Small Animal Nutrition
When you have completed this chapter, you will be able to:
1 List the energy-producing and nonenergy-producing components of food.
2 List the classes of carbohydrates and describe the catabolism of carbohydrates.
3 Differentiate between lipids and fats and describe the general structure of triglycerides.
4 Describe the structure and functions of proteins.
5 Differentiate between essential and nonessential amino acids.
6 Explain the importance of water in metabolic reactions.
7 Differentiate between microminerals and macrominerals and give examples of each.
8 List the fat-soluble and water-soluble vitamins and explain the importance of vitamins in metabolism.
9 Define the following terms: nutrient, ingredient, formula, nutrient profile, calorie, and kilocalorie.
10 Differentiate between dry, semimoist, and moist food and describe the characteristics of each.
11 Describe considerations in evaluating home-prepared diets.
12 List the legal requirements of pet food labels and considerations in evaluating pet food label information.
13 Describe the components of a nutritional assessment for dogs and cats.
14 List special considerations in feeding adult, pediatric, geriatric, pregnant, lactating, injured, and ill dogs and cats.
15 List and describe routes and procedures for providing nutritional support to hospitalized patients.
NUTRITIONAL OBJECTIVES AND PRINCIPLES
The goal of feeding companion animals is to maximize the length and quality of the animal’s life by reducing nutritional risk factors. For example, the veterinary professional will correlate diet with the life stage of the animal so that an adult dog is fed an adult maintenance food and not a food formulated to meet the needs of puppies. The nutritional goals for companion animals may differ sharply with those for food animals, where the goal in meat production is to encourage rapid weight gain and not necessarily longevity.
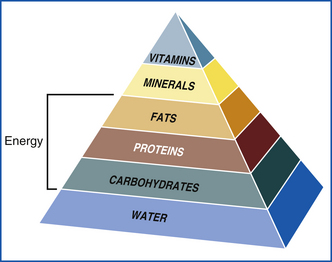
Energy is essential for sustaining life in all animals. It is derived from the components of food and food mixtures known as “the diet.” These energy-producing components include carbohydrates, fats, and proteins. Water, vitamins, and minerals are also essential for life because they are important in many biochemical reactions. However, they cannot be broken down to produce energy directly. The components of food that produce energy are classified as carbohydrates, fats, and proteins; the components of food that do not produce energy, such as water, vitamins, and minerals, are all called nutrients. Nutrients can be defined as any substance that when ingested supports life (Figure 12-1). In summary, nutrients are divided into six categories: proteins, fats, carbohydrates (which are energy producing) and water, vitamins, and minerals (which are nonenergy producing).
NUTRIENT TERMS
The terms nutrient, ingredient, formula, and nutrient profile are easily confused and sometimes used interchangeably. Nutrients are fundamental energy and metabolic substrates classified as essential or nonessential. Ingredients are the raw materials used in food compounding. The formula selects and apportions ingredients for a particular diet. The nutrient profile describes the resulting quantitative distribution of the individual nutrients within the finished formula. These definitions are important to understand and distinguish from one another because clients easily confuse them.
Many pet food companies advertise their product as being “unique” or including fine ingredients. In this way, clients are led to believe that the product has a superior nutrient profile when compared with other brands. Although listing ingredients can be useful in evaluating a pet food, the nutritive value cannot be identified solely on an ingredient statement. An analysis of a particular food can give an indication of its nutrient content and the availability of a particular nutrient, but it is the absorptive capability of the nutrient (combined with availability) that lends nutritional value. In other words, digestibility of a food is a measure of the biologic availability. A balanced diet should supply all the key nutrients and energy needed to meet the daily requirements of the animal at its particular life stage.
Feeding a food with higher digestibility may allow animals to consume less of a particular food. Consequently, feeding highly digestible food may be more economical than feeding a less expensive food with lower digestibility. In addition, because more of the food is biologically usable, there is less waste to clean up in the yard. Digestibility of a food is determined by a mathematic equation comparing the amount of a nutrient in the food and the amount of the same nutrient in the feces (Box 12-1). Above-average digestibility can be defined as protein, fat, carbohydrate, and energy digestibility more than or equal to 85%, 90%, 90%, and 85%, respectively. Food higher in fiber will be lower in digestibility
Palatability of a food involves sensory factors, such as taste, smell, color, and even texture of food (Box 12-2). Palatability is an essential component of an animal’s behavior toward a particular food, and first impressions are generally important. Sensory components, such as smell, can entice an anorectic patient to eat, particularly if the food is warm and strong smelling.
Additives are nonenergy, nonnutrient substances purposely added to food to enhance color, flavor, texture, and stability. Preservatives are defined as substances capable of inhibiting food-deteriorating microbes. Protection against microbes can also be achieved by both physical and chemical means, such as in dehydration (dry food), heat (moist and dry food), and chemical treatments (semimoist and some dry food). Many preservatives are organic acids, and their salts are added to retard oxidation, discoloration, or spoilage.
Humectants are preservative additives that bind to water to inhibit mold and fungal growth. Other chemical agents, such as antioxidants, can inhibit oxidation of fatty acids and fat-soluble vitamins, which protects them from becoming rancid and losing potency. Antioxidants, such as vitamins C and E, are natural preservatives.
ENERGY-PRODUCING NUTRIENTS
Carbohydrates can be further broken down into simple sugars, fats into triglycerides, and proteins into amino acids. The digestion, assimilation, and metabolism of each of these nutrients produce chemical energy that is stored in the atomic bonds of “storage molecules,” such as adenosine triphosphate (ATP). Storage molecules are portable and can be moved to any portion of the cell where energy is needed to complete an important job. In the case of ATP, the energy is stored in the bond that holds the last phosphate atom. When the phosphate atom breaks off, energy is released when the bond is broken. The energy can then be used to carry out a cellular process. Much of the energy that is gained from food is used to maintain and repair cell structures, such as the cell wall and the cytoskeleton. Animals that are growing, reproducing, exercising, or healing from an injury or combating a disease process have a higher degree of cellular activity than animals that are not engaged in these activities. These animals have higher energy (nutritional) demands. Oxygen synthesis and transport, heat production, muscle contraction, and the synthesis of new tissue are additional examples of cellular activity that requires energy.
As mentioned, carbohydrates provide the body with energy. The consumption of carbohydrates in excess of the body’s immediate energy needs are stored as glycogen or converted to fat. Carbohydrates include sugars, starches, and fibers.
Sugars are numerous and include monosaccharides (simple sugars) and disaccharides (complicated sugars). Multiple sugars can bond and link to form complex sugar polymers. Polymerized sugars include starch and fiber. Simple sugars and complex sugars are broken down (catabolized) to provide energy, which is stored in the form of ATP. The type of polymer that is formed depends upon the sugar template and the type of polymer bonds in the molecule. Glycogen is an animal-specific starch and can quickly depolymerize into units of glucose. Stores of glycogen, therefore, provide a rapid supply of glucose to tissues when sugar is urgently needed. Most of the glycogen in the body is stored in the liver and in skeletal muscle tissue.
Digestion of carbohydrates and starch is a multifactorial process involving complex microbes and enzymes throughout the digestive tract. Dogs and cats lack certain salivary enzymes; consequently, digestion of starchy substances is not initiated in the mouth. Food is mixed with hydrochloric acids and other proteolytic enzymes in the stomach, where primarily protein is digested. Carbohydrates and starch are primarily digested and absorbed in the small intestine.
Insoluble fibers are referred to as complex carbohydrates, such as cellulose and lignin, and they make up the structural elements of grass, plants, and wood. In the plant kingdom, starches and fibers are numerous and diverse (Box 12-3). Sources of starch include corn, wheat, rice, barley, oats, and potatoes.
Fiber differs from starch in that fiber is indigestible by the monogastric stomach and small intestines, which lack the enzymes needed to decompose them. However, fermentation of fiber does occur in the large intestine of some animals with simple stomachs. The primary function of fiber in companion animals is to increase the bulk and water content of the intestine. This effect finds applications in reducing caloric density for weight-control food while maintaining satiety. Some metabolic and gastrointestinal (GI) tract transit disorders also respond to increased levels of fiber in the food. For example, fiber is an important part of the diet for dogs with diabetes mellitus because it helps to stabilize blood sugar levels by extending the time that nutrients are absorbed.
Fiber is digestible by bacteria and protozoan microbes in the rumen, cecum, and large intestine of grazing animals. Short-chain fatty acids result from fiber digestion, which in turn are transformed into glucose. Thus fiber serves as a major energy source for grazing animals. The role of fiber in the diet generally depends on the physiology of the animal’s digestive tract, but in most species, fiber assists in regulating bowel function. In addition, the products of microbial fermentation (of fiber) play an important role in maintaining normal colonic function by decreasing pathogenic intestinal bacteria and may play a part in preventing intestinal cancer.
Lipids and Fatty Acids
Lipids that are solid at room temperature are referred to as fats, whereas lipids that are liquid at room temperature are referred to as oils. The lipid is classified as dietary fat. Dietary fats are primarily made up of units called triglycerides, composed of three fatty acids held together by a molecule of glycerol. Fatty acids are the primary components of vegetable and animal fats.
The type of fatty acid primarily determines the structure and characteristic of fat. There are several families of fatty acids, named according to the position of the first double bond. Fatty acids with no double bonds in the primary hydrocarbon chain are referred to as saturated. Subsequently the fatty acid with one double bond is called monosaturated, and the one with more than one double bond is called polysaturated.
The type and distribution of constituent fatty acids determine the physical, nutritional, and biologic characteristics of the fat and oil. Lipids have one to three molecules of fatty acids, are highly digestible, and have twice the caloric density of a similar quantity of carbohydrates or protein.
Fat also facilitates digestion. The length of the carbon chain backbone identifies a fatty acid as long-chain, medium-chain, or short-chain. Short-chain fatty acids (one to eight carbon atoms in length) from rumen fluids and gases are important sources of energy for grazing animals. Long-chain fatty acids (12 to 20+ carbon units) are the most common components of dietary fats and oils in companion animals.
The primary function of fat and fatty acids is multifold. They serve as principal sources of energy, provide palatability and texture to food, and most importantly, supply essential fatty acids and act as carriers for the fat-soluble vitamins (A, D, E, K).
Essential fatty acids are polysaturated, long-chain fatty acids that are necessary for normal body function. Mammals cannot synthesize essential fatty acids; they must be obtained by the food. There are three known essential fatty acids, linoleic, α-linoleic, and arachidonic acids. Linoleic and α-linoleic are the parent compounds from which more complex essential fatty acids are made (Box 12-4).
The essential fatty acids serve many important functions. They are an integral part of kidney and reproductive function and key components to cell membrane formation and prostaglandin production. Deficiencies of essential fatty acids include alopecia, dull hair coat, anemia, and hepatic lipidosis. In the critical patient, essential fatty acid deficiency will increase susceptibility to an infection, weaken cutaneous capillaries, and illicit poor wound healing. Fatty acid deficiency is rapidly reversible if essential fatty acids are reintroduced orally or parenterally.
Amino Acids and Protein
Amino acids are defined as any organic compound containing the amino and carboxyl group. Amino acids occur naturally in plant and animal tissue and are the chief constituents of protein. Proteins are long chains of amino acids held together by peptide bonds. There are roughly 22 known amino acid groups, but these can be arranged in a countless number of ways, each having unique properties and characteristics. Amino acids are considered the building blocks for plant and animal protein.
Proteins are essential to all living cells. Functions include the regulation of metabolism, cell membrane construction, muscle fiber formation, and tissue growth and repair. Proteins are the principle structural component of all body organs and tissues, and serve as enzymes, hormones, and antibodies.
Amino acids are classified as either essential or nonessential. Essential amino acids (Box 12-5) are substances that cannot be synthesized in the body in adequate quantities and must be supplemented in the diet. Nonessential amino acids can be synthesized from other sources. Both are of equal importance in physiologic processes. Taurine is an essential amino acid in the cat because the feline liver has limited capacity to synthesize taurine. Taurine deficiency in the cat results in retinal degeneration, reproductive insufficiency, impaired immune function, and has been linked to dilated cardiomyopathy. Clinical signs of taurine deficiency occur only after prolonged periods of depletion (i.e., 6 months to 2 years). Pet owners typically report visual changes or poor depth perception (“miscalculating” jumps).
The quantity and distribution of essential amino acids in a protein are important features determining a protein’s biologic quality. All proteins are not of equal worth, and an ideal protein contains the exact essential amino acid distribution profile to meet a specific requirement. In other words, the proportion in which it can be used for growth and maintenance of normal body systems measures the biologic value of a protein. Animal proteins generally have a higher biologic value than plant-based proteins.
Protein-containing ingredients are added to most commercial pet food to supply necessary amino acids; consequently, protein digestibility and amino acid composition must be considered in any dietary analysis. Digestibility is an important factor because the ease of digestion aids in easier absorption. Such digestible proteins are of high nutritional value; consequently, smaller amounts are added to the diet to meet an animal’s amino acid requirement. As protein quality is increased, the amount of protein needed decreases. The quality of the protein is often the limiting factor in the amount that must be fed to meet daily requirements.
The improper balance of amino acids can decrease protein quality. Even if digestibility is high, the correct balance of amino acids must be present to classify a protein high in biologic value. Pet food companies will often mix animal and plant substances to provide multiple protein sources to improve the overall quality of the food by providing a wide amino acid profile. In addition, an individual amino acid may be added to the diet if the main protein source is limited to ensure a high biologic value. High-quality protein is especially needed during periods of growth, physical exertion, pregnancy, lactation, and for the repair of damaged tissues.
Amino acids are not stored in the body like fat and carbohydrates. If the animal is unable to consume the required levels of amino acids (e.g., during starvation), the breakdown of protein in the viscera and skeletal muscle will then occur. Skeletal muscle and visceral protein breakdown provide amino acids for energy. The breakdown of circulating and structural protein into glucose is called gluconeogenesis. Gluconeogenesis is initiated by the liver and the kidneys using glycerol, lactate, and glucogenic amino acids. Prolonged starvation or food deprivation in normal animals results in a reduction in metabolic rates to slow fat and muscle catabolism in an effort to survive long-term starvation. Eventually, muscle mass will decrease over time if protein needs are not met. Other signs of protein deficiency include weight loss, dull hair coat, anorexia, immunodeficiency, poor mentation, generalized edema, and death. Note that even a deficiency of a single essential amino acid can be detrimental.
Cats are specifically adapted to high-protein, low-carbohydrate diets and rely on gluconeogenetic amino acids as a major source of energy. Continuous protein catabolism limits the cat’s ability to conserve protein, leading to higher requirements than found in the dog. Dentition patterns of the cat further demonstrate carnivorous eating behaviors, with curved and tapered teeth suitable for tearing the flesh of their prey. Animals subject to chronic anorexia or starvation are in a state of catabolism, which can be reversed by the slow reintroduction of a complete and balanced diet. Metabolic complications can occur if food is consumed or administered too rapidly. Termed “refeeding syndrome,” electrolyte shifts occur from extracellular to intracellular compartments as amino acids are reintroduced. Clinical signs can include cardiac arrhythmias, muscle weakness, hemolytic anemia, and respiratory failure.
Dietary protein in excess of the body’s requirement is converted to fat and stored as adipose tissue. Although the cat must consume twice the protein as the dog, feeding a food with proper levels of protein is essential. The metabolism of excess amino acids increases the liver and kidney workload by increasing the processing and excretory requirements for the urea and organic acid waste by-products.
Protein Requirements: Dietary protein must be consumed every day to replace amino acids lost to catabolism. Protein synthesis will be limited if certain amino acids are not present or available. In addition, pets with trauma, an infection, severe sepsis, burns will increase protein turnover. Amino acids are not stored to the same degree that excess fat and carbohydrates are stored.
Clients often inquire about the best protein intake for animals. Crude protein quantity (on the label) is the usual concern, and clients assume that more is better. However, a high protein number is not always the defining criterion for food quality. Chemical analysis for crude protein measures only total nitrogen content. Unfortunately, the essential-to-nonessential amino acid profile, protein digestibility, and amino acid bioavailability may or may not be measured or stated on the label. It is best to contact the manufacturer directly to obtain this information. Lower quantities of a higher biologic-quality protein usually represent a higher-quality food, thus a more appropriate nutritional objective.
NONENERGY-PRODUCING NUTRIENTS
Although water does not produce energy, it is considered the most important nutrient. Water is essential for almost every chemical reaction, such as the digestion (hydrolysis) of carbohydrates, proteins, and fats. Other functions of water in the body include the transport of solutes and gases, temperature regulation, lubrication of joints and eyes, and electrolyte balance. Water is the largest and heaviest component of our body, making dehydration a common threat to sick patients unwilling or unable to eat and drink. In addition, the physiologic loss of water through diarrhea, vomiting, burns, an infection, etc., in the ill or injured animal will exacerbate anorexia and weakness.
Minerals
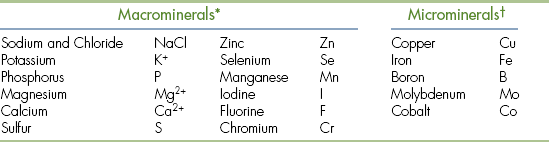
Minerals are inorganic chemicals that are an important part of a balanced diet. More than 18 mineral elements are believed to be essential for mammals. Minerals are divided into two groups: macrominerals and microminerals. Macrominerals are required in relatively large amounts, whereas microminerals are required in very small amounts and are therefore also known as “trace elements.”
Macrominerals: Macrominerals include calcium, phosphorus, magnesium, sodium, potassium, chlorine, and sulfur (Table 12-1).
Calcium and phosphorus are constituents of bone and structural proteins. They sustain the structural rigidity of bones and teeth and participate as cofactors and catalysts in many biochemical reactions. Calcium is also a necessary ingredient in normal blood clotting, nerve transmission, and muscle function.
Phosphorus is also an important macromineral and is a major constituent of bone and muscle formation, energy production, and reproduction. Deficiencies impair growth and normal physiologic processes (Table 12-2). The ratio of calcium and phosphorus is of great clinical significance and should be maintained at 1:1. An imbalance of this ratio, such as an increase of phosphorus to calcium, can lead to serious bone malformation. However, nutritional excesses are far more common than deficiencies; excessive levels of calcium and phosphorus in commercial diets have recently been linked to excessive dental plaque formation.
TABLE 12-2
Mineral Functions and Effects of Deficiency and Excess
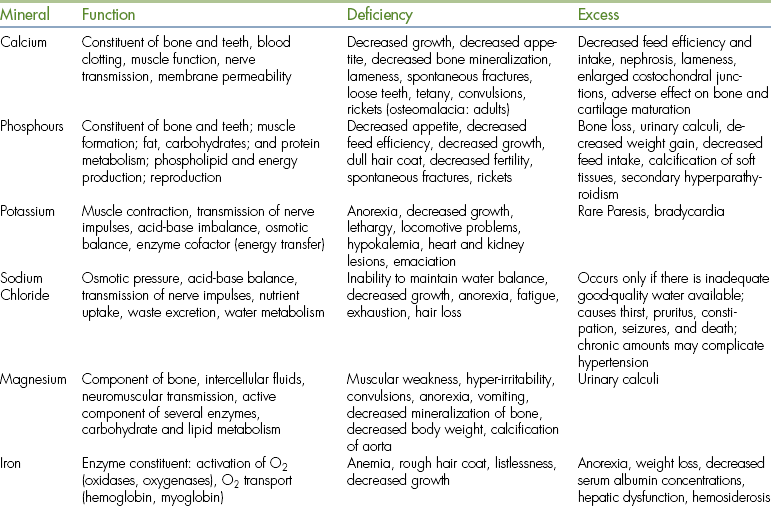
Ca, Calcium; P, phosphorus; Mg, magnesium; Zn, zinc.
From Hand MS et al, editors: Small animal clinical nutrition, et 4, Topeka, 2000, Mark Morris Institute.
Calcium deficiency results in nutritional secondary hyperparathyroidism, where there is increased bone resorption to restore circulating calcium levels. As a result, growing animals have skeletal deformities and lameness. Calcium deficiency frequently develops when inappropriate homemade food is prepared for dogs, cats, and reptiles. Conversely, high levels of calcium and phosphorus are also harmful. Developmental skeletal diseases, such as wobbler syndrome, hip dysplasia, and osteochondrosis, are thought to be associated with high calcium-phosphorus ratios. Feeding vitamin-mineral supplements, dairy products, and just overfeeding the growth or puppy diet may create a nutritional excess of calcium and/or phosphorus.
Concentrations of all macrominerals in the diet are of fundamental importance. Minerals circulate as cation (+ charge) or anion (− charge) electrolytes and play important roles in the osmotic fluid balance, nerve conduction, muscle contraction, blood clotting, blood pH buffering, and numerous other physiologic processes (see Table 12-2). Examples of macrominerals include potassium, sodium, chloride, and magnesium. Deficiencies of macrominerals are uncommon in animals fed a standard commercial diet, but can occur in cases of anorexia, starvation, or dietary insufficiency. Excess macromineral intake can result from feeding large amounts of supplements, such as bone meal, or a diet limited to meat. The owner’s supplementation leads to excess total intake when most commercial diets are already adequate in macrominerals. The technician most commonly encounters this situation among well-intentioned, but uninformed, purebred animal hobbyists.
Macrominerals are measured in the diet as a percentage (%), whereas microminerals are expressed in parts per million (ppm). When evaluating feed as a potential source of minerals, it is best to consider not only the amount of mineral contained in the food, but also on how much the mineral can be used by the animal. Mineral availability in the diet depends upon solubility, metabolic interactions with other nutrient compounds, the signalment of the animal, and the animal’s ability to store the mineral. Animals consuming meat, for example, will consume much higher levels of minerals than animals consuming plant-derived food
Microminerals: Trace elements, or microminerals, are nutrients that are required in relatively small amounts, but are, nevertheless, essential for normal health in companion animals. Important microminerals include iron, manganese, copper, iodine, and selenium. Dietary requirements for these minerals are in ppm (mg/kg) instead of the percentage amounts for macrominerals (see Table 12-1).
The micromineral iron is a central component of the hemoglobin and myoglobin molecules, which carry oxygen in blood and muscle, respectively. Iron is also important in the enzymatic processes of cellular respiration. Because of the limited capacity of the body to excrete iron, homeostasis is obtained by iron absorption. Iron is stored primarily in the liver, bone marrow, and spleen. Because most commercial pet food has high concentrations of iron, as a result of the meat content, iron deficiency is not common among healthy animals fed standard commercial diets. Iron deficiency can be seen in animals with chronic blood loss, such as those with hookworm or other parasitic infestations. A hypochromic microcytic anemia results when iron stores become depleted. Nursing pediatric patients are particularly susceptible to anemia because milk is low in iron.
Other micromineral constituents are chromium, fluoride, nickel, molybdenum, silicon, vanadium, and arsenic. Such trace elements play roles in cell membrane function, teeth and bone development, and growth and reproduction. The amounts required in the diet are low, and deficiencies are rarely seen in animals fed a balanced diet. Dietary excesses of trace elements can be toxic. The proportion of microminerals ingested must be appropriate, or pathologic conditions can result.
Both microminerals and macrominerals can interact with one another. These interactions tend to be of two types, either antagonistic or synergistic. Antagonistic interactions are defined as the presence of one mineral reducing the transport or efficacy of the other. Synergistic interactions are two minerals acting in a complementary fashion by either enhancing biologic function or sparing the other mineral. Most mineral interactions are antagonistic and occur through a number of different mechanisms, such as during processing, digestion, storage, transport, or in the excretory pathway. Even a marginal deficiency of one vitamin can alter the efficacy of another.
Vitamins
Vitamins are organic compounds necessary for normal physiologic function. Most vitamins cannot be synthesized in the body and must be present in the diet. Vitamins are classified as either fat-soluble (vitamins A, D, E, K) or water-soluble (B-complex vitamins and vitamin C).
As a result of such differences in solubility, vitamins are absorbed in the body through a variety of means.
Fat-soluble vitamins require bile salts and fat clusters for passive absorption through the wall of the duodenum and ileum. In contrast, water-soluble vitamins are absorbed via active transport. Water-soluble vitamins are poorly stored in the body, with excesses lost via the urinary tract. Consequently, frequent intake is critical. On the other hand, fat-soluble vitamins are stored in lipid deposits in all tissues and are required in smaller daily doses. As a result of such different absorptive and storage patterns, deficiencies and toxicities vary among fat- and water-soluble vitamins.
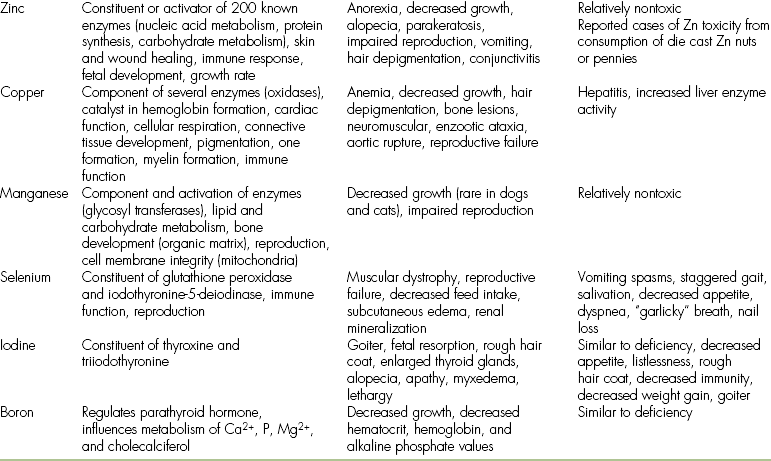
Vitamins are not energy nutrients, and not all types are essential for every species. In addition, an intake in excess of requirements does not improve performance. Oversupplementing fat-soluble vitamins may lead to toxic syndromes (Table 12-3). Conversely, water-soluble vitamins are depleted faster because of a limited storage capability, making toxicity less likely than deficiency.
TABLE 12-3
From Hand MS et al, editors: Small animal cilnical nutrition, ed 4, Topeka, 2000, Mark Marris Institute.
All commercial pet food contains vitamins. However, patients can have vitamin deficiencies. For example, cats fed home-cooked diets rich in polyunsaturated fatty acids (found in fish) are at risk for developing a deficiency of vitamin E. The deficiency causes a painful inflammation of adipose tissue and is commonly known as “yellow fat disease” or pansteatitis.
Vitamin K deficiency is also clinically observed. Vitamin K plays a critical role in the coagulation of blood, and deficiencies result in clotting abnormalities and hemorrhage. Warfarin, found in rodent poison, interferes with the availability of vitamin K and causes fatal hemorrhaging in mice and rats. Pets that consume warfarin-poisoned rodents can become poisoned themselves and may slowly bleed to death without emergency supplementation of vitamin K.
Certain vitamins, such as vitamins C and E, are antioxidants and help free the body of the damaging effects of free radicals. The supplementation of these vitamins above the normal daily requirements can be beneficial. Antioxidants function as electron donors and oxygen and free radical scavengers. They also destroy invading organisms and help to restore damaged tissues. Nutritional antioxidants in canine food helps protect immune function and improve cognitive dysfunction in senior dogs.
Breakthrough research in the field of animal nutrition has also improved senior pet food by the addition of multiple antioxidant agents and omega-3 fatty acids to support cell membranes, protect against free radical damage, and help improve skin and coat condition. In addition, antioxidant additives in pet food may be a natural alternative to synthetic preservatives and improve palatability.
There are vitamin-like compounds that exhibit properties similar to those of vitamins, but are technically not classified as true vitamins. These include carnitine, carotenoids, and bioflavonoids. Their functions include: the metabolism of fatty acids, support of electron transport, and antioxidant capability.
An emerging area of food and food technology includes the clinical use of nutraceuticals. Nutraceuticals are defined in veterinary medicine as endogenous substances that may provide medical or health benefits. They are either specifically defined by the FDA or not defined or regulated. Nutraceuticals have grown in popularity over the past decade; currently, dietary supplements are sold in health food stores, supermarkets, pharmacies, and over the Internet. Clearly, there is a need for increased scientific research in the area of alternative medicine focusing on the mechanism of action, efficacy, and safety of nutraceuticals. Information should be sought directly from the manufacturer of any nutraceutical to advise clients on product selection and use. Examples of nutraceuticals include chondroitin sulfates and glucosamines, which may inhibit inflammatory mediators and promote joint stability, and omega-3 fatty acids, for modulating the immune response in patients with cancer.
PET FOOD EVALUATION
Many clients will ask for recommendations of the best food to feed their pet and will inquire about the many differences between commercial brand foods. Other owners will ask about the suitability of home cooking or about supplementing an existing diet with table food. Note that although various homemade food can be suitable for daily maintenance, most commercial pet food is superior in nutrient content, convenience, cost, and overall quality. Published homemade pet food recipes are generally imbalanced; energy and nutrient requirements for companion animals are not linear, and long-term use will result in nutrient deficiencies or excesses.
Nutritional terms commonly used in commercial pet food includes phrases such as complete and balanced. A complete diet contains nutrients with appropriate bioavailability, and a balanced diet provides the proper amount and nutrient ratio needed for a 24-hour period. In combining these two diets, the animal fulfills both its nutrient and energy requirements. If nonenergy nutrients are in proper concentration to the energy density of the food, the diet is also considered balanced. Complementary diets combine two or more food sources to improve outcome. For example, a small amount of a canned dog food mixed with dry food increases palatability for many dogs.
Other nutritional terms include: all purpose and special purpose. All-purpose food is marketed under the premise that one particular type of diet meets nutritional demands at every life stage. Such diets are typically found in grocery stores to target the uninformed consumer and are generally sold as off-brand or generic food. Formulated for the growth and lactation periods of companion animals, such diets are not appropriate for the other stages of life. In other words, all-purpose food provides nutrients in excess of what is required by the adult or geriatric animal.
Special-purpose food provides specialized nutrition for individual needs. Special-purpose food is designed for animals with specific nutritional needs, such as the obese or obese-prone animal, the working dog, or the sick and injured pet. Special-purpose food is often sold in veterinary hospitals, where clients are educated about which diet is most beneficial for the individual needs of their pets. Many such special-purpose foods are designed to slow down progression of a disease process, such as heart or renal failure, and will require a veterinarian’s approval for purchase.
NUTRIENT CONTENT AND FORMS OF PET FOOD
Commercial pet food is prepared with varying amounts of water. Three basic forms are available to the consumer: dry, semimoist, and moist. Dry food typically has 3% to 11% water. Semimoist food has 25% to 35%, and moist food, which is the most palatable to dogs and cats, contains 70% to 83% moisture. Nutrient profiles vary with each type of food so that both high- and low-quality food can be found in every form. Thus the quality of a diet is not related to the percentage of moisture it contains.
Dry food characteristically has lower proteins, fat, and minerals on a dry-matter basis than most moist food. In addition, dry food is produced with higher caloric density and typically costs less than most moist food. Dry food may also provide a dental hygiene benefit, although neither dry food nor hard-baked treats should replace regular dental prophylaxis.
When dry pet food is made, raw ingredients are mixed and moistened into dough. The dough is kneaded, cooked, and processed via extrusion. Extrusion uses high temperatures to fully cook and shape kibbles, which leads to digestibility and palatability. It is the most common method of making dry and semimoist diets, and it is important in killing the microorganisms that may be carried in the raw materials.
Although dry pet food is less palatable than moist forms, they have the advantage of having a lower true cost (Box 12-6). The true cost of feeding is the cost of feeding a pet per day or cost per year. This important concept needs to be explained to the pet owner because there are significant differences between dry and canned food. Evaluating both types of food on a cost-per-pound or a cost-per-calorie basis may result in an economically sound decision. For example, dry food costs approximately one third as much as moist food on a cost-per-calorie basis. In general, dry pet food is the major source of calories in North America. In addition to being cost-effective, dry food is convenient, easy to use, and allows the owner to leave food out for extended periods of time. In this way, pets may eat on an ad-lib basis. Access to unlimited dry food may contribute to obesity; annual health examinations should include body condition scoring and pet food consultation as the animal ages.
Water may be added to create a “gravy” that improves the acceptability of a dry pet food. In addition, palatability may also be improved by mixing dry food with canned food Keep in mind, however, that if dry food is moistened with water and left outside in high temperatures, bacterial proliferation is possible.
Food-borne illnesses can be prevented by ensuring consumption of moist food within a few hours. Certain bacteria (e.g., Bacillus cereus) are found in soil, grains, cereal products, and other food. These bacteria may be found in small numbers in dry pet food and are normally of no health significance. However, they can rapidly increase in number when moisture levels are raised (e.g., adding water or moist food to dry pet food) at room temperature. These bacteria can produce a potent toxin that causes vomiting and diarrhea. Pet owners should be warned not to add water to dry pet food and leave them exposed to high ambient temperatures for prolonged periods. Dry pet food with added water or mixed with moist food are usually safe if consumed within a few hours.
Semimoist and soft-dry food have a moisture content ranging from 25% to 40% and are composed of a meat and cereal mixture extruded into small, attractive shapes. Artificial flavors provide a sweet, savory flavor yielding high palatability. Humectant preservatives and cellophane wrapping provide a reasonable shelf life and convenience to the pet owner. Antimicrobial additives help prevent spoilage or bacterial proliferation. It is important to know that semimoist food has readily available soluble sugars and simple carbohydrate sources that are not recommended in the obese or diabetic animal or any other animal in which blood sugar needs to be regulated. Sodium concentrations may also be elevated in semimoist and soft-dry food and must be used with caution in the pet with cardiovascular disease.
Soft-dry food is the combined result of semimoist and dry products. Such hybrid mixes give the advantages of the dry food enhanced with the palatability found in the semimoist food.
Canned or moist food is typically 70% to 83% water and has three forms: a ration loaf, an all-meat appearance, or processed meats and flours bound into a jellied matrix by gums or alginates. The high palatability of canned food results from a high content of water, protein, fat, and the inherent flavor of animal-source tissue. Moist food requires portion-controlled feeding to prevent overconsumption because most pets prefer canned products to dry food. Most moist food in North America is sold as complete diets, with all nutrients present.
Moist food is preserved with heat sterilization and vacuum techniques to ensure an anaerobic environment. Enamel liners insulate the product and provide excellent nutrient stability. The shelf life ranges from 12 to 18 months, provided care is taken in storing at normal temperatures. Palatability may decrease toward the end of the shelf life.
Moist food has a low caloric density. Moist food is expensive on a per calorie basis because fresh and frozen meat by-product ingredients are more costly than equivalent meals and flours. In addition, higher packaging costs correspond to a higher daily feeding cost to the pet owner.
The use of moist food as a combination mixer with dry food is an acceptable practice to increase palatability and control cost. Note that as the ratio of moist food increases in a mix, the palatability and percentage of fat and protein calories usually
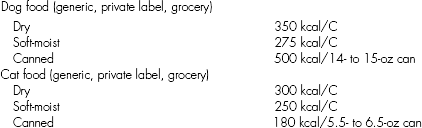
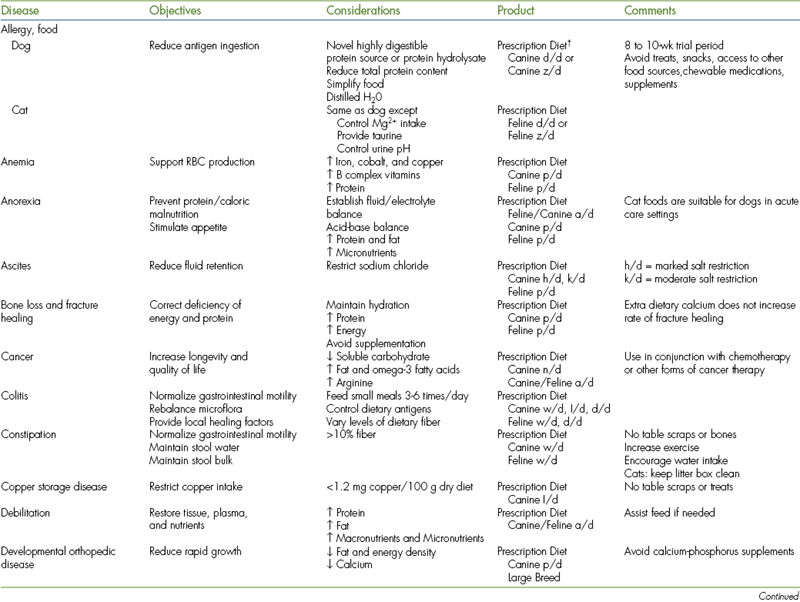
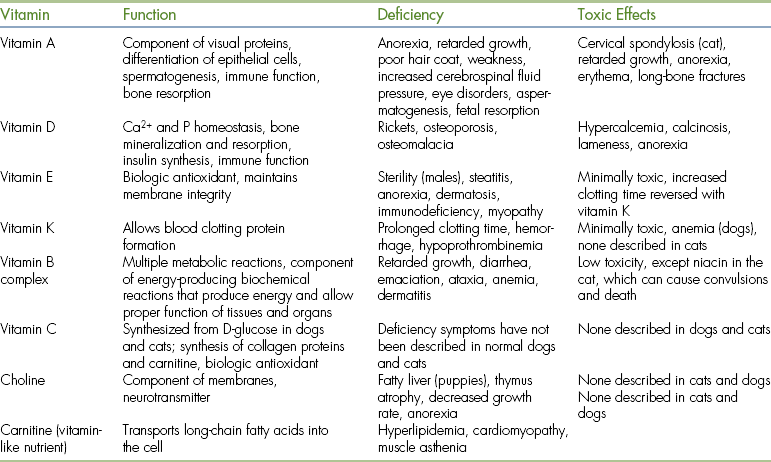
Treats are small food rewards that the pet owner may give as a training aid or to reinforce love or affection. Commercially prepared treats or snacks should not be given in excess because such practice could interfere with normal appetite, dietary balance, and may contribute to obesity (Tables 12-4 and 12-5 ). Chocolate is not recommended because it is toxic in high concentrations. Because treats may be a substantial source of calories and protein for some pets, it is important for the technician to inquire about the use of treats when completing the patient’s history. This is particularly important if the pet suffers from diseases that require dietary restrictions, such as diabetes mellitus, urolithiasis, cardiac and renal insufficiency, and obesity. Commercial treats are not subject to testing as is pet food. Nutritional excesses are common in many commercial pet food treats.
TABLE 12-4
Nutrient Characteristics of Human Snack Foods∗
∗Metabolizable energy for humans.
†Sodium content per serving/sodium content per 100 kcal.
All values from Pennington JAT: Food values of portions commonly used, ed 15, New York, 1989, Harper & Row.
TABLE 12-5
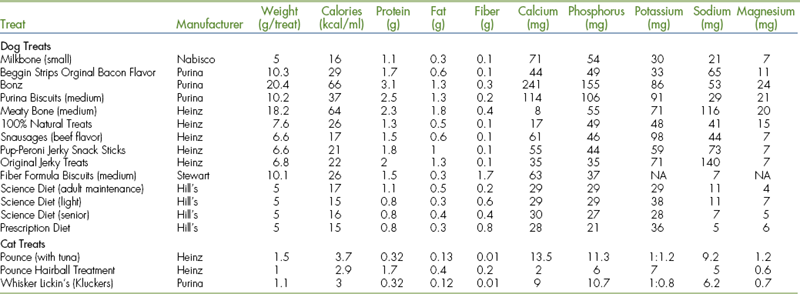
ME, Metabolizable energy; NA, not applicable.
From Hand MS et al, editors: Small animal clinical nutrition, et 4, Topeka, 2000, Mark Morris Institute.
The use of supplements should not be confused with treats. Whereas treats are nutritionally trivial when used in small amounts, the supplement is generally administered to correct a nutritional deficiency. The routine use of supplements is not necessary if the pet is provided with a balanced commercial pet food.
HOME-PREPARED DIETS
Many dog and cat owners prefer to prepare homemade food, despite the fact that most commercial food is easier to use, is less expensive, and provides better nutritional balance. Public interest in homemade diets has increased significantly as a result of the 2007 wheat gluten–related pet food recall. Homemade recipes may not be appropriate for individuals with unique physiologic requirements; consequently, close monitoring of the diet’s efficacy is essential. This may include monitoring weight changes, fecal quality and consistency, food acceptance or refusal, pet activity level, water consumption, complete blood count and serum biochemical changes, and urinalysis changes.
Formulation of a home-prepared diet also requires detailed knowledge of the specific nutrient need, nutritional value of the ingredients, knowledge of any possible dietary interactions, possible deterioration of nutrients during cooking and storage, and consideration of the time and effort required in making such a diet. It is imperative that the owner follow a veterinarian-approved recipe so that a balanced diet is made. There are no human daily supplements that can be added to make a complete and balanced homemade pet diet. If human supplements for vitamins, minerals, and choline are used, splitting the capsules into proper proportions is risky and can easily lead to administration of toxic amounts.
Although it is possible to achieve the same nutrient balance with a homemade food as with a commercially prepared food, it is important for the client to understand that homemade recipes are not tested or evaluated as is commercial pet food. Pet owners interested in feeding a homemade diet should consult with a competent veterinarian or preferably a board certified veterinary nutritionist to obtain a balanced recipe. Veterinarians and technicians together should provide pet owners with recommendations or provide guidelines in assessing homemade food. In addition, the owner’s compliance should be regulated by the veterinary professional and diets kept in conformity with the animal’s needs.
Most homemade recipes have been crudely balanced using the average nutrient content of specific food and computer formulation. Unlike commercial food, few of the numerous published homemade recipes for dogs and cats have been tested to document performance over sustained periods, including tests for palatability, digestibility, and safety. Therefore veterinarians and veterinary technicians should encourage regular dietary histories and patient monitoring for pets fed homemade food. The pet owner must be committed to ensuring consistent, proper homemade food; home-cooked food is more expensive, inconvenient, and requires a major time investment. The purchase of new equipment (kitchen scales that weigh in grams, blender or food processors, etc.) may be required by the pet owner.
The veterinary technician should help evaluate the patient on a homemade diet by noting body weight, body condition score, activity level, and conducting a thorough physical examination. Veterinary technicians should be willing to assess an existing homemade food recipe, offer nutritionally adequate recipes, and make appropriate formula substitutions for clients. Taking the time to counsel clients on the different homemade diets will prevent common problems and increase the client’s compliance.
It should be noted that many homemade diets contain excessive protein and are deficient in calories, calcium, vitamins, and minerals. Most formulations for dogs use staples such as carbohydrates and meat sources containing more phosphorus than calcium, often exceeding the animal’s nutritional requirements. Homemade feline food often is deficient in fat and has low energy density. In addition, no single supplementation can be added to meet the mineral and vitamin requirements found in most commercially prepared food.
Home-Prepared Diet Analysis
Homemade formulations can be checked for nutritional adequacy and adjusted using the following “quick check” guidelines:
• Do five food groups appear in the recipe?
• A carbohydrate, fiber source from a cooked cereal grain or potato
• A protein source, (preferably of animal origin; if multisources of protein are used, at least one source should be of animal origin)
• A source of minerals, particularly calcium
• A multivitamin and trace mineral source
• What is the type and quantity of the primary protein source?
• The overall protein quality in a homemade food can generally be improved by using an animal-source protein. Skeletal muscle protein from different animal species has very similar amino acid profiles; therefore there is no great advantage to feeding one meat source over another. Note that any cooked animal protein source should provide most of the essential amino acid requirements.
• Is the primary protein source lean or fatty?
• The fat content of different cuts of meat varies. When the specified protein source is lean, an additional animal or vegetable fat source should compose 2% to 5% of the formula to ensure energy density requirements.
• Is the carbohydrate source a cooked cereal or potato? Is it present in a higher or equal quantity than the meat source?
• The carbohydrate/protein ratio should be approximately 1:1 to 2:1 for cat food and 2:1 to 3:1 for dog food.
• Is a source of calcium and other minerals provided?
• A homemade food is almost never balanced in minerals; most homemade food requires a specific calcium supplement.
• Is a source of vitamins and other nutrients provided?
• Supplements providing vitamins, microminerals, fatty acids, taurine, and other specific nutrients of concern for cats and dogs should be used in homemade recipes. Owners should consult their veterinarian for proper supplement ratios.
Specific instructions as to feeding and storing homemade food are of utmost importance. Most homemade food lacks preservative agents and is high in moisture content; consequently, such food is very susceptible to bacterial growth. Pet owners should be advised to refrigerate or freeze homemade food and monitor food for color and odor changes. Patients that eat homemade food should be brought in for regular veterinary examinations and nutritional reviews (at least two visits per year). The technician should ask the client to record and submit a 3- to 5-day food history as part of the evaluation.
Cooking techniques need to be reviewed in the homemade diet. Although cooking improves digestibility of starch in the carbohydrates, longer periods of cooking may depreciate vitamin concentration and cause protein denaturation of meat sources.
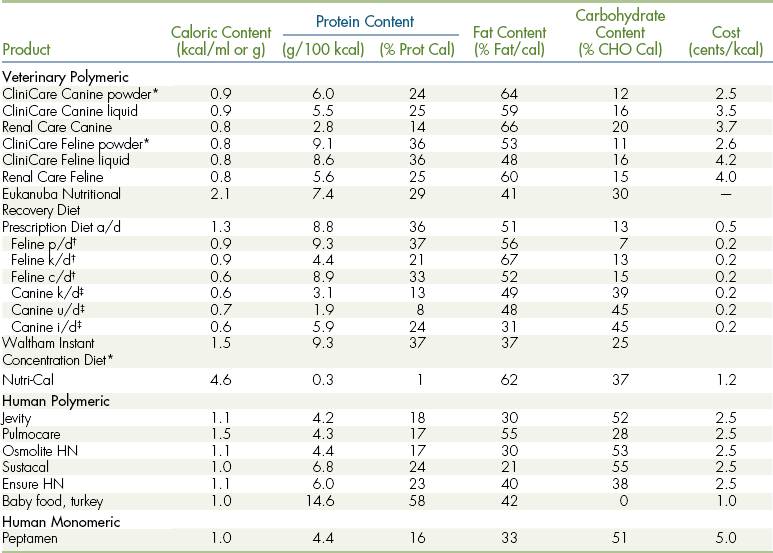
Increased digestibility and caloric density have an inverse relationship to the amount of feces produced in both homemade diets and commercially prepared food. Many owners may be concerned with the volume and firmness of feces excreted by their pet. Notice in Figure 12-2 that the quantity and texture characteristics of feces relate to the amount of dry matter eaten and its digestibility.
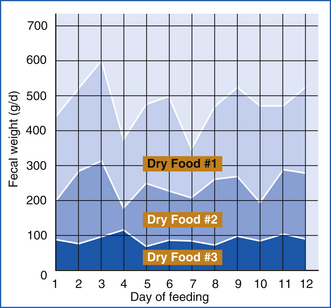
FIGURE 12-2 Increased digestibility and caloric density have an inverse relationship to fecal volume. Food 1 was a lower-energy food and produced voluminous stool volume with difficult cleanup characteristics. Food 3 featured high digestibility and was energy dense, and stool cleanup was quick and nonmessy.
Ingredients for both homemade food and commercially prepared food are packaged to provide useful information, some of which is legally required. Labels should identify both the product and target species.
PET FOOD LABELS
Pet food regulation varies from country to country; the pet food label represents a contract between the manufacturer and the consumer. The Association of American Feed Control Officials (AAFCO) establishes standards for label information and the description of ingredients on pet food sold in the United States. The AAFCO ensures that adequate information is communicated to the consumer about the food product. The association is made up of representatives from a wide range of professional organizations, including: the American Veterinary Medical Association (AVMA), the American Animal Hospital Association (AAHA), and the Pet Food Institute (PFI). Pet food labels provide useful information that enables both the veterinarian and the pet owner to make decisions about what to feed and how frequently to feed it. It should be noted that in the United States, health claims on pet food labels or in accompanying literature are subject to FDA investigation. Pet food labels are required to state:
• Product designator (e.g., cat food)
• Name and address of the manufacturer or distributor
• Guaranteed analyses in percentages for crude protein, fat, fiber, and moisture
• A list of ingredients in descending order of preponderance by weight
Many labels contain more information than what is listed previously. Feeding instructions, caloric content, and a statement that the diet is complete and balanced with respect to a particular life stage are all additional statements commonly found on pet food labels (Figure 12-3). The veterinary professional should counsel clients on how to read a pet food label (e.g., the consumer should consider whether there is a nutritional adequacy statement based on feeding trials and if there is a telephone number on the label for further inquiries).

FIGURE 12-3 A pet food label is the contract between the manufacturer and the consumer. A label provides information required by law and may have optional information, such as a statement of calorie content, the Universal Product Code, batch information, or a freshness date.
The nutritional adequacy statements on pet food labels may vary. Nutritional adequacy statements may use terms such as totally nutritious or complete and balanced. By AAFCO regulations, the nutritional adequacy of a food only requires recommended levels of essential nutrients at two different life stages: growth and reproduction. A statement such as “formulated to meet the AAFCO dog food nutrient profile” (or similar wording) only indicates laboratory analysis for a minimal chemical content. Such testing is not an animal feeding performance trial and says nothing about adequacy, bioavailability, or excesses.
The AAFCO establishes minimal standards for testing new pet food products. These protocols are used by pet food manufacturers during feeding trials to substantiate the nutritional adequacy of their product. The AAFCO animal feeding test statement (see Figure 12-3), which is required on pet food labels, lets the consumer know that the product was used in animal feeding tests and that it performed at acceptable levels. Consequently the veterinary technician should recommend feeds to clients that have the “feeding test” information on the label and not the food with the “formulated” statements, if given a choice. It is important to recognize that under current regulations, a pet food company does not have to run feeding trials on each individual product to be able to claim nutritional adequacy.
Nutritional adequacy statements are not needed on treats or snacks intended for intermittent feeding.
There are no government requirements in Canada for the substantiation of nutritional claims on pet food labels. Pet food that meets nutrient standards and passes digestibility feeding trials is given special seals of certification by the Canadian Veterinary Medical Association.
Evaluating Pet Food Labels
Although there is substantial information on pet food labels regarding food quality, there are also some pitfalls to be examined and considered. For example, percentages listed in the guaranteed analyses state only maximum and minimum levels and do not reflect the exact amounts of each nutrient. In addition, because feed labels are a legal contract between the manufacturer and consumer, the guaranteed nutrient levels are conservative and may be far different from the actual analysis. The manufacturer can often supply a more reliable source of data.
Finally the ingredients on labels are listed by weight, with the heaviest ingredients first and the lightest ones last. This often means that water-containing ingredients are listed before drier ingredients even though a dry ingredient may make up a larger portion of the food on a dry-matter basis. The guaranteed analysis, depending on the country, can also give information as to the average content of the food or at least the minimum and maximum values for key ingredients.
Ingredient Percentages
Percentage rules for listed ingredients are important to note when analyzing a diet for nutritional need. According to AAFCO rules, when a label statement identifies only one ingredient, at least 70% of the total product will consist of that named ingredient (e.g., beef). If any modifying words accompany the named ingredient, the amount of the named ingredient that must be present declines to 10% for moist food and 25% for dry food (chicken dinner, fish entree, liver stew, etc.). In addition, if a named ingredient is modified by the word with (e.g., with beef), the total portion of the named ingredient declines to 3%. Furthermore, if the term flavor is used (e.g., cheese flavor), the named flavor must be detectable only by the animal. The designator food (e.g., dog food) means that there are no rules regarding the minimum content of ingredients. Indirectly the technician may gather further quality information about a product through understanding these nuances of pet food labeling.
Percentage rules also apply to moisture content. In the United States, the maximum moisture content is 78%; pet food may exceed this amount if labeled as stew, gravy, juice, or containing a milk replacer.
MARKET CATEGORIES
Understanding market objectives for a product may assist with some aspects of assessing a food’s quality. Grocery brands are generally well-recognized pet food sold in grocery stores with large-scale advertisement and distribution. Most grocery brands are all-purpose food, balanced for the growth or lactation life stages (see Pet Food Evaluation). “Premium” grocery bands are specific-purpose food types with a more nutritional focus than traditional grocery brands. Other food types include “gourmet” food to sell the consumer on increased palatability for finicky pets.
Generic (white label) and private label (a grocery chain’s own brand) food is made at contract feed mills using least-cost formulation methods. Private label brands are common in large supermarket settings and pet retail outlets. Markets emphasize low cost and high palatability and generally sell on anthropomorphic appeal. Flavor, shape, color, ingredients, and brand name proliferation characterize these products, allowing them to engage the largest amount of shelf space.
Specialty brand pet food is often sold in veterinary hospitals, pet superstores, and regular stores. Often called “premium” or “super premium” food, they generally stress better-quality ingredients with exceptional nutritional focus. Although differences in nutritional philosophy may be noted among different manufacturers, these brands are consistent in the overall objective of emphasizing a philosophy of optimal nutrition. This specialty brand food typically uses the life-stage and special-needs approach, with a general aim at disease prevention.
COMPANION ANIMAL NUTRITION
An estimate of the energy requirement of an animal is needed to determine how much food to feed. If you recall from the Energy Producing Nutrients section of this chapter, the nutrients that provide energy include proteins, carbohydrates, and fats. When these nutrients are burned, they release energy in the form of heat. Each nutrient releases a different amount of heat, which is measured in kilocalories, or Calories (note the upper case “C”). A kilocalorie is the amount of heat (energy) needed to raise the temperature of 1 kg of water 1° C. With this in mind, the energy requirements (food) of an animal would be calculated and expressed in kilocalories.
Daily energy requirements are the number of calories needed to maintain an animal’s weight. Obviously an increase in the animal’s exercise, lactation, and growth would increase energy requirements, whereas a decrease in these activities would lower energy requirements. Increased energy demands over and above the needs for maintenance are called production energy requirements.
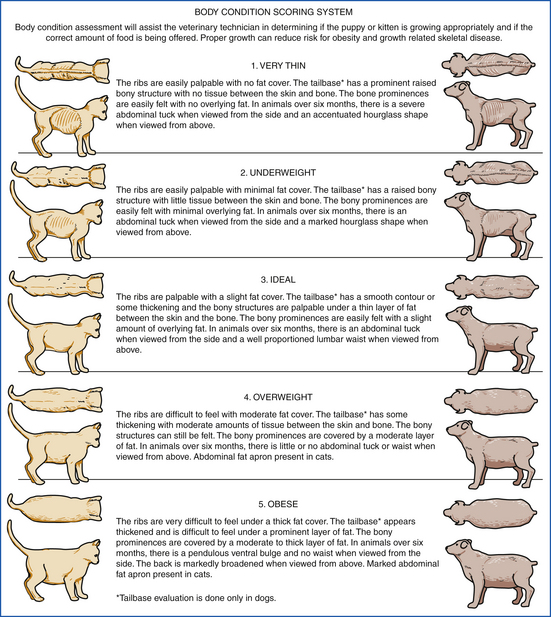
Predictive equations are useful in calculating nutrient requirements, but judging the body composition and condition of the animal is also important in determining the caloric needs of the animal. Body condition can be assessed by feeling the ribs with flat palms. Ideally the ribs should be felt, but not seen (Figure 12-4).
Body condition scoring gives the veterinary professional an estimate of an animal’s body composition. The body condition score can subjectively assess a pet’s fat stores and muscle mass. Note that the body condition scoring system was developed with regard to both age and species.
NUTRITIONAL ASSESSMENT
A thorough nutritional assessment consists of a patient’s history and a physical examination including body weight, body condition scoring, and hydration status. The primary goal of nutritional assessment is to identify the dietary needs of the patient. In the course of a disease or treatment process, a patient’s nutritional needs can change, and these changes need to be monitored regularly and discussed with the pet owner.
A baseline nutritional assessment should be made upon admission to the hospital and followed by serial assessments throughout the course of the hospitalization (see Clinical Nutrition). The veterinary technician is particularly well positioned to identify baseline data and ongoing changes in nutritional status because the technician typically spends the greatest amount of time with hospitalized patients. Nutritional intervention is crucial to recovery and survival, particularly with the critical patient, and appropriate consideration as to the type and route of nutrition should be given based on the underlying disease process or diagnosis (see Routes of Feeding and Tube Selection).
FEEDING DOGS
Dogs are typically omnivores and exhibit eating behaviors similar to their relatives the wolf (Canis lupus) and the coyote (Canis latrans). Dogs are opportunistic eaters, predators, and scavengers and have developed anatomic and physiologic traits that allow for the digestion of a variety of food. Although dogs are omnivorous, pet food advertising emphasizes the carnivorous aspects of the canine diet (“meatier is better”). Many domesticated dogs eat vegetables, grains and pastas, meat, processed food, various dairy products, and fruit. Some pet owners complain that their dog eats grass and feces, though such behavior is natural. Cayenne pepper sauce on feces has been helpful in reducing their dog’s objectionable behavior.
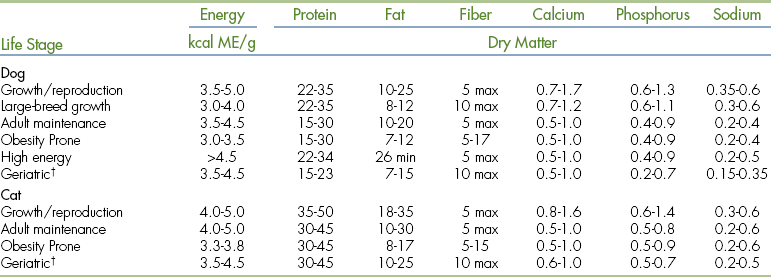
Because dogs range in size, age, and activity level, nutritional energy requirements are calculated based on the animal’s metabolic body weight, or the weight of actively metabolizing tissue. Variations in body composition and breed are also considered. In addition, nutritional requirements should be based on the particular life stage to achieve biologic performance and overall good health (Table 12-6).
∗Nutrients are expressed as % dry matter. Energy is expressed as kcal metabolizable energy (ME) per gram dry matter.
†Older animals require frequent body condition scoring. Feed intake adjustment may be required to maintain an ideal body condition because some older individuals tend to be heavy and others tend to lose weigh.
The amount of food needed to meet the nutritional requirements of healthy dogs is calculated from the energy value of the food (see Energy Producing Nutrients). Whereas most commercially prepared food contains the essential nutrients needed for a particular life stage, each companion animal should be evaluated individually because of differences in both activity and environment. Regular weighing and body condition scoring will enable the technician to provide general feeding recommendations. If treats or table scraps are added to the staple diet, their energy content must also be taken into account when calculating the amount of food to give.
The frequency of feeding normal dogs may vary. Most adult dogs in the maintenance life stage can obtain daily energy requirements by eating once a day, or two to three times a day to coincide with family meal times. Feeding dogs in the late evening should be avoided so that the owner is not inconvenienced by having to take the dog outside to eliminate in the middle of the night. In addition, large meals should be avoided before exercise, particularly in large-breed dogs, so that the possibility of gastric dilation and torsion is minimized.
Canine Pediatric Nutrition
Milk provides a complete food source for neonates, containing water, protein, fat, vitamins, and minerals. Colostrum is the key nutritional factor immediately after birth. Owners should ensure that the dam is producing colostrum and that the puppies are consuming it. This is particularly pertinent if the bitch delivered the puppies via cesarean section. Colostrum provides fluid for vital postpartum circulatory expansion and carries protective maternal antibodies that are absorbed through the intestine of the puppies. Colostrum is somewhat sticky and viscous, which can make nursing more difficult in the weaker puppy.
Most puppies are healthy and are capable of active nursing. Ensure that the mothers are lactating well and are attentive to the litter. In general, no assistance is needed from the technician or owner. Exceptions may include extremely small, toy-breed puppies for which frequent, assisted hand feedings may be needed to prevent hypothermia and hypoglycemia.
Technicians should advise clients to weigh their puppies if there is concern about poor milk production by the dam or an inadequate consumption of milk by the pups. The examination and expression of the mammary glands is also helpful when assessing milk production. Regular checks are important to ensure good milk flow and to make an early detection of mastitis or other mammary gland complications.
The normal growth rate for puppies is 2 to 4 g/day/kg of anticipated adult weight. Weight gain below this rate and accompanied by restless, hungry-seeming puppies is generally a sign that the puppies are not receiving adequate amounts of milk.
Feeding Orphan Puppies
Neonatal puppies that are unable to nurse should be fed a canine milk replacement formula. Canine milk is higher in protein and lower in lactose than bovine milk; consequently, water should be used to mix the replacement formula and not cow’s milk.
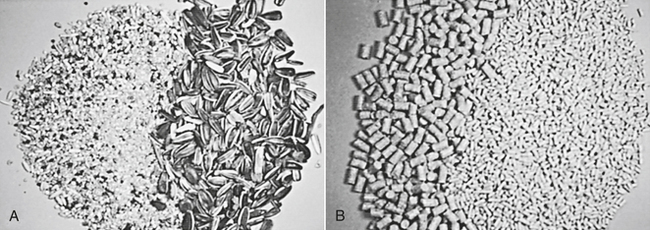
The orphan formula dose is initially 15% of the puppy’s weight per day divided into several doses. The process of feeding puppies can be facilitated by using a syringe and a flexible, rubber feeding tube (Figure 12-5). If the animal has a strong suckling reflex, a small animal nursing bottle or doll’s baby bottle may be used. The nipple may be pierced with a hot needle so that a drop forms over 1 to 2 seconds when the full bottle is tipped upside down. A syringe or eyedropper is not recommended, but can be used in an urgent situation where a bottle is not available. It is essential to deliver the liquid into the mouth slowly to prevent aspiration.
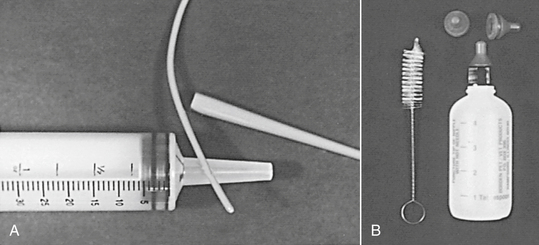
FIGURE 12-5 A, Orphan puppies and kittens are raised on species-specific milk replacement. Tube lavage with flexible feeding tube and a catheter-tip syringe is an easy and safe technique in neonatal puppies and kittens. B, Pet nursers are used in neonates with adequate sucking vigor. Always test the flow and temperature of formula in advance and sanitize equipment between uses.
If a feeding tube is used, care must be taken not to place it in the trachea. The stomach capacity of the neonate is approximately 50 ml/kg. Initially, puppies are fed 10 ml q 4 to 6 hours, and kittens are fed 5 ml q 4 to 6 hours. The amount is gradually increased by 1 ml/feeding (dog) or 1 ml/day (cat) until the recommended guidelines are reached. Although feeding frequencies vary, generally the first 3 days of life are the most critical.
Typically the stomach is full from feeding when the belly is distended or the animal turns its head away from the nursing bottle and squirms. New formula should be made at each feeding and not stored reconstituted to prevent bacterial contamination. Food substances should be room temperature before administration. All equipment should be meticulously clean or sterile. Before the litter of puppies is discharged, the veterinary technician should pretest the flow rate from each of the nipples and give explicit instructions for keeping the system clean. When the puppy reaches 2 to 3 weeks of age, the food dose should approximate 25% of the body weight divided into four to six daily feedings. Monitoring weight gain by the use of a gram scale is a good way to evaluate food intake.
If the puppies are unable to consume formula or dam’s milk on their own, a 5F or 8F infant feeding tube is typically used for gavage. Placement techniques include measuring from the tip of the nose to the last rib, marking the tube, and passing it down the left side of the mouth. A gag reflex is not present until 10 days, but easy passage to the premeasured distance usually indicates correct placement. After delivery of the fluid, kink the tube before withdrawal and withdraw it quickly to prevent aspiration. The animal should be burped after feeding by holding it at a 45-degree angle, massaging the stomach, and patting it gently on the back with fingertips only. The residual stomach volume should be measured by the gentle aspiration of stomach contents (which are then returned to the stomach) before each treatment or feeding to document that fluids are being absorbed and gastric motility is adequate.
When the puppies are able to eat solid food on their own, small amounts of food should be given incrementally until the puppies become content. Satiation is often indicated when the puppies become quiet and fall asleep.
Low birth weight is correlated with an increase in mortality. Puppies with low body weights are more prone to hypoglycemia, hypothermia, and sepsis. The bitch should also be monitored for behavior changes toward any particular pup because the bitch may shun hypothermic and ill puppies. Because body fat is generally low in puppies, the environment should be kept between 84° F and 90° F.
Eternal warming should always be provided if the neonate is separated from its mother. Warming protocols should include the use of circulating hot water blankets only; electric heating pads are not recommended. Other alternatives include warmed rice bags, hot water bottles, heat lamps, or Bair Hugger units, if hospitalized. A pan of water can increase the humidity in the environment. Neonatal incubators can be used to provide a temperature of 85° F to 90° F and a humidity of 55% to 65%.
Whichever heat source is used, the neonate should be able to crawl away from the heat source and the temperature monitored at least every 20 to 30 minutes on the recumbent patient. A thermometer should be placed near the neonate to check the ambient temperature. Hypothermia is common in neonates and is associated with shallow respirations, bradycardia, GI paralysis, and coma. Feeding is contraindicated if the animal is hypothermic (<94° F) because GI motility and digestive function can be impaired.
The neonatal body temperature should be increased slowly. The most effective method is the use of warm inspired air because it warms the core and the external shell (such as provided by the Bair Hugger units, if hospitalized) or an incubator or heated oxygen cage.
Constipation or diarrhea may occur with formula feeding. If diarrhea occurs, the formula should be diluted 1:2 with a balanced electrolyte solution until diarrhea resolves. During the administration of food substrates, the patient’s response may not be typical because the gag reflex does not develop until 10 days of age. Consequently, care should be given for the proper placement of a feeding tube. A baseline birth weight should be recorded; healthy puppies are expected to gain 1 to 1.5 g daily for each pound of anticipated adult weight. Assist elimination every 2 to 4 hours (or after each feeding) for up to 4 weeks using cotton balls soaked in warm water to wipe the caudal abdomen and anogenital region. Wipe down the entire animal with a slightly damp, warm face cloth or soft nailbrush one to two times per day.
Weaning Puppies
Peak lactation occurs at 4 weeks, and weaning concludes at 6 to 8 weeks. Begin introducing puppies to semisolid gruel made from two parts of water to 1 part high-quality, dry, canine growth-lactation pet food. Three weeks of age is a suitable time to introduce a semisolid gruel, except for toy breeds and weak animals, which need more time before they are offered solid food. Gruel can be finely chopped or mashed and placed in a shallow bowl for easy consumption. This serves as an important transition food and acclimates puppies to eating solid food. At 5 weeks of age, puppies are reducing their intake of mother’s milk and are consuming larger amounts of gruel. The ratio of water can be reduced as the puppies are slowly moved from semisolid to solid food. After weaning, the ability for the pup to digest lactose becomes less efficient. Consequently, it is important to avoid feeding weaned dogs large quantities of milk, which might cause diarrhea. In addition, puppies can exhibit competitive eating as early as 5 weeks of age; puppies should be supervised during feeding to ensure adequate and equal consumption.
Feeding Growing Dogs
Proper nutrition for growing dogs is essential for normal growth and development. An excessive intake, however, can lead to medical complications. Overfeeding, for example, can result in obesity in small breeds and rapid growth rates in large-breed dogs. Inciting stress on the juvenile skeleton by overfeeding in the large breeds can cause abnormalities, such as osteochondritis, hip dysplasia, panosteitis, and wobbler’s syndrome. Nutritional requirements change rapidly during a puppy’s growth, with growth rates varying between dog breeds. Nutrient guidelines for small- and medium-breed versus large- and giant-breed dogs are listed in Table 12-6. Supplements are generally not needed if the puppies are fed name-brand commercial diets.
Most growing puppies eat four or five times daily during the postweaning period, or until about 10 weeks of age. Meal frequency should be cut to three meals a day until they have reached approximately 50% of their adult body weight, or approximately 4 months of age. Technicians should advise pet owners to feed small meals several times a day and not allow the puppies continuous access to food because many puppies will overeat when fed ad lib.
Growing Concerns For Large-Breed Dogs
Research studies have documented that improper feeding during growth is associated with several skeletal disorders in large-breed dogs. About 22% of dogs less than 1 year of age are affected by developmental skeletal disorders, and more than 90% of these cases are influenced by nutritional factors. Such nutritional factors include free-choice feeding of a diet with excess calories and supplementing calcium during the growth phase. The onset of bone developmental disorders is usually associated with rapid growth of the long bones. As previously mentioned, the most common of these disorders are canine hip dysplasia, osteochondrosis, and hypertrophic osteodystrophy.
Calcium and dietary fat are, however, key nutrients for growing puppies. Unfortunately, some growth types of pet food contains excessive amounts of calcium, even at appropriate levels of dry-matter intake. A study of two populations of Labrador retriever puppies examined the effects of nutritional excess. One group ate ad lib, and the second group was limited to 75% of the ad-lib quantity. Serial pelvic radiography for 2 years showed significant reductions in hip laxity in the meal-limited group.
To help control the risk of abnormal orthopedic development in large- and giant-breed puppies, experts recommend that the caloric content for large-breed dogs should be less than that for smaller breeds and should contain no more than 12% fat on a dry-matter basis.
Feeding Adult Dogs
The primary objective in feeding the adult dog is to find the maintenance energy requirement and proper food dose to maintain the ideal body composition. Recommended nutrient guidelines for adult dogs are found in Table 12-6. Note that in the adult dog, ad-lib feeding is commonly associated with over consumption and obesity.
The amount of feed needed to meet energy requirements is based upon the energy value of the food. Activity levels also vary between dogs and should be taken into consideration when compiling a feeding protocol. Diverse canine breeds, specifically the variation in breed size, may reflect different metabolic rates and different growth rates. For example, small and toy breeds have a higher energy requirement per unit of body weight than the large and giant breeds because basal metabolic rate is related to total body surface area. Since the smaller breeds have a higher ratio of surface area to body weight than large breeds, they require more energy per unit of weight (lb or kg). In addition, the small breeds have relatively small stomachs, so their ability to consume food is somewhat limited. Consequently, small-breed diets should have a higher energy content and a more nutrient-dense matrix than diets designed for larger breeds. High digestibility is also an important consideration so that optimal nutrition can be provided in small meals. Small, kibble-size dry food should also be considered to aid in chewing and consumption.
Regular weighing and body condition scoring will allow both technician and owner to assess the adequacy of feeding. In addition, environment plays a key factor in energy expenditure. Note that by spaying an animal, energy requirements may decrease 10%; consequently, adjustments in diet may be necessary to prevent weight gain.
Feeding each pet separately is best, whenever possible. In the time-restricted method, feed each dog from one to three times daily with ad-lib consumption for 5 to 15 minutes. If the dog consistently leaves a little food in its dish and also maintains an ideal body condition, the conclusion must be that the animal is self-regulating its food intake at its energy requirement.
Time-restricted feeding works well for many dogs and their owners; however, some dogs ravenously overeat during the allotted time. In dogs that overeat, try volume-restricted meal feeding by serving a calculated food dose. To determine the daily volume, divide the energy requirement by the food’s caloric density. Then feed one half to one third of the daily volume two or three times per day. An average caloric density guideline for pet food is listed in Table 12-6. Other aids for calculating how much food to feed are: the feeding instructions found on the pet food label, food dose calculators, and technical information from manufacturers. Maintenance pet food is recommended for the average house pet who is 1 to 7 years of age.
It is recommended that table food be eliminated or used in moderation (10% or less). Fat trimmings quickly unbalance a base diet and lead to finicky behavior and a predisposition to obesity. Avoid feeding animal bones because sharp fragments may wedge between teeth, lacerate the esophagus, or cause GI obstruction or constipation. Nylon bones and chew toys are safer substitutes for natural bones, but still cause problems in some individuals. Table 12-6 lists guidelines for assessing pet food used in life-stage feeding.
It is best for each dog to be fed individually; however, as a result of time and labor costs, this may be impractical in animal colonies and kennels. Problems associated with group feeding include anorexia in the timid animal and overconsumption in the aggressive or dominant dog. Group feeding may also result in competitive eating. Competitive eating can trigger quick consumption of food, initiating gastric distention from swallowing or quickly gulping air (aerophagia). In larger breeds, aerophagia may predispose the animal to gastric dilation and torsion. Box 12-7 lists general feeding guidelines.
It is common for the boarded animal to be stressed or compromised and as a result stop eating. The late detection of anorexia may lead to significant medical consequences for the animals not having an adequate intake. Technicians should frequently assess the appetite of boarding animals and feed on an individual basis.
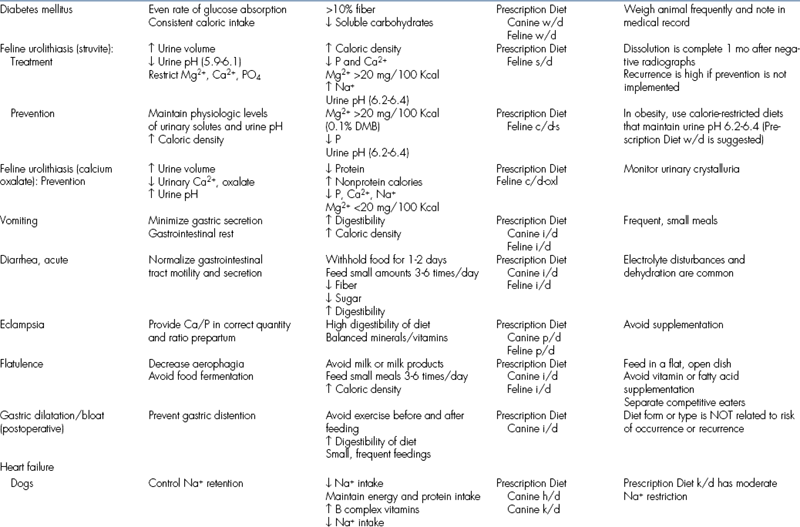
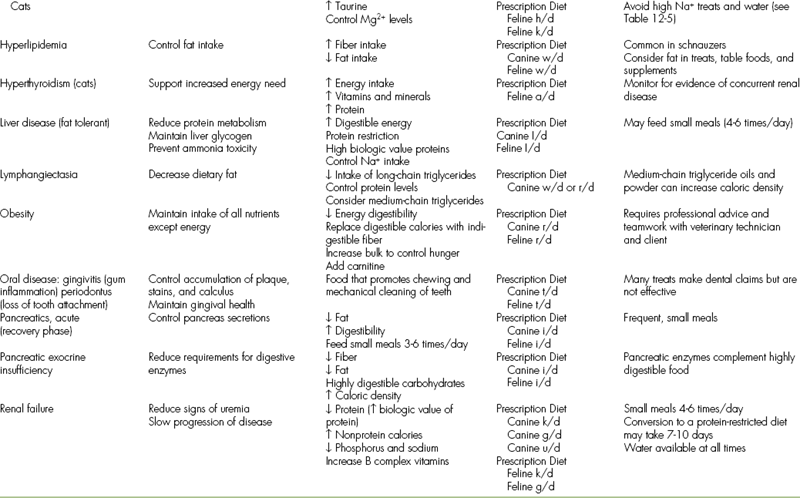
Feeding Adult Dogs With Increased Energy Needs
Increases in physical activity require extra energy to support increased muscular action. Diet and feeding protocols vary according to training schedules and the amount of work performed. Supplying extra energy to working dogs by using pet food with increased fat, caloric density, and digestibility will allow optimal performance. In addition, feeding diets with extra energy content allows dry-matter intake and gastric fill to remain at familiar, nonexcessive levels. Increasing the quantity or frequency of a regular food is a secondary option to increase performance.
The specific nutrient composition of diets for working dogs varies and depends upon the type of activity performed. In general, staples include fats and carbohydrates for intense muscular exercise. Note that in the sprinting or racing dog, short and intense bursts of energy are required, typically obtained by readily available muscle glycogen stores. Large quantities of carbohydrates may be useful because this may help maximize muscle glycogen reserves.
On the other hand, diets high in carbohydrates may be counterproductive in other working dogs and may even reduce athletic performance. High-carbohydrate diets may lead to lactic acid accumulation during prolonged exercise, resulting in muscle fatigue and/or damage. Endurance dogs therefore may benefit from higher fat diets because their muscle activity is powered primarily by aerobic fatty acid oxidation (approximately 70% to 90%).
Animals can be aerobically conditioned before extensive fieldwork. Aerobic training increases the efficiency of fatty acid metabolism in the muscles and the cardiovascular system. Such aerobic conditioning spares the rate of glycogen consumption in muscles and increases the capacity for work. At the start of aerobic conditioning, technicians can advise clients to slowly convert the dog to a more calorie-dense food and suggest feeding the majority of daily calories after the completion of training to help prevent hypoglycemia. This is particularly pertinent in hunting dogs.
Unfortunately, most clients feed the caloric-dense food before work or training. Subsequently, after the meals’ digestion, insulin is released as a result of glucose absorption, allowing for a high rate of glucose transfer into the cells. If the animal simultaneously begins hard work, the combination of the two glucose-consuming activities may precipitate hypoglycemia. If working dogs show consistent signs of hypoglycemia, even after conditioning, they may be fed 10% to 15% of the daily calorie dose as a light feeding at 2-hour intervals during work. Clients should also be reminded of the importance of an adequate water intake throughout the work period.
Feeding During Pregnancy and Lactation
During lactation, a proper nutrient intake is directly linked to successful milk production. Technicians should recommend a growth-lactation formula to meet the increased requirements. Lactation markedly increases energy, protein, and mineral requirements; nutrient requirements during lactation are greater than at any other adult life stage. After whelping, the bitch returns to her regular body weight (Figure 12-6). Expect the food intake to rise rapidly by 50% the first week and by 200% to 400% by the fourth week of lactation. Free-choice food should be available to the bitch. The water intake should also be monitored because water is the most important nutrient during lactation. After whelping, energy requirements return to maintenance levels in approximately 8 weeks. Frequent physical examinations should be performed to maintain normal health and to assess the adequacy of the diet.
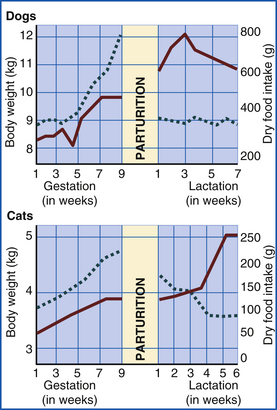
FIGURE 12-6 The pattern of normal weight gain during gestation and loss in the postpartum and lactation periods differs between cats and dogs. Solid line indicates food intake. Dashed line indicates body weight.
Key nutritional factors in the lactating bitch include highly digestible protein, increased concentrations of fat (in proportion with other nutrients), 10% to 20% soluble carbohydrates, and approximately two to five times more calcium than during the maintenance life stage (Table 12-7). Supplements are generally not needed for normal animals when high-quality pet food is used.
TABLE 12-7
Key Nutritional Factors for Reproduction
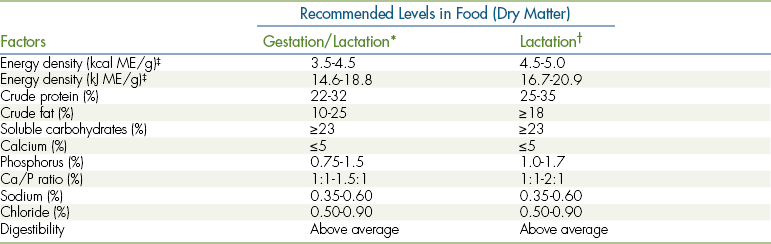
∗Gestation for all bitches and for lactation of bitches with four or fewer puppies.
†Lactation for bitches with litters of more than four puppies. Some giant-breed bitches may need this type of food during gestation to maintain body weight, particularly during late pregnancy.
‡If the caloric density of the food is different, the nutrient content in the dry matter must be adapted accordingly.
From Hand MS et al, editors: Small animal clinical nutrition, ed 4, Topeka, Kan, 2004, Mark Morris Institute.
Feeding Methods During Weaning
The food intake should be terminated for 24 hours to help the bitch slow and stop her milk production. Restricting food will reduce nutrients needed for milk production, resulting in mammary gland reduction. Technicians should advise clients not to allow any puppies to nurse because such practices do not alleviate mammary gland engorgement and may stimulate milk production.
The food intake for the bitch can be resumed using maintenance food at one third of the customary maintenance level. On the second day, two thirds of the normal feeding dose is recommended, with a full intake on day three. As lactation quickly dries from acute calorie deprivation, the bitch will more readily reject the puppies’ attempts to continue to nurse.
Obesity-Prone Animals
Definition, Causes, and Health Risks of Obesity: The incidence of obesity in companion animals is almost epidemic. Obesity is currently the most common nutritional disorder that occurs in companion animals in the United States. Surveys taken in 2007 have reported incidence rates of between 24% and 34% in adult dogs, and between 25% and 40% of the cats seen by veterinarians were considered to be overweight or obese.
Among dogs and cats, certain factors contribute to clinical obesity, including genetic background, high-calorie diets and snacks, physical inactivity, the presence of endocrine or neuroendocrine disorders, and gonadectomy. By definition, obesity means a body composition with a ratio of too much fat to lean tissue or body weight 15% to 20% greater than optimum (Figure 12-7).

FIGURE 12-7 Once formed, fat cells are present for life, though they can shrink. Animals that eat too much as juveniles experience fat-cell division and are subsequently predisposed to excess weight gain throughout their lives.
The early detection of breeds that are prone to obesity is important in preventing and treating the condition. technicians can play a vital role in recommending feeding regimens, exercise strategies, and educating the client on the health risks of obesity. Routine weighing, body condition scoring, and counseling clients during routine examinations can further benefit patients’ health.
A primary cause for obesity is overfeeding during growth life stages. A positive calorie balance during juvenile growth may induce increased numbers of fat cells (hyperplasia). Once formed, these fat cells are present for life and have minimum volumes of triglyceride content below which they cannot shrink (Crane, 1991). Therefore a lifelong predisposition for excess weight develops. Adipocyte hyperplasia is prevented by using meal feeding for puppies, kittens, and foals.
Overeating during maintenance life stages is another factor contributing toward obesity. Consuming more energy than is expended can lead to excess body fat. In addition, feeding the picky eater table food and other diets high in fat contributes significantly to obesity. Excess dietary fat is typically stored as body fat, with storage capabilities almost limitless. Volume-restricted meals and the elimination of calorie-rich treats are recommended to prevent obesity. Adult pets can be fed high-fiber, low-fat treats if snacks are important to the pet owner.
A third cause of obesity is genetic predisposition. Evidence has linked genetic inheritance with resting metabolic rates (Crane, 1991). Breeds at greater risk include the Labrador retriever, cairn terriers, cocker spaniels, long-haired dachshunds, Shetland sheepdogs, basset hounds, and beagles (Box 12-8). Mixed-breed cats tend to be more overweight than purebred cats (McIntosh, 2000).
Another cause for obesity includes a declining lean body mass and declining activity level during normal aging processes. Decreases in energy requirements may be considered in a geriatric feeding program (Markham, Hodgkins, 1989). As pets become older and less active, lean body mass is reduced. Goals for maintaining optimal nutrition in the geriatric animal include avoiding food with excessive protein, phosphorus, and sodium chloride. Refer to the section in this chapter titled Feeding the Geriatric Pet.
Competitive eating may also provoke obesity. Multianimal households or other group-feeding situations may need volume-restricted feeding and separation of the competitive individuals during feeding.
Surgical neutering of males and females can also alter metabolism, deregulate satiety, and increase the desire to feed. The technician may recommend less calorically dense food concurrent with suture removal after neutering, particularly in the obesity-prone breed.
Health Risks of Obesity: The health risks of obesity are numerous. Among the most common include:
• Type 2 diabetes and insulin resistance
• Liver, kidney, and gallbladder disease
• Colon, ovarian, endometrial neoplasia
• Musculoskeletal diseases, including joint stress, hip dysplasia, and osteoarthritis
• Muscular injuries, including cranial cruciate ligament rupture
In addition, obese patients are anesthetic risks and are typically exercise and heat intolerant. Obese patients with ailments such as cardiovascular disease, asthma, elongated soft palates, or laryngeal paralysis are even further compromised and often have increased mortality. In addition, obesity is a predisposing factor for hepatic lipidosis in cats and is associated with some endocrine diseases, such as hyperadrenocorticism, hypothyroidism, and diabetes mellitus. Chemistry and endocrine profiles in the obese animal can be particularly important in identifying compounding disorders. Because obesity is such a common disease among pets, clients should be made aware of the many health risks associated with it. Obesity-related disorders can be prevented or delayed with proper feeding and exercise
Diagnosis and Treatment of Obesity: Assessing obesity among dogs and cats can be accomplished by examining the quantity of subcutaneous fat deposits both visually and by palpation over the ribs, groin, and tail head. Radiographs of the abdomen and thorax will also reveal fat accumulations. Weighing the animal indirectly measures body composition, but using ideal weight tables for purebred animals is useful. Body condition scoring (see Figure 12-4) is a visual and useful method for combining various assessment criteria into an opinion regarding the pet’s body composition and relative fatness. The dietary history should always be included in the patient’s history.
Obesity is best prevented, but can be treated by caloric restriction and exercise. Specific treatment requires teamwork among the owner, the veterinarian, and the technician. In general, dietary recommendations include feeding calorie-restricted, low-energy food. Certain food with increased dietary fiber provide satiety and aid in weight reduction. In addition, feeding a diet high in fiber can reduce total energy intake and improve blood glucose and lipid levels. Clients should be continually reminded of the benefits of weight control because the process can be both slow and frustrating. The veterinary technician can be a critical support person for the pet owner who is enforcing a pet weight-reduction program at home. The technician should recommend to the owner a realistic time frame for weight loss so that frustration is minimized, and the weight-reduction goal is more likely to be reached and maintained. An important part of a pet weight-reduction program is the restriction of supplemental calories in the form of treats, including both human snack food and commercial pet treats (see Tables 12-4 and 12-5). This concept must be especially stressed to the owner who is easily influenced by a begging pet with a plaintive expression.
Feeding Geriatric Dogs
The definition of geriatric as it pertains to the dog is not precise because of breed variability. In general, toy and small-sized breeds are geriatric at 7 years, medium-sized dogs at 6 years, and large and giant breeds as early as 5 years of age.
Geriatric pets undergo physiologic changes similar to elderly humans. Older animals, for example, have a higher incidence of multiple organ failure, benign and malignant tumor formation, osteoarthritis, dental disease, and loss of hearing and vision. Age-associated changes in physiologic function include reduced immune response, reduced digestive and renal function, reduced glucose tolerance, and smell and/or taste perception changes. Unfortunately, no specific diet or nutrient formula can delay the onset of disease or slow down the aging process. However, the dietary practices in the first three fourths of an animal’s life can impact the nutritional consequences manifested in the last part of its life (Burkholder, 1999). Older pets become less active and have reduced lean body mass and have a reduced basal metabolic rate.
Nutritional recommendations for the geriatric pet should be influenced by the individual body condition and health history. The ideal goal in geriatric animals is the maintenance of optimum weight. Commercially available senior diets should be evaluated and only recommended based on the status of the animal. Dietary modifications should be considered if a particular disease state could be ameliorated by the absence or presence of a particular nutrient. Pet food specifically intended for seniors emphasizes moderate energy density with good palatability and reductions of some excess nutrients, as found in all-purpose pet food.
Senior food varies depending upon the manufacturer. Common nutritional factors to take into consideration when recommending a balanced senior diet in the healthy pet include reduced protein, reduced phosphorus and sodium, and increased fiber concentrations. Keep in mind that healthy older cats should not be fed a low-protein diet just because they are old; limiting protein in cats with normal renal and hepatic function can contribute to muscle loss.
Age-related behavioral changes, such as disorientation, owner interaction changes, disturbances in sleep, and loss of bladder or bowel control, may be ameliorated by diets enhanced with antioxidant formulations (Head, Zicker, 2001). Specific therapeutic diets are now available that may help combat the signs of brain aging and improve the learning ability of senior dogs. Exclusive blends of antioxidants and other nutrient formulations help protect against free radical damage, improve cell membrane health, and optimize senior health.
Calorie control may begin or be continued in some older animals. However, blanket feeding recommendations based solely on age are unwise without consideration of the individual. For example, though many geriatric animals have a propensity to put on weight, there are many that lose weight. Weight loss may be a symptom of systemic illness, dental or oral pain, a failing sense of smell, or heightened finicky tastes or fixed food addictions.
Renal Disease: As animals age, many of their organ systems function less efficiently. Chronic progressive renal disease, for example, is common in older dogs and cats. Unfortunately, there is no “quick fix” for chronic renal failure. However, dietary adjustments can slow down the progression of renal aging and prolong the life of a beloved pet.
There are a number of ways that diet can be used to improve a patient’s quality of life and alleviate clinical signs of renal disease. The optimal diet for any given dog or cat will vary according to the stage of its disease, its body condition, if concurrent diseases exist, and practical considerations, such as palatability of the diet to the pet. The progressive loss of renal function can ultimately reduce the animal’s ability to excrete phosphorus, urea, and other by-products of protein metabolism. Controlling excesses of intake during the geriatric periods does no harm, even in the absence of clinical signs of renal failure. Therefore the recommendation to avoid excessive protein, phosphorus, and sodium chloride seems medically prudent. In addition, cats with renal insufficiency have elevated potassium requirements. Commercial prescription diets are designed with these goals in mind and are readily available from a veterinarian. In addition, current research has indicated that feeding diets containing omega-3-fatty acids may be beneficial to the canine with renal insufficiency.
FEEDING CATS
Cats are not “small dogs” and are physically, physiologically, and behaviorally made to be solo-hunting, carnivorous predators. Protein metabolism is unique in cats; typically, cats require higher amounts of protein in their daily diet as compared with dogs (see Amino Acids and Protein).
Key nutritional factors for feeding cats include higher percentages of total dietary calories from an ideal protein source (biologic value of 100%) or approximately 8% in adult cats as opposed to roughly 4% in adult dogs. Carbohydrate metabolism is limited as a result of low liver glucokinase activity, making the feline liver unique in energy metabolism. In general, cats require high-protein, low-carbohydrate food. Feeding dog food to cats for convenience or economy is ill advised because of the different nutritional composition. Feeding a dog food will not specifically provide the required amount of fat and protein. To summarize, cats have obligate and daily needs for additional protein, specific requirements for certain amino acids (e.g., taurine, arginine), increased requirements for many B vitamins, and a reduced ability to digest, absorb, and metabolize carbohydrates.
Taurine is an eleventh essential amino acid in cats. AFFCO has determined that dry feline food must contain 1000 mg/kg of taurine and canned feline food must contain 2000 mg/kg of taurine to prevent diseases associated with deficiencies. Most feline food is now appropriately supplemented in taurine. Other feline-specific requirements include vitamin A, niacin, and pyridoxine. In addition, arachidonic (fatty) acids are not synthesized in the cat; consequently, arachidonic acids are required in the feline diet.
Although calculating energy requirements for cats in differing life stages can be useful, each pet should be examined individually, and nutritional recommendations should be made based on signalment, body condition score, activity level, hydration status, and medical and dietary history. It is important for the technician to consider the influence that diet has in oral health and the texture food can play in preventing dental disease. The palatability and acceptability of a particular food is often influenced by offering food at body temperature, particularly in the hospitalized or ill feline (see Clinical Nutrition).
Feline Pediatric Nutrition
An adequate colostrum intake for all kittens is critical and should be monitored immediately after birth. Like puppies, the orphaned kitten can be raised by tube lavage or pet nurser systems to administer milk replacement (Figure 12-8). It is important to ensure the correct placement of a gastric tube to prevent pulmonary aspiration. Stable environmental factors for pediatric felines are similar to pediatric canines; warm, dry bedding is paramount. Heating pads should cover only half the box for kittens and mother to crawl away from the heat source if it is too hot (see Feeding Orphaned Puppies). In addition, orphaned kittens may need assistance in urination and defecation, similar to orphaned puppies.
Kittens weigh between 85 and 120 g at birth and gain an average of approximately 100 g/week (McCune, 2003). Similar to canine pediatric care, the use of gram scales to monitor weight as an indicator for a proper nutrient intake is recommended. Caloric needs for most puppies and kittens are 22 to 26 kcal/100 g of body weight for the first 3 months of life. Feedings should be scheduled at least four times a day. In general, male kittens grow faster than females.
The formula should be warmed to about 100° F (37.8° C) before feeding. The initial feedings should have less volume (but not frequency) than those directed by the manufacturer. Over the next several days, gradually increase the volume of formula to the amount recommended by the manufacturer. Subsequent increases will be needed based on weight gain and satiation. The formula preparation should follow label instructions, and all feeding equipment must be cleaned immediately after use. The stomach capacity of the neonate is approximately 50 ml/kg. Initially, kittens are fed 5 ml every 4 to 6 hours. The amount is gradually increased by 1 ml/day until the recommended guidelines are reached. Although feeding frequencies vary, generally the first 3 days of life are the most critical.
Kittens are weaned later than puppies—generally at 7 to 9 weeks. Growth-sustaining kitten food are fed two or three times daily until the kitten is 10 months of age.
Feeding Adult Cats
During the adult maintenance life stage, it is recommended to feed a consistent diet and employ a feeding schedule to eliminate finicky behavior and food aversion.
The technician may encounter owners that vary food types as a response to the large number of cat food flavors on supermarket shelves. Providing a variety of flavors is unnecessary, and a transient “newness” factor can temporarily increase food intake and can lead to weight fluctuations.
Most cat owners tend to feed ad lib. When allowed continuous access to food, cats usually eat small, frequent meals throughout the day. A common belief is that cats are better than dogs at maintaining their body condition. However, the latest epidemiologic studies no longer support this idea. When offered a highly palatable, high-fat diet, cats fed ad lib tend to overeat, especially if they are neutered or lead a sedentary lifestyle. A survey of 500 practitioners showed that although most clients were aware of the potential for weight gain in their sterilized cats, only 10% of the veterinarians recommended that the cats be switched to a low-fat diet (Biourge, 2001).
Commercial feline treats are usually nutritionally synonymous with dry cat food (see Table 12-5). As such, they are appropriate to be used as treats, but only if given in moderation. Some cat owners prefer “natural” treats, such as raw or cooked poultry necks, oxtails, or liver. Although little harm results from the use of these treats in moderation, finicky behavior and subsequent nutritional imbalance are potential hazards. Specifically, liver contains an inverted Ca/P ratio (1:17), and potentially toxic levels of vitamin A (hypervitaminosis A) can occur with long-term consumption.
Hairballs occur commonly in cats because of their meticulous grooming habits and the sharp barbs on their tongues, which increase the apprehension and consumption of hair. Hairballs are periodically regurgitated from the oropharynx or esophagus or vomited from the stomach. Occasionally, hairballs pass into the intestinal tract where they are voided in the feces. Owners may observe periodic gagging, retching, and regurgitation or vomiting of hair and mucus. Hairballs are often tubular and usually do not contain food or bile. Although hairballs do not usually cause significant clinical disease, they can be of concern to the owner. Many laxatives, lubricants, treats, and food are available for routine management of these problems. Laxatives and lubricants should be used intermittently because large daily doses may interfere with normal digestion and nutrient absorption. Several complete and balanced moderate-fiber food is now available for control of hairball problems in cats.
Feeding Cats During Pregnancy and Lactation
During the reproductive life stage, energy and nutrient requirements must support both queen and offspring during pregnancy, lactation, and milk production. At peak lactation, energy and nutrient requirements can be three to four times normal maintenance. Because ingesting larger amounts of food may not be feasible, owners can feed a diet that is more energy and nutrient dense, with increased digestibility to reduce bulk. It is important to advise clients that supplementation, with vitamins and minerals, is not necessary as long as the queen is fed a balanced diet.
There are significant differences in the food intake between the bitch and the queen during the initial stages of lactation (see Figure 12-6). As a solitary hunter, the queen hunts less during the early part of lactation and uses the body fat stored during gestation to support her milk production. The practical significance here is that clients may question a low food consumption in their new mother cat. Such clients can be advised that the queen will eat heavily, as expected, by the third week of lactation.
Feeding Geriatric Cats
An evaluation of the geriatric individual is crucial in determining an appropriate food that will maintain a proper body weight and still provide adequate nutrient levels. In selecting the optimal diet for an older cat, overall health must be considered. The food intake should be monitored in association with changes in weight. Hyperthyroidism, for example, is characterized by chronic weight loss despite a ravenous appetite. The water intake should be noted since an increased frequency of drinking and urination may also be symptomatic of disease.
No single food can meet the needs of every geriatric cat. Dietary modification can help to optimize health in the healthy cat and to modulate disease in cats as they age. Significant protein restriction is not recommended in the healthy geriatric cat because of the high protein requirements in felines (see Amino Acids and Proteins). A moderate restriction of protein is recommended for the cat with evidence of chronic renal failure (see Clinical Nutrition). Commercial diets are available with balanced nutrient contents for optimizing the health of the elderly cat. Oral hygiene is an important factor in feline geriatrics; routine dental examinations should be performed to ensure that there is no tooth pain and that food can be apprehended and chewed.
Similar to geriatric canine nutrition, certain dietary adjustments can help improve clinical signs or even slow progression of disease (see Feeding the Geriatric Animal). The best diet, however, should be based on the individual cat’s clinical signs, body condition score, laboratory results, and stage of disease.
Feline Obesity
Feline obesity, like canine obesity, is a common nutritional problem. One important role of the technician is to educate the client and to encourage participation in weight-reduction programs. A detailed dietary history is helpful when calculating the amount of food that will be offered during a caloric-restricted diet. Fasting in obese cats is not recommended because fasting has been associated with the accumulation of lipid in the liver. This can become pathologic over a 5- to 6-week period, and it mimics idiopathic feline hepatic lipidosis (Figure 12-9).

FIGURE 12-9 Fasting in obese cats has been associated with the accumulation of lipids in the liver, which in turn causes icterus.
Obesity can be prevented if the veterinarian and the technician provide nutritional counseling during routine yearly examinations. In addition, the owners of felines that have a gonadectomy should also be counseled as to the amount of food given after surgery to prevent excessive weight gain. Dietary therapy should only be instituted after a complete physical examination, biochemical profiling, and compilation of medical history. It is important to instruct the client to gradually introduce a new food over a period of 7 days. Obese cats that are given a new diet all at once may become anorexic.
Statistics show that cats being fed high-fat (±20%) premium and superpremium diets are two to three times more likely to become overweight. Conversely, cats fed a diet containing around 10% fat are 50% less likely to be overweight. Dietary recommendations for feline obesity include feeding multiple small meals throughout the day to optimize digestive and absorptive energy expenditures. Traditionally, diets are composed of low-calorie, high-fiber substances. Recommendations for caloric restriction range from 50% to 80% of maintenance calories to achieve optimum weight (Burkholder, 2000). Commercial and prescription canned diets are now available that are tailored for the obese cat. Such canned food includes a low-carbohydrate, high-protein matrix. Cats fed some (50% is a good starting point) tailored canned food as part of their diet will reduce the carbohydrates and better control calories (dry food is very calorie dense) and will help increase the amount of water consumed daily. In addition, low-carbohydrate, high-protein formula have been clinically proven to alter a cat’s metabolism for effective weight loss and may help prevent diabetes mellitus in the aging feline. The addition of L-carnitine also helps the feline patient lose weight while maintaining lean muscle mass and decreasing the accumulation of fat in liver cells.
Feline Urolithiasis and Lower Urinary Tract Diseases
The two most common calculi that occur in cats are struvite and calcium oxalate calculi, both of which can lead to lower urinary tract diseases. The amount and balance of mineral elements in the diet of a cat can have significant effects on the formation of urinary calculi. Other important factors in calculi formation include urinary pH, urine concentration, and high dietary magnesium. Although there are many factors that can contribute to the formation of uroliths that are related to diet, uroliths are rarely, if ever, the direct result of diet. The diet can, however, have an impact on the urinary concentration of calculogenic substances.
The water intake is a major factor in determining urine concentration and to some extent frequency of urination. Other factors that can affect urine concentration include the sodium, fat, and carbohydrate content because energy metabolism results in the production of metabolic water. The digestibility of the diet will also determine the amount of water lost in the stool and the quantity of minerals that are absorbed and ultimately excreted. Other aspects of diet that can influence the development of uroliths include the dietary content of minerals, quantity of diet consumed, and the influence of diet and eating frequency on urine pH because some uroliths are more or less soluble in certain pH ranges.
Certain feline diets are formulated to induce acidic urine because of the addition of acidifiers, such as methionine, ammonium chloride, and phosphoric acid. Struvite crystal formation is not possible at a urine pH below 6.5. Particular animal proteins and corn glutens found in feline diets can also promote acidic urine, as opposed to diets composed of vegetable proteins and mineral salts, such as calcium carbonate, which promote alkaline urine.
Urine acidification is not without potential toxicity. Excessive acidity can overpower the ability of the kidneys to excrete protons and induce uncompensated metabolic acidosis. Consequently, chronic acidosis in cats can increase urinary potassium losses and could potentially slow growth, increase urine calcium excretion, and promote bone demineralization.
Acidifiers also can be toxic. Acidifying diets are recommended to safely prevent and manage struvite-related lower urinary tract disease (LUTD). Technicians should refer to the veterinarian before recommending any acidifying diets. These diets are not recommended for kittens because they are not formulated for growth and may interfere with bone formation.
Acidifying diets may also be contraindicated in the older cat; older felines are at a higher risk for calcium oxalate urolith formation and renal insufficiency. No diet will promote the dissolution of calcium oxalate uroliths, but minimize the risk of crystal formation, diets for mature and older cats should be formulated to induce a higher urinary pH. Maintaining urine acidity (pH 6.2 to 6.4) and keeping the magnesium intake at nonexcessive levels are prudent risk-control measures for struvite crystalluria. Maintaining a more alkaline urine pH (6.4 to 6.8) while avoiding excess calcium, sodium, and magnesium are prudent risk-control measures for calcium oxalate crystalluria. It is also beneficial to increase the cat’s water consumption. Feeding a canned food will decrease the cat’s urine specific gravity and increase the overall volume of urine, thus decreasing the possibility of crystal formation.
Note that the main difference between canine and feline urolithiasis is that struvite uroliths are usually associated with urinary tract infections in the dog. Feline struvite uroliths are generally sterile. Bacteria, such as staphylococci and other urease-producing organisms, generally create an alkaline environment, which enhances the formation of struvite and other uroliths. Antibiotic therapy is therefore only recommended in patients with a positive urine culture.
It is an oversimplification to state that controlling urine mineral concentrations or pH always controls feline lower urinary tract disease (FLUTD). FLUTD syndrome is multifactorial; not all causative agents or combinations of contributory factors are presently known. The term idiopathic FLUTD is used in cats where there is no known cause. Potential causes of idiopathic FLUTD include a viral infection, stress, and neurogenic inflammation. Idiopathic FLUTD is not well understood; however, water seems to be a key factor in controlling the recurrence of the disease. Canned and other high-moisture food increases total urine volume and are the preferred products for cats with idiopathic FLUTD.
FLUTD is typically caused by struvite uroliths or urethral plugs, calcium oxalate uroliths, or by a syndrome known as feline idiopathic cystitis (FIC). Clinical signs of FLUTD include urinating outside the litter box, frequency of urination, and/or straining to urinate. Prescription diets are now available that are formulated to provide nutritional management in feline patients with either struvite or calcium oxalate uroliths or FIC. Such diets contain controlled levels of magnesium, calcium, phosphorus, and oxalate to reduce building materials needed to construct potentially harmful crystals and uroliths. In addition, certain specialized prescription feline urinary diets contain limited sodium and high levels of omega-3 fatty acids that may inhibit the inflammatory cascade associated with FLUTD.
 TECHNICIAN NOTE
TECHNICIAN NOTE