Introduction
Welcome to the world of fascia!
This book is the first comprehensive text in a new field in musculoskeletal therapy and research: the fascinating world of fascia. Fascia forms a continuous tensional network throughout the human body, covering and connecting every single organ, every muscle, and even every nerve or tiny muscle fiber. After several decades of severe neglect, this “Cinderella of orthopedic science” is developing its own identity within medical research. The number of research papers on fascia in peer-reviewed journals has shown a steady rise. The first International Fascia Research Congress, held at the Conference Center, Harvard Medical School in October 2007 was followed by a second in Amsterdam in 2009 and there will shortly be a third in Vancouver in 2012. Similar to the rapidly growing field of glia research in neurology, this underestimated contextual tissue, fascia, is being found to play an important role in health and pathology.
Hypotheses which accord myofascia a central role in the mechanisms of therapies have been advanced for some time in the fields of acupuncture, massage, structural integration, chiropractic and osteopathy. Practitioners in these disciplines, especially those which do not have the longevity of osteopathy or chiropractic, are generally unaware of the scientific basis for evaluating such hypotheses. Many practitioners are unaware of the sophistication of current laboratory research equipment and methods. Laboratory researchers, in turn, may be unaware of the clinical phenomena which suggest avenues of exploration. Thirty years ago the study of physical medicine and rehabilitation included muscle strengthening, anatomy, exercise physiology, and other aspects of therapeutic modalities. What was notably less present in the scientific and medical literature was how to understand and treat disorders of the fascia and connective tissues. Since then much additional information has been developed, particularly since 2005 (see Fig. 0.1).
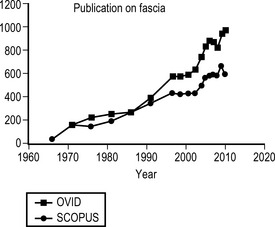
Fig. 0.1 • Number of peer reviewed scientific papers on fascia
• Papers on fascia indexed in Ovid Medline or Scopus have grown from 200 per year in the 1970s and 1980s to almost 1000 in 2010.
The purpose of this book is to organize relevant information for scientists involved in the research of the body's connective tissue matrix (fascia) as well as for professionals involved in the therapeutic manipulation of this body wide structural fabric. While it grew out of materials presented at the First and the Second International Fascia Research Congresses in 2007 and 2009 (www.fasciacongress.org), it reflects the efforts of almost 100 scientists and clinicians.
Not only a packing organ
As every medical student knows and every doctor still remembers, fascia is introduced in anatomy dissection courses as the white packing stuff that one first needs to clean off, in order “to see something”. Similarly, anatomy books have been competing with each other, in how clean and orderly they present the locomotor system, by cutting away the whitish or semitranslucent fascia as completely and skillfully as possible. Students appreciate these appealing graphic simplifications, with shiny red muscles, each attaching to specific skeletal points. However, these simplified maps do not fully describe how the real body feels and behaves, be it in medical surgery or during therapeutic palpation.
To give an example: in real bodies, muscles hardly ever transmit their full force directly via tendons into the skeleton, as is usually suggested by our textbook drawings. They rather distribute a large portion of their contractile or tensional forces onto fascial sheets. These sheets transmit these forces to synergistic as well as antagonistic muscles. Thereby they stiffen not only the respective joint, but may even affect regions several joints further away. The simple questions discussed in musculoskeletal textbooks “which muscles” are participating in a particular movement thus become almost obsolete. Muscles are not functional units, no matter how common this misconception may be. Rather, most muscular movements are generated by many individual motor units, which are distributed over some portions of one muscle, plus other portions of other muscles. The tensional forces of these motor units are then transmitted to a complex network of fascial sheets, bags, and strings that convert them into the final body movement.
Similarly, it has been shown that fascial stiffness and elasticity play a significant role in many ballistic movements of the human body. First discovered by studies of the calf tissues of kangaroos, antelopes, and later by horses, modern ultrasound studies have revealed that fascial recoil plays in fact a similarly impressive role in many of our human movements. How far you can throw a stone, how high you can jump, how long you can run, depends not only on the contraction of your muscle fibers; it also depends to a large degree on how well the elastic recoil properties of your fascial network are supporting these movements.
If the architecture of our fascial network is indeed such an important factor in musculoskeletal behavior, why has this tissue been overlooked for such a long time? There are several answers to this question. The development of new imaging and research tools now allow us to study this tissue in vivo. Another reason is that this tissue resists the classical method of anatomical research: that of splitting something into separate parts that can be counted and named. You can reasonably estimate the number of bones or muscles; yet any attempt to count the number of fasciae in the body will be futile. The fascial body is one large networking organ, with many bags and hundreds of rope-like local densifications, and thousands of pockets within pockets, all interconnected by sturdy septa as well as by looser connective tissue layers.
What is fascia?
This varied nature of fascia is reflected in the many different definitions of which exact tissue types are included under the term “fascia”. The International Anatomical Nomenclature Committee (1983) confirmed the usage of previous nomenclature committees and used the term “fascia superficialis” for the loose layer of subcutaneous tissue lying superficial to the denser layer of “fascia profunda.” While most medical authors in English-speaking countries followed that terminology, it was not congruently adopted by authors in other countries. The nomenclature proposed by the Federative Committee on Anatomical Terminology (1998), therefore attempted to lead towards a more uniform international language (Wendell-Smith 1997). It suggested that authors should no longer use the term fascia for loose connective tissue layers, such as the former “superficial fascia”, and to apply it only for denser connective tissue aggregations. However, this attempt failed significantly (Huijing & Langevin 2009). Most English textbook authorities continued to use the term “superficial fascia” to describe subcutaneous tissues (Standring 2008). In addition an increasing number of non-English authors – following the common Anglo-Saxon trend in international medicine – have started to adopt the same terminology as these American or British colleagues.
Similarly there has been confusion on the question which of the three hierarchical muscular tissue bags – epi-, peri- and endomysium – could be included as fascia. While most authors would agree to consider as fascial tissues, muscular septi and the perimysium (which is often quite dense, particularly in tonic muscles) there is less consensus on the endomysial envelopes around single muscle fibers, based on their much looser density and higher quantity of collagen types III and IV. However, almost all authors emphasize the important continuity of these intramuscular connective tissues, and this continuity was shown extending even within the muscle cell (Purslow 2009). So where does fascia stop?
Another area, still to be resolved, are the visceral connective tissues. For some authors the term fascia is restricted to muscular connective tissues. Visceral connective tissues – no matter whether they are of loose composition like the major omentum or more ligamentous like the mediastinum – are often excluded. In contrast, more clinically oriented books have placed a lot of emphasis on the visceral fasciae (Paoletti 2006, Schwind 2006).
As valuable as these proposed anatomical distinctions within soft connective tissues are, their very detail may lead to unwitting exclusion of important tissue continuities which are only perceived on the larger scale. For example, the clinical significance of the continuity of the fascia of the scalene muscles of the neck with the pericardium and mediastinum inside the thorax is often surprising in our discussions with orthopedic surgeons, although less so to osteopaths or general surgeons. Figure 0.2 shows another example of perceptual tissue exclusion, based on terminological distinction. Here one of the sturdiest portions of the iliotibial tract has been excluded from this important tissue band, since it did not fit the distinct nomenclature defined by the authors of this paper.

Fig. 0.2 • Example of a fascia dissection based on specific terminology
• This dissection was used in an otherwise excellent treatise on the iliotibial tract (ITT). Following the proposal of the Federative Committee on Anatomical Terminology (1998) to distinguish between aponeuroses and fasciae, the authors chose to describe this tissue as an aponeurosis. Congruently with this decision, their dissection and illustration therefore excluded all tissue portions with a non aponeurotic character. Unfortunately this included one of the most dense and most important portions of the iliotibial tract: the connection to the lateral iliac crest, posterior of the anterior superior iliac spine. Notice the common thickening of the iliac crest at the former attachment of this ligamentous portion (located at a straight force transmission line from the knee over the greater trochanter), reflecting the very strong pull of this tissue portion on the pelvis. (TFL: tensor fascia lata.) Illustration taken with permission from Benjamin et al 2008)
Based on this background a more encompassing definition of the term fascia was recently proposed as a basis for the first Fascia Research Congress (Findley & Schleip 2007) and was further developed (Huijing & Langevin 2009) for the following congresses. The term fascia here describes the ‘soft tissue component of the connective tissue system that permeates the human body’. One could also describe these as fibrous collagenous tissues which are part of a bodywide tensional force transmission system. This view of an interconnected tensional network is partly inspired by the tensegrity concept, as described in Chapter 3.5. The complete fascial net then includes not only dense planar tissue sheets (like septa, joint capsules, aponeuroses, organ capsules, or retinacula), which may also be called “proper fascia”, but it also encompasses local densifications of this network in the form of ligaments and tendons. Additionally it includes softer collagenous connective tissues like the superficial fascia or the innermost intramuscular layer of the endomysium. The cutis, a derivative of the ectoderm, as well as cartilage and bones are not included as parts of the fascial tensional network. However, the term fascia now includes the dura mater, the periosteum, perineurium, the fibrous capsular layer of vertebral discs, organ capsules as well as bronchial connective tissue and the mesentery of the abdomen (Fig. 0.3).
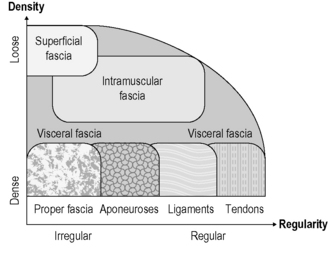
Fig. 0.3 • Different connective tissues considered here as fascial tissues
• Fascial tissues differ in terms of their density and directional alignment of collagen fibers. For example, superficial fascia is characterized by a loose density and a mostly multidirectional or irregular fiber alignment; whereas in the denser tendons or ligaments the fibers are mostly unidirectional. Note that the intramuscular fasciae – septi, perimysium and endomysium – may express varying degrees of directionality and density. The same is true – although to a much larger degree – for the visceral fasciae (including soft tissues like the omentum majus and tougher sheets like the pericardium). Depending on local loading history, proper fasciae can express a two-directional or multidirectional arrangement. Not shown here are retinaculae and joint capsules, whose local properties may vary between those of ligaments, aponeuroses and proper fasciae.
This more encompassing terminology offers many important advantages for the field. Rather than having to draw most often arbitrary demarcation lines between joint capsules and their intimately involved ligaments and tendons (as well as interconnected aponeuroses, retinacula and intramuscular fasciae), fascial tissues are seen as one interconnected tensional network that adapts its fiber arrangement and density according to local tensional demands. This terminology fits nicely to the Latin root of the term “fascia” (bundle, strap, bandage, binding together). It is also synonymous with the non-professional's understanding of the term “connective tissue”. “Connective tissue research” is too broad a term, as this includes bones, cartilage and even blood or lymph, all of which are derivatives of the embryologic mesenchyme. In addition, the contemporary field of ‘connective tissue research’ has shifted its primary focus to tiny molecular dynamics from the macroscopic considerations of several decades ago. The newly forming field of fascia research requires both macroscopic and microscopic investigations. This text has undertaken the task of serving both areas. Even if sometimes microscopic details of collagenous tissues are explored, an effort will be made to always relate these findings to the body as a whole.
While we see great advantages in our wider definition of fascial tissues, we acknowledge that more traditionally oriented authors will continue to restrict the term fascia to dense planar layers of “irregular” connective tissues, in distinction from more regular oriented tissues like aponeuroses or ligaments. In some areas such a distinction is indeed possible and may be clinically useful (e.g. at the fasciae and aponeuroses of the lumbar region). We therefore suggest including twelve additional specifying terms wherever possible, into the detailed description of a fascial tissue. These specifying terms were proposed by Huijing & Langevin (2009): dense connective tissue, areolar connective tissue, superficial fascia, deep fascia, intermuscular septa, interosseal membrane, periost, neurovascular tract, epimysium, intra- and extramuscular aponeurosis, endomysium. However, we also note that many important areas of the body are characterized by gradual transitions between such morphological categories, and a more geometrical description of local collagen architecture (in terms of dominant fiber directions, tissue thickness and density) may then be more useful to understanding specific tissue properties (see Fig. 0.2).
This textbook, as have the fascia congresses, has taken the difficult role of being oriented toward both the scientist and the clinician. Material presented spans anatomy and physiology of fascia in Part 1, through clinical conditions and therapies in Part 2, to recently developed research techniques in Part 3. We have pointed out the definitional struggles the researcher faces surrounding fascia: Which tissue? What fiber directions? What is connected to what? These research tools will allow the extension of this debate to more clinical areas as well, to help define which tissues are affected and what directions forces are applied in the clinical therapies. It is our hope that clinicians and scientists, both together and separately, will rise to these challenges to advance our basic understanding and our clinical treatment of fascia.
References
Benjamin M., Kaiser E., Milz S. Structure–function relationships in tendons: a review. J. Anat.. 2008;212:211–228.
Federative Committee on Anatomical Terminology. Terminologia Anatomica. Stuttgart: Thieme; 1998.
Findley T.W., Schleip R. Fascia research: basic science and implications for conventional and complementary health care. Munich: Elsevier Urban & Fischer; 2007.
Huijing P.D., Langevin H.M. Communicating about fascia: history, pitfalls and recommendations. International Journal of Therapeutic Massage and Bodywork. 2009;2(4):3–8.
International Anatomical Nomenclature Committee. Nomina Anatomica, fifth ed. Baltimore: Williams & Wilkins; 1983.
Paoletti S. The fasciae: anatomy, dysfunction and treatment. Seattle: Eastland Press; 2006.
Purslow P. The structure and functional significance of variations in the connective tissue within muscle. In: Huijing P.A., Hollander P., Findley T.W., Schleip R., eds. Fascia research II: basic science and implications for conventional and complimentary health care. Munich: Elsevier Urban & Fischer, 2009.
Schwind P. Fascial and membrane technique: a manual for comprehensive treatment of the connective tissue system. Edinburgh: Elsevier, 2006.
Standring S., ed. Gray's anatomy – the anatomical basis of clinical practice, fortieth ed, Edinburgh: Elsevier, 2008.
Wendell-Smith C.P. Fascia: an illustrative problem in international terminology. Surg. Radiol. Anat.. 1997;19:273–277.