CHAPTER 66 Small intestine
OVERVIEW
The small intestine consists of the duodenum, jejunum and ileum. It extends from the distal end of the pyloric canal to the ileocaecal valve, an overall length of 5 metres (3–7 metres) in the living adult. The duodenum extends up to the duodenojejunal junction, and the remaining small intestine is often referred to as the ‘small bowel’, of which the proximal two-fifths is referred to as the jejunum and the distal three-fifths as the ileum. There is no clear distinction between the two parts, but there is a gradual change in morphology from the proximal to distal ends of the small bowel. The distal 30 cm or so of the ileum is often referred to as the terminal ileum, which has some specialized physiological functions.
The duodenum lies mostly in the upper retroperitoneum. The jejunum and ileum occupy the central and lower parts of the abdominal cavity and usually lie within the boundary formed by the abdominal colon; they are attached to the posterior abdominal wall by a mesentery which allows considerable mobility of the loops of small bowel. In the supine position, loops of jejunum may be found anterior to the transverse colon, stomach and even lesser omentum, whereas in the upright position, loops of ileum may descend into the pelvis anterior to the rectum and, in women, may occupy the rectouterine pouch. The upper jejunum and some ileum are often covered anteriorly by the greater omentum. The jejunum and ileum are covered by peritoneum on all but their mesenteric borders, here the adipose connective tissue of the mesentery abuts the muscular wall. The serosal peritoneum is continuous with the peritoneum enclosing the tissues of the mesentery. Mesenteric fat covers 20% of the circumference wall of the ileum and somewhat less of the jejunum.
DUODENUM
The adult duodenum is 20–25 cm long and is the shortest, widest and most predictably placed part of the small intestine. It is only partially covered by peritoneum, although the extent of the peritoneal covering varies along its length: the proximal 2.5 cm is intraperitoneal, and the remainder is retroperitoneal. The duodenum forms an elongated ‘C’ that lies between the level of the first and third lumbar vertebrae in the supine position. The lower ‘limb’ of the C extends further to the left of the midline than the upper limb. The head and uncinate process of the pancreas lie within the concavity of the duodenum which is ‘draped’ over the prominence formed from the lumbar spine, the duodenum therefore bends in an antero-posterior direction as well as following the form of a ‘C’. The duodenum lies entirely above the level of the umbilicus and is described as having four parts (Figs 66.1, 66.2).
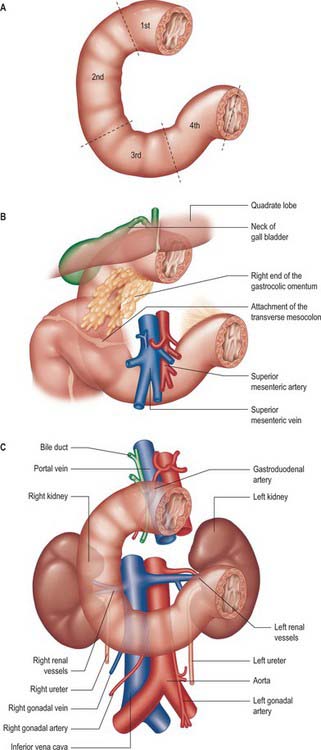
Fig. 66.1 A, The four parts of the duodenum. B&C, The relations of the duodenum: B, anterior surface; C, posterior surface.

Fig. 66.2 Contrast radiographic appearance of the duodenum showing a distended duodenal cap and the remainder of the duodenum up to the duodenojejunal flexure.
FIRST (SUPERIOR) PART
The first, and most mobile, part of the duodenum is about 5 cm long. It starts as a continuation of the duodenal end of the pylorus and ends at the superior duodenal flexure. Peritoneum covers the anterior and superior part of its posterior aspect close to the pylorus, where the duodenum forms part of the anterior wall of the epiploic foramen. Here the lesser omentum is attached to its upper border and the greater omentum to its lower border. The first 2 or 3 cm have a bland internal mucosal appearance and readily distend on insufflation during endoscopy. This part is frequently referred to as the duodenal ‘cap’. It has a triangular, homogeneous appearance during contrast radiology, shows the same pattern of internal rugae as the pylorus, and is often visible on plain radiographs of the abdomen as an isolated triangular gas shadow to the right of the first or second lumbar vertebra. The duodenum next passes superiorly, posteriorly and laterally for 5 cm before curving sharply inferiorly into the superior duodenal flexure: it rapidly becomes more retroperitoneal during this part of its course, until peritoneum only covers its anterior aspect. From the end of the duodenal cap, its internal appearance is characterized by extensive, deep mucosal folds that involve up to half of the circumference of the lumen. Even during endoscopic insufflation, these folds are pronounced (Fig. 66.3) and they are readily seen on contrast radiographs. The section from the duodenal cap to the superior duodenal flexure lies posterior and inferior to the quadrate lobe of the liver.
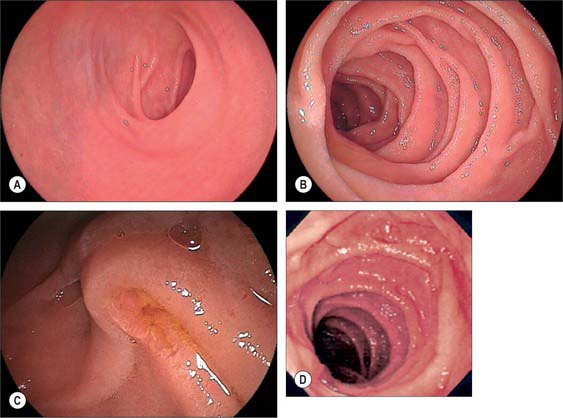
Fig. 66.3 Endoscopic appearance of the duodenum: A, Duodenal cap (first part). B, Second part showing the pronounced, ‘branched’ mucosal folds. C, Major duodenal papilla. D, Third part.
The first part of the duodenum lies anterior to the gastroduodenal artery, common bile duct and portal vein and anterosuperior to the head and neck of the pancreas. It is posterior to the neck of the gallbladder. The gastroduodenal artery lies immediately posterior to the posterior wall of the duodenum: penetrating peptic ulceration in the posterior wall and subsequent erosion of the gastroduodenal artery may lead to dramatic haemorrhage. Penetrating peptic ulceration in the anterior wall may lead to free perforation into the peritoneal cavity because the anterior surface of the first part is covered only by peritoneum.
The common hepatic and hepatoduodenal lymph nodes lie close to the first part of the duodenum and can be visualized using endoscopic ultrasound. This may be important in the staging of gastric, pancreatic or bile duct tumours. The proximity of the common bile duct to the first part of the duodenum allows endoscopic ultrasound examination of the distal common bile duct and the formation of a surgical anastomosis between bile duct and duodenum (choledochoduodenostomy) when required.
The junction of the first and second parts of the duodenum lies posterior to the neck of the gallbladder.
SECOND (DESCENDING) PART
The second part of the duodenum is 8–10 cm long. It starts at the superior duodenal flexure and runs inferiorly in a gentle curve, convex to the right side of the vertebral column and extending to the lower border of the third lumbar vertebral body. It then turns sharply medially into the inferior duodenal flexure which marks its junction with the third part of the duodenum. It is covered by peritoneum only on its upper anterior surface, lies posterior to the neck of the gallbladder and the right lobe of the liver at its start, and is crossed anteriorly by the transverse colon. The medial end of the gastrocolic omentum and the origin of the transverse mesocolon are attached to the anterior surface of the duodenum by loose connective tissue. Below the attachment of the transverse mesocolon, the connective tissue and vessels forming the mesentery of the upper ascending colon and hepatic flexure are loosely attached to its anterior surface. This section of duodenum is at risk of injury during surgical mobilization of the ascending colon.
The second part lies anterior to the hilum of the right kidney, the right renal vessels, the edge of the inferior vena cava and the right psoas major. The head of the pancreas and the common bile duct are medial and the hepatic flexure is above and lateral. A small part of the pancreatic head is sometimes embedded in the medial duodenal wall, and pancreatic ‘rests’ in the duodenal wall may produce small filling defects on contrast radiology. The internal appearance is similar to that of the distal portion of the first part of the duodenum, with pronounced mucosal folds (Fig. 66.3). The common bile duct and pancreatic duct enter the medial wall obliquely and usually unite to form the common hepatopancreatic ampulla. The narrow distal end opens on the summit of the major duodenal papilla (ampulla of Vater), which is situated on the posteromedial wall of the second part, 8–10 cm distal to the pylorus. There are variants of the ductal anatomy. The most common is a second, accessory pancreatic duct which may open 2 cm above the major papilla on a minor duodenal papilla. Peptic ulceration of the second part of the duodenum is less common than that of the first part, and tends to occur on the anterior or lateral wall.
Duodenal diverticula
The duodenum is the most common site for a diverticulum in the small intestine. Diverticula are congenital and usually solitary. They almost always arise in the medial wall of the second part of the duodenum, intimately related to the head of the pancreas, such that the major duodenal papilla may frequently be found either on the mucosal fold at the mouth of a diverticulum or arising from the mucosa within the body of a diverticulum, particularly on the superomedial wall. This may complicate interpretation of contrast radiographs of the duodenum or biliary system, and may cause difficulties during attempted endoscopic cannulation of the papilla because the diverticulum may restrict access. If the papilla is located on or close to the anterior wall of a diverticulum, the procedure of opening the ampulla with an electrocautery current during attempted cannulation (sphincterotomy) is made more hazardous because the wall is thin at this point and so there is a risk of free perforation into the peritoneal cavity.
THIRD (HORIZONTAL) PART
The third part of the duodenum starts at the inferior duodenal flexure and is approximately 10 cm long. It runs from the right side of the lower border of the third lumbar vertebra, angled slightly superiorly, across to the left, anterior to the inferior vena cava, becoming continuous with the fourth part in front of the abdominal aorta. It lies posterior to the transverse mesocolon, the origin of the small bowel mesentery and the superior mesenteric vessels. The lower portion of its anterior aspect is covered by peritoneum which is reflected anteriorly to form the posterior layer of the origin of the small bowel mesentery. The anterior surface of the left lateral end, close to the junction with the fourth part, is also covered with peritoneum.
The third part is anterior to the right ureter, right psoas major, right gonadal vessels, inferior vena cava and abdominal aorta (at the origin of the inferior mesenteric artery), and inferior to the head of the pancreas. Anteroinferiorly, loops of jejunum lie in the right and left infracolic compartments. The mid portion of the third part lies in the angle between the superior mesenteric vessels, just below their origin, anteriorly, and the abdominal aorta posteriorly: very rarely, this arrangement is associated with intermittent symptoms of obstruction of the duodenum at this point.
FOURTH (ASCENDING) PART
The fourth part of the duodenum is 2.5 cm long. It starts just to the left of the aorta, runs superiorly and laterally to the level of the upper border of the second lumbar vertebra, then turns sharply anteroinferiorly at the duodenojejunal flexure to become continuous with the jejunum. The main trunk of the inferior mesenteric vein lies either posterior to the duodenojejunal flexure or beneath the adjacent peritoneal fold. (The duodenojejunal flexure is a useful landmark to locate the vein radiologically or surgically.) The aorta, left sympathetic trunk, left psoas major, left renal and left gonadal vessels are all posterior relations, the left kidney and left ureter are posterolateral, and the upper part of the root of the small bowel mesentery, the left lateral transverse mesocolon and transverse colon, which separate it from the stomach, are anterior. The peritoneum of the root of the small bowel mesentery continues over its anterior surface. The lower border of the body of the pancreas is superior.
At its left lateral end, the fourth part becomes progressively covered in peritoneum on its superior and inferior surfaces, such that it is suspended from the retroperitoneum by a double fold of peritoneum, the ligament of Treitz, at the start of the duodenojejunal flexure. The ligament of Treitz may contain a small slip of muscle, the suspensory muscle of the duodenum. When present, the suspensory muscle contains skeletal muscle fibres that run from the left crus of the diaphragm to connective tissue around the coeliac axis, and smooth muscle fibres that run from the coeliac axis: its function is unknown. It is an important landmark in the radiological diagnosis of incomplete rotation and malrotation of the small intestine (see Ch. 73). The ligament of Treitz does not form part of the duodenal mesentery because the vascular supply to the fourth part of the duodenum continues to enter its wall from the posteromedial aspect.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
Arteries
The main vessels supplying the duodenum are the superior and inferior pancreaticoduodenal arteries. The first and second parts also receive contributions from several sources including the right gastric, supraduodenal, right gastroepiploic, hepatic and gastroduodenal arteries. Branches of the superior pancreaticoduodenal artery may contribute to the supply of the pyloric canal, with a minor degree of anastomosis to the gastric arteries in the muscular layer across the pyloroduodenal junction (Fig. 66.4).
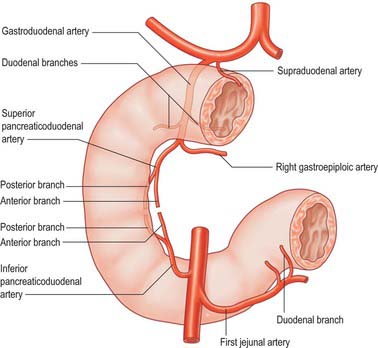
Fig. 66.4 The arterial supply of the duodenum. Only representative branches of the small vessels, which may be multiple, are shown.
Gastroduodenal artery
The gastroduodenal artery usually arises from the common hepatic artery behind, or sometimes above, the first part of the duodenum. It descends between the first part of the duodenum and the neck of the pancreas, immediately to the right of the peritoneal reflection from the posterior surface of the duodenum. It usually lies to the left of the common bile duct but occasionally is anterior. At the lower border of the first part of the duodenum it divides into the right gastroepiploic and superior pancreaticoduodenal arteries. Before its division, the lowest part of the artery gives rise to small branches that supply the pyloric end of the stomach and the pancreas, and retroduodenal branches that supply the first part and the proximal portion of the second part of the duodenum directly. Although the gastroduodenal artery usually branches from the common hepatic artery, it may also arise as a trifurcation with the right and left hepatic arteries, or from the superior mesenteric artery or the left hepatic artery (occasionally), or from the coeliac axis or right hepatic artery (rarely).
The supraduodenal artery often arises from the gastroduodenal artery behind the upper border of the first part of the duodenum and supplies the superior aspect of the first part; it may occasionally arise from the common hepatic artery or right gastric artery. Because of its close relationship to the posteromedial wall of the second part of the duodenum, deeply penetrating ulcers or tumours of the duodenum may cause torrential bleeding from the gastroduodenal ‘artery of haemorrhage’, not least because of the profuse arterial network in the region ensures a high flow rate in the vessel.
Superior pancreaticoduodenal arteries
The superior pancreaticoduodenal artery is usually double. The anterior artery is a terminal branch of the gastroduodenal artery and descends in the anterior groove between the second part of the duodenum and the head of the pancreas. It supplies branches to the first and second parts of the duodenum and to the head of the pancreas, and anastomoses with the anterior division of the inferior pancreaticoduodenal artery. The posterior artery is usually a separate branch of the gastroduodenal artery and is given off at the upper border of the first part of the duodenum. It descends to the right, anterior to the portal vein and common bile duct as the latter lies behind the first part of the duodenum. It then runs behind the head of the pancreas, crosses posterior to the common bile duct (which is embedded in the head of the pancreas), enters the duodenal wall and anastomoses with the posterior division of the inferior pancreaticoduodenal artery. The posterior artery supplies branches to the head of the pancreas, the first and second parts of the duodenum, and several branches to the lowest part of the common bile duct.
Inferior pancreaticoduodenal artery
The inferior pancreaticoduodenal artery usually arises from the superior mesenteric artery or its first jejunal branch, near the superior border of the third part of the duodenum. It crosses behind the superior mesenteric vein and divides directly into anterior and posterior branches. The anterior branch passes to the right, anterior to the lower border of the head of the pancreas, and runs superiorly to anastomose with the anterior superior pancreaticoduodenal artery. The posterior branch runs posteriorly and superiorly to the right, lying posterior to the lower border of the head of the pancreas, and anastomoses with the posterior superior pancreaticoduodenal artery. Both branches supply the pancreatic head, its uncinate process and the second and third parts of the duodenum. Occasionally the anterior and posterior branches arise separately from the superior mesenteric or first jejunal artery.
Jejunal artery branches
Branches from the first jejunal branch of the superior mesenteric artery supply the fourth part of the duodenum and frequently form an anastomosis with the terminal branch of the anterior inferior pancreaticoduodenal artery (which arises from the superior mesenteric artery). The fourth part of the duodenum therefore receives a potential collateral supply from the coeliac axis and superior mesenteric artery, which means that it is not commonly affected by ischaemia.
Veins
The duodenal veins drain ultimately into the portal vein. Submucosal and intramural veins give rise to pancreaticoduodenal veins that usually accompany the corresponding named arteries. The superior pancreaticoduodenal vein is formed medial to the mid point of the second part of the duodenum. It runs superomedially on the posterior surface of the head of the pancreas, passes posterior to the distal common bile duct and drains into the portal vein behind the neck of the pancreas. The inferior pancreaticoduodenal vein runs from the anteromedial aspect of the second part of the duodenum inferiorly in the groove between the second and third parts of the duodenum and the head of the pancreas. It usually drains into the superior mesenteric vein but may drain into the right gastroepiploic vein. Small veins from the first and upper second part of the duodenum may drain into the prepyloric vein and veins from the third and fourth parts may drain directly into the superior mesenteric vein.
Lymphatics
Duodenal lymphatics run to anterior and posterior pancreatic nodes that lie in the anterior and posterior grooves between the head of the pancreas and the duodenum: these nodes drain widely into the supra-pyloric, infrapyloric, hepatoduodenal, common hepatic and superior mesenteric nodes.
INNERVATION
The duodenum is innervated by both parasympathetic and sympathetic neurones.
Preganglionic sympathetic axons originate from neurones in the intermediolateral columns of the grey matter in the fifth to the 12th thoracic spinal segments. They travel via the greater and lesser splanchnic nerves to the coeliac plexus where they synapse on neurones in the coeliac ganglion: postganglionic axons are distributed to the duodenal wall via periarterial plexuses on the branches of the coeliac axis and superior mesenteric artery. The sympathetic nerves are vasoconstrictor to the duodenal vasculature and inhibitory to duodenal musculature.
The preganglionic parasympathetic supply is carried by vagal axons that are distributed via the coeliac plexus and which synapse on neurones in the duodenal wall. The parasympathetic supply is secretomotor to the duodenal mucosa and motor to the duodenal musculature. The sympathetic nerves are vasoconstrictor to the duodenal vasculature and inhibitory to duodenal musculature.
JEJUNUM
The jejunum has a median external diameter of 4 cm and an internal diameter of 2.5 cm. It has a thicker wall than the ileum, and an extensive arterial blood supply that makes it appear redder than the ileum in the living. The plicae circulares are most pronounced in the proximal jejunum, where they are more numerous and deeper than elsewhere in the small bowel (Fig. 66.5A). They frequently ‘branch’ around the lumen and may appear to be ranged one on top of another, giving the jejunum a characteristic appearance during single contrast radiography (Fig. 66.6). Lymphoid aggregates are almost absent from the proximal jejunum, but are present distally, although they are fewer in number and smaller than in the ileum. Where present, they are usually discoid in shape and impalpable.
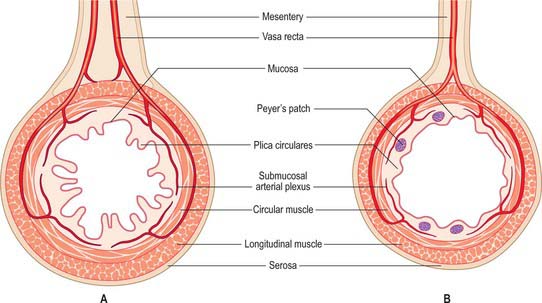
Fig. 66.5 Typical cross sections through the proximal jejunum (A) and terminal ileum (B). The mesenteric attachment is wider in the jejunum, and two leaves of vessels enter the bowel wall. The latter is also thicker in the jejunum.
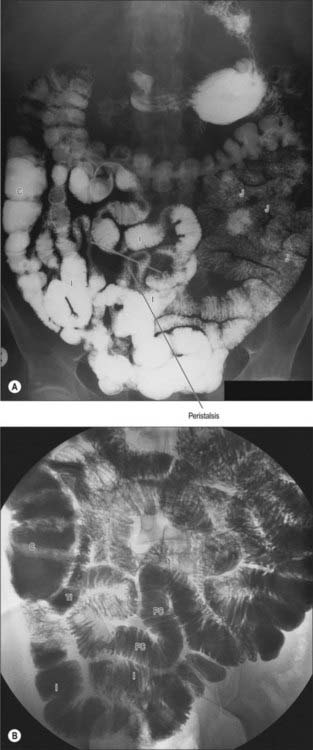
Fig. 66.6 Barium studies of the jejunum and ileum. A, Barium follow-through. The feathery appearance of the small intestine is due to the plicae circulares and is most prominent in the jejunum. The constrictions are the result of peristalsis. B, Small bowel enema (enteroclysis). The plicae circulares are clearly demonstrated by this technique. C, caecum; I, ileum; J, jejunum; PC, plicae circulares; TI, terminal part of ileum.
In the supine position the jejunum usually occupies the upper left infracolic compartment, extending down to the umbilical region. The first one or two loops often occupy a recess between the left part of the transverse mesocolon and the left kidney. On supine radiological examination, the jejunal loops are characteristically situated in the upper abdomen, to the left of the midline, whereas the ileal loops tend to lie in the lower right part of the abdomen and pelvis. This distribution can be reversed during paralytic ileus or small bowel obstruction due to rotation around the mesenteric attachment following bowel distension.
In situations where the stomach and duodenum are either unsuitable or unavailable for receiving oral nutrition, delivery of prepared feed to the jejunum is possible using either a surgically created jejunostomy or by insertion of a feeding tube. Because the jejunum is highly mobile, it is possible to bring the first or second loop of jejunum into contact with the abdominal wall to create a surgical jejunostomy. Insertion of a fine-bore feeding tube via the nose as far as the jejunum is also possible: the end of the feeding tube must lie beyond the duodenojejunal flexure to prevent reflux of the feed into the duodenum and stomach, and this is usually confirmed by radiological monitoring of the progress of the tube through the duodenum.
ILEUM
The ileum has a median external diameter of 3.5 cm and an internal diameter of 2 cm, and tends to have a thinner wall than the jejunum (Fig. 66.5B). The plicae circulares become progressively less obvious in the distal mucosa in the ileum; they tend to be single and flatter with less pronounced crests (Figs 66.6, 66.7), and the mucosa of the terminal ileum immediately proximal to the ileocaecal valve may appear almost flat. Lymphoid aggregates are larger and more numerous than in the jejunum and may be easily palpable in the terminal ileum. They are most prominent in early childhood and, when enlarged in viral infections, may form the apex of an ileo-ileal intussusception. They become less prominent prior to puberty, and attain adult morphology by late teenage years. In the supine position, the ileum lies mainly in the hypogastric region and right iliac fossa. The terminal ileum frequently lies in the pelvis, whence it ascends over the right psoas major and right iliac vessels, to end by opening into the ileocaecal valve in the right iliac fossa.
An ileal diverticulum (of Meckel) exists in 3% of adults and represents the remnant of the proximal part of the intestino-vitelline duct. It projects from the antimesenteric border of the terminal ileum and is commonly located between 50 and 100 cm from the ileocaecal valve. It is variable in length (median 5 cm), often possessing a short ‘mesentery’ of adipose tissue that extends from the ileal mesentery up to its base. The lumen of the diverticulum usually has a calibre similar to that of the ileum. The tip is normally free but occasionally it may be connected to the anterior abdominal wall near the umbilicus by a fibrous band. The mucosa is typically ileal, but small heterotopic areas of gastric body type epithelium, pancreatic, colonic or other tissues may also occur in the wall of a diverticulum. Unopposed acid secretion by heterotopic gastric body type epithelium may occasionally give rise to bleeding in the adjacent normal ileal mucosa. Diverticular inflammation may mimic acute appendicitis; since Meckel’s diverticulum and the appendix are both derived from midgut structures, pain from either structure is referred to the periumbilical region.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
Arteries
Branches from the superior mesenteric artery supply the jejunum and ileum. The arteries divide as they approach the mesenteric border, giving off numerous branches which extend between the serosal and muscular layers, supplying the muscle and forming an intricate sub-mucosal plexus that supplies the glands and villi. Although there is a profuse anastomotic network of arteries within the mesentery, anastomoses between the terminal branches close to the intestinal wall are few (Fig. 66.8). The intramural and submucosal arterial networks are not of large calibre, which means that flow along lengths of small bowel is limited to a few centimetres, and division or occlusion of several consecutive vasa recta may produce segmental, focal ischaemia. Division of more proximal vessels allows flow to continue in the arcades for moderately long lengths of intestine.
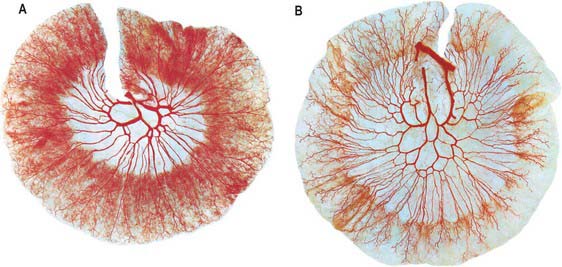
Fig. 66.8 Specimens of the jejunum (A) and ileum (B) from a cadaver where the superior mesenteric artery was injected with a red coloured mass of gelatin before fixation. Subsequently the specimens were dehydrated and then cleared in benzene followed by methyl salicylate. The largest vessels present are the jejunal and ileal branches of the superior mesenteric artery and these are succeeded by anastomotic arterial arcades, which are relatively few in number (1–3) in the jejunum, becoming more numerous (5–6) in the ileum. From the arcades, straight arteries pass towards the gut wall; frequently, successive straight arteries are distributed to opposite sides of the gut. Note the denser vascularity of the jejunal wall.
(Specimens prepared by MCE Hutchinson; photographs by Kevin Fitzpatrick on behalf of GKT School of Medicine, London.)
Superior mesenteric artery
The superior mesenteric artery originates from the aorta 1 cm below the coeliac trunk, at the level of the intervertebral disk between the first and second lumbar vertebrae (Figs 66.9, 66.10). The angle of its origin from the aorta is acute, which makes cannulation via the transfemoral route somewhat difficult. The artery runs inferiorly and anteriorly, anterior to the uncinate process of the pancreas and the third part of the duodenum, and posterior to the splenic vein and the body of the pancreas. The left renal vein lies behind it and separates it from the aorta (Fig. 66.11). The artery crosses anterior to the inferior vena cava, right ureter and right psoas major as it descends in the root of the small bowel mesentery. Its calibre progressively decreases as successive branches are given off to loops of jejunum and ileum, and its terminal branch anastomoses with the ileocolic artery.
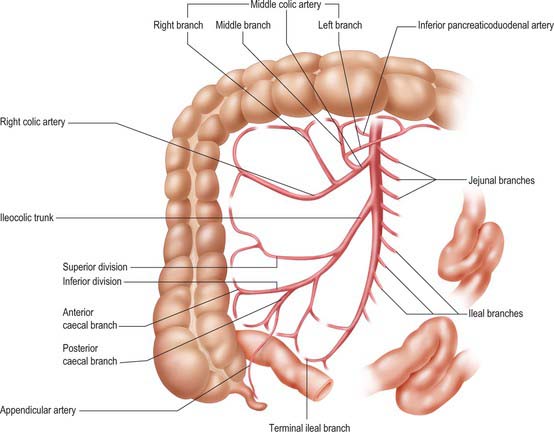
Fig. 66.9 The superior mesenteric artery and its branches. The outlines of representative ileal and jejunal loops, appendix, caecum, ascending and transverse colon are shown for reference. Only the origin of jejunal and ileal branches are shown. For details of arcades see Fig. 66.8.
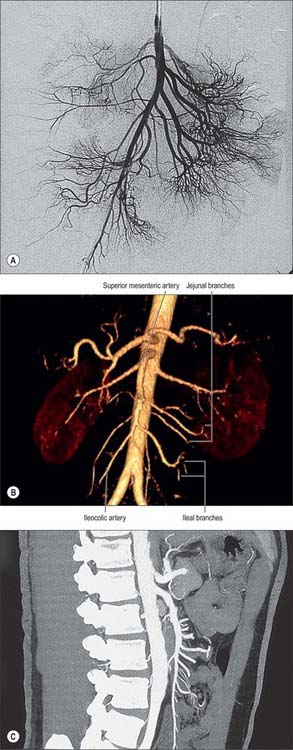
Fig. 66.10 The superior mesenteric artery and its branches. A, Digital subtraction angiogram. C, Sagittal reformat of multislice CT angiogram.
(by courtesy of Dr Adam Mitchell, Charing Cross Hospital, London). B, Surface shaded, volume rendered CT angiogram (by courtesy of Dr Nasir Khan, Chelsea and Westminster Hospital, London) (by courtesy of GE Worldwide Medical Systems)
The superior mesenteric artery gives off middle colic, right colic (sometimes), ileocolic, jejunal and ileal branches. It may be the source of the common hepatic, gastroduodenal, accessory right hepatic, accessory pancreatic or splenic arteries, and may arise from a common coeliacomesenteric trunk. Its jejunal and ileal branches form arcades within the mesentery to a varying extent. The last of these arcades is said to form a ‘marginal artery’ of the small intestine, although the latter is irregular and not a single definable vessel. Straight arteries, the vasa recta, which supply the small intestine directly without further branches, are given off from this lowest arcade.
The remnant of the vitellointestinal artery (the embryonic artery which originally connected the intestinal circulation to the yolk sac) is usually obliterated; when present, it forms the artery supplying a Meckel’s diverticulum. It is occasionally represented in the mesentery by a fibrous strand from the region of the last ileal branch.
There are usually five to ten jejunal branches which arise from the left side of the upper portion of the superior mesenteric artery (Figs 66.9, 66.10). They are distributed to the jejunum as a series of short arcades which form a single (occasionally double) tier of anastomotic arcs before giving rise to multiple vasa recta (Fig. 66.8). These vessels run almost parallel in the mesentery and are distributed alternately to opposite aspects of its wall where the two series of vessels form distinct ‘leaves’ within the mesentery. Small twigs supply regional lymph nodes and other structures in the mesentery.
Ileal branches are more numerous than the jejunal branches but smaller in calibre. They arise from the left and anterior aspects of the superior mesenteric artery. The length of the mesentery is greater in the ileum and the branches form three, four or sometimes five tiers of arcs within the mesentery before giving rise to multiple vasa recta that run directly towards the ileal wall. The ileal branches run parallel in the mesentery and are distributed to alternate aspects of the ileum. They are longer and smaller than similar jejunal vessels, particularly in the distal ileum, and do not form such definite parallel ‘leaves’ of vessels. The vascular supply in the last loop of the terminal ileum is limited. There are usually only two separate arcades, peri-serosal and in the mid-zone of the mesentery. They each receive a contribution from the ileal branch of the ileocolic artery and the last ileal branch of the superior mesenteric artery and are often larger in calibre than the mid-ileal vessels. Other than this connection, few if any vessels connect the ileocolic and superior mesenteric arteries, which makes surgical exposure of the ileocolic artery up to its origin relatively simple.
Veins
Superior mesenteric vein
The superior mesenteric vein drains the small intestine, caecum, ascending and transverse parts of the colon (Fig. 66.12; see Fig. 60.8). It is formed in the right lower mesentery of the small bowel by the union of tributaries from the terminal ileum, caecum and vermiform appendix. It ascends in the mesentery to the right of the superior mesenteric artery, passes anterior to the right ureter, inferior vena cava, third part of the duodenum and uncinate process of the pancreas, and finally joins the splenic vein behind the neck of the pancreas to form the portal vein.
Lymphatics
Lymph vessels, lacteals, are found in the mucosa and muscular coat of the small bowel. Lacteals from the villi arise from an intricate plexus in the mucosa and submucosa and are joined by vessels from lymph spaces at the bases of solitary lymphoid follicles. They drain to larger vessels at the mesenteric border of the gut. The lacteals of the muscular tunic form a close plexus that runs mostly between the two muscle layers; they communicate freely with mucosal vessels and open into vessels at the mesenteric border. Mesenteric lacteals pass between the layers of the mesentery and drain into a series of mesenteric lymph nodes which are arranged in tiers within the mesentery and which follow the same distribution as the regional arterial supply; they may form ‘chains’ along the major arteries. Elsewhere in the ileal and jejunal mesenteries the lacteals form an extensive network that affords a relatively wide field of lymph node drainage. This arrangement makes radical surgical resection of lymph nodes difficult if the vessels to the remaining unaffected small bowel are to be preserved. The mesenteric nodes drain into superior mesenteric nodes around the root of the superior mesenteric artery.
INNERVATION
The ileum and jejunum are innervated by parasympathetic and sympathetic fibres via the superior mesenteric plexus (see Figs 60.2–60.4). Preganglionic sympathetic axons originate from neurones in the intermediolateral grey matter of the mid-thoracic spinal segments and travel in the greater and lesser splanchnic nerves to the superior mesenteric ganglion where they synapse. Postganglionic axons accompany the superior mesenteric artery into the mesentery and are distributed along branches of the artery. The sympathetic nerves are vasoconstrictor to the vasculature and inhibitory to the musculature of the jejunum and ileum.
Preganglionic parasympathetic axons travel in the anterior and right vagus nerve and are secretomotor to the mucosa and motor to the musculature of the jejunum and ileum.
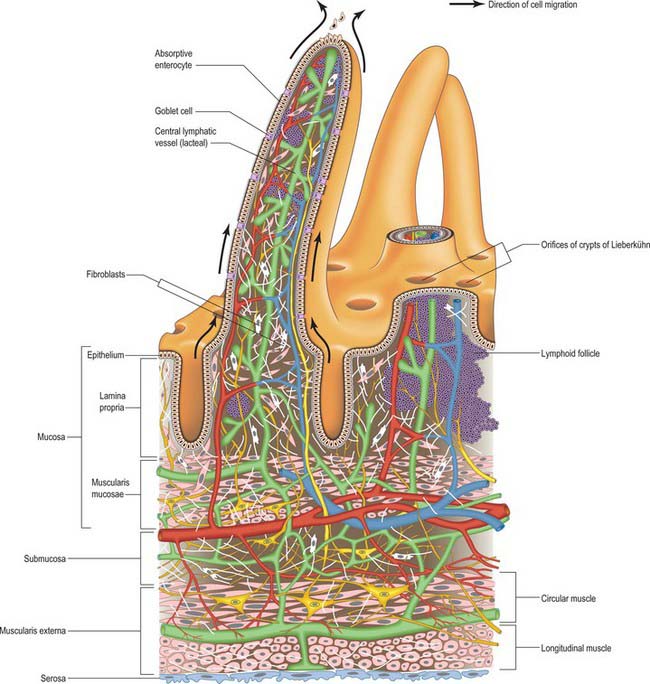
MICROSTRUCTURE
The intestinal wall is composed of mucosa, submucosa, muscularis externa and serosa or adventitia. The mucosa is thick and very vascular in the proximal small intestine, but thinner and less vascular distally. In places it is ridged by the underlying submucosa to form circular folds, plicae circulares, which protrude into the lumen; mucosal finger- or leaf-like intestinal villi cover the whole surface (Fig. 66.13). There are numerous simple tubular intestinal glands or crypts between the bases of the villi, and additional submucosal glands in the duodenum. The submucosa contains aggregates of lymphoid tissue, most numerous in the ileum.
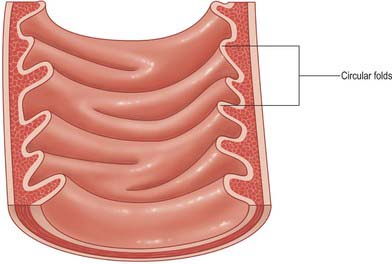
Fig. 66.13 Internal aspect of a representative sample of the proximal jejunum, showing circular folds.
Circular folds
Other than in the first part of the duodenum, large crescentic folds of mucosa project into the lumen of the small intestine, lying either transversely or slightly obliquely to its long axis (Fig. 66.14). Unlike gastric folds they are not lost during physiological distension of the intestine. Most extend round half or two-thirds of the luminal circumference, some are complete circles, some bifurcate and join adjacent folds, yet others are spiral but extend only once (occasionally two or three times) round the lumen. Larger folds are up to 8 mm deep at their broadest, but most are smaller than this, and larger folds often alternate with smaller ones. Folds begin to appear 2.5–5 cm beyond the pylorus. Distal to the major duodenal papilla they are large and close together, as they also are in the proximal half of the jejunum. From here to midway along the ileum they diminish, and they disappear almost completely in the distal ileum, which accounts for the thinness of this part of the intestinal wall. The circular folds slow the passage of the intestinal contents and increase the absorptive surface. They are visible in contrast and occasionally plain radiographs.
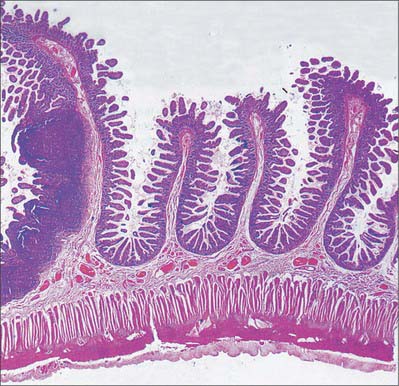
Fig. 66.14 Low-power micrograph showing several circular folds in the wall of the ileum. The folds are covered with villi projecting into the lumen and the submucosa extends into the core of each fold. Circular (innermost) and longitudinal smooth muscle layers form the underlying muscularis externa. Large masses of lymphoid tissue (Peyer’s patches) occupy the mucosa at the left of the field.
(By permission from Young B, Heath JW 2000 Wheater’s Functional Histology. Edinburgh: Churchill Livingstone.)
Intestinal villi
Intestinal villi are highly vascular projections of the mucosal surface, just visible to the naked eye (Figs 66.15-66.17). They cover the entire intestinal mucosa, increase the surface area of the lumen about eight-fold, and give it a velvety texture. Villi are large and numerous in the duodenum and jejunum, and smaller and fewer in the ileum. In the first part of the duodenum they appear as broad ridges, become tall and foliate in the distal duodenum and proximal jejunum, and then gradually shorten to a finger-like form in the distal jejunum and ileum. Villi vary in density from 10 to 40 per square millimetre and from 0.5–1.0 mm in height (Fig. 66.15). Infoldings of the mucosa dip down from the base of the villi for a short distance into the lamina propria. These crypts (of Lieberkühn), are most prominent in the proximal small intestine (Fig. 66.16).
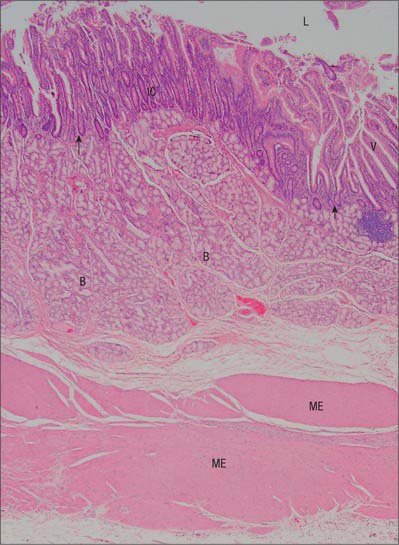
Fig. 66.15 Low power micrograph showing the wall of the duodenum, with villi (V) projecting into the lumen (L); intestinal crypts (IC) of Lieberkühn in the mucosa, seen mainly in transverse section; muscularis mucosae (arrows); submucosal seromucous (Brunner’s) glands (B) and muscularis externa (ME).
(By courtesy of Mr Peter Helliwell and Dr Joseph Mathew, Department of Histopathology, Royal Cornwall Hospitals Trust, UK.)
Mucosa
The mucosa consists of epithelium, lamina propria and muscularis mucosae.
Epithelium
A single-layered epithelium covers the intestinal villi (Figs 66.15, 66.16) and also lines the intestinal glands (crypts) that open between the bases of villi. Two types of cell, enterocytes and goblet cells, cover the surfaces of the villi, whereas microfold cells (M cells) are restricted to the dome epithelium that covers localized accumulations of lymphoid tissues. These cell types are all in contact basally with a basal lamina to which they adhere, and all are derived from a common stem cell in the intestinal crypts.
Enterocytes are columnar absorptive cells, approximately 20 μm tall. They are the most numerous type of cell in the small intestinal lining, and are responsible for nutrient absorption. Their surfaces bear up to 3000 microvilli, which greatly increase the surface area for absorption. Collectively, microvilli are visible by light microscopy as a brush (striated) border 1 μm thick: individual microvilli can be resolved only by electron microscopy. Enterocyte nuclei are elongated vertically, mainly euchromatic and located just below the centre of the cell.
The apical cell surface is resistant to protease attack because microvilli possess a specialized glycoprotein-rich surface coat (glycocalyx) which, with an overlying layer of mucus, protects the epithelium against pancreatic enzymes in the intestinal lumen. The cell coat also contains a number of digestive enzymes as integral membrane proteins. These include enzymes that degrade disaccharides and oligopeptides prior to absorption. Further details of the structure of microvilli are given on page 18).
The luminal surface is an important barrier to diffusion. Nutrients generally have to pass through enterocytes (transcellular absorption) before they reach the underlying lamina propria and its blood vessels and lymphatics (lacteals). Classical epithelial junctional complexes encircle the apical plasma membranes of adjacent enterocytes: their tight junctions form an effective barrier to non-selective diffusion between the gut lumen and the body as a whole. The lateral plasma membranes of enterocytes are highly folded, interdigitating with each other to form complex intercellular boundaries, anchored periodically by desmosomes, and making contact at gap junctions. The lateral intercellular space expands during active absorption and is an additional conduit (supplementing transport across the basal cell surface) for the passage of fluids, nutrients and other solutes to the vessels of the lamina propria.
Enterocytes have a lifespan after differentiation of about 5 days. Their position on the villus wall reflects their stage in the life cycle: at the tips of intestinal villi they undergo programmed, apoptotic, cell death and are shed from the epithelium. They are replaced at the base of the villus by stem cell mitosis.
Goblet cells are most numerous in the distal small intestine, increasing in number from the duodenum to their highest density in the terminal ileum. They have elongated basal nuclei, an apical region containing many membrane-bound mucinogen granules, and apical surfaces that bear a few short microvilli. Goblet cell mucins contribute to protection against microorganisms and toxins in the gut lumen, and also provide lubrication and mechanical protection from the intestinal contents.
Microfold cells are present where the epithelium covers lymphoid aggregates in the intestinal wall (p. 74). They are cuboidal or flattened in shape and have long, widely spaced microfolds rather than microvilli on their apical surfaces. They sample luminal antigens by endocytosis, and transport antigen to lymphocytes lying within intercellular pockets formed by deep invaginations of the M-cell basolateral plasma membranes. See page 78 for details of antigen processing and presentation.
Intestinal glands or crypts
Intestinal glands or crypts (of Lieberkühn) are tubular pits that open into the lumen throughout the intestinal mucosa via small circular apertures between the bases of the villi (Figs 66.14-66.16). Their thin walls are composed of columnar enterocytes supplemented by mucous cells, Paneth cells, stem cells and neuroendocrine cells. They are separated by a basement membrane from a rich capillary plexus within the lamina propria.
Enterocytes in the crypts secrete ions and alkaline fluid to dilute chyme and aid absorption by structurally similar cells that cover the villi.
Paneth cells are numerous in the deeper parts of the intestinal crypts, particularly in the duodenum. They are rich in zinc and contain large acidophilic granules that stain strongly with eosin or phosphotungstic haematoxylin. Paneth cells secrete lysozyme, a highly specific antibacterial enzyme, and other defensive proteins (defensins) such as tumour necrosis factor alpha (TNF-α), which protect the intestinal luminal surface.
Stem cells occur in a zone just above the basal region of the crypts and are the source of most of the cell types of the intestinal epithelium. Their progeny, transit (transient) amplifying cells, have one of the most rapid proliferation rates in the body. They migrate out of the intestinal crypts along the sides of the villi, where they differentiate mainly into the short-lived columnar enterocytes or goblet cells (which are thus continually replaced). When not dividing, their apical surfaces have fewer and more irregular microvilli than the differentiated enterocytes.
Several types of neuroendocrine cell are scattered among the walls of the intestinal crypts, and less commonly over the villi. They secrete bioactive peptides, such as gastrin, cholecystokinin and secretin, basally into the surrounding lamina propria. Crypt neuroendocrine cells are derived from stem cells, which also give rise to enterocytes and other epithelial elements. For further details of the dispersed neuroendocrine system, see page Chapter 60.
Lamina propria
The lamina propria is composed of connective tissue and provides mechanical support for the epithelium. It has a rich vascular plexus, receives nutrients absorbed by the enterocytes, and forms the cores of the villi. It contains lymphoid tissue, fibroblasts and connective tissue extracellular matrix fibres, smooth muscle cells, eosinophils, macrophages, mast cells, capillaries, lymphatic vessels and unmyelinated nerve fibres. Plasma cells are numerous. Lymphocytes may be clustered in solitary or aggregated follicles, some of which extend through the muscularis mucosae into the submucosa.
Core of the villus
Each villus has a core of delicate connective tissue that contains a large blind-ending lymphatic vessel or lacteal (so called because of its content of suspended chylomicrons, the droplets of apoprotein–lipid complex elaborated by enterocytes from absorbed dietary fats). The core also contains blood vessels, nerves and smooth muscle cells derived from fine extensions of the muscularis mucosae. Each lacteal, usually single but occasionally double, starts in a closed dilated extremity near the tip of a villus, and extends through the core to the base of the villus, where it joins a narrower lymphatic plexus in the deeper lamina propria. Its wall is a single layer of endothelial cells. Smooth muscle cells surround the lacteal throughout the villus and their contraction propels its contents into the underlying lymphatic plexus. Capillaries within the core are lined by fenestrated endothelium to facilitate the rapid intake of nutrients diffusing from the covering absorptive epithelium.
Mucosa-associated lymphoid tissue
Mucosa-associated lymphoid tissue (MALT) consists of lymphoid follicles covered by follicle-associated intestinal epithelium which includes scattered M cells. It is found mainly in the lamina propria, but sometimes expands into the submucosa, and is the source of B and T lymphocytes and other related cells involved in the immune defence of the gut wall.
Solitary lymphoid follicles are scattered along the length of the intestinal mucosa, and are most numerous in the distal ileum. Aggregated lymphoid follicles, Peyer’s patches, are circular or oval masses containing 10–260 follicles. They vary in length from 2 to 10 cm, are visible macroscopically as dome-like elevations, and usually situated in the intestinal wall opposite the mesenteric attachment. They are largest and most numerous in the ileum; small, circular and few in the distal jejunum; and rare in the duodenum. Villi are small or absent over the larger follicular groups.
Like other masses of MALT (except lymph nodes), solitary and aggregated lymphoid follicles are most prominent around the age of puberty, after which they diminish in number and size, although many persist into old age. For further details of intestinal MALT and its function, including Peyer’s patches, see Didierlaurent, Simonet & Sira (2006).
Submucosa
The submucosa is composed of loose connective tissue and contains blood vessels, lymphatics and nerves. Its ridged elevations form the cores of the circular folds. The geometry of its collagen and elastin fibres permits the considerable changes in transverse and longitudinal dimensions that accompany peristalsis, whilst still providing adequate support, elasticity and strength.
Submucosal (Brunner’s) glands
Submucosal glands are limited to the submucosa of the duodenum and often referred to as ‘Brunner’s glands’ (see Fig. 66.15). Their ducts traverse the muscularis mucosae to enter the bases of the mucosal crypts. They are largest and most numerous near the pylorus and form an almost complete layer in the proximal half of the descending duodenum, thereafter they gradually diminish in number and disappear at the duodenojejunal junction. They are small, branched tubuloacinar glands: each has several secretory acini lined by low columnar epithelial cells that produce an alkaline (pH 9) mucoid secretion which effectively neutralizes acidic chyme from the stomach. Many neuroendocrine cells are present among the acinar cells.
Muscularis externa
The muscularis externa consists of a thin external longitudinal layer and a thick internal circular layer of smooth muscle cells. It is thicker in the proximal small intestine and is mainly responsible for the differential appearance of proximal jejunum and distal ileum of CT scanning.
Serosa
Serosa is visceral peritoneum and consists of a subserous stratum of loose connective tissue covered by mesothelium. It covers the majority of the muscularis externa, the only exceptions are the part adjacent to mesenteric adipose tissue and the retroperitoneal portions of the duodenum, both of which are covered mainly by a connective tissue adventitia rather than by serosa.
Didierlaurent A, Simonet M, Sira J-C. Innate and acquired plasticity of the intestinal immune system. Cell Mol Life Sci. 2006;62:1285-1287.
Jackson JE. Vascular anatomy of the gastrointestinal tract. In: Butler P, Mitchell AWM, Ellis H. Applied Radiological Anatomy. Cambridge: Cambridge University Press, 1999.
Kadir S. Atlas of Normal and Variant Angiographic Anatomy. Philadelphia: WB Saunders, 1991.
Kraehenbuhl JP, Neutra MR. Molecular and cellular basis of immune protection of mucosal surfaces. Physiol Rev. 1992;72:853-879.
Underhill BML. Intestinal length in man. Br Med J. 1955;2:1243-1246.