help because it externalizes the situation. It is easier to see the implications when the story is about mice than when it is personal. Two litters of genetically identical mice, born at the same time are put into two different situations. One litter is allowed to develop in a stress-free environment living in a large cage with adequate food and the comfort of their litter mates and mother. One litter is allowed to develop in the same environment but once a day, as soon as they are physically able to swim, they are placed in a beaker filled with cold water and made to swim for several minutes with no way of escape. This is an incredibly stressful situation for a mouse. After 2 weeks of this daily stressor the mice are left to mature normally in a stress-free environment. Then as adults both groups of mice are taught how to do a maze. Once mice learn a maze the drive to finish the maze and get the reward is very strong. The researchers put a blinking yellow light near the end of the maze. The yellow light, very similar to the yellow of an owl's eye and universally threatening to mice, caused all of the mice to immediately stop their progress along the maze and assess the threat. The stress-free mice considered the threat, saw that it wasn't really an owl and proceeded to the reward at the end of the maze. All of the stressed, cold-water swim mice stopped their progress, over-reacted to the threat and failed to finish the maze.
The early childhood stress had changed the way the brain was hard-wired to react to stress. This may explain why a large percentage of fibromyalgia patients have a history of early childhood abuse or trauma. Patients can usually understand how this applies to their situation.
Fortunately there is a difference between mice and humans in their ability to modify subconscious responses with conscious choices. If a patient is willing to explore this situation, hypnosis, cognitive behavioral therapy, relaxation therapy and mediation may all be helpful. Providing referrals and resources in this area is an important part of recovery.
There is no one answer or approach that will be appropriate for every patient. But in general the following guidelines have been useful:
• Give permission: Acknowledge the emotion by saying “I understand how you feel. You have suffered incredibly and no one really appreciates how much courage it took just to get through each day much less 14 years of days. It makes perfect sense that you would feel like this.”
• Encourage the patient: You may be the one person in the patient's world who believes that recovery is possible. Support realistic expectation. Recovery takes about one month for every year of illness. They need to be patient and track improvements even amidst the setbacks. You are asking that they accept the diagnosis of fibromyalgia but reject the verdict.
• Reframe the experience: “Being ill has taught you a lot. You are different than you were when this started. The years were not ‘wasted’ you were just learning things that you didn't anticipate having to learn. You have learned that people will care for you just as you are, that the world will not end if you cannot clean the house every day or if a 7-year-old has to help you take out the trash, that you have resources around you to do what you have not been able to do, and that you can live within your limits and still have a life. You are wiser than you were when this started. Now, if we are lucky and all goes well, you get to get rid of the pain and keep the wisdom.”
• Living without pain: “As inconvenient, uncomfortable, challenging and difficult as the pain has been it gave you certain benefits. It gave you an excuse not to do things you didn't want to do, go to Aunt Maude's party, clean the house, do certain projects. You found out that the world did not end if you did not do these things. Now that the pain is gone the world will still not end if you do not do these things. You can simply do or not do what you want to do or not do now that you no longer have the pain as a reason. The world will still not end. Find other ways to do for yourself what the pain was doing.”
• During recovery: “Pace yourself. You will have good days and bad days and then better days. Be patient with the process. Pay more attention to the good days and don't over do it. When you have a good day, give yourself permission to do something pleasant just for you. Take time to meet your own needs. If recovery is ahead then the time you spend on yourself is an investment in the future of your health.”
• Every patient will require a different conversation depending on their personality and circumstances.
For the practitioner
A physician told his class of medical students, “It is the physician's job to hold the vision of the patient as healed until the patient can see it for himself.”
Be persistent, positive and determined but never make promises or predictions. Cautious optimism is always safe. Hopeful skepticism is reasonable.
Use objective outcome measures such as the Oswestry functional pain inventory, fibromyalgia impact questionnaire, range of motion, tender point testing by algometer, VAS pain scales and pain diagrams to document patient progress. It is easy for a recovering patient to get engrossed in their current symptoms and forget how much their symptoms have improved. It helps if they can see an objective measure of their improvement.
As you become more adept at treating difficult patients, you will attract more difficult patients. Each chronic pain patient you help knows six patients with similar symptoms or worse. Eventually you will find a patient whose physical, emotional, financial, psychological or spiritual damage is so severe it cannot be repaired in this lifetime. You can still offer the patient compassion and understanding and some palliative care. FSM can be used to provide whatever degree of comfort can be achieved or that the patient will allow.
Treating very difficult emotionally wounded and sometimes demanding patients can be challenging for the practitioner and the staff. Boundaries, compassion and clear communication are important.
You can't want the patient's recovery more than the patient wants it.
Be fully engaged in the process; do not get attached to the outcome.
Case reports
Case #1
The patient was a 53-year-old disabled police officer diagnosed with fibromyalgia 4 years prior to his initial clinic visit. He had been a motorcycle patrolman making a routine traffic stop. Before he could dismount his motorcycle the traffic offender put his car in reverse and hit the officer, knocking him and the motorcycle up onto the sidewalk. The officer slammed into a power pole and fractured both of his forearms as he put them up to protect his face from the impact. He developed full body pain after his third arm surgery and was diagnosed with fibromyalgia several years later.
He was on narcotics, two anti-depressants, acid blockers and sleep medication. His pain level on the first day was rated as a 6–7/10 with the classic cervical trauma fibro pain diagram. His physical examination showed hyperactive patellar reflexes and strong neuropathic pain in the C4, C5 and C6 dermatomes bilaterally. He was treated with 40 / 10 and the concussion protocol (Chapter 10) on the first visit. At the end of the treatment his pain was 0/10. He returned 3 days later with his pain rated as 4–5/10 and reported that he had been pain free for 24 hours. He was treated a second time with 40 / 10 protocol and also treated for myofascial trigger points in the neck and shoulder muscles (see Chapter 7). He was told to reschedule for the following week.
He canceled the next appointment. He returned to the clinic 4 weeks later and said he didn't need treatment but only came to say thank you. He canceled his appointment because he had no pain and he spent the next month withdrawing himself from all of his medications. His pain level was a 2/10 and “I can live – have a life – at a 2/10.”
Case #2
The patient was a 49-year-old woman referred by her management physician because he heard that there was a new treatment available. Her fibromyalgia started with an auto accident 18 years previously. She was on two different pain medications, sleep medication, muscle relaxants and medications for asthma and IBS. She rated her pain on the initial visit as a 7–8/10 with the characteristic pain diagram. She complained of headaches, burning mid-scapular pain, hand, arm, leg, foot, neck and back pain, and jaw pain. She had developed acne, asthma, allergies and irritable bowel syndrome since her fibromyalgia diagnosis.
Her physical examination showed hyperactive patellar reflexes with adductor crossing, sensory hyperesthesia at C3, C4, C5 bilaterally and at C6 on the right. She had 14 out of 18 tender points tender to less than 2 pounds per square inch pressure as measured by algometer.
She was treated with 40 / 10 for the first time on December 8, 2000. Her pain went from a 7/10 to a 0/10. She had 20 in-office treatments between 12/8 and 3/15. She was treated with the cervical trauma fibro protocol and protocols for myofascial trigger points, facet joint pain, disc degeneration, TMJ, irritable bowel syndrome, adrenal support and asthma during her in-office visits. She had a small two channel microcurrent unit (manufactured by Rehabilicare, Minneapolis, MN) that provided 40Hz on one channel and 1Hz on the second channel to use daily at home as needed for pain management. She had 20-minute regional massages and a gentle form of chiropractic adjusting at each visit.
She was referred for physical therapy for spinal stabilization and strengthening, kept her appointments and was compliant with home exercises. She was referred for an epidural steroid injection at C5–C6 on the right and two sets of facet injections in the neck and one facet injection in the low back.
She was prescribed supplements for irritable bowel (digestive enzymes, friendly bacteria and soluble fiber) and adrenal support. She had a wonderful attitude and a supportive family and she declared that while she had fibromyalgia she was not planning on being a fibromyalgia patient forever.
On December 8 she had 14 of 18 tender points tender to less than 2 pounds per square inch pressure. On January 12 she had 11 of 18 tender points tender to four pounds per square inch pressure. On February 8 she had 7 of 18 tender points and no longer met the diagnostic criteria for fibromyalgia. She recovered in 2 months.
Her cervical range of motion improved by 40% and was pain free. Pain medication was reduced by 95% and taken only occasionally. Muscle relaxants were taken occasionally and reduced overall by 95%. She was sleeping well without medication. Her acne resolved when she was given an oil based form of vitamin A on the assumption that she did not convert beta carotene into the active form of vitamin A in her gut. Her digestion improved and the IBS resolved. She and her family were able to retire to their dream home in the Rocky Mountains.
During a follow-up phone call 7 years later she said that she had remained pain free for 6 years until she developed ulcerative colitis after being given antibiotics for an infection. She said her fibromyalgia had returned after surgery but she knew she could get rid of it again by using her home unit. A second follow up some months later revealed that she had done just that.
Adler G., et al. Reduced Hypothalamic-Pituitary and Sympathoadrenal Responses to Hypoglycemia in Women with Fibromyalgia Syndrome. American Journal of Medicine May, 1999.
Baker, Sidney M.D. Detoxification and healing: The key to optimal health. New Canan, CT: Keats Publishing, 1997.
Bennett G.J. Melzak, Wall. Neuropathic Pain: Textbook of Pain. 3rd edition. London: Churchill-Livingstone; 1994:201-224.
Bennett R.M. Emerging concepts in the neurobiology of chronic pain: evidence of abnormal sensory processing in Fibromyalgia. Mayo Clinic Proceedings. 1999;74:385-398.
Bennett R.M., et al. Hypothalamic – pituitary- insulin like growth factor-I axis dysfunction in patients with Fibromyalgia. J. of Rheumatology. 1997;24:1384-1389.
Bendtsen L. Evidence of qualitatively altered nociception in patients with fibromyalgia. Arthritis and Rheumatism. 1998;41:1966-1971.
Bogduk N. The innervation of the cervical intervertebral discs. SPINE. 1988;13:2-8.
Bohlman H. Acute fractures and dislocations of the cervical spine. Journal of Bone and Joint Surgery. 1979;61A:1119-1142.
Busklla D., Neuman L., Valsberg G., Alkalay D., Wolfe F. Increased rates of fibromyalgia following cervical spine injury: a controlled study of 161 cases of traumatic injury. Arthritis and Rheumatism. 1997;40:446-452.
Cavanaugh J.M., Ozaktay A.C., Yamashita T., Avramov A., Getchell T.V., King A.I. Mechanisms of low back pain. Clinical Orthopedics. 1997;335:166-180.
Chen C., Cavanaugh J.M., Ozaktay A.C., Kallakuri S., King A.I. Effects of phospholipase A2 on lumbar nerve root structure and function. SPINE. 1997;22:1057-1064.
Cloward R.B. Cervical discography: Mechanisms of neck, shoulder and arm pain. Annals of Surgery. 1959;150:1052-1064.
Crofford L. Neuroendocrine abnormalities in Fibromyalgia and related disorders, the American Journal of the Medical Sciences. June. 315(6), 1998.
Crofford L.J., Engleberg N.C., Demitrack M.A. Neurohormonal perturbations in Fibromyalgia. Bailliere's Clin Rheumatol. 1996;10:365-378.
Crofford L.J., Demitrack M.A. Evidence that abnormalities of central neurohormonal systems are key to understanding Fibromyalgia and chronic fatigue syndrome. Rheumatology Disease Clinics of North America. 1996;22:267-284.
Dessein et al. Hyposecretion of adrenal androgens and the relation of serum adrenal steroids, serotonin and IgF1 to clinical features in women with Fibromyalgia. Pain. 1999;83:313-319.
Galland, Leo M.D. Four Pillars of Healing. New York, NY: Random House, 1997.
Guyton A.C. Textbook of Medical Physiology. WB Saunders Co: Seventh Edition, 1986.
Henley, Jesse Lynn M.D. Tired of being tired. Berkley Publishing group. Penguin Putnam, Inc; 2001.
Jeffries, William McK M.D. Safe uses of Cortisol, 2nd edition. Springfield, Illinois: Charles Thomas Publisher, Ltd, 1996.
Juhl J. Fibromyalgia and the serotonin Pathway. Alternative Medicine Review. 3(5), 1998.
Kandel E., Schwartz J. Principles of Neural Science, 2nd edition, New York: Elsevier Science Publishing Co., Inc.; 1985:331-336.
Lombard M.C., Larabi Y. Electrophysiological study of cervical dorsal horn cells in partially deafferented rats. Advances in Pain research and Therapy. New York: Raven Press, 1983;147-154.
Maes M., et al. Increased 24-hour urinary cortisol excretion in patients with PTSD and major depression, but not in patients with fibromyalgia. Acta Psychiatr Scand. 1998;98:328-335.
Marshall L.L., Trethewie E.R., Curtain C.C. Chemical radiculitis. A clinical, physiological and immunological study. Clinical Orthopedics. 1997;129:61-67.
McCarron R.F., Wimpee M.W., Hudkins P.G., Laros G.S. The inflammatory effect of nucleus pulposus: A possible element in the pathogenesis of low back pain. SPINE. 1987;12:760-764.
McMakin C. Microcurrent Treatment of Myofascial Pain in the Head, Neck and Face. Topics in Clinical Chiropractic. 1998;5(1):29-35.
McMakin C. Microcurrent therapy: a novel treatment method for chronic low back myofascial pain. Journal of Bodywork and Movement Therapies. 2004;8:143-153.
McMakin C., Gregory W., Phillips T. Cytokine changes with microcurrent treatment of Fibromyalgia associate with cervical spine trauma. Journal of Bodywork and Movement Therapies. 2005;9:169-176.
Mendel T., Wink C.S. Neural elements in cervical intervertebral discs. Anatomic Record. 1989;223:78A.
Moldofsky H., Scaribrik P., England R. Musculoskeletal Symptoms and non-REM Sleep Disturbance in Patients with ‘Fibrositis' Syndrome and Healthy Subjects. Psychosomatic Medicine.. 1975;37:341-351.
Mountz J.M., et al. Fibromyalgia in women: abnormalities of regional cerebral blood flow in the thalamus and the caudate nucleus are associated with low pain thresholds levels. Arthritis Rheum. 1995;38:926-938.
Neeck G., Riedel W. Hormonal Perturbations in Fibromyalgia Syndrome. Annals New York Academy of Sciences, 1999.
Netter F. Atlas of Human Anatomy. Ciba-Geigy, 1991. plate 159
Olmarker K., Rydevik B., Nordberg C. Autologous nucleus pulposus induces neurophysiologic and histologic changes in porcine cauda equina nerve roots. SPINE. 1993;18:1425-1432.
Olmarker K., Blomquist J., Stromberg J., Nannmark U., Thomsen P., Rydevik B. Inflammatogenic properties of nucleus pulposus. SPINE. 1995;20:665-669.
Ozaktay A.C., Cavanaugh J.M., Blagoev D.C. Phospholipase A2 – induced electrophysiologic and histologic changes in rabbit dorsal lumbar spine tissues. SPINE. 1995;20:2659-2668.
Ozaktay A.C., Kallakuri S., Cavanaugh J.M. Phospholipase A2 sensitivity of the dorsal root and dorsal root ganglion. SPINE. 1998;23(12):1297-1306.
Russel I.J., Vipraio G.A., Morgan W.W., Bowden C.L. Is There a Metabolic Basis for the Fibrositis Syndrome. The American Medical Journal.. 1986;81:50-54.
Sapolsky Robert. Why zebras don't get ulcers. New York: WH Freeman and Company, 1994.
Taylor J.R., Twomey L.T. Acute injuries to cervical joints. An autopsy study of neck pain. SPINE. 1993;18(9):1115-1122.
Teitelbaum Jacob, MD. From Fatigued to Fantastic. Inc New York, NY: Penguin Putnam, 2001.