
INTRODUCTION TO THE HUMAN BODY
1. TERMINOLOGY
Anatomical Position
The study of anatomy requires a clinical vocabulary that defines position, movements, relationships, and planes of reference, as well as the systems of the human body. The study of anatomy can be by body region or by body organ systems. Generally, courses of anatomy in the United States approach anatomical study by regions, integrating all applicable body systems into the study of that region. Hence, this textbook is arranged regionally but, by way of introduction for someone studying anatomy for the first time, this initial chapter will briefly introduce you to the major body systems that you will encounter in your study of anatomy. You will find it extremely helpful to refer back to this introduction as you encounter various body systems in your study of regional anatomy.
By convention, anatomical descriptions of the human body are based on a person in the anatomical position (Fig. 1-1):
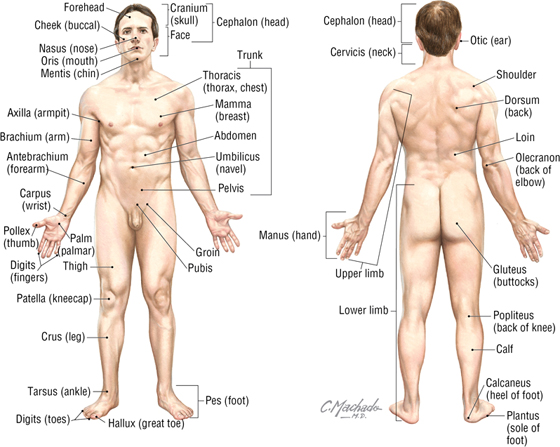
FIGURE 1-1 Anatomical Position and the Terminology Used to Describe Various Body Regions
- Standing erect and facing forward
- Arms hanging at the sides with palms facing forward
- Legs placed together with feet facing forward
Terms of Relationship and Body Planes
Anatomical descriptions often are referenced to one or more of three distinct body planes (Fig. 1-2 and Table 1-1):
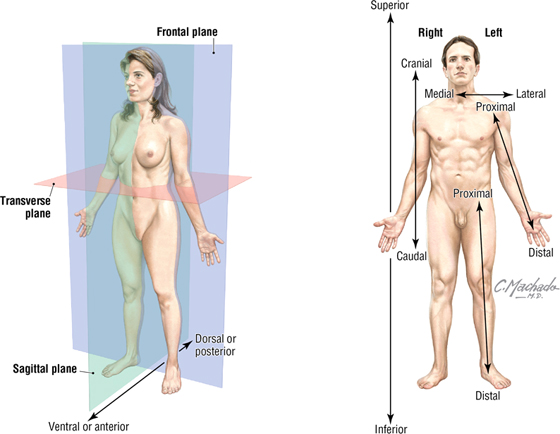
FIGURE 1-2 Body Planes and Terms of Relationship
|
TABLE 1-1 Terms of Relationship
|
 |
- Sagittal plane: vertical plane that divides the body into equal right and left halves (median or mid-sagittal plane) or a plane parallel to the median sagittal plane that divides the body into unequal right and left portions
- Frontal (coronal) plane: a vertical plane that divides the body into anterior and posterior portions (equal or unequal); this plane is at right angles to the median sagittal plane
- Transverse (axial) plane: horizontal plane that divides the body into superior and inferior portions (equal or unequal) and is at right angles to both the median sagittal and frontal planes (sometimes called cross sections)
Key terms of relationship used in anatomy and the clinic are summarized in Table 1-1. Sometimes these terms of relationship will be used in combination (e.g., superomedial, meaning closer to the head and nearer the median sagittal plane).
Movements
Body movements usually occur at the joints where two or more bones or cartilages articulate with one another. Muscles act on joints to accomplish these movements and may be described as follows: “The biceps muscle flexes the forearm at the elbow.” Figure 1-3 summarizes the terms of movement.
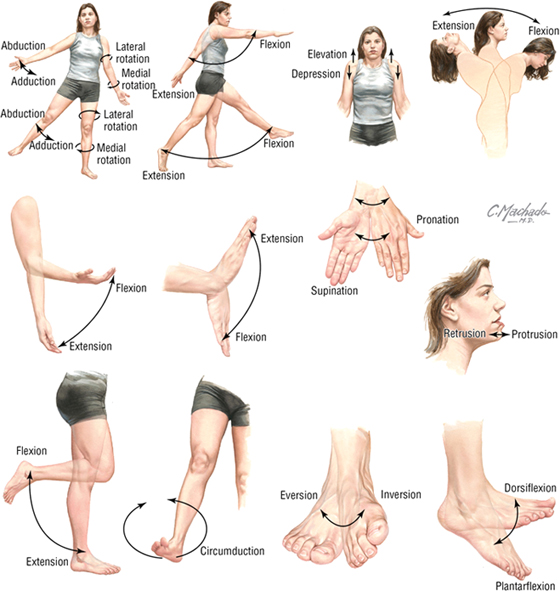
FIGURE 1-3 Terms of Movement
Anatomical Variability
The human body is remarkably complex and remarkably consistent anatomically, but normal variations do exist, often related to size, gender, age, number, shape, and attachment. Variations are particularly common in the following structures:
- Bones: fine features of bones (processes, spines, articular surfaces) may be variable depending on the forces working on that bone
- Muscles: vary with size and fine details of their attachments (it is better to learn their actions and general attachments rather than focus on detailed exceptions)
- Organs: the size and shape of some organs will vary depending on their normal physiology or pathophysiological changes that have occurred previously
- Arteries: while surprisingly consistent, some variation in the branching patterns is seen
- Veins: while consistent, variations in veins, especially in their size and number, are not uncommon and often can be traced to their complex embryologic development
2. SKIN
The skin is the largest organ in the body, accounting for about 15% to 20% of the total body mass, and functions in:
- Protection: against mechanical abrasion and in immune responses, as well as prevention of dehydration
- Temperature regulation: largely via vasodilation, vasoconstriction, fat storage, or activation of sweat glands
- Sensations: to touch by specialized mechanoreceptors such as pacinian and Meissner's corpuscles; to pain by nociceptors; and to temperature by thermoreceptors
- Endocrine regulation: by secretion of hormones, cytokines, and growth factors, and by synthesis and storage of vitamin D
- Exocrine secretions: by secretion of sweat and oily sebum from sebaceous glands
The skin consists of two layers (Fig. 1-4):
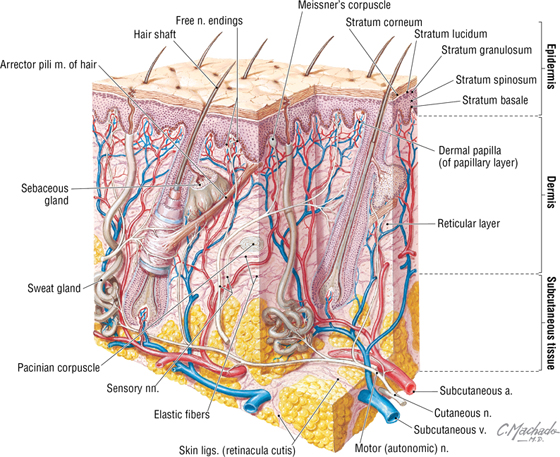
FIGURE 1-4 Layers of the Skin
- Epidermis: an outer protective layer consisting of a keratinized stratified squamous epithelium derived from the embryonic ectoderm
- Dermis: a dense connective tissue layer that gives skin most of its thickness and support, and is derived from the embryonic mesoderm
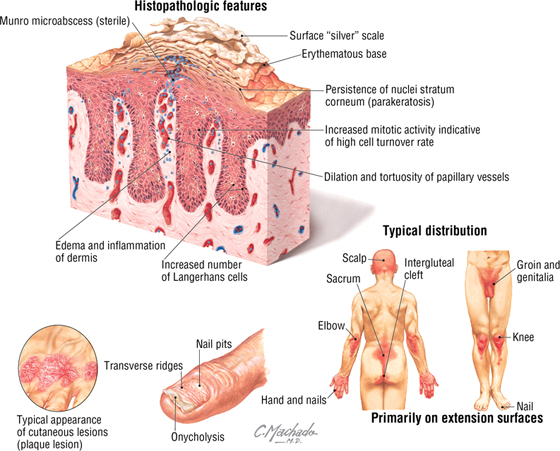
C L I N I C A L F O C U S
Psoriasis
Psoriasis is a chronic inflammatory skin disorder that affects women and men equally (approximately 1% to 3% of the population). It is characterized by defined red plaques that are capped with a surface scale of desquamated epidermis. Although the pathogenesis of the disease is unknown, a genetic predisposition seems to be involved.
C L I N I C A L F O C U S
Burns
Burns to the skin are classified into three degrees of severity based on the depth of the burn:
- First-degree: burn damage is limited to the superficial layers of the epidermis (termed a superficial burn clinically, it causes erythema)
- Second-degree: burn damage includes all of the epidermis and extends into the superficial dermis (termed a partial thickness burn, it causes blisters but spares the hair follicles and sweat glands)
- Third-degree: burn damage includes all of the epidermis and dermis, and may even involve the subcutaneous tissue and underlying deep fascia and muscle (termed a full-thickness burn, it causes charring)
Additional figures available online. See Table of Contents for Instructions for online access.

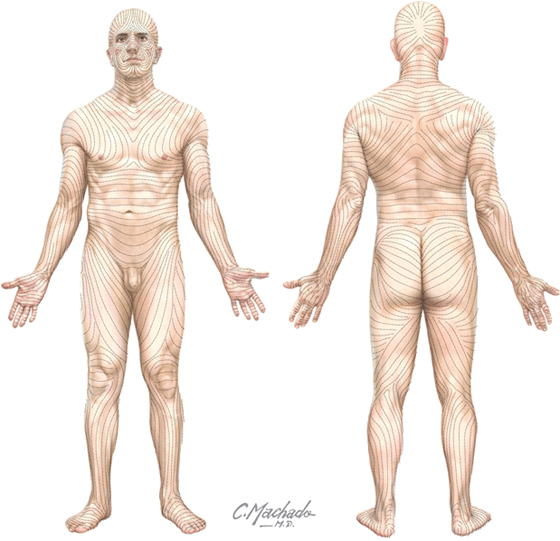
C L I N I C A L F O C U S
Langer's Lines
Collagen in the skin creates tension lines called Langer's lines. When possible, surgeons use these lines to make skin incisions. The resulting incision wounds have a tendency to gape less when the incision is parallel to Langer's lines, and this usually leaves a smaller scar after healing of the incision.
3. SKELETAL SYSTEM
Descriptive Regions
The human skeleton is divided into two descriptive regions (Fig. 1-5):
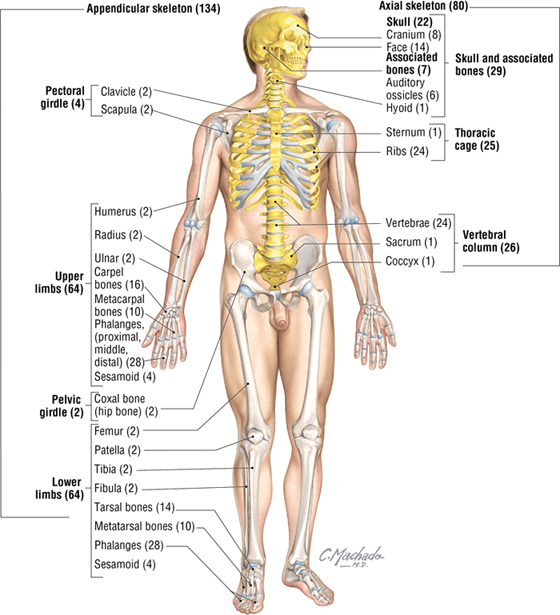
FIGURE 1-5 The Axial and Appendicular Skeleton
- Axial skeleton: bones of the skull, vertebral column (spine), ribs, and sternum, which form the “axis” or central line of the body (80 bones)
- Appendicular skeleton: bones of the limbs, including the pectoral and pelvic girdles, which attach the limbs to the body's axis (134 bones)
Shapes and Function of Bones
The skeleton is composed of a living, dynamic, rigid connective tissue that forms the bones and cartilages. Generally, humans have about 214 bones, although this number varies particularly in the number of small sesamoid bones that may be present. Cartilage is attached to some bones, especially where flexibility is important, or covers the surfaces of some bones at points of articulation. About 99% of the body's calcium is stored in bone, and many bones possess a central cavity that contains bone marrow—a collection of hemopoietic (blood-forming) cells. Most of the bones can be classified into one of five shapes (Fig. 1-6):
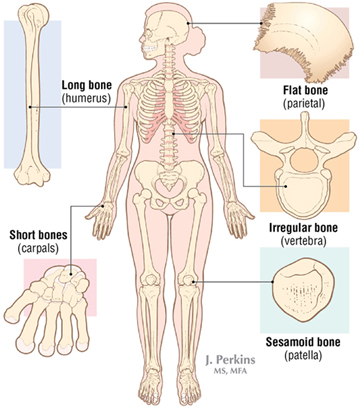
FIGURE 1-6 Bone Classification Based Upon Their Shape
- Long
- Short
- Flat
- Irregular
- Sesamoid
The functions of the skeletal system include:
- Support
- Protection of vital organs
- A mechanism, along with muscles, for movement
- Storage of calcium and other salts
- A source of blood cells
There are two types of bone:
- Compact: a relatively solid mass of bone, commonly seen as a superficial layer of bone, that provides strength
- Spongy (trabecular or cancellous): a less dense trabeculated network of bone spicules making up the substance of most bones and surrounding an inner marrow cavity
Long bones also are divided into the following descriptive regions (Fig. 1-7):
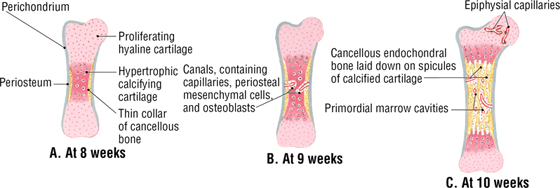
FIGURE 1-7 Growth and Ossification of Long Bones (Mid-Frontal Sections) (Contd.)
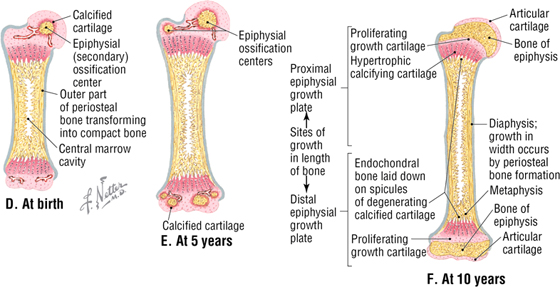
FIGURE 1-7 (Contd.) Growth and Ossification of Long Bones (Mid-Frontal Sections)
- Epiphysis: the ends of long bones, which develop from secondary ossification centers
- Epiphysial plate: site of growth in length; contains cartilage in actively growing bones
- Metaphysis: site where the bone's shaft joins the epiphysis and epiphysial plate
- Diaphysis: the shaft of a long bone, which represents the primary ossification center and the site where growth in width occurs
As a living, dynamic tissue, bone receives a rich blood supply from:
- Nutrient arteries: usually one or several larger arteries that pass through the diaphysis and supply the compact and spongy bone, as well as the bone marrow
- Metaphysial and epiphysial arteries: usually from articular branches supplying the joint
- Periosteal arteries: numerous small arteries from adjacent vessels that supply the compact bone
Markings on the Bones
Various surface features of bones (ridges, grooves, and bumps) result from the tension placed on them by the attachment of tendons, ligaments, and fascia, as well as by vessels or other structures that pass along the bone. Descriptively, these features include:
- Condyle: a rounded articular surface covered with articular (hyaline) cartilage
- Crest: a ridge (narrow or wide) of bone
- Epicondyle: a prominent ridge or eminence superior to a condyle
- Facet: a flat, smooth articular surface, usually covered with articular (hyaline) cartilage
- Fissure: a very narrow “slitlike” opening in a bone
- Foramen: a round or oval “hole” in the bone for passage of another structure (nerve or vessel)
- Fossa: a “cuplike” depression in the bone, usually for articulation with another bone
- Groove: a furrow in the bone
- Line: a fine linear ridge of bone, but less prominent than a crest
- Malleolus: a rounded eminence
- Meatus: a passageway or canal in a bone
- Process: a bony prominence that may be sharp or blunt
- Protuberance: a protruding eminence on an otherwise smooth surface
- Ramus: a thin part of a bone that joins a thicker process of the same bone
- Spine: a sharp process projecting from a bone
- Trochanter: a large, blunt process for muscle tendon or ligament attachment
- Tubercle: a small, elevated process
- Tuberosity: a large, rounded eminence that may be coarse or rough
Bone Development
Bones develop in one of two ways:
- Intramembranous formation: most flat bones develop in this way by direct calcium deposition into a mesenchymal (primitive mesoderm) precursor or model of the bone
- Endochondral formation: most long and irregular shaped bones develop by calcium deposition into a cartilaginous model of the bone that provides a scaffold for the future bone
The sequence of events in endochondral bone formation include (see Fig. 1-7):
- Formation of a thin collar of bone around a hyaline cartilage model (A)
- Cavitation of the primary ossification center and invasion of vessels, nerves, lymphatics, red marrow elements, and osteoblasts (B)
- Spongy (cancellous) endochondral bone is formed on calcified spicules (C)
- Diaphysis elongation, formation of the central marrow cavity, and appearance of the secondary ossification centers in the epiphyses (D)
- Long bone growth during childhood (E-F)
- Epiphysial fusion occurs from puberty into maturity (early to mid-twenties)
Types of Joints
Joints are the site of union or articulation of two or more bones or cartilages and are classified into one of three types (Fig. 1-8):
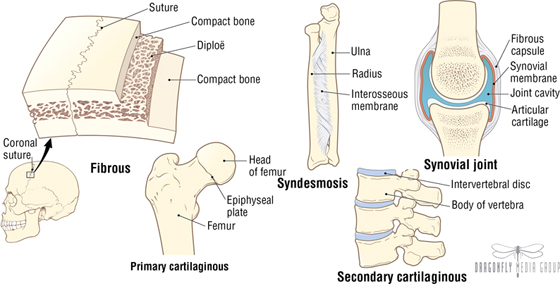
FIGURE 1-8 Types of Joints
- Fibrous (synarthroses): bones joined by fibrous connective tissue
- Cartilaginous (amphiarthroses): bones joined by cartilage, or cartilage and fibrous tissue
- Synovial (diarthroses): bones joined by a joint cavity filled with a small amount of synovial fluid and surrounded by a capsule; the bony articular surfaces are covered with hyaline cartilage
Fibrous joints include sutures (flat bones of the skull), syndesmoses (two bones connected by a fibrous membrane), and gomphoses (teeth fitting into fibrous tissue-lined sockets).
Cartilaginous joints include primary (synchondrosis) joints between surfaces lined by hyaline cartilage (epiphysial plate connecting the diaphysis with the epiphysis), and secondary (symphysis) joints between hyaline-lined articular surfaces and an intervening fibrocartilaginous disc. Primary joints allow for growth and some bending, while secondary joints allow for strength and some flexibility.
Synovial joints generally allow for considerable movement and are classified according to their shape and the type of movement that they permit (uni-, bi-, or multiaxial movement) (Fig. 1-9):
FIGURE 1-9 Types of Synovial Joints
- Hinge (ginglymus): uniaxial joints for flexion and extension
- Pivot (trachoid): uniaxial joints for rotation
- Saddle: biaxial joints for flexion, extension, abduction, adduction, and circumduction
- Condyloid (ellipsoid): biaxial joints for flexion, extension, abduction, adduction, and circumduction
- Plane (gliding): joints that only allow simple gliding movements
- Ball-and-socket (spheroid): multiaxial joints for flexion, extension, abduction, adduction, medial and lateral rotation, and circumduction
C L I N I C A L F O C U S
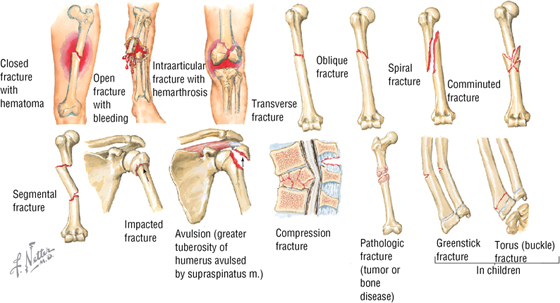
Fractures
Fractures are classified as either closed (the skin is intact) or open (the skin is perforated; often referred to as a compound fracture). Additionally, the fracture may be classified with respect to its anatomical appearance (e.g., transverse, spiral, and so on).
C L I N I C A L F O C U S
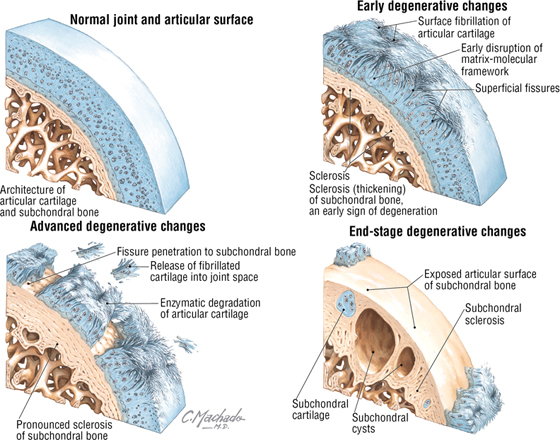
Degenerative Joint Disease
Degenerative joint disease is a catch-all term for osteoarthritis, degenerative arthritis, osteoarthrosis, or hypertrophic arthritis; it is characterized by progressive loss of articular cartilage and failure of repair. Osteoarthritis can affect any synovial joint but most often involves the foot, knee, hip, spine, and hand. As the articular cartilage is lost, the joint space (the space between the two articulating bones) becomes narrowed and the exposed bony surfaces rub against each other, causing significant pain.
4. MUSCULAR SYSTEM
Muscle cells (fibers) produce contractions (shorten in length) that result in movement, maintenance of posture, changes in shape, or the propulsion of fluids through hollow tissues or organs. There are three different types of muscle:
- Skeletal: striated muscle fibers that are attached to bone and are responsible for movements of the skeleton (sometimes simplistically referred to as voluntary muscle)
- Cardiac: striated muscle fibers that make up the walls of the heart and proximal portions of the great vessels
- Smooth: non-striated muscle fibers that line various organs, attach to hair follicles, and line the walls of most blood vessels (sometimes simplistically referred to as involuntary muscle)
Skeletal muscle is divided into fascicles (bundles), which are composed of muscle fibers (muscle cells) (Fig. 1-10). The muscle fiber cells contain longitudinally oriented myofibrils that run the full length of the cell. Each myofibril is composed of many myofilaments, which are composed of individual myosin (thick filaments) and actin (thin filaments) that slide over one another during muscle contraction.
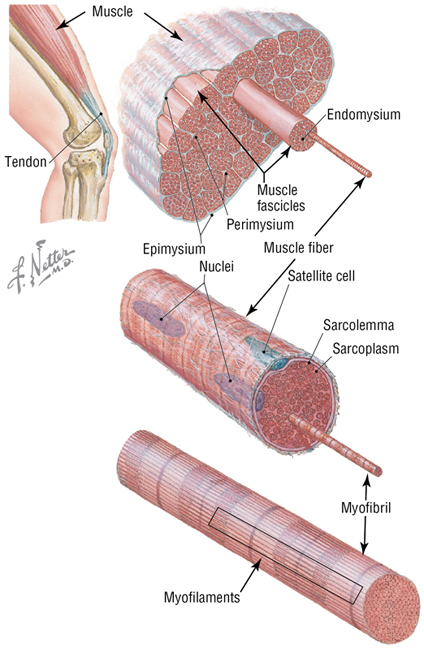
FIGURE 1-10 The Structure of Skeletal Muscle
Skeletal muscle moves bones at their joints and possesses an origin (the muscle's fixed or proximal attachment) and an insertion (the muscle's movable or distal attachment). At the gross level, anatomists classify muscle on the basis of its shape:
- Flat: has parallel fibers, usually in a broad flat sheet with a broad tendon of attachment called an aponeurosis
- Quadrate: has a four-sided appearance
- Circular: forms sphincters that close off tubes or openings
- Fusiform: has a wide center and tapered ends
- Pennate: has a feathered appearance (uni-, bi, or multipennate forms)
Muscle contraction shortens the muscle. Generally, skeletal muscle contracts in one of three ways:
- Reflexive: involuntary or automatic contraction; seen in the diaphragm during respiration or in the reflex contraction elicited by tapping a muscle's tendon with a reflex hammer
- Tonic: maintains “muscle tone,” a slight contraction that may not cause movement but allows the muscle to maintain firmness necessary for stability of a joint and important in maintaining posture
- Phasic: two types of contraction; isometric contraction, where no movement occurs but the muscle maintains tension to hold a position (stronger than tonic contraction), and isotonic contraction, where the muscle shortens to produce movement
Muscle contraction that produces movements can act in several ways, depending on the conditions:
- Agonist: the main muscle responsible for a specific movement (the prime mover)
- Antagonist: the muscle that opposes the action of the agonist; as an agonist muscle contracts, the antagonistic muscle relaxes
- Fixator: one or more muscles that steady the proximal part of a limb when a more distal part is being moved
- Synergist: complements (works synergistically) the contraction of the agonist, either by assisting with the movement generated by the agonist or by reducing unnecessary movements that would occur as the agonist contracts
5. CARDIOVASCULAR SYSTEM
The cardiovascular system consists of the heart, which pumps blood into the pulmonary circulation for gas exchange and into the systemic circulation to supply the body tissues, and the vessels that carry the blood, including the arteries, arterioles, capillaries, venules, and veins. The blood passing through the cardiovascular system consists of the following formed elements (Fig. 1-11):
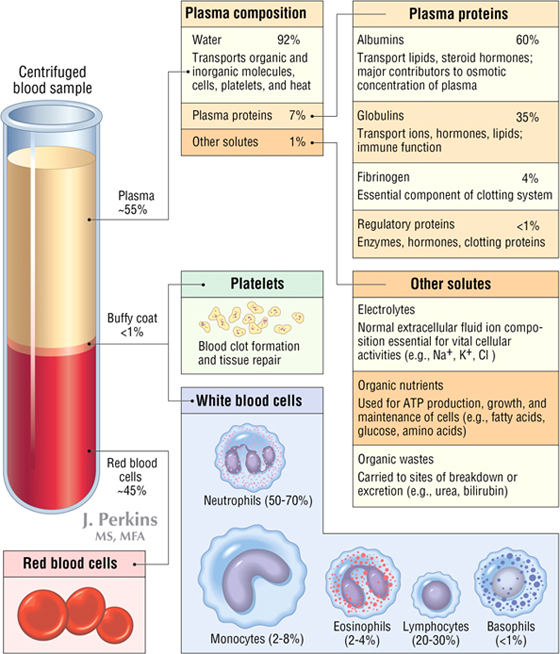
FIGURE 1-11 The Composition of Blood
- Platelets
- White blood cells (WBCs)
- Red blood cells (RBCs)
- Plasma
Blood is a fluid connective tissue that circulates through the arteries to reach the body's tissues and then returns to the heart through the veins. When blood is “spun down” in a centrifuge tube, the RBCs precipitate to the bottom of the tube, where they comprise about 45% of the blood volume. This is called the hematocrit and normally ranges from 40% to 50% in males and 35% to 45% in females. The next layer is a “buffy coat,” which comprises slightly less than 1% of the blood volume and includes WBCs (leukocytes) and platelets. The remaining 55% of the blood volume is the plasma (serum is plasma with the clotting factors removed and includes water, plasma proteins, and various solutes). The functions of blood include:
Blood Vessels
Blood circulates through the blood vessels (Fig. 1-12). Arteries carry blood away from the heart, and veins carry blood back to the heart. Arteries generally have more smooth muscle in their walls than veins and are responsible for most of the vascular resistance, especially the small muscular arteries and arterioles. Alternatively, at any point in time, most of the blood resides in the veins (about 64%) and is returned to the right side of the heart; thus veins are the capacitance vessels, capable of holding most of the blood, and are more variable and numerous than their corresponding arteries.
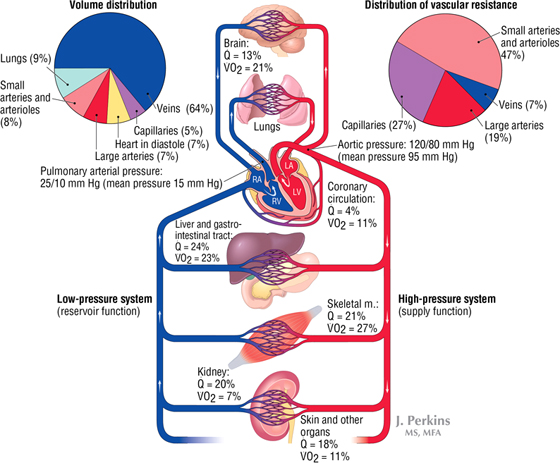
FIGURE 1-12 General Organization of the Cardiovascular System. The amount of blood flow per minute ( ), as a percent of the cardiac output, and the relative percent of oxygen used per minute (
), as a percent of the cardiac output, and the relative percent of oxygen used per minute ( O2) by the various organ systems is noted.
O2) by the various organ systems is noted.
 ), as a percent of the cardiac output, and the relative percent of oxygen used per minute (
), as a percent of the cardiac output, and the relative percent of oxygen used per minute ( O2) by the various organ systems is noted.
O2) by the various organ systems is noted.The major arteries are illustrated in Figure 1-13. At certain points along the pathway of the systemic arterial circulation, large and medium-sized arteries lie near the body's surface and can be used to take a pulse by compressing the artery against a hard underlying structure (usually a bone). The most distal pulse from the heart is usually taken over the dorsalis pedis artery on the dorsum of the foot.
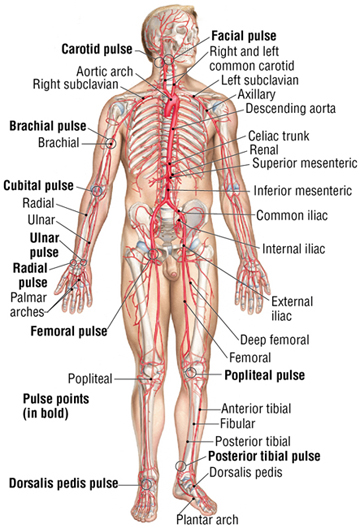
FIGURE 1-13 Major Arteries, Pulse Points, and Veins (Contd.)
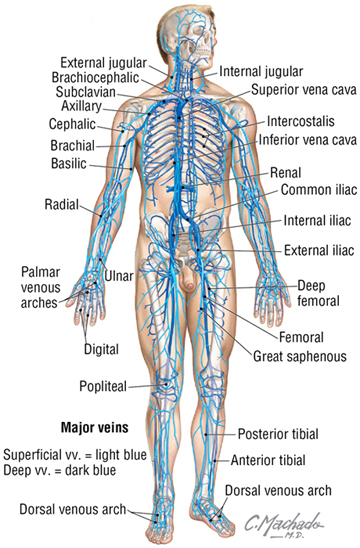
FIGURE 1-13 (Contd.) Major Arteries, Pulse Points, and Veins
The major veins are also illustrated in Figure 1-13. Veins are capacitance vessels because they are distensible and numerous and can serve as reservoirs for the blood. Because veins carry blood at low pressure and often against gravity, larger veins of the limbs and lower neck region have valves that aid in venous return to the heart. Both the presence of valves and the contractions of adjacent skeletal muscles help to “pump” the venous blood against gravity and toward the heart. In most of the body, the veins occur as a superficial set of veins in the subcutaneous tissue that connects with a deeper set of veins that parallel the arteries. Types of veins include:
- Venules: very small veins that collect blood from the capillary beds
- Veins: small, medium, and large veins that contain some smooth muscle in their walls, but not as much as their corresponding arteries
- Portal venous systems: veins that transport blood between two capillary beds (e.g., the hepatic portal system)
C L I N I C A L F O C U S
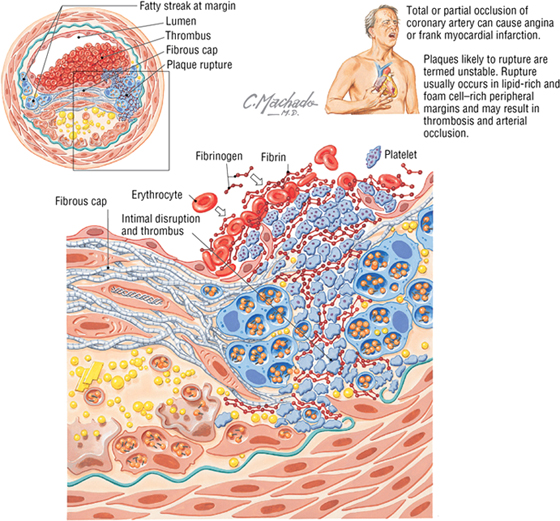
Atherogenesis
Thickening and narrowing of the arterial wall and eventual deposition of lipid into the wall can lead to one form of atherosclerosis. The narrowed artery may not be able to meet the metabolic needs of the adjacent tissues, with the danger that they may become ischemic. Multiple factors, including focal inflammation of the arterial wall, may result in this condition. When development of a plaque is such that it is likely to rupture and lead to thrombosis and arterial occlusion, the atherogenic process is termed unstable plaque formation.
Additional figures available online. See Table of Contents for Instructions for online access.

Heart
The heart is a hollow muscular (cardiac muscle) organ that is divided into four chambers (Fig. 1-14):
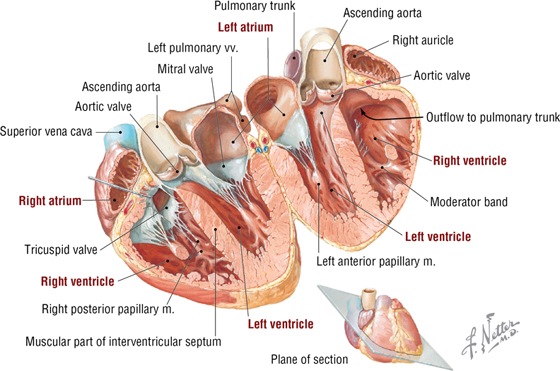
FIGURE 1-14 Chambers of the Heart
- Right atrium: receives the blood from the systemic circulation via the superior and inferior venae cavae
- Right ventricle: receives the blood from the right atrium and pumps it into the pulmonary circulation via the pulmonary trunk (artery)
- Left atrium: receives the blood from the lungs via pulmonary veins
- Left ventricle: receives the blood from the left atrium and pumps it into the systemic circulation via the aorta
The atria and ventricles are separated by atrioventricular valves (tricuspid on the right side and mitral on the left side) that prevent the blood from refluxing into the atria when the ventricles contract. Likewise, the two major outflow vessels, the pulmonary trunk from the right ventricle and the ascending aorta from the left ventricle, also possess valves called the pulmonic and aortic (semilunar) valves, respectively.
6. LYMPHATIC SYSTEM
General Organization
The lymphatic system is intimately associated with the cardiovascular system, both in the development of its lymphatic vessels and in its immune function. The lymphatic system functions to:
- Protect the body against infection by activating defense mechanisms that compose our immune system
- Collect tissue fluids, solutes, hormones, and plasma proteins and return them to the circulatory system (bloodstream)
- Absorb fat (chylomicrons) from the small intestine
Components of the lymphatic system include:
- Lymph: a watery fluid that resembles plasma but contains fewer proteins and may contain fat, together with cells (mainly lymphocytes and a few RBCs)
- Lymphocytes: the cellular components of lymph, which include T cells and B cells
- Lymph vessels: an extensive network of vessels and capillaries in the peripheral tissues that transport lymph and lymphocytes
- Lymphoid organs: collections of lymphoid tissue that include lymph nodes, aggregates of lymphoid tissue along the respiratory and GI passageways, tonsils, thymus, spleen, and bone marrow
Lymphatic Drainage
The body is about 60% fluid by weight, with 40% located in the intracellular fluid (ICF) compartment (inside the cells) and the remaining 20% in the extracellular fluid (ECF) compartment. The lymphatics are essential for returning ECF, solutes, and protein (lost via the capillaries into the ECF compartment) back to the bloodstream, thus helping to maintain a normal blood volume. On average, the lymphatics return about 3.5 to 4.0 liters of fluid per day back to the bloodstream. Additionally, the lymphatics also distribute various hormones, nutrients (fats from the bowel and proteins from the interstitium), and waste products from the ECF to the bloodstream.
Lymphatic vessels transport lymph from everywhere in the body (except the central nervous system) to major lymphatic channels. The majority of lymph ultimately collects in the thoracic lymphatic duct for delivery back to the venous system (joins the veins at the union of the left internal jugular and left subclavian veins) (Fig. 1-15). A much smaller right lymphatic duct drains the right upper quadrant of the body lymphatics to a similar site on the right side. Along the route of these lymphatic vessels, encapsulated lymph nodes are strategically placed to “filter” the lymph as it moves toward the venous system. Lymph nodes form an important site for phagocytosis of microorganisms and other particulate matter, and they initiate the body's immune responses.
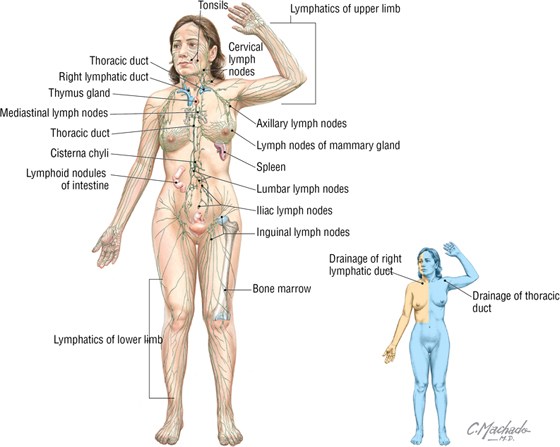
FIGURE 1-15 Overview of the Lymphatic System
Immune Response
When a foreign microorganism, virus-infected cell, or cancer cell is detected within the body, the lymphatic system mounts what is called an immune response. The detected pathogens are distinguished from the body's own normal cells, and then a response is initiated to neutralize the pathogen. The human body has evolved three major responses to protect against foreign invaders:
- Nonspecific barriers: A first line of defense is composed of physical barriers to invasion. These include the skin and mucous membranes that line the body's exterior (skin) or its respiratory, gastrointestinal, urinary, and reproductive systems (mucosa and its secretions, which may include enzymes, acidic secretions, flushing mechanisms such as tear secretion or the voiding of urine, sticky mucus to sequester pathogens, and physical coughing and sneezing to remove pathogens and irritants)
- Innate immunity: A second line of defense (if the nonspecific barrier is breached) is composed of a variety of cells and antimicrobial secretions and manifests with inflammation and fever
- Adaptive immunity: A third line of defense is characterized by specific pathogen recognition, immunologic memory, amplification of immune responses, and rapid response against pathogens that reinvade the body
7. RESPIRATORY SYSTEM
The respiratory system provides oxygen to the body for its metabolic needs and eliminates carbon dioxide. Structurally, the respiratory system includes the following (Fig. 1-16):
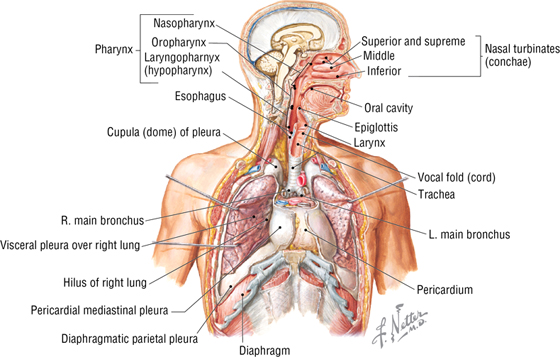
FIGURE 1-16 The Respiratory System
- Nose and paranasal sinuses
- Pharynx and its subdivisions (naso-, oro-, and laryngopharynx)
- Larynx
- Trachea
- Bronchi, bronchioles, alveolar ducts and sacs, and alveoli
- Lungs
Functionally, the respiratory system performs five basic functions:
- Filters and humidifies the air and moves it in and out of the lungs
- Provides a large surface area for gas exchange with the blood
- Helps to regulate the pH of body fluids
- Participates in vocalization
- Assists the olfactory system with the detection of smells
C L I N I C A L F O C U S
Asthma
Asthma can be intrinsic (no clearly defined environmental trigger) or extrinsic (has a defined trigger). Asthma usually results from a hypersensitivity reaction to an allergen (dust, pollen, mold), which leads to irritation of the respiratory passages and smooth muscle contraction (narrowing of the passages), swelling (edema) of the epithelium, and increased production of mucus. Presenting symptoms are often wheezing, shortness of breath, coughing, tachycardia, and feelings of chest tightness. Asthma is a pathologic inflammation of the airways and occurs in both children and adults.
Additional figures available online. See Table of Contents for Instructions for online access.

8. NERVOUS SYSTEM
General Organization
The nervous system integrates and regulates many body activities, sometimes at discrete locations (specific targets) and sometimes more globally. The nervous system usually acts quite rapidly and can also modulate effects of the endocrine and immune systems. The nervous system is separated into two structural divisions (Fig. 1-17):
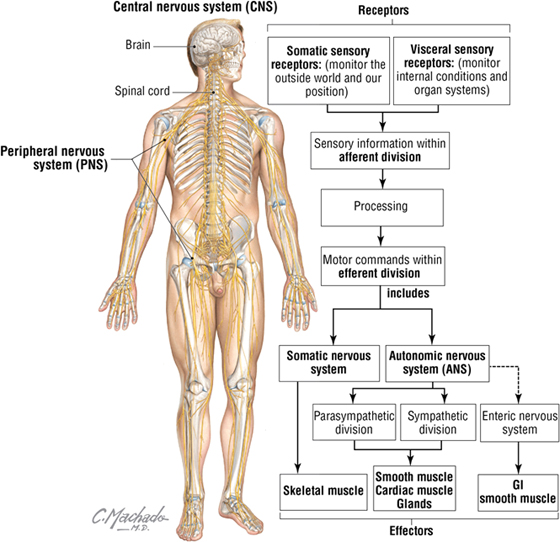
FIGURE 1-17 General Organization of the Nervous System
- Central nervous system (CNS): brain and spinal cord
- Peripheral nervous system (PNS): somatic, autonomic, and enteric nerves in the periphery
Neurons
Nerve cells are called neurons, and their structure reflects the functional characteristics of an individual neuron (Fig. 1-18). Information comes to the neuron largely via processes called axons, which terminate on the neuron at specialized junctions called synapses. Synapses can occur on neuronal processes called dendrites or on the neuronal cell body, called a soma or perikaryon.
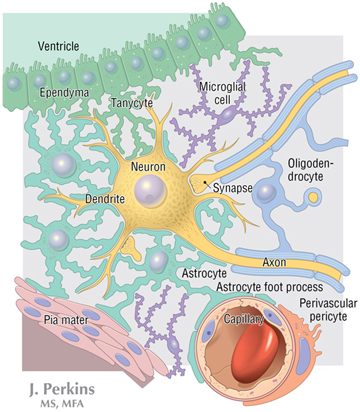
FIGURE 1-18 Cell Types Found in the CNS
Neurons convey efferent information via action potentials that course along a single axon arising from the soma that then synapses on a selective target, usually another neuron or target cell, for example, muscle cells. There are many different types of neurons. Some of the more common types include:
- Unipolar (often called pseudounipolar): one axon that divides into two long processes (sensory neurons found in the dorsal root ganglion of a spinal nerve)
- Bipolar: possesses one axon and one dendrite (rare but found in the retina and olfactory epithelium)
- Multipolar: possesses one axon and two or more dendrites (most common type)
Although the human nervous system contains billions of neurons, they can be classified largely into one of three functional types:
- Motor neurons: convey efferent impulses from the CNS or ganglia (collections of neurons outside the CNS) to target (effector) cells; somatic efferent axons target skeletal muscle and visceral efferent axons target smooth muscle, cardiac muscle, and glands
- Sensory neurons: convey afferent impulses from peripheral receptors to the CNS; somatic afferent axons convey pain, temperature, touch, pressure, and proprioception (nonconscious) sensations; visceral afferent axons convey pain and other sensations (e.g., nausea) from organs, glands, and blood vessels to the CNS
- Interneurons: convey impulses between sensory and motor neurons in the CNS, thus forming integrated networks between cells; interneurons probably comprise more than 99% of all neurons in the body
Neurons can vary considerably in size, ranging from several micrometers to over 100 micrometers in diameter. They may possess numerous branching dendrites, studded with dendritic spines that increase the receptive area of the neuron manyfold. The neuron's axon may be quite short or over 1 meter long. The axonal diameter may vary. Axons that are larger than 1 to 2 micrometers in diameter are insulated by myelin sheaths. In the CNS, axons are myelinated by a special glial cell called an oligodendrocyte, whereas axons in the peripheral nervous system (PNS) are surrounded by a glial cell called a Schwann cell. Schwann cells also myelinate many of the PNS axons they surround.
Glia
Glia are the cells that support neurons, both within the CNS (the neuroglia) and within the PNS. Glial cells far outnumber the neurons in the nervous system and contribute to most of the postnatal growth seen in the CNS. Functionally, glia:
- Provide structural isolation of neurons and their synapses
- Sequester ions in the extracellular compartment
- Provide trophic support to the neurons and their processes
- Support growth and secrete growth factors
- Support some of the signaling functions of neurons
- Myelinate axons
- Phagocytize debris and participate in inflammatory responses
- Participate in the formation of the blood-brain barrier
The different types of glial cells include the following (see Fig. 1-18):
- Astrocytes: the most numerous of the glial cells, they provide physical and metabolic support for CNS neurons and contribute to the formation of the blood-brain barrier
- Oligodendrocytes: smaller glial cells that are responsible for the formation and maintenance of myelin in the CNS
- Microglia: smallest and most rare of CNS glia (still more numerous than neurons in CNS), these phagocytic cells participate in inflammatory reactions
- Ependymal cells: line the ventricles of the brain and the central canal of the spinal cord, which contains cerebrospinal fluid (CSF)
- Schwann cells: glial cells of the PNS. They surround all axons (myelinating many of them) and provide trophic support, facilitate regrowth of PNS axons, and clean away cellular debris
Peripheral Nerves
The peripheral nerves observed grossly in the human body are composed of bundles of thousands of nerve fibers that are enclosed within a connective tissue covering and are supplied by small blood vessels. The nerve “fibers” consist of axons (efferent and afferent) that are individually separated from each other either by the cytoplasmic processes of Schwann cells or are myelinated by a multilayered wrapping of continuous Schwann cell membrane (the myelin sheath).
The peripheral nerve resembles an electrical cable of axons that is further supported by three connective tissue sleeves or coverings (Fig. 1-19):
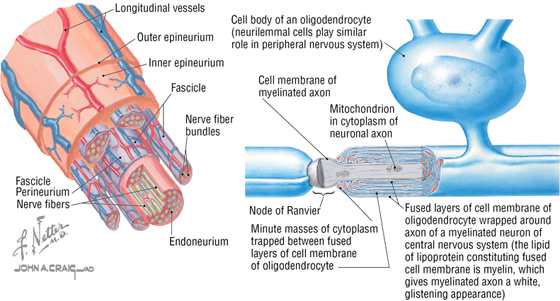
FIGURE 1-19 Features of a Typical Peripheral Nerve
- Endoneurium: a thin connective tissue sleeve that surrounds the axons and Schwann cells
- Perineurium: a dense layer of connective tissue that encircles a bundle (fascicle) of nerve fibers
- Epineurium: an outer thick connective tissue sheath that encircles bundles of fascicles; this is the “nerve” commonly seen grossly coursing in the human body
Peripheral nerves include the 12 pairs of cranial nerves arising from the brain and the 31 pairs of spinal nerves arising from the spinal cord.
Meninges
The brain and spinal cord are surrounded by three membranous connective tissue layers called the meninges. These three layers include the following (Fig. 1-20):
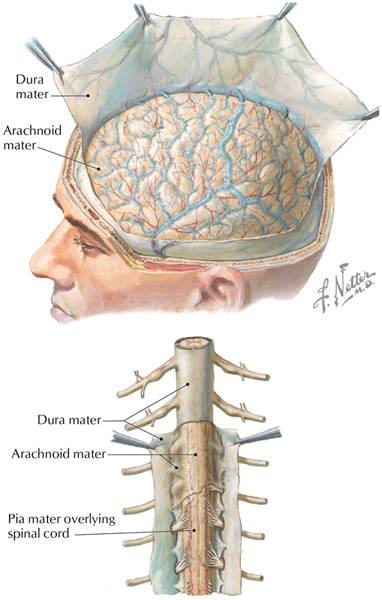
FIGURE 1-20 The CNS Meninges
- Dura mater: the thick outermost meningeal layer that is richly innervated by sensory nerve fibers
- Arachnoid mater: the fine weblike avascular membrane directly beneath the dural surface; the space between the arachnoid and the underlying pia is called the subarachnoid space and contains cerebrospinal fluid (CSF), which bathes and protects the CNS
- Pia mater: the delicate membrane of connective tissue that intimately envelops the brain and spinal cord
Cranial Nerves
Twelve pairs of cranial nerves arise from the brain, and they are identified both by their names and by Roman numerals I to XII (Fig. 1-21). The cranial nerves are somewhat unique and can contain multiple functional components:
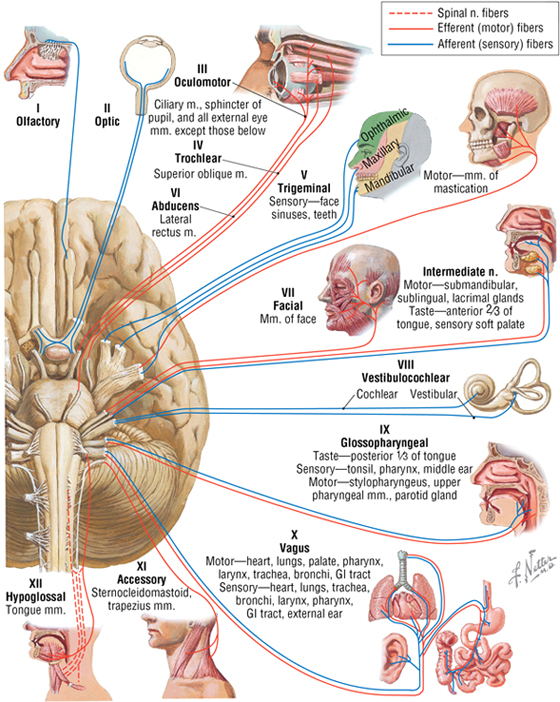
FIGURE 1-21 Overview of the Cranial Nerves
- General: same general functions as spinal nerves
- Special: functions found only in cranial nerves
- Afferent and efferent: sensory or motor functions, respectively
- Somatic and visceral: related to skin and skeletal muscle (somatic) or to smooth muscle, cardiac muscle, and/or glands (visceral)
Hence, each cranial nerve may possess multiple functional components, such as:
- General somatic afferents (GSA): contain nerve fibers that are sensory from the skin, such as those of a spinal nerve
- General visceral efferents (GVE): contain motor fibers to visceral structures (smooth muscle and/or glands), such as a parasympathetic fiber from the sacral spinal cord (S2 to S4 gives rise to parasympathetics)
- Special somatic afferents (SSA): contain special sensory fibers, such as those for vision and hearing
In general, CN I and II arise from the forebrain and are really tracts of the brain for the special senses of smell and sight. CN III, IV, and VI move the extraocular skeletal muscles of the eyeball. CN V has three divisions: V1 and V2 are sensory, and V3 is both motor to skeletal muscle and sensory. CN VII, IX, and X are both motor and sensory. CN VIII is the special sense of hearing and balance. CN XI and XII are motor to skeletal muscle. CN III, VII, IX, and X also contain parasympathetic fibers of origin (visceral), although many of the autonomic fibers will “jump” onto the branches of CN V to reach their targets. Table 1-2 summarizes the types of fibers in each cranial nerve.
|
TABLE 1-2 Cranial Nerve Fibers
|
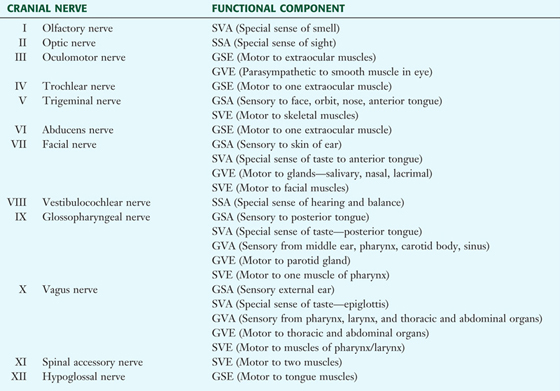 |
Spinal Nerves
The spinal cord gives rise to 31 pairs of spinal nerves (Figs. 1-22 and 1-23), which then form two major branches (rami):
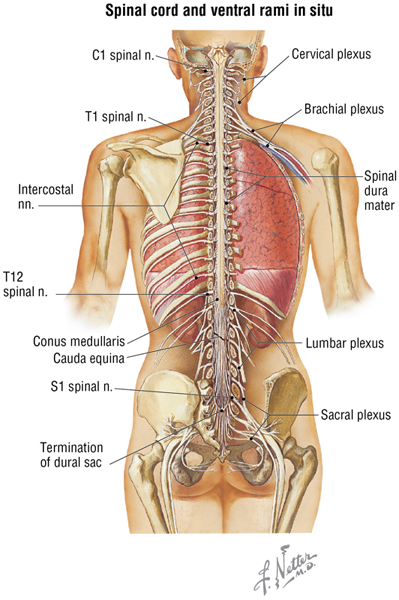
FIGURE 1-22 Overview of the Spinal Cord and Spinal Nerves
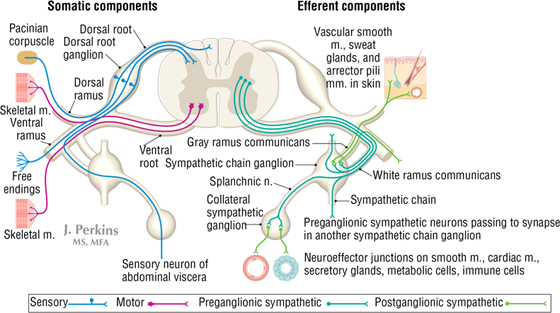
FIGURE 1-23 Elements of the PNS. For clarity, this schematic shows the arrangement of the efferent and afferent somatic nerve components of a typical spinal nerve on the left side and the efferent components of the ANS of a typical spinal nerve on the right side.
- Dorsal primary ramus: a small ramus that courses dorsally to the back conveys motor and sensory information to and from the skin and intrinsic back skeletal muscles (erector spinae and transversospinalis muscles)
- Ventral primary ramus: a much larger ramus that courses laterally and ventrally and innervates all the remaining skin and skeletal muscles of the neck, limbs, and trunk
Once nerve fibers (sensory or motor) are beyond, or peripheral to, the spinal cord proper, the fibers (axons) then reside in nerves of the peripheral nervous system (PNS). Components of the PNS include the following (see Fig. 1-23):
- Somatic nervous system: sensory and motor fibers to skin, skeletal muscle, and joints (illustrated on the left side of Figure 1-23)
- Autonomic nervous system (ANS): sensory and motor fibers to all smooth muscle (including viscera and vasculature), cardiac muscle (heart), and glands (illustrated on the right side of Figure 1-23)
- Enteric nervous system: plexuses and ganglia of the gastrointestinal tract (GI) that regulate bowel secretion, absorption, and motility (originally considered part of the ANS); linked to the ANS for optimal regulation
Features of the somatic nervous system include the following:
- It is a one-neuron motor system
- The motor (efferent) neuron is in the CNS, and an axon projects to a peripheral target (e.g., a skeletal muscle)
- The sensory (afferent) neuron (pseudounipolar) resides in a peripheral ganglion called the dorsal root ganglion (DRG) and conveys sensory information from the skin, muscle, or joint to the CNS (in this instance, the spinal cord)
The unilateral area of skin innervated by the somatic sensory fibers from a single spinal cord level is called a dermatome (see Chapter 2 for a complete description of a dermatome). Clinically, dermatome maps of the body can be helpful in localizing spinal cord or peripheral nerve lesions.
Features of the ANS division of the PNS include the following:
- It is a two-neuron motor system; the first neuron resides in the CNS and the second neuron in a peripheral autonomic ganglion
- The axon of the first neuron is termed preganglionic and the axon of the second neuron is termed postganglionic
- The ANS has two divisions: sympathetic and parasympathetic
- The sensory neuron (pseudounipolar) resides in a DRG (like the somatic system) and conveys sensory information from the viscera to the CNS
Sympathetic Division of the Autonomic Nervous System
The ANS is divided into the sympathetic and parasympathetic divisions. In contrast to the somatic division of the PNS, the ANS is a two-neuron system with a preganglionic neuron in the CNS that sends its axon into a peripheral nerve to synapse on a postganglionic neuron in a peripheral autonomic ganglion (Fig. 1-24). The postganglionic neuron then sends its axon to the target (smooth muscle, cardiac muscle, and glands). The ANS is a visceral system, since many of the body's organs are composed of smooth muscle walls or contain secretory glandular tissue.
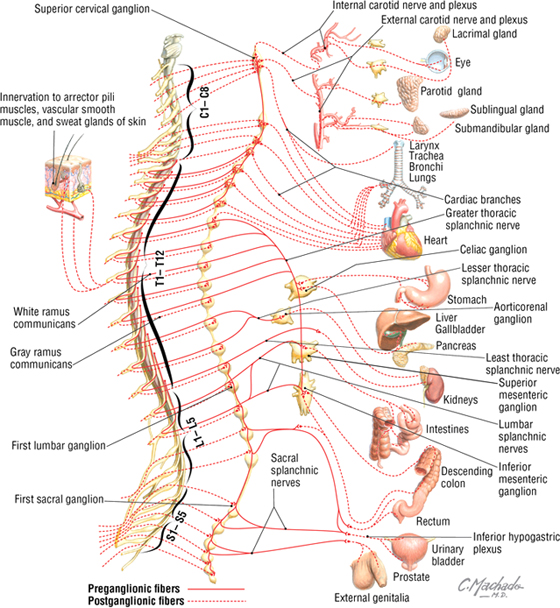
FIGURE 1-24 Overview of the Sympathetic Division of the ANS
The sympathetic division also is known as the thoracolumbar division because:
- Its preganglionic neurons are found only in the T1-L2 spinal cord levels
- Its preganglionic neurons lie within the intermediolateral gray matter of the spinal cord in the 14 segments defined above
Preganglionic axons exit the T1-L2 spinal cord in a ventral root, and then enter a spinal nerve via a white ramus communicans to enter the sympathetic chain. The sympathetic chain is a bilateral chain of ganglia just lateral to the vertebral bodies that runs from the base of the skull to the coccyx. Once in the sympathetic chain, the preganglionic axon may do one of three things:
- Synapse on a sympathetic chain postganglionic neuron at the T1-L2 level, or ascend or descend to synapse on a sympathetic chain neuron at any of the 31 spinal nerve levels
- Pass through the sympathetic chain, enter a splanchnic (visceral) nerve, and synapse in a collateral ganglion in the abdominopelvic cavity
- Pass through the sympathetic chain, enter a splanchnic nerve, pass through a collateral ganglion, and synapse on the cells of the adrenal medulla
Axons of the postganglionic sympathetic neurons may do one of four things:
- Those axons from sympathetic chain neurons reenter the spinal nerve via a gray ramus communicans and join any one of the 31 spinal nerves as they distribute widely throughout the body
- They may do the same as above but course along blood vessels in the head or join cardiopulmonary or hypogastric plexuses of nerves to distribute to head, thorax, and pelvic viscera
- They may arise from postganglionic neurons in collateral ganglia and course with blood vessels to abdominopelvic viscera
- Those postganglionic cells of the adrenal medulla are differentiated endocrine cells (paraneurons) that do not have axons but release hormones (epinephrine and norepinephrine) directly into the bloodstream
Preganglionic axons release acetylcholine (ACh) at their synapses, while norepinephrine (NE) is the transmitter released by postganglionic axons (except on sweat glands, where it is ACh). The cells of the adrenal medulla (modified postganglionic sympathetic neurons) release epinephrine and some NE into the blood, not as neurotransmitters but as hormones. The sympathetic system acts globally throughout the body to mobilize it in “fright-flight-fight” situations. The specific functions are summarized in Table 1-3.
|
TABLE 1-3 Effects of Sympathetic Stimulation on Various Structures
|
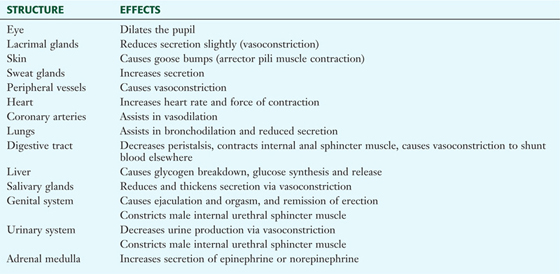 |
Parasympathetic Division of the Autonomic Nervous System
The parasympathetic division of the ANS also is a two-neuron system with its preganglionic neuron in the CNS and postganglionic neuron in a peripheral ganglion (Fig. 1-25). The parasympathetic division also is known as the craniosacral division because:
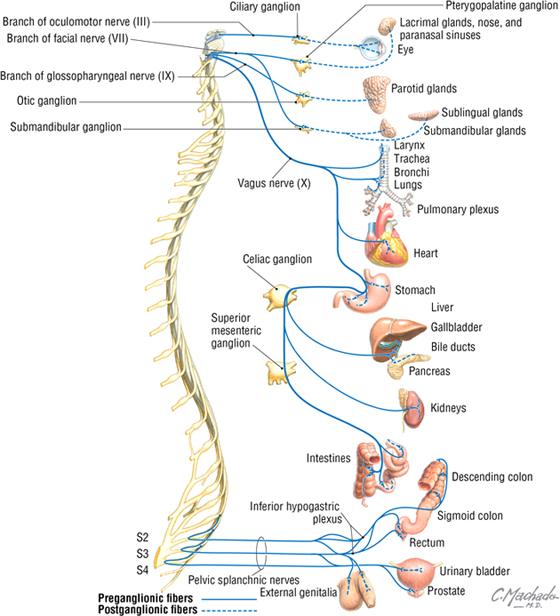
FIGURE 1-25 Overview of the Sympathetic Division of the ANS
- Its preganglionic neurons are found in cranial nerves III, VII, IX, and X, and in the sacral spinal cord at levels S2-S4
- Its preganglionic neurons reside in the four cranial nuclei associated with the four cranial nerves listed earlier or in the lateral gray matter of the sacral spinal cord at levels S2-S4
Preganglionic parasympathetic axons may do one of two things:
- Exit the brainstem in the cranial nerve (except CN X—see later) and pass to a peripheral ganglion in the head (ciliary, ptyergopalatine, submandibular, and otic ganglia) to synapse on the parasympathetic postganglionic neurons residing in these ganglion
- Exit the sacral spinal cord via a ventral root and then enter the pelvic splanchnic nerves to synapse on postganglionic neurons in terminal ganglia located in or near the viscera to be innervated
Axons of the postganglionic parasympathetic neurons may do one of two things:
- Pass from the parasympathetic ganglion in the head on existing nerves or blood vessels to innervate smooth muscle and glands of the head
- Pass from terminal ganglia in or near the viscera innervated and synapse on smooth muscle, cardiac muscle, or glands in the neck, thorax, and abdominopelvic cavity
CN X (vagus nerve) is unique. Its preganglionic axons exit the brainstem and synapse on terminal ganglia in or near the targets in the neck, thorax (heart, lungs, glands, smooth muscle), and abdominal cavity (proximal two-thirds of the GI tract and its accessory organs). Axons of the terminal ganglia neurons then synapse on their targets.
Parasympathetic axons do not pass into the limbs, as do sympathetic axons. Therefore, the vascular smooth muscle, arrector pili muscles of the skin (attached to hair follicles), and sweat glands are all innervated only by the sympathetic system. ACh is the neurotransmitter at all parasympathetic synapses.
The parasympathetic system is concerned with feeding and sexual arousal functions, and acts more slowly and focally than the sympathetic system. For example, CN X can slow the heart rate without affecting input to the stomach. In general, the sympathetic and parasympathetic systems maintain homeostasis, although as a protective measure, the body maintains a low level of “sympathetic tone” and can activate this division on a moment's notice. ANS function is regulated ultimately by the hypothalamus. The specific functions of the parasympathetic division of the ANS are summarized in Table 1-4.
|
TABLE 1-4 Effects of Parasympathetic Stimulation on Various Structures
|
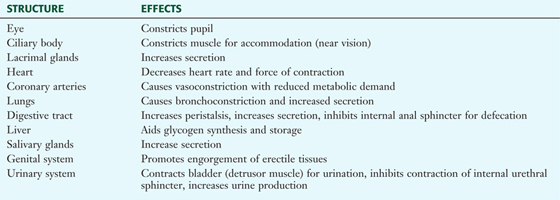 |
Enteric Nervous System
The enteric nervous system was formally considered the third division of the ANS. The word enteric refers to the bowel. This component of the PNS consists of ganglia and nerve plexuses in the walls of the GI tract. These ganglia and their neural networks include the following (Fig. 1-26):
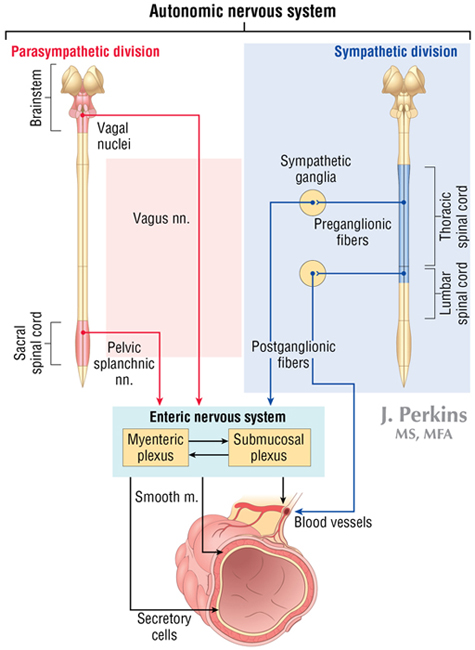
FIGURE 1-26 The Relationship of the Enteric Nervous System to the Sympathetic and Parasympathetic Divisions of the ANS
- Myenteric (Auerbach's) plexuses: ganglia and nerves located between the circular and longitudinal smooth muscle layers of the muscularis externa of the bowel wall
- Submucosal (Meissner's) plexuses: ganglia and nerves located in the submucosa of the bowel wall
The enteric nervous system has important links to both divisions of the ANS, which are critical for optimal regulation of bowel secretion, absorption, and motility. More than 20 different transmitter substances have been identified in the intrinsic neurons of the enteric nervous system, pointing to the fine degree of regulation that occurs at the level of the bowel wall. Optimal GI functioning requires coordinated interactions of the ANS, the enteric nervous system, and the endocrine system.
9. ENDOCRINE SYSTEM
The endocrine system, along with the nervous and immune systems, facilitates communication, integration, and regulation of many of the body's functions (Fig. 1-27). Specifically, the endocrine system interacts with target sites (cells and tissues), many a great distance away, by releasing hormones into the bloodstream. Generally speaking, endocrine glands and hormones share several additional features:
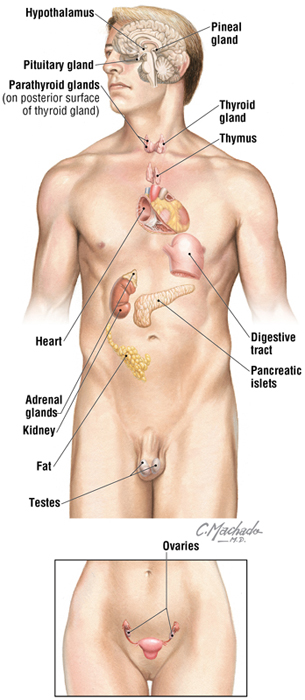
FIGURE 1-27 Major Endocrine Organs
Hormones can communicate via a variety of cell-to-cell interactions, including:
- Autocrine: on another cell as well as upon itself
- Paracrine: directly upon an adjacent or nearby cell
- Endocrine: at a great distance by the bloodstream
- Neurocrine: like a neurotransmitter except released into the bloodstream
Major hormones and the tissues responsible for their release are summarized in Table 1-5.
|
TABLE 1-5 Major Hormones
|
 |
Additionally, the placenta releases human chorionic gonadotropin (hCG), estrogens, progesterone, and human placental lactogen (hPL), whereas other cells release a variety of growth factors. Obviously, the endocrine system is widespread and critically important in regulating bodily functions.
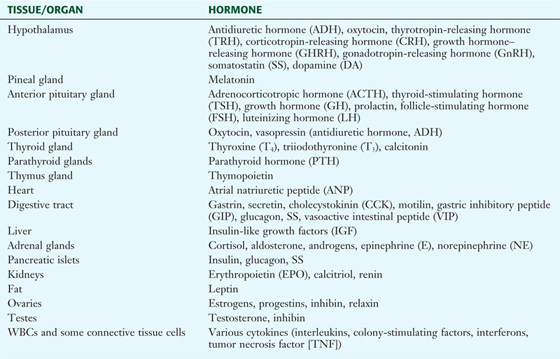
10. GASTROINTESTINAL SYSTEM
The GI system includes the epithelial-lined tube that begins with the oral cavity and extends to the anal canal and also includes GI-associated glands, including the following:
- Salivary glands: three major glands and hundreds of microscopic minor salivary glands scattered throughout the oral mucosa
- Liver: the largest solid gland in the body
- Gallbladder: its function is to store and concentrate bile needed for fat digestion
- Pancreas: an exocrine (digestive enzymes) and endocrine organ
The epithelial-lined tube that is the GI tract measures about 25 feet in length (from mouth to anal canal) and includes the following cavities and visceral structures (Fig. 1-28):
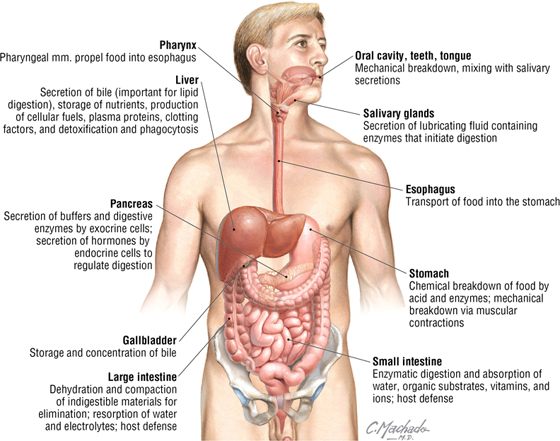
FIGURE 1-28 Overview of the Gastrointestinal System
- Oral cavity: tongue, teeth, and salivary glands
- Pharynx: throat, subdivided into the naso-, oro-, and laryngopharynx
- Esophagus
- Stomach
- Small intestine: subdivided into the duodenum, jejunum, and ileum
- Large intestine: subdivided into the cecum, ascending colon, transverse colon, descending colon, sigmoid colon, rectum, and anal canal
11. URINARY SYSTEM
The urinary system includes the following components (Fig. 1-29):
FIGURE 1-29 The Urinary System
- Kidneys: paired retroperitoneal organs that filter the plasma and produce urine; they are located high in the posterior abdominal wall just anterior to the muscles of the posterior wall
- Ureters: course retroperitoneally from the kidney to the pelvis and convey urine from the kidneys to the urinary bladder
- Urinary bladder: lies subperitoneally in the anterior pelvis, stores urine, and, when appropriate, discharges the urine via the urethra
- Urethra: courses from the urinary bladder to the exterior
- Filter plasma and begin the process of urine formation
- Reabsorb important electrolytes, organic molecules, vitamins, and water from the filtrate
- Excrete metabolic wastes, metabolites, and foreign chemicals (e.g., drugs)
- Regulate fluid volume, composition, and pH
- Secrete hormones that regulate blood pressure, erythropoiesis, and calcium metabolism
- Convey urine to the ureters, which then pass the urine to the bladder
The kidneys filter about 180 liters of fluid each day. Grossly, each kidney measures about 12 cm long × 6 cm wide × 3 cm thick and weighs about 150 grams, although variability is common. Approximately 20% of the blood pumped by the heart passes to the kidney each minute for plasma filtration, although most of the fluid and important plasma constituents are returned to the blood as the filtrate courses down the tubules of the kidney's nephrons (the kidney's filtration units).
Each ureter is about 24 to 34 cm long, lies in a retroperitoneal position, and contains a thick smooth-muscle wall. The urinary bladder serves as a reservoir for the urine and is a muscular “bag” that expels the urine when appropriate. The urethra in the female is short (3 to 5 cm) and in the male is long (about 20 cm). The male urethra runs through the prostate gland, the external urethral sphincter, and the corpus spongiosum of the penis.
12. REPRODUCTIVE SYSTEM
Female Reproductive System
The female reproductive system is composed of the following structures (Fig. 1-30):
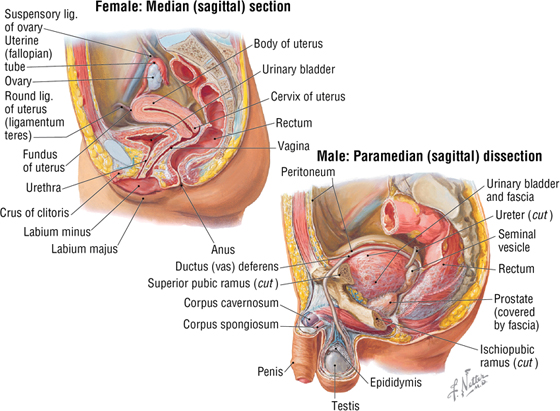
FIGURE 1-30 The Reproductive System
- Ovaries: the paired gonads of the female reproductive system; they produce the female germ cells called ova (oocytes, eggs) and secrete the hormones estrogen and progesterone
- Uterine tubes (fallopian tubes or oviducts): paired tubes that extend from the superolateral walls of the uterus and open as fimbriated funnels into the pelvic cavity adjacent to the ovary (to “capture” the oocyte as it is ovulated)
- Uterus: a pear-shaped, hollow muscular (smooth muscle) organ that protects and nourishes a developing fetus
- Vagina: a musculoelastic distensible tube (also referred to as the birth canal) approximately 8 to 9 cm long that extends from the uterine cervix (neck) to the vestibule
Male Reproductive System
The male reproductive system is composed of the following structures (see Fig. 1-30):
- Testes: the paired gonads of the male reproductive system; they are egg shaped and about the size of a chestnut, produce the male germ cells called spermatozoa, and reside in the scrotum (externalized from the abdominopelvic cavity)
- Epididymis: a convoluted tubule that receives the spermatozoa and stores them as they mature
- Ductus (vas) deferens: a muscular (smooth muscle) tube about 40 to 45 cm long that conveys sperm from the epididymis to the ejaculatory duct (seminal vesicle)
- Seminal vesicles: paired tubular glands that lie posterior to the prostate, are about 15 cm long, produce seminal fluid, and join the ductus deferens at the ejaculatory duct
- Prostate gland: a walnut-sized gland that surrounds the urethra as it leaves the urinary bladder and produces prostatic fluid, which is added to semen (sperm suspended in glandular secretions)
- Urethra: a canal that passes through the prostate gland, enters the penis, and conveys the semen for expulsion from the body during ejaculation
13. BODY CAVITIES
Organ systems and other visceral structures are often segregated into body cavities. These cavities can protect the viscera and also may allow for some expansion and contraction in size. Two major collections of body cavities are recognized (Fig. 1-31):
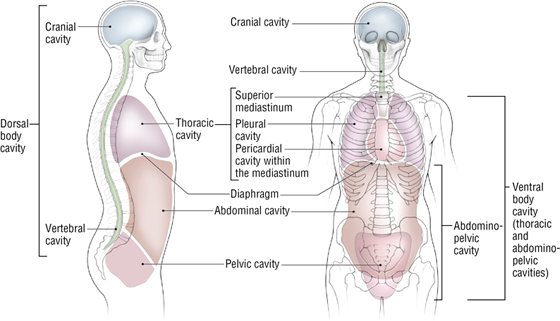
FIGURE 1-31 Major Body Cavities
- Dorsal cavities: include the brain, surrounded by the meninges and bony cranium, and the spinal cord, surrounded by the same meninges as the brain and the vertebral column
- Ventral cavities: include the thoracic and abdominopelvic cavities, separated by the abdominal diaphragm (skeletal muscle important in respiration)
The CNS (brain and spinal cord) is surrounded by three membranes (see Fig. 1-20):
- Pia mater
- Arachnoid mater
- Dura mater
The thoracic cavity contains two pleural cavities (right and left) and a single midline space called the mediastinum (middle septum) that contains the heart and structures lying posterior to it, including the thoracic descending aorta and esophagus. The heart itself resides in the pericardial sac, which has a parietal and visceral layer.
The abdominopelvic cavity also is lined by a serous membrane, called the peritoneum, which has a parietal and visceral layer.
C L I N I C A L F O C U S
Potential Spaces
Each of these spaces (pleural, pericardial, and peritoneal) is considered a “potential” space. This is because between the parietal and visceral layers, we usually find only a small amount of serous lubricating fluid (to keep organ surfaces moist and slick and hence reduce friction from movements such as respiration, heartbeat, or peristalsis); however, during inflammation or trauma (accumulation of pus or blood), fluids can collect in these spaces and restrict movement of the viscera. In this case, these “potential” spaces become real spaces and may necessitate removal of the offending fluid so as not to compromise organ function or exacerbate an ongoing infection.
14. OVERVIEW OF EARLY DEVELOPMENT
Week One of Development: Fertilization and Implantation
Fertilization normally occurs in the ampulla of the uterine tube (oviduct, fallopian tube) within 24 hours after ovulation (Fig. 1-32). The fertilized ovum (the union of sperm and egg nuclei, with a diploid number of chromosomes) is termed a zygote. Subsequent cell division (cleavage) occurs at the two-, four-, eight-, and 16-cell stages, and results in formation of a ball of cells that travels down the uterine tube toward the uterine cavity. When the cell mass reaches days three to four of development, it resembles a mulberry and is called a morula (16-cell stage). As the morula enters the uterine cavity at about day five, it develops a fluid-filled cyst in its interior and is then known as a blastocyst. At about days five to six, implantation occurs as the blastocyst literally erodes or burrows its way into the uterine wall (endometrium).
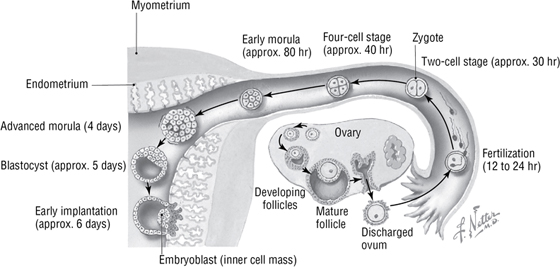
FIGURE 1-32 Schematic of Key Events of Week One of Human Development
Week Two of Development: Formation of the Bilaminar Embryonic Disc
As the blastocyst implants, it forms an inner cell mass (future embryo, embryoblast) and a larger fluid-filled cavity surrounded by an outer cell layer called the trophoblast (Fig. 1-33). The trophoblast undergoes differentiation and complex cellular interactions with maternal tissues to initiate formation of uteroplacental circulation. Simultaneously, the inner cell mass develops into two cell types (bilaminar disc):
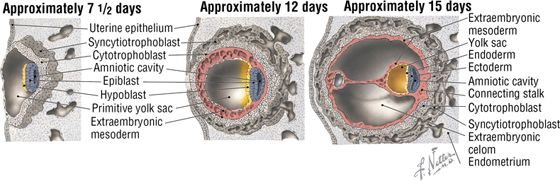
FIGURE 1-33 Bilaminar Disc Formation During Week Two of Human Development
- Epiblast: columnar cells on the dorsal surface of the embryoblast
- Hypoblast: cuboidal cells on the ventral surface of the embryoblast
The epiblast forms a cavity on the dorsal side that gives rise to the amniotic cavity; the blastocyst cavity on the ventral side becomes the primitive yolk sac, which is lined by simple squamous epithelium derived from the hypoblast. About day 12, further hypoblast cell migration forms the true yolk sac, and the old blastocyst cavity becomes coated with extraembryonic mesoderm.
Week Three of Development: Gastrulation
Gastrulation (development of the trilaminar embryonic disc) begins with appearance of the primitive streak on the dorsal surface of the epiblast (Fig. 1-34). This streak forms a groove demarcated at its cephalic end (head) by the primitive node. The node forms a midline cord of mesoderm that becomes the notochord. Migrating epiblast cells move toward the primitive streak, invaginate, and replace the underlying hypoblast cells to become the endoderm germ layer. Other invaginating epiblast cells develop between the endoderm and overlying epiblast and become the mesoderm. Finally, the surface epiblast cells form the ectoderm, the third germ layer. All body tissues are derived from one of these three embryonic germ layers.
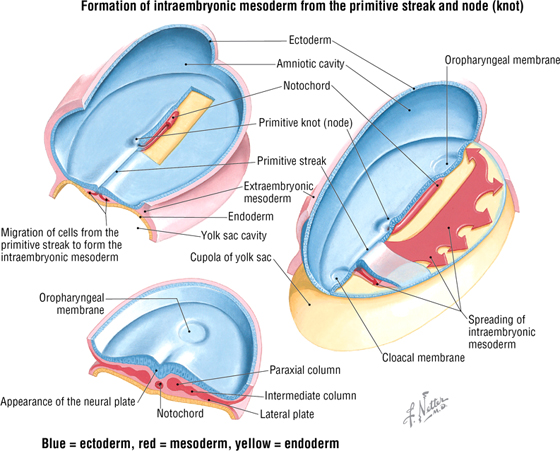
FIGURE 1-34 Gastrulation Formation During Week Three of Human Development
Overview of the Embryonic Germ Layer Derivatives
Figures 1-35 to 1-37 and the accompanying tables provide a general overview of the adult derivatives of the three embryonic germ layers that are formed during gastrulation. As you study each region of the body, refer to these summary pages to review the embryonic origins of the various tissues, as many clinical problems arise during the development in utero of these germ layer derivatives.
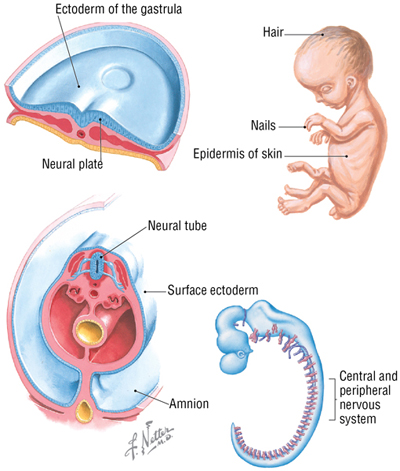
FIGURE 1-35 Ectodermal Derivatives (Contd.)
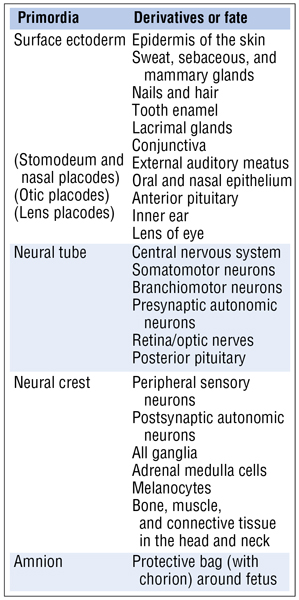
FIGURE 1-35 (Contd.) Ectodermal Derivatives
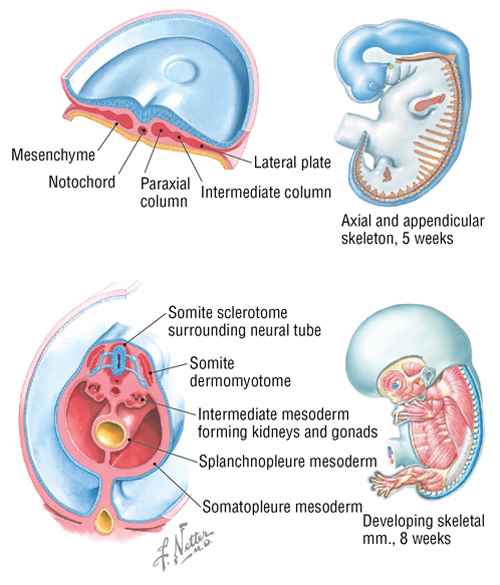
FIGURE 1-36 Mesodermal Derivatives (Contd.)
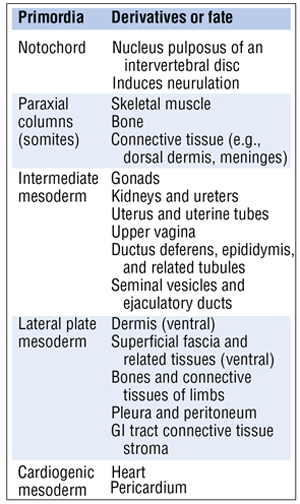
FIGURE 1-36 (Contd.) Mesodermal Derivatives
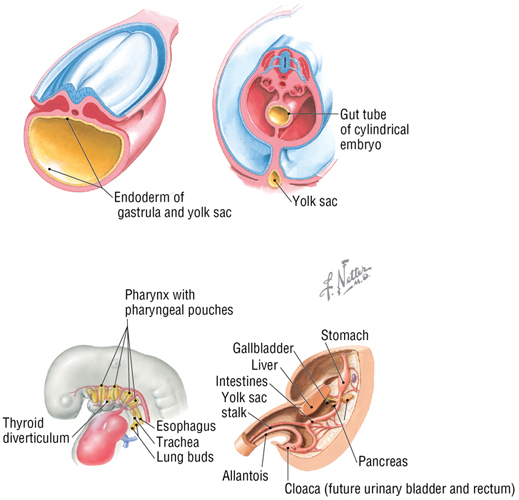
FIGURE 1-37 Endodermal Derivatives (Contd.)
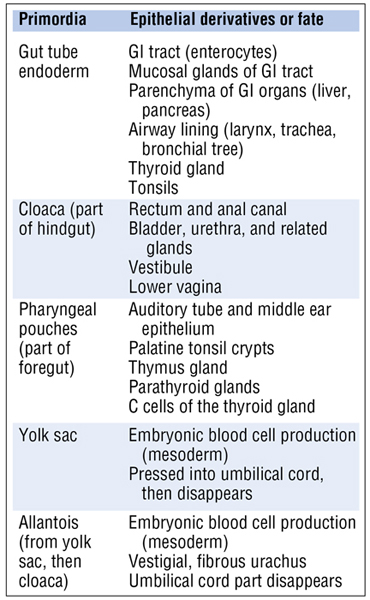
FIGURE 1-37 (Contd.) Endodermal Derivatives
In general, ectodermal derivatives include the following (Fig 1-35):
- Epidermis and various appendages associated with the skin (hair, nails, glands)
- Components of the central and peripheral nervous systems
- Some bones, muscle, and connective tissues of the head and neck (neural crest)
In general, mesodermal derivatives include the following (Fig. 1-36):
- Notochord
- Skeletal, smooth, and cardiac muscle
- Parenchyma or reticular structure and connective tissues of many organ systems
- Reproductive and urinary systems
- Most skeletal structures
- Dermis of the skin
In general, endodermal derivatives include the following (Fig. 1-37):
- Lining of the gastrointestinal tract and accessory GI organs
- Lining of the airway
- Various structures derived from the pharyngeal pouches
- Embryonic blood cells
- Derivatives associated with development of the cloaca
15. IMAGING THE INTERNAL ANATOMY
General Introduction
In 1895, Wilhelm Roentgen (Wurzberg, Germany) used X-rays generated from a cathode ray tube to make the first radiographic image, for which he ultimately was awarded the first Nobel Prize in Physics in 1901. As the X-rays (a form of electromagnetic radiation) pass through the body, they lose energy to the tissues, and only the photons with sufficient energy to make it through then expose a sheet of photographic film. It is now largely collected as digital information rather than as a photographic image on film (Table 1-6).
|
TABLE 1-6 Attenuation of X-rays Passing through the Body*
|
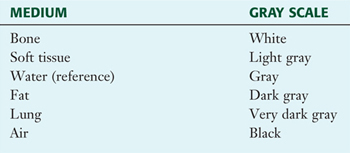 |
*Greatest to least attenuation.
Plain (Conventional) Radiographs
A plain radiograph, also known as conventional or plain film radiography, provides an image in which the patient is positioned either anterior (anteroposterior, or AP) to or posterior (posteroanterior, or PA) to the X-ray source (Fig. 1-38A). The X-ray tube also may be placed in a lateral or oblique position in reference to the patient. Contrast media (radiopaque fluids such as barium sulfate or iodine compounds) can be administered to study tubular structures such as the bowel or vessels. A double contrast study uses barium and air to image the lumen of structures such as the distal colon (Fig. 1-38B). X-rays now are collected digitally in real time by producing a stream of X-rays. Techniques are now available that can even image moving structures in the body using angiography (contrast medium in the heart and larger vessels) and fluoroscopy.
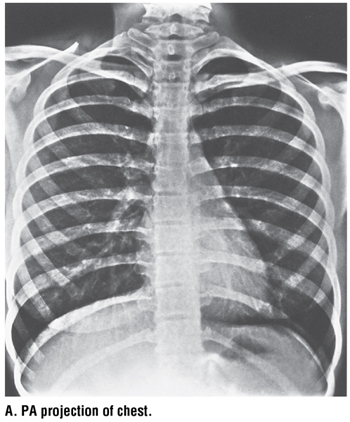
FIGURE 1-38 Plain (Conventional) Radiographs. (Reprinted with permission from A. Wicke L: Atlas of Radiologic Anatomy, 7th Edition. Philadelphia, Saunders, 2004, and B. Major NM: A Practical Approach to Radiology. Philadelphia, Saunders, 2006.) (Contd.)

FIGURE 1-38 (Contd.) Plain (Conventional) Radiographs. (Reprinted with permission from A. Wicke L: Atlas of Radiologic Anatomy, 7th Edition. Philadelphia, Saunders, 2004, and B. Major NM: A Practical Approach to Radiology. Philadelphia, Saunders, 2006.)
Computed Tomography (CT)
CT was invented in the 1972 by Sir Godfrey Hounsfield (at EMI Labs, Hayes, England), who received the Nobel Prize in Medicine or Physiology in 1979 (shared with Allen McLeod Cormack of Tufts). A CT scanner uses X-rays generated by a tube that passes around the body and collects a series of images in the axial (transverse slices) plane. A sophisticated computer program then transforms the multiple images into a single slice (Fig. 1-39A). In the 1980s, multislice (multidetector) CT scanners were developed that capture many slices as the tube rotates in a helical pattern around the patient, who is moving through the scanner on a table. Three-dimensional images can be recreated by the computer from these slices. Bone is well imaged by CT, and contrast media may be employed to enhance the imaging of hollow viscera such as the GI tract. Additionally, CT angiography (CTA) can image larger blood vessels in 2-D and 3-D following the intravascular administration of contrast material (Fig. 1-39B).
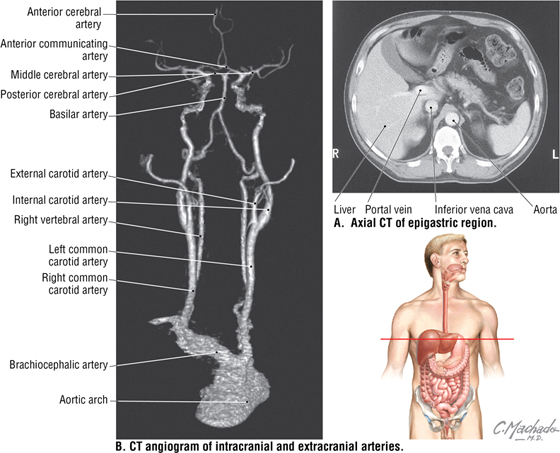
FIGURE 1-39 Computed Tomography (CT). (Reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Mosby, 2007.)
Advantages of CT include lower costs (compared to MRI), availability, 3-D capabilities, the ability to image bony features, and speed (compared to MRI). Disadvantages include its high dose of X-rays (compared to plain films), artifacts (motion and scattering), and relatively poor tissue definition compared to MRI.
Positron Emission Tomography (PET)/CT
Glucose uptake in tissues (following 18-fluorodeoxy-D-glucose administration) can be imaged by PET/CT, an especially useful technique for detecting tissues or structures with a higher metabolic rate, such as malignant tumors and inflammatory lesions.
Magnetic Resonance Imaging (MRI)
Paul Lauterbur (Illinois) and Sir Peter Mansfield (Nottingham, England) were awarded the Nobel Prize in Medicine or Physiology in 2003 for their contributions to the development of MRI. Since the first MRI of a human subject in 1977, this process has become a versatile and safe diagnostic tool. Strong magnets align hydrogen's free protons (the hydrogen in molecules of water present in almost all biological tissues). Then a radio wave pulse passes through the patient and deflects the protons, which return to their aligned state but emit small radio pulses whose strength, frequency, and time produce distinct signals. Computers then analyze these signals and create axial, coronal, and sagittal images (Fig. 1-40).
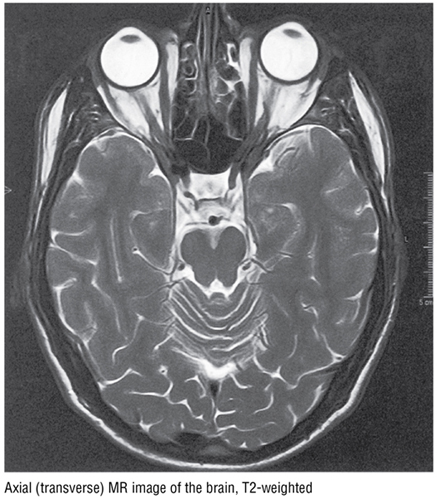
FIGURE 1-40 Magnetic Resonance Imaging (MRI). (Reprinted with permission from Wicke L: Atlas of Radiologic Anatomy, 7th Edition. Philadelphia, Saunders, 2004.)
Advantages of MRI include the lack of ionizing radiation, the ability to image all planes, and the capability to image soft tissues at very high resolution (compared to CT). Disadvantages include high cost; inability to image patients with metallic implants or foreign bodies; inability to image bone well; longer procedure time compared to CT; potential for patients to become claustrophobic in the scanner; and tendency for artifacts (movement).
C L I N I C A L F O C U S
Online Figures
Myasthenia gravis
Additional figures available online. See Table of Contents for Instructions for online access.

Ultrasound
Ultrasound uses very-high-frequency longitudinal sound waves that are generated by a transducer. The waves produced by the transducer are reflected or refracted as they collide with the soft tissue interfaces. The proportion of sound reflected is measured as acoustic impedance and represents different densities of the soft tissues. A computer then interprets these signals and produces a real-time image (Fig. 1-41).
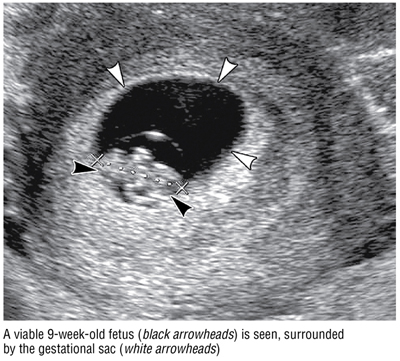
FIGURE 1-41 Ultrasound. (Reprinted with permission from Jackson S, Thomas R: Cross-Sectional Imaging Made Easy. Philadelphia, Churchill Livingstone, 2004.)