Chapter 11 Alterations in the Skin
GENERAL APPROACH TO DISEASES THAT ALTER THE SKIN
It is important to remember that the skin has a limited repertoire with regard to its presentation; many diseases with various causes may manifest with similar lesions. However, certain patterns of response to disease are also recognized. In order to manage skin problems successfully, the veterinarian must use a systematic approach by obtaining a complete history, performing a thorough physical examination, and, when appropriate, using one or more simple diagnostic techniques.1 The following sections discuss the materials and methods necessary to perform techniques commonly used to diagnose large animal skin disease.
History
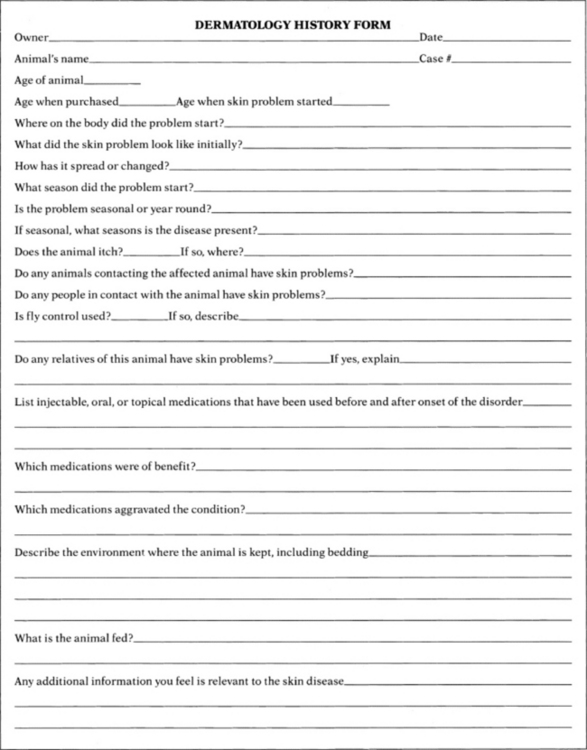
To obtain a differential diagnosis list, all the questions listed on the sample history form (Fig. 11-1) should be answered. Often it is helpful to repeat the questions to the owners at a later time or to give them a history form to complete at their leisure, which allows greater opportunity to remember details relevant to the skin disease. The goals should be to determine the initial features of the skin disease, how the problem has progressed, and what factors have influenced its progression to the present state.
Physical Examination
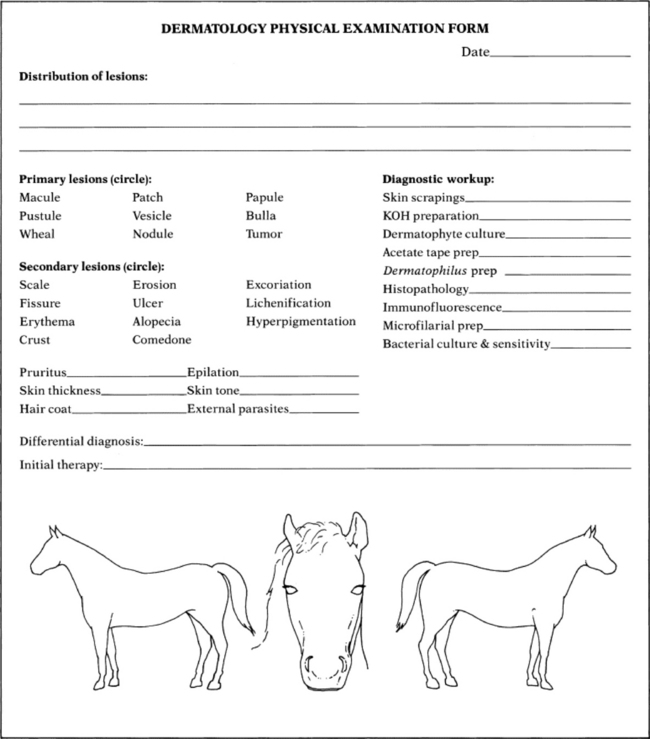
The diagrams and terms listed on the sample form (Fig. 11-2) may serve as a useful guide for recording the physical findings. The animal’s overall condition should be assessed and a general physical examination should be performed to determine if the disease is limited to the skin or if systemic signs of disease are also present. The distribution, morphology (e.g., papules, nodules, wheals, patches of alopecia), and size of skin lesions should be noted. The mucous membranes also should be examined, and the skin surface palpated to determine features not readily noted visually (e.g., crusts beneath the hair, dryness, ability to epilate hairs, and presence of peripheral lymphadenopathy).
The practitioner’s goal should be to describe accurately the animal’s clinical appearance in a written record for future reference.
Diagnostic Techniques
For most of the techniques that follow, a good-quality microscope equipped with ×4, ×10, ×40, and ×100 objectives is recommended.
SKIN SCRAPINGS
Skin scrapings are used primarily to demonstrate microscopic ectoparasites, specifically mites. Scraping is a quick, simple, inexpensive diagnostic technique that is more useful in ruminants than in horses because equine mite infestations are relatively uncommon. The materials needed to perform a skin scraping are a sterile container, mineral oil, a medical grade spatula (Fisherbrand Microspatula with Flat-Ended Blade, catalogue no. 21-401-20, Fisher Scientific; www.fisherscientific.com), glass slides, and cover slips. Although a No. 10 scalpel blade may be used, a medical grade spatula will not cut the skin in cases of sudden movement of the horse, yet is just fine enough to be able to scrape deep enough to find Demodex species mites, if indicated. If the hair coat is thick, a small area should be clipped before scraping. Multiple superficial scrapings that cover large surface areas should be performed, as well as several scrapings covering a small area that are deep enough to create capillary oozing. The collected material should be placed in a container until it can be examined microscopically. Some of the sample can then be placed on a glass slide and finely dispersed in enough mineral oil to provide a confluent layer without air bubbles beneath a cover slip. The slide should be scanned systematically with the ×10 objective. If something of significance is noted, the ×40 objective can be used to examine the specimen in more detail.
DERMATOPHYTE CULTURE
The materials necessary to perform a dermatophyte culture include dermatophyte test medium, mosquito forceps, a medical grade spatula, and sterile empty containers such as evacuated blood collection tubes. The forceps should be sterile, and each lesion to be sampled should be wiped gently with either water or isopropyl alcohol (there is some controversy as to which is better; I use water out of concern that the alcohol may inhibit fungal growth on the culture medium) to remove as many bacterial and fungal contaminants as possible and allowed to dry. Multiple small, scaling, and slightly crusted lesions should be sampled; the samples should be stored in individual containers. Broken hairs, scales, and crusts from the periphery of the lesions are collected (because dermatophytes cause peripherally expanding lesions). A spatula may be useful for scraping scales and debris from the skin surface. The forceps are used to pluck broken hairs.
If the clinician’s practice performs its own fungal cultures, the samples should be removed from the containers with a sterile forceps in a clean working area and gently pressed onto, but not buried beneath, the culture medium. The top of the culture dish or vial should be loosely replaced to allow sufficient ventilation for the culture to grow. Most dermatophytes grow at room temperature, except for some strains of Trichophyton verrucosum, which requires incubation at 37° C (98.6° F). The colony usually first appears in 5 to 7 days, although all cultures should be allowed to incubate for 3 weeks before a negative result is declared.
Dermatophyte test medium is an amber-colored Sabouraud’s dextrose agar containing phenol red, a pH indicator, and several antibacterial and antifungal agents to inhibit growth of contaminant organisms. Dermatophytes preferentially use the protein in the medium as they begin to grow, producing alkaline metabolites that cause the medium to turn red. The dermatophyte colony is typically a white to beige, powdery to fluffy growth; the colonies are never dark colored. Most saprophytic (contaminant) fungi metabolize the carbohydrates first, producing acidic metabolites that do not change the color of the medium. It should be stressed that after the carbohydrate source has been depleted, saprophytes use the proteins and produce a red color change.
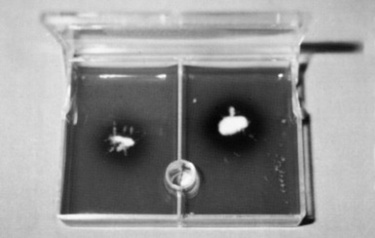
Positive identification of a dermatophyte is made in most instances if a white to beige, powdery to fluffy colony begins to appear on the medium at the same time or within 24 hours of the appearance of a red color change in the medium (Fig. 11-3). An infrequently encountered exception to this rule is growth of the saprophyte Scopulariopsis brevicaulis, a tan to light brown, smooth or mealy colony that produces a concurrent red color change in the medium. It is essential to check the cultures daily to determine if the red color change and colony growth occur nearly simultaneously. If any doubt exists about the type of colony growth, the sample should be submitted to a diagnostic laboratory for specific identification.
POTASSIUM HYDROXIDE PREPARATION
A potassium hydroxide (KOH) preparation may permit immediate diagnosis of dermatophytosis. However, examination of KOH preparations requires considerable experience, as fungal elements may be easily overlooked (false-negative result) and numerous artifacts such as fibers, cholesterol crystals, or oil droplets may be mistaken for fungal elements (false-positive result). It is always advisable to perform a dermatophyte culture in conjunction with a KOH preparation.
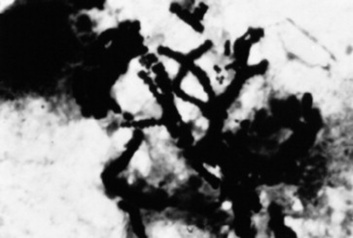
The materials necessary to perform a KOH preparation include mosquito forceps, a medical grade spatula, a sterile empty container, glass microscope slides, cover slips, a Bunsen burner, and clearing solution. As with a dermatophyte culture, it is important to sample several lesions to increase the chances of obtaining a diagnostic sample. Hairs and scales are collected from the periphery of the lesions with the mosquito forceps and the spatula. The samples are stored in the sterile container until a microscopic examination can be performed. A drop of the KOH clearing solution is placed on a glass slide, hairs and scales are added to the solution, and a cover slip is placed over the material. The slide should be scanned systematically with the ×10 objective for abnormal-appearing hairs with a fuzzy internal structure. If these features are noted, a higher-powered objective should be used for more detailed examination. A positive result with a KOH preparation demonstrates hyphae, which usually are uniform in width and septate. Beadlike chains of arthroconidia may be seen as well (Fig. 11-4).
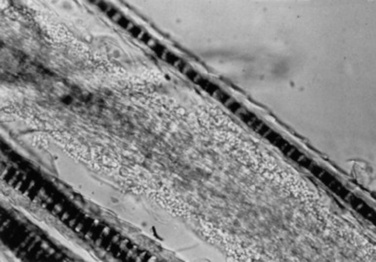
Fig. 11-4 Positive result on potassium hydroxide (KOH) preparation. Note the small, spheric fungal elements (arthroconidia) on the hair shaft.
The purpose of the clearing solution is to dissolve the hard keratin and bleach the melanin of the hair shaft so that the fungal hyphae and arthroconidia can be identified more readily. Care should be taken not to spill any clearing solution on the microscope because it can damage the lenses. Several types of clearing solutions are available. If 15% KOH is used, the slide should be heated for 15 to 20 seconds to facilitate clearing before examination. As an alternative, the preparation can be allowed to stand at room temperature for 30 minutes before viewing.
ACETATE TAPE PREPARATION
Acetate tape preparations for parasites are used primarily to diagnose infection with Oxyuris equi, although they may also be used to diagnose Chorioptes species. The materials required to perform an acetate tape preparation include acetate (nonfrosted) tape, mineral oil, and glass microscope slides. A piece of the tape is pressed over several areas in the anal and perianal region when looking for O. equi or over an affected region that has been lightly clipped when looking for Chorioptes species. The tape is then placed with the adhesive side down on a line of mineral oil that was placed lengthwise on a glass microscope slide. The purpose of the oil is to help clear the debris and facilitate examination of the preparation for parasites. The preparation is scanned with the ×10 objective for organisms.
DERMATOPHILUS PREPARATION
This test is used as an aid in identification of Dermatophilus congolensis. Crusts should be removed from the patient and the excess hair carefully trimmed from the crusts with a small pair of scissors. The crusts are minced with the scissors and mixed with several drops of saline on a glass slide. After the crusts have softened in the saline for several minutes, they should be crushed with the tip of an applicator stick. The excess debris is removed, and the slide is allowed to air dry. The slide should then be heat fixed; stained with Gram, Giemsa, or Wright stain; and examined for the characteristic bacteria. D. congolensis organisms are gram-positive, branching, filamentous bacteria that divide horizontally and longitudinally, forming parallel rows of cocci (zoospores) that commonly are described as resembling “railroad tracks” (Fig. 11-5).
CYTOLOGIC STUDIES
Cytologic studies are of value when dealing with crusts, scales, pustules, vesicles, nodules, or tumors. They can quickly indicate the presence of infectious organisms and provide a rough assessment of the spectrum of cell types present in a lesion (e.g., neoplastic, acantholytic, or inflammatory). The surface of the lesion should be gently shaved (if necessary); particular care must be taken not to rupture fragile pustules and vesicles or remove crusts. Crusts and scales are best evaluated by performing a superficial scrape with a spatula, placing the material on a microscope slide, heat-fixing, then staining with Gram, Giemsa, or Wright stain. Alternatively, acetate tape may be used to collect the material, and instead of placing the tape on a slide that has mineral oil (as is done when looking for parasites), the tape is placed on a slide on which several drops of the “blue” solution from the Wright stain have been placed. Scan for areas of interest with the ×4 objective, then use the ×100 objective with immersion oil.
Cytologic evaluation of intact pustules and vesicles is best accomplished by gently opening an intact lesion with the tip of a sterile No. 15 scalpel blade or 25-gauge needle and smearing the contents on the surface of a glass slide. The slide should be air dried, heat fixed, stained with one of the previously mentioned stains, and examined. Nodules, tumors, and swellings are best evaluated by fine-needle aspiration. A 25- or 22-gauge needle on a 12-mL syringe is introduced into the mass, and negative pressure is applied. Several passes through the mass at different angles should be performed. After negative pressure has been released, the needle is removed from the mass. The needle is then removed from the syringe, the syringe is filled with air, and the needle is reattached. The contents of the needle are pushed out onto glass slides, which are subsequently dried, fixed, and stained as described previously.
BIOPSY FOR ROUTINE HISTOPATHOLOGIC EXAMINATION
The following materials are needed to perform a skin biopsy:
It is very important not to surgically prepare a lesion that is going to be biopsied for histopathologic examination. Shaving and scrubbing remove crusts and epithelial tissue that may be important in reaching a diagnosis. Cutaneous infections caused by biopsies taken in this manner are extremely uncommon. If the clinician is concerned about infections, surgically prepare the site after the biopsy has been taken, before suturing.
Local anesthesia is sufficient for obtaining most skin biopsies. A 22- to 25-gauge needle is inserted at the margin of the lesion until the bevel is buried in the subcutaneous tissue beneath the lesion. The 2% lidocaine (0.5 to 1 mL) is injected, allowing 1 to 2 minutes for the anesthetic to take effect. Infiltration of the dermal or epidermal tissue with lidocaine should be avoided because this causes artifactual changes in the specimen.
Four techniques can be used to biopsy skin: the excisional, wedge, punch, and elliptic techniques. When the lesion to be sampled is a single nodule, the ideal biopsy technique is excisional because the lesion can be eliminated at the same time the histologic diagnosis is made. If the lesion is a tumor and too large to be excised, a generous wedge biopsy should be performed, which ideally extends from the margin to the center and includes the full depth of the lesion.
Most lesions can be sampled with a 6-mm biopsy punch. A disposable biopsy punch* usually can be used to obtain two or three biopsies before its edge is dulled and it must be discarded. The punch is placed directly over the lesion and rotated in a continuous circular motion while pressure is applied until the blade of the punch is in the subcutaneous tissue. If the punch has cut to a sufficient depth, when it is removed the tissue sample is free of the adjacent dermis and remains only loosely attached to the underlying subcutaneous tissue by a thread of connective tissue. A small pair of curved mosquito forceps is used to gently grasp the subcutaneous part of the biopsy and elevate it from the surrounding tissue. The specimen is then cut free with a pair of sharp scissors. It is important to avoid handling the epidermal and dermal parts of the sample during this procedure to minimize artifactual changes in the tissue sample. The sample is gently blotted to remove any surface hemorrhage and immediately placed in 10% buffered formalin for fixation. The site from which the sample was taken may then be cleaned with an antiseptic solution and closed with either two simple interrupted sutures or a cruciate stitch using No. 2-0 or 3-0 nonabsorbable sutures.
Although punch biopsies are convenient and easy to use, they are not appropriate for vesicular, bullous, and ulcerative lesions. For these lesions the method of choice is a surgical elliptical biopsy. The biopsy of vesicular and bullous lesions should encompass the entire lesion. Biopsy of samples of ulcerations should include abnormal tissue, the leading edge of the lesion, and normal tissue. Because an ulcer lacks epithelial tissue, the leading edge where epithelium remains may be the most rewarding in providing a histologic diagnosis. Thus the skin is biopsied so that the long axis of the ellipse crosses perpendicular to the leading edge of the ulcer (Fig. 11-6). It is important to mount surgical elliptical biopsies before placing them in formalin or they will curl during fixation, resulting in distortion of the histologic features during sectioning. To mount the specimen, the subcutaneous surface is placed on a small piece of a wooden tongue depressor or cardboard while gentle pressure is applied to the tissue so that it adheres to the surface; then the specimen is placed in the formalin.
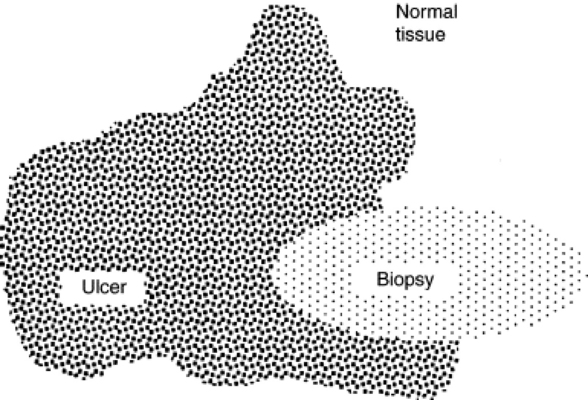
Fig. 11-6 An ulcerative lesion should be biopsied in an elliptical fashion, using a No. 15 scalpel blade, so that the long axis of the ellipse crosses perpendicular to the leading edge of the lesion.
Ideally biopsy specimens should be submitted to a veterinary histopathologist with special interest and training in dermatopathology. Submission of adequately biopsied specimens of properly chosen lesions is the clinician’s responsibility. To further increase the chances of securing clinically valuable information from the biopsy samples, the clinician must also provide the pathologist with a concise history of the skin problem, physical findings, a description of the morphology and location of the lesions, and a list of differential diagnoses. When the suspected clinical diagnoses are provided, the pathologist’s efforts can be directed specifically toward confirming or ruling out those diagnoses.
BIOPSY FOR IMMUNOPATHOLOGY
Immunopathology may be used as an adjunct to conventional histologic testing when the clinician suspects that the patient has an immune-mediated skin disease. The two methods used are direct immunofluorescence, which requires a special medium for fixation (Michel’s fixative), and immunoperoxidase techniques, which may be performed on the paraffin block prepared for the histopathologic study (i.e., the formalinized tissue section). The materials and the technique for biopsy for immunopathology are essentially identical to those for a routine histologic examination. Administration of corticosteroid medications within 3 weeks of testing may be associated with false-negative test results. It is advisable to bisect biopsy samples along their long axis, submitting half for direct immunopathology and half for histopathologic examination. It should be borne in mind that histopathology of the lesions, rather than immunopathology, is often the more accurate of the two methods in the diagnosis of autoimmune diseases; thus if faced with the choice (because of financial reasons or paucity of lesions) the clinician should always choose the former.
MICROFILARIAL PREPARATION
The microfilarial preparation technique is applicable to the diagnosis of cutaneous onchocerciasis in horses, stephanofilariasis in cattle, and elaeophorosis and parelaphostrongylosis of sheep and goats. After selecting the lesion to be sampled, a 6-mm punch biopsy is used to obtain the tissue sample in the same manner as for the histopathologic biopsy. The tissue should be split, and half preserved in 10% buffered formalin for routine histologic studies. The other half is placed on a dampened gauze sponge in a tightly closed container until the preparation can be performed. A small piece of the tissue that includes the dermis is placed on a glass slide and minced with a razor blade; a few drops of nonbacteriostatic saline are added. Bacteriostatic saline, which kills the microfilaria and thus makes their identification more difficult, should not be used. The specimen is incubated at room temperature for 15 minutes. The slide is then scanned with the ×4 objective along the margins of the tissue debris while the clinician searches for indication of motion in the saline. If the characteristic whiplash movement of the parasite is noted, a higher-powered objective should be used. If the preparation result is negative, a small amount of water is added to a Petri dish, the glass slide is rested on two wooden sticks above the water, and the cover is replaced on the dish. The preparation should be incubated for several hours or overnight and reexamined. The Petri dish helps prevent the sample from drying out.
BACTERIAL CULTURE
The method of bacterial culture depends on the type of lesion. All haired lesions should be gently shaved. Nodules and tumors should be cultured by aseptically excising the lesion or by obtaining a generous wedge of the tissue. To prevent culture contamination by surface bacteria, the nodules should be gently shaved, washed with an antiseptic soap, and dried with a sterile gauze pad. A perilesional injection of 2% lidocaine is used to anesthetize the tissue. The sample is placed in a transport medium and sent to a microbiology laboratory for culture. A papular eruption (rash) is best cultured by obtaining a sterile 6-mm punch biopsy of skin.
Crusts may be lifted up and the underside cultured via a sterile Culturette. Ulcerative lesions should not be cultured because any bacteria isolated are more likely to be opportunistic rather than primary pathogens. If the lesions are fluctuant (vesicles, pustules), the overlying skin can be opened gently with a No. 15 blade and some of the contents of the lesion transferred with the blade to the tip of a sterile culture swab. It is advisable to avoid placing the swabs directly on the skin surface, particularly when sampling small lesions, because nonpathogenic bacteria from the skin surface may be inadvertently cultured.1
PRURITUS
Definition
Pruritus is an unpleasant sensation that provokes the desire to scratch. It is designated a primary cutaneous sensation, along with heat, cold, pain, and touch. There are two broad categories of pruritus. Physiologic or spontaneous itch is a sharp, well-defined, pruritic sensation that is sufficiently intense to prompt scratching but that does not result in significant irritation of the skin; this is a frequent daily occurrence in normal individuals. Pathologic itch is the less well-defined pruritus that occurs in a variety of primary and secondary skin disorders and in systemic diseases. It is an intense cutaneous discomfort that provokes vigorous scratching.2
Mechanisms of Pruritus
The investigation of the mechanism of pruritus has been primarily in laboratory animals and humans. It is presumed that much of this knowledge is applicable to other animal species. Pruritus is a distinct sensory quality transmitted from an arborizing network of nerve endings situated at or near the dermoepidermal junction. The sensation is carried to the spinal cord through small, unmyelinated C fibers. The fibers enter the dorsal root of the spinal cord and ascend in the ventrolateral spinothalamic tract through the posterior ventral nucleus of the thalamus to the sensory cortex. The pruritic sensation may be modified in the sensory cortex by behavioral factors or competing stimuli.3,4
Many physical and chemical stimuli can evoke pruritus, and many substances have been implicated as mediating pruritus in humans. Examples of these mediators, which are assumed to have importance in domestic animals as well, include the following4:
 Histamine. Histamine has been regarded as the classic mediator of pruritus. Histamine is present in mast cells in the dermis and in blood basophils. An intradermal injection of histamine produces pruritus within 20 to 50 seconds. Because many pruritic disorders respond poorly to antihistamines given either therapeutically or prophylactically, histamine is not believed to be the sole mediator of pruritus.
Histamine. Histamine has been regarded as the classic mediator of pruritus. Histamine is present in mast cells in the dermis and in blood basophils. An intradermal injection of histamine produces pruritus within 20 to 50 seconds. Because many pruritic disorders respond poorly to antihistamines given either therapeutically or prophylactically, histamine is not believed to be the sole mediator of pruritus. Prostaglandins(E series and endoperoxidases). Prostaglandins induce pruritus by potentiating the release of proteases from keratinocytes and leukocytes and by lowering the threshold and increasing the duration of histamine-induced pruritus.
Prostaglandins(E series and endoperoxidases). Prostaglandins induce pruritus by potentiating the release of proteases from keratinocytes and leukocytes and by lowering the threshold and increasing the duration of histamine-induced pruritus. Endogenous opioid peptides. Opiates may potentiate preexisting pruritus. The opiate antagonist naloxone hydrochloride has an attenuating effect on the histamine-induced component of pruritus.
Endogenous opioid peptides. Opiates may potentiate preexisting pruritus. The opiate antagonist naloxone hydrochloride has an attenuating effect on the histamine-induced component of pruritus. Substance P. Substance P is a neurotransmitter found in the central and peripheral nervous systems. When introduced intradermally, it elicits a pruritic response.
Substance P. Substance P is a neurotransmitter found in the central and peripheral nervous systems. When introduced intradermally, it elicits a pruritic response.Many factors can potentiate existing pruritus. Neurologic factors such as boredom and fatigue can potentiate a pathologic itch and possibly transform a physiologic itch into a pathologic itch. Local axonal reflexes can potentiate pruritus; that is, if a second stimulus is applied to an area close to one that is pruritic, the second stimulus, irrespective of its type, is perceived as an itch. In addition, skin with chronic dermatitis has limited perception of stimuli, and any stimulus applied to the affected region may be perceived as either a burning sensation or an itch. This phenomenon is known as “conversion itch.” Secondary bacterial infections, vasodilatation, and inflammation result in a local increase in proteases that potentiate pruritus.3
Pruritus can be diminished by several nonpharmacologic mechanisms, the most common being application of competing stimuli. Pruritus is a minor sensation compared with the other primary sensations of heat, cold, touch, and pain; thus local application of a competing stimulus to a pruritic area often suppresses the pruritic sensation. Scratching is an example of a competing stimulus. Scratching may relieve pruritus by disturbing the rhythm of afferent impulses traveling toward the central nervous system. An alternative theory is that scratching may cause transient damage to nerve fibers that convey the pruritic sensation. Unfortunately the effect is short-lived because the epidermal damage induced by scratching causes the release of epidermal proteases that may later increase the degree of pruritus. Centrally acting factors such as diversions or distractions can also diminish the perception of pruritus by providing competing stimuli directly to the cortex rather than locally to the skin.3
Approach to the Diagnosis of Pruritus
Pruritus is the most common sign of cutaneous disease. Most often in large animals it is caused by ectoparasites or a hypersensitivity reaction, or both (e.g., Culicoides hypersensitivity), but it may also be caused by cutaneous bacterial or fungal infections (e.g., dermatophytes, Malassezia species) (Box 11-1). Because pruritus may be a feature of a more generalized disease process, it is important to take the patient’s general health into account. Hypersensitivity reactions, which are commonly pruritic, may or may not be limited to the skin. For example, anaphylaxis is a life-threatening hypersensitivity reaction that may manifest as pruritus in its early stages. Other pruritic skin diseases include immune-mediated diseases such as pemphigus foliaceus; direct irritation by chemicals; and photoactivated dermatoses. It is helpful to formulate a differential diagnosis by considering each of these broad categories of diseases and using historic information, other cutaneous signs, and appropriate diagnostic tests to narrow the list of differential diagnoses.
The following steps are a guide to the diagnosis of pruritus in the horse and ruminant:
NODULES, TUMORS, AND SWELLINGS
Definition
A nodule is a circumscribed, solid elevation larger than 1 cm in diameter that does not deform when palpated. Nodules extend into the deeper layers of the skin and are usually the result of cellular infiltrates in the dermis or subcutis. “Tumor” is a less precise term that usually refers to a neoplastic, nodular enlargement of the skin or subcutaneous tissue.3 The term “tumor” is most commonly used to describe very large nodular neoplasms. In addition to nodules and tumors, swellings include elevated lesions that pit with pressure (wheals) and fluctuant lesions (cysts and abscesses).
Mechanisms of Nodule, Tumor, and Swelling Formation
Nodular lesions can be subdivided into inflammatory and neoplastic lesions. Inflammatory nodules are composed of a massive mixed cellular infiltrate involving the dermis, the subcutis, or both. The inflammatory infiltrate may contain variable numbers of neutrophils, histiocytes, lymphocytes, plasma cells, and eosinophils. Cellular infiltration usually is stimulated by the presence of foreign material, and the nature of that material influences the composition of the inflammatory infiltrate. The foreign material may be infectious (parasite, bacteria, or fungi) or noninfectious (fibrin, crystalline material, or other inert substances). Grossly visible nodules develop as the masses of inflammatory cells accumulate in the tissues to phagocytize or wall off the foreign material. As the lesion enlarges, the dermis and subcutis are obliterated by the inflammatory infiltrate and the overlying epidermis may become atrophic, resulting in ulceration of the nodule’s surface.
Most cutaneous and subcutaneous neoplasms form nodular lesions. Cutaneous and subcutaneous neoplasms may either arise from a cell type of the epidermis, dermis, or subcutis or less commonly metastasize from another tissue of origin. Cytologically and histologically neoplasms are composed of a uniform population of pleomorphic cells with variable atypia. Neoplasms may stimulate a secondary inflammatory reaction.
Swellings include solid lesions, such as nodules and tumors, as well as urticaria, cysts, and abscesses. Urticarial lesions (wheals, hives) are often transient, localized, inflammatory lesions caused by a vascular reaction in the dermis in which vasodilatation results in fluid transudation with or without erythema. The fluid is not compartmentalized but dispersed evenly throughout the dermal tissue. The result is an elevated lesion that, unlike a nodule, pits with pressure and often dissipates within minutes to hours as the fluid is resorbed. Typically a sparse, perivascular infiltrate that is usually lymphocytic is seen, although the infiltrate may be dense and intermingled with eosinophils. Urticaria is usually well circumscribed, although with confluence the edema may assume geometric shapes.
A cyst (Latin for sac) is an epithelium-lined cavity containing fluid or semisolid material.3 A cyst usually presents as an elevated, smooth, well-circumscribed, fluctuant mass. Cutaneous cysts usually are lined by adnexal epithelium (hair follicle, sebaceous or apocrine epithelium) and are filled with cornified cellular debris and sebaceous or apocrine secretions.
An abscess is a localized, fluid-filled, fluctuant lesion; if large enough, it may be ballotted. It results from a dermal or subcutaneous accumulation of the debris of dead cells and tissue elements liquefied by the proteolytic and histolytic enzymes elaborated by polymorphonuclear cells (e.g., pus). Abscesses most commonly result from localized infection, although they occasionally result from septicemia or may be sterile.
Approach to the Diagnosis of Nodules, Tumors, and Swellings
Nodules, tumors, and swellings may arise from a variety of cutaneous disorders and, in rare cases, as signs of a systemic disease. The major categories of diseases that should be considered when forming a differential diagnosis include hypersensitivity reactions, infectious diseases, sterile inflammatory diseases, and neoplasia (Box 11-2). The primary systemic diseases that should be considered are amyloidosis, lymphosarcoma, and anaphylaxis.
The following steps are a guide to the diagnosis of nodules, tumors, and swellings in horses and ruminants:
ULCERATIONS AND EROSIONS
Definition
An ulcer is a cutaneous defect that results from a complete loss of the epidermis and usually part of the underlying dermis.3 Ulcers often heal with scarring that is caused by destruction of dermal collagen. An erosion is a cutaneous defect that results from a partial loss of the epidermis that does not penetrate beneath the basal laminar zone. Because an erosion does not involve the dermis, it heals without leaving a scar. Because the epidermis is a cutaneous barrier to invading microorganisms, ulcers and erosions often are secondarily infected.
Mechanisms of Ulcer and Erosion Formation
Ulcers and erosions are secondary lesions. Primary lesions develop spontaneously and are a direct reflection of underlying disease. Secondary lesions evolve from primary lesions or are artifacts induced by excoriation or external trauma. Primary lesions that may lead to the formation of ulcers and erosions include fluid-filled lesions such as pustules and vesicles. Rupture of these fragile lesions results in epidermal destruction and erosion or ulcer formation. Swellings such as abscesses and cysts may also rupture, resulting in ulceration, but these primary lesions are more stable and often remain intact. Nodules and tumors may become secondarily eroded or ulcerated. As the nodule or tumor enlarges, the mass exerts pressure on the overlying epidermis, leading to epidermal atrophy and ultimately a break in epidermal confluence, resulting in ulceration and erosion. The most common cause of ulceration and erosion is pruritus, which induces excoriation and hence epidermal destruction. Ulcers and erosions may also result from external trauma, such as epidermal destruction arising from mechanical, thermal, or chemical causes (Box 11-3).
Approach to the Diagnosis of Ulcerations and Erosions
To diagnose the cause of an ulcer or erosion, the clinician must first determine the primary lesion that resulted in ulceration and erosion. Ulcers and erosions occurring secondary to pustules and vesicles, to swellings such as abscesses and cysts, to nodules and tumors, to pruritus, and to external trauma must be differentiated. The list of differential diagnoses relevant to each of these groups of primary lesions is then considered.
The following steps are a guide to the diagnosis of ulcerations and erosions in horses and ruminants:
PAPULES, PUSTULES, AND VESICLES
Definition
A papule is a solid, circumscribed, elevated lesion up to 1 cm in diameter. Papules are essentially small nodules that do not extend beneath the dermis. A pustule is a fluctuant, circumscribed, elevated accumulation of pus (inflammatory cells and often necrotic debris) up to 1 cm in diameter (e.g., a small abscess). Pustules are frequently associated with infectious diseases, although sterile pustular diseases (such as pemphigus foliaceus) exist. A vesicle is a fluid-filled, acellular, circumscribed, elevated lesion up to 1 cm in diameter. A bulla is a vesicle that is larger than 1 cm in diameter. All these lesions can be either follicular or nonfollicular in orientation, depending on the underlying cause. Pustules and vesicles are rarely seen clinically because of their fragility and hence their susceptibility to rupture. Because papules are solid lesions, they are more stable and therefore more commonly encountered.
Mechanisms of Papule, Pustule, and Vesicle Formation
Papules usually form as a result of an infiltrate in the dermis, which can be either cellular or noncellular. Cellular infiltrates may include inflammatory or neoplastic cells, although neoplastic papular lesions are relatively uncommon in large animals. Inflammatory infiltrates may be mixed, containing variable numbers of neutrophils, histiocytes, lymphocytes, plasma cells, and eosinophils, or one cell type may predominate. The composition of the inflammatory cells is influenced by the underlying cause of the papule, and the possible causes are extensive. Noncellular papular infiltrates include substances such as edema fluid, amyloid, and proliferative collagen. Epidermal hypertrophy may contribute to or be the sole cause of papule formation.
Pustules form as the result of an intraepidermal, subcorneal, or, less commonly, subepidermal accumulation of inflammatory cells. Infiltration of inflammatory cells, particularly polymorphonuclear leukocytes, leads to the release of proteolytic enzymes that liquefy tissue elements and result in the formation of a fluctuant lesion. Eosinophils, acantholytic cells, and infectious organisms may also be noted in a pustule, depending on the underlying cause. The stimulus leading to pustule formation is most commonly infectious, although pustules can result from noninfectious causes such as hypersensitivity reactions and autoimmune disease.
Vesicles form either at the dermoepidermal junction (subepidermal) or in the epidermis (intraepidermal) as a result of destruction of the basement membrane zone or confluence of intercellular edema (spongiosis). Clinically the two types of vesicles are indistinguishable. Vesicles form as the result of some viral diseases, during severe inflammatory reactions (allergic contact dermatitis), or with cutaneous physical damage (mechanical, chemical, or thermal). In pemphigus foliaceus, autoantibodies presumably bind to transmembrane proteins between the epidermal cells, causing disruption of epidermal intercellular attachments. The result is intraepidermal cleft formation that leads to vesiculation. In bullous pemphigoid, complement-activating antibodies bind to antigens in the basement membrane zone, causing degranulation of mast cells, chemotaxis of neutrophils and eosinophils, and release of tissue-destructive enzymes that injure the basement membrane zone. The result is loss of dermoepidermal adherence and vesicle formation.3 Vesicles are transient, fragile lesions and therefore are rarely recognized clinically. If they are not destroyed by surface trauma, rapid infiltration by inflammatory cells transforms a vesicle into a pustule.
Approach to Diagnosis of Papules, Pustules, and Vesicles
Although papules, pustules, and vesicles may look somewhat similar on a cursory physical examination, the clinician must differentiate among the three and determine which of the lesions are present. Examination with a hand lens may help. The differential diagnoses relevant to papules, pustules, and vesicles are not necessarily the same (Box 11-4). In all cases it is important to determine if disease is limited to the skin or if the animal’s general health is compromised as well.
Papular lesions have the most extensive differential diagnoses:
 Hypersensitivity reactions. Parasitic hypersensitivities are the most common (e.g., Culicoides hypersensitivity), although drug and (rarely) food hypersensitivities should also be considered. Many hypersensitivity reactions are pruritic.
Hypersensitivity reactions. Parasitic hypersensitivities are the most common (e.g., Culicoides hypersensitivity), although drug and (rarely) food hypersensitivities should also be considered. Many hypersensitivity reactions are pruritic. Parasites. Some species simply irritate the skin with their bites (e.g., horn fly [Haematobia irritans]) without inducing a hypersensitivity reaction.
Parasites. Some species simply irritate the skin with their bites (e.g., horn fly [Haematobia irritans]) without inducing a hypersensitivity reaction. Infectious diseases (bacterial, fungal, and viral). Typically papules caused by infections have a follicular orientation.
Infectious diseases (bacterial, fungal, and viral). Typically papules caused by infections have a follicular orientation. Uncommon causes, including autoimmune diseases, such as pemphigus foliaceus, and diseases of uncertain cause, such as equine sarcoidosis.
Uncommon causes, including autoimmune diseases, such as pemphigus foliaceus, and diseases of uncertain cause, such as equine sarcoidosis.Pustules are most commonly associated with bacterial infections, although fungi and, in rare cases, parasites (Demodex species) can cause pustule formation. Sterile pustular diseases are less frequently seen (drug eruptions, sterile eosinophilic folliculitis of cattle)5 but should be included in the differential diagnoses. Vesicles are rapidly infiltrated by inflammatory cells and transformed into pustules. Diseases commonly associated with vesicles include viral diseases of ruminants, autoimmune diseases, contact dermatoses, and burns.
The following steps are a guide to the diagnosis of papules, pustules, and vesicles in horses and ruminants:
SCALING AND CRUSTING
Definition
Scale is a visible accumulation of fragments of the horny layer of the skin (stratum corneum); it represents the final product of epidermal keratinization.3 The process of forming the stratum corneum is termed cornification. Histologically scale is recognized as hyperkeratosis and can be subdivided into parakeratosis (cornification with nuclear retention) or orthokeratosis (cornification without nuclear retention). In some conditions parakeratosis and orthokeratosis may be present together. Grossly the scale varies in appearance. The color may be white, silver, yellow, brown, or gray. The consistency may be bran-flake—like, powdery, coarse, greasy, or dry. Scale can be either loose or adherent to the skin or hair shafts.
Crusts are composed of variable amounts of serum, cells (leukocytes, erythrocytes, keratinocytes), fibrin, infectious agents (bacteria and fungi), debris, and/or medications. They often cover erosions or ulcerations. Heaped-up crusts are referred to as vegetations. On the basis of their histologic composition, crusts may be subdivided into cellular, serocellular, serous, and hemorrhagic types.
Mechanisms of Scale and Crust Formation
Scale results from increased desquamation (exfoliation) of the stratum corneum. Exfoliation is the final stage of keratinization, the process by which the permanent population of cells of the basal layer of the epidermis divides, undergoes specific patterns of differentiation, and progresses toward the surface, where it is shed.3,5 Excessive exfoliation and scale formation occur when the rate of keratinization is accelerated; when trauma to the surface of the epidermis (chemical, mechanical, or thermal) loosens the stratum corneum; or when the structures sustaining epidermal intercellular cohesion (such as transmembrane proteins) are destroyed, resulting in a loss of cohesion between epidermal cells.
Because crusts are composed primarily of serum and cells, their presence on the skin surface implies that vascular and epidermal permeability has increased to permit their formation. Serum and inflammatory cells are released into the tissues from the dermal vasculature, then cross the epidermis to the skin surface either through erosions or ulcerations or by permeating between the intercellular spaces. The exudate dries on the skin surface, in combination with any medication or debris that was already present on the hair or skin, to form the visible crust. Desquamating keratinocytes may be swept up in the exudate and become part of the crusts. Bacteria frequently invade crusts after they have formed and will be noted on histologic examination, even though they may not be a factor in the pathogenesis. Fungal organisms, when present, are more likely to be important to the pathogenesis of the underlying disease process.
Approach to Diagnosis of Scaling and Crusting
The most important factor in determining the underlying cause of scale or crust formation in either a horse or a ruminant is to determine if the patient is pruritic and if some or all of the lesions are induced by self-trauma. If pruritus is a feature, the approach to diagnosis of pruritus should be used because all pruritic diseases can cause scale and crust formation. If the patient is not pruritic, the most important differential diagnoses include infectious diseases (particularly dermatophilosis and dermatophytosis), nutritional disorders, toxicities, autoimmune disease (pemphigus foliaceus), cutaneous filariasis, photosensitization, irritant contact reactions or burns, and diseases of uncertain cause (for example, in equine patients, sarcoidosis, aural plaques, and primary seborrhea) (Box 11-5).3,6 Viral diseases are important nonpruritic causes of scaling and crusting in ruminants, although they usually are associated with ulceration and erosion with involvement of the oral cavity and mucocutaneous regions.
The following steps are a guide to the diagnosis of scaling and crusting in horses and ruminants:
ABNORMAL COAT LENGTH AND DENSITY
Definition
Abnormalities in coat length and density can be subdivided into decreased coat length and density (alopecia, hypotrichosis) and increased coat length and density (hirsutism, hypertrichosis). Hirsutism, or excessive body hair, is far less common than alopecia, which is an absence of hair from areas where hair is normally present. Alopecias are usually classified as scarring (cicatricial) or nonscarring (noncicatricial). In cicatricial alopecias the hair follicles are destroyed, and hair loss is permanent because neogenesis of the hair follicle does not occur in an adult mammal. In nonscarring alopecias the hair follicles are retained; therefore the potential for regrowth remains. Both alopecia and hirsutism may be complete or partial, diffuse or focal, and congenital or acquired.
Mechanisms of Development of Abnormal Coat Length and Density
A basic understanding of the dynamics of hair structure and development is essential to an understanding of the mechanisms associated with pathologic changes in coat length and density.
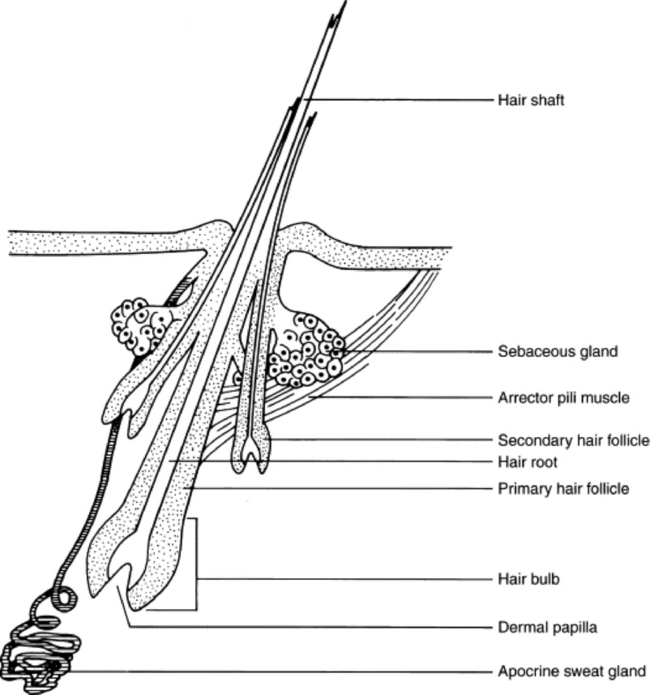
The hair follicle and the sebaceous and apocrine glands are epidermal appendages. The hair follicle forms during fetal development as a downgrowth of epidermal cells toward a group of mesenchymal cells that ultimately become the dermal papillae. The sebaceous and apocrine glands begin as buds of epithelium from the sides of the developing hair follicle.
Hair is composed of keratin and is the product of the hair follicle. The hair shaft is the part of the hair that emerges from the skin surface. The hair root is the part of the hair in the follicle. The hair bulb is a knob of epidermal cells that attaches the follicle to the dermal papilla. Both the hair follicle and the shaft have distinct layers. There are two types of hair follicles: simple and compound. A simple hair follicle produces a single hair. A compound hair follicle produces multiple hairs with bundles of hairs sharing a common skin opening and a single follicle down to the level of the sebaceous gland. Below the sebaceous gland the follicle branches so that each hair has its own hair bulb. Horses and cattle have only simple follicles. Goats and sheep have a mixture of simple and compound hair follicles (Fig. 11-7).3,5
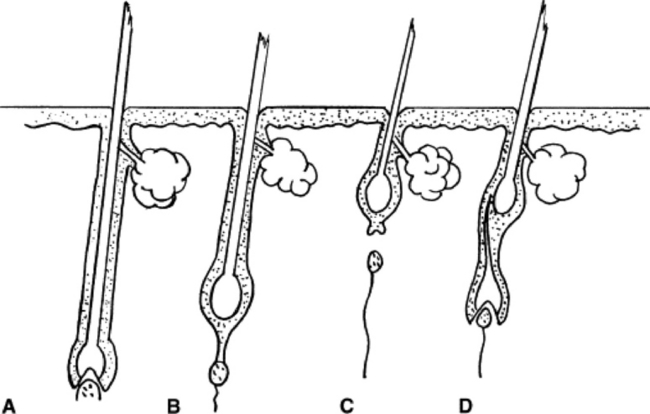
The normal hair growth cycle is divided into three repeating stages: anagen, catagen, and telogen, with the size and shape of the follicle changing during each stage (Fig. 11-8). The amount of time a follicle spends in each phase varies with the species, breed, individual, and body region. In addition, it is influenced by factors such as photoperiod, stress, and disease. Anagen is the active phase of hair growth. Catagen is the transition stage from the growing to the resting state. Catagen is short, and the hair quickly enters the telogen phase, in which hair growth stops. As the follicle reenters anagen, a new hair grows up beside the old and dislodges it. The signal that stimulates progression from telogen to anagen is unknown.
Coat abnormalities may result from a multitude of endogenous and exogenous factors that can modify the normal pattern of hair growth and development.
The length, density, and texture of the coat of a normal animal are determined genetically, and a variety of hereditary defects result in coat abnormalities. These defects may cause changes in hair length, density, or quality. Coat quality may be abnormal at birth or may become apparent sometime before 6 months of age. A given defect may alter the number of follicles present in the skin, or the number of follicles present may be normal but there may be genetic alterations in the way the hair is produced. Altered hair production may manifest as an increased or a decreased growth rate or as structural deformities that result in weak hair shafts that break easily.
Nutritional imbalances can affect growth and maintenance of the coat in various ways, depending on the species. Nutritional deficiencies may result in a shift of greater numbers of follicles into telogen, thus increasing shedding. Dietary carbohydrate and protein deficiencies reduce the length, diameter, and strength of hair. Supplementing the diet with carbohydrate and protein releases protein for keratin formation, provides energy to use protein, and maintains mitotic activity in the hair matrix. Fatty acid deficiencies affect lipid production in the skin, leading to a dry coat with increased fragility. A variety of vitamin and mineral deficiencies may also result in poor hair growth or quality.
Inflammatory skin diseases frequently result in hair loss. Infectious inflammatory processes such as dermatophytosis and pyoderma are usually directed specifically at the hair or hair follicle. Inflammatory processes directed elsewhere may still affect the hair follicle by sweeping it up as an “innocent bystander.”
Hormonal effects on hair growth are complex. Thyroid hormones, corticosteroids, sex hormones, melanocyte-stimulating hormone (MSH), adrenocorticotropic hormone (ACTH), growth hormone, and prolactin all affect hair growth. The effect of a single hormone may be modified in the presence of other hormones, and the importance or effect of any one hormone on hair growth may differ from species to species. Hormonal variations affect the hair coat quality and length by altering the period of time that hair follicles spend in any given part of the cycle, by influencing the rate of hair growth, and by inducing follicular atrophy. External factors such as changes in the photoperiod influence hair growth by altering hormonal levels.
Trauma to the skin is a frequent secondary cause of hair loss. Self-trauma induced by pruritus is the most common cause of alopecia. Hairs may be lost either from trauma to the hair shaft, resulting in breakage, or from trauma to the dermis, resulting in destruction of the hair follicle. In the former case, the hair regrows once the source of trauma has been removed. In the latter case, hair loss is permanent.
A variety of factors can result in hair loss by causing an abrupt shift of hairs into the telogen phase. Recognized causes of telogen effluvium include stress from high fever or severe illness and parturition.
Approach to Diagnosis of Abnormal Coat Length and Density
The differential diagnosis of abnormalities resulting in increased coat and length density is relatively limited and does not provide much of a diagnostic dilemma for the clinician. In the horse increased coat length and density is an acquired abnormality associated with equine hyperadrenocorticism.3 In ruminants defects are congenital and are either the result of an in utero infection (border disease) or a breed-specific hereditary defect.5
The differential diagnoses of decreased coat length and density are extensive. The initial step is to determine if the alopecia is congenital, implying a hereditary defect, or acquired. If the abnormality is acquired, the clinician must determine if it is a primary alopecia or secondary to another cutaneous abnormality such as pruritus or ulceration. If alopecia is the result of another primary cutaneous abnormality, the clinician should focus on the differential associated with that primary abnormality. Finally, to help provide a prognosis for hair regrowth, the clinician should biopsy to determine if the alopecia is scarring (cicatricial) or nonscarring (noncicatricial). Regardless of the underlying cause and its resolution, hair will not regrow with a cicatricial alopecia because by definition the hair follicle has been destroyed. In a noncicatricial alopecia the potential for hair regrowth remains if the underlying cause for hair loss can be identified and resolved (Box 11-6).
Box 11-6 Most Common Causes of Abnormal Coat Length and Density in Horses and Ruminants
Alopecia*
* Alopecia without pruritus, crusts, or other clinical signs.
The following steps are a guide to the diagnosis of decreased coat length and density in horses and ruminants:
The following steps are a guide to the diagnosis of increased coat length and density in horses and ruminants:
ABNORMAL PIGMENTATION
Definition
The following terms are used when discussing pigmentation and pigmentary abnormalities.3
 Melanin is a brown-black, light-absorbing, insoluble pigment formed in many organisms by specialized cells called melanocytes.
Melanin is a brown-black, light-absorbing, insoluble pigment formed in many organisms by specialized cells called melanocytes.Mechanisms of Pigmentation Abnormalities
Cutaneous pigmentation results from the interaction of melanocytes and keratinocytes. The degree of “baseline” pigmentation observed in an animal is genetically controlled. Melanocytes are of neural crest origin and migrate from this site during embryologic development. They are present in nearly all tissues but occur in the highest numbers in the epidermis, mucous membrane epithelium, dermis, hair follicles, leptomeninges, uveal tract, and retina. Epidermal melanocytes are found in the basal cell layer, and each melanocyte is presumed to supply melanin to 10 to 20 keratinocytes. Melanin is usually found in the deeper layers of the epidermis, although darkly pigmented animals may have melanin throughout the epidermal layers.
Melanocytes produce membrane-bound organelles called melanosomes that fuse with vesicles containing the enzyme tyrosinase. Melanin, a black-brown pigment, is produced from tyrosine in the presence of tyrosinase and copper. It is deposited on the protein matrix in the melanosomes. Once melanosomes are fully melanized, they disperse to the periphery of the dendrites of the epidermal melanocytes, and the dendritic tips are phagocytized by keratinocytes. Melanin is also synthesized and transferred to cells of the hair shaft during the anagen phase.3
In general, mechanisms associated with pathologic pigmentary disturbances in large animals are poorly understood. Hyperpigmentation results from increased amounts of melanin in the epidermis or dermis or both. The melanin may be present in melanocytes, keratinocytes, or melanophages (dermal macrophages that have phagocytized melanin pigment). Hyperpigmentation is an uncommon problem in horses because most normally have darkly pigmented skin. Hyperpigmentation may be reversible: with removal of the pigment-promoting stimulus, it tends to decline over time to the baseline level.
MSH may stimulate hyperpigmentation. MSH acts by affecting the levels of cyclic adenosine monophosphate (cAMP), resulting in increased tyrosinase activity. MSH also causes increased dispersion of melanosomes into melanocyte dendritic processes, where they are phagocytized by keratinocytes. Increased levels of ACTH, estrogens, progesterones, and androgens may also have effects on pigmentation, although the importance and mode of action in large animals is not clear.
Inflammation from a variety of causes and persistent cutaneous trauma from friction induce hyperpigmentation. Stimuli that may be factors in large animals include physical cutaneous damage (trauma, friction), chemicals (primary irritants, allergic sensitizers, photosensitizers), infectious agents, and nutritional disturbances.
Hypopigmentation is the result of a decreased amount of melanin in the epidermis or dermis (or both) and may be congenital or acquired (depigmentation). Possible mechanisms include decreased melanin production (defects in melanocyte migration during embryogenesis or disorders of melanin synthesis), decreased dispersion of melanin granules (defective transfer of melanin to keratinocytes), and increased loss of melanin (accelerated desquamation of epidermal melanin, epidermal pigment loss caused by disruption of the basement membrane with resultant pigment incontinence, or immunologic destruction of melanin or melanocytes).
Several congenital genetic abnormalities that result in partial or total hypopigmentation have been identified in large animals. Albinism is a recessive condition in which a normal complement of melanocytes is present but a biochemical defect results in lack of ability to synthesize tyrosinase, so that melanin is not produced. There is complete lack of melanin in all tissues in a true albino. Pseudoalbinism, in which there is ocular pigmentation, may be more common. Other genetic disorders include abnormal melanosome production and abnormalities in melanocyte development and migration from the neural crest (piebaldism).3,5
Acquired hypopigmentation (leukoderma) may be caused by several factors, including genetic abnormalities, trauma, inflammation, dietary imbalances, hormonal influences, and immunologic disorders. In some cases acquired hypopigmentation is idiopathic. Juvenile Arabian leukoderma appears to have a genetic basis because of the predilection for the Arabian breed and the occurrence of the disease in young animals.6 Trauma and inflammation are the most common factors associated with depigmentation, particularly in the horse. The intensity of the inflammatory reaction may bear little relation to the degree of postinflammatory leukoderma. Dietary abnormalities, particularly molybdenum toxicity and copper deficiency, are associated with faded or washed out coat color in food animals. Severe protein deficiency, such as occurs in kwashiorkor in humans, can lead to deficient melanin pigmentation. Melatonin is a hormone produced by the pineal gland that antagonizes MSH, thus causing decreased pigmentation, although an association with pathologic hypopigmentation in large animals has not been documented. Immunologic destruction of melanocytes has been documented in humans and is suspected of being a factor in acquired hypopigmentation in the dog but has not yet been documented in large animals. Idiopathic leukodermas are noted in all species.
Leukotrichia is the result of decreased amounts of melanin in the hair shaft. In most cases the pathogenesis is speculative, and the actual factors are unknown. Melanocytes in the hair bulbs can be affected independently of melanocytes in the epidermis, and leukotrichia without a coexistent leukoderma is common. Leukoderma, however, is usually accompanied by leukotrichia; thus, when the two conditions ae seen in combination, their pathogenesis is the same. Several leukotrichias that occur independently of leukoderma appear to be genetically induced because of breed predilections (e.g., reticulated leukotrichia of quarter horses and spotted leukotrichia of Arabians). In addition, viral infection is suspected as one of the causes of hyperesthetic leukotrichia of horses.
Approach to Diagnosis of Pigmentation Abnormalities
The initial approach to diagnosis of pigmentary abnormalities is to determine whether the defect is congenital or acquired. Congenital pigmentary abnormalities are almost always caused by a genetic defect, whereas acquired abnormalities most commonly do not have a hereditary basis. If the abnormality is acquired, the clinician must determine if it is a primary pigmentary abnormality or if it is associated with some other pathologic change such as inflammation or trauma. If associated changes are a feature of the disease, differential diagnosis should focus on the initial pathologic changes (Box 11-7).
The following steps are a guide to the diagnosis of pigmentation abnormalities in horses and ruminants:
1 Evans AE, Stannard AA. Diagnostic approach to equine skin disease. Compend Cont Educ (Pract Vet). 1986;8:652.
2 Shanley KJ. Pathophysiology of pruritus. Vet Clin North Am Small Anim Pract. 1988;18:971.
3 Scott DW, Miller WHJr. Equine dermatology. St Louis: Saunders, 2003.
4 Gnirs K, Prelaud P. Cutaneous manifestations of neurological diseases: review of neuropathophysiology and diseases causing pruritus. Vet Dermatol. 2005;16:137.
5 Scott DW. Large animal dermatology. Philadelphia: Saunders, 1988.
6 Stannard AA. Stannard’s illustrated equine dermatology. Vet Dermatol. 2000;11:163.