
BACK
1. INTRODUCTION
The back forms the axis (central line) of the human body and consists of the vertebral column, spinal cord, supporting muscles, and associated tissues (skin, connective tissues, vasculature, and nerves). A hallmark of human anatomy is the concept of “segmentation,” and the back is a prime example. Segmentation and bilateral symmetry of the back will be obvious as you study the vertebral column, the distribution of the spinal nerves, the muscles of the back, and its vascular supply.
Functionally, the back is involved in three primary tasks:
- Support: the vertebral column forms the axis of the body and is critical for our upright posture (standing or sitting), as a support for our head, as an attachment point and brace for movements of our upper limb, and as a support for transferring the weight of our trunk to the lower limbs
- Protection: the vertebral column protects the spinal cord and proximal portions of our spinal nerves before they distribute throughout the body
- Movements: muscles of the back function in movements of the head and upper limb and in support and movements of the vertebral column
2. SURFACE ANATOMY
Key Landmarks
Key surface landmarks are shown in Figure 2-1 and include the following bony landmarks:
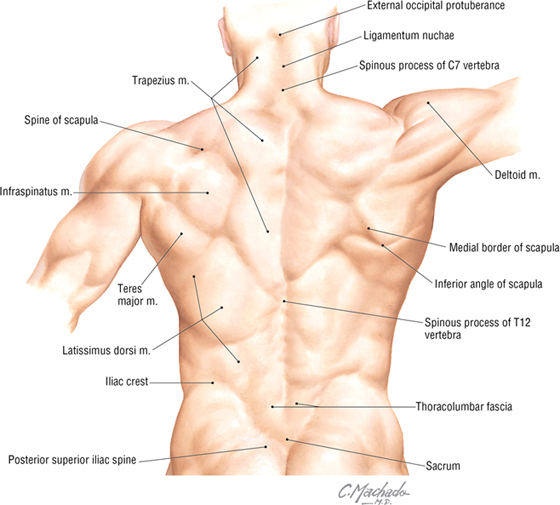
FIGURE 2-1 Key Bony and Muscular Landmarks of the Back
- Vertebrae prominens: the spinous process of the C7 vertebra, usually the most prominent process in the midline at the posterior base of the neck
- Scapula: part of the pectoral girdle that supports the upper limb; note its spine, inferior angle, and medial border
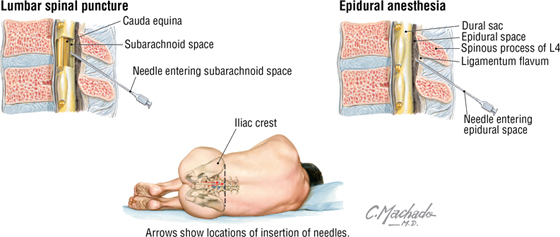
- Iliac crests: felt best when you place your hands “on your hips”; an imaginary horizontal line connecting the crests passes through the spinous process of the L4 vertebra and the intervertebral disc of L4-L5, a useful landmark for a lumbar puncture or epidural block
- Posterior superior iliac spines: an imaginary horizontal line connecting these two points passes through the spinous process of S2 (second sacral segment)
3. VERTEBRAL COLUMN
The vertebral column (spine) forms the central axis of the human body, highlighting the segmental nature of all vertebrates, and is composed of 33 vertebrae distributed as follows (Fig. 2-2):
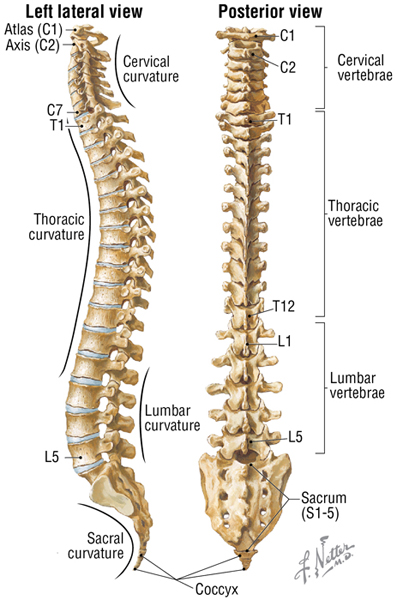
FIGURE 2-2 Vertebral Column (Contd.)
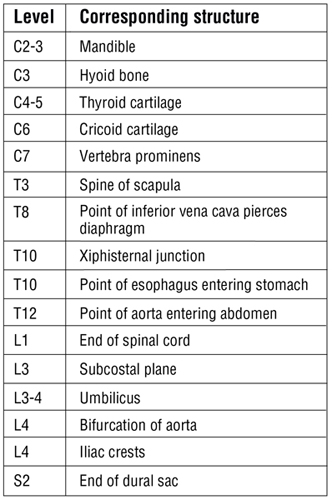
FIGURE 2-2 (Contd.) Vertebral Column
- Cervical: seven total; first two called the atlas (C1) and axis (C2)
- Thoracic: twelve total; each articulates with a pair of ribs
- Lumbar: five total; large vertebrae for support of the body's weight
- Sacrum: five fused vertebrae for stability in the transfer of weight from the trunk to the lower limbs
- Coccyx: four total; Co1 often is not fused, but Co2-Co4 are fused (a remnant of our embryonic tail)
Viewed from the lateral aspect (see Fig. 2-2), one can identify the following:
- Cervical curvature (cervical lordosis): this curvature is acquired secondarily when the infant can support the weight of its own head
- Thoracic curvature (thoracic kyphosis): a primary curvature present in the fetus (imagine the spine in the “fetal position”)
- Lumbar curvature (lumbar lordosis): this curvature is acquired secondarily when the infant assumes an upright posture and supports its weight
- Sacral curvature: a primary curvature present in the fetus
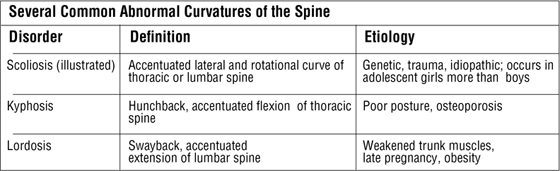
C L I N I C A L F O C U S
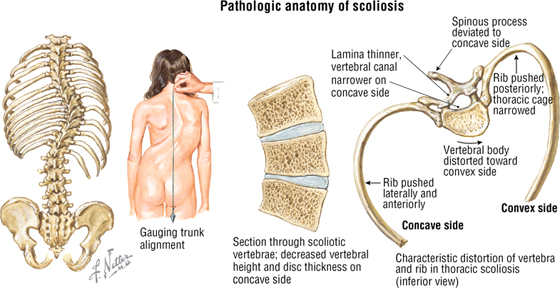
Scoliosis
Scoliosis is abnormal lateral curvature of the spine, which also includes an abnormal rotation of one vertebra upon the other. In addition to scoliosis, other accentuated curvatures of the spine include kyphosis (hunchback) and lordosis (swayback).
Typical Vertebra
A “typical” vertebra has several consistent features (Fig. 2-3):
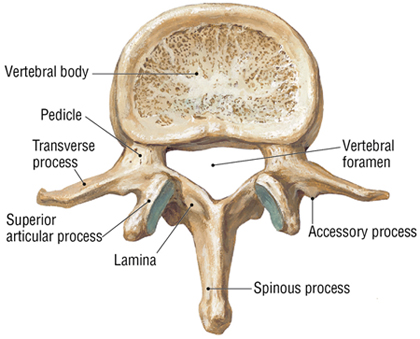
FIGURE 2-3 Features of a Typical Vertebra as Represented by the L2 Vertebra (Superior View) and by the Articulated Lumbar Vertebrae (Contd.)
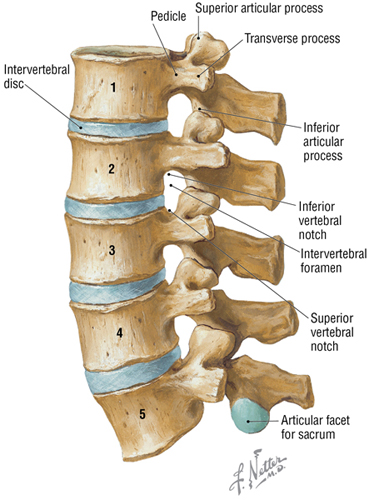
FIGURE 2-3 (Contd.) Features of a Typical Vertebra as Represented by the L2 Vertebra (Superior View) and by the Articulated Lumbar Vertebrae
- Body: the weight-bearing portion of a vertebra that tends to increase in size as one descends the spine
- Arch: a projection formed by paired pedicles and laminae
- Transverse processes: the lateral extensions from the union of the pedicle and lamina
- Articular processes (facets): two superior and two inferior facets for articulation with adjacent vertebrae
- Spinous process: a projection that extends posteriorly from the union of two laminae
- Vertebral notches: superior and inferior semicircular features that in articulated vertebrae form an intervertebral foramen (two semicircular notches form a circle)
- Intervertebral foramina: the opening formed by the vertebral notches that is traversed by spinal nerve roots and associated vessels
- Vertebral foramen (canal): a foramen formed from the vertebral arch and body that contains the spinal cord and its meningeal coverings
- Transverse foramina: apertures that exist in transverse processes of cervical vertebrae only and transmit the vertebral vessels
Regional Vertebrae
The Cervical Vertebrae
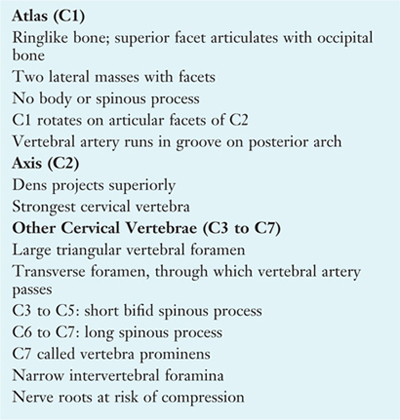
The cervical spine is composed of seven cervical vertebrae. The first two cervical vertebrae are unique and are termed the atlas (C1) and axis (C2) (Fig. 2-4). The atlas (C1) holds the head on the neck and gets its name from Atlas, the god of mythology who held the world on his shoulders. The axis (C2) is the point of articulation where the head turns on the neck, providing an “axis of rotation.” Key features of the cervical vertebrae are summarized in Table 2-1. The cervical region is a fairly mobile portion of the spine, allowing for flexion and extension as well as rotation and lateral bending.
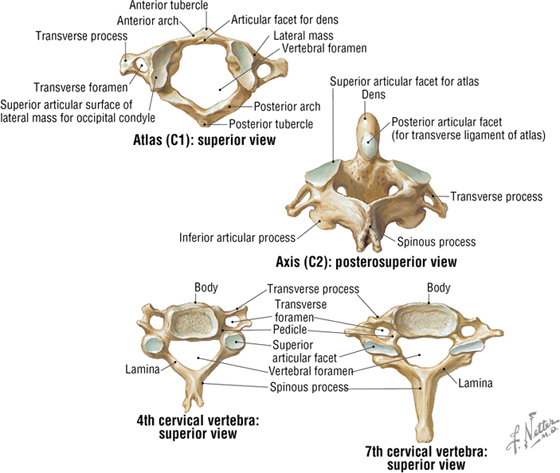
FIGURE 2-4 Representative Cervical Vertebrae
|
TABLE 2-1 Key Features of the Cervical Vertebrae
|
 |
The Thoracic and Lumbar Vertebrae
The thoracic spine is composed of 12 thoracic vertebrae (Fig. 2-5 and Table 2-2). The 12 pairs of ribs articulate with the thoracic vertebrae. This region of the spine is more rigid and inflexible than the cervical region.
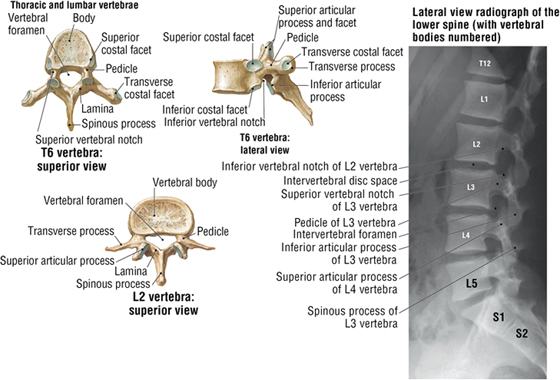
FIGURE 2-5 Representative Vertebrae (Contd.)
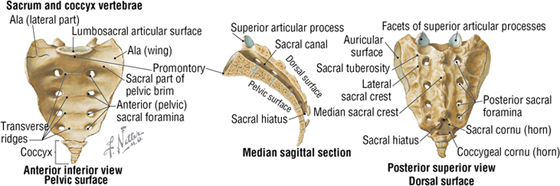
FIGURE 2-5 (Contd.) Representative Vertebrae
|
TABLE 2-2 Key Features of Vertebrae
|
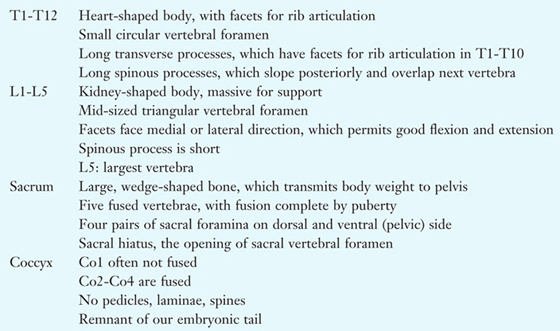 |
The lumbar spine is composed of five lumbar vertebrae (see Figs. 2-3 and 2-5, and Table 2-2). They are comparatively large for bearing the weight of the trunk and are fairly mobile, but not nearly as mobile as the cervical spine.
The Sacrum and Coccyx
The sacrum is composed of five fused vertebrae that form a single wedge-shaped bone (see Fig. 2-5 and Table 2-2). The sacrum provides support for the pelvis. The coccyx is a remnant of our embryonic tail and usually consists of four vertebrae, with the last three being fused into a single bone. The coccyx lacks vertebral arches and has no vertebral canal (see Fig. 2-5 and Table 2-2).
C L I N I C A L F O C U S
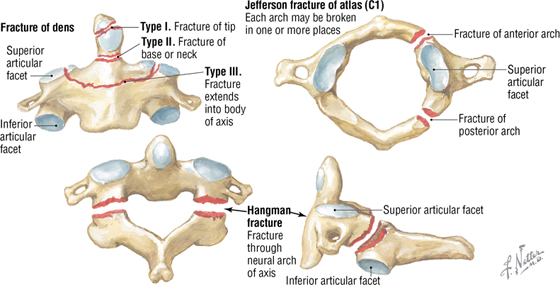
Cervical Fractures
Fractures of the axis (C2) often involve the dens and are classified as types I, II, and III. Type I fractures are usually stable, type II fractures are unstable, and type III fractures, which extend into the body, usually reunite well when immobilized. The “hangman” fracture, a pedicle fracture of the axis, can be stabilized, if survived, with or without spinal cord damage. A Jefferson fracture is a burst fracture of the atlas, often caused by a blow to the top of the head.
C L I N I C A L F O C U S
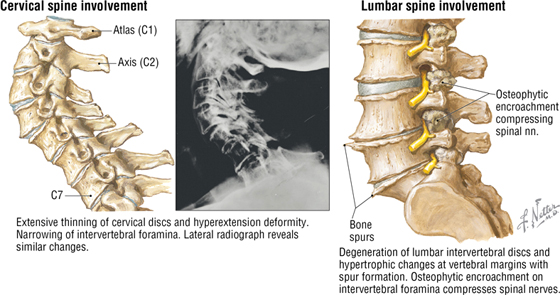
Osteoarthritis
Osteoarthritis is the most common form of arthritis and often involves erosion of the articular cartilage of weight-bearing joints, such as those of the vertebral column.
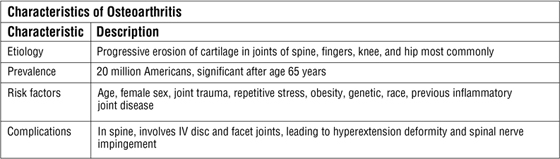
Joints and Ligaments of the Craniovertebral Spine
The craniovertebral joints include the atlanto-occipital (atlas and occipital bone of the skull) and atlantoaxial (atlas and axis) joints. Both are synovial joints that provide a relatively wide range of motion compared with other joints of the vertebral column. The atlanto-occipital joint permits one to nod the head up and down (flexion and extension), whereas the atlantoaxial joint is a pivot joint that permits one to rotate the head from side to side, as if to indicate “no.” The features of these joints and their ligaments are summarized in Figure 2-6 and Table 2-3.
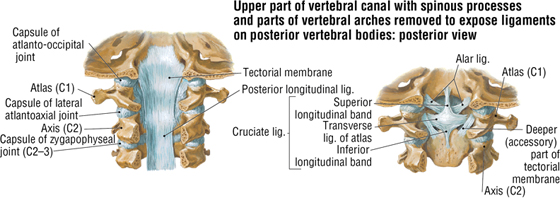
FIGURE 2-6 Craniovertebral Joints and Ligaments. (Radiograph reprinted with permission from Major N: A Practical Approach to Radiology. Philadelphia, Saunders, 2006.) (Contd.)
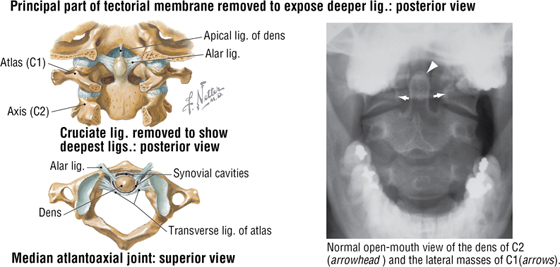
FIGURE 2-6 (Contd.) Craniovertebral Joints and Ligaments. (Radiograph reprinted with permission from Major N: A Practical Approach to Radiology. Philadelphia, Saunders, 2006.)
|
TABLE 2-3 Features of the Atlanto-occipital and Atlantoaxial Joints
|
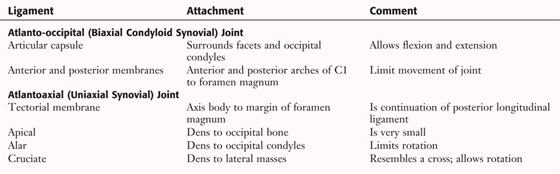 |
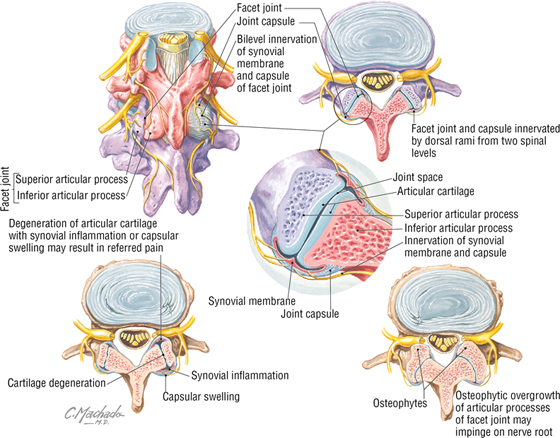
Joints and Ligaments of the Vertebral Arches and Bodies
The joints of the vertebral arches (zygapophyseal joints) occur between the superior and inferior articular processes (facets) of adjacent vertebrae and allow for some gliding or sliding movement (Fig. 2-7 and Table 2-4). The corresponding ligaments connect the spinous processes, laminae, and bodies of adjacent vertebrae.
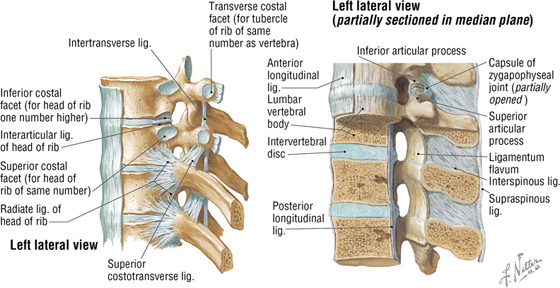
FIGURE 2-7 Joints of the Vertebral Arches and Bodies
|
TABLE 2-4 Features of the Zygapophyseal and Intervertebral Joints
|
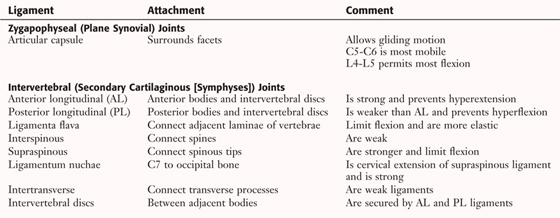 |
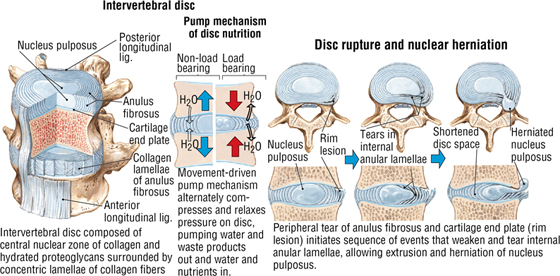
The joints of the vertebral bodies (intervertebral joints) occur between the adjacent vertebral bodies (see Fig. 2-7 and Table 2-4). These stable, weight-bearing joints also serve as shock absorbers owing to the presence of the intervertebral disc between the bodies. Intervertebral discs consist of the following:
- Outer fibrocartilaginous anulus fibrosus
- Inner gelatinous nucleus pulposus (a remnant of the embryonic notochord)
The lumbar intervertebral discs are the thickest, and the upper thoracic intervertebral discs are the thinnest. The anterior and posterior longitudinal ligaments help to stabilize these joints. Table 2-4 summarizes the features of these joints.
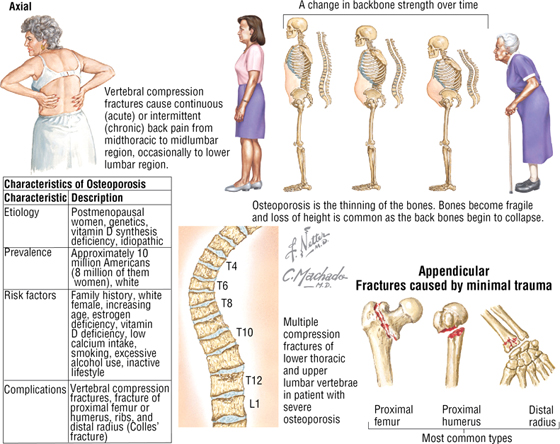
C L I N I C A L F O C U S
Osteoporosis
Osteoporosis (porous bone) is the most common bone disease and results from an imbalance in bone resorption and formation, which places bones at a great risk for fracture.
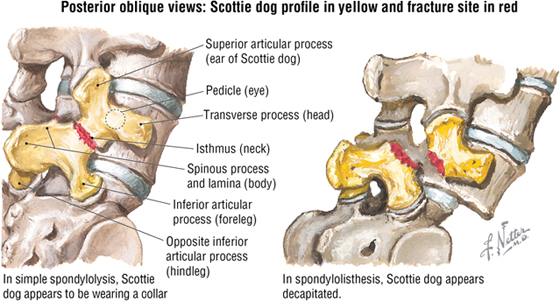
C L I N I C A L F O C U S
Spondylolysis and Spondylolisthesis
Various congenital and acquired conditions may affect the spine. Spondylolysis is a congenital defect or an acquired stress fracture of the lamina that presents with no slippage of adjacent articulating vertebrae (most common at the L5-S1 site). Its radiographic appearance is that of a “Scottie dog” with a collar (highlighted in yellow, with the fracture site indicated as the red collar). However, a bilateral defect (a complete dislocation, or luxation), called spondylolisthesis, results in an anterior displacement of the L5 body and transverse process while the posterior fragment (vertebral laminae and spinous process of L5) remains in proper alignment over the sacrum (S1). This defect has the radiographic appearance of a Scottie dog with a broken neck (highlighted in yellow, with the fracture in red). Pressure on spinal nerves often leads to low back and lower limb pain.
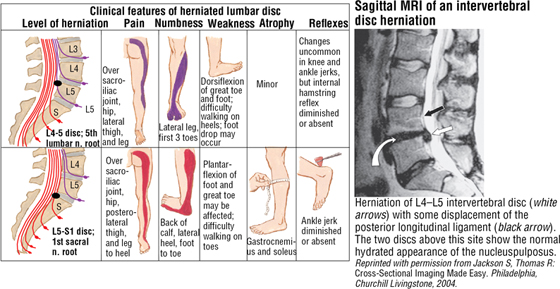
C L I N I C A L F O C U S
Low Back Pain
Low back pain, the most common musculoskeletal disorder, can have various causes. Physical examination, although not always revealing a definite cause, may provide clues to the level of spinal nerve involvement and relative sensitivity to pain. Those causes identified most often include:
- Intervertebral disc rupture and herniation
- Nerve inflammation or compression
- Degenerative changes in vertebral facet joints
- Sacroiliac joint and ligament involvement
- Metabolic bone disease
- Psychosocial factors
- Abdominal aneurysm
- Metastatic cancer
- Myofascial disorders
Additional figures available online. See Table of Contents for Instructions for online access.

C L I N I C A L F O C U S
Back Pain Associated with the Zygapophyseal (Facet) Joints
Although changes in the vertebral facet joints are not the most common cause of back pain (they account for approximately 15%), such alterations can lead to chronic pain. Although the articular surfaces of the synovial facet joints are not directly innervated, sensory nerve fibers, derived from the dorsal rami of spinal nerves, do supply the synovial linings of the capsules surrounding the joints. Two examples of painful conditions associated with facet joints include:
- Degeneration of the articular cartilage
- Osteophyte (bony outgrowth) overgrowth of the facet articular processes
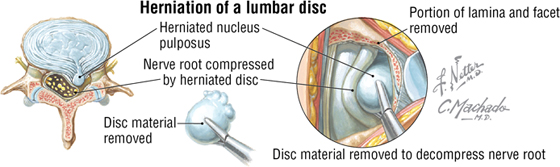
C L I N I C A L F O C U S
Intervertebral Disc Herniation
The intervertebral discs are composed of a central nuclear zone of collagen and hydrated proteoglycans called the nucleus pulposus, which is surrounded by concentric lamellae of collagen fibers that compose the anulus fibrosus. The nucleus pulposus is hydrated and acts as a “shock absorber,” compressing when load bearing and relaxing when the load is removed. Over time, the repeated compression-relaxation cycle can lead to peripheral tears of the anulus fibrosus that allow for the extrusion and herniation of the more gelatinous nucleus pulposus. Often this happens as one ages and the nucleus pulposus becomes more dehydrated, thus transferring more of the compression forces to the anulus fibrosus. This added stress may cause thickening of the anulus and tears. Most disc herniations occur in a posterolateral direction because the anulus fibrosus tears often occur at the posterolateral margins of the disc (rim lesions); moreover, the posterior longitudinal ligament reinforces the anulus such that posterior herniations are far less common. This is fortunate, because otherwise the disc would herniate into the vertebral canal and compress the spinal cord or its nerve roots.
The most common sites for disc herniation occur in the cervical region, primarily at the C5-C6 and C6-C7 levels, resulting in pain in the shoulder and upper limb or in the lumbar region, primarily at the L4-L5 and L5-S1 levels. Lumbar disc herniations are far more common than cervical herniations and result in pain over the sacroiliac joint, hip, posterior thigh, and leg.
Movements of the Spine
The essential movements of the spine are flexion, extension, lateral flexion (lateral bending), and rotation (Fig. 2-8). The greatest freedom of movement occurs in the cervical and lumbar spine, with the neck having the greatest range of motion. Flexion is greatest in the cervical region, and extension is greatest in the lumbar region. The thoracic region is relatively stable, as is the sacrum.
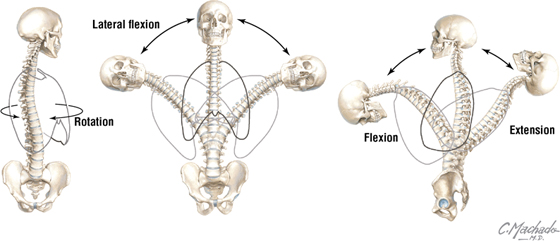
FIGURE 2-8 Movements of the Spine
The atlanto-occipital joint permits flexion and extension, as in nodding the head in acknowledgment. The atlantoaxial joint allows side-to-side movements (rotation), as in turning the head to indicate “no.” Alar ligaments limit side-to-side movement, so rotation of the atlantoaxial joint occurs with the skull and atlas rotating as a single unit, while the actual rotation occurs between the atlas and axis (see Fig. 2-6).
Movements of the spine are a function of the following features:
- Size and compressibility of the intervertebral discs
- Tightness of the joint capsules
- Orientation of the articular facets
- Muscle and ligament function
- Articulations with the thoracic cage
- Limitations imposed by the adjacent tissues and increasing age
Blood Supply to the Spine
The spine receives blood from spinal arteries derived from branches of larger arteries that serve each midline region of the body. These major arteries include the following:
- Vertebral arteries arising from the subclavian arteries in the neck
- Ascending cervical arteries arising from a branch of the subclavian arteries
- Posterior intercostal arteries arising from the thoracic aorta
- Lumbar arteries arising from the abdominal aorta
- Lateral sacral arteries arising from pelvic internal iliac arteries
Spinal arteries arise from these branches and divide into a posterior branch that supplies the vertebral arch and an anterior branch that supplies the vertebral body (Fig. 2-9). Also, longitudinal branches of radicular arteries, which arise from these spinal arteries, course along the inside aspect of the vertebral canal and supply the vertebral column.
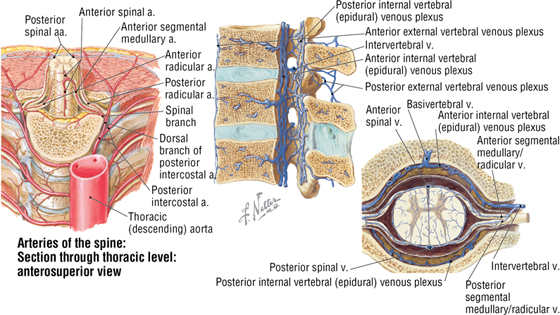
FIGURE 2-9 Arteries and Veins of the Spine
Radicular veins receive tributaries from the spinal cord and the internal vertebral veins that course within the vertebral canal; this internal venous plexus also anastomoses with a network of external vertebral veins (see Fig. 2-9). These radicular veins then drain into segmental and intervertebral veins, with the blood ultimately collecting in the segmental branches of the following:
- Superior vena cava, which drains the cervical region
- Azygos venous system, which drains the thoracic region
- Inferior vena cava, which drains the lumbar and sacral regions
C L I N I C A L F O C U S
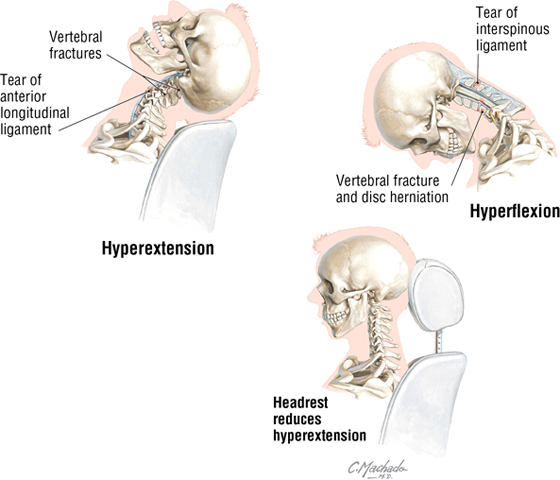
Whiplash Injury
Whiplash is a non-medical term for a cervical hyperextension injury, which is usually associated with a rear-end vehicular accident. The relaxed neck is thrown backward, or hyperextended, as the vehicle accelerates rapidly forward. Rapid recoil of the neck into extreme flexion occurs next. Properly adjusted headrests can significantly reduce the occurrence of this hyperextension injury, which often results in stretched or torn cervical muscles and, in severe cases, ligament, bone, and nerve damage.
4. MUSCLES OF THE BACK
Although the spine is the axis of the human body and courses down the body's midline, dividing it into approximately equal right and left halves, it is not midway between the anterior and posterior halves of the body. In fact, most of the body's weight lies anterior to the more posteriorly aligned vertebral column. Consequently, to support the body and spine, most of the muscles associated with the spine attach to its lateral and posterior processes, assisting the spine in maintaining an upright posture that offsets the uneven weight distribution.
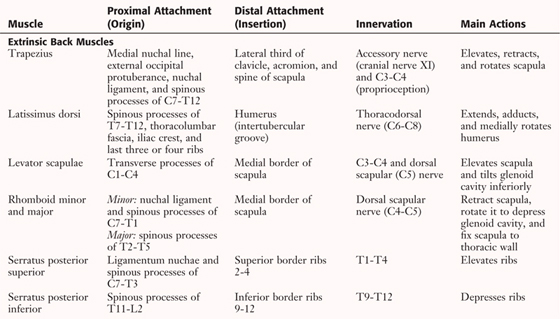
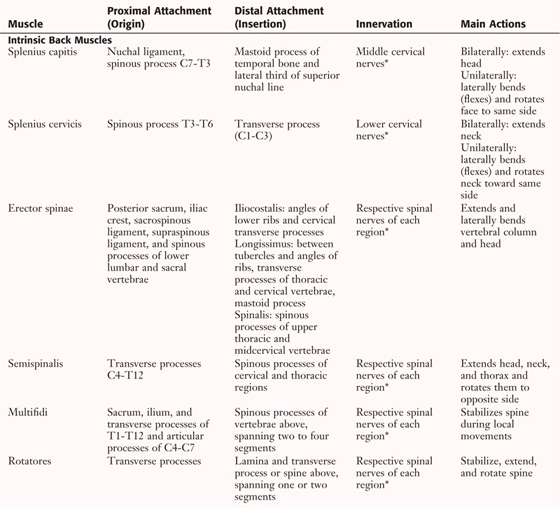
The muscles of the back are divided into two major groups:
- Extrinsic back muscles are concerned with movements of the upper limb and with respiration
- Intrinsic back muscles are concerned with movements of the spine and the maintenance of posture
Extrinsic Back Muscles
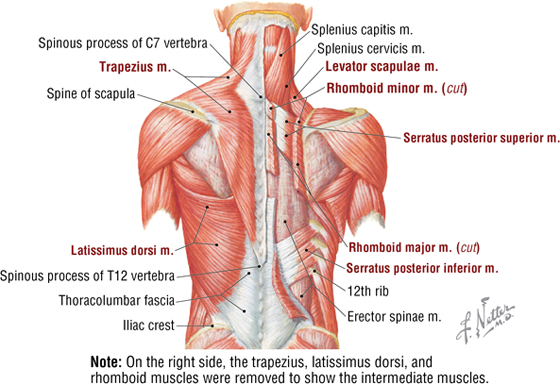
FIGURE 2-10 Extrinsic Back Muscles
|
TABLE 2-5 Muscles of the Back (Contd.)
|
 |
|
TABLE 2-5 (Contd.) Muscles of the Back
|
 |
*Dorsal rami of spinal nerves.
- Superficial muscles are concerned with movements of the upper limb (trapezius, latissimus dorsi, levator scapulae, and the two rhomboids)
- Intermediate muscles are thin accessory muscles of respiration that assist with movements of the rib cage (serratus posterior superior and inferior muscles)
Intrinsic Back Muscles
The intrinsic back muscles are the “true” muscles of the back in that they function in movements of the spine and help maintain posture. These muscles are enclosed within a deep fascial layer that extends in the midline from the medial crest of the sacrum to the nuchal ligament and skull, and spreads laterally to the transverse processes and angles of the ribs. In the thoracic and lumbar regions, the deep fascia makes up a very distinct sheath known as the thoracolumbar fascia (Fig. 2-11). The intrinsic back muscles also are included among the group of a few muscles of the body that are innervated by dorsal primary rami of a spinal nerve. From superficial to deep, they include the following three layers (see Fig. 2-11 and Table 2-5):
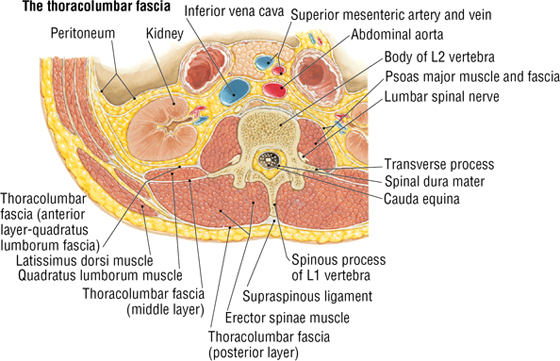
FIGURE 2-11 Intrinsic Back Muscles (Contd.)
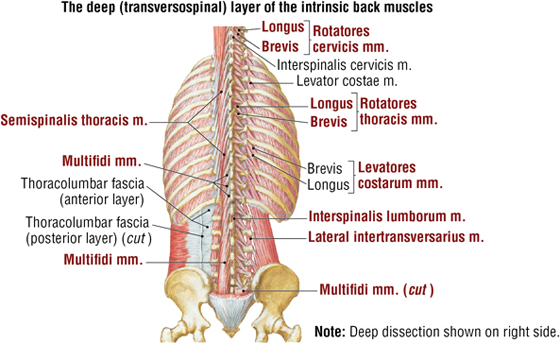
FIGURE 2-11 Intrinsic Back Muscles (Contd.)
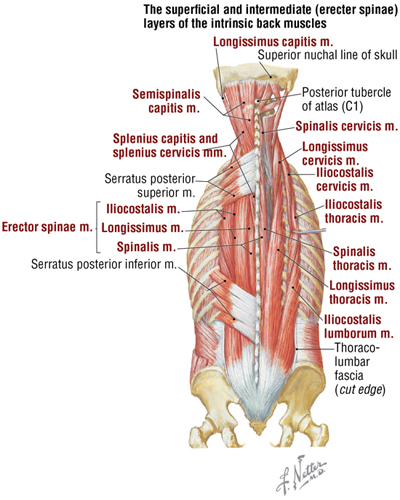
FIGURE 2-11 (Contd.) Intrinsic Back Muscles
- Superficial layer includes the splenius muscles that occupy the lateral and posterior neck
- Intermediate layer includes the erector spinae muscles that largely extend the spine
- Deep layer includes the transversospinalis muscles that fill the spaces between the transverse processes and spinous processes
The intermediate, or erector spinae, layer of muscles is the largest group of the intrinsic back muscles and is very important for maintaining posture and extending the spine. These muscles are divided into three major groups (see Fig. 2-11):
- Iliocostalis, found most laterally and associated with attachments to the ribs and cervical transverse processes
- Longissimus, the intermediate and largest column of the erector spinae muscles
- Spinalis, found most medially and the smallest of the groups with attachments to the vertebral spinous processes
Moreover, these three groups are further subdivided into regional divisions (lumborum, thoracis, cervicis, and capitis) based on their attachments as one proceeds superiorly (see Fig. 2-11).
The transversospinalis muscles are often simply referred to by clinicians as the “paraver-tebral” muscles because they form a solid mass of muscle tissue interposed and running obliquely between the transverse and spinous processes (see Fig. 2-11). They comprise three groups of muscle:
- Semispinalis group is the most superficial and is found in the thoracic and cervical regions
- Multifidus group is found deep to the semispinalis and in all spinal regions, but is most prominent in the lumbar region
- Rotatores group is the deepest group and is present in all spinal regions, but is most prominent in the thoracic region
Deep to the transversospinalis muscles lies a relatively small set of segmental muscles that assist in elevating the ribs (levatores costarum) and stabilizing adjacent vertebrae while larger muscle groups act on the spine (interspinales and intertransversarii) (see Fig. 2-11).
Suboccipital Muscles
In the back of the neck–deep to the trapezius, splenius, and semispinalis muscles—lay several small muscles that move the head and are attached to the skull, the atlas, and the axis (Fig. 2-12 and Table 2-6). These muscles compose the suboccipital muscles, which are innervated by the suboccipital nerve (dorsal ramus of C1), and form a (suboccipital) triangle demarcated by the following:
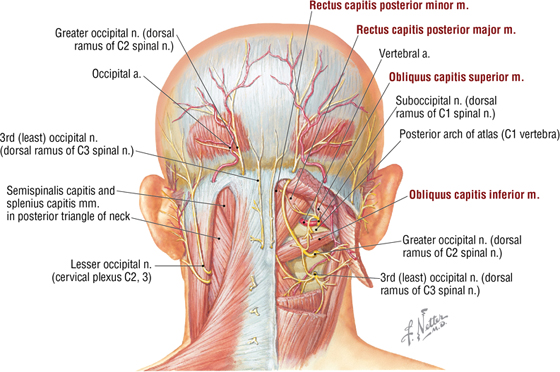
FIGURE 2-12 Suboccipital Triangle and Its Muscles
|
TABLE 2-6 Suboccipital Muscles
|
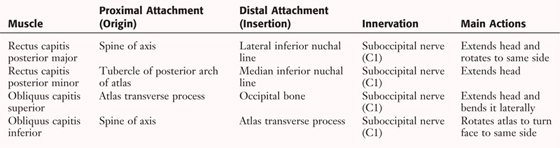 |
- Rectus capitis posterior major muscle
- Obliquus capitis superior muscle (superior oblique muscle of head)
- Obliquus capitis inferior muscle (inferior oblique muscle of head)
Deep within the suboccipital triangle, the vertebral artery (a branch of the subclavian artery in the lower anterior neck) passes through the transverse foramen of the atlas and loops medially to enter the foramen magnum of the skull to supply the brainstem. The first three pairs of spinal nerves are also found in this region (see Fig. 2-12).
5. SPINAL CORD
The spinal cord is a direct continuation of the medulla oblongata, extending below the foramen magnum at the base of the skull and passing through the vertebral (spinal) canal formed by the articulated vertebrae (Fig. 2-13).
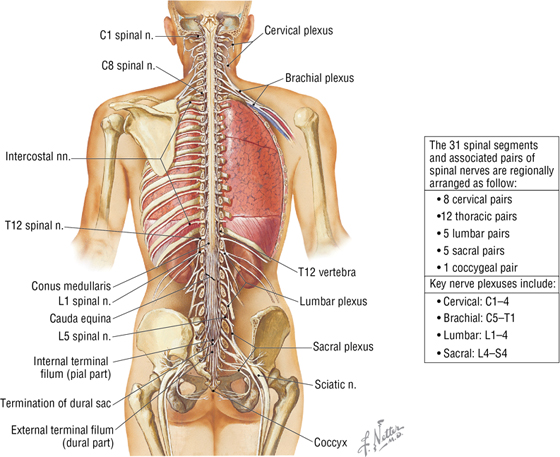
FIGURE 2-13 The Spinal Cord and Nerves In Situ
The spinal cord has a slightly larger diameter in the cervical and lumbar regions, owing in large measure to the increased presence of neurons and axons in these regions related to the innervation of the large number of muscles in the upper and lower limbs. The spinal cord ends as a tapered region called the conus medullaris, which is situated at about the level of the L1-L2 vertebrae. From this point inferiorly, the nerve rootlets course to their respective levels and form a bundle called the cauda equina (“horse's tail”). The spinal cord is anchored inferiorly by the terminal filum, which is attached to the coccyx. Features of the spinal cord include the following:
- 31 pairs of spinal nerves (8 cervical pairs, 12 thoracic pairs, 5 lumbar pairs, 5 sacral pairs, and 1 coccygeal pair)
- Each spinal nerve is formed by a dorsal and ventral root
- Motor neurons reside in the spinal cord gray matter (anterior horn)
- Sensory neurons reside in the spinal dorsal root ganglia
- Ventral rami of spinal nerves often converge to form plexuses (a mixed network of nerve axons)
Typical Spinal Nerve
The typical scheme for a somatic (which innervates skin and skeletal muscle) peripheral nerve shows a motor neuron in the spinal cord anterior horn (gray matter) sending a myelinated axon through a ventral root and into a peripheral nerve, which ends at a neuromuscular junction on a skeletal muscle (Fig. 2-14). Likewise, a nerve ending in the skin sends a sensory axon toward the spinal cord in a peripheral nerve. (Sensory axons also arise from the muscle spindles and joints and are similarly conveyed back to the spinal cord.) Thus, each peripheral nerve contains hundreds or thousands of motor and sensory axons. The sensory neuron is a pseudounipolar neuron that resides in a dorsal root ganglion (a ganglion in the periphery is a collection of neurons, just as a “nucleus” is in the brain) and that sends its central axon into the posterior horn (gray matter) of the spinal cord. At each level of the spinal cord, the gray matter is visible as a butterfly-shaped central collection of neurons, exhibiting a posterior and an anterior horn (see Fig. 2-14).
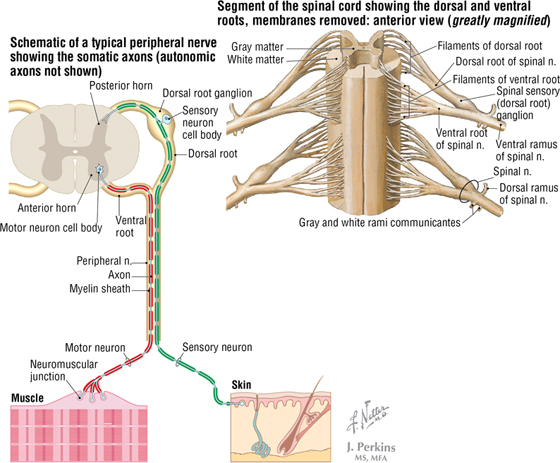
FIGURE 2-14 Typical Spinal Nerve
The spinal cord gives rise to 31 pairs of spinal nerves, which then form two major branches (rami):
- Dorsal primary ramus: a small ramus that courses dorsally to the back conveys motor and sensory information to and from the skin and intrinsic back skeletal muscles (erector spinae and transversospinalis muscles)
- Ventral primary ramus: a much larger ramus that courses laterally and ventrally and innervates all the remaining skin and skeletal muscles of the neck, limbs, and trunk
Once nerve fibers (sensory or motor) are beyond, or peripheral to, the spinal cord proper, the fibers then reside in nerves of the peripheral nervous system (PNS). Components of the PNS include the following (for an overview, see “The Nervous System” in Chapter 1):
- Somatic nervous system: sensory and motor fibers to skin, skeletal muscle, and joints (illustrated on the left side of Figure 2-15)
- Autonomic nervous system (ANS): sensory and motor fibers to all smooth muscle (including viscera and vasculature), cardiac muscle (heart), and glands (illustrated on the right side of Figure 2-15)
- Enteric nervous system: plexuses and ganglia of the gastrointestinal tract that regulate bowel secretion, absorption, and motility (originally, considered part of the ANS); linked to the ANS for optimal regulation (see Fig. 1-26)
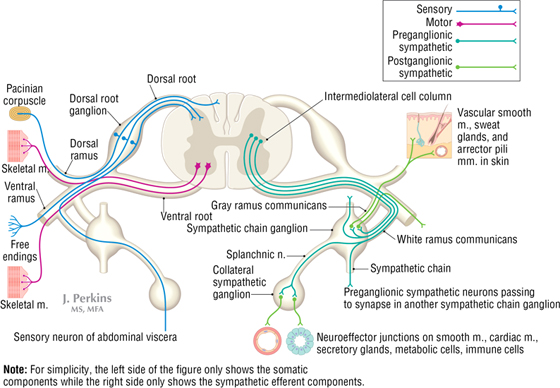
FIGURE 2-15 Schematic of the Components of a Thoracic Spinal Nerve
Thus, each peripheral nerve arising from the spinal cord contains hundreds or thousands of three types of axons (see the combined left and right sides of Fig. 2-15):
- Somatic efferent (motor) axons to skeletal muscle
- Afferent (sensory) axons from the skin, skeletal muscle, and joints or viscera
- Postganglionic sympathetic efferent axons to smooth muscle (vascular smooth muscle and arrector pili muscles in the skin) and glands (sweat and sebaceous skin glands)
Each of the 31 pairs of spinal nerves exits the spinal cord and passes through an opening in the vertebral column to gain access to the periphery. The C1 nerve pair passes between the skull and the atlas (Fig. 2-16), with subsequent cervical nerve pairs exiting the intervertebral foramen above the vertebra of the same number (e.g., C2 nerve exits via the intervertebral foramen superior to the C2 vertebra, and so on, until one gets to the C8 nerve, which then exits the intervertebral foramen above the T1 vertebra). All of the remaining thoracic, lumbar, and sacral nerves exit via the intervertebral foramen below the vertebra of the same number (see Fig. 2-16).
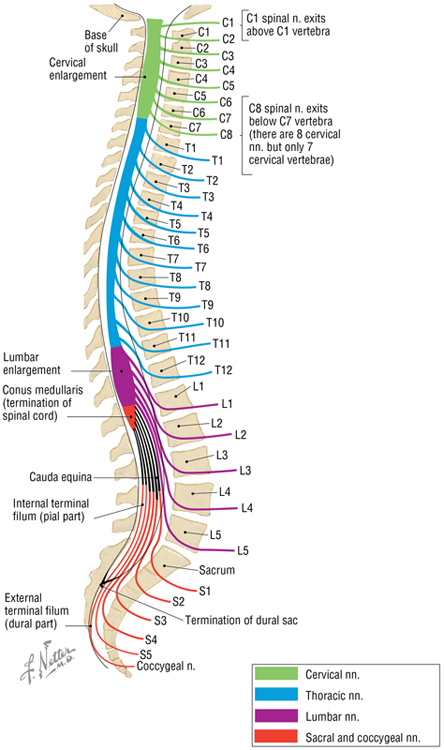
FIGURE 2-16 The Relationship of Spinal Nerves to Vertebrae
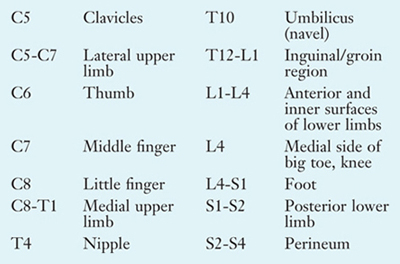
Dermatomes
The region of skin innervated by the somatic sensory nerve axons associated with a single dorsal root ganglion at a single spinal cord level is called a dermatome. Likewise, over the anterolateral head, the skin is innervated by one of the three divisions of the trigeminal cranial nerve, which we will discuss later. The neurons that give rise to these sensory fibers are pseudounipolar neurons that reside in the single dorsal root ganglion associated with the specific spinal cord level. (Note that for each level we are speaking of a pair of nerves, roots, and ganglia, as there are 31 pairs of spinal nerves, one pair for each spinal cord level.) C1, the first cervical spinal cord level, does possess sensory fibers, but they provide little, if any, contribution to the skin, so at the top of the head the dermatome pattern begins with the C2 dermatome (Fig. 2-17).
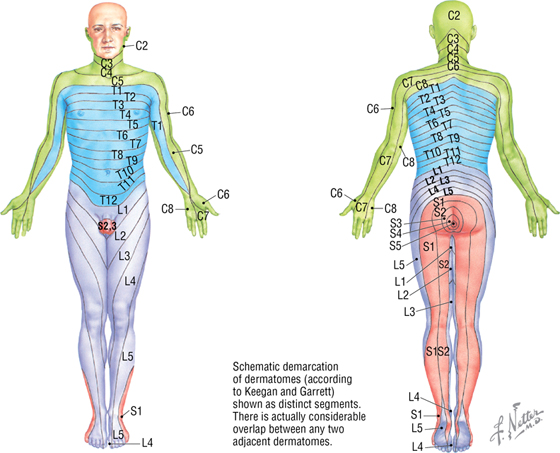
FIGURE 2-17 The Distribution of Dermatomes
The dermatomes encircle the body in a segmental fashion corresponding to the spinal cord level that receives sensory input from that segment of skin. The sensation conveyed by touching the skin is largely that of pressure and pain. Knowledge of the dermatome pattern is useful in localizing specific spinal cord segments and in assessing the integrity of the spinal cord at that level (intact or lesioned).
The sensory nerve fibers that innervate a segment of skin and constitute the “dermatome” exhibit some overlap of nerve fibers. Consequently, a segment of skin is innervated primarily by fibers from a single spinal cord level, but there will be some overlap with sensory fibers from the level above and below the primary cord level. For example, dermatome T5 will have some overlap with sensory fibers associated with the T4 and T6 levels. Thus, dermatomes give pretty good approximations of cord levels, but variation is common and overlap exists.
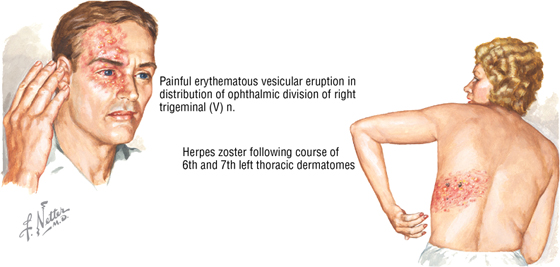
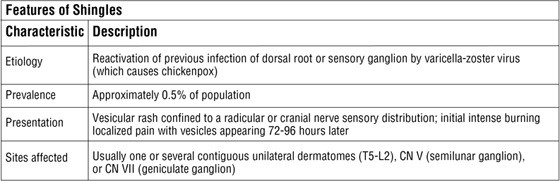
C L I N I C A L F O C U S
Herpes Zoster
Herpes zoster, or shingles, is the most common infection of the peripheral nervous system. It is an acute neuralgia confined to the dermatome distribution of a specific spinal or cranial sensory nerve root.
Spinal Meninges
The brain and spinal cord are covered by three membranes called the meninges and are bathed in cerebrospinal fluid (CSF) (Fig. 2-18). The three meningeal layers include the following:
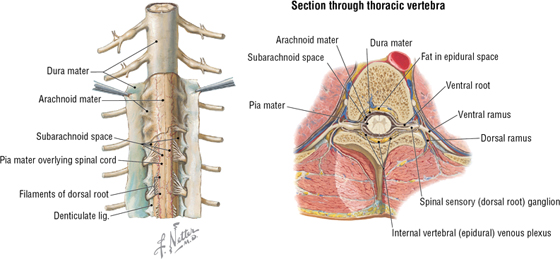
FIGURE 2-18 The Spinal Meninges and Their Relationship to the Spinal Cord
- Dura mater: a thick outer covering that is richly innervated by sensory nerve endings. The epidural (extradural) space lies between the vertebral canal walls and the spinal dural sac and contains fat and blood vessels.
- Arachnoid mater: a fine, weblike membrane that is avascular and lies directly beneath the dura mater. Wispy threads of connective tissue extend from this layer to the underlying pia and span the subarachnoid space, which is filled with CSF.
- Pia mater: a delicate, transparent inner layer that intimately covers the spinal cord. At the cervical and thoracic levels, extensions of pia form approximately 21 pairs of triangular denticulate (“having small teeth”) ligaments that extend laterally and help to anchor the cord to the dural sac. At the conus medullaris, the pia forms a single cord of tissue called the terminal filum, which pierces the dural sac at the S2 vertebral level, acquires a dural covering, and then attaches to the coccyx to anchor the spinal cord inferiorly.
CSF fills the subarachnoid space, which lies between the arachnoid and pia meningeal layers (Figs. 2-18 and 2-19). Thus, CSF circulates through the brain ventricles and then gains access to the subarachnoid space via the lateral and median apertures, where it flows around and over the brain and spinal cord to the most caudal extent of the dural sac at the S2 vertebral level.
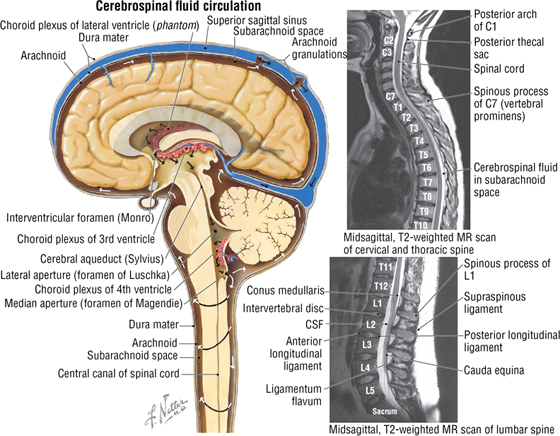
FIGURE 2-19 Cerebrospinal Fluid Circulation. (MRs reprinted with permission from Kelley LL, Petersen C: Sectional Anatomy for Imaging Professionals. Philadelphia, Mosby, 2007.)
While CSF is secreted by the choroid plexus, most of it is absorbed by the arachnoid granulations associated with the superior sagittal dural venous sinus and, to a lesser degree, by small veins on the surface of the pia mater throughout the CNS (see Fig. 2-19). About 500 mL of CSF is produced daily and does the following:
- Supports and cushions the spinal cord
- Fulfills some of the functions normally provided by the lymphatic system
- Fills the 150-mL volume of the subarachnoid space
C L I N I C A L F O C U S
A Lumbar Puncture and Epidural Anesthesia
Cerebrospinal fluid may be sampled and examined clinically by performing a lumbar puncture (spinal tap). A spinal needle is inserted into the subarachnoid space of the lumbar cistern, in the midline between the L3 and L4 or the L4 and L5 vertebral spinal processes. Because the spinal cord ends at approximately the L1 or L2 vertebral level, the needle will not pierce and damage the cord. Additionally, anesthetic agents may be administered into the epidural space (above the dura mater) to directly anesthetize the nerve fibers of the cauda equina; this is a common form of anesthesia used during childbirth in Western countries. The epidural anesthetic infiltrates the dural sac to reach the nerve roots and is usually administered at the same levels as the lumbar puncture.
Blood Supply to Spinal Cord
The spinal cord receives blood from spinal arteries derived from branches of larger arteries that serve each midline region of the body (Fig. 2-20). These major arteries include the following:
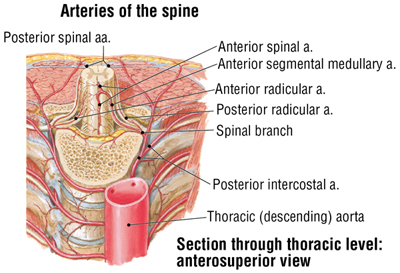
FIGURE 2-20 Blood Supply to the Spinal Cord (Contd.)
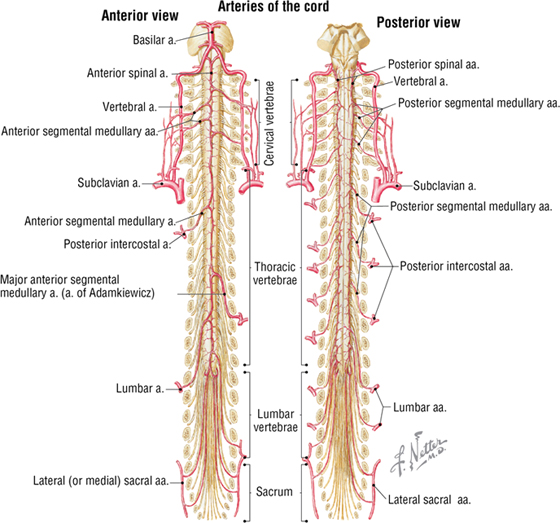
FIGURE 2-20 (Contd.) Blood Supply to the Spinal Cord
- Vertebral arteries arising from the subclavian arteries in the neck
- Ascending cervical arteries arising from a branch of the subclavian arteries
- Posterior intercostal arteries arising from the thoracic aorta
- Lumbar arteries arising from the abdominal aorta
- Lateral sacral arteries arising from pelvic internal iliac arteries
A single anterior spinal artery and two posterior spinal arteries, originating intracranially from the vertebral arteries, run longitudinally along the length of the cord and are joined segmentally in each region by segmental arteries (see Fig. 2-20). The largest of these segmental branches is the major segmental artery (of Adamkiewicz), found in the lower thoracic or upper lumbar region; it is the major blood supply for the lower two-thirds of the spinal cord. The dorsal and ventral roots are supplied by segmental radicular (medullary) arteries.
Multiple anterior and posterior spinal veins run the length of the cord and drain into segmental (medullary) radicular veins (see Fig. 2-9). Radicular veins receive tributaries from the internal vertebral veins that course within the vertebral canal. Radicular veins then drain into segmental veins, with the blood ultimately collecting in the following places:
- Superior vena cava
- Azygos venous system of the thorax
- Inferior vena cava
6. EMBRYOLOGY
Most of the bones inferior to the skull form by endochondral bone formation (see Chapter 1), that is, from a cartilaginous precursor that becomes ossified. The embryonic development of the musculoskeletal components of the back represents a classic example of segmentation, with each segment corresponding to the distribution of peripheral nerves. This process begins around the end of the third week of embryonic development (day 19), during the period called gastrulation, as discussed in Chapter 1.
The Development of Myotomes, Dermatomes, and Sclerotomes
The bones, muscles, and connective tissues of the embryo arise from several sources:
- Primitive streak mesoderm (somites)
- Lateral plate mesoderm
- Diffuse collections of mesenchyme
As the neural groove invaginates along the posterior midline of the embryonic disc, it is flanked on either side by masses of mesoderm called somites. About 42 to 44 pairs of somites develop along this central axis and subsequently develop into the following (Fig. 2-21):
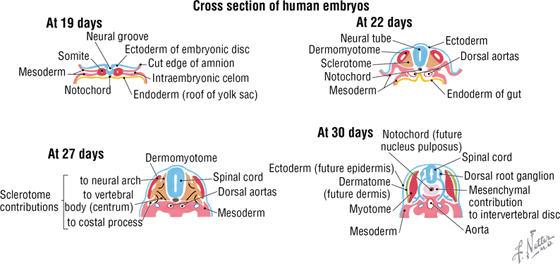
FIGURE 2-21 Somite Formation and Differentiation
- Dermomyotomes: divide further to form dermatomes (which become the dermis of the skin) and myotomes (which differentiate into segmental masses of skeletal muscle)
- Sclerotomes: medial part of each somite that along with the notochord migrates around the neural tube and forms the cartilaginous precursors of the axial skeleton
The myotomes, like the somites from which they are derived, have a segmental distribution (Fig. 2-22). Each segment is innervated by a pair of nerves originating from the spinal cord segment. A small dorsal portion of the myotome becomes an epimere (epaxial) mass of skeletal muscle that will form the true, intrinsic muscles of the back (e.g., the erector spinae) and are innervated by a dorsal primary ramus of the spinal nerve.
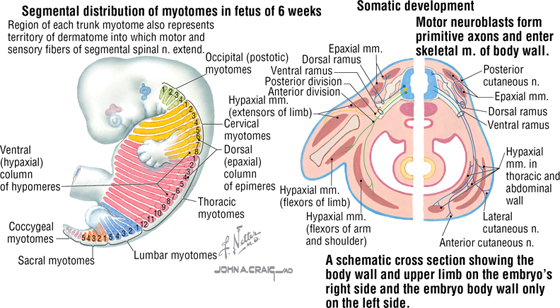
FIGURE 2-22 Myotome Segmentation into Epimeres and Hypomeres
A much larger ventral segment becomes the hypomere (hypaxial) mass of skeletal muscle, which will form the muscles of the trunk wall and limb muscles, all innervated by a ventral primary ramus of the spinal nerve. Adjacent myotome segments often merge so that an individual skeletal muscle derived from those myotomes is innervated by more than one spinal cord segment. For example, the latissimus dorsi muscle is innervated by the thoracodorsal nerve, which is composed of nerves from spinal cord segments C6-C8.
Vertebral Column Development
Each vertebra first appears as a hyaline cartilage model that then ossifies, beginning in a primary ossification center (Fig. 2-23). Ossification centers include the following:
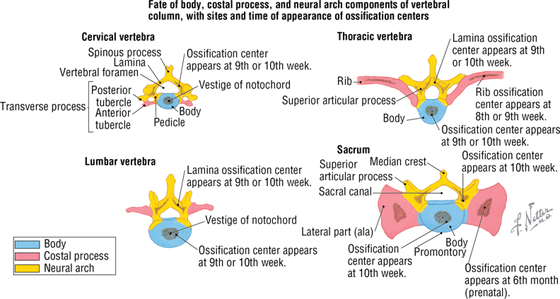
FIGURE 2-23 Ossification of the Vertebral Column
- Body: forms the vertebral body; important for support of body weight
- Costal process: forms the ribs, or in vertebrae without rib articulation, part of the transverse process; important for movement and muscle attachment
- Neural arch: includes the pedicle and lamina for protection of the spinal cord, and the spinous process for movement and muscle attachment
The body of the vertebra does not develop from a single sclerotome but rather from the fusion of two adjacent sclerotomes (fusion of the caudal half of the sclerotome above with the cranial half of the sclerotome below). The intervertebral foramen thus lies over this fusion and provides the opening for the exiting of a spinal nerve that will innervate the myotome at that particular segment.
The notochord initially is in the central portion of each vertebral body but disappears, and only persists as the central portion (nucleus pulposus) of each intervertebral disc that forms from fibrocartilage.
Neurulation and Development of the Spinal Cord
Neurulation (neural tube formation) begins concurrently with gastrulation (formation of the trilaminar embryonic disc during the third week of development). As the primitive streak recedes caudally, the midline surface ectoderm thickens to form the neural plate, which then invaginates to form the neural groove (Fig. 2-24A). The neural crest forms at the dorsal aspect of the neural groove (see Fig. 2-24B) and fuses in the midline as the groove sinks below the surface and pinches off to form the neural tube (see Fig. 2-24C). The neural tube forms the following:
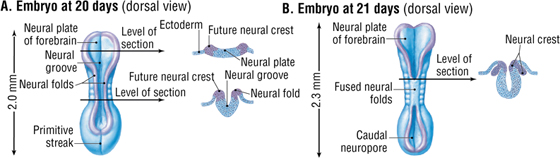
FIGURE 2-24 Neurulation (Contd.)
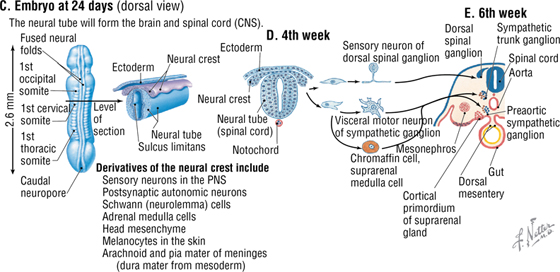
FIGURE 2-24 (Contd.) Neurulation
- Neurons of the CNS (brain and spinal cord)
- Supporting cells of the CNS
- Somatomotor neurons (innervate skeletal muscle) of the PNS
- Presynaptic autonomic neurons of the PNS
The neural crest gives rise to the following (Fig. 2-24D and E):
- Sensory neurons of the PNS
- Postsynaptic autonomic neurons
- Schwann cells of the PNS
- Adrenal medullary cells
- Head mesenchyme
- Melanocytes in the skin
- Arachnoid and pia mater meninges (the dura is from mesoderm)
The cells in the walls of the neural tube compose the neuroepithelium, which develops into three zones:
- Ependymal: the inner layer lining the central canal of the spinal cord (also lines the ventricles of the brain)
- Mantle: the intermediate layer that develops into the gray matter of the spinal cord
- Marginal: the outer layer that becomes the white matter of the spinal cord
Glial cells are found in the mantle and marginal zones. The neural tube is distinguished by a longitudinal groove on each side that forms the sulcus limitans and divides the tube into a dorsal alar plate and a ventral basal plate (Fig. 2-25). The dorsal alar plate forms the sensory derivatives of the spinal cord, and the ventral basal plate gives rise to the somatic and autonomic motor neurons, whose axons will leave the spinal cord and pass into the peripheral tissues. The sensory neurons of the dorsal root ganglia are formed from neural crest cells.
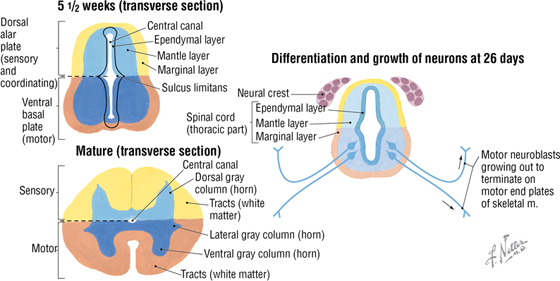
FIGURE 2-25 Alar and Basal Plates of the Spinal Cord
C L I N I C A L F O C U S
Spina Bifida
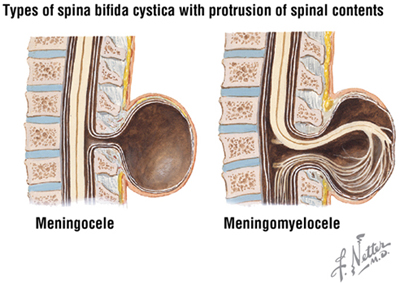
Spina bifida, one of several neural tube defects, is linked to low folic acid ingestion during the first trimester of pregnancy. Spina bifida is a congenital defect in which the neural tube remains too close to the surface such that the sclerotome cells do not migrate over the tube and form the neural arch of the vertebra (spina bifida occulta). This defect occurs most often at the L5 or S1 vertebral level and may present with neurologic findings. If the meninges and CSF protrude as a cyst (meningocele) or if the meninges and the cord itself reside in the cyst (meningomyelocele), significant neurologic problems often develop.

C L I N I C A L F O C U S
Online Figures
Myofascial pain
Acute spinal syndromes
Additional figures available online. See Table of Contents for Instructions for online access.
