Chapter 3 Statutory framework for practice
Introduction
This chapter provides an overview of the history of midwifery regulation, midwifery legislation ensuring protection of the public, and the rules and codes by which midwives are supported. The role of midwifery supervision is discussed, as well as how this differs from but works in conjunction with midwifery management, and is an integral component of clinical governance.
It is vital that midwives grasp the fundamentals of the unique professional support provided by midwifery supervision and use it to improve the quality of care given to women and their babies.
Legislation regulating the midwifery profession
Historical background
The first Midwives Act in 1902 sanctioned the establishment of a statutory body, the Central Midwives’ Board for England and Wales (CMB), prescribed its constitution and laid down statutory powers. This Act was amended in 1918, 1926, 1934, 1936 and 1950. The Midwives Act of 1951 consolidated all previous Acts.
The Nurses, Midwives and Health Visitors Act of 1979 set up the United Kingdom Central Council (UKCC) and four country boards and established a combined statutory structure for nursing, midwifery and health visiting in the UK. It established a register of the three professions, containing 15 parts, to include the different specialities of nursing. Midwives registered on Part 10. This was the first time midwives were amalgamated in law with other professional groups.
A separate Midwifery Committee was set up in Statute following protests from the Royal College of Midwives (RCM) and Assocation of Radical Midwives (ARM) that midwives would be over-ruled by nurses (Jowitt & Kargar 1997).
However, in 1987, professional-specific education officers were replaced by generic education officers. Despite protest from members at the time, the Midwifery Committee was overruled on this matter.
Ten years later, an external review of the 1979 Act was commissioned by the Health Department. This resulted in a smaller, directly elected, central council with smaller appointed national boards. The responsibility for funding nursing and midwifery education was removed and delegated to regional health authorities. National boards remained responsible for course validation and accreditation only.
Government proposals that followed in Working Paper 10 (DH 1989) suggested setting up the purchaser–provider model – hospitals would contract with education providers for the requisite number of places to fulfil local workforce planning. These recommendations were accepted by the Government (DH 1991, Northern Ireland Office 1991, Scottish Office 1991) and were incorporated into the 1992, Nurses, Midwives and Health Visitors Act, including the revised structure of the UKCC and national boards. Consolidation of the 1979 and 1992 Acts, incorporating all the reforms, was made in the 1997 Nurses, Midwives and Health Visitors Act.
Reform of the health professions
The drive to strengthen control of the healthcare professions followed several scandals involving the nursing (Clothier et al 1994) and medical professions (DH 2002a). In 1997, a further review of nursing and midwifery legislation was commissioned by the four UK health departments and complete reform of the UKCC and four national boards was recommended (JM Consulting 1998).
In February 1999, the government response accepted the need for new regulation of the ‘various health professions’ and proposed an amendment to the new Health Bill in progress at the time ‘to make provision to repeal the Nurses, Midwives and Health Visitors Act 1997’ (NHS Executive 1999).
Replacement legislation, by Order, regulating the professions was to be made subject to full consultation and publication of the Order in Draft. The Regulation of Health Care and Associated Professions under Clause 47(2) and Schedule 3.1 of the Health Bill clearly stated the scope of the Secretary of State’s powers of regulation via an ‘Order’ following a period of 3 months’ consultation.
The haste to replace primary legislation and substitute it with a Statutory Instrument by ‘Order’ for Nursing and Midwifery was a departure from the normal practice of parliamentary procedure customary during the previous century. Nursing and midwifery legislation had previously been subject to professional scrutiny throughout all the earlier stages, including publication of Green and White Papers. The midwifery protests to the restrictions of the legislation went unheeded.
Current legislation regulating midwifery
Health Act 1999 (Section 60) (DH 1999)
The current legislation for midwives drawn up under Section 62(9) of the Health Act 1999 (DH 1999) set out the Order for the establishment of the Nursing and Midwifery Council (NMC).
Modernising regulation – the new Nursing and Midwifery Council – a consultation document (NHS Executive 2000)
This consultation document proposed the new structure of the UK body: the Nursing and Midwifery Council (NMC). It recommended a smaller, more transparent Council with equal representation of elected nurses, midwives and health visitors from each country. In addition, it proposed lay membership that would be almost equal numerically to the professional membership, with a lay chair. Partnership with the public was important to reduce concern about safety issues with self-regulation.
Establishing the new Nursing and Midwifery Council (DH 2001a)
The Government drafted new legislation, with the NMC directly responsible to the independent Privy Council rather than the Secretary of State, thus removing a possible source of bias as the main employer of nurses and midwives.
Modernising regulation in the health professions – NHS consultation document (DH 2001b)
The NHS Plan (DH 2000) proposed the establishment of a UK Council of Health Regulators to act as a forum and coordinate complaints from all the professions and their regulatory bodies.
This framework was also suggested in the Kennedy report on the Bristol Royal Infirmary Inquiry (DH 2002a). This Council would be independent of the State and accountable to Parliament, as would all the professional regulatory bodies, through the new Council. This, in turn, would have the power to require changes to the regulatory framework. It would not have the power to take over or intervene in individual fitness-to-practise cases.
Nursing and Midwifery Order 2001 Statutory Instrument 2002 No. 253 (DH 2002b)
The Orders to establish the Nursing and Midwifery Council were set out in Draft and laid before Parliament in October 2001 for approval under Section 62(9) of the Health Act 1999. Royal Assent was given in February 2002. The Nursing and Midwifery Order 2001 came into force and the UK Nursing and Midwifery Council commenced office on 1 April 2002.
Trust, assurance and safety – the regulation of health professionals in the 21st century CM 7013 (DH 2007a)
This White Paper set out a major reform of the UK health professions following two reviews of professional regulation, ‘The regulation of non-medical healthcare professions’ (DH 2006a) and ‘Good doctors, safer patients’ (DH 2006b), and recommendations of the Fifth Report of the Shipman Inquiry (HM Government 2004) and recommendations of the Ayling, Neale and Kerr/Haslam Inquiries (HM Government 2007a, 2007b). It changed several areas:
It included changes to the size and membership of the Council for Healthcare Regulatory Excellence (CHRE), established in 2003 (DH 2002c) to promote best practice in regulating health professionals.
In response to a request for the CHRE to expedite its annual performance review by the Minister of State for Health in March 2008, a special report identifed areas of weakness in the management of fitness to practise by the NMC, and other issues related to approval of education provision and governance (CHRE 2008).
Recommendations were made resulting in improvements in processing cases in a timely fashion using an integrated IT case-management system, improved training of panellists on child protection issues, and improved governance with greater transparency to stakeholders. The report included referral to the Charity Commission as the NMC is a registered charity.
The Health and Social Care Act (DH 2008a) later extended CHRE’s powers to include reviewing fitness to practise where health is an issue and set up the Care Quality Commission.
The Nursing and Midwifery (Amendment) Order 2008 (DH 2008b)
This amended Paragraphs 16, 17 and 18 of Schedule 1 of the Nursing and Midwifery Order 2001 in direct response to the DH White Paper ‘Trust, assurance and safety’ (DH 2007a) and the Health and Social Care Act (DH 2008a). It updated the size and membership of the NMC Council, the Midwifery Committee and Practice Committees (Box 3.1) and came into force in January 2009.
Nursing and midwifery council
Core functions
The primary function of the NMC is as a regulator of the professions, thereby safeguarding the public, through:
The Council has the power to remove a person from the Register, thus preventing the individual from practising as a nurse, midwife or health visitor. It also has a statutory duty to inform and educate registrants and to inform the public about its work.
Membership
The Council consists of 14 members (seven registrants and seven lay members) appointed by the Appointments Commission on behalf of the Privy Council.
Role and functions of the NMC Statutory Committees
1 Midwifery Committee
The Midwifery Committee advises the NMC on any matter affecting midwifery practice (including midwives’ rules and standards), education (development of standards and guidance for pre- and post-registration midwifery education) and statutory supervision of midwives (standards for local supervising authorities and supervisors of midwives). It responds to policy trends, research and ethical issues and conducts consultations on behalf of the Council. It operates under the NMC Standing Orders 2009 (NMC 2010a).
Membership: five midwives and five lay members (at least one from each of the UK countries).
2 Investigating Committee
Panels of the Investigating Committee are responsible for considering any allegations of ‘unfitness to practise’ referred to the NMC.
A registered medical practitioner will be present if the registrant’s health is in question. These deliberations take place in private and the panel decides whether there is a case to answer. If there is, referral is made to the Health Committee or the Conduct and Competence Committee (DH 2002b). The Panel may refer immediately to an Interim Orders hearing if the registrant is thought to be an immediate threat to the public. The panel can then impose the following:
In addition, a ‘removal’ from the Register can be authorised by the Investigating Committee to correct an incorrect or fraudulent entry (NMC 2008a).
3 Health Committee
The Panel’s role is to consider: ‘any allegation referred to it by the Investigating Committee or the Conduct and Competence Committee and any application for restoration referred by the Registrar’ (DH 2002b).
4 Conduct and Competence Committee
The Panel’s role is to consider any allegations referred to it by the Investigating Committee or the Health Committee. Hearings are held in public but parts of the case may be held in private to protect the identity of the person or confidential medical evidence (NMC 2008a). A panel must consist of at least three people, and must include a lay person and a ‘due regard’ (that is, someone from the same speciality as the professional being investigated).
Conduct and Competence Committee and Health Committee Panels’ sanctions
The Conduct and Competence Committee Panel and Health Committee Panel establish, in cases referred to them, whether fitness to practise is impaired by any of the following:
All decisions are based on evidence presented at the hearing of the case. The panel will only hear information about the previous history of the ‘respondent’ and any evidence in mitigation prior to making a final decision (NMC 2010d).
The range of powers it holds in relation to sanctions are as follows:
They may decide on no further action; or make one of the following orders to the Registrar:
An appeal may be made by the registrant within 28 days of a committee’s decision.
Restoration to the Register of practitioners who have been struck off
An application may be made before the end of 5 years, or in any period of 12 months in which an application for restoration to the Register has already been made, by the person who has been struck off. The application for restoration to the Register is made via the Registrar and is forwarded to the relevant Committee that made the ‘striking-off’ order. If the Committee is satisfied that the registrant has achieved the additional education or training or experience required, then the registration fee is paid and the practitioner is restored to the Register.
If an application is unsuccessful, an appeal may be made within 28 days of the decision date. If a second or subsequent application is made while a striking-off order is in force and is rendered unsuccessful, the Committee may direct that the person be suspended indefinitely (DH 2001a).
Other requirements
The NMC are required to appoint legal assessors, medical assessors and registrant assessors to advise the Council or its committees as appropriate.
Civil Standard of Proof
The ‘Civil Standard of Proof’ was brought into force on 16th October 2008 following the DH White Paper (DH 2007a) and Health and Social Care Act 2008 (Commencement No. 3) Order 2008 (SI 2008/2717 [C. 120]) (DH 2008a). All NMC hearings have used this standard since 3rd November 2008. This means that evidence is based on the ‘balance of probabilities’ rather than the previously used ‘Criminal Standard of Proof’, where facts needed to be proved ‘beyond reasonable doubt’.
Role and functions of the NMC Non-Statutory Committees
1 Appointments Board
This board deals with the appointment, development and appraisal of Fitness to Practice panellists and processing applicants for non-Council membership of committees and local supervising authority (LSA) reviewers. It ensures relevant academic or clinical expertise on a committee and also advises Council on removal of panellists from office.
2 Audit, Risk and Assurance
This committee ensures that the business of Council is conducted with integrity and probity. It agrees internal and external auditing arrangements and management of risk. It also ensures the quality and standards for education and training are being met and approval of training institutions and programmes by monitoring the UK Quality Assurance framework contract.
3 Business Planning and Governance
This committee advises Council on all matters relating to the management of resources and the maintenance of good governance standards throughout the NMC. It appoints members to the Council, recommends any amendments to the Standing Orders or code of conduct for members, and the development, performance and appraisal of Council members (NMC 2010e).
4 Fitness to Practise
This is a strategic committee separate from the three practice committees. It advises Council on matters related to standards, conduct, performance and ethics expected of registrants (and students who are prospective registrants). It also advises on the requirements as to good character and good health expected of registrants and ensures protection of the public where fitness to practise is impaired (NMC 2004a, 2009a).
5 Professional Practice and Registration
This Committee advises on all matters relating to nursing and community public health nursing such as standards of education and training and practice guidance (midwifery standards and guidance are dealt with by the Midwifery Committee).
In addition, it advises on all aspects of registration and renewal of registration (NMC 2010f).
Functions of the NMC
Function 1: The Register
The Register is divided into parts determined by the Privy Council. There are currently three parts to the Register:
The Council determines the fee to be charged and coordinates initial registration or renewal to the Register. Visiting European Union nurses or midwives are deemed registered and can practise in the UK subject to knowledge of English and comparable qualifications (see website).
Function 2: Setting standards for education and practice
Pre-registration midwifery
The NMC is charged with establishing the pre-registration standards of education and training, including requirements for good health and good character. It ensures standards of education programmes remain high through a network of heads of midwifery education called Lead Midwives for Education (LMEs) (NMC 2010g).
It appoints ‘visitors’ to visit institutions and report back on the nature and quality of the instruction given, including facilities provided. The NMC visitors are trained for their role and are midwives drawn from the profession. Visitors are not allowed to be NMC employees or employees of the universities being visited or anyone who has a close connection with the university through, for example, lecturing. Visitors are required to complete a report summarizing the information gained and are reimbursed by the NMC for expenses incurred. If the Council is of the opinion that the standards established under Article 15(1) are not met, it may refuse to approve, or withdraw approval from, the particular institution (DH 2002b); therefore, a university would be unable to continue to teach students undertaking professional programmes until approval had been reinstated.
Institutions are required to provide information to the Council about all the programmes they offer for registration to the different parts of the Register.
Pre-registration midwifery standards and fitness to practise
A review of pre-registration midwifery education was carried out on behalf of the NMC in 2006 (Burke & Saldanha 2006). As a result, a minimum academic level of a degree for midwifery programmes was recommended by the Midwifery Committee (NMC 2007a). Other recommendations were:
Supporting birthing women in a variety of settings, such as home births and birth centres, was also recommended (NMC 2007b).
The second edition of standards to support learning and assessment in practice was published in 2008 (NMC 2008b). This ensured students were to be supported and assessed by mentors who had met the additional sign-off criteria. Sign-off mentors are now to make the final assessment of practice and confirm that the required proficiences for practice have been achieved (NMC 2008b). A triennial review of mentors and practice teachers is required to be maintained on a local register and all mentors must have completed an NMC-approved mentorship or teacher preparation (NMC 2009a&b).
Standards for pre-registration midwifery education were updated in 2009 (NMC 2009c). The length of the programmes are set at 3 years (156 weeks) and 18 months (78 weeks) for registered nurses.
The NMC set competencies required by students to achieve the standards, which are divided into four domains:
Essential skills clusters, including communication, initial consultation between the woman and midwife, normal labour and birth, initiation and continuance of breastfeeding, and medicines management, are also required (NMC 2009c).
Declaration of good health and good character of each midwifery student must be made by the LME at the education institution on successful completion of the programme ‘in order to satisfy the Registrar that an applicant is capable of safe and effective practice as a nurse or midwife’ [Article 5(2)(b)] Nursing and Midwifery Order 2001 (NMC 2008c).
Function 3: Regulating Fitness to Practise, Conduct and Performance
This function is supported by the NMC rules, standards and advice publications set out by the NMC practice committees (see Box 3.2). In midwifery, audit and monitoring of compliance is carried out by the local supervising authorities and supervisors of midwives (NMC 2009d).
Box 3.2
Rules and standards
The practice committees ensure non-compliance to the rules and standards is reviewed and individual cases are investigated.
A synopsis of the NMC rules and codes are listed below (see www.nmc-uk.org).
Midwives rules and standards (NMC 2004b)
The midwives rules and standards are currently under review and awaiting public consultation but will remain in effect until the end of 2011.
Rule 1 is a citation of when the Rules came into force in August 2004 and Rule 2 is an interpretation of the definitions.
Rules relating to midwifery practice are in Table 3.1 and rules relating to statutory supervision and local supervising authority midwives in Table 3.2.
Table 3.1 Midwives rules relating to midwifery practice
| Rule | Title | Practice issues |
|---|---|---|
| Rule 3 | Notification of intention to practise (ITP) | If a midwife practises clinically or holds a post for which midwifery is a required qualification, a midwife must notify the Local Supervising Authority, through her Supervisor of Midwives. This is required annually (usually by 31st March) or within 48 hours of care given in an emergency |
| Rule 6 | Responsibility and sphere of practice | A practising midwife is responsible for providing care to both a woman and baby and must refer to the relevant practitioner in an emergency if the situation deviates from the norm. The midwife must not give care unless she is trained to do so unless it is during an emergency |
| Rule 7 | Administration of medicines | A midwife shall supply and administer drugs only for which she has been trained and she must abide by drugs regulations |
| Rule 8 | Clinical trials | A practising midwife may only participate in clinical trials if there is a protocol approved by a relevant ethics committee |
| Rule 9 | Records | A practising midwife must keep contemporaneous records, detailed observations and a record of any medications administered to a woman or baby. It also includes arrangements for storage with the employer or LSA |
| Rule 10 | Inspection of premises and equipment | A practising midwife must allow her supervisor or the LSA access to monitor her records and equipment |
Table 3.2 Midwives rules relating to statutory supervision and local supervising authority midwives (NMC 2004b)
| Rule | Title | Statutory supervision and Lsa issues |
|---|---|---|
| Rule 4 | Notifications by local supervising authority (LSA) | The LSA is required to publish the name of the LSA officer, the date by which all ITPs should be submitted, receive the ITPs and notify the NMC annually. This is a means to ensuring a complete list of practising midwives is submitted by each LSA midwife |
| Rule 5 | Suspension from practice by a local supervising authority | Invests the power and authority to suspend a midwife from practice in order to protect the public if the midwife poses an immediate danger and is reported to the NMC. This would be progressed to an interim suspension order pending the outcome of an investigation |
| Rule 11 | Eligibility for appointment as a supervisor of midwives (SOM) | A midwife needs to be a practising midwife with 3 years’ experience and have completed a *programme for a supervisor of midwives as agreed by the NMC and maintain updated, as required of a supervisor. |
| Rule 12 | The supervision of midwives | A practising midwife shall have a SOM appointed by the LSA covering her main area of practice. The LSA must ensure that each midwife has a named SOM and meets her at least once annually to review her practice and identify her training needs. The SOM must maintain a record of all meetings. Midwives must have 24-hour access to a SOM |
| Rule 13 | The local supervising authority midwifery officer | Each LSA shall appoint an LSA midwifery officer (LSAMO). The LSAMO must be a practising midwife and meet the standards of experience and education set by the NMC |
| Rule 14 | Exercise by a local supervising authority of its functions | Where an LSA has concerns about whether an LSAMO or a SOM meets the Council’s standards, the Council should discuss their concerns |
| Rule 15 | Publication of local authority procedures | Each LSA shall publish the name and address of the LSAMO and procedure for reporting all adverse incidents relating to midwifery practice or impaired fitness to practise and how it will investigate such reports. In addition, how it will deal with complaints against LSAMOs or SOMs within its area |
| Rule 16 | Annual report | The LSA must submit an annual report to the NMC every year |
*Amendment to Rule 11– NMC (Midwives) (Amendment) Rules 2007 (SI2007/1887) – March 2008 NMC Circular 04/2008 (NMC 2008d)
‘If the programme was completed more than 5 years ago without appointment, the knowledge and experience gained is no longer valid and a new programme of preparation must be undertaken’
Confidentiality (NMC 2006a)
This advice covers all aspects of information about patients and clients and laws covering access to records.
Gifts and gratuities (NMC 2008e)
Gifts or hospitalities should be refused if they are interpreted as an attempt to gain preferential treatment.
Environment of care (NMC 2008f)
It is the responsibility of registrants to practise in a safe environment and to report concerns if problems in the environment are putting people at risk.
Accountability (NMC 2008g)
Registrants are reminded that they are professionally accountable to the NMC, accountable to the law, as well as having a contractual accountability to their employer. They must act in the best interests of the person in their care at all times.
The PREP handbook (NMC 2008h)
This comprises post-registration education and practice (PREP) guidance to ensure registrants remain updated in their field of practice. Practising for a minimum of 450 hours and maintenance of continuing professional development over the 3-year registration period must be completed. Guidance is given for returning to practice if registration has lapsed.
The code (NMC 2008i)
This includes advice regarding treating people with dignity and respect, consent, maintaining professional boundaries, working as part of a team, delegation, keeping skills up to date, using best available evidence, maintaining clear, accurate records, acting with integrity and upholding the reputation of the profession.
Standards for medicines management (NMC 2008j)
Twenty-six standards are listed under the following sections: supply and administration; dispensing; storage and transportation; practice of administration; delegation; disposal; unlicensed medicines; complementary and alternative therapies; managing adverse events; and controlled drugs. A CD-ROM is also provided which includes the relevant legislation.
Record keeping: guidance for nurses and midwives (NMC 2009e)
The principles and purpose of record-keeping are discussed, including confidentiality, access to records, and disclosure, and relevant Acts are listed.
Guidance on professional conduct for nursing and midwifery students (NMC 2010h)
This guidance covers all aspects of fitness to practise and behaviour expected of a student, including areas of concern such as cheating and plagiarism.
Raising and escalating concerns: guidance for nurses and midwives (NMC 2010b)
This draft guidance states that raising a concern should be made in a timely manner in order to safeguard the public. Examples include: a danger or risk to health and safety; issues regarding care delivery; issues relating to the environment of care, such as staffing problems; issues related to the health of a colleague; and issues related to misuse or unavailability of medical equipment. The guidance suggests contacting a supervisor of midwives, mentor or university tutor and relevant contact organizations are listed. Consultation with both the public and professionals is completed and awaiting publication in late Autumn 2010.
Advice and information for employers of nurses and midwives (NMC 2010c)
Responsibilities as an employer and recognition of misconduct, lack of competence, bad character and poor health are discussed in this guidance and how to investigate and refer to the NMC.
Midwifery supervision
Statutory supervision of midwives supports protection of the public by promoting best practice and excellence in care; preventing poor practice and intervening in unacceptable practice (NMC 2006b).
History of midwifery supervision
Statutory supervision of midwives was enshrined in the 1902 Midwives Act which set up the Central Midwives Board (CMB). Initially, the board had a medical majority and was required to discipline midwives who disobeyed or ignored the Rules or who were guilty of negligence, malpractice or misconduct (personal or professional). The CMB delegated supervision and monitoring to local supervising authorities, then under the control of county councils and county borough councils, until 1973 when they came within the NHS.
The 1936 Midwives Act empowered the CMB to make rules relating to the qualifications of medical and non-medical supervisors of midwives. It required non-medical supervisors to be practising midwives. In 1937, a Ministry of Health letter was released expanding on the detail of the 1936 Act, stating that inspectors of midwives were now to be known as supervisors of midwives; and most importantly that the supervisor should act as a ‘counsellor and friend’.
The 1973 NHS Reorganisation Act abolished LSAs under borough councils and nominated regional health authorities as LSAs. The delegation of duties to supervisors of midwives was nominated by district health authorities. The 1977 Statutory Instrument (SI) No. 1850 eradicated the role of ‘medical supervisor’ and removed the words ‘non-medical’ from the title of supervisor.
Since 1996, employment of LSA officers has been devolved to Strategic Health Authorities (SHAs). The LSA officer was now required to be a practising midwife in line with the DH document Managing the new NHS (DH 1994).
The Nursing and Midwifery Order 2001 (DH 2002b) sets out the current responsibility of the LSA for the function of statutory supervision of midwives and this is enshrined in the midwives rules and standards (NMC 2004b) (see Table 3.2).
Education and training for supervisors of midwives
In 1978 the CMB introduced courses of instruction for supervisors, initially for those in post since 1974. These courses later became mandatory before or immediately after appointment as a supervisor (UKCC 1986 44(2)). A formal open learning programme and training package ‘Preparation for supervisors of midwives’ was first developed at diploma level in 1992 by the English National Board (ENB 1992) and successful completion of the programme was required prior to being nominated to become a supervisor. UK standards for the preparation and practice of supervisors of midwives (NMC 2006b) now set out the standards of competence required in accordance with the midwives rules and standards, Rule 11 (NMC 2004b). Programmes of education are delivered by HEIs and approved and monitored annually by the NMC (NMC 2006b).
The Local Supervising Authority Midwifery Officer (LSAMO)
The LSAMO is appointed by the Strategic Health Authority in England (Health Boards in Scotland, Health Inspectorate in Wales and the Public Health Agency in Northern Ireland) and is responsible for the provision of statutory midwifery supervision on behalf of the NMC (DH 2002b, NMC 2004b).
The LSA sets standards for statutory supervision of midwives and carries out an annual audit of the standards of midwifery practice locally. This includes receipt of the annual intention to practise data from supervisors, evidence of liaison with services users, engagement with HEIs, and any investigations of misconduct or lack of competence undertaken.
The LSAMO is responsible for suspension of midwives from practice (NMC 2004b: Rule 5), ensuring a full investigation is carried out and advising the investigating supervisor of midwives (SOM) if a period of supervised practice is required (NMC 2007c).
An annual report is submitted to the NMC about the standards, local activities, good practice and trends affecting the maternity service within its area (NMC 2004b: Rule 16).
The NMC reviews the LSA profiles annually using a risk assessment approach (NMC 2009d). Based on this, a decision is made to carry out a formal review of selected LSAs to verify if they are meeting the standards and a panel is appointed by the NMC Appointments Board.
The NMC produces an analysis of all the LSAs in the form of an annual report with recommendations on the 10 standards (NMC 2009f) (Table 3.3).
Table 3.3 Rule 16 standards (NMC 2004b)
| Number | Standard |
|---|---|
| 1. | Each LSA will ensure their report is made available to the public |
| 2. | Numbers of supervisors of midwives appointments, resignations and removals |
| 3. | Details of how midwives are provided with continuous access to SOMs |
| 4. | Details of how the practice of midwives is supervised |
| 5. | Evidence that services users have been involved in monitoring supervision of midwives and assisting the LSAMO with the annual audits |
| 6. | Evidence of engagement with HEIs in relation to supervisory input into midwifery education |
| 7. | Details of any new policies related to the supervision of midwives |
| 8. | Evidence of developing trends that may impact on the practice of midwives in the LSA |
| 9. | Details of the number of complaints regarding the discharge of the supervisory function |
| 10. | Reports on all LSA investigations undertaken during the year |
The Supervisor of Midwives (SOM)
The role of the Supervisor of Midwives is unique in its protection of the public and support to midwives by providing a high standard of care to women and their babies. Supervisors provide leadership and guidance to midwives, including the provision of a 24-hour service for midwives and women (LSAMO National Forum 2009, NMC 2007c).
Supervision provides support for parents regarding choice for place of birth, concerns regarding midwifery care and maintenance of safety, for example, at a home birth (NMC 2009g). The midwife has a duty of care to the woman, as well as a contractual duty to the employer, and she may need to seek advice from her supervisor should any conflict arise.
Statutory supervision combines professional and practice responsibilities for challenging inferior practice and setting required standards, as well as carrying out clinical audit. Supervisors ensure that midwives have access to the statutory NMC rules, codes and standards and access to local clinical guidelines.
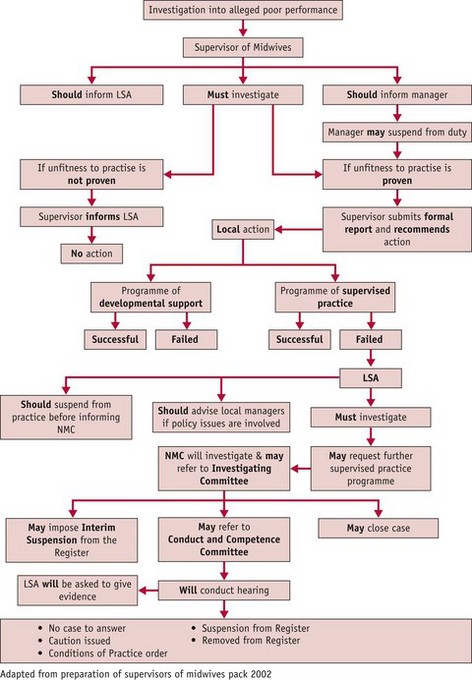
Supervision involves administrative and education tasks, including receipt of a midwife’s annual notification of intention to practise. Supervisors audit records, arrange regular meetings with individual midwives, at least once annually, and work with them to identify areas of practice requiring development (LSAMO National Forum 2009). They monitor staffing levels and skill-mix in relation to safe practice, and notify senior management when there is a shortfall. They contribute to risk management and clinical governance within the NHS, investigate any allegations of professional misconduct and report upwards to the LSA (see Fig. 3.1).
Every midwife should have a named supervisor of her or his choosing. Supervisors have a responsibility to provide support to all midwives outside the NHS, including the private sector, higher education institutions (HEIs), prisons, independent midwives and GP practice midwives (NMC 2007b, 2007c). The ratio of supervisors to midwives should be 1 : 15 (NMC 2004a).
Statutory supervision and management
Statutory supervision and management are distinct and separate from each other but must liaise, especially regarding allegations of unfitness to practise. Midwives should be appraised of the difference, and given access to a named supervisor who is not their manager, so that the roles are not confused.
Statutory supervision and clinical governance
Statutory supervision is a vital component of leadership and clinical governance within the maternity services (see Ch. 7), supporting clinical risk management by monitoring service developments and reconfigurations to identify trends, provide a framework for continuous improvement and ensure that safety and quality is assured (DH 2007b).
It provides a proactive service and can limit the volume of serious adverse incidents within an organization by the very nature of its practice and education support to every individual midwife in the UK. Specifically, supervisors can work with midwives and risk managers to carry out the recommendations of the most recent clinical guidelines, such as the NICE guidelines (NICE 2004, 2006, 2007, 2008).
Supervision can support standards for staffing maternity units, such as those identified in Safer childbirth (RCOG 2007) and those of the Health Care Commission (HCC 2008), King’s Fund (King’s Fund 2008) review of the maternity services that recommended improved staffing, training and communication skills and the RCM publication specifying the ratio of midwives to women and babies to provide safety of practice (RCM 2009). The more recent project on Safer births (NPSA 2009) is actively supported by statutory supervision.
Delivering high-quality midwifery care (DH 2009) calls for further work to be carried out on the aspects of supervision that are most effective. It challenges supervisors to include feedback from women as part of their annual review and can only serve to strengthen supervision.
Finally, the supervisor must ensure that midwives are aware of national and local safeguarding policies and are supported in their practice during any involvement in child protection cases. Multidisciplinary training can be arranged jointly by the supervisor and risk manager.
Conclusion
Midwifery legislation has provided over 100 years of statutory supervision, and protection of the public has been upheld through its quality and standards. The number of midwifery registrants referred to the regulating body for professional misconduct has remained insignificant, demonstrating a mature forward-thinking approach to continuing professional development.
Midwives have always worked closely with the users of the service throughout their history. Recent revision of the Nursing and Midwifery Order (DH 2008b) to provide parity between lay and professional members of Council is a welcome move towards greater transparency in regulation of the professions.
The formation of a UK LSAMO’s forum will provide additional support to supervisors and strengthen statutory supervision by working together to set standards and audit practice.
Finally, the revision of the Midwives Rules and Standards in 2011 should be a positive move in uniting the midwifery profession under improved regulation and alignment with other professions.