Emerging Diseases
After completing this chapter, the student should be able to do the following:
 List the six ways infectious diseases may emerge and give an example with each.
List the six ways infectious diseases may emerge and give an example with each.
 List some infectious diseases that have appeared since 1970.
List some infectious diseases that have appeared since 1970.
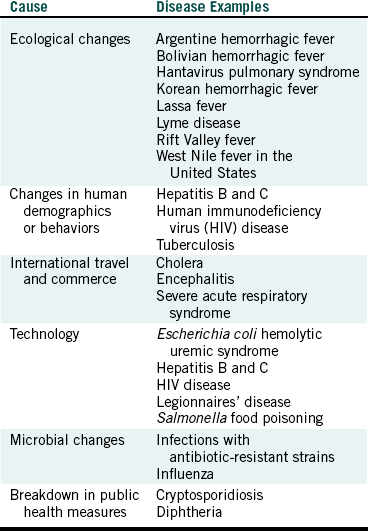
Overall infectious diseases remain the third leading cause of death in the United States and the second leading cause of death worldwide. Of the 15 million deaths that occur worldwide each year, 15 million (25%) are directly caused by infectious diseases. This is surpassed only by deaths from cardiovascular diseases at 29%. Emerging diseases are new infectious diseases that have not been recognized before as well as known infectious diseases with changing patterns. Infectious diseases can be expected to emerge continually, and the number of these diseases, as listed in Table 4-1, will continue to grow. Diseases emerge because conditions change that bring microorganisms and human beings together in new ways. These changing conditions can be grouped into six categories, as listed in Table 4-2.
TABLE 4-1
Some Recently Recognized Disease/Microorganism Associations
| Year∗ | Microorganism | Disease |
| 1970 | Coxsackievirus | Hand-foot-and-mouth disease |
| 1972 | Norwalk virus | Gastroenteritis |
| 1973 | Rotavirus | Infantile diarrhea |
| 1975 | Astrovirus | Gastroenteritis |
| 1975 | Parvovirus B19 | Fifth disease; aplastic crises–chronic hemolytic anemia |
| 1976† | Ebola virus | Ebola hemorrhagic fever |
| 1977 | Cryptosporidium parvum | Acute enterocolitis |
| 1977 | Enteric adenovirus | Gastroenteritis |
| 1977 | Hantaan virus | Hemorrhagic fever with renal syndrome |
| 1977 | Hepatitis D virus | Hepatitis D (blood-borne) |
| 1977 | Legionella pneumophila | Legionnaires’ disease |
| 1981 | Staphylococcus aureus | Toxic shock syndrome associated with tampons |
| 1982 | Escherichia coli O157:H7 | Hemorrhagic colitis; hemolytic uremic syndrome |
| 1983 | Helicobacter pylori | Gastric ulcers |
| 1983 | HIV type 1 | HIV disease; HIV infection and AIDS‡ |
| 1987 | Hepatitis E virus | Hepatitis E (waterborne, food-borne) |
| 1987 | Rift Valley fever virus | Hemorrhagic fever |
| 1988 | Human herpesvirus 6 | Roseola (actual disease known since 1910) |
| 1989 | Ehrlichia chaffeensis | Human ehrlichiosis |
| 1989 | Hepatitis C virus | Hepatitis C (blood-borne) |
| 1990 | Barmah forest virus | Polyarthritis in West Australia |
| 1990 | Haemophilus influenzae | Brazilian purpuric fever (new strain: aegyptius) |
| 1991 | Guanarito virus | Venezuelan hemorrhagic fever |
| 1991 | Hepatitis F virus | Hepatitis |
| 1992 | Bartonella henselae | Cat-scratch disease |
| 1992 | Vibrio cholerae O139 | Epidemic cholera (new strain) |
| 1993 | Sin nombre virus | Hantavirus pulmonary syndrome |
| 1994 | Sabia virus | Brazilian hemorrhagic fever |
| 1995 | Hepatitis G virus | Hepatitis G |
| 1995 | Human herpesvirus 8 | Associated with Kaposi’s sarcoma |
| 1998 | Hendra virus | Respiratory disease |
| 1998 | Menangle virus | Respiratory disease |
| 1998 | Nipah virus | Meningitis, encephalitis |
| 1999 | West Nile virus | Encephalitis |
| 2003 | Coronavirus | Severe acute respiratory syndrome (SARS) |
| 2003 | Monkeypox virus | Skin infection |
| 2004 | Torque teno virus | Acute respiratory disease |
| 2005 | Chikungunya virus | Polyarthralgia |
∗Year microorganism was isolated, identified, or first associated with disease.
†Subsequent outbreaks have occurred in 1979, 1994, 1995, 1996, 2001, and 2007.
‡HIV, human immunodeficiency virus; AIDS, acquired immunodeficiency syndrome.
ECOLOGICAL CHANGES
Ecological changes that result in disease emergence usually involve zoonotic diseases (diseases involving animals) or insect-borne diseases. Such changes involve bringing human beings into close contact with animals or insect vectors, resulting in the spread of microorganisms from animals to human beings. One example is the emergence of Korean hemorrhagic fever, a disease of human beings involving high fever and internal bleeding, caused by the Hantaan virus from rodents. When rice fields are created, field mice flourish because of the new source of food. Harvesting the rice brings human beings into close contact with these infected mice, resulting in spread of the virus.
In 1993 an unusually mild and wet summer in the southwestern United States likely enhanced contact between human beings and rodents carrying a previously unrecognized hantavirus now named Sin Nombre virus. The rodent population flourished, and human beings probably entered the wilds more frequently as a result of the favorable weather. This likely caused the initial cluster of 24 human cases of hantavirus pulmonary syndrome in this area. This syndrome produces symptoms of fever, muscle aches, nausea, vomiting, headache, and ultimately severe respiratory distress with death in about one half of those infected. Although the initial outbreak occurred in the Four Corners region of the United States (Arizona, New Mexico, Colorado, Utah), more than 300 cases now have been confirmed in the United States. The deer mouse (which is distributed widely in North America) is found to be the most common host for the Sin Nombre virus. The disease also is associated with cotton rats, rice rats, and the white-footed mouse and has now been detected in several other countries including Argentina, Brazil, Canada, Chile, Paraguay, and Uruguay.
Other rodent viruses cause human diseases, including the Machupo virus that causes Bolivian hemorrhagic fever, the Argentine hemorrhagic fever virus, and the Lassa fever virus. The exact mode of spread of microorganisms from rodents to human beings is not always known but may involve contact with rodent feces or aerosolized urine.
Another ecological change resulted in disease emergence in 1987 along the Senegal River in Mauritania, Africa. Building dams in the river valley facilitated irrigation as planned but also greatly increased the water breeding grounds for the mosquitoes that carry viruses. This caused the emergence of Rift Valley fever, a viral disease caused by a mosquito vector that results in high fever and sometimes retinitis and, rarely, fulminant hepatitis with hemorrhage. This disease also became visible again in Kenya in 1997, after that part of East Africa received torrential rains, yielding a “bumper crop” of mosquitoes. In 2000 outbreaks were seen for the first time outside of Africa, in Saudi Arabia and Yemen. In 2003 this disease reemerged in Mauritania.
Lyme disease initially was recognized in the United States in 1975 in a group of children who lived in Lyme, Connecticut. Lyme disease is caused by the bacterial spirochete Borrelia burgdorferi, which is transmitted to human beings through the bite of ticks. The disease results in a rash (associated with the tick bite) and starts with flulike symptoms. Weeks later, the subject may develop cardiac or neurologic problems, muscle aches and pains, or intermittent attacks of arthritis. The emergence of this disease likely was due to ecological changes in forests near populated sites that increased the population of the deer and the deer tick, the vector of Lyme disease in human beings. Situations that encourage human beings to venture near and into forests also contribute to this emergence, and affected individuals may include campers, hunters, hikers, bird-watchers, and even golfers. Today, about 16,000 cases of Lyme disease are reported annually throughout the United States, with most cases occurring in the northeastern states.
CHANGES IN HUMAN DEMOGRAPHICS OR BEHAVIORS
Human population movements or changes in how human beings associate with each other can create new conditions that favor disease spread. Movement and crowding of persons into cities in poor countries result in numerous infectious disease problems such as the spread of dengue virus from mosquitoes breeding in open water containers, causing dengue hemorrhagic fever. Crowding also leads to transference of other mosquito-borne diseases such as yellow fever and several forms of viral encephalitis. The movement of persons infected with human immunodeficiency virus (HIV) from the villages of Africa to large cities introduced the infection to larger susceptible populations. The movement of more than 500,000 starving Rawandans into Zaire (now the Democratic Republic of the Congo) in 1994 resulted in more than 50,000 deaths in the refugee camps from cholera and Shigella dysentery.
Human demographics also play a role in disease spread in the United States. Increased population densities, as may occur with the homeless or with institutionalized persons (e.g., prisoners), have contributed to the increase in the numbers of tuberculosis cases in the United States in recent years. Bringing children together in some day care centers has contributed to the spread of disease agents such as cytomegalovirus. Human behavior also influences disease spread and emergence. Unprotected sexual contact among members of various populations and an increase in injection drug abuse facilitate the sharing of human body fluids among individuals. If the body fluids are infected with microorganisms, the microorganisms rapidly reach new hosts. These behaviors are the primary reasons for the emergence and spread of HIV and the continued occurrence of most cases of hepatitis B and C.
The behaviors of misuse and overuse of antibiotics lead to conditions that select for antibiotic-resistant strains of bacteria, for example, antibiotics prescribed when not necessary and antibiotics used for prevention of infections. Such practices have resulted in the emergence and occurrence of harmful infections by antibiotic-resistant strains that are much more difficult to treat. Such conditions are described more fully under Microbial Changes.
INTERNATIONAL TRAVEL AND COMMERCE
In a few hours, or a few days at the most, just about anyone can travel just about anywhere. We carry our microorganisms with us when we travel and can spread them easily to others in faraway lands. Also, microorganisms that contaminate water, foods, plants, animals, insects, and goods literally can be shipped throughout the world. A recent example of this is the emergence of cholera in South and Central America. Cholera is an intestinal bacterial disease spread by contaminated water or food that results in severe diarrhea and dehydration. A new strain of the cholera causative agent (Vibrio cholerae O139 Bengal) emerged in 1992 in southern Asia, where cholera is endemic. Within a year this new strain was detected in South and Central America, where, along with V. cholerae O139, it has caused more than a million cases of cholera and resulted in about 10,000 deaths. This was the first epidemic of cholera in South and Central America in the 20th century. The exact mode of spread of strain O139 from Asia to South and Central America is not known, but transmission possibly involved the water on and in cargo ships. Vibrio cholerae has been isolated from the ballast, bilge, and sewage waters of cargo ships.
As evidence that V. cholerae O139, originally detected in Indonesia, has reached U.S. shores, this strain was isolated from oysters and oyster-eating fish in Mobile Bay, Alabama, in 1992. However, an associated epidemic or even a large outbreak of cholera has not occurred in the United States. During the period when a million cases of cholera developed in South and Central America (1991 to 1994), only 158 cases were reported in the United States. This difference likely involves better import controls and sanitation in the United States.
Another example of shipping industry involvement in disease emergence is viral encephalitis spread by the Asian tiger mosquito. Encephalitis involves infection of the central nervous system that may cause fever, headache, vomiting, nausea, lethargy, paralysis, or convulsions. Tiger mosquitoes originally were found in Asia, but they now have been detected (along with the encephalitis) in the United States, Brazil, and Africa. Apparently these mosquitoes were transported from Asia in water that collected in used automobile tires on the decks of cargo ships. Since coming to the United States in 1982, the Asian tiger mosquito has established itself in at least 21 states and is involved in causing eastern equine encephalomyelitis.
An interesting incident involving foreign commerce occurred in Reston, Virginia, in 1989. Monkeys from the Philippines were shipped to an animal care facility in Reston. The monkeys were infected with an Ebola virus (referred to as the Ebola-Reston strain) that caused a hemorrhagic fever, and the virus was spread to other monkeys in the facility. The fear was that this deadly virus might escape the facility and cause an epidemic in human beings. Fortunately, the Reston virus was different from the African strains of the Ebola virus (see the following discussion) and did not cause disease in human beings.
West Nile virus was discovered first in Uganda in 1937. The virus usually causes mild encephalitis but can produce a severe and fatal disease. This virus was first recognized in the Western Hemisphere in an outbreak in New York in 1999. By the end of 2006, 4269 cases had been reported in the United States, with 177 deaths. The disease is transmitted by ornithophilic (bird-loving) mosquitoes and also occurs in horses, many types of birds, and some other animals. The virus apparently is not spread directly from person to person or animal to person. At the same time the human outbreak in New York was detected, large die-offs of wild and captive birds were noticed in the Bronx Zoo and other parts of New York. Human cases occurred at sites near wetlands where migratory birds, ornithophilic mosquitoes, and human beings were concentrated. These events, along with the history of European cases, suggest that zoo, pet, wild, or domestic birds were responsible for introduction of this virus into the United States through normal migration or importation.
In early 2003 a disease emerged in China and the cities of Hong Kong, Hanoi, and Singapore called severe acute respiratory syndrome (SARS). The syndrome is a pneumonia-like disease caused by a previously unrecognized coronavirus from domesticated animals (possibly cats) that is spread by droplet infection or by indirect or direct contact. The first cases detected in other countries and in Canada and the United States were in individuals who recently had traveled from China or Vietnam. About 8500 cases of SARS have been identified.
TECHNOLOGY
Technological advancements involving the development of new devices and processes are important to many aspects of life. However, sometimes this new technology creates new ways to bring microorganisms and human beings together. For example, mass food processing combines large amounts of raw materials for widespread distribution. Unfortunately, a small amount of contaminated raw material can taint a large amount of processed food. Apparently this happened in 1993 when a pathogenic strain of Escherichia coli (O157:H7) contaminated meat used to make hamburger for a fast-food chain. The E. coli was distributed to restaurants over a four-state area in the northwest United States, infecting about 700 persons and causing two deaths. Another important point is that undercooking of the meat allowed the E. coli to survive and cause problems. This strain of E. coli was first recognized in 1983 and causes hemorrhagic colitis involving bloody diarrhea and abdominal cramps. A life-threatening complication called hemolytic uremic syndrome may develop, and this was the cause of the two deaths in the 1993 outbreak. Hemolytic uremic syndrome involves malfunction of the kidneys and lysis of red blood cells. Fifteen additional outbreaks with the O157:H7 strain were reported in 1993, resulting in more than 100 outbreaks now reported in the United States. Most outbreaks resulted from consumption of contaminated, undercooked ground beef, which has resulted in the FDA-ordered destruction or recall of millions of pounds of hambuger. Other outbreaks have involved contaminated fruits, yogurt, water, apple juice, coleslaw, and dried salami. Escherichia coli O157:H7 also has been spread to others in swimming pools and day care centers.
In 1994 about 4000 cases of Salmonella food poisoning occurred in 36 states because of contamination of a batch of ice cream mix processed by a large food company. The mix was prepared and pasteurized (heated to 161° F for 15 seconds to kill disease-producing bacteria) and transported to the packaging and distribution plant. Unfortunately, the mix was transported in a truck that had been used just previously to transport raw eggs. Eggs are the leading source of Salmonella food poisoning in the United States. Apparently the truck had not been disinfected properly before transporting the ice cream mix, which was not repasteurized before freezing, packaging, and distribution.
The life-saving technology of concentrating special blood products to administer to hemophiliacs and others is important. Unfortunately, such technology also has created an efficient way to transmit blood-borne viruses (e.g., HIV and hepatitis B and C viruses) to those who receive these blood products. Blood transfusion with contaminated blood presents a similar mode of spread. As of December 2001, 816,145 cases of acquired immunodeficiency syndrome have been reported to the Centers for Disease Control and Prevention in the United States. Of these, 236 had occurred in those with hemophilia or other coagulation disorders, and 8284 had occurred in transfusion recipients. Today, blood can be tested for the presence of HIV and hepatitis B and no longer serves as a significant mode of spread for these agents.
The development of water-handling devices certainly has made our lives easier, but it has led to new sites that harbor potential pathogens. For example, Legionnaires’ disease (a pneumonia caused by the bacterium Legionella pneumophila; see Chapter 7) was first recognized in 1976 among attendees at an American Legion convention in Philadelphia. A few hundred staying at a particular hotel became infected with L. pneumophila through the hotel water system or the air-conditioning system and became ill. Since then, L. pneumophila has been found to exist in our natural waters and to accumulate on surfaces of water-handling devices (e.g., cooling fins of air-conditioning units, in humidifiers, grocery store vegetable sprayer nozzles, shower heads, therapeutic whirlpools, and dental unit water lines). Inhalation of contaminated water aerosols or aspiration of oral fluids colonized with this opportunistic bacterium may lead to disease, mainly if a person’s immune system is compromised and particularly susceptible to respiratory diseases.
MICROBIAL CHANGES
Most mutations in the microbial world are probably lethal because the change destroys some mechanism necessary for multiplication. However, some mutations do not cause death and occasionally even make the microorganism more virulent or more difficult to kill. Two such examples have been mentioned already: V. cholerae O139 and E. coli O157:H7.
Another well-known example of microbial change is the influenza virus, which changes constantly. About every year, everyone becomes susceptible to the influenza virus regardless of past bouts with it. The immune system of those who have had influenza usually does not recognize the new virus and offers little or no protection. Likewise, last year’s vaccine usually does not work against this year’s new strain of virus, so annual flu shots are necessary to achieve the maximum protection.
Another major cause of disease emergence is the development of drug resistance (resistance to antibiotics) among several bacteria. Some of the changes that occur in bacteria involve the development of resistance to one or more antibiotics. For example, if resistance to penicillin has developed in a bacterium causing an infection, and penicillin (which has always taken care of the infection in the past) is administered to the infected patient, the bacterium not only will continue to make the person sick but also will continue to multiply in higher numbers, enhancing its chances of spreading to others. As this continues with subsequent patients, the resistant bacterium reaches more and more persons, causing the same disease, which can no longer be treated with the original antibiotic. With time, a large percentage of those susceptible to this bacterium become infected with the antibiotic-resistant strain. Such infection usually causes delays in effective therapy, giving the bacterium a sometimes dangerous foothold in the early stages of disease.
Several pathogenic antibiotic-resistant bacteria have emerged, including drug-resistant Streptococcus pneumoniae, vancomycin-resistant enterococci, methicillin-resistant Staphylococcus aureus, and multiple drug-resistant Mycobacterium tuberculosis, all of which are important in dentistry and are described further in Chapter 7.
BREAKDOWN IN PUBLIC HEALTH MEASURES
Countless public health measures to protect against the spread of infectious diseases have been instituted in the United States, but they must be maintained to remain effective. One measure is the production of safe drinking water (referred to as potable water). The breakdown of a water treatment process in the city of Milwaukee in 1993 resulted in about 400,000 cases of an intestinal infection caused by the protozoon Cryptosporidium parvum. This protozoon exists in the intestines of animals and thus ends up in groundwater that empties into the streams that serve as the source of the drinking water of the nation. If water treatment plants do not effectively remove this protozoon (and many other microorganisms) from the drinking water, problems can occur. Other municipal waterborne outbreaks of cryptosporidiosis have occurred in Texas, Georgia, and Oregon.
Many major cities periodically issue “boil water” notices indicating that persons should boil tap water before consuming it or using it in cooking. These notices usually result from a temporary problem at the water treatment plant or with the lines that distribute the water from the plant to homes and workplaces. Commonly, a notice will be generated if a water main (a large water distribution pipeline) breaks as a result of below-freezing temperatures, earthquakes, settling of the ground, or age of the water distribution system. These events can allow potentially contaminated groundwater into the drinking water that flows downstream from the break.
With the formation of the New Independent States from the former Soviet Union, some public health vaccination programs were relaxed, which resulted in the development of 45,000 new cases of diphtheria in 1994, with a prediction of 200,000 cases in the following year unless action was taken. Strengthening of the vaccination programs resulted in “only” 60,000 cases in 1995. Diphtheria in the United States is rare because of our effective vaccination program involving DPT inoculations (D stands for diphtheria; P stands for pertussis, the bacterium that causes whooping cough; and T stands for tetanus). About five cases a year have been reported since 1980, and since 1988 all the cases in the United States have been imported. However, if the United States were to relax its vaccination program as occurred in the former Soviet Union, we would experience similar problems because the bacterium (Corynebacterium diphtheriae) is still present, living in the throats of asymptomatic carriers.
UNEXPLAINED EMERGENCE
Ebola hemorrhagic fever was first recognized in 1976 in two outbreaks (one in northern Zaire and one in southern Sudan) that involved 602 persons in Africa. This rapidly progressing viral disease causes a high fever with bleeding from multiple sites and the ultimate shutdown of the major organs. The Ebola-Zaire strain of the virus was fatal in 88% of the cases, and the Ebola-Sudan strain was fatal in 53% of the cases. The third outbreak of Ebola hemorrhagic fever was in Sudan in 1979 and involved 34 persons. Another outbreak in 1994 in a Gabon mining camp killed 29 of the 49 persons infected. An outbreak in 1995 involving 315 cases spread through families and a hospital in and around Kikwit, Zaire, resulting in 255 deaths, which is a case fatality rate of 81%. Kikwit has a population of about 400,000 and is about 1000 km south of the site of the original outbreak in 1976 in the small village of Yambuku, Zaire. The Ebola viruses involved in the Kikwit and Yambuku outbreaks (even though the outbreaks occurred 19 years apart) have been shown to be almost identical. In 1996, 91 persons became infected in Gabon, and these cases may have been associated with eating an infected chimpanzee. In 2000 to 2001, an outbreak occurred in Uganda that involved 425 cases and 225 deaths, and another outbreak occurred in Gabon and the Democratic Republic of the Congo with 96 deaths among the 122 cases. Disease spread was associated with family and health care provider contacts with infected persons.
Great fear exists that Ebola hemorrhagic fever will break out in a small village and that those infected will carry the virus to a site of a larger population, causing a major epidemic and even a pandemic. In the 1995 outbreak, the fear was that the disease would spread from Kikwit to the capital of Zaire, Kinsasha, about 240 miles to the east. Maybe the reason this did not occur is that the disease progresses so rapidly that the victims die in a matter of days, which limits their contact with others. In the 1976, 1995, and 2001 outbreaks, person-to-person spread occurred through close personal contact with infected blood and other body fluids. Those infected included family members and health care providers, although the exact modes of spread still need to be better defined. An obvious problem in these outbreaks is the lack of modern medical facilities and barrier products that could have better protected health care workers from exposure to their infected patients. Additional outbreaks have occurred in the Democratic Republic of the Congo in 2001, 2002, and 2003. In 2004 an outbreak occurred in Sudan. All totaled, about 2000 cases of Ebola hemorrhagic fever have occurred, most of which have been fatal.
The natural reservoir (source) where the Ebola virus strains “hide out” between outbreaks is unknown, but attempts to identify the source are being made by culturing samples from local animals, insects, and the environment. The index patient in the 1995 outbreak is thought to have been a charcoal maker who worked in the forest near Kikwit, so this area was being analyzed very carefully. However, the cause of Ebola emergences is still unknown.
Centers for Disease Control and Prevention. Diphtheria epidemic—New Independent States of the former Soviet Union, 1990-1994. MMWR. 1995;44:177–181.
Centers for Disease Control and Prevention. Hantavirus pulmonary syndrome-United States, 1993. MMWR. 1994;43:45–48.
Centers for Disease Control and Prevention: Infectious disease information; Emerging infectious diseases. http://www.cdc.gov/ncidod/diseases/eid/index.htm. Accessed: November, 2007.
Centers for Disease Control and Prevention: MRSA in healthcare setting. Available at http://www.cdc.gov/ncidod/dhqp/ar_MRSA_spotlight_2006.html. Accessed: November 2006.
Centers for Disease Control and Prevention. Update: Vibrio cholerae O1-Western hemisphere, 1991-1994, and Vcholerae O139-Asia, 1994. MMWR. 1995;44:215–219.
Corso, P.S., et al. Cost of illness in the 1993 waterborne Cryptosporidium outbreak, Milwaukee, Wisconsin. Emerg Infect Dis. 2003;9:426–431.
Huang, C., et al. First isolation of West Nile virus from a patient with encephalitis in the United States. Emerg Infect Dis. 2002;8:1367–1371.
Kurashina, K., Horda, T. Nosocomial transmission of methicillin-resistant Staphylococcus aureus via the surfaces of the dental operatory. Brit Dent J. 2006;201:297–300.
Morse, S.S. Factors in the emergence of infectious diseases. Emerg Infect Dis. 1995;1:7–15.
Stratton, C.W. Dead bugs don’t mutate: susceptibility issues in the emergence of bacterial resistance. Emerg Infect Dis. 2003;9:10–16.
Wilson, M.E. Travel and the emergence of infectious diseases. Emerg Infect Dis. 1995;1:39–46.
Review Questions
______1. An emerging disease is a disease that:
a. has not been recognized before
b. has been known to occur for more than 20 years
______2. Hand-foot-and-mouth disease caused by a coxsackievirus was first recognized in:
______3. What caused hantavirus pulmonary syndrome to emerge?