Oral and Respiratory Diseases
After completing this chapter, the student should be able to do the following:
 List infectious diseases that occur in the mouth.
List infectious diseases that occur in the mouth.
 List systemic diseases that may produce oral lesions.
List systemic diseases that may produce oral lesions.
 List respiratory infectious diseases that may be spread in the dental office.
List respiratory infectious diseases that may be spread in the dental office.
 List all the known herpesviruses and the diseases they cause.
List all the known herpesviruses and the diseases they cause.
 List waterborne disease agents that may be spread through contaminated dental unit water.
List waterborne disease agents that may be spread through contaminated dental unit water.
ORAL DISEASES
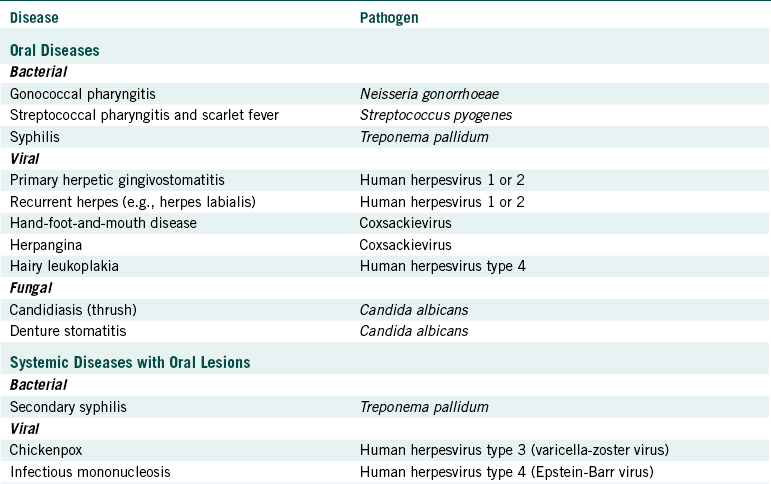
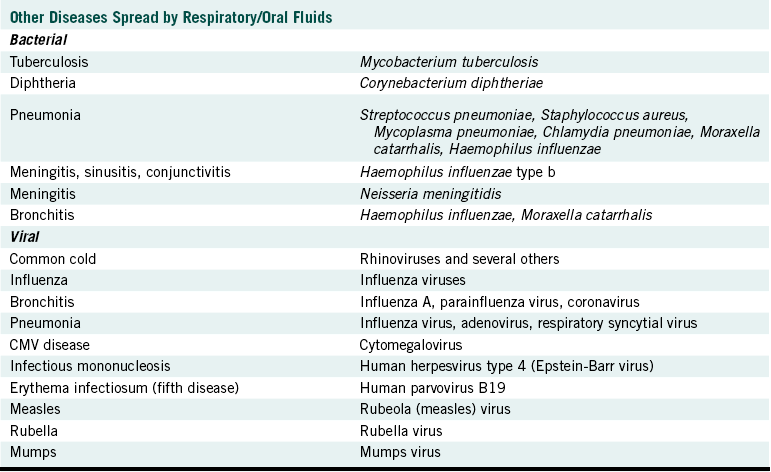
Chapter 5 discussed the plaque-associated diseases of caries and periodontal diseases. This chapter presents information on other oral diseases and respiratory diseases that may be spread in a dental office (Table 7-1). A key aspect of the potential for spread of respiratory diseases in the dental office is that dental patients (and many other persons) are asymptomatic carriers of a variety of pathogens present in their oral or respiratory fluids (Table 7-2).
Human Herpesviruses Types 1 and 2
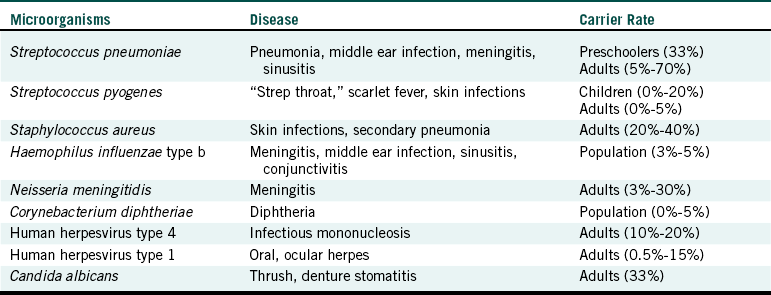
Human herpesviruses cause several diseases (Table 7-3). Human herpesvirus type 1 (herpes simplex virus 1) may cause infections of the mouth, skin, eyes, and genitals, and those who have depressed immune systems (who are immunocompromised) may have a widespread (systemic) infection.
TABLE 7-3
| Type | Other Name | Disease |
| HHV 1 | Herpes simplex type 1 | (HSV-1) Oral, ocular, and some genital herpes |
| HHV 2 | Herpes simplex type 2 | (HSV-2) Genital herpes, some oral herpes |
| HHV 3 | Varicella-zoster virus | (VZV) Chickenpox, shingles |
| HHV 4 | Epstein-Barr virus | (EBV) Infectious mononucleosis, hairy leukoplakia of tongue |
| HHV 5 | Cytomegalovirus | (CMV) CMV disease, retinitis |
| HHV 6 | None | Roseola |
| HHV 7 | None | Not yet known |
| HHV 8 | None | Kaposi’s sarcoma |
About 90% of adults have been infected with human herpesvirus 1. Only 10% of infected persons (usually children) experience the typical symptoms of oral herpes (primary herpetic gingivostomatitis). In this disease, vesicle-type lesions occur in the mouth. Most (if not all) herpesviruses cause recurrent diseases (periodic recurrence of the disease). An example is herpes labialis, sometimes called fever blisters, with lesions periodically appearing on the lips. During active human herpesvirus 1 infections, vesicles at any site of the body contain the virus, which may be spread to others by direct contact with these lesions. The human herpesvirus 1 also may be present in saliva in those with oral or lip lesions and in a small percentage of those who are infected but have no active lesions (see Table 7-2). In such instances, direct contact with lesions may cause infection of the skin, or sprays or aerosols of the saliva may result in spread of the virus to unprotected eyes of the dental team. Entrance of the virus through breaks in the skin on unprotected hands and fingers can lead to vesicle development at these sites called herpetic whitlow. Chapter 10 describes a vivid example of how the human herpesvirus 1 may be spread from a lip lesion of one patient to the mouths of other dental patients via the ungloved hands of a dental hygienist. Human herpesvirus 1 causes about 10% of genital herpes cases.
Human herpesvirus type 2 (herpes simplex virus 2) causes about 90% of genital herpes infections but occasionally causes oral infections. Although most infections are asymptomatic, human herpesvirus 2 can cause vesicle-type lesions in the mouth or on the skin in the male and female genital and anal areas or internally in the female. As with other herpesvirus infections, these vesicles may recur periodically. The vesicles contain the virus and are contagious on contact, but the virus also can be spread in the absence of symptoms. Genital herpes is one of the most common sexually transmitted diseases.
Treatment of herpesvirus infections with acyclovir usually reduces the severity and duration of the disease but does not prevent the recurrence of disease. Acyclovir is structurally similar to guanosine triphosphate, which is a building block for DNA. When acyclovir is incorporated into the viral DNA being synthesized inside of body cells infected with the virus, that DNA becomes nonfunctional, and the virus does not survive.
Oral Candidiasis
Candida albicans is a yeast that occurs in the mouth asymptomatically in about one third of adults. The yeast is an opportunistic pathogen usually causing a harmful infection only under special circumstances that give it an advantage to multiply to harmful levels. Such harmful infections are referred to as oral candidiasis and appear as whitish lesions (called thrush) or reddish areas (denture stomatitis). Circumstances that may result in oral disease might include the following:
• Conditions that disturb body defense mechanisms such as the systemic diseases of human immunodeficiency virus (HIV) infection and leukemia
• Long-term broad-spectrum antibacterial therapy that gives the unaffected yeast a better chance to grow
• Trauma to the mouth from poorly fitting dentures causing C. albicans to produce denture stomatitis
• Poor resistance in the mouth of newborns orally contaminated with the yeast during passage through mother’s infected birth canal
Yeast infections with C. albicans may occur at other sites of the body, including the skin and the vagina. Infections in the vagina are the cause of “yeast infections” in females.
Spread of C. albicans from a patient’s mouth to the dental team is theoretically possible through direct contact with lesions or sprays or aerosols of infected saliva. However, unless the contaminated member of the dental team has lowered body defenses, the contamination likely will not lead to a harmful infection.
Oral candidiasis can be treated with one of several antifungal agents, which include nystatin, ketoconazole, and clotrimazole.
Oral Syphilis and Gonorrhea
Other important oral disease agents that may have some potential for spread to the dental team are Treponema pallidum and Neisseria gonorrhoeae.
Treponema pallidum is a spirochete bacterium and is the causative agent of syphilis. About 5% to 10% of the cases of syphilis first occur in the mouth in the form of a lesion called a primary chancre, an open ulcer frequently on the tongue or lip. These lesions contain the live spirochetes, which may be spread by direct contact. The possibility of the spirochete entering small cuts or breaks in the skin of unprotected hands of the dental team exists and has been documented, in one instance causing syphilis of the finger.
Neisseria gonorrhoeae causes another sexually transmitted disease, gonorrhea, which is an infection through the mucous membranes inside the penis or vagina. This gram-negative bacterium may be spread to the mouth during certain sex practices with an infected person, and the bacterium might cause an inflammation of the throat area. Although spread of N. gonorrhoeae from a patient with oral gonorrhea to a member of the dental team has never been documented, some potential may exist for this to occur during generation of dental aerosols. Neisseria gonorrhoeae can cause eye infections.
Herpangina and Hand-foot-and-mouth Disease
Herpangina appears as vesicles on the soft palate or elsewhere in the posterior part of the mouth that break down to ulcers that last for about a week. Seldom do the vesicles appear on the gingiva, buccal mucosa, or tongue, which differentiates this disease from intraoral herpes infections. Fever, sore throat, and headache frequently accompany the vesicular stage. The lesions are caused by specific types of coxsackievirus (usually group A types 1 to 6, 8, 10, and 22). Coxsackievirus (usually type A16) also may cause a vesicular type of disease, with vesicles occurring in the mouth, on the hands, and on the feet (hand-foot-and-mouth disease). In this instance, the oral vesicles occur primarily on the cheek mucosa and tongue but sometimes on the hard palate and anywhere else in the mouth. Usually children and young adults are affected; no specific treatment is available that attacks the virus.
SYSTEMIC DISEASES WITH ORAL LESIONS
In untreated syphilis a secondary phase of the disease may appear 2 to 10 weeks after the initial lesion occurs and has subsided. This secondary phase results from spread of the T. pallidum bacteria from the initial lesion through the blood and may involve the appearance of mucous patches on mucous membranes in the mouth. The lesions contain the live spirochetes and may be spread to others by direct contact. Syphilis usually responds to penicillin therapy.
Chickenpox
Human herpesvirus type 3 (varicella-zoster virus) causes chickenpox as the primary disease (usually in the young) and shingles as the recurrent disease (usually in those over age 50). Although chickenpox commonly produces skin lesions, this disease is classified as a respiratory disease. Human herpesvirus 3 enters the body by droplet infection, invades the respiratory tract, and is spread through the bloodstream to the skin and other organs. After about 2 weeks, vesicles frequently occur in the mouth in addition to those typically present on the skin. The virus is spread through saliva and nasal secretions in addition to contact with skin lesions.
The disease is highly contagious through droplet infection and is usually mild in children but can be more severe in teenagers and adults. Occasionally an adult who escaped the primary infection as a child develops chickenpox, which is usually more severe and has a higher mortality rate because of an increased incidence of encephalitis. A vaccine for chickenpox was cleared by the U.S. Food and Drug Administration in 1996 and is described further in Chapter 9.
Infectious Mononucleosis
Human herpesvirus type 4 (Epstein-Barr virus) usually causes no or mild symptoms after infecting a child but may cause infectious mononucleosis (also known as the kissing disease) in adolescents and young adults. As might be suspected, this virus is spread from person to person through contact with saliva but also occasionally through blood transfusions. Symptoms of infectious mononucleosis commonly include fever, malaise, anorexia, fatigue, sore throat, oral ulcers, and enlarged cervical lymph nodes (those under the jaw). Other oral manifestations may include palatal petechiae (small red areas), widespread erythema (reddening) of the oral mucosa, and swelling of the uvula. This virus also is associated with hairy leukoplakia (whitish lesions on the tongue) and with malignancies such as Burkitt’s lymphoma, B cell lymphoma in the immunocompromised, and nasopharyngeal carcinoma.
RESPIRATORY DISEASES
Streptococcus pyogenes (sometimes called β-hemolytic, group A streptococcus) causes streptococcal pharyngitis (“strep throat”) and scarlet fever. Scarlet fever is “strep throat” with a skin rash. Streptococcus pyogenes is spread by droplet infection from mouth to mouth, and a few persons who become infected experience poststreptococcal complications resulting in rheumatic fever or kidney damage. Each subsequent infection with S. pyogenes or with some other streptococci can result in progressively more damage to the heart (rheumatic heart disease) or the kidney. This is why patients with a history of poststreptococcal diseases are protected from possible reactivation by receiving antibiotics before dental or medical care.
Certain protease-producing strains of S. pyogenes (sometimes referred to as “flesh-eating” bacteria) can cause a condition called necrotizing fasciitis, which produces rapidly spreading damage to muscle tissue. Fortunately, only about 1000 cases of this disease occur each year.
Children and adults carry S. pyogenes in their nose and throat area without having any symptoms and can spread the organism to others in respiratory droplets (see Table 7-2). Most harmful streptococcal infections respond well to penicillin therapy.
Tuberculosis
Tuberculosis is a lung infection caused by the bacterium Mycobacterium tuberculosis. Although tuberculosis is not a particular problem among dental professionals, it is a major health problem worldwide. About 10 million new cases of tuberculosis and 3 million associated deaths occur annually worldwide. In the United States, tuberculosis is increasing among racial/ethnic groups (non-Hispanic blacks, Hispanics, Asian/Pacific Islanders, Native Americans/Alaskan natives), but the overall number of cases has reached a plateau for the last 4 years. In 1990 almost 70% of all reported cases of tuberculosis in the United States occurred among these minorities. Between 1953 and 1984, the number of reported cases of tuberculosis in the United States steadily declined. This number began to increase through 1995, when it began to level off. In 1996 the Centers for Disease Control and Prevention (CDC) indicated that about 22,000 active tuberculosis cases were reported in the United States. In 2006 13,779 TB cases were reported to CDC from the 50 states and the District of Columbia (DC), representing a 2.1% decrease from 2005.
Adverse social conditions and economic factors, the epidemic of acquired immunodeficiency syndrome (AIDS), and immigration of persons with tuberculosis are contributing factors to the occurrence of tuberculosis in the United States. Tuberculosis is a major problem among the homeless, persons infected with HIV, and drug abusers. Tuberculosis in those with HIV disease is commonly a reactivation of an earlier asymptomatic infection, as described subsequently.
TUBERCULOSIS IN THE DENTAL OFFICE
The risk for the dental team of acquiring tuberculosis is low because prolonged exposure to an infectious environment usually is required for infection to occur, and brief contact appears to be of little risk. Spread from one person to another relates to closeness of contact and the duration of exposure to infectious droplets. Thus the key factor in spread is the concentration of infectious particles in the inhaled air. Respiratory aerosols remain airborne for several hours, but the concentration of the infectious particles decreases with time from dilution with “clean” air and eventual settling. Nevertheless, tuberculosis is acquired by breathing in respiratory droplets from an infectious person with active pulmonary tuberculosis, and the dental team must be concerned by such transmission.
The dental office should have a protocol for identifying patients who possibly have active pulmonary tuberculosis. These patients should be referred immediately for medical evaluation and have their dental care deferred until the tuberculosis is inactive or has been treated and is no longer infectious. Dental personnel should not treat patients with active tuberculosis unless they institute special isolation precautions that are usually only available in hospital clinics. The approach to the management of possible active tuberculosis patients is that described by the CDC. The CDC has published guidelines for the prevention of tuberculosis in dental health care facilities (see Appendix C).
Box 7-1 shows the risk factors for tuberculosis and the symptoms of active tuberculosis and also describes questions on a medical history that may help identify dental patients who possibly have active tuberculosis.
DISEASE PROCESS
If enough inhaled M. tuberculosis bacteria reach the lung alveoli and begin to multiply, one is said to be infected. In most persons the inflammatory and immune responses control the infection, with the only evidence of infection being a positive tuberculin skin test (see the following discussion). Cells of M. tuberculosis initially resist destruction after being engulfed by macrophages during the inflammatory response. However, after immunity develops (cell-mediated immune response; see Chapter 3), the macrophages are activated to be able to kill the engulfed bacteria and the infection does not progress to active disease. However, most infected persons (even if the cell-mediated immune response initially controls the infection) cannot completely rid the body of the tuberculosis bacteria unless they take antituberculosis drugs. For this reason, those with positive tuberculosis skin tests, even if they have never had any tuberculosis symptoms, usually are placed on a course of antituberculosis drug therapy. Patients not placed on antituberculosis drug therapy retain the bacteria in their bodies and may later progress to active disease (latent tuberculosis infection or reactivation tuberculosis).
About 10% of persons infected with M. tuberculosis progress from infection to active disease with symptoms. About half of these progress to active disease soon after the primary infection, and about half progress later in their lives. Symptomatic pulmonary tuberculosis begins with the development of an exudative condition in the lung, like pneumonia. Continued disease results in a granulomatous reaction (consolidation of tissue around the lung infection site), referred to as tubercle formation. As the disease progresses, these tubercles enlarge, may become necrotic (caseation necrosis), and break down, producing cavities (open spaces) in the lung tissue. In persons who are infected but are asymptomatic and in those with symptomatic tuberculosis, healing may occur with or without the formation of calcified lung lesions or nodules, or development of fibrous tissue with calcium deposits.
Because M. tuberculosis can survive inside of macrophages early in the infection, this bacterium can be disseminated throughout the body (wherever the macrophages go). If active disease occurs, complications may develop that can involve infections in essentially any organ of the body.
MULTIPLE DRUG-RESISTANT MYCOBACTERIUM TUBERCULOSIS
Another disturbing fact about tuberculosis is that strains of M. tuberculosis that are resistant to the drugs normally used to treat this disease recently have emerged. These strains are causing outbreaks of multiple drug-resistant tuberculosis. The CDC reported that about 15% of all tuberculosis cases tested involved strains resistant to at least one antituberculosis drug (e.g., isoniazid, rifampin, and ethambutol) and 4% were resistant to both of the two most effective antituberculosis drugs. Most of the patients involved in outbreaks of multiple drug-resistant tuberculosis have been AIDS patients; others include hospital patients and institutionalized inmates. Transmission of multiple drug-resistant tuberculosis to hospital workers and prison guards is documented. The key approach to managing these infections is to diagnose the infection and analyze the causative strain of M. tuberculosis as soon as possible so that the proper antituberculosis drugs can be administered at the earliest possible moment.
TUBERCULIN SKIN TEST
The Mantoux test, or purified protein derivative (PPD) test, is used to screen for tuberculosis infection. Purified protein derivative is prepared from cultures of M. tuberculosis and is used in the skin testing. The testing involves injecting a small amount of the PPD just under the skin (intradermally) on the underside of the forearm. The injection site is observed 48 to 72 hours later for any reaction to the PPD, although a positive reaction in some may be delayed for a week. A positive reaction is the occurrence of induration (a hardening, small nodule) at the injection site, and the degree of the positive reaction is determined by measuring the diameter of the indurated site. Box 7-2 gives the CDC guidelines for interpreting the tuberculin skin test results.
VACCINATION
A vaccine for prevention of tuberculosis has not been cleared for use in the United States. However, the bacille Calmette-Guérin vaccine is used widely throughout the rest of the world. This vaccine consists of a live attenuated (weakened) bovine strain that probably causes a nonprogressing infection as a substitute for infection with virulent tuberculosis strains. Not everyone who receives the vaccine is protected, but those who are vaccinated become PPD–tuberculin skin test positive. In such persons the skin test becomes useless as an aid for diagnosing genuine M. tuberculosis infection.
Streptococcus Pneumoniae
Many bacterial and viral agents can cause pneumonia, but Streptococcus pneumoniae is of particular importance. Until 2000, S. pneumoniae infections caused 60,000 cases of invasive disease each year and up to 40% of these were caused by pneumococci nonsusceptible to at least one drug. These figures have decreased substantially following the introduction of the pneumococcal conjugate vaccine for children. In the year 2002, there were 37,000 cases of invasive pneumococcal disease. Of these, 34% were caused by pneumococci nonsusceptible to at least one drug and 17% were due to a strain nonsusceptible to 3 or more drugs.
Streptococcus pneumoniae normally exists in the nose and throat area of human beings and is carried asymptomatically in preschoolers and adults (see Table 7-2). The bacterium is spread by droplet inhalation of respiratory/oral droplets. This bacterium also is the leading cause of middle ear infections in children and can cause bacterial meningitis, an inflammation of the membranes around the brain. A vaccine is available for the most common types of S. pneumoniae and is recommended for the elderly or others who may be predisposed to lung infections.
Human Herpesvirus Type 5
Human herpesvirus type 5 (cytomegalovirus) usually causes no symptoms on primary infection but occasionally causes disease in newborns and immunocompromised persons. The virus can be spread by contact with saliva, vaginal secretions, semen, breast milk, blood, and transplanted tissue. Human herpesvirus 5 can cause a congenital disease called cytomegalic inclusion disease that has a high fatality rate and causes mental retardation, neurologic problems, deafness, and possible damage to many internal organs. Infection in otherwise healthy adults is usually asymptomatic but may cause symptoms like those of infectious mononucleosis. Infection of immunosuppressed persons or those with AIDS can be devastating and may involve transplant patients receiving immunosuppressive drugs. Conditions that may develop in such persons include pneumonia, gastroenteritis, and hepatitis. Cytomegalovirus retinitis occurs in about 10% to 15% of AIDS patients, and cytomegalovirus colitis or cytomegalovirus esophagitis occurs in about 10% of AIDS patients.
Human Herpesviruses Types 6, 7, and 8
Human herpesvirus type 6 commonly is isolated from saliva and recently was identified as the cause of roseola (exanthema subitum). Roseola occurs as a high fever and a skin rash in infants. This virus also may cause infectious mononucleosis symptoms in some adults. Human herpesvirus type 7 also is isolated from saliva in as many as 70% to 80% of adults and children but has not yet been associated clearly with any particular disease state. Human herpesvirus type 8 has been associated recently with Kaposi’s sarcoma, a condition seen in many AIDS patients.
Influenza
The regularly occurring (seasonal) influenza is described in Chapter 9. The H1N1 influenza occurring in humans is caused by a new (novel) influenza virus. The first cases in the United States occurred in April 2009. Flu viruses spread mainly from person to person when people with influenza cough or sneeze or when a person touches something – such as a surface or object– with the flu virus on it and then touches his or her mouth or nose.
Laboratory tests originally showed that many of the genes in this new virus were very similar to influenza viruses that normally occur in pigs (swine) in North America. Further study has shown that this new virus is very different from what normally circulates in North American pigs. It has two genes from flu viruses that normally circulate in pigs in Europe and Asia and bird (avian) genes and human genes. Scientists call this a quadruple reassortant virus.
The symptoms of H1N1 flu virus in people include fever, cough, sore throat, runny or stuffy nose, body aches, headache, chills, and fatigue. Some people may experience vomiting and diarrhea. People infected with the flu, including the H1N1 type, can have respiratory symptoms without a fever. Illness with the new H1N1 virus has ranged from mild to severe. Although most people who have been sick have recovered without needing medical treatment, hospitalizations and deaths from infection with this virus have occurred.
In seasonal flu, certain people are at “high risk” of serious complications. This includes people 65 years and older, children younger than 5 years old, pregnant women, and people of any age with certain chronic medical conditions, such as diabetes, heart disease, asthma, and kidney disease. About 70% of people hospitalized with H1N1 virus infection have had one or more medical conditions previously recognized as “high risk” for serious seasonal flu-related complications.
One thing that appears to differentiate the H1N1 virus from seasonal influenza is that adults older than 64 years do not yet appear to be at increased risk of H1N1-related complications. CDC laboratory studies have shown that no children and very few adults younger than 60 years old have existing antibody to H1N1 flu virus; however, about 1/3 of adults older than 60 years may have antibodies against this virus. It is unknown how much, if any, protection against novel H1N1 flu can come from existing antibodies.
People infected with either seasonal or H1N1 flu shed virus and may be able to infect others from 1 day before getting sick to 5 to 7 days after the onset of symptoms, which is 2-3 days longer than traditional seasonal influenza. This infection period can be longer in some individuals, especially children and people with weakened immune systems and those infected with the new H1N1 virus. Immunization against H1N1 influenza is described in Chapter 9.
Other Respiratory Diseases
Table 7-1 lists other respiratory diseases that are spread by inhalation of infected respiratory/oral droplets. These include diseases caused by about 170 different types of viruses and involve influenza, the common cold, pneumonia, croup, bronchitis, erythema infectiosum, measles, mumps, and rubella. Additional bacteria are involved in causing bacterial pneumonias, meningitis, and diphtheria.
WATERBORNE DISEASE AGENTS
Many disease agents may be spread through contaminated water, including those that cause cholera, Shigella and amebic dysentery, salmonellosis, Escherichia coli colitis, cryptosporidiosis, and hepatitis A and E. Because these disease agents are not known to be spread in dental offices, they are not discussed further. However, numerous studies show that the water inside dental units and hoses for water-spray handpieces and the air/water syringes are contaminated heavily with bacteria. The level of these bacteria in dental unit water is much greater than that of tap water. When waterborne bacteria enter the dental unit, they attach to the inside walls of the water lines. These bacteria then form a biofilm on the inside of water lines that releases bacteria as the water flows out of the lines (for further discussion see Chapter 13). Although 30 to 40 different types of bacteria may be present in dental unit water, two are of particular interest because of their potential for causing opportunistic infections. One (Legionella pneumophila) causes Legionnaires’ disease and Pontiac fever, and the other (Pseudomonas aeruginosa) is an opportunistic pathogen that can cause several harmful infections.
Legionnaires’ Disease
Legionella pneumophila is a gram-negative rod-shaped bacterium that causes about 70% of the cases of Legionnaires’ disease. This disease is a pneumonia and was named after first being recognized among attendees of an American Legion convention in Philadelphia in 1976. L. pneumophila and more than 30 other species of Legionella commonly exist in natural and domestic waters, but most of the cases of Legionnaires’ disease are presumed to result from inhalation of water from water-handling systems rather than from lakes or streams. Such handling systems include air conditioning cooling towers, humidifiers, ultrasonic nebulizers, vegetable misters, respiratory therapy equipment, shower heads, industrial sprayers, and water distribution systems in some buildings.
One acquires lung infections with L. pneumophila by inhaling contaminated water or by aspirating the bacterium after it has colonized the oropharyngeal area. The infection progresses to pneumonia mostly in those who have some weakened body defenses. Erythromycin is used for treatment, and spread of the disease from person to person has not been documented.
Pontiac fever (named after the site in Michigan of the first recognized outbreak) also is caused by L. pneumophila, but this disease is not a pneumonia. Instead, the disease is an acute self-limiting condition involving flulike symptoms of fever, chills, muscle aches, headache, mild cough, and sore throat.
Although no scientific documentation exists for spread of Legionnaires’ disease in the dental office, about 10% of dental offices apparently have Legionella in the dental unit water used for patient care. Thus, some patients possibly may be exposed to this bacterium from some dental units. Comparison of past antibody response to Legionella in dental personnel with the same antibody response in nondental personnel in two separate studies also revealed that the dental personnel had a higher exposure incidence to Legionella. Thus some dental personnel at least may be exposed to Legionella by contact with aerosols from dental unit water coming out of high-speed handpieces, ultrasonic scalers, and air/water syringes.
Pseudomonas Infection
A report from England shows that two cancer-weakened dental patients acquired oral infections with P. aeruginosa that originated from dental unit water. The same study also showed that an additional 78 patients treated at the same dental unit were colonized orally for 4 to 10 weeks by the P. aeruginosa present in the dental unit water. However, none of these patients developed harmful infections with the Pseudomonas bacterium, presumably because they were not cancer-weakened or otherwise compromised. Pseudomonas aeruginosa is an important opportunistic pathogen (see Chapter 3). The bacterium occurs widely in nature and is present in low numbers in the municipal water used in a dental unit.
In addition to waterborne bacteria, dental unit water may contain low numbers of oral bacteria. Retraction of oral bacteria back into the handpiece and air/water syringes and their connecting water lines may occur when these instruments are turned off after use in the mouth. Some dental units (depending on how they are constructed) contain antiretraction valves to prevent this from occurring, but these valves fail periodically.
The CDC and the American Dental Association indicate the following:
• Dental unit water should not be used to irrigate surgical sites in which bone is exposed.
• Water lines should be flushed at the beginning of the day to reduce temporarily the number of waterborne bacteria that may have accumulated in the water overnight.
• Water lines should be flushed between patients to reduce the number of oral microorganisms that may have been retracted into the lines after each patient.
Chapter 13 gives information on how to improve the microbial quality of dental unit water.
Centers for Disease Control and Prevention: Drug-resistant Streptococcus pneumoniae disease. http://www.cdc.gov/ncidod/dbmd/diseaseinfo/drugresisstreppneum_t.htm. Accessed November 2007.
Centers for Disease Control and Prevention. Guidelines for prevention of the transmission of Mycobacterium tuberculosis in health-care facilities. MMWR. 43(RR-13), 1994.
Centers for Disease Control and Prevention, National Center for Infectious Diseases: Infectious diseases information. http://www.cdc.gov/ncidod/diseases/index.htm. Accessed December 2007.
Centers for Disease Control and Prevention: Tuberculosis 2006 at http://www.cdc.gov/tb/surv/surv2006/pdf/FullReport.pdf. Accessed November 2007.
DePoala, L.G., et al. A review of the science regarding dental unit waterlines. J Am Dent Assoc. 2002;133:1199–1206.
Donlon, R.M. Biofilms microbial life on surfaces. Emerg Infect Dis. 2002;8:881–890.
Glick, M., Goldman, H.S. Viral infections in the dental setting. J Am Dent Assoc. 1993;124:79–86.
Miller, C.H. Microbes in dental unit water. J Calif Dent Assoc. 1996;24:47–52.
Miller, C.H., Cottone, J.C. The basic principles of infectious diseases as related to dental practice. Dent Clin North Am. 1993;37:1–20.
Musher, D.M. How contagious are common respiratory tract infections? New Engl J Med. 2003;348:1256–1266.
Review Questions
______1. Which of the following microbes causes thrush and denture stomatitis?
______2. Herpetic whitlow is an infection of the:
______3. Those who have shingles previously had:
______4. Herpangina and hand-foot-and-mouth disease are caused by the same group of viruses called:
______5. The bacterium that causes strep throat also causes necrotizing fasciitis and:
______6. Which of the following is not true about tuberculosis?
a. Tuberculosis is a common occupational disease of dental workers.
b. Tuberculosis is a major health problem worldwide.
c. Human immunodeficiency virus disease and homelessness are risk factors for tuberculosis.
______7. Where does Streptococcus pneumoniae (causes lobar pneumonia) normally exist when it is not causing disease?
______8. Where does Legionella pneumophila (causes Legionnaires’ disease) normally exist when it is not causing disease?
______9. What bacterium in dental unit water has been shown to cause oral disease in immunocompromised patients?
______10. Specific oral lesions are caused by all of the following except:
______11. Which of the following statements about the bacille Calmette-Guérin vaccine for tuberculosis is not true?
a. The vaccine is cleared for use in the United States.
b. The vaccine is used widely outside the United States.
c. Not everyone who receives the vaccine is protected.
d. Vaccinated individuals show a positive skin test for tuberculosis.
______12. Which of the following microbes are well known for causing periodic recurrences after the initial infection?
______13. An opportunistic pathogen causes disease only:
b. under special circumstances that give it an advantage to multiply to harmful levels
______14. All of the following except one are herpesviruses. The exception is:
______15. All of the following except one are sexually transmitted diseases that may produce oral lesions. The exception is: