Chapter 17 Orthoses
Whilst podiatrists commonly use a variety of clinical therapies, there is one particular therapeutic technique with which podiatry, and podiatrists, have become almost synonymous: orthoses. Although patients and the public probably think of some insole derivative when they hear the term ‘orthosis’, it actually encompasses a broader range of devices, which includes silicone orthodigita, digital covers, latex shields and replaceable pads as well as the functional devices that dominate the literature concerning orthoses. Historically, these devices were manufactured by podiatrists themselves. Modern clinicians, however, have a range of good-quality, mass-manufactured devices at their disposal, which has reduced their reliance on their own manufacturing skills. The devices available range from silicone digital and plantar pads to prefabricated functional orthoses. The availability of such devices has perhaps led to some marginalising of skills of manufacture, for perfectly understandable reasons.
While this chapter will provide insight into some key issues surrounding functional orthoses – including emerging paradigms that influence orthosis design and the role of prefabricated devices – it is also written for those practitioners who still derive much professional satisfaction from manufacturing a range of individually designed orthotic devices that allows them to exercise close personal management of their patients’ condition. This management ranges from the initial consultation to either partial or complete resolution of the condition. The inclusion of partial resolution recognises that in many cases (e.g. the chronic rheumatoid foot) resolution is not possible but restoration of some functional capacity and improvements in pain is the best that can be achieved. It is hoped that this exposure to a variety of historical techniques will inspire a new range of practitioners to become involved in manufacturing orthoses themselves, not necessarily on a permanent basis, but so as to facilitate a deeper understanding and awareness of the range of devices that a skilled clinician can use to their patients’ benefit.
The use of orthoses is based on the premise that most foot problems have some mechanical factors involved in their aetiology or symptomatology. This might be some congenital variation in the structure of the foot and leg, be that bony or soft tissue, the result of a disease process such as rheumatoid arthritis, or due to neuropathy. In all cases the basic treatment philosophy remains the same: pain or pathology resulting from abnormal foot mechanics can be controlled only by mechanical means. This may be achieved by altering structure by surgical intervention to realign bones or to improve soft-tissue function, for example through gastrocnemius release to enhance ankle dorsiflexion and ‘rocker’ function, or through the use of an orthosis to actively optimise the biomechanical function of the foot and lower limb. There is a growing awareness that, in many situations, combined surgical and orthotic management provides the best treatment plan, and indeed podiatrists are now routinely involved in interdisciplinary musculoskeletal clinics where, for example, a surgeon may operate to create an environment where the orthosis provided by the podiatrist has a better chance of success in the long run, and where this likelihood is increased by enhancement of postoperative function through physiotherapy.
While the derivation of the word ‘orthosis’ seems obviously associated with the Greek ‘orthos’ meaning ‘straight’, Rose (1986) asserts that the origin of the word is actually more obscure. Accepting the term ‘prosthesis’ as an older word of ‘respectable’ Greek origin meaning ‘in addition’, and defining a device that is a replacement or substitute part, he suggests ‘orthosis’ to be a portmanteau derived from the terms ‘orthopaedics’ and ‘prosthesis’, in much the same way that ‘smog’ is a combination of ‘smoke’ and ‘fog’. Whatever the origin of the term it is widely used and accepted’ and it is more important that a definition be provided. The recent focus on functional orthoses may lead to the type of definition provided by Philps (1995) or Anthony (1991), but these can only be applied to functional devices, and so are too exclusive. By contrast, Rose (1986) adopted an inclusive definition, which encompasses a broader range of devices and is much more appealing:
A device applied direct and externally to the patient’s body with the object of supporting, correcting, or compensating for an anatomical deformity or weakness, however caused. It may be applied with the additional object of assisting, allowing or restricting movement of the body.
(Rose 1986, pp 6–7)
This definition may be applied to all forms of appliances that have a corrective function, but also to those devices that primarily accommodate and protect deformities without correcting them, for example a hallux abducto valgus shield. Although there is a temptation to divide orthoses into the categories functional and palliative, many devices combine these functions according to the nature of the pathology and the severity and duration of the mechanical abnormality, such that this division becomes somewhat arbitrary and artificial. An appliances that replaces missing parts, whether this be due to disease, trauma or surgery, is termed a prosthesis.
Where correction is possible, even if only partial, the corrective element should take precedence over the protective element, and this consideration determines the choice of materials. Considerable force is often required to correct even a simple deformity, such as a hammer toe, or to manage major deformation, such as abnormal pronation, from occurring under load. The more rigid the material the better its splinting properties, but the lower its tolerance to wear by the patient; it must be remembered that a 100% corrective orthosis is perhaps desirable to the practitioner, but if resigned to the back of the cupboard it will be 100% ineffective, and the practitioner must bear this in mind. It is good practice to build up the wear of an orthosis gradually, but if problems persist despite a prolonged break-in period it may have to be acknowledged that too ambitious an orthosis has been selected.
The plastics used in functional orthoses can be simply classified according to their ability to resist stress according to their thermoforming temperature. The higher the temperature at which they become malleable, the stronger they are; the lower the temperature, the more likely they are to deform under load. However, the thickness of the plastic is also of considerable importance and there is a direct association between rigidity and thickness. More recently introduced are carbon fibre composite materials that offer the practitioner a light, thin and flexible alternative. However, they are difficult to use, requiring a higher forming temperature and a shorter working time, so that the vacuum former must have a rapid action.
Orthoses need to be designed so that they are both tolerable in wear and optimally effective in their therapeutic design. Accommodative appliances, such as latex shields, are used in established deformities to protect vulnerable tissues from trauma and, to some extent, to limit painful movement. They may not correct the underlying fault, but they make it tolerable by relieving painful symptoms and controlling secondary lesions. They are more flexible than rigid, and usually can be well tolerated from the beginning. In some cases it may be useful to use an accommodative orthosis first before moving onto a more functional, corrective one.
Orthoses are worn either on the foot or within footwear and, as such, no matter how well designed and accurately prescribed, manufactured and fitted they may be, their effect is dependent on appropriate footwear. Orthoses and footwear must be considered together if the optimal outcome is to be achieved. The footwear must be of the correct size and shape, have adequate internal volume in the right places, and be correctly balanced both mediolaterally and anteroposteriorly. Modifications to footwear may be necessary to ensure these points. It is a sound principle that patients purchase their shoes after the orthosis is fitted. Heel height is of critical importance when fitting a functional orthosis. If heel height is such that the normal relationship between the forefoot and rearfoot is disturbed, then the shoe is totally unsuited for use with the orthosis. The range of stock orthopaedic shoes now available is such that an attractive shoe at a reasonable cost offers the opportunity to provide a comprehensive orthosis and shoe regimen for many pathologies and situations. Stock shoes have the added advantage that they often come with an insole system that can be removed to facilitate the fitting of prescribed orthoses. A review of footwear is provided in Chapter 18.
Orthotic technology is constantly developing as new materials and techniques are introduced and a greater understanding of foot mechanics evolves. Only a brief summary of its main aspects is possible here, and further reading is recommended to develop a comprehensive understanding of the subject.
PRINCIPLES OF MANAGEMENT
It is essential that practitioners develop a sound working knowledge of the materials and techniques available in order to offer their patients a complete service, even if this is to be provided by an orthosis manufacturing laboratory. At the outset of treatment a management plan should be devised in consultation with the patient, and this should encompass the rationale for orthosis therapy and also the concept that other treatments are likely to be necessary, many of which require the active participation of the patient. This includes, for example, accepting advice on footwear, undertaking exercises such as stretching and strengthening, modification of activity, undergoing anti-inflammatory therapies such as ultrasound or low-power laser treatment, and losing weight, to name some. The way that all these treatments fit together must be explained in the context of the pathology that is present, and the role of the orthosis should be emphasised. In a ‘prescription culture’, the orthosis can take the place of the pill, and other advice ignored in the hope that all that is really required is to wear something or slip something into a shoe. Patients have a right to know what the practitioner has in mind for their treatment, and they should have a clear indication of how long this might take, the extent of improvement in the condition and, in the private sector, the costs involved. Prescribed functional orthoses can cost as much as designer spectacles and the practitioner has a duty of care to maximise the chances of success.
If this is accepted as a reasonable principle of patient management, then it is incumbent upon the practitioner to be able to offer the best possible treatment advice. If the practitioner is unable to provide this the patient should be referred to a clinician with the necessary equipment and skills. Not every patient needs an orthosis, but where this is an integral part of the treatment, patient management and patient awareness of the treatment plan and any possible sequelae must be explained. This is particularly important with regard to the emergence of new paradigms of foot function influencing orthosis design, which has resulted in variations in practice. It is more vital than ever that the management plan and its rationale are explained fully to the patient in order to maximise the chance of success and minimise the risk of dissatisfaction, which can lead to claims of medical negligence.
Before embarking on the treatment plan, certain considerations are important. The physical characteristics of the patient must be assessed, including height, weight and mobility, and also the presence of physical disability that might preclude the use of certain types of orthoses. For example, if the patient is blind he or she may find it difficult to position the orthoses or move them between shoes. In such circumstances a ‘locator’ might be required, to enable the patient to differentiate left from right and to position the orthosis correctly in the shoe by touch. Should the patient have any physical disability that prevents him or her from reaching the feet, orthoses that require careful positioning would also be unsuitable. In such circumstances a full-length orthosis that shares the same dimensions of the shoe insole would be easier to fit.
A summary of the points to consider when prescribing orthoses was provided by Anthony (1991), and these key questions remain relevant and should be considered every time orthotic therapy is considered:
In addition to these questions, the effect that the materials may have on the patient’s foot warrants consideration, given the hostile in-shoe environment and the length of time for which shoes and orthoses will be worn. The potential for irritation and allergy, and the stability of the material in its working environment all influence material choice, as exemplified in the case of neuropathy. When all these factors have been considered, then orthotic therapy can be initiated, and this may involve a range of devices, from simple padding to full functional orthoses.
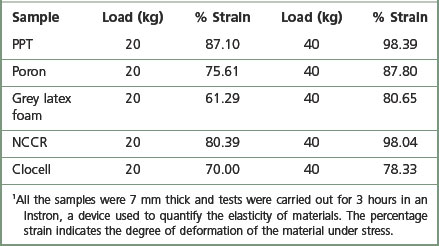
REPLACEABLE PADS
The simplest extensions of padding and strapping to more permanent orthoses are replaceable pads. These devices take many forms and are usually held in place with elasticised bands positioned around the toes and/or foot (Figs 17.1-17.3). Before embarking on the use of a replaceable pad, the practitioner will usually try to design the clinical padding and assess its potential effectiveness. The role of clinical padding in this form is often undervalued, and substantial biomechanical control can be achieved with the skilful use of clinical padding materials either attached to the foot or positioned in the shoe. Manufacture is straightforward, and devices may be made in a variety of materials, depending on the physical properties required. A device may be required simply to replace atrophied fatty padding. Such devices are protective in nature and a material is selected on the basis of its ability to resist compression over time. Newer viscoelastic foams are much more effective in resisting compressive stress than materials derived from rubber. Table 17.1 lists some materials and illustrates their compressibility and percentage relaxation under compressive stress.
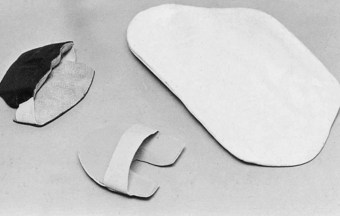
Figure 17.2 Selection of replaceable pads: orthodigital splint; dorsal pad for interphalangeal joint; Hexcelite valgus support covered in latex foam.
Forces acting on the foot can be managed in one of two ways: (a) by absorbing force in such a way that the material decelerates the rate at which the forces act on the foot – this is shock absorption; (b) by increasing the surface area to which the force is applied. It must be remembered that the orthosis should be placed in such a position that during foot-flat and heel-off the maximum area is in contact with the ground.
Technological advances in materials have provided a new range of viscoelastic products that provide effective cushioning or dampen ground reaction forces. These materials, such as Sorbothane and Viscolas or silicone polymer, allow podiatrists to provide the patient with high-quality shock absorption without recourse to cutting, shaping or covering replaceable orthoses. However, such viscoelastic materials can be heavier than traditional cushioning materials, and this could be important if supplying orthoses to sports people or those with established rheumatoid foot disease. Sheets of silicone rubber are now available in varying thicknesses and have proved most effective in the treatment of plantar keratomas or lesions over pressure areas on the toes.
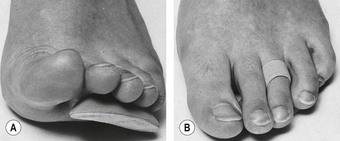
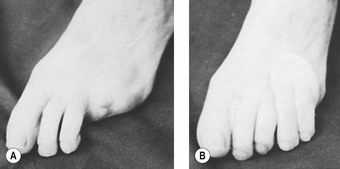
Replaceable digital orthoses may also be manufactured by the same process as used for plantar devices. However, practitioners may find that the effectiveness of digital orthoses is governed by their ability to remain in place, and secure anchoring is essential. Figure 17.1 illustrates a long prop; it is important that an assessment of the amount of movement in the interphalangeal and metatarsophalangeal joints is assessed before embarking on manufacture. Digital devices may conform to virtually any shape, provided the principle has been first assessed with conventional padding.
ELASTIC ANKLETS AND BRACELETS
An elastic anklet is useful as an alternative to figure-of-eight strapping when continuing support is required for an unstable rearfoot. Commercial devices are readily available and, while quality and price vary, there are some excellent products available. They may be used with a tarsal platform or tarsal cradle fitted into the shoe or onto an insole. A buttressed heel may also be indicated for greater ankle stability.
A metatarsal brace is an elastic bandage encircling the metatarsus, and it usually includes a plantar metatarsal pad. Commercial varieties are limited by the ability of standardised dimensions to match satisfactorily the anatomy of individual patients. However, such braces can be easily manufactured using elastic webbing or elastic net. Both materials are available in various widths, and it is advantageous to be able to design both brace and padding according to individual needs. The metatarsal brace may often be combined with a toe loop or with orthodigital splints where correction and/or protection of the digits is also desired (Fig. 17.3).
There is now available a plethora of elasticised supports specifically designed for use in sport. As people become more intent on improving their fitness and using sport as a means to better health, sportswear manufacturers have met the demand by producing supports for all joints that could possibly be stressed by sporting activity. These are usually available from pharmacists or sports shops. The most popular range of supports are those manufactured from neoprene, but care is required when fitting these devices.
INSOLES
Virtually any pathological condition affecting the plantar surface of the foot can be controlled by appropriate insoles, provided that sufficient depth is available in the footwear. It is essential that this requirement be considered whenever specially made footwear is ordered. With normal footwear, every effort must be made to save bulk by the choice of material, and by stopping the insole just behind or just in front of the metatarsal heads, depending on requirements. There are two basic types of insole:
Non-casted insoles
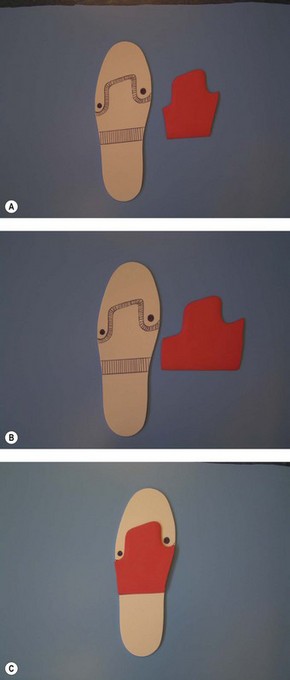
Non-casted insoles are manufactured in such a way that they form part of the shoe. The first prerequisite is the production of a template to the size and shape of the insole of the shoe. From this template the base material of the insole is then shaped accordingly and placed in the shoe. The anatomy to which the padding will conform must be transferred onto this base, and this can be done in various ways. Firstly, the anatomy can be palpated and coloured and the patient then allowed to walk in their shoes without socks for a few minutes so that marks are transferred to the base material. This provides a quasi-static impression, which may not be far enough forward. Therefore, if this method is used, the padding should be moved slightly further forward to allow for the greater elongation that occurs during more vigorous dynamic activities. A better technique involves taking a dynamic impression where a material such as leatherboard is used for the insole and the patient asked to walk for up to 2 weeks in them to transfer the pressure points to the insole. Whichever technique is used, template fit to the shoe is critical, because any movement will compromise the location of padding in relation to the foot and may compromise treatment success. From the wear marks provided on the template, appropriate padding can be designed that conforms exactly to the required anatomy. This is then adhered to the base, covered with a leather or synthetic covering and fitted to the shoe. Figure 17.4 shows the construction of a simple insole, without its top cover. It is also possible simply to remove the insole from the shoe, incorporate appropriate padding and replace the insole into the shoe. This technique helps ensure appropriate fit and padding placement.
Casted insoles
Insoles made to a cast may be accommodative orthoses, which are designed to support and protect feet that have deformities that cannot be corrected, or functional orthoses, which are designed to encourage improved mechanical function of the foot and lower limb.
Accommodative orthoses are normally prescribed for conditions where joint pathology renders correction impossible. A large number of acquired and congenital deformities fall into this category. Figure 17.5 shows an accommodative insole manufactured for a patient injured in a motorcycle accident. His knee is fused and he presents with an ankle equinus and shortening of one leg by 3.8 cm (1.5 inches). The object of the insole is to load the maximum amount of foot surface contact area by filling in the exaggerated arch with a cork/latex compound. Birko cork and ethyl vinyl acetate (EVA) foams are excellent materials for this purpose. They provide a flexible support and also incorporate forefoot padding to reduce pressure under the first and fifth metatarsal heads. In the case of a cork orthosis, a mix of cork, leather dust and fine wood flour are mixed with latex to produce a porridge, which is then spread onto the cast and, after curing, is ground to the required dimensions to fit the foot and the shoe. This is an older technique, and in contemporary practice EVA would be heated to its thermoforming temperature and then vacuum formed over the cast – a much less messy technique. In the case illustrated the orthosis was fitted into a running shoe because such shoes have the features characteristic of a good shoe. The midsole has an extra piece added to it to reduce the limb-length difference further, as only small deficits can be addressed inside the shoe due to space constraints.
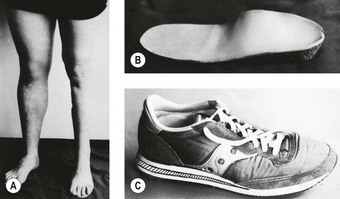
Figure 17.5 Casted insole. (A) A 1.5-inch (3.8 cm) shortening of the left leg after an accident. (B) Orthosis in cork/latex compound gives 1-inch (2.5 cm) heel raise. (C) Orthosis is worn in running shoe fitted with additional raise to the midsole (hatched).
EVA seems to be the material of choice for most accommodative orthoses, either on its own or laminated with other materials, as it is cheap, easy to work, has a good thermoforming temperature and is available in a range of densities and thicknesses. This offers the practitioner the ability to provide light, durable, low-cost devices. Such devices are particularly useful for treating the established rheumatoid or diabetic foot, or for sporting situations where full-length devices are required, such as in skiing.
FUNCTIONAL ORTHOSES
Functional orthoses are very popular, and are in routine use in the management of a whole host of disorders of the foot, ankle, lower limbs and even more proximally. Historically, there has been an emphasis on ‘motion control’, this concept originating from the perception that excessive motion, typically pronation, should be controlled aggressively to address symptoms fully. This approach has its origins in the Root model of clinical biomechanics (Root et al 1971, 1977), which promoted the control of abnormal motion as the means by which to reduce symptomatology.
The Root model has dominated clinical practice for a number of years, and has influenced research efforts that have attempted to identify the influence of orthoses on, for example, variables such as maximum calcaneal eversion and eversion velocity (Novick & Kelley 1990), and patellar glide position (Klingman et al 1997). Novick and Kelley (1990) identified significant changes in these variables, while Klingman et al (1997) found that patellar position was influenced by rearfoot posting, and this was assumed to represent the mechanism by which orthoses exerted their function. However, the importance of motion control has been challenged, and a body of research with conflicting findings has built up. For example, Zammit and Payne (2007) investigated the relationship between the degree of frontal plane rearfoot control and changes in symptoms. Despite finding a significant relationship, the actual change in the amount of motion taking place was small and suboptimal, leading to the conclusion that changes in rearfoot control are insufficient to explain the extent of symptom reduction observed. They suggested that orthoses may exert their influence via another mechanism. This conclusion is supported by other research findings. For example, Johansen et al (1994) found that an unposted orthotic shell reduced the extent of pronation by just as much as orthoses posted at rearfoot, forefoot or both. Such contradictions led Heiderscheit et al (2001) to claim that, while orthoses are an accepted and acknowledged part of the treatment of a variety of disorders, the bigger question relates to how they function.
This issue of how orthoses function was considered by Lee (2001), who discussed at length the different paradigms of foot function that currently exist. In this context a paradigm is a model, or clinical system of approach, which explains, amongst other things, mechanical foot function, how it integrates with the lower-limb kinetic chain, the origins and consequences of abnormal function, and the means by which to correct this function. Popular paradigms worthy of discussion are the Root, sagittal plane, proprioceptive (preferred motion pathway) and tissue-stress paradigms. It should be noted that, consistent with the remit of this book, what follows is merely a brief introduction to what is a complex and extensive subject, and the interested reader should gather the references cited to begin to develop a wider appreciation of the issues involved. These references provide accounts of the individual paradigms; they do not necessarily represent the first published account of the technique.
The Root paradigm
The Root paradigm focuses on the importance of the subtalar joint functioning around the neutral subtalar joint position in promoting optimal function of the foot and lower-limb musculoskeletal chain. While acknowledging that abnormal function may arise from a variety of neuromusculoskeletal abnormalities such as motor neuropathy, gastrosoleus ankle equinus or tibia varum, the model has become closely associated with the influence of bony alignment on foot function. Frontal, transverse and sagittal plane anomalies at various segments (e.g. forefoot, rearfoot, ankle, lower leg and knee) that were thought to influence foot function were described. A biomechanical examination technique was developed to assess each segment so that abnormality could be identified and an orthosis designed, and this examination still heavily influences clinical practice. The focus of the orthoses manufactured according to this paradigm characteristically incorporates frontal plane posting to influence the rearfoot and midfoot.
Problems with the Root paradigm include the importance of neutral subtalar joint function and the validity and reliability of the measurements associated with the biomechanical assessment (Keenan 1997). While problems associated with goniometry are associated with every discipline that utilises such techniques of clinical assessment, the value of the subtalar joint neutral position is of greater interest. The Root model asserts that in normal subjects the subtalar joint functions around the subtalar joint neutral position, but this is not supported by a series of recent research studies that tracked rearfoot motion in normal, healthy subjects (Cornwall & McPoil 1999, McPoil & Cornwall 1994, Pierrynowski & Smith 1996). These studies have repeatedly identified that normal subtalar joint motion – as represented by frontal plane calcaneal function – involves eversion from an initial inverted position, and a failure to reinvert until after heel lift. It should now be accepted that promoting a less pronated, as opposed to neutral, functional position should be the goal the majority of the time. A notable exception is in the case of early rheumatoid arthritis, where Woodburn et al (2002) identified that aggressive orthoses may control the development of the valgus hindfoot, which is central to the profound problem of foot pathology in this disease. This concept may be transferable to other destructive arthropathies and tendinopathies.
The sagittal plane paradigm
The sagittal plane paradigm is based on rocker theory, proposed by Perry (1992), which asserts that forward progression is dependent on optimal sagittal plane function around three pivot points (rockers) in the foot (Fig. 17.6): the posterior aspect of the calcaneus, the ankle joint, and the metatarsophalangeal joints. The paradigm proposes that it is through the sagittal function about these three fulcrums that the centre of mass of the body is efficiently transported forward. Bojsen-Moller (1979) developed this model when he realised that the normal metatarsal parabola, formed because the normal second metatarsal is longer than the first, results in two forefoot axes that cannot be used simultaneously (Fig. 17.6). His experiments to determine the functional differences between these two forefoot, propulsive rockers suggested that when load is transmitted medially through the first and second metatarsophalangeal joints there are a number of benefits. These include a more efficient windlass mechanism due to the larger diameter of the first metatarsal head leading to more effective resupination and stabilisation of the calcaneocuboid joint. The model was developed further by Dananberg (1993a,b), who suggested that normal first metatarsophalangeal function was vital to normal hip extension, which preserves the normal energy exchange between the upper limbs and the lower limbs that occurs through reciprocating pelvic motion. Dananberg (1995) also designed an orthosis expressly aimed at encouraging normal first metatarsophalangeal joint function, on the basis that this motion helps to restore various ‘autosupport’ mechanisms that are vital to optimal gait function. These orthoses are useful where a normal range of first metatarsophalangeal joint motion is present during non-weight bearing, but not used dynamically, a situation referred to as functional hallux limitus. Where there is a structural hallux limitus such orthoses are of no benefit, but rocker-bottom shoes may instead be useful. It is interesting that footwear that encourages improved sagittal plane function is now available, in the form of Masai Barefoot Technology footwear and Nike Free Trainers. This may reflect wide acceptance of this model of foot function, and certainly helps its profile.
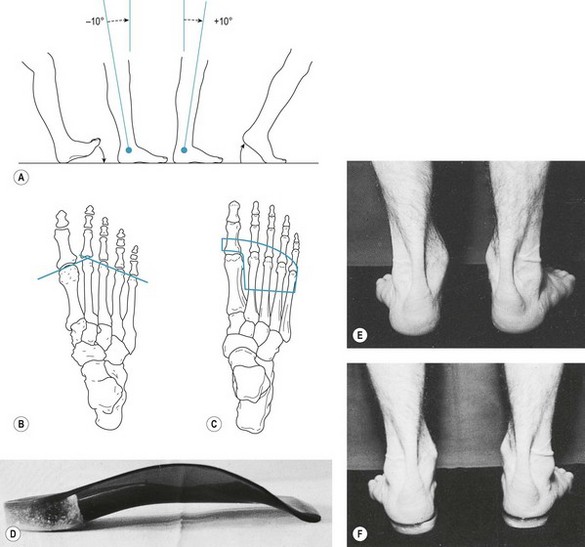
Figure 17.6 Sagittal plane and Root paradigm orthoses. Diagram a demonstrates the three Rockers which facilitate efficient forward motion. In diagram b the two possible propulsive axes that can be used in the forefoot are shown. The transverse axis – connecting MTPJt’s 1 & 2 – is associated with stable and efficient propulsion, and the blue pad outline shown in c illustrates a pad that will permit 1st ray plantarflexion, which is coupled with 1st MTPJt dorsiflexion, thereby encouraging transverse axis function. Orthoses made using the Sagittal plane paradigm are less aggressively posted that those focusing on frontal plane correction, and example of which is shown in d. The aim of such orthoses is shown in diagrams e and f, whereby the relaxed calcaneal stance position is moved towards neutral by the frontal plane posting applied.
The proprioceptive, preferred-motion-pathway paradigm
Perhaps the most revolutionary paradigm is the proprioceptive, preferred-motion-pathway paradigm proposed by Nigg (2001). In this model, impact forces are considered as input signals that ‘tune’ muscles to modify their activity in the subsequent step to minimise soft-tissue vibration and reduce joint/tendon loading. This paradigm directly challenges motion-control approaches, stating that although orthoses aim to realign the skeleton they produce only small changes, and the important factor is the influence that these orthoses, or shoes, have on muscle activity in terms of their ability to reduce energy cost. This energy-cost reduction is the common characteristic of a successful orthosis. The model can be summarised as follows (adapted from Nigg (2001)):
This paradigm is interesting because it potentially explains the apparent success of a range of different orthoses manufactured using different materials and employing different theoretical principles. As such, it deserves further investigation.
The tissue-stress paradigm
The tissue-stress paradigm was first proposed by McPoil and Hunt (1995) in response to deficiencies in the Root paradigm that they felt insurmountable. These deficits were described as: (a) the reliability of the measurement procedures, (b) the criteria for normal foot alignment, and (c) dynamic subtalar joint function. Taking an entirely pragmatic perspective, they suggested that the focus of treatment should not be dominated by a mechanical model, but rather should focus on the presenting pathology, based on the assumption that excess stress was being placed on a tissue and the optimal treatment strategy involves reducing this stress by a variety of means. Although the process set out contains several steps, it can be summarised briefly as follows:
The tissue-stress approach asserts that orthoses are part of a wider treatment approach, and an important point is that any orthoses used should provide only the control that is required to reduce stress on the affected tissue to a tolerable level so that healing can take place – as opposed to the pursuit of a theoretically ideal position.
While various other paradigms exist, those discussed above represent the main competing theories. Others, such as Kirby’s medial subtalar axis model (Kirby 2001), may have been referred to as a paradigm but essentially represents a technique by which frontal plane subtalar joint control can be enhanced. It therefore represents a development of the Root paradigm. There is an overlap between Kirby’s work and that of Close et al (1967), who presented a ‘classification of the foot based on the medial deviation of the subtalar axis’, which not only mirrors Kirby’s thoughts but also describes the normal foot as being ‘somewhat pronated’, pre-empting the findings of McPoil and Cornwall (1994, 1999) and Pierrynowski and Smith (1996), and further strengthening the argument that normal subtalar joint function does not hinge on the neutral position. What goes around comes around!
Paradigms in practice: reconciling the controversy of foot function paradigms
The existence of various paradigms fuels deep and prolonged debates amongst enthusiastic academics and clinicians, but may alienate many others. There is clearly a need to resolve these issues in a pragmatic manner that enhances clinical practice. What follows is a simple clinical guide that may help the clinician reconcile some of the issues and encourage him or her to prescribe orthoses utilising a variety of concepts.
The process of identifying the plane of origin of abnormal foot function may be enhanced through the use of digital video gait analysis, which also permits identification of the subphase of stance in which the abnormal foot function develops.
Material choice and casting techniques
The manufacture of casted orthoses demands that an impression of the foot be taken from which the orthosis can be manufactured. This commonly involves heating a shell material and vacuum forming it to the cast. The choice of materials depends on various factors, including the patient’s age, weight and occupation, the chronicity of the condition and the preferred style of footwear. Furthermore, in the case of the sports person, the nature of the sport must be considered. For example, it might involve running, jumping, physical contact, or sharp or sudden changes of direction. Materials range from rigid to flexible. It is important not to think of a rigid orthosis as necessarily providing a higher level of control: even if subtalar neutral function is less important it may still be desirable to use a rigid material, but with less posting, as this will deliver this reduced control over a longer period of time. Conversely, a less rigid material with higher posting might be more comfortable for and better tolerated by specific patients.
Carbon fibre composites, graphite, polypropylenes and polyethylenes make up the most popular range of materials. Hexcelite, Aquaplast and the new range of fibreglass fracture splinting materials can produce orthoses that can last for many months. It is possible to manufacture temporary orthoses in situ on the foot using these splinting materials because the skin on the sole of the foot can tolerate their thermoforming temperature. Children normally tolerate semi-rigid or flexible orthoses better than those of the rigid variety.
Custom functional orthoses are manufactured to a model of the patient’s foot. The mould or cast is taken using one of a variety of techniques. The traditional technique involves lying the patient prone with their foot hanging off the end of the couch. A supine technique can also be used, but control of the foot, which is plantar flexing due to gravity, is more difficult. Plaster slabs (double thickness to increase strength) are draped over the calcaneus and extended down to the forefoot, and brought over the front of the foot and brought up and smoothed into the rearfoot splint. They are smoothed together and the foot then placed in the neutral subtalar joint position, where it is held until the plaster is dry, when it can be removed. In light of the questionable requirement for the subtalar joint to function in neutral, it may be that all that is required is a cast of the foot moderately less pronated than the functional position. An alternative technique is to use an oasis-foam impression box. The patient sits in a chair and the clinician places the foot in a neutral or less pronated position before applying controlled pressure to deform the foam so that it captures the contours of the patient’s foot. Like the plaster cast in the traditional technique, the impression is then filled with plaster of Paris, which when set provides a model of the foot over which the orthosis can be formed. When plaster models are used various plaster additions are incorporated, including: a lateral expansion to permit soft-tissue spread from the non-weight-bearing casting position, to enhance fit; a forefoot platform, which provides functional correction; and a medial addition, which blends the correction platform into the device. In relation to orthosis manufacture, useful laboratory guides providing detailed information on the manufacturing process have been provided by Anthony (1991) and Philps (1995).
Children present particular difficulties when casting, and for this reason it is best to use the prone position as the child is then less likely to interfere with the process – it can be difficult to stop a child from wriggling their toes when their foot is being tickled by plaster of Paris. While casting might be required in some cases, there is a rationale for generally using prefabricated devices. In addition to a reduced cost of treating a growing foot that may require serial casted devices at considerable cost, the need for casting is removed, as is the time requirement, and all these factors may increase concordance.
Many companies now produce plastics in pre-cut template sizes ready for heating, and these eliminate the need to buy large sheets that need to be reduced to the appropriate size using a band saw. Once heated and malleable, the plastic is trimmed to its rough shape and moulded by vacuum forming until the plastic cools and conforms exactly to the shape and contours of the plantar surface of the foot. Different plastics require heating at different temperatures and for different lengths of time (Table 17.2). Prior to manufacture, it should be decided whether intrinsic or extrinsic posting is required, based on the presenting condition, range of joint movement available and the degree of correction required. Posts are best described as platforms added to the plastic shell to provide correction. An intrinsic post is one that is applied to the cast in the form of a plaster addition, so that when the shell is pressed the posting is incorporated in the shell. An extrinsic post involves the addition of material to the bottom of the shell. Irrespective of which technique is used, the principle is the same. Rigid or high-density materials, such as dental acrylic, Tensol (liquid plastic), high-density polyethylene or Birkocork, may be used for posting. These posts or wedges hold the foot in the corrected position under load, restrain it from deforming as it would otherwise do, and help restore the normal time sequence of events occurring in the foot during the gait cycle. If some accommodation is required, posts will be made of a material that will ‘give’, such as high-density rubber.
Table 17.2 Working temperatures and thermoforming times for plastics in common use
| Temperature (°C) | Time (min)1 | |
|---|---|---|
| Hexcelite | 72 | 3 |
| Aquaplast | 100 | 3 |
| Pacton | 110 | 5 |
| Evazote | 130 | 6 |
| Plastazote | 140 | 8 |
| Polythene | 140 | 10 |
| Ortholene | 165 | 14 |
| Polypropylene | 165 | 15 |
| Rohadur | 170 | 18 |
| TL61 (carbon fibre composite) | 180 | 20 |
1 Times are based on the oven being at working temperature. All materials were 3 mm thick. Thicker materials take longer to become malleable.
A rearfoot post consists of a shaped wedge placed under the heel of the shell and tapered off on the lateral side to the required angle. This controls abnormal subtalar joint pronation. Forefoot posting may be either varus or valgus, as required, for either inversion or eversion control, respectively. A bar of material is placed 0.5–1 cm behind the metatarsal heads, tapering off to the medial or lateral sides to the required angle.
Rigid orthoses thus incorporate all the required correction. However, complete functional control may not always be tolerated at first, and the orthosis should be worn for short periods, increasing daily until they can be worn all day. As an alternative to rigid orthoses, semi-rigid devices can be used, and a whole range of patients may find these more tolerable.
Custom versus prefabricated orthoses
One of the more recent introductions to the range of available functional orthoses is a rapidly growing range of prefabricated devices. These are available in a range of generic sizes that may satisfy the requirements of patients who have a relatively normal foot size with no or only minor deformity. They come with a moderate amount of intrinsic control (e.g. 4–6° of rearfoot varus posting), although most ranges have a variety of additions (e.g. rearfoot and forefoot wedges, heel raises and metatarsal domes) available that the practitioner can apply to produce an orthosis that provides a degree of customised control. Long-established prefabricated orthoses are supplied by Vasyli (previously known as AOL – Australian Orthotic Laboratory) and Formthotic. Newer ranges include those available from Talar Made, SALTS Healthcare, Algeo’s First Phase Orthotics and the Salford Insole. Each manufacturer claims that their devices are superior in terms of effectiveness and cost. A majority of these devices can be heat moulded, and it is difficult to recommend one range in particular. Those interested in prefabricated orthoses should attend a podiatry conference, where they will be able to see the ranges and speak to representatives from the manufacturers. Sceptics should consider the evidence that is emerging concerning prefabricated orthoses. For example, in a well-designed, randomised controlled trial Landorf et al (2006) found that after 1 year there was no difference in the effectiveness of prefabricated versus custom orthoses prescribed for the treatment of plantar fasciitis, and at 3 months the prefabricated devices were more effective. This was attributed to less difficulty in accustoming to the prefabricated device. In a case series, Davis et al (2008) found that there was no difference in rearfoot motion control and comfort between custom and semi-custom devices. These findings were echoed in a recent study that evaluated the influence of custom and prefabricated orthoses on plantar pressure distribution and found small, non-significant differences in only a few variables (Redmond et al 2009). Prefabricated orthoses would seem to offer potential, and certainly should not be ignored.
CAD–CAM orthoses
The computer-aided design and manufacture (CAD-CAM) of functional orthoses is now recognised by many in the profession as the way forward, enabling practitioners to prescribe and supply their patients with devices that are produced to much finer tolerances than those produced using the traditional hand-crafted methods. The ability to accurately match the flexibility of the device to the patient’s body weight, numerically apply expansions and postings, and apply a range of special accommodations has enabled practitioners to supply their patients with devices that are fit for purpose and much more easily accommodated within reasonable footwear.
The shells are produced on a computer numerically controlled (CNC) milling machine from solid blocks of polypropylene, thus avoiding any changes to the molecular structure of the material, as there is no heat moulding involved in the process. This enables the manufacturer to produce devices that do not bottom-out and carry a lifetime guarantee against breakage in normal use. Hand finishing produces devices with excellent aesthetic qualities that do not require covers unless the prescription calls for additional extensions.
The data for the design are obtained from a neutral plaster cast of the patient’s foot. Good-quality casts of the type best suited to the laboratory’s specification are essential, as is the quality and clarity of the prescription, to enable the manufacturer to produce the correct devices. The continual development of the software has created many more prescription options. The prescription data are retained on the laboratory’s database, enabling repeat prescriptions to be produced at any time. Most laboratories are willing to provide expert help to practitioners with regard to their casting technique and prescription writing.
Practitioners who manufacture their own orthoses would find it difficult to produce a product that so closely matches the requirements of the prescription.
Prescription writing for CAD-CAM direct-milled orthoses
The development of CAD-CAM direct-milled orthoses that have top and bottom surfaces designed independently has brought with it the opportunity to produce much more accurate and effective devices, as many of the inaccuracies inherent in the orthoses produced using traditional hand-crafted techniques are eliminated. With this comes the opportunity for innovative prescription writing. It is worth noting that there are a number of different CAD-CAM systems in operation, each with its own programme, and each offering a wide variety of types and quality of orthoses, not all of which are direct milled. The following information is representative of the technique involved. The skill and experience of the practitioner in making the prescription will have a marked bearing on the type of prescription selected.
The outcomes sought by the practitioner can be divided into three categories: high, medium and low levels of control.
Examples of patients who will respond well to high-level control are:
Examples of patients requiring medium-level control are:
Examples of patients requiring low-level control are:
Other factors that have a bearing on the chosen prescription include:
Types of orthosis
Figure 17.7 shows various types of CAD-CAM orthoses.
Prescription variations
Flexibility
The thickness of the shell determines the degree of flexibility and is calculated to produce either, rigid, semi-flexible or flexible devices, based on the patient’s body weight. This produces the same degree of flexibility for each patient, irrespective of his or her weight. Occupations or sports that involve carrying or moving additional weight should be taken into account.
Heel-cup height
This ranges from 9 mm to 25 mm and is usually determined by the style of the device and the size of the foot. Children with hypermobile feet require extra-deep heel cups to establish greater control. Heel-cup heights are:
Width
The scanning equipment reads the width of the foot accurately, and therefore only in cases of exceptionally large feet, where shoe fitting is a problem should a narrow device be prescribed. For sports footwear such as soccer boots, a device that is narrower in the mid-section, narrow-mid, can be used. It is sometimes advisable to send the patient’s shoes to the laboratory to have the devices customised to fit them exactly.
Postings
All postings are applied using numerical science, with no human intervention in the fabrication stage; they are therefore guaranteed to be correct as prescribed.
Forefoot posting can be applied intrinsically or extrinsically, or as a combination of both.
An intrinsic post allows the forefoot to come down to the ground, as in ‘forefoot supinatus’ conditions.
An extrinsic post is applied to the bottom surface at the distal edge, to bring the ground up to the foot.
The degree of posting used is dictated by the angle between the heel and the forefoot, together with the level of control being sought.
A bar post is added to the bottom surface of the distal edge, creating greater lateral column stability. Bar posts can range in thickness from 2 mm to 5 mm.
Rearfoot posting is applied extrinsically as an integral part of the shell. The degree of posting is dictated by the angle between the bisection of the calcaneum and the midline of the leg, together with the level of control being sought.
All these measurements are taken with the midtarsal area held in its most stable position, normally referred to as ‘subtalar neutral’.
In Blake-style posting the distal edge of the forefoot is aligned parallel to the bottom surface of the rearfoot post. This produces a less forgiving device.
Accommodations
Problem solving
Devices do not fit shoes
This is usually found when patients do not wear the proper type or size of shoes. The devices are made to accurately match the size of the foot, and patients have a responsibility to ensure that their shoes accommodate the devices neatly. The importance of the shoe gripping securely in the midfoot area by means of a lace or strap must also be stressed.
Devices cut into the lateral side of the heel
This is due to the sagittal plane blockade not being completely overcome, therefore causing the foot to torque and rub against the heel cup. The prescription may need to be revised.
First metatarsal irritation
Orthoses can often cause irritation to the distal plantar first metatarsal. Where this occurs there can be a temptation to decrease or flatten the orthosis in this area. However, this can indicate that greater control is required, and by adding a small amount of rearfoot posting the first metatarsal declination angle can be influenced to reduce contact with the shell. Therefore, increasing, not decreasing, control is the solution.
Devices are too tight at the heel
Soft-tissue expansions are calculated as a percentage of the size of the heel. Patients that have very large fatty heel pads may produce a greater amount of expansion and encounter this type of problem. Such cases require a wider than normal heel cup.
EEC DIRECTIVE ON THE MANUFACTURE OF ORTHOSES
Directive 93/42 EEC, which came into effect on 14 June 1998, requires all manufacturers of medical devices, who place these on sale, to have registered with the competent authority (in the UK the Medical Devices Agency (MDA)).
The regulations require all such devices to display the CE mark of conformity, with the exception of custom-made devices, devices intended for clinical investigation and systems that comprise only CE-marked parts.
From a practitioner’s perspective, therefore, prefabricated devices will already comply with the directive. Those practitioners who supply their own manufactured orthoses should be registered with the competent authority and their devices should carry the CE mark of conformity. The guidance issued by the Society of Chiropodists and Podiatrists (UK) on who should or should not be registered is given in Box 17.1.
Box 17.1 Podiatric requirements for registering with the Medical Devices Agency (MDA)
Published by permission of the Society of Chiropodists and Podiatrists.
This legislation is complex and those requiring further information on interpretation of the legislation in the context of particular clinical/orthotics laboratory practices should seek expert help.
SILIPOS
This company produces a range of insoles manufactured in a cross-linked, three-dimensional polymer gel. Its structure reduces shearing stress, while the USP mineral grade oil softens and lubricates the skin. The material is also available in a range of digital pads, which protect a variety of pressure points, and in sheet form for use in the production of chairside appliances. It is important to stress that Silipos digital pads must be removed every evening and not left in position, as ulceration can occur if they are left on the foot continuously.
HEEL ORTHOSES
There are a number of orthoses that may be made specifically for conditions affecting the heel. A heel cup may be fabricated on a cast of the heel using the plastics already described or fibreglass. Such devices are well tolerated because they take up little room and can be worn in a wide variety of shoes. Wedges or posts may be incorporated in such devices, either at the time of manufacture or at a later stage. The devices are corrective in nature. However, palliative heel orthoses may be required for lesions on the plantar aspect of the heel, such as calcaneal bursitis, and for the area around the insertion of the Achilles tendon where the bursae are often subject to irritation from footwear. Skaters are particularly vulnerable to retrocalcaneal bursitis because of the rigidity of the counter surrounding the heel of skating boots. These heel orthoses can be manufactured on casts or made directly onto the heel using silicone.
Painful intractable hyperkeratotic lesions frequently occur on the area of the heel following trauma. The formation of scar tissue in such cases leaves the practitioner no other course than to rely on palliative orthoses. Most often, these devices are best fabricated in latex for wear on the foot. However, simple heel pads can also be made to fit into the shoe and can be removed for use in other shoes as required.
LATEX TECHNIQUE
Deformities of the toes, such as hallux abducto valgus and hammer toes, are often chronic and require protection more or less permanently. In such cases, devices made in latex are often the most effective type of orthosis. Such techniques are now rarely used, but represent a rewarding technique for the patient and podiatrist alike. Irrespective of the area involved, the principle of manufacture is the same. For the purposes of illustration, the fabrication of a hallux abducto valgus shield is described, but the technique is suitable for digital orthoses as well.
The most important feature is the accuracy of the negative cast. This may be taken in a variety of materials but the most effective are the elastic impression compounds. Dental impression materials are ideal for this purpose, and the most cost-effective of these is dental alginate.
The negative is then filled with plaster, and when this has set the alginate is stripped, bit by bit, to ensure that the positive remains intact. Any blemishes on the positive are removed with fine sandpaper, and, if necessary, porosities may be filled in with a thin mixture of plaster. The positive is then allowed to dry. Care must be taken not to overheat the cast as this might reverse the chemical process, causing the cast to become crumbly.
The positive is then dipped in latex, each layer being allowed to dry, until several layers have been built up on the cast. At this stage, the correct type of pad is applied according to the therapeutic function required. If an open-cell foam is used, the pad is first covered with adhesive. This seals the pad and prevents latex from permeating into the foam, and it also traps air within the open-cell structure, thereby improving the physical properties of the material. The cast is then dipped twice more to complete the process before being removed from the cast and trimmed. In some cases, it is preferable to cover the cast in a layer of soft leather such as chamois to provide a soft lining for the appliance. If this method is employed, the edges of the leather must be sealed and the appropriate adhesive used, otherwise degradation of the leather may result, due to interaction with the solvents used to stabilise the adhesives.
It is sometimes necessary or convenient to speed up the process for latex orthoses. This may be done either by heating the cast before dipping or by using a hot-air blower such as a hair dryer to dry each dip. In this way it is possible to manufacture a latex orthosis from start to finish in 15 minutes. A variety of latex digital shields are shown in Figure 17.8.
DIGITAL APPLIANCES FOR THE LESSER TOES
All necessary designs of digital appliances for the lesser toes can be produced by any of the methods previously outlined for hallux abducto valgus shields. The necessity for negative and positive casting when the latex technique is used, coupled with the smaller size of digital appliances, lends great advantages to the direct moulding techniques utilising silicone rubbers or thermoplastic materials. Silicone rubbers are well proven as the most suitable materials for digital orthoses. They can also be fabricated from orthotic plastic, but it is then usually necessary to line them with softer material for good tissue tolerance. Plastics used for this purpose are designed for finger-splinting, as they are soft and malleable. This combination increases the corrective effect of an appliance while maintaining patient tolerance.
The principle of reciprocal dorsoplantar padding is the most effective basis for digital appliances, and this has been previously described. When moulded in silicones or thermoplastics, orthodigital splints are infinitely adjustable to individual needs. They may be either full or partial. When full, they completely cover the dorsum of the proximal phalanges and the plantar surfaces of the intermediate and distal phalanges of the middle three toes. When partial, they are reduced in size to fit one or two toes only, or to form a long prop. Maximum effect is thus obtained with minimum bulk. Deformities and lesions of the fifth toe are particularly amenable to well-designed partial splints in silicones or thermoplastics.
SILICONES
The use of silicone elastomers in orthoses and prostheses is probably the most significant advance in this field for many years. In the short time since their introduction, rapid progress has resulted in new opportunities of treatment for digital deformity in both the old and the young. The silicones used in podiatry are derivatives of the elastomers used in dentistry, although in recent years materials designed specifically for podiatry have become available.
Silicones are generally presented as a putty to which a catalyst is added. After a period, the putty is transformed into a flexible solid. The material, while undergoing its change of state, maintains a putty-like consistency for a period of 2–8 minutes, depending on the putty/catalyst ratio and the room temperature. This space of time allows the practitioner to fabricate the device. After final setting, the material must be able to withstand repeated functional loading without dimensional change or fracture. There is a wide variety of possible formulae, but the practitioner must be aware of any alterations that he may make as they will directly affect the properties of tension and compression, and setting time, and therefore the subsequent usage of the material.
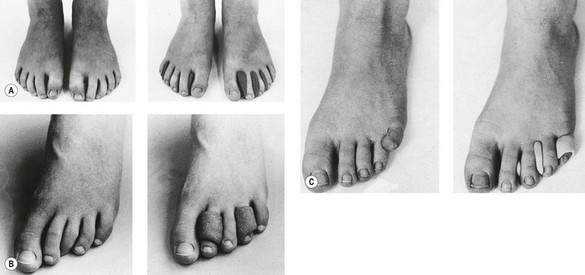
By far the most rewarding application of this material lies in the correction of congenital digital deformities in children. The same techniques may be used to correct toe deformities in older patients, if sufficient motion is present in the affected joints, and the same methods have been applied to the maintenance of correction following corrective digital surgery. Basically, the splint is fashioned around the toes and, as the silicone sets, the toes are held in their corrected position until the elastic properties of the material are strong enough to withstand the deforming forces. Figures 17.9 and 17.10 illustrate a variety of basic techniques for correcting the common congenital toe deformities, and Figure 17.11 shows silicone toe prostheses.
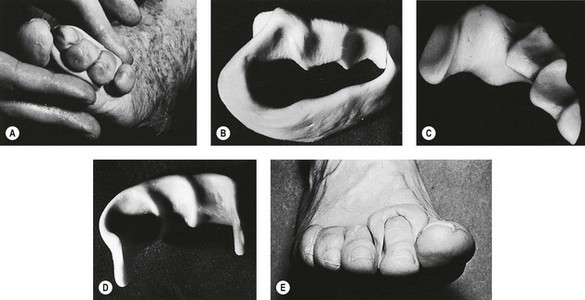
Figure 17.9 Silicone orthodigital splints. (A) Moulding splint at first stage of correction. (B) Full silicone splint. (C) Partial splint with interdigital wedge for first cleft. (D) Silicone long prop. (E) Single dorsoplantar splint for hammer toe.

Figure 17.11 Silicone prop and interdigital wedge to maintain position of hallux after Keller’s arthroplasty.
When using these materials in the field of postoperative maintenance, one must work closely with the surgeon who performed the operation. It is essential that the podiatrist has a good knowledge of the surgical techniques that have been employed so that any splint manufactured for the patient acts as an integral part of the patient’s therapy. Figure 17.11 shows a silicone orthosis that was fitted 2 weeks after the patient had undergone a Keller’s arthroplasty and capsulotomy of the second and third toes. Assessment of the inherent strength of the lesser digits is important if attempting to manufacture a splint to maintain the position of the hallux, in order to avoid moving the lesser digits laterally.
THERMOPLASTICS
Thermoplastic materials are usually products of additional polymerisation. They will soften on heating and harden once cooled without any chemical change taking place. Polymers that are thermoplastic can be moulded to a desired shape when heat and pressure are applied. The most common thermoplastic materials used in podiatry are derivatives of polyethylene, although polypropylene materials are also used.
This range of synthetic materials has four main areas of application: (1) firm splinting, (2) impression medium, (3) moulded lining, and (4) modelling and construction.
The firm splinting material is polyethylene sheet, which is not expanded in manufacture and consequently contains no pockets of gas. It is used for direct moulding to positive casts in the production of orthotic shells.
The impression material is the expanded polyethylene which, when inserted into the shoe as a template insole, provides an accurate dynamic impression of pressure areas. The template can then be built up with appropriate padding to produce a permanent insole.
As a lining material, the thermoplastic may be expanded polyethylene or expanded vinyl acetate. After the material is heated, moulding is carried out directly on the foot and additional padding and outer layers are added in sequence. This method can be used for hallux abducto valgus shields and similar appliances (e.g. heel cups for bedridden patients to prevent bed sores).
These materials may also be used for taking negative casts. However, if they are to be used for this purpose, care has to be taken to ensure there is no deformation of the cast after removal from the foot, and it is sometimes of help to mould a rigid material around the thermoplastic to retain its shape and dimension.
The softer of the two materials is the expanded vinyl acetate (Evazote), which looks identical to expanded polyethylene (Plastozote) but feels much smoother and softer and has a lower tensile strength. Quite complex curvatures can be achieved by moulding these materials, and one of the benefits is that a seamless lining is obtained.
Footwear that conforms accurately to the shape of the foot can be simply constructed by using the various densities and thicknesses of expanded polyethylene. One style is that of the clog with an enclosed front and no heel counter. The sole block is first cut out with a leather knife or on a band saw and the foot is placed on top. The upper is then shaped and covered in an appropriate material (e.g. Yampi). It is then moulded round the foot with the foot in place on the sole block, and the upper is adhered around the edge of the base. An outer sole can then be added and trimmed. The pair of clogs may weigh no more than 200 g, an important consideration in many cases.
An even lighter style is that of the sandal with a block sole and two or three straps to hold it onto the foot. More complicated styles can also be produced, which, when compared with traditional surgical footwear, are extremely attractive in terms of weight, fitting, style and price.
Almost any shape can be produced by cutting, heating, moulding and buffing thermoplastic materials (Fig. 17.12). To produce a moulded article, the material is heated in an oven at about 130°C until it is soft enough to mould. It cools in a minute or two and retains its moulded shape, at which stage adhesive can be applied. In some cases, the adhesive may be applied before heating, so that the moulding and fixing is done in one stage. Synthetic contact adhesives are suitable for fixing these thermoplastics. Good surface finishing is achieved easily, particularly when this is done on a grinding machine. When heating thermoplastics, it should be remembered that they are all inflammable, giving off strong toxic fumes, if allowed to get too hot. An oven with thermostatic controls is advised and a fire extinguisher should always be at hand.
Hot-water plastics (Polyform, Aquaplast Hexcelite, X-Lite Plus)
These orthotic splinting plastics are of particular use when an immediate appliance is required, and this technique is of great value in saving practitioner time. Its essential features are as follows: low temperature moulding; chairside technique; production time of a few minutes; rapid remoulding of part of or the whole device; no waste material, small offcuts are reusable; and readily adjustable thickness, as the material can be built up or thinned out as required.
Low-temperature moulding
In standard thickness (3 mm) the material can be softened in boiling water (100°C) for between 1 and 3 minutes to become completely workable and thinned out to an extremely thin layer. At 65–70°C it becomes workable in about 54–60 seconds, but the moulding characteristics are not as precise as with the 100°C softening temperature. The plastic will not soften below 60°C.
The material should be dried on a towel before being moulded; it will remain workable for about 3–5 minutes. Fingers should be moistened to maintain a good ‘slip’ feeling on surface moulding. When moulding, any excess material can be trimmed away easily with scissors. Most patients have good tolerance to the hot material directly on the skin, but an intermediate layer of expanded thermoplastic can be included if thought advisable. Cooling can be speeded up by immersion in cold water. If the material is thinned out when moulding, and cooled in ice-water, the hardened state can be expected in about 10–15 seconds.
Chairside technique
The whole device can be produced in as little as 2 minutes but should not normally take more than 10 minutes, allowing for modifications and adjustments.
Rapid remoulding
The advantage of this plastic over silicone rubber is that it can always be remoulded and reshaped by heating part or all of the device. As conditions respond to the orthosis, so the device can be adjusted to correspond to such correction.
No waste
Any small pieces can be reheated and moulded into one new piece. The new material can be flattened into a new sheet of any thickness on a smooth worktop. It will retain its cohesive properties after being heated and dried. Cold material is easily bonded to warm material by using a non-flammable Polyform adhesive. A finished device can be completely remade by placing it back into hot water. If the material has been thinned out while moulding, then in order to obtain the original or greater thickness, it will be necessary to fold over and double the material or to add other sheets.
Complex construction
Where more complex structures are required, and trial and error may be necessary to achieve optimum results, small balls of the plastic may be added, such as under the longitudinal axis of a three-quarter length valgus insole, to gain the desired degree of spring. A valgus insole is very quickly made and can be altered at any time with ease. Heel cups are also easily made and, by careful stretching of the material, can be produced quickly and accurately. Double curvatures are not difficult to make as long as the material is well heated. Combinations of Polyform with silicone rubbers or expanded thermoplastics give good results.
Where a soft appliance lacks strength, Polyform can be added to the original device as a reinforcement or cradle. An analogy is the gumshield worn by boxers, which consists of a strong plastic shell lined with soft material that has been moulded directly to the interior of the mouth. Expanded thermoplastics can be stuck to the Polyform sheet prior to heating and moulding to give an excellent fit when finished. Individual areas of the material can be heated using a hot-air gun, and additional moulding or alterations can be performed.
Hexcelite (X-Lite Plus)
This is a remouldable plastic impregnated over soft cotton. The material forms a mesh and, as such, combines features of excellent moulding with ventilation. It is self-bonding, light and has considerable strength. It is a relatively inexpensive material and can be heated in water at 72°C. It sets in 3 minutes and, when malleable, it will bond whether wet or dry. It has many uses and the podiatrist need only to use imagination to provide a wide array of semi-rigid orthoses. It can be used to manufacture night splints for hallux abducto valgus and it can also be used to splint lesser toes following surgery. By bonding several layers together, functional orthoses can be made in a matter of minutes. These insoles may be made directly on the patient’s foot or manufactured on a cast. Posts may be added in the same material. The Hexcelite should be moulded together by rolling with a rolling pin. Any synthetic contact adhesive is suitable for use with Hexcelite.
CONCLUSION
As can be seen from the number of techniques described, it is inappropriate to think of the term ‘orthosis’ as describing a narrow range of devices dominated by simple and functional insoles and silicone wedges. Podiatrists have a rich history of skilful manufacture of a range of devices and it is vital, for the management of idiosyncratic and challenging patients and rewarding practice, that practitioners embrace a range of techniques.
Alfredson H, Cook J. A treatment algorithm for managing Achilles tendinopathy: new treatment options. British Journal of Sports Medicine. 2007;41:211-216.
Anthony RJ. The manufacture and use of the functional foot orthosis. London: Karger; 1991.
Bojsen-Moller F. Calcaneocuboid joint and stability of the longitudinal arch of the foot at high and low gear push off. Journal of Anatomy. 1979;129:165-176.
Bojsen-Moller F, Lamoreux L. Significance of free-dorsiflexion of the toes in walking. Acta Orthopaedica Scandinavica. 1979;50(4):471-479.
Close JR, Inman VT, Poor PM, et al. The function of the subtalar joint. Clinical Orthopaedics and Related Research. 1967;50:159-179.
Cornwall MW, McPoil TG. Three-dimensional movement of the foot during the stance phase of walking. Journal of the American Podiatric Medicine Association. 1999;89(2):56-66.
Dananberg HJ. Lower extremity mechanics and their effect on lumbosacral function. Spine: State of the Art Reviews. 1995;9:389-405.
Dananberg HJ. Gait style as an etiology to chronic postural pain: Part 1. Functional hallux limitus. Journal of the American Podiatric Medicine Association. 1993;83:433-441.
Dananberg HJ. Gait style as an etiology to chronic postural pain. Part II. Postural compensatory process. Journal of the American Podiatric Medicine Association. 1993;83:615-624.
Davis IS, Zifchock RA, DeLeo AT. A comparison of rearfoot motion control and comfort between custom and semicustom foot orthotic devices. Journal of the American Podiatric Medicine Association. 2008;98(5):394-403.
Heiderscheit B, Hamill J, Tiberio D. A biomechanical perspective: do foot orthoses work? British Journal of Sports Medicine. 2001;35:4-5.
Johansen MA, Donatelli R, Wooden MJ, et al. Effects of three different posting methods on controlling abnormal subtalar pronation. Physical Therapy. 1994;74(2):149-161.
Keenan AM. A clinician’s guide to the practical implications of the recent controversy of foot function. Australasian Journal of Podiatric Medicine. 1997;31:87-93.
Kirby KA. The medial heel skive technique: improving pronation control in foot orthoses. Journal of the American Podiatric Medicine Association. 1992;82:177-188.
Kirby KA. Subtalar joint axis location and rotational equilibrium theory of foot function. Journal of the American Podiatric Medicine Association. 2001;91:465.
Klingman RE, Liaos SM, Hardin KM. The effect of subtalar joint posting on patellar glide in subjects with excessive rearfoot pronation. Journal of Orthopaedic & Sports Physical Therapy. 1997;25(3):185-191.
Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis. Archives of Internal Medicine. 2006;166:1305-1310.
Lee WE. Podiatric biomechanics: a historical appraisal and discussion of the Root model as a clinical system of approach in the present context of theoretical uncertainty. Clinics in Podiatric Medicine and Surgery. 2001;18(4):555-684.
McPoil TG, Cornwall MW. Relationship between neutral subtalar joint position and pattern of rearfoot motion during walking. Foot and Ankle International. 1994;15:141.
McPoil TG, Hunt GC. An evaluation and treatment paradigm for the future. In Hunt GC, McPoil TG, editors: Physical therapy of the foot and ankle, 2nd edn, Edinburgh: Churchill Livingstone, 1995.
Nigg BM. The role of impact forces and foot pronation: a new paradigm. Clinical Journal of Sport Medicine. 2001;11:2-9.
Novick A, Kelley DL. Position and movement changes of the foot with orthotic intervention during the loading response of gait. Journal of Orthopaedic & Sports Physical Therapy. 1990;11(7):301-312.
Perry J. Gait analysis: normal and pathological function. Thorofare, NJ: Slack; 1992.
Philps JW. The functional foot orthosis, 2nd edn. Edinburgh: Churchill Livingstone; 1995.
Pierrynowski MR, Smith SB. Rear foot inversion/eversion during gait relative to the subtalar joint neutral position. Foot and Ankle International. 1996;17:406.
Redmond AC, Landorf KB, Keenan AM. Contoured, prefabricated foot orthoses demonstrate comparable mechanical properties to contoured, customised foot orthoses: a plantar pressure study. Journal of Foot and Ankle Research. 2009;2:20.
Root ML, Orien WP, Weed JH, et al. Biomechanical examination of the foot, Vol. 1. Los Angeles, CA: Clinical Biomechanics Corp; 1971.
Root ML, Orien WP, Weed JH. Biomechanical examination of the foot, Vol. 2. Normal and abnormal function of the foot. Los Angeles, CA: Clinical Biomechanics Corp; 1977.
Rose GK. Orthotics: principles and practice. London: Heinemann Medical; 1986.
Sasaki T, Yasuda K. Clinical evaluation of the treatment of osteoarthritic knees using a newly designed wedge insole. Clinical Orthopaedics and Related Research. 1987;221:181-187.
Woodburn J, Helliwell PS, Barker S. A randomized controlled trial of foot orthoses in rheumatoid arthritis. J Rheumatol. 2002;29:1377-1383.
Zammit GV, Payne CB. Relationship between positive clinical outcomes of foot orthotic treatment and changes in rearfoot kinematics. Journal of the American Podiatric Medicine Association. 2007;97(3):207-212.